Abstract
Ocular pain is a common complaint which forces the patient to seek immediate medical attention. It is the primeval first response of the body to any severe condition of the eye such as trauma, infections and inflammation. The pain can be due to conditions directly affecting the eye and ocular adnexa; or indirect which would manifest as referred pain from other organ structures such as the central nervous system. Paradoxically, there are several minor and non-sight threatening conditions, which also leads to ocular pain and does not merit urgent hospital visits. In this perspective, we intend to provide guidelines to the practising ophthalmologist for teleconsultation when a patient complains of pain with focus on how to differentiate the various diagnoses that can be managed over teleconsultation and those requiring emergency care in the clinic. These guidelines can decrease unnecessary hospital visits, which is the need of the hour in the pandemic era and also beyond. Patients who are under quarantine and those who are unable to travel would be benefitted, and at the same time, the burden of increased patient load in busy hospital systems can be reduced.
Keywords: COVID-19 pandemic, differential diagnosis of ocular pain, ocular pain, telemedicine, teleophthalmology
Ocular pain is one of the most common causes for the patient referral to the emergency clinic.[1] The origin of pain could be from the eye or referred to the eye due to shared innervation with the trigeminal nerve. Some conditions in ophthalmology have classic symptomatology for pain and other associated features such as decreased vision, congestion and photophobia which can lead to a presumptive diagnosis. While examination in the clinic is ideal, it may not be possible always. The patient may be located in a remote area or there may be lack of availability of ophthalmologist. Such a situation is common in countries where the ratio of ophthalmologist to patient can be far lower in a rural versus urban setting. Thomas et al. reported the ophthalmologist-patient ratio in urban India was 1:25,000, but in rural India, it was 1:1:250,000.[2]
Teleconsultation in medicine has been popular in various streams since several years world-over.[3,4] In Indian ophthalmology, its use was limited to community ophthalmology. Now diabetic retinopathy and retinopathy of prematurity (RoP) screening via telemedicine are being routinely used in many institutes.[5,6] With the current pandemic situation due to the COVID-19 infection around the world, the scope and utility of teleophthalmology can be expanded to include screening of the patients' complaints of pain and thus categorize the patient as an ocular emergency or to be scheduled for routine care. The patient can use a smart phone device to take external photographs of his/her eye and share the same by “WhatsApp” or other similar portals. In simpler conditions, a hospital visit can be avoided altogether by providing simple medical advice over the teleconsultation, decreasing the potential risk of COVID-19 spread.
Many protective measures and guidelines has been developed after emergence of COVID-19 infection. But as per recommendation by the WHO, social distancing is the only possible effective tool to stop its transmission.[7] Ophthalmology clinics are restricting patients numbers to prevent the spread of infection to both patients and healthcare workers. In the absence of vaccines or definitive treatment, it is expected that the disease may be recrudescent in crops and continue even as long as for two years.[8] Teleconsultation, if used effectively and on a large scale, would help reduce the load of patients in the clinic. In this article, we describe the role of teleconsultation for diagnosis of ocular pain. This review will cover most of the common differential diagnoses causing ocular pain.
Process of tele-ophthalmology and instructions for taking photographs with a smart phone
The telephone numbers for teleconsultation should be prominently displayed on the entrance to the premises and updated in print media, official websites or in social media. Based on the availability of personnel in the hospital or the practice, the management can decide on who can answer the call (either doctor or the phone call can be triaged by the hospital staff). In the case of established practices, an electronic consent and a payment gateway can also be created. The doctor will then proceed to take the history and determine the complaints of the patient as pertaining to pain. While on call, the doctor can provide simple instructions for taking a photograph of the eye using the patient's smart phone as follows:
The room illumination should be adequate, and the patient should be facing the light source, such as standing against a window (in case of photophobia, the patient may be able to open the eye only for a short while). The flash should be turned on
The “zoom” of the camera should be turned up to 2-2.5 times
If the patient is taking his/her own picture: the “selfie mode” can be used, but the regular mode is better
The phone should be held horizontal and about 4 inches away from the eye, moving the phone closer to the eye gradually with the patient's eye looking into the camera located in the back of the phone 4 inches away
The person taking the photo should ensure that the eye is well centred and in focus
The sender should first review the picture to ensure the image is clear before sending it
Based on the condition, the patient/attendant may be asked to take pictures whilst looking in various gazes, or of the eyelids etc
Alternatively, the patient can be asked to send a small video clip looking in various gazes.
Ocular trauma
Blunt or penetrating trauma to the eye is a frequently reported ocular emergency. The patient would give a history of injury, and would have mild to moderate or severe pain, based on the nature and force of the injury and the extent of ocular damage. The pain would be in and around the eye and orbit, with swelling of lids, ecchymosis, congestion and subconjunctival haemorrhage [Fig. 1a]. Lacerations could be located in the lid [Fig. 1b] or could include conjunctival tears, corneal lacerations, scleral tears, and globe rupture. The globe could appear disfigured especially in the case of blow out fractures of the orbit. The patient would also report decreased vision, which could be due to penetrating injuries or due to corneal edema, hyphema, lens involvement including traumatic cataract and ruptured lens capsule [Fig. 1c and d], vitreous haemorrhage, retinal detachment, commotio retinae and traumatic optic neuropathy. In the case of trauma, teleophthalmology has a limited role in treatment and the patient would have to report to the hospital immediately.
Figure 1.
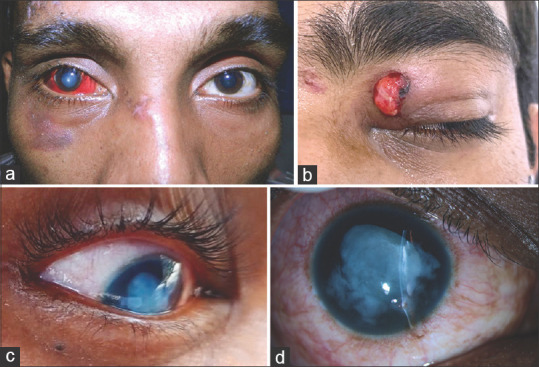
(a-d) A.50-year old man with pain after injury, note subconjunctival haemorrhage, steamy cornea, dislocated lens into the anterior chamber. (b) Sudden onset pain following trauma to his left eye in a 29-year old. Left upper lid ptosis, with a lid laceration and soft tissue prolapse are noted. He subsequently underwent repair. (c and d) A 23-year-old complained of severe pain after broomstick injury. The image, although of poor quality, shows white matter in the anterior chamber (hydrated lens matter) (c). He was later noted to have ruptured lens capsule and cortical matter in AC (d)
Ocular surface, conjunctiva and cornea
Conjunctival and corneal non-infectious conditions start with pricking sensation and dull pain which is intense on eye movements as the disease progresses. Unlike other ocular causes of pain, the patient's pain is alleviated with instillation of topical anesthesia due to pain abolishment. Redness, watering and discharge are hallmarks for anterior segment and ocular surface diseases. Additional symptoms may indicate a specific disease process such as: itching and eye rubbing with mucoid discharge and sectoral bulbar congestion point towards allergic eye disease. Acute onset mild pain/irritation with diffuse conjunctival congestion mild discharge indicates viral or bacterial conjunctivitis.
Conjunctival or corneal foreign body
Activities such as hammering, or grinding can result in penetrating trauma and retained intraocular foreign body. Sub-tarsal foreign body should be suspected when the patient has pain on lid movements and is located only on lid eversion. The patient with visible conjunctival non-impacted foreign bodies can be instructed to remove the same with a clean bud gently and washing the eye with clean potable water thereafter, only in the scenario that the patient is unable to visit the hospital. Corneal foreign bodies and deeper conjunctival foreign bodies are best attended to at the hospital emergency room and removal should not be attempted in a non-hospital setting.
Recurrent corneal erosions (RCE)
RCEs usually present acutely with severe pain in the eye and exacerbates on lid movements. It classically occurs on awakening due to sudden forceful opening of lids against the cornea. Past injury with sharp object like fingernail or paper may be elicited, where it would be unilateral or in corneal epithelial or basement membrane dystrophies where bilateral involvement is noted.[9] The patient can be advised to use lubricating eye drops and rest the eye by keeping it closed. In any case, the patient would need to visit the hospital for further management.
Dry eyes
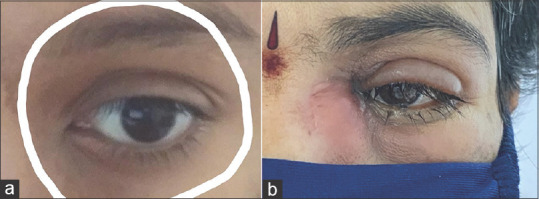
Patients often complain of discomfort due to nociceptive kind of pain, along with sandy/gritty sensation and dryness [Fig. 2a and b]. In severe stages of dry eyes, there is severe pain secondary to ocular surface punctate erosions.[10] Occupational history such as computer professionals, history of prior refractive surgery, and history of systemic conditions such as rheumatoid arthritis or symptoms of dry mouth should be enquired. Milder cases can be managed over teleconsultation.
Figure 2.
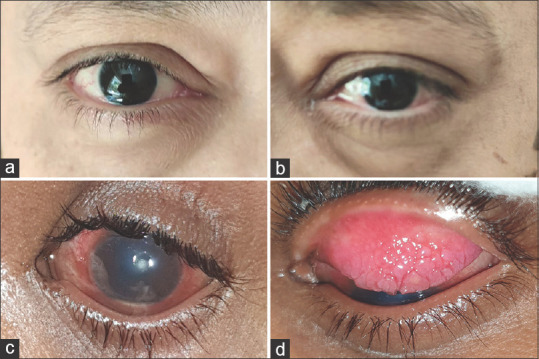
(a and d) A 45 year old lady complained of bilateral gritty sensation, mild pain and eye rubbing. Mild conjunctival congestion was noted temporally in both eyes, but other findings were normal. She was diagnosed as dry eye, and improved with lubricants. (c and d) 12-year-old child with acute severe pain and unable to open the eye sent this picture which showed dense congestion, central corneal lesion and hypopyon (c). Examination in the emergency clinic conformed infected shield ulcer. Lid eversion showed giant papillae (d), characteristic for vernal keratoconjunctivitits
Pain in children
Children usually cannot express pain and hence it is important to know some of the common causes of pain in children for effective management. These include conjunctival or corneal foreign bodies, allergic eye diseases and phlycten. Allergic eye disease is usually seen in young children, with a chief complaint of eye rubbing. Moderate or severe pain with discharge and photophobia suggest development of shield ulcer or corneal involvement and suggest severe allergic disease [Fig. 2c and d]. Usually, the upper tarsal conjunctival giant papillae can lead to mechanical ptosis of the upper lid which may be noted in the external photograph. Acute onset pain with localized circumcorneal congestion and whitish ulcer is noted with phlycten. It is usually seen with blepharitis or systemic diseases such as tuberculosis. It responds well with topical steroids. The patient would need to be seen in the hospital.
Microbial keratitis
Pain from microbial keratitis is severe due to the rich innervation of cornea. There is associated lid edema, severe congestion, watering, photophobia, defective vision and white spot. Only in rare situations, pain may not be severe (such as in viral neurotrophic keratitis). Lid edema, congestion, corneal scar, hypopyon, and presence of infiltrate can be judged from a good quality photo. However, micro-perforation and depth of the infiltrate is difficult to assess from an image unless it is a descemetocele. Bacteria and fungi together constitute a major portion of the etiology of microbial keratitis [Fig. 3a]. The ophthalmologist can often be incorrect in making a presumptive diagnosis based on symptoms. Microbiological work-up is considered as the gold standard for diagnosis and management of microbial keratitis patient and has to be done at the earliest. While disproportionate pain has been described in Acanthamoeba keratitis, in Indian patients, severe pain is not reported.[11] In HSV keratitis, the epithelial form (dendritic ulcer) and necrotizing stromal keratitis are the commonest manifestations where patients would present with acute pain and may have previous such episodes or presence of previous corneal scar.[12] In the case of Herpes zoster ophthalmicus (HZO) and keratitis, the classical feature of initial vesicular rash and radicular pain along the ophthalmic dermatome, preceded by a prodrome of burning, dysesthesia and pain should be enquired for on history. Localized pain in and around the eye can occur secondary to keratitis or uveitis [Fig. 3b]. Post-herpetic neuralgia also occur and lasts for years following complete resolution of the skin rashes.[13] On suspicion of HZO, the patient should be immediately counselled for hospital visit in order to promptly start appropriate therapy and avoid post-herpetic neuralgia and corneal complications. In all cases of infectious keratitis, the patients need to visit the clinic.
Figure 3.
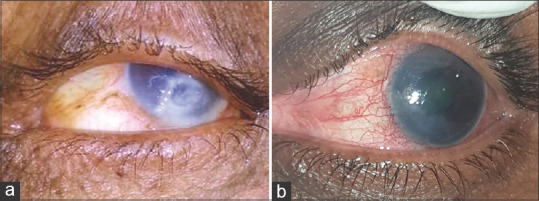
(a) Digital picture of a 62-year-old one-eyed patient who complained of severe pain in his left eye following trauma one week ago and loss of vision. The left eye shows an inferior large infiltrate with central thinning and epithelial defect. He was advised to rush immediately to the hospital for further care. (b) 50-year-old patient with history or recurrent severe pain and decreased vision with past history of being diagnoses and treated for HZO with keratouveitis. The shared picture shows evident congestion and corneal haziness due to edema. The patient was advised to start topical corticosteroids and follow up as soon as possible
To summarize, in infectious keratitis, only small (infiltrate < 1 mm), non-visual threatening lesions can be started on initial therapy (broad spectrum antibiotics) till the patient reaches the clinic. With repeated consultation over the next 12-24 hours, and sharing of photographs of the patient's eye, a few cases can be managed especially in those situation where the patient cannot travel due to lock-down, or is from a highly exposed pandemic area. The other utility of teleconsultation is for follow up. Once the initial consultation has been completed at the clinic, and appropriate microbiological work up is performed, the patient can be started on appropriate therapy and followed up till resolution. Repeat hospital visits can be avoided by daily teleconsultations.
Glaucoma
Glaucoma is usually a painless disease, which has earned it the sobriquet of “silent thief of sight.” In primary open angle glaucoma (POAG), steroid induced glaucoma, creeping ACG, and juvenile open angle glaucoma (JOAG), the Intraocular Pressure (IOP) may be higher but pain is not noted due to the chronic nature. However, there are certain situations in which glaucoma does present with pain and this is usually an ophthalmic emergency. The pain in glaucoma is related to the rapid rise of IOP. Acute angle closure glaucoma (ACG) and secondary glaucomas are more likely to present with pain. Sudden severe pain in the affected eye, with blurred vision (due to corneal edema) and coloured haloes are characteristics of sudden rise of IOP. These halos are seen at twilight, typically around the headlights of oncoming cars and are described as blue-green central and red-orange in the periphery. The pain may be referred to the orbit, head, ears, sinuses, and even teeth (along the distribution of the trigeminal nerve). Autonomic stimulation may result in complaints of nausea, vomiting, sweating, and bradycardia which may at times result in presentations to the general emergency wards before ophthalmic consultation is sought. In a patient with ocular and constitutional symptoms as described above reports with pain, the ophthalmologist should think about glaucoma. If unilateral, the patient can be asked to palpate and compare the two eyes and assess if one eye feels harder than the other. Glaucomatous pain cannot be managed over tele-ophthalmology but instead the patient would definitely need to report to the hospital. In primary angle closure glaucoma, conjunctival congestion, steamy cornea, shallow anterior chamber, vertically oval pupil and some degree of iris sphincter atrophy are present and some of these features may be picked up on a well taken close up picture of the eye. The other eye angles would also be narrow.[14] Certain drugs likeTopiramate can cause secondary angle closure, present with dull or severe pain and blurred vision due to acquired myopia.[15] Hypertensive uveitis would accompanied by ciliary pain and tenderness.[16] Migraine can be associated with normal tension glaucoma.[17]
In summary, the cause of ocular pain may sometimes be glaucoma. While the diagnosis cannot be made for certain (except for acute angle closure in some cases) based on teleconsultation. However, the ophthalmologist may gain several clues from teleophthalmology.
Epicleritis and scleritis
Episcleritis
Episcleritis is inflammation of the vascularised tissue between conjunctiva and sclera. This self-limiting disease is not associated with any complications or visual loss. The condition usually subsides within 2-21 days.[18] The patient would have mild to no pain, or might report tenderness of the affected site. The patient typically reports redness of the eye first noted by family members, rather than the patients themselves, and recurrent episodes are common [Fig. 4a]. This condition can be treated on tele-consultation with thorough review of history and pain. It has been our clinical observation that this condition was a commonly sought reason for teleconsultation and could be managed successfully without hospital visits.
Figure 4.
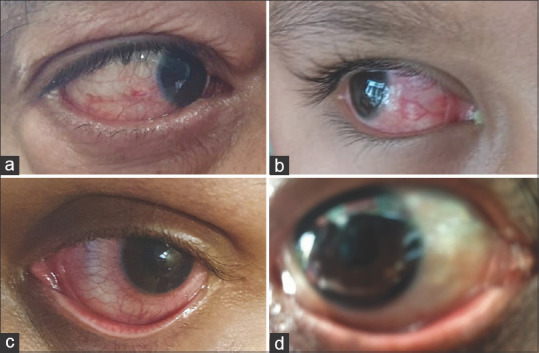
(a) Smart-phone picture of a 52 year-old-man with mild pain and redness since the past one month with recurrent episodes. The photograph shows diffuse congestion of the temporal episcleral vessels. (b) A 7-year-old boy noted history of severe pain and redness for one week. The photograph shows deep congestion nasally, which was diagnosed as scleritis. (c) A 25-year-old man with recurrent episodes of redness and pain, photophobia, who was being treated as conjunctivitis, the picture taken by the patient shows circumcorneal congestion. With a presumptive diagnosis if uveitis, he was asked to report to the hospital where the diagnosis was confirmed. (d) A 45-year old man reported severe pain since waking up. He was a known patient diagnosed previously as severe dry eye with filamentary keratitis, with chronic ocular graft versus host disease. The photograph sent by the patient is blurred and does not help reach any presumptive diagnosis
Scleritis
Scleritis is characterised by painful inflammation and occurs due to auto-immune process or secondary to infection. If untreated, it can lead to local tissue destruction and visual loss. It is one of the most painful ocular condition and is to be taken care of as an emergency. It is insidious in onset and usually severe in almost all cases (except is some cases of scleromalacia perforans). Analgesics provide only fleeting relief. The patient complains of the pain radiating to the forehead, ear, face, scalp and jaw. It can be severe enough to awaken the patient from sleep at night. Touching the temple or the eye can trigger severe pain and sometimes there can be painful eye movements especially in posterior scleritis.[19,20] During teleconsultation, it is very important to ask the patient to take photographs of the eye not just in primary gaze, but in all gazes with the lids retracted, in order not to miss the pattern of congestion [Fig. 4b]. Recent history of trauma or surgery to the eye and appearance of a lesion either at the incision site or the injury site can suggest a possible infective etiology. However, management of scleritis would require hospital visits and cannot be managed over teleconsultation.
Uveitis
The pain in uveitis is more often dull aching or throbbing type.[21] Recurrent episodes, subsiding with topical steroids would be characteristic. Acute inflammation causes irritation of the ciliary nerves leading to spasm of ciliary muscles and therefore pain. Specific uveitis entities such as HLA B-27 uveitis, herpetic uveitis or Zoster can also be very painful.[22] Typical history of pain and photophobia, with a densely congested eye without discharge suggest a differential diagnosis of anterior uveitis. The pattern of congestion can be picked up with an external photograph also [Fig. 4c]. The most frequent misdiagnosis is conjunctivitis (especially in anterior uveitis). Pain in the initial stages is mild in conjunctivitis and gets moderate with associated photophobia if cornea is involved. In addition, conjunctivitis would have lid edema, matting of eye lashes and typical watery or purulent discharge. Other diagnoses to be considered on tele-ophthalmological consultation are other causes of acute red eye such as episcleritis, scleritis, drug toxicity, and angle closure glaucoma. During tele-ophthalmology, not all pictures sent by the patient would be clear enough [Fig. 4d] to differentiate the exact pathology and in case of doubt, the patient would need to visit the hospital.
Retinal diseases
Retina is one of the few structures in the body which does not have pain receptors. Hence even if the retina develops tears or detachment there are no symptoms of pain.
Ocular ischemic Syndrome (OIS) may present with pain in 40% of its cases.[23] This may be either due to elevated IOP or ischemia. Pain is usually dull, aching and insidious, and may radiate from periorbital area to face and head and is worse when upright. Since OIS may involve systemic conditions like carotid artery stenosis or giant cell arteritis (GCA), a multidisciplinary approach involving the physician and neurologist is necessary.[23,24] Hence, a hospital visit is essential and urgent considering the likelihood of other systemic comorbidities.
Post-operative endophthalmitis is a rare but serious condition. 75% of the patients present with pain within a week of surgery, hence excess pain in a post-operative patient can be alarming symptom.[25] The pain is severe and can be associated with nausea and vomiting (due to sudden rise in IOP), sudden drop in vision, discharge and swelling of eye lid and adnexa and it necessitates immediate consultation. Endophthalmitis can occur after cataract surgery, glaucoma surgery or even after intravitreal injections.[26] In cases where the patient cannot follow up after surgery, instructions regarding dangerous symptoms should be explained. Teleconsultation should ideally not be a replacement for routine follow-up visits in the long run, but during lockdown periods or those patients suddenly exposed to the COVID-19 virus or in a quarantined patient, telemedicine may be the only consultation available.
Conditions causing severe panuveitis such as Vogt Koyanagi Harada Disease (VKH) in its prodromal phase may be characterised by orbital pain and flu-like illness, followed by bilateral blurring of vision. Examination would show classical features of multiple serous retinal detachments, hyperaemia and edema of disc,[27] but can only be diagnosed after a hospital visit and teleconsultation can help prioritize it at the earliest.
Acute retinal necrosis (ARN) is another severe panuveitic entity (infectious in origin) that may be associated with periorbital pain secondary to inflammation or scleritis followed by loss of vision and warrants emergency visit.[28]
Retinal conditions due to trauma: any penetrating injury needs urgent evaluation at hospital. Blunt trauma can lead to commotio retinae, retinal detachment, macular hole, vitreous haemorrhage. Though all these conditions are painless, trauma per se can cause pain. Diagnosing and treating the retinal sequelae of ocular trauma requires urgent hospital visit.
Neuro-ophthalmology
So far, majority of the conditions discussed above present with pain emanating from the affected eye. However in neuro-ophthalmology conditions, pain can be in the orbital areas accompanied by headache. The most common neurophthalmic conditions associated with eye pain are described.
Optic neuropathies
In optic neuritis the typical pain is acute and dull, with decreased brightness and faded colours;[29] localising to retroorbital, periocular or orbital area with worsening on eye movements (papillitis[30] and visual loss noted subsequently.
In both papilledema and Idiopathic Intracranial Hypertension (IIH), the pain is chronic and dull. The hallmark feature is an associated severe headache which is worse in the morning attributable to raised intracranial pressure.[30,31]
While Non Arteritic Ischemic Optic Neuropathy (NAION) is generally painless, in GCA there is characteristic temporal dull boring pain which precedes the onset of visual loss by a couple of weeks. This pain may be associated with severe temporal headache, scalp tenderness, jaw claudication and pain while chewing.[32]
Eye pain in cranial nerve palsies
In isolated third nerve palsy, there is unilateral stabbing pain with ptosis, outward and downward deviation of the eye [Fig. 5a and b]. In fourth nerve involvement, trochleitis leads to pain on movements and tenderness in the superonasal area.[33] Multiple cranial nerve involvement such as III, IV, V1, V2 and VIth indicates involvement of the cavernous sinus. These lesions are associated with a stabbing eye pain and a severe headache. The lesions involving the cavernous sinus with characterisation of pain can be grouped as ischemic/compressive (malignant infiltration, lymphoma, infection, cavernous sinus thrombosis) and inflammatory (Tolosa Hunt syndrome).[33,34] An MRI of the brain remains the cornerstone for establishing the correct diagnosis. Horner syndrome has unilateral ptosis and miosis with which may be accompanied with ipsilateral decrease in the corneal sensations.[35]
Figure 5.
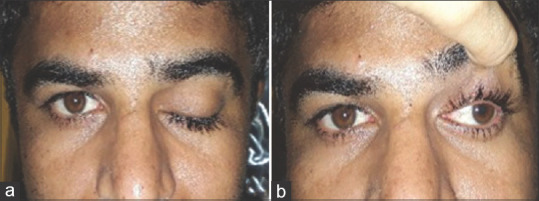
(a and b) 35-year old man with sudden onset pain and complete drooping of his left eye lid. The picture shows complete ptosis of his left eye (a) and on elevating the lid, the outward position of the eye is very evident (b). The anisocoria is also evident suggesting the diagnosis of third nerve palsy involving the pupil
Eye pain in ocular asthenopia
Uncorrected refractive errors, latent strabismus, anomalies of accommodation and convergence can lead to ocular asthenopia. Asthenopia refers to frontal or periorbital dull chronic eye pain, eye fatigue and burning sensation of eyes associated with frontal headache or brow ache exacerbated with visual effort. Teleconsultation may not aid the primary diagnosis. However, the availability of online software programmes for correcting orthoptic anomalies may be useful in monitoring the resolution of anomalies of accommodation and fusion.
Eye pain in migraine
Migraine is a common headache syndrome which presents as episodic severe unilateral hemicranial headache, variably associated with nausea, vomiting, phonophobia and photophobia. An increased incidence of dry eye disease is found to exist in individuals with migraine, which could be a cause of eye pain in these patients.[36]
To summarize, in this era of pandemic, teleconsultation may help in reducing the clinic visits in neurophthalmic conditions. Based on the initial symptoms, a differential diagnosis can be considered and preliminary investigations can be advised which include appropriate neuroimaging even prior to a physical consultation in some cases, or the patient can be triaged directly to the neurologist. Appropriately guided nine gaze photographs or evaluating ocular motility through video conferencing may aid in diagnosis of the cranial nerve palsies and redirecting them towards the systemic investigations for the suspected etiology, thus cutting down on hospital visits.
Eyelid, orbit and ocular adnexa
Similar to neuro-ophthalmology, in conditions involving the eyelids, adnexa or orbit, the pain may be located around the eye or may be referred pain from the orbit, sinuses or the cranial cavity.[37] Infections and inflammation are commonly associated with pain. Hordeolum or stye[38] is a common cause of lid pain, which has a simple management that helps expedite the resolution of the inflammation.[39] The condition can be easily diagnosed on teleconsultation with the help of a photograph. Eyelid massage for pus point, warm compresses and topical antibiotic ointments help in local control. Other causes of eyelid pain include preseptal cellulitis, which can be diagnosed and managed on teleconsultation as it is frequently allergic and can resolve with oral analgesics and antihistaminics [Fig. 6a].
Figure 6.
(a) 25 year old female with complaints of left eye sharp/stabbing pain around the left eye with diffuse swelling since 1 day. The picture shows mild edema and ptosis of her left upper eyelid. She was diagnosed as preseptal cellulitis and the condition subsided with oral antibiotics and analgesics. (b) Digital photograph of the patient's left eye showing acute dacryocystitis presenting with severe pain, swelling and erythema over the lacrimal area and lid edema and discharge
Orbital cellulitis is a common complication of sinusitis and can be associated with sight threatening and intracranial complications.[40] Pain, fever, and malaise are noted. Proptosis, limited extra-ocular motility, chemosis and a dilated pupil suggest orbital involvement. The patients would need to be called in for urgent care as this condition requires an urgent imaging study, CT or MRI is indicated in these patients.
Orbital inflammations such idiopathic orbital inflammatory disease (IOID) and thyroid eye disease (TED) can present with pain.[41] In case of frank features such as proptosis, eyelid retraction, conjunctival congestion and chemosis are noted on teleconsultation, a baseline thyroid function test should be advised, and the patient should report for further management.
Complaints of painful ophthalmoplegia with signs of ocular inflammation[42] can be due to orbital myositis. Dacryoadenitis is the most common inflammatory lesion of the lacrimal gland,[43] with the patient having mild pain and “S” shaped eyelid and inflammatory signs around the lacrimal gland. Orbital vascular lesions, typically the veno-lymphatic malformations, can sometime present with acute proptosis and pain.[43] Rupture of macrocyst or veno-lymphatic malformation (VLM) leads to chocolate cyst causing acute pain, proptosis and exposure keratopathy.[44] Panophthalmitis is an acute, painful, purulent infection of all the coats of the eye and can be secondary to endophthalmitis.[45] The pain is often so severe[46] that it can be relieved only by evisceration. Admission and systemic antibiotics followed by systemic steroids are recommended. Adenoid cystic carcinoma is the most common primary epithelial malignancy of the lacrimal gland.[47] Due to perineural invasion, patients often present with pain. Proptosis with downward and medial displacement of the globe may be seen. Acute dacryocystitis[48] [Fig. 6b] presents with pain, erythema of the skin over the lacrimal sac, tearing, discharge and at times abscess formation (which would be very painful), and a draining fistula. Once the acute inflammation resolves dacryocystorhinostomy may be considered. However, nasal surgery during the current coronavirus epidemic carries a higher risk of aerosol transmission and awaiting resolution with medical treatment in the acute phase seems to be advantageous.
In summary, since teleconsultations in eyelid, orbit and adnexal diseases can be instituted by reviewing external photographs of the patients and the dependence on visual acuity testing is relatively limited, tele-ophthalmology seems to hold promise in reducing the requirement for patient travel and the risks involved therein.
Conclusion
With detailed knowledge of various causes of ocular pain and their characteristics, as outlined in this perspective, teleconsultation can be used to triage patients with pain. Tables 1 and 2 show the various diseases and the feasibility of diagnosis and management of these conditions on teleconsultation. While it cannot replace physical examination in the clinic, one can diagnose and manage specific mild conditions. It also has a significant utility in follow-up cases. We recommend that ophthalmologists can use the questionnaire for ophthalmic history (Appendix 1: Pain questionnaire), and also utilize the flow chart (Appendix 2: Flow chart) as a quick reckoner for the diagnosis of the condition based on the characteristics of pain. Managing mild cases via teleconsultation has its advantages both for the patient and the health care system. However, there are several limitations of teleophthalmology. Active participation of the patient and family is needed and they should have a minimum technical knowledge and resources for sharing images. Photographs and even video calls do not provide as much information as can be gained by slit lamp examination and important tests such as intraocular pressure measurement are not possible. Furthermore, several other issues such as informed consent of the patient, payment for the consultation, medico-legal liability for the treating doctor and prescription of medication, needs further deliberation and policy formation. Despite all of these limitations, triaging patients based on ocular pain is still a useful modality to decrease patient travel especially during the COVID-19 pandemic era.
Table 1.
Teleconsultation in the diagnosis, initial and follow up management of intraocular conditions related to ocular pain
| Anatomical location | Diagnosis | Diagnosis on tele-consultation | Initial investigations or management on tele-consultation | Follow-up management on tele-consultation |
|---|---|---|---|---|
| Conjunctiva | Conjunctivitis | Yes | No | No |
| Retained conjunctival foreign body | Yes | No | Yes | |
| Allergic keratoconjunctivitis | Yes | Yes (mild cases only) | Yes | |
| Dry Eyes | Yes | Yes (mild cases only) | ||
| Phlyctenular keratoconjunctivitis | Yes | No | No | |
| Cornea | Microbial keratitis | Yes | Infiltrate <1 mm – Yes Infiltrate >1 mm - No |
Infiltrate <1 mm-Yes Infiltrate >1 mm - No |
| Corneal foreign body | Yes | No | Yes | |
| Recurrent corneal erosions | Yes | Yes (mild cases only) | No | |
| Filamentary keratitis | Yes | No | No | |
| Superior limbic keratoconjunctivitis | Yes | No | No | |
| Stevens Johnsons syndrome sequael | Yes | No | No | |
| Glaucoma | All types | No | No | No |
| Sclera | Episcleritis | Yes | Yes | Yes |
| Scleritis | Yes | No | No | |
| Uvea | Uveitis | Yes | No | No |
| Retina and Vitreous | Ocular Ischemic Syndrome | No | No | No |
| Endophthalmitis | Can suspect | No | No | |
| Vogt Koyanagi Harada Syndrome | No | No | No | |
| Acuter retinal necrosis | No | No | No | |
| Trauma urgent referral | Yes | No | No |
Table 2.
Teleconsultation in the diagnosis, initial and follow up management of neuro-ophthalmic, eyelid, adnexa and orbital conditions related to ocular pain
| Anatomical location | Diagnosis | Diagnosis on tele-consultation | Initial Investigations, management on tele-consultation | Follow-up management on tele-consultation |
|---|---|---|---|---|
| Neurophthalmology | 1. Optic neuropathies | No | No | No |
| 2. Cranial Nerve palsies | Yes | No | No | |
| 3. Ocular Asthenopia | Possible | Yes | Yes | |
| 4. Migraine | Possible | Yes | Yes | |
| Eyelid, Orbit and Ocular Adnexa | 1. Stye | Yes | Yes | Yes |
| 2. Preseptal cellulitis | Yes | Yes | Yes | |
| 3. Orbital cellulitis | Yes | No | Yes | |
| 4. Orbital inflammations | Yes | Yes (mild cases only) | Yes | |
| 5. Panophthalmitis | Yes | No | Yes | |
| 6. Orbital tumors | Yes (some cases) | No (may need surgical intervention) | Yes | |
| 7. Acute dacryocystitis | Yes | No | Yes |
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
For Somasheila I Murthy, Sujata Das and Tarjani V Dave: Hyderabad Eye Research Foundation.
Conflicts of interest
There are no conflicts of interest.
Appendix 1: Pain questionnaire
Teleconsultation Questionnaire
-
Demographic profile :
Age
Gender
Occupation – Are you working from home with excessive laptop/desktop usage ?
-
History of presenting illness : Ocular Pain –
- Only one eye or both eyes affected ?
-
Site : Where is the pain
- Inside the eye ?
- Around the eye ?
- Behind the eye ?
- Headache ?
- Does the location of pain move ?
-
Duration of pain
- Since how many days are you experiencing the pain ?
- How was the onset of pain – sudden or gradual ?
- Is the pain transient or permanent ? If transient – what is the frequency and onset to peak ?
- Is this the first episode or you have had similar problem before – did you consult an eye doctor that time ?
- Was the pain preceded by any particular event (trauma/fingernail injury etc) ?
- What is the severity of pain ? Mild/Moderate/Severe
-
What is the nature of pain ?
- Sharp/stabbing
- Scratchy/sandy/gritty sensation
- Dull ache/boring
- Feeling something is inside your eye (foreign body sensation) ?
- Does the pain worsen with the movement of eyes ?
-
Associated ocular/systemic symptoms ?
- Is there associated vision loss /blurred vision ?
- Have u ever noticed coloured haloes around light especially in twilight ?
- Is there accompanying redness / discharge /crusting of eyelids
- Is there associated watering of eyes ?
- Do you also experience itching /eye rubbing ? If yes – Is it occasional / frequent ?
- Do you have difficulty in opening of eyelids / intolerance to light ?
- Is there accompanying nausea/ vomiting ?
- Any associated cold/cough/fever/running nose ?
- Is there associated double vision ?
- Do you feel your eye movements are limited ?
- Do you feel your eyes are appearing bigger/bulging ?
- Is there associated scalp tenderness / jaw claudication / pain on chewing /facial pain
- If headache – describe the nature and site of headache
- Any aggravating /relieving factors ?
- Any particular time of the day when pain is worse ?
Do you wear glasses ? How old are the glasses ? Do you have a prescription ? Read out the number for the same / send a snapshot
Do you use contact lenses ? Are you still wearing them ? If no since how many days have you discontinued ?
Have you undergone any eye surgery? When ? Please send a snapshot of the discharge summary if available .
Have you instilled any eye drops/medications for the pain ? Which – if possible send a snap shot ? Was it in consultation with a doctor ? How many times have you put it ? Is there any relief or worsening with it ?
-
Are you on long term eye medications –
- Name : If possible send a snapshot along with the prescription ?
- Since when
- How do you store these drops ?
- Did you check the expiry date ?
- When were the current drops opened ?
-
Any systemic history of
- Diabetes mellitus
- Hypertension
- Hyper/Hypothyroidism
- Ischemic heart disease
- Tuberculosis
- Any other systemic illness/medications ?
Are you allergic to any medications ?
If a female – ask for LMP ?
Any family history of glaucoma ?
Are you getting adequate sleep of 7-8 hours ?
Can you click a picture of both eyes one by one and send ?
Appendix 2: Flow chart
Flow chart
References
- 1.Siegfried I, Jacobs J, Olympia RP. Adult emergency department referrals from urgent care centers. Am J Emerg Med. 2019;37:1949–54. doi: 10.1016/j.ajem.2019.01.029. [DOI] [PubMed] [Google Scholar]
- 2.Thomas R, Paul P, Rao GN, Muliyil JP, Mathai A. Present status of eye care in India. Surv Ophthalmol. 2005;50:85–101. doi: 10.1016/j.survophthal.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 3.Jerant AF, Epperly TD. Fundamentals of telemedicine. Mil Med. 1997;162:304–9. [PubMed] [Google Scholar]
- 4.Wootton R, Loane M, Mair F, Moutray M, Harrisson S, Sivananthan S, et al. The potential for telemedicine in home nursing. J Telemed Telecare. 1998;4:214–8. doi: 10.1258/1357633981932262. [DOI] [PubMed] [Google Scholar]
- 5.Avidor D, Loewenstein A, Waisbourd M, Nutman A. Cost-effectiveness of diabetic retinopathy screening programs using telemedicine: A systematic review. Cost Eff Resour Alloc. 2020;18:16. doi: 10.1186/s12962-020-00211-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vinekar A, Mangalesh S, Jayadev C, Gilbert C, Dogra M, Shetty B. Impact of expansion of telemedicine screening for retinopathy of prematurity in India. Indian J Ophthalmol. 2017;65:390–5. doi: 10.4103/ijo.IJO_211_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coronavirus Disease 2019 (COVID-19): Symptoms of Coronavirus. Centre for Disease Control and Prevention (CDC) [Last accessed on 2020 Apr 13]. Available from: https://wwwcdcgov/coronavirus/2019-ncov/symptoms-testing/symptomshtml .
- 8.Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860–8. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Das S, Seitz B. Recurrent corneal erosion syndrome. Survey Ophthalmol. 2008;53:3–15. doi: 10.1016/j.survophthal.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 10.Belmonte C, Nichols JJ, Cox SM, Brock JA, Begley CG, Bereiter DA, et al. TFOS DEWS II pain and sensation report. Ocul Surf. 2017;15:404–37. doi: 10.1016/j.jtos.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma S, Garg P, Rao GN. Patient characteristics, diagnosis, and treatment of non-contact lens related Acanthamoeba keratitis. Br J Ophthalmol. 2000;84:1103–8. doi: 10.1136/bjo.84.10.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Valerio GS, Lin CC. Ocular manifestations of herpes simplex virus. Curr Opin Ophthalmol. 2019;30:525–31. doi: 10.1097/ICU.0000000000000618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leisegang TJ. Herpes zoster virus infection. Curr Opin Ophthalmol. 2004;15:531–6. doi: 10.1097/01.icu.0000143686.68103.46. [DOI] [PubMed] [Google Scholar]
- 14.Rao A, Padhy D, Das G, Sarangi S. Evolving paradigms in classification of primary angle closure glaucoma. Semin Ophthalmol. 2017;32:228–36. doi: 10.3109/08820538.2015.1053620. [DOI] [PubMed] [Google Scholar]
- 15.Murphy RM, Bakir B, O'Brien C, Wiggs JL, Pasquale LR. Drug-induced bilateral secondary angle-closure glaucoma: A literature synthesis. J Glaucoma. 2016;25:99–105. doi: 10.1097/IJG.0000000000000270. [DOI] [PubMed] [Google Scholar]
- 16.Baneke AJ, Lim KS, Stanford M. The pathogenesis of raised intraocular pressure in uveitis. Curr Eye Res. 2016;41:137–49. doi: 10.3109/02713683.2015.1017650. [DOI] [PubMed] [Google Scholar]
- 17.Danias J, Podos SM. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Am J Ophthalmol. 1999;127:623–5. doi: 10.1016/s0002-9394(99)00088-4. [DOI] [PubMed] [Google Scholar]
- 18.Diaz JD, Sobol EK, Gritz DC. Treatment and management of scleral disorders. Surv Ophthalmol. 2016;61:702–17. doi: 10.1016/j.survophthal.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 19.Oray M, Meese H, Foster CS. Diagnosis and management of non-infectious immune-mediated scleritis: Current status and future prospects. Expert Rev Clin Immunol. 2016;12:827–37. doi: 10.1586/1744666X.2016.1171713. [DOI] [PubMed] [Google Scholar]
- 20.Watson PG. Doyne memorial lecture, 1982.The nature and the treatment of scleral inflammation. Trans Ophthalmol Soc UK. 1982;102:257–81. [PubMed] [Google Scholar]
- 21.Agrawal RV, Murthy S, Sangwan V, Biswas J. Current approach in diagnosis and management of anterior uveitis. Indian J Ophthalmol. 2010;58:11–9. doi: 10.4103/0301-4738.58468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rathinam SR, Namperumalsamy P. Global variation and pattern changes in epidemiology of uveitis. Indian J Ophthalmol. 2007;55:173–83. doi: 10.4103/0301-4738.31936. [DOI] [PubMed] [Google Scholar]
- 23.Mendrinos E, Machinis TG, Pournaras CJ. Ocular ischemic syndrome. Surv Ophthalmol. 2010;55:2–34. doi: 10.1016/j.survophthal.2009.02.024. [DOI] [PubMed] [Google Scholar]
- 24.Carroll SC, Gaskin BJ, Danesh-Meyer HV. Giant cell arteritis. Clin Exper Ophthalmol. 2006;34:159–73. doi: 10.1111/j.1442-9071.2006.01186.x. [DOI] [PubMed] [Google Scholar]
- 25.Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol. 1995;113:1479–96. [PubMed] [Google Scholar]
- 26.Shah CP, Garg SJ, Vander JF, Brown GC, Kaiser RS, Haller JA Post-Injection Endophthalmitis (PIE) Study Team. Outcomes and risk factors associated with endophthalmitis after intravitreal injection of anti-vascular endothelial growth factor agents. Ophthalmology. 2011;118:2028–34. doi: 10.1016/j.ophtha.2011.02.034. [DOI] [PubMed] [Google Scholar]
- 27.Read RW, Holland GN, Rao NA, Tabbara KF, Ohno S, Arellanes-Garcia L, et al. Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: Report of an international committee on nomenclature. Am J Ophthalmol. 2001;131:647–52. doi: 10.1016/s0002-9394(01)00925-4. [DOI] [PubMed] [Google Scholar]
- 28.Vemulakonda GA, Pepose J, Gelder RNV. Acute retinal necrosis syndrome. In: Ryan SJ, Sadda SR, Schachat AP, editors. Retina-Medical Retina. 5th ed. Amsterdam, Netherlands: Saunders Elsevier Inc; 2013. pp. 1523–32. [Google Scholar]
- 29.Agostoni E, Frigerio R, Protti A. Controversies in optic neuritis pain diagnosis. Neurol Sci. 2005;26(Suppl 2):s75–8. doi: 10.1007/s10072-005-0413-y. [DOI] [PubMed] [Google Scholar]
- 30.Fazzone HE, Lefton DR, Kupersmith MJ. Optic neuritis: Correlation of pain and magnetic resonance imaging. Ophthalmology. 2003;110:1646–9. doi: 10.1016/S0161-6420(03)00477-9. [DOI] [PubMed] [Google Scholar]
- 31.Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology. 2002;59:1492–5. doi: 10.1212/01.wnl.0000029570.69134.1b. [DOI] [PubMed] [Google Scholar]
- 32.Starling AJ. Diagnosis and management of headache in older adults. Mayo Clin Proc. 2018;93:252–62. doi: 10.1016/j.mayocp.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 33.Smith JH, Garrity JA, Boes CJ. Clinical features and long term prognosis of trochlear headaches. Eur J Neurol. 2014;21:577–85. doi: 10.1111/ene.12312. [DOI] [PubMed] [Google Scholar]
- 34.Kline LB, Hoyt WF. The Tolosa-Hunt syndrome. J Neurol Neurosurg Psychiatry. 2001;71:577–82. doi: 10.1136/jnnp.71.5.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Crimson BS, Thompson HS. Raeder's syndrome: A clinical review. Surv Ophthalmol. 1980;24:199–210. doi: 10.1016/0039-6257(80)90041-7. [DOI] [PubMed] [Google Scholar]
- 36.Shetty R, Deshpande K, Jayadev C, Wadia K, Mehta P, Shroff R, et al. The impact of dysfunctional tear films and optical aberrations on chronic migraine. Eye and Vision. 2017;4:25. doi: 10.1186/s40662-017-0070-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pflipsen M, Massaquoi M, Wolf S. Evaluation of the painful eye. Am Fam Physician. 2016;93:991–8. [PubMed] [Google Scholar]
- 38.Carlisle RT, Digiovanni J. Differential diagnosis of the swollen red eyelid. Am Fam Physician. 2015;92:106–12. [PubMed] [Google Scholar]
- 39.Lindsley K, Nichols JJ, Dickersin K. Non-surgical interventions for acute internal hordeolum. Cochrane Database Syst Rev. 2017;1:CD007742. doi: 10.1002/14651858.CD007742.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mahalingam S, Hone R, Lloyd G, Grounds R, Shamil E, Wong G, et al. The management of periorbital cellulitis secondary to sinonasal infection: A multicenter prospective study in the United Kingdom. Int Forum Allergy Rhinol. 2020;10:726–37. doi: 10.1002/alr.22535. [DOI] [PubMed] [Google Scholar]
- 41.Gupta A, Sadeghi PB, Akpek EK. Occult thyroid eye disease in patients presenting with dry eye symptoms. Am J Ophthalmol. 2009;147:919–23. doi: 10.1016/j.ajo.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 42.Montagnese F, Wenninger S, Schoser B. “Orbiting around” the orbital myositis: Clinical features, differential diagnosis and therapy. J Neurol. 2016;263:631–40. doi: 10.1007/s00415-015-7926-x. [DOI] [PubMed] [Google Scholar]
- 43.Mombaerts I. The many facets of dacryoadenitis. Curr Opin Ophthalmol. 2015;26:399–407. doi: 10.1097/ICU.0000000000000183. [DOI] [PubMed] [Google Scholar]
- 44.Hill RH, 3rd, Shiels WE, 2nd, Foster JA, Czyz CN, Stacey A, Everman KR, et al. Percutaneous drainage and ablation as first line therapy for macrocystic and microcystic orbital lymphatic malformations. Ophthalmic Plast Reconstr Surg. 2012;28:119–25. doi: 10.1097/IOP.0b013e318242ab0f. [DOI] [PubMed] [Google Scholar]
- 45.Hagiya H, Semba T, Morimoto T, Yamamoto N, Yoshida H, Tomono K. Panophthalmitis caused by Streptococcus dysgalactiae subsp.equisimilis: A case report and literature review. J Infect Chemother. 2018;24:936–40. doi: 10.1016/j.jiac.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 46.Pappuru RR, Dave VP, Pathengay A, Gangakhedkar S, Sharma S, Narayanan R, et al. Endophthalmitis progressing to panophthalmitis: Clinical features, demographic profile, and factors predicting outcome. Semin Ophthalmol. 2018;33:671–4. doi: 10.1080/08820538.2017.1416411. [DOI] [PubMed] [Google Scholar]
- 47.Hung JY, Wei YH, Huang CH, Chen LW, Fuh CS, Liao SL. Survival outcomes of eye-sparing surgery for adenoid cystic carcinoma of lacrimal gland. Jpn J Ophthalmol. 2019;63:344–51. doi: 10.1007/s10384-019-00671-w. [DOI] [PubMed] [Google Scholar]
- 48.Mills DM, Bodman MG, Meyer DR, Morton AD, 3rd ASOPRS Dacryocystitis Study Group. The microbiologic spectrum of dacryocystitis: A national study of acute versus chronic infection. Ophthalmic Plast Reconstr Surg. 2007;23:302–6. doi: 10.1097/IOP.0b013e318070d237. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Flow chart


