Abstract
Ethnopharmacological relevance
Traditional pharmacopeias have been developed by multiple cultures and evaluated for efficacy and safety through both historical/empirical iteration and more recently through controlled studies using Western scientific paradigms and an increasing emphasis on data science methodologies for network pharmacology. Traditional medicines represent likely sources of relatively inexpensive drugs for symptomatic management as well as potential libraries of new therapeutic approaches. Leveraging this potential requires hard evidence for efficacy that separates science from pseudoscience.
Materials and methods
We performed a review of non-Western medical systems and developed case studies that illustrate the epistemological and practical translative barriers that hamper their transition to integration with Western approaches. We developed a new data analytics approach, in silico convergence analysis, to deconvolve modes of action, and potentially predict desirable components of TM-derived formulations based on computational consensus analysis across cultures and medical systems.
Results
Abstraction, simplification and altered dose and delivery modalities were identified as factors that influence actual and perceived efficacy once a medicine is moved from a non-Western to Western setting. Case studies on these factors highlighted issues with translation between non-Western and Western epistemologies, including those where epistemological and medicinal systems drive markets that can be epicenters for zoonoses such as the novel Coronavirus. The proposed novel data science approach demonstrated the ability to identify and predict desirable medicinal components for a test indication, pain.
Conclusions
Relegation of traditional therapies to the relatively unregulated nutraceutical industry may lead healthcare providers and patients to underestimate the therapeutic potential of these medicines. We suggest three areas of emphasis for this field: First, vertical integration and embedding of traditional medicines into healthcare systems would subject them to appropriate regulation and evidence-based practice, as viable integrative implementation mode. Second, we offer a new Bradford-Hill-like framework for setting research priorities and evaluating efficacy, with the goal of rescuing potentially valuable therapies from the nutraceutical market and discrediting those that are pseudoscience. Third, data analytics pipelines offer new capacity to generate new types of TMS-inspired medicines that are rationally-designed based on integrated knowledge across cultures, and also provide an evaluative framework against which to test claims of fidelity and efficacy to TMS made for nutraceuticals.
Keywords: Pain, Traditional medicine, Indigenous medicine, Healthcare economics, Phytomedicine, Network pharmacology
Abbreviations: TRP, Transient Receptor Potential channel; WHO, World Health Organization; TCM, Traditional Chinese Medicine; TM, Traditional Medicine; CAM, Complementary and Alternative Medicine; TTTM, Translated/Transformed Traditional Medicines; ISCA, In silico convergence analysis; TMS, Traditional Medical System
Graphical abstract
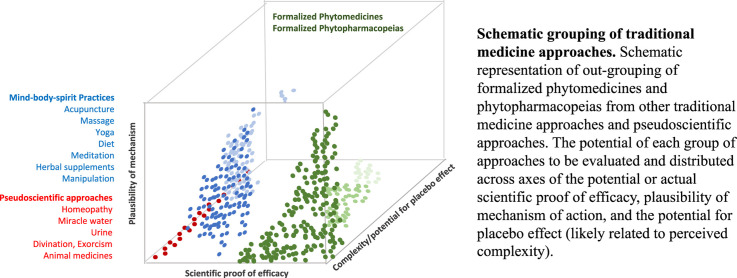
Schematic grouping of traditional medicine approaches. Schematic representation of out-grouping of formalized phytomedicines and phytopharmacopeias from other traditional medicine approaches and pseudoscientific approaches. The potential of each group of approaches to be evaluated and distributed across axes of the potential or actual scientific proof of efficacy, plausibility of mechanism of action, and the potential for placebo effect (likely related to perceived complexity).
1. Introduction: TM practices across cultures and geographies
Practices known as traditional medicines (TM) include ethnomedical beliefs and traditions specific to individual cultures, as well as traditional medical systems practiced more widely across multiple cultural contexts. The World Health Organization (WHO) defines traditional medicine as “the sum total of the knowledge, skills, and practices based on the theories, beliefs, and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness” (World Health Organization, 2013). Each culture has its set of ethnomedical beliefs and practices associated with health and illness, which shape diagnosis, treatment, and expected outcome. Indigenous medical practices employ a wide range of diagnostic and treatment modalities, including, for example, divination, preparation and use of medicines from plant and animal sources, practitioner-led mending of social transgressions, massage, and a wide range of spiritual/religious rituals incorporating singing, chanting, dancing, and other bodily movements and vocalizations. These practices are guided by and logically consistent with the culturally specific beliefs about what contributes to health and illness, and how illness should be treated. While similarities across the medical practices of many indigenous groups can be seen (e.g., many cultures employ herbal preparations therapeutically), the underlying cultural rationales may differ significantly (Rubel and Haas, 1996).
Traditional medicine is often contrasted with ‘scientific’ medicine. This is problematic terminology since it is colonizing (with the latter being assumed to be the purview of Western practitioners, assuming a lack of science in indigenous cultures and relegating these medical systems to ‘folk medicine’) and outdated since in numerous medical systems there are now significant evidence bases using the Western definitions of efficacy (such as randomized or otherwise controlled trials, in vitro and in vivo proofs of mechanism) that support some uses of TM. However, WHO notes that “inappropriate use of traditional medicines or practices can have negative or dangerous effects” and that “further research is needed to ascertain the efficacy and safety”. Indeed, there are multi-dimensional problems associated with the prevalence of TM, a field contaminated by fraudulent practitioners, adulterated medications, pseudoscience, unsafe supply chains, toxic components and alternative medical approaches vaguely and improperly abstracted from their original use and formulations. There is also an extensive global nutraceutical (defined as pharmacological alternatives that claim physiological benefit) industry that sits in a space between Western and TM systems, often claims fidelity to some form of traditional knowledge, and is poorly regulated. The (World Health Organization, 2013) call to action from WHO to develop evidence bases for the use or rejection of TM has a number of inherent challenges and challenges rooted in tensions between Western and traditional medicine, and consideration of these is the impetus for the current review.
2. Background: medical systems
This section provides brief descriptions of some of the more professionalized medical systems (TCM, Kampo, Ayurveda, Unani). The differences between more and less formal medical systems are not meant to be value judgments on the quality or validity of the practices. Instead, they are meant to provide descriptive insight for the following discussion of different medical systems. However, the more professionalized medical systems exemplify both the promises and pitfalls of trying to establish an evidence base for use of TM and we focus on discussion of them and leave for other studies an in-depth treatment of African, Native North American, Shamanic and other important medical approaches (Abdullahi, 2011; Adekson, 2016; Isaac et al., 2018; Macfarlane, 2009; Nauman, 2007; Steinhorn et al., 2017; Van Wyk, 2020; Wambebe, 2018).
The degree of formalization, standardization, and professionalization varies considerably across indigenous medical practices. While all culturally specific medical beliefs and practices are systematic in the sense that they are organized according to cultural logic and that they integrate into the ways and values of society, many indigenous ethnomedical practices are relatively informal in their structure and social organization. By contrast, systems like Traditional Chinese Medicine (TCM) and Ayurveda have formal, professional training and licensure of practitioners defined and overseen by state government authorities, have standardized written medical texts (including pharmacopeias which are critical guides for formulation, compounding, etc.) shared widely among students and practitioners, and have professional associations and institutions (Leslie, 1998; Leslie and Young, 1992). These medical systems are often practiced across a diverse cultural landscape, alongside more regional ethnomedical traditions, in a syncretic fashion (Chitindingu et al., 2014). Examples derived from the historical and contemporary landscape of medical systems of interest in this paper are presented in brief below:
Traditional Chinese Medicine (TCM). Mental and physical practices as well as phytomedicine, animal and mineral remedies, the Doctrines of Chinese medicine are rooted in cosmological concepts such as yin–yang and five phases known as water, wood, fire, earth and metal. TCM describes health as the harmonious interaction of these entities and the outside world, and disease as a disharmony. TCM diagnoses trace symptoms to patterns of the underlying disharmony, by measuring the physiological indicators. TCM was developed over ~3500 years with standardization efforts from 1950s onwards in the People's Republic of China (Hsu, 2018).
Kampo medicine. Kampo is a component of medical practice in contemporary Japan that has its origins in Chinese medical practices first developed in the Han Dynasty (206 BC-AD 220) (Otsuka, 2016). The medicines and associated practices were first introduced to Japan via Korea in the seventh to ninth centuries AD, with a subsequent influx of Chinese medical practices beginning in 1498 (Inoue et al., 2017). Though Kampo shares many elements with Traditional Chinese Medicine, it also developed into a uniquely Japanese practice between the two periods of Chinese introduction and subsequent to Japan cutting off contact with outsiders in 1630 CE (Inoue et al., 2017; Otsuka, 2016). During the Meiji Restoration (beginning in 1868), Kampo fell out of favor due to being perceived as not modern, and the Japanese government adopted German medical practice as the country's standard (Inoue et al., 2017; Otsuka, 2016). After the end of the second world war, Kampo underwent a renaissance in popularity. In 1976, it was included in the Japan National Insurance Programme, and today it is taught in all Japanese medical schools alongside Western biomedicine (Inoue et al., 2017; Otsuka, 2016).
Ayurveda. Ayurveda (Mukherjee et al., 2017) is an Indian medical system, based around epistemology of three energies (doshas): Vata is the energy of movement; pitta is the energy of digestion or metabolism and kapha is the energy of lubrication and structure. The cause of disease in Ayurveda is viewed as a lack of proper cellular function due to an excess or deficiency of vata, pitta or kapha. Disease can also be caused by the presence of toxins. Balance in constitution is ideal and the natural order; imbalance is disorder. Health is order; disease is disorder. Ayurvedic therapeutic approaches include phytomedicine, meditative practices, physical manipulation, diet, environment.
Traditional European medicine. Medicine in pre-Enlightenment Europe was a combination of elements derived from Greek and Roman medical writings, acquired through translations from Greek and Arabic sources, along with a mix of relatively poorly documented indigenous practices (Horden 2009; Leonti and Verpoorte 2017) (Horden, 2009; Leonti and Verpoorte, 2017). The more systematic of these practices were largely based on humourism, which is the belief that disease is caused by imbalance among the four “humours” (blood, phlegm, yellow bile, and black bile) (Hebron 2017) (Hebron, 2017). Humoural medicine sought to treat disease symptoms by inducing symptoms (often with extreme methodologies such as purging and bloodletting) seen as opposite to those of diseases rather than treating the underlying causes. Disease was viewed as caused by an excess of one humour and thus would be treated by inducing its opposite, however damaging. Unani is an Arab-Persian medical system also practiced widely in India. It is focused on prevention of disease and is similar to early European medicine in its idea of imbalances between fundamental humours. It focused on three therapeutic paths: Izalae Sabab (elimination of cause), Tadeele Akhlat (normalization of humours) and Tadeele Aza (normalization of tissues/organs).
Islamic medicine greatly informed the development of Western medicine through the dissemination of its essential texts, especially via the Ottoman Empire (Masic, 2017), and promotes holistic approaches to health as well as a ground-breaking emphasis on public hygiene and the authentication of phytomedicines (Masic, 2017).
Allopathic Western medicine. Strongly influenced by Greek philosophy and Arab/Islamic medicine prior to 1500 (Majeed, 2005), Allopathic Western medicine developed an increasingly evidence-based framework from the Renaissance through enlightenment and the industrial age. Allopathic Western medicine is science-based, modern medicine, that uses medications or surgery to treat or suppress symptoms or the ill effects of disease. Allopathic Western medicine utilized an evidence-based regulatory framework that demands a continuum of proofs of mechanism and efficacy prior to delivery.
A full discussion of timelines, geographies, and the complexities of comparing medical systems cross-culturally is beyond the scope of this paper, but we refer readers to Leonti and Verpoorte (2017) (Leonti and Verpoorte, 2017) for an excellent recent review of geographic and temporal influence of different medical traditions on each other. See also Etkin et al. (2008) (Etkin et al., 2008) and Etkin (2006) (Etkin, 2006) for discussion of cultural factors influencing therapeutic practice, and Leslie (1998) (Leslie, 1998) on comparative study of Asian medical systems.
3. Tensions between traditional and Western medicine
The relationship between TM and Western medicine is complex but there is an urgency to the development of frameworks to navigate the tensions between these two systems of knowledge. Frustration with ‘superstition’ and the very real threats deriving from the pseudoscience that contaminates most nutraceutical or naturopathic approaches leads Western allopathic medicine to strongly reject ‘alternative’ approaches, a position that may in fact play into the anti-establishment and anti-elite narratives of those promoting these approaches in an increasingly polarized society such as the US. However, there are realities in both the West and developing countries that Western medications are, or are becoming, out of reach economically for many patients (Ewen et al., 2017) (Wirtz et al., 2017). In developing nations there is a moral imperative to establish a framework for safe and effective use of these medicines since they may be all that is available, although this can be countered by an argument that such a reliance stifles medical progress towards a contemporary, Western system of treatment. The argument about costs extends also to markets such as the US where spiraling costs are removing conventional medicine from the low income or elderly patients (Briesacher et al., 2007) (Morgan and Lee, 2017; Zivin et al., 2010). Further, there is the potential critique that Western medicine is ‘throwing the baby out with the bathwater’ with respects to their reluctance to integrate TM into the current healthcare system. In a rejection of non-Western approaches rooted in the frustration and the clear threats of pseudoscience and quality-control issues described above, the opportunity for symptomatic management with TM-derived formulations that can be shown to be efficacious and utilized under the supervision of practicing physicians within “standard of care” guidelines is missed (Nishimura et al., 2009; Watanabe et al., 2011). Furthermore, the decreased costs and increased availability associated with rational integration of TM is not leveraged (Arita et al., 2016). Moreover, reconsideration of the position of rejection based on new evidence (such as ‘re-discovery’ of a compound that is a component of an established TM as efficacious using Western drug screening approaches, or new data showing efficacy of a TM formulation using a Western clinical trial format) is not taking place in a systematized way and is not driving a pathway for drugs out of the nutraceutical and into the pharmaceutical realm. The latter is especially problematic due to the requirements of the intellectual property system that forms the profit base for the pharmaceutical industry, as well as obvious issues with opportunistic cultural appropriation and bioprospecting that ‘re-discovery’ can create in a system that rewards corporations. A clear-sighted re-evaluation of TM with the goal of rational, evidence-based integration and de-relegation from nutraceuticals into regulated mainstream medicine may be desirable but requires some significant study of advantages and disadvantages of non-Western approaches (see Etkin (1988), Etkin and Elisabetsky (2005), and Browner et al. (1988) for discussions of ethnopharmacological methods for cross-cultural evaluation of medical systems; see also Farquhar (1994), Wolfgram (2009)) (Browner et al., 1988; Etkin, 1988; Etkin and Elisabetsky, 2005; Farquhar, 1994; Wolfgram, 2009). This paper evaluates various aspects of this challenge with a specific focus on plant-derived medicines, establishing these as an outgroup from other alternative medical approaches.
4. De-grouping: plant derived medicinal compound mixtures as an outgroup in CAM
The central thesis of this section is that plant-derived complex compound mixtures used in TM may be differentiated from several other groupings of complementary and alternative medicines (CAM) and therapies and should be considered separately when evaluating their potential. There is a very large number of approaches grouped under CAM, with varying degrees of evidence base for efficacy, biological mechanistic plausibility and potential for differentiation from placebo effects. Instruments such as indices of biological plausibility, variants of the Bradford-Hill criteria (Lucas and McMichael, 2005) or Koch's postulates, and statistical evidence from pre-clinical and clinical experimental settings can be used to discern the potential value of such CAM. We propose an adaptation of the Bradford-Hill criteria (Table 1 ) for application to CAM. Some CAM are gaining acceptance via demonstration of potential mechanism, statistical out-performance of the placebo effect and a clinical evidence base. For example, these include plant-derived medicines and acupuncture. In contrast, there are elements of the CAM spectrum that will likely never rise to these levels, such as homeopathy, miraculous water, urine therapy, and others. In the middle ground there are CAM that are in motion as their biological plausibility, evidence base and societal acceptance morph. For example, as mainstream appreciation of integrative medicine approaches that integrate mind-body-spirit wellness concepts and practices increases (and patient demand for them increases) there are CAM that are gaining acceptance across mainstream healthcare providers, major medical systems, and insurers. Some of these include yoga and other movement practices, massage, acupuncture, diet and herbs, chiropractice, visualization, meditation and spiritual practices.
Table 1.
Adapted Bradford-Hill criteria for evaluation of traditional medical approaches.
| Bradford-Hill Criteria (BHC) | Re-stated BHC definition for application to TM evaluation | Approach/Recommendations |
|---|---|---|
| Strength | Prescriptions that strongly affect therapeutic outcomes are the most credible. | Invest in robust programs of study that enable reductionist evaluation of a potential therapeutic for its statistical improvement over placebo or control, and its relative efficacy to standard-of-care approaches. Strengthen systems to educate consumers, discredit and prevent adoption of therapeutic approaches that are ineffective. |
| Consistency | Multiple methodologies, studies and context support the association between therapy and outcome. | Design in vitro and in vivo experiments, and clinical trials that employ best practices (reductionist experimentation, randomized controlled trials, prospective and retrospective observational studies) to assess the statistical improvement over placebo offered by a candidate therapeutic. Measure specific clinical indicators of outcome not general health, weakly associated phenomena or perceived value. |
| Specificity | The prescribed exposure is necessary and sufficient to generate the therapeutic outcome. | Apply reductionist approaches in in vitro, in vivo and clinical work; Disaggregate effects from confounding exposures (e.g. other medicines, CAMs) in clinical data analysis; Systematize capture and inclusion of patient reported outcomes (PRO) in considerations of efficacy in a manner that can apply statistical tests. |
| Temporality | The prescribed exposure must precede the therapeutic outcome. | Design in vitro, in vivo and clinical studies appropriately; Incorporate temporality into judgement of biological plausibility (e.g., s time taken to act consistent with the behavior of the disease?). |
| Biological gradient | The likelihood of a causal therapeutic association is increased if a biological gradient or dose–response curve can be demonstrated. | Design in vitro, in vivo and clinical studies appropriately; Account for dose, modality and formulation when converting potential therapeutics between medical systems; Generate dose-response relationships with an emphasis on effect sizes that statistically out-perform placebo; Contextualize dose-effectiveness relationships by comparison with an appropriate standard-of-care approach; Contextualize reports on efficacy with analyzes of safety and side effect profiles, again in reference to standard-of care approaches. |
| Plausibility | A plausible biological mechanism for efficacy exists | Use in silico and computational approaches for unbiased identification of potential therapeutic components and associate them with plausible mechanisms before applying them in laboratory or clinic; Understand that what is viewed as biologically plausible depends upon the ‘biological knowledge of the day’ and consistently surveilled literature to re-evaluate potential therapeutics in light of new scientific evidence for potential mechanisms; |
| Coherence | A cause-and-effect interpretation of a therapeutic association between therapy and outcome should fit with the known facts of the natural history, biology and be temporally appropriate. | Establish standards for publication of data that summates all arguments for strength (efficacy), coherence and plausibility, safety and side-effect profiles based on experimental and scholarly analysis. |
| Experiment | Therapeutic actions taken on the basis of a demonstrated cause-and-effect association alter the frequency or severity of the outcome. | Use in silico and computational approaches for unbiased identification of potential therapeutic components and associate them with plausible mechanism before applying them in laboratory or clinic; Design in vitro and in vivo experiments, and clinical trials that employ best practices (reductionist experimentation, randomized controlled trials, prospective and retrospective observational studies) to assess the statistical improvement over placebo offered by a candidate therapeutic. Measure specific clinical indicators of outcome not general health, weakly associated phenomena or perceived value. |
| Analogy | Analogous proven examples of therapies exist. | Develop open source resources that collate and curate examples of analogous therapies with rigorous evidence bases; Develop a system for regular meta-analyses that compares scholarly evidence across indications and contexts. |
The more complex the medical intervention, even if sham, then the higher the potential for placebo effect (Geers et al., 2018). For interventions with low biological plausibility and high potential for placebo effect there has been extensive discussion as to their utility and whether they should be covered by insurers or recommended by providers. In reality, the use of insurance coverage as a proxy for regulation is inadequate in markets such as the U.S, where consumers have every right and opportunity to self-medicate, and is broadly irrelevant in many other countries. This is a complex debate with viewpoints ranging from the pragmatic to the radical: ranging from those arguing against any unproven therapy being embraced in mainstream medicine to those for whom a placebo effect that ‘does no harm’ can still be useful in care (Snow, 2016). It seems unlikely that the latter is true for many applications because nutraceuticals can do harm due to duplicative dosing, as well as unknown and unmonitored interactions with other nutraceuticals or prescription medicines that can occur. In TM, the definition of harm can be far broader than effects upon personhood of an informed consumer, making an argument for enhanced regulation according to global standards. Examples of this potential for broad impact beyond individual health can be found within the animal medicine practices of China, southeast Asia and Africa. The pursuit of animal supply chains endangers species and upsets the balance of ecosystems. The trade in animal parts suborns cruelty and juxtaposes zoonoses with humans. For example there were a few days in early 2020 when it seemed that pangolins were a secondary reservoir for SARS-Cov2 and that their trade as a medicinal component was an initiating event in the global COVID-19 pandemic (Cyranoski, 2020; Zhang et al., 2020). In this case, as in the earlier implication of civet as a reservoir in the prior SARS-1 outbreak, the data were erroneous but at the very least placed the species in brief danger of retaliatory or preventative culling (Luk et al., 2019).
Plant-derived compounds and therapeutic mixtures – if correctly designed and administered - are an out-group when compared to most CAM in terms of their high biological plausibility and relatively high evidence base for proof of efficacy (shown schematically in Graphical Abstract). While, in general, the more complex a therapy the higher likelihood of placebo effect (Kaptchuk, 2002; Paterson and Dieppe, 2005), in the case of phytomedicines their actual complexity may be masked by an apparently simple delivery regimen, and so their potential for placebo effect may be hard to predict and needs individualized study. We note that it was extremely hard to place indigenous medical practices as experienced within their cultural context and with fidelity to delivery modalities, doses and formulations on this schematic. There are precisely zero Cochrane analyses on this subject and few papers in PubMed that approach this problem in the context of cultural medicine, and this may reflect the bias inherent in indexing primarily English-language studies.
Both high biological plausibility (plausibility of mechanism) and lower potential for statistical out-performance of placebo are perhaps uniquely strong features of plant-derived medicines. These are pharmaceuticals and so by any definition their mechanism of action is through a receptor interaction with a small molecule that initiates cellular, tissue, organ and organismal effects on a biological system. The success of plant-derived mainstream drugs such as taxol, aspirin and artemisinin has decreased a priori skepticism of plant-derived therapies, and there is a burgeoning literature in identifying active compounds and their biological targets (Cragg and Newman, 2005). Moreover, in some TM settings, there is an active in-culture will and process for de-convolving and ‘proving’ the mechanism of action of traditional formulations, both as a validation and as a source of potential pharmaceutical approaches (e.g., Japan, China, Korea, India). However, in other settings, including some indigenous groups, this de-convolution and abstraction of medicines from their cultural context is viewed as neo-colonial, economically exploitative, and counter-cultural to indigenous values (Mark et al., 2019). Moreover, it may be viewed as conceptually unnecessary where indigenous practitioners and users of TM believe that simply being in touch with or using their cultural form of medicine brings spiritual benefits in and of itself. Proof-of-mechanism itself assists in decreasing skepticism, and indeed the differentiation between herbal medicines and allopathy is artificial when the efficacy of the herbal medicines has been demonstrated in controlled clinical studies. Western medicine has focused on the ‘bench to bedside’ paradigm, and there is the potential for the reverse ‘bedside to bench’ deconvolution and ‘rediscovery’ of active constituents from non-Western medical formulations. However, mechanism may not be a pre-requisite to the successful use of herbal medicine when there is clinical evidence or observable benefit, reflected in some of the simplified regulatory frameworks based on traditional use evidence that have been established in Europe (the Traditional Herbal Medicine Directive), Canada and Australia.
5. Transformation as a barrier to the study of efficacy: apples to oranges
When adopted outside its traditional or root culture, traditional medicine is often classified as a form of alternative medicine (AM), for example by Western professional medical organizations, insurers and healthcare systems. This problematically leads to lack of regulation (e.g., in the U.S. where these approaches are at best relegated to the nutraceutical market largely outside the FDA sphere of regulation) and a lack of fidelity to original formulations, dose schedules, delivery methods and indications. It may also be regarded as patronizing and neo-colonial by many indigenous and traditional practitioners who work within their own epistemological framework for effectiveness (Mark et al., 2019) (Wolfgram, 2009). We refer to these as Translated/Transformed Traditional Medicines (TTTM). It is in these contexts, rather than in indigenous settings with fidelity to the TMS under study, that many of these TTTM have been studied for efficacy and dismissed as either statistically insignificantly different from placebo or ineffective compared to a standard of care drug. In addition, TTTM, especially in the form of nutraceuticals adopted by an already heavily medicated population such as that of the US, have a false perception of ‘naturalness equates to safety’ when in fact there are numerous drug-nutraceutical interactions that pose hazards to health and natural products can be intrinsically harmful. An additional issue arises in the directionality of the perceived drug interaction, where a patient already exposed to multiple prescription drugs adds a nutraceutical and that is viewed as the toxic, drug interaction. Further, the regulatory system itself where marketing authorizations are ruled by International Commission on Harmonization (ICH) guidelines (e.g., US, Europe, Japan, Australia) use quality, efficacy and safety (in that order) as benchmarks for approval. This leads to a focus on quality and consistency rather than efficacy, and allows the manufacture of products referring to tradition, but technically unrelated to the traditional preparations.
The types of transformation/abstraction that occurs when medicine moves between cultures, and particularly from a traditional framework to the Western nutraceutical market can be summarized as follows:
-
•
Simplification and abstraction. TM formulations in systems such as Kampo or TCM are typically multiple herbs each of which may contain tens to hundreds of bioactive or potentially bioactive constituents. These are, by definition, polypharmacy approaches that may leverage synergy between plant components (Williamson, 2005). They are formulations that are ‘multi-targeting’ of parallel or complementary physiological or pathophysiological processes. Typical nutraceuticals simplify these mixtures to one or a few components while not down-scaling the claims of efficacy, which in turn do not have to be robustly proven so long as the labeling of dietary supplement is maintained. This simplification may translate to the loss of helpful interactions that contribute to efficacy in a poly-pharmacy formulation and may eliminate compounds that are minor or obscure constituents (bioactive components, excipients, etc.) contributing to efficacy but are not immediately obvious candidates for inclusion in a nutraceutical formulation.
-
•
Delivery modality, formulation and dose schedules. Asian medical systems are strongly biased towards modalities that emphasize powders and teas, and chronic delivery of low doses, usually daily. This strongly contrasts with the Western prevalence of tablets and encapsulation in medical and pseudo-medical settings. These different delivery modalities will fundamentally change the pharmacodynamic and pharmacokinetics of the compounds. Similarly, formulation with natural excipients or even nano-izing agents (Iitsuka et al., 2018) that are components of the TM may not be replicated with the filling agents, preservatives and other components that are more usually found in nutraceutical formulations for Western markets. Dose amounts may also be significantly altered as they are transposed between cultures, through either lowering to homeopathic amounts or heightening daily doses, based on considerations of lability and stability rather than evidence-based efficacy.
-
•
Conceptual basis for action and epistemology. The worldview and medical knowledge of the historical developers of TM, and indeed even of contemporary practitioners is fundamentally different from the underlying philosophy and knowledge base of Western medicine.
In this section we examine a series of case studies that illustrate the abstraction, transformation and epistemological conflicts that arise when TM enters a context such as the US nutraceutical market.
From ‘Awa to kava to Happy Camper. An extraction of Piper methysticum is used in several indigenous Pacific cultures as a drink associated with ritual, conflict resolution and socialization. The drink is known by the following names in the Pacific: ʻawa (Hawaiʻi), ʻava (Samoa), yaqona (Fiji), sakau (Pohnpei), seka (Kosrae), and malok or malogu (Vanuatu), with kava being a generic term (Showman et al., 2015). ‘Awa is non-psychoactive and non-stimulant, providing instead sensations of well-being, calm and is a mild soporific. It has a low side effect profile, with 1999–2001 reports of hepatotoxicity being now overwritten, and chronic use associated with a reversible icthyoform dermopathy in some Pacific populations (Kuchta et al., 2015; Showman et al., 2015). There is good clinical evidence that it is an anti-anxiolytic which is consistent with its use in traditional contexts (Sarris et al., 2013) and it may have potential for facilitation of tobacco cessation (Wang et al., 2020). Despite one widely cited fallacious report (Steiner, 2000), there is no epidemiological evidence for any protective effects in cancer although some of its components may show pro-apoptotic effects when applied to isolated cell lines in vitro or in murine models (Celentano et al., 2019; Einbond et al., 2017; Triolet et al., 2012). In the Pacific, ‘Awa is extracted using a tepid water extraction, broadly filtered using available materials (from Hibiscus mucilage to waste fabric or coffee filters). Nutraceutical formulations have largely relied on alcohol extraction which will significantly change the composition from the traditional aqueous extraction (Ji et al., 2018). Notably, one vendor from Fiji approaches yaqona with fidelity to cultural methods. ‘Awa in non-traditional use is subject to abstraction from contextual use and applications, adulteration resulting from economic issues and supply chain pressure, and altered extraction methods. Expansionist claims present on sales and promotional websites are bootstrapped from its effectiveness as an anti-anxiolytic and mild sedative action to stress, PMS, sleep disorders, neurodegeneration, cancer, migraines, infections, ‘cravings’, digestive health, inflammation, and rheumatism (VH Nutrition, 2020; Scaccia, 2018; Walle, 2018). There is no evidence base for these expanded claims.
From Rikkunshito to Licorice. ‘Rikkunshito’ is a Japanese Kampo (Nishimura et al., 2009) prescribed for loss of appetite due to various stomach issues. It consists of 8 distinct herbal medicines, ginseng, Atractylodes rhizome, Poria sclerotium, pinellia tuber, citrus unshiu peel, jujube, glycyrrhiza and ginger. ‘Rikkunshi-tō' (六君子湯, りっくんしとう) is a Japanese Kampo prescribed for loss of appetite due to various stomach issues. It consists of 8 distinct herbal medicines: Ninjin rhizome (人参, にんじん, ginseng; Panax ginseng C.A. Mey, Araliaceae), Byakujutsu rhizome (白朮, びゃくじゅつ; Atractylodes japonica Koidz, Asteraceae), Bukuryō sclerotium (茯苓, ぶくりょう; Wolfiporia extensa (Peck) Ginns, Polyporaceae (syn. Poria cocos F.A. Wolf)), Hange tuber (半夏, はんげ; Pinellia ternata (Thunb.) Makino, Araceae), Chinpi peel (陳皮, ちんぴ, Citrus reticulata subsp. Unshiu (Markov) Rivera & et al., Rutaceae), Taisō fruit (大棗, たいそう, jujube; Ziziphus jujuba Mill, Rhamnaceae), Kanzō root (甘草, かんぞう, licorice; Glycyrrhiza uralensis Fisch. Ex DC, G. inflata Batalin, and G. glabra L, Fabaceae), and Shōkyō root (生姜, しょうきょう, ginger; Zingiber officinale Roscoe, Zingiberaceae). Pinellia tuber is an anti-nausea component and citrus unshiu peel is anti-emetic. In this Kampo, Glycyrrhiza is not used to cure a symptom of stomach trouble. The function of Glycyrrhiza in this Kampo is to be an adjustment, harmonizing force, or pivot between another seven herbal medicines based on epistemology. Mechanistically, it, in fact, may be an excipient or nano-izing agent (Iitsuka et al., 2018; Zhou et al., 2019) and/or broad immunostimulant (Iitsuka et al., 2018). Glycyrrhiza, or the root and stolon (runner) of licorice, is used in 72% of the 294 Kampo formulations. Moreover, it is supplied as part of a polypharmacological preparation not as a single component medicine. In terms of delivery modality, Kampo preparations include tablets, encapsulations and polypharmacological teas which will exhibit different pharmacodynamics to preparations seen in the Western nutraceutical market. Thus, when one sees multiple examples of Licorice capsules and Licorice extracts for digestive relief in the U.S nutraceutical market, there is clearly a disconnect between the Asian ‘inspiration’ for the use of licorice and the practicality of its marketing as a nutraceutical. Licorice may, however, have value outside of digestive relief, but with caveats that could only be revealed using detailed scientific analyses: a Cochrane methodology meta-analysis concluded that there were “… positive effects of licorice consumption on the reduction of body weight and BMI of patients. However, the results also show the increase in blood pressure of patients associated with the hypernatremia caused by licorice. Consequently, licorice consumption should be avoided by hypertensive patients ( Luis et al., 2018 ).” Of course, licorice nutraceuticals sold as dietary supplements carry no such warnings.
From penetration to pangolin scales. Pangolin, which is a scaled mammal indigenous to Asia and sub-Saharan Africa is highly trafficked. In traditional Chinese medicine, and similarly in Vietnam, pangolin scales are prescribed for a wide range of mechanistically unconnected disorders loosely unified by the idea of a blockage, these range from female infertility, lactation problems, intestinal discomfort, to blood clots. The epistemological basis for this association is not connected to any potential bioactive constituent of the scales (which are almost entirely medically inert keratin). Rather, the concept of a connection between pangolins and blockages derives from aspects of their structure and function on the animal, especially the fact that they are armored with scales which embody protection and penetration and let them move through dense growth, and that they grub into hidden spaces with long penetrative tongues. The Chinese name for pangolin, chuan shan jia, “penetrating-the-mountain scales” emphasizes this idea and uses ideograms that represent penetration, even of massive obstructions such as mountains. Thus the epistemology of why pangolin scales might be thought to be effective does not translate to modernity, yet the trade persists and is perpetuated by inclusion in both Chinese and Vietnamese official pharmacopeia (Lv et al., 2020).
Post-COVID: implications for management of pre-existing conditions through TM. The metabolic syndrome and its associated conditions (cardiovascular disease, hyperlipidemia, type 2 diabetes, obesity, kidney disease, neuropathy, glaucoma) have been major health burdens in both Western and developing nations in recent decades. These are chronic conditions with long-term implications for morbidity and associated mortality. However, the COVID-19 pandemic has sharpened our focus on these conditions as they are clearly associated with greatly increased risk of short-term mortality from COVID-19 as well.
TM for management of metabolic syndrome disorders . There are management solutions for metabolic syndrome disorders that have successfully translated from TM phytomedical settings to application in Western medicine for control of glycemia and insulin secretion (Allen et al., 2013; Medagama, 2015; Wang et al., 2017). These include allicin (from garlic), cinnemaldehyde and cinnamon catechins (from cinnamon) which are found in many TM formulations. While the etiology of these disorders may not have been historically stated in terms that translate to Western understandings, we see indications such as ‘lethargy, kidney yang deficiency, frequent urination’ in historical prescribing frameworks and in more recent times the linkages to more modern diagnostic criteria. These compounds have made major inroads into nutraceutical use and there is relatively strong evidence for their use in peer-reviewed studies. Interestingly, they seem to be TTTM success stories where their application as isolated compounds in Westernized modalities is quite successful.
Contextualization of potency and modes of action. Where there are some limitations in terms of potency relative to ‘standard of care’ drugs (Leach and Kumar, 2012; Wang et al., 2017; Yeh et al., 2003) it may be important to consider a number of factors, such as: the consequences of abstracting a single compound from a multi-ingredient formula or a suite of therapeutic interventions; weighing the very low side-effect profiles of these GRAS (Generally Regarded as Safe, FDA) phytomedicines against modest therapeutic benefits, which may result in risk/benefit profiles comparable to or better than more potent pharmaceuticals; and the need to identify a mode of action that can then be used in SAR to improve potency.
In the case of allicin and cinnemaldehyde, the TRPA1 ion channel has been documented as a target receptor but, given the prevailing understanding of this channel as a nociceptor, the main interpretation of this ligand-receptor relationship has been in the mechanism of the burning sensation associated with those compounds, However, recent data from our team (AJS, unpublished data) has shown a definitive in vivo proof-of-mechanism for TRPA1 ligands in the lowering of blood sugar. This study shows that TRPA1 knockout mice have chronically decreased blood sugar that this can be replicated by TRPA1 ligands and provides a biochemical mechanism by which this cation channel links to central metabolic pathways via a novel regulatory interaction with creatine kinase. This study provides a mode of action that is foundational for the credibility of these approaches as well as their future optimization.
As relatively low-cost solutions to some of the underlying conditions that are major health burdens and risk factors for COVID-associated mortality, these therapies may be of particular use in economically disadvantaged settings.
6. Lost in translation: epistemological contrasts between TM and western scientific medicine
In addition to the dichotomy between polypharmacy and the Western ‘magic bullet’ or ‘one drug, one active constituent, one receptor’ approach, there are complex epistemological and metaphysical/philosophical distinctions between TM and Western medicine. We can use Chinese TM as an example: Kavoussi (2007) tells us that Chinese TM is “a proto-scientific ( Kuhn, 1970 ) observational system of health observances and practices based on a symptomatological classification of disease using two elementary dynamical-processes pattern categorization schemas: a hierarchical and combinatorial inhibiting–activating model (Yin-Yang), and a non-hierarchical and associative five-parameter semantic network (5-Elements/Agents)”. The fundamental thought-architecture of TCM is a combination of two key dynamical-processes pattern categorization schemas: (1) A metaphysical view of ontogenesis as the product of influence by an inhibiting and an activating force (Yin, Yang). Events (symptoms) that occur are assessed for their impact on the net state between Yin and Yang (Qi) that maps to predicted outcomes and for which there are prescriptive pharmacological and behavioral indications. (2) TCM utilizes a five-element system that identifies essential parameters of health or sickness, places intensity/value judgements on them and documents their linkages, all of which is used to guide prescription. There is a discretization of all possible health or sickness phenomena into five mutually-exclusive variables of Water, Wood, Fire, Earth and Metal. Each variable is further divided into a finite set of states ranging from deficient to excessive, which is the basic diagnostic indicator for treatment. A system of vectors interlinks all variables with ‘‘parental” influences that divide into two healthy, the Generating (Sheng) and the Controlling (Ke), and two unhealthy, the Overacting (Cheng) and the Insulting (Wu), vectors that influence diagnosis and prescription. Layered over this entire framework are spiritual, superstition, and magical dimensions of belief that would influence decision-making and prescribed practice advised by practitioners.
A patient presentation to a Chinese TM practitioner in historical times would therefore have prompted a pattern recognition process by which a series of vector connections would be applied to the matrix to indicate a course of action. An experiential experimental/observation framework would have been applied longitudinally during a practitioner's career and between practitioners laterally and generationally to add another layer of directionality to actions based on apparent efficacy or lack thereof. Historically, these decisions were made without the benefit of structure-function relationships in anatomical, physiological or molecular levels of understanding and the concept of disease causality would have been largely anachronous. So, what does this epistemological contrast mean for TM in a contemporary context?
Practice. Contemporary TM practitioners are more likely to occupy a liminal space where the traditional empirical framework is informed by modern expertise and understandings of anatomy, physiology, disease mechanisms, pharmacology and molecular biology. In China and Japan, there are both traditional pharmacies with a primarily TM mission and worldview, and a type of integration of Western and TM in medical provider settings more usually associated with the former. For example, Kampo-based medicine was integrated into the Japanese health care system in 1961 (Yakubo et al., 2014). Medical doctors in Japan learn Western medicine in medical school but they can also prescribe Kampo-based medication (Watanabe et al., 2014). There is a type of vertical integration of Kampo into Japanese medicine. Kampo medicines for mild symptomatic management (e.g. for headache, allergies, cold and flu) are sold side by side with Western formulations in pharmacies (Nishimura et al., 2009; Watanabe et al., 2011). A physician might prescribe Kampo for symptomatic management of mild disorders with approximately a similar frequency to a Western prescription, but as symptoms increase in severity the focus shifts into a vertical progression through more advanced diagnostic tools (e.g. imaging, blood tests, molecular diagnostics), interventions, and therapies (Katayama et al., 2013; Melby et al., 2019). This type of deployment of Kampo by medical providers appears reconciled with their Westernized, Hippocratic (‘do no harm’) training and ethos based on four principles: (i) historical and traditional understandings of efficacy and applications, (ii) a burgeoning peer-reviewed scientific literature that has tested, validated and provided plausible mechanisms of action for many TCM and Kampo formulations, (iii) historical and contemporary understandings of low side effect profiles and (iv) the compartmentalization of these therapies into symptomatic management and the avoidance of a false sense of equivalency with the type of intervention needed for major disorders. It is worth noting that (ii) has been facilitated by the lack of barriers to this type of validation that we see in TCM, Kampo, and, to some extent Ayurveda, in contrast with many indigenous medical systems. In the former contexts there has been the development, in country, of a major biomedical research infrastructure and there seem to be few barriers to validation of these therapeutic approaches using modern biomedical and paradigms and methodologies. In contrast, for indigenous medical systems developed in areas such as the Pacific and Oceania, by American First Nations and other oppressed and colonized peoples, this type of ‘validation’ is viewed as neo-colonial, imperialistic and often as a route to further exploitation of traditional knowledge and wisdom (Mark et al., 2019). Absent a parallel effort placing intellectual property, inclusion in the scientific endeavor, and control over the research process into the hands of indigenous peoples, it seems likely that these this barriers will persist with the parallel effects of: (i) not bringing potentially important indigenously-derived medicines or their therapeutically active components into the medical mainstream, and (ii) increasing the likelihood of cultural appropriation and inappropriate abstraction/translation of indigenous medicine by the nutraceutical industry.
Translation. The epistemological framework for TM prescribing (for example for TCM and Kampo) and development of indication-prescription relationships uses a set of assumptions and anachronistic knowledge that would seem to have no utility or translatability to modern medicine. However, the empirical evidence basis for efficacy of a formulation deriving from potentially hundreds of years of observation-iteration cycles is not easily dismissed, and indeed there is burgeoning validation from peer-reviewed studies using controlled methodologies that many of these formulations indeed contain components that have been independently identified by Western medicine as therapeutically active and mechanistically plausible (e.g., artemisinin, cinnemaldehyde, salicylate, capsaicin, others) (Baranidharan et al., 2013; Namazi et al., 2019; Sunshine et al., 2000). The epistemological challenge comes when trying to draw a line between a decision to prescribe made using an ancient or historical worldview and then extrapolating that to a decision to formulate a nutraceutical. Just because a component is in a formulation indicated for ‘stomach issues” there may not have been the diagnostic granularity to differentiate say, between food poisoning or an ulcer, and a particular component may have had a primarily excipient or unrelated quasi-beneficial role (e.g. the inclusion of Xiancao or ginseng in many TCM formulations as an aid to immortality, or at least general vitality). Translation and inclusion of components to nutraceuticals based on this type of correlative performance expectation and bootstrapping across cultures, geographies and time is at best overly optimistic, and may be disingenuous, misleading and harmful. This is particularly concerning when claims become expansive and create false equivalencies as part of this bootstrapping process.
7. Resolution: viable implementation models and research imperatives for integrative therapeutic approaches
Integrative implementation models. Relegation of all non-Western medicines to the unregulated nutraceutical industry is unsafe and an abdication of ethical responsibility. It also potentially risks missing therapeutic opportunities. When we review integration of Kampo in Japanese healthcare and TCM in China (Teng et al., 2016), it is clear that benefits occur at levels from the individual provider to the system. The defining driver is the inclusion of Kampo or TCM into the national pharmacopeia, which links to coverage by the national insurance system and payment models. This creates a need for training and licensure and for these approaches to be covered in allopathic medical school curricula, where there will be a parallel emphasis on critical thinking and evidence-based practice. There is vertical integration of TM and allopathic approaches across rural and urban provider settings as well as across age and socioeconomic demographics, at least partly avoiding the idea that these are ‘barefoot medicine’ approaches to be foisted on the rural poor. The TM solutions are positioned within the vertical progression of treatment firmly (Arai et al., 2014) at the level of symptomatic management, and are not touted as cures. The pursuit of an evidence base for components of TM is an important aspiration and is a driver for the ‘Western disease’ based prescription approach that matches components, via a model of plausible efficacy, with symptoms, without requiring fidelity to the historical/traditional epistemologies of prescribing patterns. In this sense the TM formulations simply become a very large library of potential bioactive components that can be prescribed according to modern medical paradigms and in which polypharmacy can be preserved to varying degrees or not at all. Innovative approaches such as the development of a statistical decision support system (Yoshino et al., 2016) for the opposite paradigm (making the traditional pattern diagnosis accessible to contemporary physicians with little Kampo training) are also being developed. While this leaves aside questions of efficacy, it is a move towards standardization that will allow for later comparative study.
Research imperatives. Scientific training and research institutions, scientific journals and funding agencies should leverage their ability to influence the field towards well-designed studies that are unbiased, prioritize comparison with placebos, are statistically rigorous, and do not legitimize the employment of components from threatened species or those that are potential zoonotic reservoirs. Scientists and publishers bear responsibility for the publication of studies that perpetuate pseudo-scientific tropes, are self-reinforcing, and do not triangulate or layer evidence. The application of modified Bradford-Hill, or other similar schema could be adopted as a required or recommended component of a publication that seeks to evidence efficacy for a TM approach. The language bias of systematic reviews towards English language publications needs to be addressed, as it may be either hiding in-country proofs of efficacy or, perhaps more likely, missing an opportunity to call out poor quality studies regardless of their language origin.
Data analytics and prediction. Data science has the potential to transform understanding and evaluation of TM. Here, we discuss two examples and present one case study of the utility of data analytics in TM.
First, the application of DNA barcoding to TM offers opportunities for maintaining fidelity of supply chains, detecting adulteration, detecting the use of threatened or zoonotic reservoir animal components, and monitoring the consistency of formulations (Chen et al., 2014, 2017; Pedales et al., 2016). Misformulation, which can arise both from cynical inclusion of ingredients, to genuine misidentification of hard-to distinguish plant materials, can cause poisoning, allergic reactions and liver toxicity. In this context, DNA barcoding of the entire materia medica has the potential to improve safety and efficacy.
Second, the value of unbiased computational studies that link components to mechanisms based on the explosion of understanding in chemical biology should be a priority for the field as a potential foundation on which further layers of rational study can be built. Computational studies are relatively resource-friendly and have significant predictive power that can then be used to focus and rationally design the more cost-, labor- and time-intensive pre-clinical and clinical studies. There are several examples of open-access computational pipelines to deconvolution of TM, suggestions of plausible mechanisms and hypothesis generation for subsequent testing. KAMPO-DB (Sawada et al., 2018) and BATMAN-TCM (bioinformatics analysis tool for molecular mechanism of Traditional Chinese Medicine (Liu, Z. et al., 2016b)) and others are (Tao et al., 2018) annotative and relational. They are linked databases with user interfaces and various output choices that generate lists of components based on constituent analysis of target proteins, biological pathways, gene ontologies, target genes and multi-omic databases. Kampo-DB, in particular, is an advance because it incorporates a molecular modeling process where targets are predicted through application of AI and machine learning to docking simulations, which has also been applied by other groups (Tao et al., 2018). BATMAN-TCM was initially published in a study where its predictions for efficacy and application of a TCM in a cardioprotectant were then experimentally validated. Such databases have the potential to accelerate mechanisms and mode of actions, link therapies to new potential target applications, and rapidly accelerate the validation (and exclusion) of TM. Integration with toxicological and drug iteration databases would seem to be a necessary next step for the annotative and relational approaches (Ikegami et al., 2004). We note also the recent publication of an analytics study of plant representation in African medicine, which highlights the sophistication of African ethnopharmacology (Van Wyk, 2020), which couple with metabolomic studies suggests eventual development of similar computational pipelines will be possible for these medical systems (Anokwuru et al., 2020).
Third, new data science pipelines (HT, AJS, unpublished) are being developed that provide an additional layer of analysis from relational and mode-of-action prediction approaches used in prior network pharmacology (Zhang et al., 2019). We developed a process called In silico Convergence Analysis (ISCA) which looks at an indication (e.g. pain, hyperglycemia) across TM systems from multiple cultures and seeks to identify compound-level commonalities in the solution sets that different cultures have arrived at through empirical/historical experimentation. We envision that these analyses will eventually develop a transcultural virtual ‘meta-pharmacopeia’. We propose that validation of this approach could lead to three potential benefits to the field: (1) Using convergence in formulation composition between TM systems to make connections between components and targets that provide new insights into modes and mechanisms of action. (2) Predicting minimal and/or essential compound sets that reflect consensus understandings of efficacy across TMS and can be used to formulate new therapeutic mixtures for subsequent pre-clinical and clinical testing in particular indications. (3) Providing compositional benchmarks and reality-checks for evaluation of claimed fidelity to TM in nutraceutical formulations.
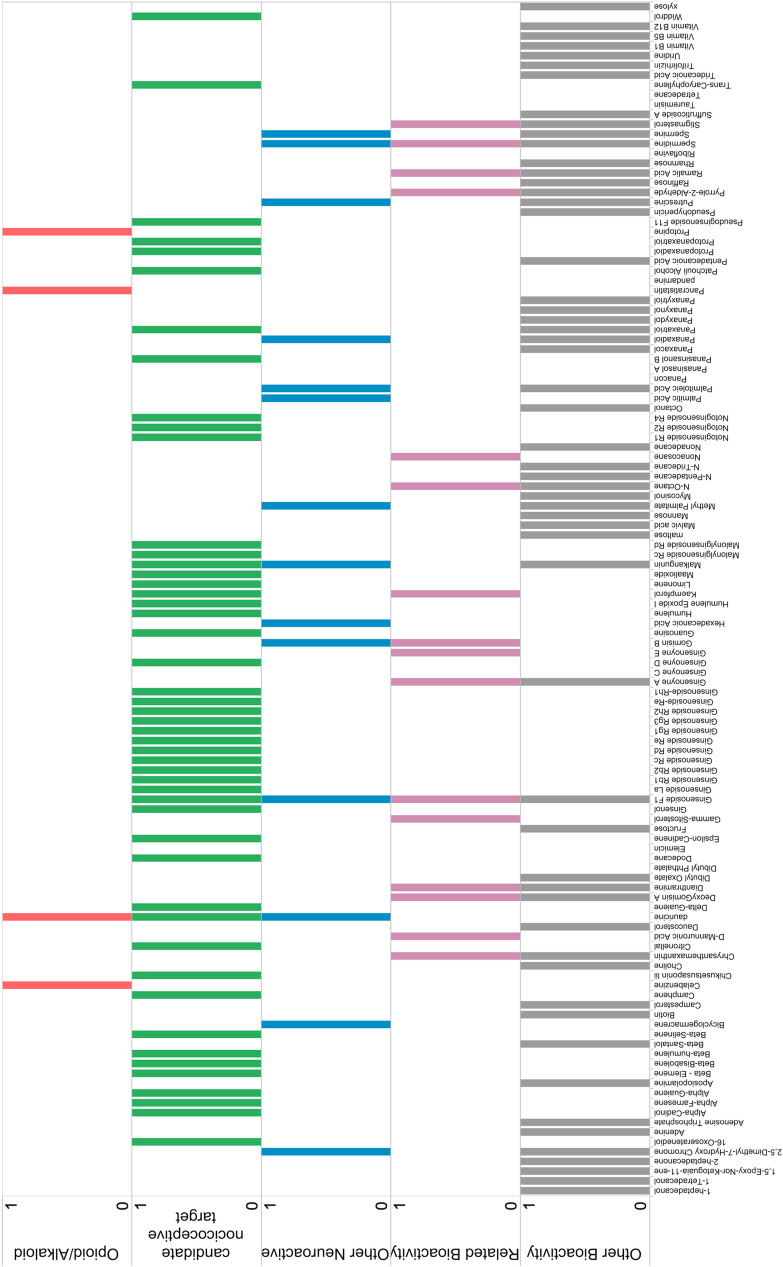
In our first set of studies (unpublished and in Jansen et al. (2019)), we evaluated pain and hyperglycemia. As an example, our ISCA approach to pain is shown in Fig. 1, Fig. 2 and described below. We started with formulations derived from TCM and Kampo approaches to pain that had been validated in controlled studies (2 Kampo and 2 TCM formulations; Goshajinkigan, Gohsuyuto, Xie Xin Tang, Si Mo Tang (Cook and Emken, 1990; Hamaguchi et al., 2017; Liu, T. et al., 2016a; Odaguchi et al., 2006)). Formulation component lists (~800–2000 components) were generated using databases such as BATMAN-TCM and KAMPO-DB and were triaged for obviously non-bioactive components (leading to lists of ~200–400 compounds). For pain we identified a convergent set of compounds that were represented in 2 (one Kampo, one TCM) or all 4 proposed analgesic formulations. In one of the pairwise comparisons, 121 compounds were shared between the 2 (one Kampo and one TCM) formulations. These were then re-categorised (Fig. 2) using literature analysis into opioid/alkaloid candidate analgesics (alkaloids related to known opioid receptor ligands or ion channel ligands, 4 convergent compounds) (Bienz et al., 2002; Kai et al., 1998; National Center for Biotechnology Information; Nichols and Lee, 2018; Qi et al., 2019; Saeed et al., 1997; Song et al., 2000; Xu et al., 2005; Zhong et al., 1995), potential ligands for nociceptive ion channels (terpenes, 49 convergent compounds), components with other demonstrated neuroactivity (15 convergent compounds), components with bioactivity indirectly related to pain (anti-inflammatory, anti-oxidants, 16 convergent compounds) and compounds with other types of bioactivity but no obvious link to analgesia (56 convergent compounds) (Antwi et al., 2018; Bommareddy et al., 2019; Crupi and Cuzzocrea, 2017; Devi et al., 2015; Do et al., 2019; Henry and Maisch, 1890; Herout and Sykora, 1958; Huang et al., 2015; Hui et al., 2015; Kimura et al., 2001; Ko et al., 2017; Kumar and Muller, 2000; Kwon et al., 2018; Le et al., 2018; Li et al., 2009; Madeo et al., 2018; National Center for Biotechnology Information; Ng et al., 2008; Qian, 2002; Shim et al., 2018; Wang et al., 2019; Ye et al., 2018; Zeisel, 1981). These data are summarized in Fig. 1. Finally, we identified divergent compounds that were non-overlapping between different cultural solutions to the indication of pain (Sun and Yang, 2019), which may mean they are low priority for further study or that there are yet unknown relationships that render them interesting.
Fig. 1.
In silico convergence analysis (ISCA) of TCM and Kampo pain formulations.In silico Convergence Analysis (ISCA) examines an indication (e.g. pain) across TM systems from multiple cultures and seeks to identify compound-level commonalities in the formulations that different cultures have arrived at through empirical/historical experimentation. Two Kampo and two TCM formulations indicated for pain were assessed using ISCA. Formulation component lists (~800–2000 components) were generated using databases such as BATMAN-TCM and KAMPO-DB and triaged for obviously non-bioactive components (leading to lists of ~200–400 compounds). We identified a convergent set of compounds that were represented in 2 (one Kampo, one TCM) or all 4 proposed analgesic formulations. In one of the pairwise comparisons, 121 compounds were shared between the 2 (one Kampo and one TMC) formulations. These were then re-categorised using literature analysis into opioid/alkaloid candidate analgesics (alkaloids related to known opioid receptor ligands, 4 convergent compounds red bars), potential ligands for nociceptive ion channels (terpenes, 49 convergent compounds, green bars), components with other demonstrated neuroactivity (15 convergent compounds, blue bars), components with bioactivity indirectly related to pain (anti-inflammatory, anti-oxidants, 16 convergent compounds, purple bars) and compounds with other types of bioactivity but no obvious link to analgesia (56 convergent compounds grey bars). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
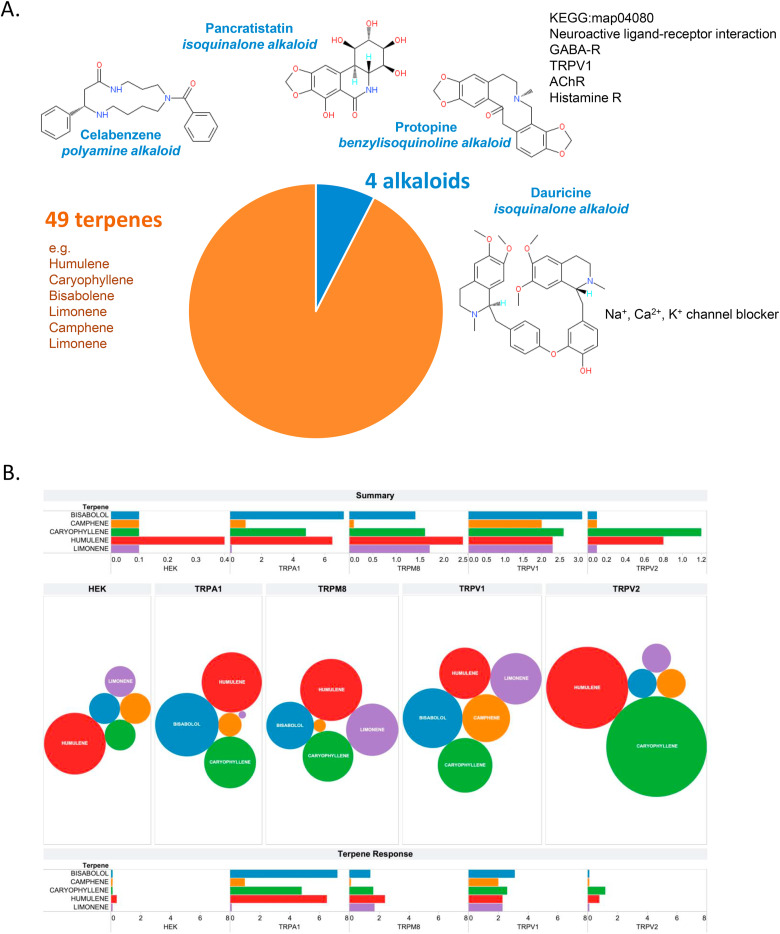
Convergent compounds identified through ISCA of Kampo and TCM formulations for pain. A. Summary of convergent compounds represented in both Kampo and TCM formulations. These include terpenes (orange sector) and alkaloids (blue sector), with specific compounds illustrated. B. Terpenes found in the ISCA include effective ligands and potential agonists-desensitizers for nociceptive TRP channels. HEK cells inducibly expressing the indicated ion channels were loaded with Fluo-4 acetoxymethyl ester in a modified Ringer solution containing 1 mM CaCl2 Cells were stimulated with vehicle or the indicated terpene at a concentration of 1 μM, or matched vehicle, and time-resolved fluorescence measurements were collected in a Molecular Devices Flexstation 3. The peak attained increases in relative fluorescence units (RFU) were calculated, vehicle subtracted and plotted. Comparison plots show the relative intensity of the intracellular free calcium mobilization initiated by each terpene (with the diameter of each circle representing the peak intensity, upper panel, and as histograms, lower panel). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
We, and others, have previously shown that agonist ligands for the nociceptive TRPV ion channels can act as analgesics through agonist-mediated chronic desensitization of the channel. This has been demonstrated for example using the archetypal TRPV1 ligand capsaicin as a pain therapy and we have demonstrated it for cannabinoid and terpene ligands for TRPV1 (Backonja et al., 2010; De Caro et al., 2019; Jansen et al., 2019; Starkus et al., 2019; Talavera et al., 2020). Nocioceptive TRPs have an extensive pharmacopeia of plant secondary metabolites (Baj et al., 2019). Thus, agonist ligands for TRPVs that are found in plant secondary metabolomes can act as analgesics. We asked if TRPV1 ligands were present in the convergent compound set identified by ISCA. We find the potential for TRPV agonists-desensitizers in both the alkaloids (e.g. celabenzene is a polyamine and related compounds are potent TRPV1 ligands (Ahern et al., 2006); Protopine is a component of extracts implicated in TRPV1 regulation) (Haustedt et al., 2014) and terpenes (Jansen et al., 2019; Oz et al., 2015; Rodrigues et al., 2016) identified in the convergent compound list. Notably in the divergent list there is significant representation of gingerols and related compounds (Kamatou et al., 2012), which are TRPV1 ligands and may therefore have the capacity to agonize/desensitize these nociceptive channels. The inclusion of these compounds seems specific to the analgesic solution set arrived at by TCM, but not Kampo, for these particular formulations.
Fig. 2 summarizes this ISCA case study for pain. Fig. 2A presents a summary of the convergent compounds identified. Our interpretation of these data is that the formulation is polypharmaceutical, with stacking and overlapping of multiple compounds of likely moderate efficacy rather than one high efficacy compound that would be more reflective of the Western paradigm. It contains multiple relatively low specific activity ligands that may possibly be agonist-desensitizers for TRP channels (Fig. 2B and C) (Jansen et al., 2019; Starkus et al., 2019), and a few probably higher potency (but still weak relative to opioids used in Western medicine) alkaloids (Fig. 2B). There are also anti-inflammatory and antioxidants in the formulations that have the potential to contribute to reducing tissue inflammation, decreasing pain sensation and accelerating healing. Outside the realm of direct receptor-ligand interactions, both convergent and divergent compound sets contain possible excipients and delivery-enhancing agents such as saponins. Viewed through a Chinese/Japanese epistemology, the data in Fig. 2 would seem to reflect the TCM/Kampo concept of JUN-CHEN-ZUO-SHI (‘Monarch, Minister, Assistant and Envoy’) (Huang et al., 2017; Lin and Li, 2009; Zhao et al., 2015) medicine assembly from compounds that fall into the categories of denominator (a drug that directly targets the pathological factor related to a disease), an assistant/enhancer (that enhances the effect of the denominator) or corrector/addresser (that limits adverse effects), and a messenger (delivery, excipient component).
Our convergent compound set found further overlap and potential validation when we compared it with published studies: For example, ginsenosides, sitosterol and arachidonic acid metabolites converge between our study (Sun and Yang, 2019) and that of Sun and Yang (Fufang Danshen formulation). A study by Zheng et al. (2020) of endometriosis pain formulations overlapped with our in numerous terpenes, gingerols, and sitosterol). Huang et al. (2017) studied dysmenorrheal pain (Xuangui formulation) and identified gingerols, terpenes, and arachidonic acid metabolites that overlap with our findings. Sun and Yang identified dauricine, sitosterol and a number of other compounds overlapping with our list in their network pharmacology analysis for pain (Sun and Yang, 2019). These data demonstrate that ICSA had the potential to identify active, multi-agent, compound mixtures with plausible mechanisms of action/molecular targets, that are now candidates for further study as analgesics in laboratory and clinic.
8. Summary
At best, integration of TM with Western medicine offers democratized, cheaper, accessible and effective symptomatic management. At worst it widens health gaps, peddles pseudoscience and condemns the poor to ineffective care. Evidence is the only viable currency in this debate, and the regulatory abdication of placing these therapies into the nutraceutical market in the U.S. means that we need to look primarily to TM host cultures for the needed evidence-based research. Computational methodologies hold great promise for rapid assessment of mechanistically plausible bioactive components as well as the identification of unrecognized or interacting components of the polypharmaceutical formulations. The unregulated translation of TM into Western nutraceuticals is a highly permissive step for unfounded claims of efficacy, simplification, and reformulation that would likely destroy any efficacy if it existed, and the creation of false equivalence with Western medicine that will harm health outcomes if relied upon by consumers. The moral, regulatory, and scientific space in which nutraceuticals exploit and Western science under-studies these TM needs to be re-evaluated.
Author contributions
Experiments and data analysis: LMN, AJB, LA, MS, JA; Experimental design and interpretation: HT, CNA, AJS, EK; Conception and writing of paper: HT, CJ, EK, AJS, JB, CNA.
Acknowledgements
We thank the reviewers of this manuscript for their guidance and specific contributions of ideas and suggested citations. This work was funded or otherwise supported by: The Howard Hughes Medical Institute ‘Inclusive Excellence’ program grant #52008701 (HT) culture-based research seed program (to JDB); GB Sciences Research Award (to HT); NIH COBRE P20GM113134 (AJS); NIH R15DK00978 (HT); NSF AISL #1811691 (HT); NSF INCLUDES #1744526 (HT). We thank Ms. Cai Yan Fan for valuable insights on JUN-CHEN-ZUO-SHI.
References
- Abdullahi A.A. Trends and challenges of traditional medicine in Africa. Afr. J. Tradit., Complementary Altern. Med. 2011;8(5 Suppl. l):115–123. doi: 10.4314/ajtcam.v8i5S.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adekson M.O. Similarities and differences between Yoruba traditional healers (YTH) and native American and Canadian healers (NACH) J. Relig. Health. 2016;55(5):1717–1728. doi: 10.1007/s10943-016-0251-6. [DOI] [PubMed] [Google Scholar]
- Ahern G.P., Wang X., Miyares R.L. Polyamines are potent ligands for the capsaicin receptor TRPV1. J. Biol. Chem. 2006;281(13):8991–8995. doi: 10.1074/jbc.M513429200. [DOI] [PubMed] [Google Scholar]
- Allen R.W., Schwartzman E., Baker W.L., Coleman C.I., Phung O.J. Cinnamon use in type 2 diabetes: an updated systematic review and meta-analysis. Ann. Fam. Med. 2013;11(5):452–459. doi: 10.1370/afm.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anokwuru C.P., Tankeu S., van Vuuren S., Viljoen A., Ramaite I.D.I., Taglialatela-Scafati O., Combrinck S. Unravelling the antibacterial activity of Terminalia sericea root bark through a metabolomic approach. Molecules. 2020;25(16):3683. doi: 10.3390/molecules25163683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antwi A.O., Obiri D.D., Osafo N., Essel L.B., Forkuo A.D., Atobiga C. BioMed Res. Int. 2018;2018 doi: 10.1155/2018/3984068. Article ID 3984068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arai Y.C., Yasui H., Isai H., Kawai T., Nishihara M., Sato J., Ikemoto T., Inoue S., Ushida T. The review of innovative integration of Kampo medicine and Western medicine as personalized medicine at the first multidisciplinary pain center in Japan. EPMA J. 2014;5(1):10. doi: 10.1186/1878-5085-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arita R., Yoshino T., Hotta Y., Miyamoto Y., Osawa I., Takemoto O., Watanabe K. National cost estimation of maoto, a Kampo medicine, compared with oseltamivir for the treatment of influenza in Japan. Traditional & Kampo Medicine. 2016;3(1):59–62. [Google Scholar]
- Backonja M.M., Malan T.P., Vanhove G.F., Tobias J.K., Group C.S. NGX-4010, a high-concentration capsaicin patch, for the treatment of postherpetic neuralgia: a randomized, double-blind, controlled study with an open-label extension. Pain Med. 2010;11(4):600–608. doi: 10.1111/j.1526-4637.2009.00793.x. [DOI] [PubMed] [Google Scholar]
- Baj A., Bistoletti M., Bosi A., Moro E., Giaroni C., Crema F. Marine toxins and nociception: potential therapeutic use in the treatment of visceral pain associated with gastrointestinal disorders. Toxins. 2019;11(8):449–486. doi: 10.3390/toxins11080449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baranidharan G., Das S., Bhaskar A. A review of the high-concentration capsaicin patch and experience in its use in the management of neuropathic pain. Ther Adv Neurol Disord. 2013;6(5):287–297. doi: 10.1177/1756285613496862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bienz S., Detterbeck R., Ensch C., Guggisberg A., Hausermann U., Meisterhans C., Wendt B., Werner C., Hesse M. Putrescine, spermidine, spermine, and related polyamine alkaloids. Alkaloids - Chem. Biol. 2002;58:83–338. doi: 10.1016/s0099-9598(02)58003-2. [DOI] [PubMed] [Google Scholar]
- Bommareddy A., Brozena S., Steigerwalt J., Landis T., Hughes S., Mabry E., Knopp A., VanWert A.L., Dwivedi C. Medicinal properties of alpha-santalol, a naturally occurring constituent of sandalwood oil: review. Nat. Prod. Res. 2019;33(4):527–543. doi: 10.1080/14786419.2017.1399387. [DOI] [PubMed] [Google Scholar]
- Briesacher B.A., Gurwitz J.H., Soumerai S.B. Patients at-risk for cost-related medication nonadherence: a review of the literature. J. Gen. Intern. Med. 2007;22(6):864–871. doi: 10.1007/s11606-007-0180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browner C.H., Bernard R.O.d.M., Rubel A.J., Benoist J., Cerroni-Long E.L., Charzewska J., Colby B.N., Garro L.C., Gonzalez N.L., Good B., Hall R.L., Janzen J.M., Kleinman A., Pollak-Eltz A. A methodology for cross-cultural ethnomedical research [and comments and reply] Curr. Anthropol. 1988;29(5):681–702. [Google Scholar]
- Celentano A., Tran A., Testa C., Thayanantha K., Tan-Orders W., Tan S., Syamal M., McCullough M.J., Yap T. The protective effects of Kava (Piper Methysticum) constituents in cancers: a systematic review. J. Oral Pathol. Med. 2019;48(7):510–529. doi: 10.1111/jop.12900. [DOI] [PubMed] [Google Scholar]
- Chen S., Pang X., Song J., Shi L., Yao H., Han J., Leon C. A renaissance in herbal medicine identification: from morphology to DNA. Biotechnol. Adv. 2014;32(7):1237–1244. doi: 10.1016/j.biotechadv.2014.07.004. [DOI] [PubMed] [Google Scholar]
- Chen X., Xiang L., Shi L., Li G., Yao H., Han J., Lin Y., Song J., Chen S. Identification of crude drugs in the Japanese pharmacopoeia using a DNA barcoding system. Sci. Rep. 2017;7:42325. doi: 10.1038/srep42325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chitindingu E., George G., Gow J. A review of the integration of traditional, complementary and alternative medicine into the curriculum of South African medical schools. BMC Med. Educ. 2014;14:40. doi: 10.1186/1472-6920-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook H.W., Emken E.A. Geometric and positional fatty acid isomers interact differently with desaturation and elongation of linoleic and linolenic acids in cultured glioma cells. Biochem. Cell. Biol. 1990;68(3):653–660. doi: 10.1139/o90-094. [DOI] [PubMed] [Google Scholar]
- Cragg G.M., Newman D.J. Plants as a source of anti-cancer agents. J. Ethnopharmacol. 2005;100(1–2):72–79. doi: 10.1016/j.jep.2005.05.011. [DOI] [PubMed] [Google Scholar]
- Crupi R., Cuzzocrea S. Springer; Singapore: 2017. Alginates and Their Biomedical Applications. [Google Scholar]
- Cyranoski D. Mystery deepens over animal source of coronavirus. Nature. 2020;579(7797):18–19. doi: 10.1038/d41586-020-00548-w. [DOI] [PubMed] [Google Scholar]
- De Caro C., Cristiano C., Avagliano C., Bertamino A., Ostacolo C., Campiglia P., Gomez-Monterrey I., La Rana G., Gualillo O., Calignano A., Russo R. Characterization of new TRPM8 modulators in pain perception. Int. J. Mol. Sci. 2019;20(22):5544–5558. doi: 10.3390/ijms20225544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devi K.P., Malar D.S., Nabavi S.F., Sureda A., Xiao J., Nabavi S.M., Daglia M. Kaempferol and inflammation: from chemistry to medicine. Pharmacol. Res. 2015;99:1–10. doi: 10.1016/j.phrs.2015.05.002. [DOI] [PubMed] [Google Scholar]
- Do T.Q., Truong B.N., Mai H.D.T., Nguyen T.L., Nguyen V.H., Nguyen H.D., Nguyen T.D., Nguyen T.C., Luong T.V., Giang L.T., Chau V.M., Pham V.C. New dianthramide and cinnamic ester glucosides from the roots of Aconitum carmichaelii. J. Asian Nat. Prod. Res. 2019;21(6):507–515. doi: 10.1080/10286020.2018.1454436. [DOI] [PubMed] [Google Scholar]
- Einbond L.S., Negrin A., Kulakowski D.M., Wu H.A., Antonetti V., Jalees F., Law W., Roller M., Redenti S., Kennelly E.J., Balick M.J. Traditional preparations of kava (Piper methysticum) inhibit the growth of human colon cancer cells in vitro. Phytomedicine. 2017;24:1–13. doi: 10.1016/j.phymed.2016.11.002. [DOI] [PubMed] [Google Scholar]
- Etkin N. University of Arizona Press; Tucson: 2006. Edible Medicines. [Google Scholar]
- Etkin N.L. Cultural constructions of efficacy. In: van der Geest S., Whyte S.R., editors. The Context of Medicines in Developing Countries: Studies in Pharmaceutical Anthropology. Springer Netherlands; Dordrecht: 1988. pp. 299–326. [Google Scholar]
- Etkin N.L., Baker J.D., Busch J.N. Cultural factors influencing therapeutic practice. In: Heggenhougen H.K., editor. International Encyclopedia of Public Health. Academic Press; Oxford: 2008. pp. 56–59. [Google Scholar]
- Etkin N.L., Elisabetsky E. Seeking a transdisciplinary and culturally germane science: the future of ethnopharmacology. J. Ethnopharmacol. 2005;100(1–2):23–26. doi: 10.1016/j.jep.2005.05.025. [DOI] [PubMed] [Google Scholar]
- Ewen M., Zweekhorst M., Regeer B., Laing R. Baseline assessment of WHO's target for both availability and affordability of essential medicines to treat non-communicable diseases. PloS One. 2017;12(2) doi: 10.1371/journal.pone.0171284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farquhar J. first ed. Routledge; New York: 1994. Knowing Practice: the Clinical Encounter of Chinese Medicine. [Google Scholar]
- Geers A.L., Brinol P., Vogel E.A., Aspiras O., Caplandies F.C., Petty R.E. The application of persuasion theory to placebo effects. Int. Rev. Neurobiol. 2018;138:113–136. doi: 10.1016/bs.irn.2018.01.004. [DOI] [PubMed] [Google Scholar]
- Hamaguchi T., Yoshino T., Horiba Y., Watanabe K. Goshajinkigan for low back pain: an observational study. J. Alternative Compl. Med. 2017;23(3):208–213. doi: 10.1089/acm.2016.0276. [DOI] [PubMed] [Google Scholar]
- Haustedt, L., Siems, K., Kluge, G., Krohn, M., Kleber, A., 2014. Plant Extracts for Modulating TRPV1 Function. European Patent Application EP2700431A1.
- Hebron M. Humors in renaissance philosophy. In: Sgarbi M., editor. Encyclopedia of Renaissance Philosophy. Springer International Publishing; 2017. pp. 1–3. [Google Scholar]
- Henry C., Maisch C. Chemical notes. American Journal of Pharmacy and the Sciences. 1890:338–341. [Google Scholar]
- Herout V., Sykora V. The chemistry of cadinenes and cadinols. Tetrahedron. 1958;4(3–4):246–255. [Google Scholar]
- Horden P. What's wrong with early medieval medicine? Soc. Hist. Med. 2009;24(1):5–25. [Google Scholar]
- Hsu E. 2018. Traditional Chinese Medicine: its Philosophy, History, and Practice, the International Encyclopedia of Anthropology; pp. 1–10. [Google Scholar]
- Huang A.C., Sefton M.A., Sumby C.J., Tiekink E.R., Taylor D.K. Mechanistic studies on the autoxidation of alpha-guaiene: structural diversity of the sesquiterpenoid downstream products. J. Nat. Prod. 2015;78(1):131–145. doi: 10.1021/np500819f. [DOI] [PubMed] [Google Scholar]
- Huang J., Li L., Cheung F., Wang N., Li Y., Fan Z., Yin F., Yang J., Gao R., He Y., Feng Y. Network pharmacology-based approach to investigate the analgesic efficacy and molecular targets of xuangui dropping pill for treating primary dysmenorrhea. Evid Based Complement Alternat Med. 2017;2017:7525179. doi: 10.1155/2017/7525179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui L.M., Zhao G.D., Zhao J.J. delta-Cadinene inhibits the growth of ovarian cancer cells via caspase-dependent apoptosis and cell cycle arrest. Int. J. Clin. Exp. Pathol. 2015;8(6):6046–6056. [PMC free article] [PubMed] [Google Scholar]
- Iitsuka H., Koizumi K., Inujima A., Suzaki M., Mizuno Y., Takeshita Y., Eto T., Otsuka Y., Shimada R., Liu M., Ikeda K., Nakano M., Suzuki R., Maruyama K., Zhou Y., Sakurai H., Shibahara N. Discovery of a sugar-based nanoparticle universally existing in boiling herbal water extracts and their immunostimulant effect. Biochem Biophys Rep. 2018;16:62–68. doi: 10.1016/j.bbrep.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami F., Fujii Y., Satoh T. Toxicological considerations of Kampo medicines in clinical use. Toxicology. 2004;198(1–3):221–228. doi: 10.1016/j.tox.2004.01.029. [DOI] [PubMed] [Google Scholar]
- Inoue M., Hayashi S., Craker L.E. IntechOpen; 2017. Culture, History and Applications of Medicinal and Aromatic Plants in Japan, Aromatic and Medicinal Plants - Back to Nature. Hany A. El-Shemy. [DOI] [Google Scholar]
- Isaac G., Finn S., Joe J.R., Hoover E., Gone J.P., Lefthand-Begay C., Hill S. Native American perspectives on health and traditional ecological knowledge. Environ. Health Perspect. 2018;126(12):125002. doi: 10.1289/EHP1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen C., Shimoda L.M.N., Kawakami J.K., Ang L., Bacani A.J., Baker J.D., Badowski C., Speck M., Stokes A.J., Small-Howard A.L., Turner H. Myrcene and terpene regulation of TRPV1. Channels. 2019;13(1):344–366. doi: 10.1080/19336950.2019.1654347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji X., Peng Q., Yuan Y., Liu F., Wang M. Extraction and physicochemical properties of polysaccharides from Ziziphus Jujuba cv. Muzao by ultrasound-assisted aqueous two-phase extraction. Int. J. Biol. Macromol. 2018;108:541–549. doi: 10.1016/j.ijbiomac.2017.12.042. [DOI] [PubMed] [Google Scholar]
- Kai L., Wang Z.F., Xiao J.S. L-type calcium channel blockade mechanisms of panaxadiol saponins against anoxic damage of cerebral cortical neurons isolated from rats. Zhongguo Yaoli Xuebao. 1998;19(5):455–458. [PubMed] [Google Scholar]
- Kamatou G.P., Vermaak I., Viljoen A.M. Eugenol--from the remote Maluku Islands to the international marketplace: a review of a remarkable and versatile molecule. Molecules. 2012;17(6):6953–6981. doi: 10.3390/molecules17066953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaptchuk T.J. The placebo effect in alternative medicine: can the performance of a healing ritual have clinical significance? Ann. Intern. Med. 2002;136(11):817–825. doi: 10.7326/0003-4819-136-11-200206040-00011. [DOI] [PubMed] [Google Scholar]
- Katayama K., Yoshino T., Munakata K., Yamaguchi R., Imoto S., Miyano S., Watanabe K. Prescription of kampo drugs in the Japanese health care insurance program. Evid Based Complement Alternat Med. 2013;2013:576973. doi: 10.1155/2013/576973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavoussi B. Chinese medicine: a cognitive and epistemological review. Evid Based Complement Alternat Med. 2007;4(3):293–298. doi: 10.1093/ecam/nem005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura T., Ho I.K., Yamamoto I. Uridine receptor: discovery and its involvement in sleep mechanism. Sleep. 2001;24(3):251–260. doi: 10.1093/sleep/24.3.251. [DOI] [PubMed] [Google Scholar]
- Ko E.Y., Cho S.H., Kang K., Kim G., Lee J.H., Jeon Y.J., Kim D., Ahn G., Kim K.N. Anti-inflammatory activity of hydrosols from Tetragonia tetragonoides in LPS-induced RAW 264.7 cells. EXCLI J. 2017;16:521–530. doi: 10.17179/excli2017-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuchta K., Schmidt M., Nahrstedt A. German kava ban lifted by court: the alleged hepatotoxicity of kava (piper methysticum) as a case of ill-defined herbal drug identity, lacking quality control, and misguided regulatory politics. Planta Med. 2015;81(18):1647–1653. doi: 10.1055/s-0035-1558295. [DOI] [PubMed] [Google Scholar]
- Kuhn T.S. Cambridge University Press; London: 1970. Criticism and the Growth of Knowledge. [Google Scholar]
- Kumar K.S., Muller K. Depsides as non-redox inhibitors of leukotriene B(4) biosynthesis and HaCaT cell growth, 2. Novel analogues of obtusatic acid. Eur. J. Med. Chem. 2000;35(4):405–411. doi: 10.1016/s0223-5234(00)00132-x. [DOI] [PubMed] [Google Scholar]
- Kwon H.J., Lee H., Choi G.E., Kwon S.J., Song A.Y., Kim S.J., Choi W.S., Hwang S.H., Kim S.C., Kim H.S. Ginsenoside F1 promotes cytotoxic activity of NK cells via insulin-like growth factor-1-dependent mechanism. Front. Immunol. 2018;9:2785. doi: 10.3389/fimmu.2018.02785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le H.T., Nguyen H.T., Min H.Y., Hyun S.Y., Kwon S., Lee Y., Le T.H.V., Lee J., Park J.H., Lee H.Y. Panaxynol, a natural Hsp90 inhibitor, effectively targets both lung cancer stem and non-stem cells. Canc. Lett. 2018;412:297–307. doi: 10.1016/j.canlet.2017.10.013. [DOI] [PubMed] [Google Scholar]
- Leach M.J., Kumar S. Cinnamon for diabetes mellitus. Cochrane Database Syst. Rev. 2012;9:CD007170. doi: 10.1002/14651858.CD007170.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonti M., Verpoorte R. Traditional Mediterranean and European herbal medicines. J. Ethnopharmacol. 2017;199:161–167. doi: 10.1016/j.jep.2017.01.052. [DOI] [PubMed] [Google Scholar]
- Leslie C. University of California Press; Berkeley: 1998. Asian Medical Systems: A Comparative Study. [Google Scholar]
- Leslie C., Young A. University of California Press; Berkeley: 1992. Paths to Asian Medical Knowledge. [Google Scholar]
- Li X.L., Wang C.Z., Mehendale S.R., Sun S., Wang Q., Yuan C.S. Panaxadiol, a purified ginseng component, enhances the anti-cancer effects of 5-fluorouracil in human colorectal cancer cells. Canc. Chemother. Pharmacol. 2009;64(6):1097–1104. doi: 10.1007/s00280-009-0966-0. [DOI] [PubMed] [Google Scholar]
- Lin T., Li T. Discussion on the three levels of the prescription-composition principle of TCM. Dtsch. Z. Akupunkt. 2009;52:27–30. [Google Scholar]
- Liu T., Wang N., Zhang L., Zhong L. Chinese herbal medicine for functional abdominal pain syndrome: from clinical findings to basic understandings. Evid Based Complement Alternat Med. 2016;2016:8652523. doi: 10.1155/2016/8652523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Guo F., Wang Y., Li C., Zhang X., Li H., Diao L., Gu J., Wang W., Li D., He F. BATMAN-TCM: a bioinformatics analysis tool for molecular mechanism of traditional Chinese medicine. Sci. Rep. 2016;6:21146. doi: 10.1038/srep21146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas R., McMichael A. Association or causation: evaluating links between “environment and disease”. 2005. https://www.who.int/bulletin/volumes/83/10/792.pdf Accessed: May 1 2020. [PMC free article] [PubMed]
- Luis A., Domingues F., Pereira L. Metabolic changes after licorice consumption: a systematic review with meta-analysis and trial sequential analysis of clinical trials. Phytomedicine. 2018;39:17–24. doi: 10.1016/j.phymed.2017.12.010. [DOI] [PubMed] [Google Scholar]
- Luk H.K.H., Li X., Fung J., Lau S.K.P., Woo P.C.Y. Molecular epidemiology, evolution and phylogeny of SARS coronavirus. Infect. Genet. Evol. 2019;71:21–30. doi: 10.1016/j.meegid.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv H., Li Z., Xie Z., Hu X., Li H., Sun J., Chen X., Wen C. Innovated formulation of TCM pangolin scales to develop a nova therapy of rheumatoid arthritis. Biomed. Pharmacother. 2020;126:109872. doi: 10.1016/j.biopha.2020.109872. [DOI] [PubMed] [Google Scholar]
- Macfarlane J. Common themes in the literature on traditional medicine in Papua New Guinea. P N G Med J. 2009;52(1–2):44–53. [PubMed] [Google Scholar]
- Madeo F., Carmona-Gutierrez D., Kepp O., Kroemer G. Spermidine delays aging in humans. Aging. 2018;10(8):2209–2211. doi: 10.18632/aging.101517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majeed A. How Islam changed medicine. BMJ. 2005;331(7531):1486–1487. doi: 10.1136/bmj.331.7531.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark G., Boulton A., Kerridge D. Rongoā māori is not a complementary and alternative medicine: rongoā māori is A way of life. International Journal of Human Rights Education. 2019;3(1) [Google Scholar]
- Masic I. Contribution of Arabic medicine and pharmacy to the development of health care protection in Bosnia and Herzegovina - the second part. Med. Arch. 2017;71(6):439–448. doi: 10.5455/medarh.2017.71.439-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medagama A.B. The glycaemic outcomes of Cinnamon, a review of the experimental evidence and clinical trials. Nutr. J. 2015;14:108. doi: 10.1186/s12937-015-0098-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melby M.K., Yoshino T., Tonob D., Horiba Y., Watanabe K. Differences in demographics and complementary and alternative medicine use between patients attending integrative kampo versus biomedical clinics in Japan. Compl. Ther. Med. 2019;46:202–209. doi: 10.1016/j.ctim.2019.06.003. [DOI] [PubMed] [Google Scholar]
- Morgan S.G., Lee A. Cost-related non-adherence to prescribed medicines among older adults: a cross-sectional analysis of a survey in 11 developed countries. BMJ Open. 2017;7(1) doi: 10.1136/bmjopen-2016-014287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee P.K., Harwansh R.K., Bahadur S., Banerjee S., Kar A., Chanda J., Biswas S., Ahmmed S.M., Katiyar C.K. Development of Ayurveda - tradition to trend. J. Ethnopharmacol. 2017;197:10–24. doi: 10.1016/j.jep.2016.09.024. [DOI] [PubMed] [Google Scholar]
- Namazi N., Khodamoradi K., Khamechi S.P., Heshmati J., Ayati M.H., Larijani B. The impact of cinnamon on anthropometric indices and glycemic status in patients with type 2 diabetes: a systematic review and meta-analysis of clinical trials. Compl. Ther. Med. 2019;43:92–101. doi: 10.1016/j.ctim.2019.01.002. [DOI] [PubMed] [Google Scholar]
- National Center for Biotechnology Information PubChem database. Ginsenoyne A, CID=5317632. https://pubchem.ncbi.nlm.nih.gov/compound/Ginsenoyne-A Accessed May 1 2020.
- Nauman E. Native American medicine and cardiovascular disease. Cardiol. Rev. 2007;15(1):35–41. doi: 10.1097/01.crd.0000197977.68113.32. [DOI] [PubMed] [Google Scholar]
- Ng F., Yun H., Lei X., Danishefsky S.J., Fahey J., Stephenson K., Flexner C., Lee L. (3R, 9R, 10R)-Panaxytriol: a molecular-based nutraceutical with possible application to cancer prevention and treatment. Tetrahedron Lett. 2008;49(50):7178–7179. doi: 10.1016/j.tetlet.2008.09.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichols C.G., Lee S.J. Polyamines and potassium channels: a 25-year romance. J. Biol. Chem. 2018;293(48):18779–18788. doi: 10.1074/jbc.TM118.003344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishimura K., Plotnikoff G.A., Watanabe K. Kampo medicine as an integrative medicine in Japan. Japan Medical Association Journal. 2009;52(3):147–149. [Google Scholar]
- Odaguchi H., Wakasugi A., Ito H., Shoda H., Gono Y., Sakai F., Hanawa T. The efficacy of goshuyuto, a typical Kampo (Japanese herbal medicine) formula, in preventing episodes of headache. Curr. Med. Res. Opin. 2006;22(8):1587–1597. doi: 10.1185/030079906X112769. [DOI] [PubMed] [Google Scholar]
- Otsuka K. second ed. Singing Dragon; London and Philadelphia: 2016. Kampo: A Clinical Guide to Theory and Practice. [Google Scholar]
- Oz M., Lozon Y., Sultan A., Yang K.H., Galadari S. Effects of monoterpenes on ion channels of excitable cells. Pharmacol. Ther. 2015;152:83–97. doi: 10.1016/j.pharmthera.2015.05.006. [DOI] [PubMed] [Google Scholar]
- Paterson C., Dieppe P. Characteristic and incidental (placebo) effects in complex interventions such as acupuncture. BMJ. 2005;330(7501):1202–1205. doi: 10.1136/bmj.330.7501.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedales R.D., Damatac A.M., Limbo C.A., Marquez C.M., Navarro A.I., Molina J. DNA barcoding of philippine herbal medicinal products. J. AOAC Int. 2016;99(6):1479–1489. doi: 10.5740/jaoacint.16-0185. [DOI] [PubMed] [Google Scholar]
- Qi Y., Zang R., Lu H., Wang Z., Ma Z. Network pharmacology and bioinformatics approach reveals the hypolipidemic mechanism of Dan Tian Jiang Zhi pill. Med. Chem. Res. 2019;29:243–254. [Google Scholar]
- Qian J.Q. Cardiovascular pharmacological effects of bisbenzylisoquinoline alkaloid derivatives. Acta Pharmacol. Sin. 2002;23(12):1086–1092. [PubMed] [Google Scholar]
- Rodrigues T., Sieglitz F., Bernardes G.J. Natural product modulators of transient receptor potential (TRP) channels as potential anti-cancer agents. Chem. Soc. Rev. 2016;45(22):6130–6137. doi: 10.1039/c5cs00916b. [DOI] [PubMed] [Google Scholar]
- Rubel A., Haas M. Sargent and Johnson, Medical Anthropology: Contemporary Theory and Method. Praeger; New York: 1996. Ethnomedicine. [Google Scholar]
- Saeed S.A., Gilani A.H., Majoo R.U., Shah B.H. Anti-thrombotic and anti-inflammatory activities of protopine. Pharmacol. Res. 1997;36(1):1–7. doi: 10.1006/phrs.1997.0195. [DOI] [PubMed] [Google Scholar]
- Sarris J., Stough C., Bousman C.A., Wahid Z.T., Murray G., Teschke R., Savage K.M., Dowell A., Ng C., Schweitzer I. Kava in the treatment of generalized anxiety disorder: a double-blind, randomized, placebo-controlled study. J. Clin. Psychopharmacol. 2013;33(5):643–648. doi: 10.1097/JCP.0b013e318291be67. [DOI] [PubMed] [Google Scholar]
- Sawada R., Iwata M., Umezaki M., Usui Y., Kobayashi T., Kubono T., Hayashi S., Kadowaki M., Yamanishi Y. KampoDB, database of predicted targets and functional annotations of natural medicines. Sci. Rep. 2018;8(1):11216. doi: 10.1038/s41598-018-29516-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scaccia A. Kava: inside the all-natural high that's sweeping America. 2018. https://www.rollingstone.com/culture/culture-news/kava-inside-the-all-natural-high-thats-sweeping-america-125828/ Accessed May 1 2020.
- Shim S., Sung S., Lee M. Ginsenoyne C, a polyacetylene isolated from Panax Ginseng inhibit inflammatory mediators via regulating extracellular regulated kinases signaling. Phcog. Mag. 2018;14(57):358–362. [Google Scholar]
- Showman A.F., Baker J.D., Linares C., Naeole C.K., Borris R., Johnston E., Konanui J., Turner H. Contemporary Pacific and Western perspectives on 'awa (Piper methysticum) toxicology. Fitoterapia. 2015;100:56–67. doi: 10.1016/j.fitote.2014.11.012. [DOI] [PubMed] [Google Scholar]
- Snow J. Context effects in western herbal medicine: fundamental to effectiveness? Explore. 2016;12(1):55–62. doi: 10.1016/j.explore.2015.10.004. [DOI] [PubMed] [Google Scholar]
- Song L.S., Ren G.J., Chen Z.L., Chen Z.H., Zhou Z.N., Cheng H. Electrophysiological effects of protopine in cardiac myocytes: inhibition of multiple cation channel currents. Br. J. Pharmacol. 2000;129(5):893–900. doi: 10.1038/sj.bjp.0703132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starkus J., Jansen C., Shimoda L.M.N., Stokes A.J., Small-Howard A.L., Turner H. Diverse TRPV1 responses to cannabinoids. Channels. 2019;13(1):172–191. doi: 10.1080/19336950.2019.1619436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiner G.G. The correlation between cancer incidence and kava consumption. Hawaii Med. J. 2000;59(11):420–422. [PubMed] [Google Scholar]
- Steinhorn D.M., Din J., Johnson A. Healing, spirituality and integrative medicine. Ann. Palliat. Med. 2017;6(3):237–247. doi: 10.21037/apm.2017.05.01. [DOI] [PubMed] [Google Scholar]
- Sun Y., Yang J. A bioinformatics investigation into the pharmacological mechanisms of the effect of Fufang Danshen on pain based on methodologies of network pharmacology. Sci. Rep. 2019;9(1):5913. doi: 10.1038/s41598-019-40694-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunshine A., Laska E., Meisner M. Oral aspirin in post-operative pain: a quantitative, systematic review. Pain. 2000;88(3):309–311. doi: 10.1016/S0304-3959(00)00316-X. [DOI] [PubMed] [Google Scholar]
- Talavera K., Startek J.B., Alvarez-Collazo J., Boonen B., Alpizar Y.A., Sanchez A., Naert R., Nilius B. Mammalian transient receptor potential TRPA1 channels: from structure to disease. Physiol. Rev. 2020;100(2):725–803. doi: 10.1152/physrev.00005.2019. [DOI] [PubMed] [Google Scholar]
- Tao W., Tian L., Zhang W., Dan C., Yun Z., Hong L., Zhi L., Ping W., Jun Z., Ling Z. Use of network pharmacology and molecular docking to investigate the mechanism by which ginseng ameliorates hypoxia. Biomed. Environ. Sci. 2018;31(11):855–858. doi: 10.3967/bes2018.114. [DOI] [PubMed] [Google Scholar]
- Teng L., Zu Q., Li G., Yu T., Job K.M., Yang X., Di L., Sherwin C.M., Enioutina E.Y. Herbal medicines: challenges in the modern world. Part 3. China and Japan. Expet Rev. Clin. Pharmacol. 2016;9(9):1225–1233. doi: 10.1080/17512433.2016.1195263. [DOI] [PubMed] [Google Scholar]
- Triolet J., Shaik A.A., Gallaher D.D., O'Sullivan M.G., Xing C. Reduction in colon cancer risk by consumption of kava or kava fractions in carcinogen-treated rats. Nutr. Canc. 2012;64(6):838–846. doi: 10.1080/01635581.2012.689917. [DOI] [PubMed] [Google Scholar]
- Van Wyk B.E. A family-level floristic inventory and analysis of medicinal plants used in Traditional African Medicine. J. Ethnopharmacol. 2020;249:112351. doi: 10.1016/j.jep.2019.112351. [DOI] [PubMed] [Google Scholar]
- Nutrition, Kava kava. https://www.amazon.com/700mg-Capsules-Methysticum-Extract-Supply/dp/B07B3PLXNY. (Accessed: May 1 2020).
- Walle G. Kava kava: benefits, side effects and dosage. 2018. https://www.healthline.com/nutrition/kava-kava#section1 Accessed: May 1 2020.
- Wambebe C. first ed. CRC Press; Boca Raton: 2018. African Indigenous Medical Knowledge and Human Health. [Google Scholar]
- Wang J., Zhang X., Lan H., Wang W. Effect of garlic supplement in the management of type 2 diabetes mellitus (T2DM): a meta-analysis of randomized controlled trials. Food Nutr. Res. 2017;61(1):1377571. doi: 10.1080/16546628.2017.1377571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Wu S., Liu S. Integration of (+)-catechin and beta-sitosterol to achieve excellent radical-scavenging activity in emulsions. Food Chem. 2019;272:596–603. doi: 10.1016/j.foodchem.2018.08.098. [DOI] [PubMed] [Google Scholar]
- Wang Y., Narayanapillai S.C., Tessier K.M., Strayer L.G., Upadhyaya P., Hu Q., Kingston R., Salloum R.G., Lu J., Hecht S.S., Hatsukami D.K., Fujioka N., Xing C. The impact of one-week dietary supplementation with kava on biomarkers of tobacco use and nitrosamine-based carcinogenesis risk among active smokers. Canc. Prev. Res. 2020;13(5):483–492. doi: 10.1158/1940-6207.CAPR-19-0501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe K., Matsuura K., Gao P., Hottenbacher L., Tokunaga H., Nishimura K., Imazu Y., Reissenweber H., Witt C. 2011. Traditional Japanese Kampo Medicine: Clinical Research between Modernity and Traditional Medicine - the State of Research and Methodological Suggestions for the Future. Evidence-Based Complementary and Alternative Medicine : eCAM 2011. Article ID. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe K., Plotnikoff G.A., Sakiyama T., Reissenweber-Hewel H. Collaboration of Japanese kampo medicine and modern biomedicine. Evid. base Compl. Alternative Med. 2014;2014 doi: 10.1155/2014/646947. Article ID: 646947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson E.M. Interactions between herbal and conventional medicines. Expet Opin. Drug Saf. 2005;4(2):355–378. doi: 10.1517/14740338.4.2.355. [DOI] [PubMed] [Google Scholar]
- Wirtz V.J., Hogerzeil H.V., Gray A.L., Bigdeli M., de Joncheere C.P., Ewen M.A., Gyansa-Lutterodt M., Jing S., Luiza V.L., Mbindyo R.M., Moller H., Moucheraud C., Pecoul B., Rago L., Rashidian A., Ross-Degnan D., Stephens P.N., Teerawattananon Y., t Hoen E.F., Wagner A.K., Yadav P., Reich M.R. Essential medicines for universal health coverage. Lancet. 2017;389(10067):403–476. doi: 10.1016/S0140-6736(16)31599-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfgram M. University of Michigan; Ann Arbor: 2009. Ayurveda in the Age of Biomedicine: Discursive Asymmetries and Counter-strategies. [Google Scholar]
- World Health Organization . 2013. WHO Traditional Medicine Strategy; pp. 2014–2023. [Google Scholar]
- Xu R., Fidler J., Musser J. Bioactive compounds from Tripterygium wilfordii. Stud. Nat. Prod. Chem. 2005;32:773–801. [Google Scholar]
- Yakubo S., Ito M., Ueda Y., Okamoto H., Kimura Y., Amano Y., Togo T., Adachi H., Mitsuma T., Watanabe K. Pattern classification in kampo medicine. Evid. base Compl. Alternative Med. 2014;2014:535146. doi: 10.1155/2014/535146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye F., Li J., Wu Y., Zhu Z.D., Mollo E., Gavagnin M., Gu Y.C., Zhu W.L., Li X.W., Guo Y.W. Sarinfacetamides A and B, nitrogenous diterpenoids with tricyclo[6.3.1.0(1,5)]dodecane scaffold from the south China sea soft coral sarcophyton infundibuliforme. Org. Lett. 2018;20(9):2637–2640. doi: 10.1021/acs.orglett.8b00842. [DOI] [PubMed] [Google Scholar]
- Yeh G.Y., Eisenberg D.M., Kaptchuk T.J., Phillips R.S. Systematic review of herbs and dietary supplements for glycemic control in diabetes. Diabetes Care. 2003;26(4):1277–1294. doi: 10.2337/diacare.26.4.1277. [DOI] [PubMed] [Google Scholar]
- Yoshino T., Katayama K., Horiba Y., Munakata K., Yamaguchi R., Imoto S., Miyano S., Mima H., Watanabe K. Predicting Japanese Kampo formulas by analyzing database of medical records: a preliminary observational study. BMC Med. Inf. Decis. Making. 2016;16:118. doi: 10.1186/s12911-016-0361-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeisel S.H. Dietary choline: biochemistry, physiology, and pharmacology. Annu. Rev. Nutr. 1981;1:95–121. doi: 10.1146/annurev.nu.01.070181.000523. [DOI] [PubMed] [Google Scholar]
- Zhang R., Zhu X., Bai H., Ning K. Network pharmacology databases for traditional Chinese medicine: review and assessment. Front. Pharmacol. 2019;10:123. doi: 10.3389/fphar.2019.00123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T., Wu Q., Zhang Z. Probable pangolin origin of SARS-CoV-2 associated with the COVID-19 outbreak. Curr. Biol. 2020;30(7):1346–1351. doi: 10.1016/j.cub.2020.03.022. e1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X., Zijian L., Fan T., Zheng J. A novel drug discovery strategy inspired by traditional medicine philosophies. Science. 2015;347(6219 Suppl. l):S38–S40. [Google Scholar]
- Zheng W., Wu J., Gu J., Weng H., Wang J., Wang T., Liang X., Cao L. Modular characteristics and mechanism of action of herbs for endometriosis treatment in Chinese medicine: a data mining and network pharmacology-based identification. Front. Pharmacol. 2020;11:147. doi: 10.3389/fphar.2020.00147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong G.G., Sun C.W., Li Y.Y., Qi H., Zhao C.Y., Jiang Y., Wang X.M., Yang S.J., Li H. Calcium channel blockade and anti-free-radical actions of panaxadiol saponins Rb1, Rb2, Rb3, Rc, and Rd. Zhongguo Yaoli Xuebao. 1995;16(3):255–260. [PubMed] [Google Scholar]
- Zhou J., Zhang J., Gao G., Wang H., He X., Chen T., Ke L., Rao P., Wang Q. Boiling licorice produces self-assembled protein nanoparticles: a novel source of bioactive nanomaterials. J. Agric. Food Chem. 2019;67(33):9354–9361. doi: 10.1021/acs.jafc.9b03208. [DOI] [PubMed] [Google Scholar]
- Zivin K., Ratliff S., Heisler M.M., Langa K.M., Piette J.D. Factors influencing cost-related nonadherence to medication in older adults: a conceptually based approach. Value Health. 2010;13(4):338–345. doi: 10.1111/j.1524-4733.2009.00679.x. [DOI] [PMC free article] [PubMed] [Google Scholar]