Abstract
Objective/Hypothesis
Review the published literature of telemedicine's use within otorhinolaryngology (ORL), highlight its successful implementation, and document areas with need of future research.
Study Design
State of the Art Review.
Methods
Three independent, comprehensive searches for articles published on the subject of telemedicine in ORL were conducted of literature available from January 2000 to April 2020. Search terms were designed to identify studies which examined telemedicine use within ORL. Consensus among authors was used to include all relevant articles.
Results
While several, small reports document clinical outcomes, patient satisfaction, and the cost of telemedicine, much of the literature on telemedicine in ORL is comprised of preliminary, proof‐of‐concept reports. Further research will be necessary to establish its strengths and limitations.
Conclusions
Particularly during the coronavirus disease of 2019 pandemic, telemedicine can, and should, be used within ORL practice. This review can assist in guiding providers in implementing telemedicine that has been demonstrated to be successful, and direct future research. Laryngoscope, 131:744–759, 2021
Keywords: coronavirus disease of 2019, telehealth, telemedicine, review, otorhinolaryngology
INTRODUCTION
Telemedicine has enabled providers to care for patients in increasingly efficient, effective, and cost‐saving manners. 1 , 2 Many specialties have taken advantage of these technologies, primarily in triaging new patients and for follow‐up of postoperative patients. 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 While the utilization of telemedicine has gradually increased over the past decades in the United States, 11 the 2019 novel coronavirus (coronavirus disease of 2019 [COVID‐19]) pandemic has thrust both its necessity and implementation into the forefront of medical practice. Similar to other medical fields, otorhinolaryngology (ORL) is experiencing challenges in attempting to maximize continued quality patient care, while minimizing risk to patients and providers. 12 , 13
ORL presents unique barriers to telemedicine implementation due to pervasive necessity of in‐person examination techniques and procedures. 14 The objective of this review is to document the manners in which telemedicine has already been implemented across the various subspecialties of ORL as a guide for current practitioners, highlight limitations of telemedicine, and elucidate areas in need of further study.
MATERIALS AND METHODS
Three independent searches of Scopus, PubMed, Google Scholar, and Google for articles published on the subject of telemedicine in ORL were conducted from January 2000 to April 2020 (Fig. 1). Search terms were designed to identify studies which examined telemedicine use within ORL (Appendix S1). A total of 219 unique articles were found. Articles were sorted according to the following categories: head and neck oncology, otology/neurotology, laryngology, rhinology, facial plastic and reconstructive surgery, and pediatrics, and selected based on relevance. Case reports, and articles with a focus outside ORL were excluded. A qualitative literature review was summarized (Table I). Implications for practice and potential opportunities for additional investigation were discussed and established among all authors.
Fig 1.
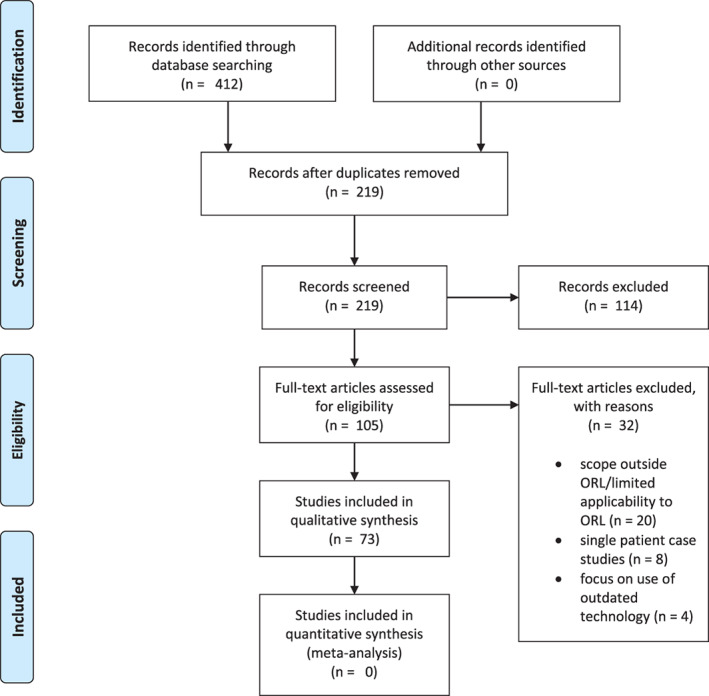
Inclusion and exclusion criteria flow diagram [Color figure can be viewed in the online issue, which is available at www.laryngoscope.com.]
Table I.
Summary of Telemedicine Best Practices by Sub‐Specialty.
| Discipline | Scope of telemedicine use | Benefits | Limitations | Recommendations for practice | Areas for future research |
|---|---|---|---|---|---|
| H&N Oncology |
|
|
|
|
|
| Otology/Neurotology |
|
|
|
|
|
| Laryngology |
|
|
|
|
|
| Rhinology |
|
|
|
|
|
| Facial Plastics and Reconstructive Surgery |
|
|
|
|
|
| Pediatric ORL |
|
|
|
|
|
RESULTS
Head and Neck Oncology
Findings
Compared to the other ORL subspecialties, head and neck surgical oncology has demonstrated relatively wide adoption of telemedicine (Table II). A study conducted by Dorrian et al. concluded that initial assessment by telemedicine lowered equipment costs for providers, travel costs for patients, and unnecessary transfers to specialist centers, without compromising diagnostic accuracy or patient satisfaction. 17 Within the Veterans Affairs (VA) system, Beswick et al. demonstrated the safe use of a telemedicine protocol for preoperative visits in patients with high‐grade head and neck malignancies. 18 Kohlert et al. found that head and neck surgical oncology cases accounted for 48.6% of all ORL consults to a regional electronic consulting service. 19
Table II.
Summary of Articles in Qualitative Review for Head and Neck Oncology.
| Author (year) | Discipline | Level of evidence | Country of origin | Study design and methods | Number of participants/sample size | Outcome measured | Key findings | Common themes |
|---|---|---|---|---|---|---|---|---|
| Alemi (2017) | Head and Neck Oncology | 3 | United States | Observational two‐site study with retrospective review | 60 | Total time spent performing flap assessment, travel time, ratings of perceived quality of flap assessment by house staff | House staff unanimously reported that the remote methodology reduced the total time spent on the assessments as well as travel time, without compromising the perceived quality of the flap assessment | Communication between clinicians; Equivalency of diagnosis or outcomes |
| Beswick (2016) | Head and Neck Oncology | 3 | United States | Retrospective chart review and feasibility study | 15 | Time from referral to initial consultation and surgery, travel costs and time, carbon dioxide emissions | Reduced time to surgery for patients with high grade malignancies; reduced patient travel times and costs | Patient satisfaction |
| Dorrian (2009) | Head and Neck Oncology | 4 | United Kingdom | Case series, and feasibility study with cost analysis | 42 | Travel costs and time, carbon dioxide emissions | Preliminary cost analysis showed tele‐ENT became cheaper than travel at a threshold of 35 patients/year | Feasibility; Decreased costs |
| Hwang (2012) | Head and Neck Oncology | 3 | South Korea | Retrospective chart review with matched controls | 123 | Patient demographics, operative details, flap complications, overall survival | Sharing of digital photographs of flaps between providers facilitated better communication within the care team with earlier detection of flap compromise and ultimately increased overall flap survival | Communication between clinicians; Improved patient outcomes |
| Kohlert (2017) | Head and Neck Oncology | 2 | United States | Prospective regional observational study | 109 | Response time, time of consult, number of referrals, perceived value of service by PCPs | Head and neck oncology cases accounted for 48.6% of all ORL consults to a regional electronic consulting service, with the most frequent pathologies assessed being oral/mucosal lesions and thyroid nodules or goiters | Applicability of telemedicine |
| Lopez (2009) | Head and Neck Oncology | 4 | United States | Prospective single‐institution quality assurance study | 154 | Diagnostic concurrence, physician satisfaction ratings | Virtual slide telepathology resulted in complete concurrence with the primary diagnosis in 139 (90.3%) of cases | Applicability of telemedicine; Equivalency of diagnosis or outcomes |
| Rimmer (2018) | Head and Neck Oncology | 3 | United States | Retrospective chart review | 250 | Patient demographics, visit type, wait time, travel distance, travel time, patient survey responses | The majority of visits were postoperative encounters. 95% of patients reported they were satisfied with their visit. Commute times decreased by an estimated 78 minutes | Improved access to care; Patient satisfaction |
| Weinstein (2007) | Head and Neck Oncology | 4 | United States | Retrospective case series and feasibility study | 171 | Physician satisfaction ratings, patient satisfaction ratings | Use of telepathology and teleradiology has facilitated virtual tumor boards | Applicability of telemedicine; Communication between clinicians; Patient satisfaction |
Head and neck cancer care plans are often developed in a multi‐disciplinary tumor board that includes otolaryngologists, pathologists, radiologists, medical and radiation oncologists. Several studies note that a combination of real‐time videoconferencing, and safely shared laboratory, imaging, and pathology data facilitate tumor board workflow, streamlining cooperation between colleagues. 20 , 21 , 22
Lastly, telemedicine has proven effective in easing provider demands in the postoperative setting. Rimmer et al. reported that, in appropriately selected patients, telemedicine postoperative visits were safe, time‐saving, and satisfactory to patients. 21 Recent studies on remote free flap monitoring provide clear examples of how telemedicine can not only expedite care, but also improve patient outcomes. 23 Similarly, Hwang and Mun found that sharing of digital photographs of flaps between providers facilitated better communication within the care team, earlier detection of flap compromise, and ultimately increased overall flap survival. 24
Recommendations for practice
We strongly recommend that telemedicine be utilized to expedite workup of new tumors, especially when there is concern for high‐grade/aggressive pathology. This can be accomplished through streamlining referral systems, obtaining imaging based on electronic consultation, and hosting multi‐disciplinary discussions on audio/visual platforms. Furthermore, we recommend that telemedicine be strongly considered in postoperative head and neck surgery visits when feasible. Successful use of remote free flap monitoring suggests there is also a role for inpatient head and neck telemedicine implementation (Table I). There is a further need for controlled studies comparing telemedicine to in‐person assessment of head and neck cancer patients in terms of cost, safety, surveillance adherence, and oncologic outcomes.
Otology and Neurotology
Findings
The field of otology/neurotology demonstrated early adaptation of telemedicine, driven by a high patient volume and lack of specialist centers, particularly in rural settings. Advances in recorded otoscopy have bolstered promise in remote evaluation, but given the degree of specialized training and equipment required, concerns exist regarding the accuracy and safety of these technologies (Table III).
Table III.
Summary of Articles in Qualitative Review for Otology/Neurotology.
| Author (year) | Discipline | Level of evidence | Country of origin | Study design and methods | Number of participants/sample size | Outcome measured | Key findings | Common themes |
|---|---|---|---|---|---|---|---|---|
| Arriaga (2010) | Otology/Neurotology | 4 | United States | Retrospective case series and feasibility study | 450 | Breakdown of procedures and diagnoses performed, patient satisfaction ratings | A telemedicine‐assisted neurotology clinic was successfully implemented in post‐Hurricane Katrina Louisiana. Patient satisfaction was equivalent between on‐site and telemedicine evaluations | Improved access to care; Feasibility; Patient satisfaction |
| Biagio (2014) | Otology/Neurotology | 4 | South Africa | Prospective case series | 140 | Patient demographics, independent ratings of video‐otoscopy quality, patient outcomes | Substantial agreement between diagnoses made from video‐otoscopy recordings and those from onsite evaluations. Quality of the video‐otoscopy recordings rated as acceptable or better in 87% of cases. | Improved access to care; Equivalency of diagnosis or outcomes; Importance of image or video quality |
| Bush (2016) | Otology/Neurotology | 2 | United States | Systematic review | 12 | Type of service offered, assessment of electrode‐specific measures and speech recognition, remote gain assessments, patient satisfaction ratings | Auditory rehabilitation services with hearing aids and cochlear implants may be offered via telemedicine. A significant concern is internet bandwidth limitations of remote clinics | Applicability of telemedicine |
| Erkkola‐Anttinen (2018) | Otology/Neurotology | 1 | Finland | Prospective, randomized control trial | 699 | Diagnostic quality of tympanic membrane measured with a structured video analysis independently by three physicians, parent's experience questionnaire, comparing teaching schedules for smartphone otoscopy performed by parents | After instruction, parents were able to perform smartphone otoscopy, however videos of sufficient technical quality for diagnosis were only obtained in 67% of cases | Equivalency or diagnosis or outcomes; Importance of image or video quality |
| Fletcher (2019) | Otology/Neurotology | 2 | United States | Prospective comparative within‐subject control study. | 13 | Routine audiometry, word recognition testing, AzBio and CNC testing | Cochlear implant evaluation testing results were comparable across remote and in‐person conditions | Equivalency of diagnosis or outcomes |
| Gupta (2017) | Otology/Neurotology | 4 | India | Case series, feasibility study | 3000 | Practice patterns, type of service offered, practice costs | Remote screening of otologic pathologies by trained technicians with a telemedicine device is feasible and cost‐effective in a rural area | Feasibility |
| Henry (2017) | Otology/Neurotology | 1 | United States | Prospective randomized control trial | 300 | Tinnitus Functional Index scores, to measure effectiveness of coping skills education provided with progressive tinnitus management | The group which underwent a telephone‐based skills education program showed far greater improvement in symptoms management than the in‐person wait‐list group | Patient satisfaction; Applicability of telemedicine |
| Hofstetter (2010) | Otology/Neurotology | 3 | United States | 16‐year retrospective analysis | 3000 | Time in months to obtain in‐person appointment after initial consultation, before and after implementation of telemedicine | Average wait time for an in‐person appointment dropped dramatically after store‐and‐forward telemedicine was incorporated into practice | Patient satisfaction |
| Kokesh (2008) | Otology/Neurotology | 4 | United States | Case series, prospective study | 70 | Intraprovider comparative concordance ratings, interprovider diagnostic concordance | Video‐otoscopy images of the tympanic membrane are comparable to an in‐person examination for assessment and treatment of patients following tympanostomy tubes. | Equivalency of diagnosis or outcomes |
| Kokesh (2009) | Otology/Neurotology | 3 | United States | Retrospective chart review | 1458 | Number and type of encounters, referrals patterns, travel costs | Travel costs and burdens to the patient were significantly reduced in a store‐and‐forward model where an audiologist communicates with an otolaryngologist | Feasibility; Decreased costs |
| Kokesh (2010) | Otology/Neurotology | 3 | United States | Case series with retrospective chart review | 90 | Recommended surgery from telemedicine and in‐person evaluation, estimated operative time | SAF telemedicine is as effective as in‐person evaluation for planning elective ear surgery | Equivalency of diagnosis or outcomes |
| Kokesh (2011) | Otology/Neurotology | 2 | United States | Retrospective observational study | 9559 | Technical requirements, clinical outcomes, patient costs and travel times | Similar clinical outcomes, and improved patient wait times and travel costs compared to in‐person specialty visits, for store‐and‐forward electronic consultations made to the Alaska Federal Health Care Access Network (AFHCAN) | Equivalency of diagnosis or outcomes; Patient satisfaction; Improved access to care. |
| Krumm (2011) | Otology/Neurotology | 5 | United States | Expert opinion and literature review | NA | Applications of teleaudiology as demonstrated in the literature | In otology, telehealth has historically been applied to tinnitus rehabilitation, and treatments involving cochlear implants and hearing aids | Applicability of telemedicine; Feasibility |
| Lundberg (2014) | Otology/Neurotology | 2 | South Africa, Sweden | Prospective observational study with matched controls | 180 | Concordance between onsite otomicroscopy and asynchronous assessments of video‐otoscopy recordings, calculated with intra‐ and inter‐rater agreements | The OMGRADE scale (image‐based grading scale for otitis media) accurately assesses for otitis media using video‐otoscopy recordings | Feasibility; Equivalency of diagnosis or outcomes |
| Luryi (2019) | Otology/Neurotology | 3 | United States | Retrospective single‐site study | 20 | AzBio scores, impedances, comfort and threshold levels, survey responses. | Threshold, comfort, and impedance levels not significantly different between telehealth and live sessions; high degree of patient satisfaction | Communication between clinicians; Equivalency of diagnosis or outcomes; Importance of image or video quality; Patient satisfaction |
| Mandavia (2018) | Otology/Neurotology | 4 | Nepal, United Kingdom | Cross‐sectional study; feasibility study | 56 | Concordance in primary diagnosis and decision to refer, determine through inter‐rater agreements | Development of a mobile video‐otoscopy device shows promise for use by trained nonmedical workers to screen for ear disease in remote settings | Improved access to care; Feasibility; Communication between providers |
| McCool (2018) | Otology/Neurotology | 3 | United States | Retrospective chart review | 1385 | telemedicine eligibility based on prespecified criteria, travel time | 62% of otolaryngology encounters in a VA hospital would likely be eligible for telemedicine. Patients with inner and middle ear problems were more likely eligible for telemedicine | Applicability of telemedicine; Patient satisfaction |
| Moberly (2017) | Otology/Neurotology | 4 | United States | Case series, prospective study | 210 | Diagnosis of digital otoscope eardrum images by 12 neurotologists, percentage correct compared to gold standard of diagnosis, level of confidence in diagnosis reported by reviewers | Digital otoscope images provided sufficient information for neurotologists to make correct diagnoses for some pathologies while others were more difficult to diagnose based on a still image | Equivalency of diagnosis or outcomes; Importance of image or video quality |
| Moshtaghi (2017) | Otology/Neurotology | 4 | United States | Prospective blinded observational study | 57 | Diagnostic concordance with classification of TM by blinded neurotologist, patient satisfaction ratings | Diagnosis made using smartphone otoscopy resulted in a concordant diagnosis 96% of the time; high degree of patient satisfaction | Equivalency of diagnosis or outcomes; Importance of image or video quality |
| Shah (2018) | Otology/Neurotology | 4 | United States | Case series, prospective study | 80 | Interrater reliability between video diagnosis and original diagnosis on pneumatic otoscopy | iPhone otoscopy provides reliable images when used by otolaryngologists but images obtained by parents are not suitable for use in diagnosis | Equivalency of diagnosis or outcomes; Importance of image or video quality |
In a landmark study, Kokesh et al. described a “store‐and‐forward model (SAF),” wherein audiologists and advanced practice providers obtain patient histories and otologic examinations and forward these to otolaryngologists. 25 , 26 , 27 Compared to in‐person visits, SAF evaluations demonstrated decreased wait times and reduced patient travel costs.
Recent technological advances have allowed for the recording and storage of otoscopic examinations, allowing for SAF neurotology consults, with high level of accordance with in‐person diagnoses. 16 , 28 , 29 , 30 , 31 , 32 , 33 With a focus on otitis media, Biagio et al. used video‐otoscopy recordings in children recorded by facilitators with limited training. 16 The quality of the video‐otoscopy recordings was noted to be acceptable or better in 87% of cases. In a study by Erkkola‐Anttinen et al., parents of pediatric patients were trained to use otoscopes attached to smartphones for diagnosis of acute otitis media, though videos of sufficient technical quality were only obtained in 67% of cases. 34 The primary concerns regarding video‐otoscopy are poor image quality and examination reliability. Subtle findings such as mild retraction pocket, atelectasis, pinhole perforation, or small cholesteatoma may not be apparent on low‐quality images. 34 Other limitations include access to at‐home equipment, such as otoscopes, specula, and image‐capturing devices, as well as high‐speed internet needed to transmit high‐resolution images. 34 , 35 , 36
Telehealth has been applied to tinnitus rehabilitation, cochlear implant fitting, programming, and maintenance, as well as hearing aid assessment and programming. 37 , 38 A VA study of tinnitus management utilizing a skills education program delivered via telephone showed far greater improvement in symptom management than the wait‐list group. 39 Luryi et al. examined the role of telemedicine in cochlear implant programming of VA patients, and concluded that cochlear implant threshold, comfort, and impedance levels were readily obtained via telehealth and did not differ significantly to in‐person sessions. 15 When assessing the feasibility of remote evaluation of cochlear implant candidacy, Fletcher et al. reported comparable testing results across remote and in‐person conditions in a within‐subject control study. 40
Despite the demonstrated applicability of telemedicine to neurotology, there is documented needs for improvement. Several studies note that a reliable standardized grading scale or diagnostic guide could be of significance in remote evaluation of otitis media to ensure more uniform, standardized assessments. 31 , 41
Recommendations for practice
We recommend that telemedicine be used for the diagnosis, workup, and management of otologic pathologies in select circumstances (Table I). The feasibility of remote evaluation and programming of both hearing aids and cochlear implants have been demonstrated and may be particularly useful in rural areas with limited access to care. Auditory rehabilitation following cochlear implantation is another promising application for remote health, yet does not come without risks (Table I). Further research assessing the use of telemedicine in diagnosing and triaging inner ear pathologies, otologic/neurotologic tumors, and other common pathologies is warranted.
Laryngology
Findings
To assess the feasibility of remote vocal rehabilitation, Mashima et al. compared treatment outcomes between patients seen in person or by video teleconference. 42 The authors reported no differences in outcomes between the groups, supporting noninferior use of telemedicine in vocal rehabilitation. Doarn et al. developed an online portal to provide home practice support for children between weekly voice therapy sessions. 43 In addition to facilitating increased communication with clinicians, the study documented an increase in patient adherence to therapy recommendations.
While telemedicine has been successfully applied to vocal rehabilitation, it faces challenges in diagnosis of laryngeal pathologies the examination of which requires technical skill and experience (Table IV). Given the significant challenges of transmission risk and limited PPE in the COVID‐19 pandemic, alteration of typical methods of voice and swallowing triage, evaluation, and management must be considered. To address this, Ku et al. published clinical practice guidelines for the management of dysphagia in the COVID‐19 pandemic, suggesting use of telemedicine for triage and remote evaluation. 44
Table IV.
Summary of Articles in Qualitative Review for Laryngology.
| Author (year) | Discipline | Level of evidence | Country of origin | Study design and methods | Number of participants/sample size | Outcome measured | Key findings | Common themes |
|---|---|---|---|---|---|---|---|---|
| Bloom (1998) | Laryngology | 3 | Canada | Retrospective chart review | 77 | CT findings, pathologic analysis, and endoscopic data | CT is valuable in the assessment of laryngeal cancer, but performs more poorly in staging advanced laryngeal cancer and predicting clinical outcomes following radiotherapy | Potential alternative to invasive procedure |
| Bryson (2018) | Laryngology | 5 | United States | Case report and expert opinion | 2 | Speed of audiovisual transmission, time delay | Two patients were successfully evaluated remotely with real‐time interaction | Feasibility; Communication between clinicians |
| Doarn (2019) | Laryngology | 4 | United States | Case series | 10 | Utilization of the web portal by participants, time spent practicing exercises, responses to parental questionnaire | Successfully designed and implemented an online portal to provide supported home practice for children between weekly voice therapy sessions, found an increase in patient adherence to therapy recommendations | Applicability of telemedicine; Communication between patient and physician; Patient satisfaction |
| Ferri (1999) | Laryngology | 3 | Italy | Retrospective chart review | 187 | CT findings, pathologic analysis, and endoscopic data, staging accuracy | Both laryngoscopy and CT have a role in diagnosis and staging of laryngeal cancer | Potential alternative to invasive procedure |
| Ku (2020) | Laryngology | 5 | United States | Expert opinion and literature review | NA | Practical workflow for managing dysphagia during the COVID‐19 pandemic | Provides clinical practice guidelines to balance risks of SARS‐CoV‐2 exposure with the risks associated with dysphagia | Applicability of telemedicine |
| Mashima (2003) | Laryngology | 2 | United States | Prospective observational study | 72 | Perceptual judgments of voice quality, acoustic analyses of voice, patient satisfaction ratings, and fiber‐optic laryngoscopy | No differences in outcome measures between the conventional group and the remote video teleconference group | Equivalency of diagnosis or outcomes; importance of image or video quality |
| Nasr (2013) | Laryngology | 2 | Egypt | Comparative cross‐sectional study | 68 | Detection rate of vocal cord nodules, polyps, and cysts from laryngeal ultrasound compared to CT scan | Laryngeal ultrasound performed comparably to CT scan for detection of all pathologies studied | Equivalency of diagnosis or outcomes; Potential alternative to invasive procedure |
| Tsui (2012) | Laryngology | 5 | China | Current review | NA | Reviews recent clinical applications of ultrasound imaging in laryngeal examinations | Combining functional ultrasound imaging with Doppler imaging may be used to evaluate laryngeal tissues | Potential alternative to invasive procedure |
| Wormald (2008) | Laryngology | 4 | Ireland | Prospective blinded single‐site study | 78 | Presence or absence of a vocal fold paralysis as determined by an automated classifier | The automated speech analysis system demonstrated 92% sensitivity and 75% specificity for detecting vocal fold paralysis | Equivalency of diagnosis or outcomes; Potential alternative to invasive procedure |
| Xia (2013) | Laryngology | 4 | China | Case series | 72 | Detection rate of ultrasonography compared to CT and laryngoscopy | Ultrasonography may be used as a valuable supplementary imaging method to CT and laryngoscopy in the assessment of laryngeal carcinoma | Potential alternative to invasive procedure |
For remote voice and swallowing disorder diagnosis, one strategy is the use of non‐image‐based tools like voice recordings, as described by Wormald et al. 45 Using an automated speech analysis system, the authors demonstrated 92% sensitivity and 75% specificity for detecting vocal fold paralysis. With regards to other laryngeal pathology, computed tomography (CT) scans and ultrasonography have the benefit of being noninvasive and amenable to store‐and‐forward telemedicine although such may miss early, small glottic cancers and subtle laryngeal lesions. 46 , 47 , 48 , 49 , 50
Bryson et al. detailed recommendations for remote laryngoscopy evaluation, including use of stroboscopy, archiving capability, and internet connection. However, a proxy practitioner capable of performing the procedure would be necessary, such as a speech and language pathologist or primary care provider. As in otology, any remote diagnostic modalities must prioritize high‐quality imaging to meet standards of care. 51
Recommendations for practice
We strongly recommend that telemedicine be applied to voice therapy, as it has been shown to meet standards of care with increased provider and patient satisfaction. Machine learning‐driven detection of vocal pathologies has also shown to be effective, and further studies examining this diagnostic modality are warranted. There has been early investigation into fiberoptic laryngoscopy with remote analysis by otolaryngologists, but this practice has not been well‐established and faces barriers to implementation. Imaging is an option to supplement and, at times, replace in‐person laryngoscopy, but further research is needed to demonstrate its reliability.
Rhinology
Findings
Similar to laryngoscopy, nasal endoscopy is considered high risk for exposure to COVID‐19. 52 Furthermore, anesthetic sprays have aerosolizing potential, which increases risk of transmission not just to the direct provider but to adjacent personnel. Due to the clinical needs and risks of nasal endoscopy, investigating alternatives to this procedure is of significant interest (Table V). CT sinus imaging can be used as an alternative to endoscopy. 53 A number of studies have revealed high diagnostic concordance between nasal endoscopy and CT in the evaluation of sinus disorders. 53 , 54 An obvious benefit is that any diagnostic imaging is especially amenable to remote evaluation. Another alternative is remote intranasal imaging, with setups similar to those described for video‐otoscopy or laryngoscopy. A small number of studies have described systems for remotely performed nasal endoscopy with digital recording and SAF transmission, including use of smartphone‐compatible systems, though this has similar limitations to neurotolgy and laryngology with regards to implementing remote procedures. 55 , 56
Table V.
Summary of Articles in Qualitative Review for Rhinology.
| Author (year) | Discipline | Level of evidence | Country of origin | Study design and methods | Number of participants/sample size | Outcome measured | Key findings | Common themes |
|---|---|---|---|---|---|---|---|---|
| Bousquet (2019) | Rhinology | 5 | France | Expert opinion and proposal of guidelines | NA | Use of mobile technology in patients with allergic rhinitis and asthma multimorbidity | Development of a mobile app which allowed patients to keep an allergy diary improved adherence to treatment plan and communication with their physician | Communication between patient and physician; Patient satisfaction |
| Deosthale (2017) | Rhinology | 2 | India | Prospective observational study, within‐subject design | 54 | Sensitivity and specificity of diagnosis by nasal endoscopy or CT scan | CT scan may be an alternative to nasal endoscopy in certain patients with chronic rhinosinusitis | Potential alternative to invasive procedure |
| Khanwalkar (2019) | Rhinology | 2 | United States | Prospective cohort study | 249 | Patient reported outcome measures, including pain | A mobile platform may effectively track postoperative outcomes of septoplasty and functional endoscopic sinus surgery, and improve patient engagement | Communication between patient and physician; Patient satisfaction |
| Lohyia (2016) | Rhinology | 2 | India | Prospective cohort study | 100 | Scored endoscopic findings and CT scans, clinical diagnosis based on established guidelines | No significant difference was found in diagnostic accuracy between CT and nasal endoscopy for patients with chronic rhinosinusitis | Potential alternative to invasive procedure |
| Mistry (2017) | Rhinology | 5 | United Kingdom | Expert opinion | NA | Detailed overview of mobile endoscopic imaging system use and applications | The endoscope‐I is a compact, portable, endoscopic viewing system which allows real‐time feedback to the patient and physician | Applications of telemedicine; Feasibility; Communication between clinicians |
| VanLue (2007) | Rhinology | 5 | United States | Expert opinion | NA | Describes development of a microportable imaging system for nasal endoscopy | Digital recording and SAF transmission used in conjunction with the microportable imaging system may be useful in telemedicine | Applications of telemedicine; Feasibility; Communication between clinicians |
| Seim (2018) | Rhinology | 2 | United States | Prospective observational study | 21 | Physician diagnostic agreement, patient satisfaction scores | Through synchronous telemedicine, conditions including epistaxis may be evaluated remotely | Communication between clinicians; Equivalency of diagnosis or outcomes; Patient satisfaction |
| Setzen (2020) | Rhinology | 5 | United States | Current review | NA | Evaluation of elective vs. urgent cases, procedural alternatives, billing | CT sinus imaging may be an alternative to nasal endoscopy. Remote evaluation of epistaxis is feasible but must identify high‐risk patients | Alternatives to procedure |
Epistaxis is another common rhinologic referral and may be amenable to remote evaluation. 52 , 57 Telemedicine can help identify triggers, risk factors, and manage mild bleeding in low‐acuity patients. Red flags in the patient history or failure to control bleeding with conservative measures should prompt in‐person evaluation. 52
Specifically regarding follow‐up care in rhinology, Khanwalkar et al. used mobile technology to track postoperative outcomes following septoplasty and functional endoscopic sinus surgery. 58 Mobile technology has also been successfully used in the management of allergic rhinitis. 59
Recommendations for practice
Telemedicine has demonstrated applicability in rhinology, and we recommend that it be used for follow‐up in the management of allergic rhinitis (AR). Further study is needed in remote management of nonallergic rhinosinusitis. While there is a need to limit intranasal endoscopy in the time of COVID‐19, sole use of CT imaging for diagnosis is a deviation from standards of care and may have medicolegal implications. Further research is needed to establish the efficacy of CT as a substitute to nasal endoscopy. Development of guidelines for triage and remote evaluation of potentially emergent conditions such as epistaxis and invasive processes is also needed.
Facial Plastic and Reconstructive Surgery
Findings
Telemedicine is readily applicable to many aspects of facial plastic and reconstructive surgery (Table VI). Evaluation of facial soft tissue relationships and defects is already heavily based on digital photographic documentation and analysis. 60 , 61 As such, assessment of facial trauma may be particularly amenable to remote assessment. Fonseca et al. reported high concordance between in‐person evaluations of facial trauma patients and evaluations carried out through smartphone videoconferencing with review of CT imaging. 62 A remote approach for triage can avoid unnecessary transfers for patients that do not require urgent intervention, and possibly reduce length of hospitalization.
Table VI.
Summary of Articles in Qualitative Review for Facial Plastic and Reconstructive Surgery.
| Author (year) | Discipline | Level of evidence | Country of origin | Study design and methods | Number of participants/sample size | Outcome measured | Key findings | Common themes |
|---|---|---|---|---|---|---|---|---|
| Appold (2017) | Facial Plastic and Reconstructive Surgery | 5 | United States | Expert opinion | NA | NA | Telemedicine appointments after facial plastic survey allow for closer follow‐up of postoperative sites, evaluation of wound healing, and response to patient concerns | Communication between patient and physician; Patient satisfaction |
| Chen (2018) | Facial Plastic and Reconstructive Surgery | 4 | United States | Prospective observational study, no cohort design | 36,836 | Patient satisfaction survey scores and results | Patient trust and confidence in provider, and ability to communicate with the provider, is more important than perceived office environment to maintaining satisfaction | Communication between patient and physician; Patient satisfaction |
| Fonsesca (2020) | Facial Plastic and Reconstructive Surgery | 1 | Brazil | Prospective randomized control trial | 50 | Patient demographics, physical examination and CT scan findings, selected treatment option. | Substantial concordance of physical examination findings, CT scan interpretation, and treatment plan selection between in‐person evaluations and smartphone videoconferencing | Communication between clinicians; equivalency of diagnosis or outcomes |
| Douglas (2018) | Facial Plastic and Reconstructive Surgery | 4 | United States | Prospective single‐site study | 41 | Ratings of overall satisfaction, quality of interaction, and ability to communicate | 83% of patients reported they would prefer telemedicine services for future nonurgent plastic surgery consultations in a VA health system | Patient satisfaction |
| Pozza (2017) | Facial Plastic and Reconstructive Surgery | 4 | United States | Case series | 57 | Patient satisfaction survey, postoperative complication rate | Postoperative telephone follow‐ups after cosmetic surgery enhance the patient's postoperative experience and alert the surgeon to early postoperative problems | Communication between patient and physician; Patient satisfaction |
Frequent video or image‐based communication between patient and provider may improve patient satisfaction by facilitating closer postoperative follow‐up and wound care. After telemedicine was utilized by a VA Plastic Surgery Department for assessment of nonurgent pathologies like skin lesions and wound care, 83% of patients reported that they would prefer telemedicine over traditional evaluation for similar future visits. 63 High levels of patient satisfaction were also achieved with smartphone‐based follow‐up of facial cosmetic surgery and reviewing images remotely. 64 , 65 These reports of improved patient experience likely stem from improved perception of communication.
Limitations for telemedicine implementation in facial plastic surgery include the ability to obtain and transmit appropriately oriented, high‐quality images for facial analysis, as well as the barriers to patient–surgeon relationship which, while affected in all sub‐specialties, are particularly important in this arena. 61
Recommendations for practice
We recommend that telemedicine be used in certain niches within facial plastic and reconstructive surgery such as facial trauma and wound management. While facial analysis can be achieved remotely, questions remain on how to readily obtain high‐resolution photos with properly lighting and orientation. Areas of needed study include viability of remote facial soft tissue image capture and feasibility of remote surgical planning for cosmetic surgery.
Pediatric ORL
Findings
Many disorders in pediatric ORL overlap with adults, and the application of telemedicine to pediatric ORL complaints, such as otitis media, has been described in the previous sections. Telemedicine has a wide applicability in pediatric ORL for obtaining patient history and assessing need for common surgeries such as obstructive sleep apnea, recurrent tonsillitis, and recurrent otitis media (Table VII). 66 , 67 Telemedicine has also been used for postoperative follow‐up of common pediatric ORL procedures, such as tonsillectomy and adenoidectomy. 68 For general pediatric care in the outpatient setting, telemedicine may improve communication with parents. 69
Table VII.
Summary of Articles in Qualitative Review for Pediatric Otolaryngology.
| Author (year) | Discipline | Level of evidence | Country of origin | Study design and methods | Number of participants/sample size | Outcome measured | Key findings | Common themes |
|---|---|---|---|---|---|---|---|---|
| Burke (2015) | Pediatrics | 5 | United States | Expert opinion, literature review | NA | Uses of telemedicine in pediatric patient and parent education, access to care, barriers to implementation | For general pediatric care in the outpatient setting, telemedicine may even improve communication with parents | Communication between patient and physician |
| Shaffer (2020) | Pediatrics | 4 | United States | Retrospective case series | 82 | Patient symptoms recorded on a standardized form by nurses, treatment, referrals, and clinical outcomes | A clinical pathway for managing tympanostomy tube otorrhea beginning with phone triage was developed, obviating clinic visits in 82.9% of patients with a 75.6% cure rate | Applications of telemedicine; Feasibility |
| Smith (2005) | Pediatrics | 4 | United States | Case series, feasibility study | 64 | Referral patterns, clinical outcomes | Videoconferencing may be used effectively for pre‐screening potential surgical admissions to a tertiary hospital | Applicability of telemedicine; Feasibility |
| Smith (2008) | Pediatrics | 4 | Australia | Retrospective chart review | 68 | Concordance between videoconference and in‐person consultation findings | The diagnosis was concurrent in 99% of cases. Surgical management decisions were concurrent in 93% of cases | Communication between clinicians; communication between patient and physician; Equivalency of diagnosis or outcomes |
| Yang (2016) | Pediatrics | 1 | South Korea | Randomized control trial | 61 | Ratings of parents' knowledge of postoperative care and ratings of children's anxiety | Postoperative tonsillectomy care education using smartphone text messaging increases parents' knowledge and reduces children's anxiety | Communication between clinicians; Patient satisfaction |
Telemedicine has also been used to evaluated and manage pediatric acute tympanostomy tube otorrhea. Shaffer and Dohar reported that 83% of patients were diagnosed and treated without emergency room or office assessment, with no adverse outcomes recorded. 70
Recommendations for practice
We recommend that telemedicine be used when feasible to enhance communication and access between parents and providers in pediatric ORL, and to streamline referrals and work‐up prior to in‐patient consultation. Further study is required to identify and describe most impactful applications. Common pediatric emergencies like aerodigestive foreign bodies and postoperative complications like posttonsillectomy hemorrhage, however, will continue to require urgent in‐person evaluation.
DISCUSSION
In the era of COVID‐19, minimizing virus transmission has become a critical part of patient care, propelling telemedicine into the forefront of the healthcare conversation. To help meet the urgent need for telehealth implementation, federal agencies have increased coverage and suspended barriers to telehealth utilization. 71 , 72 , 73 A general limitation of telemedicine is that patients in rural or medically underserved regions lack access to requisite technology. In 2018, 26.3% of Medicare beneficiaries lacked digital access at home. 74 In the Coronavirus Preparedness and Response Supplemental Appropriations Act, the Centers for Medicare and Medicaid Services are now allowing nonrural Medicare patients to utilize telehealth services from home. 71 The Office of Civil Rights of the Department of Health and Human Services (HHS) has suspended certain Health Insurance Portability and Accountability Act requirements broadening the technological applications that may be used to implement telehealth communications with patients during the COVID‐19 pandemic. 72 Furthermore, the Office of Inspector General of the HHS has waived telehealth co‐payments for Medicare patients. 73
While many states have temporarily relaxed licensure requirements to allow physicians to provide telemedicine across state and Medicare began reimbursing audio‐only visits at the same rate as video and in‐person visits reimbursement reform may be necessary to ensure that a full range of telehealth services is covered by insuring providers. 75 , 76 Furthermore, remotely assisting personnel must seek payment directly from the billing physician, requiring a contractual arrangement with the physician. 77
Fortunately, telemedicine is not new to ORL, and has precedents in each of the main subspecialties (Table I). Applications of telemedicine within ORL, as in other fields, fall into three distinct categories: synchronous care with and without assistant providers, as well as asynchronous care or SAF. Synchronous care without assistance includes interactions between the otolaryngologist and the patient without an assistant. These evaluations have been proven useful for head and neck oncology triaging and postoperative visits, vocal rehabilitation, endoscopic sinus surgery postoperative evaluation, allergic rhinitis management, facial trauma evaluation, and facial plastic postoperative evaluation. 17 , 18 , 19 , 25 , 45 , 58 , 60 , 62 , 64
The second category involves synchronous care with the presence of an assistant. Such assistants may be able to perform or facilitate remote diagnostic procedures such as inpatient flap checks, otoscopic evaluation, voice rehabilitation, and swallowing evaluation, as well as pre‐ and postoperative evaluation of pediatric patients. 23 , 35 , 36 , 44 , 45 , 66 , 67 , 68 , 70 Personnel must have adequate experience and training, without which the patient may be significantly at risk of pain, injury, or misdiagnosis. 15 , 52 Robust telehealth networks must be created, wherein otolaryngologists can easily work with a patient's primary care provider to offer remote services and consultation. 60
The third category is asynchronous care or SAF telemedicine, in which primary data are collected, transmitted to the consultant, and evaluated at a later time point. Pathologies appropriate for asynchronous care are inherently nonurgent. Utilization of SAF techniques have already proven useful in head and neck oncology consultations, remote otologic and audiologic evaluation, cochlear implant and hearing aid management, laryngeal ultrasonography, nasolaryngoscopy, as well as CT sinus review. 16 , 19 , 26 , 27 , 28 , 29 , 31 , 32 , 34 , 35 , 38 , 39 , 41 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57
CONCLUSION
Telemedicine has been successfully utilized to varying degrees in the past. Further studies must include rigorous design controls, and standardization of populations and outcome measures to reduce heterogeneity and improve applicability. 78 The COVID‐19 pandemic has propelled its necessity and utilization into the mainstays of current ORL practice. Now is the time to establish standards of practice that are safe, effective, and affordable for providers and patients.
Author contributions
AKS and DAK conceptualized and designed the study, performed literature reviews, drafted and critically revised the manuscript. RJ, JS, ELS, and ML critically reviewed, performed and interpreted data/literature reviews, and revised the manuscript. NK conceptualized and designed the study, critically reviewed the manuscript draft and revisions.
Supporting information
Appendix S1. Full description of literature search methods.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
BIBLIOGRAPHY
- 1. Stensland J, Speedie SM, Ideker S, House J, Thompson T. The relative cost of outpatient telemedicine services. Telemed J 1999;5:245–256. [DOI] [PubMed] [Google Scholar]
- 2. Caffery LJ, Farjian M, Smith AC. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: a scoping review. J Telemed Telecare 2016;22:504–512. [DOI] [PubMed] [Google Scholar]
- 3. Latifi R, Weinstein RS, Porter JM, et al. Telemedicine and telepresence for trauma and emergency care management. Scand J Surg 2007;96:281–289. [DOI] [PubMed] [Google Scholar]
- 4. Couturier P, Tyrrell J, Tonetti J, Rhul C, Woodward C, Franco A. Feasibility of orthopaedic teleconsulting in a geriatric rehabilitation service. J Telemed Telecare 1998;4(1_Suppl):85–87. [DOI] [PubMed] [Google Scholar]
- 5. Warshaw EM, Hillman YJ, Greer NL, et al. Teledermatology for diagnosis and management of skin conditions: a systematic review. J Am Acad Dermatol 2011;64:759–772.e721. [DOI] [PubMed] [Google Scholar]
- 6. Gardiner S, Hartzell TL. Telemedicine and plastic surgery: a review of its applications, limitations and legal pitfalls. J Plast Reconstr Aesthet Surg 2012;65:e47–e53. [DOI] [PubMed] [Google Scholar]
- 7. Holt B, Faraklas I, Theurer L, Cochran A, Saffle JR. Telemedicine use among burn centers in the United States: a survey. J Burn Care Res 2012;33:157–162. [DOI] [PubMed] [Google Scholar]
- 8. Moffet H, Tousignant M, Nadeau S, et al. In‐home telerehabilitation compared with face‐to‐face rehabilitation after total knee arthroplasty: a noninferiority randomized controlled trial. J Bone Joint Surg Am 2015;97:1129–1141. [DOI] [PubMed] [Google Scholar]
- 9. Vyas KS, Hambrick HR, Shakir A, et al. A systematic review of the use of telemedicine in plastic and reconstructive surgery and dermatology. Ann Plast Surg 2017;78:736–768. [DOI] [PubMed] [Google Scholar]
- 10. Sohn GK, Wong DJ, Yu SS. A review of the use of telemedicine in dermatologic surgery. Dermatol Surg 2020;46:501–507. [DOI] [PubMed] [Google Scholar]
- 11. Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005–2017. JAMA 2018;320:2147–2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bann DV, Patel VA, Saadi R, et al. Best practice recommendations for pediatric otorhinolaryngology during the COVID‐19 pandemic. Otolaryngol Head Neck Surg 2020;10:19. [DOI] [PubMed] [Google Scholar]
- 13. Calton B, Abedini N, Fratkin M. Telemedicine in the time of coronavirus. J Pain Symptom Manage 2020;60:e12–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zou L, Ruan F, Huang M, et al. SARS‐CoV‐2 viral load in upper respiratory specimens of infected patients. N Engl J Med 2020;382:1177–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Luryi AL, Tower JI, Preston J, Burkland A, Trueheart CE, Hildrew DM. Cochlear implant mapping through telemedicine—a feasibility study. Otol Neurotol 2020;41:e330–e333. [DOI] [PubMed] [Google Scholar]
- 16. Biagio L, Swanepoel DW, Laurent C, Lundberg T. Video‐otoscopy recordings for diagnosis of childhood ear disease using telehealth at primary health care level. J Telemed Telecare 2014;20:300–306. [DOI] [PubMed] [Google Scholar]
- 17. Dorrian C, Ferguson J, Ah‐See K, et al. Head and neck cancer assessment by flexible endoscopy and telemedicine. J Telemed Telecare 2009;15:118–121. [DOI] [PubMed] [Google Scholar]
- 18. Beswick DM, Vashi A, Song Y, et al. Consultation via telemedicine and access to operative care for patients with head and neck cancer in a veterans health administration population. Head Neck 2016;38:925–929. [DOI] [PubMed] [Google Scholar]
- 19. Kohlert S, Murphy P, Tse D, Liddy C, Afkham A, Keely E. Improving access to otorhinolaryngology–head and neck surgery expert advice through eConsultations. Laryngoscope 2018;128:350–355. [DOI] [PubMed] [Google Scholar]
- 20. Weinstein RS, Lopez AM, Barker GP, et al. The innovative bundling of teleradiology, telepathology, and teleoncology services. IBM Syst J 2007;46:69–84. [Google Scholar]
- 21. Rimmer RA, Christopher V, Falck A, et al. Telemedicine in otorhinolaryngology outpatient setting—single center head and neck surgery experience. Laryngoscope 2018;128:2072–2075. [DOI] [PubMed] [Google Scholar]
- 22. López AM, Graham AR, Barker GP, et al. Virtual slide telepathology enables an innovative telehealth rapid breast care clinic. Hum Pathol 2009;40:1082–1091. [DOI] [PubMed] [Google Scholar]
- 23. Alemi AS, Seth R, Heaton C, Wang SJ, Knott PD. Comparison of video and in‐person free flap assessment following head and neck free tissue transfer. Otorhinolaryngol Head Neck Surg 2017;156:1035–1040. [DOI] [PubMed] [Google Scholar]
- 24. Hee Hwang J, Mun G‐H. An evolution of communication in postoperative free flap monitoring: using a smartphone and mobile messenger application. Plast Reconstr Surg 2012;130:125–129. [DOI] [PubMed] [Google Scholar]
- 25. Kokesh J, Ferguson AS, Patricoski C. Preoperative planning for ear surgery using store‐and‐forward telemedicine. Otolaryngol Head Neck Surg 2010;143:253–257. [DOI] [PubMed] [Google Scholar]
- 26. Kokesh J, Ferguson AS, Patricoski C, LeMaster B. Traveling an audiologist to provide otorhinolaryngology care using store‐and‐forward telemedicine. Telemed e‐Health 2009;15:758–763. [DOI] [PubMed] [Google Scholar]
- 27. Hofstetter PJ, Kokesh J, Ferguson AS, Hood LJ. The impact of telehealth on wait time for ENT specialty care. Telemed e‐Health 2010;16:551–556. [DOI] [PubMed] [Google Scholar]
- 28. Arriaga MA, Nuss D, Scrantz K, et al. Telemedicine‐assisted neurotology in post‐Katrina Southeast Louisiana. Otol Neurotol 2010;31:524–527. [DOI] [PubMed] [Google Scholar]
- 29. McCool RR, Davies L. Where does telemedicine fit into otolaryngology? An assessment of telemedicine eligibility among otolaryngology diagnoses. Otolaryngol Head Neck Surg 2018;158:641–644. [DOI] [PubMed] [Google Scholar]
- 30. Mandavia R, Lapa T, Smith M, Bhutta MF. A cross‐sectional evaluation of the validity of a smartphone otoscopy device in screening for ear disease in Nepal. Clin Otolaryngol 2018;43:31–38. [DOI] [PubMed] [Google Scholar]
- 31. Lundberg T, Biagio L, Laurent C, Sandström H, Swanepoel DW. Remote evaluation of video‐otoscopy recordings in an unselected pediatric population with an otitis media scale. Int J Pediatr Otolarygol 2014;78:1489–1495. [DOI] [PubMed] [Google Scholar]
- 32. Gupta N, Chalwa N, Gupta D, et al. Community triage of otology patients using a store‐and‐forward telemedicine device: a feasibility study. Ear Nose Throat J 2017;96:246–249. [PubMed] [Google Scholar]
- 33. Kokesh J, Ferguson AS, Patricoski C, et al. Digital images for postsurgical follow‐up of tympanostomy tubes in remote Alaska. Otolaryngol Head Neck Surg 2008;139:87–93. [DOI] [PubMed] [Google Scholar]
- 34. Erkkola‐Anttinen N, Irjala H, Laine MK, Tähtinen PA, Löyttyniemi E, Ruohola A. Smartphone otoscopy performed by parents. Telemed e‐Health 2018;25:477–484. [DOI] [PubMed] [Google Scholar]
- 35. Moshtaghi O, Sahyouni R, Haidar YM, et al. Smartphone‐enabled otoscopy in neurotology/otology. Otorhinolaryngol Head Neck Surg 2017;156:554–558. [DOI] [PubMed] [Google Scholar]
- 36. Shah MU, Sohal M, Valdez TA, Grindle CR. iPhone otoscopes: currently available, but reliable for tele‐otoscopy in the hands of parents? Int J Pediatr Otolaryngol 2018;106:59–63. [DOI] [PubMed] [Google Scholar]
- 37. Bush ML, Thompson R, Irungu C, Ayugi J. The role of telemedicine in auditory rehabilitation: a systematic review. Otol Neurotol 2016;37:1466–1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Krumm M, Syms MJ. Teleaudiology. Otolaryngol Clin North Am 2011;44:1297–1304. [DOI] [PubMed] [Google Scholar]
- 39. Schmidt CJ, Kaelin C, Henselman L, Henry JA. Need for mental health providers in progressive tinnitus management: a gap in clinical care. Fed Pract 2017;34:6–9. [PMC free article] [PubMed] [Google Scholar]
- 40. Fletcher KT, Dicken FW, Adkins MM, et al. Audiology telemedicine evaluations: potential expanded applications. Otolaryngol Head Neck Surg 2019;161:63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Moberly AC, Zhang M, Yu L, et al. Digital otoscopy versus microscopy: how correct and confident are ear experts in their diagnoses? J Telemed Telecare 2017;24:453–459. [DOI] [PubMed] [Google Scholar]
- 42. Mashima PA, Birkmire‐Peters DP, Syms MJ, Holtel MR, Burgess LPA, Peters LJ. Telehealth: voice therapy using telecommunications technology. Am J Speech Lang Pathol 2003;12:432–439. [DOI] [PubMed] [Google Scholar]
- 43. Doarn CR, Zacharias S, Keck CS, Tabangin M, DeAlarcon A, Kelchner L. Design and implementation of an interactive website for pediatric voice therapy—the concept of in‐between care: a Telehealth model. Telemed e‐Health 2018;25:415–422. [DOI] [PubMed] [Google Scholar]
- 44. Ku PKM, Holsinger FC, Chan JYK, et al. Management of dysphagia in the patient with head and neck cancer during COVID‐19 pandemic: practical strategy. Head Neck 2020;42:1491–1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wormald RN, Moran RJ, Reilly RB, Lacy PD. Performance of an automated, remote system to detect vocal fold paralysis. Ann Otol Rhinol Laryngol 2008;117:834–838. [DOI] [PubMed] [Google Scholar]
- 46. Bloom C, Just N, Remy H, Black M, Rossignol M. Laryngeal cancer: is computed tomography a valuable imaging technique? A retrospective analysis. Can Assoc Radiol J 1998;49:370–377. [PubMed] [Google Scholar]
- 47. Ferri T, De Thomasis G, Quaranta N, Bacchi G, Bottazzi D. The value of CT scans in improving laryngoscopy in patients with laryngeal cancer. Eur Arch Otorhinolaryngol 1999;256:395–399. [DOI] [PubMed] [Google Scholar]
- 48. Tsui P‐H, Wan Y‐L, Chen C‐K. Ultrasound imaging of the larynx and vocal folds: recent applications and developments. Curr Opin Otolaryngol Head Neck Surg 2012;20:437–442. [DOI] [PubMed] [Google Scholar]
- 49. Xia CX, Zhu Q, Zhao HX, Yan F, Li SL, Zhang SM. Usefulness of ultrasonography in assessment of laryngeal carcinoma. Br J Radiol 2013;86:20130343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Nasr W, Amer H, Askar S, Enaba M. Laryngeal ultrasound as effective as CT scans for the diagnosis of various laryngeal lesions. Egypt J Otolaryngol 2013;29:93–98. [Google Scholar]
- 51. Bryson PC, Benninger MS, Band J, Goetz P, Bowen AJ. Telemedicine in laryngology: remote evaluation of voice disorders‐setup and initial experience. Laryngoscope 2018;128:941–943. [DOI] [PubMed] [Google Scholar]
- 52. Setzen M, Svider PF, Pollock K. COVID‐19 and rhinology: a look at the future. Am J Otolaryngol 2020;41:102491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Deosthale NV, Khadakkar SP, Harkare VV, et al. Diagnostic accuracy of nasal endoscopy as compared to computed tomography in chronic Rhinosinusitis. Indian J Otolaryngol Head Neck Surg 2017;69:494–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lohiya SS, Patel SV, Pawde AM, Bokare BD, Sakhare PT. Comparative study of diagnostic nasal endoscopy and CT paranasal sinuses in diagnosing chronic rhinosinusitis. Indian J Otolaryngol Head Neck Surg 2016;68:224–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mistry N, Coulson C, George A. endoscope‐i: an innovation in mobile endoscopic technology transforming the delivery of patient care in otolaryngology. Expert Rev Med Devices 2017;14:913–918. [DOI] [PubMed] [Google Scholar]
- 56. VanLue M, Cox KM, Wade JM, et al. Development of a microportable imaging system for otoscopy and nasoendoscopy evaluations. Cleft Palate Craniofac J 2007;44:121–125. [DOI] [PubMed] [Google Scholar]
- 57. Seim NB, Philips RHW, Matrka LA, et al. Developing a synchronous otolaryngology telemedicine clinic: prospective study to assess fidelity and diagnostic concordance. Laryngoscope 2018;128:1068–1074. [DOI] [PubMed] [Google Scholar]
- 58. Khanwalkar AR, Shen J, Kern RC, et al. Utilization of a novel interactive mobile health platform to evaluate functional outcomes and pain following septoplasty and functional endoscopic sinus surgery. Int Forum Allergy Rhinol 2019;9:345–351. [DOI] [PubMed] [Google Scholar]
- 59. Bousquet J, Hellings PW, Agache I, et al. Allergic rhinitis and its impact on asthma (ARIA) phase 4 (2018): change management in allergic rhinitis and asthma multimorbidity using mobile technology. J Allergy Clin Immunol 2019;143:864–879. [DOI] [PubMed] [Google Scholar]
- 60. Kokesh J, Ferguson AS, Patricoski C. The Alaska experience using store‐and‐forward telemedicine for ENT care in Alaska. Otolaryngol Clin North Am 2011;44:1359–1374. [DOI] [PubMed] [Google Scholar]
- 61. Chen K, Congiusta S, Nash IS, et al. Factors influencing patient satisfaction in plastic surgery: a Nationwide analysis. Plast Reconstr Surg 2018;142:820–825. [DOI] [PubMed] [Google Scholar]
- 62. Fonseca ASF, Goldenberg DC, Stocchero GF, Luiz AVC, Gemperli R. Validation of videoconference with smartphones in telemedicine facial trauma care: analysis of concordance to on‐site evaluation. Ann Plast Surg 2016;77:433–437. [DOI] [PubMed] [Google Scholar]
- 63. Douglas S, Geiger E, McGregor A, et al. Telehealth in plastic surgery: a veterans affairs hospital perspective. Plast Reconstr Surg 2018;6:e1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Pozza ED, D'Souza GF, DeLeonibus A, Fabiani B, Gharb BB, Zins JE. Patient satisfaction with an early smartphone‐based cosmetic surgery postoperative follow‐up. Aesthet Surg J 2017;38:101–109. [DOI] [PubMed] [Google Scholar]
- 65. Appold K. Using telemedicine in otolaryngology. 2017. Available at: https://www.enttoday.org/article/using-telemedicine-otolaryngology/. Accessed January 5, 2020.
- 66. Smith A, Williams J, Agnew J, Sinclair S, Youngberry K, Wootton R. Real‐time telemedicine for paediatric ENT pre‐admission screening. J Telemed Telecare 2005;11(Suppl. 2):S86–S89. [DOI] [PubMed] [Google Scholar]
- 67. Smith AC, Dowthwaite S, Agnew J, Wootton R. Concordance between real‐time telemedicine assessments and face‐to‐face consultations in paediatric otolaryngology. Med J Aust 2008;188:457–460. [DOI] [PubMed] [Google Scholar]
- 68. Yang JY, Lee H, Zhang Y, Lee JU, Park JH, Yun EK. The effects of tonsillectomy education using smartphone text message for mothers and children undergoing tonsillectomy: a randomized controlled trial. Telemed e‐Health 2016;22:921–928. [DOI] [PubMed] [Google Scholar]
- 69. Burke BL Jr, Hall RW. Section on telehealth C. Telemedicine: pediatric applications. Pediatrics 2015;136:e293–e308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Shaffer AD, Dohar JE. Evidence‐based telehealth clinical pathway for pediatric tympanostomy tube otorrhea. Int J Pediatr Otolaryngol 2020;134:110027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020. H.R.6074—116th Congress (2019–2020). Public Law No: 116‐123.
- 72. US Department of Health and Human Services . Notification of enforcement discretion for telehealth remote communications during the COVID‐19 nationwide public health emergency. Washington, DC: US Department of Health and Human Services; 2020. [Google Scholar]
- 73. Department of Health and Human Services, Office of Inspector General . OIG policy statement regarding physicians and other practitioners that reduce or waive amounts owed by federal health care program beneficiaries for telehealth services during the 2019 novel coronavirus (COVID‐19) outbreak. Washington, DC: Department of Health and Human Services, Office of Inspector General; 2020. [Google Scholar]
- 74. Roberts ET, Mehrotra A. Assessment of disparities in digital access among Medicare beneficiaries and implications for telemedicine. JAMA Intern Med 2020;10:1001–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Federation of State Medical Boards. U.S. states and territories modifying requirements for telehealth in response to COVID‐19. 2020. Available at: https://www.fsmb.org/siteassets/advocacy/pdf/states-waiving-licensure-requirements-for-telehealth-in-response-to-covid-19.pdf. Accessed April 8, 2020.
- 76. CMS Newsroom. Medicare telemedicine healthcare provider fact sheet. Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Published 2020. Accessed April 8, 2020.
- 77. Physicians and Other Clinicians . CMS flexibilities to fight COVID‐19. 2020. Available at: https://www.cms.gov/files/document/covid-19-physicians-and-practitioners.pdf. Accessed April 8, 2020.
- 78. Krupinski EA, Bernard J. Standards and guidelines in telemedicine and telehealth. Healthcare (Basel, Switzerland) 2014;2:74–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Full description of literature search methods.


