Abstract
Purpose
To investigate the effect of the coronavirus disease 2019 (COVID-19) pandemic on the clinical presentation of acute, primary rhegmatogenous retinal detachment (RRD).
Design
Single-center, consecutive case series with historical controls.
Participants
Consecutive patients seeking treatment for primary RRD in a 50-day period during the COVID-19 pandemic (March 9–April 27, 2020) and the corresponding 50-day period during the previous year (March 4–April 22, 2019) in the United States.
Methods
The cohorts were compared to assess demographic variables and clinical presentations. Multivariate logistic regression was used to identify factors predictive of presenting macular attachment status.
Main Outcome Measures
The primary outcome was the proportion of patients with macula-on RRD at presentation. Secondary outcomes included visual acuity (VA), duration of symptoms before presentation, proportion seeking treatment within 1 day of symptom onset, and presence of primary proliferative vitreoretinopathy (PVR).
Results
Eighty-two patients were included in the 2020 cohort compared with 111 patients in the 2019 primary control cohort. Demographic factors were similar between the groups. Significantly fewer patients demonstrated macula-on RRD in the 2020 cohort (20/82 patients [24.4%]) than in the 2019 cohort (55/111 patients [49.5%]; P = 0.001). Patients in the 2020 cohort showed worse median VA at presentation (1.00 logarithm of the minimum angle of resolution [logMAR; Snellen equivalent, 20/200] in 2020 vs. 0.48 logMAR [Snellen equivalent, 20/60] in 2019; P = 0.008), fewer patients sought treatment within 1 day of symptoms (16/80 patients [19.5%] in 2020 vs. 41/106 patients [36.9%] in 2019; P = 0.005), and a greater proportion demonstrated primary PVR (11/82 patients [13.4%] in 2020 vs. 5/111 patients [4.5%] in 2019; P = 0.03). In multivariate analysis, younger age (P = 0.03) and established patient status (P = 0.02) were independent predictors of macula-on status in the 2020 cohort.
Conclusions
Patients with primary RRD during the 2020 COVID-19 pandemic were less likely to have macula-on disease and more likely to delay seeking treatment and to show worse vision and PVR.
Keywords: COVID-19, Retinal detachment
Abbreviations and Acronyms: COVID-19, coronavirus disease 2019; logMAR, logarithm of the minimum angle of resolution; PVR, proliferative vitreoretinopathy; RRD, rhegmatogenous retinal detachment; VA, visual acuity
Coronavirus disease 2019 (COVID-19) is the result of a zoonotic virus spread by human-to-human transmission and was declared a pandemic by the World Health Organization on March 11, 2020.1 In the United States, the pandemic has strained healthcare resources and has led to stay-at-home orders with the closure of nonessential activities, including nonurgent healthcare services.2 In addition to those patients directly infected, the outbreak also has impacted patients seeking care for medical problems for a variety of reasons that are unrelated to COVID-19. Closure or curtailment of physician office hours, restriction of elective procedures, and postponement of preventative health visits have reduced patients’ access to health professionals. At the same time, patients’ concerns for exposure, coupled with distancing measures, may have led patients to stay at home even when an acute medical condition develops. Tam et al3 suggested that patients who experienced myocardial infarctions in Southern China had delayed seeking treatment during the COVID-19 pandemic. Groups in the United States and Spain also found a decreased number of ST-elevation myocardial infarctions, postulating that the gap in cases may represent delayed care.4, 5, 6 Schirmer et al7 showed that patients with acute cerebrovascular accidents during the pandemic had delayed seeking treatment and had a longer duration of symptoms when compared with a control group.
We sought to evaluate whether these systemic factors have led to delayed ophthalmic care, using rhegmatogenous retinal detachment (RRD) as the index disease. Macula-threatening RRD is an urgent ophthalmic condition and may result in significant vision loss. Importantly, the visual prognosis of patients with RRD partially depends on macular status. Both delay in presentation and delay in surgical repair of macula-off retinal detachments are associated with worse visual acuity (VA) and surgical outcomes.8, 9, 10, 11 Prior studies have suggested that a delay of 7 days can lead to worse visual outcomes, whereas some recent studies have suggested that a delay in even 3 days leads to worse VA outcomes.12 , 13 The purpose of this study was to investigate the effect of the initial COVID-19 pandemic on the clinical presentation of acute, primary RRD to a tertiary referral-based retina subspecialty practice setting.
Methods
This investigation was a retrospective cohort study of patients undergoing evaluation and repair of acute, primary RRD by Mid Atlantic Retina/Retina Service of Wills Eye Hospital, Philadelphia, Pennsylvania. This retina service is a multiprovider, multilocation practice that spans the Philadelphia metropolitan area and includes the 24-hour Wills Eye emergency room. All patients seeking treatment over a 50-day period during the COVID-19 pandemic (March 9–April 27, 2020) were included. This period was selected because it begins on the week that COVID-19 was declared a pandemic by the World Health Organization. The 2019 historical control group includes all patients seeking treatment during a corresponding 50-day period the previous year (March 4–April 22, 2019), encompassing an identical range of weekdays. A secondary, 2018 historical control group includes all patients seeking treatment during a corresponding 50-day period in 2018 (March 5–April 23, 2018). Twenty-five physicians completed preoperative evaluation in 2020, 22 did so in 2019, and 23 did so in 2018. Eighteen of the physicians were the same from 2019 to 2020. Patients were excluded if they had history of previous retinal detachment in the same eye or if they had chronic symptomatic vision loss for more than 30 days, because onset would have been before the pandemic. Only the first eye was included for any patients with bilateral RRD in the same period. The study received institutional review board approval, adhered to the tenets of the Declaration of Helsinki, and complied with the Health Insurance Portability and Accountability Act. Informed consent was waived per Institutional Review Board protocol.
Detailed demographic, preoperative, and intraoperative data were collected during electronic health record review. Race was self-identified with categories of “White or Caucasian,” “Black or African American,” “Asian or Pacific Islander,” “Native American or Alaskan Native,” “Decline to specify,” or “Other.” Patients’ median regional income was used as a quantitative surrogate for socioeconomic status, tabulated from the American Communities Survey 2017 of median income by zip code. Patients were subdivided based on whether they had established care with the practice previously. A patient was considered established if the patient had been seen by the retina practice previously within a 3-year period before presentation; otherwise, the patient was considered to be “new.” The distance that patients lived from the site of surgical repair was calculated based on the latitude and longitude difference between the patient’s zip code and Wills Eye Hospital.
The primary outcome was the proportion of patients demonstrated macula-on RRD, as opposed to macula-off RRD (defined as the presence of subfoveal fluid) on preoperative clinical evaluation. Secondary outcomes included presenting Snellen VA, proportion of patients with symptom duration of less than 1 day, mean duration of RRD symptoms (vision loss, flashes, floaters, or visual field defect), and the presence of grade C or higher primary proliferative vitreoretinopathy (PVR). The historical control group from 2019 was used as a comparator for all primary and secondary outcomes. The secondary control group from 2018 was compared with the 2019 primary control group to establish the reproducibility of patient characteristics. It was decided a priori that outcomes between the 2018 and 2020 groups would not be compared directly to avoid multiple testing bias.
IBM SPSS software version 26 (IBM Corporation, Armonk, NY) was used for statistical analysis. Snellen VAs were converted to the logarithm of the minimum angle of resolution (logMAR) scale for all statistical analyses. An acuity of counting fingers was converted to 2, and one of hand movements was converted to 3, as described previously.14 For comparison of categorical variables between the two cohorts, including the primary outcome of macula status, a 2-tailed Fisher exact test was used. Normality of the quantitative variables, logMAR VA, and duration of symptoms was assessed using the Shapiro-Wilk test. Because both were found to be nonnormal, a Mann–Whitney U test was used for comparison of distributions. Multivariate logistic regression analysis was performed to assess for predictors of macula status controlling for all available demographic factors: age, median regional income, established patient status, gender, and race. A multivariate stepwise model was used to identify relevant demographic variables with a probability to enter of less than 0.05 and a probability to remove of more than 0.10. A P value of less than 0.05 was considered statistically significant.
Results
A total of 82 patients sought treatment for primary RRD during the 2020 pandemic period, whereas 111 and 103 patients sought treatment for primary RRD during the corresponding 2019 and 2018 control periods, respectively. The patient-reported duration of symptoms was available from chart review for 80 of the 82 patients in the 2020 cohort, 106 of the 111 patients in the 2019 control cohort, and all 103 of the patients in the 2018 control cohort.
Patient Demographics between Cohorts
No significant differences were found in presenting age, gender, proportion of patients identifying as White, mean regional household income, established patient status, and mean geographic distance among the 2020, 2019, and 2018 cohort groups (Table 1 ). The vast majority of patients self-identified as White in each cohort, with less than 10% identifying with any other category, with no statistically significant difference. Two traveling patients in the 2019 cohort (one from South Carolina and the other from the United States Virgin Islands) and 1 traveling patient in the 2018 cohort (from Minnesota) had home addresses of more than 500 miles from the practice location and were excluded from geographic distance analysis. The 2020 cohort did not include any traveling patients.
Table 1.
Baseline Characteristics of Patients with Rhegmatogenous Retinal Detachment Seeking Treatment during the 2020 Coronavirus Disease 2019 Pandemic, Those in the Primary 2019 Control Cohort, and Those in the Secondary 2018 Control Cohort
| 2018 Control | 2019 Control | 2020 Cohort | |
|---|---|---|---|
| No. of patients | 103 | 111 | 82 |
| Male gender (%) | 67.0 | 62.2 | 68.3 |
| Age (yrs), mean ± SD | 56.3 ± 14.5 | 59.0 ± 13.5 | 58.5 ± 13.3 |
| White race (%) | 82.5 | 80.1 | 85.4 |
| Mean zip code-derived median regional income (USD), mean ± SD | 76 265 ± 24 973 | 79 859 ± 27 910 | 74 598 ± 23 279 |
| Established patient (%) | 17.5 | 23.4 | 18.3 |
| Distance from repair site (miles), mean ± SD | 22.9 ± 18.7 | 26.5 ± 24.6 | 23.4 ± 23.4 |
SD = standard deviation; USD = United States dollars.
No significant differences were found in demographic characteristics between the 2018 and 2019 control cohorts or between the 2019 control and 2020 pandemic cohorts.
Retinal Detachment Characteristics
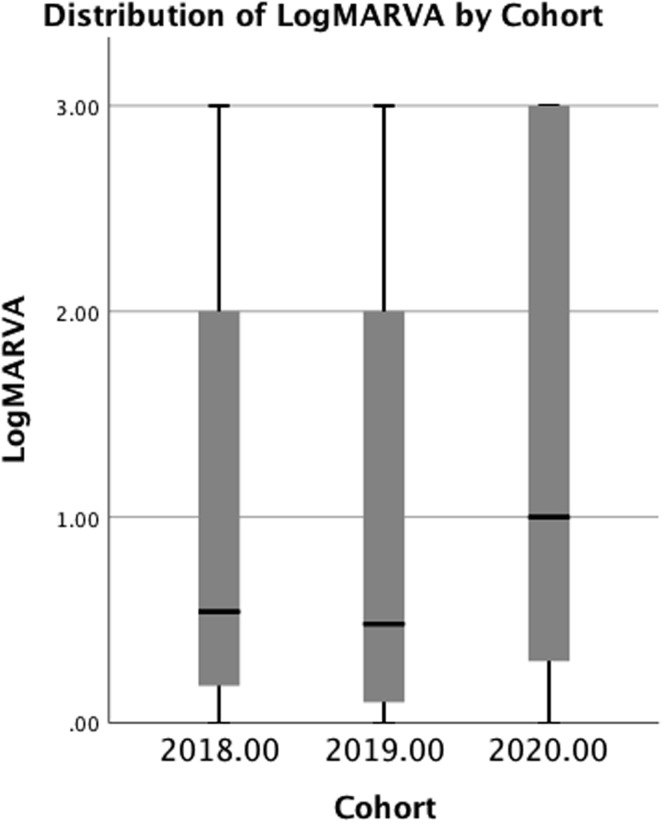
We compared the 2018 and 2019 control cohorts to evaluate for consistency in yearly presentation of RRD characteristics. No difference was found with respect to any of the primary or secondary outcomes between the 2018 and 2019 control cohorts (Fig 1 ; Table 2 ). Significantly fewer patients in the 2020 cohort demonstrated macula-on RRD during the pandemic (20 patients [24.4%]) compared with the 2019 cohort (55 patients [49.5%]; Table 2; P = 0.001). No significant difference was found in the overall distribution of the duration of symptoms in the 2020 pandemic group (median, 5.50 days; range, <1 day–1 month) compared with the 2019 control group (median, 4.00 days; range, <1 day–1 month; P = 0.06). However, fewer patients sought treatment within 1 day of symptoms in the 2020 cohort (16 patients [19.5%]) compared with the 2019 control cohort (41 patients [36.9%]; P = 0.005). Median presenting VA was worse in the pandemic 2020 cohort (1.00 logMAR; Snellen equivalent, 20/200) compared with the 2019 control group (0.48 logMAR; Snellen equivalent, 20/60; P = 0.008; Fig 1). Finally, more patients in the 2020 cohort demonstrated primary grade C PVR or higher at presentation (11 patients [13.4%]) compared with the 2019 control group (5 patients [4.5%]; P = 0.03).
Figure 1.
Box-and-whisker plot illustrating distribution of presenting logarithm of the minimum angle of resolution (logMAR) visual acuity (VA) in each cohort. The dark line depicts the median and the boxes depict the interquartile range. No significant difference was found in the distributions between the 2019 and 2018 control cohorts. Median VA in the 2020 cohort distribution was significantly worse than the 2019 cohort distribution (P = 0.008).
Table 2.
Presenting Characteristics of Rhegmatogenous Retinal Detachment in the 2020 Coronavirus Disease 2019, 2019 Primary Control, and 2018 Secondary Control Groups
| 2018 Control | 2019 Control | 2020 Cohort | |
|---|---|---|---|
| No. of patients | 103 | 111 | 82 |
| Macula-on disease (%) | 44.7 | 49.5 | 24.4 |
| VA (logMAR), median (interquartile range) | 0.54 (0.18–2.00) | 0.48 (0.10–2.00) | 1.00(0.3–3.00) |
| Duration of symptoms (days), median (interquartile range) | 3 (1–7) | 4 (1–7) | 5.5 (2–7) |
| Seeking treatment within 1 day of symptom onset (%) | 43.7 | 38.7 | 20.0 |
| Primary PVR (%) | 3.8 | 4.5 | 13.4 |
logMAR = logarithm of the minimum angle of resolution; PVR = proliferative vitreoretinopathy; VA = visual acuity.
No difference was found in the presenting characteristics between the 2018 and 2019 control groups. A significant decrease was found in patients with macula-on disease at presentation (P < 0.001), a significant decrease was found in the proportion of patients seeking treatment within 1 day of symptoms (P = 0.005), and significant increase was found in the proportion of patients with primary PVR at presentation (P = 0.03) in the 2020 cohort compared with the 2019 control group. The median logMAR VA was worse for the 2020 cohort compared with the 2019 control group, with a significant difference in distributions (P = 0.008). P < 0.05 significance shown in boldface.
Demographic Predictors of Macula Status
A multivariate logistic regression analysis, including age, gender, race, mean household income, and established patient status, was used to identify predictors of macula status. In the 2019 control cohort, none of these factors were associated with macula status. In the 2020 cohort, both younger age (P = 0.03) and established patient status (P = 0.02) were predictive of macula-on RRD, whereas White race, regional household income, and gender were not.
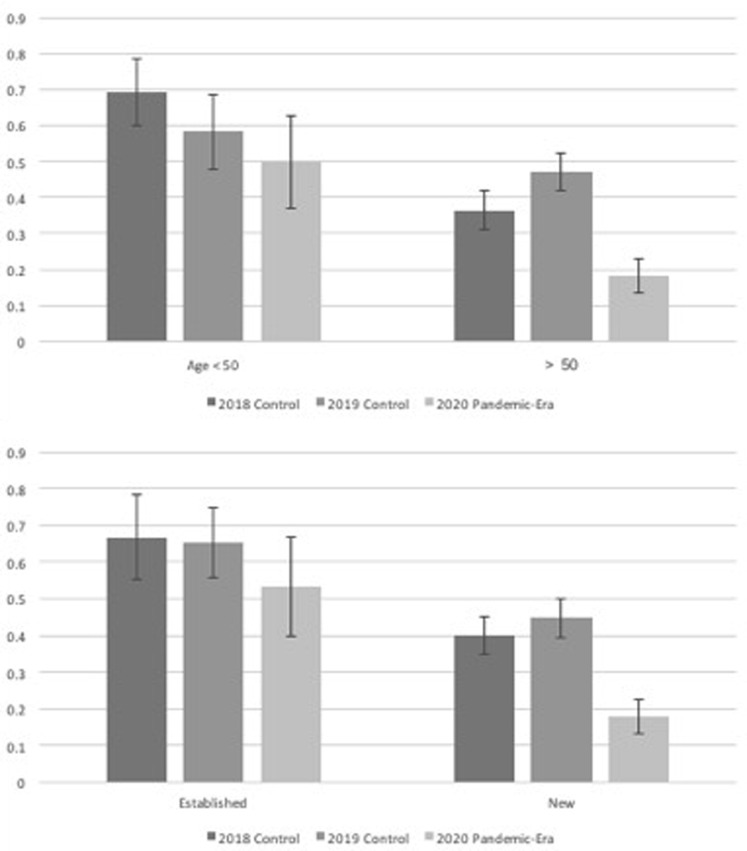
Age Subgroups
We next analyzed differences in RRD presentation between younger and older age groups. When evaluating the subgroup of patients older than 50 years, significantly fewer patients were found to have macula-on presentation in the 2020 pandemic cohort (12/66 [18.2%]) compared with the 2019 control cohort (41/87 [47.1%]; P < 0.001; Fig 2A). In contrast, we found a similar proportion of patients with macula-on disease at presentation for those 50 years of age or younger between the 2020 and 2019 cohorts (2020, 8/16 [50.0%]; 2019, 14/24 [58.3%]; P = 0.62). No difference was found in the proportion of patients with macula-on disease at presentation for either age subgroup between the 2019 and 2018 control groups (older than 50 years, P = 0.17; 50 years of age and younger, P = 0.44).
Figure 2.
Bar graph showing proportion of patients with macula-on rhegmatogenous retinal detachment by (A) age and (B) established patient subgroups. No difference was found in the group younger than 50 years with respect to macula status between the cohorts, whereas fewer patients showed macula-on rhegmatogenous retinal detachment in the 2020 cohort (P < 0.001) compared with the 2019 control. For established patients, no significant difference was found with respect to macula status between the cohorts, whereas significantly fewer patients showed macula-on rhegmatogenous retinal detachment in 2020 among new patients (P = 0.001) compared with the 2019 control group.
Established Patient Status
We also analyzed whether established or new patients were more likely to seek treatment for macular detachment and to delay seeking treatment. Patients in both subgroups showed similar demographic factors, including age, gender, race, and regional household income. Among established patients, the proportion with macula-on disease at presentation was similar between the 2020 cohort and 2019 control cohort. Among new patients, fewer patients had macula-on disease at presentation (2020 cohort, 17.9%; 2019 control, 44.7%; P = 0.001; Fig 2B). No significant differences were found for either new (P = 0.54) or established (P = 0.93) patient subgroups between the 2019 and 2018 control groups.
Discussion
In this study, we evaluated the demographic and presenting characteristics, time to presentation, and demographic differences of patients with acute RRD during the COVID-19 pandemic. We found signs of delayed presentation and increased RRD chronicity. We observed a significant decrease in the proportion of patients with macula-on disease seeking treatment during the COVID-19 pandemic as compared with a demographically similar cohort during the same period 1 year prior; this control group (from 2019) also was validated by comparison with a corresponding control group from the prior year (2018) to ensure that an accurate control group was used in this study.
We selected RRD as an index disease for study because its symptoms are considered urgent and warrant prompt evaluation. In our study, the presence or absence of subfoveal fluid (macular attachment status) was chosen as the primary outcome because it was documented consistently, served as an objective measure across all patients, and often correlates with visual outcome.15 The presence of primary grade C PVR is another poor prognostic factor associated with delayed presentation and also was observed significantly more often during the COVID-19 pandemic.16 Finally, worse logMAR VA and fewer number of patients seeking treatment within 1 day of symptom onset during the pandemic also support the hypothesis of delayed presentation.
In our study, patients 50 years of age and younger were spared the pandemic-era effect of delayed presentation with similar rates of macula-on disease compared with a historical control group. This may be because the morbidity and mortality of COVID-19 are perceived to be lower in younger patients. On average, younger patients probably did not face the same risk of pandemic-related morbidity, and for this reason, possibly had a lower threshold for seeking treatment. Similarly, the subgroup of established patients showed an equal rate of macular involvement between the cohorts. As previous studies have shown, worse patient education and comprehension of retinal detachment symptoms and morbidity correlate with delayed presentation.17 , 18 Patients established with a retina practice may be more educated on the signs, symptoms, and morbidity of retinal detachments. Moreover, particularly in the setting of limited outpatient healthcare availability, established patients also may face fewer logistical barriers to evaluation on symptom onset, tilting the patient’s risk-to-benefit analysis toward a lower threshold for seeking treatment. Patients often may seek treatment initially from other providers, many of whom are not open to new patients, leading to delay in evaluation and referral.
A limitation of our investigation is that we analyzed patients who sought treatment in an acute context and may have discounted patients with a severe delay in seeking treatment. The 2020 cohort included fewer patients (n = 82) compared with the 2019 and 2018 control cohorts (111 and 118 patients, respectively). Given the nature of our study, we are unable to comment on whether this difference is significant on a population level. Our study may have a selection bias in undercounting delayed presentation because patients still might not have sought care despite visual symptoms. We chose an analogous time in the previous year instead of the time immediately preceding the COVID-19 pandemic because there may be significant variation on seeking treatment over the course of the year, especially with respect to seasonal weather changes and seasonal travel of patients (especially elderly, retired patients) between regions of the United States. The patients’ distances to the surgical site were similar, suggesting a similar geographic spread and catchment area of the practice as a whole. The presence of early PVR was not always assessed consistently. For this reason, we commented on the presence of only grade C PVR, which was documented consistently. Further work also needs to be carried out to analyze the long-term follow-up and anatomic and functional outcomes between the cohorts, because this was outside the scope of the current investigation. The generalizability of the study also is unknown because our findings may be unique to our local geographical area and patient population. The specific age and racial demographic breakdown of our region may limit its generalizability to the United States as a whole. The incidence of COVID-19 also has affected different localities and demographics with varying intensities.
In our practice, no difference was found in the timing of surgery between 2020 and prior years after an RRD was diagnosed. None of the patients in our cohort showed symptoms positive for COVID-19 or positive testing results, so COVID-19 illness was not expected to influence the time to presentation. However, some differences were found in the outpatient evaluation of patients in 2020. Patients were not allowed visitors, for example, and both providers and patients were wearing masks during the evaluation. The physicians performing the evaluations were slightly different between each year, although 18 of 23 physicians were the same in 2019 compared with 2020. Overall, these differences were not expected to affect a patient’s presenting macula status or VA.
Although observations in recent cardiology literature have reported a delayed presentation and overall decrease in ST-elevation myocardial infarction among the general population during the COVID-19 pandemic in affected areas, these studies assumed that decreased presentation was the result of decreased population incidence.4, 5, 6 The highly publicized study by Tam et al3 suggests that patients delayed seeking treatment for ST-elevation myocardial infarction during the COVID-19 pandemic; however, because of a low volume of only 7 patients in the COVID-19 group and high variation in presentation times at baseline, the results were not statistically significant. The cerebrovascular accident study by Schirmer et al7 found a statistically significant delay in seeking treatment during the pandemic for cerebrovascular accident, an emergent condition not related to COVID-19, that parallels the findings in our study. An analysis by Wickham et al19 of care delivery and patient presentation at Moorfields Eye Hospital during the pandemic suggested the total presentation of retinal detachments was decreased in the relevant pandemic timespan compared with the control group, but the study did not address demographic or anatomic factors. However, our data show that evidence of advanced pathologic features and delayed presentation exist even among the patients who sought treatment.
Our study found a significantly delayed presentation during the pandemic of an emergent condition not related to COVID-19. We showed that despite available ophthalmic care, the environmental milieu of social distancing and stay-at-home orders during the COVID-19 pandemic may have an unintended consequence for outcomes of retinal detachments. The exact causation of the delay in care deserves further study from an ophthalmologic and public health standpoint to ensure that patients receive timely care for vision-threatening conditions such as RRD. Given the persistence of COVID-19 across the United States and potentially recurrent waves of transmission, we emphasize the need for continued public education regarding concerning visual symptoms and the need for continued ophthalmologic care.
Manuscript no. 2020-1346.
Footnotes
Disclosure(s): All authors have completed and submitted the ICMJE disclosures form. The author(s) have made the following disclosure(s): M.A.K.: Consultant – Allergan
Y.Y.: Consultant – Alcon
M.A.K.: Consultant – Genentech, Allergen; Lecturer – Genentech, Regeneron
D.X.: Consultant – Alimera
HUMAN SUBJECTS: Human subjects were included in this study. The human ethics committees at Wills Eye Hospital approved the study. All research complied with the Health Insurance Portability and Accountability Act (HIPAA) of 1996 and adhered to the tenets of the Declaration of Helsinki. Informed consent was waived per Institutional Review Board protocol.
No animal subjects were included in this study.
Author Contributions:
Conception and design: Patel, Starr, Ammar, Khan, Yonekawa, Klufas, Regillo, Ho, Xu
Analysis and interpretation: Patel, Starr, Ammar, Khan, Yonekawa, Klufas, Regillo, Ho, Xu
Data collection: Patel, Peck, Xu
Obtained funding: N/A; Study was performed as part of regular employment duties at Wills Eye Hospital. No additional funding was provided.
Overall responsibility: Patel, Peck, Starr, Ammar, Khan, Yonekawa, Klufas, Regillo, Ho, Xu
References
- 1.World Health Organization COVID-19 situation reports. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Accessed 25.04.20.
- 2.Omer S.B., Malani P., Rio C del. The COVID-19 pandemic in the US: a clinical update. JAMA. 2020;323(18):1767–1768. doi: 10.1001/jama.2020.5788. [DOI] [PubMed] [Google Scholar]
- 3.Tam C.-C.F., Cheung K.-S., Lam S. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circulation. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Metzler B., Siostrzonek P., Binder R.K. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41(19):1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodríguez-Leor O., Cid-Álvarez B., Ojeda S. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. RECIC. 2020;20:82–89. [Google Scholar]
- 7.Schirmer C.M., Ringer A.J., Arthur A.S. Delayed presentation of acute ischemic strokes during the COVID-19 crisis. J NeuroInterv Surg. 2020;12:639–642. doi: 10.1136/neurintsurg-2020-016299. [DOI] [PubMed] [Google Scholar]
- 8.Rehman Siddiqui M.A., Abdelkader E., Hammam T. Socioeconomic status and delayed presentation in rhegmatogenous retinal detachment. Acta Ophthalmol. 2010;88:e352–e353. doi: 10.1111/j.1755-3768.2009.01771.x. [DOI] [PubMed] [Google Scholar]
- 9.Ryan E.H., Ryan C.M., Forbes N.J. Primary Retinal Detachment Outcomes Study report number 2: phakic retinal detachment outcomes. Ophthalmology. 2020;127(8):1077–1085. doi: 10.1016/j.ophtha.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Mitry D., Awan M.A., Borooah S. Long-term visual acuity and the duration of macular detachment: findings from a prospective population-based study. Br J Ophthalmol. 2013;97:149–152. doi: 10.1136/bjophthalmol-2012-302330. [DOI] [PubMed] [Google Scholar]
- 11.Tani P., Robertson D.M., Langworthy A. Prognosis for central vision and anatomic reattachment in rhegmatogenous retinal detachment with macula detached. Am J Ophthalmol. 1981;92:611–620. doi: 10.1016/s0002-9394(14)74651-3. [DOI] [PubMed] [Google Scholar]
- 12.Greven M.A., Leng T., Silva R.A. Reductions in final visual acuity occur even within the first 3 days after a macula-off retinal detachment. Br J Ophthalmol. 2019;103:1503–1506. doi: 10.1136/bjophthalmol-2018-313191. [DOI] [PubMed] [Google Scholar]
- 13.van Bussel E.M., van der Valk R., Bijlsma W.R., La Heij E.C. Impact of duration of macula-off retinal detachment on visual outcome: a systematic review and meta-analysis of literature. Retina. 2014;34:1917–1925. doi: 10.1097/IAE.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 14.Holladay J.T. Proper method for calculating average visual acuity. J Refract Surg. 1997;13:388–391. doi: 10.3928/1081-597X-19970701-16. [DOI] [PubMed] [Google Scholar]
- 15.Wickham L., Ho-Yen G.O., Bunce C. Surgical failure following primary retinal detachment surgery by vitrectomy: risk factors and functional outcomes. Br J Ophthalmol. 2011;95:1234–1238. doi: 10.1136/bjo.2010.190306. [DOI] [PubMed] [Google Scholar]
- 16.Adelman R.A., Parnes A.J., Michalewska Z., Ducournau D. Clinical variables associated with failure of retinal detachment repair: the European Vitreo-Retinal Society Retinal Detachment Study report number 4. Ophthalmology. 2014;121:1715–1719. doi: 10.1016/j.ophtha.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 17.Goezinne F., La Heij E.C., Berendschot T.T.J.M. Patient ignorance is the main reason for treatment delay in primary rhegmatogenous retinal detachment in The Netherlands. Eye. 2009;23:1393–1399. doi: 10.1038/eye.2008.272. [DOI] [PubMed] [Google Scholar]
- 18.Eijk E.S.V., Busschbach J.J.V., Timman R. What made you wait so long? Delays in presentation of retinal detachment: knowledge is related to an attached macula. Acta Ophthalmol. 2016;94:434–440. doi: 10.1111/aos.13016. [DOI] [PubMed] [Google Scholar]
- 19.Wickham L., Hay G., Hamilton R. The impact of COVID policies on acute ophthalmology services—experiences from Moorfields Eye Hospital NHS Foundation Trust. Eye. 2020;34:1189–1192. doi: 10.1038/s41433-020-0957-2. [DOI] [PMC free article] [PubMed] [Google Scholar]