A 64-year-old man diagnosed with coronavirus disease (COVID-19) by polymerase chain reaction test 2 days after having fever was admitted to another hospital. He had a history of gastric ulcer, duodenal ulcer and no known hypercoagulable conditions. Although the patient was treated with favipiravir and ciclesonide, he was intubated owing to the deterioration of his respiratory function on Day 10 of hospitalization. When his condition worsened, he was transferred to our hospital for extracorporeal membrane oxygenation (ECMO) on Day 15 of hospitalization. On admission, his level of consciousness was E1VTM1 on the Glasgow Coma Scale. His electrocardiographic waveform showed sinus rhythm. Fibrin degradation product level was 471.3 μg/mL, prothrombin time-international normalized ratio was 1.52, activated partial thromboplastin time was 39.4 s, and fibrinogen level was 410 mg/dL. Enhanced computed tomography (CT) findings were as follows: (i) multiple cerebral infarctions including left middle cerebral artery infarction (Figure 1a), (ii) bilateral renal infarction (Figure 1b) and (iii) splenic infarction (Figure 1b). We judged that there was no adaptation to ECMO. Favipiravir, meropenem, teicoplanin, a steroid for acute respiratory distress syndrome, and antithrombotic therapy with enoxaparin sodium were administered. Despite appropriate treatment, the patient died on Day 26 in our hospital. Written informed consent was obtained from the patient’s family for publication. A copy of the written consent is available for review upon request.
Figure 1.
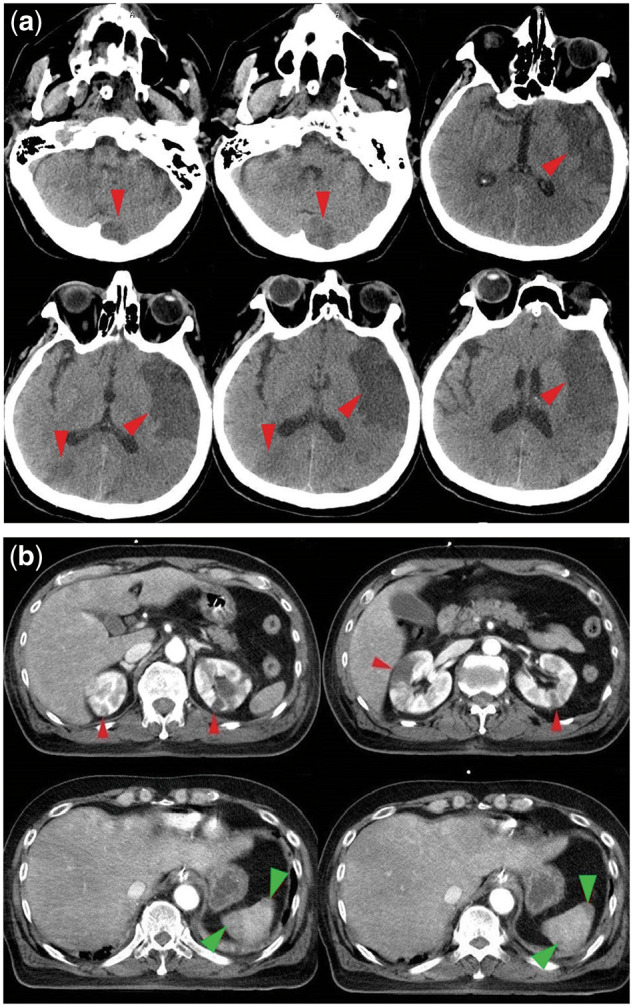
(a) Cerebral infarction on head CT. (b) Bilateral renal infarction (red arrow) and splenic infarction (green arrow) on enhanced abdominal CT.
Thrombosis is a serious complication of severe COVID-19 and has a high incidence rate.1–4 Klok et al.2 reported that pulmonary embolism was the most common thrombotic event followed by ischemic stroke among 31 thrombotic events. Conversely, no renal and splenic infarction in a COVID-19 case has been reported. Although Helms et al.3 also reported 14 COVID-19 patients with thrombo-embolic complications, no cases had a thrombosis in the abdominal organs. While it is clear that COVID-19 is more likely to cause thrombosis, cases of infarction in multiple organs have not been regularly reported, and thus, our COVID-19 case with multiple infarctions is rare. Anticoagulant treatment with heparin reduces mortality in COVID-19 patients with high D-dimer or high sepsis-induced coagulopathy (SIC) score5; this suggests that infarctions may be an important factor associated with mortality in COVID-19 patients. In this case as well, it may have been possible to rescue the patient if the possibility of thrombosis was evaluated from at an early stage and if treatment for thrombosis was administered.
To our knowledge, this is a rare COVID-19 case with not only cerebral infarction but also multiple organ infarctions. Clinicians should be aware that infarction, an important life-threatening complication, may occur in any organ, and early anti-thromboembolism treatment should be considered in COVID-19 patients.
Consent for publication
Written informed consent was obtained from the patient’s family for publication of this case report and the accompanying images. A copy of the written consent is available for review upon request.
Supplementary Material
Acknowledgments
We would like to thank Kenichiro Uchida, MD, PhD, Tetsuro Nishimura, MD, PhD and Hiromasa Yamamoto, MD, PhD for participation in the treatment of this patient as members of the Trauma and Critical Care Center Department, Osaka City University Hospital. We would like to thank Koichi Yamada, MD, PhD for participation in the treatment as members of the Infectious Disease Medicine Department, Osaka City University Hospital. We would like to thank Editage (www.editage.com) for their assistance with English language editing.
Conflict of interest. The authors state that they have no conflict of interest.
Contributor Information
W Imoto, Department of Infection Control Science, Osaka City University Graduate School of Medicine, Osaka, Japan, Department of Infectious Disease Medicine, Osaka City University Hospital, Osaka, Japan and Department of Respiratory Medicine, Osaka City University Graduate School of Medicine, Osaka, Japan.
S Kaga, Department of Traumatology and Critical Care Medicine, Osaka City University Graduate School of Medicine, Osaka, Japan and Department of Trauma and Critical Care Center, Osaka City University Hospital, Osaka, Japan.
T Noda, Department of Infection Control Science, Osaka City University Graduate School of Medicine, Osaka, Japan and Department of Infectious Disease Medicine, Osaka City university Hospital, Osaka, Japan.
Y Mizobata, Department of Traumatology and Critical Care Medicine, Osaka City University Graduate School of Medicine, Osaka, Japan and Department of Trauma and Critical Care Center, Osaka City University Hospital, Osaka, Japan.
H Kakeya, Department of Infection Control Science, Osaka City University Graduate School of Medicine, Osaka, Japan and Department of Infectious Disease Medicine, Osaka City University Hospital, Osaka, Japan.
References
- 1. Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC State-of-the-Art Review. J Am Coll Cardiol 2020; 75:2950–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers D, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020; 191:145–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, et al. ; CRICS TRIGGERSEP Group (Clinical Research in Intensive Care and Sepsis Trial Group for Global Evaluation and Research in Sepsis). High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med 2020; 46:1089–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Besutti G, Bonacini R, Iotti V, Marini G, Riva N, Dolci G, et al. Abdominal visceral infarction in 3 patients with COVID-19. Emerg Infect Dis 2020; 26:1926–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost 2020; 18:1094–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


