Abstract
Caring for an individual with autism spectrum disorder (ASD) in ideal circumstances can be stressful, and the Coronavirus disease (COVID-19) pandemic created a high degree of disruption to life and stress to families living with an individual with ASD. We conducted an online survey of families in Michigan that revealed higher levels of stress in caregivers of younger individuals with ASD and those with greater severity of ASD symptoms. Stress around therapeutic service disruption, finances, and illness predominated and greater stress was reported for caregivers of individuals receiving greater intensity of services pre-COVID-19. Respondents voiced concerns about receiving respite care during COVID-19, and those expressing interest in respite also reported greater symptom severity in the person with ASD.
Electronic supplementary material
The online version of this article (10.1007/s10803-020-04760-5) contains supplementary material, which is available to authorized users.
Keywords: Autism spectrum disorder, COVID-19, Families, Stress
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by deficits in social communication along with restricted, repetitive patterns of behavior, interests, or activities (American Psychiatric Association 2013). The reported prevalence of ASD has continued to increase in recent years, with current estimates now 1 in 54 children in the United States (US) (Maenner et al. 2020). Parenting a child with ASD can be stressful (Bonis 2016); meeting the needs of individuals with ASD can be challenging due to the severity and chronicity of the condition, the mental health comorbidities, intensive interventions needed by persons with ASD and the difficulty obtaining services (Vohra et al. 2014). In fact, caring for a child with ASD is associated with greater parenting stress than any other disability (Hayes and Watson 2013), and caregivers also endure significant financial burden in the process (Kogan et al. 2008).
Coronavirus disease 2019 (COVID-19) is caused by a novel virus that results in severe acute respiratory symptoms, and it developed into a global pandemic impacting more than four million people in the five months since it was first identified in December 2019 (Johns Hopkins University Center for Systems Science and Engineering 2020). The US declared a pandemic emergency on March 13, 2020 (The White House 2020), and many states moved to declare stay-at-home orders (Tolbert et al. 2020) which were meant to prevent rapid spread of the virus and minimize the risk of overwhelming healthcare systems (Kenyon 2020).
Michigan issued a state of emergency the same day their first case was announced (March 10, 2020), and followed with a “stay-at-home” protective order 2 weeks later (Office of Governor Gretchen Whitmer 2020), with closure of all Michigan schools for the rest of the academic year. This resulted in many families being restricted to home (except for essential activities such as grocery shopping and pharmacy visits), many people being furloughed or laid off due to the economic impact on their workplaces, and about 1.5 million students, including almost 21,000 students with ASD, unable to access educational or therapeutic services. Prior to COVID-19, Michigan had mandated Medicaid and many commercial insurances to cover Applied Behavior Analysis (ABA) services for individuals with ASD up to age 21 (Michigan Autism Legislation PA 99 and PA 100,2012). Due to the stay-at-home order, center-based and home-based ABA and other rehabilitative services such as outpatient speech and occupational therapy were not accessible to individuals with ASD.
There have been surveys about the impact of COVID-19 on families, especially around mental health (both for mothers and other family members), child care (for working parents) and household finances (for stay-at-home parents) (COVID-19 Addendum to Motherly’s 2019 State of Motherhood survey 2019). A study from Italy reported on challenges faced by families with their children’s behavior issues and stressors related to lockdown (Colizzi et al. 2020). Another study from China (Xie et al. 2020) found that students reported high levels of anxiety and depression during the COVID-19 outbreak there. However, given that no published data exists yet in the US for caregivers of individuals with ASD, we sought to conduct this study with the objective to query current and projected functioning status, levels of disruption and stress, causes of those stressors, and priorities for support reported by families of children/individuals with ASD during COVID-19. The primary aim was to explore the extent and causes of stressors experienced by families of individuals; and the secondary aim was to determine whether there was an association between working status of parent, level of severity of individual with ASD, and previous levels of support on current expressed distress due to COVID-19.
Methods
Survey Design
Given the abrupt onset of the COVID-19 shutdowns, the Autism Alliance of Michigan (AAoM) anticipated that people with ASD and their families would experience a surge in, and alteration of, social service support needs including respite resources, tele-therapy, and local support groups. In order to ascertain whether and in what way stressors and support needs had shifted due to COVID-19, a survey was rapidly developed to quantitatively and qualitatively assess current and anticipated future states. An online Qualtrics survey was designed to collect information about demographic factors for both the individual with ASD (age and severity of ASD symptoms) and caregiver (employment status and relation to individual with ASD), as well as questions about disruption and stress that the COVID-19 restrictions had caused the family. The degree of disruption (“How disruptive to daily activities have the COVID-19 changes been for you and the individual with ASD?”) and stress (“What are the stress levels of you and the individual with ASD?”) were asked on a scale of 0 indicating no disruption/stress to 10 indicating severe disruption/stress. Respondents were asked to report the frequency of service utilization before the COVID-19 pandemic, measured for school, community mental health center, therapy center, and parent group with an ordinal scale variable (No services from this provider/A few times per year/1–3 times per month/1–4 times per week / Daily services). Respondents were asked to evaluate the severity of ASD in eight domains using ten-point scales which were summed to create an 80-point severity score that was treated as a continuous, normally distributed variable for analysis. The ASD symptom severity sum was derived from individual severity ratings in domains of verbal communication difficulties, non-verbal communication difficulties, self-abusive behavior, aggression, inflexibility, restricted & repetitive interests, sleep difficulties, and safety concerns. Respondents indicated greatest stressors (“What is causing the most stress for you and your family?”) with check-box options: individual with ASD being home all the time, being separated from the individual with ASD, finances, concern about becoming ill, lack of care other than myself for individual with ASD, as well as a free-text “other” option. An additional measure was gathered asking whether in-home respite services would be accepted (Yes, Maybe, or No) and, if so, how useful those respite services would be (5-point Likert).
The survey was piloted through interviews of 18 families who were not included in the study. The study was reviewed and deemed exempt by the Western Michigan University Homer Stryker M.D. School of Medicine Institutional Review Board (IRB).
Participant Recruitment and Survey Dissemination
The Autism Alliance of Michigan (AAoM) is a non-profit agency that leads efforts to raise expectations and expand opportunities for people impacted by ASD across the lifespan. Their family navigators educate the community about ASD and advocate for families for interventions, employment support and independent living. The COVID-19 survey was distributed to a geographically diverse subset of 1000 families from the AAoM database as a program evaluation within 3 days after the stay-at-home order was issued in Michigan. In addition, a link to the survey was included in their newsletter and on their Facebook page. Incomplete and duplicate responses were excluded from analysis and an opt-out of including data in research allowed for delinking the data for program evaluation from the research project.
Statistical Analysis
All statistical analysis was completed using SAS software, version 9.4 (Cary, NC, USA). Survey respondent demographics were summarized using mean (standard deviation) for numeric data and frequency (percent) for categorical.
The primary outcome variables measured the level of disruption and level of stress due to the COVID-19 pandemic, assessed by the respondent for both themselves (“you”) as well as the individual with ASD (“ASD”). This resulted in four outcome measures each taking on values 0–10. These are treated as continuous, normally distributed variables for analysis.
Generalized linear models were used to assess these four outcomes’ relationships with several possible predictors including the continuous variables for age of the ASD individual, the severity score for the ASD individual, and utilization of services during the COVID-19 pandemic; several five-level ordinal variables measuring utilization of services pre-COVID-19; nominal variables for the employment and at-home status of the caregiver andurban/rural location status, and the indicator variables for greatest stressors.
A step-down model building strategy was used to remove insignificant predictors from the models based on Type-III sum of squares p-values. For each of the four outcome measures, the final model’s significant predictors and their associated p-values were reported. Finally, thematic analysis of free text responses regarding concerns about in-home respite services as well as “other stressors” was done by two authors and responses assigned to one or more sub-themes.
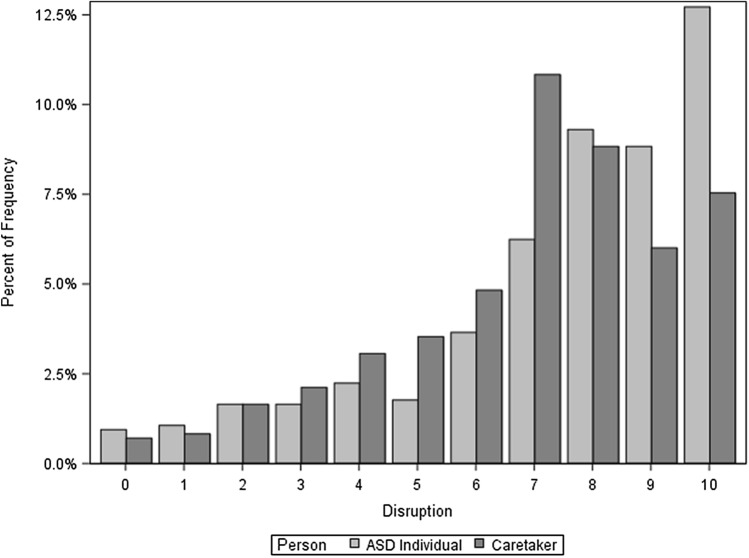
Two 97.5% confidence intervals (with an overall confidence level of 95%) were used to estimate the difference in mean ASD symptom severity score between caregivers who said “Yes” to in-home respite and those who said “Maybe” and then between those who answered “Maybe” and those who answered “No.” Following a six-week data collection period from March 26th, 2020 through May 4th, 2020, the survey respondents and final data sample inclusion of 471 respondents, who hailed from 58 counties in Michigan, are displayed in Fig. 1.
Fig. 1.
Data collection flowchart
Results
A summary of the demographic information from these respondents is presented in Table 1. Twelve were “self” respondents and the remaining were caregivers (n = 459). Of 24 “other” respondents, “child,” “son” or “daughter,” was indicated several times, but we could not verify if the respondent was a parent or a descendent of the person with ASD. Two responses indicated “caregiver,” one “cousin”, and one response was an individual with ASD with a child who also had ASD.
Table 1.
Demographics of survey responses (n = 471)
| Frequency | Percent (%) | |
|---|---|---|
| Relationship to ASD | ||
| Parent | 414 | 87.9 |
| Grandparent | 16 | 3.4 |
| Self | 12 | 2.6 |
| Sibling | 4 | 0.9 |
| Foster parent | 1 | 0.2 |
| Other | 24 | 5.1 |
| Location | ||
| Rural | 107 | 23.2 |
| Urban | 354 | 76.8 |
| Employment | ||
| Employed | 222 | 47.4 |
| Unemployed | 246 | 52.6 |
| Age | ||
| 21 and under | 402 | 86.6 |
| Over 21 | 62 | 13.4 |
| ASD severity* | ||
| Low | 183 | 38.9 |
| Medium | 233 | 49.5 |
| High | 55 | 11.7 |
*ASD severity scores of 0–26 are considered low severity, 27–53 as medium, and 54–80 as high
The 12 self-reporters ranged in age from 20 to 52 with a mean (S.D.) of 30.8 (9.6) years of age. The severity scores ranged from 0 to 57 with a mean (S.D.) of 23.3 (20.8). Eight (66.7%) were unemployed, seven of whom reported being at home. Of the four who were employed, two reported being at home. Overall, nine (75%) of self-reporters indicated they were at home. Seven (58%) self-reported a disruption score of 7 or more, and 7 (58%) self-reported a stress score of 7 or more.
For the 456 caregiver-reporters who answered the employment question, 238 (52.2%) were unemployed, 225 (94.5%) of whom reported being at home. The cause of unemployment was not queried. Of the 218 who were employed, 154 (70.6%) reported being at home. Overall, 379 (83.1%) of caregivers indicated they were at home. Among caregivers, the age of the person with ASD ranged from 2 to 46 years of age with a mean (S.D.) of 11.8 (7.9) years. The severity scores ranged from 0 to 80 and appeared approximately normally distributed with a mean (S.D.) of 32.9 (16.9).
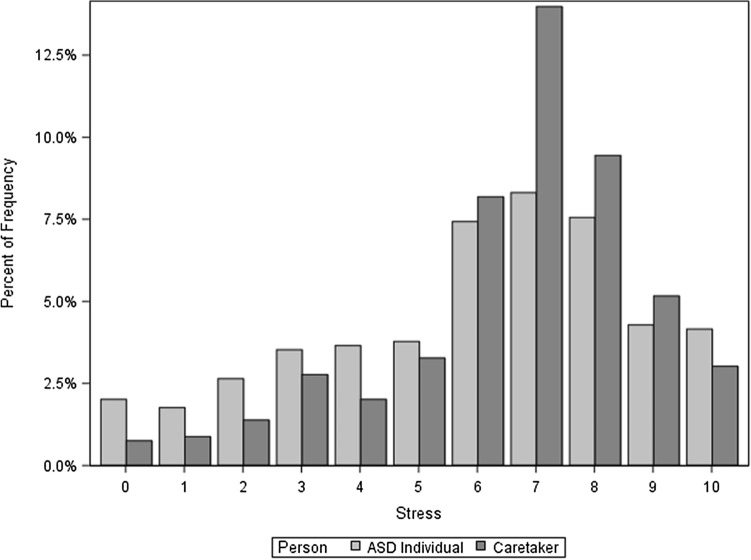
We display the reported degree of disruption in Fig. 2. The mean (S.D.) disruption score for the respondent was 6.9 (2.4), with 280 (66.4%) respondents selecting 7 or more. The mean (S.D.) disruption score for the ASD individual was 7.5 (2.6) with 314 (74.2%) respondents selecting 7 or more.
Fig. 2.
Comparative bar chart of disruption score for caregiver and ASD individual
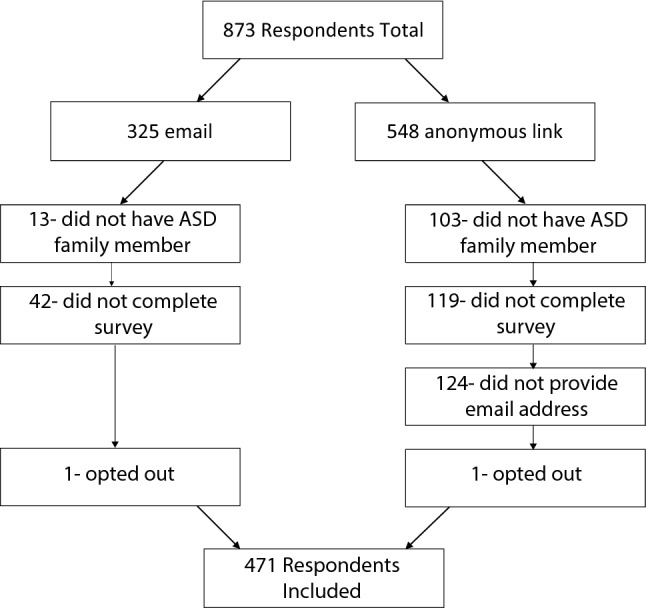
We display the reported degree of stress in Fig. 3. The mean (S.D.) stress score for the respondent was 6.6 (2.2), with 251 (62.1%) respondents selecting 7 or more. The mean (S.D.) stress score for the ASD individual was 6.0 (2.7), with 193 (49.5) respondents selecting 7 or more.
Fig. 3.
Comparative bar chart of stress score for caregiver and ASD individual
Caregivers reported 0 (no support) to 10 (great support) scores regarding usage of services during the COVID-19 pandemic, with the greatest amount of support from family, friends, etc. (mean ± S.D.: 4.8 ± 3.8), followed by school (3.3 ± 3.5), therapy center (2.9 ± 3.5), mental health services (1.3 ± 2.6), and then parent support group (1.1 ± 2.5). The responses of frequency of services utilized before the pandemic are shown in Table 2.
Table 2.
Utilization of common support services before the COVID-19 pandemic
| Service | Frequency (%) | ||||
|---|---|---|---|---|---|
| Daily | 1–4 times/week | 1–3 times/month | A few times/year | Never | |
| School | 199 (43.9) | 83 (18.3) | 34 (7.5) | 20 (4.4) | 117 (25.8) |
| Community mental health | 27 (6.1) | 32 (7.2) | 68 (15.3) | 50 (11.3) | 267 (60.1) |
| Therapy Center | 88 (19.7) | 141 (31.6) | 59 (13.2) | 26 (5.8) | 132 (29.6) |
| Parent Support Group | 13 (2.9) | 18 (4) | 59 (13.3) | 47 (10.6) | 308 (69.2) |
Responding to the greatest stressor question, 250 caregivers (54.5%) indicated worrying about the individual with ASD being home all the time; 239 (52.1%) indicated concern about becoming ill or the individual with ASD becoming ill; 141 (30.7%) indicated stress about finances; 102 (22.2%) indicated worrying about lack of care other than myself for individual with ASD; and 23 (5%) indicated stress from being separated from individual with ASD. Thematic analysis of the “other” responses for the 186 caregiver-reporters who utilized this field revealed nine sub-themes (excluding “unclassifiable”) which were then grouped into three over-arching themes reported in Table 3. The two primary concerns from self-reporters were concern about being home all the time and finances, each checked by 6 (50%) of respondents.
Table 3.
Thematic analysis of “Other stressor” free text responses
| Overarching theme | Frequency (%) | Sub-theme | Frequency | Examples |
|---|---|---|---|---|
| Caregiver stressor | 47 (25.3) | Financial | 4 | • “Insurance doesn't cover services, paying out of pocket” |
| Health | 9 |
• “Inavalibility of prescriptions” • “Keeping them from being exposed” |
||
| Concerns for other children | 7 |
• “Sibling 3 years old also home” • “Second child is showing signs of ASD now as sell” |
||
| Parental stressors | 31 |
• “Having to work at the same time as having to keep my son busy with learning activities” • “Losing my job because I have no one to watch our two children” |
||
| Person with ASD stressor | 77 (41.4) | Behavior concerns | 16 |
• “Regression and aggression” • “he wont stop eating” |
| Isolation | 21 |
• “Family being together in a small apartment all day, every day is hard for even non-ASD family members” • “He needs the interaction with the people in his office” |
||
| Change in routine | 44 |
• “He is in a specialized group home and on no kind of schedule.” • “No current routine need one set up!!” |
||
| Service stressor | 66 (35.5) | School absence | 26 |
• “Just trying to work from home and figure out how to continue her education as best as I can without being a teacher” • “Her education slipping and becoming further behind” |
| ABA or therapeutic concerns | 44 |
• "Lack of services (no ABA, no speech, no special education in person)" • “Missing essential therapies due to distancing” |
||
| Unclassifiable | 13 |
• “Depression” • “Fear ‘normal’ will never return” • “Uncertainty” |
Frequencies of sub-themes do not sum to the frequency of the overarching theme because each free-response can have more than one sub-theme. Syntactical errors in responses are direct verbatim from respondents
The model selection strategy detailed in methods (statistical analysis) above resulted in four models for each of the four outcomes, each with a different set significant predictor variables, displayed in Table 4. Each model's row gives the slope and p-value of the predictors that were deemed significant.
Table 4.
Slopes and associated p-values for the outcomes measuring disruption and stress level of caregivers and individuals with ASD
| Predictors | ||||||
|---|---|---|---|---|---|---|
| ASD severity score | ASD age | Frequency of school utilization pre-COVID-19 (daily vs. never) | Worry about the individual with ASD being home all the time | Concern about becoming ill or the individual with ASD becoming ill | Stress from being separated from individual with ASD | |
| Outcomes | ||||||
| Disruption—you | 0.024 | 0.505 | 0.484 | |||
| (P = 0.0005) | (P = 0.0314) | (P = 0.0362) | ||||
| Disruption—ASD | 0.024 | 1.088 | 0.85 | 1.264 | ||
| (P = 0.0011) | (P = 0.0004) | (P = 0.0008) | (P = 0.0369) | |||
| Stress—you | 0.02 | − 0.032 | 0.622 | 0.6 | ||
| (P = 0.0012) | (P = 0.0168) | (P = 0.0034) | (P = 0.004) | |||
| Stress—ASD | 0.038 | 0.04 | 1.63 | |||
| (P < 0.0001) | (P = 0.0133) | (P < 0.0001) | ||||
Positive slopes represent the increase in outcome score from the presence of that stress cause
P-values are italicized for ease of discriminating them from the slopes, which are frequently small
We found ASD severity score to be significant in every single outcome, with all positive slopes indicating that higher ASD severity scores correspond to higher levels of disruption or stress for either caregiver or ASD individual. Likewise, worrying about the individual with ASD being home all the time was a significant predictor of all four outcome measures. The positive slopes for this variable indicate that this stress corresponded with higher levels of stress and disruption for both the caregiver and the ASD individual. Age of ASD individual was significantly associated with the stress measures for both the caregiver and the person with ASD. Controlling for the other significant variables, ASD age was negatively correlated with stress for caregivers, with an increase of age of ASD individual by one year corresponding to a decrease in stress score by 0.032 (p = 0.0168). In contrast, ASD age was positively correlated with stress for ASD individual, with an increase of age of ASD individual by one year corresponding to an increase of stress score by 0.04 (p = 0.0133).
Greater usage of school before COVID-19 was significantly associated with higher disruption scores for the individual with ASD. Individuals with ASD who attended school daily had an increased disruption score of 1.088 (p = 0.0004) over ASD individuals who never attended school, controlling for the other significant variables. Similarly, caregiver indication of stress from being separated from the person with ASD was associated with an increase of 1.264 in the ASD disruption score (p = 0.0369), controlling for the other significant variables.
Concern about caregiver him/herself becoming ill or the person with ASD becoming ill was significantly associated with both higher stress levels and higher disruption levels for the caregiver with an increase in stress score for the caregiver of 0.6 (p = 0.004) and an increase in disruption score of 0.484 (p = 0.0362), controlling for the other significant variables.
Asked about interest in in-home respite services, 3 (27%) self-reporters said “Yes,” 4 (36%) said “Maybe,” and another 4 said “No.” Among caregiver-reporters, 124 (27.1%) said “Yes,” 143 (31.3%) said “Maybe,” and 190 (41.6%) said “No.” There was a significant relationship between ASD severity and interest of caregiver in in-home respite services. The mean ASD severity score reported by caregivers in the “Yes” group was 6.2 (97.5% CI: 1.8–10.7) points higher than the mean ASD severity score reported by caregivers in the “Maybe” group, and the mean of the “Maybe” group was 5.9 (97.5% CI: 1.9–9.8) points higher than the mean of the “No” group. The thematic analysis yielded eleven sub-themes (excluding “unclassifiable”), which were then grouped into four over-arching themes presented in Table 5.
Table 5.
Thematic analysis of free text responses of concerns about in-home respite services
| Overarching theme | Frequency (%) | Sub-theme | Frequency | Examples |
|---|---|---|---|---|
| COVID-19 concern | 133 (50.6) | Fear of illness | 109 |
• “Bringing illness into the home” • “Do not want to spread Covid 19.” |
| Need for social distancing | 24 |
• “It goes against social distancing guidelines.” • “Less people in my home as possible.” |
||
| Respite provider concern | 51 (19.4) | Stranger/trust | 27 | • “Making sure the person is trustworthy and has had a complete security check.” |
| Resistance from person with ASD | 16 | • “I would have a concern that he would not click with the person.” | ||
| Qualifications/training | 4 | • “ behavioral challenges that can be too severe to hand off to a new/untrained person” | ||
| Risk of abuse | 4 | • “We have had previous abuse” | ||
| Family concern | 23 (8.8) | Financial | 3 | • “If medicaid would cover it.” |
| Disruptive to routine | 14 | • “They don't know my kid or what his specific needs are and it would take too much time to tell them to make it worth it.” | ||
| Logistics/space | 6 | • “house is small so there is not enough room.” | ||
| Not desired | 56 (21.3) | Already have this | 6 | • “I already have a respite provider that I hired in” |
| Not needed | 50 | • “Doesnt need it at this time” |
The frequencies of sub-themes do not sum to the frequency of the overarching theme because each free-response can have more than one sub-theme
Discussion
To our knowledge, this is the first published study of families facing challenges with ASD during the COVID-19 pandemic in the US. Our study revealed that during the COVID-19 crisis, individuals with ASD and their families report high levels of stress and disruption to life. The greatest areas of stress were around isolation, illness and finance, and we noted many free-text responses revealing a desire of families to communicate the burden with which they are living.
Not surprisingly, the more severe symptoms the individual with ASD is reported to have, the greater the reported degree of stress by the caregiver. This is consistent with literature even during non-pandemic times (Hall and Graff 2011; Rivard et al. 2014). Additionally, caregivers report a higher degree of stress when the individual with ASD is younger, while they report individuals with ASD who are older are experiencing greater stress. Clinical experience leads us to posit that caregivers of younger individuals are experiencing stress due to the lack of service access, and the isolation and extended time spent providing proxy services while caring for the individual in addition to other family needs. Past studies have suggested that improved coping/caregiver ability to manage the needs and care for the individual with ASD over time likely also contributes to lesser stress the older the individual with ASD is (Fitzgerald et al. 2002; Lounds et al. 2007). The finding of higher stress reported for individuals who previously had services (specifically school services) is understandable since interventions have been previously shown to reduce caregiver stress (Krakovich et al. 2016). This is especially pertinent at a time like the current pandemic where school related interventions (educational and therapeutic) in Michigan were not accessible in the aftermath of the stay-at-home declaration and even when reintroduced, were limited in scope and delivery (virtual and online). One salient finding amplified in a pandemic situation is the fear of falling ill, and our study found this fear to be a significant predictor of stress, similar to previous studies where parental fear of illness increases stress, particularly around caring for a child with ASD (Weiss et al. 2014). We understand why our study respondents reported illness as a significant concern given that there is currently no definitive treatment or vaccine against COVID-19. Another important finding is the concern about isolation; while stay-at-home orders are meant to “flatten the curve” of COVID-19 transmission, social isolation can have deleterious effects on mental health (Leigh-Hunt et al. 2017). This can further increase the stress on families coping with ASD during a pandemic crisis.
Respite care is both an unmet need in families challenged with ASD and other developmental disabilities (Lindly et al. 2016) as well as a source of reduced stress for parents of individuals with ASD (Harper et al. 2013). Due to the stressors of isolation and lack of services as a result of the COVID-19 pandemic, we were surprised to find that only 27% of respondents were comfortable in obtaining in-home respite services. However, it became clear that symptom severity of the individual with ASD was positively related to willingness to consider respite services even with the inherent health risk. In weighing the relative risks and benefits from in-person interaction during a pandemic, caregivers of more severely symptomatic individuals were more likely to accept the risks for the benefits of outside assistance. This difference in evaluation may inform which families return to in-person educational, therapeutic, and recreational services as those options become more available.
Ultimately, the purpose of our study was to inform the AAoM Navigator program, which delivers professional case management service to Michigan families affected by ASD via one-on-one support to help them navigate and overcome the many barriers they face when trying to access care and support for their loved ones (Autism Alliance of Michigan, n.d.). It was important for the program to hear from the stakeholders that they serve, and the survey information will be used to adjust approaches and tailor information to address specific needs and concerns of families. Previously, patient navigators have been well received by families who care for an individual with ASD in terms of accessing needed services (Roth et al. 2016). The Navigator program will share important resources with families around coping during COVID-19 in general such as the COVID-19 toolkit (Hume et al. 2020) and other recommendations (Narzisi 2020), as well as connect families with local resources for respite, virtual parent support groups and tele-therapies where available.
Limitations to this study include only sampling Michigan respondents which may not be generalizable to other states and regions of the country with different approaches to the COVID-19 pandemic around stay-at-home orders or school closings. Self-selection bias is inherent with online survey methodology employing nonprobability sampling. For respondents via Facebook or the newsletter, a response rate could not be calculated. Given the evolving nature of the pandemic, it is possible that survey administered at different time-frames would have yielded different concerns. We did not independently confirm diagnoses reported by respondents or level of severity nor use additional standardized measures for adaptive functioning. We conducted the study in the early days of the COVID-19 pandemic and resulting stay-at-home orders with schools and therapies generally inaccessible to families of individuals with ASD. It is likely that a prolonged situation with social isolation and lack of services, compounded by economic downturn and attendant job loss would compound the stress and disruption felt by families of individuals with ASD. We are hopeful there would be follow-up studies building on our work across the US and in other regions to examine how perceptions of families change as we enter the different stages of the pandemic.
However, we believe the timeliness of our survey has enabled a “first look” at the concerns of families challenged with ASD in our state. The importance of advocacy and service provision organizations supporting families during this crisis is reflected in final caregiver responses on the survey: “Thank you for reaching out. I find it deeply disturbing that I have not received a questionnaire like this from our [therapy provider]. Despite many calls up the chain of command, to date, [therapy provider] has done nothing to offer a transition plan or alternative forms of support.” and “This is a wonderful idea to survey parents during this difficult time. Thank you.”
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
The authors wish to acknowledge the wonderful families across Michigan who took the effort to respond to the survey in a time of great uncertainty and to the Western Michigan University Homer Stryker M.D. School of Medicine Institutional Review Board for guidance.
Authors Contribution
All authors conceived of the study, participated in its design and coordination, and drafted the manuscript; JM also participated in the collection and interpretation of the data and JB performed the statistical analysis. All authors read and approved the final manuscript.
Funding
No grants or other financial support was obtained for this study.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The research behind this manuscript did involve human subjects (survey design) and all procedures were approved by the Western Michigan University Homer Stryker M.D. School of Medicine Institutional Review Board (IRB). Appropriate consent language was included in communicating with subjects and no requirement of documentation of informed consent was deemed necessary by the IRB since the study was considered “no more than minimal risk” to participants.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders (DSM-5) Arlington, VA: American Psychiatric Pub; 2013. [Google Scholar]
- Autism Alliance of Michigan. 2020. MiNavigator Program. Retrieved June 12, 2020, from https://autismallianceofmichigan.org/project/minavigator/
- Bonis S. Stress and parents of children with autism: a review of literature. Issues in Mental Health Nursing. 2016;37(3):153–163. doi: 10.3109/01612840.2015.1116030. [DOI] [PubMed] [Google Scholar]
- Colizzi M, Sironi E, Antonini F, Ciceri ML, Bovo C, Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: an online parent survey. Brain Sciences. 2020;10(6):341. doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Addendum to Motherly’s 2019 State of Motherhood survey. (2020). www.motherly.com
- Fitzgerald M, Birkbeck G, Matthews P. Maternal burden in families with children with autistic spectrum disorder. Irish Journal of Psychological Medicine. 2002;33(1):2–17. [Google Scholar]
- Hall HR, Graff JC. The relationships among adaptive behaviors of children with autism, family support, parenting stress, and coping. Issues in Comprehensive Pediatric Nursing. 2011;34(1):4–25. doi: 10.3109/01460862.2011.555270. [DOI] [PubMed] [Google Scholar]
- Harper A, Dyches TT, Harper J, Roper SO, South M. Respite care, marital quality, and stress in parents of children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2013;43(11):2604–2616. doi: 10.1007/s10803-013-1812-0. [DOI] [PubMed] [Google Scholar]
- Hayes SA, Watson SL. The impact of parenting stress: a meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders. 2013;43(3):629–642. doi: 10.1007/s10803-012-1604-y. [DOI] [PubMed] [Google Scholar]
- Hume, K., Waters, V., Sam, A., Steinbrenner, J., Perkins, Y., Dees, B., & et al. (2020). Supporting individuals with autism through uncertain times. https://afirm.fpg.unc.edu/supporting-individuals-autism-through-uncertain-times
- Johns Hopkins University Center for Systems Science and Engineering. (2020). Coronavirus COVID-19 global cases. https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
- Kenyon C. Flattening-the-curve associated with reduced COVID-19 case fatality rates—an ecological analysis of 65 countries. Journal of Infection. 2020;81(1):e98–e99. doi: 10.1016/j.jinf.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan MD, Strickland BB, Blumberg SJ, Singh GK, Perrin JM, van Dyck PC. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005–2006. Pediatrics. 2008;122(6):e1149–e1158. doi: 10.1542/peds.2008-1057. [DOI] [PubMed] [Google Scholar]
- Krakovich TM, McGrew JH, Yu Y, Ruble LA. Stress in parents of children with autism spectrum disorder: an exploration of demands and resources. Journal of Autism and Developmental Disorders. 2016;46(6):2042–2053. doi: 10.1007/s10803-016-2728-2. [DOI] [PubMed] [Google Scholar]
- Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- Lindly OJ, Chavez AE, Zuckerman KE. Unmet health services needs among us children with developmental disabilities. Journal of Developmental & Behavioral Pediatrics. 2016;37(9):712–723. doi: 10.1097/DBP.0000000000000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lounds J, Seltzer MM, Greenberg JS, Shattuck PT. Transition and change in adolescents and young adults with autism: longitudinal effects on maternal well-being. American Journal of Mental Retardation: AJMR. 2007;112(6):401–417. doi: 10.1352/0895-8017(2007)112[401:TACIAA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Maenner MJ, Shaw KA, Baio J, Washington A, Patrick M, DiRienzo M, et al. Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR. Surveillance Summaries. 2020;69(4):1–12. doi: 10.15585/mmwr.ss6904a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michigan Autism Legislation PA 99 and PA 100, (2012). https://www.michigan.gov/autism/0,4848,7-294-63681---,00.html
- Narzisi A. Handle the autism spectrum condition during coronavirus (COVID-19) stay at home period: ten tips for helping parents and caregivers of young children. Brain Sciences. 2020;10(4):207. doi: 10.3390/brainsci10040207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Governor Gretchen Whitmer. (2020). Executive Order No. 2020–21. https://www.michigan.gov/whitmer/0,9309,7-387-90499_90705-522626--00.html
- Rivard M, Terroux A, Parent-Boursier C, Mercier C. Determinants of stress in parents of children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2014;44(7):1609–1620. doi: 10.1007/s10803-013-2028-z. [DOI] [PubMed] [Google Scholar]
- Roth BM, Kralovic S, Roizen NJ, Spannagel SC, Minich N, Knapp J. Impact of autism navigator on access to services. Journal of Developmental & Behavioral Pediatrics. 2016;37(3):188–195. doi: 10.1097/DBP.0000000000000261. [DOI] [PubMed] [Google Scholar]
- The White House. (2020). Proclamation on declaring a national emergency concerning the novel coronavirus disease (COVID-19) outbreak. https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/
- Tolbert, J., Hall, C., Orgera, K., Singer, N., Mengistu, S., & Tian, M. (2020). State Data and Policy Actions to Address Coronavirus. https://www.kff.org/coronavirus-covid-19/issue-brief/state-data-and-policy-actions-to-address-coronavirus/
- Vohra R, Madhavan S, Sambamoorthi U, St Peter C. Access to services, quality of care, and family impact for children with autism, other developmental disabilities, and other mental health conditions. Autism. 2014;18(7):815–826. doi: 10.1177/1362361313512902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss JA, Wingsiong A, Lunsky Y. Defining crisis in families of individuals with autism spectrum disorders. Autism. 2014;18(8):985–995. doi: 10.1177/1362361313508024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, Song R. Mental health status among children in home confinement during the coronavirus disease 2019 Outbreak in Hubei Province. JAMA Pediatrics China. 2020 doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.