Abstract
Background
Despite increasing numbers of older adults undergoing surgery and the known risks of opioids, little is known about the potential association between opioid prescribing and serious falls and fall-related injuries after surgery.
Objective
To determine the incidence and risk factors of serious falls and fall-related injuries after elective, outpatient surgery.
Design
Retrospective cohort study of 20% national sample of Medicare claims among beneficiaries ≥ 65 years of age with Medicare Part D claims and who underwent elective outpatient surgery from January 1, 2009, through December 31, 2014.
Participants
Opioid-naïve patients ≥ 65 years undergoing elective, minor, outpatient surgical procedures. The exposure was opioid prescription fills in the perioperative period (i.e., 30 days before up until 3 days after surgery) converted to total oral morphine equivalents (OME) over a period 30 days prior to and 30 days after surgery.
Main Measures
Serious falls and fall-related injuries within 30 days after surgery, examined through Poisson regression analysis with reported fall and fall-related injury rates adjusted for potential confounders.
Key Results
Among 44,247 opioid-naïve surgical patients, 76.3% filled an opioid prescription in the perioperative period. Overall, 0.62% of patients suffered a serious fall or fall-related injury within 30 days after surgery. Risk factors for serious falls or fall-related injuries after surgery included older age (80–84 years: RR 1.64, 95% CI 1.12–2.40; 85 years and older: RR 1.81, 95% CI 1.25–2.86), female sex (RR 3.04, 95% CI 2.29–4.05), Medicaid eligibility (RR 1.63, 95% CI 1.17–2.26), and higher amounts of opioids filled following surgery (≥ 225 OME: RR 2.29, 95% CI 1.72–3.07).
Conclusions
Serious falls after elective, outpatient surgery are uncommon, but correlated with age, sex, Medicaid eligibility, and the amount of opioids filled in the perioperative period. Judicious prescribing of opioids after surgery is paramount and is an opportunity to improve the safety of surgical care among older individuals.
Electronic supplementary material
The online version of this article (10.1007/s11606-020-06015-6) contains supplementary material, which is available to authorized users.
KEY WORDS: opioid, surgery, older adults, falls
INTRODUCTION
Each year in the USA, more than 25% of adults aged 65 years and older will suffer a fall.1, 2 Falls not only result in morbidity and mortality, but also have significant adverse effects on an individual’s independence and quality of life.2, 3 The high incidence and need for long-term care for older patients who suffer falls lead to substantial healthcare costs. For example, in 2015, medical costs due to older adult falls totaled about $50 billion dollars, and is expected to increase as the population continues to age.4
In addition to longevity, population aging is also associated with a greater prevalence of acute and chronic disease requiring treatment. Although the association of medications with falls among older individuals has been described, much less is known regarding the association of falls and aspects of surgical care.2, 4 Currently, more than half of all patients undergoing surgery are 65 years or older.5 Aging results in physiologic decline in all organ systems,6 which affects not only the metabolism of anesthetic medications7 but also those medications given after surgery such as opioids.8 It is well-established that opioids among older adults can lead to detrimental events such as long bone fractures, cognitive decline, respiratory complications, and mortality among patients on chronic opioid therapy.9–14 However, little is known about the risks of opioids on postoperative falls and fall-related injuries among older adults who are opioid naïve.
Identifying the risks of opioids on older adult falls and fall-related injuries after surgery can provide opportunities to improve the safety of surgical care. In a cohort of Medicare beneficiaries aged ≥ 65 years old undergoing elective, outpatient surgery, we compared postoperative risk of serious falls by opioid dose. We hypothesized that higher doses of opioids prescribed after surgery would be associated with an increased risk of falls and fall-related injuries within 30 days after surgery.
METHODS
Data Sources and Study Population
We identified patients from a 20% national sample of Medicare beneficiaries ≥ 65 years who underwent a surgical procedure between January 1, 2009, and December 31, 2014. We used the Medicare Provider Analysis and Review (MEDPAR), Carrier Claims, Outpatient Claims, and Part D event claim files. This study was deemed exempt by the Human Research Protection Office at the University of Michigan.
We included patients undergoing one of the following elective, outpatient surgical procedures: varicose vein removal, hemorrhoidectomy, laparoscopic cholecystectomy, transurethral prostate surgery, thyroidectomy, parathyroidectomy, carpal tunnel release, umbilical hernia repair, and inguinal hernia repair. Procedures were identified using Current Procedural Terminology Fourth Edition (CPT-4) (Appendix Table 1). To examine outpatient surgery, we only included patients undergoing procedures who were immediately discharged after their procedure or had a 23-h observation admission. If a patient had multiple eligible surgeries, we only included the first surgical and postoperative period.
Opioid initiation was defined as having a pharmacy dispensing claim for any opioid during the exposure window, without any opioid claims during the preceding washout period. The exposure window was defined as the perioperative period from 30 days prior to until 3 days after surgery; patients frequently fill opioid prescriptions prior to surgery to have immediate access to the medication after surgery. The washout period—during which the absence of any opioid prescription was required—was defined as the 365 days to 31 days prior to the exposure window. Therefore, any patient who filled one or more opioid prescriptions within 12 months to 31 days prior to surgery was excluded. To address death or potential censoring events, we applied the inclusion criteria of continuous enrollment in Medicare Parts A, B, and D 12 months prior to and 30 days after their surgical date. Therefore, if a patient passed away during the 30 days after surgery, they were excluded from analysis.
Outcome Assessment
The primary outcome was a serious fall or fall-related injury within 30 days after the surgery date. Using an algorithm commonly described in the literature, we identified a serious fall injury by ICD-9 codes in claims data combined from inpatient and emergency encounters.15–18 Fall-related injuries were also identified according to previously published methods.19
Opioid Medication Exposure
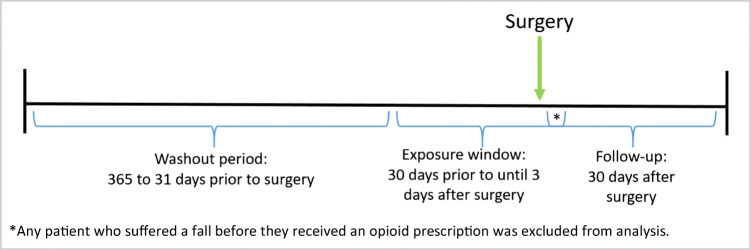
The exposure of interest was filling an opioid prescription in the perioperative period, which was defined as 30 days prior to and 3 days after the surgical date. If a patient filled an opioid prescription in the perioperative period, then the total amount of opioids filled between 30 days prior to and 30 days after surgery was calculated and converted to oral morphine equivalent (OME) units.20 We categorized the total OME over this timeframe (30 days before to 30 days after) as < 150, 150–225, or ≥ 225 units. Study design is outlined in Figure 1.
Figure 1.
Study design schematic. Washout period to identify comorbidities and previous fills of opioids occurred 365 days to 31 days prior to surgery. Exposure to opioids in the perioperative period was defined as 30 days prior to until 3 days after surgery. Follow-up was evaluated 30 days after surgery. An asterisk indicates that any patient who suffered a fall before they received an opioid prescription was excluded from analysis.
Covariates
Baseline covariates included patient age (categorized as 65–69, 70–74, 75–79, 80–84, ≥ 85 years old), sex, race/ethnicity, geographic region of residence based on United States Department of Agriculture (USDA) Economic Research Service Rural-Urban Continuum Codes (metropolitan versus non-metropolitan),21 and Medicaid eligibility. Medicaid eligibility was defined using the State Reported Dual Eligible Status Code. Additionally, we classified the Charlson Comorbidity Index into different groups (i.e., none = 0, mild = 1–2, moderate = 3–4, severe ≥ 5).22 ICD-9-CM diagnosis codes 305.1 and V15.82 were used to identify previous or current tobacco use. Mental health diagnoses included mood disorders, suicidality or self-harm, personality disorders, schizophrenia and other psychotic disorders, substance use disorders (i.e., alcohol and other substance-related disorders), and other mental health disorders (Appendix Table 2).23 Pain disorders defined as those from arthritis, back, neck, or other pain were identified. Healthcare utilization variables included hospitalization and any skilled nursing facility stay within 12 months prior to the patient’s surgical date. Co-prescription with a sedative, hypnotic, or anxiolytic (Appendix Table 3) was identified during the exposure window (30 days prior to up until 3 days after surgery). Frailty index was calculated24 and categorized25 as previously published.
Statistical Analyses
Descriptive statistics were used to describe the demographic and clinical characteristics of the cohort. We estimated the association between total OME units and serious falls and fall-related injuries using multivariate Poisson regression and accounting for clustering within surgeons, resulting in adjusted risk ratios (RR) and 95% confidence intervals (CI). The Poisson distribution was appropriate, and there was no evidence of overdispersion based on the evaluation of deviance or Pearson chi-square statistics.26 Goodness-of-fit chi-square test was performed to evaluate the model fit. We then conducted a sensitivity analysis, based on VanderWeele’s method to estimate potential issues with unmeasured confounders and to assess the robustness of our estimated associations.27 We estimated the minimum strength of association on the risk ratio scale that an unmeasured confounder would need to have with both opioid medication exposure and serious falls to fully explain away the estimated association. Analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC) and Stata version 15.1 (StataCorp, College Station, TX), and statistical significance was defined as p < 0.05.
RESULTS
We identified 44,247 patients who underwent an elective, outpatient procedure between January 1, 2009, and December 31, 2014, and were opioid-naïve during the washout period as previously defined. We summarize demographic and clinical variables in Table 1. The two most common age groups were 70–74 years old (29.2%) and 65–69 years old (26.8%). Most patients in our cohort were male (58.9%). Additionally, majority of patients were White (89.1%) and resided in an urban setting (70.5%). Overall, pain disorders were relatively common; for example, about two-thirds of patients had a diagnosis for arthritis (62.5%) while more than a quarter of patients had a diagnosis of back pain (29.5%).
Table 1.
Demographic and clinical variables of cohort (N = 44,247)
| Characteristics | Overall | Total OME from 30 days prior to 30 days after surgery | |||||||
|---|---|---|---|---|---|---|---|---|---|
| < 150 | 150–225 | ≥ 225 | p value | ||||||
| N | % | N | % | N | % | N | % | ||
| Age, years | < 0.001 | ||||||||
| 65–69 | 11,857 | 26.8 | 3974 | 23.5 | 3110 | 26.3 | 4773 | 30.9 | |
| 70–74 | 12,923 | 29.2 | 4738 | 28.0 | 3399 | 28.7 | 4786 | 31.0 | |
| 75–79 | 9414 | 21.3 | 3690 | 21.8 | 2558 | 21.6 | 3166 | 20.5 | |
| 80–84 | 6209 | 14.0 | 2695 | 15.9 | 1726 | 14.6 | 1788 | 11.6 | |
| ≥ 85 | 3844 | 8.7 | 1846 | 10.9 | 1055 | 8.9 | 943 | 6.1 | |
| Gender | < 0.001 | ||||||||
| Male | 26,071 | 58.9 | 9231 | 54.5 | 7123 | 60.1 | 9717 | 62.9 | |
| Female | 18,176 | 41.1 | 7712 | 45.5 | 4725 | 39.9 | 5739 | 37.1 | |
| Race | < 0.001 | ||||||||
| White | 39,430 | 89.1 | 15,130 | 89.3 | 10,609 | 89.5 | 13,691 | 88.6 | |
| Black | 1514 | 3.4 | 529 | 3.1 | 358 | 3.0 | 627 | 4.1 | |
| Hispanic | 1818 | 4.1 | 728 | 4.3 | 457 | 3.9 | 633 | 4.1 | |
| Other | 1293 | 2.9 | 499 | 3.0 | 370 | 3.1 | 424 | 2.7 | |
| Missing | 192 | 0.4 | 57 | 0.3 | 54 | 0.5 | 81 | 0.5 | |
| Resided in metropolitan county | < 0.001 | ||||||||
| Yes | 31,174 | 70.5 | 12,009 | 70.9 | 8143 | 68.7 | 11,022 | 71.3 | |
| No | 13,008 | 29.4 | 4910 | 29.0 | 3687 | 31.1 | 4411 | 28.5 | |
| Missing | 65 | 0.2 | 24 | 0.1 | 18 | 0.2 | 23 | 0.2 | |
| Division | < 0.001 | ||||||||
| East North Central | 4965 | 11.2 | 1899 | 11.2 | 1302 | 11.0 | 1764 | 11.4 | |
| East South Central | 2039 | 4.6 | 756 | 4.5 | 527 | 4.5 | 756 | 4.9 | |
| Middle Atlantic | 3459 | 7.8 | 1286 | 7.6 | 843 | 7.1 | 1330 | 8.6 | |
| Mountain | 3898 | 8.8 | 1432 | 8.5 | 1113 | 9.4 | 1353 | 8.8 | |
| New England | 6828 | 15.4 | 2728 | 16.1 | 1856 | 15.7 | 2244 | 14.5 | |
| Pacific | 2181 | 4.9 | 745 | 4.4 | 663 | 5.6 | 773 | 5.0 | |
| South Atlantic | 7116 | 16.1 | 2716 | 16.0 | 1711 | 14.4 | 2689 | 17.4 | |
| West North Central | 3507 | 7.9 | 1332 | 7.9 | 788 | 6.7 | 1387 | 9.0 | |
| West South Central | 4304 | 9.7 | 1602 | 9.5 | 1261 | 10.6 | 1441 | 9.3 | |
| Unknown | 5950 | 13.5 | 2447 | 14.4 | 1784 | 15.1 | 1719 | 11.1 | |
| Charlson Comorbidity Index | 0.026 | ||||||||
| None (CCI 0) | 16,062 | 36.3 | 6118 | 36.1 | 4332 | 36.6 | 5612 | 36.3 | |
| Mild (CCI 1, 2) | 17,421 | 39.4 | 6563 | 38.7 | 4723 | 39.9 | 6135 | 39.7 | |
| Moderate (CCI 3, 4) | 7098 | 16.0 | 2780 | 16.4 | 1834 | 15.5 | 2484 | 16.1 | |
| Severe (CCI ≥ 5) | 3666 | 8.3 | 1482 | 8.8 | 959 | 8.1 | 1225 | 7.9 | |
| Medicaid eligibility | 5479 | 12.4 | 1954 | 11.5 | 1395 | 11.8 | 2130 | 13.8 | < 0.001 |
| Any hospitalization in previous year | 4562 | 10.3 | 1865 | 11.0 | 1190 | 10.0 | 1507 | 9.8 | < 0.001 |
| Skilled nursing facility stay in previous year | 561 | 1.3 | 285 | 1.7 | 128 | 1.1 | 148 | 1.0 | < 0.001 |
| History of tobacco use | 3471 | 7.8 | 1230 | 7.3 | 916 | 7.7 | 1325 | 8.6 | < 0.001 |
| Year of surgery | < 0.001 | ||||||||
| 2009 | 6568 | 14.8 | 2585 | 15.3 | 1576 | 13.3 | 2407 | 15.6 | |
| 2010 | 6676 | 15.1 | 2470 | 14.6 | 1666 | 14.1 | 2540 | 16.4 | |
| 2011 | 6753 | 15.3 | 2611 | 15.4 | 1931 | 16.3 | 2211 | 14.3 | |
| 2012 | 7200 | 16.3 | 2774 | 16.4 | 2022 | 17.1 | 2404 | 15.6 | |
| 2013 | 7712 | 17.4 | 2995 | 17.7 | 2083 | 17.6 | 2634 | 17.0 | |
| 2014 | 9338 | 21.1 | 3508 | 20.7 | 2570 | 21.7 | 3260 | 21.1 | |
| Mental health disorders | |||||||||
| Adjustment | 477 | 1.1 | 192 | 1.1 | 133 | 1.1 | 152 | 1.0 | 0.368 |
| Anxiety | 3133 | 7.1 | 1200 | 7.1 | 784 | 6.6 | 1149 | 7.4 | 0.033 |
| Mood | 3650 | 8.3 | 1417 | 8.4 | 918 | 7.8 | 1315 | 8.5 | 0.061 |
| Suicide or self-harm | 34 | 0.1 | 18 | 0.1 | 7 | 0.1 | 9 | 0.1 | 0.213 |
| Disruptive | 97 | 0.2 | 29 | 0.2 | 23 | 0.2 | 45 | 0.3 | 0.055 |
| Personality | 41 | 0.1 | 20 | 0.1 | 8 | 0.1 | 13 | 0.1 | 0.348 |
| Psychosis | 505 | 1.1 | 186 | 1.1 | 132 | 1.1 | 187 | 1.2 | 0.605 |
| Other mental health disorders | 871 | 2.0 | 318 | 1.9 | 238 | 2.0 | 315 | 2.0 | 0.542 |
| Alcohol or substance abuse disorders | 280 | 0.6 | 92 | 0.5 | 68 | 0.6 | 120 | 0.8 | 0.019 |
| Pain disorders | |||||||||
| Arthritis | 27,673 | 62.5 | 11,057 | 65.3 | 7266 | 61.3 | 9350 | 60.5 | < 0.001 |
| Back | 11,411 | 25.8 | 4466 | 26.4 | 3005 | 25.4 | 3940 | 25.5 | 0.095 |
| Neck | 5418 | 12.2 | 2198 | 13.0 | 1412 | 11.9 | 1808 | 11.7 | 0.001 |
| Other pain | 13,182 | 29.8 | 5168 | 30.5 | 3521 | 29.7 | 4493 | 29.1 | 0.019 |
| SHA and opioid filled concurrently during perioperative period | 2129 | 4.8 | 396 | 2.3 | 667 | 5.6 | 1066 | 6.9 | < 0.001 |
| Frailty index | < 0.001 | ||||||||
| Non-frail (FI ≤ 0.1) | 5997 | 13.6 | 2175 | 12.8 | 1665 | 14.1 | 2157 | 14.0 | |
| Pre-frail (0.1 < FI ≤ 0.2) | 33,819 | 76.4 | 12,876 | 76.0 | 9062 | 76.5 | 11,881 | 76.9 | |
| Mildly to severely frail (FI > 0.2) | 4431 | 10.0 | 1892 | 11.2 | 1121 | 9.5 | 1418 | 9.2 | |
OME, oral morphine equivalent; SHA, sedative, hypnotic, or anxiolytic
Among a cohort of opioid naïve patients undergoing surgery, 76.3% filled an opioid prescription in the perioperative period. Additionally, 4.8% of surgical patients also had a concurrent fill for a sedative, hypnotic, or anxiolytic in the perioperative period.
The distributions of total OME over 30 days after surgery were as follows: 38.3% filled < 150 OME, 26.8% filled 150–225 OME, and 34.9% filled ≥ 225 OME (Table 1). Distributions of age (p < 0.001), gender (p < 0.001), race (p < 0.001), type of geographic residence (i.e., rural versus urban) (p < 0.001), location (p < 0.001), comorbidities (p = 0.026), and Medicaid eligibility (p < 0.001) differed significantly across the levels of opioid exposure in the perioperative period. Additionally, there were differences in prior hospitalization (p < 0.001) and stay in skilled nursing facility (p < 0.001) in the previous year, history of tobacco use (p < 0.001), year of surgery (p < 0.001), mental health disorders such as anxiety (p = 0.033) and alcohol or substance abuse disorders (p = 0.019), and arthritis (p < 0.001) and neck pain disorders (p < 0.001) between the groups. Concurrent fill of sedatives, hypnotics, and anxiolytics and opioid analgesics was highest among patients at the highest level of opioid exposure (≥ 225 OME) compared with the other levels of opioid exposure (p < 0.001). Distribution of frailty differed between the three groups of opioid exposure (p < 0.001).
Amounts of Opioids Filled and Incidence of Serious Falls or Fall-Related Injuries After Surgery
Across all surgical patients, 0.62% (273 out of 44,247) suffered a serious fall or fall-related injury within 30 days after surgery. Moreover, the incidence of serious falls and fall-related injuries increased with higher total amounts of opioids (OME) prescribed over 30 days after surgery. For example, the incidence of falls and fall-related injuries among patients who were prescribed ≥ 225 OME was 0.91%, 150–225 was 0.48%, and < 150 was 0.45% (Table 2).
Table 2.
Incidence of serious falls and fall-related injuries within 30 days of surgery by differing amounts of opioids
| Total OME from 30 days prior to 30 days after surgery | N | % |
|---|---|---|
| < 150 | 76 | 0.45 |
| 150–225 | 57 | 0.48 |
| ≥ 225 | 140 | 0.91 |
| Overall | 273 | 0.62 |
OME, oral morphine equivalent
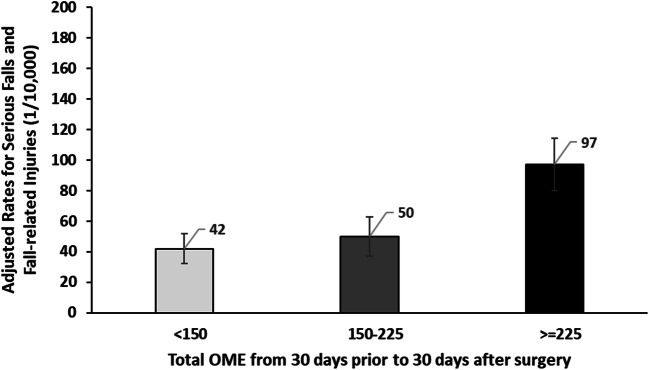
Higher Total Opioid Prescriptions Independently Associated with Serious Falls and Fall-Related Injuries After Surgery
Higher total OME over 30 days before through 30 days after surgery were strongly associated with increased risks of serious falls after surgery (Fig. 2). After controlling for clinical covariates, patients who filled ≥ 225 OMEs after surgery were over twice as likely to fall after surgery compared with the group who filled < 150 OME (≥ 225 OME: RR 2.29, 95% CI 1.72–3.07).
Figure 2.
Adjusted rates for serious falls and fall-related injuries (1/10,000). Higher amounts of opioids (as measured by total OME) filled in the perioperative period increased the risk of serious falls and fall-related injuries after surgery.
Other Factors Contributing to Falls After Surgery
After controlling for demographic and clinical covariates in multivariable analysis, older age was associated with serious falls after surgery (80–84 years: RR 1.64, 95% CI 1.12–2.40; 85 years and older: RR 1.89, 95% CI 1.25–2.86). Females were also more likely to fall than men after surgery (RR 3.04, 95% CI 2.29–4.05). Additionally, patients who were eligible for Medicaid were more likely to suffer a fall or fall-related injury (RR 1.63, 95% CI 1.17–2.26). There were no other covariates that were associated with a risk of serious falls or fall-related injuries after surgery in our multivariable analysis (Table 3).
Table 3.
Poisson regression (clustering within surgeon) for serious falls and fall-related injuries after surgery
| IRR | CI_low | CI_high | p value | |
|---|---|---|---|---|
| Age, years | ||||
| 65–69 (reference) | 1 | NA | NA | NA |
| 70–74 | 1.03 | 0.73 | 1.45 | 0.873 |
| 75–79 | 1.24 | 0.87 | 1.77 | 0.236 |
| 80–84 | 1.64 | 1.12 | 2.40 | 0.011 |
| ≥ 85 | 1.89 | 1.25 | 2.86 | 0.002 |
| Female (male as reference) | 3.04 | 2.29 | 4.05 | < .001 |
| Race | ||||
| White (reference) | 1 | NA | NA | NA |
| Black | 0.47 | 0.21 | 1.08 | 0.075 |
| Hispanic | 0.40 | 0.16 | 0.97 | 0.043 |
| Other | 0.46 | 0.17 | 1.22 | 0.118 |
| Missing | 2.10 | 0.57 | 7.74 | 0.263 |
| Medicaid eligibility (no as reference) | 1.63 | 1.17 | 2.26 | 0.004 |
| Charlson Comorbidity Index | ||||
| None (CCI 0) | 1 | NA | NA | NA |
| Mild (CCI 1, 2) | 0.78 | 0.59 | 1.03 | 0.081 |
| Moderate (CCI 3, 4) | 1.13 | 0.80 | 1.60 | 0.487 |
| Severe (CCI ≥ 5) | 0.77 | 0.46 | 1.28 | 0.31 |
| History of tobacco use | 1.07 | 0.67 | 1.69 | 0.787 |
| At least 1 mental health disorder | 0.88 | 0.64 | 1.23 | 0.463 |
| Pain disorders | ||||
| Arthritis | 1.29 | 0.95 | 1.75 | 0.097 |
| Back | 0.92 | 0.69 | 1.24 | 0.588 |
| Neck | 1.14 | 0.80 | 1.61 | 0.469 |
| Other pain | 0.96 | 0.74 | 1.24 | 0.734 |
| Total OME from 30 days prior to 30 days after surgery | ||||
| < 150 | 1 | NA | NA | NA |
| 150–225 | 1.17 | 0.83 | 1.65 | 0.373 |
| ≥ 225 | 2.29 | 1.72 | 3.07 | < .001 |
| Any hospitalization in previous year | 0.71 | 0.45 | 1.10 | 0.128 |
| Skilled nursing facility stay in previous year | 1.55 | 0.66 | 3.62 | 0.31 |
| Overlapping of SHA and opioid filled during perioperative period | 1.47 | 0.95 | 2.26 | 0.085 |
| Frailty index | ||||
| Non-frail (FI ≤ 0.1) | 1 | NA | NA | NA |
| Pre-frail (0.1 < FI ≤ 0.2) | 0.87 | 0.57 | 1.32 | 0.511 |
| Mildly to severely frail (FI > 0.2) | 1.56 | 0.91 | 2.69 | 0.109 |
Sensitivity Analysis
We assessed the robustness of the estimated incidence rate ratio of exposure to opioids (≥ 225 OMEs, IRR = 2.29; 95% CI 1.72–3.07) by calculating the minimum strength of association that unmeasured confounders would need to have with both opioid medication exposure and having a serious fall or a fall-related injury to explain away the association. The unmeasured confounders would need to be at least 4.01-fold of the risk ratio, a relatively strong confounding association to explain away the relative risk of 2.29. Even the lower bound of the 95% confidence interval, 1.72, would require unmeasured confounders to have a relative risk of 2.83, a reasonably high confounding association, to move the lower bound to include a risk ratio of 1, to demonstrate no statistical significance from the reference group. Given the results of our sensitivity analysis, we conclude that the estimates of association presented here between opioid exposure and serious falls or fall-related injuries are robust.
DISCUSSION
For the first time in US history, older adults aged 65 years and up will outnumber children under 18 years by the year 2035 and will account for more than 20% of the population.28 Currently, older patients already comprise 50% of all surgical patients, and this proportion is only expected to rise over time. Caring for older patients in the perioperative period presents unique challenges for the medical and surgical teams—especially with regard to postoperative pain management. In this study, higher amounts of opioid prescriptions filled in the perioperative period were significantly associated with an increased risk of serious falls and fall-related injuries sustained after elective, outpatient surgery. This association is consistent with prior studies which have identified opioid use as a potential risk factor for falls in the elderly population.28–30 It is possible that the potential adverse effects of opioid therapy, such as sedation and dizziness,31 may compromise coordination and increase the risk of falls, particularly in the older population with a higher prevalence of visual impairment and loss of balance.32 Of note, our analysis indicated that among the opioid-naïve cohort there may be particular sensitivity to the effects of opioid therapy; thus, there may not be sufficient awareness of the potential risks of treatment in these patients compared with those who are maintained on chronic therapeutic doses of opioids.
Fortunately, the incidence of serious falls and fall-related injuries in our population was low (0.62%). As this cohort underwent elective, outpatient procedures, we anticipated that fall rates would be low given that most patients would have had preoperative surgical clearance and review prior to undergoing surgery. Hence, it is worth noting that while this cohort had a relatively low incidence of serious falls and fall-related injuries, they may be less likely to fall compared with patients who are not undergoing surgery.
Opioid prescribing was very common among older patients undergoing elective, outpatient procedures such that more than three-quarters of patients filled an opioid prescription in the perioperative period. These prescription doses were consistently above the now recommended quantities for opioid prescribing for minor procedures. Moreover, 34.9% of patients filled opioid prescriptions containing more than 225 OMEs, which is alarming given that opioids may not even be warranted for pain after these outpatient surgical procedures.33 Although we do not have information regarding patient consumption using claims data alone, higher prescribing of opioids has been shown to be associated with higher consumption.34 While other studies have suggested that adverse events are more likely with higher amounts of opioids prescribed, to our knowledge, this is the first analysis demonstrating a significant association between higher amounts of opioids prescribed and serious falls after surgery. Patients who filled ≥ 225 OMEs (or more than 45 hydrocodone/acetaminophen 5 mg/325 mg) after surgery were over twice as likely to suffer a fall or fall-related injury after surgery compared with the group who filled < 150 OME, which highlights the importance of minimizing opioid prescriptions whenever possible to decrease the risk of serious falls among older patients undergoing surgery.
This analysis also found that females are more likely to fall than men after surgery, which is concordant with other studies.30, 35 This potentially suggests a sex-specific disparity in risk of falls associated with opioid use perioperatively. Additionally, increased age, after controlling for demographic and clinical covariates, was also significantly associated with an increased risk of serious falls or fall-related injuries after surgery. This has also been identified in other studies,35 emphasizing the importance of early recognition of at-risk patients prior to attempting high daily prescription opioid therapy. Going forward, tailoring perioperative pain management therapy in these at-risk populations is an important opportunity to reduce opioid-related risk, and reducing opioid prescribing could reduce this rare, but potentially catastrophic postoperative adverse event. Encouragingly, recent evidence suggests that for many elective, outpatient, relatively minor procedures, opioids may not be necessary or only in low doses for short courses.33, 36, 37
Although surgeons may be prescribing the initial prescription in the perioperative period, non-surgeons involved in the care of these patients are critically important to putting these findings into practice, ultimately reducing the risk of this devastating adverse event after surgery. Best practice guidelines based on patient-reported usage of opioids after surgery are being widely disseminated to surgeons and other surgical providers with hopes that these measures will reduce overprescribing in the perioperative period.38, 39 However, data suggests that a substantial proportion of patients are provided opioid prescriptions in the postoperative period from all provider types.40, 41 For example, nearly one-third of all opioid prescriptions provided to opioid-naïve patients in the first three months after surgery are prescribed by non-surgical providers.40 Therefore, it is imperative for all medical providers to be cognizant that higher opioid doses after elective, outpatient surgery are likely unnecessary and could lead to serious falls and fall-related injuries.
There are several possible limitations of this study. First, this study is an analysis of administrative claims data, as such lacking specificity to determine the extent of pain that patients experience following surgery or more granular patient factors that could be influencing opioid consumption. Therefore, it is impossible to know if the prescription rates are overly high or inappropriately low compared with patient-reported pain scores. Second, from claims data, it is also difficult to discern technical nuances of procedures, as these differ from surgeon-to-surgeon and are not included as details of the database. Third, this dataset only captured falls that ultimately warranted medical care, thus would not have captured less-serious, minor falls which were unreported. Fourth, we did not include the use of non-opioid alternative prescriptions as these are readily available, and patients may have purchased these medications on their own over the counter without insurance coverage. Therefore, the extent to which these alternative therapies may have influenced the utilization of opioids following procedures in these populations cannot be discerned from this analysis. Fifth, this study includes only patients who filled prescriptions, and it is possible that the number of patients who received a prescription, but did not fill the prescription, is actually much higher than reported. In addition, this patient cohort was captured from data reported in the years 2009–2014; thus, the opioid prescribing practices may have been different from those now exhibited in 2020. Additionally, we did not account for effects of polypharmacy or potentially inappropriate medications,42 which certainly could have been associated with increased risk of falls, as others have found.43 Finally, this patient cohort was largely comprised of Medicare beneficiaries, which may not be generalizable to all patients.
CONCLUSIONS
Serious falls and fall-related injuries after elective, outpatient surgery, while uncommon, were associated with older age, sex, Medicaid eligibility, and higher total amounts of opioids filled in the perioperative period. This finding emphasizes the importance of judicious prescribing of opioids for postsurgical pain and represents an opportunity to improve the safety of care among older individuals.
Electronic supplementary material
(DOCX 14 kb)
(DOCX 15 kb)
(DOCX 13 kb)
(DOCX 15 kb)
Acknowledgments
The authors gratefully acknowledge Anne Butler, PhD, MS, who contributed expertise in pharmacoepidemiology and assisted with study design.
Funding Information
This study was supported by the National Institutes of Health (NIH) National Institute on Drug Abuse (NIDA) (R01DA042859) awarded to J.F.W. and C.M.B. K.B.S. was supported, in part, by the NIH National Institute of Neurological Disorders and Stroke (NINDS) (F32NS098561). These funding sources had no role in study design, data collection or analysis, interpretation of data, writing the report, or the decision to submit the findings for publication.
Compliance with Ethical Standards
Conflict of Interest
Dr. Santosa reported no biomedical financial interests or potential conflicts of interest. Ms. Lai reported no biomedical financial interests or potential conflicts of interest. Dr. Brummett reported no biomedical financial interests or potential conflicts of interest. Mr. Oliver reported no biomedical financial interests or potential conflicts of interest. Dr. Hu reported no biomedical financial interests or potential conflicts of interest. Dr. Englesbe reported no biomedical financial interests or potential conflicts of interest. Ms. Blair reported no biomedical financial interests or potential conflicts of interest. Dr. Waljee reported no biomedical financial interests or potential conflicts of interest.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily reflect the official views of the NIH.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hartholt KA, Lee R, Burns ER, van Beeck EF. Mortality From Falls Among US Adults Aged 75 Years or Older, 2000-2016. Jama. 2019;321(21):2131–3. doi: 10.1001/jama.2019.4185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jin J. Prevention of Falls in Older AdultsPrevention of Falls in Older AdultsPrevention of Falls in Older Adults. Jama. 2018;319(16):1734. doi: 10.1001/jama.2018.4396. [DOI] [PubMed] [Google Scholar]
- 3.Al-Aama T. Falls in the elderly: spectrum and prevention. Can Fam Physician. 2011;57(7):771–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J Am Geriatr Soc. 2018;66(4):693–8. doi: 10.1111/jgs.15304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall MJ, Schwartzman A, Zhang J, Liu X. Ambulatory Surgery Data From Hospitals and Ambulatory Surgery Centers: United States. Natl Health Stat Rep. 2010;2017(102):1–15. [PubMed] [Google Scholar]
- 6.Robinson TN, Wu DS, Pointer LF, Dunn CL, Moss M. Preoperative cognitive dysfunction is related to adverse postoperative outcomes in the elderly. J Am Coll Surg. 2012;215(1):12–7. doi: 10.1016/j.jamcollsurg.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang R, Wolfson M, Lewis MC. Unique Aspects of the Elderly Surgical Population: An Anesthesiologist’s Perspective. Geriatric Orthop Surg Rehabil. 2011;2(2):56–64. doi: 10.1177/2151458510394606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Naples JG, Gellad WF, Hanlon JT. The Role of Opioid Analgesics in Geriatric Pain Management. Clin Geriatr Med. 2016;32(4):725–35. doi: 10.1016/j.cger.2016.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dublin S, Walker RL, Jackson ML, Nelson JC, Weiss NS, Von Korff M, et al. Use of opioids or benzodiazepines and risk of pneumonia in older adults: a population-based case-control study. J Am Geriatr Soc. 2011;59(10):1899–907. doi: 10.1111/j.1532-5415.2011.03586.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daoust R, Paquet J, Moore L, Gosselin S, Gélinas C, Rouleau DM, et al. Incidence and Risk Factors of Long-term Opioid Use in Elderly Trauma Patients. Ann Surg. 2018;268(6):985–91. doi: 10.1097/sla.0000000000002461. [DOI] [PubMed] [Google Scholar]
- 11.Makris UE, Abrams RC, Gurland B, Reid MC. Management of persistent pain in the older patient: a clinical review. Jama. 2014;312(8):825–36. doi: 10.1001/jama.2014.9405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Prescription of Long-Acting Opioids and Mortality in Patients With Chronic Noncancer Pain. Jama. 2016;315(22):2415–23. doi: 10.1001/jama.2016.7789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shorr RI, Griffin MR, Daugherty JR, Ray WA. Opioid analgesics and the risk of hip fracture in the elderly: codeine and propoxyphene. J Gerontol. 1992;47(4):M111–5. doi: 10.1093/geronj/47.4.M111. [DOI] [PubMed] [Google Scholar]
- 14.Hanlon JT, Boudreau RM, Roumani YF, Newman AB, Ruby CM, Wright RM, et al. Number and dosage of central nervous system medications on recurrent falls in community elders: the Health, Aging and Body Composition study. J Gerontol A Biol Sci Med Sci. 2009;64(4):492–8. doi: 10.1093/gerona/gln043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bowling CB, Hall RK, Khakharia A, Franch HA, Plantinga LC. Serious Fall Injury History and Adverse Health Outcomes After Initiating Hemodialysis Among Older U.S. Adults. J Gerontol A Biol Sci Med Sci. 2018;73(9):1216–21. doi: 10.1093/gerona/glx260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shimbo D, Barrett Bowling C, Levitan EB, Deng L, Sim JJ, Huang L, et al. Short-Term Risk of Serious Fall Injuries in Older Adults Initiating and Intensifying Treatment With Antihypertensive Medication. Circ Cardiovasc Qual Outcomes. 2016;9(3):222–9. doi: 10.1161/circoutcomes.115.002524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tinetti ME, Han L, Lee DS, McAvay GJ, Peduzzi P, Gross CP, et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174(4):588–95. doi: 10.1001/jamainternmed.2013.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bowling CB, Bromfield SG, Colantonio LD, Gutierrez OM, Shimbo D, Reynolds K, et al. Association of Reduced eGFR and Albuminuria with Serious Fall Injuries among Older Adults. Clin J Am Soc Nephrol. 2016;11(7):1236–43. doi: 10.2215/cjn.11111015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim SB, Zingmond DS, Keeler EB, Jennings LA, Wenger NS, Reuben DB, et al. Development of an algorithm to identify fall-related injuries and costs in Medicare data. Injury Epidemiol. 2016;3(1):1. doi: 10.1186/s40621-015-0066-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Waljee JF, Zhong L, Hou H, Sears E, Brummett C, Chung KC. The Use of Opioid Analgesics following Common Upper Extremity Surgical Procedures: A National, Population-Based Study. Plast Reconstr Surg. 2016;137(2):355e–64e. doi: 10.1097/01.prs.0000475788.52446.7b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.USDA Rural-Urban Continuum Codes. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/. Accessed 1 Sept 2018 2018.
- 22.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 23.Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, et al. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim DH, Schneeweiss S, Glynn RJ, Lipsitz LA, Rockwood K, Avorn J. Measuring Frailty in Medicare Data: Development and Validation of a Claims-Based Frailty Index. J Gerontol A Biol Sci Med Sci. 2018;73(7):980–7. doi: 10.1093/gerona/glx229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orkaby AR, Nussbaum L, Ho YL, Gagnon D, Quach L, Ward R, et al. The Burden of Frailty Among U.S. Veterans and Its Association With Mortality, 2002-2012. J Gerontol A Biol Sci Med Sci. 2019;74(8):1257–64. doi: 10.1093/gerona/gly232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.A. P. Analysis of Count Data Using the SAS System. Proceedings of the SAS Global Forum 2000 Conference. SAS Institute Inc., Cary, NC. https://support.sas.com/resources/papers/proceedings/proceedings/sugi26/p247-26.pdf.
- 27.VanderWeele TJ, Ding P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann Intern Med. 2017;167(4):268–74. doi: 10.7326/m16-2607. [DOI] [PubMed] [Google Scholar]
- 28.Recent opioid use associated with increased risk of falls in older people. Drug and therapeutics bulletin. 2018;56(7):74. doi:10.1136/dtb.2018.7.0638 [DOI] [PubMed]
- 29.Bedson J, Chen Y, Ashworth J, Hayward RA, Dunn KM, Jordan KP. Risk of adverse events in patients prescribed long-term opioids: A cohort study in the UK Clinical Practice Research Datalink. Eur J Pain. 2019;23(5):908–22. doi: 10.1002/ejp.1357. [DOI] [PubMed] [Google Scholar]
- 30.Daoust R, Paquet J, Moore L, Emond M, Gosselin S, Lavigne G, et al. Recent opioid use and fall-related injury among older patients with trauma. CMAJ. 2018;190(16):E500–e6. doi: 10.1503/cmaj.171286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain. 2004;112(3):372–80. doi: 10.1016/j.pain.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 32.Moden B, Merlo J, Ohlsson H, Rosvall M. Psychotropic drugs and falling accidents among the elderly: a nested case control study in the whole population of Scania, Sweden. J Epidemiol Community Health. 2010;64(5):440–6. doi: 10.1136/jech.2009.098947. [DOI] [PubMed] [Google Scholar]
- 33.Howard R, Waljee J, Brummett C, Englesbe M, Lee J. Reduction in Opioid Prescribing Through Evidence-Based Prescribing Guidelines. JAMA Surg. 2018;153(3):285–7. doi: 10.1001/jamasurg.2017.4436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Howard R, Fry B, Gunaseelan V, Lee J, Waljee J, Brummett C, et al. Association of Opioid Prescribing With Opioid Consumption After Surgery in Michigan. JAMA Surg. 2018:e184234. doi:10.1001/jamasurg.2018.4234 [DOI] [PMC free article] [PubMed]
- 35.Pandya U, O’Mara MS, Wilson W, Opalek J, Lieber M. Impact of preexisting opioid use on injury mechanism, type, and outcome. J Surg Res. 2015;198(1):7–12. doi: 10.1016/j.jss.2015.05.033. [DOI] [PubMed] [Google Scholar]
- 36.Rose KR, Christie BM, Block LM, Rao VK, Michelotti BF. Opioid Prescribing and Consumption Patterns following Outpatient Plastic Surgery Procedures. Plast Reconstr Surg. 2019;143(3):929–38. doi: 10.1097/prs.0000000000005351. [DOI] [PubMed] [Google Scholar]
- 37.Grandizio LC, Zhang H, Dwyer CL, Goldberg SH, Klena JC. Opioid Versus Nonopioid Analgesia After Carpal Tunnel Release: A Randomized, Prospective Study. Hand (New York, N.Y.). 2019:1558944719836211. doi:10.1177/1558944719836211 [DOI] [PMC free article] [PubMed]
- 38.Howard R, Vu J, Lee J, Brummett C, Englesbe M, Waljee J. A Pathway for Developing Postoperative Opioid Prescribing Best Practices. Ann Surg. 2020;271(1):86–93. doi: 10.1097/sla.0000000000003434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vu JV, Howard RA, Gunaseelan V, Brummett CM, Waljee JF, Englesbe MJ. Statewide Implementation of Postoperative Opioid Prescribing Guidelines. N Engl J Med. 2019;381(7):680–2. doi: 10.1056/NEJMc1905045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Klueh MP, Hu HM, Howard RA, Vu JV, Harbaugh CM, Lagisetty PA, et al. Transitions of Care for Postoperative Opioid Prescribing in Previously Opioid-Naïve Patients in the USA: a Retrospective Review. J Gen Intern Med. 2018;33(10):1685–91. doi: 10.1007/s11606-018-4463-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cron DC, Lee JS, Dupree JM, Syrjamaki JD, Hu HM, Palazzolo WC, et al. Provider Characteristics Associated With Outpatient Opioid Prescribing After Surgery. Ann Surg. 2020;271(4):680–5. doi: 10.1097/sla.0000000000003013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.American Geriatrics Society 2019 Updated AGS Beers Criteria(R) for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674-94. doi:10.1111/jgs.15767 [DOI] [PubMed]
- 43.Montero-Odasso M, Sarquis-Adamson Y, Song HY, Bray NW, Pieruccini-Faria F, Speechley M. Polypharmacy, Gait Performance, and Falls in Community-Dwelling Older Adults. Results from the Gait and Brain Study. J Am Geriatr Soc. 2019;67(6):1182–8. doi: 10.1111/jgs.15774. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 14 kb)
(DOCX 15 kb)
(DOCX 13 kb)
(DOCX 15 kb)