Abstract
Women are more likely than men to be diagnosed with anxiety disorders and to be prescribed benzodiazepines. People with substance use disorders are at a heightened risk for the misuse of benzodiazepines, yet little is known about sex differences in the prevalence, correlates or patterns of benzodiazepine misuse in this population. The aim of this study was to characterize sex differences in benzodiazepine misuse in a sample of adults receiving substance use disorder treatment (N = 352). Almost half of the sample had been prescribed a benzodiazepine and more than 40% had misused a benzodiazepine. Women were more likely to have a lifetime prescription than men, but were not more likely to report misuse or regular misuse. Consistent with data for other substances, women were more likely to report misusing benzodiazepines to cope and reported greater anxiety sensitivity. The vast majority (97%) of participants reported co-use of benzodiazepines with other substances and 65% of women reporting misusing benzodiazepines via a non-oral route of administration (e.g., intranasal). Although benzodiazepine misuse prevalence was not substantively different between men and women, several sex differences in clinical characteristics and patterns of use were identified. Further research on the nature of sex differences in benzodiazepine misuse is needed to inform targeted treatment for both men and women with substance use disorders.
Keywords: Sex differences, Benzodiazepines, Prescription drug misuse, Substance use disorder
1. Introduction
Prescription drugs are among the most commonly misused substances in the United States (Center for Behavioral Health Statistics and Quality, 2019). Although much research and public health attention has focused on the misuse (i.e., use without a prescription or at a higher dose or greater frequency than prescribed) of opioid analgesics, troubling public health trends are also evident for benzodiazepines (Agarwal & Landon, 2019; Olfson, King, & Schoenbaum, 2015). Much like opioids, the number of benzodiazepine prescriptions and the potency of those prescriptions have increased over the past two decades (Agarwal & Landon, 2019; Bachhuber, Hennessy, Cunningham, & Starrels, 2016), with corresponding increases in emergency department visits (Bachhuber, Maughan, Mitra, Feingold, & Starrels, 2016) and overdose deaths (Bachhuber, Hennessy, et al., 2016). In 2018, benzodiazepine misuse was more common than cocaine use in the United States (Center for Behavioral Health Statistics and Quality, 2019).
Women are more likely than men to be prescribed medications such as opioids and benzodiazepines (Agarwal & Landon, 2019; Campbell et al., 2010; Olfson, King, & Schoenbaum, 2015), and thus may be particularly vulnerable to problems with their misuse. Significant sex differences have been identified among people who misuse opioid analgesics across an array of clinical features, most predominantly indicating that psychiatric comorbidity and functional impairment are substantially worse in women relative to men (Green, Grimes Serrano, Licari, Budman, & Butler, 2009; McHugh et al., 2013). However, very little is known about sex differences among those who misuse benzodiazepines.
Women are almost twice as likely to have a benzodiazepine prescription than men (Agarwal & Landon, 2019; Olfson et al., 2015) and thus have more exposure to these medications. This may be attributable—at least in part—to the higher prevalence of anxiety and traumatic stress related disorders in women relative to men (McLean, Asnaani, Litz, & Hofmann, 2011). However, evidence from large representative general population surveys indicate a similar prevalence of benzodiazepine misuse in men and women (Center for Behavioral Health Statistics and Quality, 2019). People with substance use disorders (SUDs) have much higher rates of benzodiazepine misuse than the general population (Votaw, Witkiewitz, Valeri, Bogunovic, & McHugh, 2019). Among people with alcohol or opioid use disorder, women are more likely to report benzodiazepine misuse, but not more likely to have a sedative use disorder (Votaw, Witkiewitz et al., 2019; Votaw, Geyer, Rieselbach, & McHugh, 2019). Although these studies have characterized the prevalence of sex differences in benzodiazepine misuse in people with SUDs, studies of sex differences in the nature (e.g., correlates, patterns of use, motives for use) of benzodiazepine misuse are less common.
Studies have examined the role of anxiety in benzodiazepine misuse in people with SUDs. These have consistently demonstrated that higher anxiety sensitivity (the fear of anxiety symptoms and sensations) is associated with benzodiazepine misuse in women, but not men (Hearon et al., 2011; McHugh et al., 2017; McHugh, Geyer, Karakula, Griffin, & Weiss, 2018). This is consistent with data from studies in the general population (i.e., not exclusively in people with SUDs) that have found that women are more likely than men to report misusing benzodiazepines to cope (Boyd, Austic, Epstein-Ngo, Veliz, & McCabe, 2015; McCabe & Cranford, 2012). Little else is known about sex differences in benzodiazepine misuse patterns, particularly in clinically important domains, such as route of administration and co-use with other substances. These types of features are of particular interest due to their contribution to risk for nonfatal and fatal overdose (Gudin, Mogali, Jones, & Comer, 2013). Characterizing such sex differences can help us to further understand the clinical features of benzodiazepine misuse and consider potential targets for intervention.
The overarching aim of the current study is to characterize sex differences in adults with SUDs who report a history of benzodiazepine misuse. Our first aim was to examine whether there was a sex difference in the prevalence of lifetime benzodiazepine prescription or benzodiazepine misuse. We hypothesized that women would be more likely than men to have been prescribed and to have misused benzodiazepines. Our second aim was to examine sex differences in reasons for benzodiazepine misuse, including the reason for first initiating misuse and motives for past-year misuse. We hypothesized that women would be more likely than men to report misusing benzodiazepines for coping-related reasons and that women would report more anxiety sensitivity. Finally, in an exploratory aim, we examined sex differences in clinical features (e.g., pain, drug craving) and patterns of use (e.g., route of administration, co-use with other substances) among participants who reported benzodiazepine misuse. This study was a planned secondary data analysis from a larger, ongoing survey study.
2. Material and methods
2.1. Participants
Participants were recruited for a cross-sectional survey study from an inpatient detoxification and stabilization unit in an academically affiliated psychiatric hospital. Study recruitment was conducted between June 2017 and July 2018. Participants were eligible if they had a diagnosis of a current substance use disorder (according to DSM-5 criteria), were 18 or older, and could read and provide informed consent. A total of 356 participants were enrolled in the study; 4 participants did not complete the benzodiazepine measure and 3 declined to report sex and thus the final sample consisted of 349 participants.
The sample consisted of 40.4% women and reported a mean age of 39.2 years (SD = 13.0). The sample was predominantly White (90.4%) and non-Hispanic/Latinx (95.3%). Less than 3% of the sample did not complete a high school education, 20.5% completed high school or equivalent, 37.3% completed some college, 26.2% received a 4-year college degree, and 13.4% completed post-college education. Most participants were employed either full- (42.9%) or part-time (8.9%), followed by unemployed (27.7%), disabled (10.6%), retired (5.1%) and<5% for student or homemaker. The most common primary substance use disorder (i.e., substance use disorder that was the current focus of treatment) was alcohol use disorder (65.2%), followed by opioid use disorder (27.1%), sedative use disorder (5.1%) and other substance use disorder (2.6%).
2.2. Procedures
Potentially eligible participants were recruited through presentations made by research staff at the beginning of treatment groups. Research assistants provided potential participants with further information regarding the study and interested participants then completed the written informed consent process. Of those who were approached or expressed initial interest, 12% of patients declined participation. Participants completed a 20–30-minute survey using a tablet computer. Data were collected using a HIPAA-compliant data collection platform (REDCap) (Harris et al., 2009). For brevity, only measures used in this report are included below. Diagnostic information was extracted from the electronic medical record. Participants did not received compensation for their participation. All study procedures were approved by the local Institutional Review Board.
2.3. Measures
Benzodiazepine History Questionnaire. This 17-item questionnaire assessed history and patterns of lifetime and past-year benzodiazepine misuse, including any misuse and regular misuse (defined as three times per week or more). Respondents were specifically instructed not to include benzodiazepines prescribed only for detoxification. This measure was adapted from a similar measure of opioid analgesic misuse (Weiss et al., 2011), with the addition of items assessing co-use (i.e., simultaneous use) of benzodiazepines with other substances. This measure assessed the motive for initially misusing benzodiazepines, using a list of 17 motives (e.g., to relieve nervousness/anxiety, to feel high/euphoria, to decrease the effects of cocaine/other stimulants). For ease of interpretation, these were combined into coping (e.g., to relieve nervousness/anxiety, to improve sleep), enhancement (e.g., to feel high/euphoria, out of curiosity) and substance-related (e.g., to decrease the effects of cocaine/other stimulants, to help with opioid withdrawal).
Drug Use Motives Questionnaire. This 15-item questionnaire was used to assess the reasons (i.e., motives) for past-year benzodiazepine misuse (Cooper, Russell, Skinner, & Windle, 1992; Mueser, Nishith, Tracy, DeGirolamo, & Molinaro, 1995). The measure consisted of three subscales assessing coping (e.g., to relax, get rid of worries), enhancement (e.g., use to get high) and social (e.g., to celebrate) motives for use. Respondents were asked to report how often they misused benzodiazepines for each reason on a scale of 1 (almost never/never) to 4 (almost always/always). Scores range from 5 to 20 for each subscale. Measure instructions were modified to specify that respondents should answer all questions based on their motives for misusing benzodiazepines.
Craving Scale. This is a 3-item questionnaire that assesses drug and alcohol craving (Weiss et al., 1995). This measure has been previously validated for opioid, alcohol and cocaine craving (McHugh et al., 2014, 2016; Weiss et al., 2003). Each item is scored from 0 to 9 and the 3 items are averaged to provide an overall craving score ranging from 0 to 9 with higher scores reflecting more craving. Participants were asked to respond to questions based on the primary substance for which they were seeking treatment. This was included in the current study as a general marker of substance use disorder severity.
Anxiety Sensitivity Index. This 18-item questionnaire assessed the tendency to interpret the physical (e.g., rapid heartbeat, upset stomach), cognitive (e.g., unable to keep mind on task), and social (e.g., worry others will notice their anxiety) aspects of anxiety as harmful or dangerous (Taylor et al., 2007). Participants rated how much they agreed with each statement from 0 (very little) to 4 (very much), and the total score ranges from 0 to 72 with higher scores reflecting greater anxiety sensitivity.
Brief Pain Inventory. Chronic pain was defined as significant pain (not including everyday aches and pains) lasting for longer than 3 months (Merskey & Bogduk, 1994). This was assessed using questions from the Brief Pain Inventory (Cleeland & Ryan, 1994). The first item was modified to specify that only pain not due to drug withdrawal should be reported, consistent with prior research (Weiss et al., 2011).
2.4. Data analysis
We first evaluated the data for evidence of skewness and univariate outliers. We examined sex differences in lifetime receipt of benzodiazepine prescription and benzodiazepine misuse and regular misuse using χ2 tests (Aim 1). We then compared men and women on motives for use using t-tests or χ2 tests (Aim 2). Finally, in our exploratory aim we examined sex differences among people with benzodiazepine misuse with respect to clinical features (drug craving, pain, psychiatric comorbidity), and use patterns (route of administration) using t-tests or χ2 tests. Due to the use of multiple tests for our exploratory aim (5 tests), we adjusted alpha for these analyses using the Sidak correction (alpha = 0.01). We also report effect sizes to facilitate the interpretation of these findings and to inform hypothesis generation in light of the limited available literature on this topic.
3. Results
3.1. Aim 1. Prevalence of benzodiazepine use and misuse
Descriptive results by sex are presented in Table 1. Approximately half of the sample, 174 participants (49.4%) had been prescribed a benzodiazepine by a medical professional in their lifetime. Women were more likely to be prescribed benzodiazepines than men χ2 (1, N = 349) = 6.52, p = .01.
Table 1.
Sample Characteristics by Sex.
| Women | Men | Test Statistic | p | |
|---|---|---|---|---|
| Characteristics of Total Sample (N = 349) | ||||
| Lifetime Prescription, n (%) | 82 (58%) | 92 (44%) | 6.52 | 0.01 |
| Lifetime Misuse, n (%) | 53 (38%) | 90 (43%) | 1.12 | 0.29 |
| Lifetime Regular Misuse, n (%) | 35 (25%) | 63 (25%) | 0.42 | 0.52 |
| Initial Reason for Misuse, n (% of those with lifetime misuse) | 6.66 | < 0.05 | ||
| Coping | 36 (68%) | 44 (49%) | ||
| Enhancement | 10 (19%) | 36 (40%) | ||
| Substance-Related | 7 (13%) | 9 (10%) | ||
| Characteristics of Participants with Past-Year Benzodiazepine Misuse (n = 110) | ||||
| DUMQ Coping Subscale | 15.97 (4.38) | 13.89 (4.80) | 2.23 | 0.03 |
| DUMQ Enhancement Subscale | 12.92 (4.66) | 12.03 (4.56) | 0.97 | 0.33 |
| DUMQ Social Subscale | 8.50 (4.22) | 8.03 (4.05) | ** | 0.43 |
| Anxiety Sensitivity Index Total Score | 33.45 (17.78) | 26.42 (15.62) | 2.39 | |
| Craving Scale Total Score | 6.30 (2.32) | 4.58 (2.44) | 4.04 | < 0.001 |
| Initial Source of Misused Benzodiazepines | 9.39 | < 0.01 | ||
| Given by Friends or Family | 30 (60%) | 43 (49%) | ||
| Legitimate Prescription | 12 (24%) | 23 (26%) | ||
| Bought Illegally or Illegitimate Prescription | 8 (16%) | 42 (48%) | ||
| Route of Administration | 6.62 | < 0.01 | ||
| Oral | 20 (38%) | 54 (60%) | ||
| Other | 33 (62%) | 36 (40%) |
When asked about lifetime benzodiazepine misuse (i.e., “have you ever used benzodiazepines without a prescription to you or at a higher dose or more frequently than prescribed”), 143 participants (40.6%) reported a lifetime history of misuse. Participants with a lifetime benzodiazepine prescription were more like to misuse in their lifetime, χ2 (1, N = 349) = 5.43, p < .05. There were no sex differences in prevalence of lifetime history of benzodiazepine misuse, χ2 (1, N = 349) = 1.12, p = .29. Among those participants who reported a history of benzodiazepine misuse, 98 participants (68.5%) reported having ever misused benzodiazepines at least 3 times per week (i.e., regular misuse); there were no sex differences in the lifetime history of regular misuse, χ2 (1, N = 144) = 0.42, p = .52. Fig. 1 depicts the results of Aim 1.
Fig. 1.

Lifetime Benzodiazepine Prescriptions, Misuse and Regular Misuse (use at least 3 times per week) by Sex. N = 349 (141 women, 208 men).
3.2. Aim 2. Motives for benzodiazepine misuse
All participants with lifetime misuse (n = 143) were asked to identify the primary reason for which they first misused benzodiazepines. Coping was the most common motive for initial misuse in both men and women, followed by enhancement and substance-relative motives. A significant sex difference was observed, χ2 (2, 140) = 6.33, p < .05. Specifically, coping was more common in women (67.3%) than men (50%) and enhancement was less common among women (19.2%) compared to men (39.8%). Substance-related motives were comparable in women (13.5%) and men (10.2%).
Participants who reported past-year benzodiazepine misuse (n = 112) also completed a measure of the frequency of motives for benzodiazepine misuse (Drug Use Motives Questionnaire). We used independent samples t-tests to examine sex differences in motives for benzodiazepine misuse in the past year (see Fig. 2). Of note, in contrast to our assessment of motives for initial misuse, past-year motives were not mutually exclusive (i.e., people could report both coping and enhancement motives). Consistent with hypotheses, women reported more frequently misusing benzodiazepines to cope than men, t (108) = 2.23, p = .03. There was no difference between men and women in frequency of enhancement motives, t(108) = 0.97, p = .33. Given skewness of the social motives data (Skewness = 1.28, SE = 0.23), we used a nonparametric test (Independent-Samples Mann-Whitney U Test) to examine sex differences in social motives; results indicated no significant difference (p = .43).
Fig. 2.
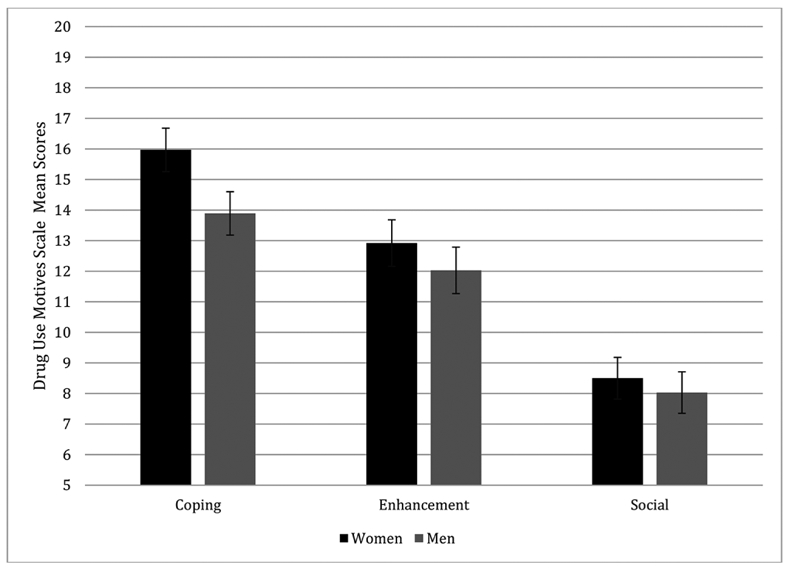
Motives for Benzodiazepine Misuse by Sex.
Consistent with these findings indicating more coping motives for misuse among women, women reported greater anxiety sensitivity (M = 33.45, SD = 17.78) than men (M = 26.42, SD = 15.62), t (130) = 2.39, p < .05. Of the Anxiety Sensitivity Index subscales, only the physical subscale was significantly different between women and men (t[133] = 2.59, p < .05); yet, the effect size difference for all three subscales was in the magnitude of a small to medium effect size (d = 0.29 or higher) larger in women.
3.3. Exploratory aim. Benzodiazepine misuse severity, correlates and use patterns
Women with a lifetime history of benzodiazepine misuse reported significantly more craving for their primary substance (6.30 vs. 4.58 out of 9 for women and men, respectively; t[133] = 4.04, p < .001). There were no sex differences in the presence of a co-occurring psychiatric disorder χ2 (1,143) = 0.18, p = .67 or the presence of chronic pain, χ2 (1, 129) = 0.86, p = .36.
Sex differences were also observed in the initial source of misused benzodiazepines, χ2 (2, 139) = 9.39, p < .01. The most common initial source for both men and women was “given to you by friends or family” (59% of women and 49% of men); however, women were twice as likely to report a legitimate prescription as their first source (26% of women vs. 13% of men) and men were more than twice as likely to report that they bought benzodiazepines or obtained an illegitimate prescription (39% of men compared to 16% of women).
More than half of male participants reported that they exclusively misused benzodiazepines orally (60%), compared to 38% of women. The most common other route of administration was intranasal (55% of women and 35% of men). These differences did not meet significance at the adjusted alpha level, χ2 (1. 143) = 6.62, p < .05.
Data on the simultaneous misuse of benzodiazepines with other substances indicated that the vast majority of participants co-used benzodiazepines with other drugs in the prior year (97% of men and 95% of women); however, the pattern varied by sex, with men more likely to combine benzodiazepines with cannabis and women more likely to combine benzodiazepines with stimulants. These findings are presented in Fig. 3.
Fig. 3.
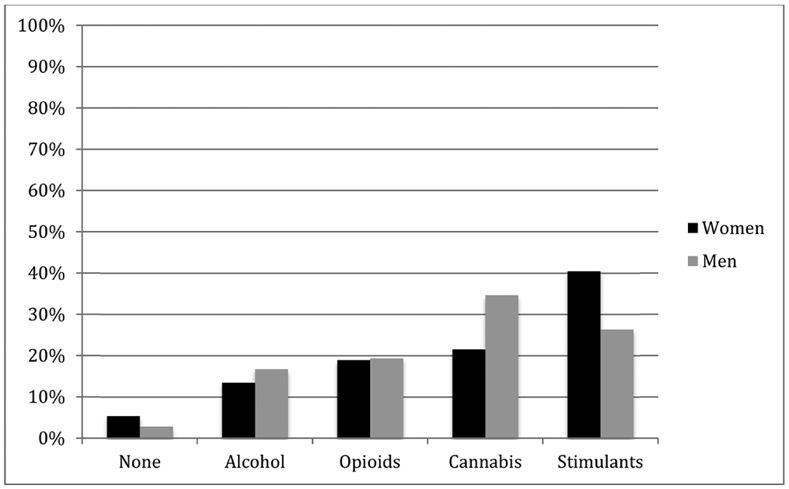
Co-Use of Benzodiazepines with Other Substances in the Past Year (categories are not mutually exclusive). N = 112 (38 women, 74 men).
4. Discussion
The aim of this study was to identify sex differences in the prevalence and characteristics of benzodiazepine misuse in individuals with SUDs. We found that half of our sample had been medically prescribed benzodiazepines, with a larger number of women having received a prescription (58%) than men (44%). More than 40% of the sample reported lifetime misuse and one-quarter reported regular misuse (3 times per week or more) in their lifetime. However, there were no sex differences in the prevalence of misuse or regular misuse of benzodiazepines. These findings are generally consistent with the literature, which suggests much higher prescription rates in women but no consistent sex difference in the prevalence of misuse (see for review, Votaw et al., 2019).
When considering sex differences in the characteristics of benzodiazepine misuse, many differences emerged, several of which were large in magnitude. Our findings showed that for both sexes, the most commonly reported motivation for first initiating misuse was coping, with more than half of men and more than two-thirds of women reporting that this was their initial reason for misuse. Coping was also the most frequent motive for past-year benzodiazepine misuse, although enhancement motives were also reported. Of note, some participants may have initiated misuse within the past use and thus first misuse and past-year misuse may have overlapped. Furthermore, we cannot rule out the possibility that coping motives captured coping with symptoms of anxiety or other distress caused by acute or protracted withdrawal, due to difficulty discriminating these symptoms. This finding adds to the literature suggesting that the misuse of prescription drugs for a reason that is consistent with an indicated medical purpose (e.g., reducing anxiety) is highly prevalent. Consistent with data from other substance use disorders (e.g., opioid use disorder; McHugh et al., 2013), coping motives were more commonly reported among women than among men, and women reported more anxiety sensitivity than men.
Our final exploratory aim sought to characterize sex differences in correlates and patterns of use in adults misusing benzodiazepines. Further sex differences emerged, suggesting a generally more severe profile in women, characterized by higher levels of craving for their primary drug and higher likelihood of more severe routes of administration. Women were more 20% more likely than men to misuse benzodiazepines via inhalation, however, this did not reach our adjusted significance level. Although replication of these findings is needed, these findings suggest a more severe pattern of benzodiazepine misuse in women.
Our study has several clinical implications. First, our findings further highlight the high prevalence of lifetime benzodiazepine misuse in both men and women with other SUDs, particularly among treatmentseekers. The majority of participants who reported lifetime misuse had at some time misused benzodiazepines regularly and thus were at risk for an array of negative consequences such as physiological dependence and development of a sedative use disorder. Accordingly, screening for benzodiazepine misuse is essential in this population. Second, our findings contribute to the growing literature suggesting that the clinical features of prescription drug misuse differ between men and women. Women have greater exposure than men to benzodiazepines via legitimate prescription and are more likely to report misusing these medications for coping reasons, highlighting the importance of identifying and treating psychiatric conditions in women. Nonetheless, coping motives were also the most common reason for misuse among men, and thus consideration of psychiatric comorbidity is important in both sexes. We did not formally assess substance use disorder diagnosis and thus future studies would benefit from the addition of assessment of the presence of sedative use disorder. Additionally, the Benzodiazepine History Questionnaire has not been formally validated. Finally, benzodiazepine misuse often occurred in a risky pattern, characterized by a non-oral route of administration and co-use with other substances, raising significant concerns about overdose and other health risks. In a large clinical trial of treatment for prescription opioid dependence (Prescription Opioid Addiction Treatment Study), non-oral route of administration (e.g., intranasal) was the single best predictor of outcome poor outcome (Dreifuss et al., 2013).
There are several limitations to this study. The sample was drawn from an inpatient detoxification and stabilization program composed of predominately White, non-Hispanic participants and thus generalizability to other samples cannot be assumed. Although using a previously validated measure of drug use motives was a strength, it may not adequately capture the variety of potential motives for misuse (e.g., to mitigate withdrawal). Our question assessing initial misuse included a broader array of motives and found that using for substance-related reasons (e.g., to enhance or lessen the effects of another drug) was present in a minority (10–15%) of participants. Such motives may be more common later in the course of benzodiazepine misuse; studies are needed to test this hypothesis. Furthermore, this study was cross-sectional in nature; longitudinal studies examining benzodiazepine misuse trajectories over time will be important to better understanding sex differences in this population.
Similar to opioid analgesics (Green et al., 2009; McHugh et al., 2013), substantial sex differences were apparent in the clinical characteristics of people with SUDs who misuse benzodiazepines. Although some of these findings are consistent with the opioid analgesic literature, such as the higher prevalence of coping motives among women, other findings are in contrast to the opioid literature (e.g., greater likelihood of a non-oral route of administration in women). Women had greater anxiety, drug craving and non-oral route of administration;replication of this pattern is important to understanding the impact of benzodiazepine misuse among women.
HIGHLIGHTS.
Women with substance use disorder were more likely to be prescribed benzodiazepines.
There was no sex difference in the prevalence of benzodiazepine misuse.
Women were more likely than men to misuse to cope.
Women reported higher anxiety sensitivity and more drug craving.
The co-use of benzodiazepines with other drugs was reported by 97% of the sample.
Acknowledgments
Role of funding sources
Funding for this study was provided by the Sarles Young Investigator Award, the Charles Engelhard Foundation and NIDA Grant R21 DA046937. These funding sources had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Drs. McHugh, Griffin and Bogunovic and Ms. Geyer and Chase report no potential conflicts of interest or other interests relevant to this manuscript. Dr. Weiss has been a consultant to Indivior, Alkermes, Braeburn Pharmaceuticals, GW Pharmaceuticals, US World Meds, Janssen Pharmaceuticals and Daiichi Sankyo.
References
- Agarwal SD, & Landon BE (2019). Patterns in outpatient benzodiazepine prescribing in the United States. JAMA Netw Open, 2(1), e187399 10.1001/jamanetworkopen.2018.7399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachhuber MA, Hennessy S, Cunningham CO, & Starrels JL (2016). Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996–2013. American Journal of Public Health, 106(4), 686–688. 10.2105/ajph.2016.303061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachhuber MA, Maughan BC, Mitra N, Feingold J, & Starrels JL (2016). Prescription monitoring programs and emergency department visits involving benzodiazepine misuse: Early evidence from 11 United States metropolitan areas. International Journal of Drug Policy, 28, 120–123. 10.1016/j.drugpo.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CJ, Austic E, Epstein-Ngo Q, Veliz PT, & McCabe SE (2015). A prospective study of adolescents' nonmedical use of anxiolytic and sleep medication. Psychology of Addictive Behavior, 29(1), 184–191. 10.1037/adb0000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell CI, Weisner C, LeResche L, Ray GT, Saunders K, Sullivan MD, Banta-Green CJ, Merrill JO, Silverberg MJ, Boudreau D, Satre DD, & Von Korff M (2010). Age and gender trends in long-term opioid analgesic use for noncancer pain. American Journal of Public Health, 100(12), 2541–2547. 10.2105/AJPH.2009.180646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2019). 2018 National Survey on Drug Use and Health: Detailed Tables. Retrieved from Rockville, MD: www.samhsa.gov. [Google Scholar]
- Cleeland CS, & Ryan KM (1994). Pain assessment: Global use of the Brief Pain Inventory. Annals of the Academy of Medicine Singapore, 23(2), 129–138. [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, & Windle M (1992). Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment, 4(2), 123–132. [Google Scholar]
- Dreifuss JA, Griffin ML, Frost K, Fitzmaurice GM, Potter JS, Fiellin DA, Selzer J, Hateh-Maillette M, Sonne SC, & Weiss RD (2013). Patient characteristics associated with buprenorphine/naloxone treatment outcome for prescription opioid dependence: Results from a multisite study. Drug and Alcohol Dependence, 131(1-2), 112–118. 10.1016/j.drugalcdep.2012.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green TC, Grimes Serrano JM, Licari A, Budman SH, & Butler SF (2009). Women who abuse prescription opioids: Findings from the Addiction Severity Index-Multimedia Version® Connect prescription opioid database. Drug and Alcohol Dependence, 103(1-2), 65–73. 10.1016/j.drugalcdep.2009.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudin JA, Mogali S, Jones JD, & Comer SD (2013). Risks, management, and monitoring of combination opioid, benzodiazepines, and/or alcohol use. Postgraduate Medicine, 125(4), 115–130. 10.3810/pgm.2013.07.2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hearon BA, Calkins AW, Halperin DM, McHugh RK, Murray HW, & Otto MW (2011). Anxiety sensitivity and illicit sedative use among opiate-dependent women and men. American Journal of Drug and Alcohol Abuse, 37(1), 43–47. 10.3109/00952990.2010.535581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, & Cranford JA (2012). Motivational subtypes of nonmedical use of prescription medications: Results from a national study. Journal of Adolescent Health, 51(5), 445–452. 10.1016/j.jadohealth.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, DeVito EE, Dodd D, Carroll KM, Potter JS, Greenfield SF, Connery HS, & Weiss RD (2013). Gender differences in a clinical trial for prescription opioid dependence. Journal of Substance Abuse Treatment, 45(1), 38–43. 10.1016/j.jsat.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Fitzmaurice GM, Carroll KM, Griffin ML, Hill KP, Wasan AD, & Weiss RD (2014). Assessing craving and its relationship to subsequent prescription opioid use among treatment-seeking prescription opioid dependent patients. Drug and Alcohol Dependence, 145, 121–126. 10.1016/j.drugalcdep.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Fitzmaurice GM, Griffin ML, Anton RF, & Weiss RD (2016). Association between a brief alcohol craving measure and drinking in the following week: Alcohol craving and drinking. Addiction, 111(6), 1004–1010. 10.1111/add.13311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Geyer R, Karakula S, Griffin ML, & Weiss RD (2018). Nonmedical benzodiazepine use in adults with alcohol use disorder: The role of anxiety sensitivity and polysubstance use. American Journal on Addictions, 27(6), 485–490. 10.1111/ajad.12765. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Votaw VR, Bogunovic O, Karakula SL, Griffin ML, & Weiss RD (2017). Anxiety sensitivity and nonmedical benzodiazepine use among adults with opioid use disorder. Addictive Behaviors, 65, 283–288. 10.1016/j.addbeh.2016.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean CP, Asnaani A, Litz BT, & Hofmann SG (2011). Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research, 45(8), 1027–1035. 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merskey H, & Bogduk N (1994). Classification of chronic pain: Descriptions of chronic pain syndromes and definitions of pain terms (2nd ed.). Seattle: International Association for the Study of Pain Press. [Google Scholar]
- Mueser KT, Nishith P, Tracy JI, DeGirolamo J, & Molinaro M (1995). Expectations and motives for substance use in schizophrenia. Schizophrenia Bulletin, 21(3), 367–378. [DOI] [PubMed] [Google Scholar]
- Olfson M, King M, & Schoenbaum M (2015). Benzodiazepine use in the United States. JAMA Psychiatry, 72(2), 136–142. 10.1001/jamapsychiatry.2014.1763. [DOI] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Cardenas SJ (2007). Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment, 19(2), 176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Votaw VR, Geyer R, Rieselbach MM, & McHugh RK (2019). The epidemiology of benzodiazepine misuse: A systematic review. Drug and Alcohol Dependence, 200, 95–114. 10.1016/j.drugalcdep.2019.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Votaw VR, Witkiewitz K, Valeri L, Bogunovic O, & McHugh RK (2019). Nonmedical prescription sedative/tranquilizer use in alcohol and opioid use disorders. Addictive Behaviors, 88, 48–55. 10.1016/j.addbeh.2018.08.010. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, & Hufford C (1995). Craving in hospitalized cocaine abusers as a predictor of outcome. The American Journal of Drug and Alcohol Abuse, 21(3), 289–301. 10.3109/00952999509002698. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Mazurick C, Berkman B, Gastfriend DR, Frank A, Barber JP, Blaine J, Salloum I, & Moras K (2003). The relationship between cocaine craving, psychosocial treatment, and subsequent cocaine use. AJP, 160(7), 1320–1325. 10.1176/appi.ajp.160.7.1320. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Potter JS, Fiellin DA, Byrne M, Connery HS, Dickinson W, … Ling W (2011). Adjunctive counseling during brief and extended buprenorphine-naloxone treatment for prescription opioid dependence: A 2-phase randomized controlled trial. Archives of General Psychiatry, 68(12), 1238–1246. 10.1001/archgenpsychiatry.2011.121. [DOI] [PMC free article] [PubMed] [Google Scholar]


