Abstract
Background
Early life adversity associates with poor sleep in adulthood and is believed to sensitize individuals to later stressors. Infectious disease outbreaks increase psychological stress, and life events impact sleep quality. American Indians have been disproportionately affected by the COVID-19 pandemic.
Objective
Investigate whether childhood trauma predicts changes in sleep quality following onset of the pandemic and test whether pandemic stress contributes to changes in sleep.
Methods
In a sample of 210 American Indian adults (Age M (SD) = 55.09 (13.10), 59.5% female) demographics, childhood trauma and sleep quality were measured at Time 1. One month following the onset of the pandemic, psychological stress specific to the pandemic and sleep quality were measured.
Results
Using linear regression controlling for age, sex, income, and sleep quality at Time 1, childhood adversity predicted both psychological stress specific to the pandemic and changes in sleep quality from Time 1 to Time 2 (β = 0.33, t(205) = 4.88, P < .001, ΔR2 = 0.10) and (β = 0.24, t(204) = 3.48, P < .001, ΔR2 = 0.05), respectively. Mediation analyses indicated a significant indirect effect between childhood adversity and changes in sleep quality through COVID-19 stress (indirect effect [standard error, SE] = (0.03[0.01], 95% confidence interval = [0.003, 0.03]).
Conclusions
In American Indians childhood trauma predicts greater declines in sleep quality associated with the onset of the COVID-19 pandemic, in part because greater psychological stress related to COVID-19. Future work should identify factors which alleviate stress related to life events for individuals who experienced childhood trauma in order to improve health behaviors and health.
Keywords: Childhood trauma, Sleep, American Indians, COVID-19
Introduction
American Indians (AIs) experience high levels of trauma beginning in childhood.1 , 2 In response to childhood trauma, it is posited that the brain coordinates behavioral, psychological, and physiological responses to stress in order to help the individual adapt to the demands of their environment.3 To the extent that these profiles persist into adulthood, they can contribute to health-relevant behaviors and individual differences in the way that individuals respond to future stressful events.
In other racial and ethnic groups, it is well established that childhood trauma associates with poor sleep quality and increased sleep disturbances in adolescence and into adulthood.4, 5, 6, 7, 8, 9 Given that individuals who experience childhood trauma are at increased risk to experience psychological distress,10 , 11 one pathway that may contribute to the relationship between childhood trauma and sleep across the life-span is psychological distress. Previous work provides support for this idea, with psychological distress acting as a mediator between childhood trauma and sleep quality in adolescence.6 Previous work extended these findings, with childhood trauma predicting greater declines in sleep quality in response to a major life event: the transition into university life.12 However, these relationships have not been examined in AI populations.
While research on sleep in AI populations is somewhat limited, existing data indicate that AIs experience relatively poor sleep compared to other racial and ethnic groups.13 , 14 Furthermore, in previous work, psychosocial factors including life stress predicted sleep outcomes in AI college students.15 Based on these findings and data from other racial and ethnic groups indicating that life events and stressors negatively impact sleep,16, 17, 18 it is possible that in AIs, childhood trauma may predict changes in sleep in response to life stressors.
On March 11, 2020, the novel coronavirus disease (COVID-19) was labeled as a pandemic; soon after, it was acknowledged as a national emergency in the United States. Previous work provides evidence that infectious disease outbreaks, such as the COVID-19 pandemic, elicit psychological responses.19, 20, 21 The uncertainty that characterizes these outbreaks can contribute to increased levels of psychological stress.22 , 23 However, as with other stressors, the nature of psychological responses to these outbreaks varies across individuals.24 , 25 While early life trauma has not previously been identified as a factor that predicts responses to infectious disease outbreaks, it has been shown to sensitize individuals to future stressful events26, 27, 28, 29, 30, 31 and has predicted traumatic stress following a natural disaster,32 combat-related post-traumatic stress disorder,33 and psychological responses to traumatic violent events.34
Based on the described relationships between childhood trauma, psychological stress response to life stressors, and sleep quality, it was hypothesized that in the context of the COVID-19 pandemic, AI adults who reported high levels of childhood trauma may experience greater declines in sleep quality compared to AI adults with lower levels of early life trauma, and that this relationship may be mediated by higher levels of psychological stress associated with the COVID-19 pandemic.
Methods
AI participants were drawn from a previous cross-sectional survey study in AI adults. Participants for this study were recruited using a Qualtrics research panel and social media advertising targeting AI participants provided their contact information for participation in possible follow-up studies. After receiving Institutional Review Board approval, all 300 participants were contacted. Out of these participants, a sample of 210 interested AI adults was obtained. All participants provided written informed consent online before completing the surveys. Time 1 data were collected during the final week of February, 2020, and the second wave of data reported here was collected during the final week of April and the first week of May, 2020. Participants were given $10 Amazon gift cards for the completion of surveys. To be eligible for participation, participants had to self-identify as AI and be over the age of 18, and these criteria were the same for the larger previous study from which participants were drawn from. There were no statistically significant differences in age, income, or early life trauma between those who chose to participate in this study and those who did not. Surveys administered at Time 1 included demographic questions, a measure of sleep quality, and a measure of early life trauma. Several other measures were administered at Time 1 that are not relevant to the current report, including measures of historical loss and other health behaviors. At the second wave of data collection, we repeated the measure of sleep quality, and asked about psychological stress they were experiencing related to the COVID-19 pandemic.
Measures
Early life trauma
The Risky Family Questionnaire was used to assess childhood exposure to physical, mental, and emotional abuse or neglect.35 Using a 5-point Likert scale (1 = not at all and 5 = very often), participants indicated the frequency with which certain events or situations occurred during childhood (ages 5-15). Example items from this measure include, “How often would you say there was quarreling, arguing or shouting between your parents?” and “How often would you say that a parent or other adult in the household behaved violently toward a family member or visitor in your home.” Responses to each item are summed to create a total score, with higher numbers reflecting more early life trauma. The measure demonstrated good internal reliability (Cronbach a = 0.92).
Sleep
The 19-item Pittsburgh Sleep Quality Index (PSQI) was administered.36
The PSQI assesses sleep quality and sleep disturbances during the previous month. The scale consists of 19 items which are used to derive a total of 7 component scores: sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, sleep medication, and daytime dysfunction. The 7 component scores are summed to produce a global PSQI score. Global PSQI scores (possible range of 0-21; higher scores represent more severe sleep complaints) were computed for each participant at Time 1 and Time 2. These data provided a measure of global sleep quality before the COVID-19 pandemic and 1 month into the pandemic. While this measure does not consistently associate with polysomnography measures of sleep,37 a recent study found that the PSQI associates with some objective measures of sleep quality including sleep efficiency.38 Cronbach's alpha for this measure was 0.73 at Time 1 and 0.75 at Time 2.
COVID-19-specific psychological stress
As a measure of psychological stress specific to the COVID-19 pandemic, using a 7-point Likert scale from 1 = not at all stressed to 7 = extremely stressed, participants responded to the following question, “How stressed do you feel when you think about the coronavirus COVID-19 pandemic?” This measure was created specifically for this study.
Socioeconomic status
As a measure of socioeconomic status, participants reported their annual household income on a scale from 1 (US $20,000 and below) to 6 (U S$110,000 and above).39 , 40
Data analysis
All statistical analyses were conducted using SPSS (Version 24; IBM, Armonk, NY). We used linear regression models for the main analyses. Continuous covariates were centered prior to use in statistical models with z-scores. Early life trauma, as measured by the Risky Family Questionnaire, was modeled as a continuous predictor. The primary hypothesis was tested using a linear regression, with early life trauma predicting changes in sleep quality from Time 1 to Time 2, while controlling for age, sex, income, and sleep quality at Time 1. In a separate hierarchical linear regression model, the relationship between early life trauma and COVID-19-specific psychological stress was investigated. In each of these hierarchical regression models, the covariates were entered into Step 1, and early life trauma was entered in Step 2. Next, to test for indirect effects of early life trauma on changes in sleep quality through psychological stress related to the pandemic, a bootstrapping approach was utilized.41 A point estimate of the indirect effect was derived from the mean of 5000 estimates of the indirect pathways, and 95% confidence intervals (CIs) were computed using the cutoffs for the 2.5% highest and lowest scores of the distribution. Indirect effects were considered statistically significant when the CI did not include 0.
Results
Participants were 210 AI adults ranging in age from 30 to 99. In this sample, 59.5% of participants reported that their biological sex was female. Approximately half of the sample (52.2%) reported that their annual income was less than $40,000, 13.7% were between $40,0001 and $60,000, 11.2% were between $60,001 and $80,000, 8.8% were between $80,0001 and $100,000, and 14.1% of the sample reported an annual income above $100,001. Descriptive statistics are listed in Table 1, and Pearson correlations between main variables of interest are reported in Table 2 .
Table 1.
Descriptive statistics, N = 210.
| Range | Mean | Standard deviation | |
|---|---|---|---|
| Age (Time 1) | 30-99 | 55.09 | 13.10 |
| Childhood trauma | 10-50 | 22.58 | 10.72 |
| PSQI global sleep quality (Time 1) | 0-21 | 3.87 | 1.94 |
| PSQI global sleep quality (Time 2) | 0-21 | 6.42 | 3.21 |
| COVID-19-specific stress | 1-7 | 3.90 | 1.91 |
Table 2.
Bivariate Pearson correlations between main variables of interest.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Age (Time 1) | - | |||||
| 2. Income (Time 1) | 0.06 | - | ||||
| 3. Childhood trauma (Time 1) | −0.23⁎⁎ | −0.19⁎⁎ | - | |||
| 4. PSQI global sleep quality (Time 1) | −0.08 | −0.09 | 0.05 | - | ||
| 5. PSQI global sleep quality (Time 2) | −0.04 | −0.17* | 0.23⁎⁎ | 0.56⁎⁎ | - | |
| 6.Covid-19-specific psychological stress | −0.15* | −0.10 | 0.31⁎⁎ | −0.19⁎⁎ | 0.28⁎⁎ | - |
PSQI, Pittsburgh Sleep Quality Index.
Correlation significant at the 0.05 level (2-tailed).
Correlation significant at the 0.01 level (2 tailed).
Early life trauma and changes in sleep quality
In a linear regression model with the previously described covariates, early life trauma predicted changes in global sleep quality (β = 0.24, t(204) = 3.48, P < .001, ΔR2 = 0.05), with greater reports of early life trauma associating with greater declines in global sleep quality from Time 1 to Time 2 (Table 3a ).
Table 3a.
Hierarchical linear regression model with childhood trauma predicting changes in global sleep quality.
| β | P | ΔR2 | Lower CI | Upper CI | |
|---|---|---|---|---|---|
| Step 1 | |||||
| Age | 0.07 | .32 | −0.01 | 0.04 | |
| Sex | −0.02 | .74 | −0.84 | 0.59 | |
| Income | −0.10 | .18 | −0.36 | 0.07 | |
| PSQI global sleep quality (Time 1) | −0.10 | .16 | −0.31 | 0.05 | |
| Step 2 | |||||
| Childhood trauma (RFQ) | 0.24 | .001 | 0.05 | 0.03 | 0.09 |
PSQI, Pittsburgh Sleep Quality Index; RFQ, Risky Family Questionnaire; Step 1 includes covariates, step 2 includes the addition of the predictor childhood trauma.
Early life trauma and COVID-19-specific stress
In a linear regression model controlling for age, sex, income, early life trauma predicted levels of psychological stress specific to the COVID-19 pandemic (β = 0.33, t(205) = 4.88, P < .001, ΔR2 = 0.10), with greater reports of early life trauma associating with more reported psychological stress related to the pandemic (Table 3b ).
Table 3b.
Hierarchical linear regression model with childhood trauma predicting COVID-19-specific psychological stress.
| β | P | ΔR2 | Lower CI | Upper CI | |
|---|---|---|---|---|---|
| Step 1 | |||||
| Age | −0.10 | .12 | −0.03 | 0.003 | |
| Sex | 0.06 | .39 | −0.26 | 0.65 | |
| Income | −0.08 | .22 | −0.22 | 0.05 | |
| Step 2 | |||||
| Childhood trauma (RFQ) | 0.33 | .001 | 0.10 | 0.03 | −0.07 |
RFQ, Risky Family Questionnaire; Step 1 includes covariates, step 2 includes the addition of the predictor childhood trauma.
Role of COVID-19-specific stress in relationship between early life trauma and changes in sleep quality
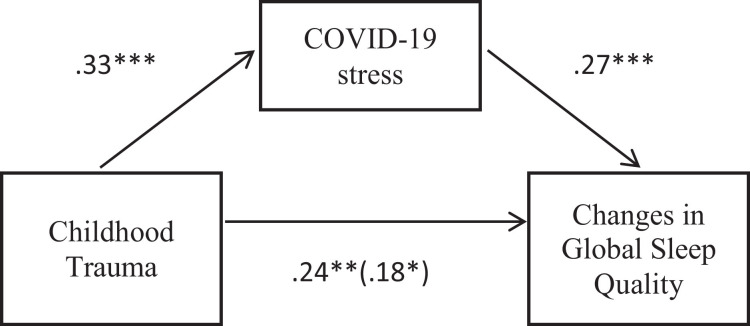
Using the previously described method,41 a significant indirect effect of early life trauma on changes in sleep quality through COVID-19-specific psychological stress was found (indirect effect (standard error, SE) = 0.02(0.01), 95% CI = [0.003, 0.32]; Fig. 1 ).
Fig. 1.
Standardized regression coefficients for direct and indirect effects of childhood trauma on changes in global sleep quality. The standardized regression coefficient between childhood trauma and changes in global sleep quality, controlling for COVID-19 stress, is shown in parentheses. Note: ***= P < .001, **=P < .01, *=P < .05.
Discussion
To the author's knowledge, the findings reported here represent the first evidence in AIs that childhood trauma predicts changes in sleep quality associated with a life stressor, the COVID-19 pandemic. This is important since AIs are a health disparity population with poor sleep outcomes compared to other racial and ethnic groups. These findings are in line with previous work indicating that psychological stress is a pathway through which life events or stressors may negatively affect sleep quality.12 , 16 The findings also add to a growing literature documenting cross-sectional associations between childhood trauma and sleep quality in adulthood, as well as relationships between childhood trauma and changes in sleep quality associated with a life event.4, 5, 6, 7, 8, 9 , 12
The psychological stress that contributed to the relationship between early life trauma and changes in sleep quality in this study was related to the COVID-19 pandemic. Specifically, participants reported the degree of psychological stress they felt when they thought about the pandemic, and individuals who reported more trauma in childhood reported experiencing more psychological stress. In turn, higher levels of psychological stress related to the pandemic predicted greater declines in global sleep quality from the sleep quality measured before the pandemic. This pattern of findings may have particularly important implications for AIs, since, as noted previously, prior research and epidemiological data indicate that relative to other racial and ethnic groups, AIs have worse sleep outcomes. Furthermore, these findings raise the possibility that compromised sleep quality related to life stressors and psychological stress may contribute to existing disparities in incidence of mental and physical health conditions for which sleep is implicated.
These findings have important clinical implications for AIs. As a population, AIs experience significant disparities in mental and physical health and sleep health.1 , 2 , 13 , 14 Given that these data indicate that in AI adults, early life trauma predicts the degree to which life events affect sleep quality and psychological distress, clinicians should consider screening for adverse childhood experiences when targeting psychological distress and sleep disruption in AIs. Furthermore, interventions targeting sleep in AI adults should consider using a trauma-informed approach. Finally, psychological distress related to the event contributed to the observed relationship between early life trauma and changes in sleep quality following the onset of the COVID-19 pandemic. As such, it may be particularly important to help AI adults who experienced high levels of trauma during childhood to successfully manage stress related to life events in order to avoid significant declines in sleep quality.
There are important limitations associated with this work. First, these data were collected online, which may limit the representation of AIs who do not have easy access to computers or the internet. Future work should aim to include AI individuals who do not have access to computers or internet, by distributing paper and pencil surveys to eligible participants. As noted previously, only a small percentage of the participants resided on a tribal reservation at the time of data collection. It is possible that the pattern of findings could be affected by whether AI adults are living in urban settings compared to on a tribal reservation. In the future, investigations could focus exclusively on AIs living on tribal reservations to explore this possibility. It is also possible that there were other life events and stressors which occurred between Time 1 and Time 2 which could have contributed to changes in sleep quality that were not measured. However, the relationship that was observed between childhood trauma and changes in sleep quality was mediated by psychological stress specific to the COVID-19 pandemic. The measure of childhood trauma was self-report and could be subject to recall bias. For example, analyses of these data indicate that report of childhood trauma decreases with age. It is possible that as individuals age, they are less able to recall childhood events.
Unfortunately, participants were not asked about the number of people participants resided with at the time of data collection or collect information about their sleep environment (eg, sharing bedrooms with other people). However, the PSQI measure does provide the opportunity for individuals to indicate factors that negatively impact their sleep quality, and this information is taken into account when calculating the global sleep quality measure. The PSQI measure of global sleep quality is subjective and could be affected by mood or affect at the time of survey completion. This research used the PSQI because data were collected online in order to obtain a sample of AIs from across the United States. Furthermore, the goal was to measure habitual sleep over a month-long period, which is not easily obtained with polysomnography. The PSQI is also advantageous in that the majority of sleep-related epidemiological work is based on self-reported sleep measures, which allows for interpretation of these findings relative to other research. While self-report measures do have important limitations, the PSQI measure of global sleep quality has previously been associated with psychological distress and disease outcomes.38 , 42 , 43 Finally, it is possible that behavioral health conditions such as a post-traumatic stress disorder diagnosis could affect patterns of stress responses to the COVID-19 pandemic. Future work should consider this possibility.
Conclusion
The COVID-19 pandemic has affected lives on a global scale; however, initial evidence indicates that AIs are disproportionately affected by the virus, in part due to higher incidence of underlying chronic conditions.44, 45, 46, 47 It is well known that poor sleep is a risk factor for poor mental and physical health48, 49, 50, 51 and that childhood trauma associates with increased risk for chronic mental and physical health disorders.52, 53, 54, 55, 56 These findings raise the possibility that changes in sleep quality associated with a life stressor may be one pathway through which childhood trauma may contribute to increased risk for poor health in a health disparity population. Overall, in a sample of AI adults, these findings suggest that childhood trauma may contribute to a greater psychological stress response to life events and may increase the degree to which these life events impact sleep quality. As the COVID-19 pandemic continues, if these psychological and behavioral patterns persist, they could, over time, contribute to adverse downstream health outcomes and exacerbate existing AI health disparities. Future work should focus on identifying factors that may alleviate stress related to life events for individuals who experienced childhood trauma, in order to reduce the negative impact of trauma on health behaviors and future risk for poor health.
Conflict of interest
The author has no conflicts of interest to disclose.
Footnotes
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number U54GM115371. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Espey DK, Jim MA, Cobb N. Leading causes of death and all-cause mortality in American Indians and Alaska natives. Am J Pub Health. 2014;104:S303–S311. doi: 10.2105/AJPH.2013.301798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warne D, Dulacki K, Spurlock M. Adverse childhood experiences among American Indians in South Dakota and associations with mental health conditions, alcohol use, and smoking. J Health Care Poor Underserved. 2017;28:1559–1577. doi: 10.1353/hpu.2017.0133. [DOI] [PubMed] [Google Scholar]
- 3.Hostinar CE, Gunnar MR. The developmental effects of early life stress: an overview of current theoretical frameworks. Curr Dir Psychol Sci. 2013;22:400–406. doi: 10.1177/0963721413488889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baiden P, Fallon B, den Dunnen W, Boateng GO. The enduring effects of early childhood adversities and troubled sleep among Canadian Adults: a population-based study. Sleep Med. 2015;16:760–767. doi: 10.1016/j.sleep.2015.02.527. [DOI] [PubMed] [Google Scholar]
- 5.Kajeepeta S, Gelaye B, Jackson CL, Williams MA. Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Med. 2015;16:320–330. doi: 10.1016/j.sleep.2014.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mcphie M, Weiss JA, Wekerle C. Psychological distress as a mediator of the relationship between childhood maltreatment and sleep quality in adolescence: results from the maltreatment and adolescent pathways (MAP) longitudinal study. Child Abuse Negl. 2014;38:2044–2052. doi: 10.1016/j.chiabu.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 7.Ramswah HJ, Ancoli-Israel S, Sullivan SG, Hitchcock CA. Neuroticism mediates the relationship between childhood adversity and sleep quality. Behavioral Sleep Med. 2011;9:130–143. doi: 10.1080/15402002.2011.583895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Y, Raffeld MR, Slopen N, Hale L, Dunn EC. Childhood adversity and insomnia in adolescence. Sleep Med. 2016;21:12–18. doi: 10.1016/j.sleep.2016.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Counts CJ, Grubin FC, John-Henderson NA. Childhood socioeconomic status and risk in early family environments: predictors of global sleep quality in college students. Sleep Health. 2018;4:301–306. doi: 10.1016/j.sleh.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Edwards KM, Probst DR, Rodenhier-Stampfli KA, Gidycz CA, Tansill EC. Multiplicity of child maltreatment and biopsychosocial outcomes in young adulthood: The moderating role of resiliency characteristics among female survivors. Child Maltreat. 2014;19:188–198. doi: 10.1177/1077559514543354. [DOI] [PubMed] [Google Scholar]
- 11.Min M, Farkas K, Minnes S, Singer LT. Impact of childhood abuse and neglect on substance use and psychological distress in adulthood. J Trauma Stress. 2007;20:833–844. doi: 10.1002/jts.20250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.John-Henderson NA, Williams SE, Brindle R, Ginty AT. Changes in sleep quality and levels of psychological distress during the adaptation to university: the role of childhood adversity. Br J Psychol. 2018;109:694–707. doi: 10.1111/bjop.12314. [DOI] [PubMed] [Google Scholar]
- 13.Chapman DP, Croft JB, Liu Y, Perry GS, Presley- Cantrell LR, Ford ES. Excess frequent insufficient sleep in American Indians/Alaska natives. J Environ Public Health. 2013;259:645. doi: 10.1155/2013/259645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ehlers CL, Wills DN, Lau P, Gilder DA. Sleep quality in an adult American Indian community sample. J Clin Sleep Med. 2017;15:385–391. doi: 10.5664/jcsm.6486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.John-Henderson NA, Palmer CA, Thomas A. Life stress, sense of belonging and sleep in American Indian college students. Sleep Health. 2019;5:352–358. doi: 10.1016/j.sleh.2019.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sin NL, Almeida DM, Crain TL, Kossek EE, Berkman LF, Buxton OM. Bidirectional, temporal associations of sleep with positive events, affect, and stressors in daily life across a week. Ann Behav Med. 2017;51:402–415. doi: 10.1007/s12160-016-9864-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Laethem M, Beckers DGJ, Dijksterhuis A, Geurts SAE. Stress, fatigue, and sleep quality leading up to and following a stressful life event. Stress Health. 2017;33:459–469. doi: 10.1002/smi.2730. [DOI] [PubMed] [Google Scholar]
- 18.Van Laethem M, Beckers DG, van Hooff ML, Dijksterhuis A, Geurts SA. Day-to-day relations between stress and sleep and the mediating role of perseverative cognition. Sleep Med. 2016;24:71–79. doi: 10.1016/j.sleep.2016.06.020. [DOI] [PubMed] [Google Scholar]
- 19.Shah K, Kamrai D, Mekala H, Mann B, Desai K, Patel RS. Focus on mental health during the Coronavirus (COVID-19) pandemic: Applying learnings from the past outbreaks. Cureus. 2020;12(3):e7405. doi: 10.7759/cureus.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sim K, Huak Chan Y, Nah Chong P., Choon Chua H., Wen Soon S. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J Psychosomat Res. 2010;68:195–202. doi: 10.1016/j.jpsychores.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiang Y, Yang Y, Li W. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatr. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng C, Cheung M. Psychological responses to outbreak of severe acute respiratory syndrome: a prospective, multiple time-point study. J Pers. 2005;73:261–285. doi: 10.1111/j.1467-6494.2004.00310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee S, Kang W, Cho A, Kim T, Park J. Psychological impact of the 2015 MERS outbreak in hospital workers and quarantined hemodialysis patients. Comparative Psychiatr. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lau J, Kim J, Tsui H, Griffiths S. Perceptions related to human avian influenza and their associations with anticipated psychological and behavioral responses at the onset of outbreak in the Hong Kong Chinese general population. Am J Infect Control. 2007;35:38–49. doi: 10.1016/j.ajic.2006.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams L, Regagliolo A, Rasmussen S. Predicting psychological responses to Influenza A, H1N1 ("Swine flu"): the role of illness perceptions. Psychol Health Med. 2012;17:383–391. doi: 10.1080/13548506.2011.626564. [DOI] [PubMed] [Google Scholar]
- 26.Asselmann E, Stender J, Grabe HJ. Assessing the interplay of childhood adversities with more recent stressful life events and conditions in predicting panic pathology among adults from the general population. J Affect Disord. 2018;225:715–722. doi: 10.1016/j.jad.2017.08.050. [DOI] [PubMed] [Google Scholar]
- 27.Gouin JP, Glaser R, Malarkey WB, Beversdorf D, Kiecolt-Glaser JK. Childhood abuse and inflammatory responses to daily stressors. Ann Behav Med. 2012;44:287–292. doi: 10.1007/s12160-012-9386-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harkness KL, Bruce AE, Lumley MN. The role of childhood abuse and neglect in the sensitization to stressful life events in adolescent depression. J Abnorm Psychol. 2006;115:730–741. doi: 10.1037/0021-843X.115.4.730. [DOI] [PubMed] [Google Scholar]
- 29.McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol Med. 2010;40:1647–1658. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nakai Y, Inoue T, Toda H. The influence of childhood abuse, adult stressful life events and temperaments on depressive symptoms in the nonclinical general adult population. J Affect Disord. 2014;158:101–107. doi: 10.1016/j.jad.2014.02.004. [published correction appears in J Affect Disord. 2015 May 1;176:8] [DOI] [PubMed] [Google Scholar]
- 31.Shapero BG, Black SK, Liu RT. Stressful life events and depression symptoms: the effect of childhood emotional abuse on stress reactivity. J Clin Psychol. 2014;70:209–223. doi: 10.1002/jclp.22011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Neuner F, Schauer E, Catani C, Ruf M, Elbert T. Post-tsunami stress: a study of posttraumatic stress disorder in children living in three severely affected regions in Sri Lanka. J Trauma Stress. 2006;19:339–347. doi: 10.1002/jts.20121. [DOI] [PubMed] [Google Scholar]
- 33.Bremner JD, Southwick SM, Johnson DR, Yehuda R, Charney DS. Childhood physical abuse and combat-related posttraumatic stress disorder in Vietnam veterans. Am J Psychiatry. 1993;150:235–239. doi: 10.1176/ajp.150.2.235. doi: 10.1176/ajp.150.2.235. [DOI] [PubMed] [Google Scholar]
- 34.Andrews B, Brewin CR, Rose S, Kirk M. Predicting PTSD symptoms in victims of violent crime: The role of shame, anger, and childhood abuse. J Abnorm Psychol. 2000;109:69–73. doi: 10.1037/0021-843X.109.1.69. [DOI] [PubMed] [Google Scholar]
- 35.Taylor SE, Lerner JS, Sage RM, Lehman BJ, Seeman TE. Early environment, emotions, responses to stress, and health. J Pers. 2004;72:1365–1393. doi: 10.1111/j.1467-6494.2004.00300.x. [DOI] [PubMed] [Google Scholar]
- 36.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 37.Kaplan KA, Hirshman J, Hernandez B. When a gold standard isn't so golden: Lack of prediction of subjective sleep quality from sleep polysomnography. Biol Psychol. 2017;123:37–46. doi: 10.1016/j.biopsycho.2016.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Buysse DJ, Hall ML, Strollo PJ. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4:563–571. [published correction appears in J Clin Sleep Med. 2010 Feb 15;6(1):table of contents] [PMC free article] [PubMed] [Google Scholar]
- 39.Kraus MW, Adler N, Chen TW. Is the association of subjective SES and self-rated health confounded by negative mood? An experimental approach. Health Psychol. 2013;32:138–145. doi: 10.1037/a0027343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.John-Henderson NA, Stellar JE, Mendoza-Denton R, Francis DD. Socioeconomic status and social support: social support reduces inflammatory reactivity for individuals whose early-life socioeconomic status was low. Psychol Sci. 2015;26:1620–1629. doi: 10.1177/0956797615595962. [DOI] [PubMed] [Google Scholar]
- 41.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–731. doi: 10.3758/BF03206553. [DOI] [PubMed] [Google Scholar]
- 42.Casement MD, Harrington KM, Miller MW, Resick PA. Associations between Pittsburgh Sleep Quality Index factors and health outcomes in women with posttraumatic stress disorder. Sleep Med. 2012;13:752–758. doi: 10.1016/j.sleep.2012.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jennings JR, Muldoon MF, Hall M, Buysse DJ, Manuck SB. Self-reported sleep quality is associated with metabolic syndrome. Sleep. 2007;30:219–223. doi: 10.1093/sleep/30.2.219. [DOI] [PubMed] [Google Scholar]
- 44.Zhou Y, Chi J, Lv W, Wang Y. Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (COVID-19) Diabetes Metab Res Rev. 2020:e3377. doi: 10.1002/dmrr.3377. [published online ahead of print, 2020 Jun 26] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hamer M, Kivimäki M, Gale CR, Batty GD. Lifestyle risk factors for cardiovascular disease in relation to COVID-19 hospitalization: a community-based cohort study of 387,109 Adults in UK. Preprint. medRxiv. 2020;2020.05.09.20096438. Published 2020 May 13. doi:10.1101/2020.05.09.20096438
- 46.Krouse HJ. COVID-19 and the widening gap in health inequity. Otolaryngol Head Neck Surg. 2020;163(1):65–66. doi: 10.1177/0194599820926463. [DOI] [PubMed] [Google Scholar]
- 47.Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59:137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dijk DJ. Sleep and health: beyond sleep duration and sleepiness? J Sleep Res. 2012;21:355–356. doi: 10.1111/j.1365-2869.2012.01036.x. [DOI] [PubMed] [Google Scholar]
- 49.Lao XQ, Liu X, Deng HB. Sleep quality, sleep duration, and the risk of coronary heart disease: a prospective cohort study with 60,586 adults. J Clin Sleep Med. 2018;14:109–117. doi: 10.5664/jcsm.6894. Published 2018 Jan 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Suzuki E, Yorifuji T, Ueshima K. Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: a population-based cohort study. Prev Med. 2009;49:135–141. doi: 10.1016/j.ypmed.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 51.Zhai L, Zhang H, Zhang D. sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety. 2015;32:664–670. doi: 10.1002/da.22386. [DOI] [PubMed] [Google Scholar]
- 52.Sweeting JA, Garfin DR, Holman EA, Silver RC. Associations between exposure to childhood bullying and abuse and adulthood outcomes in a representative national U.S. sample. Child Abuse Negl. 2020;101 doi: 10.1016/j.chiabu.2019.104048. [DOI] [PubMed] [Google Scholar]
- 53.Tracy EL, Tracy CT, Kim JJ, Yang R, Kim E. Cascading effects of childhood abuse on physical health issues in later adulthood through trait anxiety and poor daily sleep quality. J Health Psychol. 2020 doi: 10.1177/1359105320909876. [published online ahead of print, 2020 Mar 1] 1359105320909876. [DOI] [PubMed] [Google Scholar]
- 54.Chen E, Turiano NA, Mroczek DK, Miller GE. Association of reports of childhood abuse and all-cause mortality rates in women. JAMA Psychiatry. 2016;73:920–927. doi: 10.1001/jamapsychiatry.2016.1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hayashi Y, Okamoto Y, Takagaki K. Direct and indirect influences of childhood abuse on depression symptoms in patients with major depressive disorder. BMC Psychiatry. 2015;15:244. doi: 10.1186/s12888-015-0636-1. Published 2015 Oct 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schulz P, Beblo T, Ribbert H. How is childhood emotional abuse related to major depression in adulthood? The role of personality and emotion acceptance. Child Abuse Neglect. 2017;72:98–109. doi: 10.1016/j.chiabu.2017.07.022. [DOI] [PubMed] [Google Scholar]