ABSTRACT
Burkholderia mallei
is a highly pathogenic bacterium that causes the fatal zoonosis glanders. The organism specifies multiple membrane proteins, which represent prime targets for the development of countermeasures given their location at the host-pathogen interface. We investigated one of these proteins, Pal, and discovered that it is involved in the ability of B. mallei to resist complement-mediated killing and replicate inside host cells in vitro, is expressed in vivo and induces antibodies during the course of infection, and contributes to virulence in a mouse model of aerosol infection. A mutant in the pal gene of the B. mallei wild-type strain ATCC 23344 was found to be especially attenuated, as BALB/c mice challenged with the equivalent of 5,350 LD50 completely cleared infection. Based on these findings, we tested the hypothesis that a vaccine containing the Pal protein elicits protective immunity against aerosol challenge. To achieve this, the pal gene was cloned in the vaccine vector Parainfluenza Virus 5 (PIV5) and mice immunized with the virus were infected with a lethal dose of B. mallei. These experiments revealed that a single dose of PIV5 expressing Pal provided 80% survival over a period of 40 days post-challenge. In contrast, only 10% of mice vaccinated with a PIV5 control virus construct survived infection. Taken together, our data establish that the Peptidoglycan-associated lipoprotein Pal is a critical virulence determinant of B. mallei and effective target for developing a glanders vaccine.
KEYWORDS: Burkholderia mallei, glanders, virulence, mouse aerosol infection, vaccine, protective antigen
Introduction
Burkholderia mallei is a host-adapted Gram-negative bacterium and causes the incapacitating and highly fatal zoonotic disease glanders, which affects primarily horses, donkeys, and mules. The organism is extremely contagious through contact with diseased equids and humans are susceptible to infection. Glanders is endemic in Asia, South America, Africa, and the Middle East and the disease is closely monitored by the World Organization of Animal Health as it is considered a biosecurity and biosafety threat [1–3].
Comparative analyses indicate that B. mallei evolved from the bacterium Burkholderia pseudomallei through genomic reduction. The latter is commonly found in water and wet soils of countries bordering the equator and causes the global emerging tropical disease melioidosis [4–6]. The genes retained by B. mallei have a high level of sequence identity with their B. pseudomallei orthologs and the two species share many virulence determinants [7–10]. The clinical and pathological manifestations of disease caused by the organisms are also very similar. In humans, infection typically occurs through punctured skin and the respiratory route, and the most common manifestations are life-threatening pneumonia and bacteremia [3,4,11,12]. Pathogenesis is complex and entails the synchronized expression of genes supporting intracellular and extracellular replication of bacteria, colonization of deep tissues and organ systems, and development of hallmark chronic lesions that are difficult to treat and eliminate [13–16].
Glanders and melioidosis lack reliable modern diagnostic tools and require extended therapy with low success rate due in part to the intrinsic resistance of B. mallei and B. pseudomallei to antibiotics [17,18]. No vaccine exists to protect animals or humans and there is concern that these highly pathogenic bacteria could be used as bioweapons, hence their classification as Tier 1 Select Agents by U.S federal agencies. Fortunately, the genetic, virulence, and disease similarities between B. mallei and B. pseudomallei suggest the feasibility of devising medical countermeasures that protect against both organisms. This premise is supported by studies showing that antibodies against in vivo expressed Burkholderia antigens [19], vaccination with Burkholderia live attenuated strains [19,20] and outer membrane vesicles [21,22], and polysaccharide-based vaccines [23,24] provide cross-species protection in animal models of melioidosis and glanders.
Immunoreactive proteins expressed by B. mallei and B. pseudomallei during human infections have been identified using immunoproteomic approaches and represent high value targets for developing countermeasures [25–28]. One particular B. pseudomallei antigen, designated BPSL2765 (locus tag in the genome of strain K96243), was found to induce immune responses linked to lower incidence of chronic and recurrent melioidosis [26]. Immunization with subunit vaccines containing BPSL2765 was also shown to provide partial protection against intraperitoneal challenge in a mouse model of melioidosis [29,30].
Comparative sequence analyses and determination of the crystal structure of BPSL2765 indicated that the protein is an ortholog of the well-characterized Peptidoglycan-associated lipoprotein (Pal) of Gram-negative bacteria [31]. Pal is a component of the Tol-Pal system, which comprises the five core proteins TolQ, TolR, TolA, TolB, and Pal. The Tol-Pal proteins form a complex that spans the inner and outer membranes and is required for maintaining cell wall integrity and can be exploited for the entry of macromolecules such as bacteriocins and bacteriophages [32,33]. The first amino acid of the mature Pal protein is a lipidated cysteine and the hydrophobic N-terminus anchors Pal in the outer membrane while the C-terminal region interacts with the meso-diaminopimelate residue of peptidoglycan in the periplasm. Pal also interacts with the TolB and TolA proteins, which are located in the periplasm and the inner membrane, respectively. The other components of the Tol-Pal system, TolQ and TolR, are located in the inner membrane and interact with TolA. Together, the Tol-Pal proteins form a cross-bridge between the outer membrane, peptidoglycan cell wall, and inner membrane [32,33].
Despite in-depth characterization in many organisms, the biological role of Pal in B. mallei and B. pseudomallei was not investigated previously and its value as a vaccine target against aerosol exposure has not been determined. The goals of this study were to engineer a B. mallei pal mutant strain, investigate the phenotypic traits of the mutant, and develop a delivery system to test the vaccinogenic potential of the antigen in a mouse model of infection.
Materials and methods
In silico analyses
The ExPASy Bioinformatics Resource Portal (https://www.expasy.org) was used to analyze nucleotide and protein sequences. LipoP 1.0 (http://www.cbs.dtu.dk/services/LipoP/) and SignalP 5.0 (http://www.cbs.dtu.dk/services/SignalP/) were used to identify signal sequence cleavage sites within proteins. Conserved domains were identified with the NCBI Conserved Domain Database (CDD; https://www.ncbi.nlm.nih.gov/cdd/). NCBI BLAST (https://blast.ncbi.nlm.nih.gov/Blast.cgi) was used to search bacterial genomes and identify pal orthologs.
Plasmids, bacterial strains, and growth conditions
Table 1 lists the strains and plasmids used in this study. Burkholderia mallei strains were routinely propagated in Brucella medium (BD) containing glycerol (5% vol/vol) at a temperature of 37°C. The medium was supplemented with zeocin (7.5 ug/mL), kanamycin (5 ug/mL), and/or Polymyxin B (5 ug/mL) when appropriate. For infection experiments (cell culture, mouse challenge), B. mallei was grown on agar plates for 2 days and bacteria were suspended to a concentration of 1 × 109 CFU per mL in phosphate-buffered saline (PBS). The suspensions were then serially diluted and used to infect cell cultures and mice. For all experiments, 100-uL portions of the bacterial suspensions (and dilutions) were spread onto agar plates to determine the number of CFU in the inoculum. Escherichia coli strains were cultured in low-salt Luria-Bertani (LSLB) medium at 37°C. The medium was supplemented with chloramphenicol (15 ug/mL), kanamycin (50 ug/mL), zeocin (50 ug/mL), and/or tetracycline (15 ug/mL) when appropriate.
Table 1.
Strains and plasmids.
| Strain or plasmid | Description | Source or reference |
|---|---|---|
| B. mallei | ||
| ATCC 23344 | Wild-type strain; polymyxin B resistant, kanamycin and zeocin sensitive | [10] |
| pal KO | Isogenic pal mutant strain of ATCC 23344; resistant to polymyxin B and zeocin, sensitive to kanamycin | This study |
| E. coli | ||
| EPI300 | Strain used for general recombinant DNA manipulations; sensitive to kanamycin, zeocin, tetracycline, and chloramphenicol | epicenter/Lucigen |
| EC100D pir+ | Strain used for recombinant DNA manipulations of plasmid pKAS46 and derivatives; sensitive to kanamycin and zeocin | epicenter/Lucigen |
| S17 | Strain used for conjugational transfer of plasmids to B. mallei; sensitive to kanamycin, zeocin, and polymyxin B | [34] |
| TUNER | Protein expression strain used to purify His-tagged PalBm and LolCBm proteins; chloramphenicol sensitive | Millipore Sigma |
| Plasmids | ||
| pBHR1 | Cloning vector; confers resistance to chloramphenicol and kanamycin | MoBiTec |
| pBHR1∆ Dra | pBHR1 containing a 339 nt deletion in the chloramphenicol resistance marker; confers resistance only to kanamycin | [43] |
| pPalBm | pBHR1 in which a 812 nt DNA fragment containing the pal gene of B. mallei ATCC 23344 was inserted; confers resistance only to kanamycin | This study |
| pEM7/ZEO | Source of the zeocin resistance cassette; confers resistance to zeocin | ThermoFisher Scientific |
| pACYC184 | Cloning vector; confers resistance to chloramphenicol and tetracycline | New England Biolabs Inc. |
| pACYCPalBm | pACYC184 in which a 1,332 nt DNA fragment containing the pal gene of B. mallei ATCC 23344 was inserted; confers resistance to tetracycline | This study |
| pACYCPalBmZEO | pACYCPalBm in which a zeocin resistance cassette was inserted near the middle of the pal gene; confers resistance to tetracycline and zeocin | This study |
| pKAS46 | Gene replacement vector; confers resistance to kanamycin | [35] |
| pKASPalBmZEO | pKAS46 containing the pal gene interrupted with a zeocin resistance cassette from pACYCPalBmZEO; confers resistance to kanamycin and zeocin | This study |
| pETcoco-1 | His-tagged protein expression vector; confers resistance to chloramphenicol | Millipore Sigma |
| pHisPalBm | pETcoco-1 in which a gene fragment encoding amino acids 22 to 170 of B. mallei ATCC 23344 Pal was inserted; confers resistance to chloramphenicol | This study |
| pHisLolCBm | pETcoco-1 in which a gene fragment encoding amino acids 47 to 243 of B. mallei ATCC 23344 LolC was inserted; confers resistance to chloramphenicol | This study |
| pMHD11 | pZL185 (PIV5 genome) in which a gene fragment encoding amino acids 22 to 170 of B. mallei ATCC 23344 Pal was inserted; confers resistance to chloramphenicol | This study |
| Viruses | ||
| PIV5-PalBm (MHD11) | PIV5 expressing amino acids 22 to 170 of B. mallei ATCC 23344 Pal protein | This study |
| PIV5-BatA | PIV5 expressing amino acids 30 to 307 of B. mallei ATCC 23344 BatA protein | [41] |
| PIV5-Tb | PIV5 expressing Ag85B protein of M. tuberculosis | [40] |
Cells and culture conditions for work with PIV5 viruses
BHK21 cells (CCL-10, ATCC) were cultured in DMEM containing Tryptose Phosphate Broth (ThermoFisher Scientific, 10% vol/vol), fetal bovine serum (FBS, 5% vol/vol), penicillin (100 IU/mL), and streptomycin (100 ug/mL). MDBK-A cells (USDA) were grown in DMEM supplemented with 10% FBS and the concentration of penicillin/streptomycin listed above. All cultures were maintained at 37°C with 5% CO2.
Bacterial recombinant DNA methodologies
Standard molecular biology techniques were performed as described elsewhere [36]. Genomic DNA was obtained from Burkholderia strains with the Easy-DNA gDNA purification kit (ThermoFisher Scientific). The QIAprep Spin Miniprep kit (Qiagen) was used to isolate plasmid DNA. PCR was carried out with the FailSafe PCR System (epicenter/Lucigen) according to the manufacturer’s recommendations. DNA fragments were cloned into plasmids using T4 DNA ligase and restriction endonucleases purchased from New England Biolabs Inc. The E. coli strains EPI300 and EC100D pir+ were used to propagate plasmids.
A DNA fragment of 812 nucleotides (nt) containing the B. mallei ATCC 23344 pal gene was synthesized with unique 5ʹ-EcoRI and 3ʹ-NcoI restriction sites for directional cloning (GenScript custom gene synthesis services). The DNA fragment was cloned into the corresponding sites of vector pBHR1 yielding plasmid pPalBm. A larger DNA fragment of 1,332 nt (with additional flanking sequences upstream and downstream of the pal gene) was also synthesized and cloned into pACYC184 in a similar manner, producing plasmid pACYCPalBm, and a 0.4 kb zeocin resistance marker from plasmid pEM7/ZEO was inserted into a PstI site near the middle of the pal ORF. The resulting construct, pACYPalBmZEO, was digested with DraI and Bsu36I and a 2.2 kb DNA fragment containing the pal ORF disrupted with the zeocin cassette was purified using the High Pure PCR product purification kit (Roche Life Sciences), treated with the End-It DNA end repair kit (epicenter/Lucigen), and cloned into the EcoRV site of plasmid pKAS46, producing construct pKASPalBmZEO.
A PCR product encoding amino acids 22 to 170 of the pal ORF was amplified from genomic DNA of B. mallei ATCC 23344 using the oligonucleotides primers P1 (5ʹ-CTA GCT AGC AAG TCG GGC GTG AAG CT-3ʹ)[NheI site underlined] and P2 (5ʹ-TTA ATT AAA GTT ACT GTT GAT AGA CGA-3ʹ)[PacI site underlined]. The amplicon was purified, digested with NheI and PacI, and cloned in the protein expression plasmid pETcoco-1. This approach created the construct pHisPalBm, which contains the pal gene product fused to an N-terminal histidine tag (His-tag). A similar strategy was used to clone a PCR product encoding amino acids 47 to 243 of the B. mallei ATCC 23344 lolC ORF into pETcoco-1, yielding plasmid pHisLolCBm; the primers P3 (5ʹ-CCC AAG CTT GTG CTG TCG GTG ATG AA-3ʹ)[HindIII site underlined] and P4(5-CCC TTA ATT AAA GCT CGC GCG CAA CC-3ʹ)[PacI site underlined] were used to generate the amplicon containing the lolC gene fragment.
Electroporation was used to introduce plasmids into E. coli strains. The plasmids pBHR1∆Dra, pPalBm, and pKASPalBmZEO were introduced into B. mallei via conjugative transfer using the E. coli strain S17, as previously outlined [37,38]. The plasmids pHisPalBm and pHisLolCBm were sequenced to verify that the cloned DNA did not contain mutations that would result in amino acid substitutions.
Construction of B. mallei ATCC 23344 pal mutant strain
After the transfer of plasmid pKASPalBmZEO into B. mallei ATCC 23344, Polymyxin B resistant colonies were selected for resistance to zeocin and sensitivity to kanamycin. These colonies were then tested by PCR with primers P1 and P2, which produced amplicons of 0.5 kb in WT B. mallei ATCC 23344 and 0.9 kb in the B. mallei pal KO mutant (data not shown). This 0.4-kb difference in size was consistent with the aforementioned insertion of a zeocin resistance marker into a PstI site near the middle of the pal gene and confirmed allelic exchange in the genome of the mutant.
After the transfer of plasmids pBHR1∆Dra and pPalBm into the B. mallei pal KO mutant strain, Polymyxin B resistant colonies were selected for resistance to zeocin and kanamycin. Plasmid DNA was purified from these colonies and tested with restriction endonucleases to authenticate the constructs (data not shown).
Construction of PIV5 producing the B. mallei Pal protein
A gene fragment encoding amino acids 22–170 of the B. mallei ATCC 23344 Pal protein was synthesized with codon usage optimized for human cells (GenScript custom gene synthesis services). The DNA fragment was cloned between the SH and HN genes of PIV5 in the plasmid ZL185, which contains the entire genome of the virus. The resulting construct, PIV5-PalBm, was rescued and confirmed by RT-PCR sequencing as described previously [39]. PIV5 viruses expressing Mycobacterium tuberculosis protein Ag85B (PIV5-Tb) [40] and the B. mallei ATCC 23344 autotransporter BatA (PIV5-BatA) [41] were used as negative and protection benchmark controls in vaccination studies, respectively. WT PIV5, PIV5-PalBm, PIV5-Tb, and PIV5-BatA viruses were propagated in MDBK cells as reported elsewhere [39].
Growth curves and plaque assay
Six-well plates seeded with MDBK cells were infected in triplicate with WT PIV5 or PIV5-PalBm at a multiplicity of infection (MOI) of 0.01. One hundred μL samples of supernatant were then collected daily over 5 days. The virus titers in supernatant samples were determined by plaque assay as described previously using BHK21 cells [40].
Animal experiments
Female BALB/c mice (6–8 weeks of age) were obtained from Envigo. Challenge with bacteria was performed via the aerosol route as previously reported [42]. The infected animals were monitored daily for clinical symptoms and humane endpoints were strictly observed. Mice showing signs of intermediate to severe distress were euthanized per AVMA guidelines. At study endpoints, tissues were harvested from euthanized survivors, homogenized, diluted, and spread onto agar plates to determine bacterial burden.
Vaccination with PIV5 viruses was performed intranasally (IN). Mice were first anesthetized intraperitoneally with 250 mg/kg tribromoethanol (Millipore Sigma). The animals were then held in supine position and 5–10 uL droplets of PIV5 virus stock were delivered to the nostrils; a dose of 107 PFU in a final volume of 40 uL was administered. Six weeks later, mice were challenged with 8,000 CFU of B. mallei ATCC 23344 (10 LD50) via the aerosol route using a Microsprayer device as previously described by our group [42]. The controls in these experiments consisted of age- and weight-matched animals that were vaccinated IN with PBS.
Antigen preparation and analysis
Whole cell lysates were prepared from plate-grown bacteria suspended in 5 mL PBS to a concentration of 1 × 109 CFU per mL. Bacteria were pelleted by centrifugation, washed once with PBS, resuspended in 0.5 mL Bugbuster HT Protein Extraction Reagent (Millipore Sigma) supplemented with 1 uL/mL of rLysozyme Solution (Millipore Sigma), and incubated for 30 min at 65°C. Western blot analyses were carried out as previously published [19,43,44]. The E. coli strain TUNER containing plasmids pHisPalBm and pHisLolCBm was used to produce His-tagged PalBm and LolCBm proteins, respectively. Protein expression was induced by the addition of 1 mM isopropyl-β-D-thiogalactopyranoside to broth cultures and incubating for 5 hours. Following this, bacteria were centrifuged and treated with Bugbuster HT Protein Extraction Reagent containing 1 uL/mL of rLysozyme Solution. Both His-tagged PalBm and LolCBm proteins were soluble and purified with a His-Bind Purification kit (Millipore Sigma). Protein concentrations were determined with a BCA Protein assay kit (ThermoFisher Scientific). For ELISA, Immulon 2HB plates (ThermoFisher Scientific) were coated with antigen preparations or paraformaldehyde-inactivated B. mallei cells and antibody reactivity was measured as previously outlined [19,43].
To investigate protein expression in cells infected with PIV5 viruses, monolayers of MDBK cells were first infected with PIV5-PalBm and WT PIV5 (MOI of 10). After a 24 hr incubation period, cells were lysed with 1X Laemmli Sample Buffer (Bio-Rad) in PBS with 2-mercaptoethanol and heated at 95°C for 5 min. Samples were then resolved on a 4–20% gradient acrylamide gel by SDS-PAGE and transferred to an Amersham Hybond LFP PVDF membrane (GE Healthcare Life Sciences); purified His-tagged PalBm protein was included as a control in these experiments. Upon protein transfer, the PVDF membrane was incubated with mouse anti-PalBm polyclonal antibodies followed by incubation with Cy3-conjugated goat anti-mouse IgG (Jackson ImmunoResearch). A duplicate PVDF membrane was also probed with a mouse antibody against the PIV5 gene product P/V (Pk) antibody. The reactivity of antibodies with protein bands was visualized using a Typhoon FLA 7000 system (GE Healthcare Life Sciences).
Antibodies
Immune serum containing antibodies against PalBm and LolCBm was produced by immunizing mice with His-tagged PalBm and His-tagged LolCBm mixed with adjuvant, respectively. Mice were given three vaccine doses subcutaneously at 14 days interval. Each dose consisted of 25 ug purified protein mixed in a ratio of 1:1 with Freund’s Adjuvant (Millipore Sigma; complete for prime, incomplete for boost). Immune serum was collected via the tail bleed procedure, pooled, and used in Western blot analyses. The monoclonal antibodies PalBm MAb#1 and PalBm MAb#2 were obtained by fusing spleen cells (from a vaccinated mouse) with Sp2/mIL6 cells (ATCC CRL 2016) as previously reported [19,43]. The supernatant from cultures of cells secreting the antibodies were used in Western blot analyses.
Macrophage killing assays
The mouse cell line J774A.1 (ATCC TIB-67) was cultured and infected with bacteria as previously outlined by our group [19,37,43,45]. The antibiotic streptomycin was used at a concentration of 50 ug/mL to kill extracellular bacteria.
Serum killing assays
Plate-grown organisms were used in all experiments. Bacterial suspensions were prepared in buffer supplemented with 5 mM MgCl2 and 1.5 mM CaCl2, mixed with normal human serum at a final concentration of 25% (vol/vol), and the mixtures were incubated at 37ºC. At time 0, 30, 60, and 120 min, duplicate 10 uL aliquots were removed and plated onto agar medium to determine the number of viable bacteria, as previously reported [46].
Data analysis
The Kaplan-Meier method was used to plot survival data and the Log-rank Mantel-Cox and Gehan-Breslow-Wilcoxon tests were used to perform statistical analyses. The student’s t and Mann–Whitney tests were used to analyze ELISA, bacterial burden data, and cell culture assay results. The two-stage linear step-up multiple t test procedure of Benjamini, Krieger, and Yekutieli was used to analyze the data from macrophage and serum killing assays. These analyses were performed using the GraphPad Prism software and P values < 0.05 are reported as statistically significant. The method of Reed and Muench [47] was used to calculate LD50 values of B. mallei WT and recombinant strains.
Research compliance
All work with live B. mallei was performed in BSL3/ABSL3 laboratory space with approvals from the University of Georgia’s Institutional Biosafety and Animal Care and Use Committees (IBC and IACUC, respectively), and in compliance with the rules and regulations of the U.S. Federal Select Agent Program.
Results
In silico characterization of the B. mallei pal gene
Comparative sequence analyses identified the ortholog of the B. pseudomallei K96243 pal gene on chromosome I of the B. mallei ATCC 23344 genome (locus tag BMA2082). The open reading frame (ORF) encompasses 513 nucleotides (nt) and encodes a lipoprotein of 170 amino acids (aa) with a molecular mass of 18, 762. Analyses using the SignalP 5.0 and LipoP 1.0 servers detected a leader peptide at the N-terminus of the B. mallei Pal protein (PalBm) with a signal peptidase II cleavage site between residues 20 and 21 (i.e. GALAA20 | C21KSGV), which would provide a free cysteine residue for lipid modification of the mature protein.
Analysis with NCBI CDD indicated that PalBm belongs to the OmpA_C-like Superfamily (domain ID cl28145; E value of 4.39e-64), which comprises peptidoglycan-associated lipoproteins of the Tol-Pal system. Consistent with this finding, orthologs of the tolQ (BMA2078), tolR (BMA2079), tolA (BMA2080), and tolB (BMA2081) genes were identified upstream of the pal ORF in the B. mallei ATCC 23344 genome. This particular arrangement of the genes encoding Tol-Pal system components (i.e. tolQRABpal) is conserved in most sequenced genomes of Gram-negative bacteria [32].
NCBI BLAST searches identified pal orthologs in the genomes of all B. mallei (n = 51) and B. pseudomallei (n > 1, 000) strains that are available through the service. The proteins encoded by these pal genes were all identical. An ortholog of pal was also identified in the genome of the closely related organism Burkholderia thailandensis, with the gene product showing 99% identity. The Pal protein of other Burkholderia species, including cenocepacia, cepacia, and multivorans, exhibited 84% identity with PalBm.
In vitro characterization of the B. mallei pal gene
To study the function of the pal gene, we constructed a mutant strain of B. mallei ATCC 23344. Mutagenesis was achieved via genomic recombination of a DNA fragment containing the pal ORF disrupted with a zeocin resistance cassette. For complementation purposes, the plasmids pBHR1ΔDra (vector control) and pPalBm (specifies constitutive expression of PalBm) were introduced in the pal knockout (KO) mutant.
To examine expression of PalBm, whole cell lysates from wild-type (WT) and recombinant bacteria were analyzed by Western blotting with the monoclonal antibody PalBm MAb#2. As anticipated, no reactivity was observed with the mutant carrying the control plasmid pBHR1ΔDra (Figure 1(a), lane 2). We found that the monoclonal antibody does not react with the lysate from WT B. mallei ATCC 23344 (Figure 1(a), lane 1); PalBm-specific polyclonal antisera and a second monoclonal antibody (PalBm MAb#1) also failed to show reactivity (data not shown). Western blotting with polyclonal antibodies against the B. mallei LolC protein was used to demonstrate that equivalent amounts of lysates were analyzed for all strains (Figure 1(b)). Based on these results, we concluded that PalBm is not produced at detectable levels by WT organisms cultured under standard laboratory conditions. As shown in lane 3 of Figure 1(a), introduction of plasmid pPalBm in the pal KO mutant strain results in the production of an 18 kDa protein reacting with antibody PalBm MAb#2, which is consistent with the predicted molecular mass of the B. mallei pal gene product.
Figure 1.
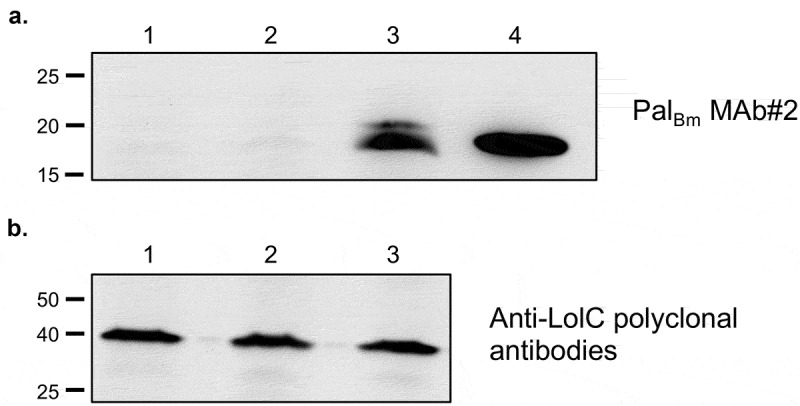
Western blot analysis of B. mallei WT and recombinant strains. Whole cell lysates were prepared from WT B. mallei ATCC 23344 bacteria (lane 1) and the pal KO mutant strain carrying the plasmids pBHR1∆Dra (lane 2) and pPalBm (lane 3) and analyzed by Western blotting with the monoclonal antibody PalBm MAb#2 (panel A) and polyclonal antibodies against the LolC protein (panel B, used as loading control to demonstrate that equivalent amounts of proteins were analyzed). Molecular mass markers are shown to the left in kilodaltons. Lane 4 in panel A corresponds to 5 ug of purified of His-tagged PalBm protein (used as positive control to demonstrate reactivity and specificity of PalBm MAb#2).
Mutations in the Tol-Pal system of Gram-negative bacteria typically result in disruption of cell envelope integrity and hypersensitivity to osmotic stress, antimicrobial peptides, detergents, and membrane-acting antibiotics [32]. With this in mind, we assessed the susceptibility of the B. mallei pal KO mutant to high concentration of potassium chloride (osmotic stress) and Polymyxin B (antibiotic). The latter consists of a cationic polypeptide with an attached fatty acid tail and initially binds to negatively charged LPS, allowing the hydrophobic tail to interact with bacterial membranes and destabilize them [48]. Suspensions of B. mallei WT and recombinant organisms were serially diluted and spotted onto agar plates supplemented with 100 mM potassium chloride (Figure 2(b)) and 20 ug/mL Polymyxin B (Figure 2(c)). Each dilution was also spotted onto medium without additive to verify that the pal mutation does not cause a global growth defect (Figure 2(a)). We found that the pal KO mutant exhibits increased sensitivity to both osmotic stress and Polymyxin B compared to WT strain ATCC 23344, as evidenced by lack of visible growth when 102 and 103 CFU of bacteria carrying plasmid pBHR1ΔDra were spotted onto agar plates. Consistent with these results, the calculated minimum inhibitory concentration of Polymyxin B for the pal KO mutant harboring the control plasmid is approximately 10-fold lower than for WT organisms (Figure 3(a,b), respectively). Introduction of plasmid pPalBm in the mutant, and concomitant production of the pal gene product, restored susceptibility of the pal KO strain to osmotic stress (Figure 2(b)) and Polymyxin B (Figures 2(c) and 3(c)) to WT levels.
Figure 2.
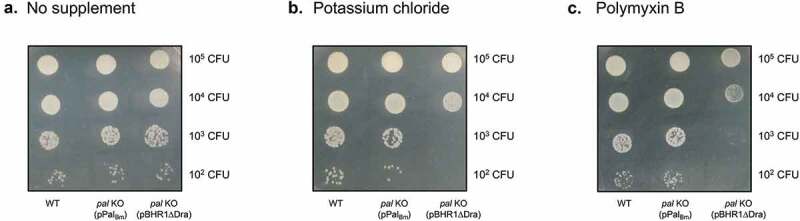
Effect of osmotic and antibiotic stresses on the growth of B. mallei WT and recombinant strains. Plate-grown organisms were suspended in PBS to a concentration of 1 × 109 CFU/mL. Ten-fold serial dilutions of bacterial suspensions were then spotted onto agar plates and incubated at 37ºC for 40 hours. (a) Medium without supplement. (b) Medium supplemented with 100 mM potassium chloride for osmotic stress. (c) Medium supplemented with 20 ug/mL of the antibiotic Polymyxin B. The number of CFU spotted on the agar plates is shown to the right of each panel. Images are representative of 3 independent experiments.
Figure 3.
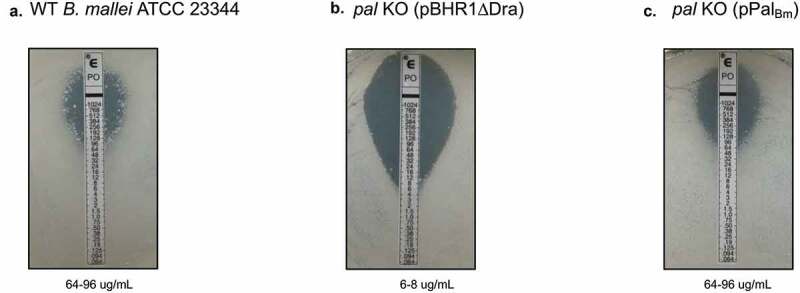
Polymyxin B sensitivities of B. mallei WT and recombinant strains. Plate-grown organisms were suspended in PBS to a concentration of 1 × 109 CFU/mL. Portions of bacterial suspensions (108 CFU) were then spread onto agar plates and E strips containing a gradient of Polymyxin B concentrations (0.064–1024 ug/mL, Biomerieux) were applied onto the inoculated medium. After incubation at 37ºC for 40 hours, minimal inhibitory concentration (MIC) values were determined by reading the intersection of the test strip with the lower part of the ellipse-shaped area of bacterial growth inhibition. (a) WT B. mallei ATCC 23344. (b) pal KO mutant carrying vector control pBHR1∆Dra. (c) pal KO mutant carrying plasmid pPalBm. Images are representative of 3 independent experiments. MIC values are shown at the bottom of each panel.
The ability to thrive within host cells is an important pathogenicity trait of B. mallei [13,14,49,50]. Thus, we determined the intracellular fitness of the pal KO mutant using J774 murine macrophage cells. These experiments established that the pal mutation substantially reduced fitness over a period of 7 hours (Figure 4(a)). By dividing the number of viable intracellular organisms at the experimental endpoint (CFU at 10 hours) by the number of phagocytized bacteria (CFU at 3 hours), fitness indexes of 1.38 and 0.08 were calculated for the WT strain and the pal KO mutant carrying control plasmid pBHR1∆Dra, respectively. To complement these assays, we compared the growth of the strains in broth medium and found that they replicated at similar rates (Figure 4(b)). These data indicate that the intracellular fitness phenotype of the pal KO mutant is not the result of a generalized growth defect. Introduction of plasmid pPalBm in the mutant and constitutive production of the PalBm protein restored intracellular fitness to WT levels (Figure 4(a), calculated fitness index of 0.97). Taken together, these data demonstrate a role for PalBm in the ability of B. mallei to survive and replicate inside host cells.
Figure 4.
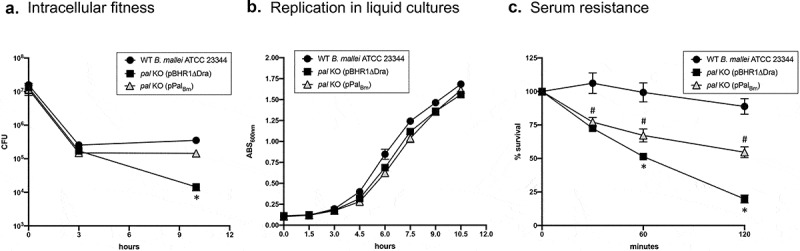
Serum resistance, intracellular fitness, and in vitro replication rate in liquid cultures of B. mallei WT and recombinant strains. (a) Plate-grown bacteria were suspended in PBS and used to infect 3 wells of duplicate tissue culture plates seeded with murine J774 macrophages (multiplicity of infection of 10:1). The infected cells were incubated for 1 hour at 37ºC to allow phagocytosis of the bacteria, washed, and treated with antibiotic for 2 hours to kill extracellular bacteria. Cells from one tissue culture plate were lysed, diluted, and plated onto agar medium to determine the number of bacteria phagocytized. The other tissue culture plate was incubated for an additional 7 hours, after which the cells were washed, lysed, diluted, and spread onto agar plates to calculate the number of intracellular organisms. The results are expressed as the mean CFU per well. The assays were performed on 3 separate occasions. The graph shows cumulative results. The error bars correspond to standard errors of the mean. The asterisk indicates that the reduction in the number of intracellular pal KO bacteria carrying the vector pBHR1∆Dra at 10 hours post-infection, compared to WT B. mallei and the pal KO mutant carrying plasmid pPalBm, is statistically significant. The reduction in the number of intracellular pal KO bacteria carrying plasmid pPalBm at 10 hours post-infection, compared to WT B. mallei, was not statistically significant. (b) Plate-grown bacteria were suspended in broth to an optical density at wavelength 600 nm (ABS600 nm) of 0.1. Following this, suspended bacteria were incubated at 37ºC with shaking (200-rpm) and the optical density of cultures was measured at the indicated time intervals. Strains were tested on at least 2 separate occasions. The graph shows cumulative results. The error bars correspond to standard errors of the mean. (c) Plate-grown bacteria were suspended in PBS supplemented with Mg+2 and Ca+2 and aliquots containing 103 CFU were placed in duplicate tubes. Following this, normal human serum was added to the bacteria at a final concentration of 25% and the mixtures were incubated at 37ºC. Portions were removed at the indicated time points and plated onto agar medium to determine the number of viable organisms. The results are expressed as the mean percentage of the original inoculum (time 0 min) remaining at each time point. The assays were performed on 4 separate occasions. The graph shows cumulative results. The error bars correspond to standard errors of the mean. The asterisk indicates that the reduction in the number of pal KO bacteria carrying the vector pBHR1∆Dra and surviving exposure to serum, compared to WT B. mallei and the pal KO mutant carrying plasmid pPalBm, is statistically significant. The hashtag indicates that the reduction in the number of pal KO bacteria carrying plasmid pPalBm and surviving exposure to serum, compared to WT B. mallei, is statistically significant.
Serum resistance is another important pathogenicity trait of B. mallei, specifically resistance to complement membrane attack complex deposition and cell lysis [51,52]. Given the role of Tol-Pal system components in maintaining the integrity of the bacterial cell envelope and the increased sensitivity of the B. mallei pal KO mutant to osmotic stress and the membrane-acting antibiotic Polymyxin B (Figure 2), we compared the susceptibilities of WT and recombinant strains to normal human serum in vitro. As shown in Figure 4(c), nearly 90% of WT organisms survived exposure to serum for 120 min. In contrast, only 20% of pal KO mutant bacteria carrying the vector control pBHR1∆Dra remained viable. The increased sensitivity of the mutant to complement-mediated lysis was detected as early as 30 min upon exposure to serum (72% survival compared to 106% for WT strain ATCC 23344). Complementation of the pal mutation with plasmid pPalBm partially restored serum resistance. No statistically significant difference was observed between survival of the mutant carrying plasmids pBHR1∆Dra and pPalBm after 30 min incubation with serum (72–77% survival), but bacteria constitutively producing PalBm show increased viability after 60 min (67% survival compared to 50% for the mutant carrying the control plasmid) and at the experimental endpoint (55% survival compared to 20% for control organisms). These data are consistent with the pal mutation causing a defect in the integrity of the B. mallei cell envelope, which in turn sensitizes the organism to complement-mediated lysis.
In vivo characterization of the B. mallei pal gene
Based on the results of in vitro intracellular fitness and serum killing assays, we hypothesized that the pal gene contributes to pathogenesis in vivo. To test this, we calculated the median lethal dose (LD50) of the pal KO mutant strain in a mouse aerosol infection model. At study endpoints, we collected tissues from survivors and determined bacterial loads as an indicator of in vivo fitness. Compared to WT organisms, the calculated LD50 value for pal KO bacteria carrying the control plasmid pBHR1∆Dra was >5,000-fold higher (Figures 5(a) and 6(a)). No B. mallei organisms were cultured from the lungs, spleen or liver of any of the mice inoculated with the mutant, even those challenged with a high dose of 1.9 × 106 CFU (Panels B, C, and D in Figures 5 and 6). In contrast, the lungs and spleen of all mice inoculated with as few as 17 CFU of the parent strain ATCC 23344 were colonized with B. mallei (Figure 5(b,d)). Introduction of the plasmid pPalBm in the mutant and constitutive production of the PalBm protein restored virulence and in vivo fitness, but not entirely. The LD50 of the complemented pal KO strain was found to be approximately 30-fold higher that WT B. mallei, and target tissues of many (but not all) survivors challenged with low doses of 15 and 150 CFU were colonized (Figures 5 and 6). Taken together, the data from the two independent LD50 experiments demonstrate that the pal gene product contributes to the virulence of B. mallei.
Figure 5.
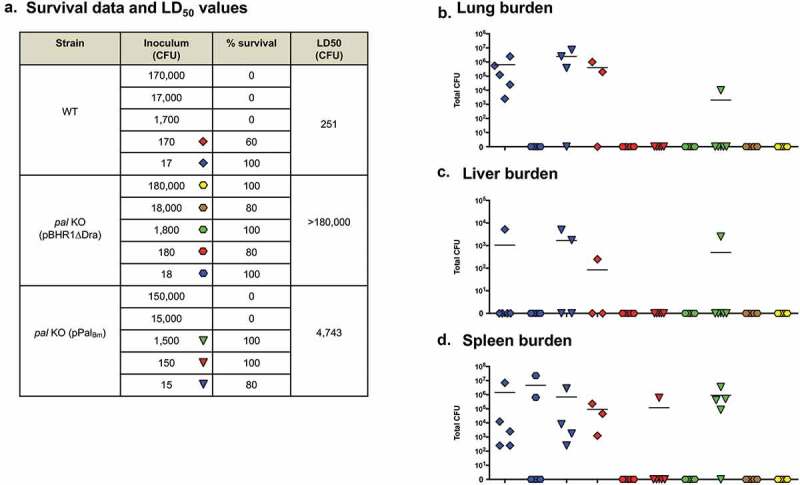
Median lethal dose comparison for B. mallei WT and recombinant strains. BALB/c mice were inoculated with a Microsprayer device to aerosolize the indicated numbers of bacterial CFU directly into the lungs (n = 5 mice/dose). The animals were then monitored daily for clinical signs of illness and morbidity. (a) Survival data and calculated LD50 values. (b–d) Tissues were collected from mice that survived challenge (day 22), homogenized, diluted, and spread on agar plates to determine bacterial loads. The symbols represent data from individual animals; horizontal lines represent the mean total number of CFU for each group.
Figure 6.
Median lethal dose comparison for B. mallei WT and recombinant strains (repeat experiment). BALB/c mice were inoculated with a Microsprayer device to aerosolize the indicated numbers of bacterial CFU directly into the lungs (n = 5 mice/dose). The animals were then monitored daily for clinical signs of illness and morbidity. (a) Survival data and calculated LD50 values. (b–d) Tissues were collected from mice that survived challenge (day 27), homogenized, diluted, and spread on agar plates to determine bacterial loads. The symbols represent data from individual animals; horizontal lines represent the mean total number of CFU for each group.
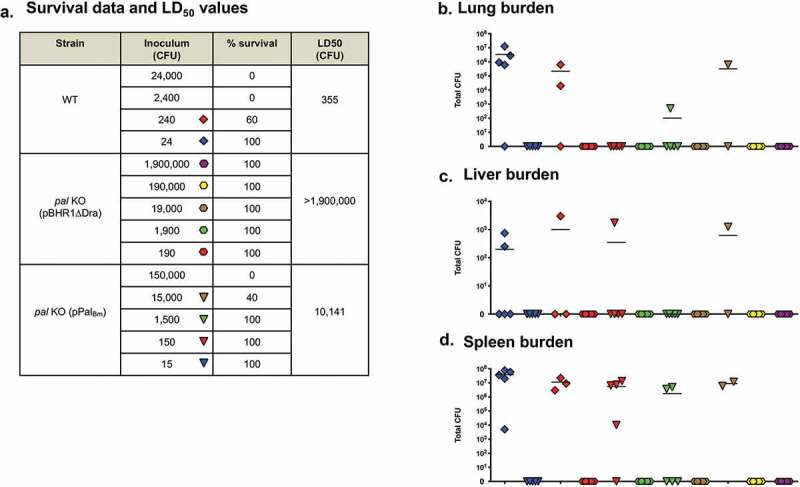
To gain insight into the immune response to WT and recombinant strains during infection, we also collected serum from survivors at study end points and measured immunoglobulin titers by ELISA using whole bacteria as well as purified His-tagged PalBm. As shown in Figure 7(a), challenge with the mutant carrying the vector control pBHR1∆Dra resulted in low titers against whole bacteria (<3,200) compared to titers measured in the serum of mice that survived infection with WT B. mallei and pal KO organisms harboring plasmid pPalBm. These results are consistent with the considerably reduced virulence and in vivo fitness of the mutant, and suggest rapid clearance of bacteria lacking expression of PalBm. In accordance with Western blot data showing different production levels of the pal gene product (Figure 1(a)), serum samples from mice challenged with the complemented mutant were found to contain higher antibody titers against the PalBm protein than the serum of survivors infected with WT B. mallei (Figure 7(b)). As expected, the serum of mice inoculated with pal KO bacteria carrying plasmid pBHR1∆Dra did not show detectable titers of PalBm-specific antibodies. Collectively, these data show that B. mallei produces Pal in vivo during infection, which in turn elicits production of PalBm-specific antibodies. The data also suggest that the extent of the antibody response against PalBm correlates with the amount of protein produced by bacteria.
Figure 7.
ELISA using serum from mice challenged with B. mallei WT and recombinant strains. Serum samples were serially diluted and placed in duplicate wells of plates coated with whole paraformaldehyde-fixed B. mallei ATCC 23344 bacteria (panel A) and with purified His-tagged PalBm protein (panel B). Alkaline-phosphatase-conjugated goat anti-IgG mouse antibodies (light and heavy chains) were used for detection. Serum samples were tested in duplicate on at least 2 separate occasions. The results are expressed as the mean (plus standard error) reciprocal endpoint titers. Naïve serum was used to establish background reactivity, and the endpoint titers correspond to the highest immune serum dilutions giving ELISA values greater than the mean value of naïve serum plus 3 standard deviations. The labels on the x-axis show the source of immune serum samples (collected from survivors in experiments to determine the LD50 of B. mallei WT and recombinant strains, see Figures 5 and 6). The asterisks indicate that the increase in serum titers, compared to samples from mice infected with pal KO (pBHR1∆Dra) bacteria, is statistically significant. The hashtags indicate that the increase in serum titers, compared to samples from mice infected with WT bacteria, is statistically significant.
To evaluate the usefulness of the mutant as a live attenuated vaccine, groups of mice were inoculated with the pal KO strain and, 4 weeks later, were infected with ~10LD50 of B. mallei ATCC 23344 organisms. The results of these experiments are outlined in Table 2 and show that vaccinating mice with the pal KO mutant strain does not protect against lethal challenge with WT bacteria.
Table 2.
Vaccine studies to evaluate protection by the pal KO mutant strain.
| Treatment | # mice challenged | Survival (10 days post challenge) |
|---|---|---|
| pal KO vaccination (dose = 190 CFU) | 4 | 0/4 |
| pal KO vaccination (dose = 1,900 CFU) | 5 | 0/5 |
| pal KO vaccination (dose = 19,000 CFU) | 5 | 0/5 |
| pal KO vaccination (dose = 190,000 CFU) | 5 | 0/5 |
| pal KO vaccination (dose = 1,900,000 CFU) | 5 | 0/5 |
| PBS vaccination | 5 | 0/5 |
BALB/c mice were inoculated with the indicated dose of the pal KO mutant strain using a Microsprayer device. Thirty days later, the animals were challenged with 6,000 CFU of B. mallei ATCC 23344 using the Microsprayer. Age- and weight-matched mice vaccinated with PBS using a were used as controls.
Vaccination with a virus vector expressing PalBm protects against challenge with B. mallei
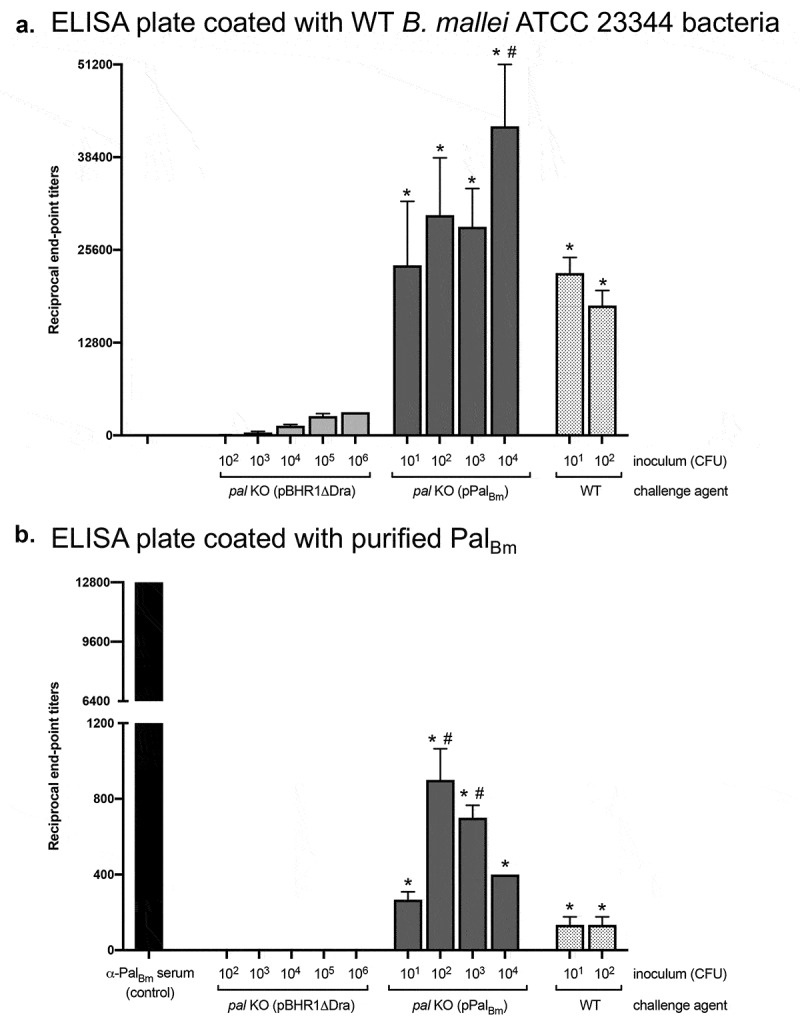
Based on the aforementioned in vitro and in vivo data, we hypothesized that delivering PalBm with a virus vaccine vector system would elicit excellent protective immunity. This premise is supported by our studies showing that vaccination with Parainfluenza Virus 5 (PIV5) expressing the conserved Burkholderia autotransporter protein BatA protected 74% and 60% of mice against death upon infection with B. mallei and B. pseudomallei, respectively [41]. Therefore, a gene fragment corresponding to amino acids 22–170 of PalBm was cloned in PIV5 using a well-established reverse genetics approach developed by our group (Figure 8(a)) [39–41,53]. To verify that the recombinant construct drives expression of the PalBm protein, lysates from MDBK cells infected with PIV5-PalBm and WT PIV5 viruses were tested by Western blotting. As shown in Figure 8(b), PalBm-specific antibodies did not react with the control WT PIV5 lysate but reacted with a protein of 18-kDa in cells infected with PIV5-PalBm. Purified His-tagged PalBm protein was used as positive control. An antibody against the PIV5 P/V gene product was also used as loading control to show that comparable amounts of the lysates were analyzed. The replication rates of the viruses were compared in a multi-cycle growth curve experiment over a period of 5 days and found to be equivalent (Figure 8(c)), with PIV5-PalBm reaching similar titers as WT PIV5. Hence, PalBm expression does not reduce in vitro infectivity or fitness of PIV5. The genome of PIV5-PalBm was also sequenced to verify that the pal gene fragment was properly cloned in its intended location (data not shown).
Figure 8.
Characterization of recombinant PIV5 virus expressing PalBm. (a) Schematic of PIV5-PalBm vaccine construct. NP, nucleoprotein; V, V protein; P, phosphoprotein; M, matrix protein; F, fusion protein; SH, small hydrophobic protein; HN, hemagglutinin-neuraminidase protein; L, RNA-dependent RNA polymerase; PalBm, B. mallei Pal protein residues 22–170. (b) Equivalent protein amounts of lysates from cells infected with PIV5-PalBm and PIV5 viruses were analyzed by Western blotting with mouse PalBm-specific polyclonal and PIV5-P/V antibodies. Lane 1 = mock infected cells; Lane 2 = purified His-tagged PalBm; Lane 3 = cells infected with WT PIV5 virus; Lane 4 = cells infected with PIV5-PalBm virus (c) MDBK cells were infected in triplicate with PIV5-PalBm and PIV5 viruses at an MOI of 0.01. Aliquots of supernatant from the infected cell cultures were collected at 24-hour intervals for a period of 5 days post-infection and titers were determined by plaque assays using BHK21 cells. The results are expressed as the mean (± standard error of the mean) log10 PFU/mL. There was no statistically significant difference between viruses.
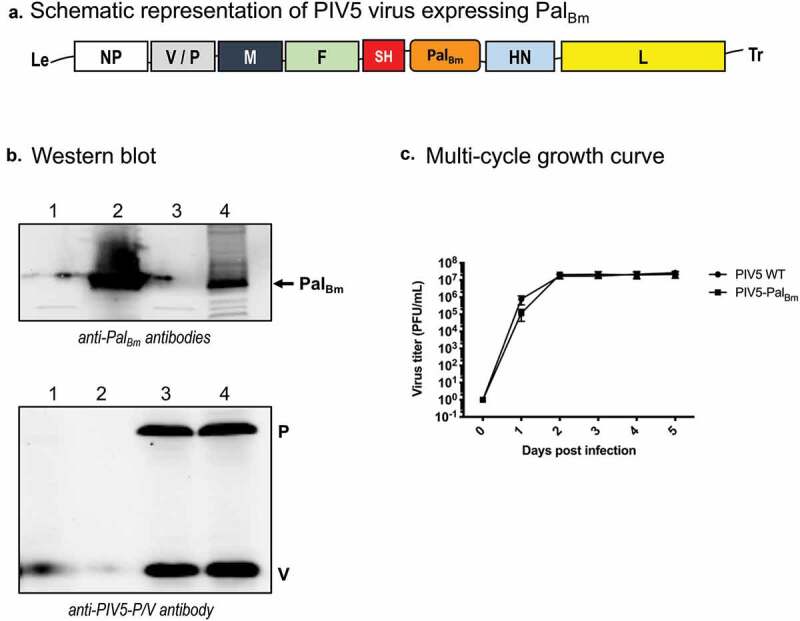
To investigate whether delivering PalBm with a virus vector system elicits protection, mice were vaccinated intranasally (IN) with PIV5-PalBm and, six weeks later, infected via the aerosol route with B. mallei ATCC 23344. Control groups consisted of age- and weight-matched mice treated with PBS, animals immunized with the aforementioned efficacy benchmark PIV5-BatA, and mice vaccinated with a PIV5-Tb construct expressing Mycobacterium tuberculosis protein Ag85b (PIV5 vector control) [40]. As shown in Figure 9(a,b), all PBS control mice reached humane endpoints within 5 days post-challenge. Likewise, animals vaccinated with the control virus PIV5-Tb rapidly succumbed to infection and showed negligible survival. In contrast, immunization with PIV5-PalBm protected 90% and 80% of mice against death during acute and chronic infection, respectively, which was comparable to the survival rates observed in animals vaccinated with the efficacy benchmark control virus PIV5-BatA. At study endpoints, we determined bacterial loads in target organs of survivors and discovered that no B. mallei was present in the liver of n = 7 out of 8 mice immunized with PIV5-PalBm whereas all animals given the PIV5-Tb and PIV5-BatA vaccines were colonized with B. mallei (Figure 9(d)). Three mice from each cohort vaccinated with PIV5-BatA and PIV5-PalBm had no bacteria in the lungs and the sole survivor immunized with the control PIV5-Tb vaccine had also cleared the agent (Figure 9(c)). All mice were colonized in the spleen (Figure 9(e)). Collectively, the data show that a single dose of PIV5-PalBm provides excellent survival against B. mallei lethal aerosol challenge and promotes bacterial clearance from target organs, in particular the liver.
Figure 9.
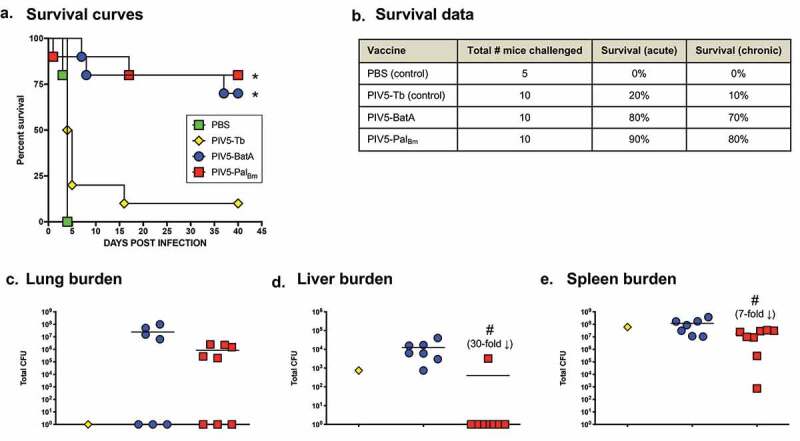
Vaccination with PIV5-PalBm provides protection against challenge with a lethal dose of WT B. mallei. BALB/c mice vaccinated intranasally with PIV5 viruses were challenged with 10 LD50 of B. mallei ATCC 23344 using a Microsprayer device and monitored daily for clinical signs of illness and morbidity. (a) Kaplan-Meier survival curves. (b) Survival data during the acute (days 1 through 10 post-challenge) and chronic (days 11 through 40 post-challenge) phases of infection. (c–e) At study end-points, tissues collected from survivors were homogenized, diluted, and spread on agar plates to determine bacterial loads. Symbols represent individual animals; horizontal lines show the mean total CFU for each group. The asterisks indicate that the survival curves were found to be significantly different from mice vaccinated with PBS and the control vaccine PIV5-Tb. The hashtags indicate that the decrease in bacterial burden, compared to mice vaccinated with PIV5-BatA, is statistically significant. Although a 30-fold decrease in lung bacterial burden was observed between mice vaccinated with PIV5-PalBm and PIV5-BatA, this decrease was not statistically significant (panel C).
Discussion
Published work by other groups and the data herein underscore the value of the Pal protein for developing countermeasures against highly pathogenic Burkholderia species. The pal gene is present in the genomes of all B. mallei and B. pseudomallei isolates sequenced to date and the encoded proteins are identical. We showed that PalBm plays a role in B. mallei intracellular fitness and serum resistance (Figure 4), and is expressed in vivo as evidenced by the titer of PalBm-specific antibodies in the serum of mice infected with the organism (Figure 7(b)). Moreover, we showed that a B. mallei mutant lacking the protein is greatly attenuated in virulence and completely cleared from host tissues even at high challenge doses (Figures 5 and 6). Immune response against the Pal protein of B. pseudomallei (PalBp) has been linked to resolution of chronic and recurrent melioidosis in human patients [26]. Experimental subunit vaccines containing purified PalBp were also shown to provide partial protection against lethal intraperitoneal challenge with B. pseudomallei in mice [29,30], and our data indicate that delivering PalBm with a viral vaccine system elicits outstanding protection against aerosol exposure to B. mallei (Figure 9). Thus, Pal possesses many qualities of a strong candidate for devising medical intervention strategies and targeting the protein may interfere with the ability of B. mallei and B. pseudomallei to establish themselves in the host, persist, and cause infection.
We discovered that B. mallei ATCC 23344 does not produce detectable amounts of Pal when cultured under routine laboratory conditions. These results are consistent with published proteomics data for the organism. Specifically, Schell and colleagues analyzed outer membrane protein preparations from ATCC 23344 cells grown under multiple conditions and their data show that Pal (i.e. BMA2082) was present in very low abundance and only in some of the conditions tested [54]. A review of the literature indicated that Pal is produced at readily detectable levels by most organisms in which expression of the protein has been studied including E. coli [55], Haemophilus influenzae [56], Erwinia chrysanthemi [57], Pseudomonas aeruginosa [58], and Haemophilus ducreyi [59]. Hence, the pal gene appears to be more stringently regulated in B. mallei.
Despite low expression levels, PalBm significantly contributes to maintaining the integrity of the B. mallei cell envelope as illustrated by the hypersensitivity of the pal KO mutant to osmotic stress and the membrane-acting antibiotic Polymyxin B (Figures 2 and 3). The plasmid pPalBm, which specifies constitutive production of PalBm, restored susceptibility of the pal KO strain to osmotic stress and Polymyxin B to WT levels. The in vitro phenotypic characterization of WT and recombinant bacteria also revealed a connection between PalBm and the ability of B. mallei to thrive intracellularly and withstand complement-mediated killing. While the pPalBm construct restored intracellular fitness to parental levels, the serum resistance defect was partially complemented (Figure 4). Similar observations were previously made in a Klebsiella pneumoniae strain deleted for pal [60]. The mutant exhibited reduced protection from serum and neutrophil killing; the serum resistance defect was partially rescued by complementation with an intact copy of the K. pneumoniae pal gene and intracellular fitness was fully restored to WT levels. Likewise, a mutation in the gene encoding the Haemophilus influenzae Pal ortholog P6 protein was shown to result in increased sensitivity to normal human serum and complementation partly restored resistance [56]. Lack of full complementation of the serum resistance phenotype of the pal KO mutant is likely due to a gene dosage effect and overproduction of PalBm by the complemented strain (Figure 1(a)). The disproportionate amounts of PalBm in the cell envelope may have the unintended effect of destabilizing bacterial membranes and sensitizing the organism to complement-mediated lysis.
Several studies have highlighted a significant role for Pal in the pathogenesis of bacterial infection. For instance, the virulence of a pal deletion mutant of Burkholderia cenocepacia was reduced by 88-fold in a Galleria mellonella larvae model [61]. Deletion of the pal gene increased the LD50 of K. pneumoniae in a mouse model of intraperitoneal infection from less than 1 × 102 CFU for WT organisms to ~2 × 105 CFU [60]. An isogenic pal mutant strain of H. ducreyi was also found to be considerably attenuated in a human challenge model [59]. Our data demonstrate that a mutation in the pal gene of B. mallei ATCC 23344 is highly attenuating, as mice inoculated with 2, 500 LD50 all survived challenge and completely cleared the organism from target tissues (Figures 5 and 6). Introduction of the plasmid pPalBm in the pal KO mutant restored virulence, but not back to parental levels; the LD50 of the complemented strain was still approximately 30-fold higher than WT B. mallei. In light of our results showing that serum samples from the mice infected with complemented pal KO bacteria contain higher antibody titers against PalBm than the serum of survivors infected with WT B. mallei (Figure 7(b)), we propose that the ostensively incomplete rescuing of the virulence phenotype results from increased immune clearance via targeting of the PalBm protein overexpressed by the complemented mutant. Alternatively, partial complementation may be due to gene dosage effect. Our laboratory as well as other groups have reported similar difficulties studying membrane proteins and complementing in vivo virulence defects with plasmid-based systems [19,43,62,63]. Collectively, our data indicate that Pal contributes to the virulence of B. mallei, although its specific role is not clearly defined yet. We can not exclude the possibility that the intracellular fitness, serum resistance, and in vivo virulence phenotypes of the pal KO mutant are indirectly caused by a general defect in cell membrane integrity. Additional studies are ongoing to clarify the specific role of the pal gene product in these phenotypic traits.
The Pal proteins of several organisms have been shown to possess excellent vaccinogenic potential [32,64,65]. One of the best studied examples is the aforementioned P6 protein, which is considered a lead vaccine candidate for prevention of non-typeable H. influenzae infections in humans (acute otitis media in children, sinusitis, exacerbations in COPD patients, pneumonia). Subunit vaccines containing P6 induce protective immune responses in several animal models including an infant rat model of invasive infection [66,67], a rat pulmonary clearance model [68], and otitis media models in chinchillas and mice [69–71]. An analysis of antibody titers to P6 in children has indicated that immune responses to the protein correlate with protection from H. influenzae otitis media [72–74]. Moreover, T-cell responses to P6 in COPD patients are associated with protection from exacerbations caused by H. influenzae [75]. Consistent with these studies, the antibody response to the Pal protein of B. pseudomallei was shown to be 10-fold higher in plasma from human patients who had only one episode of melioidosis than those with recurrent bouts of disease [26]. Experimental subunit vaccines containing PalBp were also shown to provide 50% survival in mice challenged intraperitoneally with B. pseudomallei [29,30]. Our data complement and expand upon these findings by demonstrating that one dose of the PIV5 viral vaccine vector expressing PalBm affords excellent protection against death upon exposure to B. mallei lethal aerosol challenge.
The exact mechanism of protection elicited by the PIV5-PalBm vaccine is not clear at the moment. The analyses of serum and bronchoalveolar samples from immunized mice indicate little to no antibody titers against PalBm (data not shown). Based on these results and our published work using the PIV5 platform to develop bacterial vaccines for Mycobacterium tuberculosis [40] and highly pathogenic Burkholderia species [41], T-cell responses are likely the predominant effectors of protection in our model system. Future work should compare and contrast the kinetics, levels, and functionality of humoral as well as cellular responses stimulated by the PIV5-PalBm vaccine prior to and during infection, test vaccine efficacy against lethal aerosol challenge with B. pseudomallei, and investigate prime-boost vaccination approaches to bolster protective immunity and bacterial clearance from target organs. These studies will identify critical immune components associated with protection and guide efforts for the rational design of PIV5-based vaccines targeting PalBm and/or other established immunoprotective antigens such as BatA (see Figure 9) [41], with the goal of achieving sterilizing immunity and complete protection against acute and chronic infections by B. mallei and B. pseudomallei. Interestingly, the Pal protein of Burkholderia species cepacia, cenocepacia, and multivorans exhibit 84% sequence identity with PalBm. These bacteria form the Burkholderia cepacia complex (Bcc) and are important opportunistic pathogens causing infections in people with cystic fibrosis and for which the availability of effective countermeasures is a critical unmet need [76]. With this in mind, it may be possible to expand the use of the PIV5-PalBm vaccine to these organisms.
Funding Statement
This work was supported by award R01 AI117290 from the National Institutes of Health-National Institute of Allergy and Infectious Diseases (NIH-NIAID).
Disclosure statement
The authors have no potential conflict of interest to report.
References
- [1].Khan I, Wieler LH, Melzer F, et al. Glanders in animals: a review on epidemiology, clinical presentation, diagnosis and countermeasures. Transbound Emerg Dis. 2013;60(3):204–221. [DOI] [PubMed] [Google Scholar]
- [2].Kettle AN, Wernery U.. Glanders and the risk for its introduction through the international movement of horses. Equine Vet J. 2016;48(5):654–658. [DOI] [PubMed] [Google Scholar]
- [3].Carr-Gregory B, Waag DM. Glanders. In: Dembek ZF, editor. Medical aspects of biological warfare. Borden Institute, Office of the Surgeon General, AMEDD Center and School, Texas, US; 2007. p. 121–146. [Google Scholar]
- [4].Wiersinga WJ, Virk HS, Torres AG, et al. Melioidosis. Nat Rev Dis Primers. 2018;4:17107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Perumal Samy R, Stiles BG, Sethi G, et al. Melioidosis: clinical impact and public health threat in the tropics. PLoS Negl Trop Dis. 2017;11(5):e0004738. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [6].Limmathurotsakul D, Golding N, Dance DA, et al. Predicted global distribution of Burkholderia pseudomallei and burden of melioidosis. Nat Microbiol. 2016;1:1. [DOI] [PubMed] [Google Scholar]
- [7].Losada L, Ronning CM, DeShazer D, et al. Continuing evolution of Burkholderia mallei through genome reduction and large-scale rearrangements. Genome Biol Evol. 2010;2:102–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Song H, Hwang J, Yi H, et al. The early stage of bacterial genome-reductive evolution in the host. PLoS Pathog. 2010;6(5):e1000922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Holden MT, Titball RW, Peacock SJ, et al. Genomic plasticity of the causative agent of melioidosis, Burkholderia pseudomallei. Proc Natl Acad Sci U S A. 2004;101(39):14240–14245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Nierman WC, DeShazer D, Kim HS, et al. Structural flexibility in the Burkholderia mallei genome. Proc Natl Acad Sci U S A. 2004;101(39):14246–14251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Van Zandt KE, Greer MT, Gelhaus HC. Glanders: an overview of infection in humans. Orphanet J Rare Dis. 2013;8:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wiersinga WJ, Currie BJ, Peacock SJ. Melioidosis. N Engl J Med. 2012;367(11):1035–1044. [DOI] [PubMed] [Google Scholar]
- [13].Stone JK, DeShazer D, Brett PJ, et al. Melioidosis: molecular aspects of pathogenesis. Expert Rev Anti Infect Ther. 2014;12(12):1487–1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Galyov EE, Brett PJ, Deshazer D. Molecular Insights into Burkholderia pseudomallei and Burkholderia mallei Pathogenesis. Annu Rev Microbiol. 2010;64:495–517. [DOI] [PubMed] [Google Scholar]
- [15].David J, Bell RE, Clark GC. Mechanisms of disease: host-pathogen interactions between Burkholderia species and lung epithelial cells. Front Cell Infect Microbiol. 2015;5:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hatcher CL, Muruato LA, Torres AG. Recent advances in Burkholderia mallei and B. pseudomallei research. Curr Trop Med Rep. 2015;2(2):62–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lipsitz R, Garges S, Aurigemma R, et al. Workshop on treatment of and postexposure prophylaxis for Burkholderia pseudomallei and B. mallei infection, 2010. Emerg Infect Dis. 2012;18(12):e2-e2. online report. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Rhodes KA, Schweizer HP. Antibiotic resistance in Burkholderia species. Drug Resist Updat. 2016;28:82–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Zimmerman SM, Dyke JS, Jelesijevic TP, et al. Antibodies against in vivo-expressed antigens are sufficient to protect against lethal aerosol infection with Burkholderia mallei and Burkholderia pseudomallei. Infect Immun. 2017;85:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Khakhum N, Bharaj P, Myers JN, et al. Evaluation of Burkholderia mallei Deltaton B Deltahcp1 (CLH001) as a live attenuated vaccine in murine models of glanders and melioidosis. PLoS Negl Trop Dis. 2019;13(7):e0007578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Norris MH, Khan MSR, Chirakul S, et al. Outer membrane vesicle vaccines from biosafe surrogates prevent acute lethal glanders in mice. Vaccines (Basel). 2018;6:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Baker SM, Davitt CJH, Motyka N, et al. A Burkholderia pseudomallei outer membrane vesicle vaccine provides cross protection against inhalational glanders in mice and non-human primates. Vaccines (Basel). 2017;5:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Torres AG, Gregory AE, Hatcher CL, et al. Protection of non-human primates against glanders with a gold nanoparticle glycoconjugate vaccine. Vaccine. 2015;33(5):686–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Gregory AE, Judy BM, Qazi O, et al. A gold nanoparticle-linked glycoconjugate vaccine against Burkholderia mallei. Nanomedicine. 2015;11(2):447–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Felgner PL, Kayala MA, Vigil A, et al. A Burkholderia pseudomallei protein microarray reveals serodiagnostic and cross-reactive antigens. Proc Natl Acad Sci U S A. 2009;106(32):13499–13504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Suwannasaen D, Mahawantung J, Chaowagul W, et al. Human immune responses to Burkholderia pseudomallei characterized by protein microarray analysis. J Infect Dis. 2011;203(7):1002–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Varga JJ, Vigil A, DeShazer D, et al. Distinct human antibody response to the biological warfare agent Burkholderia mallei. Virulence. 2012;3(6):510–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Su YC, Wan KL, Mohamed R, et al. A genome level survey of Burkholderia pseudomallei immunome expressed during human infection. Microbes Infect. 2008;10(12–13):1335–1345. [DOI] [PubMed] [Google Scholar]
- [29].Hara Y, Mohamed R, Nathan S. Immunogenic Burkholderia pseudomallei outer membrane proteins as potential candidate vaccine targets. PLoS One. 2009;4(8):e6496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Champion OL, Gourlay LJ, Scott AE, et al. Immunisation with proteins expressed during chronic murine melioidosis provides enhanced protection against disease. Vaccine. 2016;34(14):1665–1671. [DOI] [PubMed] [Google Scholar]
- [31].Gourlay LJ, Peri C, Ferrer-Navarro M, et al. Exploiting the Burkholderia pseudomallei acute phase antigen BPSL2765 for structure-based epitope discovery/design in structural vaccinology. Chem Biol. 2013;20(9):1147–1156. [DOI] [PubMed] [Google Scholar]
- [32].Godlewska R, Wisniewska K, Pietras Z, et al. Peptidoglycan-associated lipoprotein (Pal) of gram-negative bacteria: function, structure, role in pathogenesis and potential application in immunoprophylaxis. FEMS Microbiol Lett. 2009;298(1):1–11. [DOI] [PubMed] [Google Scholar]
- [33].Duche D, Similarities HL. Differences between colicin and filamentous phage uptake by bacterial cells. EcoSal Plus. 2019;8:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Simon R, Priefer U, Puhler A. A broad host range mobilisation system for in vivo genetic engineering: transposon mutagenesis in gram-negative bacteria. Bio/Technology. 1983;1:784–791. [Google Scholar]
- [35].Skorupski K, Taylor RK. Positive selection vectors for allelic exchange. Gene. 1996;169(1):47–52. [DOI] [PubMed] [Google Scholar]
- [36].Sambrook J, Russell DW. Molecular cloning: a laboratory manual. 3rd ed. Cold Spring Harbor Laboratory Press, New York, USA; 2001. [Google Scholar]
- [37].Balder R, Lipski S, Lazarus JJ, et al. Identification of Burkholderia mallei and Burkholderia pseudomallei adhesins for human respiratory epithelial cells. BMC Microbiol. 2010;10:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Burtnick M, Bolton A, Brett P, et al. Identification of the acid phosphatase (acpA) gene homologues in pathogenic and non-pathogenic Burkholderia spp. facilitates TnphoA mutagenesis. Microbiology. 2001;147(Pt 1):111–120. [DOI] [PubMed] [Google Scholar]
- [39].He B, Paterson RG, Ward CD, et al. Recovery of infectious SV5 from cloned DNA and expression of a foreign gene. Virology. 1997;237(2):249–260. [DOI] [PubMed] [Google Scholar]
- [40].Chen Z, Gupta T, Xu P, et al. Efficacy of parainfluenza virus 5 (PIV5)-based tuberculosis vaccines in mice. Vaccine. 2015;33(51):7217–7224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Lafontaine ER, Chen Z, Huertas-Diaz MC, et al. The autotransporter protein BatA is a protective antigen against lethal aerosol infection with Burkholderia mallei and Burkholderia pseudomallei. Vaccine: X. 2019;13:100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Lafontaine ER, Zimmerman SM, Shaffer TL, et al. Use of a safe, reproducible, and rapid aerosol delivery method to study infection by Burkholderia pseudomallei and Burkholderia mallei in mice. PLoS One. 2013;8(10):e76804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Zimmerman SM, Michel F, Hogan RJ, et al. The autotransporter BpaB contributes to the virulence of Burkholderia mallei in an aerosol model of infection. PLoS One. 2015;10(5):e0126437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Bullard B, Lipski SL, Lafontaine ER. Hag directly mediates the adherence of Moraxella catarrhalis to human middle ear cells. Infect Immun. 2005;73(8):5127–5136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Lafontaine ER, Balder R, Michel F, et al. Characterization of an autotransporter adhesin protein shared by Burkholderia mallei and Burkholderia pseudomallei. BMC Microbiol. 2014;14:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Aschenbroich SA, Lafontaine ER, Lopez MC, et al. Transcriptome analysis of human monocytic cells infected with Burkholderia species and exploration of pentraxin-3 as part of the innate immune response against the organisms. BMC Med Genomics. 2019;12(1):127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Reed LJ, Muench H. A simple method for estimating fifty percent end points. Am J Hyg. 1938;27:793–797. [Google Scholar]
- [48].Poirel L, Jayol A, Nordmann P. Polymyxins: antibacterial activity, susceptibility testing, and resistance mechanisms encoded by plasmids or chromosomes. Clin Microbiol Rev. 2017;30(2):557–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Willcocks SJ, Denman CC, Atkins HS, et al. Intracellular replication of the well-armed pathogen Burkholderia pseudomallei. Curr Opin Microbiol. 2016;29:94–103. [DOI] [PubMed] [Google Scholar]
- [50].Aschenbroich SA, Lafontaine ER, Hogan RJ. Melioidosis and glanders modulation of the innate immune system: barriers to current and future vaccine approaches. Expert Rev Vaccines. 2016;(9):1–19. [DOI] [PubMed] [Google Scholar]
- [51].Burtnick MN, Brett PJ, Woods DE. Molecular and physical characterization of Burkholderia mallei O antigens. J Bacteriol. 2002;184(3):849–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Larsen JC, Johnson NH. Pathogenesis of Burkholderia pseudomallei and Burkholderia mallei. Mil Med. 2009;174(6):647–651. [PubMed] [Google Scholar]
- [53].Chen Z. Parainfluenza virus 5-vectored vaccines against human and animal infectious diseases. Rev Med Virol. 2018;28:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Schell MA, Zhao P, Wells L. Outer membrane proteome of Burkholderia pseudomallei and Burkholderia mallei from diverse growth conditions. J Proteome Res. 2011;10(5):2417–2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Michel LV, Shaw D, Hellman J, et al. Dual orientation of the outer membrane lipoprotein Pal in Escherichia coli. Microbiology. 2015;161(6):1251–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Murphy TF, Kirkham C, Lesse AJ. Construction of a mutant and characterization of the role of the vaccine antigen P6 in outer membrane integrity of nontypeable Haemophilus influenzae. Infect Immun. 2006;74(9):5169–5176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Dubuisson JF, Vianney A, Hugouvieux-Cotte-Pattat N, et al. Tol-Pal proteins are critical cell envelope components of Erwinia chrysanthemi affecting cell morphology and virulence. Microbiology. 2005;151(Pt 10):3337–3347. [DOI] [PubMed] [Google Scholar]
- [58].Lim A Jr., De Vos D, Brauns M, et al. Molecular and immunological characterization of OprL, the 18 kDa outer-membrane peptidoglycan-associated lipoprotein (PAL) of Pseudomonas aeruginosa. Microbiology. 1997;143(Pt 5):1709–1716. [DOI] [PubMed] [Google Scholar]
- [59].Fortney KR, Young RS, Bauer ME, et al. Expression of peptidoglycan-associated lipoprotein is required for virulence in the human model of Haemophilus ducreyi infection. Infect Immun. 2000;68(11):6441–6448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Hsieh PF, Liu JY, Pan YJ, et al. Klebsiella pneumoniae peptidoglycan-associated lipoprotein and murein lipoprotein contribute to serum resistance, antiphagocytosis, and proinflammatory cytokine stimulation. J Infect Dis. 2013;208(10):1580–1589. [DOI] [PubMed] [Google Scholar]
- [61].Dennehy R, Romano M, Ruggiero A, et al. The Burkholderia cenocepacia peptidoglycan-associated lipoprotein is involved in epithelial cell attachment and elicitation of inflammation. Cell Microbiol. 2017;19:5. [DOI] [PubMed] [Google Scholar]
- [62].Cao L, Lim T, Jun S, et al. Vulnerabilities in Yersinia pestis caf operon are unveiled by a salmonella vector. PLoS One. 2012;7(4):e36283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Yang X, Thornburg T, Suo Z, et al. Flagella overexpression attenuates Salmonella pathogenesis. PLoS One. 2012;7(10):e46828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Lei L, Yang F, Zou J, et al. DNA vaccine encoding OmpA and Pal from Acinetobacter baumannii efficiently protects mice against pulmonary infection. Mol Biol Rep. 2019;46(5):5397–5408. [DOI] [PubMed] [Google Scholar]
- [65].Mobarez AM, Rajabi RA, Salmanian AH, et al. Induction of protective immunity by recombinant peptidoglycan associated lipoprotein (rPAL) protein of Legionella pneumophila in a BALB/c mouse model. Microb Pathog. 2019;128:100–105. [DOI] [PubMed] [Google Scholar]
- [66].Green BA, Quinn-Dey T, Zlotnick GW. Biologic activities of antibody to a peptidoglycan-associated lipoprotein of Haemophilus influenzae against multiple clinical isolates of H. influenzae type b. Infect Immun. 1987;55(12):2878–2883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Yang YP, Munson RS Jr., Grass S, et al. Effect of lipid modification on the physicochemical, structural, antigenic and immunoprotective properties of Haemophilus influenzae outer membrane protein P6. Vaccine. 1997;15(9):976–987. [DOI] [PubMed] [Google Scholar]
- [68].Kyd JM, Dunkley ML, Cripps AW. Enhanced respiratory clearance of nontypeable Haemophilus influenzae following mucosal immunization with P6 in a rat model. Infect Immun. 1995;63(8):2931–2940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].DeMaria TF, Murwin DM, Leake ER. Immunization with outer membrane protein P6 from nontypeable Haemophilus influenzae induces bactericidal antibody and affords protection in the chinchilla model of otitis media. Infect Immun. 1996;64(12):5187–5192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Green BA, Vazquez ME, Zlotnick GW, et al. Evaluation of mixtures of purified Haemophilus influenzae outer membrane proteins in protection against challenge with nontypeable H. influenzae in the chinchilla otitis media model. Infect Immun. 1993;61(5):1950–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Sabirov A, Kodama S, Hirano T, et al. Intranasal immunization enhances clearance of nontypeable Haemophilus influenzae and reduces stimulation of tumor necrosis factor alpha production in the murine model of otitis media. Infect Immun. 2001;69(5):2964–2971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Hotomi M, Yamanaka N, Saito T, et al. Antibody responses to the outer membrane protein P6 of non-typeable Haemophilus influenzae and pneumococcal capsular polysaccharides in otitis-prone children. Acta Otolaryngol. 1999;119(6):703–707. [DOI] [PubMed] [Google Scholar]
- [73].Yamanaka N, Faden H. Antibody response to outer membrane protein of nontypeable Haemophilus influenzae in otitis-prone children. J Pediatr. 1993;122(2):212–218. [DOI] [PubMed] [Google Scholar]
- [74].Kodama H, Faden H, Harabuchi Y, et al. Cellular immune response of adenoidal and tonsillar lymphocytes to the P6 outer membrane protein of non-typeable Haemophilus influenzae and its relation to otitis media. Acta Otolaryngol. 1999;119(3):377–383. [DOI] [PubMed] [Google Scholar]
- [75].Abe Y, Murphy TF, Sethi S, et al. Lymphocyte proliferative response to P6 of Haemophilus influenzae is associated with relative protection from exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;165(7):967–971. [DOI] [PubMed] [Google Scholar]
- [76].Pradenas GA, Ross BN, Torres AG. Burkholderia cepacia complex vaccines: where do we go from here? Vaccines (Basel). 2016;4(2):10. [DOI] [PMC free article] [PubMed] [Google Scholar]


