Abstract
Objective
Text messaging has been proposed as a method for increasing the reach of interventions for harmful alcohol and other drug use. This paper describes the design of an automated text messaging adjunct to a substance use intervention intended to support adolescents and young adults attempting to change their alcohol and other drug use behavior. Feasibility and acceptability testing was conducted as part of this pilot study.
Method
Five focus groups were conducted to refine text message content and finalize pilot intervention design. Automated, daily, substance use-related reminder text messages were sent to pilot intervention participants (n = 39), who were recruited from outpatient treatment.
Results
Of those who were invited, 63% enrolled in the study and 89.7% remained enrolled in the study as measured by completing at least one assessment after baseline. Participants reported a positive experience with the messages, particularly supportive/empowering messages and commitment reminder messages.
Conclusions
These findings suggest that text messaging is a feasible and acceptable method for delivery of substance use-related reminder content as an adjunct to substance use intervention.
Keywords: Text messaging, short message service, mobile phone, mHealth, substance use disorders, reminders
Introduction
The use of alcohol or other drugs that lead to unwanted negative consequences, or substance use disorder (SUD), is a major health and safety concern that typically begins during adolescence or young adulthood.1 Adolescence is the developmental period during which individuals go through some of the most rapid changes they will ever experience and is followed by the major life transition to young adulthood.2–5 This time of change, maturation, and transition makes individuals especially susceptible to the initiation of substance use.2,6 Adolescent and young adult substance use can cause a variety of immediate consequences (e.g., hangover, assault, risky sexual behavior, impaired driving,) and has been correlated with a number of future consequences (e.g., academic failure, relationship difficulties, physical illness, impaired adult cognitive functioning).7–12 Early onset of substance use increases the likelihood an individual will continue to misuse substances for an extended period of time,8,9,13 and is associated with increased negative health outcomes over time.2,14–16 Because of the quantity and severity of consequences associated with early initiation of substance use, the long-term consequences related to age of initiation, and the challenging nature of working with adolescents and young adults, numerous specialized interventions have been developed to target these populations.17–19
Individuals attempting to change their substance use often underestimate the difficulty in learning to control urges and the effort required to enact successful behavior change. Consistent findings of high relapse rates underscore susceptibility to relapse, which is considered a defining feature of SUD.20–22 The National Institute on Drug Abuse (NIDA) has stated that recovery from SUD is a long-term process that frequently requires multiple courses of treatment. It also suggests that substance use relapses should be treated similarly to chronic illness relapses—relapse can occur and should be seen as an indicator that treatment needs to be adjusted or resumed.23 Relapse is a challenge that is especially problematic for adolescents and young adults.
Marlatt’s cognitive-behavioral relapse model posits that relatively stable or tonic factors and phasic responses in a high-risk situation influence relapse timing and severity.24 The behavioral economics concept of delay discounting (defined as a tendency to place less value on rewards that are temporally delayed), a concept widely used as a measure of impulsiveness, may be one factor that influences adolescent and young adult relapse.25,26 Addictions research has found higher levels of delay discounting predict poorer treatment outcome, decreased time to relapse, and increased addiction severity.27–29 Results suggest that adolescents are more susceptible to delay discounting than adults.30
Adolescent substance use may also impair neurocognitive functioning including memory.31 When individuals seek to change a behavior they sometimes rely on prospective memory.32,33 Event-based prospective memory is considered to be a cognitively demanding task, requiring an individual to shift their focus from an ongoing task to a perspective memory cue (e.g., remembering to stop at the grocery store after seeing the grocery sign while driving home).34 Additionally, interruptions during delays in prospective memory tasks have been found to distract from task completion.35 Some research suggests external memory aids, such as paired imagery or reminders, may help enhance prospective memory.33,36,37
Reminders are a behavioral strategy (and potential prospective memory aid) that can help individuals complete a variety of health promotion behaviors such as medical practice adherence and appointment attendance.38,39 In the context of substance use behavior change, reminders can help individuals remain mindful of their behavior change decision, the reasons for their decisions, and potential pitfalls that might occur between treatment sessions. For individuals prone to devaluing future rewards, reminders can help them recall why they want to change. Therapists and treatment or support group members may remind individuals during meetings of their reasons for decisions to change substance use (e.g., to quit using drugs due to potential consequences); possible cues (triggers) that might stimulate drug use; and what circumstances might interfere with following through on their decisions (e.g., invitations to parties).
Most adolescents and young adults have replaced more traditional reminder mechanisms such as alarm clocks, paper calendar, and watches with smartphones and smartwatches.40,41 Mobile phone use does not appear to be limited by individual factors such as age or socioeconomic status.42 Adolescents and young adults send and receive mobile phone-based text messages, or short messaging service (SMS), at an extraordinary rate—on average over six text messages per waking hour, over 100 messages per day, and over 3,300 messages per month.43–45
Given high mobile phone ownership rates among people of all ages, it is not surprising that research into mHealth (i.e., the use of mobile computing and communication technologies in health care and public health) has increased rapidly since the early 2000s.46,47 There is emerging evidence about what components make mHealth interventions effective. For example, interventions using an individualized or decreasing number of messages over intervention course appear to be more effective than interventions using a fixed number of messages.48 mHealth-based SUD interventions have been investigated and found to be effective for individuals across an array of populations.49 More recently, researchers have begun to investigate the impact of SMS and other mHealth reminders as an adjunct to treatment. One pilot study investigated the use of text message reminders as an adjunct to cognitive-behavioral therapy (CBT) for depression among an outpatient, adult Latino population.50 All participants received a 16-week manualized CBT treatment for depression. Participants in the text message adjunct condition received a daily adjunct to treatment (based on a CBT module), a daily mood rating prompt, an optional daily medication reminder, a weekly reminder to attend psychotherapy, and a monthly opt-out message to cease message delivery. Participants reported an overall positive experience receiving the messages and indicated the messages helped them feel closer to the group.
The purpose of this pilot study was to assess the feasibility and acceptability of an SMS adjunct to SUD intervention in a sample of adolescents and young adults drawn from SUD treatment agencies and SUD interventions for young adults who violated alcohol and drug policies on a college campus. Recruitment and retention rates were used to assess feasibility and acceptability was assessed by reviewing quantitative and qualitative participant feedback. We hypothesized that participants would react positively to the SMS and that they would respond at high rates to messages inquiring about perceived helpfulness of messages. Additionally, the study allowed us to investigate SMS timing, frequency, duration, and content preferences.
Method
Participants
Focus groups
Twenty-four focus group participants, ages 13-17 (Mage = 14.7, 66.7% female), were recruited from SUD treatment agencies in Washington State. Participants were recruited using flyers with study information. Eligibility criteria was age (13–17 years old) and enrollment in outpatient SUD treatment.
Pilot intervention
The pilot study was part of a larger study that recruited 59 participants. The pilot study included 39 adolescents and young adults ages 13–22 (Mage = 18.5, 51.3% male) who received substance use-related text messages. A majority of participants identified as non-Hispanic White (77%; 30/39), and the remainder identified as Asian/Asian-American (15%; 6/39) or Other (8%; 3/39). All participants reported lifetime alcohol use (100%) and most reported lifetime cannabis use (92.3%). Lifetime use was less frequently reported for sedatives (12.8%), hallucinogens (20.5%), and opioids (20.5%). Participants were recruited from two substance use treatment providers, (1) outpatient treatment centers located throughout the United States that use The Seven Challenges (a manualized evidence-based cognitive-behavioral/problem solving therapy that includes a focus on harm reduction and relapse prevention) (18%; 7/39) and (2) providers of brief motivational interventions for substance use at a large west-coast university that used the Alcohol Skills Training Workshop framework (82%; 32/39). Recruitment methods were similar. Both used flyers (either printed or projected via PowerPoint) with study information for adolescents and young adults to contact the research team via the study website, social media, email, or phone. Participants recruited from the Alcohol Skills Training Workshops were invited to provide contact information if they preferred the research team contact them. Participants were screened for eligibility either over the phone or online. In order to meet eligibility criteria, participants had to be between 13 and 22 years old, have their own SMS-capable cellphone, and have a stated commitment to substance use behavior change (e.g., decided to set limits or abstain entirely). Individuals were not eligible for the pilot study if they participated in the focus groups.
Procedure
Focus groups
Prior to beginning the trial, a list of 100 substance use-related messages were created by the authors. The list was primarily influenced by harm reduction psychotherapy51 and motivational interviewing52 strategies and techniques. The messages were classified as belonging to one of four content categories: supportive/empowering (e.g., “You are in control.”); threatening/consequential (e.g., “If you slip up you’re going to get in trouble”); commitment reminders (e.g., “This decision is for a better life.”); and educational (e.g., “Think about your future. Your health matters.”). See Appendix A for full message list.
Five, hour-long focus groups were conducted to help refine text message content and finalize study design. The focus group procedure was approved by the University of Washington Institutional Review Board (#49761) and a waiver of parental consent was obtained. Participants were recruited from existing groups at treatment agencies and took place after regularly scheduled meetings to minimize participant burden. Focus groups were conducted by the first author. Participants were invited to share their opinions about the overall study and specific facets of the study including message content, message timing, message frequency, duration of messaging, and other details related to participation. Open-ended questions (e.g., “If you could receive a text [message] saying whatever you want to help support your decision [to change], what would you want?”) were used to generate participant responses. They helped inform the final message list that was used in the study as well as other factors such as message timing. Focus groups were audio recorded and then transcribed. Participants were compensated $30 for their participation in the focus groups.
Focus group responses were analyzed using a modified version of the Rapid Identification of Themes from Audio Recordings.53 Each of the focus group transcripts were reviewed by the first author and a research assistant. A coding form to summarize responses to each question and document preliminary themes related to study design was entered into an Excel spreadsheet to identify and compare response themes across questions (rows) for each participant (columns). The first and second author reviewed the spreadsheet to identify common themes related to study preferences and engaged in a consensus process to settle disagreements and finalize themes.
Pilot intervention
Participants in the pilot study were recruited using flyers and were screened/enrolled online or over the phone. The study was approved by the University of Washington Institutional Review Board (#1405) and a waiver of written documentation of consent and a waiver of parental consent was obtained. Participants were enrolled in the study for eight weeks and selected 28 messages to receive from a list of 100 substance-use related messages. They received daily SMS for the first four weeks. Four SMS were sent per day for the first two weeks, and two SMS per day during the third and fourth week. In order to decrease message fatigue, the message order was randomized. During the four weeks of SMS, participants also received an SMS at the end of each day that asked them to rate the perceived helpfulness of the messages during the past day. Final feedback about the study was obtained four weeks after sending the study SMS.
Messages were sent using Twilio, a cloud-based messaging service. On weekdays when participants received four SMS per day, messages were sent at 10 AM, 2 PM, 6 PM, and 10 PM within a +/− 30-minute interval (e.g., a random time between 9:30 AM and 10:30 AM). On weekends, the message delivery schedule was delayed one hour. When participants were receiving two SMS per day, participants randomly received a message one of the first two message times (10 AM or 2 PM) and one of the second two message times (6 PM or 10 PM) within a +/− 30-minute interval. Weekend messages were similarly delayed an hour when receiving two SMS per day.
Participants were emailed and texted an invitation and reminders to complete study surveys. Participants were compensated after each of the four surveys they completed—up to a total of $40. To ensure participants completed surveys within an appropriate timeframe, they were informed the response deadline for compensation was one week after survey invitation was sent. Participants were compensated using electronic gift certificates.
Measures
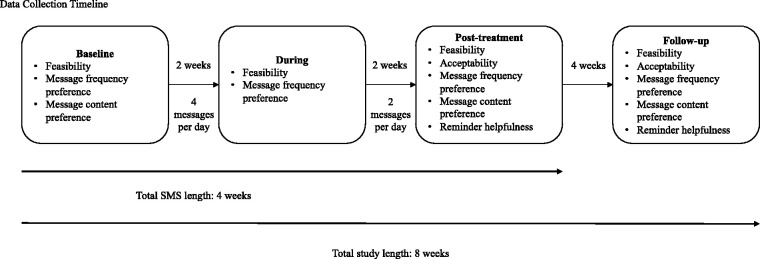
Surveys were completed online. They occurred at four times, (1) when participants signed up for the study (baseline), (2) after receiving two weeks of SMS (two weeks after baseline; during), (3) after receiving the full four weeks of SMS (two weeks after during; post-treatment), and (4) four weeks after the end of SMS (four weeks after post; follow-up). See Figure 1 for study flowchart.
Figure 1.
Data collection timeline.
Feasibility
Assessment of feasibility was completed by analyzing recruitment and retention rates. An a priori threshold of greater than or equal to 80% recruitment and retention rate was selected as meeting a threshold for acceptable feasibility.
Acceptability
At post-treatment and follow-up, participants answered 14 yes/no questions regarding perceived ways the SMS were supportive (e.g., “They felt like a friend supporting me.”), helpful (e.g., “The helped me stay on track.”), and otherwise liked (e.g., “They reminded me of my decision.”) or disliked (e.g., “I couldn't relate to the messages,” “They got boring.”). Additionally, participants were invited to answer open-ended prompts regarding what they liked or disliked about the study. Participants also responded to a daily prompt asking how much they liked the messages they received that day. Responses were made using a 1 (not at all) to 5 (very much) response scale.
Message frequency preference
Participants were asked for preferences regarding: (1) amount of daily SMS they would prefer to receive (“If you could choose to receive any number of text messages per day for any length of time, how many would you want?”) and (2) length of time they like to receive SMS (“For how many weeks?”). Frequency preference was assessed at all four time points.
Message content preference
Participants were asked to select the messages they would most like to receive at baseline. At post-treatment, participants were asked to select the three messages they liked most.
Helpfulness of reminders
Participants were asked multiple questions to further understand what benefits message may offer including (1) how helpful they found the messages as a reminder of their substance use behavior change goals (“How much did the messages help keep your decision in mind to not use drugs or to limit your use of drugs?”) and (2) how supportive the messages felt (“How much did the messages help support you in not using drugs or using within your limits?”). Responses were made on a 1 (no reminder/support) to 7 (constant reminder/support) response scale. Helpfulness of reminders was assessed at post-treatment and follow-up.
Open-ended questions
At post-treatment and follow-up, participants were invited to complete six open-ended questions regarding thoughts and opinions about the study, the SMS content (“If you could choose your own messages, what would they say?”), and SMS timing (e.g., “What are the times of day (or situations) that you most likely would be tempted to drink or use drugs?”).
Results
Focus groups
Focus group participants provided suggestions for new message content and feedback on study design (e.g., message timing). In each focus group, a general theme among a minority of participants suggested a preference to receive threatening or consequential messages (e.g., “If you use, you're disappointing your entire family… It's like the stick instead of the carrot. The carrot is the incentive and the stick is the bad side of things. So, it's reminding you the bad side of using… Or, you could just be like, ‘We're calling the police on you’”). For other participants, this message content elicited feeling of rebelliousness (e.g., “I'd probably be pretty defiant [if I received that type of message]”). Another common theme indicated a preference for messages that would support or enhance participants (e.g., “Something to boost your self-esteem on a daily basis,” “You can do it,” “You got this”). Others liked supportive reminders (e.g., “Sometimes, when I’m trying not to use it helps to remember that everything I do comes back to me and it’s all my responsibility, even if I don’t see it that way”). Additionally, there was discussion about the format and delivery method of the messages (e.g., “More exclamation points,” “It should be all caps. Blinking would be good,” “Emoji of a guy drinking,” “You could Snapchat something”) although no consensus could be reached (e.g., “It might be helpful. It might be distracting,” “It would probably make me want to get ****ed up”).
Additional participant feedback included a preference for messages being sent later on weekends than on weekdays (e.g., “If [the messages] wake me up on the weekend I’d kill you”). However, others didn’t mind receiving messages while they slept (e.g., “You get a notification when you turn on the phone [in the morning]”) and a few preferred to receive messages while they’re asleep so that “when I wake up I just get [the message].” Participants reported a wide range of preferences from quantity of messages received ranging from low (e.g., “One”) to high (e.g., “I want these every second of the day… all the time,” “A year would be cool”). They also indicated a preference for decreasing the amount of messages over time (e.g., “Probably [get tired of the messages] after a week or two weeks,” “I might get used to them”) but consensus was not reached with regard to an ideal amount.
Pilot intervention
Feasibility
Only a subset of individuals self-referring to be assessed for study eligibility responded to study screening prompts (62.8%; 115 individuals responded of 183 self-referring for screening). Ninety-three of 115 screened participants (80.9%) were determined to meet eligibility criteria (seven participants did not meet age criteria; 15 participants did not meet behavior change goal criteria). Of the eligible participants, 63% (59/93) enrolled in the larger study, falling below the a priori feasibility criteria of 80% or greater. With respect to retention of participants receiving substance use-related messages, 89.7% (35/39) of participants remained enrolled in the study as measured by completing at least one more assessment after baseline. This rate met the a priori cutoff for acceptable feasibility. The average number of assessments completed after baseline was 2.49 (maximum of 3). Additionally, 84.6% (33/39) of participants completed at least one of the post-treatment or follow-up assessments and 74.3% (29/39) of participants completed all assessments.
Acceptability
Participants responded to 14 yes/no questions assessing aspects of the messages that they liked and disliked. At post-treatment, participants selected on average 7.58 “likes” and 4.63 “dislikes”. At follow-up, participants selected on average 7.72 “likes” and 4.45 “dislikes”. The ratio of likes to dislikes indicated that participants were 1.68 times more likely to report a like than dislike.
In the post-treatment and follow-up surveys, participants were asked to reflect on the amount of messages received during the study. At post-treatment, 24.2% (8/33) of participants reported feeling they received “way too many messages,” 57.6% (19/33) of participants reported feeling they received “too many messages,” and 18.2% (6/33) of participants reported feeling they received the “right amount of messages.” At follow-up, 27.6% (8/29) of participants reported feeling they received “way too many messages,” 31% (9/29) of participants reported feeling they received “too many messages,” 34.5% (10/29) of participants reported feeling they received the “right amount of messages,” 6.9% (2/29) of participants reported feeling they received “way too few” messages.
Although all participants were informed that sending a “STOP” text message to the study would end study messages and withdraw participants from the study, none used the “STOP” message option to withdraw from the study.
Message frequency preference
The baseline, during, post-treatment, and follow-up surveys, assessed participant preference for message frequency (e.g., how many messages per day) and quantity (e.g., how many weeks of messaging). At baseline (56.4%; 22/39), during (29.4%; 10/34), and follow-up assessments (31%; 9/29), participants most commonly reported preferring to receive one message per day. At post-treatment, participants most commonly reported a preference to receive two messages per day (39.4%; 13/33). At baseline (34.2%; 13/38) participants most commonly reported preference to receive messages for four weeks. At during (20.6%; 7/34) and post-treatment (24.2%; 8/33) participants most commonly reported a tie in preference to receive messages for two and four weeks. At follow-up (24.1%; 7/29) participants most commonly selected two weeks.
Message content preference
At baseline, participants were asked to select 28 messages, from a list of 100 messages, that they would most like to receive. The most frequently selected message content category was supportive/empowering messages (M = 8.59, S.D. = 2.56) followed by commitment reminder messages (M = 7.90, S.D. = 2.26), educational messages (M = 6.10, S.D. = 2.20), and threatening/consequential messages (M = 5.41, S.D. = 2.78). The most frequently selected message (“Live smart. Think of the future”) was classified as an educational message (it was also the first message presented to participants). It was followed by a supportive/empowering message (“You are in control”). The most frequently selected commitment reminder message was a tie (“This decision is for a better life” and “It’s your decision. Today counts”) and they were the third most frequently selected, overall. The most frequently selected threatening/consequential message (“Choose your friends wisely”) was the 25th most frequently selected message overall.
At post-treatment, participants were asked to identify their three favorite messages received. The most frequently selected messages were supportive/empowering messages (M = 1.24, S.D. = 0.91) followed by commitment reminders (M = 0. 76, S.D. = 0.79), threatening/consequential messages (M = 0.62, S.D. = 0.78), and educational messages (M = 0.31, S.D. = 0.54). The complete message list is available in Appendix A.
Helpfulness of reminders
Mean scores of helpfulness of reminders and impact of message support over time are reported in Table 1. Mean scores indicated that reminder helpfulness and support ranged from moderate to moderately strong. Mean perceived helpfulness of reminders was significantly greater than mean perceived supportiveness of messages at post-treatment (t(32) = 3.44, p = 0.002) and follow-up (t(28) = 2.58, p = 0.015).
Table 1.
Helpfulness of reminder and impact of message support (N = 39).
|
Post-treatment |
Follow-up |
||||
|---|---|---|---|---|---|
| N | Mean | S.D. | N | Mean | S.D |
| How much did the messages help keep your decision in mind to not use drugs or to limit your use of drugs? | |||||
| 33 | 4.08 | 1.56 | 29 | 4.24 | 1.22 |
| How much did the messages help support you in not using drugs or using within your limits? | |||||
| 33 | 3.30 | 1.26 | 29 | 3.52 | 1.21 |
Open-ended questions
Participants were invited to answer open-ended questions at post-treatment and follow-up regarding their opinion about message content, message timing, and the study in general. Participant feedback regarding message content was positive, ranging from “It sometimes made me think more about the substance use than I would have” to “It made me keep my mind clear. If I was thinking about using I would go back and read those messages and it made me feel in control.” Participants expressed mixed opinions regarding message content with some favoring threatening messages (“I think the most effective ones are the ones that include stats about deaths or harm related to drugs or alcohol.”) and others preferring supportive messages (“Text messages that included positive vibes instead of the ones that were intimidating were more helpful.”).
Participants responded to open-ended questions assessing preferred times to receive SMS on weekdays and weekends. Weekday response included: time of day (e.g., nights), scheduled events (e.g., “frat parties”, “social events”, “hanging out with girlfriend”), and specific days/times (e.g., “Tuesday and Thursday at 9:30 PM”). Weekend response were similar with differences seen in the types of events reported: time of day (e.g., nights), scheduled events (e.g., “tailgates”, “parties”, “concerts”, “hanging out with friends”), specific days and times (e.g., “Friday and Saturday nights at 10 PM”), and mood-state (e.g., “boredom”).
Despite a relatively low response rate, open-ended responses regarding the study were primarily positive: “I think that maybe this study could be used for people trying to quit vaping as well. It will provide resolution for those people like me.”; “The study seems very interesting and that it could definitely prove to be a beneficial way to help others work on their goals for managing their use of alcohol/drugs. Text messages are definitely an effective way to get a message to someone and is a good way to remind people of their goals.” However, for some participants the messages may have been less relevant, “It is a good idea, I think other people would like it a lot. It seems to really care about the people who want to stop using. Since I do not have an issue the messages were slightly misguided for me. I do drink alcohol on the occasion, but its once or twice a month so nothing I need help for either. Thanks.” See Table 2 for all comments.
Table 2.
Participant response to open-ended question regarding opinion toward messages and study (N = 39).
| Text messages that included positive vibes instead of the ones that were intimidating were more helpful and the concept of the study was good. |
| This was my first psych study and I was very happy to be a part of it!* |
| Thank you for doing this! These texts acted as a subtle reminder and were very helpful. |
| I think that maybe this study could be used for people trying to quit vaping as well. It will provide resolution for those people like me. |
| Way too many messages that felt very robotic and not personal.** |
| It is a good idea, I think other people would like it a lot. It seems to really care about the people who want to stop using. Since I do not have an issue the messages were slightly misguided for me. I do drink alcohol on the occasion, but its once or twice a month so nothing I need help for either. Thanks. |
| In the end it helped me on my journey to getting sober.** |
| I think they should be concentrated around a timeline that people say they tend to use drugs. It’s annoying to get a text telling me to stay away from drugs or remember my goals while I’m in my 9:30am lectures. |
| Just more custom tailored to the person. Some of mine were kind of religious sounding and I am agnostic.* |
| It was an interesting experience that definitely made me think about my consumption of alcohol and drugs! |
| I think they help slightly but they’re only as good as someone wants them to be. It also depends on personality. |
| I think the most effective ones are the ones that include stats about deaths or harm related to drugs or alcohol.** |
| They seemed very corny. And it might have been better to not have us pick them because they get very redundant. |
| The study seems very interesting and that it could definitely prove to be a beneficial way to help others work on their goals for managing their use of alcohol/drugs. Text messages are definitely an effective way to get a message to someone and is a good way to remind people of their goals. |
*Edited for grammar.
**Edited for punctuation.
Discussion
This pilot study aimed to determine the acceptability and feasibility of an SMS adjunct to SUD treatment. Focus group feedback informed the final message content and study design. Feedback supported offering threatening messages, with the understanding that they likely would be preferred by a minority of participants. There also was interest in receiving supportive/empowering messages as well as commitment reminder messages. Exclamation points were incorporated into some of the messages and messages were tapered over time as a result of feedback. Additionally, suggestions to modify message timing (e.g., different weekday and weekend delivery times) to better suit adolescent and young adult life were incorporated into study design. The results of the pilot study suggest that an SMS adjunct to substance use intervention is acceptable to adolescents and young adults while feasibility had mixed results. While participant recruitment fell below the a priori cutoff, the relatively low dropout rate suggests that participants were willing to continue to engage with the study. Additionally, participants generally found the intervention to be acceptable, as indicated by open-ended question feedback and the ratio of message likes and dislikes.
Greater average selection of SMS likes than dislikes suggest the messages were satisfactory and helpful for participants. Most responses to open-ended questions were positive and some participants specifically stated that they felt the messages helped them change their substance use. Additionally, it is notable that despite being informed of the “STOP” message option, no participant chose to withdraw from the study in this way. The research team chose to pre-populate participant contact information into the SMS programming. The rationale behind this decision was to attempt to remove or decrease any additional participant burden to receiving intervention content. The apparent acceptability of this approach bodes well and this strategy may be effective for other studies to implement as a means to increase rates of participant engagement with mHealth interventions.
Low smartphone application (app) download rates are reported as a common barrier to participant engagement with mHealth interventions. Possible explanations for this include lack of motivation, knowledge (e.g., not knowing how to download the application), or ability (e.g., not having a smartphone) to interact with the technology.54–56 In the current study, there are several potential explanations for low recruitment rates including, difficulty in recruiting participants throughout the country via phone and email, the study may have been perceived as being too much of a burden or time-commitment (estimated maximum of 90 minutes to complete all surveys), and insufficient recruitment efforts (maximum of seven contacts per participant).
Participants reported a preference to receive a lesser “dose” (i.e., daily SMS frequency and length of SMS intervention) of SMS than they received in the pilot study, similar to previous findings regarding decreasing SMS.48 The results suggest limiting the amount of contact per day and providing support for a brief period of time is preferred by most. However, a minority of participants indicated a preference for a substantially longer period of support. There also were specific times of day and event-specific preference for receiving messages. This supports the importance of tailoring the dose of interventions when possible and underscores the importance of continued research on interventions for high-risk event-specific substance use, such as spring break and 21st birthdays.57–59 When considering these results, it is important to note that a majority of participants were young adults mandated to an Alcohol Skills Training Workshop and these responses may not be representative of individuals with a severe SUD.
At baseline, the most “popular” (i.e., frequently selected) message category were supportive/empowering messages while the least popular messages were threatening/consequential. At post-treatment, the most popular message category remained the same while the least popular messages were educational. It is unclear whether individuals can accurately identify and select the messages that will be most effective in supporting substance use behavior change, and it is likely this ability varies between individuals. However, in terms of message preference it appears that supportive/empowering messages are the most popular. The threatening/consequential message popularity results appear similar to the findings from the focus group, appreciated by some and disliked by others. This may suggest that there may be a class of individuals who believe that threatening messages would help them engage in substance use behavior change.
Limitations
There were several limitations to this pilot study. First, the focus groups were conducted only with adolescents (ages 13-17) and the pilot study included adolescents and young adults. It is possible that other themes and message preferences would have been discovered with a more representative sample of focus group participants. Second, while participants were asked to respond to daily messages as a method of ascertaining whether or not they were receiving and reading the messages, it is impossible to know if participants were actually reading the messages or not. Third, the order in which messages were presented at baseline for selection by participants was randomized and presented the same way for all participants. The first visible message (e.g., in the top left of the screen) was the most frequently selected. It is possible that this was the most popular message due to its content, however, it was not nearly as popular when re-assessed at post-treatment. Continual re-randomization of the message list may have revealed a difference distribution of message preference at baseline. Fourth, the study was static and unable to modify or tailor the SMS dose or content to participant preference. Participants were sent each message three times and it is possible that participants experienced decreased attention due to lack of novelty. Fifth, there was a relatively low response rate to open-ended questions which makes interpretation challenging. Lastly, a majority of participants were young adults mandated to a brief motivational intervention and their results are likely not generalizable to individuals with a severe SUD.
Conclusion
Despite study limitations, the largely positive feedback to this pilot intervention provides encouragement for expanding and testing the use of SMS as an adjunct to substance use intervention. This study demonstrates the acceptability of an SMS adjunct to substance use intervention and offers insights to potential solutions to improve mHealth intervention recruitment. Additionally, the study highlights the importance of tailoring SMS dosing, content, and timing for message recipients, when possible. It suggests that different types of substance use-related content may be preferred by some participants and not others. Specifically, it appears that threatening/consequential message content may be well received by some participants and disliked by others; while supportive/empowering message content appears to be preferred be a larger amount of individuals. Finally, it is important to consider the amount and length of time SMS are being sent to participants. It appears that for this population, sending relatively few messages for a brief period of time is preferable to many messages for longer periods of time.
Supplemental Material
Supplemental material, sj-pdf-1-dhj-10.1177_2055207620965052 for Text message reminders as an adjunct to a substance use intervention for adolescents and young adults: Pilot feasibility and acceptability findings by Frank J Schwebel and Mary E Larimer in Digital Health
Acknowledgements
FS would like to thank his graduate advisor (Dr. Mary Larimer) as well as the other members of his dissertation committee (Drs. Ron Smith, William George, and Sean Munson) for their invaluable guidance over the course of the project.
Contributorship
FS and ML conceived the study. FS developed the protocol, gained ethical approval, recruited participants, completed data analysis, and wrote the first draft of the manuscript. ML provided substantial assistance in editing and preparing the manuscript for submission. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
The University of Washington Institutional Review Board approved this study (00001405).
Funding
This work was supported by the Alcohol and Drug Abuse Institute (ADAI 0314-5) and the National Institute on Alcohol Abuse and Alcoholism (F31 AA025531, T32 AA018108).
Guarantor
FS.
Peer review
Dr Slawa Rokicki, Harvard University, has reviewed this manuscript.
ORCID iD
Frank J Schwebel https://orcid.org/0000-0002-9668-5707
Supplemental material
Supplemental material for this article is available online.
References
- 1.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2017 national survey on drug use and health SMA 18-5068, NSDUH Series H-53, Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2018.
- 2.Casey BJ, Jones RM. Neurobiology of the adolescent brain and behavior: implications for substance use disorders. J Am Acad Child Adolesc Psychiatry 2010; 49: 1189–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lenz B. The transition from adolescence to young adulthood: a theoretical perspective. J Sch Nurs 2001; 17: 300–306. [DOI] [PubMed] [Google Scholar]
- 4.Schulenberg JE, Maggs JL. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. J Stud Alcohol Suppl 2002; 14: 54–70. [DOI] [PubMed] [Google Scholar]
- 5.Winters KC, Arria A. Adolescent brain development and drugs. Prev Res 2011; 18: 21–24. [PMC free article] [PubMed] [Google Scholar]
- 6.Arain M, Haque M, Johal L, et al. Maturation of the adolescent brain. Neuropsychiatr Dis Treat 2013; 9: 449–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allen CD, Rivier CL, Lee SY. Adolescent alcohol exposure alters the Central brain circuits known to regulate the stress response. Neuroscience 2011; 182: 162–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lubman DI, Yücel M, Hall WD. Substance use and the adolescent brain: a toxic combination? J Psychopharmacol (Oxford) 2007; 21: 792–794. [DOI] [PubMed] [Google Scholar]
- 9.Marshall EJ. Adolescent alcohol use: Risks and consequences. Alcohol Alcohol 2014; 49: 160–164. [DOI] [PubMed] [Google Scholar]
- 10.Milich R, Lynam D, Zimmerman R, et al. Differences in young adult psychopathology among drug abstainers, experimenters, and frequent users. J Subst Abuse 2000; 11: 69–88. [DOI] [PubMed] [Google Scholar]
- 11.National Research Council and Institute of Medicine. Reducing underage drinking: a collective responsibility. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- 12.Schwebel FJ, Whiteside U, Bittinger JN, et al. College student drinking In: Miller SC, Fiellin DA, Rosenthal RR, et al. (eds) The ASAM principles of addiction medicine. Baltimore, MD: Wolters Kluwer, 2019, pp. 580–593. [Google Scholar]
- 13.Johnston LD, O’Malley PM, Miech RA, et al. Monitoring the future national survey results on drug use, 1975-2016: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research: The University of Michigan, 2017. [Google Scholar]
- 14.National Institute on Drug Abuse. Principles of adolescent substance use disorder treatment: a research-based guide. USA: National Institute on Drug Abuse.
- 15.Poudel A, Gautam S. Age of onset of substance use and psychosocial problems among individuals with substance use disorders. BMC Psychiatry 2017; 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Richmond-Rakerd LS, Slutske WS, Wood PK. Age of initiation and substance use progression: a multivariate latent growth analysis. Psychol Addict Behav 2017; 31: 664–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dimeff LA, Baer JS, Kivlahan DR, et al. Brief alcohol screening and intervention for college students (BASICS): a harm reduction approach. New York: Guilford Press, 1999. [Google Scholar]
- 18.Marlatt GA, Baer JS, Kivlahan DR, et al. Screening and brief intervention for high-risk college student drinkers: results from a 2-year follow-up assessment. J Consult Clin Psychol 1998; 66: 604–615. [DOI] [PubMed] [Google Scholar]
- 19.Monti PM, Colby SM and, O’Leary TA. (eds). Adolescents, alcohol, and substance abuse: reaching teens through brief interventions. New York: Guilford Press, 2001. [Google Scholar]
- 20.Breslin FC, Zack M, McMain S. An information-processing analysis of mindfulness: implications for relapse prevention in the treatment of substance abuse. Clin Psychol Sci Pract 2006; 9: 275–299. [Google Scholar]
- 21.Dennis M, Scott CK. Managing addiction as a chronic condition. Addict Sci Clin Pract 2007; 4: 45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McLellan AT, Lewis DC, O’Brien CP, et al. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA 2000; 284: 1689–1695. [DOI] [PubMed] [Google Scholar]
- 23.National Institute on Drug Abuse. Principles of drug addiction treatment: a research based guide. 3rd ed Rockville, MD: National Institute on Drug Abuse, 2018. [Google Scholar]
- 24.Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was zen, this is tao. Am Psychol 2004; 59: 224–235. [DOI] [PubMed] [Google Scholar]
- 25.A da M, Gonçalves FL, Bizarro L. Delay discounting: concepts and measures. Psychol Neurosci 2012; 5: 135–146. [Google Scholar]
- 26.Bickel WK, Marsch LA. Toward a behavioral economic understanding of drug dependence: delay discounting processes. Addiction 2001; 96: 73–86. [DOI] [PubMed] [Google Scholar]
- 27.Amlung M, Vedelago L, Acker J, et al. Steep delay discounting and addictive behavior: a meta-analysis of continuous associations: delay discounting and addiction. Addiction 2017; 112: 51–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sheffer CE, Christensen DR, Landes R, et al. Delay discounting rates: a strong prognostic indicator of smoking relapse. Addict Behav 2014; 39: 1682–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stanger C, Ryan SR, Fu H, et al. Delay discounting predicts adolescent substance abuse treatment outcome. Exp Clin Psychopharmacol 2012; 20: 205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steinberg L, Graham S, O′Brien L, et al. Age differences in future orientation and delay discounting. Child Dev 2009; 80: 28–44. [DOI] [PubMed] [Google Scholar]
- 31.Squeglia LM, Jacobus J, Tapert SF. The influence of substance use on adolescent brain development. Clin EEG Neurosci 2009; 40: 31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brewer GA, Marsh RL, Clark-Foos A, et al. A comparison of activity-based to event-based prospective memory. Appl Cognit Psychol 2011; 25: 632–640. [Google Scholar]
- 33.Guynn MJ, McDaniel MA, Einstein GO. Prospective memory: when reminders fail. Mem Cognit 1998; 26: 287–298. [DOI] [PubMed] [Google Scholar]
- 34.Rummel J, Wesslein A-K, Meiser T. The role of action coordination for prospective memory: task-interruption demands affect intention realization. J Exp Psychol Learn Mem Cogn 2017; 43: 717–735. [DOI] [PubMed] [Google Scholar]
- 35.Schaper P, Grundgeiger T. The effect of different distractions on remembering delayed intentions. Memory 2018; 26: 154–170. [DOI] [PubMed] [Google Scholar]
- 36.Insel KC, Einstein GO, Morrow DG, et al. Multifaceted prospective memory intervention to improve medication adherence. J Am Geriatr Soc 2016; 64: 561–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Y, Pérez-Quiñones MA. Exploring the role of prospective memory in location-based reminders. In: Proceedings of the 2014 ACM international joint conference on pervasive and ubiquitous computing adjunct publication – UbiComp’14 Adjunct, 2014, pp. 1373–1380. Seattle, Washington: ACM Press.
- 38.Fry JP, Neff RA. Periodic prompts and reminders in health promotion and health behavior interventions: systematic review. J Med Internet Res 2009; 11: e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schwebel FJ, Larimer ME. Using text message reminders in health care services: a narrative literature review. Internet Interv 2018; 13: 82–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pew Research Center. Mobile Fact Sheet. https://www.pewresearch.org/internet/fact-sheet/mobile/ (2019, accessed 30 September 2020).
- 41.Nelson TD, Nelson JM. Evidence-based practice and the culture of adolescence. Prof Psychol Res Pract 2010; 41: 305–311. [Google Scholar]
- 42.Menin J. New York city mobile services study. Research Brief, Department of Consumer Affairs, New York City, 2015.
- 43.Cocotas A. Chart of the day: kids send a mind boggling number of texts every month. Business Insider Incorporated, www.businessinsider.com/chart-of-the-day-number-of-texts-sent-2013-3 (2013, accessed 29 September 2020).
- 44.Madden M, Lenhart A, Duggan M, et al. Teens and technology 2013. Youth Today, http://mqil.youthtoday.org/hotdocs/PIP_TeensandTechnology2013.pdf
- 45.The Nielsen Company. U.S. teen mobile report calling yesterday, texting today, using apps tomorrow. The Nielsen Company, www.nielsen.com/us/en/insights/news/2010/u-s-teen-mobile-report-calling-yesterday-texting-today-using-apps-tomorrow.html (2010, accessed 29 September 2020).
- 46.Berrouiguet S, Baca-García E, Brandt S, et al. Fundamentals for future Mobile-Health (mHealth): a systematic review of mobile phone and web-based text messaging in mental health. J Med Internet Res 2016; 18: e135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Free C, Phillips G, Felix L, et al. The effectiveness of M-health technologies for improving health and health services: a systematic review protocol. BMC Res Notes 2010; 3: 250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Head KJ, Noar SM, Iannarino NT, et al. Efficacy of text messaging-based interventions for health promotion: a meta-analysis. Soc Sci Med 2013; 97: 41–48. [DOI] [PubMed] [Google Scholar]
- 49.Marsch LA, Carroll KM, Kiluk BD. Technology-based interventions for the treatment and recovery management of substance use disorders: a JSAT special issue. J Subst Abuse Treat 2014; 46: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aguilera A, Bruehlman-Senecal E, Demasi O, et al. Automated text messaging as an adjunct to cognitive behavioral therapy for depression: a clinical trial. J Med Internet Res 2017; 19: e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Marlatt GA, Witkiewitz K. Harm reduction approaches to alcohol use: health promotion, prevention, and treatment. Addict Behav 2002; 20: 867–886. [DOI] [PubMed] [Google Scholar]
- 52.Miller WR. Motivational interviewing with problem drinkers. Behav Psychother 1983; 11: 147–172. [Google Scholar]
- 53.Neal JW, Neal ZP, VanDyke E, et al. Expediting the analysis of qualitative data in evaluation: a procedure for the rapid identification of themes from audio recordings (RITA). Am J Eval 2015; 36: 118–132. [Google Scholar]
- 54.Ramsey A, Lord S, Torrey J, et al. Paving the way to successful implementation: identifying key barriers to use of technology-based therapeutic tools for behavioral health care. J Behav Health Serv Res 2016; 43: 54–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bucci S, Schwannauer M, Berry N. The digital revolution and its impact on mental health care. Psychol Psychother 2019; 92: 277–297. [DOI] [PubMed] [Google Scholar]
- 56.Lord S, Moore SK, Ramsey A, et al. Implementation of a substance use recovery support mobile phone app in community settings: qualitative study of clinician and staff perspectives of facilitators and barriers. JMIR Ment Health 2016; 3: e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Geisner IM, Rhew IC, Ramirez JJ, et al. Not all drinking events are the same: exploring 21st birthday and typical alcohol expectancies as a risk factor for high-risk drinking and alcohol problems. Addict Behav 2017; 70: 97–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Patrick ME, Lee CM, Neighbors C. Web-based intervention to change perceived norms of college student alcohol use and sexual behavior on spring break. Addict Behav 2014; 39: 600–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pedersen ER, Neighbors C, Atkins DC, et al. Brief online interventions targeting risk and protective factors for increased and problematic alcohol use among American college students studying abroad. Psychol Addict Behav 2017; 31: 220–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-dhj-10.1177_2055207620965052 for Text message reminders as an adjunct to a substance use intervention for adolescents and young adults: Pilot feasibility and acceptability findings by Frank J Schwebel and Mary E Larimer in Digital Health