Introduction
The coronavirus epidemic has rapidly brought to the forefront the importance of remote interactions between patients and providers. Chronic pain medicine is no exception, and patients and providers across the country have adopted telemedicine and shifted the paradigm for chronic pain care. The Centers for Medicare and Medicaid Services (CMS) has also signaled that the “relaxation” of telemedicine guidelines and reimbursement are likely to continue (albeit to a lesser extent) as the coronavirus crisis improves [1]. Telemedicine includes audio and/or video interactions with patient and provider in two distinct locations and includes remote consultation, diagnosis, monitoring, and counseling [2, 3].
Although telemedicine has existed for more than two decades, its rapid expansion has been paralleled by new questions surrounding its appropriateness and utility in the field of chronic pain [4, 5]. Thus, there is a critical need for guidance surrounding telemedicine during the COVID crisis, as well as for a sustainable plan to continue some degree of telemedicine as the crisis abates regionally across the country.
Previous studies have examined the benefits of telemedicine for a physical therapy intervention in low back pain using apps for mobile devices [6]. Another Cochrane review looked at the efficacy of telemedicine for remote psychological therapy in children and adolescents with pain [7]. Practice guidelines and recommendations for telemedicine already exist for fields such as dermatology, and a cost analysis of telemedicine in chronic pain has also been completed [8–10]. Despite these previous studies, there is a lack of suggested best practice approaches for the utilization of telemedicine in chronic pain assessment and treatment.
Given the wealth of information important to convey to Pain Medicine readers regarding telemedicine for chronic pain care, this commentary will use a bullet point format to present combined expert opinions regarding the utility, implementation, and our experiences of telemedicine in several multidisciplinary academic and community-based pain medicine practices, in a single metropolitan area.
Benefits of Telemedicine (Audio and Video) in Chronic Pain (Table 1)
Table 1.
Benefits of telemedicine (audio and video) in chronic pain
| Benefits of Audio and Video Telemedicine in Chronic Pain Medicine |
|---|
| Psychosocial and motivational factors |
| Convenience and improved access |
| Gaps in medical care can be bridged by telemedicine |
| Comprehensive evaluations can be performed remotely |
-
Psychosocial and Motivational Factors
With observation in the home environment, the provider may get a more informal assessment of mental status.
Other social information can be observed, including living environment, interactions with family and others in the household, and witnessing a snapshot of patients' lives at home.
Observation of other at-home behaviors may yield information on tobacco use/alcohol use/hobbies/etc.
The provider can get a sense of the patient’s commitment to and compliance with past and future recommendations. For instance, is the patient taking the telemedicine call from a bed or couch that they appear to use the entire day?
-
Convenience and Efficiency for Patients and Providers
No travel and parking issues, including savings on parking fees and gas. Child care costs may be avoided when the patient stays at home.
Improved access for patients in rural, underserved areas and patients who reside long distances from the clinic.
Patients do not need to sit in a waiting room with other patients, which may improve the patient's sense of privacy and minimize infectious disease exposures.
Time is saved on patient processing inefficiencies—such as moving patients into rooms and discharging patients.
Offers additional flexibility for patients' schedules (numerous visits have been conducted with patients in a work break room or at their place of employment).
Allows additional scheduling flexibility for providers who want to work nontypical clinic hours with less commute time for providers.
Lower no-show rates are seen for patients with telemedicine visits.
Peace-of-mind and rapid assessment for providers who want to quickly check in with a patient who has a potential complication.
-
Telemedicine Can Fill Gaps in Transitional Care (May or May Not Be Billable in These Situations)
Telemedicine evaluation can be completed in a skilled nursing facility before discharge as a way to coordinate transitions of care.
Telemedicine could be used to coordinate outpatient pain care before discharge from an outside hospital or emergency room.
-
Telemedicine Evaluations Can Still Be Comprehensive in Nature
When a video telemedicine evaluation is coupled with a review of patient-reported outcomes obtained via a separate Web-based application (such as pain, function, mood, expectations, and sleep ratings), a comprehensive history and assessment can be performed efficiently.
This includes the assessment of appropriateness for procedures and the outcomes of any previous treatment.
The Collaborative Health Outcomes Information Registry (CHOIR) software platform we use addresses these needs, for example [11].
-
Remote telemedicine vital sign monitoring equipment is becoming available [12]
Drawbacks of Telemedicine (Audio and Video) in Chronic Pain (Table 2)
-
Potential for Diminished Quality of the Patient–Provider Interaction
Without in-person visits, nonverbal cues that contribute to establishing a patient–provider relationship are lost, making it difficult to discuss complex issues related to pain care.
Possible introduction of bias through only seeing the home environment and social cues without a face-to-face encounter.
-
Limited Ability to Perform a Physical Exam
The establishment of a differential diagnosis for common pain complaints requires a proper physical exam. For example, low back pain can present as a finding of multiple clinical conditions, which can be narrowed based on a musculoskeletal and neurological exam.
Physical examination may help differentiate disease progression from variation due to natural history.
Certain procedures may not get insurance pre-authorization without a face-to-face visit with a thorough musculoskeletal and neurological exam.
-
Psychological/Social History Challenges
Limited ability to assess pain behaviors and patient hygiene (related to tobacco use/alcohol status, for example).
-
Patient Engagement Issues
Additional distractors at home such as television, computer, and others in the home that may be off the screen.
Potential lack of privacy for the patient [13].
Telemedicine connection issues—video connection can be unreliable. Lag time often exists, which limits a fluid conversation.
-
Financial Considerations
Questions persist on local and national reimbursement for telemedicine and the lack of co-pays and hospital facility fees for telemedicine visits.
Telemedicine visits may result in a loss of facility fees, although telemedicine has the potential to expand access to and add additional patients to a practice.
During a COVID-19 emergency, telemedicine phone appointments can be billed by time.
Table 2.
Drawbacks of telemedicine (audio and video) in chronic pain
| Drawbacks of Audio and Video Telemedicine in Chronic Pain Medicine |
|---|
| Diminished quality of the provider/patient interaction |
| Limited ability to perform a physical exam |
| Psychological/social history challenges |
| Patient engagement issues |
| Potential financial implications for a provider’s hospital or clinic |
Appropriateness of New and/or Follow-up Patients for Telemedicine in Chronic Pain
The authors provide the following guidelines based on our experiences with telemedicine, consideration of key aspects of chronic pain care, and literature review (see Figure 1). A green, yellow, and red scheme aids in stratifying the following different situations. While considering each situation, the authors weighed the benefits and drawbacks outlined above to arrive on a recommendation for appropriateness. In settings with more information available to the pain provider, such as a single health system with access to records through EMR, many drawbacks of telemedicine are overcome. A telemedicine initial evaluation may also provide a starting point to gather additional information.
Figure 1.
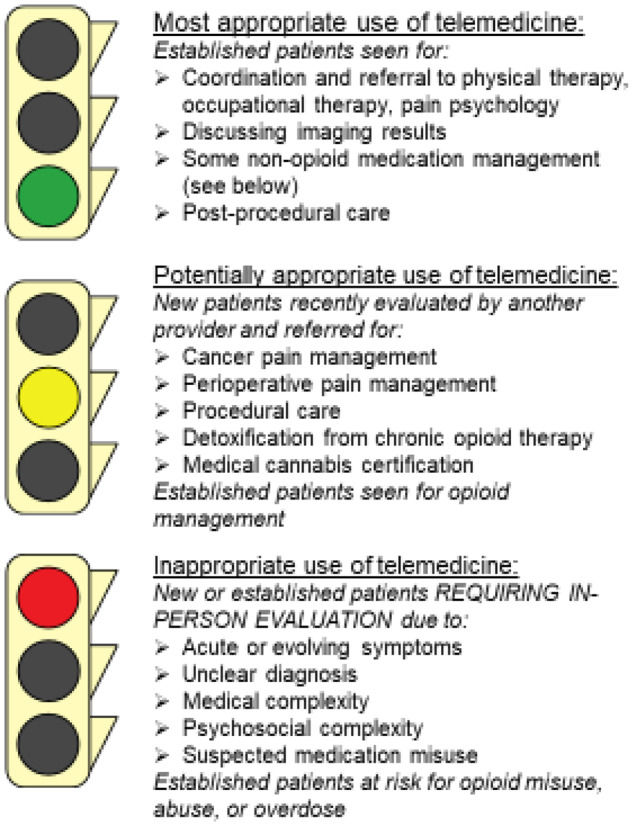
Consensus opinion about the appropriateness of telemedicine for common clinical scenarios encountered in pain management practice.
-
Most Appropriate Use of Telemedicine (GREEN)
-
Established follow-up patients
If patients are known to the provider, then there is less risk of several drawbacks, including a lack of exam or less information about patient compliance, and greater likelihood of benefits including patient access. Prior exams and vital signs can help guide treatment.
Coordination and referral to physical therapy, occupational therapy, and psychology for established patients is appropriate for telemedicine.
Discussions of imaging results are appropriate, if symptoms have been stable since the last in-person visit. Visual aids and spine models can be difficult to use, however.
Noncontrolled substance medication management is appropriate for the most part. See the YELLOW- Established follow-up patients: Management of controlled substances section for considerations associated with controlled substances.
Postprocedural care visits with telemedicine allow for follow-up after procedures to assess efficacy, establish future treatment plans, and coordinate future in-person visits. Additionally, more frequent follow-up could be conducted after advanced procedures, such as during spinal cord stimulation trials, to aid in monitoring percutaneous leads.
-
-
Potentially Appropriate Use of Telemedicine (YELLOW)
-
New patients recently evaluated by a provider for specific treatments
Cancer pain management. Telemedicine can improve access for cancer patients. Pain often limits access for these patients to clinic visits, and introductory telemedicine visits can present patients with options for future in-person treatment. An initial evaluation may be appropriate in assisting with medication management and planning interventional approaches including intrathecal pump implantation or neurolytic procedures.
Perioperative pain management. If information is available through a centralized electronic medical record, coordination of care following discharge from either the hospital or other facility may be possible through telemedicine, including assistance in tapering perioperative opioids.
Procedural care. If patients have been evaluated by another provider with a documented physical exam and the provider is referring to consider a specific, indicated procedure, the pain practitioner could consider evaluating the patient remotely and then scheduling the procedure. The appropriateness of this highly depends on the specifics of the pain practice regarding referral source and procedure location (office vs surgery center) as well as the procedure in question (e.g., epidural steroid injection vs spinal cord stimulator).
Detoxification from chronic opioid therapy. Buprenorphine detoxification via telemedicine may be appropriate for new and return patients who either misuse or wish to stop chronic opioid therapy. Psychological evaluation before detoxification is recommended to determine readiness. Periodic psychological sessions thereafter may assist with compliance.
Medical cannabis certification. Cannabis certification and recertification may be appropriate for low-risk patients determined by an absence of significant psychiatric illness and illicit substance use. Certification may be limited to a three-month period until an in-person visit is performed. Exact state laws and regulations would determine suitability. Verbal consent for cannabis use may be obtained by telemedicine. Toxicology is deferred until an in-person visit is performed for recertification.
-
Established follow-up patients: Management of controlled substances
Opioid management during telemedicine in established patients would be most appropriate if the patients are low risk for opioid misuse as determined by history of either misuse or other opioid misuse risk assessments and previous adherence to opioid treatment agreements.
Improved access to care, with equivalent patient monitoring for opioid-associated risks, may be achieved by alternating telemedicine with in-person visits over time.
Opioid titration and tapering may be easier during telemedicine, as frequent visits needed to assess progress will be less burdensome on patients.
Urine/saliva toxicology before cannabis certification and recertification may be deferred in low-risk patients until an in-person visit can be performed. Toxicology may be performed at an outside laboratory if needed during telemedicine visits.
-
-
Inappropriate Use of Telemedicine (RED)
-
New or established patients requiring in-person evaluation with a physical exam
Acute and evolving symptoms, including the presence of new or progressive weakness, functional decline, numbness, bowel or bladder incontinence, and other red flag symptoms that have not been addressed recently by another provider, require an in-person exam and potential urgent/emergent management.
Diagnostically challenging patients need a physical exam before determining a treatment plan, for example, patients with chronic low back pain who have not been evaluated by other specialists and are lacking a documented exam to aid in identification of a pain generator.
Medically complex patients who need vital sign monitoring before medication management.
Psychosocially complex patients may benefit from in-person evaluation to assess pain behaviors, compliance, and engagement.
New patients with suspected medication misuse require in-person evaluation for an exam, pill count, and drug screen to promptly identify and properly manage substance use disorders.
-
Established patients at high risk for medication misuse, abuse, and/or opioid overdose
Patients who are high risk for negative outcomes of chronic opioid therapy may require in-person visits. This is likely to be a case-by-case decision. Some markers for higher-risk patients may include higher daily oral morphine equivalents (such as >90 morphine equivalents per day), multiple controlled substances being simultaneously prescribed, concerns for polypharmacy, and prior evidence of opioid misuse [14].
-
Audio-Only Telemedicine Discussion
Audio-only visits may be used due to a patient or provider not having the available technology, equipment, or skill to set up the software, no high-speed internet, religious beliefs, or visual impairment.
-
Benefits
Improved access for patients who are not able to use video visits, but otherwise could not present for an in-person visit.
Providers may experience less bias without visual awareness of patient’s surroundings.
Telephone conversations are commonplace and therefore allow for easier listening and more natural flow of conversations.
Patients may feel safer and less vulnerable if their home environment is not exposed.
May be more efficient without technological glitches that accompany video visits.
-
Drawbacks
Less engagement of patient and provider without visual cues and body language visualization.
Patients may get the feeling of a more impersonal, disconnected provider.
No additional information can be observed from patient, including less mental status information.
Privacy issues still exist with at-home conversations that may not be applicable in a closed clinic room.
Discussions of personal information while at home may still make patients feel unsafe.
Questionable reimbursement with audio-only visits.
Telebehavioral Health in Pain Medicine
The provision of telebehavioral health services is appropriate for most patients receiving behavioral health care in pain medicine clinics [15]. Specific guidance on the appropriateness of telebehavioral health services is provided below using a green/yellow/red scheme similar to that above.
-
Most Appropriate Use (GREEN)
-
Diagnosis and treatment
Mental health problems, including depression, anxiety, post-traumatic stress disorder, and substance use disorders, tend to commonly co-occur with chronic pain [16]. As patients receiving behavioral health care in pain medicine largely experience moderately severe mental health problems and primarily depression and anxiety as well as mild substance use disorders, these patients tend to be excellent candidates for telebehavioral health services [15].
For some patients, telebehavioral health is the preferred way to receive care because they can do so from home, which can reduce stigma [15]. Also, some patients feel safer and more relaxed receiving behavioral health care at home [17].
-
-
Potentially Appropriate Use (YELLOW)
Telebehavioral health services can be appropriate for patients experiencing suicidal ideation who do not qualify for a higher level of care (e.g., intensive outpatient program, inpatient hospitalization) [18]. However, behavioral health providers need to be prepared to intervene if risk of suicide becomes higher.
Patients with privacy concerns may not be candidates for telemedicine. Some patients are uncomfortable receiving telebehavioral health services due to concern about communications (e.g., video, phone, e-mail) being breached and overheard by others in the home [18]. If concerns cannot be allayed, then the patients should receive behavioral health services in clinic.
Some patients are easily distracted [18]. Distractibility can be a problem when meeting with a patient in clinic, but this can be even more of a problem when patients are in their own residences.
Assessment of suitability for implantable devices via a telebehavioral health visit is complicated by loss of behavioral observations and remote use of psychological testing. Although telebehavioral health evaluations for this purpose can be considered, we recommend in-person evaluations at this time.
-
Inappropriate Use (RED)
Some patients will refuse to receive telebehavioral health services, and this decision should be respected.
Patients requiring a higher level of behavioral health care than can be safely offered in an outpatient pain medicine clinic are also naturally inappropriate for telebehavioral health services for chronic pain.
Telemedicine for Trainees
The utilization of telemedicine is an important training experience for residents and fellows.
Many telemedicine software applications allow three-way video and audio telemedicine conferences that can help incorporate trainees.
Telemedicine allows for continued training of residents and fellows during times of lower patient volume.
The Role of Advanced Practice Providers in Telemedicine
Advanced practice providers (APPs) play two main roles in pain medicine; 1) addressing patient issues that are considered mild to moderate and 2) triaging patient issues that are considered severe.
Patients with chronic pain often have pain-related concerns that they need addressed. These concerns may be related to changes in their pain, medication effectiveness or adverse side effects, new pain-related symptoms, etc. APPs can address these scenarios without having to escalate to the physician [19].
Occasionally patients experience abrupt changes in their pain, side effects, or other concerns that necessitate the attention of the physician. In this case, the APP’s role is to interview the patient and then communicate to the physician for intervention.
APPs can treat and evaluate telemedicine patients in multiple clinics or inpatient units and bridge gaps in care.
Utilization of APPs can save time and allow physicians to focus on other tasks [20].
In conclusion, despite several limitations of telemedicine, significant strengths exist, such that the authors foresee continued use of telemedicine to improve multidisciplinary pain care beyond the emergency response to the COVID-19 pandemic. Innovations, including remote monitoring of vital signs, consolidation of electronic medical record systems, and comprehensive evaluation of patient-reported outcomes over the Internet, will expand the appropriate use of telemedicine in pain management.
References
- 1.Centers for Medicare and Medicaid Services. Medicare telemedicine health care provider fact sheet. 2020. Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet (accessed May 2020).
- 2. Waller M, Stotler C.. Telemedicine: A primer. Curr Allergy Asthma Rep 2018;18(10):54. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare and Medicaid Services. Telemedicine. Available at: https://www.medicaid.gov/medicaid/benefits/telemedicine/index.html (accessed May 2020).
- 4. Mann D, Chen J, Chunara R, Testa P, Nov O.. COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zajtchuk R, Gilbert GR.. Telemedicine: A new dimension in the practice of medicine. Dis Mon 1999;45(6):197–262. [DOI] [PubMed] [Google Scholar]
- 6. Amorim A, Pappas E, Simic M, et al. Integrating mobile-health, health coaching, and physical activity to reduce the burden of chronic low back pain trial (IMPACT): A pilot randomised controlled trial. BMC Musculoskelet Disord 2019;20(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fisher E, Law E, Dudeney J, Eccleston C, Palermo T.. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2019;4:CD011118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Abbott L, Miller R, Janda M, et al. Practice guidelines for teledermatology in Australia. Australas J Dermatol 2020;61(2):e174–83. [DOI] [PubMed] [Google Scholar]
- 9. Krupinski E, Bernard J.. Standards and guidelines in telemedicine and telehealth. Healthcare (Basel) 2014;2(1):74–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pronovost A, Peng P, Kern R.. Telemedicine in the management of chronic pain: A cost analysis study. Can J Anaesth 2009;56(8):590–6. [DOI] [PubMed] [Google Scholar]
- 11. Dressler A, Gillman A, Wasan A.. A narrative review of data collection and analysis guidelines for comparative effectiveness research in chronic pain using patient reported outcomes and electronic health records. J Pain Res 2019;12:491–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhao F, Li M, Tsien JZ.. Technology platforms for remote monitoring of vital signs in the new era of telemedicine. Expert Rev Med Devices 2015;12(4):411–29. [DOI] [PubMed] [Google Scholar]
- 13. Chaet D, Clearfield R, Sabin JE, et al. Ethical practice in telehealth and telemedicine. J Gen Intern Med 2017;32(10):1136–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dowell D, Haegerich T, Chou R.. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA 2016;315(15):1624–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yellowlees P, Shore J.. Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals. Washington, DC: American Psychiatric Publishing; 2018. [Google Scholar]
- 16. Darnall B. Psychological Treatment for Patients with Chronic Pain. Washington, DC: American Psychological Association; 2019. [Google Scholar]
- 17. Zimmerman J. Providing psychological services in the face of uncertainty: A Q&A series. Providing Psychological Services in the Face of Uncertainty Series. 2020. Available at: https://www.youtube.com/watch? v=-vsqspzqmvY (accessed May 5, 2020).
- 18.Guidelines for conducting mental health services with technology. 2020. Available at: https://en.wikiversity.org/wiki/Helping_Give_Away_Psychological_Science/Telepsychology (accessed May 5, 2020).
- 19. Reed K. Telemedicine: Benefits to advanced practice nursing and the communities they serve. J Am Acad Nurse Pract 2005;17(5):176–80. [DOI] [PubMed] [Google Scholar]
- 20. Ward M, Merchant K, Carter K, et al. Use of telemedicine for ED physician coverage in critical access hospitals increased after CMS policy clarification. Health Aff 2018;37(12):2037–44. [DOI] [PubMed] [Google Scholar]


