Abstract
Coronavirus disease 2019 (COVID-19) increases the risk of several non-pulmonary complications such as acute myocardial injury, renal failure or thromboembolic events. A possible unifying explanation for these phenomena may be the presence of profound endothelial dysfunction and injury. This review provides an overview on the association of endothelial dysfunction with COVID-19 and its therapeutic implications. Endothelial dysfunction is a common feature of the key comorbidities that increase risk for severe COVID-19 such as hypertension, obesity, diabetes mellitus, coronary artery disease or heart failure. Preliminary studies indicate that vascular endothelial cells can be infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and evidence of widespread endothelial injury and inflammation is found in advanced cases of COVID-19. Prior evidence has established the crucial role of endothelial cells in maintaining and regulating vascular homeostasis and blood coagulation. Aggravation of endothelial dysfunction in COVID-19 may therefore impair organ perfusion and cause a procoagulatory state resulting in both macro- and microvascular thrombotic events. Angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs) and statins are known to improve endothelial dysfunction. Data from smaller observational studies and other viral infections suggests a possible beneficial effect in COVID-19. Other treatments that are currently under investigation for COVID-19 may also act by improving endothelial dysfunction in patients. Focusing therapies on preventing and improving endothelial dysfunction could improve outcomes in COVID-19. Several clinical trials are currently underway to explore this concept.
Keywords: COVID-19, SARS-CoV2, Coronavirus, Endothelial dysfunction, Renin angiotensin system, Statin
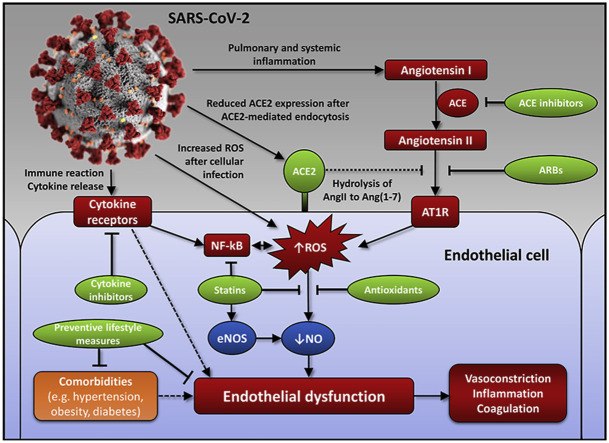
Graphical abstract
Highlights
-
•
New evidence implicates endothelial dysfunction in the pathophysiology of COVID-19.
-
•
It may explain complications such as multi-organ damage or thrombotic events.
-
•
Targeted interventions such as RAS inhibitors or statins may improve outcomes.
-
•
Studies on interventions that affect endothelial dysfunction are underway in COVID-19.
1. Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic is significantly affecting socioeconomic and healthcare systems worldwide. The pathophysiology of its associated disease, coronavirus disease 2019 (COVID-19), is still largely unclear and under active investigation. This article provides an overview on recent evidence linking endothelial dysfunction with COVID-19 and its potential implications for preventing adverse outcomes and treating the disease.
1.1. Endothelial dysfunction: a common denominator in patients at risk for COVID-19
Preliminary studies indicate that patients with cardiovascular risk factors and/or established cardiovascular disease have the highest risk of being hospitalized with COVID-19 and developing a more severe disease course. These risk factors include older age (>65 years), hypertension, obesity, diabetes mellitus, chronic lung disease, coronary artery disease and heart failure [[1], [2], [3], [4]].
Interestingly, a common denominator of all these cardiometabolic diseases is endothelial dysfunction. The endothelium is crucial for maintaining vascular tone and homeostasis – dysfunction is associated with vasoconstriction, inflammation, permeability, and coagulation. It is associated with major risk factors such as age, hypertension, diabetes mellitus, and obesity, as well as development and progression of cardiovascular diseases [5]. Classically, endothelial function is assessed by measuring the dilatation of brachial or coronary arteries in response to shear stress or external stimuli [6]. Newer methods also allow the assessment of smaller vascular beds such as the retinal microcirculation [7].
1.2. SARS-CoV-2 target endothelial cells
The primary site of infection in COVID-19 is the upper and lower respiratory tract. There, SARS-CoV-2 infects goblet secretory cells of the nasal mucosa and alveolar type II pneumocytes by binding to membrane-bound angiotensin-converting enzyme 2 (ACE2) [8]. After priming of the virus spike protein and cleavage of ACE2 by the human protease TMPRSS2, the virus is internalized into the cell and viral replication begins. In severe COVID-19, there is a progressive infection of alveolar pneumocytes with significant viral shedding resulting in apoptosis and necrosis [9]. Interferon-mediated upregulation of ACE2 may facilitate infection of adjacent pneumocytes [8]. The subsequent immune reaction leads to progressive interstitial and alveolar edema, which impairs gas exchange and may eventually result in acute respiratory distress syndrome (ARDS).
Already shortly after the outbreak, reports suggested that COVID-19 affects other organs beyond the lung, most importantly the heart and kidney [10,11]. In severe COVID-19, evidence of acute myocardial injury (elevation of cardiac troponins) is common, and is associated with impaired prognosis. In light of the tissue tropism of SARS-CoV-2 for ACE2-expressing cells, another major organ of the body is an important target of infection: the vascular endothelium [57]. Indeed, ACE2 is expressed abundantly on vascular endothelial cells of both small and large arteries and veins [56]. We recently demonstrated viral inclusion structures within endothelial cells of glomerular capillary loops and signs of widespread endotheliitis in the heart, lung, kidney, liver and gastrointestinal tract in pathological specimens from 3 patients with severe COVID-19 [12]. Endothelial injury and dysfunction may be the result of direct infection by SARS-CoV-2 (e.g. by inducing intracellular oxidative stress [13]) as well as due to the profound systemic inflammatory response. In light of the potential association of COVID-19 with endothelial injury, it seems plausible that patients with preexisting endothelial dysfunction are vulnerable to a more severe disease course given the crucial role of endothelial cells for vascular homeostasis and organ perfusion.
1.3. COVID-19-associated endotheliitis triggers organ damage and thrombotic events
Systemic endotheliitis can explain end-organ damage in severe COVID-19. In a case series from New York [14], one third of COVID-19 patients with electrocardiographic signs of active ischemia showed non-obstructive coronary artery disease, and thus microvascular dysfunction as a likely cause of ischemia. Myocardial inflammation as evidenced by increased cardiac troponins or magnet resonance imaging abnormalities is not uncommon in severe COVID-19 [15,16]. SARS-CoV-2 has been isolated from cardiac autopsy samples, however, this was not regularly associated with an infiltration of immune cells as seen in myocarditis [17]. The virus may rather affect the endothelium leading to secondary myocardial inflammation and dysfunction. The phenotype of myocardial dysfunction and ischemic electrocardiographic features in the absence of coronary obstruction or myocarditis is reminiscent of Takotsubo syndrome, which is also associated with endothelial dysfunction [18].
Vascular endothelial cells play a critical role in vascular homeostasis and the coagulation system. While healthy endothelial cells naturally express factors that induce vascular relaxation and increase blood flow, inhibit platelet aggregation and coagulation, and promote fibrinolysis, dysfunctional endothelial cells shift the balance towards vascular contraction and thrombus formation [19]. Most cardiovascular risk factors indeed cause a decreased endothelial production of vasorelaxing and antithrombotic mediators and a concomitantly increased formation of contracting and prothrombotic factors [20]. In severe COVID-19, markers of both endothelial and platelet activation are increased compared to controls [21]. Extensive microthrombosis promoted and aggravated by endothelial dysfunction could explain the profound elevation of D-dimers and thrombocytopenia in severe COVID-19 [3]. In line with these haematologic findings, recent reports show increased risk of both venous and arterial thrombotic events in COVID-19 [22,23]. A recent case series also suggested that pulmonary microthrombi and pulmonary endothelial dysfunction explain the unusual dead-space and shunt physiology found in severe COVID-19 patients [24]. Indeed, significant pulmonary endotheliitis, microvascular thrombosis and evidence of pulmonary endothelial infection by SARS-CoV2 was observed in another pathological case series [25]. Pulmonary microvascular dysfunction may therefore be an underlying mechanism behind the phenomenon of severe hypoxia despite relatively preserved lung mechanics in COVID-19 [26]. In children with COVID-19-associated chilblains of the extremities, profound endothelial inflammation along with endothelial infection with SARS-CoV2 was observed in a small case series [27].
1.4. Targeting endothelial dysfunction in COVID-19
Most therapies under active investigation for COVID-19 focus on inhibition of viral replication and suppression of the excessive immune response. However, in light of the above, treatment of endothelial dysfunction is a promising approach to protect vulnerable patients and to improve outcomes in COVID-19. Many studies have demonstrated the possibility to enhance vascular function via lifestyle interventions and drug therapies [28]. Two widely used drug classes, renin angiotensin system (RAS) inhibitors and statins, have been shown in an abundant number of studies to consistently improve endothelial function in patients. Both drug classes exert pleiotropic effects on the endothelium and promote endothelium-induced stimulation of vascular relaxation as well as endothelium-mediated inhibition of thrombus formation.
1.4.1. RAS inhibitors
Angiotensin II is a well-known mediator of endothelial dysfunction, which is in part mediated by increased oxidative stress following angiotensin II receptor type 1 activation [29]. Indeed, both ACE inhibitors and angiotensin receptor blockers (ARBs) have been shown to improve endothelial dysfunction [30,31]. They may also attenuate procoagulatory states by reducing the expression of tissue factor in endothelial cells and other cell types [32]. The use of RAS inhibitors is not without controversy in COVID-19: They are associated with an upregulation of ACE2, which may (theoretically) increase susceptibility to infection. However, ACE2 is a part of the natural host response against pulmonary infections [33] and antagonizes RAS activation by hydrolysis of angiotensin II into angiotensin (1–7), a vasodilator with anti-oxidant and anti-inflammatory effects [34]. ACE2 is downregulated after invasion of SARS-CoV-2 into cells. This may lead to unopposed RAS activation resulting in endothelial injury and a pro-inflammatory and pro-thrombotic state in COVID-19 – which may be amendable by pharmacological RAS blockade [35]. Indeed, the use of RAS inhibitors was not associated with a higher risk of SARS-CoV-2 infection or an adverse outcome in recent observational studies [[36], [37], [38], [39]]. In a Spanish population-based study, a borderline-significant reduced risk for COVID-19 hospital admissions was found with ACE inhibitors and a lower risk for patients with diabetes who were treated with RAS inhibitors vs. non-users [40]. A trend of lower COVID-19-related mortality with RAS inhibitors was also found in a meta-analysis of four studies [41]. In a UK cohort study, RAS inhibitors were associated with a lower risk of COVID-19 [42]. Recently, results from the first randomized trial on this topic were presented (BRACE-CORONA) [43]. In this trial, discontinuation of RAS inhibitors in hospitalized patients with COVID-19 had no beneficial effect compared to continuation of therapy. Therefore, it is recommended to continue RAS inhibitors in COVID-19 patients who are already on such therapies as long as there are no acute contraindications such as severe kidney injury, significant hyperkalemia or symptomatic hypotension. Whether general RAS blockade in COVID-19 is beneficial needs to be confirmed in clinical trials. Several intervention studies with ACE inhibitors and ARBs currently explore this hypothesis (Table 1 and Supplementary Table 1).
Table 1.
Selecteda randomized controlled trials (ongoing or planned) on interventions in COVID-19 that are also known to improve endothelial function.
| Trial identifier (Trial acronym) | Description of intervention | Country | Estimated enrollment |
|---|---|---|---|
| NCT04328012 (COVIDMED) | Losartan vs placebo (other arms: lopinavir/ritonavir, hydroxychloroquine) in patients with COVID-19 and not on previous RAS inhibition | USA | 4000 |
| NCT04330300 (CORONACION) | Continuation of RAS inhibitors vs. switch to different antihypertensive drug in patients with COVID-19, hypertension and previously on a RAS inhibitor | Ireland | 2414 |
| NCT04366050 (RAMIC) | Ramipril vs. placebo for 14 days in patients with COVID-19 in non-intensive care setting | USA | 560 |
| NCT04343001 (CRASH-19) | Aspirin, losartan, simvastatin or combinations thereof vs. standard of care (2 × 2 x 2) in hospitalized COVID-19 patients | International | 10,000 |
| EudraCT-2020-001319-26 (FJD-COVID-ESTATINAS) | Rosuvastatin vs. no treatment in patients with COVID-19 who required hospitalization | Spain | 1080 |
| NCT04333407 (C-19-ACS) | Atorvastatin combined with aspirin, clopidogrel, omeprazole and very-low dose rivaroxaban vs. control in patients with COVID-19 and elevated cardiovascular risk | International | 3170 |
| NCT04380402 (STATCO19) | Atorvastatin vs. standard-care of atorvastatin as an adjunctive treatment in COVID-19 in non-ICU patients not on prior statin therapy | USA | 300 |
| NCT04401150 (LOVIT-COVID) | Intravenous vitamin C vs. placebo in hospitalized COVID-19 patients | Canada | 800 |
| NCT04342728 (COVIDAtoZ) | Vitamin C, zinc or the combination vs. standard of care in ambulatory COVID-19 patients | USA | 520 |
| NCT04335084 (HELPCOVID-19) | Vitamin C, hydroxychloroquine, vitamin D and zinc vs. placebo for the prevention of COVID-19 infection in non-infected patients | USA | 600 |
| NCT04400890 | Plant polyphenol supplement vs. placebo on top of vitamin D in outpatients with mild COVID-19 | USA | 200 |
| NCT04404218 (ACAI) | Acai palm berry extract for 30 days vs. placebo in patients with mild to moderate COVID-19 | Canada | 480 |
COVID-19, coronavirus disease 2019; NCT, national clinical trial identifier; RAS, renin angiotensin system.
For the complete list see Supplementary Table 1.
1.4.2. Statins
Statins are another promising drug class for treating endothelial dysfunction and preventing vascular damage in COVID-19. Similar to RAS inhibitors, statins improve endothelial function in patients with or at risk for cardiovascular disease [44]. They improve endothelial function via different mechanisms, including reduction of oxidized low-densitiy lipoprotein cholesterol, increased expression and improved coupling of endothelial nitric oxide synthase (eNOS), suppression of pro-oxidant enzymes such as NADPH oxidase and inhibition of nuclear factor kappa B (NF-κB) and other pro-inflammatory transcriptional and signal transduction pathways [[45], [46], [47]]. Independent of nitric oxide, statins prevent tissue factor expression in endothelial cells [48] which may favorably affect blood coagulation and platelet activation [46]. We previously showed that statins improve endothelial dysfunction in rheumatoid arthritis [49], suggesting that they may be particularly helpful in inflammatory conditions characterized by endothelial dysfunction. Some evidence points toward a beneficial effect in viral pneumonias such as influenza [50]. Larger studies on the effects of statins in COVID-19 are still pending. A small observational study in elderly nursing home subjects suggested a higher chance of a symptom-free COVID-19 infection in statin-users vs. non-users [39]. In a retrospective cohort study in China, statin use was associated with lower mortality compared to non-use in COVID-19 [51]. Several intervention studies studying the role of statins in COVID-19 have recently been announced (Supplementary Table 1). Until then, it seems prudent to continue statins in COVID-19 patients who already received the drugs before infection and initiate statins in all patients who meet cardiovascular guideline-criteria supporting their use.
1.4.3. Anti-inflammatory therapies
Several anti-inflammatory therapies under investigation for COVID-19 may partly act by improving endothelial function. For example, improvement of endothelial dysfunction has been described for tumor necrosis factor alpha inhibitors [52] or anti-IL-6 receptor antibodies [53].
1.4.4. Other approaches
Beyond drug therapies, the importance of effective preventive measures cannot be overstated during the current pandemic. In that regard, improving or maintaining a normal endothelial function by well-established lifestyle measures (i.e. keeping a normal weight, regular physical activity, abstaining from smoking and consuming a healthy and nutritious diet) may be helpful to reduce the risk of COVID-19. Specific supplemental interventions that reduce endothelial dysfunction (e.g. antioxidants [54], flavanols [55]) could also be considered for further testing. Of note, several trials studying the effects of vitamin C, antioxidants and polyphenols in COVID-19 have been started (Supplementary Table 1).
2. Conclusions
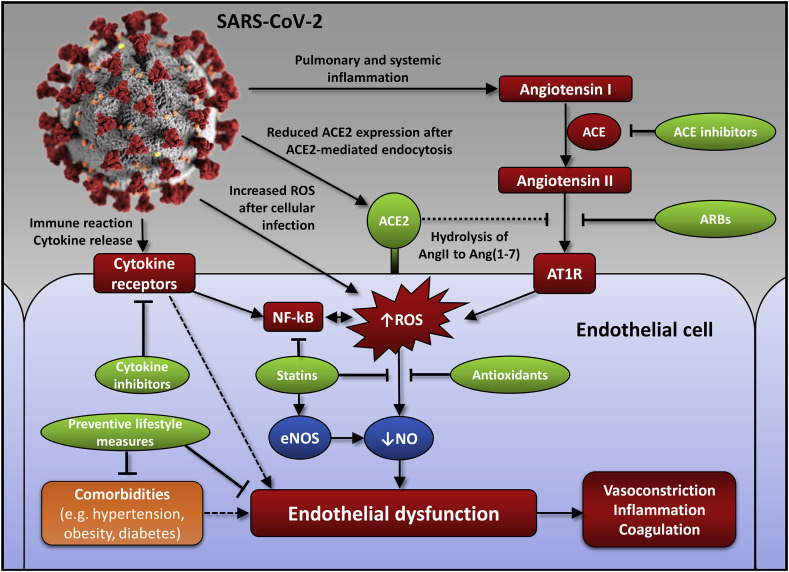
Accumulating evidence points toward an important role of endothelial dysfunction in the pathogenesis of COVID-19 (Fig. 1 ). Therapies aiming to improve endothelial dysfunction such as RAS inhibitors or statins may be particularly helpful to prevent and manage systemic complications of SARS-CoV-2 infection. Based on the current evidence, we recommend to continue RAS inhibitors and statins in patients with COVID-19 as long as there are no acute contraindications. For prevention, we recommend that patients with a cardiovascular indication as per current guidelines should be prescribed RAS inhibitors and statins along with optimal lifestyle measures. Whether these therapies are beneficial in COVID-19 patients without such indications needs to be evaluated and tested in upcoming clinical trials.
Fig.1.
Mechanisms of endothelial dysfunction in COVID-19.
SARS-CoV-2 could aggravate endothelial dysfunction and lead to systemic complications by several mechanisms. (1) The inflammatory reaction in COVID-19 can activate the renin angiotensin system (RAS) either directly via increasing angiotensin I (Ang I), or indirectly by reducing the surface expression of angiotensin-converting enzyme 2 (ACE2). ACE2 is responsible for the hydrolysis of Ang II into the vasodilator Ang (1-7), which opposes the actions of Ang II thereby counterbalancing RAS activation. (2) Activation of the angiotensin II type 1 receptor (AT1R), along with direct infection of endothelial cells by the virus, (3) increases reactive oxygen species (ROS) and activates nuclear factor kappa B (NF-kB), which inactivates nitric oxide (NO) to peroxynitrite and reduces its production by uncoupling endothelial NO synthase (eNOS). (4) Activation of several cytokine receptors (e.g. tumor necrosis factor alpha receptor, interleukin 6 receptor) can directly or indirectly impair endothelial function. Endothelial dysfunction in turn impairs organ perfusion by disrupting the balance between vasoconstriction and dilatation, increases inflammation and leads to a pro-thrombotic state in both larger and smaller vessels, such as by increasing tissue factor and favoring platelet activation. This vicious cycle may be amendable by treatments targeting different steps of the cascade, such as ACE inhibitors, angiotensin receptor blockers (ARBs), cytokine inhibitors (e.g. interleukin 6 receptor antibodies) or statins. Statins may be helpful by reducing oxidized LDL levels and NADPH oxidase activity, which decrease reactive oxygen species (ROS), directly or indirectly affecting the transcription of NF-kB or by improving coupling of eNOS. Measures to prevent and treat important comorbidities could also be helpful along with selected supplements such as antioxidants.
Author contributions
M.P.N. A.J.F. and F.R. conceptualized the manuscript. M.P.N. created and finalized the manuscript, table and figure. B.H., F·C.T., F.R. and A.J.F. critically revised and expanded sections of the manuscript. No compensation was paid for any work on the manuscript.
Declaration of competing interest
M.P.N. declares speaker fees by Imedos Systems, an independent grant award sponsored by Amgen, and congress travel support by Amgen, Orion Pharma, Servier and St. Jude Medical, unrelated to this article.
B.H. declares speaker fees and travel support by Novartis, unrelated to this article.
F·C.T. declares travel support from Amgen and Bayer, unrelated to this article.
F.R. has been paid for the time spent as a committee member for clinical trials, advisory boards, other forms of consulting and lectures or presentations. These payments were made directly to the University of Zurich and no personal payments were received in relation to these trials or other activities.
A.J.F. declares fees from Alnylam, Amgen, AstraZeneca, Fresenius, Imedos Systems, Novartis, Pfizer, Roche, Vifor, and Zoll, unrelated to this article.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.atherosclerosis.2020.10.014.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Cdc COVID-response team: preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 - United States, february 12-march 28, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu C., Chen X., Cai Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in wuhan, China. JAMA Intern Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guo T., Fan Y., Chen M. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brunner H., Cockcroft J.R., Deanfield J. Endothelial function and dysfunction. Part II: association with cardiovascular risk factors and diseases. a statement by the working group on endothelins and endothelial factors of the European society of hypertension. J. Hypertens. 2005;23:233–246. doi: 10.1097/00004872-200502000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Flammer A.J., Anderson T., Celermajer D.S. The assessment of endothelial function: from research into clinical practice. Circulation. 2012;126:753–767. doi: 10.1161/CIRCULATIONAHA.112.093245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nägele M.P., Barthelmes J., Ludovici V. Retinal microvascular dysfunction in heart failure. Eur. Heart J. 2018;39:47–56. doi: 10.1093/eurheartj/ehx565. [DOI] [PubMed] [Google Scholar]
- 8.Ziegler C.G.K., Allon S.J., Nyquist S.K. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181:1016–1035 e1019. doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mason R.J. Pathogenesis of COVID-19 from a cell biology perspective. Eur. Respir. J. 2020;55 doi: 10.1183/13993003.00607-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fanelli V., Fiorentino M., Cantaluppi V. Acute kidney injury in SARS-CoV-2 infected patients. Crit. Care. 2020;24:155. doi: 10.1186/s13054-020-02872-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varga Z., Flammer A.J., Steiger P. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khomich O.A., Kochetkov S.N., Bartosch B. Redox biology of respiratory viral infections. Viruses. 2018:10. doi: 10.3390/v10080392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bangalore S., Sharma A., Slotwiner A. ST-segment elevation in patients with covid-19 - a case series. N. Engl. J. Med. 2020;382:2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Puntmann V.O., Carerj M.L., Wieters I. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.3557. Published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chatzizisis Y.S., Gajanan G., Bhatt D.L. Management of acute myocardial injury in patients with confirmed or suspected COVID-19. Atherosclerosis. 2020;305:58–60. doi: 10.1016/j.atherosclerosis.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lindner D., Fitzek A., Brauninger H. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.3551. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Naegele M., Flammer A.J., Enseleit F. Endothelial function and sympathetic nervous system activity in patients with Takotsubo syndrome. Int. J. Cardiol. 2016;224:226–230. doi: 10.1016/j.ijcard.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 19.Yau J.W., Teoh H., Verma S. Endothelial cell control of thrombosis. BMC Cardiovasc. Disord. 2015;15:130. doi: 10.1186/s12872-015-0124-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holy E.W., Akhmedov A., Speer T. Carbamylated low-density lipoproteins induce a prothrombotic state via LOX-1: impact on arterial thrombus formation in vivo. J. Am. Coll. Cardiol. 2016;68:1664–1676. doi: 10.1016/j.jacc.2016.07.755. [DOI] [PubMed] [Google Scholar]
- 21.Goshua G., Pine A.B., Meizlish M.L. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7:e575–e582. doi: 10.1016/S2352-3026(20)30216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lodigiani C., Iapichino G., Carenzo L. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb. Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bikdeli B., Madhavan M.V., Jimenez D. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Poor H.D., Ventetuolo C.E., Tolbert T. COVID-19 critical illness pathophysiology driven by diffuse pulmonary thrombi and pulmonary endothelial dysfunction responsive to thrombolysis. Clin. Transl. Med. 2020;10(2):e44. doi: 10.1002/ctm2.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ackermann M., Verleden S.E., Kuehnel M. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in covid-19. N. Engl. J. Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gattinoni L., Coppola S., Cressoni M. COVID-19 does not lead to a "typical" acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2020;201:1299–1300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colmenero I., Santonja C., Alonso-Riano M. SARS-CoV-2 endothelial infection causes COVID-19 chilblains: histopathological, immunohistochemical and ultrastructural study of seven paediatric cases. Br. J. Dermatol. 2020 doi: 10.1111/bjd.19327. Published Online 20 June 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Daiber A., Steven S., Weber A. Targeting vascular (endothelial) dysfunction. Br. J. Pharmacol. 2017;174:1591–1619. doi: 10.1111/bph.13517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wen H., Gwathmey J.K., Xie L.H. Oxidative stress-mediated effects of angiotensin II in the cardiovascular system. World J. Hypertens. 2012;2:34–44. doi: 10.5494/wjh.v2.i4.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shahin Y., Khan J.A., Samuel N. Angiotensin converting enzyme inhibitors effect on endothelial dysfunction: a meta-analysis of randomised controlled trials. Atherosclerosis. 2011;216:7–16. doi: 10.1016/j.atherosclerosis.2011.02.044. [DOI] [PubMed] [Google Scholar]
- 31.Li S., Wu Y., Yu G. Angiotensin II receptor blockers improve peripheral endothelial function: a meta-analysis of randomized controlled trials. PloS One. 2014;9 doi: 10.1371/journal.pone.0090217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Muller D.N., Mervaala E.M., Dechend R. Angiotensin II (AT(1)) receptor blockade reduces vascular tissue factor in angiotensin II-induced cardiac vasculopathy. Am. J. Pathol. 2000;157:111–122. doi: 10.1016/S0002-9440(10)64523-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sodhi C.P., Nguyen J., Yamaguchi Y. A dynamic variation of pulmonary ACE2 is required to modulate neutrophilic inflammation in response to Pseudomonas aeruginosa lung infection in mice. J. Immunol. 2019;203:3000–3012. doi: 10.4049/jimmunol.1900579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Santos R.A.S., Sampaio W.O., Alzamora A.C. The ACE2/angiotensin-(1-7)/MAS Axis of the renin-angiotensin system: focus on angiotensin-(1-7) Physiol. Rev. 2018;98:505–553. doi: 10.1152/physrev.00023.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verdecchia P., Cavallini C., Spanevello A. The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur. J. Intern. Med. 2020;76:14–20. doi: 10.1016/j.ejim.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reynolds H.R., Adhikari S., Pulgarin C. Renin-angiotensin-Aldosterone system inhibitors and risk of covid-19. N. Engl. J. Med. 2020;382:2441–2448. doi: 10.1056/NEJMoa2008975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fosbol E.L., Butt J.H., Ostergaard L. Association of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with COVID-19 diagnosis and mortality. J. Am. Med. Assoc. 2020;324:168–177. doi: 10.1001/jama.2020.11301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Flacco M.E., Acuti Martellucci C., Bravi F. Treatment with ACE inhibitors or ARBs and risk of severe/lethal COVID-19: a meta-analysis. Heart. 2020;106:1519–1524. doi: 10.1136/heartjnl-2020-317336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De Spiegeleer A., Bronselaer A., Teo J.T. The effects of ARBs, ACEis, and statins on clinical outcomes of COVID-19 infection among nursing home residents. J. Am. Med. Dir. Assoc. 2020;21:909–914 e902. doi: 10.1016/j.jamda.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Abajo F.J., Rodriguez-Martin S., Lerma V. Use of renin-angiotensin-aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study. Lancet. 2020;395:1705–1714. doi: 10.1016/S0140-6736(20)31030-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gao C., Cai Y., Zhang K. Association of hypertension and antihypertensive treatment with COVID-19 mortality: a retrospective observational study. Eur. Heart J. 2020;41:2058–2066. doi: 10.1093/eurheartj/ehaa433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hippisley-Cox J., Young D., Coupland C. Risk of severe COVID-19 disease with ACE inhibitors and angiotensin receptor blockers: cohort study including 8.3 million people. Heart. 2020;106:1503–1511. doi: 10.1136/heartjnl-2020-317393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lopes R. Brace corona: continuing vs. Suspending ACE inhibitors and ARBs in COVID-19 in, European society of cardiology congress 2020 (online congress) https://programme.escardio.org/ESC2020/Live-Sessions/31202-hot-line-brace-corona Source.
- 44.Reriani M.K., Dunlay S.M., Gupta B. Effects of statins on coronary and peripheral endothelial function in humans: a systematic review and meta-analysis of randomized controlled trials. Eur. J. Cardiovasc. Prev. Rehabil. 2011;18:704–716. doi: 10.1177/1741826711398430. [DOI] [PubMed] [Google Scholar]
- 45.Penny W.F., Ben-Yehuda O., Kuroe K. Improvement of coronary artery endothelial dysfunction with lipid-lowering therapy: heterogeneity of segmental response and correlation with plasma-oxidized low density lipoprotein. J. Am. Coll. Cardiol. 2001;37:766–774. doi: 10.1016/s0735-1097(00)01180-3. [DOI] [PubMed] [Google Scholar]
- 46.Margaritis M., Channon K.M., Antoniades C. Statins as regulators of redox state in the vascular endothelium: beyond lipid lowering. Antioxidants Redox Signal. 2014;20:1198–1215. doi: 10.1089/ars.2013.5430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ramasubbu K., Estep J., White D.L. Experimental and clinical basis for the use of statins in patients with ischemic and nonischemic cardiomyopathy. J. Am. Coll. Cardiol. 2008;51:415–426. doi: 10.1016/j.jacc.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 48.Eto M., Kozai T., Cosentino F. Statin prevents tissue factor expression in human endothelial cells: role of Rho/Rho-kinase and Akt pathways. Circulation. 2002;105:1756–1759. doi: 10.1161/01.cir.0000015465.73933.3b. [DOI] [PubMed] [Google Scholar]
- 49.Hermann F., Forster A., Chenevard R. Simvastatin improves endothelial function in patients with rheumatoid arthritis. J. Am. Coll. Cardiol. 2005;45:461–464. doi: 10.1016/j.jacc.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 50.Fedson D.S. Pandemic influenza: a potential role for statins in treatment and prophylaxis. Clin. Infect. Dis. 2006;43:199–205. doi: 10.1086/505116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang X.-J., Qin J.-J., Cheng X. In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19. Cell Metabol. 2020;32(2):176–187. doi: 10.1016/j.cmet.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hurlimann D., Forster A., Noll G. Anti-tumor necrosis factor-alpha treatment improves endothelial function in patients with rheumatoid arthritis. Circulation. 2002;106:2184–2187. doi: 10.1161/01.cir.0000037521.71373.44. [DOI] [PubMed] [Google Scholar]
- 53.Ruiz-Limon P., Ortega R., Arias de la Rosa I. Tocilizumab improves the proatherothrombotic profile of rheumatoid arthritis patients modulating endothelial dysfunction. NETosis, and inflammation, Transl Res. 2017;183:87–103. doi: 10.1016/j.trsl.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 54.Peterhans E. Oxidants and antioxidants in viral diseases: disease mechanisms and metabolic regulation. J. Nutr. 1997;127:962S–965S. doi: 10.1093/jn/127.5.962S. [DOI] [PubMed] [Google Scholar]
- 55.Flammer A.J., Sudano I., Wolfrum M. Cardiovascular effects of flavanol-rich chocolate in patients with heart failure. Eur. Heart J. 2012;33:2172–2180. doi: 10.1093/eurheartj/ehr448. [DOI] [PubMed] [Google Scholar]
- 56.Hamming I., Bulthuis M.L.C., Lely A.T. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2014;203(2):631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Monteil V., Kwon H., Prado P. Inhibition of SARS-CoV-2 Infections in Engineered Human Tissues Using Clinical-Grade Soluble Human ACE2. Cell. 2020;181(4):905–913. doi: 10.1016/j.cell.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.