Abstract
Few studies have evaluated hypertension incidence in relation to walking, which is a common physical activity among adults. We examined the association between walking and hypertension incidence in 83,435 postmenopausal women who at baseline were aged 50–79 years, without known hypertension, heart failure, coronary heart disease, or stroke, and reported the ability to walk at least one block without assistance. Walking volume (metabolic equivalent hours per week; MET-hr/wk) and speed (miles per hour; mph) were assessed by questionnaire. Incident physician-diagnosed hypertension treated with medication was ascertained through annual questionnaires. During a mean 11-year follow-up, 38,230 hypertension cases were identified. After adjustment for covariates including non-walking activities, a significant inverse association with hypertension was observed across categories of baseline walking volume (0 [referent], >0–3.5, 3.6–7.5, >7.5 MET-hr/wk), hazard ratio [HR]: 1.00 [ref], 0.98, 0.95, 0.89, trend p<0.001. Faster walking speeds (<2, 2–3, 3–4, >4 mph) also were associated with lower hypertension risk, HR: 1.00 [ref], 1.07, 0.95, 0.86, 0.79, trend p<0.001. Further adjustment for walking duration (hr/wk) had little impact on the association for walking speed (HR: 1.00 [ref], 1.08, 0.96, 0.86, 0.77, trend p<.001). Significant inverse associations for walking volume and speed persisted after additional control for baseline blood pressure. Results for time-varying walking were comparable to those for baseline exposures. This study showed that walking at guideline recommended volumes (>7.5 MET-hr/wk) and at faster speeds (≥2 mph), is associated with lower hypertension risk in postmenopausal women. Walking should be encouraged as part of hypertension prevention in older adults.
Keywords: Exercise, Epidemiology, Hypertension, Women, Longitudinal, Prevention
INTRODUCTION
Age-related blood pressure (BP) dysregulation and increases in hypertension prevalence are attributed to changes in arterial structure and function occurring with aging.1,2 It is estimated that by 2030 there will be 73 million U.S. citizens aged 65 years and older, 55% of whom will be postmenopausal women.3 Compared with their younger premenopausal counterparts, postmenopausal women experience a greater rise in mean BP with increasing age, and a higher prevalence of hypertension.4–6 Given the significant health consequences associated with hypertension,7,8 identification of modifiable factors by which older women might lessen their risk of hypertension has important public health implications.
Physical activity (PA) has been inversely associated with hypertension incidence in observational studies.9 Sex-specific results have been inconsistent, with a number of studies yielding non-significant findings in women.10–13 Available studies have not focused on women 60 and older, in whom hypertension prevalence is high. Evidence for an association between walking and hypertension incidence is sparse. Because walking is the most frequently reported activity among older adults,14 understanding its potential role in hypertension prevention has relevance to population aging.
The present study prospectively examined the association between walking and hypertension incidence in the Women’s Health Initiative (WHI). Our hypothesis was that greater walking volume and speed would each be associated with lower hypertension risk. We further hypothesized that walking speed would be associated with hypertension risk independent of walking duration.
METHODS
Data that support the findings of this study are available from the corresponding author upon reasonable request and with permission from the WHI.
The WHI enrolled 161,808 postmenopausal women, aged 50–79 years, into one or more of three clinical trials (CT; Hormone Therapy [estrogen plus progestin, or estrogen alone]; Dietary Modification; Calcium and Vitamin D Supplementation) or a prospective observational study (OS) at 40 U.S. centers. The WHI was designed to examine determinants of morbidity and mortality in postmenopausal women.15–17
The current analyses included CT and OS women who at baseline: (a) were without a history of hypertension treated with medication, and (b) whose baseline measured BP was systolic <140 mmHg and diastolic <90 mmHg. Although guidelines now define hypertension as systolic and diastolic BP ≥130 and ≥80 mmHg,18 we used a definition consistent with practice guidelines at the time of baseline measurements (1993–1998).19 Walking information was missing in 5,943 women; they were excluded. Characteristics of these women were similar to those included, except for slightly lower current menopausal hormone therapy use (38.5% vs 42.9%) and college education (77.2% vs 81.4%) (Table S1). Hypertension rates (per 1000 person-years) were 50.9 and 45.8 in women missing and not missing walking, respectively. Participants were further excluded if at baseline they reported not being able to walk at least one block unassisted, had a history of heart failure, coronary heart disease or stroke, or had <1 year of follow-up, resulting in 83,435 women (32,790 CT; 50,645 OS) for analysis (Figure S1). Institutional Review Board approval and participant informed consent was obtained at WHI centers. This study conformed to STROBE guidelines for human observational studies.
Walking and Physical Activity Assessment
Walking was assessed using self-administered questionnaires at baseline and again periodically during follow-up (CT: years 1, 3, 6, 9, annually thereafter; OS annually year 3 and after). Frequency, duration, and speed of usual walking for at least 10 minutes consecutively was queried (Supplement). Walking volume was computed as the product of walking frequency, duration, and the metabolic equivalent (MET) intensity value corresponding to walking speed response choices (<2 mph: 2 METs; 2–3 mph: 3 METs; 3–4 mph: 4 METs; >4 mph: 5 METs),20 yielding walking MET-hr/wk. Non-walking recreational PA volume was self-reported and summarized as MET-hr/wk (Supplement). Walking and PA assessed by this questionnaire is reproducible (ICC = 0.51–0.77)21 and moderately correlated (r = 0.45–0.52) with criterion measures22 in similarly aged women.
Hypertension Ascertainment
Incidence of physician-diagnosed hypertension treated with medication was identified using postbaseline health questionnaires completed annually (OS) or biannually (CT). The case finding question read: “Since the date given on the front of this form, has a doctor prescribed pills for high blood pressure or hypertension?”. Strong agreement exists for WHI hypertension status based on this question and Medicare claims (kappa=0.84; unpublished data). Response reproducibility is high (kappa=0.86) for repeated assessments at enrollment.23
Covariate Assessment
Information on sociodemographics, medical history, dietary intake, and smoking was obtained using self-administered questionnaires. Waist circumference, weight, and height were measured in clinic; body mass index (BMI; kg/m2) was calculated.16 Seated BP was measured after five minutes of rest using auscultatory methods with cuff size based on measured arm circumference.24 Physical function was assessed using the RAND-36 instrument.25 Dietary sodium intake and the Healthy Eating Index (HEI) 26 was determined using the WHI food frequency questionnaire.27 Neighborhood socioeconomic status (nSES; 0–100) was derived using variables on education, employment, household income, and socioeconomic indicators based on U.S. census tracts; higher scores reflect more affluence.
Statistical Analysis
Baseline characteristics were summarized according to walking categories using chi-square tests and analysis of variance. Kaplan-Meier plots characterized the unadjusted annualized incidence of hypertension over walking categories; logrank tests determined statistical significance. Cox proportional hazards regression was used to estimate hazard ratios (HR) and 95% confidence intervals (CI) for incident hypertension according to walking exposures.
Person-time for each participant was from the date of baseline examination (OS) or randomization (CT) to date of the questionnaire on which hypertension diagnosis was reported, censoring on loss to follow-up or death, or August 29, 2014, whichever occurred first. Follow-up was stopped in 2014 because a PA intervention trial was initiated in WHI around this time,28 and because revised hypertension guidelines were published in 2017.18 To avoid potential biases associated with participation in the PA intervention or with changes in BP monitoring and treatment, we ended follow-up prior to these time points. All statistical models controlled for WHI component (CT or OS) and randomization to trial arms. Model 1 included age and race-ethnicity. Model 2 further controlled for education, alcohol, smoking, dietary sodium and HEI, menopausal hormone therapy, diabetes, hyperlipidemia, cancer, and non-walking PA. We then added covariates separately to Model 2: baseline systolic and diastolic BP (Model 3), BMI (Model 4; repeated using waist), and physical functioning (Model 5). In order to explore whether walking speed contributed to hypertension risk independently from walking duration, we estimated HRs according to walking speed categories controlling for Model 2 covariates and additionally for walking duration (hr/wk). Multicollinearity was assessed using variance inflation factors which were not large (<1.3 in multivariable Model 2) suggesting meaningful collinearity was unlikely. For all analyses, the referent group was women who reported no walking (0 MET-hr/wk, non-walkers). Walking volume was defined as tertiles (>0–3.5, 3.6–7.5, >7.5 MET-hr/wk). Walking speed was defined according to questionnaire response choices (<2, 2–3, 3–4, >4 mph). Ordinal scoring was used to evaluate linear trend across walking categories. We also conducted analyses using time-varying exposures for walking volume and speed based on postbaseline reassessments. For walking volume, rather than use different tertile cut-points at each assessment, we evaluated volume as a continuous parameter in the time-varying analysis. Walking speed was based on fixed category definitions at all assessments; the time-varying analysis proceeded accordingly. Covariates were as in Model 2. To evaluate consistency between subgroups, we examined associations across baseline categories of age (50–59, 60–69, ≥70 years), race-ethnicity (white, black, Hispanic, Asian/Pacific Islander; insufficient data for Native Americans), systolic and diastolic BP (tertiles), BMI (<18.0, 18.0–24.9, 25.0–29.9, ≥30 kg/m2), and non-walking PA (0, >0–9.3, >9.3 MET-hr/wk). Statistical interactions were tested using cross-product terms controlling for Model 2 covariates. Sensitivity analyses using Model 2 covariates were conducted to evaluate robustness of our primary analyses. In separate models, we excluded (1) hypertension cases identified in follow-up years 1–3, (2) women with limited functional ability, (3) women reporting anti-hypertension use in the absence of known hypertension, (4) women randomized to hormone CT intervention arm because hypertension incidence was higher in these women,29 and (5) women who reported any vigorous intensity non-walking PA. Statistical tests were conducted at two-sided alpha 0.05 using SAS (Windows v9.4; Cary, NC).
RESULTS
The mean age of participants was 61.9 years, the majority of whom were white and educated beyond high school (Table 1). Participants were from middle or higher socioeconomic strata (mean nSES, 76.7). Mean BMI, systolic and diastolic BP were 26.7 kg/m2, 118.0 and 72.3 mmHg, respectively. Prevalence of current smoking (7.1%), hyperlipidemia (9.7%), diabetes (1.9%), and cancer (9.3%) were relatively low. Participants had high physical functioning (mean RAND-36 score, 87.2). All characteristics in Table 1 were significantly associated with walking volume, except smoking history and dietary sodium. Similar patterns were seen with walking speed (Table S2). All characteristics, except ADL score, differed significantly with hypertension incidence (Table S3).
Table 1.
Baseline characteristics for the overall cohort and according to categories of walking volume (N=83,435).
| Characteristic | Overall (n=83,435) | Walking Volume (MET-hr/wk) | P trend | |||
|---|---|---|---|---|---|---|
| 0 (n=24,253) | >0–3.5 (n=16,122) | 3.6–7.5 (n=22,791) | >7.5 (n=20,269) | |||
| Walking volume (MET-hr/wk) | 5.2 ± 6.3 | 0.0 ± 0.0 | 1.7 ± 0.8 | 5.2 ± 1.5 | 14.3 ± 5.9 | <0.001 |
| Non-walking PA (MET-hr/wk) | 13.8 ± 14.3 | 6.4 ± 10.4 | 8.8 ± 9.9 | 14.1 ± 10.9 | 26.4 ± 16.2 | <0.001 |
| Age (years) | 61.9 ± 7.03 | 61.4 ± 7.0 | 62.0 ± 7.1 | 62.4 ± 7.1 | 61.9 ± 7.0 | <0.001 |
| 50–59 | 40.3 | 43.0 | 40.1 | 37.7 | 40.1 | |
| 60–69 | 43.6 | 42.3 | 43.3 | 44.3 | 44.4 | |
| 70–79 | 16.2 | 14.7 | 16.6 | 18.1 | 15.6 | |
| Race-ethnicity | <0.001* | |||||
| White | 86.6 | 83.69 | 86.5 | 88.5 | 88.3 | |
| African American | 5.5 | 7.58 | 5.2 | 4.3 | 4.7 | |
| Hispanic | 4.0 | 4.63 | 4.2 | 3.6 | 3.3 | |
| Native American | 0.4 | 0.37 | 0.3 | 0.3 | 0.4 | |
| Asian/Pacific Islander | 2.5 | 2.67 | 2.6 | 2.4 | 2.3 | |
| Education | <0.001† | |||||
| High school or less | 18.6 | 22.6 | 19.0 | 16.8 | 15.6 | |
| College/some college | 48.6 | 49.1 | 48.7 | 48.4 | 48.0 | |
| Post-graduate | 32.8 | 28.3 | 32.3 | 34.8 | 36.3 | |
| nSES score‡ | 76.7 ± 8.0 | 76.0 ± 8.2 | 76.4 ± 8.0 | 77.0 ± 7.8 | 77.4 ± 7.8 | <0.001 |
| Smoking | 0.120§ | |||||
| Never | 50.6 | 50.2 | 51.5 | 51.0 | 49.9 | |
| Former | 42.3 | 40.2 | 40.5 | 43.0 | 45.4 | |
| Current | 7.1 | 9.6 | 8.0 | 6.0 | 4.8 | |
| Alcohol use | <0.001§ | |||||
| Never | 9.1 | 10.3 | 9.6 | 8.6 | 8.1 | |
| Former | 15.6 | 17.6 | 15.5 | 14.8 | 14.4 | |
| Current | 75.2 | 72.2 | 74.9 | 76.6 | 77.6 | |
| Hormone therapy use | <0.001§ | |||||
| Never | 41.8 | 42.5 | 43.6 | 41.2 | 40.0 | |
| Former | 15.3 | 15.4 | 15.1 | 15.8 | 14.8 | |
| Current | 42.9 | 42.1 | 41.2 | 43.0 | 45.2 | |
| Diabetes | 1.9 | 2.4 | 2.2 | 1.6 | 1.4 | <0.001 |
| Hyperlipidemia | 9.7 | 9.8 | 9.7 | 10.1 | 9.1 | 0.016 |
| Cancer | 9.3 | 8.8 | 9.3 | 9.7 | 9.5 | 0.023 |
| ADL Score∥ | 4.0 ± 0.2 | 4.0 ± 0.2 | 4.0 ± 0.3 | 4.0 ± 0.2 | 4.0 ± 0.2 | <0.001 |
| Physical function score# | 87.2 ± 13.5 | 84.2 ± 15.1 | 85.4 ± 14.5 | 88.1 ± 12.4 | 91.3 ± 10.2 | <0.001 |
| Systolic BP (mmHg) | 118.0 ± 11.5 | 118.6 ± 11.3 | 118.6 ± 11.4 | 118.1 ± 11.5 | 117.3 ± 11.7 | <0.001 |
| Diastolic BP (mmHg) | 72.3 ± 7.6 | 72.5 ± 7.7 | 72.5 ± 7.7 | 72.2 ± 7.6 | 72.0 ± 7.6 | <0.001 |
| BMI (kg/m2) | 26.7 ± 5.2 | 27.7 ± 5.7 | 27.4 ± 5.5 | 26.3 ± 4.8 | 25.3 ± 4.4 | <0.001 |
| Waist (cm) | 83.2 ± 12.5 | 85.6 ± 13.3 | 84.8 ± 12.8 | 82.4 ± 11.7 | 79.9 ± 11.0 | <0.001 |
| Healthy Eating Index diet score | 67.9 ± 10.6 | 64.9 ± 11.1 | 67.1 ± 10.5 | 69.1 ± 10.0 | 70.6 ± 9.8 | <0.001 |
| Dietary sodium intake (mg) | 2697.1 ± 1206.0 | 2664.9 ± 1239.2 | 2736.6 ± 1198.0 | 2715.6 ± 1163.6 | 2683.2 ± 1217.8 | 0.907 |
| Study component | <0.001 | |||||
| Clinical Trial | 39.3 | 45.6 | 42.5 | 37.1 | 31.9 | |
| Observational Study | 60.7 | 54.4 | 57.5 | 62.9 | 68.1 | |
| HT intervention | 7.9 | 9.2 | 8.4 | 7.5 | 6.4 | <0.001** |
Data are mean ± standard deviation or percentage.
Abbreviations: PA, physical activity; nSES, neighborhood socioeconomic status; BMI, body mass index; HTN, hypertension; MET, metabolic equivalent; BP, blood pressure; HT, hormone therapy.
p-value compares percentage of white vs. non-white participants.
p-value compares percentage of high school vs. some college and/or college graduate.
Neighborhood socioeconomic status, range 0–100; higher scores indicate more affluent status.
p value compares percentage of never vs. ever.
Activities of daily living score, range 4–12; higher values reflect greater limitations.
Physical function score, range 0–100; higher values reflect greater physical function.
p-value compares active vs. placebo and/or not randomized.
During a mean 10.8 year follow-up, 38,230 (45.8%) hypertension cases were documented. The crude incidence rate was 42.4 cases per 1,000 person-years. The annualized cumulative incidence of hypertension was lower (p<0.001) across incremental categories of walking volume and speed; differences somewhat greater for walking speed (Figure S2). The hypertension incidence rate (per 1,000 person-years) in non-walkers was 45.8, whereas rates in women in the upper category of walking volume (>7.5 MET-hr/wk) and speed (>4 mph) were 38.0 and 30.1, respectively (Table 2).
Table 2.
Rates and relative risks of hypertension according to categories of walking volume and speed at baseline (N=83,435).
| Exposure | HTN cases (rate*) | HR (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 2† | Model 3 | Model 4 | Model 5 | ||
| Walking Volume (MET-hr/wk) | |||||||
| 0 (n=24,253) | 11,619 (45.8) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| >0–3.5 (n=16,122) | 7,549 (44.0) | 0.95 (0.93–0.98) | 0.98 (0.95–1.01) | --- | 0.97 (0.94–1.00) | 0.98 (0.95–1.01) | 0.98 (0.95–1.01) |
| 3.6–7.5 (n=22,791) | 10,343 (41.6) | 0.90 (0.88–0.93) | 0.95 (0.92–0.97) | --- | 0.96 (0.93–0.99) | 0.98 (0.95–1.01) | 0.97 (0.95–1.00) |
| > 7.5 (n=20,269) | 8,719 (38.0) | 0.83 (0.81–0.86) | 0.89 (0.87–0.92) | --- | 0.91 (0.88–0.93) | 0.95 (0.92–0.98) | 0.93 (0.91–0.96) |
| P trend | --- | <0.001 | <0.001 | --- | <0.001 | 0.036 | 0.001 |
| Walking Speed (mph) | |||||||
| <2 (n=8,971) | 4,389 (51.1) | 1.08 (1.04–1.11) | 1.07 (1.03–1.10) | 1.08 (1.04–1.12) | 1.06 (1.02–1.09) | 1.05 (1.01–1.09) | 1.05 (1.01–1.09) |
| 2–3 (n=29,782) | 13,680 (42.3) | 0.91 (0.88–0.93) | 0.95 (0.92–0.97) | 0.96 (0.93–0.98) | 0.95 (0.92–0.97) | 0.97 (0.95–1.00) | 0.97 (0.95–1.00) |
| 3–4 (n=19,305) | 8,124 (35.9) | 0.80 (0.78–0.83) | 0.86 (0.84–0.89) | 0.86 (0.83–0.89) | 0.89 (0.86–0.92) | 0.93 (0.90–0.95) | 0.90 (0.87–0.93) |
| >4 (n=1,124) | 418 (30.1) | 0.71 (0.64–0.78) | 0.79 (0.71–0.87) | 0.77 (0.69–0.85) | 0.81 (0.74–0.90) | 0.89 (0.81–0.99) | 0.84 (0.76–0.93) |
| P trend | --- | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Abbreviations as in Table 1.
Incidence rate, number of cases/ 1000 person-years.
Model 1: includes study component (WHI OS or CT), randomization to trial arms, age and race-ethnicity.
Model 2: includes Model 1 + education, alcohol, smoking, diet score, dietary sodium, diabetes, hyperlipidemia, cancer, and non-walking PA.
Model 2: includes Model 2 + walking duration (hours/week).
Model 3: includes Model 2 + Systolic and Diastolic BP.
Model 4: includes Model 2 + BMI.
Model 5: includes Model 2 + physical functioning score.
Following adjustment for Model 2 covariates and when compared to non-walkers, relative hazards of hypertension were lower across incremental tertiles of walking volume (HR: 1.00 [ref], 0.98, 0.95, 0.89; trend p<0.001) (Table 2). An inverse association with hypertension risk was evident for faster walking speeds, although women at the slowest speed had elevated risk (Model 2 HR: 1.00 [ref], 1.07, 0.95, 0.86, 0.79; trend p<0.001); comparable when further adjusted for walking duration (HR: 1.00 [ref], 1.08, 0.96, 0.86, 0.77; trend p<0.001). Additional adjustment for baseline BP (Model 3), BMI (Model 4), and physical functioning (Model 5) attenuated the associations with walking volume and speed but the inverse trends remained significant. Adjusting for waist circumference instead of BMI did not alter results (not shown).
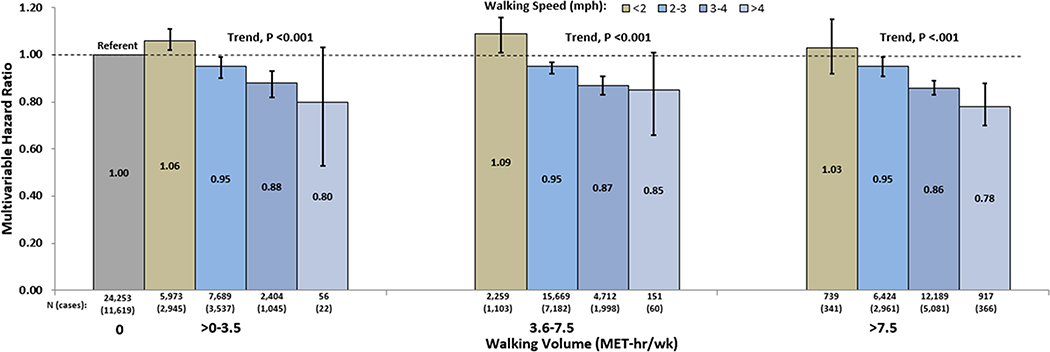
To further understand how walking volume and speed influence hypertension risk, we estimated associations between speed and hypertension within categories of walking volume (Figure 1). Compared to non-walkers, within each walking volume category there was an inverse gradient in hypertension risk over walking speeds ≥2 mph (Trend, P<.001). Both women whose volume was consistent with PA recommendations (>7.5 MET-hr/wk) and those whose volume was below this recommendation had significantly lower hypertension risks with increasing walking speeds ≥2 mph. We then repeated the analysis within categories of walking duration (hr/wk) and observed a similar pattern of results (Figure S3). Lower hypertension risks were evident at speeds ≥2 mph in both women whose walking duration achieved recommendations (≥2.5 hr/wk) and whose did not. The elevated hypertension risk associated with walking <2 mph was evident within categories of walking volume and duration.
Figure 1. Association between walking speed and hypertension within categories of walking volume.
Covariates as in Model 2, Table 2. Bars are 95% CI. Walking 7.5 MET-hr/wk is the minimal volume required to meet guideline recommendations.32
Analyses using time-varying walking volume showed a 7% lower hypertension risk for each 7.5 MET-hr/wk increment (comparable to recommended PA levels; Model 2 HR=0.93, 95% CI: 0.92–0.94), which was similar to findings for baseline walking volume as a continuous variable (HR=0.95, 95% CI: 0.94–0.96). For time-varying walking speed, compared to non-walkers, HRs (95% CI; Model 2) were 1.03 (1.00–1.06), 0.94 (0.92–0.97), 0.83 (0.80–0.86), 0.63 (0.55–0.72) across walking speed categories <2, 2–3, 3–4 >4 mph, respectively; comparable to baseline results (Table 2).
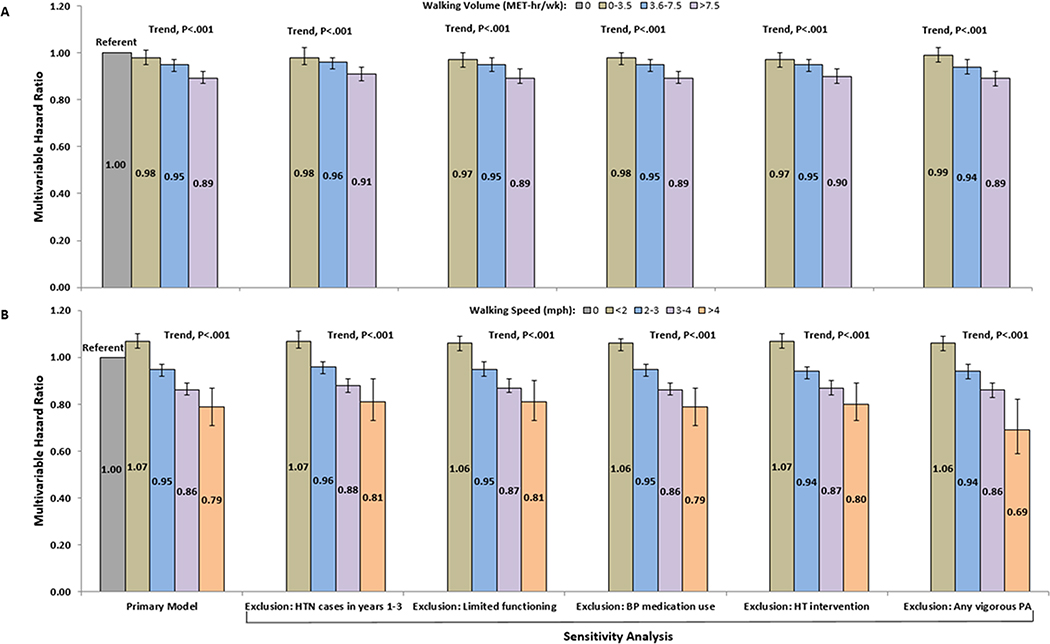
Table 3 displays stratified associations for baseline walking volume. To preserve statistical power, HRs are for a 7.5 MET-hr/wk increment. Results were consistent across strata of race-ethnicity, baseline BP and BMI (interaction p>0.10, all). The association was somewhat stronger in women aged 50–59 (interaction p<0.001) and women reporting no non-walking PA (interaction p=0.03). Stratified results were similar for baseline walking speed (Table S4). Robustness of the primary results were evaluated in five sensitivity analyses (specified in Methods) yielding findings similar to the primary results for both walking exposures (Figure 2).
Table 3.
Associations between walking volume and hypertension stratified on baseline subgroups.
| Characteristic | Cases (rate*) | HR† (95% CI) | P Interaction |
|---|---|---|---|
| All women (83,435) | 38,230 (42.2) | 0.95 (0.94, 0.97) | --- |
| Age, years | <0.001 | ||
| 50–59 (n = 32,286) | 13,478 (35.3) | 0.94 (0.93–0.96) | |
| 60–69 (n = 34,979) | 16,934 (45.8) | 0.97 (0.96–0.98) | |
| ≥ 70 (n = 12,969) | 6,328 (53.5) | 0.99 (0.96–1.01) | |
| Race-ethnicity | 0.172 | ||
| White (n = 69,732) | 31,755 (41.1) | 0.95 (0.94–0.96) | |
| Black (n = 4,320) | 2,392 (64.7) | 0.99 (0.96–1.03) | |
| Hispanic (n = 3,050) | 1,313 (47.1) | 1.02 (0.97–1.07) | |
| Asian/Pacific Islander (n = 2,025) | 782 (38.6) | 1.01 (0.95–1.09) | |
| Systolic BP (tertiles), mmHg | 0.185 | ||
| ≤ 112.0 (n = 26,868) | 7,431 (21.5) | 0.96 (0.94–0.99) | |
| 112.5–124.0 (n = 27,537) | 12,914 (43.0) | 0.97 (0.95–0.99) | |
| ≥ 124.5 (n = 25,755) | 16,356 (73.4) | 0.97 (0.95–0.98) | |
| Diastolic BP (tertiles), mmHg | 0.713 | ||
| ≤ 69.0 (n = 26,865) | 9,498 (29.7) | 0.97 (0.95–0.99) | |
| 69.5–76.0 (n = 27,788) | 12,413 (40.5) | 0.96 (0.94–0.98) | |
| ≥ 76.5 (n = 25,496) | 14,781 (60.9) | 0.96 (0.94–0.97) | |
| BMI, kg/m2 | 0.820 | ||
| <18.5 (n = 1,575) | 566 (31.2) | 0.95 (0.88–1.03) | |
| 18.5–24.9 (n = 33,760) | 13,007 (32.7) | 0.99 (0.98–1.01) | |
| 25.0–29.9 (n = 27,957) | 13,571 (45.9) | 0.97 (0.95–0.98) | |
| ≥ 30 (n = 16,942) | 9,596 (60.4) | 0.99 (0.97–1.01) | |
| Non-walking PA, MET-hr/wk | 0.011 | ||
| 0 (n = 26,414) | 12,612 (46.2) | 0.94 (0.93–0.96) | |
| >0–9.3 (n = 27,051) | 12,562 (42.9) | 0.96 (0.94–0.98) | |
| > 9.3 (n = 26,769) | 11,566 (38.0) | 0.98 (0.96–0.99) | |
Figure 2. Sensitivity analyses for walking volume (A) and speed (B).
Covariates as in Model 2, Table 2. Bars are 95% CI. Functional exclusion was for RAND-36 score <60 or ADL score >4. Medication exclusion was for blood pressure medication without history of diagnosed-treated hypertension.
DISCUSSION
Regular PA is associated with lower hypertension risk.30,31 Few studies have focused on women or on walking, which is a prevalent activity in adults.14 After controlling for sociodemographic, lifestyle and clinical factors, we observed significantly lower hypertension risks of 11% and 21% (Table 2, Model 2) in postmenopausal women reporting the highest walking volume and speed. Walking speed remained significantly associated with lower hypertension risk after adjusting for walking duration (hr/wk). Within each category of walking volume (and of walking duration), an inverse association between hypertension risk and walking speed was evident at speeds ≥2 mph. Despite further controlling for baseline BP, BMI or waist, and physical functioning, significant inverse trends persisted for each walking exposure. Associations were not different across race-ethnicity, baseline BP, or BMI subgroups; however, were somewhat stronger in women aged 50–59 and those reporting no recreational PA. Results based on time-varying walking and extensive sensitivity analyses were similar to primary findings for both exposures. Associations for continuous walking volume (per 7.5 MET-hr/wk increment) were somewhat smaller than categorical analysis comparing women in the highest category (>7.5 MET-hr/wk) with non-walkers, however, the continuous model effect size reflects an average relative risk over the entire range of walking volume. Our results indicate that walking at casual speed (e.g., 30-minute mile) to meet or exceed guideline recommended volume (or duration) is associated with lower hypertension risk in later life. Because inactivity prevalence is high in older adults, even a modest relative risk (e.g., HR = 0.89, Table 2, Model 2) could have relevance in reducing the burden of hypertension’s consequences, such as CHD and stroke.32
Two previous studies on hypertension evaluated walking. Hayashi et al. followed-up 6,017 middle-aged men33 and found a 29% lower hypertension risk associated with walking ≥21 compared to ≤10 minutes/day. Williams et al. studied 15,945 walkers (79% women, mean age 61) recruited from community walking events,34 and observed a 7% lower hypertension risk for each 12.6 MET-hr/wk increment in walking volume. This is consistent with our finding of a 5% lower hypertension risk for each 7.5 MET-hr/wk increment in baseline walking volume.
We observed a stronger association with hypertension for walking speed than volume. Speeds ≥2 mph were inversely associated with hypertension risk within each category of walking volume (Figure 1) and duration (Figure S3). For women walking at recommended volumes of activity (>7.5 MET-hr/wk), risk reductions of 5%, 14%, and 22% were associated with speeds of 2–3, 3–4, and >4 mph, respectively. Importantly, even when walking volume or duration was less than guideline recommendations (>0 to 7.5 MET-hr/wk; >0 to 2.5 hr/wk), women walking at speeds ≥2 mph had significantly lower hypertension risks. This suggests faster walking speed might confer BP benefit beyond volume or duration of walking. Disentangling these interrelationships, however, is challenging. Speed reflects the intensity of walking activity. Intensity of PA is correlated with health benefits,35 including BP outcomes.36 Greater intensity through faster walking might provoke more potent BP regulating mechanisms. Walking speed is positively correlated with maximal oxygen uptake.37 Thus, walking speed could be a marker of cardiorespiratory fitness, which is inversely associated with hypertension incidence in women.38 Higher walking speed requires better physical functioning, which is inversely associated with BP in WHI women.39 Controlling for physical function attenuated the association between walking speed and hypertension (Table 2, Model 5).
Interestingly, women whose walking speed was <2 mph had a significantly higher 5–8% risk of hypertension compared to non-walkers (Table 2). CVD incidence also has been elevated at this walking speed in WHI.40 Despite extensive adjustments and sensitivity analyses, residual confounding by comorbidity could account for higher risk at the slowest walking speed.
Several mechanisms could explain an association between walking and hypertension. Modulation of total peripheral resistance is important for BP regulation during PA.41 This is likely mediated by neurohumoral adaptations (decreased sympathetic nervous activity, lower circulating catecholamines and cortisol, improved baroreflex sensitivity, improved renal function, improved sodium-water regulation) and vascular alterations (improved endothelial function, reduced atherosclerotic burden, increased capillary recruitment capacity, angiogenesis) occurring with PA.41,42 Enhanced body composition and insulin sensitivity, and lower systemic inflammation also are plausible mechanisms.42 Many such physiologic adaptations to regular PA are documented in older adults.42,43
Study strengths include focus on postmenopausal women and the large number of incident hypertension cases. The extensive health and lifestyle information permitted evaluation of several confounding and modifying factors, which enhances confidence in our results. Reverse causation bias is a concern when prospectively assessing associations between hypertension and walking, each could be influenced by pre-clinical cardiovascular manifestations. We cannot completely rule this out as an alternative explanation for the observed inverse associations. However, we excluded participants with evidence of baseline heart failure, CHD, stroke, and severe functional limitations. We observed consistency between our primary results and sensitivity analyses that additionally excluded participants with any functional limitations and hypertension cases occurring during early follow-up (an approach often used in epidemiologic studies).44 Follow-up was ended before the 2017 BP guideline change to avoid potential surveillance bias.
Limitations included self-reported walking information. Because walking was assessed separately from other PA types with good reproducibility in WHI age and race-ethnic subgroups,21 less misclassification error may have occurred than when summarizing multiple PA domains. Consistency of results for time-varying and baseline exposures is reassuring. Ascertainment of hypertension cases was through self-reported information. WHI participants have reliably reported history of treated hypertension.23 Information on family history of hypertension was insufficient for analysis. The WHI enrolled volunteers recruited across the U.S. and may not be a representative cross-section of postmenopausal women, a consideration when generalizing our results.
Perspectives
Results from this prospective study indicate walking is associated with lower hypertension incidence in postmenopausal women, independent of non-walking PA. Walking at a casual pace (e.g., 30-minute mile) to achieve the nationally recommended volume (7.5 MET-hr/wk) or duration (2.5 hr/wk) was associated with significantly lower hypertension risk. For women who did not meet recommendations on volume or duration, walking faster was associated with lower hypertension risk. Importantly, associations between walking and hypertension were consistent across categories of baseline BP and measures of adiposity, suggesting that BP benefit through walking is accessible even for women with elevated hypertension risk due to high normal BP or obesity. If our results are confirmed, it seems reasonable to contemplate design of a randomized clinical trial evaluating walking for the primary prevention of hypertension in adults.
Supplementary Material
Novelty and Significance.
What is new?
Walking (an understudied exposure) was prospectively evaluated with hypertension risk
Postmenopausal women (an understudied population) were studied exclusively
What is relevant?
Elevated BP is highly prevalent in older women
Lifestyle modifications are cornerstone to hypertension prevention strategies
Walking is an accessible and enjoyable activity in older adults
Summary.
Greater walking volume and speed were associated with lower hypertension risk in postmenopausal women. This carries tremendous implications for enhancing hypertension prevention strategies through targeted promotion of walking, the most common recreational activity in later life when the burden of high BP and its clinical consequences is considerable.
Acknowledgements
WHI Investigators: Supplemental File.
Funding: The WHI is funded by the National Heart, Lung, and Blood Institute, U.S. Department of Health and Human Services, through contracts HHSN268201600018C, HHSN268201600001C, HHSN268201600002C, HHSN268201600003C, HHSN268201600004C.
Footnotes
Conflicts/Disclosures: None
Short List of WHI Investigators
Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland)
Jacques Rossouw, Shari Ludlam, Dale Burwen, Joan McGowan, Leslie Ford, and Nancy Geller; Clinical Coordinating Center: Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg; Investigators and Academic Centers: (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (MedStar Health Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Iowa, Iowa City/Davenport, IA) Robert Wallace; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker
Full list of investigators who have contributed to WHI science, please visit: https://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Long%20List.pdf
REFERENCES
- 1.Franklin SS, Gustin IV W, Wong ND, Larson MG, Weber MA, Kannel WB et al. Hemodynamic patterns of age-related changes in blood pressure: the Framingham Heart Study. Circulation 1997; 96: 308–315. [DOI] [PubMed] [Google Scholar]
- 2.Schellinger IN, Mattern K, Raaz U. The Hardest Part: Arterial Stiffness in the Context of Healthy Aging. Arteriosclerosis, thrombosis, and vascular biology 2019; 39: 1301–1306. [DOI] [PubMed] [Google Scholar]
- 3.Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States. US Census Bureau: Hyattsville, MD, 2014. [Google Scholar]
- 4.Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension Prevalence and Control Among Adults: United States, 2015–2016. NCHS data brief, no. 289. National Center for Health Statistics: Hyattsville, MD, 2017. [PubMed] [Google Scholar]
- 5.Barton M, Meyer MR. Postmenopausal hypertension: mechanisms and therapy. Hypertension 2009; 54: 11–18. [DOI] [PubMed] [Google Scholar]
- 6.Yanes LL, Reckelhoff JF. Postmenopausal hypertension. American Journal of Hypertension 2011; 24: 740–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forouzanfar MH, Afshin A, Alexander LT, Anderson HR, Bhutta ZA, Biryukov S et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet 2016; 388: 1659–1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA 2017; 317: 165–182. [DOI] [PubMed] [Google Scholar]
- 9.Huai P, Xun H, Reilly KH, Wang Y, Ma W, Xi B. Physical activity and risk of hypertension: a meta-analysis of prospective cohort studies. Hypertension 2013; 62: 1021–1026. [DOI] [PubMed] [Google Scholar]
- 10.Carnethon MR, Evans NS, Church TS, Lewis CE, Schreiner PJ, Jacobs DR et al. Joint associations of physical activity and aerobic fitness on the development of incident hypertension: coronary artery risk development in young adults. Hypertension 2010; 56: 49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hu G, Barengo NC, Tuomilehto J, Lakka TA, Nissinen A, Jousilahti P. Relationship of physical activity and body mass index to the risk of hypertension: a prospective study in Finland. Hypertension 2004; 43: 25–30. [DOI] [PubMed] [Google Scholar]
- 12.Haapanen N, Miilunpalo S, Vuori I, Oja P, Pasanen M. Association of leisure time physical activity with the risk of coronary heart disease, hypertension and diabetes in middle-aged men and women. International Journal of Epidemiology 1997; 26: 739–747. [DOI] [PubMed] [Google Scholar]
- 13.Pereira MA, Folsom AR, McGovern PG, Carpenter M, Arnett DK, Liao D et al. Physical activity and incident hypertension in black and white adults: the Atherosclerosis Risk in Communities Study. Preventive Medicine 1999; 28: 304–312. [DOI] [PubMed] [Google Scholar]
- 14.Simpson ME, Serdula M, Galuska DA, Gillespie C, Donehoo R, Macera C, Mack K. Walking trends among U.S. adults. American Journal of Preventive Medicine 2003; 25: 95–100. [DOI] [PubMed] [Google Scholar]
- 15.Hays J, Hunt JR, Hubbell FA, Anderson GL, Limacher M, Allen C et al. The Women’s Health Initiative recruitment methods and results. Annals of Epidemiology 2003; 13: S18–S77. [DOI] [PubMed] [Google Scholar]
- 16.WHI Study Group. Design of the Women’s Health Initiative clinical trial and observational study. Controlled Clinical Trials 1998; 19: 61–109. [DOI] [PubMed] [Google Scholar]
- 17.Anderson GL, Manson J, Wallace R, Lund B, Hall D, Davis S et al. Implementation of the Women’s Health Initiative study design. Annals of Epidemiology 2003; 13: S5–S17. [DOI] [PubMed] [Google Scholar]
- 18.Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Journal of the American College of Cardiology 2018; 71: e127–e248. [DOI] [PubMed] [Google Scholar]
- 19.The JNCV 5th report on detection, evaluation and treatment of high blood pressure. Archives of Internal Medicine 1993; 153: 154–183. [PubMed] [Google Scholar]
- 20.Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Medicine & Science in Sports & Exercise 2011; 43: 1575–1581. [DOI] [PubMed] [Google Scholar]
- 21.Meyer A-M, Evenson KR, Morimoto L, Siscovick D, White E. Test-retest reliability of the WHI Physical Activity Questionnaire. Medicine & Science in Sports & Exercise 2009; 41: 530–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pettee Gabriel K, Mcclain JJ, Lee CD, Swan PD, Alvar BA, Mitros MR et al. Evaluation of physical activity measures used in middle-aged women. Medicine & Science in Sports & Exercise 2009; 41: 1403–1412. [DOI] [PubMed] [Google Scholar]
- 23.Langer RD, White E, Lewis CE, Kotchen JM, Hendrix SL, Trevisan M. The Women’s Health Initiative Observational Study: baseline characteristics of participants and reliability of baseline measures. Annals of Epidemiology 2003; 13: S107–S121. [DOI] [PubMed] [Google Scholar]
- 24.Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M et al. Human blood pressure determination by sphygmomanometry. Circulation 1993; 88: 2460–2470. [DOI] [PubMed] [Google Scholar]
- 25.Hays RD, Sherbourne CD, Mazel RM. The RAND 36-item health survey 1.0. Health Economics 1993; 2: 217–227. [DOI] [PubMed] [Google Scholar]
- 26.Guenther PM, Kirkpatrick SI, Reedy J, Krebs-Smith SM, Buckman DW, Dodd KW et al. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. The Journal of Nutrition 2013; 144: 399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patterson RE, Kristal AR, Tinker LF, Carter RA, Bolton MP, Agurs-Collins T. Measurement characteristics of the Women’s Health Initiative food frequency questionnaire. Annals of Epidemiology 1999; 9: 178–187. [DOI] [PubMed] [Google Scholar]
- 28.ClinicalTrials.gov Women’s Health Initiative Strong and Healthy Study (WHISH). https://clinicaltrials.gov/ct2/show/NCT02425345 (accessed 16 Feb 2018).
- 29.Swica Y, Warren MP, Manson JE, Aragaki AK, Bassuk SS, Shimbo D et al. Effects of oral conjugated equine estrogens with or without medroxyprogesterone acetate on incident hypertension in the Women’s Health Initiative hormone therapy trials. Menopause 2018; 25: 753–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.US Department of Health and Human Services. Physical Activity Guidelines for Americans. 2008.
- 31.U.S. Department of Health> and Human Services. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. 2018. [Google Scholar]
- 32.Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Archives of Internal Medicine 1995; 155: 701–709. [PubMed] [Google Scholar]
- 33.Hayashi T, Tsumura K, Suematsu C, Okada K, Fujii S, Endo G. Walking to work and the risk for hypertension in men: the Osaka Health Survey. Annals of Internal Medicine. 1999; 131: 21–26. [DOI] [PubMed] [Google Scholar]
- 34.Williams PT, Thompson PD. Walking versus running for hypertension, cholesterol, and diabetes mellitus risk reduction. Arteriosclerosis, thrombosis, and vascular biology. 2013; 33: 1085–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shephard RJ. Absolute versus relative intensity of physical activity in a dose-response context. Medicine & Science in Sports & Exercise 2001; 33: S400–18. [DOI] [PubMed] [Google Scholar]
- 36.Cornelissen VA, Arnout J, Holvoet P, Fagard RH. Influence of exercise at lower and higher intensity on blood pressure and cardiovascular risk factors at older age. Journal of Hypertension 2009; 27: 753–762. [DOI] [PubMed] [Google Scholar]
- 37.Yates T, Zaccardi F, Dhalwani NN, Davies MJ, Bakrania K, Celis-Morales CA et al. Association of walking pace and handgrip strength with all-cause, cardiovascular, and cancer mortality. European Heart Journal 2017; 38: 3232–3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barlow CE, LaMonte MJ, FitzGerald SJ, Kampert JB, Perrin JL, Blair SN. Cardiorespiratory fitness is an independent predictor of hypertension incidence among initially normotensive healthy women. American Journal of Epidemiology 2005; 163: 142–150. [DOI] [PubMed] [Google Scholar]
- 39.Stefanick ML, Brunner RL, Leng X, Limacher MC, Bird CE, Garcia DO et al. The relationship of cardiovascular disease to physical functioning in women surviving to age 80 and above in the Women’s Health Initiative. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences 2016; 71: S42–S53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Manson JE, Greenland P, LaCroix AZ, Stefanick ML, Mouton CP, Oberman A et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. New England Journal of Medicine 2002; 347: 716–725. [DOI] [PubMed] [Google Scholar]
- 41.Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA. Exercise and hypertension. Medicine & Science in Sports & Exercise 2004; 36: 533–553. [DOI] [PubMed] [Google Scholar]
- 42.Chodzko-Zajko WJ, Proctor DN, Singh MAF, Minson CT, Nigg CR, Salem GJ et al. Exercise and physical activity for older adults. Medicine & Science in Sports & Exercise 2009; 41: 1510–1530. [DOI] [PubMed] [Google Scholar]
- 43.Stewart KJ, Bacher AC, Turner KL, Fleg JL, Hees PS, Shapiro EP et al. Effect of exercise on blood pressure in older persons: a randomized controlled trial. Archives of Internal Medicine 2005; 165: 756–762. [DOI] [PubMed] [Google Scholar]
- 44.Willett WC, Dietz WH, Colditz GA. Guidelines for healthy weight. New England Journal of Medicine 1999; 341:427–434. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.