ABSTRACT
Plasmid-launched live-attenuated vaccines (PLLAV), also called infectious DNA (iDNA) vaccines, combine the assets of genetic immunization with the potency of replication-competent live viral vaccines. However, due to their origin as bacterial plasmid DNA, efficient delivery of PLLAV may be hampered by innate signaling pathways such as the cGAS-STING-mediated sensing of cytosolic DNA, resulting in an unfavorable proinflammatory and antiviral response locally at the site of immunization. Employing several complementary cell-based systems and using the yellow fever vaccine (YF17D) and the respective PLLAV-YF17D, we screened a panel of small molecules known to interfere with antiviral signaling for their proviral activity and identified two potent inhibitors of the TANK-binding kinase 1 (TBK1), BX795 and CYT387, to enhance YF17D replication and hence efficacy of PLLAV-YF17D transfection. In tissue culture, BX795 could fully revert the block that plasmid transfection poses on YF17D infection in a type I interferon dependent manner, as confirmed by (i) a marked change in gene expression signatures, (ii) a rescue of full YF17D replication, and (iii) a massively increased virus yield. Inhibitors of TBK1 may hence be considered an adjuvant to potentiate novel PLLAV vaccines, which might boost PLLAV delivery toward their use in vivo.
KEYWORDS: Plasmid-launched live-attenuated vaccine, TBK1, BX795, proviral, innate antiviral immunity, interferon signaling, self-amplifying RNA vaccine
Introduction
Live-attenuated vaccines such as the yellow fever 17D vaccine (YF17D) are among the most efficacious vaccines available that may vigorously induce polyfunctional and long-lasting immunity against deadly infectious diseases1. YF17D is the essential and only tool to quench yellow fever outbreaks2 and is the backbone of an international effort to eliminate yellow fever epidemics (EYE) by 2026.3 However, despite its unrivaled track record, the YF17D legacy vaccine has several shortcomings that limit its wider use and deployment, including (i) a complex production process requiring embryonated chicken eggs and (ii) the instability of the final drug product with a limited shelf life and a need for a strict cold chain for stockpile and shipment, complicating the rapid emergency response.4,5 Likewise, recent yellow fever epidemics in Angola (2016), DRC (2016/17) Brazil (2017–2019), and Nigeria (2018/2019) required a massive intervention6,7 including a revision of longstanding WHO guidelines and the endorsement of splitting doses to cope with the unprecedented vaccine demand8,9. There is hence a growing demand for the established YF17D and also likely for new yellow fever vaccines that could help filling this gap.10,11,12,13-14
Plasmid-based production and delivery of live-attenuated vaccines (plasmid-launched live-attenuated vaccines, also dubbed infectious DNA or iDNA) has been proposed as a valid alternative to classical live vaccines,15 combining the potency of LAV and the ease of production, quality control, and logistics associated with the original genetic immunization using pDNA. Briefly, a PLLAV comprises the full-length cDNA of a live-attenuated RNA virus that initiates the productive replication of the encoded vaccine after transfection into a permissive mammalian cell or tissue. The virus thus produced can amplify and spread like the genuine live vaccines, causing a self-limiting infection and finally inducing immunity in the vaccinated subject (for an animated video tutorial see https://youtu.be/U8-f1PTamCc). Proof of concept of the PLLAV approach was successfully demonstrated for yellow fever vaccination in several pre-clinical mouse models.16,17–18 As for other nucleic acid-based vaccines such as pDNA, mRNA, and self-replication RNA vaccines, previously encountered problems with the delivery of nucleic acid-based vaccines can successfully be overcome by, e.g., electroporation19 or formulation into lipid-nanoparticles.20,21
Intriguingly, relatively little is known about the molecular and cellular events at the inoculation site of PLLAV and pDNA in general (in contrast to those triggered by the respective live vaccines), and how these events relate to PLLAV potency. We set out to study the cell biology of PLLAV-YF17D delivery using a screening approach for anti-inflammatory and immunomodulatory small-molecule inhibitors interfering with innate antiviral signaling. Using this chemical–biological approach, we identified the TANK-binding kinase 1 (TBK1) as an important modulator of PLLAV transfection efficacy. TBK1 together with its close homolog Inhibitor of Nuclear Factor kappa-B kinase subunit epsilon (IKKε) acts downstream of the cGAS-STING signaling pathway.22,23 The cGAS-STING axis, in turn, recognizes cytoplasmic DNA of microbial origin, which may mount a strong antiviral response24,25 and may, therefore, be considered a potential bottleneck for PLLAV-based vaccination. Hence, small-molecule inhibitors of TBK1 may help to overcome pDNA-mediated type I interferon (IFN-I) signaling, and may thus serve as adjuvants with a unique and novel molecular mechanism of action, in particular for PLLAV as well as for other types of self-amplifying nucleic acid-based vaccines.
Materials and methods
Cells and reporter cell lines
Baby hamster kidney cells26 African green monkey kidney cells (Vero E6), human adenocarcinomic alveolar epithelial cells (A549), human embryonic kidney cells (HEK293 T), and mouse fibroblast (L929) were maintained in MEM medium supplemented with 10% fetal calf serum (FCS), 5% sodium carbonate, and 5% glutamine. The HEK_ISRE_GFP/Luc (HEK-ISRE) reporter cell line was generated by transduction of HEK293 T with a lentiviral vector (pGreenFire1-ISRE-EF1-Puro, SBI System Bioscience, catalog TR016VA-P) expressing the Green Fluorescent Protein (GFP) and the firefly luciferase (FFLuc) under the control of the Interferon-Stimulated Response Element (ISRE) and selection of puromycin resistance.
Viruses and virus-encoding plasmids
The live-attenuated yellow fever vaccine strain 17D (YF17D; Stamaril®, Sanofi-Pasteur) was purchased via the Pharmacy of the University Hospital Leuven and propagated on Vero E6 cells to generate a virus stock. The generation of the YF17D-derived reporter viruses YF17D/mCherry and YF17D/Nluc expressing, respectively, the red fluorescent protein mCherry and the bioluminescent (furimazine-converting) Nanoluciferase (NLuc, see Supplementary Fig. S1 A) has been described elsewhere.27,28 Virus stocks were titrated by plaque assay on BHK21 J cells.18,27,28 The synthetic DNA construct PLLAV-YF17D/mCherry, encoding a full-length infectious cDNA clone of the YF17D/mCherry virus (Supplementary Fig. S1 B) expressed under the control of the SV40 promoter,29 was grown in E. coli EPI300-T cells (Epicenter) and purified as endotoxin-free supercoiled plasmid DNA using standard alkaline lysis and affinity chromatography techniques as described previously.28 PLLAV-YF17D/mCherry_CMV-eGFP is a derivative of PLLAV-YF17D/mCherry in which a CMV promoter-driven GFP reporter cassette was inserted in the plasmid backbone as a second cistron that is expressed upon transfection independent of YF17D replication (Supplementary Fig. S1 B and C).
Small-molecule bioactive compounds
Small molecules known to interfere with innate immune signaling (summarized in Table 1) were purchased from Invivogen and Sigma-Aldrich, and stocks were prepared as per instructions from the suppliers. Universal type I interferon (IFN-I) was purchased from Novus Biologicals (catalog 11200–1).
Table 1.
Compounds targeting innate immune signaling pathways screened for proviral activity in YF17D-infected mammalian cellsa.
| Compound name (CAS no.)b | Cellular target | Mechanism of action | Reference |
|---|---|---|---|
| BX795 (702675–74-9) |
TBK1/IKKe | Inhibitor | Clark et al.33 |
| CYT387 (1056634–68-4) |
JAK1/JAK2 & TBK1/IKKe | Inhibitor | Tyner et al.34 |
| YM201636 (371942–69-7) |
PIKfyve | Inhibitor | Kawasaki et al.35 |
| 2ʹ3’-cGAM(PS)2 (Rp/Sp) (1637675–05-8) |
STING | Agonist | Ablasser et al.33 |
| ODN2088 (I: tlrl-2088)b |
TLR9 | Antagonist | Krieg et al.36,37,38 |
| Amlexanox (68302–57-8) |
TBK1 | Inhibitor | Niederberger et al.35 |
| DMXAA (117570–53-3) |
STING | Agonist (selective for murine ortholog) | Conlon et al.39 |
| A151 (I: tlrl-ttag151)b |
TLR9, AIM2 and cGAS | Antagonist | Steinhagen et al.40 |
| PF06928215 (S: PZ038-5 MG)b |
cGAS | Inhibitor | Hall et al.41 |
| Ru.521 (I: inh-ru521)b |
cGAS | Inhibitor | Vincent et al.42 |
aIf not available, the catalog no. at the supplier is given (I–Invivogen; S – Sigma-Aldrich).
bProviral (or antiviral) activity over overt cytotoxic activity (cytotoxic or cytostatic effect) in treated non-infected cell controls.
Screening for small molecules interfering with innate immune signaling
Initial assessment of the activity of small molecules was done on BHK21-J, Vero E6, A549, and L929 cells using a standard antiviral assay format.30,31,41 In brief, cells were pre-seeded in 96-well plates overnight, infected with a 100-times median tissue-culture infectious dose (TCID50) of YF17D as determined on BHK21-J cells, and treated with a twofold serial dilution of each compound. Virus and compounds were left on the cells during the entire course of the experiment until analysis. Cells were incubated at 37°C and the virus-induced cytopathic effect (CPE) quantified after 5 d by an MTS [3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2 H-tetrazolium salt] dye conversion assay (Promega). The resulting fold decrease (i.e., less CPE, antiviral effect) or increase (i.e., more pronounced CPE, proviral effect) in viral replication was calculated in relation to YF17D infected, non-treated control cells (virus control, VC). A compound was scored to have proviral (or antiviral) activity when the CPE in infected and treated cells exceeded (or diminished) that of the virus control by at least 50% and in absence of overt cytotoxic activity (cytotoxic or cytostatic effect) in treated non-infected cell controls at the same compound concentration. YF17D/NLuc was used to infect the naturally resistant murine L929 cells and infection quantified using NLuc bioluminescence (NanoGlo®, Promega) as a proxy for virus replication.
To corroborate the interference with innate antiviral signaling in particular, the observed pro- and antiviral activities were confirmed in virus yield assays using IFN-I primed A549 cells. To that end, cells were pretreated with 10 international units (IU) mL−1 of IFN-I prior to YF17D infection to induce an antiviral state; pilot experiments had revealed that the antiviral state thus induced, reduced viral replication by at least 100-fold (data not shown). Four hours after priming, cells were incubated with YF17D for 1 h at room temperature, after which the inoculum was replaced by fresh medium. Cells were then either left untreated (VC) or were treated with BX795, CYT387, or YM201636 (5 µM each). After 6 d, infectious virus progeny in the supernatant was quantified by endpoint titration (TCID50 by CPE on BHK21-J cells). All assays were performed at least in duplicate with each n = 6 technical repeats.
Hit validation and molecular mechanism of action using HEK-ISRE reporter cells
For validation, HEK-ISRE cells were treated with 5 µM BX795 or left untreated. After 2 h, 10 IU mL−1 IFN-I was added and cells were incubated at 37°C for another 48 h prior to cell lysis and assessment of the luciferase activities (Promega).
The effect of compound treatment on the infectivity of YF17D/mCherry as well as on the IFN-I response during viral infection was visualized using the same HEK-ISRE cells. Cells were infected with YF17D/mCherry and either (a) left untreated, (b) received a single treatment with BX795, CYT387, or YM201636, or (c) received a dual treatment with compound plus IFN-I. GFP (IFN-I signaling) and mCherry expression (YF17D replication) was monitored by fluorescence microscopy. After 3 d, cells were trypsinized, fixed in 2% paraformaldehyde, stained with Zombie Aqua (Biolegend) to discriminate from dead cells, and GFP and/or mCherry positive cell populations were quantified by flow cytometry.
Effect of BX795 on YF17D replication initiated from PLLAV
To determine the effect of BX795 on the efficacy by which YF17D replication can be initiated from transfected PLLAV (plasmid-launched live-attenuated vaccine), PLLAV-YF17D/mCherry (expressing YF17D/mCherry reporter virus upon transfection)27 was used for the transfection of A549 cells. A549 cells (grown in 6 well plates, 300.000 cells per well) were transfected with 2.5 µg of plasmid using TransIT®-LT1 transfection reagent (Mirus) in the absence of compound or presence of either BX795 (5 µM) or the specific cGAS inhibitor PF06928215 (50 µM).41The expression of mCherry was monitored by fluorescence microscopy as a proxy for the successful launching of productive YF17D replication.
Differential gene expression following plasmid transfection as influenced by BX795
To study the differential gene expression, a panel of 30 genes known to be activated in response to plasmid transfection and/or during yellow fever infection, as well as two housekeeping genes, was selected to assemble a custom Taqman qRT-PCR array (Supplementary Table 1). RNA was extracted from A549 cells transfected with PLLAV-YF17D/mCherry in the presence or absence of BX795 along with untreated cells as control using Trizol43 and subjected to cDNA synthesis (High Capacity cDNA Reverse Transcription Kit, catalog no. 4368814) following the manufacturer’s instructions, and qPCR was done using custom Taqman qRT-PCR plates (custom-made plates). Data collected from three technical repeats were analyzed using the Quant Studio Design and Analysis software (version 1.5.1, Thermo Fischer Scientific) and Data Assist software (version 3.01, Thermo Fischer Scientific).
Results
The live-attenuated YF17D virus was used to screen for small-molecule inhibitors of innate antiviral signaling (Figure 1B) that may exert a proviral effect. After an initial cell-based phenotypic screen32 of a large selection of compounds (Table 1), the two TBK-1 inhibitors BX79533 and CYT38734 were found to increase YF17D-induced CPE on human A549 cells in a dose-dependent manner, with median effective concentrations of around 5 µM each (Figure 2A). The TLR-9 signaling inhibitor YM20163635, by contrast, showed some antiviral effect. These results were confirmed in mouse L929 cells using the YF17D/NLuc reporter virus and bioluminescence as a proxy for viral infection (Figure 2B). Intriguingly, a proviral effect was not observed when using BHK21-J or Vero E6 cells (data not shown); both are known to be deficient in IFN-I production. To further link the molecular mechanism of action (MoA) of these inhibitors to cellular IFN-I signaling, A549 cells were primed with 10 IU mL−1 of IFN-I to induce an antiviral state (see Supplementary Figures S2 B and S3 B) prior to YF17D infection. Under these conditions, BX795 and CYT387 could rescue productive viral replication and the production of infectious vaccine virus progeny by about 4 log10-fold compared to IFN-I inhibition (Figure 2C).
Figure 1.
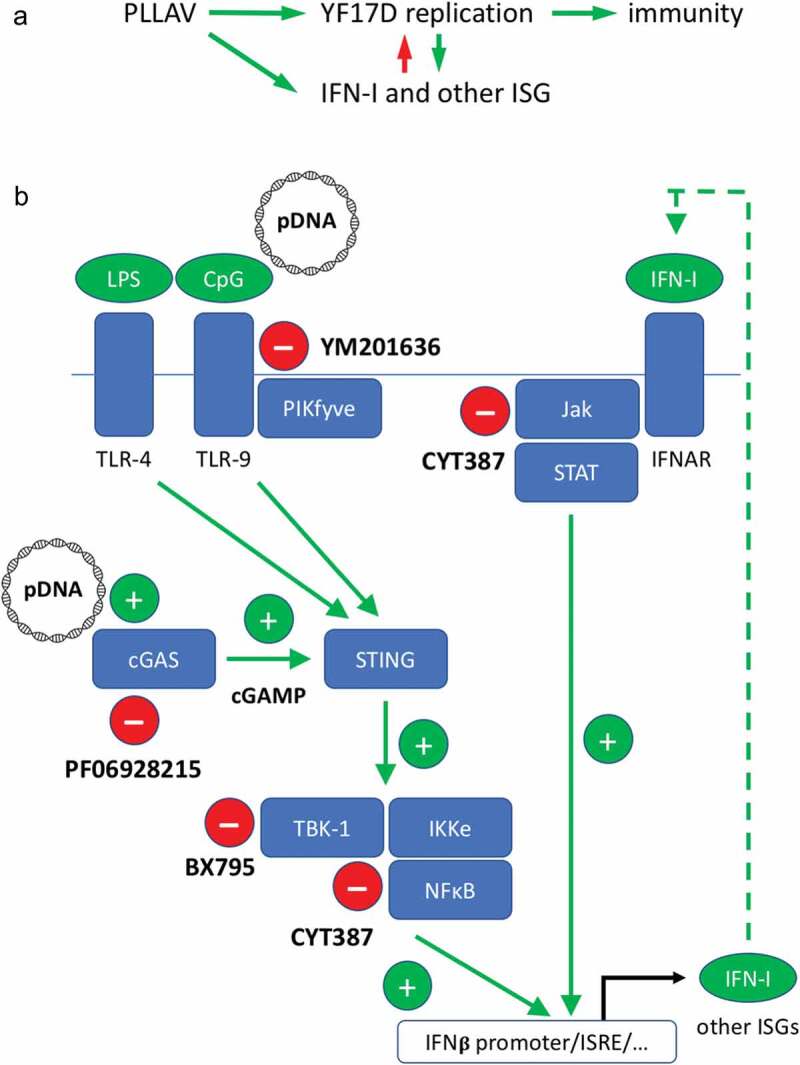
Interference of YF17D vaccination and a plasmid-launched live-attenuated vaccine candidate derived thereof (PLLAV-YF17D) with innate antiviral responses. (A) The original live-attenuated YF17D induces vigorous innate and adaptive immune responses. The virus-induced expression of type I interferons (IFN-I) and other antiviral, proinflammatory, and immunomodulatory genes (ISG, IFN-stimulated genes) constitutes a direct negative feedback loop on viral replication. Launching of YF17D by transfection of PLLAV-YF17D may disturb the natural balance by inducing overexpression of particular ISG. (B) Schematic view on the induction of innate antiviral signaling by plasmid DNA (pDNA). Cells express several innate DNA sensors including the ubiquitous cytoplasmic cGAS [cyclic 2ʹ,3ʹ-GAMP c(GAMP) synthetase], and membrane-associated sensors that can be triggered by other molecular patterns frequently present in bacterial pDNA preparations, such as CpG (by Toll-like receptor 7, TLR-7) and bacterial endotoxins (LPS, by TLR-4). Binding of pDNA to cGAS induces the synthesis of the second messenger cGAMP. The cGAMP and TLR-9/4 signals are integrated by STING, activating, in turn, several downstream signaling cascades involving the TANK-binding kinase 1 (TBK-1) and occasionally resulting in the induction of numerous ISGs via IFN sensitive response elements (ISRE) or similar promoters. The production and secretion of IFN-I lead to an autocrine and paracrine signal amplification involving the IFN-I receptor (IFNAR) and Jak/STAT pathway. For simplicity, the subcellular compartmentation of individual components (e.g., localization of STING to mitochondrial outer membranes and its concomitant involvement in other antiviral pathways such as MAVS signaling or nuclear transcription of ISGs) is not depicted in the sketch. For a description of small-molecule inhibitors interfering with innate pDNA signaling see Table 1.
Figure 2.
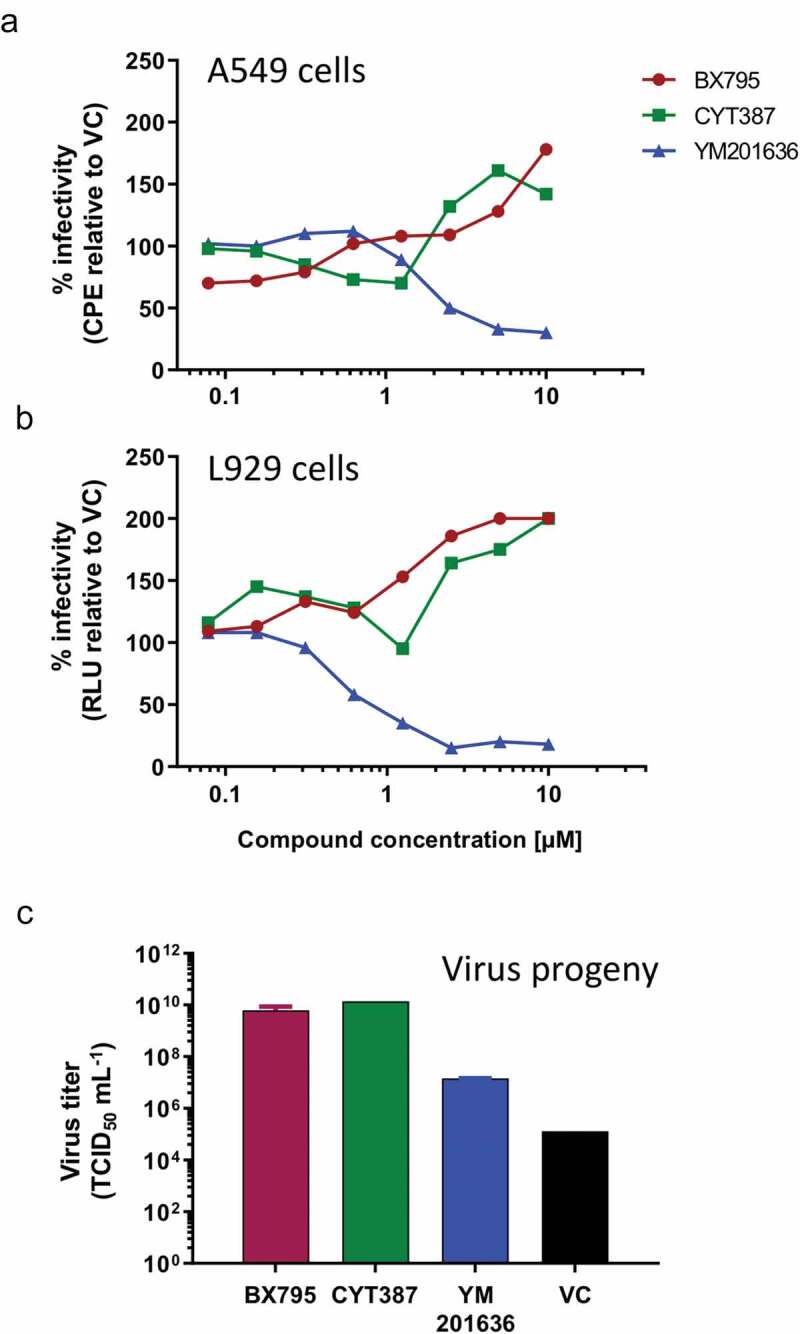
Proviral activity of inhibitors of intracellular innate DNA signaling. Dose-dependent enhancement of the YF17D-induced CPE on human A549 cells (A) and YF17D/NLuc induced bioluminescence on murine L929 cells (B) by the TBK-1 inhibitors BX795 and CYT387. The inhibitor of TLR signaling YM201636, by contrast, showed an antiviral effect. Within the range of concentration tested, none of the compounds showed any direct toxicity to the cells. (C) Rescue of virus replication resulting in IFN-I treated A549 cells and increased production of infectious progeny following treatment (5 µM) with the TBK-1 inhibitors BX795 and CYT387. Data shown are means of at least duplicate experiments run each in sixfold technical repeats. CPE, virus-induced cytopathic effect; RLU, relative light units; VC, non-treated virus control; TCID50, median tissue culture infectious dose.
HEK-ISRE reporter cells expressing GFP and FFLuc under the control of an ISRE were generated to directly visualize the activity of innate signaling at the cellular level upon YF17D/mCherry infection (Supplementary Figure S2). Using these reporter cells, we could confirm that YF17D infection is both (i) an inducer of IFN-I signaling, and (ii) is itself highly sensitive to IFN-I inhibition which is consistent with existing data44 (Figure 1A, Figure 3A; for single-cell analysis by flow cytometry, see also Supplementary Figure 3A). Inhibition of TBK-1 could enhance YF17D replication (Figure 3B and Supplementary Figure 3A) as well as rescue the production of infectious viral progeny, even in the presence of IFN-I (Supplementary Figure 3B).
Figure 3.
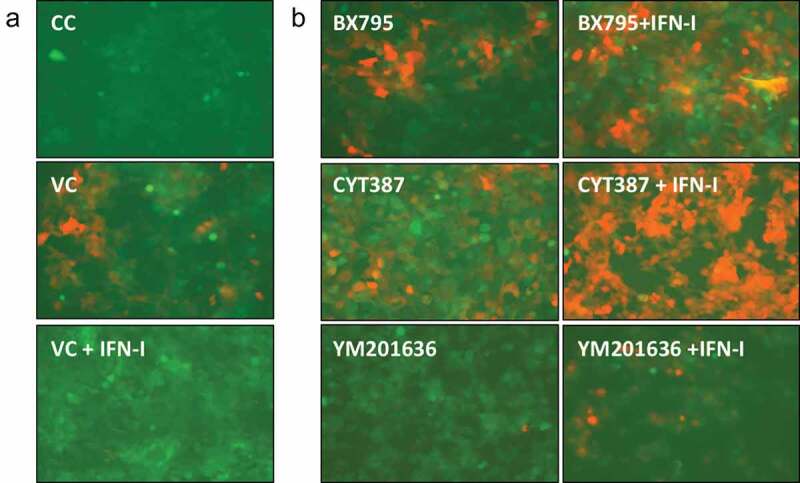
Antagonism of IFN-I signaling by proviral compound in HEK-ISRE reporter cells. (A) YF17D/mCherry infection (red) enhances overall GFP reporter gene expression (green) in infected HEK-ISRE cells (VC) if compared to background expression levels in uninfected cell controls (CC). Treatment with IFN-I (10 IU/mL) further enhances GFP expression yet fully eliminates viral replication. (B) Treatment with the TBK-1 inhibitors BX795 and CYT387 increases the number of infected HEK-ISRE cells, even in the presence of exogenously added IFN-I (right panel, +IFN-I). The inhibitor of TLR signaling YM201636, by contrast, showed an antiviral effect.
IFN-I deficient BHK21-J cells and cGAS deficient HEK293T45 readily support the launching of YF17D replication from transfected pDNA (Supplementary Figure S1C). By contrast, transfection with plasmid pDNA (i.e., the PLLAV-YF17D/mCherry) render A549 cells resistant to YF17D/mCherry replication (Figure 4A, upper panel), somewhat mimicking the effect of exogenously added IFN-I. This inhibition mediated by pDNA is a likely consequence of the induction of antiviral ISGs (Figure 4C and Supplementary Figure 5) via the cGAS-Sting TBK1 pathway known to be functional in A459 cells46 (as well as in L929 cells)47 (Figure 4B). Accordingly, inhibition of the latter pathway by BX795 (targeting TBK-1) can rescue YF17D replication, which is comparable to the direct inhibition of the cytoplasmic DNA sensor cGAS by the specific enzyme inhibitor PF0628215,41 albeit to a lesser extent (Figure 4A, lower panel). An analysis of the respective patterns for differentially expressed genes (DEG, Figure 4C) showed that BX795 treatment, which was earlier shown to attenuate cytokine production in other STING-dependent cellular systems,48 could also revert DEG expression in PLLAV-YF17D/mCherry transfected cells to baseline levels (untreated cell controls) for several ISGs tested (e.g., MX1, OAS3, STAT1). Some DEG, including key factors involved in IFN-I induction (e.g., TMEM173/STING, IRF9) as well as some functionally less well-characterized DEG (i.e., involved in cellular RNA turnover, e.g., DHX36, PNPT2) were downregulated even below basal levels (Supplementary Figure 5).
Figure 4.
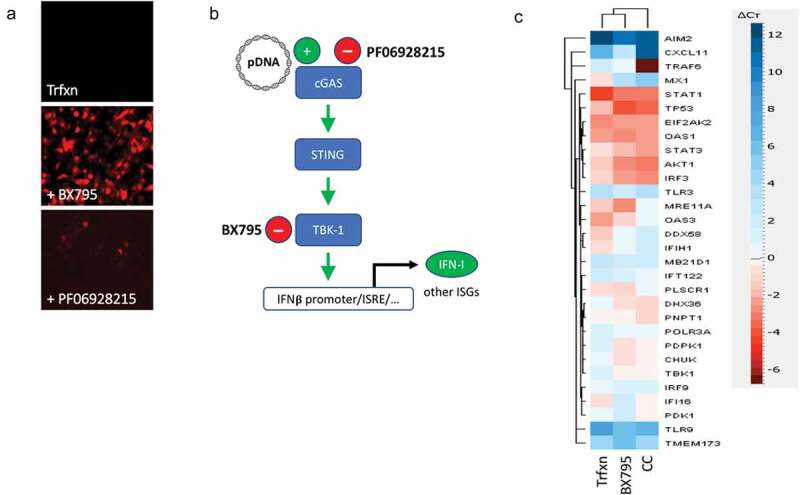
Failure to launch YF17D/mCherry replication from transfected pDNA (PLLAV-YF17D/mCherry) can be rescued by inhibitors of TBK-1 and cGAS. (A) A549 cells lose their susceptibility for viral infection and fail to support YF17D/mCherry replication when transfected with pDNA (Trfxn, transfection). Viral replication can be rescued by treatment with BX795 (5 µM) or by direct inhibition of the upstream pDNA sensor cGAS by the specific enzyme inhibitor PF06928215 (50 µM). (B) Schematic representation of the cGAS-STING-TBK1 pathway involved in the inhibition of YF17D replication by pDNA, as supported by the use of the specific small-molecule inhibitors. (C) Heatmap of differentially expressed genes comparing A549 cells transfected with PLLAV-YF17D/mCherry (i) without further treatment (Trfxn) and (ii) with concomitant BX795 treatment (BX795) versus (iii) untreated cell controls (CC). BX795 treatment counteracted (downregulated) many genes induced by pDNA transfection. Data are shown based on the means of triplicate experiments analyzed by the Quant Studio Data Assist software (version 3.01). For a full list of the 32 genes included in the qRT-PCR array see Supplementary Table 1. For individual data sets see Supplementary Figure 5.
Discussion
In general, the potency of PLLAV-based vaccines depends on two main factors: (i) the immunogenicity of the actual live vaccine virus thus produced (i.e., the active component or ‘antigen’) and (ii) the efficacy of its uptake and delivery (i.e., pharmacokinetics of the ‘drug substance’). Yellow fever vaccination using PLLAV-YF17D requires the cellular uptake of pDNA by a susceptible producer cell that supports the launching of viral replication and production of the initial live YF17D ‘antigen’ in vivo. As PLLAV consists of pDNA of bacterial origin, several innate receptors recognizing molecular pathogen-associated patterns (PAMP) are likely to be triggered once the vaccine is administered, in particular the ubiquitously expressed cytoplasmic DNA sensor cGAS (Figure 1B). The in vivo potency of PLLAV-YF17D may hence suffer from a very similar issue as observed in transfected cells in tissue culture (Figure 1B and Supplementary Figure 1C).
Using two small-molecule inhibitors of TBK-1, BX795 and CYT387, we show that YF17D replication that is very sensitive to IFN-I inhibition (Figure 3A) can massively be enhanced, up to 1000-fold and higher virus yields (Figure 2C) in cells that are initially refractory to productive infection due to an antiviral state induced by either IFN-I treatment (Supplementary Figure S3) or transfection of pDNA (Supplementary Figure 4B). The latter antiviral effect of transfected pDNA has been described before and can experimentally be overcome by a targeted knockout of cGAS and STING in cultured cells.49 Likewise, we show here that also direct pharmacological inhibition of cGAS by the specific enzyme inhibitor PF062821541 can phenocopy such a genetic ablation (Figure 4A, B). The overall greater effect achieved by BX795, i.e., by inhibition of a kinase downstream in the cGAS-STING axis, can partially be explained by the reportedly poor bioavailability of PF0628215.41 Nevertheless, some pleiotropic effects of BX79550 may synergize, especially considering that multiple upstream signaling pathways converge at and are integrated by TBK1.33 Such a synergy of pleiotropic effect is even more likely responsible for the proviral effect observed for CYT387. CYT387 (originally developed as Momelotinib® as chemotherapeutic agent) is known to be more promiscuous in targeting also the Jak-STAT pathway downstream of the IFN-I receptors51 (Figure 1B).
Overall, a similar effect of both BX795 and CYT387 used here as chemical probes, i.e., of two structurally non-related inhibitors with different molecular MoA (BX795 targeting TBK1 dimerization;52 CYT387 as original kinase inhibitor competing with ATP binding), corroborates the importance of TBK1 in the cGAS-STING signaling as it concerns the potency and efficacy of PLLAV vaccines. Interestingly, a strong and sometimes detrimental (overshooting) induction of an IFN-I mediated antiviral response has also been reported for self-amplifying RNA vaccines.53,54 Of note, the respective TLR and RLR involved in cellular recognition of SAM RNAs signal via the same TBK1 pathway, implying that also these vaccines may benefit from a similar immunomodulatory strategy.
A first attempt to directly translate our in vitro findings into a tool to enhance PLLAV vaccination in vivo remained non-conclusive, and a co-administration of BX795 or PF06928215 did not immediately result in any obvious improvement of PLLAV-YF17D vaccination in mice, neither regarding an increased YF17D replication at the injection site (using bioluminescence imaging of mice injected with PLLAV-YF17D/NLuc as surrogate readout) nor in higher seroconversion rates (data not shown). This failure may readily be explained by a suboptimal exposure to the compounds used.41 Moreover, YF17D replication is highly restricted in mice.44 Hence, the use of PLLAV-YF17D in wild-type mice may constitute a poor in vivo model to study to what extent small-molecule inhibitors may modulate the launching efficacy of PLLAV. Instead, PLLAV vaccines derived from other viruses that are readily infectious in mice (e.g., alphaviruses55) may be preferred, and a focus on inhibitors of the cGAS/STING/TBK1 axis that show a better bioavailability and more favorable pharmacokinetics.
In conclusion, the strong observed activation of innate immunity by PLLAV and other self-amplifying nucleic acid-based vaccines may be detrimental for immunization purposes and hence is not desired, much in contrast to classical pDNA vaccines that rather seem to benefit from a strong proinflammatory environment. For PLLAV (and likely SAM), a tempering of the cGAS-STING-TBK1 pathway by small-molecule inhibitors may markedly increase initial vaccine replication and may, therefore, provide a promising approach to optimize PLLAV delivery by controlling the local inflammatory response to enhanced vaccine potency, likely along with dose sparing.
Supplementary Material
Acknowledgments
The authors thank Sarah Debaveye, Jerome Villers, and Geert Schoofs for their excellent technical assistance. BHK21-J and Vero E6 cells were a generous gift of Prof. Peter Bredenbeek, Leiden University Medical Center (LUMC), Leiden, The Netherlands.
Funding Statement
This project was supported by KU Leuven IOF Hefboom [IOF HB/13/010] and KU Leuven C3 [C32/16/039] grants and received funding from the European Union’s Horizon 2020 Framework Programme research and innovation program under RABYD-VAX grant agreement No. [733176]. MAS was granted a Senior Postdoctoral Fellowship by the KU Leuven Rega Foundation.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/21645515.2020.1765621.
References
- 1.Pulendran B. Learning immunology from the yellow fever vaccine: innate immunity to systems vaccinology. Nat Rev Immunol. 2009;9(10):741–47. doi: 10.1038/nri2629. [DOI] [PubMed] [Google Scholar]
- 2.Collins ND, Barrett ADT.. Live attenuated yellow fever 17D vaccine: a legacy vaccine still controlling outbreaks in modern day. Curr Infect Dis Rep. 2017;19(3). doi: 10.1007/s11908-017-0566-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO . Eliminate yellow fever epidemics (EYE): a global strategy, 2017–2026. Wkly Epidemiol Rec. 2017;92(16):193–204. [PubMed] [Google Scholar]
- 4.Chen LH, Hamer DH. Vaccination challenges in confronting the resurgent threat from yellow fever. JAMA. 2017;318(17):1651. doi: 10.1001/jama.2017.14258. [DOI] [PubMed] [Google Scholar]
- 5.Barrett ADT. Yellow fever in angola and beyond – the problem of vaccine supply and demand. N Engl J Med. 2016;375(4):301–03. doi: 10.1056/NEJMp1002530. [DOI] [PubMed] [Google Scholar]
- 6.Wilder-Smith A, Monath TP. Responding to the threat of urban yellow fever outbreaks. Lancet Infect Dis. 2017;17(3):248–50. doi: 10.1016/S1473-3099(16)30588-6. [DOI] [PubMed] [Google Scholar]
- 7.Barrett ADT. The reemergence of yellow fever. Science. 2018;361(6405):847–48. doi: 10.1126/science.aau8225. [DOI] [PubMed] [Google Scholar]
- 8.WHO . Weekly Epidemiological Rec. Meeting of the strategic advisory group of experts on immunization, October 2016—conclusions and recommendations. 2016;91(48):561–84. [PubMed] [Google Scholar]
- 9.Visser LG. Fractional-dose yellow fever vaccination: how much more can we do with less? Curr Opin Infect Dis. 2019;32(5):390–93. doi: 10.1097/QCO.0000000000000576. [DOI] [PubMed] [Google Scholar]
- 10.Bassi MR, Larsen MAB, Kongsgaard M, Rasmussen M, Buus S, Stryhn A, Thomsen AR, Christensen JP. Vaccination with replication deficient adenovectors encoding YF-17D antigens induces long-lasting protection from severe yellow fever virus infection in mice. PLoS Negl Trop Dis. 2016;10(2):e0004464. doi: 10.1371/journal.pntd.0004464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maciel M, Cruz F da SP, Cordeiro MT, da Motta MA, Cassemiro KMS de M, Maia R de CC, de Figueiredo RCBQ, Galler R, Freire M da S, August JT, et al. A DNA vaccine against yellow fever virus: development and evaluation. PLoS Negl Trop Dis. 2015;9(4):e0003693. doi: 10.1371/journal.pntd.0003693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schäfer B, Holzer GW, Joachimsthaler A, Coulibaly S, Schwendinger M, Crowe BA, Kreil TR, Barrett PN, Falkner FG. Pre-clinical efficacy and safety of experimental vaccines based on non-replicating vaccinia vectors against yellow fever. PLoS One. 2011;6(9):e24505. doi: 10.1371/journal.pone.0024505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pereira RC, Silva ANMR, Souza MCO, Silva MV, Neves PPCC, Silva AAMV, Matos DDCS, Herrera MAO, Yamamura AMY, Freire MS, et al. An inactivated yellow fever 17DD vaccine cultivated in Vero cell cultures. Vaccine. 2015;33(35):4261–68. doi: 10.1016/j.vaccine.2015.03.077. [DOI] [PubMed] [Google Scholar]
- 14.Monath TP, Fowler E, Johnson CT, Balser J, Morin MJ, Sisti M, Trent DW. An inactivated cell-culture vaccine against yellow fever. N Engl J Med. 2011;364(14):1326–33. doi: 10.1056/NEJMoa1009303. [DOI] [PubMed] [Google Scholar]
- 15.Pushko P, Lukashevich IS, Weaver SC, Tretyakova I. DNA-launched live-attenuated vaccines for biodefense applications. Expert Rev Vaccines. 2016;15(9):1223–34. doi: 10.1080/14760584.2016.1175943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tretyakova I, Nickols B, Hidajat R, Jokinen J, Lukashevich IS, Pushko P. Plasmid DNA initiates replication of yellow fever vaccine in vitro and elicits virus-specific immune response in mice. Virology. 2014;468-470:28–35. doi: 10.1016/j.virol.2014.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jiang X, Dalebout TJ, Lukashevich IS, Bredenbeek PJ, Franco D. Molecular and immunological characterization of a DNA-launched yellow fever virus 17D infectious clone. J Gen Virol. 2015;96(4):804–14. doi: 10.1099/jgv.0.000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kum DB, Mishra N, Vrancken B, Thibaut HJ, Wilder-Smith A, Lemey P, Neyts J, Dallmeier K. Limited evolution of the yellow fever virus 17d in a mouse infection model. Emerging Microbes Infect. 2019;8(1):1734–46. doi: 10.1080/22221751.2019.1694394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lambricht L, Lopes A, Kos S, Sersa G, Préat V, Vandermeulen G. Clinical potential of electroporation for gene therapy and DNA vaccine delivery. Expert Opin Drug Deliv. 2016;13(2):295–310. doi: 10.1517/17425247.2016.1121990. [DOI] [PubMed] [Google Scholar]
- 20.Geall AJ, Verma A, Otten GR, Shaw CA, Hekele A, Banerjee K, Cu Y, Beard CW, Brito LA, Krucker T, et al. Nonviral delivery of self-amplifying RNA vaccines. Proceedings of the National Academy of Sciences of the United States of America. 2012. doi: 10.1073/pnas.1209367109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brito LA, Chan M, Shaw CA, Hekele A, Carsillo T, Schaefer M, Archer J, Seubert A, Otten GR, Beard CW, et al. A cationic nanoemulsion for the delivery of next-generation RNA vaccines. Mol Ther. 2014;22(12):2118–29. doi: 10.1038/mt.2014.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fitzgerald KA. IKK[epsi] and TBK1 are essential components of the IRF3 signaling pathway. Nature Immunol. 2003;4(5):491–96. doi: 10.1038/ni921. [DOI] [PubMed] [Google Scholar]
- 23.Sharma S, TenOever BR, Grandvaux N, Zhou GP, Lin R, Hiscott J. Triggering the interferon antiviral response through an IKK-related pathway. Science. 2003;300(5622):1148–51. doi: 10.1126/science.1081315. [DOI] [PubMed] [Google Scholar]
- 24.Burdette DL, Vance RE. STING and the innate immune response to nucleic acids in the cytosol. Nat Immunol. 2013;14(1):19–26. doi: 10.1038/ni.2491. [DOI] [PubMed] [Google Scholar]
- 25.Wu J, Sun L, Chen X, Du F, Shi H, Chen C, Chen ZJ. Cyclic GMP-AMP is an endogenous second messenger in innate immune signaling by cytosolic DNA. Science. 2013;339(6121):826–30. doi: 10.1126/science.1229963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lindenbach BD, Rice CM. trans-Complementation of yellow fever virus NS1 reveals a role in early RNA replication. J Virol. 1997;71(12):9608–17. doi: 10.1128/jvi.71.12.9608-9617.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kum DB, Mishra N, Boudewijns R, Gladwyn-Ng I, Alfano C, Ma J, Schmid MA, Marques RE, Schols D, Kaptein S, et al. A yellow fever–Zika chimeric virus vaccine candidate protects against Zika infection and congenital malformations in mice. Npj Vaccines. 2018;3(1). doi: 10.1038/s41541-018-0092-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kum DB, Boudewijns R, Ma J, Mishra N, Dominique Schols JN, KD . A chimeric yellow fever-Zika virus vaccine candidate fully protects against yellow fever virus infection in mice. Emerging Microbes Infect. 2020;9(1):520–33. doi: 10.1080/22221751.2020.1730709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dallmeier K, Neyts J. Simple and inexpensive three-step rapid amplification of cDNA 5′ ends using 5′ phosphorylated primers. Anal Biochem. 2013;434(1):1–3. doi: 10.1016/j.ab.2012.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Segura Guerrero NA, Sharma S, Neyts J, Kaptein SJF. Favipiravir inhibits in vitro Usutu virus replication and delays disease progression in an infection model in mice. Antiviral Res. 2018;160:137–42. doi: 10.1016/j.antiviral.2018.10.026. [DOI] [PubMed] [Google Scholar]
- 31.Bardiot D, Koukni M, Smets W, Carlens G, McNaughton M, Kaptein S, Dallmeier K, Chaltin P, Neyts J, Marchand A. Discovery of indole derivatives as novel and potent dengue virus inhibitors. J Med Chem. 2018;61(18):8390–401. doi: 10.1021/acs.jmedchem.8b00913. [DOI] [PubMed] [Google Scholar]
- 32.Kaptein SJF, De Burghgraeve T, Froeyen M, Pastorino B, Alen MMF, Mondotte JA, Herdewijn P, Jacobs M, De Lamballerie X, Schols D, et al. A derivate of the antibiotic doxorubicin is a selective inhibitor of dengue and yellow fever virus replication in vitro. Antimicrob Agents Chemother. 2010;54(12):5269–80. doi: 10.1128/AAC.00686-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clark K, Plater L, Peggie M, Cohen P. Use of the pharmacological inhibitor BX795 to study the regulation and physiological roles of TBK1 and IκB kinase : a distinct upstream kinase mediates ser-172 phosphorylation and activation. J Biol Chem. 2009;284(21):14136–46. doi: 10.1074/jbc.M109.000414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tyner JW, Bumm TG, Deininger J, Wood L, Aichberger KJ, Loriaux MM, Druker BJ, Burns CJ, Fantino E, Deininger MW. CYT387, a novel JAK2 inhibitor, induces hematologic responses and normalizes inflammatory cytokines in murine myeloproliferative neoplasms. Blood. 2010;115(25):5232–40. doi: 10.1182/blood-2009-05-223727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kawasaki T, Takemura N, Standley DM, Akira S, Kawai T. The second messenger phosphatidylinositol-5-phosphate facilitates antiviral innate immune signaling. Cell Host Microbe. 2013;14(2):148–58. doi: 10.1016/j.chom.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 36.Ablasser A, Goldeck M, Cavlar T, Deimling T, Witte G, Röhl I, Hopfner KP, Ludwig J, Hornung V. CGAS produces a 2′-5′-linked cyclic dinucleotide second messenger that activates STING. Nature. 2013. doi: 10.1038/nature12306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krieg AM, Wu T, Weeratna R, Efler SM, Love-Homan L, Yang L, Yi K, Short D, Davis HL. Sequence motifs in adenoviral DNA block immune activation by stimulatory CpG motifs. Proceedings of the National Academy of Sciences of the United States of America. 1998. doi: 10.1073/pnas.95.21.12631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Niederberger E, Moser C, Kynast K, Geisslinger G. The non-canonical IκB Kinases IKKε and TBK1 as potential targets for the development of novel therapeutic drugs. Curr Mol Med. 2013;13(7):1089–97. doi: 10.2174/1566524011313070004. [DOI] [PubMed] [Google Scholar]
- 39.Conlon J, Burdette DL, Sharma S, Bhat N, Thompson M, Jiang Z, Rathinam VAK, Monks B, Jin T, Xiao TS, et al. Mouse, but not human STING, binds and signals in response to the vascular disrupting agent 5,6-dimethylxanthenone-4-acetic acid. J Immunol. 2013;190(10):5216–25. doi: 10.4049/jimmunol.1300097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Steinhagen F, Zillinger T, Peukert K, Fox M, Thudium M, Barchet W, Putensen C, Klinman D, Latz E, Bode C. Suppressive oligodeoxynucleotides containing TTAGGG motifs inhibit cGAS activation in human monocytes. Eur J Immunol. 2018;48(4):605–11. doi: 10.1002/eji.201747338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hall J, Brault A, Vincent F, Weng S, Wang H, Dumlao D, Aulabaugh A, Aivazian D, Castro D, Chen M, et al. Discovery of PF-06928215 as a high affinity inhibitor of cGAS enabled by a novel fluorescence polarization assay. PLoS One. 2017;12(9):e0184843. doi: 10.1371/journal.pone.0184843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vincent J, Adura C, Gao P, Luz A, Lama L, Asano Y, Okamoto R, Imaeda T, Aida J, Rothamel K, et al. Small molecule inhibition of cGAS reduces interferon expression in primary macrophages from autoimmune mice. Nat Commun. 2017. doi: 10.1038/s41467-017-00833-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee W, Lee SH, Kim M, Moon JS, Kim GW, Jung HG, Kim IH, Oh JE, Jung HE, Lee HK, et al. Vibrio vulnificus quorum-sensing molecule cyclo(Phe-Pro) inhibits RIG-I-mediated antiviral innate immunity. Nat Commun. 2018. doi: 10.1038/s41467-018-04075-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Erickson AK, Pfeiffer JK. Dynamic viral dissemination in mice infected with yellow fever virus strain 17D. J Virol. 2013;87(22):12392–97. doi: 10.1128/jvi.02149-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sun L, Wu J, Du F, Chen X, Chen ZJ. Cyclic GMP-AMP synthase is a cytosolic DNA sensor that activates the type I interferon pathway. Science. 2013;339(6121):786–91. doi: 10.1126/science.1232458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stewart CE, Randall RE, Adamson CS. Inhibitors of the interferon response enhance virus replication in vitro. PLoS One. 2014;9(11):e112014. doi: 10.1371/journal.pone.0112014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cheng WY, He XB, Jia HJ, Chen GH, Jin QW, Long ZL, Jing ZZ. The cGas-sting signaling pathway is required for the innate immune response against ectromelia virus. Front Immunol. 2018;9. doi: 10.3389/fimmu.2018.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pokatayev V, Yan N. Methods of assessing STING activation and trafficking. In: Mossmar K, editor. Methods in molecular biology. New York: Human Press; 2017. p. 167–74. doi: 10.1007/978-1-4939-7237-1_10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Langereis MA, Rabouw HH, Holwerda M, Visser LJ, van Kuppeveld FJM. Knockout of cGAS and STING rescues virus infection of plasmid DNA-transfected cells. J Virol. 2015;89(21):11169–73. doi: 10.1128/jvi.01781-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jaishankar D, Yakoub AM, Yadavalli T, Agelidis A, Thakkar N, Hadigal S, Ames J, Shukla D. An off-target effect of BX795 blocks herpes simplex virus type 1 infection of the eye. Sci Transl Med. 2018;10(428):eaan5861. doi: 10.1126/scitranslmed.aan5861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Monaghan KA, Khong T, Burns CJ, Spencer A. The novel JAK inhibitor CYT387 suppresses multiple signalling pathways, prevents proliferation and induces apoptosis in phenotypically diverse myeloma cells. Leukemia. 2011;25(12):1891–99. doi: 10.1038/leu.2011.175. [DOI] [PubMed] [Google Scholar]
- 52.Tu D, Zhu Z, Zhou AY, Yun CH, KE L, Toms AV, Li Y, GP D, Chan E, Thai T, et al. Structure and ubiquitination-dependent activation of TANK-binding kinase 1. Cell Rep. 2013;3(3):747–58. doi: 10.1016/j.celrep.2013.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pepini T, Pulichino A-M, Carsillo T, Carlson AL, Sari-Sarraf F, Ramsauer K, Debasitis JC, Maruggi G, Otten GR, Geall AJ, et al. Induction of an IFN-mediated antiviral response by a self-amplifying RNA vaccine: implications for vaccine design. J Immunol. 2017;198(10):4012–24. doi: 10.4049/jimmunol.1601877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huysmans H, Zhong Z, De Temmerman J, Mui BL, Tam YK, Mc Cafferty S, Gitsels A, Vanrompay D, Sanders NN. Expression kinetics and innate immune response after electroporation and LNP-mediated delivery of a self-amplifying mRNA in the skin. Mol Ther Nucleic Acids. 2019;17:867–78. doi: 10.1016/j.omtn.2019.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tretyakova I, Tibbens A, Jokinen JD, Johnson DM, Lukashevich IS, Pushko P. Novel DNA-launched Venezuelan equine encephalitis virus vaccine with rearranged genome. Vaccine. 2019. May 31;37(25):3317–25. doi: 10.1016/j.vaccine.2019.04.072. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


