More implementation research is needed to further close the gap between research and practice in lifestyle interventions for people with severe mental illness
Keywords: Lifestyle, Severe mental illness, Implementation, Schizophrenia, Physical activity
Abstract
The scandal of premature mortality in people with serious mental illness is well established. Despite an increase in studies evaluating the efficacy of lifestyle interventions, translating this evidence into routine clinical care and policies is challenging, in part due to limited effectiveness or implementation research. We highlight the challenge of implementation that is increasingly recognized in clinical practice, advocate for adopting implementation science to study the implementation and systematic update of effective interventions in practice and policy, and provide directions for future research.
Implications.
Practice: Implementation research can help expedite the translation of findings from randomized controlled trials (RCTs) into routine clinical practice.
Policy: Policies regarding the physical health of people with severe mental illness need to be informed not only by RCT evidence but also implementation research to guide the design and delivery of effective interventions in real-world conditions.
Research: In addition to a call for more effectiveness studies conducted in real-world settings, concurrently studying the implementation and systematic uptake of effective interventions in practice and policy is an essential step to translate effective lifestyle interventions into routine mental health care.
People with severe mental illness (SMI) experience a reduced life expectancy up to 20 years compared to the general population, predominantly due to poor physical health [1–5]. Modifiable cardiometabolic risk factors, such as physical inactivity, a sedentary lifestyle, smoking, and dietary risks, contribute significantly to these negative health outcomes [6–10]. Interventions that address these risk factors are increasingly recognized as important components of treatment for this vulnerable population. For example, many systematic reviews and meta-analyses have demonstrated the efficacy of physical activity interventions on cardiometabolic health, psychiatric symptoms, quality of life, and global and cognitive functioning in people with SMI [11–17], with the most efficacious interventions executed at sufficient levels of intensity and delivered by qualified exercise professionals (e.g. exercise physiologists and physiotherapists) [16,17].
In 2016, the Society of Behavioral Medicine (SBM), together with the American College of Sports Medicine (ACSM), called for the expansion of the U.S. health plan coverage for exercise programming for people with SMI [18]. This was in response to the limited availability of such programs in routine care in contrast to the considerable evidence demonstrating the efficacy of “lifestyle interventions,” that is, programs which aim to promote an active and healthy lifestyle. The gap between this increase in evidence and policies aiming to address the reduced life expectancy of people with SMI and changes in routine care was stressed in several editorials as well, calling for action [19–23]. The overwhelming majority of evidence to date has focused on the efficacy of lifestyle interventions, using randomized controlled trials (RCTs) to answer the question “does it work?” [24]. While essential, such studies have limited external validity, frequently involving individuals who are already looking to change their health behaviors and who are often less severely unwell [20]. Further, efficacy studies are typically performed under ideal conditions, which are unlikely to reflect typical resourcing of interventions under real-world conditions. Therefore, positive findings from RCTs cannot automatically translate into routine clinical care.
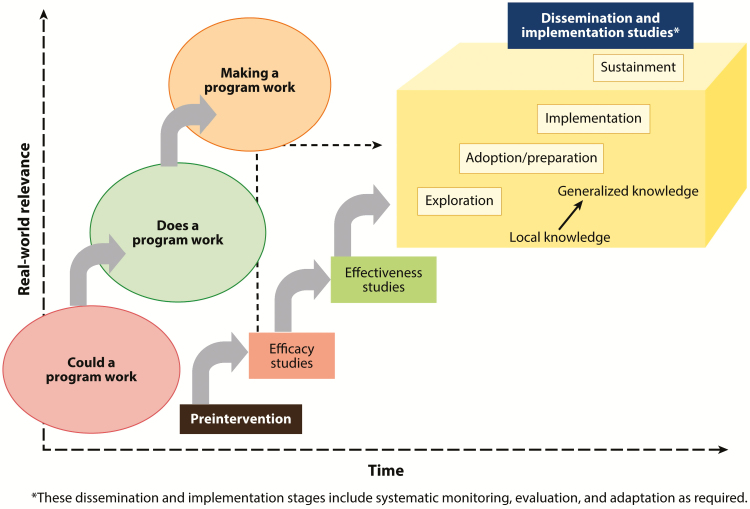
Thus, if efficacy is shown, studies evaluating the effectiveness of interventions in real-world settings can help to understand how to “make a program work” in routine clinical practice, as outlined in the model of Brown et al. [24] (Fig. 1). Such studies will help answer the question as to how patients with SMI can include lifestyle changes in their daily lives in real-world settings [25–27], which is also relevant in light of the limited evidence regarding the maintenance and long-term health benefits of lifestyle interventions [16,27,28].
Fig 1.
The traditional translational pipeline from preintervention, efficacy, effectiveness to dissemination and implementation studies. Adapted from Brown et al. [24].
Implementing and then sustaining (i.e., integration within an organization) evidence-based interventions within routine clinical care is a complex process. Specific characteristics of real-world clinical settings and multilevel barriers for successful implementation are two key challenges in this [29,30]. In this context, knowledge on factors at the individual level (e.g., patients and health care professionals) [31–35] and using co-design principles with adequate representation from and consultation with those individuals is vitally important [36,37]. This could contribute to a more tailored approach, improving the meaningfulness and suitability for both patients and health care professionals and thereby their autonomous motivation, which was suggested to enhance sustainable engagement [38–41]. However, environmental (e.g., community/system and policy influences) and organizational level factors (i.e., ensuring adequate resourcing, organizational culture) also are crucial, although less frequently studied [18,25,29,30,42]. Regarding resourcing, this may also include involving and upskilling existing workforce as it is not always possible to attract and retain lifestyle-oriented health care professionals, for example, in more rural and remote geographic regions [43]. A better understanding of implementation-related factors can reveal why interventions may or may not work in a “real-world” context and how they can be sustained over the longer term, which would support efforts to embed these services in routine clinical practice. Such factors are relevant for health care professionals and people living with SMI. This also applies to policymakers and other key stakeholders, to ensure the long-term impact of investments in lifestyle interventions and deinvestment in interventions with limited evidence base or proven efficacy [30,44,45].
Implementation science, that is, studying methods to promote the systematic uptake of evidence-based interventions into practice and policy, is designed to address such difficulties. In addition to more effectiveness studies, we advocate for more implementation research to further close the gap between research and practice in lifestyle interventions for people with SMI. Such studies should assess measures of acceptability, adoption, fidelity, implementation costs, and sustainability in addition to clinical markers [46] (Fig. 1). A practical guide to support this type of research is PRACTical planning for Implementation and Scale-up (PRACTIS). PRACTIS was introduced as a step-by-step approach to implementing physical activity interventions in both inpatient and community real-world settings and can be applied to other areas of public health prevention [29]. It describes four iterative steps. The first step focuses on the characterization of the parameters of the implementation setting, such as the size of the target population, how implementers will be engaged, trained, and supported, and the identification of champions. It also includes how associated costs and resources will be sustainably funded and alignment with and integration into organizational missions, policies, and job descriptions. The second step includes identifying and engaging key stakeholders across multiple levels within the implementation setting. The third and fourth step focus on the identification of contextual barriers and facilitators to implementation and addressing potential barriers. PRACTIS supports implementation efforts by outlining “a structure for researchers and stakeholders, with varying levels of implementation experience and expertise, to navigate the complex considerations and decision-making processes involved in translating evidence-based interventions into practice” [29]. It should be recognized that these steps are not a fixed linear process as uncertainty and unpredictability (e.g., organizational changes) are inherent to real-world settings [47]. Although effectiveness and implementation studies are typically considered to be separate research designs, they can be combined to expedite the translation of research findings into routine practice [48]. Studying the implementation of lifestyle interventions includes evaluation of costs and adverse events as well, which are crucial in the context of sustainable implementation [16,17]. Furthermore, there is a need for support implementation research through appropriate funding schemes as well as encouraging and promoting the publication of implementation-based findings in addition to efficacy studies from traditional RCTs. In addition to a call for more effectiveness studies conducted in real-world settings, concurrently studying the implementation and systematic uptake of effective interventions in practice and policy is an essential step to drive this field forward. We should ensure that the implementation of such interventions does not become the “elephant in the room.” The challenge of implementation is widely recognized and we need more than efficacy studies to address this. It is time to focus on how we can implement and deliver interventions in routine clinical practice in order to achieve long-term change and improve the health status of people with SMI.
Compliance with Ethical Standards
Conflicts of Interest: All authors declare that they have no conflicts of interest.
Authors’ Contributions: J.D., L.C., J.F. and S.R. conceptualized the manuscript idea. J.D., L.C. and S.R. wrote the initial draft and subsequent revisions of the manuscript. All authors contributed to the interpretation and discussion and provided critical feedback on the final paper.
References
- 1. Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: A systematic review and meta-analysis. Lancet Psychiatry. 2017;4(4):295–301. [DOI] [PubMed] [Google Scholar]
- 2. Piotrowski P, Gondek TM, Królicka-Deręgowska A, Misiak B, Adamowski T, Kiejna A. Causes of mortality in schizophrenia: an updated review of European studies. Psychiatr Danub. 2017;29(2):108–120. [DOI] [PubMed] [Google Scholar]
- 3. Tanskanen A, Tiihonen J, Taipale H. Mortality in schizophrenia: 30-year nationwide follow-up study. Acta Psychiatr Scand. 2018;138(6):492–499. [DOI] [PubMed] [Google Scholar]
- 4. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Correll CU, Solmi M, Veronese N, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: A large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry. 2017;16(2):163–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. de Leon J, Diaz FJ. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr Res. 2005;76(2–3):135–157. [DOI] [PubMed] [Google Scholar]
- 7. Stubbs B, Chen LJ, Chung MS, Ku PW. Physical activity ameliorates the association between sedentary behavior and cardiometabolic risk among inpatients with schizophrenia: A comparison versus controls using accelerometry. Compr Psychiatry. 2017;74:144–150. [DOI] [PubMed] [Google Scholar]
- 8. Vancampfort D, Probst M, Scheewe T, et al. Relationships between physical fitness, physical activity, smoking and metabolic and mental health parameters in people with schizophrenia. Psychiatry Res. 2013;207(1–2):25–32. [DOI] [PubMed] [Google Scholar]
- 9. Firth J, Stubbs B, Teasdale SB, et al. Diet as a hot topic in psychiatry: A population-scale study of nutritional intake and inflammatory potential in severe mental illness. World Psychiatry. 2018;17(3):365–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Teasdale SB, Ward PB, Samaras K, et al. Dietary intake of people with severe mental illness: Systematic review and meta-analysis. Br J Psychiatry. 2019;214(5):251–259. [DOI] [PubMed] [Google Scholar]
- 11. Dauwan M, Begemann MJ, Heringa SM, Sommer IE. Exercise improves clinical symptoms, quality of life, global functioning, and depression in schizophrenia: A systematic review and meta-analysis. Schizophr Bull. 2016;42(3):588–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rosenbaum S, Tiedemann A, Sherrington C, Curtis J, Ward PB. Physical activity interventions for people with mental illness: A systematic review and meta-analysis. J Clin Psychiatry. 2014;75(9):964–974. [DOI] [PubMed] [Google Scholar]
- 13. Vera-Garcia E, Mayoral-Cleries F, Vancampfort D, Stubbs B, Cuesta-Vargas AI. A systematic review of the benefits of physical therapy within a multidisciplinary care approach for people with schizophrenia: An update. Psychiatry Res. 2015;229(3):828–839. [DOI] [PubMed] [Google Scholar]
- 14. Firth J, Cotter J, Elliott R, French P, Yung AR. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med. 2015;45(7):1343–1361. [DOI] [PubMed] [Google Scholar]
- 15. Firth J, Stubbs B, Rosenbaum S, et al. Aerobic exercise improves cognitive functioning in people with schizophrenia: A systematic review and meta-analysis. Schizophr Bull. 2017;43(3):546–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stubbs B, Vancampfort D, Hallgren M, et al. EPA guidance on physical activity as a treatment for severe mental illness: A meta-review of the evidence and Position Statement from the European Psychiatric Association (EPA), supported by the International Organization of Physical Therapists in Mental Health (IOPTMH). Eur Psychiatry. 2018;54:124–144. [DOI] [PubMed] [Google Scholar]
- 17. Czosnek L, Lederman O, Cormie P, Zopf E, Stubbs B, Rosenbaum S. Health benefits, safety and cost of physical activity interventions for mental health conditions: A meta-review to inform translation efforts. Ment Health Phys Act. 2019;16:140–151. [Google Scholar]
- 18. Pratt SI, Jerome GJ, Schneider KL, et al. Increasing US health plan coverage for exercise programming in community mental health settings for people with serious mental illness: A position statement from the Society of Behavior Medicine and the American College of Sports Medicine. Transl Behav Med. 2016;6(3):478–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stewart R. Mental disorders and mortality: So many publications, so little change. Acta Psychiatr Scand. 2015;132(5):410–411. [DOI] [PubMed] [Google Scholar]
- 20. Bartels SJ. Can behavioral health organizations change health behaviors? The STRIDE study and lifestyle interventions for obesity in serious mental illness. Am J Psychiatry. 2015;172(1):9–11. [DOI] [PubMed] [Google Scholar]
- 21. Mitchell AJ, De Hert M. Promotion of physical health in persons with schizophrenia: Can we prevent cardiometabolic problems before they begin? Acta Psychiatr Scand. 2015;132(2):83–85. [DOI] [PubMed] [Google Scholar]
- 22. McGrath JJ. No mental health without physical health - A call to arms. Epidemiol Psychiatr Sci. 2016;25(3):195–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Suetani S, Rosenbaum S, Scott JG, Curtis J, Ward PB. Bridging the gap: What have we done and what more can we do to reduce the burden of avoidable death in people with psychotic illness? Epidemiol Psychiatr Sci. 2016;25(3):205–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brown CH, Curran G, Palinkas LA, et al. An overview of research and evaluation designs for dissemination and implementation. Annu Rev Public Health. 2017;38:1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Liu NH, Daumit GL, Dua T, et al. Excess mortality in persons with severe mental disorders: A multilevel intervention framework and priorities for clinical practice, policy and research agendas. World Psychiatry. 2017;16(1):30–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vancampfort D, Stubbs B, Ward PB, Teasdale S, Rosenbaum S. Why moving more should be promoted for severe mental illness. Lancet Psychiatry. 2015;2(4):295. [DOI] [PubMed] [Google Scholar]
- 27. Naslund JA, Whiteman KL, McHugo GJ, Aschbrenner KA, Marsch LA, Bartels SJ. Lifestyle interventions for weight loss among overweight and obese adults with serious mental illness: A systematic review and meta-analysis. Gen Hosp Psychiatry. 2017;47:83–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jakobsen AS, Speyer H, Nørgaard HCB, et al. Effect of lifestyle coaching versus care coordination versus treatment as usual in people with severe mental illness and overweight: Two-years follow-up of the randomized CHANGE trial. PLoS One. 2017;12(10):e0185881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Koorts H, Eakin E, Estabrooks P, Timperio A, Salmon J, Bauman A. Implementation and scale up of population physical activity interventions for clinical and community settings: The PRACTIS guide. Int J Behav Nutr Phys Act. 2018;15(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lennox L, Maher L, Reed J. Navigating the sustainability landscape: A systematic review of sustainability approaches in healthcare. Implement Sci. 2018;13(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, Vancampfort D. Motivating factors and barriers towards exercise in severe mental illness: A systematic review and meta-analysis. Psychol Med. 2016;46(14):2869–2881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Robson D, Haddad M, Gray R, Gournay K. Mental health nursing and physical health care: A cross-sectional study of nurses’ attitudes, practice, and perceived training needs for the physical health care of people with severe mental illness. Int J Ment Health Nurs. 2013;22(5):409–417. [DOI] [PubMed] [Google Scholar]
- 33. Stanton R, Happell B, Reaburn P. Investigating the exercise-prescription practices of nurses working in inpatient mental health settings. Int J Ment Health Nurs. 2015;24(2):112–120. [DOI] [PubMed] [Google Scholar]
- 34. Chapman JJ, Fraser SJ, Brown WJ, Burton NW. Physical activity preferences, motivators, barriers and attitudes of adults with mental illness. J Ment Health. 2016;25(5):448–454. [DOI] [PubMed] [Google Scholar]
- 35. Way K, Kannis-Dymand L, Lastella M, Lovell GP. Mental health practitioners’ reported barriers to prescription of exercise for mental health consumers. Ment Health Phys Act. 2018;14:52–60. [Google Scholar]
- 36. Wheeler AJ, Roennfeldt H, Slattery M, Krinks R, Stewart V. Codesigned recommendations for increasing engagement in structured physical activity for people with serious mental health problems in Australia. Health Soc Care Community. 2018;26(6): 860–870. [DOI] [PubMed] [Google Scholar]
- 37. Matthews E, Cowman M, Denieffe S. Using experience-based co-design for the development of physical activity provision in rehabilitation and recovery mental health care. J Psychiatr Ment Health Nurs. 2017;24(7):545–552. [DOI] [PubMed] [Google Scholar]
- 38. Farholm A, Sørensen M, Halvari H. Motivational factors associated with physical activity and quality of life in people with severe mental illness. Scand J Caring Sci. 2017;31(4):914–921. [DOI] [PubMed] [Google Scholar]
- 39. Hargreaves J, Lucock M, Rodriguez A. From inactivity to becoming physically active: The experiences of behaviour change in people with serious mental illness. Ment Health Phys Act. 2017;13:83–93. [Google Scholar]
- 40. Lundström S, Ahlström BH, Jormfeldt H, Eriksson H, Skärsäter I. The meaning of the lived experience of lifestyle changes for people with severe mental illness. Issues Ment Health Nurs. 2017;38(9):717–725. [DOI] [PubMed] [Google Scholar]
- 41. Ward MC, White DT, Druss BG. A meta-review of lifestyle interventions for cardiovascular risk factors in the general medical population: Lessons for individuals with serious mental illness. J Clin Psychiatry. 2015;76(4):e477–e486. [DOI] [PubMed] [Google Scholar]
- 42. Bartels S, Brunette M, Aschbrenner K, Daumit G. Implementation of a system-wide health promotion intervention to reduce early mortality in high risk adults with serious mental illness and obesity. Implement Sci. 2015;10(suppl 1):A15. [Google Scholar]
- 43. Patel V, Hanlon C.. Where There Is No Psychiatrist: A Mental Health Care Manual. 2nd ed. Cambridge, UK: Royal College of Psychiatrists; 2018. [Google Scholar]
- 44. Wiltsey Stirman S, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: A review of the empirical literature and recommendations for future research. Implement Sci. 2012;7:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Braithwaite J, Churruca K, Long JC, Ellis LA, Herkes J. When complexity science meets implementation science: A theoretical and empirical analysis of systems change. BMC Med. 2018;16(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]