Abstract
Purpose:
COVID-19 related pan- India lockdown brought teleophthalmology to the forefront. The study ventures to understand the relevance of this modality in a government setup. The objective is to understand the feasibility, clinical profile and addressability of patients using teleconsultation in ophthalmology at a tertiary care government medical university during the COVID-19 Lockdown in India.
Methods:
An online survey targeting faculty members and resident doctors in a tertiary eye center in a government medical university in north India was conducted. Various aspects of teleconsultation were analyzed including the number and preferential mode of consultations, commonest complaints and diagnoses made. Frequency and factors mandating physical examination of patients was also analyzed.
Results:
The questionnaire was sent to 40 ophthalmologists of whom 38 responded. A total of 4880 teleconsultations were given. The commonest mode of communication was by WhatsApp messages (65.6%) and E-mail was the least preferred medium. More than 80% consultations were from previously seen patients. Red eye was the commonest presenting complaint (22.8%), followed by watering (18.7%) and foreign body sensation (14.5%). Computer vision syndrome was the commonest diagnosis (25.9%) followed by conjunctivitis (17.7%) and refractive error (17.7%). About 40% required physical examination, mostly due to uncertain diagnosis (22%) or inadequate response to prescribed treatment (19%).
Conclusion:
Teleconsultation was feasible in a government medical university for providing ophthalmic services during lockdown. WhatsApp was the preferred communication modality, computer vision syndrome was the most frequent tentative diagnosis and approximately 60% did not require in-person physical examination.
Keywords: COVID-19, lockdown, novel coronavirus, teleconsultation, teleophthalmology
Pan-India lockdown with intent to control the spread of novel Corona Virus (COVID-19) was an unprecedented phase for the routine healthcare services where the out-patient departments (OPD) throughout the country were shut and the patients were advised to visit the hospital only in case of dire emergency.[1,2]
In view of the foregoing, the Ministry of Health and Family Welfare of India acknowledged the necessity of delivering healthcare through use of telemedicine.[3] As a result of this, teleophthalmology which the majority of ophthalmologists hitherto refrained from using came to the forefront. Teleophthalmology implies use of telecommunication to facilitate ophthalmic care delivery at a distance, usually remote areas where health facilities are not accessible.[4] In conventional teleophthalmology, as we knew till now, a paramedic or a trained worker was available at the remote location to capture the information whereas in the current situation the entire information was provided by the patient or the attendant themselves.[3] Moreover, before these times teleophthalmology was used as a supplement to conventional ophthalmology but in these times it served as a substitute. We felt that analysis of these consultations could provide useful information for future development of this technology. This survey was thus conducted at our tertiary care center to address the relevance of teleconsultation in Ophthalmology during the initial 50 days of pan-India lockdown.
Methods
The survey-based descriptive cross-sectional study was conducted at department of Ophthalmology in a tertiary care government medical university of north India catering to a large rural and urban population primarily of low socio-economic status. The target group for survey included all the faculty members and the residents. The online link was disseminated to the 40 potential participants through WhatsApp, text messages and e-mails on 14th May 2020. The survey tool used was www.surveymonkey.com. It comprised of ten questions [Annexure 1] and addressed two broad areas: firstly, the respondents' feedback on feasibility of using teleconsultation; and secondly, the clinical profile of the consulting patient and addressability of their problems. In questions where multiple responses were sought, each response was to be given equal weightage e.g., for a question where each of the 40 respondents gave 3 responses, a total of 120 responses were analysed.
The survey questions and options were designed by the investigators based on sample of 20 patients who had been given teleconsultation. They were modified after responses and suggestions from 5 other ophthalmologists who attempted the survey in an initial study. These ophthalmologists and investigators were excluded from answering the final survey. While acquiring the response, the participants were acquainted with the subject “teleconsultation during COVID-19 lockdown” and a short message appreciating about the critical value of their input in research with emphasis on the anonymity of the response was circulated. The message also indicated that the survey would take 2 minutes to complete. The platform was then closed on 17th May 2020. As no identification details of either the patients or the respondent were collected ethical clearance was not sought. Statistical Analysis: SPSS software was used for statistical analysis. The association between categorical variables was assessed using Fisher exact test or Chi-squared test. P value <0.05 was considered statistically significant.
Results
Out of the 40 invited members, 38 (95%) participated in the online survey. The participants were asked if they had given any teleconsultation during the lockdown period. 32 (84%) participants indicated that they had used one or more available media for teleconsultation. Six (15.7%) participants who denied giving any teleconsultation were asked to indicate the reason for the same. Most common reason observed for not using the facility was the concern for possible legal implications in 3 (50%) cases. Two (33.3%) participants declared unavailability of the technology, while one (16.6%) did not trust the modality. These respondents were requested not to participate in the survey further [Fig. 1].
Figure 1.
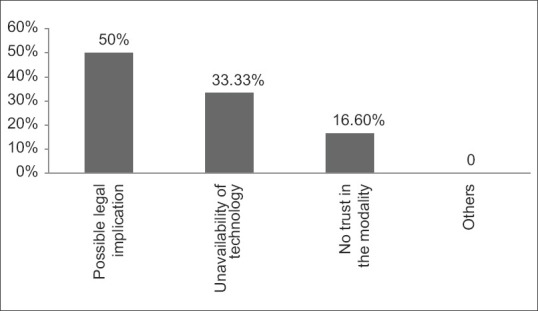
Graph showing reasons for reluctance in using teleconsultation by participants
Approximately, 4880 tele-consultations were given by 32 doctors during 50 days lockdown period with an average of 3 consultations per doctor per day. The patients reached out to the doctors directly or through the departmental landline number through which they were redirected to the respective clinician. 65.6% (n = 21) considered WhatsApp as the most preferred medium followed by Voice call by 18 (56.25%), video call by three (9.38%), phone based application by one (3.13%) in that order. None preferred e-mail for giving consultation. Thirty-one (96.8%) doctors indicated that <20% new patients sought consultation. Only one response was outside this range (p-value 0.003) indicating that majority of consultations (approximately 80%) sought were from already registered (old) patients.
The respondents were asked about the clinical profile of the consulting patients. They were asked to indicate three most common presenting complaints and clinical diagnoses made by them. Overall, the three most common complaints of the patients were redness, watering and foreign body sensation as indicated by 22 (22.8%), 18 (18.7%) and 14 (14.5%) responses respectively [Fig. 2]. The three most common diagnoses were computer vision syndrome/dry eyes, conjunctivitis and refractive error made in 25 (25.9%), 17 (17.7%) and 17 (17.7%) of responses, respectively. The details of clinical profile have been graphically represented [Fig. 3].
Figure 2.
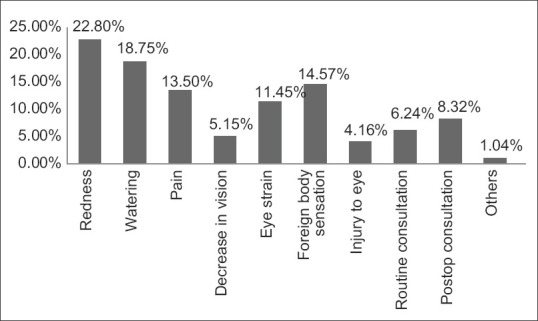
Graph showing frequency of presenting complaints of patients
Figure 3.
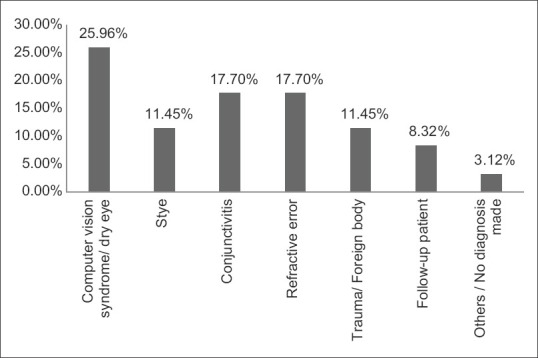
Graph showing frequency of probable diagnosis made by participants
About 40% patients were advised physical examination. Amongst those who were advised so, the frequent reasons indicated were difficulty in diagnosis in 22 (22.8%), not relieved by earlier treatment in 19 (19.7%) and severe trauma in 10 (10.4%) responses, respectively [Fig. 4].
Figure 4.
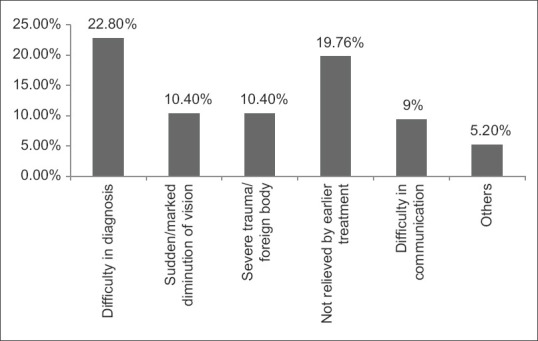
Graph showing reasons for advising physical examination of the patients
Discussion
As the world stands wrecked by novel corona virus pandemic, the healthcare delivery dwindles with an unforeseen and unique challenge of nationwide lockdown in many countries including India. With the routine out-patient departments and elective surgeries suspended, the patients can approach for in-patient care only in emergency situations.[5] Ophthalmologists had to bear the brunt of the disease in its early spread in December, when one such specialist got infected and succumbed to death in Wuhan.[6] This unveiled the possible risk of disease transmission through ocular route.[7,8,9] With this impending peril, tele ophthalmology, which was a mere bystander for over a decade, has taken a centre stage in routine health care delivery. This virtual care modality has been brought to forefront to mitigate the need of proximity of patient and the ophthalmologist. It served as a lifeline for about 2 months when conventional services were hampered. It was used for the first time by many patients and doctors, but it is easy to predict that it would be used more frequently in the coming times.
The reason for reluctance of 15.7% doctors to use this modality was their concern about the associated legal liability. Communications were made by the governing bodies, encouraging its use but clear directive by the Medical Council of India (MCI) would be helpful in increasing its popularity.[3]
With the routine OPD closed for almost 2 months, 4880 teleconsultations were given during this period. This number, although less as compared to the pre lockdown OPD consultations (approximately 12,500) given in the same duration, is still satisfactory given the grimness of the ongoing pandemic. The possible reasons for reduced consultations during lockdown could be deferring non-emergency conditions by the patients, lack of mobility, apprehension towards visiting a hospital, poor means of communication at the patient's end, unawareness amongst the rural section which forms the major subset of footfalls in our centre and patients' apprehension about the data confidentiality. This also explains the reduced number of new patients advised through teleconsultation during the lockdown period. The government institutions' OPD prescription unlike that of private practitioners' seldom bears a contact number. Adding a phone number in prescriptions and publicising the same may increase the usage.
All teleconsultations were given free of cost. The most preferred modality indicated by the majority of participants was through WhatsApp messages. WhatsApp messages allow convenience of sharing images which not only overcomes the limitation of verbal communication but also compensates for a gross torch light view of the eye. William AM et al. in their recently published study reported virtual video calls as an effective tool for triage as well as management of low-risk cases.[10] Video call provides facility of real-time interaction with the patient but needs high quality connectivity at both the ends. Furthermore, ensuring privacy and synchronous convenience of time in video consults are a concern. The least preferred mode indicated in our study was email probably because of the infrequent usage and inconvenience in cross questioning.[3] In a survey conducted by Nair AG et al. telephonic consultation (54.9%) was the most preferred mode of consultation, followed by social media apps like WhatsApp and telegram while video calls were least preferred.[11] Das AV et al. emphasised on the use of browser-based electronic medical records system (eyeSmart EMR) for ease of recording and retrieving the patients' data.[12,13,14]
The common presenting complaints were redness, foreign body sensation and watering. This was similar to that reported by Das AV et al. in their study.[12] The frequent probable diagnoses made included computer vision syndrome, conjunctivitis and refractive error. The plausible reason for increased number of cases with computer vision syndrome is the compulsion to stay at home during lockdown which increased the screen time i.e., the time spent using the smartphone, television or computer screen.[15]
Unlike as in routine OPD settings, not all patients seeking teleconsultation required physical examination. About 60% consultations were successfully managed without it. Among those requiring face to face consultation, majority comprised of those not adequately responsive to prescribed treatment, with severe ocular trauma, with sudden/marked diminution of vision or in whom the information available through teleconsultation was inadequate to reach a presumptive diagnosis. Thus, only a fraction of those consulting through virtual means were called for in-patient review at the centre. This “triage” of patients significantly reduces the burden on the traditional eye care delivery. It is the clinical discretion of the attending ophthalmologist to decide whether the virtual advice is sufficient or in-patient review is essential.
Teleophthalmology is not without limitations. The virtual technology cannot supersede in- person clinical examination. There is a pertinent risk of diagnostic error and impending medicolegal implications. The data security and confidentiality are other issues that need to be tackled. The technology, although in an accelerating phase, requires innovations to cater the less reached out patients from the low socio-economic strata. Nevertheless, the usefulness of leveraging this modality cannot be underestimated in this global pandemic crisis where minimising the risk of exposure is an utmost priority.[16]
The findings of this study can provide guidelines for development of mobile applications and triage of patients by ophthalmologists. Moreover, this also suggests that routine use of telemedicine is a feasible option even in delivering day to day eye care facilities even in government hospital primarily catering to lower socioeconomic strata. Widespread availability of mobile phones and social media applications can be used effectively in establishing patient-doctor interaction without compromising social distancing. It can also serve as a guide for symptoms of patients who can be communicated that sudden or marked decrease in vision, trauma and absence of relief after initial teleconsultation requires physical examination.
Limitations of this study include recall bias, heterogeneous skill of respondents ranging for junior residents to experienced consultants and a small study group.
Conclusion
During lockdown in India, teleconsultation in a government university was feasible, WhatsApp was the preferred modality, computer vision syndrome the commonest diagnosis and up to 60% of the patients did not require physical examination.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Annexure 1: Survey Questions
Feasibility
-
Have you given any teleconsultation during lockdown period?
-
a)Yes
-
b)No
-
a)
-
If you answered Yes to Question No 1, skip this question. If the answer was No, what was the reason for not giving teleconsultation? Multiple options may be marked.
-
a)Concerned about legal implications
-
b)Do not trust the modality
-
c)Unavailability of technology
-
d)Others
-
a)
An approximate number of consultations given per day?
-
Most preferred means of consultation (Select 1)
-
a)WhatsApp
-
b)Voice Call
-
c)Video Call
-
d)Email
-
e)Any other phone based application (App) or website
-
f)Others
-
a)
-
Least preferred means of consultation (Select 1)
-
a)WhatsApp
-
b)Voice Call
-
c)Video Call
-
d)Email
-
e)Phone based application (App) or website
-
f)Others
Patient Profile
-
a)
-
Percentage of patients seeking 1st-time consultation from you (New patients)
-
a)<10%
-
b)10-20%
-
c)20- 50%
-
d)>50%
-
a)
-
Most frequent complaints of the patient? Select any 3
-
a)Redness
-
b)Watering
-
c)Pain
-
d)Decrease in vision
-
e)Eye strain
-
f)Foreign body sensation
-
g)Injury to eye
-
h)Routine consultation
-
i)Post-operative consultation
-
j)Others
-
a)
-
Probable diagnoses made by you. Select 3 most frequent
-
a)Computer vision syndrome/dry eye
-
b)Stye
-
c)Conjunctivitis
-
d)Refractive error
-
e)Trauma/Foreign body
-
f)Follow up patient
-
g)Others/No diagnosis made
Addressability
-
a)
What percentage of patients were advised a physical examination?
-
Amongst the patients advised physical examination what were the commonest reasons? Select 3 most frequent
-
a)Difficulty in diagnosis
-
b)Sudden or marked decrease in vision
-
c)Severe trauma/foreign body
-
d)Not relieved by earlier treatment
-
e)Difficulty in communication
-
f)Others
-
a)
References
- 1.Coronavirus [Internet] World Health Organization. World Health Organization; Available from: https://wwwwhoint/emergencies/diseases/novel-coronavirus-2019 . Last cited on 2020 May 17. [Google Scholar]
- 2.Khanna RC, Cicinelli MV, Gilbert SS, Honavar SG, Murthy GS. COVID-19 pandemic: Lessons learned and future directions. Indian J Ophthalmol. 2020;68:703–10. doi: 10.4103/ijo.IJO_843_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Telemedicine [Internet] Ministry of health and family welfare. 2020. Available from: https://wwwmohfwgovin/pdf/Telemedicinepdf . Last cited on 2020 May 17.
- 4.Prathiba V, Rema M. Teleophthalmology: A model for eye care delivery in rural and underserved areas of India? Ann Fam Med. 2011:683267. doi: 10.1155/2011/683267. doi: 10.1155/2011/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Recommendations for urgent and nonurgent patient care [Internet] American Academy of Ophthalmology. 2020. Available from: https://wwwaaoorg/headline/new-recommendations-urgent-nonurgent-patient-care . Last cited on 2020 May 17.
- 6.LiWenliang [Internet] Enwikipediaorg 2020 Wikipedia. Available from: https://enwikipediaorg/wiki/Li_Wenliang (doctor) Last cited on 10 June 2020.
- 7.Lu CW, Liu XF, Jia ZF. 2019 nCoV transmission through the ocular surface must not be ignored. Lancet (London, England) 2020;395(10224):e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang D, Xu H, Rebaza A, Sharma L, Dela Cruz CS. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir Med. 2020;8:e13. doi: 10.1016/S2213-2600(20)30066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coronavirus kills Chinese whistleblower ophthalmologist [Internet] American Academy of Ophthalmology. 2020. Available from: https://wwwaaoorg/headline/coronavirus-kills-chinese-whistleblower-ophthalmol . Last cited on 2020 May 17.
- 10.Williams AM, Kalra G, Commiskey PW, Bowers EMR, Rudolph BR, Pitcher MD, et al. Ophthalmology practice during the coronavirus disease 2019 pandemic: The University of Pittsburgh experience in promoting clinic safety and embracing video visits. Ophthalmol Ther. 2020;6:1–9. doi: 10.1007/s40123-020-00255-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: Results of a survey. Indian J Ophthalmol. 2020;68:725–30. doi: 10.4103/ijo.IJO_797_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Das AV, Rani PK, Vaddavalli PK. Tele-consultations and electronic medical records driven remote patient care: Responding to the COVID-19 lockdown in India. Indian J Ophthalmol. 2020;68:1007–12. doi: 10.4103/ijo.IJO_1089_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reeves JJ, Hollandsworth HM, Torriani FJ, Taplitz R, Abeles S, Tai-Seale M, et al. Rapid response to COVID 19: Health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc. 2020;27:853–9. doi: 10.1093/jamia/ocaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kammari P, Ambadker MC, Loomba A, Deepthi N, Shravani M, Vadapalli R, et al. A novel technology tool to capture the clinical information of patients across rural vision centers in a three-tier eye care network in India using the eyeSmart EMR App. Rural Remote Health. 2019;19:5255. doi: 10.22605/RRH5255. [DOI] [PubMed] [Google Scholar]
- 15.Krishna T, Panag LGHS, Philip SA. WFH, online classes, binge watching during lockdown have started another 'outbreak' [Internet] ThePrint. 2020. Available from: https://theprintin/ health/wfh online classes binge-watching-during-lockdown-have-started-another-outbreak/419060 . Last cited on 17 May 2020.
- 16.Saleem SM, Pasquale LR, Sidoti PA, Tsai JC. Virtual ophthalmology: Telemedicine in a Covid 19 era. Am J Ophthalmol. 2020 doi: 10.1016/j.ajo.2020.04.029. S0002 9394(20)30214-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


