Abstract
Background
Two out of three family members experience symptoms of posttraumatic stress, depression, or anxiety lasting for months after the ICU stay. Interventions aimed at mitigating these symptoms have been unsuccessful.
Research Question
To understand the emotional experiences of family members of critically ill patients and to identify coping strategies used by family members during the ICU stay.
Study Design
and Methods: As part of a mixed methods study to understand sources of distress among ICU family members, semistructured interviews were conducted with ICU family members. Family members completed surveys at the time of interview and at 90 days to assess for symptoms of depression, anxiety, and posttraumatic stress.
Results
Semistructured interviews and baseline surveys were conducted with 40 ICU family members; 78% of participants (n = 31) completed follow-up surveys at 90 days. At the time of interview, 65% of family members had symptoms of depression, anxiety, or posttraumatic stress. At 90 days, 48% of surveyed family members had symptoms of psychological distress. Three primary emotions were identified among ICU family members: sadness, anger, and fear. A diverse array of coping strategies was used by family members, including problem-solving, information seeking, avoidance/escape, self-reliance, support seeking, and accommodation.
Interpretation
This study emphasizes similarities in emotions but diversity in coping strategies used by family members in the ICU. Understanding the relationship between ICU experiences, emotional responses, and long-term psychological outcomes may guide targeted interventions to improve mental health outcomes of ICU family members.
Key Words: cognitive function, decision-making, depression, ICU, psychology
FOR EDITORIAL COMMENT, SEE PAGE 1305
Family members of patients in the ICU experience significant acute distress. In addition to facing the critical illness of a loved one, family members are asked to make difficult surrogate decisions in an unfamiliar and sometimes overwhelming environment. Months after the ICU experience, two out of three family members of ICU patients experience symptoms of depression, anxiety, or posttraumatic stress.1, 2, 3, 4
Take-home Points.
Study Question: This study aimed to understand the emotional experiences of family members of critically ill patients and to identify coping strategies used by family members during the ICU stay.
Results: Three core emotions (sadness, anger, and fear) were commonly felt by family members of ICU patients, and family members used a diverse array of coping strategies. Two-thirds of family members had symptoms of depression, anxiety, or posttraumatic stress during the ICU stay, and almost one-half of those surveyed still had symptoms at 3 months.
Interpretation: The relationship between ICU experiences, emotions, and coping strategies may be a key target for interventions to reduce symptoms of depression, anxiety, and posttraumatic stress among family members of ICU patients.
Although the presence of these adverse psychological symptoms is well described, the underlying causes of distress, and the coping strategies that might mitigate the development, severity, and impact of symptoms, are poorly understood. This lack of understanding hinders the development of interventions to effectively support family members. For example, trials using diaries, decision aids, communication facilitators, or training programs have not been consistently successful at reducing these symptoms.5, 6, 7, 8, 9, 10
We conducted a mixed methods study to explore emotional experiences and coping strategies of family members of patients in the ICU. Using a mixed methods approach allowed for an in-depth analysis of family member experiences through interviews, within the context of psychological symptoms during and after ICU care. We theorized that multiple sources of distress would impact family members beyond the patient’s critical illness.
Methods
We used a convergent parallel mixed methods study design using interviews and surveys to examine causes of distress among family members of ICU patients. Qualitative interview data were gathered in parallel with baseline and follow-up quantitative survey data from the same participants. Qualitative analysis was initially inductive. We used an interpretive description approach as the methodologic framework for the study, which sought to understand family members’ diverse experiences while also creating practical knowledge for physicians.11 Interpretive description has been used previously for qualitative studies and encompasses inductive analysis, iterative data gathering using constant comparative analysis, data immersion, thematic description, and interpretation.11, 12, 13, 14 Once the larger themes of emotional experiences and coping strategies were identified, we mapped themes to Ekman’s theory,15,16 which categorizes six universal emotions across cultures, and Skinner’s schema,17 which classifies coping strategies based on a systematic review of the coping strategies literature.
Study Participants
The study design was approved by the institutional review board of the University of Michigan Medical School (No. HUM00118718). Family members were recruited between February 2017 and January 2018 from two ICUs at the University of Michigan. Eligible participants were adult family members of patients who received mechanical ventilation in the ICU for at least 72 h. These family members were thought to be more likely to be present at the patient’s bedside, to have had discussions with ICU providers, and because patients on mechanical ventilation have higher mortality than other ICU patients. Maximum variation sampling was used to identify potential participants of varying age, sex, race/ethnicity, and relationship to the patient.18,19
Semistructured Interviews
A semistructured interview guide was created based on a review of the literature and our own clinical experiences (e-Appendix 1). Interviews were aimed at eliciting the subjective experiences of family members in the ICU to explore causes of distress. The interview guide was iteratively refined and pilot tested in a focus group of nine family members with prior ICU experience from the University of Michigan Patient and Family Centered Care Program.
Two investigators (J. M. and T. S. V.) conducted interviews, with each interview typically conducted by a single investigator. Interviews were audio-recorded, transcribed by a medical transcriptionist, checked for data integrity, and imported to Dedoose software (SocioCultural Research Consultants, LLC) to support data organization and analysis. Each interview was coded independently by at least two investigators (J. M., E. P. C., K. L., and T. S. V.) with differences in coding resolved by consensus (see e-Table 1 for the final codebook). The study team met periodically to compare interviews using the constant comparative method, discuss themes, and iteratively revise the code structure (see e-Appendix 2 for additional information). Previously coded interviews were recoded as needed after each major revision. The team also evaluated the depth and breadth of the data elicited in relation to sample size and the study’s exploratory aims. By these criteria and based on existing recommendations for mixed methods research, we estimated the final sample size of 40 to provide adequate information power.20,21
After initial exploratory and descriptive coding of the early interviews, focused coding proceeded around major conceptual themes. To further deep immersion in the data and support comparative analysis, two investigators (J. M. and E. A. H.) wrote case summaries of each interview focusing on patterns within the major themes.
Surveys
Patient age, sex, number of days in the ICU, and number of days on mechanical ventilation were collected at the time of interview. Family members were surveyed twice. The initial survey was administered at the end of each interview and gathered information about symptoms of psychological distress and demographic data. The follow-up survey was conducted approximately 90 days later to assess for symptoms of psychological distress.
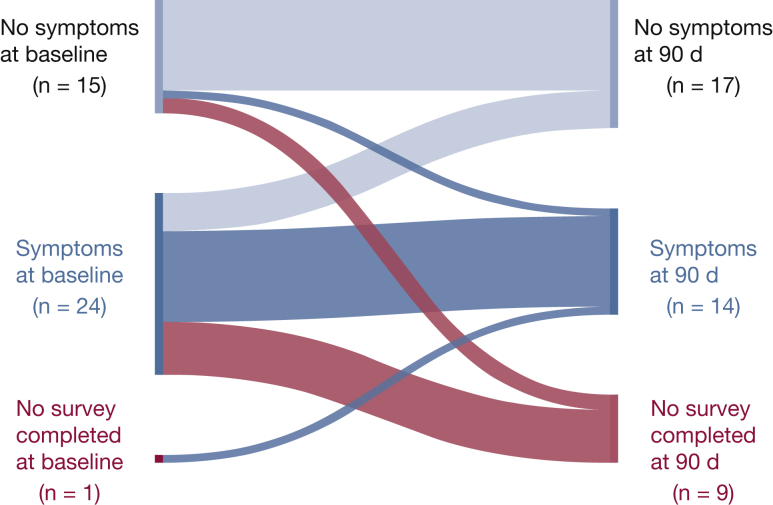
In both the initial and follow-up surveys, participants completed the Hospital Anxiety and Depression Scale to evaluate for symptoms of anxiety and depression.22 Scores range from 0 (no distress) to 21 (maximum distress) with scores ≥ 8 suggesting clinically significant symptoms. The Posttraumatic Stress Disorder Checklist-Civilian Version was used to evaluate for symptoms of posttraumatic stress.23 Because baseline surveys were conducted during the hospital stay, a time point when some family members may still be undergoing acute stress, we used the Posttraumatic Stress Disorder Checklist-Civilian Version because it has been used previously to assess for symptoms of acute stress in the hospital.24 To depict symptoms at baseline and follow-up, a Sankey25 diagram was created using SankeyMATIC (Steve Bogart).
Integration of Qualitative and Quantitative Data
Descriptive statistics were used to summarize the study sample. Initial and follow-up survey data were converted to categorical variables for import to Dedoose and included direction and magnitude of change in measures of distress. Visual mixed methods tools in Dedoose and in Excel (Microsoft, Inc) were used to explore potential patterns linking survey data with the qualitative analysis. Specifically, qualitative and quantitative data were collated by participant and by categorical groups to compare relationships between and among quantitative variables and qualitative themes.
After data were analyzed, member-checking was performed with a focus group of nine family members to help broadly assess the validity of the analysis.26 The focus group included study participants and individuals from the University of Michigan Patient and Family Centered Care Program.
Role of Funding Sources
This study was funded by the Blue Cross Blue Shield of Michigan Foundation, the University of Michigan Pilot and Exploratory Projects in Palliative Care Program, and the National Institutes of Health (to T. S. V.). The funding sources played no role in the design, conduct, or reporting of this study.
Results
Semi-structured interviews were conducted with 40 ICU family members during the ICU stay (Table 1). Thirty-nine family members completed surveys at the time of interview with one initial survey partially completed. Follow-up surveys at 90 days were completed by 78% of participants (n = 31), with surveys completed an average of 92 days (standard deviation, range, 83-101) after the initial interview. ICU family members were predominantly women (70%) and white (69%), with an average age of 52 years. At the time of the follow-up survey, 30% (n = 12) of patients were known to be alive at 3-month follow-up, 48% (n = 19) did not survive, and the remaining 22% (n = 9) were lost to follow-up.
Table 1.
Characteristics of Family Members
| Characteristics | Family Member (n = 40) | Patient (n = 39) |
|---|---|---|
| Age, y | 52 ± 12 | 58 ± 16 |
| Female | 28 (70) | 16 (41) |
| Working full-time | 18 (46) | 5 (13) |
| Four-year college degree | 12 (31) | |
| Race/ethnicity | ||
| White | 27 (69) | |
| Black | 7 (18) | |
| Asian | 3 (8) | |
| Hispanic/Latino(a) | 1 (3) | |
| Black and American Indian or Alaska Native | 1 (3) | |
| Relationship to patient | ||
| Child | 13 (33) | |
| Spouse | 9 (23) | |
| Parent | 6 (15) | |
| Sibling | 6 (15) | |
| Other | 6 (15) |
Values are mean ± SD or No. (%).
At the time of interview, 65% of family members had symptoms of depression, anxiety, or posttraumatic stress (33% had symptoms of depression, 65% had symptoms of anxiety, and 36% had symptoms of posttraumatic stress). Of 31 ICU family members surveyed at 90 days, 48% had symptoms of psychological distress (Fig 1, Table 2), with 13% of family members having symptoms of depression, 29% with symptoms of anxiety, and 39% with symptoms of posttraumatic stress.
Figure 1.
Psychological symptoms in ICU family members at baseline and follow-up.
Table 2.
Symptoms of Depression, Anxiety, or Posttraumatic Stress at Baseline and Follow up
| Psychological Symptomsa | Baselineb | Follow-upb |
|---|---|---|
| Depression | 6 (33) | 4 (13) |
| Anxiety | 15 (65) | 9 (29) |
| Posttraumatic stress | 14 (36) | 12 (39) |
| Total | 26 (65) | 15 (48) |
Values are No. (%). HADS = Hospital Anxiety and Depression Scale; PCL-C = Post-Traumatic Stress Disorder Checklist-Civilian Version.
Psychological symptoms were assessed using the HADS and the PCL-C. Scores on HADS ≥ 8 indicate clinical symptoms. PCL-C scores ≥ 31 indicate acute or posttraumatic stress.
Baseline symptoms were assessed at time of ICU interview. Follow-up symptoms were assessed approximately 90 d after initial interview.
Emotional Experiences
During interviews, family members described a range of emotional experiences, and three primary emotions were identified: sadness, anger, and fear. Sadness was the most common emotion identified, followed by anger and fear. The other primary emotions within Ekman’s theory (disgust, happiness, and surprise) were not commonly described by family members. Although emotions experienced by ICU family members were similar, family members described very different experiences that resulted in these emotions.
Sadness
Sadness was prominent in family member interviews, and sources of sadness included seeing the patient critically ill, facing a future of chronic critical illness, feelings of regret and guilt, making decisions as a surrogate decision-maker, and anticipating loss. Seeing the patient often evoked sadness: “It was hard to see how rough the breathing machine was with her. That made me feel sad” (participant 2). Seeing stability, without improvement or decline, was distressing to some family members. For example, “The lack of change is the worst part…you can feel your hope is kind of extinguished…the sameness every day, being exactly the same is brutal. That’s depressing” (participant 1). When discussing end-of-life surrogate decision-making, one family member remarked “It’s hard to make those decisions…it’s hard to say goodbye” (participant 17). Regret and guilt were common themes related to sadness. As one family member noted, “Gosh, I could have spent more time” (participant 29). Family members also anticipated loss: “Whenever God sees fit, that person’s gone, and you won’t see them until you’re gone…It’s just so depressing because people aren’t replaceable” (participant 14).
Anger
Family members described varied sources of anger, particularly related to experiences with ICU staff, hospital facilities, the patient, other family members, and themselves. As one participant explained, “You’re kind of weighing between sad, woe is me, and angry that you’re there, and like angry at him, angry at me, angry at everyone for being in that position” (participant 1). Inadequate communication with ICU staff appeared to be a source of anger. For example, “I would have wanted more information…if they would have just taken a couple minutes” (participant 18). Family members also felt angry when they thought staff were not listening to them. One objected, “Don’t treat me like I’m an imbecile” (participant 25). Some family members thought staff were not respecting the patient’s wishes, for example, “I understand that they’re looking at it from a medical aspect and a logical aspect, but we’re looking at it from emotional, logical, and medical” (participant 38). Some ICU family members directed anger toward other family members: “We told them, ‘you’re not here for him…you’re here for you because you feel bad because you haven’t seen him’” (participant 11). Family members also expressed frustration about lack of adequate ICU waiting room space.
Fear
Sources of fear included uncertainties of the future, seeing their loved one as critically ill, and thinking about how their life would change as a result of their family member’s critical illness. Many family members expressed fear about the future: “My worst fear is for [the medical team] to walk in and say, ‘Nothing more we can do’” (participant 37). Seeing the patient in the ICU setting was a fearful experience for many family members. For example, “When I came up here, I saw that she was hooked up to the ventilator…I’m thinking, ‘Oh Lord. This is it’” (participant 34). Some family members described fears about how the patient’s illness would adversely affect them: “How am I supposed to sustain…her benefits is [sic] a big key in how we’ve been able to sustain” (participant 14). Fear of the unknown was a common experience: “The fear is something’s gonna happen, and we know it happens fast, so I’m never gonna get back in time” (participant 5) and “Not knowing just tears you up inside” (participant 17).
Coping Strategies
Family members reported diverse strategies to cope with distress in the ICU. Using the coping strategy classification system of Skinner et al,17 we found isolated examples of all 12 coping strategies across all interviews that were distilled into six core coping strategies used by ICU family members: problem-solving, information seeking, avoidance/escape, self-reliance, support seeking, and accommodation (Table 3). Problem-solving and information seeking were described together because the coping strategies were related.
Table 3.
Coping Strategies Used by ICU Family Members
| Coping Strategy/Style of Coping | Example(s) From ICU Family Members |
|---|---|
| Problem-solving | |
| Strategizing | Talking through concerns |
| Instrumental action | Involvement in patient care Advocacy |
| Planning | Making tentative funeral plans Discussing advance directives |
| Information seeking | |
| Reading | Of the internet, laboratory results, electronic medical record |
| Observation | Of staff, patient, monitors |
| Asking others | Asking staff or other family members for information Seeking to know what is happening when it is happening Preference for having information, whether good or bad news |
| Helplessness | |
| Cognitive interference | Forgetting to take daily medication |
| Cognitive exhaustion | Difficulty concentrating at work |
| Avoidance/escape | |
| Cognitive avoidance | Pushing away thoughts of the future, or of death Deferment (ie, “taking it a day at a time”) Not making plans; not thinking about future decisions until required |
| Behavioral avoidance | Avoiding rounds, conflict, certain staff, seeing other patients |
| Wishful thinking | Seeking hope from staff, through prayer Belief in miracles Managing hope by balancing with realism Hoping medical crisis will lead to better self-care |
| Self-reliance | |
| Strength | Relying on one’s own inner strength |
| Emotion regulation | Emotional containment, stoicism Avoiding crying in front of others or for fear of not being able to stop Hopefulness; creating positive atmosphere Avoiding getting hopes up |
| Emotional expression | Crying readily, or after a period of containment Laughter and humor |
| Behavior regulation | Food: eating, getting guest trays, going to restaurants, taking supplements Sleep: returning home to sleep, getting hotel room, leaving patient’s room to sleep Exercise and relaxation: walking, going outdoors, seeing sights, meditation |
| Behavioral expression | Physically destructive behavior as substitute for emotional venting |
| Emotional approach/anticipation | Anticipating an emotional rollercoaster Not wanting “sugar-coated” information |
| Support seeking | |
| Contact seeking | Seeking company, proximity to people Seeking personable interactions with staff Social media, phone, text, and e-mail |
| Comfort seeking | Mutual support, keeping each other motivated Seeking out staff members who bring comfort |
| Instrumental aid | Fundraising or logistical support from coworkers, employers, friends Family members taking turns being at hospital, or communicating news to other family Transportation assistance |
| Spiritual support | Clergy, chaplain, faith community, prayers of others, scripture reading Own faith, prayer, meditation Belief in miracles, in healing power of positivity, or that God will provide |
| Isolation | |
| Seeking solitude | Finding a place in the hospital or elsewhere to be alone |
| Avoiding others | Avoiding hostile relatives Drawing patient room curtains |
| Accommodation | |
| Distraction | Reading for pleasure, talking, joking, working |
| Cognitive restructuring | Reframing, rationalizing, or reasoning as a means of self-calming Adjusting expectations or anticipating cognitive adjustments |
| Acceptance | Fatalism, or surrender to “God’s plan” Ceasing to worry about what is not under one’s control Choosing to trust (hospital, staff, one’s own decisions) |
| Normalization | Keeping up normal routines at home, and with children |
| Deference | Putting own needs second to patient, staff, other family Seeking to please staff in hopes of receiving better patient care |
| Negotiation | |
| Bargaining | Asking staff for more time to make decisions |
| Persuasion | Advocating for patient or self Persuading family members or staff during decision-making |
| Priority setting | Prioritizing advocacy for patient over self-advocacy Communicating patient care priorities to staff Deferring problems that can be addressed later |
| Submission | |
| Intrusive thoughts | Thoughts of patient “popping out” while trying to do something else |
| Opposition | Physical or verbal aggression with staff or other family |
Problem-solving and Information Seeking
Family members often advocated for the patient, served in surrogate decision-making roles, and preferred to know as much information as possible, saying that even bad news was “better than not knowing” (participant 17). Many family members asked staff questions or learned about health conditions online. Family members noted that they observed staff in the ICU to learn about the different providers and their roles, sometimes to gain confidence before leaving the patient’s bedside.
Avoidance/Escape
Family members commonly used delayed emotional processing while in the ICU as a means of protecting themselves emotionally while still making decisions. Many family members described how they “take it one day at a time.” Delaying emotional processing of potential adverse outcomes may be adaptive in the acute context of the ICU because family members in the ICU are often experiencing a short-term crisis with hope of a positive resolution to this crisis over the long-term. Many family members described feeling hopeful, including one family member who expressed, “I’m a firm believer in until you take your last breath, there’s hope” (participant 28). Others sought hope through signals from staff, trust in staff, or trust in their own decisions.
Self-reliance
Many family members thought it was their role to withhold their emotions from others to maintain a positive atmosphere. As one participant stated, “I’m alright. I’m not supposed to feel” (participant 39). Conversely, other family members described emotional expression as a coping strategy. As one family member described: “A moment of joy, a moment of humor, or something that makes you just smile…When you find those, that’s when you can process a little bit better” (participant 35). Another family member described releasing pent-up anger by blowing up a boat (participant 30). Others prioritized sleep and exercise.
Support Seeking
Family members commonly depended on social and spiritual support. One participant said “I’d probably have a nervous breakdown” if she did not have her family’s emotional support (participant 3). Another described feeling a sense of peace after accepting that her family member’s illness was out of her control. Family members sought out staff or members of their faith community for support.
Accommodation
Family members tended to adjust their expectations after experiencing a patient’s critical illness, such as viewing cancer not as a death sentence, but a “battle.” Maintaining a sense of normalcy was described by family members who continued routines at home despite their loved one being critically ill.
Integration of Qualitative and Quantitative Data
Common themes from qualitative interview data were integrated with survey data using visual mixed methods tools in Dedoose and Excel to explore potential patterns linking qualitative analysis with survey data. Nearly all participants, regardless of the presence of symptoms, discussed sadness, anger, and coping strategies during the interview. In contrast, fear or anxiety was discussed among all participants with symptoms but was not universally discussed by participants without symptoms.
Discussion
Three core emotions (sadness, anger, and fear) were commonly felt by family members of ICU patients, despite diverse experiences leading to these emotions. Six major coping strategies were common among family members: problem-solving, information seeking, avoidance/escape, self-reliance, support seeking, and accommodation. Two-thirds of family members had symptoms of depression, anxiety, or posttraumatic stress during the ICU stay, and almost one-half of those surveyed at 3 months still had symptoms. Although rates of posttraumatic stress increased slightly at follow-up, rates of anxiety and depression at follow-up were about one-half of rates during the ICU stay, demonstrating that these symptoms may resolve for some but persist for others.
A mixed methods approach was used to combine rich perspectives of family members with quantitative outcomes of psychological symptoms both during and after the ICU stay. This approach permitted the description of lived experiences via qualitative data while also quantifying the burden of psychological symptoms via surveys, representing a complex and rich discussion of how the ICU impacts families. The quantitative analysis found that nearly one-half of ICU family members had symptoms of depression, anxiety, or posttraumatic stress 90 days after the initial ICU interview. The qualitative analysis demonstrated that there are core emotions commonly experienced by ICU family members and that there are a diverse set of strategies used by these family members to cope with emotions. Although these data are interesting individually, the integration of quantitative and qualitative data found no meaningful patterns related to emotional experiences and coping strategies within the context of symptoms of psychological distress. This may be because of the nature of the study design, which started with a broad, inductive qualitative analysis. Subsequent studies may consider sampling based on prespecified hypotheses related to particular emotions or coping strategies of interest.
Several interventions have aimed at reducing symptoms of psychological distress among ICU family members, including diaries, training programs, decision aids, or communication facilitators.5, 6, 7, 8, 9, 10 Results from these trials have been equivocal, and there exists no obvious strategy that physicians can use to reduce psychological symptoms among family members.
Our results provide a foundation for improving future interventions. For example, previous interventions may have been unsuccessful because they focused on promoting emotional processing.5, 6, 7, 8, 9, 10 We found that delayed emotional processing, or “taking it a day at a time,” was a common strategy used by family members. ICU physicians should remain open to the strategies used by family members to cope with stress and emotions even though certain coping strategies may run counter to common practices and beliefs among ICU physicians. Understanding the context of a family member’s emotional response and coping strategies is critical for providers to support family members during the ICU experience. Additionally, the individuality of coping strategies used by family members should be taken into account when designing future interventions to reduce ICU family member distress.
This study must be interpreted in the context of several limitations. Participants in our study were sampled to elicit diverse perspectives; therefore, the ICU family members in this study may not be representative of all ICU family members. Family members were recruited from the bedside of patients on mechanical ventilation at a single academic institution. Experiences of these family members may differ from other family members. Certain factors that could influence the development of adverse psychological outcomes, such as the extent of social support, presence of other life stressors, or the possibility of preexisting psychological illness, may have been uncaptured if not brought up during the interview. Family members were surveyed after the interview, which could have influenced survey results. Additionally, most family members who did not follow-up had symptoms at baseline. It is possible that the presence of symptoms at baseline affected decisions to participate in follow-up.
Interpretation
This study has important implications for patients, family members, and physicians. Interventions seeking to prevent or reduce adverse psychological symptoms among family members of ICU patients have largely been unsuccessful. This work highlights mechanisms for the development of these symptoms and provides potential targets for new interventions.
The diverse emotional experiences of family members of ICU patients often revolve around three core emotions: sadness, anger, and fear. Family members used certain coping strategies that may counter common practices of ICU physicians. The relationship between ICU experiences, emotions, and coping strategies may be a key target for interventions to reduce symptoms of depression, anxiety, and posttraumatic stress among family members of ICU patients.
Acknowledgments
Author contributions: T. S. V. is the study guarantor. T. S. V. contributed to study concept and design, and obtained funding. J. M. and T. S. V. contributed to acquisition of data. E. A. H., J. M., E. P. C., K. L., and T. S. V. contributed to analysis and interpretation of data. E. A. H., J. M., and T. S. V. contributed to drafting of the manuscript. E. A. H., J. M., D. K. C., A. F., T. J. I., E. P. C., K. L., and T. S. V. contributed to critical revision of the manuscript for important intellectual content.
Financial/nonfinancial disclosures: None declared.
Role of sponsors: The funding organizations had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Other contributions: This manuscript does not necessarily represent the view of the US Government or the Department of Veterans Affairs.
Additional information: The e-Appendixes and e-Table can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: This work was supported by the Blue Cross Blue Shield of Michigan Foundation, the University of Michigan Pilot and Exploratory Projects in Palliative Care Program, and the National Institutes of Health [Grant K23 HL140165].
Supplementary Data
References
- 1.Pochard F., Azoulay E., Chevret S. Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med. 2001;29(10):1893–1897. doi: 10.1097/00003246-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Azoulay E., Pochard F., Kentish-Barnes N. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 3.Lemiale V., Kentish-Barnes N., Chaize M. Health-related quality of life in family members of intensive care unit patients. J Palliat Med. 2010;13(9):1131–1137. doi: 10.1089/jpm.2010.0109. [DOI] [PubMed] [Google Scholar]
- 4.Hopkins R.O. Emotional processing/psychological morbidity in the ICU. In: Netzer G., editor. Families in the Intensive Care Unit. Springer International Publishing; Cham, Switzerland: 2018. pp. 31–47. [Google Scholar]
- 5.Garrouste-Orgeas M., Flahault C., Vinatier I. Effect of an ICU diary on posttraumatic stress disorder symptoms among patients receiving mechanical ventilation: a randomized clinical trial. JAMA. 2019;322(3):229. doi: 10.1001/jama.2019.9058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cox C.E., White D.B., Hough C.L. Effects of a personalized web-based decision aid for surrogate decision makers of patients with prolonged mechanical ventilation: a randomized clinical trial. Ann Intern Med. 2019;170(5):285. doi: 10.7326/M18-2335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cox C.E., Hough C.L., Carson S.S. Effects of a telephone- and web-based coping skills training program compared with an education program for survivors of critical illness and their family members. A randomized clinical trial. Am J Respir Crit Care Med. 2018;197(1):66–78. doi: 10.1164/rccm.201704-0720OC. [DOI] [PubMed] [Google Scholar]
- 8.Carson S.S., Cox C.E., Wallenstein S. Effect of palliative care-led meetings for families of patients with chronic critical illness: a randomized clinical trial. JAMA. 2016;316(1):51. doi: 10.1001/jama.2016.8474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White D.B., Angus D.C., Shields A.-M. A randomized trial of a family-support intervention in intensive care units. N Engl J Med. 2018;378(25):2365–2375. doi: 10.1056/NEJMoa1802637. [DOI] [PubMed] [Google Scholar]
- 10.Curtis J.R., Downey L., Back A.L. Effect of a patient and clinician communication-priming intervention on patient-reported goals-of-care discussions between patients with serious illness and clinicians: a randomized clinical trial. JAMA Intern Med. 2018;178(7):930. doi: 10.1001/jamainternmed.2018.2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thorne S. 2nd ed. Routledge; New York, NY: 2016. Interpretive Description: Qualitative Research for Applied Practice. [Google Scholar]
- 12.Thorne S. Data analysis in qualitative research. Evid Based Nurs. 2000;3:68–70. [Google Scholar]
- 13.Srivastava P., Hopwood N. A practical iterative framework for qualitative data analysis. Int J Qual Methods. 2009;8(1):76–84. [Google Scholar]
- 14.Sandelowski M., Barroso J. Classifying the findings in qualitative studies. Qual Health Res. 2003;13(7):905–923. doi: 10.1177/1049732303253488. [DOI] [PubMed] [Google Scholar]
- 15.Ekman P. Universals and cultural differences in facial expression of emotion. In: Cole J., editor. Nebraska Symposium on Motivation. University of Nebraska Press; Lincoln, NE: 1972. pp. 207–283. [Google Scholar]
- 16.Ekman P., Friesen W.V., Ellsworth P. What emotion categories or dimensions can observers judge from facial behavior? In: Ekman P., editor. Emotion in the Human Face. Cambridge University Press; New York, NY: 1982. pp. 39–55. [Google Scholar]
- 17.Skinner E.A., Edge K., Altman J., Sherwood H. Searching for the structure of coping: a review and critique of category systems for classifying ways of coping. Psychol Bull. 2003;129(2):216–269. doi: 10.1037/0033-2909.129.2.216. [DOI] [PubMed] [Google Scholar]
- 18.Davidson J.E., Aslakson R.A., Long A.C. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45(1):103–128. doi: 10.1097/CCM.0000000000002169. [DOI] [PubMed] [Google Scholar]
- 19.Braun U.K., Beyth R.J., Ford M.E., McCullough L.B. Voices of African American, Caucasian, and Hispanic surrogates on the burdens of end-of-life decision making. J Gen Intern Med. 2008;23(3):267–274. doi: 10.1007/s11606-007-0487-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malterud K., Siersma V.D., Guassora A.D. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–1760. doi: 10.1177/1049732315617444. [DOI] [PubMed] [Google Scholar]
- 21.Creswell J.W., Plano Clark V.L. 3rd ed. SAGE; Los Angeles, CA: 2018. Designing and Conducting Mixed Methods Research. [Google Scholar]
- 22.Zigmond A., Snaith R. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 23.Weathers F.W., Litz B.T., Keane T.M., Palmieri P.A., Marx B.P., Schnurr P.P. 2013. The PTSD Checklist for DSM-5 (PCL-5)https://www.ptsd.va.gov/professional/assessment/documents/PCL5_criterionA_form.PDF Accessed July 13, 2020. [Google Scholar]
- 24.Davydow D.S., Zatzick D., Hough C.L., Katon W.J. In-hospital acute stress symptoms are associated with impairment in cognition 1 year after intensive care unit admission. Ann Am Thorac Soc. 2013;10(5):450–457. doi: 10.1513/AnnalsATS.201303-060OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bogart S. SankeyMATIC. http://www.sankeymatic.com/ Accessed January 9, 2020.
- 26.Creswell J.W., Miller D.L. Determining validity in qualitative inquiry. Theory Pract. 2000;39(3):124–130. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.