Abstract
Aim:
To explore if there is an interaction effect between gender (men and women) and profession (nurses and physicians) in posttraumatic growth (PTG).
Background:
PTG is defined as a positive psychological change experienced as a result of struggling with highly challenging life circumstances. It may take the form of improved self-image, a deeper understanding of self, increased spirituality, and/or enhanced interpersonal relationships. Gender and profession were found separately to be associated with PTG, but to date were not examined under interaction effect.
Methods:
We employed a cross-sectional study conducted in the tertiary medical center in Israel using a convenience sample. One hundred and twenty-eight nurses and seventy-eight physicians gave their consent and agreed to fill out self-report questionnaires regarding personal and professional data and PTG Inventory.
Findings:
The correlation matrix revealed that being a woman was associated with higher PTG total scale (r = 0.242; P ≤ 0.001) and its subscales except for spiritual change that showed no evidence of statistical effect. Similar pattern was found for being a nurse with PTG total scale (r = 0.223; P ≤0.001) and its subscales except for relating to others that showed no evidence of statistical effect. However, the interaction effect revealed that among men, there was no difference in the level of PTG and its subscales based on profession (Physicians men = 62.54 (20.82) versus Nurses men = 60.26 (22.39); F = 9.618; P = 0.002). Among women, nurses had a significantly higher scores in PTG (Physicians women = 61.81 (18.51) versus Nurses women = 73.87 (12.36); F = 9.618; P = 0.002) and its subscales in comparison to physicians except for subscale relating to other.
Conclusions:
Our findings suggest implications for research and practice namely exploring PTG among nurses and physicians would benefit from applying interaction effect of gender and profession. For practice, advocating PTG within the health care organization is needed to be tailored with gender and professional sensitivity.
Key words: gender, nurses, physicians, posttraumatic growth, profession
Introduction
Health care professions, especially physicians and nurses, are among the occupational group that exposed to higher work-related stress, results from their responsibility for health and well-being of patients, and their continues exposure to death, injury, or victims (eg, Ogińska-Bulik, 2006; Stucky et al., 2009). These factors triggered psychological reactions which were documented by a large body of literature in two ways that can co-exist: the first relates to negative reactions namely, secondary traumatic stress, burnout, and compassion fatigue (eg, Cocker and Joss, 2016; El-Bar et al., 2013; Hamama et al., 2019), while the second composed of positive reactions namely, posttraumatic growth (PTG) and satisfaction fatigue (eg, Hamama-Raz and Minerbi, 2019; Manning-Jones et al., 2016; 2017; Shoji et al., 2014). In the current research, we aimed to focus on the positive reactions of work-related stress in health care professions namely PTG.
Posttraumatic growth
PTG relates to the salutogenic aspects of human experience in the face of adverse event (Höltge et al., 2018); it was defined by Tedeschi and Calhoun (2004) as “the experience of positive change that occurs as a result of the struggle with highly challenging life crises” (p. 1). PTG is manifested in five domains, including an increased appreciation for life in general, more meaningful interpersonal relationships, an increased sense of personal strength, changed priorities, and a richer existential and spiritual life (Tedeschi and Calhoun, 1996; 2004). Thus, those who have experience of challenging life events may feel as stronger and better able to deal with difficult events in the future and may also experience a greater sense of intimacy and belonging. Additionally, they may gain a greater sense of purpose and appreciation for life, and new priorities regarding what is most important. In line with this notion, Malhotra and Chebiyan’s overview (2016) stated that PTG can be placed within either of two descriptions: in the first, PTG is presented as a by-product of attempts to cope with life-changing traumatic events, where these attempts manifest in the development of a life narrative and wisdom. In the second description, PTG is presented as a coping strategy which may include construal of meaning, meaning-making coping process, interpretative process, or form of self-enhancing appraisal or positive illusion with an adaptive function for psychological adjustment. Actually, according to the Conservation of Resources theory (Hobfoll, 1989; 2011), individuals seek to build and retain resources as a result from actual or threatened loss of resources after coping with stressful circumstances. Resource gains can help to offset the impact of resource losses. Given this, PTG is an important source of resource gain after stressful events that could help to buffer against resource loss caused by work-related stressors. Given this notion, in the current study, we assessed PTG as a by-product result of health care providers’ (ie, physicians and nurses) exposure to a variety of work-related stress.
PTG among health care professions
Previous researches which explored the link between profession affiliation and PTG among health care provider revealed that PTG is a very common phenomenon in all health care providers (ie, therapists, social workers, counsellors, nurses, and physicians – for a review see Manning-Jones et al., 2015). Nevertheless, when comparing nurses and physicians’ PTG level, most of the studies indicated that nurses reported on higher level of PTG than physicians (eg, Manning-Jones et al., 2016; Shiri et al., 2008; Taubman Ben-Ari and Weintroub, 2008). Only Rodríguez-Rey et al. (2017) found among professionals working in pediatric intensive care personnel and personnel working at other pediatric wards that PTG was not different among physicians, nurses and nursing assistants. Possible explanation which was suggested by the researchers referred to the difference in the character of their work. Specifically, nurse’s role involves much closer contact with patients and more intimate involvement in their physical, physiological, and mental needs (Taubman Ben-Ari and Weintroub, 2008). Additionally, nurses’ responsibilities regarding patients’ care required them to spend long time with them, whereas physicians meet the patients for shorter periods of time during their daily rounds. In line with this notion, Moriel et al. (2017) show through a qualitative research via focus groups conducted with practicing nurses and physicians that physicians perceive nurses as the patients’ advocates, having much closer interaction with patients “patients see the nurse as liaison and caregiver—and one of nurses’ primary roles is that of patient assessor” (p. 8). Nurses concurred on three main physician roles: prescriber, decision-maker, and educator. Another explanation which may account for the profession’s differences in PTG level was related to gender as nursing has traditionally been and remains a female-dominated profession in Western countries (Kouta and Kaite, 2011; Solbrække et al., 2013).
PTG and gender
The scientific literature that explored PTG among women and men indicate that women show higher levels of PTG than men who experience similar traumatic events (eg, Helgeson et al., 2006; Vishnevsky et al., 2010). According to Vishnevsky et al.’s (2010) meta-analysis, possible explanation for this difference refers to women’s tendency to engage in deeper thought than men. The tendency to think deeply on constructive issues, such as an increased awareness of personal strengths or an appreciation of the importance of social connections, has been suggested as a mechanism leading to greater reports of PTG.
Nevertheless, in references to health care professional – previous studies revealed no gender differences. Specifically, in Manning-Jones et al.’s studies (2016; 2017) who explored differences between several distinct groups of health professionals including nurses and physicians, no significant differences emerged between women and men with regard to PTG. Likewise, Rodríguez-Rey et al. (2017) who investigated PTG among staff in pediatric intensive care units in comparison to other pediatric units revealed that PTG scores did not differ by gender. Also, Kang et al. (2018) reported no gender differences with PTG among nurses and physicians and other ambulance workers in Chania.
The current research
In the current study, we sought to focus on PTG among physicians and nurses and to explore the interaction effect between gender and profession in PTG – two factors which were found separately to be associated with PTG (eg, Kang et al., (2018; Manning-Jones et al., 2015; Manning-Jones et al., 2016; Rodríguez-Rey et al., 2017; Taubman Ben-Ari and Weintroub, 2008), but to date were not examined under interaction effect. We expected that the interaction between these two factors will exhibit much more detailed picture concerning PTG among hospital personnel.
Methods
Procedure
The study was conducted in a tertiary hospital in Israel with 750 physician and nurses. The sampling used was a convenience sample by approaching directly the hospital personnel (physicians and nurses) and asking them to answer a self-repot questionnaires assuring confidentiality and explaining the voluntary nature of their participation. Data collection took place between 15/April and 1/June/2019. The estimated sample size using 5% margin of error, 90% confidence interval yielded a needed sample of 200 participants. Our final sample size was 206. Participants were recruited from every ward of the hospital, and the only inclusion criterion was a licensed physician or nurse.
Ethics statement
The Institutional Review Board and Ethics Committee of the hospital approved the study protocol. Participants were informed that their participation is entirely voluntary and that data obtained from the survey would be analyzed in an anonymous format.
Measures
Participants completed the following self-report questionnaires:
Personal and professional data – which served as the independent variables for this study. We inquired regarding gender, age, marital status, profession, education, and degree of religiosity. In addition, participants were asked to indicate their years in the profession, their years in the current department, employment scope (part-time employment percentage or full-time employment). Self-rated health was assessed with a single question: “In general, how do you rate your health?” The scale ranged from 1 to 4 (1 = “bad” to 4 = “excellent”). This measure was found to be valid and highly associated with objective indicators of health (Benyamini et al. 2003).
PTG – the dependent variable for this study. It was measured by the PTG Inventory (PTGI; Tedeschi and Calhoun, 1996; Original Cronbach’s alpha was 0.90), Hebrew version (Laufer and Solomon 2006; Cronbach’s alpha of the Hebrew version was 0.94) in order to assess positive changes after negative life events. This 21-item scale is composed of one global score of PTG and five subscales. Each subscale is measuring a different facet of post traumatic growth: New Possibilities (5 items), Relating to Others (7 items), Personal Strength (4 items), Spiritual Change (2 items), and Appreciation of Life (3 items). The answers were given in a six-point Likert response format ranging from I did not experience this change as a result of my crisis (scored 0), to I experienced this change to a very great degree as a result of my crisis (scored 5). The PTGI has no cut-off values. The higher the score, the more PTG the person has This is considered positive as it means the person shows more affinity to new possibilities, higher relations to others, more personal strength, more positive spiritual change, and higher appreciation of life.
Cronbach’s alpha and basic descriptive statistics for the current study were 0.94 for total PTGI score (mean score = 67.33; SD = 18.15) and for each subscale: New Possibilities (α = 0.86; mean score = 15.44; SD = 5.32), Relating to Others (α = 0.87; mean score = 22.30; SD = 6.28), Personal Strength (α = 0.82; mean score = 14.20; SD = 3.70), Spiritual Change (α = 0.61; mean score = 5.13; SD = 2.54), and Appreciation of Life (α = 0.82; mean score = 10.08; SD = 3.28).
Data analysis
Before commencing the analytic plan, we have checked for data integrity and missing values. One participant had missing values and has been omitted from the study leading to a final sample of 206 participants.
The analytic plan had two stages: First: we present a simple correlation matrix for the study variables. Second, we used multivariate analysis of covariance (MANCOVA) with gender (men/women) and position (nurse/physician) as independent variables. Age, marital status, years of experience in medicine, years of experience in the department, and percentage of employment served as covariates. The dependent variables were the total PTGI score and the five subscales namely: New possibilities, Relating to others, Personal strength, Spiritual change, and Appreciation of life. The analysis was accompanied by effect size as measured by partial eta square. Interaction effects were accompanied by corresponding figures. Data were analyzed using IBM SPSS ver. 25.
Results
The study was conducted in tertiary hospital in Israel among health care providers, namely physicians and nurses. The mean age was 41.48 (SD = 17.70), 62% of the participants were women (n = 130), 61.8% of the participants were nurses (n = 128), and the rest were physicians. Among women, the profession distribution was 97 nurses and 32 physicians. Among men, the position distribution was 46 physicians and 31 nurses. About 75.8% of the participants reported being in a committed relationship (n = 157). The mean years of experience in medicine was 12.83 (SD = 10.68), and the mean years of experience in the department was 9.40 (SD = 9.78). The participants employed in a full-time job was 165 (79.7% of the sample), and the rest in varied capacity ranging from 40% to 95%.
The correlation matrix revealed that being a woman was associated with higher PTG total scale and its subscales except for Spiritual change that was not found to be significant. Similar pattern was found for being a nurse with PTG total scale and its subscales except for Relating to others that was not found to be significant. For more information, see Table 1.
Table 1.
Correlation matrix of the study variables (N = 206)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
| 1. Age | |||||||||||||
| 2. Gender | 0.096 | ||||||||||||
| 3. Profession | 0.051 | 0.348*** | |||||||||||
| 4. Marital status | 0.178** | 0.103 | −0.022 | ||||||||||
| 5. Years of medical experience | 0.537*** | 0.117 | 0.130 | 0.218*** | |||||||||
| 6. Years of experience in the current department | 0.398*** | 0.151* | 0.172* | 0.129 | 0.665*** | ||||||||
| 7. Work capacity | −.074 | −0.158* | −0.093 | −0.103 | −0.229*** | −0.191** | |||||||
| 8. PTG – RTO | .023 | 0.257*** | 0.115 | −0.007 | 0.046 | −0.009 | 0.025 | ||||||
| 9. PTG – NP | −.018 | 0.199** | 0.261*** | −0.094 | −0.011 | −0.045 | 0.012 | 0.743*** | |||||
| 10. PTG –PS | −.028 | 0.205** | 0.210** | −0.036 | 0.051 | 0.037 | 0.056 | 0.729*** | 0.758*** | ||||
| 11. PTG – SC | −.019 | 0.121 | 0.233** | −0.003 | −0.034 | 0.002 | −0.022 | 0.506*** | 0.576*** | 0.440*** | |||
| 12. PTG – AOL | −.033 | 0.224*** | 0.178** | −0.017 | 0.061 | −0.065 | −0.063 | 0.706*** | 0.812*** | 0.735*** | 0.512*** | ||
| 13. PTG – TOT | −.012 | 0.242*** | 0.223*** | −0.043 | 0.029 | −0.023 | 0.017 | 0.906*** | 0.915*** | 0.868*** | 0.661*** | .867*** |
PTG = posttraumatic growth; PTG – RTO = Relating to Others, PTG – NP = New Possibilities, PTG – PS = Personal Strength, PTG – SC = Spiritual Change, PTG – AOL = Appreciation of Life, PTG – TOT = Total.
Note: Gender Coded as 1 = Men; 2 = Women. Profession coded as 1 = Nurses; 2 = Physicians.
* = P ≤ 0. 005; ** = P ≤ 0.01; *** = P ≤ 0.001;
Following the correlation matrix, the MANCOVA results revealed a significant main effect of gender regarding PTG scores and its subscales except for spiritual change. F statistics ranged from 4.146 to 12.335, and P-value was ranged from 0.043 to 0.001. Effect size as measured partial η2 ranged from 0.021 to 0.059. The main effect of profession regarding PTG scores and its subscales revealed only two significant results namely new possibilities (F = 7.634; P = 0.006; partial η2 = 0.037) and spiritual change (F = 7.426; P = 0.007; partial η2 = 0.036). In order to be concise, the mean scores and standard deviation for the PTGI and its subscales are presented in Table 2.
Table 2.
Mean scores and standard deviations of the posttraumatic growth inventory and its subscales (n = 206)
| Scale | Sex | Profession | Mean | SD |
|---|---|---|---|---|
| Total PTGI Score | Men | Physician | 62.5435 | 20.82809 |
| Nurse | 60.2581 | 22.38745 | ||
| Women | Physician | 61.8125 | 18.51144 | |
| Nurse | 73.8660 | 12.35637 | ||
| Relating to others | Men | Physician | 20.8913 | 7.27928 |
| Nurse | 19.1935 | 7.63509 | ||
| Women | Physician | 22.1250 | 6.47950 | |
| Nurse | 24.0619 | 4.55250 | ||
| New possibilities | Men | Physician | 13.9348 | 5.66236 |
| Nurse | 14.2581 | 6.67317 | ||
| Women | Physician | 13.4063 | 5.07911 | |
| Nurse | 17.2990 | 4.02380 | ||
| Personal strength | Men | Physician | 13.3478 | 4.50292 |
| Nurse | 13.0323 | 4.30878 | ||
| Women | Physician | 13.0313 | 3.67629 | |
| Nurse | 15.3918 | 2.62820 | ||
| Spiritual change | Men | Physician | 4.6739 | 2.76530 |
| Nurse | 4.8065 | 2.63843 | ||
| Women | Physician | 3.9688 | 2.26451 | |
| Nurse | 5.8557 | 2.29124 | ||
| Appreciation of life | Men | Physician | 9.3913 | 3.70272 |
| Nurse | 8.7419 | 3.57741 | ||
| Women | Physician | 9.2500 | 3.15206 | |
| Nurse | 11.1134 | 2.71522 |
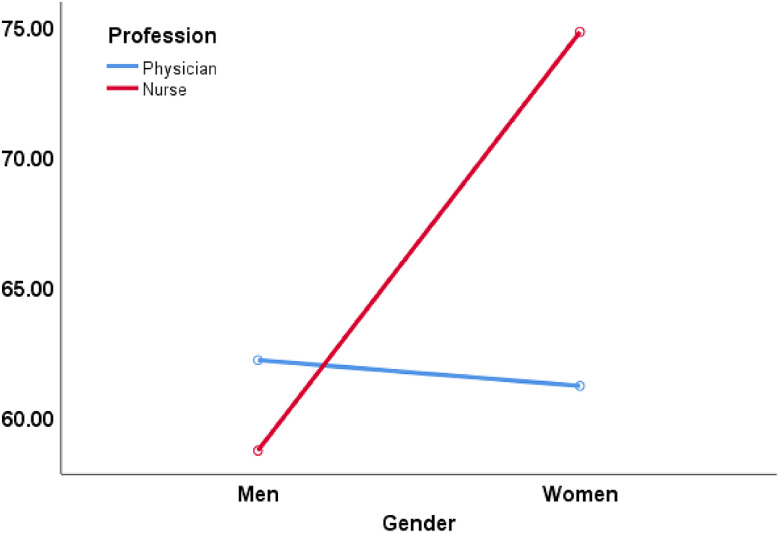
Contrary to main effects, we found a pronounced and significant interaction effect (Gender × Profession) regarding PTG scores and its subscales. F statistics ranged from 4.725 to 9.618, and P-value was ranged from 0.031 to 0.002. Effect size was measured by partial η2 ranged from 0.023 to 0.047. It seems that a pronounced interaction effect between gender and profession was across the board, meaning this interaction effect was found in the general PTG score and in each of its subscales. Among men, there was no difference in the level of PTG and its subscales based on profession. However, among women, nurses had a significantly higher scores in PTG and its subscales in comparison to physicians except for PTG subscale Relating to others (this result albeit significant in the MANCOVA was found as non-significant in a t-test among women split based on profession). See Figure 1 for the PTG interaction. PTG subscales figures are presented in the online supporting material.
Figure 1.
Interaction of gender × position regarding PTG total score.
Another interesting results revealed that years of experience in the profession (F = 4.103; P = 0.044; partial η2 = 0.020) and years of experience in the current department (F = 7.044; P = 0.009; partial η2 = 0.035) were associated significantly with PTG subscale Appreciation of life (Table 3).
Table 3.
Results of the MANCOVA (N = 206)
| Source | Dependent variable | Type III sum of squares | df | F | Sig. | Partial Eta squared |
|---|---|---|---|---|---|---|
| Age | Relating to others | 2.147 | 1206 | 0.058 | 0.810 | 0.000 |
| New possibilities | 1.677 | 1206 | 0.067 | 0.796 | 0.000 | |
| Personal strength | 18.181 | 1206 | 1.447 | 0.230 | 0.007 | |
| Spiritual change | 0.117 | 1206 | 0.019 | 0.890 | 0.000 | |
| Appreciation of life | 13.090 | 1206 | 1.341 | 0.248 | 0.007 | |
| Posttraumatic growth | 122.911 | 1206 | 0.418 | 0.519 | 0.002 | |
| Marital status | Relating to others | 15.715 | 1206 | 0.426 | 0.515 | 0.002 |
| New possibilities | 62.606 | 1206 | 2.499 | 0.116 | 0.013 | |
| Personal strength | 9.255 | 1206 | 0.737 | 0.392 | 0.004 | |
| Spiritual change | 0.001 | 1206 | 0.000 | 0.989 | 0.000 | |
| Appreciation of life | 6.614 | 1206 | 0.677 | 0.411 | 0.003 | |
| Posttraumatic growth | 320.926 | 1206 | 1.091 | 0.298 | 0.006 | |
| Years of experience in profession | Relating to others | 34.566 | 1206 | 0.936 | 0.334 | 0.005 |
| New possibilities | 5.166 | 1206 | 0.206 | 0.650 | 0.001 | |
| Personal strength | 10.272 | 1206 | 0.818 | 0.367 | 0.004 | |
| Spiritual change | 4.780 | 1206 | 0.784 | 0.377 | 0.004 | |
| Appreciation of life | 40.058 | 1206 | 4.103 | 0.044 | 0.020 | |
| Posttraumatic growth | 254.385 | 1206 | 0.865 | 0.354 | 0.004 | |
| Years of experience in the current department | Relating to others | 60.779 | 1206 | 1.646 | 0.201 | 0.008 |
| New possibilities | 61.636 | 1206 | 2.460 | 0.118 | 0.012 | |
| Personal strength | 2.457 | 1206 | 0.196 | 0.659 | 0.001 | |
| Spiritual change | 0.095 | 1206 | 0.016 | 0.901 | 0.000 | |
| Appreciation of life | 68.759 | 1206 | 7.044 | 0.009 | 0.035 | |
| Posttraumatic growth | 690.121 | 1206 | 2.346 | 0.127 | 0.012 | |
| Percentage of employment | Relating to others | 62.473 | 1206 | 1.692 | 0.195 | 0.009 |
| New possibilities | 22.751 | 1206 | 0.908 | 0.342 | 0.005 | |
| Personal strength | 44.843 | 1206 | 3.570 | 0.060 | 0.018 | |
| Spiritual change | 0.322 | 1206 | 0.053 | 0.819 | 0.000 | |
| Appreciation of life | 0.000 | 1206 | 0.000 | 0.997 | 0.000 | |
| Posttraumatic growth | 479.569 | 1206 | 1.630 | 0.203 | 0.008 | |
| Gender | Relating to others | 455.534 | 1206 | 12.335 | 0.001 | 0.059 |
| New possibilities | 103.872 | 1206 | 4.146 | 0.043 | 0.021 | |
| Personal strength | 62.420 | 1206 | 4.970 | 0.027 | 0.025 | |
| Spiritual change | 1.954 | 1206 | 0.320 | 0.572 | 0.002 | |
| Appreciation of life | 65.247 | 1206 | 6.684 | 0.010 | 0.033 | |
| Posttraumatic growth | 2311.952 | 1206 | 7.859 | 0.006 | 0.038 | |
| Profession | Relating to others | 1.247 | 1206 | 0.034 | 0.854 | 0.000 |
| New possibilities | 191.240 | 1206 | 7.634 | 0.006 | 0.037 | |
| Personal strength | 40.056 | 1206 | 3.189 | 0.076 | 0.016 | |
| Spiritual change | 45.285 | 1206 | 7.426 | 0.007 | 0.036 | |
| Appreciation of life | 17.740 | 1206 | 1.817 | 0.179 | 0.009 | |
| Posttraumatic growth | 1046.726 | 1206 | 3.558 | 0.061 | 0.018 | |
| Gender × profession | Relating to others | 174.508 | 1206 | 4.725 | 0.031 | 0.023 |
| New possibilities | 199.643 | 1206 | 7.969 | 0.005 | 0.039 | |
| Personal strength | 98.730 | 1206 | 7.860 | 0.006 | 0.038 | |
| Spiritual change | 40.526 | 1206 | 6.646 | 0.011 | 0.033 | |
| Appreciation of life | 74.159 | 1206 | 7.597 | 0.006 | 0.037 | |
| Posttraumatic growth | 2829.293 | 1206 | 9.618 | 0.002 | 0.047 |
* = P ≤ 0.05; ** = P ≤ 0.01; *** = P ≤ 0.001.
Discussion
The present study aimed to explore if there was an interaction effect between gender (women and men) and profession with the assessment of PTG among nurses and physicians in a tertiary care hospital. The results reveled that PTG among nurses and physicians is better to be assessed in light of this interaction effect, and not as separate factors that are linked to PTG. Specifically, our main findings show that among men, PTG was not different in male nurses and male physicians. However, when it comes to women, nurses exhibited higher scores of PTG and its subscales (except for PTG subscale relating to others) in comparison to women physicians. These findings were not previously known, as previous studies did not explore the interaction effect of gender and profession. Thus, we cannot suggest reinforcement or disapproving of the current results.
Yet, possible explanation may be related to the differences between women physicians in comparison to their male counterparts. According to Robinson (2003), women physicians may lack role models, face challenges of dual-career couples, have to reconcile with a finite number of years for childbearing, face lack of parity in salaries, receive a lower number of promotions to leadership positions, and experience higher rates of sexual harassment. Moreover, Roter and her colleagues (2002) found in their meta-analytic review about medical communication among physicians that women physicians engage in more communication that can be considered patient-centered and have longer visits than their male colleagues. The aforementioned factors may affect their work-related stress and in turn their PTG experience. In line with this notion, previous studies showed that the higher the distress among health care providers, the lower their personal growth (eg, Hagenaars and van Minnen, 2010; Măirean, 2016). Nevertheless, our results did not reveal profession differences with PTG subscale of Relating to others between women nurses versus women physicians. According to Tedeschi and Calhoun (1996; 2004), this subscale refers to recognition of one’s vulnerability which can lead to more willingness to accept help, more expressiveness, and increased self-disclosure. The individual may perceive a higher emotional connection with others, as well as a feeling of closeness in interpersonal relationships. Possible explanation may stem from women’s gender-specific socialization messages regarding roles, emotions, and cognitions. Sociologists describe the sex role socialization as “instrumental” for men and “expressive” for women. Expressive socialization includes learning to nurture, to be affiliative, and to be sensitive to needs of others (Strasen, 1992). Given that, it may be reasonable to assume that this factor of PTG will not be different in both professions as it in the essence of being a woman.
With regard to the absence of difference with PTG scores among male nurses versus male physicians, it may be that masculine attributes are more dominant than profession. In line with this notion, Wu et al. (2015) suggested that male nurses distanced themselves from the more emotive aspects of care as a form of protection, objectively providing patient and family care. Likewise, Hollup (2014) noted that male nurses may find it difficult to assume the caregiver role while negotiating a feminized environment because it disrupts the gender normative view of masculinity. Moreover, according to Roter and Hall, (2015), women physicians exhibit more emotional response to their patients in comparison to male physicians, by talking more about emotions, and by expressing empathy and concern. These findings confirmed the role gender attributes as being above the profession’s differences.
Concerning the typical investigation of the link between profession and PTG, our results confirmed previous researches (eg, Manning-Jones et al., 2016; Shiri et al., 2008; Taubman Ben-Ari and Weintroub, 2008) showing that nurses reported on higher level of PTG than physicians. Possible explanation which was also suggested by the researchers (eg, Moriel et al., 2017; Taubman Ben-Ari and Weintroub, 2008) referred to the difference in the character of their work. Specifically, nurse’s role involves much closer contact with patients and more intimate involvement in their physical, physiological, and mental needs. As such, they might be exposed to higher work-related stress but at the same time may enjoy from high PTG due to the positive link between posttraumatic stress and PTG (eg, Hamama-Raz and Minerbi, 2019). Another possible explanation might stem from the availability and the enactment of peer social support among nurses in comparison to physicians. According to Duffy et al. (2015), nurses may have more opportunities to share and communicate work stressors due to the presence of more co-workers from the same profession. However, among physicians the opportunities to share their emotions experienced after exposure to work-related stressors available only with few co-workers present (Bruce et al., 2005).
With regard to the link between gender and PTG, our findings revealed that being a woman was associated with higher PTG total scale and its subscales except for Spiritual change. This result was not found in previous researches in references to health care professional (eg, Kang et al., 2018; Manning-Jones et al., 2016, 2017; Rodríguez-Rey et al., 2017); however, among the general population (men and women who experience similar traumatic events), indeed women show higher levels of PTG than men (eg, Helgeson et al., 2006; Vishnevsky et al., 2010). Possible explanation may stem from Vishnevsky et al.’s (2010) meta-analysis that suggests to relate to women’s tendency to engage in deeper thought than men. This tendency may increase awareness of personal strengths or an appreciation of the importance of social connections and has been suggested as a mechanism leading to greater reports of PTG (Vishnevsky et al., 2010). In line with this notion, the Theory of Cognitive Adaptation (Taylor, 1983) posits that humans cope with threats in their lives by creating a set of positive illusions, which serve to protect their psychological health. As such, Czajkowska (2017) claimed that “These positively slanted cognitions are not considered delusional or inaccurate but rather represent a sign of mental as they create space for hope, personal growth, and flexibility” (p. 1). With the aforementioned, it might be that woman’s tendency to engage in deeper thought enables to experience higher PTG.
Finally, our results revealed that participants’ years of experience in the profession and years of experience in the department were linked positively with PTG subscale – Appreciation of life. Tedeschi and Calhoun (1996; 2004) noted that due to the cognitive reconstruction, the individual’s priorities in life change and one experiences a greater appreciation of life in general and for the “smaller things” in life. In line with this notion, it might be that through the seniority of years in their profession, nurses and physicians were able to identify desirable elements of their existence that their patients are missing, as well as experiences that they fortunate to avoid. As such they appreciate much more the simple facets of their life (Hyatt-Burkhart, 2014).
Limitations
The above discussion should be considered within several limitations. First, the present study is based on cross-sectional data; that is, the participants were asked to respond one single time, absent longitudinal follow-up, which did not allow to draw conclusions about causality. Thus, future studies recommended to employ longitudinal design that may provide indications of the nature of changes in health care providers’ PTG over time. Second, the sample is based on a single medical center, which may limit the potential generalizability of the results. Third, the Spiritual change had low reliability index meaning that the results of this subscale should be interpreted with cautious. Fourth, we may have a sampling bias as we used a convenience sampling in our study. Fifth, in a large sample, most correlations in a correlation matrix will show evidence of a statistical effect. Hence, these results should be interrupted with cautious. However, in order to overcome this, we have used the effect size in the MANCOVA procedure in order to reduce this bias.
Future studies might replicate the present one at other medical centers in other medical systems. Finally, the study relies on self-reports and thus might suffer from a social desirability bias.
Implications
Taking into account the findings, this study carries implications in both research and clinical practice in several directions. With regard to research implication, the study results suggest to explore PTG among health care providers according to interaction effect of gender (women and men) with profession (nurses and physicians), as evaluating each factor separately might provide only partial findings regarding PTG. Considering the practical implications, the study’s results reinforce the need for tailoring intervention programs aimed at increasing PTG through gender and profession sensitivity, and not by gender or professional as a single factor. This can be achieved by encouraging nurses and physicians to take action (according the Action-Focused Growth model – Hobfoll et al., 2007) in searching in line with their gender role a variety of sources of meaning, including defining their personal values, finding new goals, and perhaps, revising their life priorities. All of these are different aspects of the PTG process which should be translated into personal and social actions in order to renew feelings of competency (Hobfoll et al., 2007) based on the interaction effects of gender and profession (See also Templeton et al., 2019).
Conclusions
The current study highlights the need for a more cohesive view of PTG among hospital workers rather than the traditional binary perception of PTG from either gender or profession. Future studies evaluating the interaction effect of gender with profession in PTG are warranted (among other professions), in order to further establish the need to incorporate such interaction effect in health care personnel.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1463423620000377.
click here to view supplementary material
Financial Support
The research was not funded by any organization.
Conflicts of Interest
The authors declare no conflicts of interest.
Ethical Standards
The study was approved by the last author’s Institutional Review Board, situated in a medical center in Israel (No. 0057-19-ASF). The participants were included after giving their informed consent
Availability of data and materials
Data are available from the corresponding author on reasonable request
References
- Benyamini Y, Blumstein T, Lusky A and Modan B (2003) Gender differences in the self-rated health–mortality association: Is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? Gerontologist 43, 396–405. [DOI] [PubMed] [Google Scholar]
- Bruce SM, Conaglen HM and Conaglen JV (2005) Burnout in physicians: A case for peer support. Internal Medicine Journal 35, 272–278. [DOI] [PubMed] [Google Scholar]
- Cocker F and Joss N (2016) Compassion fatigue among healthcare, emergency and community service workers: A systematic review. International Journal of Environmental Research and Public Health 13, 618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czajkowska Z (2017). Theory of Cognitive Adaptation. Encyclopedia of Personality and Individual Differences, 1–3.
- Duffy E, Avalos G and Dowling M (2015). Secondary traumatic stress among emergency nurses: A cross-sectional study. International Emergency Nursing 23, 53-58. [DOI] [PubMed] [Google Scholar]
- El-Bar N, Levy A, Wald HS and Biderman A (2013) Compassion fatigue, burnout and compassion satisfaction among family physicians in the Negev area-a cross-sectional study. Israel Journal of Health Policy Research 2, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagenaars MA and van Minnen A (2010) Posttraumatic growth in exposure therapy for PTSD. Journal of Traumatic Stress 23, 504–508. [DOI] [PubMed] [Google Scholar]
- Hamama L, Hamama-Raz Y, Stokar Y, Pat-Horenczyk R, Brom D and Harlev-Bron E (2019) Burnout and perceived social support in physicians and nurses: The mediating role of secondary traumatization. Journal of Advanced Nursing. doi: 10.1111/jan.14122. [DOI] [PubMed] [Google Scholar]
- Hamama-Raz Y and Minerbi R (2019) Coping strategies in secondary traumatization and post-traumatic growth among nurses working in a medical rehabilitation hospital: A pilot study. International Archives of Occupational Environmental Health 92, 93–100. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Reynolds KA and Tomich PL (2006) A meta-analytic review of benefit finding and growth. Journal of Consulting and Clinical Psychology 74, 797–816. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE (1989) Conservation of resources: A new attempt at conceptualizing stress. American Psychologist 44, 513–524. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE (2011) Conservation of resources theory: Its implication for stress, health, and resilience In Folkman S, editor, The Oxford Handbook of Stress, Health, and Coping. New York: Oxford University Press, 127–147. [Google Scholar]
- Hobfoll SE, Hall BJ, Canetti-Nisim D, Galea S, Johnson RJ and Palmieri PA (2007). Refining our understanding of traumatic growth in the face of terrorism: Moving from meaning cognitions to doing what is meaningful. Applied Psychology: An International Review 56, 345–366. [Google Scholar]
- Hollup O (2014) The impact of gender, culture, and sexuality on Mauritian nursing: Nursing as a non-gendered occupational identity or masculine field? Qualitative study. International Journal of Nursing Studies 51, 752–760. [DOI] [PubMed] [Google Scholar]
- Höltge J, Mc Gee SL, Maercker A and Thoma MV (2018) A salutogenic perspective on adverse experiences. European Journal of Health Psychology 25, 53–69. [Google Scholar]
- Hyatt-Burkhart D (2014) The experience of vicarious posttraumatic growth in mental health workers. Journal of Loss and Trauma 19, 452–461. [Google Scholar]
- Kang X, Fang Y, Li S, Liu Y, Zhao D, Feng X, Wang Y and Li P (2018) The benefits of indirect exposure to trauma: The relationships among vicarious posttraumatic growth, social support, and resilience in ambulance personnel in China. Psychiatry Investigation 15, 452–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouta C and Kaite CP (2011) Gender discrimination and nursing: A literature review. Journal of Professional Nursing 27, 59–63. [DOI] [PubMed] [Google Scholar]
- Laufer A and Solomon Z (2006) Posttraumatic symptoms and posttraumatic growth among Israeli youth exposed to terror incidents. Journal of Social and Clinical Psychology 25, 429–447. [Google Scholar]
- Măirean C (2016) Secondary traumatic stress and posttraumatic growth: Social support as a moderator. The Social Science Journal 53, 14–21. [Google Scholar]
- Malhotra M and Chebiyan S (2016) Posttraumatic growth: Positive changes following adversity-an overview. International Journal of Psychology and Behavioral Sciences 6, 109–118. [Google Scholar]
- Manning-Jones S, de Terte I and Stephens C (2015) Vicarious posttraumatic growth: A systematic literature review. International Journal of Wellbeing 5, 125–139. [Google Scholar]
- Manning-Jones S, de Terte I and Stephens C (2016) Secondary traumatic stress, vicarious posttraumatic growth, and coping among health professionals: A comparison study. New Zealand Journal of Psychology 45, 20–29. [Google Scholar]
- Manning-Jones S, de Terte I and Stephens C (2017) The relationship between vicarious posttraumatic growth and secondary traumatic stress among health professionals. Journal of Loss and Trauma 22, 256–270. [Google Scholar]
- Moriel D, Felix K and Quinlan P (2017) Roles and responsibilities: Asking nurses and physicians what they know, do not know and want to know about the other’s profession. Journal of Research in Interprofessional Practice and Education 7 10.22230/jripe.2017v7n1a253 [DOI] [Google Scholar]
- Ogińska-Bulik N (2006) Occupational stress and its consequences in healthcare professionals: the role of type D personality. International Journal of Occupational Medicine and Environmental Health 19, 113–122. [DOI] [PubMed] [Google Scholar]
- Robinson GE (2003) Stresses on women physicians: Consequences and coping techniques. Depression and Anxiety 17, 180–189. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Rey R, Palacios A, Alonso-Tapia J, Pérez E, Álvarez E, Coca A, Mencía S, Marcos AM, Mayordomo-Colunga J, Fernández F, Gómez F, Cruz J, Barón L, Calderón RM and Belda S (2017) Posttraumatic growth in pediatric intensive care personnel: Dependence on resilience and coping strategies. Psychological Trauma: Theory, Research, Practice, and Policy 9, 407–415. [DOI] [PubMed] [Google Scholar]
- Roter DL and Hall JA (2015) Women doctors don’t get the credit they deserve. Journal of General Internal Medicine 30, 273–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roter DL, Hall JA and Aoki Y (2002) Physician gender effects in medical communication: A meta-analytic review. JAMA 288, 756–764. [DOI] [PubMed] [Google Scholar]
- Strasen L (1992) The Image of Professional Nursing: Strategies for Action. Lippincott Williams & Wilkins. [Google Scholar]
- Shiri S, Wexler ID, Alkalay Y, Meiner Z and Kreitler S (2008) Positive and negative psychological impact after secondary exposure to politically motivated violence among body handlers and rehabilitation workers. Psychotherapy and Psychosomatics 196, 906–911. [DOI] [PubMed] [Google Scholar]
- Shoji K, Bock J, Cieslak R, Zukowska K, Luszczynska A and Benight CC (2014) Cultivating secondary traumatic growth among healthcare workers: The role of social support and self-efficacy. Journal of Clinical Psychology 70, 831–846. [DOI] [PubMed] [Google Scholar]
- Solbrække KN, Solvoll B-A and Heggen KM (2013) Reframing the field of gender and nursing education. Gender and Education 25, 640–653. [Google Scholar]
- Stucky ER, Dresselhaus TR, Dollarhide A, Shively M, Maynard G, Jain S, Wolfson T, Weinger MB and Rutledge T (2009) Intern to attending assessing stress among physicians. Academic Medicine 84, 251–257. [DOI] [PubMed] [Google Scholar]
- Taubman Ben-Ari O and Weintroub A (2008) Meaning in life and personal growth among pediatric physicians and nurses. Death Studies 32, 621–645. [DOI] [PubMed] [Google Scholar]
- Taylor SE (1983) Adjustment to threatening events: A theory of cognitive adaptation. American Psychologist 38, 1161–1173. [Google Scholar]
- Tedeschi RG and Calhoun LG (1996) The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress 9, 455–471. [DOI] [PubMed] [Google Scholar]
- Tedeschi RG and Calhoun LG (2004) Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry 15, 1–18. [Google Scholar]
- Templeton KC, Bernstein J, Sukhera LM, Nora C, Newman H, Burstin C, Guille C, Lynn L, Schwarze ML, Sen S and Busis N (2019) Gender-based differences in burnout: Issues faced by women physicians. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. 10.31478/201905 [DOI]
- Vishnevsky T, Cann A, Calhoun LG, Tedeschi RG and Demakis GJ (2010) Gender differences in self-reported posttraumatic growth: A meta-analysis. Psychology of Women Quarterly 34, 110–120. [Google Scholar]
- Wu TW, Oliffe JL, Bungay V and Johnson JL (2015) Male ICU nurses’ experiences of taking care of dying patients and their families: A gender analysis. American Journal of Men’s Health 9, 44–52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1463423620000377.
click here to view supplementary material
Data Availability Statement
Data are available from the corresponding author on reasonable request