Abstract
Orthopaedic practices have been markedly affected by the emergence of the COVID-19 pandemic. Despite the ban on elective procedures, it is impossible to define the medical urgency of a case solely on whether a case is on an elective surgery schedule. Orthopaedic surgical procedures should consider COVID-19-associated risks and an assimilation of all available disease dependent, disease independent, and logistical information that is tailored to each patient, institution, and region. Using an evidence-based risk stratification of clinical urgency, we provide a framework for prioritization of orthopaedic sport medicine procedures that encompasses such factors. This can be used to facilitate the risk-benefit assessment of the timing and setting of a procedure during the COVID-19 pandemic.
Globally, as of May 2, 2020, there were 3,233,191 confirmed cases of COVID-19 with 227,489 associated deaths.1 In the Unites States alone, there were 1,067,127 confirmed cases of Coronavirus disease 2019 (COVID-19) with 57,406 deaths.1
Few states have published guidelines specific to orthopaedic surgery during the COVID-19 outbreak, leaving hospital systems and surgeons with the responsibility of balancing the benefits of surgery with the risks to public health.2 Before March 24, 30 states published guidance regarding the discontinuation of elective procedures and 16 states provided a definition of “elective” procedures or specific guidance for determining which procedures should continue to be performed. Only five states provided guidelines specifically mentioning orthopaedic surgery; of those, four states explicitly allowed for trauma-related procedures and four states provided guidance against performing arthroplasty.2 On April 16, 2020, The White House released a three-phased guideline, called Opening Up America Again, for state and local authorities to follow when reopening their economies. In phase 1, for states and regions that satisfy the gating criteria, “elective surgeries” can resume when appropriate and on an outpatient basis.3
Mi et al4 showed that clinical characteristics and early prognosis of COVID-19 in patients with fractures were more severe than those reported for adult patients with COVID-19 without fractures, suggesting that fractures can worsen the course of the infection. Catellani et al5 concluded that surgical treatment of femoral fragility fractures in COVID-19-positive patients not only contributed to the overall patients' mobility but also improved the physiologic ventilation, O2 saturation, and assisted respiration, indicating that appropriate treatment improves the patients' overall clinical status. Dephillipo et al6 reported on acute orthopaedic injuries they recommend as “surgically necessary” for elective-urgent procedures at Ambulatory Surgical Centers (ASCs); however, they did not provide literature support to these recommendations, nor did they identify the timeframe in which surgeries should be performed. Therefore, an evidence-based risk stratification for orthopaedic pathologies has yet to be established. In addition, in the context of a pandemic, it is important to integrate the disease-intrinsic factors to external factors (eg, epidemic situation, healthcare system situation, and patient characteristics) to decide whether time-sensitive surgeries should be performed in a specific patient in a particular scenario.
The purpose of this manuscript is to provide a clear framework for the prioritization of orthopaedic sport medicine procedures. This evidence-based risk stratification based on clinical urgency facilitates the risk-benefit assessment of whether, when, and in what setting, surgery should be performed during the COVID-19 pandemic. The authors discuss all phases of the pandemic, the initiation, and acceleration intervals, as well as the deceleration intervals, when elective surgeries are gradually allowed back. A framework for prioritization, such as the one presented in this study, is recommended by the American College of Surgeons, and it will continue to serve as an important guide, both during and after the pandemic.
Risk Stratification
We synthesized the current knowledge of common orthopaedic sport-medicine ailments from published literature and expert opinion to develop consensus statements and tables for each topic. For each condition, the assessment tables contain coded cells, with green boxes representing favorable situations to perform surgery, yellow moderate, and red unfavorable.
Disease Independent or External Factors Risk Assessment
Ultimately, disease independent or “external” factors must determine the safe resumption of nonemergent orthopaedic surgery. The changes in risk are a continuum, and we must take that into consideration when stratifying those parameters and adapting them to categorical variables. Therefore, they should be evaluated on a case-by-case basis and seen as relative considerations and not absolute, especially when it comes to patient risk and transmission risk because that are rapidly evolving areas of knowledge. Table 1 presents a suggested guideline for risk stratification based on external factors. Factors included in disease-independent factors are as follows:
Status of the epidemic. This depends on the local infection rate and containment. This is determined by federal and local authorities as well as the Centers for Disease Control and Prevention (CDC).
Hospital capacity. This relates to the hospital availability of resources (eg, equipment and personal) to care for patients with COVID-19 and other patients during the current time point and future projections, the expected progression of pandemic. This is determined by the local health systems and authorities that collect and provide resources as well as facilitate integration between different systems to distribute patient load.
ASCs availability. Theoretically, ASC settings not associated with active care of sick patients are a safer setting for patients. It is important to remember that personal protective equipment are a common good shared across the whole healthcare system (including hospitals and urgent cares); therefore, the availability of those personal protective equipment depends on the demands of centers taking care of patients with COVID-19.
Patient risk for COVID-19 complications. Older patients and patients with comorbidities are at higher risk for developing acute respiratory distress syndrome, need for intensive care unit (ICU) admission, and death. Therefore, they are at increased risk when entering healthcare facilities, more so in hospitals than ASCs, and during emergency states of the epidemic. In addition, if they develop complications, they further overload hospital resources. Also, patients who are already infected have increased risk of complications compared with noninfected peers.
ASA physical status classification system. Patients with comorbidities are at higher risk for developing acute respiratory distress syndrome, need for ICU admission, and death. In addition, they might need longer hospital stay (which further increases the risk of COVID-19 and non-COVID-19 complications) and uses more hospital resources that might be in a nonideal situation.
Transmission risk of COVID-19 assessment because of patient status. Patients who are known to be infected with COVID-19 are more likely to transmit the disease to healthcare providers (HCPs) and other patients, especially if they are symptomatic, and more so in severe forms of disease. For patients with unknown status because of lack of testing, the risk is influenced by the situation of the epidemic and close contacts. Surgeons can consider testing to better evaluate the risk, understanding that false positive and false negative exists.
Table 1.
Disease-independent Risk Assessment Table for Assisting in Surgical Decision-making
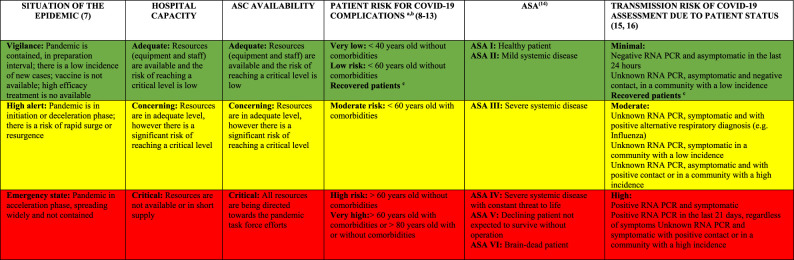 |
ASC = ambulatory surgical center, ASA = American Society of Anesthesiologists, IgG = immunoglobulin G, PCR = polymerase chain reaction
Patients already infected with COVID-19 have a higher risk when compared with noninfected peers.
Decreases when the situation of the epidemic and the hospital capacity improve to green.
Previously positive RNA PCR, currently symptomatic, 14 days after IgG positive, or those with resolved symptoms that started >21 days ago.
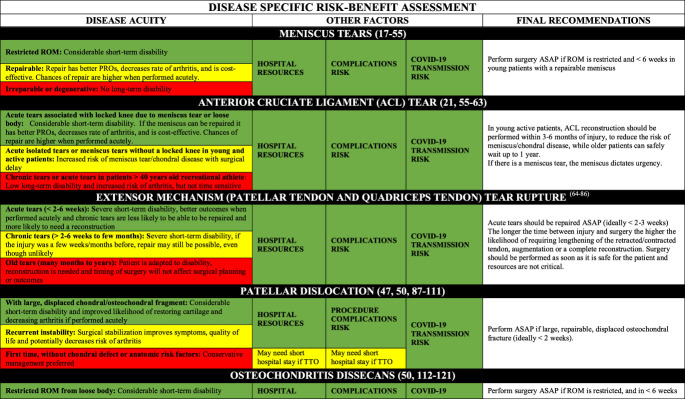
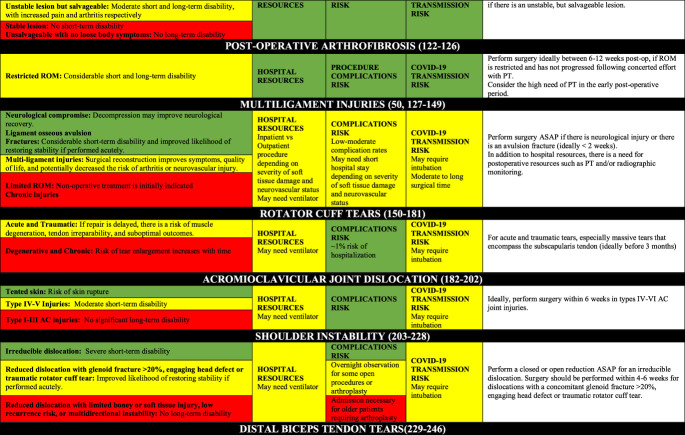
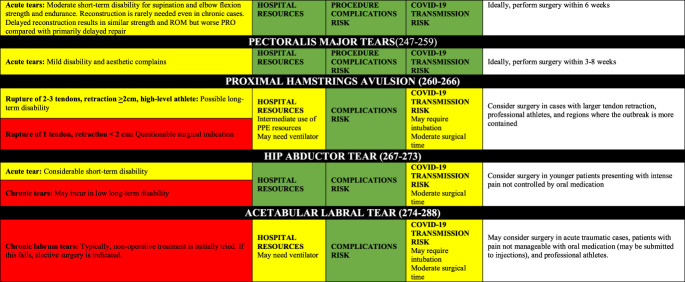
Disease-Specific Risk Assessment
Tables 2 contains the disease-specific risk-benefit assessment. For each pathology/procedure, the authors provide the following regarding the frequency and utilization of resources for each case: the incidence, number of surgeons/assistants, anesthesia methods, surgical time, cost, short- and long-term disability, cost-effectiveness, risk for COVID-19 complications, risk for surgical complications, postsurgical needs for social/home support. Appendix 1, http://links.lww.com/JG9/A84, contains a detailed review regarding disease-specific risk assessment.
Table 2.
Disease-Specific Risk Assessment Table for Assisting in Surgical Decision-making
|
AC = acromioclavicular, ACL = anterior cruciate ligament, ASAP = as soon as possible, PPE = personal protective equipment, PROs = patient-reported outcomes, PT = physical therapy, ROM = range of motion
In addition, the ideal timing for surgery depends on short-term and long-term outcomes, as well as time sensitivity. Of note, limb-threatening (eg, vascular compromise and compartment syndrome) and life-threatening (eg, open fractures and polytrauma) conditions are emergencies and are not included here. The nonemergent surgeries can be classified as the following:
Urgent surgery (green boxes): Strong evidence that any delay will result in inferior outcomes, or strong consensus that surgery within weeks is necessary for acceptable outcomes. Should be performed as soon as possible (a few days to a few weeks).
Time-sensitive surgery (yellow boxes): Moderate to strong evidence that delayed surgery contributes to inferior surgical outcomes (should be performed in a few weeks to a few months).
Not time-sensitive/elective surgery (red boxes): Absence of moderate to strong evidence of a notable relationship between surgical timing and outcomes, and the absence of consensus on delayed surgery on outcomes. They can be postponed a few months without major ramifications to the patient other than a lengthier time dealing with pain and life limitations/restrictions; however, it is important to highlight that they are necessary to improve patients' symptoms and quality of life and should not be postponed indefinitely.
Hospital resource use, procedure complications risk, and transmission of COVID-19 risk because the procedure for each procedure were summarized in Table 2.
In combining Tables 1 and 2, one can have a comprehensive understanding of the risks and benefits of proceeding with surgery. In addition, there are many important considerations orthopaedic surgeons must consider during the COVID-19 pandemic. We urge that those “low-risk geographic areas” to exercise caution because some states have reported few cases, but this may be because of slow pace of testing, where many more people are believed to be infected. There is a higher patient risk and associated liability in performing surgery in an “emergency state” area. In these areas, particularly if the hospital capacity is critical, only perform surgeries that are urgent (green boxed) and have other favorable green boxes.
Patient-Related Factors
If a patient has COVID-19, consider postponing surgery, decreasing the patient's risk of complications (surgery suppresses the immune system) and transmission to healthcare providers (HCPs) and other patients. Procedures and operations should be performed if delaying the procedure or operation is likely to prolong the patient's hospital stay while waiting for the surgery, increasing the likelihood of later hospital admission or causing harm, all increasing the risk of the patient acquiring COVID-19. In patients who are suspected to be infected with COVID-19 (eg, have typical symptoms, have close contact with infected persons, or live in a community with high incidence), consider testing RNA polymerase chain reaction (PCR) testing. This not only benefits the patient but also improves the hospital management/operations. For “gray area cases” (mostly yellow boxes), do no harm by assessing the patient's risk with your own judgement. No substitute exists for sound surgical judgement. For elective surgery (red-boxed diseases), surgery should wait until most other categories have normalized (green boxes). In addition, consideration should be given to the fact that there may be a large need for physical therapy postoperatively for an optimal result, which may not be available during certain phases of the pandemic.
Hospital Setting
If the patient needs to stay in the hospital, especially for many days, hospital capacity is more relevant than it is for outpatient surgery, for which the status of ASCs is more important. Inpatient procedures not only take on a bed that may be a scarce resource but it also places the patient at a higher risk for acquiring COVID-19. ASCs should have arrangements with a hospital if overnight stay for outpatient surgery becomes necessary because surgeons try to bring more patients to ASCs. In addition, it needs to be taken into consideration if it is anticipated that after surgery, the patient will need other resources, such as intensive care unit (ICU) bed and blood products.
Proceeding With Surgeries
Once the surgeon decides to proceed with surgery, all appropriate precautions should be taken. The CDC infection control guidelines can be found at https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control.html. The American College of Surgeons offers guidance on considerations for optimal surgical protection before, during, and after operations. For full guidelines, go to https://www.facs.org//media/files/covid19/considerations_optimum_surgeon_protection.ashx.
The evidence-based risk stratification presented in this study has the limitation of not being clinically validated, similar to the guidelines from the World Health Organization, CDC, or other institutions. However, we think we provide a comprehensive review of the literature that is optimal and the best available, considering the urgency and complexity of these times and the limited literature regarding this topic.
Conclusion
The medical urgency of a case cannot be defined solely on whether a case is on an elective surgery schedule. Plans for orthopaedic case triage should avoid blanket policies and instead depend on disease-specific data and expert opinion from qualified orthopaedic surgeons. Although COVID-19 is a risk to all, it is one of several competing risks for patients with functional limitations necessitating orthopaedic surgical care. Therefore, we provide guidelines based on an assimilation of all available disease-dependent, disease-independent, and logistical information to help guide surgeons and institutions in the decision-making process.
Footnotes
None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Hinckel, Mr. Baumann, Dr. Ejnisman, Dr. Cavinatto, Dr. Martusiewicz, Dr. Tanaka, Dr. Tompkins, Dr. Sherman, Dr. Chahla, Dr. Frank, Dr. Yamamoto, Dr. Bicos, Dr. Arendt, Dr. Fithian, and Dr. Farr.
References
- 1.World Health Organization (WHO): Coronavirus disease 2019 (COVID-19) Situation Report 2020. 2020. https://covid19.who.int/. Accessed May 2, 2020. [Google Scholar]
- 2.Sarac NJ, Sarac BA, Schoenbrunner AR, et al. : A review of state guidelines for elective orthopaedic procedures during the COVID-19 outbreak. J Bone Joint Surg Am 2020;102:942-945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White House: Opening Up America Again: Guidelines 2020. 2020. https://www.whitehouse.gov/openingamerica/. Accessed May 2, 2020. [Google Scholar]
- 4.Mi B, Chen L, Xiong Y, Xue H, Zhou W, Liu G: Characteristics and early prognosis of COVID-19 infection in fracture patients. J Bone Joint Surg Am 2020;705:750-758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Catellani F, Coscione A, D'Ambrosi R, Usai L, Roscitano C, Fiorentino G: Treatment of proximal femoral fragility fractures in patients with COVID-19 during the SARS-CoV-2 outbreak in Northern Italy. J Bone Joint Surg 2020;102:e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DePhillipo NN, Larson CM, O'Neill OR, LaPrade RF: Guidelines for ambulatory surgery centers for the care of surgically necessary/time-sensitive orthopaedic cases during the COVID-19 pandemic. J Bone Joint Surg Am 2020;102:933-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention: Pandemic Intervals Framework 2020. https://www.cdc.gov/flu/pandemic-resources/national-strategy/intervals-framework.html. Accessed May 2, 2020. [Google Scholar]
- 8.World Health Organization: Coronavirus disease 2019 (COVID-19) Situation Report – 81. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200410-sitrep-81-covid-19.pdf?sfvrsn=ca96eb84_2. Accessed May 2, 2020. [Google Scholar]
- 9.Verity R, Okell L, Dorigatti I, et al. : Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect Dis 2020;20:669-677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention: Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep 2020;69:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grasselli G, Zangrillo A, Zanella A, et al. : Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the lombardy region, Italy. JAMA 2020;323:1574-1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guan WJ, Ni ZY, Hu Y, et al. : Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou F, Yu T, Du R, et al. : Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020;395:1054-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Daabiss M: American Society of Anaesthesiologists physical status classification. Indian J Anaesth 2011;55:111-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Y, Yan LM, Wan L, et al. : Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis 2020;20:656-657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tan W, Lu Y, Zhang J, et al. : Viral kinetics and antibody responses in patients with COVID-19. medRxiv 2020.03.24.20042382; doi: 10.1101/2020.03.24.20042382. [DOI] [Google Scholar]
- 17.Maffulli N, Binfield PM, King JB, Good CJ: Acute haemarthrosis of the knee in athletes. A prospective study of 106 cases. J Bone Joint Surg Br 1993;75:945-949. [DOI] [PubMed] [Google Scholar]
- 18.Askenberger M, Ekström W, Finnbogason T, Janarv PM: Occult intra-articular knee injuries in children with hemarthrosis. Am J Sports Med 2014;42:1600-1606. [DOI] [PubMed] [Google Scholar]
- 19.Fithian DC, Paxton EW, Stone ML, et al. : Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114-1121. [DOI] [PubMed] [Google Scholar]
- 20.Nietosvaara Y, Aalto K, Kallio PE: Acute patellar dislocation in children: Incidence and associated osteochondral fractures. J Pediatr Orthop 1994;14:513-515. [DOI] [PubMed] [Google Scholar]
- 21.Lubowitz JH, Appleby D: Cost-effectiveness analysis of the most common orthopaedic surgery procedures: Knee arthroscopy and knee anterior cruciate ligament reconstruction. Arthroscopy 2011;27:1317-1322. [DOI] [PubMed] [Google Scholar]
- 22.Beamer BS, Walley KC, Okajima S, et al. : Changes in contact area in meniscus horizontal cleavage tears subjected to repair and resection. Arthroscopy 2017;33:617-624. [DOI] [PubMed] [Google Scholar]
- 23.Lee SJ, Aadalen KJ, Malaviya P, et al. : Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med 2006;34:1334-1344. [DOI] [PubMed] [Google Scholar]
- 24.LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF: Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am 2014;96:471-479. [DOI] [PubMed] [Google Scholar]
- 25.Geeslin AG, Civitarese D, Turnbull TL, Dornan GJ, Fuso FA, LaPrade RF: Influence of lateral meniscal posterior root avulsions and the meniscofemoral ligaments on tibiofemoral contact mechanics. Knee Surg Sports Traumatol Arthrosc 2016;24:1469-1477. [DOI] [PubMed] [Google Scholar]
- 26.Clark CR, Ogden JA: Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg Am 1983;65:538-547. [PubMed] [Google Scholar]
- 27.Kazemi M, Li LP, Savard P, Buschmann MD: Creep behavior of the intact and meniscectomy knee joints. J Mech Behav Biomed Mater 2011;4:1351-1358. [DOI] [PubMed] [Google Scholar]
- 28.Krych AJ, McIntosh AL, Voll AE, Stuart MJ, Dahm DL: Arthroscopic repair of isolated meniscal tears in patients 18 years and younger. Am J Sports Med 2008;36:1283-1289. [DOI] [PubMed] [Google Scholar]
- 29.Cannon WD, Jr, Vittori JM: The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med 1992;20:176-181. [DOI] [PubMed] [Google Scholar]
- 30.Padalecki JR, Jansson KS, Smith SD, et al. : Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: In situ pull-out repair restores derangement of joint mechanics. Am J Sports Med 2014;42:699-707. [DOI] [PubMed] [Google Scholar]
- 31.Bernard CD, Kennedy NI, Tagliero AJ, et al. : Medial meniscus posterior root tear treatment: A matched cohort comparison of nonoperative management, partial meniscectomy, and repair. Am J Sports Med 2020;48:128-132. [DOI] [PubMed] [Google Scholar]
- 32.Faucett SC, Geisler BP, Chahla J, et al. : Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: Clinical and economic effectiveness. Am J Sports Med 2019;47:762-769. [DOI] [PubMed] [Google Scholar]
- 33.Hohmann E, Angelo R, Arciero R, et al. : Degenerative meniscus lesions: An expert consensus statement using the modified Delphi technique. Arthroscopy 2020;36:501-512. [DOI] [PubMed] [Google Scholar]
- 34.Pihl K, Ensor J, Peat G, et al. : Wild goose chase—No predictable patient subgroups benefit from meniscal surgery: Patient-reported outcomes of 641 patients 1 year after surgery. Br J Sports Med 2020;54:13-22. [DOI] [PubMed] [Google Scholar]
- 35.Sonesson S, Kvist J, Yakob J, Hedevik H, Gauffin H: Knee arthroscopic surgery in middle-aged patients with meniscal symptoms: A 5-year follow-up of a prospective, randomized study. Orthop J Sports Med 2020;8:2325967119893920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Everhart JS, Higgins JD, Poland SG, Abouljoud MM, Flanigan DC: Meniscal repair in patients age 40 years and older: A systematic review of 11 studies and 148 patients. Knee 2018;25:1142-1150. [DOI] [PubMed] [Google Scholar]
- 37.Moatshe G, Cinque ME, Godin JA, Vap AR, Chahla J, LaPrade RF: Comparable outcomes after bucket-handle meniscal repair and vertical meniscal repair can be achieved at a minimum 2 years' follow-up. Am J Sports Med 2017;45:3104-3110. [DOI] [PubMed] [Google Scholar]
- 38.Cinque ME, Geeslin AG, Chahla J, Dornan GJ, LaPrade RF: Two-tunnel transtibial repair of radial meniscus tears produces comparable results to inside-out repair of vertical meniscus tears. Am J Sports Med 2017;45:2253-2259. [DOI] [PubMed] [Google Scholar]
- 39.Ardizzone CA, Houck DA, McCartney DW, Vidal AF, Frank RM: All-Inside repair of bucket-handle meniscal tears: Clinical outcomes and prognostic factors. Am J Sports Med 2020; Mar 20 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 40.LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS: Posterior meniscal root repairs: Outcomes of an anatomic transtibial pull-out technique. Am J Sports Med 2017;45:884-891. [DOI] [PubMed] [Google Scholar]
- 41.Dragoo JL, Konopka JA, Guzman RA, Segovia N, Kandil A, Pappas GP: Outcomes of arthroscopic all-inside repair versus observation in older patients with meniscus root tears. Am J Sports Med 2020;48:1127-1133. [DOI] [PubMed] [Google Scholar]
- 42.Kurzweil PR, Lynch NM, Coleman S, Kearney B: Repair of horizontal meniscus tears: A systematic review. Arthroscopy 2014;30:1513-1519. [DOI] [PubMed] [Google Scholar]
- 43.Thoreux P, Rety F, Nourissat G, et al. : Bucket-handle meniscal lesions: Magnetic resonance imaging criteria for reparability. Arthroscopy 2006;22:954-961. [DOI] [PubMed] [Google Scholar]
- 44.Felisaz PF, Alessandrino F, Perelli S, et al. : Role of MRI in predicting meniscal tear reparability. Skeletal Radiol 2017;46:1343-1351. [DOI] [PubMed] [Google Scholar]
- 45.Cinque ME, DePhillipo NN, Moatshe G, et al. : Clinical outcomes of inside-out meniscal repair according to anatomic zone of the meniscal tear. Orthop J Sports Med 2019;7:2325967119860806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van der Wal RJ, Thomassen BJ, Swen JW, van Arkel ER: Time interval between trauma and arthroscopic meniscal repair has No influence on clinical survival. J knee Surg 2016;29:436-442. [DOI] [PubMed] [Google Scholar]
- 47.Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: A systematic review. Am J Sports Med 2012;40:459-468. [DOI] [PubMed] [Google Scholar]
- 48.Hupperich A, Salzmann GM, Niemeyer P, et al. : What are the factors to affect outcome and healing of meniscus bucket handle tears? Arch Orthop Trauma Surg 2018;138:1365-1373. [DOI] [PubMed] [Google Scholar]
- 49.Feeley BT, Liu S, Garner AM, Zhang AL, Pietzsch JB: The cost-effectiveness of meniscal repair versus partial meniscectomy: A model-based projection for the United States. Knee 2016;23:674-680. [DOI] [PubMed] [Google Scholar]
- 50.Wu Z, McGoogan JM: Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; Feb 24 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 51.Small NC: Complications in arthroscopy: The knee and other joints: Committee on complications of the arthroscopy association of North America. Arthroscopy 1986;2:253-258. [PubMed] [Google Scholar]
- 52.Salzler MJ, Lin A, Miller CD, Herold S, Irrgang JJ, Harner CD: Complications after arthroscopic knee surgery. Am J Sports Med 2014;42:292-296. [DOI] [PubMed] [Google Scholar]
- 53.Jameson SS, Dowen D, James P, et al. : The burden of arthroscopy of the knee: A contemporary analysis of data from the English NHS. J Bone Joint Surg Br 2011;93:1327-1333. [DOI] [PubMed] [Google Scholar]
- 54.Kumaraswamy V, Ramaswamy AG, Sundar S, et al. : A new scoring system for prediction of meniscal repair in traumatic meniscal tears. Knee Surg Sports Traumatol Arthrosc 2019;27:3454-3460. [DOI] [PubMed] [Google Scholar]
- 55.Lester JD, Gorbaty JD, Odum SM, Rogers ME, Fleischli JE: The cost-effectiveness of meniscal repair versus partial meniscectomy in the setting of anterior cruciate ligament reconstruction. Arthroscopy 2018;34:2614-2620. [DOI] [PubMed] [Google Scholar]
- 56.Farnworth LR, Lemay DE, Wooldridge T, et al. : A comparison of operative times in arthroscopic ACL reconstruction between orthopaedic faculty and residents: The financial impact of orthopaedic surgical training in the operating room. Iowa Orthop J 2001;21:31-35. [PMC free article] [PubMed] [Google Scholar]
- 57.Wyatt RW, Inacio MC, Liddle KD, Maletis GB: Prevalence and incidence of cartilage injuries and meniscus tears in patients who underwent both primary and revision anterior cruciate ligament reconstructions. Am J Sports Med 2014;42:1841-1846. [DOI] [PubMed] [Google Scholar]
- 58.Chhadia AM, Inacio MC, Maletis GB, Csintalan RP, Davis BR, Funahashi TT. Are meniscus and cartilage injuries related to time to anterior cruciate ligament reconstruction? Am J Sports Med 2011;39:1894-1899. [DOI] [PubMed] [Google Scholar]
- 59.Orthoguidelines. When ACL reconstruction is indicated, moderate evidence supports reconstruction within five months of injury to protect the articular cartilage and menisci. http://www.orthoguidelines.org/go/cpg/detail.cfm?id=1251. Accessed May 2, 2020. [Google Scholar]
- 60.Jarvela T, Moisala AS, Sihvonen R, Jarvela S, Kannus P, Jarvinen M: Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: Prospective, randomized, clinical study with 2-year results. Am J Sports Med 2008;36:290-297. [DOI] [PubMed] [Google Scholar]
- 61.Stone JA, Perrone GS, Nezwek TA, et al. : Delayed ACL reconstruction in patients >/=40 years of age is associated with increased risk of medial meniscal injury at 1 year. Am J Sports Med 2019;47:584-589. [DOI] [PubMed] [Google Scholar]
- 62.Stewart BA, Momaya AM, Silverstein MD, Lintner D: The cost-effectiveness of anterior cruciate ligament reconstruction in competitive athletes. Am J Sports Med 2017;45:23-33. [DOI] [PubMed] [Google Scholar]
- 63.Abram SGF, Judge A, Beard DJ, Price AJ: Rates of adverse outcomes and revision surgery after anterior cruciate ligament reconstruction: A study of 104,255 procedures using the National Hospital Episode Statistics Database for England, UK. Am J Sports Med 2019;47:2533-2542. [DOI] [PubMed] [Google Scholar]
- 64.Clayton RA, Court-Brown CM: The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury 2008;39:1338-1344. [DOI] [PubMed] [Google Scholar]
- 65.Saragaglia D, Pison A, Rubens-Duval B: Acute and old ruptures of the extensor apparatus of the knee in adults (excluding knee replacement). Orthop Traumatol Surg Res 2013;99(suppl 1):S67-S76. [DOI] [PubMed] [Google Scholar]
- 66.Ilan DI, Tejwani N, Keschner M, Leibman M: Quadriceps tendon rupture. J Am Acad Orthop Surg 2003;11:192-200. [DOI] [PubMed] [Google Scholar]
- 67.Boudissa M, Roudet A, Rubens-Duval B, Chaussard C, Saragaglia D: Acute quadriceps tendon ruptures: A series of 50 knees with an average follow-up of more than 6 years. Orthopaedics Traumatol Surg Res 2014;100:213-216. [DOI] [PubMed] [Google Scholar]
- 68.Matava MJ. Patellar tendon ruptures. J Am Acad Orthop Surg 1996;4:287-296. [DOI] [PubMed] [Google Scholar]
- 69.Negrin LL, Nemecek E, Hajdu S: Extensor mechanism ruptures of the knee: Differences in demographic data and long-term outcome after surgical treatment. Injury 2015;46:1957-1963. [DOI] [PubMed] [Google Scholar]
- 70.Serino J, Mohamadi A, Orman S, et al. : Comparison of adverse events and postoperative mobilization following knee extensor mechanism rupture repair: A systematic review and network meta-analysis. Injury 2017;48:2793-2799. [DOI] [PubMed] [Google Scholar]
- 71.Ecker ML, Lotke PA, Glazer RM: Late reconstruction of the patellar tendon. J Bone Joint Surg Am 1979;61:884-886. [PubMed] [Google Scholar]
- 72.Siwek CW, Rao JP: Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am: 1981;63:932-937. [PubMed] [Google Scholar]
- 73.Gilmore JH, Clayton-Smith ZJ, Aguilar M, Pneumaticos SG, Giannoudis PV: Reconstruction techniques and clinical results of patellar tendon ruptures: Evidence today. Knee 2015;22:148-155. [DOI] [PubMed] [Google Scholar]
- 74.Greis PE, Lahav A, Holmstrom MC: Surgical treatment options for patella tendon rupture, part II: Chronic. Orthopedics 2005;28:765-769; quiz 70-1. [DOI] [PubMed] [Google Scholar]
- 75.Guido W, Christian H, Elmar H, Elisabeth A, Christian F: Treatment of patella baja by a modified Z-plasty. Knee Surg Sports Traumatol Arthrosc 2016;24:2943-2947. [DOI] [PubMed] [Google Scholar]
- 76.Harato K, Kobayashi S, Udagawa K, et al. : Surgical technique to bring down the patellar height and to reconstruct the tendon for chronic patellar tendon rupture. Arthrosc Tech 2017;6:e1897-e901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nguene-Nyemb AG, Huten D, Ropars M: Chronic patellar tendon rupture reconstruction with a semitendinosus autograft. Orthopaedics Traumatol Surg Res 2011;97:447-450. [DOI] [PubMed] [Google Scholar]
- 78.Scuderi C: Ruptures of the quadriceps tendon; study of twenty tendon ruptures. Am J Surg 1958;95:626-634. [DOI] [PubMed] [Google Scholar]
- 79.Maffulli N, Del Buono A, Loppini M, Denaro V: Ipsilateral hamstring tendon graft reconstruction for chronic patellar tendon ruptures: Average 5.8-year follow-up. J Bone Joint Surg Am 2013;95:e1231-e1236. [DOI] [PubMed] [Google Scholar]
- 80.Wiegand N, Naumov I, Vamhidy L, Warta V, Than P: Reconstruction of the patellar tendon using a Y-shaped flap folded back from the vastus lateralis fascia. Knee 2013;20:139-143. [DOI] [PubMed] [Google Scholar]
- 81.Konrath GA, Chen D, Lock T, et al. : Outcomes following repair of quadriceps tendon ruptures. J Orthop Trauma 1998;12:273-279. [DOI] [PubMed] [Google Scholar]
- 82.Miskew DB, Pearson RL, Pankovich AM: Mersilene strip suture in repair of disruptions of the quadriceps and patellar tendons. J Trauma 1980;20:867-872. [DOI] [PubMed] [Google Scholar]
- 83.Rougraff BT, Reeck CC, Essenmacher J: Complete quadriceps tendon ruptures. Orthopedics 1996;19:509-514. [PubMed] [Google Scholar]
- 84.Belhaj K, El Hyaoui H, Tahir A, et al. : Long-term functional outcomes after primary surgical repair of acute and chronic patellar tendon rupture: Series of 25 patients. Ann Phys Rehabil Med 2017;60:244-248. [DOI] [PubMed] [Google Scholar]
- 85.Kelly DW, Carter VS, Jobe FW, Kerlan RK: Patellar and quadriceps tendon ruptures—Jumper's knee. Am J Sports Med 1984;12:375-380. [DOI] [PubMed] [Google Scholar]
- 86.Bushnell BD, Whitener GB, Rubright JH, Creighton RA, Logel KJ, Wood ML: The use of suture anchors to repair the ruptured quadriceps tendon. J Orthop Trauma 2007;21:407-413. [DOI] [PubMed] [Google Scholar]
- 87.Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ: Incidence of first-time lateral patellar dislocation: A 21-year population-based study. Sports Health 2018;10:146-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gravesen KS, Kallemose T, Blønd L, Troelsen A, Barfod KW: High incidence of acute and recurrent patellar dislocations: A retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg Sports Traumatol Arthrosc 2018;26:1204-1209. [DOI] [PubMed] [Google Scholar]
- 89.Zhang GY, Ding HY, Li EM, et al. : Incidence of second-time lateral patellar dislocation is associated with anatomic factors, age and injury patterns of medial patellofemoral ligament in first-time lateral patellar dislocation: A prospective magnetic resonance imaging study with 5-year follow-up. Knee Surg Sports Traumatol Arthrosc 2019;27:197-205. [DOI] [PubMed] [Google Scholar]
- 90.Christensen TC, Sanders TL, Pareek A, Mohan R, Dahm DL, Krych AJ: Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am J Sports Med 2017;45:2105-2110. [DOI] [PubMed] [Google Scholar]
- 91.Xi H, Peng G, Chou SH: Finite-volume lattice Boltzmann schemes in two and three dimensions. Phys Rev E Stat Phys Plasmas Fluids Relat Interdiscip Topics 1999;60:3380-3388. [DOI] [PubMed] [Google Scholar]
- 92.Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA: Factors associated with an increased risk of recurrence after a first-time patellar dislocation: A systematic review and meta-analysis. Am J Sports Med 2020;48:2552-2562. [DOI] [PubMed] [Google Scholar]
- 93.Previtali D, Roumenov SM, Pagliazzi G, Filardo G, Zaffagnini S, Candrian C: Recurrent patellar dislocations without untreated predisposing factors: MPFL reconstruction vs other medial soft tissue surgical techniques—A meta-analysis. Arthroscopy 2020;36:1725-1734. [DOI] [PubMed] [Google Scholar]
- 94.Zaffagnini S, Previtali D, Tamborini S, Pagliazzi G, Filardo G, Candrian C: Recurrent patellar dislocations: Trochleoplasty improves the results of medial patellofemoral ligament surgery only in severe trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 2019;27:3599-3613. [DOI] [PubMed] [Google Scholar]
- 95.Neri T, Parker DA, Beach A, et al. : Medial patellofemoral ligament reconstruction with or without tibial tubercle transfer is an effective treatment for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2019;27:805-813. [DOI] [PubMed] [Google Scholar]
- 96.Sappey-Marinier E, Sonnery-Cottet B, O'Loughlin P, et al. : Clinical outcomes and predictive factors for failure with isolated MPFL reconstruction for recurrent patellar instability: A series of 211 reconstructions with a minimum follow-up of 3 years. Am J Sports Med. 2019;47:1323-1330. [DOI] [PubMed] [Google Scholar]
- 97.Hiemstra LA, Kerslake S, Loewen M, Lafave M: Effect of trochlear dysplasia on outcomes after isolated soft tissue stabilization for patellar instability. Am J Sports Med 2016;44:1515-1523. [DOI] [PubMed] [Google Scholar]
- 98.Jaquith BP, Parikh SN: Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. J Pediatr Orthop 2017;37:484-490. [DOI] [PubMed] [Google Scholar]
- 99.Chotel F, Knorr G, Simian E, Dubrana F, Versier G, French Arthroscopy S: Knee osteochondral fractures in skeletally immature patients: French multicenter study. Orthopaedics Traumatol Surg Res 2011;97(suppl 8):S154-S159. [DOI] [PubMed] [Google Scholar]
- 100.Kramer DE, Pace JL: Acute traumatic and sports-related osteochondral injury of the pediatric knee. Orthop Clin North Am 2012;43:227-236. [DOI] [PubMed] [Google Scholar]
- 101.Fabricant PD, Yen YM, Kramer DE, et al. : Fixation of traumatic chondral-only fragments of the knee in pediatric and adolescent athletes: A retrospective multicenter report. Orthop J Sports Med 2018;6:2325967117753140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Howells NR, Barnett AJ, Ahearn N, Ansari A, Eldridge JD. Medial patellofemoral ligament reconstruction: A prospective outcome assessment of a large single centre series. J Bone Joint Surg Br 2012;94:1202-1208. [DOI] [PubMed] [Google Scholar]
- 103.Nwachukwu BU, So C, Schairer WW, et al. : Economic decision model for first-time traumatic patellar dislocations in adolescents. Am J Sports Med 2017;45:2267-2275. [DOI] [PubMed] [Google Scholar]
- 104.Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C: A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 2012;40:1916-1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Parikh SN, Nathan ST, Wall EJ, Eismann EA: Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med 2013;41:1030-1038. [DOI] [PubMed] [Google Scholar]
- 106.Tanaka MJ, Bollier MJ, Andrish JT, Fulkerson JP, Cosgarea AJ: Complications of medial patellofemoral ligament reconstruction: Common technical errors and factors for success: AAOS exhibit selection. J Bone Joint Surg Am 2012;94:e87. [DOI] [PubMed] [Google Scholar]
- 107.Johnson AA, Cosgarea AJ, Wolfe EL: Complications of tibial tuberosity osteotomy. Sports Med Arthrosc Rev 2017;25:85-91. [DOI] [PubMed] [Google Scholar]
- 108.Johnson AA, Wolfe EL, Mintz DN, Demehri S, Shubin Stein BE, Cosgarea AJ: Complications after tibial tuberosity osteotomy: Association with screw size and concomitant distalization. Orthopaedic J Sports Med 2018;6:2325967118803614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tanaka MJ, Munch JL, Slater AJ, Nguyen JT, Shubin Stein BE: Incidence of deep venous thrombosis after tibial tubercle osteotomy: A single case series study. Orthop J Sports Med 2014;2:2325967114544457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Aydoğmuş S, Duymuş TM, Keçeci T: An unexpected complication after headless compression screw fixation of an osteochondral fracture of patella. Case Rep Orthop 2016;2016:7290104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sanders TL, Pareek A, Johnson NR, Stuart MJ, Dahm DL, Krych AJ: Patellofemoral arthritis after lateral patellar dislocation: A matched population-based analysis. Am J Sports Med 2017;45:1012-1017. [DOI] [PubMed] [Google Scholar]
- 112.Weiss JM, Shea KG, Jacobs JC, Jr, et al. : Incidence of osteochondritis dissecans in adults. Am J Sports Med 2018;46:1592-1595. [DOI] [PubMed] [Google Scholar]
- 113.Pareek A, Sanders TL, Wu IT, Larson DR, Saris DBF, Krych AJ: Incidence of symptomatic osteochondritis dissecans lesions of the knee: A population-based study in olmsted county. Osteoarthritis and cartilage/OARS, Osteoarthritis Res Soc 2017;25:1663-1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sanders TL, Pareek A, Obey MR, et al. : High rate of osteoarthritis after osteochondritis dissecans fragment excision compared with surgical restoration at a mean 16-year follow-up. Am J Sports Med 2017;45:1799-1805. [DOI] [PubMed] [Google Scholar]
- 115.Wang K, Waterman B, Dean R, et al. : The influence of physeal status on rate of reoperation after arthroscopic screw fixation for symptomatic osteochondritis dissecans of the knee. Arthroscopy 2020;36:785-794. [DOI] [PubMed] [Google Scholar]
- 116.Perelli S, Molina Romoli AR, Costa-Paz M, Erquicia JI, Gelber PE, Monllau JC: Internal fixation of osteochondritis dissecans of the knee leads to good long-term outcomes and high degree of healing without differences between fixation devices. J Clin Med 2019;8:1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wall EJ, Polousky JD, Shea KG, et al. : Novel radiographic feature classification of knee osteochondritis dissecans: A multicenter reliability study. Am J Sports Med 2015;43:303-309. [DOI] [PubMed] [Google Scholar]
- 118.Adjei J, Nwachukwu BU, Zhang Y, et al. : Health state utilities in children and adolescents with osteochondritis dissecans of the knee. Orthop J Sports Med 2019;7:2325967119886591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kramer DE, Yen YM, Simoni MK, et al. : Surgical management of osteochondritis dissecans lesions of the patella and trochlea in the pediatric and adolescent population. Am J Sports Med 2015;43:654-662. [DOI] [PubMed] [Google Scholar]
- 120.Kocher MS, Czarnecki JJ, Andersen JS, Micheli LJ: Internal fixation of juvenile osteochondritis dissecans lesions of the knee. Am J Sports Med 2007;35:712-718. [DOI] [PubMed] [Google Scholar]
- 121.Kocher MS, Micheli LJ, Yaniv M, Zurakowski D, Ames A, Adrignolo AA: Functional and radiographic outcome of juvenile osteochondritis dissecans of the knee treated with transarticular arthroscopic drilling. Am J Sports Med 2001;29:562-566. [DOI] [PubMed] [Google Scholar]
- 122.Sanders TL, Kremers HM, Bryan AJ, Kremers WK, Stuart MJ, Krych AJ: Procedural intervention for arthrofibrosis after ACL reconstruction: Trends over two decades. Knee Surg Sports Traumatol Arthrosc 2017;25:532-537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M: Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med 1991;19:332-336. [DOI] [PubMed] [Google Scholar]
- 124.Ekhtiari S, Horner NS, de Sa D, et al. : Arthrofibrosis after ACL reconstruction is best treated in a step-wise approach with early recognition and intervention: A systematic review. Knee Surg Sports Traumatol Arthrosc 2017;25:3929-3937. [DOI] [PubMed] [Google Scholar]
- 125.Mayr HO, Brandt CM, Weig T, et al. : Long-term results of arthroscopic arthrolysis for arthrofibrosis after anterior cruciate ligament reconstruction. Arthroscopy 2017;33:408-414. [DOI] [PubMed] [Google Scholar]
- 126.Fabricant PD, Tepolt FA, Kocher MS: Range of motion improvement following surgical management of knee arthrofibrosis in children and adolescents. J Pediatr Orthop 2018;38:e495-e500. [DOI] [PubMed] [Google Scholar]
- 127.Arom GA, Yeranosian MG, Petrigliano FA, Terrell RD, McAllister DR: The changing demographics of knee dislocation: A retrospective database review. Clin Orthop Relat Res 2014;472:2609-2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wascher DC, Dvirnak PC, DeCoster TA: Knee dislocation: Initial assessment and implications for treatment. J Orthop Trauma 1997;11:525-529. [DOI] [PubMed] [Google Scholar]
- 129.Wascher DC: High-velocity knee dislocation with vascular injury. Treatment principles. Clin Sports Med 2000;19:457-477. [DOI] [PubMed] [Google Scholar]
- 130.Moatshe G, Dornan GJ, Loken S, Ludvigsen TC, LaPrade RF, Engebretsen L: Demographics and injuries associated with knee dislocation: A prospective review of 303 patients. Orthop J Sports Med 2017;5:2325967117706521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Shields L, Mital M, Cave EF: Complete dislocation of the knee: Experience at the Massachusetts general hospital. J Trauma 1969;9:192-215. [PubMed] [Google Scholar]
- 132.Dedmond BT, Almekinders LC: Operative versus nonoperative treatment of knee dislocations: A meta-analysis. Am J Knee Surg 2001;14:33-38. [PubMed] [Google Scholar]
- 133.Richter M, Bosch U, Wippermann B, Hofmann A, Krettek C: Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med 2002;30:718-727. [DOI] [PubMed] [Google Scholar]
- 134.Peskun CJ, Whelan DB: Outcomes of operative and nonoperative treatment of multiligament knee injuries: An evidence-based review. Sports Med Arthrosc Rev 2011;19:167-173. [DOI] [PubMed] [Google Scholar]
- 135.Caborn DN, Johnson BM: The natural history of the anterior cruciate ligament-deficient knee. A review. Clin Sports Med 1993;12:625-636. [PubMed] [Google Scholar]
- 136.Maffulli N, Binfield PM, King JB: Articular cartilage lesions in the symptomatic anterior cruciate ligament-deficient knee. Arthroscopy 2003;19:685-690. [DOI] [PubMed] [Google Scholar]
- 137.Potter HG, Jain SK, Ma Y, Black BR, Fung S, Lyman S: Cartilage injury after acute, isolated anterior cruciate ligament tear: Immediate and longitudinal effect with clinical/MRI follow-up. Am J Sports Med 2012;40:276-285. [DOI] [PubMed] [Google Scholar]
- 138.Tandogan RN, Taser O, Kayaalp A, et al. : Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: Relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc 2004;12:262-270. [DOI] [PubMed] [Google Scholar]
- 139.Moatshe G, Dornan GJ, Ludvigsen T, Loken S, LaPrade RF, Engebretsen L: High prevalence of knee osteoarthritis at a minimum 10-year follow-up after knee dislocation surgery. Knee Surg Sports Traumatol Arthrosc 2017;25:3914-3922. [DOI] [PubMed] [Google Scholar]
- 140.Neuman P, Englund M, Kostogiannis I, Friden T, Roos H, Dahlberg LE: Prevalence of tibiofemoral osteoarthritis 15 years after nonoperative treatment of anterior cruciate ligament injury: A prospective cohort study. Am J Sports Med 2008;36:1717-1725. [DOI] [PubMed] [Google Scholar]
- 141.Risberg MA, Oiestad BE, Gunderson R, et al. : Changes in knee osteoarthritis, symptoms, and function after anterior cruciate ligament reconstruction: A 20-year prospective follow-up study. Am J Sports Med 2016;44:1215-1224. [DOI] [PubMed] [Google Scholar]
- 142.Plancher KD, Siliski J: Long-term functional results and complications in patients with knee dislocations. J Knee Surg 2008;21:261-268. [DOI] [PubMed] [Google Scholar]
- 143.Engebretsen L, Risberg MA, Robertson B, Ludvigsen TC, Johansen S: Outcome after knee dislocations: A 2-9 years follow-up of 85 consecutive patients. Knee Surg Sports Traumatol Arthrosc 2009;17:1013-1026. [DOI] [PubMed] [Google Scholar]
- 144.Mariani PP, Santoriello P, Iannone S, Condello V, Adriani E: Comparison of surgical treatments for knee dislocation. Am J Knee Surg 1999;12:214-221. [PubMed] [Google Scholar]
- 145.Fanelli GC, Giannotti BF, Edson CJ: Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction. Arthroscopy 1996;12:521-530. [DOI] [PubMed] [Google Scholar]
- 146.Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ: Surgical management of knee dislocations. J Bone Joint Surg Am 2004;86-a:262-273. [DOI] [PubMed] [Google Scholar]
- 147.Levy BA, Dajani KA, Whelan DB, et al. : Decision making in the multiligament-injured knee: An evidence-based systematic review. Arthrosc 2009;25:430-438. [DOI] [PubMed] [Google Scholar]
- 148.Hirschmann MT, Zimmermann N, Rychen T, et al. : Clinical and radiological outcomes after management of traumatic knee dislocation by open single stage complete reconstruction/repair. BMC Musculoskelet Disord 2010;11:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Werner BC, Gwathmey FW, Jr, Higgins ST, Hart JM, Miller MD: Ultra-low velocity knee dislocations: Patient characteristics, complications, and outcomes. Am J Sports Med 2014;42:358-363. [DOI] [PubMed] [Google Scholar]
- 150.Aagaard KE, Abu-Zidan F, Lunsjo K: High incidence of acute full-thickness rotator cuff tears. Acta Orthop 2015;86:558-562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 2010;19:116-120. [DOI] [PubMed] [Google Scholar]
- 152.Churchill RS, Ghorai JK: Total cost and operating room time comparison of rotator cuff repair techniques at low, intermediate, and high volume centers: Mini-open versus all-arthroscopic. J Shoulder Elbow Surg 2010;19:716-721. [DOI] [PubMed] [Google Scholar]
- 153.Narvy SJ, Didinger TC, Lehoang D, et al. : Direct cost analysis of outpatient Arthroscopic rotator cuff repair in medicare and non-medicare populations. Orthop J Sports Med 2016;4:2325967116668829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Li L, Bokshan SL, Ready LV, Owens BD: The primary cost drivers of arthroscopic rotator cuff repair surgery: A cost-minimization analysis of 40,618 cases. J Shoulder Elbow Surg 2019;28:1977-1982. [DOI] [PubMed] [Google Scholar]
- 155.Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA: The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am 2006;88:1699-1704. [DOI] [PubMed] [Google Scholar]
- 156.Spross C, Behrens G, Dietrich TJ, et al. : Early arthroscopic repair of acute traumatic massive rotator cuff tears leads to reliable reversal of pseudoparesis: Clinical and radiographic outcome. Arthroscopy 2019;35:343-350. [DOI] [PubMed] [Google Scholar]
- 157.Hantes ME, Karidakis GK, Vlychou M, Varitimidis S, Dailiana Z, Malizos KN: A comparison of early versus delayed repair of traumatic rotator cuff tears. Knee Surg Sports Traumatol Arthrosc 2011;19:1766-1770. [DOI] [PubMed] [Google Scholar]
- 158.Haviv B, Rutenberg TF, Bronak S, Yassin M: Arthroscopic rotator cuff surgery following shoulder trauma improves outcome despite additional pathologies and slow recovery. Knee Surg Sports Traumatol Arthrosc 2018;26:3804-3809. [DOI] [PubMed] [Google Scholar]
- 159.Keener JD, Galatz LM, Teefey SA, et al. : A prospective evaluation of survivorship of asymptomatic degenerative rotator cuff tears. J Bone Joint Surg Am 2015;97:89-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Maman E, Harris C, White L, Tomlinson G, Shashank M, Boynton E: Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am 2009;91:1898-1906. [DOI] [PubMed] [Google Scholar]
- 161.Safran O, Schroeder J, Bloom R, Weil Y, Milgrom C. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med 2011;39:710-714. [DOI] [PubMed] [Google Scholar]
- 162.Moosmayer S, Tariq R, Stiris M, Smith HJ: The natural history of asymptomatic rotator cuff tears: A three-year follow-up of fifty cases. J Bone Joint Surg Am 1997;344:275-283. [DOI] [PubMed] [Google Scholar]
- 163.Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F: Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res 1997;344:275-283. [PubMed] [Google Scholar]
- 164.Chalmers PN, Granger E, Nelson R, Yoo M, Tashjian RZ: Factors affecting cost, outcomes, and tendon healing after arthroscopic rotator cuff repair. Arthroscopy 2018;34:1393-1400. [DOI] [PubMed] [Google Scholar]
- 165.Safran O, Derwin KA, Powell K, Iannotti JP. Changes in rotator cuff muscle volume, fat content, and passive mechanics after chronic detachment in a canine model. J Bone Joint Surg Am. 2005;87:2662-2670. [DOI] [PubMed] [Google Scholar]
- 166.Heikel HV: Rupture of the rotator cuff of the shoulder. Experiences of surgical treatment. Acta Orthop Scand 1968;39:477-492. [DOI] [PubMed] [Google Scholar]
- 167.Warner JJ, Higgins L, Parsons IM, IV, Dowdy P: Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg 2001;10:37-46. [DOI] [PubMed] [Google Scholar]
- 168.Kreuz PC, Remiger A, Erggelet C, Hinterwimmer S, Niemeyer P, Gachter A: Isolated and combined tears of the subscapularis tendon. Am J Sports Med 2005;33:1831-1837. [DOI] [PubMed] [Google Scholar]
- 169.Petersen SA, Murphy TP: The timing of rotator cuff repair for the restoration of function. J Shoulder Elbow Surg 2011;20:62-68. [DOI] [PubMed] [Google Scholar]
- 170.Duncan NS, Booker SJ, Gooding BW, Geoghegan J, Wallace WA, Manning PA: Surgery within 6 months of an acute rotator cuff tear significantly improves outcome. J Shoulder Elbow Surg 2015;24:1876-1880. [DOI] [PubMed] [Google Scholar]
- 171.Bassett RW, Cofield RH: Acute tears of the rotator cuff. The timing of surgical repair. Clin Orthop Relat Res 1983;175:18-24. [PubMed] [Google Scholar]
- 172.Mukovozov I, Byun S, Farrokhyar F, Wong I: Time to surgery in acute rotator cufftear: A systematic review. Bone Joint Res 2013;2:122-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Bjornsson HC, Norlin R, Johansson K, Adolfsson LE: The influence of age, delay of repair, and tendon involvement in acute rotator cuff tears: Structural and clinical outcomes after repair of 42 shoulders. Acta Orthop 2011;82:187-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Namdari S, Henn RF, III, Green A: Traumatic anterosuperior rotator cuff tears: The outcome of open surgical repair. J Bone Joint Surg Am 2008;90:1906-1913. [DOI] [PubMed] [Google Scholar]
- 175.Mather RC, III, Koenig L, Acevedo D, et al. : The societal and economic value of rotator cuff repair. J Bone Joint Surg Am 2013;95:1993-2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL: National trends in rotator cuff repair. J Bone Joint Surg Am 2012;94:227-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Traven SA, Horn RW, Reeves RA, Walton ZJ, Woolf SK, Slone HS: The 5-factor modified frailty index predicts complications, hospital admission, and mortality following arthroscopic rotator cuff repair. Arthroscopy 2020;36:383-388. [DOI] [PubMed] [Google Scholar]
- 178.Kosinski LR, Gil JA, Durand WM, DeFroda SF, Owens BD, Daniels AH: 30-Day readmission following outpatient rotator cuff repair: An analysis of 18,061 cases. Phys Sportsmed 2018;46:466-470. [DOI] [PubMed] [Google Scholar]
- 179.Padaki AS, Boddapati V, Mathew J, Ahmad CS, Jobin CM, Levine WN: The effect of age on short-term postoperative complications following arthroscopic rotator cuff repair. JSES Open Access 2019;3:194-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Dickinson RN, Kuhn JE, Bergner JL, Rizzone KH: A systematic review of cost-effective treatment of postoperative rotator cuff repairs. J Shoulder Elbow Surg 2017;26:915-922. [DOI] [PubMed] [Google Scholar]
- 181.Keener JD, Galatz LM, Stobbs-Cucchi G, Patton R, Yamaguchi K: Rehabilitation following arthroscopic rotator cuff repair: A prospective randomized trial of immobilization compared with early motion. J Bone Joint Surg Am 2014;96:11-19. [DOI] [PubMed] [Google Scholar]
- 182.Gorbaty JD, Hsu JE, Gee AO: Classifications in brief: Rockwood classification of acromioclavicular joint separations. Clin Orthop Relat Res 2017;475:283-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Smith TO, Chester R, Pearse EO, Hing CB: Operative versus non-operative management following rockwood grade III acromioclavicular separation: A meta-analysis of the current evidence base. J OrthopTraumatol 2011;12:19-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Deans CF, Gentile JM, Tao MA: Acromioclavicular joint injuries in overhead athletes: A concise review of injury mechanisms, treatment options, and outcomes. Curr Rev Musculoskelet Med 2019;12:80-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Tauber M: Management of acute acromioclavicular joint dislocations: Current concepts. Arch Orthop Trauma Surg 2013;133:985-995. [DOI] [PubMed] [Google Scholar]
- 186.Beitzel K, Cote MP, Apostolakos J, et al. : Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy 2013;29:387-397. [DOI] [PubMed] [Google Scholar]
- 187.Bannister GC, Wallace WA, Stableforth PG, Hutson MA: The management of acute acromioclavicular dislocation. A randomised prospective controlled trial. J Bone Joint Surg Br 1989;71:848-850. [DOI] [PubMed] [Google Scholar]
- 188.Wang YC, Yong MA, Wei-Zhong YU, Wang H: Surgical treatment of acute Rockwood III acromioclavicular dislocations-Comparative study between two flip-button techniques. Sci Rep: 2020;10:4447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Abdelrahman AA, Ibrahim A, Abdelghaffar K, Ghandour TM, Eldib D: Open versus modified arthroscopic treatment of acute acromioclavicular dislocation using a single tight rope: Randomized comparative study of clinical outcome and cost-effectiveness. J Shoulder Elbow Surg 2019;28:2090-2097. [DOI] [PubMed] [Google Scholar]
- 190.Horst K, Dienstknecht T, Pishnamaz M, Sellei RM, Kobbe P, Pape HC: Operative treatment of acute acromioclavicular joint injuries graded rockwood III and IV: Risks and benefits in tight rope technique vs. k-wire fixation. Patient Saf Surg 2013;7:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Dias JJ, Steingold RF, Richardson RA, Tesfayohannes B, Gregg PJ: The conservative treatment of acromioclavicular dislocation. Review after five years. J bone Joint Surg Br 1987;69:719-722. [DOI] [PubMed] [Google Scholar]
- 192.Virk MS, Apostolakos J, Cote MP, Baker B, Beitzel K, Mazzocca AD: Operative and nonoperative treatment of acromioclavicular dislocation: A critical analysis review. JBJS Rev 2015;3:1-12. [DOI] [PubMed] [Google Scholar]
- 193.Rawes ML, Dias JJ: Long-term results of conservative treatment for acromioclavicular dislocation. J Bone Joint Surg Br 1996;78:410-412. [PubMed] [Google Scholar]
- 194.Reid D, Polson K, Johnson L: Acromioclavicular joint separations grades I-III: A review of the literature and development of best practice guidelines. Sports Med 2012;42:681-696. [DOI] [PubMed] [Google Scholar]
- 195.Johansen JA, Grutter PW, McFarland EG, Petersen SA: Acromioclavicular joint injuries: Indications for treatment and treatment options. J Shoulder Elbow Surg 2011;20(suppl 2):S70-S82. [DOI] [PubMed] [Google Scholar]
- 196.Rolf O, Hann von Weyhern A, Ewers A, Boehm TD, Gohlke F: Acromioclavicular dislocation rockwood III-V: Results of early versus delayed surgical treatment. Arch orthopaedic Trauma Surg 2008;128:1153-1157. [DOI] [PubMed] [Google Scholar]
- 197.Weinstein DM, McCann PD, McIlveen SJ, Flatow EL, Bigliani LU: Surgical treatment of complete acromioclavicular dislocations. Am J Sports Med 1995;23:324-331. [DOI] [PubMed] [Google Scholar]
- 198.Dumontier C, Sautet A, Man M, Apoil A: Acromioclavicular dislocations: Treatment by coracoacromial ligamentoplasty. J Shoulder Elbow Surg 1995;4:130-134. [DOI] [PubMed] [Google Scholar]
- 199.von Heideken J, Bostrom Windhamre H, Une-Larsson V, Ekelund A: Acute surgical treatment of acromioclavicular dislocation type V with a hook plate: Superiority to late reconstruction. J Shoulder Elbow Surg 2013;22:9-17. [DOI] [PubMed] [Google Scholar]
- 200.Martetschlager F, Horan MP, Warth RJ, Millett PJ: Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med 2013;41:2896-2903. [DOI] [PubMed] [Google Scholar]
- 201.Shin SJ, Kim NK: Complications after arthroscopic coracoclavicular reconstruction using a single adjustable-loop-length suspensory fixation device in acute acromioclavicular joint dislocation. Arthroscopy 2015;31:816-824. [DOI] [PubMed] [Google Scholar]
- 202.Frank RM, Romeo AA, Richardson C, et al. : Outcomes of latarjet versus distal tibia allograft for anterior shoulder instability repair: A matched cohort analysis. Am J Sports Med 2018;46:1030-1038. [DOI] [PubMed] [Google Scholar]
- 203.Kirkley A, Werstine R, Ratjek A, Griffin S: Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: Long-term evaluation. Arthroscopy 2005;21:55-63. [DOI] [PubMed] [Google Scholar]
- 204.Kirkley A, Griffin S, McLintock H, Ng L: The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability. The Western Ontario Shoulder Instability Index (WOSI). Am J Sports Med 1998;26:764-772. [DOI] [PubMed] [Google Scholar]
- 205.Brophy RH, Marx RG: The treatment of traumatic anterior instability of the shoulder: Nonoperative and surgical treatment. Arthroscopy 2009;25:298-304. [DOI] [PubMed] [Google Scholar]
- 206.Zacchilli MA, Owens BD: Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am 2010;92:542-549. [DOI] [PubMed] [Google Scholar]
- 207.Rowe CR: Prognosis in dislocations of the shoulder. J Bone Joint Surg Am 1956;38-A:957-977. [PubMed] [Google Scholar]
- 208.Leroux T, Wasserstein D, Veillette C, et al. : Epidemiology of primary anterior shoulder dislocation requiring closed reduction in Ontario, Canada. Am J Sports Med 2014;42:442-450. [DOI] [PubMed] [Google Scholar]
- 209.Barber FA, Click SD, Weideman CA: Arthroscopic or open Bankart procedures: What are the costs? Arthroscopy 1998;14:671-674. [DOI] [PubMed] [Google Scholar]
- 210.Makhni EC, Lamba N, Swart E, et al. : Revision arthroscopic repair versus latarjet procedure in patients with recurrent instability after initial repair attempt: A cost-effectiveness model. Arthroscopy 2016;32:1764-1770. [DOI] [PubMed] [Google Scholar]
- 211.Uffmann WJ, Christensen GV, Yoo M, et al. : A cost-minimization analysis of intraoperative costs in arthroscopic bankart repair, open latarjet, and distal tibial allograft. Orthop J Sports Med 2019;7:2325967119882001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Kennon JC, Songy CE, Marigi E, et al. : Cost analysis and complication profile of primary shoulder arthroplasty at a high-volume institution. J Shoulder Elbow Surg 2020;29:1337-1345. [DOI] [PubMed] [Google Scholar]
- 213.Politzer CS, Bala A, Seyler TM, Bolognesi MP, Garrigues GE: Use and cost of reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humerus fractures. Orthopedics 2020;43:119-125. [DOI] [PubMed] [Google Scholar]
- 214.Min K, Fedorka C, Solberg MJ, Shaha SH, Higgins LD: The cost-effectiveness of the arthroscopic bankart versus open latarjet in the treatment of primary shoulder instability. J Shoulder Elbow Surg 2018;27:S2-S9. [DOI] [PubMed] [Google Scholar]
- 215.Kordasiewicz B, Kicinski M, Malachowski K, Boszczyk A, Chaberek S, Pomianowski S: Arthroscopic latarjet stabilization: Analysis of the learning curve in the first 90 primary cases: Early clinical results and computed tomography evaluation. Arthroscopy 2019;35:3221-3237. [DOI] [PubMed] [Google Scholar]
- 216.Dugas JR, Crozier MW: Traumatic anterior instability: Treatment options for initial instability. Sports Med Arthrosc Rev 2018;26:95-101. [DOI] [PubMed] [Google Scholar]
- 217.Friedman LGM, Lafosse L, Garrigues GE: Global perspectives on management of shoulder instability: Decision making and treatment. Orthop Clin North Am 2020;51:241-258. [DOI] [PubMed] [Google Scholar]
- 218.Vezeridis PS, Ishmael CR, Jones KJ, Petrigliano FA: Glenohumeral dislocation arthropathy: Etiology, diagnosis, and management. J Am Acad Orthopaedic Surgeons 2019;27:227-235. [DOI] [PubMed] [Google Scholar]
- 219.White AE, Patel NK, Hadley CJ, Dodson CC: An algorithmic approach to the management of shoulder instability. J Am Acad Orthop Surg Glob Res Rev 2019;3():e19.00168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Cole PA, Gauger EM, Schroder LK: Management of scapular fractures. J Am Acad Orthop Surg 2012;20:130-141. [DOI] [PubMed] [Google Scholar]
- 221.Aydin N, Enes Kayaalp M, Asansu M, Karaismailoglu B: Treatment options for locked posterior shoulder dislocations and clinical outcomes. EFORT Open Rev 2019;4:194-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Yamamoto N, Itoi E: Osseous defects seen in patients with anterior shoulder instability. Clin Orthop Surg 2015;7:425-429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Brelin A, Dickens JF: Posterior shoulder instability. Sports Med Arthrosc Rev 2017;25:136-143. [DOI] [PubMed] [Google Scholar]
- 224.Best MJ, Tanaka MJ: Multidirectional instability of the shoulder: Treatment options and considerations. Sports Med Arthrosc Rev 2018;26:113-119. [DOI] [PubMed] [Google Scholar]
- 225.Illyes A, Kiss J, Kiss RM: Electromyographic analysis during pull, forward punch, elevation and overhead throw after conservative treatment or capsular shift at patient with multidirectional shoulder joint instability. J Electromyogr Kinesiol 2009;19:e438-47. [DOI] [PubMed] [Google Scholar]
- 226.Balg F, Boileau P: The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 2007;89:1470-1477. [DOI] [PubMed] [Google Scholar]
- 227.Barlow JD, Grosel T, Higgins J, Everhart JS, Magnussen RA: Surgical treatment outcomes after primary vs recurrent anterior shoulder instability. J Clin Orthop Trauma 2019;10:222-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Hurley ET, Lim Fat D, Farrington SK, Mullett H: Open versus arthroscopic latarjet procedure for anterior shoulder instability: A systematic review and meta-analysis. Am J Sports Med 2019;47:1248-1253. [DOI] [PubMed] [Google Scholar]
- 229.Kelly MP, Perkinson SG, Ablove RH, Tueting JL: Distal biceps tendon ruptures: An epidemiological analysis using a large population database. Am J Sports Med 2015;43:2012-2017. [DOI] [PubMed] [Google Scholar]
- 230.Lang NW, Bukaty A, Sturz GD, Platzer P, Joestl J: Treatment of primary total distal biceps tendon rupture using cortical button, transosseus fixation and suture anchor: A single center experience. Orthop Traumatol Surg Res 2018;104:859-863. [DOI] [PubMed] [Google Scholar]
- 231.Tanner C, Johnson T, Muradov P, Husak L. Single incision power optimizing cost-effective (SPOC) distal biceps repair. J Shoulder Elbow Surg 2013;22:305-311. [DOI] [PubMed] [Google Scholar]
- 232.Ford SE, Andersen JS, Macknet DM, Connor PM, Loeffler BJ, Gaston RG: Major complications after distal biceps tendon repairs: Retrospective cohort analysis of 970 cases. J Shoulder Elbow Surg 2018;27:1898-1906. [DOI] [PubMed] [Google Scholar]
- 233.Feller R, Illing D, Allen C, Presson A, Tyser A, Kazmers N: Evaluation of factors influencing surgical treatment costs for distal biceps rupture. J Shoulder Elbow Surg. 2020;29:e229-e237. [DOI] [PubMed] [Google Scholar]
- 234.Frank T, Seltser A, Grewal R, King GJW, Athwal GS: Management of chronic distal biceps tendon ruptures: Primary repair vs. semitendinosus autograft reconstruction. J Shoulder Elbow Surg 2019;28:1104-1110. [DOI] [PubMed] [Google Scholar]
- 235.Cerciello S, Visona E, Corona K, Ribeiro Filho PR, Carbone S: The treatment of distal biceps ruptures: An overview. Joints 2018;6:228-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Srinivasan RC, Pederson WC, Morrey BF: Distal biceps tendon repair and reconstruction. J Hand Surg Am 2020;45:48-56. [DOI] [PubMed] [Google Scholar]
- 237.Frank RM, Cotter EJ, Strauss EJ, Jazrawi LM, Romeo AA: Management of biceps tendon pathology: From the glenoid to the radial tuberosity J Am Acad Orthop Surg 2018;26:e77-e89. [DOI] [PubMed] [Google Scholar]
- 238.Freeman CR, McCormick KR, Mahoney D, Baratz M, Lubahn JD: Nonoperative treatment of distal biceps tendon ruptures compared with a historical control group. J Bone Joint Surg Am 2009;91:2329-2334. [DOI] [PubMed] [Google Scholar]
- 239.Legg AJ, Stevens R, Oakes NO, Shahane SA: A comparison of nonoperative vs. endobutton repair of distal biceps ruptures. J Shoulder Elbow Surg 2016;25:341-348. [DOI] [PubMed] [Google Scholar]
- 240.Baker BE, Bierwagen D: Rupture of the distal tendon of the biceps brachii. Operative versus non-operative treatment. J Bone Joint Surg Am 1985;67:414-417. [PubMed] [Google Scholar]
- 241.Chillemi C, Marinelli M, De Cupis V: Rupture of the distal biceps brachii tendon: Conservative treatment versus anatomic reinsertion—Clinical and radiological evaluation after 2 years. Arch Orthop Trauma Surg 2007;127:705-708. [DOI] [PubMed] [Google Scholar]
- 242.Morrey BF, Askew LJ, An KN, Dobyns JH: Rupture of the distal tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg Am 1985;67:418-421. [PubMed] [Google Scholar]
- 243.Morrey ME, Abdel MP, Sanchez-Sotelo J, Morrey BF: Primary repair of retracted distal biceps tendon ruptures in extreme flexion. J Shoulder Elbow Surg 2014;23:679-685. [DOI] [PubMed] [Google Scholar]
- 244.Grant JA, Bissell B, Hake ME, Miller BS, Hughes RE, Carpenter JE: Relationship between implant use, operative time, and costs associated with distal biceps tendon reattachment. Orthopedics 2012;35:e1618-e1624. [DOI] [PubMed] [Google Scholar]
- 245.Matzon JL, Graham JG, Penna S, et al. : A prospective evaluation of early postoperative complications after distal biceps tendon repairs. J Hand Surg Am 2019;44:382-386. [DOI] [PubMed] [Google Scholar]
- 246.Amarasooriya M, Bain GI, Roper T, Bryant K, Iqbal K, Phadnis J: Complications after distal biceps tendon repair: A systematic review. Am J Sports Med 2020: Feb 24 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 247.ElMaraghy A, Devereaux M: Response to the letter to the editor regarding: A systematic review and comprehensive classification of pectoralis major tears. J Shoulder Elbow Surg 2013;22:e25-e26. [DOI] [PubMed] [Google Scholar]
- 248.Butt U, Mehta S, Funk L, Monga P: Pectoralis major ruptures: A review of current management. J Shoulder Elbow Surg 2015;24:655-662. [DOI] [PubMed] [Google Scholar]
- 249.Haley CA, Zacchilli MA: Pectoralis major injuries: Evaluation and treatment. Clin Sports Med. 2014;33:739-756. [DOI] [PubMed] [Google Scholar]
- 250.Schepsis AA, Grafe MW, Jones HP, Lemos MJ: Rupture of the pectoralis major muscle. Outcome after repair of acute and chronic injuries. Am J Sports Med 2000;28:9-15. [DOI] [PubMed] [Google Scholar]
- 251.Hanna CM, Glenny AB, Stanley SN, Caughey MA: Pectoralis major tears: Comparison of surgical and conservative treatment. Br J Sports Med 2001;35:202-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Aarimaa V, Rantanen J, Heikkila J, Helttula I, Orava S: Rupture of the pectoralis major muscle. Am J Sports Med 2004;32:1256-1262. [DOI] [PubMed] [Google Scholar]
- 253.Zvijac JE, Schurhoff MR, Hechtman KS, Uribe JW: Pectoralis major tears: Correlation of magnetic resonance imaging and treatment strategies. Am J Sports Med 2006;34:289-294. [DOI] [PubMed] [Google Scholar]
- 254.Kakwani RG, Matthews JJ, Kumar KM, Pimpalnerkar A, Mohtadi N: Rupture of the pectoralis major muscle: Surgical treatment in athletes. Int Orthop 2007;31:159-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Garrigues GE, Kraeutler MJ, Gillespie RJ, O'Brien DF, Lazarus MD: Repair of pectoralis major ruptures: Single-surgeon case series. Orthopedics 2012;35:e1184-e1190. [DOI] [PubMed] [Google Scholar]
- 256.Lau BH, Butterwick DJ, Lafave MR, Mohtadi NG: Retrospective review of pectoralis major ruptures in rodeo steer wrestlers. Adv Orthop 2013;2013:987910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.de Castro Pochini A, Andreoli CV, Belangero PS, et al. : Clinical considerations for the surgical treatment of pectoralis major muscle ruptures based on 60 cases: A prospective study and literature review. Am J Sports Med 2014;42:95-102. [DOI] [PubMed] [Google Scholar]
- 258.Merolla G, Paladini P, Artiaco S, Tos P, Lollino N, Porcellini G: Surgical repair of acute and chronic pectoralis major tendon rupture: Clinical and ultrasound outcomes at a mean follow-up of 5 years. Eur J Orthop Surg Traumatol 2015;25:91-98. [DOI] [PubMed] [Google Scholar]
- 259.Bak K, Cameron EA, Henderson IJ: Rupture of the pectoralis major: A meta-analysis of 112 cases. Knee Surg Sports Traumatol Arthrosc 2000;8:113-119. [DOI] [PubMed] [Google Scholar]
- 260.Koulouris G, Connell D: Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol 2003;32:582-589. [DOI] [PubMed] [Google Scholar]
- 261.Bodendorfer BM, Curley AJ, Kotler JA, et al. : Outcomes after operative and nonoperative treatment of proximal hamstring avulsions: A systematic review and meta-analysis. Am J Sports Med 2018;46:2798-2808. [DOI] [PubMed] [Google Scholar]
- 262.Belk JW, Kraeutler MJ, Mei-Dan O, Houck DA, McCarty EC, Mulcahey MK: Return to sport after proximal hamstring tendon repair: A systematic review. Orthop J Sports Med 2019;7:2325967119853218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Konan S, Haddad F: Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop 2010;34:119-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Sarimo J, Lempainen L, Mattila K, Orava S: Complete proximal hamstring avulsions: A series of 41 patients with operative treatment. Am J Sports Med 2008;36:1110-1115. [DOI] [PubMed] [Google Scholar]
- 265.Subbu R, Benjamin-Laing H, Haddad F: Timing of surgery for complete proximal hamstring avulsion injuries: Successful clinical outcomes at 6 weeks, 6 months, and after 6 months of injury. Am J Sports Med 2015;43:385-391. [DOI] [PubMed] [Google Scholar]
- 266.Birmingham P, Muller M, Wickiewicz T, Cavanaugh J, Rodeo S, Warren R: Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg Am 2011;93:1819-1826. [DOI] [PubMed] [Google Scholar]
- 267.Bunker TD, Esler CN, Leach WJ: Rotator-cuff tear of the hip. J Bone Joint Surg Br 1997;79:618-620. [DOI] [PubMed] [Google Scholar]
- 268.Thaunat M, Clowez G, Desseaux A, et al. : Influence of muscle fatty degeneration on functional outcomes after endoscopic gluteus medius repair. Arthroscopy 2018;34:1816-1824. [DOI] [PubMed] [Google Scholar]
- 269.Lindner D, Shohat N, Botser I, Agar G, Domb BG: Clinical presentation and imaging results of patients with symptomatic gluteus medius tears. J Hip Preserv Surg 2015;2:310-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Bogunovic L, Lee SX, Haro MS, et al. : Application of the Goutallier/Fuchs rotator cuff classification to the evaluation of hip abductor tendon tears and the clinical correlation with outcome after repair. Arthroscopy 2015;31:2145-2151. [DOI] [PubMed] [Google Scholar]
- 271.Suppauksorn S, Nwachukwu BU, Beck EC, Okoroha KR, Nho SJ: Superior gluteal reconstruction for severe hip abductor deficiency. Arthrosc Tech 2019;8:e1255-e1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Chandrasekaran S, Darwish N, Vemula SP, Lodhia P, Suarez-Ahedo C, Domb BG: Outcomes of gluteus maximus and tensor fascia lata transfer for primary deficiency of the abductors of the hip. Hip Int 2017;27:567-572. [DOI] [PubMed] [Google Scholar]
- 273.Domb BG, Botser I, Giordano BD: Outcomes of endoscopic gluteus medius repair with minimum 2-year follow-up. Am J Sports Med 2013;41:988-997. [DOI] [PubMed] [Google Scholar]
- 274.Heerey JJ, Kemp JL, Mosler AB, et al. : What is the prevalence of hip intra-articular pathologies and osteoarthritis in active athletes with hip and groin pain compared with those without? A systematic review and meta-analysis. Sports Med 2019;49:951-972. [DOI] [PubMed] [Google Scholar]
- 275.Frank JM, Harris JD, Erickson BJ, et al. : Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: A systematic review. Arthroscopy 2015;31:1199-1204. [DOI] [PubMed] [Google Scholar]
- 276.Mather RC, III, Nho SJ, Federer A, et al. : Effects of arthroscopy for femoroacetabular impingement syndrome on quality of life and economic outcomes. Am J Sports Med 2018;46:1205-1213. [DOI] [PubMed] [Google Scholar]
- 277.Suarez JC, Ely EE, Mutnal AB, et al. : Comprehensive approach to the evaluation of groin pain. J Am Acad Orthopaedic Surgeons 2013;21:558-570. [DOI] [PubMed] [Google Scholar]
- 278.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA: Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin orthopaedics Relat Res 2003;417:112-120. [DOI] [PubMed] [Google Scholar]
- 279.Sankar WN, Nevitt M, Parvizi J, Felson DT, Agricola R, Leunig M: Femoroacetabular impingement: Defining the condition and its role in the pathophysiology of osteoarthritis. J Am Acad Orthopaedic Surgeons 2013;21(suppl 1):S7-S15. [DOI] [PubMed] [Google Scholar]
- 280.Wenger DE, Kendell KR, Miner MR, Trousdale RT: Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res 2004;426:145-150. [DOI] [PubMed] [Google Scholar]
- 281.Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH: Cam impingement causes osteoarthritis of the hip: A nationwide prospective cohort study (CHECK). Ann Rheum Dis 2013;72:918-923. [DOI] [PubMed] [Google Scholar]
- 282.Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ: Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med 2010;38:99-104. [DOI] [PubMed] [Google Scholar]
- 283.Dierckman BD, Ni J, Hohn EA, Domb BG: Does duration of symptoms affect clinical outcome after hip arthroscopy for labral tears? Analysis of prospectively collected outcomes with minimum 2-year follow-up. J Hip Preserv Surg 2017;4:308-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Aprato A, Jayasekera N, Villar R: Timing in hip arthroscopy: Does surgical timing change clinical results? Int orthopaedics 2012;36:2231-2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Kamath AF, Componovo R, Baldwin K, Israelite CL, Nelson CL: Hip arthroscopy for labral tears: Review of clinical outcomes with 4.8-year mean follow-up. Am J Sports Med 2009;37:1721-1727. [DOI] [PubMed] [Google Scholar]
- 286.Lodhia P, Gui C, Chandrasekaran S, Suarez-Ahedo C, Dirschl DR, Domb BG: The economic impact of acetabular labral tears: A cost-effectiveness analysis comparing hip arthroscopic surgery and structured rehabilitation alone in patients without osteoarthritis. Am J Sports Med 2016;44:1771-1780. [DOI] [PubMed] [Google Scholar]
- 287.Nakano N, Lisenda L, Jones TL, Loveday DT, Khanduja V: Complications following arthroscopic surgery of the hip: A systematic review of 36 761 cases. Bone Joint J 2017;99-B:1577-1583. [DOI] [PubMed] [Google Scholar]
- 288.Kester BS, Capogna B, Mahure SA, Ryan MK, Mollon B, Youm T. Independent risk factors for revision surgery or conversion to total hip arthroplasty after hip arthroscopy: A review of a large statewide database from 2011 to 2012. Arthroscopy 2018;34(2):464-470. [DOI] [PubMed] [Google Scholar]


