Abstract
Aim:
To examine health care practitioners’ views of the support women, partners, and the couple relationship require when affected by birth trauma, barriers to gaining such support, and potential improvements.
Background:
Ongoing distress following psychologically traumatic childbirth, also known as birth trauma, can affect women, partners, and the couple relationship. Birth trauma can lead to post traumatic stress symptoms (PTSS) or disorder (PTSD). Whilst there is a clear system of care for a PTSD diagnosis, support for the more prevalent experience of birth trauma is not well-defined.
Method:
An online survey of health care practitioners’ views of the support parents require for birth trauma, barriers to accessing support, and potential improvements. Practitioners were recruited in 2018 and the sample for the results presented in the article ranged from 95 to 110.
Results:
Practitioners reported differing needs of support for women, partners, and the couple as a unit. There was correlation between practitioners reporting having the skills and knowledge to support couples and feeling confident in giving support. The support most commonly offered by practitioners to reduce the impact on the couple relationship was listening to the couple. However practitioners perceived the most effective support was referral to a debriefing service. Practitioners observed several barriers to both providing support and parents accessing support, and improvements to birth trauma support were suggested.
Conclusions:
Practitioners indicate that some women, partners, and the couple as a unit require support with birth trauma and that barriers exist to accessing effective support. The support that is currently provided often conflicts with practitioners’ perception of what is most effective. Practitioners indicate a need to improve the identification of parents who need support with birth trauma, and more suitable services to support them.
Key words: barrier, birth trauma, health care practitioner, parent, relationship, support
Introduction
If a woman or her partner perceives birth as traumatic, it can result in ongoing emotional distress, often referred to as birth trauma. Whilst the term birth trauma lacks universal acceptance or standard definition (Elmir et al., 2010) it is widely used, and recognised that it can lead to post-traumatic stress symptoms (PTSS) or disorder (PTSD) (White et al., 2006; Yildiz et al., 2017). The prevalence of birth trauma is difficult to establish as this term is often used interchangeably with PTSS and PTSD. However, evidence suggests approximately 20%–40% of women report their birth as traumatic (Creedy et al., 2000; Soet et al., 2003; Alcorn et al., 2010; Ayers et al., 2018), with health care practitioners perceiving 30% of women and a quarter of partners to be affected by birth trauma (Delicate et al., 2020). Systematic reviews find that up to 16.8% of women experience clinically significant post-traumatic stress symptoms such as: re-experiencing, hyperarousal, avoidance, and negative alterations to cognition (Dekel et al., 2017) and post-partum PTSD affects 3% to 4% of women overall (Yildiz et al., 2017). There is also evidence to suggest that birth trauma can effect partners causing them ongoing distress (Etheridge and Slade, 2017), depression (Hinton et al., 2014), and PTSS (Bradley et al., 2008).
Birth trauma and PTSD are highly comorbid with anxiety (Dikmen-Yildiz et al., 2017), depression (Ayers et al., 2016), and secondary tokophobia (Hofberg and Brockington, 2000). For mothers, post-partum PTSD is associated with not initiating breastfeeding (Garthus-Niegel et al., 2018a) and perceived reduced bond with their baby (Dekel et al., 2018). There is evidence to suggest that birth trauma can have a negative impact on couple relationships such as strain on the relationship and loss of intimacy (Delicate et al., 2018a). Likewise, post-partum PTSS is associated with experiencing depression symptoms, which are related to poor relationship satisfaction (Garthus-Niegel et al., 2018b). Whilst reduction of couple relationship satisfaction is a common observation in the transition to parenthood, the impact of birth trauma appears to be more negative (Delicate et al., 2018b). The quality of the couple relationship is an important issue as it is associated with individual well-being and child outcomes (Cowan and Cowan, 2019).
Parents affected by birth trauma may require support to address trauma symptoms and overcome any impact these have on their life. It is important that such support addresses the needs of women, partners, and the relationships between them and their infant (NHS England, 2015). This support may come from health care practitioners such as midwives, health visitors (public health nurse), physicians/general practitioners (GP), or specialist mental health care practitioners (Ayers and Shakespeare, 2015). In addition, parents may also access support from third sector (non-profit and non-government) organisations and engage with non-clinical services such as parent education (Ayers and Delicate, 2016).
Whilst awareness of the importance of perinatal mental health care is rising, clinical guidelines seldom refer to birth trauma. An exception is seen in the UK which has a public funded national health service (NHS) guided by the National Institute for Health and Care Excellence (NICE). NICE recommend that practitioners offer advice and support to women who report birth as traumatic and consider that their partner may also be affected and require help (NICE, 2020). Where post-partum PTSD is identified, a stepped system of care is recommended of: (1) watchful waiting and (2) trauma-focussed cognitive behaviour therapy or eye movement desensitisation and reprocessing (NICE, 2018a).
When tailored to meet the needs of post-partum women, trauma-focussed psychological therapies have been shown to be effective in reducing PTSD symptoms in the early post-partum period (Furuta et al., 2018). Midwife-led debriefing, whilst routinely provided for birth trauma (Ayers et al., 2006) has no robust evidence for effectiveness (Bastos et al., 2015; de Graaff et al., 2018). However, women appear to value debriefing services, also known as birth listening and reflections, particularly women with high levels of PTSS (Meades et al., 2011; Baxter, 2019). Further birth trauma support strategies reported in the literature include: expressive writing (Di Blasio et al., 2015); sharing of birth stories online (Blainey and Slade, 2015); social support (Vesel and Nickasch, 2015); art therapy (Hogan, 2015); hypnosis (Slater, 2015); and information from websites, books and helplines (Thomson et al., 2017).
Women and partners indicate that they want support for birth trauma (Ayers et al., 2006; Etheridge and Slade, 2017), but multi-level barriers exist to accessing perinatal mental health services (Smith et al., 2019). On an individual level, parents can lack awareness of perinatal mental health symptoms (Russell et al., 2017; Das and Hodkinson, 2019), stigma can exist around disclosing mental health concerns (NCT, 2017), and guilt at being emotionally unwell at a perceived time of happiness (Smith et al., 2019). Partners may be particularly reluctant to seek help for their own perinatal mental health (Darwin et al., 2017), and can feel unjustified talking about birth trauma when they witnessed the trauma as oppose to women who go through the physical process of birth (Etheridge and Slade, 2017).
Barriers to health care practitioners supporting parents with birth trauma can exist through lack of knowledge (de Vries et al., 2018) and limited competence in supporting perinatal mental health (Borglin et al., 2015), which could stem from limitations in perinatal mental health training (NHS England, 2015). The quality of inter-personal relationships between parents and health care practitioners can create obstacles to identifying parents with mental health problems (NCT, 2017). Barriers can be created due to lack of continuity of care (Bayrampour et al., 2018), parents having limited time with health care practitioners, and maternal perception that post-partum health care is focussed on infant health (Byrne et al., 2017).
The organisation of health care can present further problems for accessing services, not least deficits in funding for perinatal mental health services (Bauer et al., 2014) and birth trauma specifically (Thomson and Garrett, 2019). Perinatal mental health services are prone to focus on the treatment of depression (Higgins et al., 2018) and moderate to severe disorders in mothers (Russell et al., 2017). The well-being of partners continues to be overlooked by perinatal services with a general lack of tailored support (Baldwin et al., 2018). Research suggests that perinatal mental health outcomes could be improved by consistent, routine assessment with reliable referral pathways, and specialist support services (Noonan et al., 2017; Viveiros and Darling, 2019).
Awareness of perinatal mental health problems is increasing (Ayers and Shakespeare, 2015), and recommendations exist for the identification and support of mental health problems in women and partners (Oates, 2015; NICE, 2020). To date, birth trauma research has mainly focussed on the effect upon and treatment of birthing women, and has largely disregared the needs of partners and the couple as a unit. A recent study of UK health care practitioner found that over one third of women and one quarter of partners are perceived to be affected by birth trauma; with up to 30% of couple relationships being impacted (Delicate et al., 2020). This study also explored the role of support for those affected by birth trauma and these findings are presented in the current article.
The results reported in the present article, aimed to explore the current birth trauma support offered to women and partners as individuals, and a couple, along with practitioners’ views of the most effective support for reducing the impact of birth trauma on the couple relationship. Furthermore, the study aimed to investigate practitioners’ perception of: barriers to couples accessing support; barriers to practitioners giving couples support; and potential improvements in support for couples affected by birth trauma.
Method
The results presented in this article are taken from a wider study which has already reported on health care practitioners perceptions of the observed rates and impact of birth trauma (Delicate et al., 2020). The study employed an online survey of health care practitioners to aid ease of participation and assist sample size and range of practitioner roles represented in the sample (Wright, 2005).
Participants
Practitioners were eligible to participate if they were currently working in clinical or non-clinical roles within the UK, supporting parents in the first-year post-partum. A self-selecting convenience sample of UK health care practitioners was utilised, and sample size was not predetermined as the survey was exploratory.
Procedures
A survey was designed by the authors to address the research aims. The survey questions and response criteria were drawn from existing literature and the design process utilised a small trial with practitioners to refine questions and answer categories. At the beginning of the survey, birth trauma was defined as having experienced ‘emotionally traumatic childbirth causing ongoing distress’ and participants were instructed to respond to the survey based on their experience of working with parents in the first-year post-partum. Ethical approval for the study was obtained from the School of Health Sciences at City, University of London.
Participants were recruited between May and September 2018 through social media (Facebook and Twitter) and organisations such as the Institute of Health Visiting; NCT; Midwives Information and Resources Service (MIDIRS); and the Royal College of General Practitioners. Recruitment information enabled practitioners to link to and download the participant information sheet. Participation was voluntary and anonymous and to participate, practitioners were required to give consent at the start of the survey hosted by Qualtrics. Contact information in the form of an email was only collected if the participant indicated they wished to receive a summary of the study findings. Data were collected and stored within the web-based survey tool Qualtrics and exported to the statistics software SPSS 25 for analysis.
Analyses
Geographical data was checked and any participants from outside the UK were removed from the sample. The sample was examined using frequencies for practitioner role and length of qualification. Frequencies were calculated for statements about perceived support needs for women, partners, and couples plus practitioner knowledge, skills, and confidence with birth trauma support. Kendall’s tau-b correlations were used to assess relationships between responses to parents’ support needs and practitioner aptitude.
Frequencies were calculated for the support practitioners currently offered to couples and which support practitioners viewed as most effective for reducing the impact on the couple relationship. Fisher’s exact tests were used to examine differences between the support offered to couples, and practitioner’s perception of its effectiveness. The frequencies with which practitioners signposted women, partners, and couples to other organisations were calculated. Practitioner’s views of the barriers to couples accessing support, and practitioners providing couples with support were examined using frequencies.
Open question responses for practitioners’ views on gaps in support services for couples affected by birth trauma, what would help couples access suitable support, and enable practitioners to support couples affected by birth trauma, were analysed using an approach similar to content analysis. For each question, participant responses were coded, and related codes grouped into categories. Due to apparent similarities, categories were compared between questions and rationalised to form over-arching themes for the open question data collectively.
Results
A sample of 202 health care practitioners engaged in the study and their characteristics are given in prior publication of study findings (Delicate et al., 2020). However, due to participant attrition as the survey progressed, the sample for results reported in this article is 110, and sample characteristics detailed in Table 1.
Table 1.
Article sample (n = 110)
| Practitioner Role | n (%) |
|---|---|
| Doula | 13 (11.8) |
| Family Support Worker (Social Care) | 2 (1.8) |
| General Practitioner (Physician) | 3 (2.7) |
| Health Visitor (Public Health Nurse) | 29 (26.4) |
| Breastfeeding Counsellor | 1 (0.9) |
| Maternity Care Assistant | 2 (1.8) |
| Midwife | 31 (28.2) |
| Parent Educator | 24 (21.8) |
| Psychological Counsellor/Therapist | 5 (4.5) |
Parent support needs and practitioner aptitude
Practitioners reported differing levels of need for support from women, partners, and couples, which are detailed in Table 2 along with practitioners’ perception of their own aptitude for giving birth trauma support. Practitioners reported that 54.5% (n = 60) of ‘women want me to support them’ with birth trauma ‘a lot’ or ‘a great deal’. Compared to 6.5% (n = 7) of ‘partners want me to support them’ and 19.1% (n = 21) of ‘couples want me to support them’ with birth trauma ‘a lot’ or ‘a great deal’. A strong positive correlation was found between practitioner responses to ‘I have the skills and knowledge required to support couples’ and ‘I feel confident in supporting couples’ (τb = 0.80, p ≤ 0.00). Moderate positive correlations were found between practitioner responses to ‘I have the resources to offer support to couples’ and ‘I feel confident in supporting couples’ (τb = 0.54, p ≤ 0.00), and ‘I have the resources to offer support to couples’ and ‘I have the skills and knowledge required to support couples’ (τb = 0.60, p ≤ 0.00).
Table 2.
Parent support needs and practitioner aptitude
| Not at all | A little | A moderate amount | A lot | A great deal | |
|---|---|---|---|---|---|
| Statement | n (%) | n (%) | n (%) | n (%) | n (%) |
| Women want me to support them (n = 110) | 2 (1.8) | 18 (16.4) | 30 (27.3) | 44 (40.0) | 16 (14.5) |
| Partners want me to support them (n = 107) | 22 (20.6) | 60 (56.1) | 18 (16.8) | 6 (5.6) | 1 (0.9) |
| Couples want me to support them (n = 110) | 41 (37.3) | 46 (41.8) | 11 (10.0) | 10 (9.1) | 2 (1.8) |
| I have the resources to offer support to couples (n = 109) | 21 (19.3) | 40 (36.7) | 30 (27.5) | 13 (11.9) | 5 (4.6) |
| I have the skills and knowledge required to support couples (n = 110) | 10 (9.1) | 41 (37.3) | 31 (28.2) | 22 (20.0) | 6 (5.5) |
| I feel confident in supporting couples (n = 109) | 9 (8.3) | 35 (32.1) | 36 (33.0) | 21 (19.3) | 8 (7.3) |
| I feel that supporting couples is part of my role (n = 110) | 6 (5.5) | 20 (18.2) | 20 (18.2) | 31 (28.2) | 33 (30.0) |
Birth trauma support
Data for the birth trauma support offered by health care practitioners is detailed in Table 3. The most offered support to couples experiencing birth trauma was listening to the couple (94.5%, n = 104), then referral to a birth listening/debriefing service (72.7%, n = 80), then self-help for example books and websites (53.6%, n = 59). Conversely, the support practitioners felt was most effective in reducing the impact of birth trauma on the couple relationship was birth listening/debriefing service (73.6%, n = 81), then listening to the couple (72.7%, n = 80), then referral to a mother and baby unit (46.4%, n = 51). There were significant differences between practitioner’s rate of offering support and rating it most effective support in reducing the impact on a couple’s relationship for: watchful waiting; listening to the couple; self-help; and charitable/third sector organisations (Fishers Exact Test, p < 0.001).
Table 3.
Current birth trauma support (n = 110)
| Offered to Couples Affected by Birth Trauma |
Viewed Most Effective in Reducing Impact on Couple Relationship |
Difference Fisher’s Exact Test |
|
|---|---|---|---|
| n (%) | n (%) | P | |
| Watchful Waiting | 42 (38.2) | 14 (12.7) | <0.001* |
| Listening to the couple | 104 (94.5) | 80 (72.7) | <0.001* |
| Self Help for example Books and Websites | 59 (53.6) | 23 (20.9) | <0.001* |
| Charitable/third-sector organisation | 54 (49.1) | 29 (26.4) | <0.001* |
| Birth listening/Debriefing service | 80 (72.7) | 81 (73.6) | 0.337 |
| Individual Psychotherapy | 12 (10.9) | 33 (30.0) | 0.178 |
| Couple Psychotherapy | 7 (6.4) | 30 (27.3) | 1.00 |
| Couple Relationship Therapy | 8 (7.3) | 33 (30.0) | 0.051 |
| Mother and Baby Unit | 56 (50.9) | 51 (46.4) | 0.712 |
Significant.
When indicating which type of birth trauma support they felt was most effective, two thirds of practitioners (66.4%, n = 73) selected three support types, over a quarter (29.1%, n = 32) selected five or more choices. Of the practitioners (n = 22) that indicated ‘other’ as a form of support, 31.8% (n = 7) stated that rewind therapy was offered, six of those seven practitioners indicating they thought rewind therapy was most effective in reducing the impact on the couple relationship.
Referral to other organisations, presented in Table 4, showed some similarities for third sector services and resources women, partners, and couples were informed about. The Birth Trauma Association (women 44.2%, n = 42; partner 33.7%, n = 32; couple 36.8%, n = 35), PANDA (women 32.6%, n = 31; partner 21.1%, n = 20; couple 20.0%, n = 19), Children Centre (women 30.5%, n = 29; partner 14.7%, n = 14; couple 20.0%, n = 19), Relate (women 29.5%, n = 28; partner 24.2%, n = 23; couple 46.3%, n = 44); and MIND (women 27.4%, n = 26; partner 24.2%, n = 23; couple 23.2%, n = 22). In open text responses to ‘other’ referrals were: local perinatal mental health charities (n = 12); birth afterthoughts (n = 4); rewind therapy (n = 3); Fatherhood Institute (n = 1); emotional freedom therapy (n = 1); and the GP (n = 1).
Table 4.
Signposting to organisations (n = 95)
| Signpost Women | Signpost Partners | Signpost Couples | |
|---|---|---|---|
| Organisation | n (%) | n (%) | n (%) |
| Big White Wall | 1 (1.1) | 1 (1.1) | 2 (2.1) |
| Birth Trauma Association | 42 (44.2) | 32 (33.7) | 35 (36.8) |
| Birth Trauma Chat | 9 (9.5) | 4 (4.2) | 7 (7.4) |
| Children Centre | 29 (30.5) | 14 (14.7) | 19 (20.0) |
| Family Action | 3 (3.2) | 2 (2.1) | 3 (3.2) |
| Homestart | 18 (18.9) | 5 (5.3) | 12 (12.6) |
| MIND | 26 (27.4) | 23 (24.2) | 22 (23.2) |
| NCT | 16 (16.8) | 11 (11.6) | 15 (15.8) |
| OnePlusOne | 10 (10.5) | 9 (9.5) | 7 (7.4) |
| PANDA | 31 (32.6) | 20 (21.1) | 19 (20.0) |
| Parent Infant Partnership | 8 (8.4) | 8 (8.4) | 7 (7.4) |
| Relate | 28 (29.5) | 23 (24.2) | 44 (46.3) |
| Tavistock Relationship | 6 (6.3) | 6 (6.3) | 10 (10.5) |
| The Relationship Foundation | 4 (4.2) | 5 (5.3) | 5 (5.3) |
Barriers to birth trauma support
Table 5 details practitioners views of the barriers that exist to couples receiving support and practitioners providing support. The three most commonly reported barriers to couples accessing support services that practitioners reported to see ‘a lot’ or ‘a great deal’ were: ‘long waiting times for support services’ (68.6%, n = 72); ‘stigma around disclosing problems with couple relationships’ (67.3%, n = 70); and ‘lack of suitable services’ (61.3%, n = 65). The three most commonly reported barriers to practitioners providing support to couples that practitioners reported experiencing ‘a lot’ or ‘a great deal’ were: ‘absence of suitable service to refer couple to’ (52.5%, n = 52); ‘lack of time to spend personally supporting parents’ (48.5%, n = 48); and ‘lack of contact with partners to identify those with birth trauma’ (45.8%, n = 44).
Table 5.
Barriers to obtaining birth trauma support
| Not at all | A little | A moderate amount | A lot | A great deal | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Barrier to couples accessing support services | |||||
| Concerns that requesting support will imply poor parenting (n = 105) | 15 (14.3) | 34 (32.4) | 27 (25.7) | 16 (15.2) | 13 (12.4) |
| Lack of awareness of childbirth related post-traumatic stress (n = 102) | 0 (0.0) | 21 (20.6) | 31 (30.4) | 33 (32.4) | 17 (16.7) |
| Lack of childcare provision to access support service (n = 104) | 11 (10.6) | 35 (33.7) | 23 (22.1) | 25 (24.0) | 10 (9.6) |
| Lack of contact time with health care professionals (n = 106) | 2 (1.9) | 14 (13.2) | 26 (24.5) | 39 (36.8) | 25 (23.6) |
| Lack of suitable services (n = 106) | 1 (0.9) | 17 (16.0) | 23 (21.7) | 36 (34.0) | 29 (27.4) |
| Long waiting times for support services (n = 105) | 1 (1.0) | 13 (12.4) | 19 (18.1) | 39 (37.1) | 33 (31.4) |
| Stigma around disclosing mental health problems (n = 105) | 0 (0.0) | 14 (13.3) | 27 (25.7) | 33 (31.4) | 31 (29.5) |
| Stigma around disclosing problems with couple relationship (n = 104) | 0 (0.0) | 10 (9.6) | 24 (23.1) | 37 (35.6) | 33 (31.7) |
| Barrier to practitioner providing support to couples | |||||
| Absence of suitable screening tool (n = 97) | 20 (20.6) | 24 (24.7) | 15 (15.5) | 19 (19.6) | 19 (19.6) |
| Absence of suitable service to refer couple to (n = 99) | 6 (6.1) | 18 (18.2) | 23 (23.2) | 31 (31.3) | 21 (21.2) |
| Lack of contact with mothers to identify those with birth trauma (n = 97) | 30 (30.9) | 21 (21.6) | 24 (24.7) | 12 (12.4) | 10 (10.3) |
| Lack of contact with partners to identify those with birth trauma (n = 96) | 11 (11.5) | 15 (15.6) | 26 (27.1) | 27 (28.1) | 17 (17.7) |
| Lack of training in this area (n = 101) | 13 (12.9) | 18 (17.8) | 25 (24.8) | 25 (24.8) | 20 (19.8) |
| Lack of time to spend personally supporting parents (n = 99) | 8 (8.1) | 17 (17.2) | 26 (26.3) | 23 (23.2) | 25 (25.3) |
| Parents reluctance to accept support (n = 98) | 16 (16.3) | 37 (37.8) | 34 (34.7) | 9 (9.2) | 2 (2.0) |
| Lack of collaboration with other health care professionals (n = 98) | 11 (11.2) | 25 (25.5) | 28 (28.6) | 21 (21.4) | 13 (13.3) |
A strong positive correlation was found between practitioners’ rating of ‘stigma around disclosing mental health problems’ and ‘stigma around disclosing problems with couple relationship’ as barriers to parents accessing support (τb = 0.73, p ≤ 0.00). Exploring barriers to practitioners providing support, a positive correlation was seen between rating of ‘lack of contact with mothers to identify those with birth trauma’ and ‘lack of contact with partners to identify those with birth trauma’ (τb = 0.63, p ≤ 0.00).
Potential improvements to birth trauma support
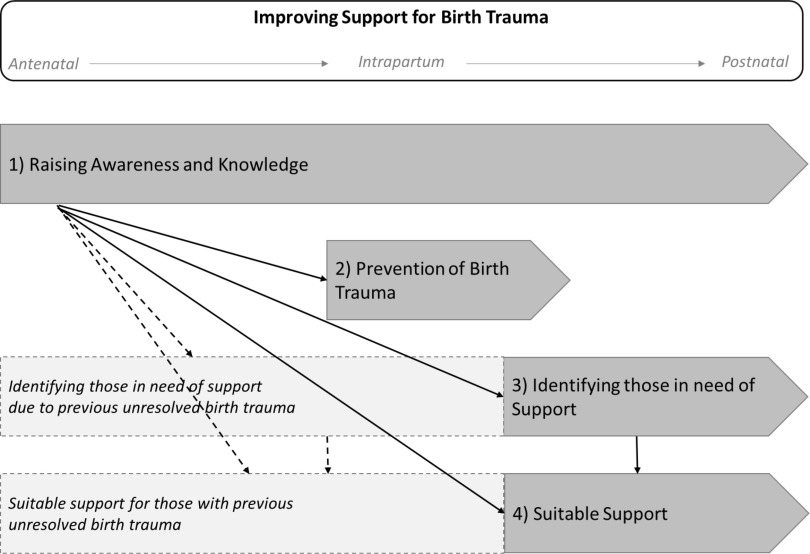
Four themes emerged from the responses to questions about practitioners’ views on: ‘what are the gaps in support services for couples affected by birth trauma’ (n = 84); ‘what would help couples access suitable support for birth trauma’ (n = 77); and ‘what would help practitioners to support couples affected by birth trauma’ (n = 73). Theme 1) raising awareness and knowledge of birth trauma, 2) prevention of birth trauma 3) identifying those in need of support with birth trauma, and 4) need for suitable birth trauma support. These four themes for potential improvements to birth trauma support are presented with supporting data in Table 6, and Figure 1 proposes how the themes may interact in the perinatal phase.
Table 6.
Data supporting themes for potential improvements to birth trauma support
| Question | What are the gaps in support services for couples affected by birth trauma? (n = 84) | What would help couples access suitable support for birth trauma? (n = 77) | What would help practitioners to support couple affected by birth trauma? (n = 73) |
|---|---|---|---|
| Theme 1 | ‘There is no validation of a traumatic birth ever. So parents go home without any information on support services and are left to suffer alone and do their own research.’ (doula) | ‘Information at all stages of contact [with parents], public awareness campaigns’(GP) | ‘Wider emphasis on the postnatal period and mental health. Birth trauma is often forgotten!’ (midwife) |
| Raising awareness and knowledge of birth trauma | ‘The assumption that healthy Mum and baby must be the only measure of a positive birth, not considering the emotional side of birth.’ (midwife) | ‘Greater recognition of trauma in those professionals who see the couples early on…for everybody in the world to never again say “a healthy baby is all that matters”.’ (parent educator) | ‘Further training in supporting couples with this specific issue.’ (health visitor) |
| Theme 2 | ‘In my view, more should be done to avoid the trauma in the first place by addressing the gaps in midwifery training and the lack of woman centered care in birth.’ (lactation consultant) | ‘Reducing the point of trauma, ensuring consent, dignity and environment are priorities.’ (midwife) | ‘A trauma led care pathway with flagging tool to determine likelihood of trauma and more immediate feedback of couples experiences.’ (midwife) |
| Prevention of birth trauma | ‘Securely funded, well signposted local support groups specifically for perinatal issues…thorough physical and mental postnatal check from GP and midwife and health visitor where appropriate, which include questions designed to flag potential ptsd’. (parent educator) | ‘All healthcare professionals involved in birth should have training on how to prevent birth trauma.’ (health visitor) | ‘Autonomy to discuss in immediate postnatal period without fear of reprimand for causing complaint.’ (midwife) |
| Theme 3 | ‘Often difficult to see as couple due to partner working or not wanting to admit there is a problem.’ (health visitor) | ‘A thorough postnatal screening tool used across the professions for both parents with adequate services to back it up.’ (parent educator) | ‘Better communication between the multi-professional teams.’(health visitor) |
| Identifying those in need of support with birth trauma | ‘Issues not being picked up or diagnosed quickly enough after birth. Watching and waiting too long sometimes.’ (health visitor) | ‘Continuity of care, someone…who had built a relationship of trust so couples would feel able and willing to disclose deeply personal problems.’ (parent educator) | ‘Protected time to spend talking about birth experiences with every couple soon after birth.’ (health visitor). |
| Theme 4 | ‘There’s virtually nothing unless either the person is incredibly debilitated by the trauma and can’t look after their child or the person actively demands help.’ (counsellor). | ‘Publicising really clearly what is on offer and destigmatising the support.’ (parent educator). | ‘Better joined-up services, clear referral/support pathways, access to written materials or online resources.’ (health visitor) |
| Need for suitable birth trauma support | ‘Support available weekends and evenings once father returns to work.’ (health visitor) | ‘More services and less waiting lists. Immediate referral after traumatic delivery in hospital.’ (midwife) | ‘Easy to refer service with specialist knowledge.’ (family support worker) |
Figure 1.
Themes for improving support for parents affected by birth trauma
Theme 1, raising awareness and knowledge of birth trauma, was highlighted as important for both parents and practitioners. Within this theme was a need to improve information to parents and enhanced training for practitioners in how to support couples with birth trauma. Theme 2 was prevention of birth trauma, which was identified as possible through improvements to intrapartum care to ensure care is respectful and based on informed consent. Likewise, improvements to mental health care could enable secondary prevention of PTSD after birth trauma.
Theme 3 was identifying those in need of support with birth trauma. This was highlighted as possible through practitioners having more time to spend with parents and continuity to build a relationship, particularly with partners. Similarly, increased communication between practitioners was reported as a potential facilitator to recognising parents in need of support, as was having an effective birth trauma assessment tool. Theme 4 was the need for suitable birth trauma support. Practitioners expressed the need for clearer referral pathways to specialist services that can address differing levels of birth trauma distress. Such support needing to be available in a timely way and be accessible by women, partners, and couples.
Discussion
The findings presented in this paper aimed to examine health care practitioners’ views of the support women, partners, and the couple relationship require when affected by birth trauma, barriers to gaining such support, and potential improvements. Perception of support needs varied according to whether it was for the women, partners, or the couple as a unit. The most offered support was practitioners listening to parents, followed by referral to birth debriefing, and signposting to self-help. Findings highlighted potential barriers to getting birth trauma support along with insight of possible improvements.
Results suggest that practitioners see less demand for birth trauma support from the couple as a unit, or partners, compared to women. Conversely, practitioners highlighted lack of contact with partners as a barrier to providing birth trauma support, and a potential improvement being enhanced services for partners. Further indications that perinatal health services need to consider the needs of partners (Burgess and Goldman, 2018) and engage them in support services (Nystedt and Hildingsson, 2018). Collaborative working in perinatal mental health is associated with reducing barriers to parents accessing support (Smith et al., 2019) and more effective support for families (Myors et al., 2013). The findings of the current study support these findings and suggest improved communication between professionals could improve the identification of couples in need of support. This is pertinent as current variation in birth trauma assessment creates a barrier to effective support through omission of those in need (Delicate et al., 2020).
Despite no conclusive evidence for the routine use of birth debriefing (Bastos et al., 2015), study results are consistent with previous research suggesting it is provided by many post-partum services in the UK (Ayers et al., 2006), with practitioners in the survey perceiving debriefing to be the most effective support for couples affected by birth trauma. Whilst research has shown that some women like and seek out debriefing (Baxter, 2019), its effectiveness as an intervention is questionable and likely to be influenced by its timing and the level of trauma symptoms (Meades et al., 2011).
Similarly, the current study found some practitioners referring to rewind therapy which is not currently an evidenced-based PTSD treatment (NICE, 2018b). However, at the time of this study, rewind therapy was being promoted to NHS practitioners as a birth trauma treatment (Mullan, 2017) and was accredited by the Royal College of Midwives despite no evidence for its effectiveness. This questionable use of rewind therapy for birth trauma may be due to it being available and accredited at a time when health professionals are looking for birth trauma treatments in the absence of any solid evidence about effective interventions for birth trauma. In addition, more intensive, evidenced-based treatments for PTSD may be inappropriate if women or their partners do not have PTSD, as well as being more costly.
Likewise, widespread referral to self-help reported by practitioners in the survey could be due to a lack of suitable services to refer to, or long waiting lists for receiving treatment (Thomson and Garrett, 2019). However, it may serve to reinforce the notion that parents often need to cope on their own with birth trauma (Delicate et al., 2020). Significant differences were found between rates of referral to, and perceived effectiveness for reducing the impact on the couple relationship for: watchful waiting; listening to the couple; signposting to self-help; and referral to third party/charitable organisations. Therefore, some practitioners are referring parents to support they perceived to be inferior, with most practitioners suggesting effective treatment consist of support from multiple sources. This reinforces previous research that more evidenced-based birth trauma interventions (Lapp et al., 2010) and referral pathways are required (NHS England, 2018).
Reported barriers to practitioners supporting parents were in concordance with previous research findings: lack of time to spend with parents (Noonan et al., 2018); limited perinatal mental health training (de Vries et al., 2018); and absence of suitable services to refer parents to (Bayrampour et al., 2018). The correlation between practitioners reporting having the skills and knowledge to support couples and feeling confident in giving support further emphasises the need for increased perinatal mental health training for practitioners (NHS England, 2015; Thomson and Garrett, 2019). There is limited evidence regarding the most effective way to train practitioners, and indeed which practitioners are best placed to support parents with birth trauma.
Developed from the present study results, Figure 1 depicts potential improvements in birth trauma support across the perinatal phase. Increased awareness and knowledge of birth trauma with parents may reduce barriers to parents accessing support (Smith et al., 2019), through easing stigma, improving help seeking behaviours, and developing acceptance of support (Button, 2017). A key element of raising awareness and knowledge of birth trauma in practitioners is through effective professional education and training (de Vries et al., 2018; Thomson and Garrett, 2019). To enable practitioners working with parents to have the time and resources to support parents birth trauma awareness also need to improve at service commissioning and development level (Bauer et al., 2014).
Knowledgeable practitioners and birth trauma aware health care practitioners could help prevent birth trauma. In the antenatal phase prevention can result from assessing and dealing with prior mental health vulnerability and enabling effective birth preparation (Simpson et al., 2018). During intrapartum care, prevention could be enabled by reducing obstetric interventions and facilitating a positive birth experience (Ayers et al., 2016; Dekel et al., 2017). Post-partum, birth trauma aware practitioners and services are needed to help identify those in need of support and assist them in gaining the support they require.
Whilst reassurance and a watch and wait approach is suitable in the early weeks post-partum (NICE, 2018a), the current study suggests that improvements are required to effectively identify women, partners, and couples affected with birth trauma. Consistent with other perinatal mental health problems, once birth trauma is identified, practitioners need clear referral pathways to support capable of addressing varying levels of distress (Noonan et al., 2017). It is recognised that identifying those in need of support, and therefore need for suitable support may be appropriate for some parents antenatally due to prior birth trauma (Greenfield et al., 2019).
Strengths and limitations
The main limitation of the present study is the use a self-selecting convenience sample which is not representative of the range of post-partum health care practitioners working with parents. Sample size was relatively small and low participant rates from some practitioner groups means their perspective is under-represented in the findings. Study results should be construed as exploratory due to the use of an unvalidated survey, practitioners responding retrospectively based on a range of observations of parents but not clinical diagnoses.
In contrast, the study findings add to a limited body of evidence of health care practitioners’ perspectives of birth trauma. Results illustrate current practice in birth trauma support, practitioners’ proficiency, and insight into how support may be improved. These findings are important for health care practitioners, service providers, commissioners, and researchers engaged in the perinatal phase. Results also have implications for the development of policy and practice to aid the prevention of birth trauma and the provision of effective support services.
Conclusions
Practitioners indicated that some women, partners, and the couple as a unit require support for birth trauma and identified some barriers to accessing effective support. Suggested improvements include preventing birth being perceived as traumatic in the first instance, raising birth trauma awareness in practitioners and parents, and improving identification of those requiring support. The birth trauma support that is currently being offered is often not evidence based and relies on practitioner’s perceptions of effectiveness and/or availability. It is important that further research is conducted into appropriate birth trauma treatments and that services offer evidence-based support to meet the needs of parents as individuals and the couple as a unit.
Acknowledgments
Authors would like to thank the health care practitioners who took part in the survey.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1463423620000407.
click here to view supplementary material
Financial Support
Amy Delicate is funded by a doctoral match-funded scholarship from City, University of London and NCT.
Conflict of Interest
This research has not been subjected to any financial or personal relationships, which could have inappropriately influenced the results from the study.
Ethical Standards
Ethical approval for the study was obtained from the School of Health Sciences ethics committee at City, University of London.
References
- Alcorn K, O’Donovan A, Patrick J, Creedy D and Devilly G (2010) A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events. Psychological Medicine 40, 1849–1859. doi: 10.1017/S0033291709992224. [DOI] [PubMed] [Google Scholar]
- Ayers S, Bond R, Bertullies S and Wijma K (2016) The aetiology of post-traumatic stress following childbirth: a meta-analysis and theoretical framework. Psychological Medicine 46, 1121–1134. doi: 10.1017/S0033291715002706. [DOI] [PubMed] [Google Scholar]
- Ayers S, Claypool J and Eagle A (2006) What happens after a difficult birth? Postnatal debriefing services. British Journal of Midwifery 14, 157–161. doi: 10.12968/bjom.2006.14.3.20577. [DOI] [Google Scholar]
- Ayers S and Delicate A (2016) Perinatal Mental Health Retrieved 15 January 2019 from http://openaccess.city.ac.uk/17201/1/Ayers_Delicate_perinatalmentalhealth_Perspectives_final%2520V2.pdf
- Ayers S and Shakespeare J (2015) Should perinatal mental health be everyone’s business? Primary Health Care Research & Development 16, 323–325. doi: 10.1017/S1463423615000298. [DOI] [PubMed] [Google Scholar]
- Ayers S, Wright D and Thornton A (2018) Development of a measure of postpartum PTSD: the city birth trauma scale. Frontiers in Psychiatry 9, 409. doi: 10.3389/fpsyt.2018.00409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin S, Malone M, Sandall J and Bick D (2018) Mental health and wellbeing during the transition to fatherhood: a systematic review of first time fathers’ experiences. JBI Database of Systematic Reviews and Implementation Reports 16, 2118–2191. doi: 10.11124/JBISRIR-2017-003773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastos M, Furuta M, Small, R , McKenzie-McHarg K and Bick D (2015) Debriefing interventions for the prevention of psychological trauma in women following childbirth. Cochrane Database of Systematic Reviews 4. doi: 10.1002/14651858.CD007194.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter J (2019) Postnatal debriefing: women’s need to talk after birth. British Journal of Midwifery 27, 563–571. doi: 10.12968/bjom.2019.27.9.563. [DOI] [Google Scholar]
- Bauer A, Parsonage M, Knapp M, Iemmi V and Adelaja B (2014) Costs of perinatal mental health problems Retrieved 9 January 2020 from https://www.centreformentalhealth.org.uk/sites/default/files/2018-09/costsofperinatal.pdf
- Bayrampour H, Hapsari A and Pavlovic J (2018) Barriers to addressing perinatal mental health issues in midwifery settings. Midwifery 59, 47–58. doi: 10.1016/j.midw.2017.12.020. [DOI] [PubMed] [Google Scholar]
- Blainey S and Slade P (2015) Exploring the process of writing about and sharing traumatic birth experiences online. British Journal of Health Psychology 20, 243–260. doi: 10.1111/bjhp.12093. [DOI] [PubMed] [Google Scholar]
- Borglin G, Hentzel J and Bohman D (2015) Public health care nurses’ views of mothers’ mental health in paediatric healthcare services: a qualitative study. Primary Health Care Research & Development 16, 470–480. [DOI] [PubMed] [Google Scholar]
- Bradley R, Slade P and Leviston A (2008) Low rates of PTSD in men attending childbirth: a preliminary study. British Journal of Clinical Psychology 47, 295–302. doi: 10.1348/014466508X279495. [DOI] [PubMed] [Google Scholar]
- Burgess A and Goldman R (2018) Who’s the Bloke in the Room? Fathers During Pregnancy and at the Birth in the UK Retrieved 27 November 2019 from https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=burgess+who+is+the+bloke+in+the+room&btnG=
- Button S (2017) Seeking help for perinatal psychological distress: a meta-synthesis of women’s experiences. British Journal of General Practice 67, e692–699. doi: 10.3399/bjgp17X692549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne V, Egan J, Mac Neela P and Sarma K (2017) What about me? The loss of self through the experience of traumatic childbirth. Midwifery, 51, 1–11. doi: 10.1016/j.midw.2017.04.017. [DOI] [PubMed] [Google Scholar]
- Cowan C and Cowan P (2019) Enhancing parenting effectiveness, fathers’ involvement, couple relationship quality, and children’s development: Breaking down silos in family policy making and service delivery. Journal of Family Theory & Review 11, 92–111. doi: 10.1111/j.1741-3737.2010.00809.x. [DOI] [Google Scholar]
- Creedy D, Shochet I and Horsfall J (2000) Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth 27, 104–111. doi: 10.1046/j.1523-536x.2000.00104.x. [DOI] [PubMed] [Google Scholar]
- Darwin Z, Galdas P, Hinchliff S, Littlewood E, McMillan D, McGowan L and Gilbody S (2017) Fathers’ views and experiences of their own mental health during pregnancy and the first postnatal year: a qualitative interview study of men participating in the UK Born and Bred in Yorkshire (BaBY) cohort. BMC Pregnancy and Childbirth 17, 45. doi: 10.1186/s12884-017-1229-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das R and Hodkinson P (2019) New Fathers, Mental Health and Social Media Retrieved 9 January 2020 from http://epubs.surrey.ac.uk/852847/
- de Graaff L, Honig A, van Pampus M and Stramrood C (2018) Preventing post-traumatic stress disorder following childbirth and traumatic birth experiences: a systematic review. Acta Obstetricia et Gynecologica Scandinavica 97, 648–656. doi: 10.1111/aogs.13291. [DOI] [PubMed] [Google Scholar]
- Dekel S, Stuebe C and Dishy G (2017) Childbirth induced posttraumatic stress syndrome: a systematic review of prevalence and risk factors. Frontiers in Psychology 8, 560. doi: 10.3389/fpsyg.2017.00560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dekel S, Thiel F, Dishy G and Ashenfarb A (2018) Is childbirth-induced PTSD associated with low maternal attachment? Archives of Women’s Mental Health 22, 119–122. doi: 10.1007/s00737-018-0853-y. [DOI] [PubMed] [Google Scholar]
- Delicate A, Ayers S, Easter A and McMullen S (2018. a) The impact of childbirth-related post-traumatic stress on a couple’s relationship: a systematic review and meta-synthesis. Journal of Reproductive and Infant Psychology 36, 102–115. doi: 10.1080/02646838.2017.1397270. [DOI] [PubMed] [Google Scholar]
- Delicate A, Ayers S, and McMullen S (2018. b) A systematic review and meta-synthesis of the impact of becoming parents on the couple relationship. Midwifery 61, 88–96. doi: 10.1016/j.midw.2018.02.022. [DOI] [PubMed] [Google Scholar]
- Delicate A, Ayers S, and McMullen S (2020) Health-care practitioners’ assessment and observations of birth trauma in mothers and partners. Journal of Reproductive and Infant Psychology, 1–13. doi: 10.1080/02646838.2020.1788210. [DOI] [PubMed] [Google Scholar]
- de Vries N, Stramrood C, Sligter L, Sluijs A and Van Pampus M (2018) Midwives’ practices and knowledge about fear of childbirth and postpartum posttraumatic stress disorder. Women and Birth 33, e95–104. doi: 10.1016/j.wombi.2018.11.014. [DOI] [PubMed] [Google Scholar]
- Di Blasio P, Camisasca E, Caravita S, Ionio C, Milani L and Valtolina G (2015) The effects of expressive writing on postpartum depression and posttraumatic stress symptoms. Psychological Reports 117, 856–882. doi: 10.2466/02.13.PR0.117c29z3. [DOI] [PubMed] [Google Scholar]
- Dikmen-Yildiz P, Ayers S and Phillips L (2017) Depression, anxiety, PTSD and comorbidity in perinatal women in turkey: a longitudinal population-based study. Midwifery 55, 29–37. doi: 10.1016/j.midw.2017.09.00. [DOI] [PubMed] [Google Scholar]
- Elmir R, Schmied V, Wilkes L and Jackson D (2010) Women’s perceptions and experiences of a traumatic birth: a meta-ethnography. Journal of Advanced Nursing 66, 2142–2153. doi: 10.1111/j.1365-2648.2010.05391.x. [DOI] [PubMed] [Google Scholar]
- Etheridge J and Slade P (2017) Nothing’s actually happened to me: the experiences of fathers who found childbirth traumatic. BMC Pregnancy and Childbirth 17, 80. doi: 10.1186/s12884-017-1259-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuta M, Horsch A, Ng E, Bick D, Spain D and Sin J (2018) Effectiveness of trauma-focused psychological therapies for treating post-traumatic stress disorder symptoms in women following childbirth: a systematic review and meta-analysis. Frontiers in Psychiatry 9, 591. doi: 10.3389/fpsyt.2018.00591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garthus-Niegel S, Horsch A, Ayers S, Junge-Hoffmeister J, Weidner K and Eberhard-Gran M (2018. a) The influence of postpartum PTSD on breastfeeding: a longitudinal population-based study. Birth 45, 193–201. doi: 10.1111/birt.12328. [DOI] [PubMed] [Google Scholar]
- Garthus-Niegel S, Horsch A, Handtke E, von Soest T, Ayers S, Weidner K and Eberhard-Gran M (2018. b) The impact of postpartum posttraumatic stress and depression symptoms on couples’ relationship satisfaction: a population-based prospective study. Frontiers in Psychology 9, 1–10. doi: 10.3389/fpsyg.2018.01728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield M, Jomeen J and Glover L (2019) It can’t be like last time: choices made in early pregnancy by women who have previously experienced a traumatic birth. Frontiers in Psychology 10, 1–13. doi: 10.3389/fpsyg.2019.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins A, Downes C, Carroll M, Gill A and Monahan M (2018) There is more to perinatal mental health care than depression: public health nurses reported engagement and competence in perinatal mental health care. Journal of Clinical Nursing 27, e476–e487. doi: 10.1111/jocn.13986. [DOI] [PubMed] [Google Scholar]
- Hinton L, Locock L and Knight M (2014) Partner experiences of ‘near-miss’ events in pregnancy and childbirth in the uk: a qualitative study, PLoS One 9, 91735. doi: 10.1371/journal.pone.0091735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofberg K and Brockington I (2000) Tokophobia: an unreasoning dread of childbirth: a series of 26 cases. The British Journal of Psychiatry 176, 83–85. doi: 10.1192/bjp.176.1.83. [DOI] [PubMed] [Google Scholar]
- Hogan S (2015) Mothers make art: using participatory art to explore the transition to motherhood. Journal of Applied Arts and Health 6, 23–32. doi: 10.1386/jaah.6.1.23_1. [DOI] [Google Scholar]
- Lapp L, Agbokou C, Peretti C and Ferreri F (2010) Management of post traumatic stress disorder after childbirth: a review. Journal of Psychosomatic Obstetrics & Gynecology 31, 113–122. doi: 10.3109/0167482X.2010.503330. [DOI] [PubMed] [Google Scholar]
- Meades R, Pond C, Ayers, S and Warren F (2011) Postnatal debriefing: have we thrown the baby out with the bath water? Behaviour Research and Therapy 49, 367–372. doi: 10.1016/j.brat.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Mullan J (2017) Birth trauma resolution. MIDIRS Midwifery Digest 27, 345–348. [Google Scholar]
- Myors K, Schmied V, Johnson M and Cleary M (2013) Collaboration and integrated services for perinatal mental health: an integrative review. Child and Adolescent Mental Health 18, 1–10. doi: 10.1111/j.1475-3588.2011.00639.x [DOI] [PubMed] [Google Scholar]
- NCT (2017) The Hidden Half Executive Summary Key Findings and Recommendations Retrieved 18 January 2019 from www.nct.org.uk/hiddenhalf
- NHS England (2015) Improving Access to Perinatal Mental Health Services in England – a review Retrieved 15 January 2019 from https://www.maternalmentalhealth.org.uk/wp-content/uploads/2015/09/NHSIQ-Improving-access-to-perinatal-mental-health-services-in-England-0915.pdf
- NHS England (2018) The Perinatal Mental Health Care Pathways Retrieved 21 November 2019 from https://www.england.nhs.uk/wp-content/uploads/2018/05/perinatal-mentalhealth-care-pathway.pdf
- NICE (2018. a) Post-traumatic Stress Disorder NICE Guideline Retrieved 18 January 2019 from https://www.nice.org.uk/guidance/ng116/resources/posttraumatic-stress-disorder-pdf-66141601777861
- NICE (2018. b) Post-traumatic Stress Disorder [D]: evidence reviews for psychological, psychosocial and other non-pharmacological interventions for the treatment of PTSD in adults Retrieved 18 June 2019 from https://www.nice.org.uk/guidance/ng116/evidence/evidence-review-d-psychological-psychosocial-and-other-nonpharmacological-interventions-for-the-treatment-of-ptsd-in-adults-pdf-6602621008 [PubMed]
- NICE (2020) Antenatal and Postnatal Mental Health: clinical management and service clinical management and service guidance guidance Retrieved 17 February 2020 from https://www.nice.org.uk/guidance/cg192
- Noonan M, Doody O, Jomeen J and Galvin R (2017) Midwives’ perceptions and experiences of caring for women who experience perinatal mental health problems: an integrative review. Midwifery 45, 56–71. doi: 10.1016/j.midw.2016.12.010. [DOI] [PubMed] [Google Scholar]
- Noonan M, Jomeen J, Galvin R and Doody O (2018) Survey of midwives’ perinatal mental health knowledge, confidence, attitudes and learning needs. Women and Birth 31, e358–e366. doi: 10.1016/j.wombi.2018.02.002. [DOI] [PubMed] [Google Scholar]
- Nystedt A and Hildingsson I (2018) Women’s and men’s negative experience of child birth: a cross-sectional survey. Women and Birth 31, 103–109. doi: 10.1016/j.wombi.2017.07.002. [DOI] [PubMed] [Google Scholar]
- Oates M (2015) Perinatal mental health services: recommendations for the provision of services for childbearing women. Retrieved 22 January 2019 from http://www.rcpsych.ac.uk/publications/
- Russell K, Ashley A, Chan G, Gibson S and Jones R (2017) Maternal mental health: women’s voices. London: Royal College of Obstetricians and Gynaecologists; Retrieved 9 January 2020 from https://www.rcog.org.uk/globalassets/documents/patients/information/maternalmental-healthwomens-voices.pdf [Google Scholar]
- Simpson M, Schmied V, Dickson C and Dahlen H (2018) Postnatal post-traumatic stress: an integrative review. Women and Birth 31, 367–379. doi: 10.1016/j.wombi.2017.12.003. [DOI] [PubMed] [Google Scholar]
- Slater P (2015) Post-traumatic stress disorder managed successfully with hypnosis and the rewind technique: two cases in obstetric patients. International Journal of Obstetric Anesthesia 24, 272–275. doi: 10.1016/j.ijoa.2015.03.003. [DOI] [PubMed] [Google Scholar]
- Smith M, Lawrence V, Sadler E and Easter A (2019) Barriers to accessing mental health services for women with perinatal mental illness: systematic review and meta-synthesis of qualitative studies in the UK. BMJ Open 9, e024803. doi: 10.1136/bmjopen-2018-024803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soet J, Brack G and Di Iorio C (2003) Prevalence and predictors of women’s experience of psychological trauma during childbirth. Birth 30, 36–46. doi: 10.1046/j.1523-536X.2003.00215.x. [DOI] [PubMed] [Google Scholar]
- Thomson G, Beck C and Ayers S (2017) The ripple effects of a traumatic birth: risk, impact and implications for practice In Thomson G and Schmied V, editors, Psychosocial resilience and risk in the perinatal period. Routledge: London, 154–169. doi: 10.4324/9781315656854. [DOI] [Google Scholar]
- Thomson G and Garrett C (2019) Afterbirth support provision for women following a traumatic/distressing birth: survey of NHS hospital trusts in England. Midwifery 71, 63–70. doi: 10.1016/j.midw.2019.01.004. [DOI] [PubMed] [Google Scholar]
- Vesel J and Nickasch B (2015) An evidence review and model for prevention and treatment of postpartum posttraumatic stress disorder. Nursing for Women’s Health 19, 504–525. doi: 10.1111/1751-486X.12234. [DOI] [PubMed] [Google Scholar]
- Viveiros C and Darling E (2019) Perceptions of barriers to accessing perinatal mental health care in midwifery: a scoping review. Midwifery 70, 106–118. doi: 10.1016/J.MIDW.2018.11.011. [DOI] [PubMed] [Google Scholar]
- White T, Matthey S, Boyd K and Barnett B (2006) Postnatal depression and post-traumatic stress after childbirth: prevalence, course and co-occurrence. Journal of Reproductive and Infant Psychology 24, 107–120. doi: 10.1080/02646830600643874. [DOI] [Google Scholar]
- Wright K (2005) Researching internet-based populations: advantages and disadvantages of online survey research, online questionnaire authoring software packages, and web survey services. Journal of Computer-Mediated Communication 10, doi: 10.1111/j.1083-6101.2005.tb00259.x. [DOI] [Google Scholar]
- Yildiz P, Ayers S and Phillips L (2017) The prevalence of posttraumatic stress disorder in pregnancy and after birth: a systematic review and meta-analysis. Journal of Affective Disorders 208, 634–645. doi: 10.1016/j.jad.2016.10.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1463423620000407.
click here to view supplementary material