Abstract
Diabetic foot ulcer (DFU) is currently a global concern and it requires urgent attention, as the cost allocation by the government for DFU increases every year. This review was performed to provide scientific evidence on the advanced biomaterials that can be utilised as a first-line treatment for DFU patients. Cellulose/collagen dressings have a biological property on non-healing wounds, such as DFU. This review aims to analyse scientific-based evidence of cellulose/collagen dressing for DFU. It has been proven that the healing rate of cellulose/collagen dressing for DFU patients demonstrated a significant improvement in wound closure as compared to current standard or conventional dressings. It has been scientifically proven that cellulose/collagen dressing provides a positive effect on non-healing DFU. There is a high tendency for cellulose/collagen dressing to be used, as it highly promotes angiogenesis with a rapid re-epithelisation rate that has been proven effective in clinical trials.
Keywords: dressing, cellulose, collagen, diabetic foot ulcer, wound closure, rapid healing
1. Introduction
1.1. Diabetic Foot Ulcer
Diabetic Foot Ulcer (DFU) is a chronic condition that resulted from uncontrolled diabetes that leads to peripheral artery disease or neuropathy. A single or combination of both abnormalities will trigger the development of DFU. DFU usually leads to progressive bone, joint, and soft tissue deterioration with commonly seen in the ankle and foot [1], causing severe complications that inflict more than 50% of amputations in diabetic patients. This is mainly caused by impaired wound healing due to the thickening of the basement membrane, foreign body infection, low proliferation rate, irregular keratinocyte differentiation, and slow angiogenesis that perpetuates the foot deformity. In this case, amputation and surgical debridement is the only available treatment to prevent further systemic spread of infection [2,3]. Meanwhile, DFU has been categorised as a significant mortality determinant in a study that revealed half of the subjects who developed DFU tend to die within five years [4]. The global prevalence rate of DFU has been estimated to be around 6.3% and Asia recorded around 5.5%. There is a high possibility for amputation within the first year of infection, which is around 34.1% with a mortality rate of 5.5% [5]. Figure 1 shows the condition of DFU.
Figure 1.
Diabetic Foot ulcer. Figure reused from Netten and co-workers [24]. Used under the creative. Commons license http://creativecommons.org/licenses/by/4.0/.
1.2. Diabetic Foot Ulcer Scenario in Malaysia
Malayjsia has been ranked as the highest diabetes cases recorded in Asia and it is one of the highest in the world [6], with around 3.6 million patients [7]. By 2025, it is expected that around seven million adults will suffer from diabetes and potentially to develop DFU. The prevalence rate was identified to be approximately 31.3% for adults above 18 years old [7]. According to the wound care unit at Hospital Kuala Lumpur (HKL), 70% of the patients are diabetic patients who are suffering from foot ulcers and more than 12,000 patients have visited the wound care unit since 2013. Diabetic patients may take up to three months to completely heal with proper care and this is four times higher when compared to the normal healing rate [8]. According to the data that were collected from the general hospitals in Malaysia (2009), there is a notable increase in patients with foot complications from 1549 subjects screened for diabetics. From this, 5% demonstrated an absence of foot pulse, 3.9% with a healed ulcer, 3.8% patients with leg amputations, 2% subjects who undergone angioplasty or vascular surgery, while 1.5% with an active ulcer or gangrene. The majority of about 27% patients have been confirmed with foot infection, while the remaining patients have been diagnosed with infection at various sites in the body, particularly in the urinary tract, skin, respiratory tract, and eye [9].
1.3. Socioeconomic Burden
Globally, it is estimated that £252 million was allocated for DFU treatment annually. This excludes the indirect cost due to the loss of productivity, quality of life, and family status. The total expenditure for the management of diabetic foot ulcer ranged from US$9 billion to US$13 billion in a year. A minor limb amputation costs around US$43,800, whereas a major amputation can cost up to US$66,215. This cost excludes rehabilitation care and medications [10]. In Malaysia, 13% of the total healthcare budget has been allocated for the management of diabetic patients in 2011, including societal expenditure, which can reach up to MYR3.52 billion per year [7]. In 2014, the Malaysian government allocated approximately MYR30 billion (USD6.8 billion) for the clinical sector in which diabetic foot infection remains a major burden [11].
1.4. Current Treatment for Diabetic Foot Ulcer
Total contact cast (TCC) is an offloading device providing mechanical support in treating DFU patients and it is currently the gold standard treatment [12,13]. It acts by redistributing the pressure in the plantar surface to the body mass as well as maintaining the subject’s mobility, which prevents the breakdown of new skin [14]. TCC is also known to be an affordable ambulatory technique [15] to assist many diabetic patients. Although the use of TCC provides several benefits, it leads to immobilisation and user’s safety is a major concern, as it requires skillful clinicians to apply it efficiently. Nevertheless, there is a notable difficulty when inspecting the wounds due to the distinctive obstacles faced during removing the attached device [12,13].
Other treatments, such as negative pressure wound therapy (NPWT), dermapace system (DS), and maggot debridement therapy (MDT), are the currently available treatments that have been used widely to treat DFU patients. NPWT is an existing modality to draw out the exudates from the ulcerated area through a pressure produced by a vacuum [16,17]. Upon extracting the excess fluid, this device creates a moisture microenvironment triggering the blood flow to the ulcerated region by removing wound healing inhibitors. This situation stimulates the formation of granulation tissue that induces stress at the wound bed and directly elevated the proliferation of the cell. This process contributes to wound healing [17,18].
DS utilises shock wave energy that resembles sound waves to the surface of the wound, which triggers the body’s wound healing pathway [19,20]. This device accelerates the process of angiogenesis that increases the production of growth factor (GF). Meanwhile, the transmitted wave assists in reducing inflammation that exists in the wound bed as well as to the tissues surrounding the wound. The application of this device to DFU resulted in notable wound closure [21]. MDT is also one of the current treatment options available for treating DFU. This therapy works by removing dead tissues that are present in the wound area using larva [20,22,23]. In this procedure, artificial and sterile grown larvae known as Phaenicia sericata/Lucilia sericata will be applied to the wound area to disinfect the wound region [22,24]. The larvae will remove the dead-tissue and release proteolytic enzyme to the wound region, which will then lyse the non-viable tissues in the ulcerated region contributing to the process of wound closure [25].
1.5. Contraindication and Complications of Current Available Treatment
Few issues need to be taken into consideration when using TCC. It is not advisable to apply TCC in patients with osteomyelitis, deep abscess, or gangrene. Extra care is also needed when applying TCC in unsteady gait patients. In certain case, there is a high possibility of skin breakage at the surrounding area of the existing ulcer if TCC is applied for a long period or have a sensitive skin [14]. Although, over time, the ulcers tend to have an improvement with TCC, it still takes over a year to completely heal especially for a chronic ulcer. This is because chronic ulcer requires frequent dressing of at least every two weeks. It could contribute to the high cost and affects the socioeconomic background of the patients [13,14,26,27]. Nevertheless, there are high risks of hazards for TCC applications, including gait instability, iatrogenic ulcers due to the discrepancy in the length of the limbs, falls [26], stiffness of the joints, atrophy of the muscle, and new ulcer formation [15]. The use of TCC is a “force compliance” making the patients less active compared to other available off-loading devices. This results in reduced vertical force in the foot, which may lead to posture instability. TCC application could result in iatrogenic infection or skin abrasion and the application of this cast for a long duration will result in muscle atrophy and deterioration in the density of the bone [27].
The application of NPWT in DFU patients for a long period with lack of proper care, such as fixing it too tight, might result in other complications. A recent retrospective case study, including 57 DFU patients treated with NPWT complications showed 49% of the patients developed maceration of skin at the borders of the wound, 14% of bleeding, 12% of necrosis at the wound area, 7% of developed systemic signs or infection, while 2% with severe pain during changing the dressing [28]. This therapy has been known as an expensive treatment as compared to the currently available conventional DFU treatment [29].
In contrast, even though DS provides several benefits, the disadvantage of this device outweighs its advantages. The advantages include the loss of sensation, local bruising, dizziness, nausea, infection in the wound site or beyond the wound, fever [19,20], and migraine [19]. The utilisation of MDT for DFU seems to be less effective, as it does not reduce the load of bacteria or improving the wound healing rate but only reduce the duration to debride the ulcerated region. At the same time, this therapy does induce anxiety among the patients as well as lead to the formation of erythema due to the digestive enzyme that is released by the maggots during the therapy session [30,31]. Figure 2 shows the current available treatment for DFU.
Figure 2.
Current available treatment for Diabetic Foot Ulcer (DFU) [32]. Used under the attributions of creative. Commons license http://creativecommons.org/licenses/by/4.0/.
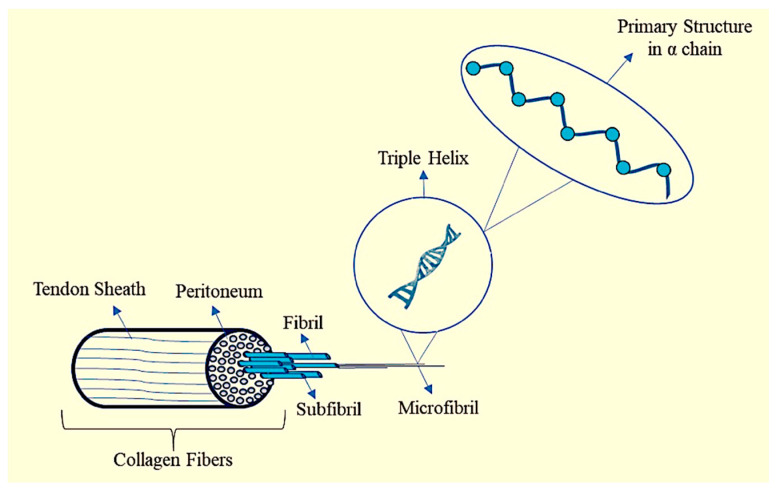
2. Collagen
Collagen is a natural fibrous protein in the body that makes up the connective tissues [33,34] in various sites. There about 28 different types of collagen that have been further classified according to their distribution and structure [35]. Collagen is a biocompatible structural protein, less immunogenicity, biodegradable, and biomimetic, which makes it an ideal source of biological materials for tissue engineering and regenerative medicine. The composition and functionality of the collagen fibres influence the cellular response that is commonly regulated by integrin. This phenomenon is achieved by a biological process that is known as fibrillogenesis [36]. Fibrillogenesis is a process of collagen network formation and interaction within the cellular level to form higher-order three-dimensional structure. Usually, these fibres are stabilised through a cross-linking intervention after a collagen scaffold formation to sustain its bioactivity and bioavailability [37,38]. By modifying each phase of fabrication based on the specific need of the tissues, bioscaffolds can be customised in order to improve its therapeutic effects [39]. Meanwhile, cross-linking can be achieved through a synthetic or natural polymer [40]. Genipin, oxidised alginate, dialdehyde starch, and procyanidin are natural-based crosslinkers [41], whereas synthetic crosslinker includes actin [42], polylactic acid, poly ahydroxyesters, and polyl glycolic acid [43]. Generally, crosslink molecules are equipped with two or more reactive ends that have the capacity to bind with the triple helix structure of the collagen. The crosslink can either appear inside or between the microfibre of the collagen. The microfibrils interdigitate and cross-link, thereby intactly avoiding detachment from one another [44]. Collagen can be extracted through chemical or enzymatic hydrolysis approaches. The extraction process was initiated with the removal of the inter- and intra-molecular bond. It was first pre-treated with alkaline (NaOH) or acid solution to expel non-collagenous substances. In chemical-based extraction of collagen, the pre-treated material commonly will be added with an acid-based solvent, such as 0.5 M of acetic acid, and stored up to 72 h. The precipitation step with salt (NaCI) solution until the supernatant becomes visible is crucial to allow the protein to bind prior to dialyse for two days with distilled water (constantly changed every 12 h). Otherwise, 0.5 M of acetic acid will be combined with enzymes, such as flavourzyme, alcalase, or pepsin, in the enzymatic collagen extraction. The solution will be continuously stirred at 4 °C up to 48 h, followed by filtration and dialysed for two days with distilled water to obtain the purified collagen [45]. Although chemical extraction is efficient [45], it is highly corrosive [46]. Meanwhile, enzymatic extraction of collagen requires a long duration to complete and it has a high possibility to contain incomplete hydrolysis process [46]; however, this method produces fewer waste products [45]. Figure 3 shows the structure of collagen.
Figure 3.
Structure of collagen.
3. Collagen-Based Treatment for DFU
Diabetes mellitus (DM) is one of the major concerns worldwide with DFU and is the most common complication of DM. A variety of advanced technology has been widely invented to cater this critical issue, especially collagen, which is known to be used the most. Collagen type I (Col-I) is deem required to attract GFs towards the wound site and to initiate wound healing and tissue regeneration. However, in the DFU case, the epidermis is ulcerated, leading to the disruption of the extracellular matrix contributing to tissue integrity loss resulting in Col-I deficiency. Besides that, it hinders the normal proliferation and migration of fibroblasts to the wound area and eventually slows down the wound healing [47]. Scientifically, it was proven that collagen accelerates wound healing and enhances re-epithelisation [48,49]. A study that was conducted by Ulrich and co-workers (2011) [43] recorded 32 DFU outpatients were successfully managed with oxidised regenerated cellulose (ORC) or collagen matrix. These patients who underwent this intervention show inhibition of protease, plasmin, and elastase, the most common causes of wound healing interruption. The excess level of elastase will interfere with the mechanism of normal collagen production, whereas plasmin has a significant role in hemolysis. These proteins (protease, plasmin, and elastase) distinctively act to degrade the fibronectin, endogenous protease inhibitors, and GF that are the essential elements in the wound healing process. In contrast, the intervention with ORC or collagen matrix at the specified wound region demonstrated an acceleration in ulcer healing on the 28th day as well as providing an optimum microenvironment for wound healing [48].
Meanwhile, a pilot study was performed on 22 patients with neuropathic DFU in order to evaluate the efficacy of wound dressing in wound closure with the intervention of equine pericardium collagen dressing. The dressing was consecutively changed every three to four days and in the fourth week, 94% of the patients showed a notable improvement in the wound region with 13% of complete heal, and both described a significant reduction in the ulcerated region (p < 0.0001). These findings indicated that collagen-derived dressing is safe and effective in accelerating ulcers healing [50]. A similar study was done on 124 chronic neuropathic DFU patients with formulated collagen gel (FCG), which comprise 2.6% of bovine collagen and adenovirus serotype 5 (Ad5). Upon implanting FCG at the wound site, 35% of ulcer closure has been identified on the 12th week. It showed that FCG enhances the expression of PDGF in order to accelerate wound healing. The presence of collagen in this product was proven to create a compatible and stable microenvironment at the injury site. This phenomenon was undertaken by holding the Ad5 at the ulcerated region by promoting the attraction via electrostatic force for GF to bind and encourage the formation of granulation tissue [51].
Furthermore, a comparative case-control study that was performed by Munish and co-workers (2015) described a significantly enhanced ulcer healing after being treated with collagen-based dressing [47]. The effectiveness of the treatment was evaluated through a study that was conducted on 25 patients with chronic DFU. The weekly assessment of the wound region was successfully performed from the first week of treatment until the 12th week. The 1st week of assessment identified two subjects that were completely healed and 12 subjects that showed a significant reduction in the size of the ulcer. Furthermore, the 12th week assessment showed 21 patients with completely healed and four patients with ulcer reduction. The enhancement of stimulation and differentiation of erythroid, granulocytes, and megakaryocyte precursor cells confirmed to increase defence mechanism. Because collagen biomaterial is slowly biodegraded; thus, it can act as a provisional bio-template for cell attachment, migration, and proliferation, as well as rapid wound maturation [52,53].
In contrast, the application of collagen powders to the ulcerated area create a more active site that allowed the fibronectin-binding as well as showing an increased in fibroblasts viability that plays the main role to accelerate wound healing [47]. Sprinkling collagen particles to the ulcerated region has been proven to decrease wound area with an absence of allergic response [53] and potentially to promote faster wound closure [54]. This is possible due to the ability of the collagen to retain its triple helix structure that preserved the thermal stability, mechanical strength, and functionality. This powdered collagen enhanced biomolecules interaction and the formation of a better three-dimension bio-scaffolding for cell migration prior to granulation tissue formation [46]. Additionally, it helps to hinder protease activity without affecting the performance and behaviour of GF [55]. On top of that, collagen can shrink the thickness of the scar, as it can regulate the collagenase activity and decomposition of the extracellular matrix through keratinocyte differentiation. Hence, collagen is assumed to be responsible for the scar size reduction as well as shorten the period of re-epithelisation [56].
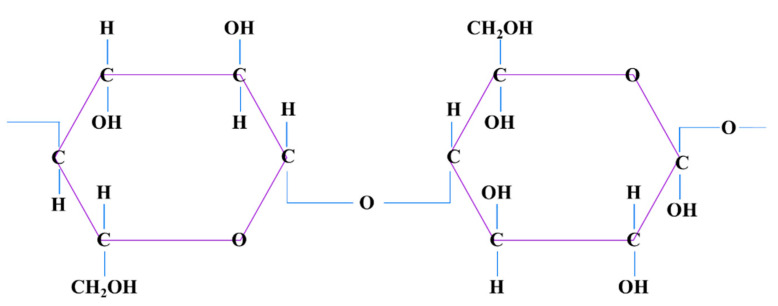
4. Cellulose
Generally, cellulose is well known for its abundance of availability from plant sources. Cellulose is known to poses a strong intermolecular bond, which makes it impossible to dissolve in most of the solvents. Meanwhile, in a liquid state, cellulose exhibits great stability, optical, and mechanical characteristics [32,33], and, due to its ability to retain moisture, it can expedite the wound healing mechanism [34]. Generally, cellulose can be classified into natural and synthetic. Natural cellulose is derived from vascular plants, animals, or minerals. Synthetic cellulose is man-made modified cellulose from natural cellulose source [57,58]. Natural and synthetic cellulose are both bound together by intra- and inter-hydrogen bonds. Plant cellulose usually contains impurities such as lignin and hemicellulose whereas bacterial cellulose appears pure by nature. This makes the plant cellulose possess less crystalline property when compared to the bacterial cellulose [59]. Figure 4 shows the structure of cellulose.
Figure 4.
Cellulose structure.
5. Cellulose as a Protective Barrier
Cellulose can provide front-line protection against foreign material, including all types of cellulose derivatives. The bacterial cellulose (BC) is originated from a membrane of biosynthetic microfibrillar cellulose formed by Acetobacter Xylinum or other types of selected bacteria [60]. The bacteria are a non-harmful pathogen that possess the ability to provide a moisture surface to improve the debridement process and to expedite the re-epithelisation in chronic ulcers. In a wet state, the membrane of the cellulose has 84–89% crystallinity property, mechanical strength, and the capability to absorb water [61,62], which gives the capacity to shorten the duration of healing phases [61]. Besides that, BC has been scientifically proven to be biocompatible, biodegradable, non-toxic, and exceptionally pure that chemically resemble cellulose-derived from plants. Thus, BC has shown the intrinsic features that are suitable for a bio-scaffold as a protective barrier for skin injury in various form such as wound dressing [37].
Nevertheless, exudates may slow down the process of healing as it makes the tissue to separate from the wound region. When considering this, any wound dressing must be designed to reach the ability to absorb, retain and release liquid to achieve an optimum balance of wound healing microenvironment. Thus, BC stands as a defence mechanism through the pore size surface area and the presence of hydrophilic compounds that supports the water holding and release capability as well as assists in the elimination of exudates from the wound site [37]. An in vitro study that was conducted by Loh et al., (2018) showed that BC-incorporated hydrogel can maintain the viability of the cell and promote cell attachment [63,64]. This is due to the BC property, which forms a tight barrier between the environment and the wound. This serves as a protective compound against bacterial infection that will accelerate wound healing rate as compared to the negative control in an in vitro study [65]. The application of bacterial cellulose also showed a 75% reduction in the wound region in a non-healing lower extremity ulcer [66].
A recent study conducted by Pinho and co-workers (2018) presented that cotton cellulose functionalised with hydrogels can function as a carrier to deliver drugs through the hydrogel. This framework allows for the bioactive chemicals, painkillers, antibiotics, and other therapeutic substances to be transferred to the wound area. When this happens, the trapped molecules migrate from the polymeric network to the wound bed through a sustained release cycle [67]. This is done by switching the position with the exudate, thereby eliminating the exudates from the wounded site. This, in turn, serves as a physical shield against microorganisms being deposited and proliferated on the wound surface [68].
Seratica and co-workers (2010) stated that, with the presence of a unique characteristic of cellulose, partial-thickness wound healed better with MC dressing. A 100% healing rate on the fifth day in an in vivo model has been reported. Clinical testing involving 13 subjects showed a complete heal from a venous ulcer on the eighth week upon applying cellulose-based wound dressing [55]. This was made possible as MC possesses a greater impact with a greater tensile strength, crystallinity, and water absorption capacity compared to the plant cellulose. Plant cellulose provides a semi-permeable membrane at the wound region to improve angiogenesis and fibrinolysis [68,69].
In addition, a study showed a complete ulcer healing in a diabetic-induced mouse treated with nano bio-composite ointments comprise of bamboo cellulose within the 18th day and there was a notable deposition of collagen and regeneration of tissue at the wound region. The study confirmed that cellulose derived from plants incorporated with silver nanoparticles has anti-microbial characteristics and it can accelerate acute wound healing, as the test results showed an effective absorption of exudates, exchange of gas, and biocompatibility at the wound site [70,71]. Besides, the exploration of hybrid cellulose/collagen dressing for DFU is the alternative approach in wound healing management as demonstrated in Table 1.
Table 1.
Cellulose/collagen dressing for DFU.
| Author | Aim | Study Design | Sample Size | Follow Up | Findings | Conclusion |
|---|---|---|---|---|---|---|
| Manizate and co-workers (2012) [55] | Compare the efficiency of bovine native collagen with silver ion (Ag) and sodium carboxymethylcellulose with Ag | Comparative, post-market clinical evaluation | 10 patients | 1st and 4th week | -50% of the wound exhibit S. Aureus -By the 4th week, the bacteria load increases up to 1.53 × 105 ppm |
-Bovine native collagen dressing shows rapid wound closure. |
| Gottrup and co-workers (2013) [68] | Compare collagen/oxidised regenerated cellulose (ORC)/silver therapy to standard treatment | Randomized control trial | 39 patients | Every 2 week for 14 weeks | -Decreased concentration of elastase, MMP-9 -low MMP-9:TIMP-1 concentration -Absence of infection and adverse effects |
-Collagen/ORC/silver therapy shows improved wound healing. |
| Ulrich and co-workers (2011) [43] | Evaluate the effect of collagen matrix/oxidized regenerated cellulose in wound exudate of DFU patients | Comparative clinical study | 32 patients | 14th, 28th, 42th, and 56th day | -Reduced level of MMP-2 -Reduction in plasmin, elastase and gelatinase |
-Wound size reduction on 14th and 28th days in ORC treated groups. |
| Griffin and co-workers (2019) [69] | Comparative study between the effectiveness of oxidized regenerated cellulose and ovine collagen extracellular matrix | Comparative study | 3230 patients | 4th, 8th, 12th, and 16th week | -82% of the healed wound with ORC dressing -15.2% of a worsened wound with ovine collagen extracellular matrix dressing |
-ORC decreases healing duration by improving granulation tissue formation in a short period. |
| Dumont and co-workers (2018) [61] | Evaluate the effectiveness of collagen-based dressing for DFU patients | Clinical follow-up | 6 male & 1 female | 38th to 64th day | -Increased formation of granulation tissue -complete surface healing at the wound site |
-Fast skin restoration -Decreased healing tine. -Decreased rate of infection. |
| Kloeters and co-workers (2015) [62] | Evaluate the effectiveness of oxidized regenerated collagen-cellulose matrix in pressure ulcer | Clinical assessment | 33 patients | Weekly for 12 weeks | -Decreased level of plasmin and elastase activity -reduction in the surface area of the wound -Absence of infection and intolerance towards oxidized regenerated cellulose/collagen matrix dressing. |
-Notable fast healing rate. |
| Solway and co-workers (2011) [65] | Study the effectiveness of microbial cellulose in DFU | Parallel open-label trial | 34 patients | Weekly till complete wound closure | -Increased formation of granulation tissue and maintenance of moist environment at the wound area -High tensile strength and crystallinity of the microbial cellulose |
-Rapid wound healing with a short period of re epithelisation |
| Li and co-workers (2020) [72] | Access the efficiency of naturally occurring bacterial cellulose-hyper branched cationic polysaccharide derivative on wound healing of diabetic rats |
In vivo study | Not specified | 1st, 4th and 7th day | -Good viability of cell -Low concentration of LDH -No effect on apoptosis -Inhibition in MMP-9 |
-Increased wound healing rate. |
| Song and co-workers (2018) [63] | Evaluate the effect of Selenium-loaded cellulose film in diabetic induced rats | In vivo study | 48 male rats | 3rd and 12th day | -Low elongation, high tensile strength, excellent microporous structure and high-water absorption capacity -Absence of toxicity |
-Notable rapid wound healing. -Notable stimulation in the angiogenesis pathway. |
| Li and co-workers (2020) [64] | Evaluate the effectiveness of carboxymethyl cellulose/K-carrageena/graphene oxide/konjac glucomannan hydrogel in diabetic induced mice | In vitro and in vivo study | 18 mice | 4th, 7th, 14th and 21st day | -The presence of permeable surface, high mechanical strength and great swelling capacity, supports the viability of the cell and has bactericidal property. | -Notable rapid wound recuperating. -Advanced fibroblast production and rapid re-epithelialization were seen. |
6. Cellulose/Collagen Dressing for DFU
Collagen that is readily available in human skin mainly functions as an extracellular matrix that acts as a three-dimensional scaffold in the body microstructure [73]. This scenario explains the main reason for human body comprises up to 70–80% of collagen and various types of proteins. Six different types of collagen are present in the human body, specifically existing in the human skin and collagen type I particularly makes up 70% of the human skin composition [74]. Generally, the existence of collagen is essential to stimulate the migration of fibroblasts during injuries in which at later stage increase the deposition of secreted collagen at the wound bed to accelerate wound healing [75,76]. It has always been observed through newly formed skin at the wound site. On the contrary, the imbalance of collagen synthesis and degradation, especially in diabetic patient’s skin, commonly exhibited severe stiffness with poor flexibility [77]. In addition, the inflammatory phases of wound healing in diabetic patients were prolonged and the deposition of granulation tissue was hindered, leading to a slow phase in wound healing [78,79]. In a worst-case scenario, DFU patients commonly presented with a high blood glucose level in the body will have altered blood circulation. This hyperglycaemic condition induces oxidative stress on the nerve cells, leading to nerve damage, which triggers a condition known as neuropathy. This scenario explains the diabetic patients lose their sensation mostly in their limbs and unaware of developed blister or ulcers at the later stage. Over time, the optimum balance of collagen metabolism (production and degradation) was lost due to the prolonged conditions with the additional appearance of the ulcerated epidermis [80,81]. When considering this issue, collagen-based wound dressing was developed and introduced in order to accomplish the demand of the current therapeutic needs in wound management system [78]. Following that, the use of collagen is scientifically proven in assisting wound healing process from an in vivo model until the clinical trial stage.
Manizate and co-workers (2012) conducted a comparative and prospective clinical study in 10 DFU patients, in which particular wounds were applied with either a sodium carboxy-methylcellulose or bovine native collagen dressing. The result demonstrated that bovine native collagen dressing that was incorporated with silver ion exhibited a normal activity of fibroblasts and protect the GF from being affected by the presence of matrix metalloproteinases (MMPs). In addition, it provides a moist environment to accelerate wound healing and also absorbs excessive exudates [69]. This finding was supported by Rangaraj and co-workers (2011), who stated that collagen dressing hindered the MMPs activity [74]. MMPs originated from natural endopeptidase that was frequently secreted by the normal cells, such as lymphocyte, granulocytes, and activated macrophage, into the extracellular matrix. A high level of MMPs will disrupt the interaction between GF and the extracellular matrix of the skin. The imbalance of MMPs and particular regulators will lead to an excess level of degradation activity. This causes a severe loss of extracellular matrix, thus slowing the re-epithelisation process during wound healing [81]. From the study conducted by Rangaraj and co-workers (2011), it has been proven that collagen balances the level of MMPs during an injury [74].
Another randomised control study was conducted by Gottrup and co-workers (2013) to evaluate the effect of oxidised regenerated cellulose (ORC) or collagen matrix as compared to the existing standard treatment. In this study, 39 DFU patients were chosen randomly and were divided into two groups, namely ORC dressing or collagen matrix and standard dressing comprising of 24 and 15 patients, respectively. By the fourth week, 50% of wound closure was observed among the subjects with ORC dressing. Weekly assessment at the 14th week unravelled a significant improvement in wound healing. Additionally, 52% of the subjects were completely healed by ORC dressing on the 14th week. No notable adverse effects or infection and a reduction in elastase were observed in patients receiving ORC treatments [62]. Elastase is a peptidase that is also a factor contributing to anti-healing by interfering with the synthesis of the collagen [48] and it can activate MMPs by degrading the existing connective tissue [82]. Thus, collagen dressing can act as a substrate for elastase activity that reduces the activity of elastase. Collagen tends to bind with elastase and this binding will not only alter the activity of elastase, but significantly improve wound closure.
A similar study was conducted by Ulrich and co-workers (2011), studying the effect of ORC or collagen matrix on the level of plasmin, gelatinase, and elastase in wound exudate of DFU patients. The study revealed a significant reduction in the above-measured enzyme, together with MMPs and the wound size. Plasmin originated from serine protease family has the potential to turn on the MMPs in the extracellular matrix. This accelerates the degradation of fibronectin, protease inhibitors, and GFs. These factors are essential elements in wound healing, whereas the imbalance of gelatinase concentration affected the level of collagen type IV degradation [48]. This phenomenon explained the rapid wound closure within a short period of time, as collagen has the potential to regulate the level of protease enzyme in an exudate. Similarly, a study that was conducted by Griffin and co-workers (2019) proved that the early application of ORC or collagen matrix dressing has the potential to increase the formation of granulation tissue [69]. This later will be transformed into matured connective tissue during the remodelling phase to restore the tissue function [83]. The study described that ORC dressing for DFU patients has 82% effectiveness for the complete healing of ulcer as compared to ovine collagen extracellular matrix dressing with 15.2% worse condition on the existing ulcer upon application of the dressing to the affected region [71].
A study was done by Dumont and co-workers (2018), using a tridimensional collagen-based matrix, GBT013, a collagen-based dressing applied to the DFU patients proved that collagen has the ability to deteriorate MMPs and increases cell proliferation rate. It has been demonstrated to have more than 44% reduction in the ulcerated area of non-healing ulcers [72]. A randomised and prospective study on protease-modulated ORC dressing or collagen matrix was performed by Kloeters and co-workers (2015) for treating pressure on sore ulcers. The subjects receiving ORC or collagen matrix treatment showed a positive healing rate with a drastic reduction of plasmin level from the fifth until 28th day and elastase from the fifth day with 100% absence of intolerant towards the treatment and infection. Through this study, it has been proven that low level of plasmin activity accelerates angiogenesis by increasing the level of VEGF that plays a pivotal role in wound healing [64]. This finding has been further supported by Tahergorabi and co-workers (2012), revealing that VEGF has a higher potential to mediate abnormal angiogenesis [81].
Besides that, Solway and co-workers (2011), through their parallel open-label trial study, proved that microbial cellulose (MC) dressing for DFU patients enhances re-epithelisation and rapid wound closure in a short period of time. This is possible due to the presence of a microporous structure of the MC, which initiates the coagulation process by trapping platelets to stop the bleeding at the ulcerated area. Therefore, the MC acts as a temporary scaffold supporting the activity of keratinocytes, fibroblasts, and endothelial that endures the formation of granulation tissue, leading to rapid re-epithelisation process. By this, a conducive microenvironment with moisture-retaining capacity is created to enhance the wound healing phases [68]. Similar speculation has been offered by the MC to accelerate wound healing process from the inflammatory phase until the proliferative phase by initiating tissue regeneration, neuro-vascularisation, and cell differentiation. Nevertheless, MC triggers fibroblasts activity by attracting the ability of fibroblasts to infiltrate the wound site. Therefore, the increment of collagen deposition would enhance rapid wound healing through wound contraction mechanism [84,85].
Besides that, a recent study that was performed by Li and co-workers (2020) using a hyperbranched cationic polysaccharide-derived bacterial cellulose (BC) encapsulated with small interfering RNA (siRNA) was tested on a diabetic-induced mice model. The study described that BC dressing reduces MMPs level by releasing siMMP-9. At the same time, in vitro testing showed that siMMP-9 has less impact on cell membrane integrity, considerably low level of cytotoxic, and no keratinocyte cell death has been identified. This characteristic of BC incorporated with siRNA has been proven to expedite wound healing rate than that of diabetic-induced mice [72]. The finding was supported by Song and co-workers (2018), who revealed the effect of selenium-loaded cellulose film on a diabetic-induced rat model. The experiment proved that the tested biomaterial has an excellent microporous structure with high tensile strength. These properties contributed to the rapid contraction of the wound, thus accelerating the rate of wound healing as compared to the control. In addition, there was a notable increase in angiogenesis with matured blood vessels in diabetic rats [63].
Meanwhile, fabricated carboxymethyl cellulose (CC) incorporated with Ag-ZnO tested on in vitro model showed a permeable surface that is necessary for the formation of the tissue as well as bactericidal property towards Staphylococcus aureus and Escherichia coli. Nevertheless, this biomaterial exhibits greater swelling characteristics that are capable of absorbing liquid from wound exudate and supporting cell viability, especially the fibroblasts as the main player in the wound healing process. This fabricated biomaterial has been tested in vivo resulted in rapid wound healing with faster re-epithelisation and advanced development of extracellular matrices [86]. These results simply indicate that CC incorporated with Ag-ZnO is a hybrid biomaterial executed both healing property and a protective mechanism by acting as an antibacterial agent towards gram-negative and gram-positive bacteria. This was further clarified by Basu (2018), where the group unravelled that CC provides a conducive microenvironment favouring granulation tissue. This happens with the presence of polysaccharides to stop the bleeding at the wound region and CC absorbs the liquid from the wound exudate through ion exchange. Thus, the formation of granulation tissue and newly formed tissue will decrease the duration of the wound healing process. This situation occurs following the degradation of the polymer at the injury site that has been proven to stimulate the aggregation of the inflammatory cells, followed by fibroblast and epithelial cells migration [83]. Consequently, there will be rapid healing with notable wound closure at the site of the injury with the intervention of CC [87,88].
7. Synergistic Effect of Cellulose/Collagen Dressing
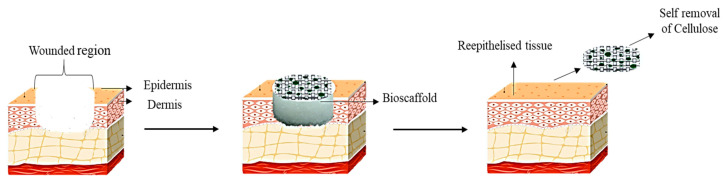
Through electrospinning, cellulose acetate-collagen can be fabricated, and this fabricated biomaterial showed an abundance of mesenchymal cell proliferation on the scaffold indicating the capability to be used as wound dressing [31]. An in vitro study conducted by Vatankhah and co-workers (2013) showed that fibroblasts attached to the electrospun nanofibres after seven days. This indicates the capability of collagen secretion due to the high affinity of the cell to the scaffold [85]. This positive outcome of in vivo study serves as the main reason for the electrospinning cellulose acetate being proposed to be used in wound dressing. Another study shows that the hybridization of collagen or chondroitin sulfate incorporated with keratinocytes and sodium carboxymethyl cellulose incorporated with fibroblasts showed a compact stratified surface layer resembling epidermis. This indicates that the hybridisation of these scaffolds is a perfect biomaterial to be used as wound dressing [33] and hybridisation of cellulose and collagen enhances in vitro proliferation of fibroblasts [34]. Therefore, collagen presents an essential key factor in providing biological and structural integrity resembling native ECM. It is a complex system in which related substances undergoing continual remodelling to regulate the activity of the cell and tissue function. Furthermore, collagen is known as surface-active and is capable of breaching the lipid-free interface [35] and, upon placing the collagen scaffold at the ulcerated region, more fibroblasts will be attracted to the wound region to accelerate the normal healing pathway [36]. Meanwhile, cellulose is capable of absorbing exudate from the injured tissue, retaining moisture microenvironment, and accelerating the granulation tissue formation [37]. Thus, cellulose/collagen dressing is expected to accelerate the ulcers healing process by dual functions through the presence of collagen and cellulose, in order to attract fibroblasts and absorb the exudates from the injured tissue, respectively. An absence of any foreign materials will eventually contribute to a rapid healing mechanism. Over time, the collagen scaffold will be absorbed in the wounded region as it is highly biodegradable. In contrast, cellulose will fall off together with the scab as cellulose is not degraded by the human body. Figure 5 shows the possible mechanism of action of the cellulose/collagen in diabetic foot ulcer patients.
Figure 5.
Mechanism of action of cellulose/collagen in ulcerated region.
8. Advantages of Cellulose/Collagen Dressings
Cellulose/collagen dressing is reported to have benefits over the currently available conventional dressing in the market. Despite any sources of derivative of cellulose, it is proven to be highly biocompatible to clinical applications. However, cellulose obviously cannot be digested in the human body due to the lack of enzymes for breaking down the beta acetal linkages. Apparently, cellulose can dry and fall off together with wound scab over time upon healing completion. Meantime, collagen is compatible with humans due to its amino acid structure (R-G-D). As so, cellulose/collagen provides more beneficial effects in comparison to other dressings. Table 2 shows the advantages of cellulose/collagen dressing when compared to conventional dressing.
Table 2.
Advantage of cellulose/collagen dressing.
| Cellulose/Collagen Dressing | Conventional Dressing |
|---|---|
| Reduced reactive oxygen species in the wound [89] | Slow granulation tissue deposition [90] |
| Ability to absorb wound exudates [59] | High possibility for pathogenic organism to harbor [90] |
| Accelerates wound healing/promote rapid healing [91] | Dry, so it’s impossible to retain moist microenvironment [92] |
| Reduced length of stay in hospital [52] | Loss efficiency when loaded with absorbed wound exudates [93] |
| Shortened course of treatment [94] | Often requires extra care and frequent changing [95] |
| Improvement in wound reduction area [96] | |
| Rapid granulation tissue formation [90] | |
| Improved re-epithelisation and GF concentration [88] | |
| Absence/reduced bacterial invasion at the wound site [97] | |
| Cost effective [89] | |
| Easy application and good adherence to the wound bed [98] |
9. Conclusions
This review summarises the positive effect of collagen as an advanced treatment for DFU patients as compared to cellulose, which is the most suitable to be used as a protective barrier due to its antibacterial characteristics. The hybridisation of collagen and cellulose is proven to enhance wound healing with rapid re-epithelisation and newly formed tissue. Further studies are needed in order to examine the mechanism of action for the hybridisation of collagen/cellulose dressing for DFU following the current high demand.
Acknowledgments
All the authors would like to express our gratitude to the faculty of Medicine, UKM for the guidance and resources to complete this review.
Abbreviations
| DFU | Diabetic foot ulcer |
| TCC | Total Contact Cast |
| NPWT | Negative Pressure wound therapy |
| AM | Amniotic membrane |
| DM | Diabetes mellitus |
| ORC | oxidized regenerated cellulose |
| GF | growth factor |
| FCG | formulated collagen gel |
| BC | bacterial cellulose |
| MC | Microbial cellulose |
| siRNA | small interfering RNA |
| CC | carboxymethyl cellulose |
Author Contributions
Conceptualization, R.N. and R.N.; methodology, R.N.; software, R.N.; validation, M.B.F.; formal analysis, M.B.F.; investigation, R.N.; resources, M.B.F.; data curation, R.N.; writing—original draft preparation, R.N.; writing—review and editing, M.B.F.; visualization, R.N.; supervision, M.B.F.; project administration, M.B.F.; funding acquisition, M.B.F. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded through the grant provided by Transdisciplinary Research Grant Scheme (TRGS/1/2019/UKM/02/1/3) in the form of database subscription. The funders do not have any contribution and decision to publish or preparation of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Ethical Approval and Consent to Participate
This study was approved by the National University of Malaysia (UKM) Research ethics committee with approval code of UKM PPI/111/8/JEP-2020-152.
References
- 1.Mishra S.C., Chhatbar K.C., Kashikar A., Mehndiratta A. Diabetic foot. BMJ. 2017;359:j5064. doi: 10.1136/bmj.j5064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fauzi A.A., Chung T.Y., Latif L.A. Risk factors of diabetic foot Charcot arthropathy: A case-control study at a Malaysian tertiary care centre. Singap. Med. J. 2016;57:198–203. doi: 10.11622/smedj.2016074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsourdi E., Barthel A., Rietzsch H., Reichel A., Bornstein S.R. Current aspects in the pathophysiology and treatment of chronic wounds in diabetes mellitus. Biomed. Res. Int. 2013;2013:385641. doi: 10.1155/2013/385641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeyaraman K., Berhane T., Hamilton M., Chandra A.P., Falhammar H. Mortality in patients with diabetic foot ulcer: A retrospective study of 513 cases from a single Centre in the Northern Territory of Australia. BMC Endocr. Disord. 2019;19:1. doi: 10.1186/s12902-018-0327-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chun D., Kim S., Kim J., Yang H.-J., Kim J.H., Cho J., Yi Y., Kim W.J., Won S.H. Epidemiology and Burden of Diabetic Foot Ulcer and Peripheral Arterial Disease in Korea. J. Clin. Med. 2019;8:748. doi: 10.3390/jcm8050748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rakin E. [(accessed on 24 June 2020)];Business Insider Malaysia. Malaysia July 25, 2018, Malaysia Has the Highest Rate of Diabetes in Asia—Doctors Have Classified the Disease as Another’ Silent Killer. Available online: https://www.businessinsider.my/malaysia-highest-rate-diabetes-silent-killer-asia.
- 7.Malaysia Has 3.6 Million Diabetics, Says Dzulkefly|The Star Online. [(accessed on 24 May 2020)];2019 Available online: https://www.thestar.com.my/news/nation/2019/03/27/malaysia-has-36-million-diabeticssays-dzulkefly.
- 8.Murugappan R. Kuala Lumpur 2019. [(accessed on 14 June 2020)]; Caring for Chronic Wounds Can be Complicated. The Star. Available online: https://www.thestar.com.my/lifestyle/health/2019/06/12/caring-for-chronic-wounds.
- 9.Mafauzy M., Hussein Z., Chan S.P. The Status of Diabetes Control in Malaysia: Results of Diabcare 2008. Med. J. Malays. 2011;66:175–181. [PubMed] [Google Scholar]
- 10.Raghav A., Khan Z.A., Labala R.K., Ahmad J., Noor S., Mishra B.K. Financial burden of diabetic foot ulcers to world: A progressive topic to discuss always. Ther. Adv. Endocrinol. Metab. 2018;9:29–31. doi: 10.1177/2042018817744513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lam A.W., Zaim M.R., Helmy H.H., Ramdhan I.M. Economic Impact of Managing Acute Diabetic Foot Infection in a Tertiary Hospital in Malaysia. Malays. Orthop. J. 2014;8:46–49. doi: 10.5704/moj.1403.018. [DOI] [Google Scholar]
- 12.Raspovic A., Landorf K.B. A survey of offloading practices for diabetes-related plantar neuropathic foot ulcers. J. Foot Ankle Res. 2014;7:35. doi: 10.1186/s13047-014-0035-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whitelaw S. The total contact cast : Controversy in offloading the diabetic foot. Br. J. Community Nurs. 2012;17:16–20. doi: 10.12968/bjcn.2012.17.sup12.s16. [DOI] [Google Scholar]
- 14.Shaw M. Foot Ulcers: A Different Technique to Total Contact Casting for Healing Chronic Foot Ulcers. J. Nurs. Healthc. 2017;1:1–4. [Google Scholar]
- 15.Yadav S.L. Prosthetics and Orthotics International. SAGE Publications; Lyon, France: 2015. To evaluate the efficacy of Total Contact Cast (TCC) compared to Patellar Tendon Bearing (PTB) cast with walking iron in the treatment of neuropathic plantar foot ulcer; p. 483. [Google Scholar]
- 16.Ranaweera A. Negative Pressure Wound Therapy. DermNet N. Z. [(accessed on 15 May 2020)];2013 Available online: https://dermnetnz.org/topics/negative-pressure-wound-therapy/
- 17.Ma Z., Li Z., Shou K., Jian C., Li P., Niu Y., Qi B., Yu A. Negative pressure wound therapy: Regulating blood flow perfusion and microvessel maturation through microvascular pericytes. Int. J. Mol. Med. 2017;40:1415–1425. doi: 10.3892/ijmm.2017.3131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meloni M., Izzo V., Vainieri E., Giurato L., Ruotolo V., Uccioli L. Management of negative pressure wound therapy in the treatment of diabetic foot ulcers. World J. Orthop. 2015;6:387–393. doi: 10.5312/wjo.v6.i4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Voelker R. Diabetic Foot Ulcers Heal With Shock Wave Therapy. JAMA. 2018;319:649. doi: 10.1001/jama.2018.0480. [DOI] [PubMed] [Google Scholar]
- 20.Inserro A. FDA Approves First Shock Wave Device to Treat Diabetic Foot Ulcers. AJMC. [(accessed on 23 July 2020)];2017 Available online: https://www.ajmc.com/view/fda-approves-first-shock-wave-device-to-treat-diabetic-foot-ulcers.
- 21.Snyder R., Galiano R., Mayer P., Rogers L.C., Alvarez O. Diabetic foot ulcer treatment with focused shockwave therapy: Two multicentre, prospective, controlled, double-blinded, randomised phase III clinical trials. J. Wound Care. 2018;27:822–836. doi: 10.12968/jowc.2018.27.12.822. [DOI] [PubMed] [Google Scholar]
- 22.Tian X., Liang X.M., Song G.M., Zhao Y., Yang X.L. Maggot debridement therapy for the treatment of diabetic foot ulcers: A meta-analysis. J. Wound Care. 2013;22:462–469. doi: 10.12968/jowc.2013.22.9.462. [DOI] [PubMed] [Google Scholar]
- 23.Azad A.K., Yee B.-L., Azizi W.M., Adham S. Maggot debridement therapy for diabetic foot ulcer: Experience from Maggot treatment Centers. Asian J. Pharm. Pharmacol. 2016;2:23–25. [Google Scholar]
- 24.Netten J.J.V., Clark D., Lazzarini P.A., Janda M., Reed L.F. The validity and reliability of remote diabetic foot ulcer assessment using mobile phone images. Sci. Rep. 2017;7:1–10. doi: 10.1038/s41598-017-09828-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Naik G., Harding K. Maggot debridement therapy: The current perspectives. Chronic Wound Care Manag. Res. 2017;4:121–128. doi: 10.2147/CWCMR.S117271. [DOI] [Google Scholar]
- 26.Ali R., Qureshi A., Yaqoob M.Y., Shakil M. Total contact cast for neuropathic diabetic foot ulcers. J. Coll. Physicians Surg. Pak. 2008;18:695–698. [PubMed] [Google Scholar]
- 27.Applewhite A.J. Following the Evidence for Total Contact Casting as First-Line Treatment of DFUs in the Wound Clinic. Today’s Wound Clin. [(accessed on 16 June 2020)];2016 Available online: https://www.todayswoundclinic.com/articles/following-evidence-total-contact-casting-first-line-treatment-dfus-wound-clinic.
- 28.Messenger G., Masoetsa R., Hussain I. A Narrative Review of the Benefits and Risks of Total Contact Casts in the Management of Diabetic Foot Ulcers. J. Am. Coll. Clin. Wound Spec. 2017;9:19–23. doi: 10.1016/j.jccw.2018.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.García Oreja S., Navarro González-Moncayo J., Sanz Corbalán I., García Morales E., Álvaro Afonso F.J., Lázaro Martínez J.L. Complications associated with the negative pressure therapy in the treatment of the diabetic foot ulcers: Retrospective case series. Rev. Española Podol. 2017;28:e27–e31. doi: 10.1016/j.repod.2017.06.001. [DOI] [Google Scholar]
- 30.Liu S., He C.Z., Cai Y.T., Xing Q.P., Guo Y.Z., Chen Z.L., Su J.L., Yang L.P. Evaluation of negative-pressure wound therapy for patients with diabetic foot ulcers: Systematic review and meta-analysis. Ther. Clin. Risk Manag. 2017;13:533–544. doi: 10.2147/TCRM.S131193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jordan A., Khiyani N., Bowers S., Lukaszczyk J., Stawicki S. Maggot debridement therapy: A practical review. Int. J. Acad. Med. 2018;4:34. doi: 10.4103/ijam.ijam_6_18. [DOI] [Google Scholar]
- 32.Total Contact Casting Wikipedia. Creative Commons Attribution-ShareAlike License. [(accessed on 27 June 2020)];2018 Available online: https://en.wikipedia.org/wiki/Total_contact_casting.
- 33.McIntosh J. What Is Collagen, and Why Do People Use It? [(accessed on 23 May 2020)];Med. News Today. 2017 Available online: https://www.medicalnewstoday.com/articles/262881.
- 34.Pawelec K.M., Best S.M., Cameron R.E. Collagen: A network for regenerative medicine. J. Mater. Chem. B. 2016;4:6484–6496. doi: 10.1039/C6TB00807K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ricard-Blum S. The Collagen Family. Cold Spring Harb. Perspect. Biol. 2011;3:1–19. doi: 10.1101/cshperspect.a004978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.He L., Mu C., Shi J., Zhang Q., Shi B., Lin W. Modification of collagen with a natural cross-linker, procyanidin. Int. J. Biol. Macromol. 2011;48:354–359. doi: 10.1016/j.ijbiomac.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 37.Lorenz J.S., Schnauß J., Glaser M., Sajfutdinow M., Schuldt C., Käs J.A., Smith D.M. Synthetic Transient Crosslinks Program the Mechanics of Soft, Biopolymer-Based Materials. Adv. Mater. 2018;30:e1706092. doi: 10.1002/adma.201706092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shah R., Stodulka P., Skopalova K., Saha P. Dual crosslinked collagen/chitosan film for potential biomedical applications. Polymers. 2019;11:2094. doi: 10.3390/polym11122094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shoulders M.D., Raines R.T. Collagen Structure and Stability. Annu. Rev. Biochem. 2009;78:929–958. doi: 10.1146/annurev.biochem.77.032207.120833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schmidt M.M., Dornelles R.C.P., Mello R.O., Kubota E.H., Mazutti M.A., Kempka A.P., Demiate I.M. Collagen extraction process. Int. Food Res. J. 2016;23:913–922. [Google Scholar]
- 41.Yang H., Shu Z. The extraction of collagen protein from pig skin. J. Chem. Pharm. Res. 2014;6:683–687. [Google Scholar]
- 42.Moore J. Examining The Potential Of Collagen Powders In The Diabetic Foot|Podiatry Today. Pod. Today. 2015;28:18–22. [Google Scholar]
- 43.Ulrich D., Smeets R., Unglaub F., Wöltje M., Pallua N. Effect of oxidized regenerated cellulose/collagen matrix on proteases in wound exudate of patients with diabetic foot ulcers. J. Wound Ostomy Cont. Nurs. 2011;38:522–528. doi: 10.1097/WON.0b013e31822ad290. [DOI] [PubMed] [Google Scholar]
- 44.Fleischli J.G., Laughlin T.J., Fleischli J.W. Equine pericardium collagen wound dressing in the treatment of the neuropathic diabetic foot wound a pilot study. J. Am. Podiatr. Med. Assoc. 2009;99:301–305. doi: 10.7547/0980301. [DOI] [PubMed] [Google Scholar]
- 45.Blume P., Driver V.R., Tallis A.J., Kirsner R.S., Kroeker R., Payne W.G., Wali S., Marston W., Dove C., Engler R.L., et al. Formulated collagen gel accelerates healing rate immediately after application in patients with diabetic neuropathic foot ulcers. Wound Repair Regen. 2011;19:302–308. doi: 10.1111/j.1524-475X.2011.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fauzi M.B., Lokanathan Y., Nadzir M.M., Aminuddin S., Ruszymah B.H.I., Chowdhury S.R. Attachment, proliferation, and morphological properties of human dermal fibroblasts on ovine tendon collagen scaffolds: A comparative study. Malays. J. Med. Sci. 2017;24:33–43. doi: 10.21315/mjms2017.24.2.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Munish T., Ramneesh G., Sanjeev S., Jasdeep S., Jaspal S., Nikhil G. Collagen Based Dressing and Standard Dressing in Diabetic Foot Ulcer. J. Evol. Med. Dent. Sci. 2015;4:3614–3621. doi: 10.14260/jemds/2015/521. [DOI] [Google Scholar]
- 48.Chalimidi K.R., Kumar Y., Kini U.A. Efficacy of Collagen Particles in Chronic Non Healing Ulcers. J. Clin. Diagn. Res. 2015;9:PC03. doi: 10.7860/JCDR/2015/11782.6001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shanmugam S., Professor A., Assistant Professor S. A comprehensive study on effect of collagen dressing in diabetic foot ulcer. Int. Arch. Integr. Med. 2017;4:163–167. [Google Scholar]
- 50.Lee D.-S., Lee Y.-N., Han S.-K., Namgoong S. Effect of Collagen Dressing on Diabetic Wound Healing—A Pilot Study. J. Korean Wound Manag. Soc. 2015;11:1–10. [Google Scholar]
- 51.Wen Y., Wang H., Chen B., Chen Y., Zhang T., Xu T., Sun W. Association of Information Sources and Knowledge on HIV/AIDS in Rural China. Int. J. Collab. Res. Intern. Med. Public Health. 2015;7:13–23. [PMC free article] [PubMed] [Google Scholar]
- 52.Pei Y., Yang J., Liu P., Xu M., Zhang X., Zhang L. Fabrication, properties and bioapplications of cellulose/collagen hydrolysate composite films. Carbohydr. Polym. 2013;92:1752–1760. doi: 10.1016/j.carbpol.2012.11.029. [DOI] [PubMed] [Google Scholar]
- 53.Sahana T.G., Rekha P.D. Biopolymers: Applications in wound healing and skin tissue engineering. Mol. Biol. Rep. 2018;45:2857–2867. doi: 10.1007/s11033-018-4296-3. [DOI] [PubMed] [Google Scholar]
- 54.Lavanya D., Kulkarni P., Dixit M., Raavi P.K. Sources of cellulose and their applications—A review. Int. J. Drug Formul. Res. 2011;2:19–38. [Google Scholar]
- 55.Manizate F., Fuller A., Gendics C., Lantis J.C. A prospective, single-center, nonblinded, comparative, postmarket clinical evaluation of a bovine-derived collagen with ionic silver dressing versus a carboxymethylcellulose and ionic silver dressing for the reduction of bioburden in variable-etiology, bi. Adv. Ski. Wound Care. 2012;25:220–225. doi: 10.1097/01.ASW.0000414705.56138.65. [DOI] [PubMed] [Google Scholar]
- 56.Mohamad N., Loh E.Y.X., Fauzi M.B., Ng M.H., Mohd Amin M.C.I. In vivo evaluation of bacterial cellulose/acrylic acid wound dressing hydrogel containing keratinocytes and fibroblasts for burn wounds. Drug Deliv. Transl. Res. 2018;9:444–452. doi: 10.1007/s13346-017-0475-3. [DOI] [PubMed] [Google Scholar]
- 57.Portal O., Clark W.A., Levinson D.J. Microbial Cellulose Wound Dressing in the Treatment of Nonhealing Lower Extremity Ulcers|Wounds Research. Wounds. 2009;21:1–3. [PubMed] [Google Scholar]
- 58.Galateanu B., Bunea M.-C., Stanescu P., Vasile E., Casarica A., Iovu H., Hermenean A., Zaharia C., Costache M. In Vitro Studies of Bacterial Cellulose and Magnetic Nanoparticles Smart Nanocomposites for Efficient Chronic Wounds Healing. Stem Cells Int. 2015;2015:195096. doi: 10.1155/2015/195096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Portela R., Leal C.R., Almeida P.L., Sobral R.G. Bacterial cellulose: A versatile biopolymer for wound dressing applications. Microb. Biotechnol. 2019;12:586–610. doi: 10.1111/1751-7915.13392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xi Loh E.Y., Fauzi M.B., Ng M.H., Ng P.Y., Ng S.F., Ariffin H., Mohd Amin M.C.I. Cellular and Molecular Interaction of Human Dermal Fibroblasts with Bacterial Nanocellulose Composite Hydrogel for Tissue Regeneration. ACS Appl. Mater. Interfaces. 2018;10:1–57. doi: 10.1021/acsami.8b16645. [DOI] [PubMed] [Google Scholar]
- 61.Dumont I.J., Lepeut M., Segalen C., Guillemin Y., Gouze J.N. Use of gbt013, a collagen-based dressing, for the healing of diabetic foot ulcers a case series. J. Am. Podiatr. Med. Assoc. 2018;108:419–429. doi: 10.7547/16-102. [DOI] [PubMed] [Google Scholar]
- 62.Kloeters O., Unglaub F., de Laat E., van Abeelen M., Ulrich D. Prospective and randomised evaluation of the protease-modulating effect of oxidised regenerated cellulose/collagen matrix treatment in pressure sore ulcers. Int. Wound J. 2015;13:1231–1236. doi: 10.1111/iwj.12449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Song S.H., Kim J.E., Koh E.K., Sung J.E., Lee H.A., Yun W.B., Hong J.T., Hwang D.Y. Selenium-loaded cellulose film derived from Styela clava tunic accelerates the healing process of cutaneous wounds in streptozotocin-induced diabetic Sprague–Dawley rats. J. Dermatol. Treat. 2018;29:606–616. doi: 10.1080/09546634.2018.1425357. [DOI] [PubMed] [Google Scholar]
- 64.Li X.-X., Dong J.-Y., Li Y.-H., Zhong J., Yu H., Yu Q.-Q., Lei M. Fabrication of Ag–ZnO@ carboxymethyl cellulose/K-carrageenan/graphene oxide/konjac glucomannan hydrogel for effective wound dressing in nursing care for diabetic foot ulcers. Appl. Nanosci. 2020;10:729–738. doi: 10.1007/s13204-019-01194-z. [DOI] [Google Scholar]
- 65.Solway D.R., Clark W.A., Levinson D.J. A parallel open-label trial to evaluate microbial cellulose wound dressing in the treatment of diabetic foot ulcers. Int. Wound J. 2011;8:69–73. doi: 10.1111/j.1742-481X.2010.00750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Loh E.Y.X., Mohamad N., Fauzi M.B., Ng M.H., Ng S.F., Mohd Amin M.C.I. Development of a bacterial cellulose-based hydrogel cell carrier containing keratinocytes and fibroblasts for full-thickness wound healing. Sci. Rep. 2018;8:1–12. doi: 10.1038/s41598-018-21174-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Singla R., Soni S., Patial V., Kulurkar P.M., Kumari A., Mahesh S., Padwad Y.S., Yadav S.K. In vivo diabetic wound healing potential of nanobiocomposites containing bamboo cellulose nanocrystals impregnated with silver nanoparticles. Int. J. Biol. Macromol. 2017;105:45–55. doi: 10.1016/j.ijbiomac.2017.06.109. [DOI] [PubMed] [Google Scholar]
- 68.Gottrup F., Cullen B.M., Karlsmark T., Bischoff-Mikkelsen M., Nisbet L., Gibson M.C. Randomized controlled trial on collagen/oxidized regenerated cellulose/silver treatment. Wound Repair Regen. 2013;21:216–225. doi: 10.1111/wrr.12020. [DOI] [PubMed] [Google Scholar]
- 69.Griffin L., Carter M.J., D’Agostino R., McGowan L.D. Comparative Effectiveness of Two Collagen-containing Dressings: Oxidized Regenerated Cellulose (ORC)/Collagen/Silver-ORC Dressing Versus Ovine Collagen Extracellular Matrix|Wounds Research. Wounds. 2019;31:E73–E76. [PubMed] [Google Scholar]
- 70.Hickey R.J., Pelling A.E. Cellulose biomaterials for tissue engineering. Front. Bioeng. Biotechnol. 2019;7:45. doi: 10.3389/fbioe.2019.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pinho E., Soares G. Functionalization of cotton cellulose for improved wound healing. J. Mater. Chem. B. 2018;6:1887–1898. doi: 10.1039/C8TB00052B. [DOI] [PubMed] [Google Scholar]
- 72.Li N., Yang L., Pan C., Saw P.E., Ren M., Lan B., Wu J., Wang X., Zeng T., Zhou L., et al. Naturally-occurring bacterial cellulose-hyperbranched cationic polysaccharide derivative/MMP-9 siRNA composite dressing for wound healing enhancement in diabetic rats. Acta Biomater. 2020;18:298–314. doi: 10.1016/j.actbio.2019.11.005. [DOI] [PubMed] [Google Scholar]
- 73.Serafica G., Mormino G., Oster G.A., Lentz K.E., Koehler K.P. Microbial Cellulose Wound Dressing for Treating Chronic Wounds. 7,704,523. U.S. Patent. 2010 Apr 27;
- 74.Rangaraj A., Harding K., Leaper D. Role of collagen in wound management. Wounds UK. 2011;7:54–63. [Google Scholar]
- 75.Li B., Wang J.H.C. Fibroblasts and myofibroblasts in wound healing: Force generation and measurement. J. Tissue Viability. 2011;20:108–120. doi: 10.1016/j.jtv.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Goulding V. Wound healing. Diabet. Foot J. 2015;18:75–80. [Google Scholar]
- 77.How Diabetes Impacts Wound Healing. Wound Source. [(accessed on 12 July 2020)];2017 Available online: https://www.woundsource.com/blog/how-diabetes-impacts-wound-healing#:~:text=High%20blood%20glucose%20causes%20stiffening,complications%20in%20diabetes%20wound%20healing.
- 78.Nguyen T.T., Mobashery S., Chang M. Roles of matrix metalloproteinases in cutaneous wound healing. In: Alexandrescu D.V., editor. Wound Healing—New Insights into Ancient Challenges. InTech; London, UK: 2016. pp. 37–70. [DOI] [Google Scholar]
- 79.Auf Dem Keller U., Sabino F. Matrix metalloproteinases in impaired wound healing. Met. Med. 2015;2:8. doi: 10.2147/MNM.S68420. [DOI] [Google Scholar]
- 80.Häkkinen L., Larjava H., Koivisto L. Granulation tissue formation and remodeling. Endod. Top. 2012;24:94–129. doi: 10.1111/etp.12008. [DOI] [Google Scholar]
- 81.Tahergorabi Z., Khazaei M. Imbalance of angiogenesis in diabetic complications: The mechanisms. Int. J. Prev. Med. 2012;3:827–838. doi: 10.4103/2008-7802.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Park S.U., Lee B.K., Kim M.S., Park K.K., Sung W.J., Kim H.Y., Han D.G., Shim J.S., Lee Y.J., Kim S.H., et al. The possibility of microbial cellulose for dressing and scaffold materials. Int. Wound J. 2012;11:35–43. doi: 10.1111/j.1742-481X.2012.01035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Basu P., Narendrakumar U., Arunachalam R., Devi S., Manjubala I. Characterization and Evaluation of Carboxymethyl Cellulose-Based Films for Healing of Full-Thickness Wounds in Normal and Diabetic Rats. ACS Omega. 2018;3:12622–12632. doi: 10.1021/acsomega.8b02015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nurwito B.S., Maulida H.N. Electrospun fibers as a wound dressing material using combination of cellulose acetate/collagen seeding stem cell. Asian J. Microbiol. Biotechnol. Environ. Sci. Pap. 2018;20:43–47. [Google Scholar]
- 85.Vatankhah E., Prabhakaran M.P., Jin G., Mobarakeh L.G., Ramakrishna S. Development of nanofibrous cellulose acetate/gelatin skin substitutes for variety wound treatment applications. J. Biomater. Appl. 2014;28:909–921. doi: 10.1177/0885328213486527. [DOI] [PubMed] [Google Scholar]
- 86.Kilic Bektas C., Kimiz I., Sendemir A., Hasirci V., Hasirci N. A bilayer scaffold prepared from collagen and carboxymethyl cellulose for skin tissue engineering applications. J. Biomater. Sci. Polym. Ed. 2018;29:1764–1784. doi: 10.1080/09205063.2018.1498718. [DOI] [PubMed] [Google Scholar]
- 87.Chattopadhyay S., Raines R.T. Collagen-based biomaterials for wound healing. Biopolymers. 2014;101:821–833. doi: 10.1002/bip.22486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Naomi R., Ratanavaraporn J., Fauzi M.B. Comprehensive Review of Hybrid Collagen and Silk Fibroin for Cutaneous Wound Healing. Materials. 2020;13:3097. doi: 10.3390/ma13143097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wu S., Applewhite A.J., Niezgoda J., Snyder R., Shah J., Cullen B., Schultz G., Harrison J., Hill R., Howell M., et al. Oxidized regenerated cellulose/collagen dressings: Review of evidence and recommendations. Adv. Ski. Wound Care. 2017;30:S1–S18. doi: 10.1097/01.ASW.0000525951.20270.6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Singh O., Gupta S., Soni M., Moses S., Shukla S., Mathur R. Collagen dressing versus conventional dressings in burn and chronic wounds: A retrospective study. J. Cutan. Aesthet. Surg. 2011;4:16. doi: 10.4103/0974-2077.79180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Matthews K.H. Drug delivery dressings. In: Farrar D., editor. Advanced Wound Repair Therapies. Elsevier Inc.; York, UK: 2011. pp. 361–394. [Google Scholar]
- 92.Pilehvar-Soltanahmadi Y., Dadashpour M., Mohajeri A., Fattahi A., Sheervalilou R., Zarghami N. An overview on application of natural substances incorporated with electrospun nanofibrous scaffolds to development of innovative wound dressings. Mini-Rev. Med. Chem. 2017;18:414–427. doi: 10.2174/1389557517666170308112147. [DOI] [PubMed] [Google Scholar]
- 93.Kamoun E.A., Kenawy E.R.S., Chen X. A review on polymeric hydrogel membranes for wound dressing applications: PVA-based hydrogel dressings. J. Adv. Res. 2017;8:217–233. doi: 10.1016/j.jare.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Li H., Cheng W., Liu K., Chen L., Huang Y., Wang X., Lv Z., He J., Li C. Reinforced collagen with oxidized microcrystalline cellulose shows improved hemostatic effects. Carbohydr. Polym. 2017;165:30–38. doi: 10.1016/j.carbpol.2017.02.023. [DOI] [PubMed] [Google Scholar]
- 95.Hermans M.H.E., Bolton L.L. Air exposure versus occlusion: Merits and disadvantages of different dressings. J. Wound Care. 1993;2:362–365. doi: 10.12968/jowc.1993.2.6.362. [DOI] [PubMed] [Google Scholar]
- 96.Klein R.J. Use of Oxidized Regenerated Cellulose (ORC)/Collagen/Silver-ORC Dressings alone or subsequent to advanced wound therapies in complex wounds. Wounds. 2020;32:37–43. [PubMed] [Google Scholar]
- 97.Growney Kalaf E.A., Hixon K.R., Kadakia P.U., Dunn A.J., Sell S.A. Electrospun biomaterials for dermal regeneration. In: Kny E., Uyar T., editors. Electrospun Materials for Tissue Engineering and Biomedical Applications: Research, Design and Commercialization. Woodhead Publishing; Sawston, Cambridge, UK: 2017. pp. 179–231. [Google Scholar]
- 98.Moraes P.R., Saska S., Barud H., Lima L.R., Martins V.D., Plepis A.M., Ribeiro S.J., Gaspar A.M. Bacterial cellulose/collagen hydrogel for wound healing. Mater. Res. 2016;19:106–116. doi: 10.1590/1980-5373-MR-2015-0249. [DOI] [Google Scholar]