Abstract
Epithelial ovarian cancer (EOC) is the deadliest gynecological cancer, and the major cause of death is mainly attributed to metastasis. MicroRNAs (miRNAs) are a group of small non-coding RNAs that exert important regulatory functions in many biological processes through their effects on regulating gene expression. In most cases, miRNAs interact with the 3′ UTRs of target mRNAs to induce their degradation and suppress their translation. Aberrant expression of miRNAs has been detected in EOC tumors and/or the biological fluids of EOC patients. Such dysregulation occurs as the result of alterations in DNA copy numbers, epigenetic regulation, and miRNA biogenesis. Many studies have demonstrated that miRNAs can promote or suppress events related to EOC metastasis, such as cell migration, invasion, epithelial-to-mesenchymal transition, and interaction with the tumor microenvironment. In this review, we provide a brief overview of miRNA biogenesis and highlight some key events and regulations related to EOC metastasis. We summarize current knowledge on how miRNAs are dysregulated, focusing on those that have been reported to regulate metastasis. Furthermore, we discuss the role of miRNAs in promoting and inhibiting EOC metastasis. Finally, we point out some limitations of current findings and suggest future research directions in the field.
Keywords: epithelial ovarian cancer, metastasis, microRNAs (miRNAs)
1. Introduction
Ovarian cancer is the fifth leading cause of cancer-related deaths in females [1]. Based on the cell origin where ovarian tumors arise, ovarian cancer is classified into three categories: epithelial, germ cell, and stromal ovarian cancer. Several types of extremely rare ovarian cancer, such as small cell carcinoma and sarcomas, have also been reported [2]. Among them, epithelial ovarian cancer (EOC) accounts for more than 85% of ovarian cancer cases and is responsible for most ovarian cancer-related deaths [3]. EOC is further grouped into five different histological subtypes, including high-grade serous carcinomas (HGSC), low-grade serous carcinomas (LGSC), endometrioid carcinomas (EC), clear cell carcinomas (CCC), and mucinous carcinomas (MC) [3]. Though the morbidity of ovarian cancer is lower than that in endometrial and cervical cancers, it has the highest mortality rate among gynecological cancers [1]. The five-year survival rate of EOC is less than 45% [4], and relapse and poor prognosis occur in 80% of patients with advanced stages [5,6]. EOC is difficult to detect at the early stages as there are no effective screening methods and the presenting symptoms are vague. Therefore, patients are often diagnosed at the advanced stages when the tumor metastasis is already taking place [5].
MicroRNAs (miRNAs) are small non-coding RNAs that regulate gene expression within cells [7,8]. Studies have shown that 30–60% of human protein-coding genes are regulated by miRNAs [9]. Through regulation of the target gene expression, miRNAs are reported to control many biological processes, including proliferation, differentiation, cell cycle progression, apoptosis, and immune response [10]. Aberrant expression of miRNAs is implicated in many diseases, including cancer. Studies have demonstrated that miRNAs are involved in the progression of EOC [11,12]. Their levels are up- or down-regulated in EOC tumors and/or patient plasma samples, and their abnormal expression is highly associated with EOC metastasis [11,13]. In this review, we provide a brief overview of the biogenesis and mechanisms of actions of miRNAs and metastasis in EOC. We then discuss the dysregulation of miRNAs in EOC and the roles of miRNAs in promoting or suppressing cellular processes related to metastasis. Finally, we point out some limitations of current studies and suggest future research directions.
2. Overview of miRNAs
Depending on the genomic location, miRNAs can generally be classified as intragenic or intergenic. Intragenic miRNAs, which account for approximately 50% of the annotated miRNAs in humans, are generated from a host gene, mainly within the introns of protein-coding genes [14]. Expression of intragenic miRNAs is usually coupled with their host genes, while the transcription of intergenic miRNAs is directed by their own promoters [15,16]. However, it has also been reported that some intragenic miRNAs are transcribed independently of their host genes, generating pri-miRNA that also undergoes splicing [17].
The transcription of the primary miRNA (pri-miRNA) by RNA polymerase II is the first step of canonical miRNA biogenesis. Depending on the source of the miRNA, the pri-miRNA may be the mRNA of the host gene or an independent transcription unit, both containing a 5′ m7G cap and a 3′ poly-A tail [18,19]. Subsequently, pri-miRNAs undergo extensive processing within the nucleus. In the canonical pathway, the pri-miRNAs are converted into ~70 nt hairpin miRNA precursors (pre-miRNAs) via the microprocessor complex, which consists of an RNase III endonuclease, DROSHA, and the double-stranded-RNA-binding protein, DGCR8 (DiGeorge syndrome Critical Region 8) [20,21,22]. DGCR8 acts as the regulatory subunit that recognizes specific motifs within pri-miRNAs while DROSHA functions as the catalytic subunit. The pre-miRNA is then exported to the cytoplasm via a member of the nuclear transport receptor family, Exportin 5 (XPO5), together with Ran-GTP [20,23,24]. In the non-canonical pathway, precursor miRNAs are processed independently of the DROSHA/DGCR8 complex in the nucleus and exported outside the nucleus via Exportin 1 [25,26].
In the cytoplasm, the pre-miRNAs are further processed into mature miRNAs by another RNase III endonuclease, Dicer [20,27]. Dicer cleaves pre-miRNA near the terminal loop, resulting in a short, on average 22 nt, RNA duplex [27,28,29]. Two mature miRNAs, originating from the 5′ and 3′ ends of the miRNA duplex and denoted with the postfix -5p and -3p, respectively, can be generated through an unwinding process, guided by Argonaute (AGO) [30,31]. The miRNA duplex is unwound in an ATP-dependent manner and directly interacts with AGO via the 5′ and 3′ nucleotides of the miRNA, creating a stable association [32,33,34]. The strand that is incorporated into the miRNA-induced silencing complex (miRISC) is referred to as the “guide strand” and the other strand, known as the “passenger strand”, is degraded [35,36]. Four AGO proteins (AGO1–4) have been characterized in humans and they are all capable of interacting with miRNAs [37].
In most reported cases, miRNAs repress their target genes at the post-transcriptional level [38]. They bind to partial complementary sequences in the 3′ untranslated region (UTR) of their target mRNAs, called the miRNA response element (MRE), inducing mRNA degradation and inhibiting translation initiation [39]. The AGO-bound miRNA and MRE interactions act as a guide to enable additional miRISC components to regulate target mRNA stability and protein output. GW182, which interacts directly with AGO, is crucial in localizing the poly-A tail of target mRNA to miRISC, as well as in the recruitment of deadenylase and decapping complexes [40]. PAN2/3 and CCR4/NOT deadenylase complexes are recruited via interaction with tryptophan motifs of GW182 [41,42]. Subsequently, mRNA poly(A) deadenylation is initiated by PAN2/3 and completed by CCR4/NOT complexes [41,42], followed by m7G decapping, facilitated by decapping protein 2 (DCP2) and associated proteins [43]. The unstable deadenylated and decapped mRNA can then be degraded by 5′–3′ exoribonuclease 1 (XRN1) [44]. In addition, miRNAs repress the translation initiation process through the release of eukaryotic initiation factors, eIF4A1 and eIF4A2, from the target mRNAs; as such, in some cases, miRNA can affect protein levels while leaving mRNA stability unaffected [45] (Figure 1).
Figure 1.
Biogenesis and functions of miRNA. MicroRNAs (miRNAs) are usually transcribed by polymerase II in the nucleus to generate primary microRNAs (pri-miRNA) transcripts. In the canonical pathway, the maturation of miRNAs is then performed by the microprocessor complex comprising of DROSHA, RNase III, and DCGR8. The microprocessor complex cleaves both strands of pri-miRNAs near the base of the primary stem loop, generating pre-miRNAs. Following cleavage, pre-miRNAs are actively transported from the nucleus to the cytoplasm by the Exportin 5/Ran-GTP complex. In the cytoplasm, RNase III endonuclease Dicer recognizes and cleaves pre-miRNA near the terminal loop, releasing a small RNA duplex. Subsequently, either strand (-5p or -3p) of the miRNA duplex is loaded into an AGO protein to form a miRNA-induced silencing complex (miRISC). Functionally, miRNAs direct the miRISC complex to target genes and modulate its expression by promoting either mRNA degradation and/or translation inhibition in the cytoplasm. The AGO protein of miRISC complex binds GW182 family proteins, which serve as scaffolds for multiple proteins including PAN2/3, and CCR4-NOT complexes. While the miRISC complex hinders the binding of eIF4F complex, PAN2/3 and CCR4-NOT mediate the poly(A) deadenylation of target mRNAs. The target mRNA is further decapped by a decapping complex and subjected to degradation via the exoribonuclease XRN1. In addition, the miRISC complex can be transported into the nucleus via Importin 8/RAN-GTP complex and binds to target gene promoters to regulate its transcription.
More recently, it has been shown that miRNAs have binding sites on other regions of the mRNAs, including coding regions and 5′ UTR, or on DNA promoter regions [46]. Interestingly, it was found that the binding of miRNA to the coding regions or 5′ UTR of mRNA exerts a silencing effect on gene expression while the interaction of miRNA with the promoter region could induce transcription [47,48,49]. Conversely, there is some evidence supporting miRNAs’ role in promoting translation under specific conditions [50,51].
3. Ovarian Cancer Metastasis
Metastasis is a complex multistep process in which cancer cells disseminate from primary tumors and start new tumors at different sites in the body. This process is regulated by a specific set of genes and signaling pathways. EOC cells mainly metastasize through the transcoelomic pathway [52], in which cells disseminate from the primary EOC tumor by undergoing epithelial-to-mesenchymal transition (EMT) [52] and float freely as spheroids in the ascitic fluid within the peritoneal cavity. The metastatic cells then attach onto the mesothelium lining or invade deeper into the peritoneal organs [53]. In addition, metastatic ovarian cancer cells can transit in the blood or lymph vessels and undergo extravasation to establish new tumors in hematogenous and lymphatic metastasis [53,54]. EOC metastasis to secondary sites accounts for approximately 90% of all ovarian cancer deaths [53]. Therefore, understanding the underlying mechanisms of EOC metastasis could lead to the development of more effective therapeutic tools.
EMT is a biological process which is activated during normal embryonic and organ development, as well as tissue repair [55]. The role of EMT in tumor metastasis has been established in many types of cancers, including EOC [56,57,58]. In EMT, epithelial cells undergo phenotypic alterations through the loss of cell polarity, cell–cell attachment, and gain mesenchymal phenotypes, such as fibroblastoid morphology with increased migratory and invasive properties. EMT is a critical step in ovarian cancer metastasis [59]. Downregulation of epithelial cadherin (E-cadherin, CDH1) and upregulation of mesenchymal neural cadherin (N-cadherin, CDH2) are key elements of EMT. E-cadherin is a transmembrane glycoprotein that associates with β-catenin at the adherens junctions [59]. Loss of E-cadherin results in the destabilization of adherens junctions, promoting cell migration, invasion, and metastasis. E-cadherin expression is repressed directly by many transcription factors, including Snail (SNAI1), Slug (SNAI2), and zinc finger E-box binding homeobox (ZEB)1 and ZEB2, and indirectly by TWIST and TCF4 [60,61]. In addition, Vimentin (VIM), a component of intermediate filaments, is abundantly expressed in mesenchymal cells [62] and exerts inhibitory effects on E-cadherin expression, and cell–cell adhesion, while promoting cell migration and invasion [63]. Therefore, Vimentin is not only an EMT marker but also directly promotes EMT in EOC.
In EOC, EMT is induced by several signaling pathways, including transforming growth factor- β (TGF-β)/Smads, Wnt/β-catenin, PI3K/AKT, Hedgehog, Sonic, and Notch [64]. Wnt signaling promotes the localization of β-catenin into the nucleus, which, in turn, interacts with T-cell factors (TCF/LEF) to regulate transcription [65]. The pathway inhibits E-cadherin by promoting the expression of E-cadherin repressors, such as Snail, Slug, and TWIST [65,66]. TGF-β also enhances EMT through its downstream mediators, SMAD2, SMAD3, and SMAD4 [67]. In addition, the MAPK and PI3K/AKT pathways, activated by many growth factors, or through cross-talks with other signaling molecules, also play critical roles in promoting EMT. For example, epidermal growth factor (EGF) signals through the ERK1/2 and PI3K/AKT pathways to induce EMT [68]. Hepatocyte growth factor (HGF) acts through its receptor, c-Met, and enhances EMT by activating multiple signaling pathways, including MAPK, Wnt/β-catenin, and PI3K/AKT [69,70,71]. Hedgehog glioma-associated oncogene1 (Shh-Gli1) positively regulates EMT via crosstalk with PI3K-AKT [72]. In addition to functions in mitotic progression, Aurora kinase A (AURKA) has been reported to regulate EOC cell migration and invasion in vitro and in vivo [73]. Treatments with AUKA inhibitors, such as alisertib, inhibited migration, adhesion, and EMT via the PI3K/AKT/mTOR- and Sirtuin-1-mediated pathways [73,74], suggesting a potential therapeutic advancement in controlling EOC dissemination. Finally, focal adhesion kinase (FAK) is an important component of various pro-metastatic signaling pathways which promote cancer metastasis, including cell motility [75], cell survival [76,77], invasion [78,79], and EMT [80]. Increased FAK levels are found in several cancers, including EOC [79,80]. In addition, FAK activation, which is determined by p-FAK, increases with tumor progression [80].
Actin filament dynamics are regulated strictly to maintain cell shape and control cell motility [53]. The increase in EOC cell mobility is mediated by actin filament remodeling via the activation of GTPase signaling pathways. For example, GTPase RAP1B has been reported to activate Src and JNK to facilitate integrin-mediated actin remodeling and thereby promote metastasis [81]. DAAM1, which is upregulated in EOC tumors, activates RHOA, induces the formation of microfilaments, and promotes cell migration and invasion [82]. In addition, Lim kinase 1 (LIMK1), a member of serine-threonine protein kinases that acts downstream of RHO GTPase signaling, also participates in actin remodeling in EOC [83]. LIMK1 is a key player in the reorganization of the actin cytoskeleton by inactivating actin-binding factor cofilin through phosphorylation [84]. LIMK1 protein levels are upregulated in EOC and correlated with poor differentiation [83]. In addition, knockout of LIMK1 inhibited migration and invasion of EOC cells [83], supporting its role in promoting EOC cell mobility.
Most EOC metastasis occurs in the peritoneal cavity. Once escaping the primary site, ovarian tumor cells transit in the ascitic fluid as single cells or aggregated cells, referred to as spheroids, and exhibit cancer stem-like properties [85,86]. Cancer cells then adhere to the mesothelium lining of the peritoneum through the binding of integrin receptors to the extracellular matrix (ECM) elements of the mesothelial cells [53]. The integrin-ECM interaction was suggested to activate integrin-linked kinase (ILK) through phosphorylation, promoting a phosphorylation cascade of a variety of ILK-intracellular substrates, including protein kinase B (PKB/AKT), glycogen synthase kinase-3 (GSK-3), and myosin light chain at focal adhesions, and promoting cell adhesion and invasion to the mesothelium [87]. In addition, ovarian tumor cells increase the production of proteolytic enzymes, such as matrix metalloproteases (MMPs), which recognize and degrade ECM elements, enhancing invasive behavior. MMPs play a role in EMT and they are also activated by genes and signaling pathways that induce EMT [88]. In EOC, it has been reported that knockdown of SNAI1 reduced MMP2 but upregulated its inhibitor, TIMP2, suggesting that Snail induces MMP activity [89]. Moreover, EOC cells avoid apoptosis while detaching from primary sites and circulating in ascites or transiting to a distant location by resisting anoikis, a programmed cell death which is activated to inhibit anchorage-independent growth or cell adhesion to an inappropriate matrix [90]. Among steps that occur in cancer metastasis, escaping apoptosis is critical in tumor development and metastasis [91].
Interaction between cancer cells and the tumor environment also plays a role in metastasis. Hypoxia is commonly observed in fast-growing tumors with an insufficient supply of oxygen. Under hypoxic conditions, the association of stabilized hypoxia-inducible factor (HIF)-1α and HIF-2α [92] with HIF-1β induces the expression of downstream target genes that are involved in cell invasion, and metastasis [93]. LOX, one of the target genes induced by HIF-1 complex, has been shown to cross-link collagen and provide a linear track for cell migration [94,95]. In addition, HIF-1 complex modulates the downregulation of DMN2, resulting in decreased endocytosis, an energy-consuming cellular process [94]. Hypoxia has also been reported to down-regulate BRCA1 expression via Retinoblastoma-associated protein E2F transcription factor and suppresses homologous recombination in hypoxic cancer cells, potentially increasing genomic instability [96,97]. Furthermore, the behaviors of metastatic EOC cells are influenced by secreted factors residing in ascites. Cytokine CXCL12 and hyaluronic acid in ascitic fluid have been demonstrated to interact with CXCR4 and CD44 receptors on EOC cell surface respectively, stimulating cell migration, angiogenesis, and localization to the peritoneal surface [53,98,99,100].
Lastly, the metastasis of EOC cells is enhanced by an immunosuppressive microenvironment. Tumor-infiltrating lymphocytes (TILs), such as T cells, B cells, macrophages, and natural killer cells, were also found to be present in ascites and pelvic peritoneal biopsies of advanced ovarian cancer patients [101]. Among them, tumor-associated macrophages (TAMs) play a role in the suppression of adaptive immunity. TAMs induced the imbalance of Treg/Th17 and promoted angiogenesis and metastasis via cross-talk with endothelial cells in EOC [102,103]. In addition, TIL-produced cytokines, such as IL-6, IL-10, ARG-1, and CCL-2, have been reported to promote tumor progression and metastasis, and are involved in immune subversion [104,105]. In addition, EOC cells promote immune evasion via downregulating tumor-associated surface ligands. MHC class I chain-related molecules A and B (MICA and MICB) are widely expressed on epithelial tumor cells and targeted by cytotoxic lymphocytes such as CD8+ T cells and natural killer (NK) cells [106]. Downregulation and internalization of MICA/B have been reported in EOC [106,107], allowing EOC malignant cells to escape immune surveillance.
4. Dysregulation of miRNA Expression in Ovarian Cancer
The expression of miRNAs is highly specific to cell types and developmental stages [108,109]. However, aberrant expression of miRNAs is commonly observed in EOC and associates with its progression [59]. Many miRNAs have been identified to be differentially expressed in EOC. These changes in miRNA abundance are often associated with alterations in cell migration, invasion, and metastasis, as listed in Table 1. Abnormal levels of miRNAs have been detected in tumor tissues, plasma, urine, and/or ascitic fluids. Such dysregulation can be attributed to alterations in DNA copy number, epigenetic regulation, and miRNA biogenesis.
Table 1.
Metastasis-related miRNAs in epithelial ovarian cancer (EOC).
| miRNA/ miRNA Family |
Altered Expression in EOC and Clinical Significance | Target Gene | In Vitro/In Vivo Effects | Citations |
|---|---|---|---|---|
| Pro-Metastatic miRNAs | ||||
| miRNAs upregulated in tumor tissues | ||||
| miR-19a | Upregulated in metastatic HGSC tissues compared to normal ovarian tissues | ND | ND | [134] |
| miR-182 | Upregulated in HGSC tissues compared to fallopian tube tissues | MTSS1 | Promotes cell invasion in vitro, and tumor growth and metastasis in vivo | [135,136] |
| miR-328-3p | Upregulated in cancer stem-like cells isolated from HGSC tissues compared to bulk cancer cells | DDB2 | Increases ALDH+ population and promotes spheroid formation and CSC properties in vitro and tumor growth and metastasis in vivo | [137] |
| miR-130a | Upregulated in HGSC tissues compared to normal fallopian tube tissues | TSC1 | Promotes cell proliferation, invasion, and EMT and tumor growth and metastasis in vivo | [138] |
| miR-301b-3p | Upregulated in HGSC tissues compared to paired adjacent normal tissues; positively correlated with tumor stage, lymph node metastasis, and poor survival | CPEB3 | Promotes cell migration and invasion in vitro | [139] |
| miR-520h | Upregulated in EOC tissues compared to benign ovarian tumors and highest in HGSC compared to MC, EC, and CCC subtypes; correlated with tumor stage, increased ascites, lymph node metastasis, and poor survival | SMAD7 | Promotes cell proliferation, invasion, and EMT in vitro and tumor growth and metastasis in vivo | [130] |
| miR-21 | Upregulated in serous EOC, EC, and MC tissues compared to ovarian cysts and normal ovarian tissues; positively correlated with tumor stage and lymph node metastasis | ND | Promotes cell proliferation, migration, and invasion in vitro | [140] |
| miR-205 | Upregulated in EC subtype compared to normal endometrial tissues | ESRRG | Promotes cell proliferation, migration, and invasion in vitro | [141] |
| miR-146a | Upregulated in omental metastatic serous EOC tumors compared to primary EOC tumors | ND | Promotes spheroid formation and cisplatin resistance in vitro | [133] |
| miR-551b | Upregulated in recurrent serous EOC tissues compared to primary EOC tumors; associated with advanced stage |
FOXO3
TRIM31 |
Promotes cell proliferation, invasion, and colony formation in vitro and tumor burden in vivo | [142] |
| miR-551b-3p | Upregulated in HGSC tissues compared to normal ovarian tissues; associated with poor outcome | STAT3 promoter | Promotes cell proliferation, spheroid formation, and survival in vitro and tumor burden in vivo | [143] |
| miR-18b | Upregulated in EOC tissues compared to normal ovarian tissues; positively correlated with tumor grade and lymph node metastasis | PTEN | Promotes cell migration and invasion in vitro | [144] |
| miR-19b | Upregulated in EOC tissues compared to matched non-tumor tissues; positively correlated with tumor stage and lymph node metastasis | PTEN | Promotes cell migration and invasion in vitro | [145] |
| miR-23a | Upregulated in EOC tissues compared to adjacent normal tissues | DLG2 | Promotes cell proliferation, migration, and invasion in vitro and tumor growth in vivo | [146] |
| miR-181a | Upregulated in recurrent EOC tissues compared to primary EOC tissues; associated with poor survival | SMAD7 | Promotes cell migration, invasion, survival, and EMT in vitro and tumor growth and metastasis in vivo | [110] |
| miR-181b | Upregulated in EOC tissues compared to normal ovarian tissues | LATS2 | Promotes cell proliferation and invasion in vitro | [147] |
| miR-182-5p | Upregulated in EOC tissues compared to non-tumor ovarian tissues | FOXF2 | Promotes cell proliferation, and invasion in vitro and tumor growth in vivo | [148] |
| miR-194 | Upregulated in EOC tissues compared to normal ovarian epithelium tissues | PTPN12 | Promotes cell proliferation, migration and invasion in vitro | [149] |
| miR-196a | Upregulated in EOC compared to paired normal ovarian tissues; positively correlated with tumor stage, and lymph node metastasis | ND | ND | [150] |
| miR-205 | Upregulated in EOC tissues compared to normal ovarian tissues; correlated with tumor stage and poor survival |
TCF21
PTEN SMAD4 |
Promotes cell proliferation, migration, and invasion in vitro and tumor growth and metastasis in vivo | [151,152,153] |
| miR-216a | Upregulated in EOC tissues compared to normal ovarian tissues; correlated with tumor stage, lymph node metastasis, and poor survival | PTEN | Promotes cell migration and invasion and EMT in vitro | [154] |
| miR-552 | Upregulated in EOC tissues compared to paired non-tumor tissues; associated with metastasis, recurrence, and poor survival | PTEN | Promotes cell proliferation, migration, and invasion in vitro | [155] |
| miR-616 | Upregulated in EOC tissues compared to adjacent non-tumor tissues; associated with metastasis, tumor stage and grade, and poor survival | TIMP2 | Promotes cell migration, invasion, and EMT in vitro and metastasis in vivo | [111] |
| miR-630 | Upregulated in EOC tissues with high levels of hypoxia compared to low levels of hypoxia; associated with poor survival | DICER1 | Promotes cell migration, invasion, and EMT in vitro and tumor growth and metastasis in vivo | [156] |
| miR-939 | Upregulated in EOC tissues compared to matched adjacent normal tissues | APC2 | Promotes cell proliferation, colony formation, cell migration, invasion, and EMT in vitro | [157,158] |
| miRNAs upregulated in secreted exosomes and circulating body fluids | ||||
| miR-376a | Upregulated in EOC tissues compared to paired adjacent normal tissues and in blood samples of EOC patients compared to healthy controls; associated with advanced stages |
KLF15
CASP8 |
Promotes cell proliferation, migration, and invasion in vitro and tumor growth in vivo | [125] |
| miR-590-3p | Upregulated in EOC tissues compared to normal ovarian tissues, and in plasma of EOC patients compared to those with benign gynecologic disorders; correlated with tumor grade |
FOXA2
FOXO3 CCNG2 |
Promotes colony and spheroid formation, cell migration, and invasion in vitro and tumor burden in vivo | [112,159] |
| miR-29-3p | Upregulated in exosomes secreted by M2 macrophages compared to those derived from THP-1 cells; associated with poor survival | STAT3 | Promotes Tregs/Th17 imbalance in vitro and tumor growth and metastasis in vivo | [102] |
| miR-30a-5p | Upregulated in urine samples of serous EOC patients compared to healthy controls and higher in stage I/II compared to stage III/V; associated with lymphatic metastasis | ND | Promotes cell proliferation and migration in vitro | [160] |
| miR-149-3p | Upregulated in peritoneal exosomes of EOC patients compared to healthy controls; associated with poor survival | ND | ND | [129] |
| miR-222-5p | Upregulated in peritoneal exosomes of EOC patients compared to healthy controls; associated with poor survival | ND | ND | [129] |
| Anti-Metastatic miRNAs | ||||
| miRNAs down-regulated in tumor tissues | ||||
| miR-145 | Downregulated in HGSC compared to normal FT tissues |
MTDH
TWIST SOX9 HMGA2 |
Inhibits cell proliferation, invasion, migration, EMT, and spheroid formation in vitro and tumor growth and metastasis in vivo | [161,162,163] |
| miR-509-3p | Positively associated with survival in HGSC | YAP1 | Inhibits cell invasion, migration, and spheroid formation in vitro | [164] |
| miR-1236-3p | Downregulated in HGSC tissues compared to normal FT tissues | ZEB1 | Inhibits cell invasion, migration, and EMT in vitro | [165] |
| miR-574-3p | Decreased in EOC tissues compared to normal ovarian tissues, significantly lower in serous EOC tissues compared to non-serous EOC tissues; negatively associated with tumor stage | EGFR | Inhibits cell invasion and migration in vitro | [166] |
| miR-25 | Downregulated in integrated mesenchymal EOC subtype compared to epithelial EOC subtype based on TCGA database | SNAI2 | Inhibits cell invasion, migration, and EMT in vitro and tumor growth and metastasis in the orthotopic xenograft mouse model | [167] |
| miR-101 | Decreased in integrated mesenchymal OC subtype compared to integrated epithelial OC subtype from TCGA database |
ZEB1
FN1 |
Inhibits cell invasion, migration, and EMT in vitro and tumor growth and intraperitoneal metastasis in vivo | [168,169] |
| miR-7 | Downregulated in metastatic EOC tissues from omentum or peritoneum compared to primary EOC tissues; associated with metastasis | EGFR | Inhibits cell invasion, migration, and EMT in vitro | [68] |
| miR-17-5p | ND |
ITGA5
ITGB1 |
Suppresses cell adhesion and invasion in vitro and peritoneal metastasis in vivo | [170] |
| miR-106b | Decreased in EOC tissues compared to normal ovarian tissues and benign tumors; negatively associated with tumor stage and grade | RHOC | Inhibits cell proliferation, invasion, and migration in vitro and tumor growth in vivo | [171] |
| miR-23b | Decreased in EOC tissues compared to normal ovarian tissues and benign tumors | CCNG1 | Inhibits cell proliferation, invasion, and migration in vitro and tumor growth in vivo | [172] |
| miR-26b | Downregulated in EOC tissues compared to normal ovarian surface epithelial tissues; inversely correlated with stage and grade, and higher risk with distant metastasis, recurrence, and poor survival | KPNA2 | Inhibits cell proliferation, migration, spheroid formation, and EMT in vitro and tumor growth and lung metastasis in vivo | [131,132] |
| miR-29c-3p | Downregulated in EOC tissues compared to normal ovarian tissues | ND | Inhibits cell proliferation, invasion, migration, and EMT in vitro | [173] |
| miR-32 | Downregulated in EOC tissues compared to adjacent normal tissues and in recurrent EOC tissues compared to primary tumors | BTLA | Inhibits cell proliferation, migration, and invasion in vitro | [174] |
| miR-34a | Downregulated in EOC tissues compared to paired adjacent normal ovarian tissues; negatively associated with late stage | SNAI1 | Inhibits cell invasion, EMT, spheroid formation, and apoptosis in vitro | [175] |
| miR-100 | Downregulated in EOC tissues compared to matched adjacent normal ovarian tissues; negatively associated with advanced stage, lymph node metastasis, and poor survival | PLK1 | Inhibits cell proliferation in vitro | [176] |
| miR-124 | Downregulated in EOC tissues compared to normal ovarian tissues, and lower in metastatic EOC tissues compared to primary EOC tissues |
SPHK1
PDCD6 |
Inhibits cell proliferation, colony formation, cell invasion, and migration in vitro | [117,177] |
| miR-130b | Downregulated in EOC tissues compared to adjacent non-tumor tissues |
ZEB1
STAT3 |
Inhibits cell invasion, migration, and EMT in vitro | [178] |
| miR-133a | Downregulated in EOC tissues compared to normal ovarian tissues; negatively associated with late stage and lymph node metastasis | ND | Inhibits cell proliferation, invasion, and migration and induces apoptosis in vitro | [179] |
| miR-133a-3p | Downregulated in EOC tissues compared to adjacent non-tumor tissues | ND | Inhibits cell proliferation, invasion, and EMT in vitro | [180] |
| miR-133b | Downregulated in EOC tissues compared to normal ovarian epithelial tissues and benign ovarian cyst tissues; negatively associated with tumor grade and lymph node metastasis | CTGF | Inhibits cell invasion, migration, and EMT in vitro | [181] |
| miR-135a | Downregulated in EOC tissues compared to ovarian cystadenomas; negatively associated with stage, lymph node metastasis, and poor survival | HOXA10 | Inhibits cell proliferation and adhesion and promotes apoptosis in vitro | [182] |
| miR-135a-3p | Downregulated in EOC tumors compared to paired adjacent non-tumor tissues; negatively correlated with advanced stage and poor OS | CCR2 | Inhibits cell proliferation, migration, invasion, and EMT in vitro and tumor growth and lung metastasis in vivo | [183] |
| miR-137 | Downregulated in EOC tissues compared to paired adjacent tissues | SNAI1 | Inhibits cell invasion, spheroid formation, and EMT in vitro | [175] |
| miR-138 | Downregulated in EOC tissues compared to contralateral normal ovarian tissues; negatively associated with lymph node metastasis |
SOX4
HIF1A SOX12 LIMK1 |
Inhibits cell proliferation and invasion in vitro and tumor metastasis in the orthotopic xenograft mouse model | [83,184,185] |
| miR-139 | Downregulated in EOC tissues compared to paired adjacent normal tissues | HDGF | Inhibits cell proliferation, migration, and invasion in vitro | [186] |
| miR-139-3p | Downregulated in EOC compared to adjacent normal ovarian; negatively associated with advanced stage, lymph node metastasis, and poor survival | ELAVL1 | Inhibits cell proliferation, colony formation, invasion, and migration in vitro and tumor growth and lung metastasis in vivo | [187] |
| miR-139-5p | Downregulated in EOC tissues compared to precancerous tissues; negatively associated with stage, lymph node metastasis and poor survival | ROCK2 | Inhibits cell proliferation, colony formation, migration, and invasion in vitro and tumor growth in vivo | [188,189] |
| miR-145-5p | Downregulated in EOC tissues compared to paired adjacent normal ovarian tissues | SMAD4 | Inhibits cell proliferation and migration and promotes apoptosis in vitro | [190] |
| miR-148a-3p | Downregulated in EOC tissues compared to adjacent non-tumor tissues | ROCK1 | Inhibits cell proliferation, invasion, and migration in vitro, as well as tumor growth in vivo | [114] |
| miR-152 | Downregulated in EOC tissues compared to paired adjacent normal ovarian tissues |
ADAM17
WNT1 ERBB3 |
Inhibits cell proliferation, invasion, migration, and EMT in vitro | [178,191] |
| miR-150 | Downregulated in EOC tissues compared to normal ovarian tissues; negatively correlated with advanced tumor stage and grade and poor survival | ZEB1 | Inhibits cell proliferation, invasion, migration, EMT, and spheroid formation in vitro | [133,192] |
| miR-186 | Downregulated in cisplatin-resistant EOC cells compared to cisplatin-sensitive EOC cells; decreased expression is associated poor OS | TWIST1 | Inhibits cell proliferation, invasion, migration, and EMT in vitro and tumor growth and EMT in vivo | [193] |
| miR-193b | Downregulated in EOC compared to matched adjacent normal ovarian tissues and in omental metastasis compared to paired adjacent normal omentum; negatively correlated with stage, grade, ascites, lymph node metastasis, tumor size, and poor survival | uPA | Inhibits cell adhesion, proliferation, colony formation, invasion and migration in vitro, and inhibits tumor growth and metastasis in the orthotopic xenograft mouse model | [194,195] |
| miR-199a-5p | Downregulated in EOC cells under hypoxia compared to in normoxic condition |
HIF1A
HIF2A |
Inhibits cell migration in vitro and inhibits tumor growth and peritoneal seeding in vivo | [94] |
| miR-202-5p | Downregulated in EOC tissues compared to paired adjacent normal ovarian tissues; positively associated with patient survival | HOXB2 | Inhibits cell proliferation, invasion, migration, and EMT in vitro | [196] |
| miR-206 | Downregulated in EOC tissues compared to noncancerous glioma tissues; negatively associated with lymph node and distant metastasis |
c-MET
CCND1 CCND2 |
Suppresses cell proliferation, migration, and invasion in vitro | [197,198] |
| miR-208a-5p | Downregulated in metastatic EOC tissues compared to nonmetastatic EOC tissues | DAAM1 | Inhibits cell invasion, migration, and microfilaments formation in vitro | [82] |
| miR-215 | Downregulated in EOC tissues compared to adjacent normal; negatively associated with stage and lymph node metastasis | NOB1 | Inhibits cell proliferation, colony formation, migration, and invasion in vitro and tumor growth in vivo. | [199] |
| miR-217 | Downregulated in EOC tissues compared to paired adjacent normal ovarian tissues; negatively associated with stage, histological grade, and lymph node metastasis |
IGF1R
IL6 |
Inhibits cell proliferation, colony formation, invasion, and migration, and reduces M0 macrophages differentiation in vitro and tumor growth in vivo | [105,200] |
| miR-218 | Downregulated in EOC tissues compared to adjacent normal; negatively associated with stage and lymph node metastasis | RUNX2 | Inhibits cell proliferation, colony formation, invasion, and migration in vitro and tumor growth in vivo | [201] |
| miR-219-5p | Decreased in EOC tissues compared to adjacent normal tissues |
TWIST1
HMGA2 |
Inhibits cell proliferation, invasion, and migration in vitro and tumor growth in vivo | [202,203] |
| miR-335 | Downregulated in EOC tissues compared to normal ovarian tissues, in omental metastatic tissues compared to primary tumors; negatively associated with poor survival and recurrence | ND | ND | [204] |
| miR-338-3p | Downregulated in EOC tissues compared to normal fallopian samples based on TCGA database; negatively associated with stage, grade, and metastasis |
MACC1
RUNX2 |
Inhibits cell proliferation, colony formation, invasion, migration, and EMT in vitro and tumor growth and metastasis in vivo | [70,205,206] |
| miR-340 | Downregulated in EOC tissues compared to normal adjacent ovarian |
FHL2
NFKB1 |
Inhibits cell proliferation, invasion, and migration in vitro and tumor growth and intraperitoneal metastasis in vivo | [207,208] |
| miR-363 | Downregulated in EOC compared to paired adjacent normal ovarian tissues; negatively associated with advanced stage, lymph node metastasis, and poor prognosis | NOB1 | Inhibits cell proliferation, colony formation, invasion, and migration in vitro and tumor growth in vivo | [209] |
| miR-365 | Downregulated in EOC tissues compared to adjacent normal ovarian tissues; negatively associated with stage, grade, and lymph node metastasis | WNT5A | Inhibits cell proliferation, colony formation, invasion, migration, and EMT in vitro, and tumor growth in vivo | [210] |
| miR-373 | Downregulated in EOC tumors compared to benign epithelial ovarian tumors | RAB22A | Inhibits cell invasion, migration and EMT in vitro and peritoneal metastasis in vivo | [211,212] |
| miR-375 | Downregulated EOC tissues compared to normal ovarian tissues | YAP1 | Inhibits cell proliferation, invasion, migration, and EMT in vitro and tumor growth, metastasis, and EMT in vivo | [115] |
| miR-377 | Downregulated in EOC tissues compared to adjacent normal ovarian tissues; positively correlated with survival | CUL4A | Suppresses cell proliferation, invasion, migration, and EMT in vitro | [213] |
| miR-494 | Downregulated in EOC tissues compared to normal adjacent tissues; negatively associated with stage, tumor size, and lymph node metastasis | SIRT1 | Inhibits cell proliferation, invasion, and migration in vitro | [214] |
| miR-378g | Downregulated in EOC tissues compared to normal ovarian tissues | CHI3L1 | Inhibits cell proliferation, migration, and TGF-β1-induced EMT in vitro | [215] |
| miR-421 | ND | PDGFRA | Inhibits cell proliferation, invasion, and tubule formation in vitro, and tumor growth and angiogenesis in vivo | [216] |
| miR-448 | Downregulated in EOC tissues compared to adjacent normal ovarian tissues | CXCL12 | Inhibits cell proliferation, migration and invasion in vitro and tumor growth in vivo | [99] |
| miR-450a | Downregulated in EOC tissues compared to normal ovarian tissues |
TIMMDC1
MT-ND2 ACO2 ATP5B |
Inhibits cell clonogenicity, invasion, migration, and EMT and promotes anoikis in vitro and intraperitoneal tumor growth in vivo | [217] |
| miR-455 | Downregulated in EOC tissues compared to normal adjacent tissues; negatively associated with stage, tumor size, and lymph node metastasis | NOTCH1 | Inhibits cell proliferation and invasion in vitro | [218] |
| miR-489 | Downregulated in EOC tissues compared to normal ovarian tissues; negatively associated with poor survival, stage, grade, lymph node, and distant metastasis | XIAP | Inhibits cell proliferation, invasion, migration and EMT in vitro | [219] |
| miR-497 | Downregulated in EOC tissues compared to normal ovarian tissues; negatively associated with tumor stage, lymph node metastasis, and poor survival | SMURF1 | Inhibition of cell migration and invasion in vitro | [220] |
| miR-503-5p | Downregulated in response to NF-kB pathway activation in SKOV3 cells | CD97 | Inhibits colony formation, migration and invasion in vitro | [221] |
| miR-506 | Decreased expression is associated with stage and poor survival in EOC |
SNAI2
VIM CDH2 |
Inhibits cell invasion, migration, and EMT in vitro, and EMT, tumor growth, and metastasis in the orthotopic xenograft mouse model | [63,222] |
| miR-532-5p | Downregulated in EOC compared to normal ovarian; negatively associated with stage, grade, and distant metastasis | TWIST1 | Inhibits cell proliferation, colony formation, and invasion in vitro | [223] |
| miR-548c | Decreased in EOC tissues compared to normal ovarian tissues; negatively associated with advanced stage and poor survival | TWIST1 | Inhibits cell proliferation, migration, invasion, stemness, and EMT in vitro | [224] |
| miR-584 | Downregulated in EOC tissues compared to paracancerous tissues; negatively associated with distant and lymphatic metastasis and poor survival | LPIN1 | Inhibits cell proliferation, colony formation, and migration in vitro | [225] |
| miR-596 | ND | LETM1 | Inhibits cell proliferation, invasion, and migration in vitro and tumor growth in vivo | [226] |
| miR-612 | Downregulated in EOC tissues compared to matched non-tumor tissues | HOXA13 | Inhibits cell proliferation, invasion, and migration, and promotes apoptosis in vitro | [227] |
| miR-654-3p | Downregulated in EOC cells compared to IOSE80 cells | AKT3 | Inhibits cell invasion, migration and sphere formation in vitro and tumor growth in vivo | [228] |
| miR-665 | Decreased in EOC tissues compared to normal ovarian tissues | HOXA10 | Inhibits cell proliferation and migration in vitro | [229] |
| miR-708 | Downregulated in EOC tissues compared to normal ovarian tissues; negatively associated with stage | RAP1B | Inhibits cell invasion, migration, cell adhesion, and EMT in vitro and tumor growth and metastasis in vivo | [81] |
| miR-874-3p/5p | Downregulated in EOC tissues compared to normal ovarian epithelial tissues | SIK2 | Inhibits cell proliferation, colony formation, invasion, and migration in vitro | [230] |
| miR-936 | Downregulated in EOC tissues compared to adjacent normal tissues; negatively associated with tumor size, stage, and lymphatic metastasis | FGF2 | Inhibits cell proliferation, invasion, and migration in vitro and tumor growth in vivo. | [231] |
| miR-4454 | Downregulated in metastatic EOC tissues compared to primary EOC tissues; positively associated with patient survival |
SPARC
BAG5 |
Inhibits cell proliferation, colony formation, migration, and invasion in vitro, and peritoneal metastasis in vivo. | [232] |
| miR-6089 | Downregulated in EOC tissues compared to paratumor tissues | MYH9 | Suppresses cell proliferation, migration, invasion, and EMT in vitro, and tumor growth and metastasis in vivo | [233] |
| miR-6126 | Downregulated in EOC tissues compared to normal ovarian tissues; inversely correlated with tumor progression and positively associated with survival | ITGB1 | Inhibits cell invasion, migration, and tube formation in vitro and angiogenesis and tumor growth in the orthotopic xenograft mouse model | [234] |
| miRNAs down-regulated in secreted exosomes and circulating body fluids | ||||
| miR-125a | Downregulated in serum of EOC patients compared to healthy controls |
GALNT14
ARID3B |
Inhibits cell proliferation, invasion, and EMT in vitro | [235,236] |
| miR-125b | Downregulated in tissues and serum of EOC patients compared to adjacent normal ovarian tissues and serum of healthy control respectively; negatively associated with stage and lymph node and distant metastasis |
SET
GAB2 |
Inhibits cell invasion, migration, and EMT in vitro and metastasis in vivo | [113,237,238] |
| miR-212 | Downregulated in EOC tissues and serum compared to paired adjacent normal ovarian tissues and healthy controls respectively; negatively correlated with tumor stage and metastasis | HBEGF | Inhibits cell proliferation, invasion, and migration in vitro | [239] |
| miR-122 | Downregulated in serum of serous EOC patients compared to benign controls | P4HA1 | Inhibits cell invasion, migration, and EMT in vitro, and intraperitoneal metastasis in vivo | [127,240] |
| miR-148a | Downregulated in plasma of EOC patients compared to healthy controls; negatively associated with tumor grade, stage, lymph node metastasis, and poor survival | ND | Inhibits cell proliferation, invasion, and migration in vitro | [241] |
| miR-199a | Downregulated in serum of EOC patients compared to normal controls; negatively associated with tumor grade, lymph node and distant metastasis, and poor survival | ND | ND | [128] |
| miRNAs with both pro- and anti-metastatic effects | ||||
| miR-9 | Upregulated in metastatic EOC tissues compared to paired primary EOC tissues | CDH1 | Promotes cell migration, invasion, and EMT in vitro | [242] |
| Downregulated in recurrent serous EOC tissues compared to primary EOC tissues | TLN1 | Inhibits cell proliferation, migration, and invasion in vitro | [243,244] | |
| miR-141 | Upregulated in EOC tissues compared to normal ovarian tissues, and serum of EOC patients compared to healthy controls; positively associated with tumor stage, lymph node metastasis, and poor survival |
KLF12
SIK1 MAPK14 |
Promotes proliferation, anoikis resistance, and survival in vitro, and tumor growth and metastasis in vivo | [126,245,246] |
| Downregulated in integrated mesenchymal subtype of EOC compared to normal ovarian epithelial tissues | ND | Inhibits cell migration, invasion, and EMT in vitro | [222,247] | |
| miR-200a | Upregulated in EOC tumors compared to normal ovarian tissues and in serum of EOC patients compared to healthy controls; positively associated with aggressiveness, late stage, and lymph node metastasis |
PTEN
MAPK14 |
Promotes cell migration and invasion in vitro | [126,246,248] |
| Downregulated in vasculogenic mimicry positive EOC tissues compared to vascular mimicry negative ovarian tissues and in integrated mesenchymal subtype compared to ovarian normal epithelial tissues; negatively associated with stage, ascites, and metastasis and positively correlated with patient survival |
IL8
CXCL1 EPHA2 |
Inhibits tube formation, vasculogenic mimicry, and cell invasion in vitro, and angiogenesis and metastasis in vivo | [222,249,250] | |
| miR-200b | Upregulated serum of EOC patients compared to healthy controls; positively associated with tumor stage, lymph node metastasis, and poor survival | ND | ND | [126] |
| Downregulated in vasculogenic mimicry positive EOC tissues compared to vascular mimicry negative ovarian tissues; negatively associated with stage, ascites, and metastasis and positively correlated with patient survival |
IL8
CXCL1 |
Inhibits tube formation, vasculogenic mimicry, and cell invasion in vitro, and angiogenesis and metastasis in vivo | [249] | |
| miR-200c | Upregulated in SOC tissues and serum of EOC patients compared to heathy controls; associated with tumor stage, lymph node metastasis, and poor survival | ND | ND | [126,251] |
| Upregulated in EOC tumors compared to normal ovarian tissues; inversely associated with tumor stage and lymph node metastasis |
ZEB2
TUBB3 |
Inhibits cell migration and invasion in vitro | [252,253] | |
| miR-203 | Upregulated in EOC tissues compared with adjacent normal tissues | PDHB | Promotes cell proliferation, migration, and glycolysis in vitro, and tumor metastasis in vivo | [118] |
| Downregulated in SOC tissues compared to adjacent normal ovarian tissue; positively associated with patient survival |
SNAI2
BIRC5 |
Inhibits cell proliferation, invasion, migration, and EMT in vitro, and tumor growth in vivo | [119,254] | |
ND: not determined.
4.1. Aberrant Expression of Metastasis-Associated miRNAs in EOC
In EOC tumors compared to normal ovarian tissues, upregulation of miR-181a [110], miR-616 [111] and miR-590-3p [112], and downregulation of miR-125b [113], miR-148a-3p [114], and miR-375 [115] levels have been reported. However, inconsistent findings have also been reported. For example, miR-124-3p, miR-148a-3p, miR-203a, and miR-375 were detected exhibiting differential expression in EOC specimens with both downregulation and upregulation [114,116,117,118,119]. Several other miRNAs listed in Table 1 have also been shown to be either up- or down-regulated in different studies. The reasons for such discrepancies are unclear; however, it may be related to sample size and/or heterogeneity within tumor samples or between different EOC subtypes. In addition, some of these studies did not specify the subtypes of tumors or only used a few tumor samples. Different EOC subtypes have unique origins and specific molecular features and, therefore, it is possible to exhibit different miRNA expression patterns. To date, only a few studies have examined miRNAs in different subtypes of EOC. Using microarray analyses to compare serous, endometrioid, and clear cell tumors with normal ovarian tissues, Iorio et al. (2007) found that while some miRNAs were commonly up- or down-regulated among different subtypes of EOCs, some miRNAs were dysregulated only in a specific subtype [120]. It has also been indicated that miR-510 expression was higher in LGSC and CCC subtypes but lower in HGSC compared to normal ovarian tissues [121]. Choosing proper controls is a challenging task in EOC research. Many researchers used normal ovarian or adjacent non-cancerous tissues as controls. However, it is now believed that the majority of EOCs are originated outside the ovary [3,122]. For example, HGSCs are thought to be derived from fallopian tube (FT) and ovarian surface epithelium while ECs and CCCs are originated from endometriosis [3]. The origin of MCs and LSGCs is still unclear, but they are frequently found to be associated with borderline tumors [3]. Therefore, comparison between tumor tissues and normal ovarian tissues may not provide accurate information about miRNA dysregulation. A recent study compared miRNA expression profiles between endometriosis and EOC tissues and suggested the potential role of miR-93, miR-325, and miR-492 in the malignant transformation of endometriosis to EOC [123]. Further investigation of miRNA expression in different subtypes in comparison with their tissues of origin would provide insights into their diagnostic and/or prognostic significance.
In addition to tumor tissues, the aberrant expression of miRNAs has also been detected in extracellular vesicles, especially exosomes, of EOC patients [124]. Interestingly, malignant cells have been reported to secrete more exosomes when compared with normal cells [124]. Consistent with the dysregulation of miRNA levels found in EOC tissues, miR-590-3p [112] and miR-376a [125] were found to be upregulated in plasma and serum samples of EOC patients, respectively. Expressions of miR-200a [126] and miR-20a [106] were increased while miR-122 [127] and miR-199a [128] expressions were decreased in the serum of EOC patients. Furthermore, upregulation of miR-149-3p and miR-222-5p was detected in peritoneal exosomes which were isolated from ascites of EOC patients [129].
The dysregulation of miRNAs is correlated with EOC pathological features, such as tumor stage, grade, and lymph node and uterus invasion. Levels of miR-520h were gradually increased from stage I to stage III/IV of EOC tumors [130]. Upregulation of miR-520h was associated with increased ascite volumes and poor survival of EOC patients. In contrast, decreased levels of miR-26b were negatively correlated with tumor stage, grade, and ascite volumes [131,132]. In addition, abnormal miRNA levels have been reported to be associated with EOC metastasis. Bioinformatic analysis demonstrated that there was a correlation between downregulation of miR-216 with lymphovascular invasion, upregulation of miR-133a-2, miR-145, and miR-126 with uterus invasion, and upregulation of miR-302c with pelvic peritoneum invasion [120]. Furthermore, analysis from primary and metastatic EOC specimens indicated that downregulation of miR-124-2, miR-125b-1, miR-137, miR-203a, and miR-375 was highly associated with lymph node and distant metastasis [116]. miR-146a [133] and miR-19a [134] were also increased in metastatic EOC tumors comparing to the primary tumors, while miR-7 levels were decreased in metastatic EOC tumors compared to the primary tumors [68]. The upregulation and downregulation of these miRNAs are associated with advanced stage, lymph node metastasis, and survival of EOC patients. Therefore, miRNAs may potentially be used as prognostic biomarkers.
4.2. Dysregulations of miRNAs by Genetic and Epigenetic Alterations
Genetic alteration is one of the mechanisms underlying the dysregulation of miRNAs in cells. Using high-resolution array comparative genomic hybridization (aCGH), Zhang et al. revealed that 37.1% of genomic regions containing miRNA genes showed DNA copy number variations in EOC [255]. Among the miRNA genes analyzed, 21 out of 47 intronic miRNA genes showed high degrees of copy number variations. Further analyses showed that dysregulation of most of these miRNAs was associated with DNA copy number abnormalities [255]. Downregulation of let-7a3 was correlated with a loss of DNA copy number while upregulation of miR-9-1 and miR-213 was associated with a gain of DNA copy number [255]. Similarly, 3q26 amplification has been detected frequently in HGSC [143]. One of the miRNA precursors located in this region, mir-551b, is amplified in 1/3 of HGSC patients. The dominant form of its mature miRNA, miR-551b-3p, is also elevated in HGSC tissues compared to normal ovarian tissue and associated with poor prognosis. Furthermore, 32% of CCC patients showed 17q23-25 amplification which contains mir-21 gene [256]. Although the correlation of 17q23-25 amplification and miR-21 overexpression is low, the presence of 17q23-25 amplification increased miR-21 overexpression in the CCC cases by 25%. These studies suggest that alteration of DNA copy number contributes to the dysregulation of some miRNAs.
Alteration in the methylation of CpG islands in miRNA gene promoters has also been linked to the dysregulation of miRNAs in EOC. Analysis of two datasets from GEO showed that miR-340 was downregulated in EOC tissues [207]. Interrogation of the 2-kb region upstream of mir-340 by EMBOSS in EOC cells revealed three CpG islands. In addition, treatment with methylation inhibitors, 5-Aza-dC or TSA, increased the levels of miR-340 in EOC cells, suggesting that the downregulation of miR-340 is due to hypermethylation of its promoter [207]. Hypermethylation in the CpG islands of multiple miRNA genes, including mir-124a-2, mir-127, mir-125b-1, mir-129-2, mir-137, mir-193a, mir-203a, mir-34b/c, mir-130b, mir-1258, mir-9-1, mir-9-3, mir-107, mir-130b, mir-124-3, mir-339, and mir-375, has also been found in EOC tumors compared to the paired normal ovarian tissues [116,257,258]. A strong correlation between hypermethylation and downregulation in miR-125b-5p, miR-129-5p, miR-132-3p, miR-137, and miR-193a-5p was also observed [116]. Interestingly, hypermethylation of mir-125b-1, mir-137, mir-34b/c, mir-203a, mir-130b, and mir-375 is associated with metastasis [116,257]. Similarly, hypomethylation in mir-21, mir-203, mir-205, and mir-191 promoters has been reported in EOC tissues with the association with their overexpression [116,120]. Thus, hypomethylation and hypermethylation of the promoter regions of miRNA genes play an important role in the aberrant expression of miRNAs.
4.3. Dysregulation of miRNAs by Alteration in miRNA Biogenesis
The first step of miRNA biogenesis is the transcription of the pri-miRNAs. As a consequence, dysregulation of factors that regulate transcription in general may lead to a change in the abundance of mature miRNA. p53, whose mutations occur in 96% of cases of HGSC [259], promotes the expression of miR-145 and miR-34b/c, and mutations of p53 are associated with lower expression of these miRNAs [161,259,260]. In addition, it has been demonstrated that c-Myb binds directly to the promoter of mir-520h to induce its expression [130]. c-Myb has been reported to be upregulated in EOC tissues compared to aged-matched control tissues and activation of TGF-β signaling induced upregulation of c-Myb and miR-520h [130,261]. Similarly, PPARγ response elements (PPRE) have been identified in the mir-125b promoter and activation of PPARγ leads to an increase in miR-125b levels [262]. However, miR-125b is reported to be downregulated [262] while PPARγ is upregulated [263] in EOC tissues compared to normal ovarian tissues. Despite of the upregulation, PPARγ was shown to inhibit proliferation and induce apoptosis by modulating p63 and p73 upregulation [264]. Therefore, it is unclear if PPARγ contributes to the downregulation of miR-125b. On the other hand, several transcription factors have been shown to inhibit miRNA expression. Overexpression of an ETS transcription factor, PEA3, or its activation by EGF signaling, significantly reduced pri-miR-125a and mature miR-125a levels and the binding of PEA3 to the mir-125a promoter has been confirmed by ChIP analysis [236]. Similarly, miR-6089 transcription was found to be directly inhibited by c-Jun which is activated by MYH9 via the Wnt/β-catenin signaling pathway [233]. Aberrant activation of EGFR and Wnt/β-catenin signaling is well documented in EOC [66,265]. Therefore, it is possible that the hyperactivation of these signaling pathways contributes to the downregulation of miR-125a and miR-6089, respectively.
Once transcribed, pri-miRNAs are processed into pre-miRNAs and finally mature miRNAs. These processing events are critical rate-limiting steps that regulate the levels of mature miRNAs within cells [38]. Abnormalities in DNA copy number of DICER1 and AGO2 have been detected in 32.7% and 57.4% of primary EOC tumors, respectively [255]. In addition, single-nucleotide mutations were found in DICER1 and DROSHA genes [266]; however, the functional roles of these mutations are unclear. Lower mRNA levels of DICER and DROSHA were detected in 60% and 51%, respectively, of EOC tumors examined and associated with advanced tumor stage and poor survival of EOC patients [266]. DDX1, an RNA-binding protein that was identified to associate with the microprocessor complex, has been reported to play a key role in miRNA processing [21,267,268]. Low DDX1 expression is significantly associated with poor overall survival of serous EOC [269]. Silencing of DDX1 reduced the levels of mature miR-200a, miR-29c, miR-141, and miR-101 [269]. Interestingly, phosphorylation of DDX1 by the protein kinase Ataxia telangiectasia mutated (ATM) in response to DNA damage enhanced pri-miRNA processing [269]. Dicer, DROSHA, AGO2, and cofactors play critical roles in the controlled expression of mature miRNAs, and their dysregulation can lead to abnormal miRNA levels. Further investigation on the dysregulation of these components and their effects on specific miRNA expression levels would provide an insight into the mechanisms of miRNA dysregulation in EOC.
Single-nucleotide polymorphisms found in miRNAs, referred to as miRSNPs, may also contribute to the alteration of mature miRNA levels. The genetic variant rs11614913 of miR-196a-2 has been detected in multiple cancer types, including gastric [270], head and neck cancer [271], and breast cancer [272]. Genotype distribution analysis of miR-196a-2 polymorphism revealed that CT and CC genotypes are frequently observed in EOC patients [273]. In addition, the recessive genetic model indicated that the risk of EOC is higher in CC genotype carriers compared to the ones carrying wild-type homozygous TT and CT alleles. Furthermore, it was shown that miR-196a-2 rs11614913 influenced the production of mature miR-196a-2. There was a significant upregulation of mature miR-196a-2 detected in the CC genotype compared to the TT genotype of EOC tissue samples [273]. However, a recent study showed no significant difference in the frequency of miR-196a-2 rs11614913 in HGSC patients compared to healthy controls [274]. Therefore, whether miR-196a-2 rs11614913 variant is a risk factor in EOC requires further study.
5. Roles of miRNAs in Ovarian Cancer Metastasis
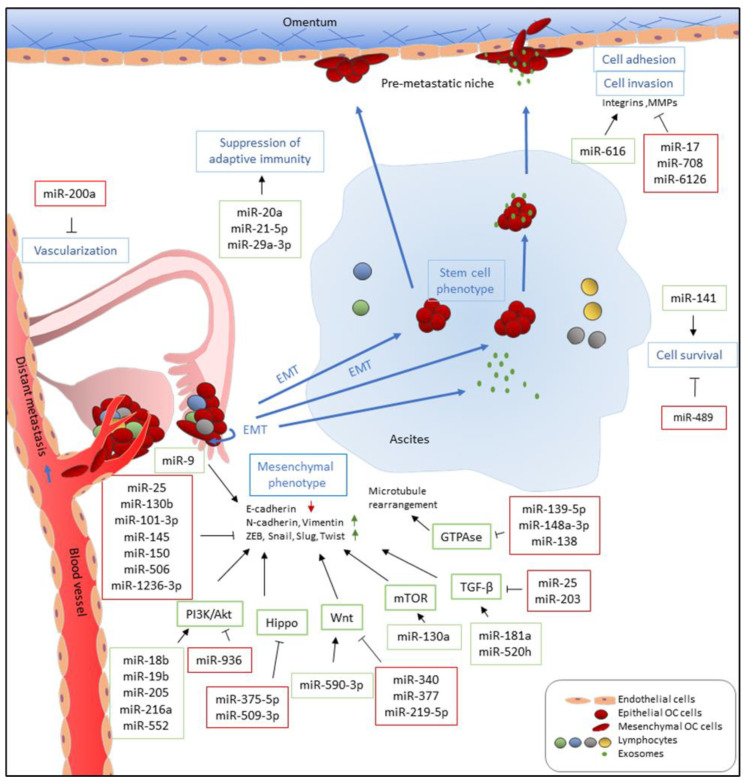
Numerous studies have reported the functions of miRNAs in EMT, cell migration, invasion, and metastasis in EOC. In addition, miRNAs also participate in inducing angiogenesis and modulating tumor microenvironments [102,105,106], which contribute to tumor metastasis (Figure 2). The majority of studied miRNAs exert negative regulatory effects on metastasis, while some miRNAs serve as positive regulators of metastasis. In addition, some miRNAs have been reported to exhibit both pro-metastatic and anti-metastatic effects, probably depending on the genes they targeted under different cancer contexts.
Figure 2.
Functions of miRNAs in EOC metastasis. miRNAs which are upregulated and promote metastasis-related processes are depicted in green boxes while downregulated miRNAs which inhibit metastatic-related processes are listed in red boxes. miRNAs directly and indirectly regulate epithelial-to-mesenchymal transition (EMT) by targeting E-cadherin and E-cadherin repressors, such as ZEB, Snail, Slug, and Twist, and associated signaling pathways. miR-9 directly targets E-cadherin to activate EMT while miR-25, miR-101-3p, miR-130b, miR-145, miR-150, and miR-1236-3b directly inhibit expression of E-cadherin repressors, including ZEB1, SNAI2, and TWIST1. Multiple miRNAs, such as miR-18b, miR-19b, miR-205, miR-216b, and miR-552, promote EMT by targeting PTEN, leading to the activation of the PI3K/AKT pathway. In addition, upregulation of miR-590-3p, miR-130a, miR-181a, and miR-520h induces Wnt, mTOR, and TGF-β signaling, respectively, which are known pathways that promote EMT. In contrast, miR-936, miR-375-5p, miR-509-3p, miR-340, miR-377, miR-219-5p, miR-25, and miR-203 attenuate PI3K/AKT, Hippo, Wnt, and TGF-β signaling pathways and inhibit cell migration, invasion, and EMT. Furthermore, downregulation of miR-139-5p, miR-148a-3p, and miR-138, which has been reported to inhibit ROCKs and LIMK1 expression, increases cell motility via GTPase signaling. Metastatic EOC cells float in ascites as single cells or spheroids which exhibit stem cell-like properties. To survive after detaching from primary site and inside ascites, metastatic EOC cells upregulate miR-141 and downregulate miR-489 to modulate anoikis resistance. In the transcoelomic pathway, EOC metastatic cells then adhere to the mesothelium lining and invade peritoneal organs. Upregulation of miR-616 and downregulation of miR-17 and miR-6126 increase cell adhesion via increased expression and activities of integrins and MMPs which recognize and degrade the extracellular matrix (ECM) of the mesothelial cells, respectively. In addition, downregulation of miR-708 increases focal adhesion formation through promoting focal adhesion kinase (FAK) activities. EOC metastasis occurs in an immune-suppressive environment which are modulated by miRNAs. miR-21-5p and miR-29a-3p promote adaptive immune suppression via upregulation of tumor-associated macrophages (TAMs) and induction Treg/Th17 imbalance while miR-20a downregulates MICA/B to avoid recognition by cytotoxic T-cells. Furthermore, EOC tumors increase vascularization and angiogenesis via downregulation of miR-200a, implicating them in distant metastasis through a perfusion pathway.
5.1. MicroRNAs that Promote Metastasis
Multiple miRNAs have been reported to promote EOC metastasis by targeting CDH1 as well as its associated pathways, such as AKT, TGF-β, and Wnt/β-catenin, to induce EMT. CDH1 is directly inhibited by miR-9, which was found to be upregulated in serous ovarian cancer tissues and cell lines [242]. Overexpression of miR-9 in EOC cells promoted migration and invasion, as well as upregulating the mesenchymal markers, N-cadherin and Vimentin [242]. Furthermore, overexpression of miR-181a enhanced, while inhibition of miR-181a reduced, EMT, migration, invasion, and chemoresistance in vitro by targeting SMAD7, which negatively regulates TGF-β signaling [110]. Injection of miR-181a-overexpressing cells into the ovarian bursa of nude mice resulted in a significant increase in tumor burden and dissemination. These results, together with the findings that miR-181a is enriched in recurrent tumors compared to primary tumors and negatively correlated with patient survival [110], strongly suggest that miR-181a is a key regulator of EOC metastasis. Similarly, miR-520h targets SMAD7, resulting in EMT and tumor growth promotion, as supported by in vitro and in vivo studies [130]. Meanwhile, miR-182 inhibits BRCA1, a tumor suppressor involved in DNA repair, and MTSS1, a metastasis suppressor [275], and upregulates the EMT promoter HMGA2, thus increasing EOC cell invasiveness in vitro and tumor metastasis in vivo [136]. miR-182 was also found to target a transcription factor FOXF2 and to exert promoting effects on EOC cell migration and invasion [148].
PTEN, a tumor suppressor that negatively regulates PI3K/AKT pathway [276], is targeted by several miRNAs that promote metastasis. Specifically, miR-18b [144], miR-19b [145], miR-205 [153], miR-216a [154], and miR-552 [155] have been reported to directly target PTEN and enhance cell migration, invasion, and/or EMT in vitro when these miRNAs are overexpressed, but reduced these properties when endogenous miRNAs were inhibited. In vivo, miR-205 overexpression resulted in the formation of a larger number of intraperitoneal tumors [153]. Other target genes have also been identified for miR-205. In the EC subtype, miR-205 is upregulated in tumors and its overexpression enhances cell migration and invasion by targeting ESRRG [141]. The effect of miR-205 on promoting EOC cell migration and invasion has also been confirmed by other studies [277,278]. miR-130a was discovered to target TSC1, a negative regulator of the mTOR pathway [279], and increased proliferation, invasion, and EMT in vitro, as well as tumor growth and metastasis in vivo [138]. Interestingly, miR-130a is upregulated in HGSC, and, in response to inflammatory stimuli, NFκB binds to the miR-130a promoter to induce its expression [138]. These findings suggest that a mechanism by which inflammation promotes EOC metastasis is to induce miR-130a expression, which, in turn, activates mTOR signaling.
Studies from our lab have shown that miR-590-3p is upregulated in EOC tumor tissues and plasma samples [112]. Overexpression of miR-590-3p promotes, while inhibition of miR-590-3p suppresses, EOC cell proliferation, migration, and invasion, as well as spheroid formation in 3D cultures in vitro [112,159]. Subcutaneous and intraperitoneal injection of EOC cells overexpressing miR-590-3p revealed that miR-590-3p promotes tumor growth and metastasis [112]. We further showed that FOXA2 is a direct target of miR-590-3p, while Versican (VCAN), a proteoglycan commonly overexpressed in cancer, is transcriptionally inhibited by FOXA2. Interestingly, we found that VCAN mRNA levels are positively correlated with vascular and lymphovascular invasion, and that low FOXA2/high VCAN is associated with poor patient survival [112]. In addition to FOXA2, miR-590-3p also targets cyclin G2 (CCNG2) and FOXO3. CCNG2 is an atypical cyclin that negatively regulates cell proliferation [280], migration, invasion, EMT, and tumor metastasis by suppressing Wnt/β-catenin [281]. FOXO3 has been shown to activate CCNG2 transcription in EOC cells [282]. By targeting these two genes, miR-590-3p enhances β-catenin signaling [159]. These findings support the role of miR-590-3p in promoting EOC metastasis.
Matrix metalloproteinases (MMPs) play an important role in cell invasion and metastasis, and their activity is inhibited by tissue inhibitors of MMPs (TIMPs) [283]. It has been reported that miR-616 expression is positively correlated with EOC metastasis, advanced stage, poor differentiation, and lower patient survival, and its upregulation promotes invasion, migration, and EMT in vitro. TIMP2 was identified as a direct target of miR-616. In addition, more lung metastatic nodules were observed when EOC cells transfected with miR-616 were injected through the tail vein into nude mice, suggesting that miR-616 promotes tumor metastasis [111].
Dicer, a key enzyme involved in miRNA biogenesis, was reported to be negatively correlated with advanced EOC stages and positively associated with better patient outcomes [266]. Rupaimoole et al. reported that DICER1 was targeted by miR-630 in EOC under hypoxic conditions [156]. In vitro studies showed that miR-630 induced migration and invasion, as well as EMT. In an orthotopic mouse model of ovarian cancer, delivery of miR-630 via liposomal nanoparticles significantly enhanced tumor growth and distant metastasis [156]. Interestingly, treatment with a combination of anti-miR-630 and anti-vascular endothelial growth factor (VEGF) antibody resulted in a strong reduction in tumor growth and metastasis [156], suggesting the therapeutic potential of this approach. Paradoxically, another study found that Dicer was overexpressed in ovarian tumor stromal cells and played a pro-inflammatory and pro-metastatic role by down-regulating miR-6780b, which inhibits the NFκB pathway in fibroblasts [284]. Thus, Dicer may exert cell type-specific effects on EOC metastasis.
Thrombocytosis was reported to be positively associated with advanced stage and grade of EOC. In addition, it is frequently observed in patients with lymph node metastases, increased volumes of ascites, and decreased overall survival [158,285]. Tang et al. discovered that when EOC cells were cocultured with platelet microparticles (PMP), there was an increase in cell proliferation, migration, and EMT, suggesting the induction of EMT from platelet-delivered molecules [158]. In addition, in vitro analysis showed that PMPs contained miR-939 which promoted EMT in EOC cells. Finally, the uptake of miRNA-containing PMPs by EOC cells was suggested to be mediated by secretory phospholipase A2 type IIA [158]. These studies showed a mechanistic link between thrombocytosis and EOC progression. However, how miR-939 induces EMT remains to be investigated.
The immune microenvironment is known to be involved in EOC progression, including metastasis. miRNAs may also play a role in promoting EOC metastasis by altering the immune microenvironment. miR-29a-3p and miR-21-5p increased the ratio of regulatory and helper 17 T cells (Treg/Th17) and tumor growth and metastasis in vivo [102]. A higher Treg/Th17 ratio was observed in EOC and in metastatic peritoneal tissues. Both miRNAs were present at high levels in exosomes released from M2 macrophages. STAT3, which is involved in immune cell differentiation, was identified to be inhibited by both miRNAs [102]. These findings suggest that miR-29a-3p and miR-21-5p induce an immunosuppressive microenvironment to facilitate EOC development in part by targeting STAT3. Unlike in immune cells, STAT3 exerts tumor-promoting effects on EOC cells [286]. Interestingly, miR-551-3b may bind directly to STAT3 promoter, leading to the recruitment of RNA polymerase II and transcription factor TWIST1, activating STAT3 transcription and promoting metastasis [143]. In addition, miR-551-3b promotes EOC stem cell proliferation, invasion, and chemoresistance by downregulating FOXO3 and TRIM31 [142]. Another instance of immune suppression is miR-20a, which may reduce natural killer cell cytotoxicity towards EOC cells by inhibiting MICA/B, resulting in immune evasion [106]. Serum levels of miR-20a were elevated in EOC subjects, with high expression associated with poor survival [106]. These studies provided insights into the role of miRNAs in cancer immune modulation.
5.2. MicroRNAs that Suppress Metastasis
5.2.1. MicroRNAs Suppress Metastasis by Directly Targeting Transcription Factors that Regulate EMT Markers
Master regulators of EMT, including ZEBs, SNAIs, and TWISTs, operate largely as transcription repressors to repress CDH1 transcription [287]. Overexpression of miR-101-3p, miR-130b, and miR-1236-3p inhibits EOC cell invasion and migration, increases E-cadherin, and decreases mesenchymal markers by directly targeting ZEB1 [165,168,178]. Similarly, SNAI1 and SNAI2 are targets of multiple miRNAs [119,167,175,222]. Using the TCGA database and tissue samples from EOC patients, Yang et al. identified miR-506 as a positive prognostic predictor of EOC patients [222]. MiR-506 was found to upregulate E-cadherin and downregulate SNAI2 and VIM, as well as inhibited cell invasion and migration. In addition to SNAI2, miR-506 also directly targeted VIM and CDH2 [63]. Furthermore, in vivo miR-506 delivery via nanoparticles reduced the number and weight of tumor nodules in the intraperitoneal metastasis model [222], providing strong evidence that miR-506 suppresses metastasis. On the other hand, miR-145 has been shown to interact with the 3′ UTR of TWIST1 and SOX9 and exert inhibitory effects on EMT [193]. Importantly, when nude mice were inoculated intraperitoneally with miR-145-overexpressing EOC cells, there were fewer metastases and less ascites than the control mice [162]. These findings suggest that miR-145 suppresses metastasis and one of the possible mechanisms is to inhibit TWIST1 and, therefore, EMT. miR-25 has also been reported to target SNAI2 and inhibit TGF-β-induced EMT, cell migration, and invasion [167]. Through direct inhibition of EMT marker genes, these miRNAs suppress EMT and metastasis.
5.2.2. MicroRNAs Suppress Metastasis by Targeting Growth Factors and Related Signaling Pathways
Several miRNAs have been shown to modulate the metastatic potential of EOC cells by targeting growth factors and their downstream signaling pathways. Ectopic expression of miR-139, miR-212, and miR-936 inhibited cell proliferation, invasion, and migration by targeting hepatoma-derived growth factor (HDGF), heparin-binding epidermal growth factor (HBEGF), and fibroblast growth factor 2 (FGF2), respectively [186,231,239]. Moreover, Li et al. found that low miR-936 expression in EOC tissues was associated with large tumor size, advanced stage, and lymphatic metastasis. They also demonstrated that miR-936 inhibited tumor growth in vivo, as well as significantly deactivated the PI3K/AKT pathway shown by decreased p-PI3K and p-AKT levels [231]. Similarly, miR-217 directly targeted insulin-like growth factor 1 receptor (IGF1R) and suppressed EOC cell proliferation, colony formation, invasion, and migration, as well as inhibited subcutaneous tumor growth [200]. In addition, miR-421 directly targeted platelet derived growth factor receptor A (PDGFRA) and inhibited CD44+/CD133+ serous human ovarian cancer stem cell proliferation, invasion, angiogenesis, and tumor growth [216]. These findings suggest that miR-421 exerts an anti-metastatic effect by suppressing PDGF signaling. Finally, miR-503-5p targets CD97, a member of the epidermal growth factor-seven transmembrane (EGF-TM7) family that induces JAK2/STAT3 signaling [288,289], to inhibit EOC cell proliferation, migration, and invasion [221].
Several anti-metastatic miRNAs have been reported to negatively regulate the Wnt signaling in EOC. Using EOC tissue samples and the TCGA database, Huang et al. and Yu et al. identified miR-340 and miR-377 as positive prognostic biomarkers of EOC patients [207,213]. By targeting Four-and-a-half LIM domains protein 2 (FHL2) and Cullin 4A (CUL4A), miR-340 and miR-377 decreased EOC cell migration and invasion, downregulated the Wnt/β-catenin pathway, and inhibited EMT [207,213]. Furthermore, miR-340-overexpressing EOC cells decreased the volume of ascites and peritoneal metastases in vivo. In addition to FHL2, miR-340 also targets NFKB1 [208]. These findings strongly support a role for miR-340 in inhibiting EOC metastasis. miR-219-5p also inhibited cell proliferation, invasion, and migration, and downregulated the Wnt/β-catenin pathway by targeting TWIST1 [202]. Overexpression of miR-219-5p downregulated both TWIST and β-catenin levels [202], suggesting that decreased expression of TWIST led to the downregulation of β-catenin via AKT/GSK3β axis [290]. Besides modulating TWIST expression directly, miR-219-5p was reported to target the oncofetal protein, high-mobility group A2 (HMGA2), and reduced subcutaneous tumor growth in vivo [203]. These findings show that these miRNAs have anti-metastatic effects and one of the mechanisms is by downregulating the Wnt/β-catenin signaling pathway. Additional studies using in vivo EOC metastasis models are required to further confirm their roles in suppressing EOC metastasis.
Yes-associated protein 1 (YAP1) is a downstream target of the Hippo signaling pathway which promotes the progression of various tumors, including colorectal, bladder, and liver cancers [291,292,293]. Several miRNAs have been reported to target YAP1 in EOC. miR-509-3p, which was identified as a positive prognostic predictor in EOC patients, inhibited EOC cell invasion, migration, and spheroid formation by targeting YAP1 [164], suggesting a potential role in inhibiting EOC metastasis. Similarly, miR-375-5p also directly targeted YAP1 and inhibited EOC cell proliferation, invasion, migration, and EMT. Importantly, live animal bioluminescence imaging revealed that inhibition of miR-375-5p resulted in an increase in primary tumor growth and liver and spleen metastases [115], supporting a role for miR-375-5p in repressing EOC metastasis.
Regulation of the Rho pathway by miRNAs modulates cell motility and tumor metastasis [294]. Chen et al. reported that miR-106b, whose expression in EOC tissues was negatively associated with tumor grade and stage, directly targeted RHOC and reduced cell proliferation, invasion, and migration, as well as inhibited tumor growth in vivo [171]. Similarly, Rho-associated coiled-coil-containing protein kinases (ROCKs), including ROCK1 and ROCK2, are targets of miR-148a-3p and miR-139-5p, respectively [114,188,189]. Overexpression of miR-148a-3p and miR-139-5p inhibited cell proliferation, invasion, and migration in vitro, as well as suppressed EOC growth in nude mice [114,188,189]. On the other hand, miR-138 targets LIMK1, which is activated by signaling through the Rho family GTPases and reported to be a marker for malignant progression in EOC, to inhibit EOC cell proliferation, invasion, and migration [83].
5.2.3. MicroRNAs Suppress Metastasis by Regulating Adhesion Molecules
Several miRNAs have been reported to downregulate FAK signaling to inhibit EOC metastasis. miR-708, a significantly downregulated miRNA in highly invasive EOC tissues with advanced stages and metastasis, was shown to inhibit focal adhesion formation, cell invasion, and migration, accompanied by decreased p-FAK and p-Paxillin expression, by targeting Ras family small GTP-binding protein (RAP1B) [81]. Overexpression of miR-708 reduced abdominal metastases in the orthotopic metastasis model [81], providing strong evidence that miR-708 suppresses EOC metastasis. In addition, miR-4454 inhibited cell invasion and migration by targeting secreted protein acidic and rich in cysteine (SPARC), a glycoprotein associated with metastatic EOC [295], to inhibit FAK activity. Importantly, when miR-4454-overexpressing EOC cells were inoculated intraperitoneally to the nude mice, fewer peritoneal metastases were observed [232]. These findings indicate that miR-4454 inhibits EOC metastasis and one possible mechanism is to suppress FAK activation.
The integrin α5β1 pair is a negative prognostic biomarker in EOC patients and participates in cancer cell adherence and mesothelial layer clearance in EOC metastasis [296,297,298]. miR-17, whose expression was negatively correlated with ITGA5 and ITGB1 expression in various EOC cell lines, decreased cell adhesion and invasion, as well as reduced peritoneal metastatic nodules in vivo by targeting ITGA5 and ITGB1. In addition, miR-17 also repressed ILK phosphorylation and MMP-2 expression [170]. miR-6126, secreted by EOC cells via exosomes, acts on endothelial cells to suppress angiogenesis and on EOC cells to inhibit migration and invasion by directly targeting ITGB1 [234]. Interestingly, miR-6126 delivery via DOPC nanoliposomes into an orthotopic mouse model of ovarian cancer suppressed tumor growth and angiogenesis. Moreover, miR-6126 was found to correlate with better overall survival of EOC patients [234]. These findings strongly support that miR-6126 suppresses metastasis.
5.2.4. MicroRNAs Suppress Metastasis by Directly Targeting HOX Genes
Homeobox (HOX) genes encode developmental regulators which are crucial for growth and differentiation. The dysregulation of HOX genes has been observed in various cancers [299]. HOXA10 is overexpressed in EOC and is associated with poor survival [300]. By targeting HOXA10 and CCR2, miR-135a, which is a positive prognostic biomarker in EOC patients, decreased EOC cell proliferation, adhesion, migration, and invasion, reduced Bcl-2 and N-cad expression, as well as increased p53, caspase-3, and E-cadherin expression. Importantly, overexpression of miR-135a reduced subcutaneous tumor growth and lung metastases [182,183], suggesting that miR-135a suppresses metastasis. Similarly, miR-665 also targets HOXA10 and inhibits EOC cell proliferation and migration [229]. On the other hand, miR-612 and miR-202-5p directly target HOXA13 and HOXB2, respectively. Both miRNAs were found to inhibit cell proliferation, invasion, and migration [196,227]. In addition, miR-202-5p inhibited EMT in vitro and was identified as a positive prognostic predictor in EOC patients [196].
5.2.5. MicroRNAs Suppress Metastasis by Directly Targeting HIF
EOC cells with high levels of hypoxia-inducible factor (HIF) are more likely to disseminate from primary sites to the peritoneal cavity [301]. Moreover, HIF enhances tissue remodeling genes and is associated with EOC patient morbidity and mortality [302]. Joshi et al. reported that HIF transcriptionally suppressed miR-199a-5p in EOC cells, and miR-199a-5p interacted with the 3′ UTR of HIF1A and HIF2A to downregulate their levels, forming a feedback loop [94]. Ectopic miR-199a-5p expression decreased cell migration in vitro and inhibited tumor growth and peritoneal seeding upon intraperitoneal injection of EOC cells in vivo. The down-regulation of HIF also resulted in a decrease in LOX, an ECM remodeling enzyme and a negative prognostic biomarker in EOC patients [94]. LOX has also been reported to promote EOC cell migration and metastasis [95]. These findings provide strong evidence that miR-199a-5p suppresses metastasis, and its indirect regulation of the matrix/tissue remodeling gene expression may be one of the underlying mechanisms.
5.3. miRNAs that Have Been Reported to Promote and Inhibit Metastasis
Several miRNAs have been found to exert differential effects on metastasis. For example, the miR-200 family (miR-141/200a/200b/200c/429) has been reported to be either upregulated or downregulated in aggressive EOC and both expression levels were associated with poor survival [120,126,222,248,249,251,303]. Several studies have reported tumor-promoting effects of miR-141 in EOC, including enhancing cell proliferation, survival, anoikis resistance, chemoresistance, and peritoneal metastasis [245,304]. Mechanistically, miR-141 has been reported to target KLF12 and SIK1, which are known to exert tumor-suppressive functions, inhibiting anoikis and p53-dependent apoptosis in EOC [245,305]. However, another study found that miR-141 and miR-200a induced tumor growth in a mouse model, but also sensitized tumors to chemotherapeutic drugs by targeting p38α to regulate oxidative stress [246]. miR-141 [134,247] and miR-200a [134] have also been reported to have inhibitory effects on EOC cell migration and invasion; however, a direct target was not determined in these studies. Similarly, miR-200a was reported to promote cell migration and invasion by targeting PTEN in a HGSC cell line [3], OVCAR3 [248], while impeding vasculogenic mimicry through targeting EPHA2, leading to decreased cell invasion in SKOV3 cells [250], which are thought to represent the EC subtype [3]. Opposing to the association between the upregulation of miR-200a and miR-200b and poor clinical outcomes, miR-200a and miR-200b overexpression reduced IL-8 and CXCL1 levels and inhibited cell migration, invasion, angiogenesis, and intraperitoneal metastasis in vivo [249]. Interestingly, growing evidence indicates that the miR-200 family may inhibit EMT via direct repression of ZEB1/2 [134,252,306]. Therefore, it has been proposed that the expression of the miR-200 family members is downregulated initially to enhance EMT and increase the invasiveness of EOC cells, and is then upregulated to induce mesenchymal-to-epithelial-transition (MET) and achieve re-epithelialization of tumor cells in distant metastatic sites [307]. It has been suggested that the downregulation of miR-200s occurs during the progression of tumor cells gaining metastatic capability [308]. Furthermore, metastatic EOC tissues showed increased MET markers when compared to primary cancer tissues [309], suggesting a possible downregulation of the miR-200 family at some point during the re-epithelialization process. Whether or not the miR-200 family has subtype- and/or stage-specific effects on metastasis requires further investigation.
In addition to the miR-200 family, other studies reported that in the SKOV3 cell line, miR-9 either increased migration and invasion by targeting CDH1 or inhibited migration and invasion by targeting TLN1 [242,244]. These studies also examined miR-9 expression in tissue samples, but observed a higher expression in serous EOC metastases compared to primary tumors [242] and lower expression in recurrent serous EOC tumors compared to primary EOC tissues [243]. The opposing effects of miR-9 also have been reported in other cancers, with varied targets and functional roles which are more likely dependent on tissue or cell type [310,311,312]. Similarly, miR-203 promoted OVCA429 and OVCA433 cell proliferation and migration in vitro, as well as tumor metastasis in vivo, by targeting pyruvate dehydrogenase B (PDHB) and the subsequent enhancement of glycolysis [118]. In contrast, ectopic miR-203 expression in SKOV3 and OVCAR3 cells attenuated EMT, cell migration, and invasion in vitro and tumor growth in vivo, by targeting SNAI2 [118] and BIRC5 [254]. The reasons for such discrepancies are not clear; however, the relative levels of different target genes and their functions in tumor development may contribute to the differential effects of miRNAs.
6. Conclusions and Future Direction
Cancer metastasis is one of the main factors that leads to poor clinical outcomes for EOC patients. Accumulating evidence demonstrates that miRNAs play important roles in EOC metastasis. Aberrant expression of miRNAs has been reported in EOC. Such dysregulation can be attributed to alterations at the DNA level, such as amplification and hypermethylation at the promoter regions of miRNA genes. In addition, altered transcriptional controls and defects in miRNA biogenesis machinery also contribute to the abnormality of miRNA levels. Many studies have reported that miRNA expression profiles correlate with clinical features, such as tumor stage, grade, and overall survival of patients, raising the possibility of using miRNAs as diagnostic and/or prognostic markers.
Due to the heterogeneity of EOC, it is a challenge to find effective biomarkers for detecting EOC in different tumors [313]. miRNA profiling studies have sometimes reported inconsistent findings. One of the underlying issues could be the controls used. Some researchers used normal ovarian tissues as the control while others used benign tumors. Methylation patterns of some miRNA genes have been shown to be correlated with metastasis [116,257]. In addition, miRNAs are detected in biological fluids, which can serve as a non-invasive tool for EOC diagnosis. Further efforts in validating the specificity and sensitivity of miRNA signatures in a large cohort of EOC patients are needed for the development of miRNAs as diagnostic and prognostic biomarkers.
Metastasis of ovarian cancer is orchestrated by several interconnected biological processes, including EMT, increase in cell mobility and migration, destruction of the ECM, formation of spheroids, avoidance of apoptosis, angiogenesis, and immune suppression [91]. Some miRNAs have been reported to promote metastasis, mainly by targeting negative regulators of these processes. On the other hand, most miRNAs that have been studied exert suppressive effects on metastasis, mainly by inhibiting transcription factors that induce the expression of mesenchymal markers, or key signaling pathways that promote EMT, motility, and tumor angiogenesis. Therefore, the upregulation of metastasis-promoting miRNAs and downregulation of metastasis-suppressing miRNAs would lead to a dysregulated signaling network and promote metastasis. However, more work is required to better understand the role of miRNAs and the underlying mechanisms by which they regulate metastasis. Among the studies reported so far, some are comprehensive, but most only examined the effects of miRNAs using established EOC cell lines in vitro. Therefore, further in vivo experiments would verify the roles of those miRNAs in metastasis of EOC. Moreover, miRNAs can target many genes and it is possible that they could exert tumor-promoting or tumor-suppressive effects, depending on the relative abundance and/or functions of target genes in different tumor contexts. Most studies have been focused on one or a few target genes. Additional studies in identifying critical targets that are directly involved in the induction of EOC metastasis would enhance our understanding of the roles of miRNAs in these processes. Finally, EOC consists of multiple histological subtypes, each one with unique origins and distinct molecular features [3]. More work on examining the dysregulation and functions of miRNAs in different subtypes of EOC is warranted as it may help to develop precise therapeutics. miRNAs have been suggested as promising therapeutic targets for cancer treatment [314]. miRNA-based therapies have been established for lung cancer treatment and further trials are anticipated to address clinical treatment efficacy [314]. It is possible that the restoration of down-regulated miRNAs that inhibit metastasis or inhibition of up-regulated miRNAs that promote metastasis could be used in the future as a therapeutic approach for EOC.
Funding
Studies performed in our lab were supported by grants from Canadian Institutes of Health (MOP-89931, PJT-153146, and PJT-419466), Canada Foundation of Innovation (CFI-356111), and the York Research Chair Program to C.P. J.O. received a graduate scholarship from Natural Science and Engineering Canada (NSERC). C.Y. and K.D. were supported by an NSERC undergraduate student research award with supplemental funding from the Faculty of Science, York University.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2019. CA Cancer J. Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Boussios S., Moschetta M., Zarkavelis G., Papadaki A., Kefas A., Tatsi K. Ovarian sex-cord stromal tumours and small cell tumours: Pathological, genetic and management aspects. Crit. Rev. Oncol. Hematol. 2017;120:43–51. doi: 10.1016/j.critrevonc.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 3.National Academies of Sciences, Engineering, and Medicine . Ovarian Cancers: Evolving Paradigms in Research and Care. The National Academies Press; Washington, DC, USA: 2016. p. 396. [DOI] [PubMed] [Google Scholar]
- 4.Lupia M., Cavallaro U. Ovarian cancer stem cells: Still an elusive entity? Mol. Cancer. 2017;16:64. doi: 10.1186/s12943-017-0638-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webb P.M., Jordan S.J. Epidemiology of epithelial ovarian cancer. Best Pract. Res. Clin. Obstet. Gynaecol. 2017;41:3–14. doi: 10.1016/j.bpobgyn.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 6.Matulonis U.A., Sood A.K., Fallowfield L., Howitt B.E., Sehouli J., Karlan B.Y. Ovarian cancer. Nat. Rev. Dis. Primers. 2016;2:16061. doi: 10.1038/nrdp.2016.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lagos-Quintana M., Rauhut R., Lendeckel W., Tuschl T. Identification of novel genes coding for small expressed RNAs. Science. 2001;294:853–858. doi: 10.1126/science.1064921. [DOI] [PubMed] [Google Scholar]
- 8.Ambros V. microRNAs: Tiny regulators with great potential. Cell. 2001;107:823–826. doi: 10.1016/S0092-8674(01)00616-X. [DOI] [PubMed] [Google Scholar]
- 9.Friedman R.C., Farh K.K., Burge C.B., Bartel D.P. Most mammalian mRNAs are conserved targets of microRNAs. Genome Res. 2009;19:92–105. doi: 10.1101/gr.082701.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vidigal J.A., Ventura A. The biological functions of miRNAs: Lessons from in vivo studies. Trends Cell Biol. 2015;25:137–147. doi: 10.1016/j.tcb.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Staicu C.E., Predescu D.V., Rusu C.M., Radu B.M., Cretoiu D., Suciu N., Cretoiu S.M., Voinea S.C. Role of microRNAs as Clinical Cancer Biomarkers for Ovarian Cancer: A Short Overview. Cells. 2020;9:169. doi: 10.3390/cells9010169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen S.N., Chang R., Lin L.T., Chern C.U., Tsai H.W., Wen Z.H., Li Y.H., Li C.J., Tsui K.H. MicroRNA in Ovarian Cancer: Biology, Pathogenesis, and Therapeutic Opportunities. Int. J. Environ. Res. Public Health. 2019;16:1510. doi: 10.3390/ijerph16091510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roberts C.M., Cardenas C., Tedja R. The Role of Intra-Tumoral Heterogeneity and Its Clinical Relevance in Epithelial Ovarian Cancer Recurrence and Metastasis. Cancers. 2019;11:1083. doi: 10.3390/cancers11081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Godnic I., Zorc M., Jevsinek Skok D., Calin G.A., Horvat S., Dovc P., Kovac M., Kunej T. Genome-wide and species-wide in silico screening for intragenic MicroRNAs in human, mouse and chicken. PLoS ONE. 2013;8:e65165. doi: 10.1371/journal.pone.0065165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Rie D., Abugessaisa I., Alam T., Arner E., Arner P., Ashoor H., Astrom G., Babina M., Bertin N., Burroughs A.M., et al. An integrated expression atlas of miRNAs and their promoters in human and mouse. Nat. Biotechnol. 2017;35:872–878. doi: 10.1038/nbt.3947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim Y.K., Kim V.N. Processing of intronic microRNAs. EMBO J. 2007;26:775–783. doi: 10.1038/sj.emboj.7601512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramalingam P., Palanichamy J.K., Singh A., Das P., Bhagat M., Kassab M.A., Sinha S., Chattopadhyay P. Biogenesis of intronic miRNAs located in clusters by independent transcription and alternative splicing. RNA. 2014;20:76–87. doi: 10.1261/rna.041814.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirigin F.F., Lindstedt K., Sellars M., Ciofani M., Low S.L., Jones L., Bell F., Pauli F., Bonneau R., Myers R.M., et al. Dynamic microRNA gene transcription and processing during T cell development. J. Immunol. 2012;188:3257–3267. doi: 10.4049/jimmunol.1103175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee Y., Kim M., Han J., Yeom K.H., Lee S., Baek S.H., Kim V.N. MicroRNA genes are transcribed by RNA polymerase II. EMBO J. 2004;23:4051–4060. doi: 10.1038/sj.emboj.7600385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim Y.K., Kim B., Kim V.N. Re-evaluation of the roles of DROSHA, Export in 5, and DICER in microRNA biogenesis. Proc. Natl. Acad. Sci. USA. 2016;113:E1881–E1889. doi: 10.1073/pnas.1602532113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gregory R.I., Yan K.P., Amuthan G., Chendrimada T., Doratotaj B., Cooch N., Shiekhattar R. The Microprocessor complex mediates the genesis of microRNAs. Nature. 2004;432:235–240. doi: 10.1038/nature03120. [DOI] [PubMed] [Google Scholar]
- 22.Triboulet R., Chang H.M., Lapierre R.J., Gregory R.I. Post-transcriptional control of DGCR8 expression by the Microprocessor. RNA. 2009;15:1005–1011. doi: 10.1261/rna.1591709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bohnsack M.T., Czaplinski K., Gorlich D. Exportin 5 is a RanGTP-dependent dsRNA-binding protein that mediates nuclear export of pre-miRNAs. RNA. 2004;10:185–191. doi: 10.1261/rna.5167604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lund E., Dahlberg J.E. Substrate selectivity of exportin 5 and Dicer in the biogenesis of microRNAs. Cold Spring Harb. Symp. Quant. Biol. 2006;71:59–66. doi: 10.1101/sqb.2006.71.050. [DOI] [PubMed] [Google Scholar]
- 25.Ruby J.G., Jan C.H., Bartel D.P. Intronic microRNA precursors that bypass Drosha processing. Nature. 2007;448:83–86. doi: 10.1038/nature05983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Babiarz J.E., Ruby J.G., Wang Y., Bartel D.P., Blelloch R. Mouse ES cells express endogenous shRNAs, siRNAs, and other Microprocessor-independent, Dicer-dependent small RNAs. Genes Dev. 2008;22:2773–2785. doi: 10.1101/gad.1705308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grishok A., Pasquinelli A.E., Conte D., Li N., Parrish S., Ha I., Baillie D.L., Fire A., Ruvkun G., Mello C.C. Genes and mechanisms related to RNA interference regulate expression of the small temporal RNAs that control C. elegans developmental timing. Cell. 2001;106:23–34. doi: 10.1016/S0092-8674(01)00431-7. [DOI] [PubMed] [Google Scholar]
- 28.Bernstein E., Caudy A.A., Hammond S.M., Hannon G.J. Role for a bidentate ribonuclease in the initiation step of RNA interference. Nature. 2001;409:363–366. doi: 10.1038/35053110. [DOI] [PubMed] [Google Scholar]
- 29.Knight S.W., Bass B.L. A role for the RNase III enzyme DCR-1 in RNA interference and germ line development in Caenorhabditis elegans. Science. 2001;293:2269–2271. doi: 10.1126/science.1062039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hammond S.M., Bernstein E., Beach D., Hannon G.J. An RNA-directed nuclease mediates post-transcriptional gene silencing in Drosophila cells. Nature. 2000;404:293–296. doi: 10.1038/35005107. [DOI] [PubMed] [Google Scholar]
- 31.Gregory R.I., Chendrimada T.P., Cooch N., Shiekhattar R. Human RISC couples microRNA biogenesis and posttranscriptional gene silencing. Cell. 2005;123:631–640. doi: 10.1016/j.cell.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 32.Yoda M., Kawamata T., Paroo Z., Ye X., Iwasaki S., Liu Q., Tomari Y. ATP-dependent human RISC assembly pathways. Nat. Struct. Mol. Biol. 2010;17:17–23. doi: 10.1038/nsmb.1733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hammond S.M., Boettcher S., Caudy A.A., Kobayashi R., Hannon G.J. Argonaute2, a link between genetic and biochemical analyses of RNAi. Science. 2001;293:1146–1150. doi: 10.1126/science.1064023. [DOI] [PubMed] [Google Scholar]
- 34.Kawamata T., Tomari Y. Making RISC. Trends Biochem. Sci. 2010;35:368–376. doi: 10.1016/j.tibs.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 35.Su H., Trombly M.I., Chen J., Wang X. Essential and overlapping functions for mammalian Argonautes in microRNA silencing. Genes Dev. 2009;23:304–317. doi: 10.1101/gad.1749809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kadekar S., Nawale G.N., Karlsson K., Alander C., Oommen O.P., Varghese O.P. Synthetic Design of Asymmetric miRNA with an Engineered 3′ Overhang to Improve Strand Selection. Mol. Ther. Nucleic Acids. 2019;16:597–604. doi: 10.1016/j.omtn.2019.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meister G., Landthaler M., Patkaniowska A., Dorsett Y., Teng G., Tuschl T. Human Argonaute2 mediates RNA cleavage targeted by miRNAs and siRNAs. Mol. Cell. 2004;15:185–197. doi: 10.1016/j.molcel.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 38.O’Brien J., Hayder H., Zayed Y., Peng C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. (Lausanne) 2018;9:402. doi: 10.3389/fendo.2018.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huntzinger E., Izaurralde E. Gene silencing by microRNAs: Contributions of translational repression and mRNA decay. Nat. Rev. Genet. 2011;12:99–110. doi: 10.1038/nrg2936. [DOI] [PubMed] [Google Scholar]
- 40.Pfaff J., Meister G. Argonaute and GW182 proteins: An effective alliance in gene silencing. Biochem. Soc. Trans. 2013;41:855–860. doi: 10.1042/BST20130047. [DOI] [PubMed] [Google Scholar]
- 41.Christie M., Boland A., Huntzinger E., Weichenrieder O., Izaurralde E. Structure of the PAN3 pseudokinase reveals the basis for interactions with the PAN2 deadenylase and the GW182 proteins. Mol. Cell. 2013;51:360–373. doi: 10.1016/j.molcel.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 42.Jonas S., Izaurralde E. Towards a molecular understanding of microRNA-mediated gene silencing. Nat. Rev. Genet. 2015;16:421–433. doi: 10.1038/nrg3965. [DOI] [PubMed] [Google Scholar]
- 43.Behm-Ansmant I., Rehwinkel J., Doerks T., Stark A., Bork P., Izaurralde E. mRNA degradation by miRNAs and GW182 requires both CCR4:NOT deadenylase and DCP1:DCP2 decapping complexes. Genes Dev. 2006;20:1885–1898. doi: 10.1101/gad.1424106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Braun J.E., Truffault V., Boland A., Huntzinger E., Chang C.T., Haas G., Weichenrieder O., Coles M., Izaurralde E. A direct interaction between DCP1 and XRN1 couples mRNA decapping to 5’ exonucleolytic degradation. Nat. Struct. Mol. Biol. 2012;19:1324–1331. doi: 10.1038/nsmb.2413. [DOI] [PubMed] [Google Scholar]
- 45.Wilczynska A., Bushell M. The complexity of miRNA-mediated repression. Cell Death Differ. 2015;22:22–33. doi: 10.1038/cdd.2014.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xu W., San Lucas A., Wang Z., Liu Y. Identifying microRNA targets in different gene regions. BMC Bioinform. 2014;15(Suppl. 7):S4. doi: 10.1186/1471-2105-15-S7-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dharap A., Pokrzywa C., Murali S., Pandi G., Vemuganti R. MicroRNA miR-324-3p induces promoter-mediated expression of RelA gene. PLoS ONE. 2013;8:e79467. doi: 10.1371/journal.pone.0079467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Forman J.J., Legesse-Miller A., Coller H.A. A search for conserved sequences in coding regions reveals that the let-7 microRNA targets Dicer within its coding sequence. Proc. Natl. Acad. Sci. USA. 2008;105:14879–14884. doi: 10.1073/pnas.0803230105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang J., Zhou W., Liu Y., Liu T., Li C., Wang L. Oncogenic role of microRNA-532-5p in human colorectal cancer via targeting of the 5’UTR of RUNX3. Oncol. Lett. 2018;15:7215–7220. doi: 10.3892/ol.2018.8217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Truesdell S.S., Mortensen R.D., Seo M., Schroeder J.C., Lee J.H., LeTonqueze O., Vasudevan S. MicroRNA-mediated mRNA translation activation in quiescent cells and oocytes involves recruitment of a nuclear microRNP. Sci. Rep. 2012;2:842. doi: 10.1038/srep00842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Orom U.A., Nielsen F.C., Lund A.H. MicroRNA-10a binds the 5’UTR of ribosomal protein mRNAs and enhances their translation. Mol. Cell. 2008;30:460–471. doi: 10.1016/j.molcel.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 52.Tan D.S., Agarwal R., Kaye S.B. Mechanisms of transcoelomic metastasis in ovarian cancer. Lancet Oncol. 2006;7:925–934. doi: 10.1016/S1470-2045(06)70939-1. [DOI] [PubMed] [Google Scholar]
- 53.Yeung T.L., Leung C.S., Yip K.P., Au Yeung C.L., Wong S.T., Mok S.C. Cellular and molecular processes in ovarian cancer metastasis. A Review in the Theme: Cell and Molecular Processes in Cancer Metastasis. Am. J. Physiol. Cell Physiol. 2015;309:C444–C456. doi: 10.1152/ajpcell.00188.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lengyel E. Ovarian cancer development and metastasis. Am. J. Pathol. 2010;177:1053–1064. doi: 10.2353/ajpath.2010.100105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Micalizzi D.S., Farabaugh S.M., Ford H.L. Epithelial-mesenchymal transition in cancer: Parallels between normal development and tumor progression. J. Mammary Gland Biol. Neoplasia. 2010;15:117–134. doi: 10.1007/s10911-010-9178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Onder T.T., Gupta P.B., Mani S.A., Yang J., Lander E.S., Weinberg R.A. Loss of E-cadherin promotes metastasis via multiple downstream transcriptional pathways. Cancer Res. 2008;68:3645–3654. doi: 10.1158/0008-5472.CAN-07-2938. [DOI] [PubMed] [Google Scholar]
- 57.Mani S.A., Yang J., Brooks M., Schwaninger G., Zhou A., Miura N., Kutok J.L., Hartwell K., Richardson A.L., Weinberg R.A. Mesenchyme Forkhead 1 (FOXC2) plays a key role in metastasis and is associated with aggressive basal-like breast cancers. Proc. Natl. Acad. Sci. USA. 2007;104:10069–10074. doi: 10.1073/pnas.0703900104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Davidson B., Trope C.G., Reich R. Epithelial-mesenchymal transition in ovarian carcinoma. Front. Oncol. 2012;2:33. doi: 10.3389/fonc.2012.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Palma Flores C., Garcia-Vazquez R., Gallardo Rincon D., Ruiz-Garcia E., Astudillo de la Vega H., Marchat L.A., Salinas Vera Y.M., Lopez-Camarillo C. MicroRNAs driving invasion and metastasis in ovarian cancer: Opportunities for translational medicine (Review) Int. J. Oncol. 2017;50:1461–1476. doi: 10.3892/ijo.2017.3948. [DOI] [PubMed] [Google Scholar]
- 60.Peinado H., Olmeda D., Cano A. Snail, Zeb and bHLH factors in tumour progression: An alliance against the epithelial phenotype? Nat. Rev. Cancer. 2007;7:415–428. doi: 10.1038/nrc2131. [DOI] [PubMed] [Google Scholar]
- 61.Yang J., Weinberg R.A. Epithelial-mesenchymal transition: At the crossroads of development and tumor metastasis. Dev. Cell. 2008;14:818–829. doi: 10.1016/j.devcel.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 62.Tsai J.H., Yang J. Epithelial-mesenchymal plasticity in carcinoma metastasis. Genes Dev. 2013;27:2192–2206. doi: 10.1101/gad.225334.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sun Y., Hu L., Zheng H., Bagnoli M., Guo Y., Rupaimoole R., Rodriguez-Aguayo C., Lopez-Berestein G., Ji P., Chen K., et al. MiR-506 inhibits multiple targets in the epithelial-to-mesenchymal transition network and is associated with good prognosis in epithelial ovarian cancer. J. Pathol. 2015;235:25–36. doi: 10.1002/path.4443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kalluri R., Weinberg R.A. The basics of epithelial-mesenchymal transition. J. Clin. Investig. 2009;119:1420–1428. doi: 10.1172/JCI39104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nusse R., Clevers H. Wnt/beta-Catenin Signaling, Disease, and Emerging Therapeutic Modalities. Cell. 2017;169:985–999. doi: 10.1016/j.cell.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 66.Nguyen V.H.L., Hough R., Bernaudo S., Peng C. Wnt/beta-catenin signalling in ovarian cancer: Insights into its hyperactivation and function in tumorigenesis. J. Ovarian Res. 2019;12:122. doi: 10.1186/s13048-019-0596-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rafehi S., Ramos Valdes Y., Bertrand M., McGee J., Prefontaine M., Sugimoto A., DiMattia G.E., Shepherd T.G. TGFbeta signaling regulates epithelial-mesenchymal plasticity in ovarian cancer ascites-derived spheroids. Endocr. Relat. Cancer. 2016;23:147–159. doi: 10.1530/ERC-15-0383. [DOI] [PubMed] [Google Scholar]
- 68.Zhou X., Hu Y., Dai L., Wang Y., Zhou J., Wang W., Di W., Qiu L. MicroRNA-7 inhibits tumor metastasis and reverses epithelial-mesenchymal transition through AKT/ERK1/2 inactivation by targeting EGFR in epithelial ovarian cancer. PLoS ONE. 2014;9:e96718. doi: 10.1371/journal.pone.0096718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moran-Jones K. The Therapeutic Potential of Targeting the HGF/cMET Axis in Ovarian Cancer. Mol. Diagn. Ther. 2016;20:199–212. doi: 10.1007/s40291-016-0201-8. [DOI] [PubMed] [Google Scholar]
- 70.Zhang R., Shi H., Ren F., Feng W., Cao Y., Li G., Liu Z., Ji P., Zhang M. MicroRNA-338-3p suppresses ovarian cancer cells growth and metastasis: Implication of Wnt/catenin beta and MEK/ERK signaling pathways. J. Exp. Clin. Cancer Res. CR. 2019;38:494. doi: 10.1186/s13046-019-1494-3. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 71.Zhang Y., Xia M., Jin K., Wang S., Wei H., Fan C., Wu Y., Li X., Li X., Li G., et al. Function of the c-Met receptor tyrosine kinase in carcinogenesis and associated therapeutic opportunities. Mol. Cancer. 2018;17:45. doi: 10.1186/s12943-018-0796-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ke Z., Caiping S., Qing Z., Xiaojing W. Sonic hedgehog-Gli1 signals promote epithelial-mesenchymal transition in ovarian cancer by mediating PI3K/AKT pathway. Med. Oncol. (Northwood Lond. Engl.) 2015;32:368. doi: 10.1007/s12032-014-0368-y. [DOI] [PubMed] [Google Scholar]
- 73.Do T.V., Xiao F., Bickel L.E., Klein-Szanto A.J., Pathak H.B., Hua X., Howe C., O’Brien S.W., Maglaty M., Ecsedy J.A., et al. Aurora kinase A mediates epithelial ovarian cancer cell migration and adhesion. Oncogene. 2014;33:539–549. doi: 10.1038/onc.2012.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Boussios S., Mikropoulos C., Samartzis E., Karihtala P., Moschetta M., Sheriff M., Karathanasi A., Sadauskaite A., Rassy E., Pavlidis N. Wise Management of Ovarian Cancer: On the Cutting Edge. J. Pers. Med. 2020;10:41. doi: 10.3390/jpm10020041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mitra S.K., Hanson D.A., Schlaepfer D.D. Focal adhesion kinase: In command and control of cell motility. Nat. Rev. Mol. Cell Biol. 2005;6:56–68. doi: 10.1038/nrm1549. [DOI] [PubMed] [Google Scholar]
- 76.Cance W.G., Golubovskaya V.M. Focal adhesion kinase versus p53: Apoptosis or survival? Sci. Signal. 2008;1:pe22. doi: 10.1126/stke.120pe22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Frisch S.M., Schaller M., Cieply B. Mechanisms that link the oncogenic epithelial-mesenchymal transition to suppression of anoikis. J. Cell Sci. 2013;126:21–29. doi: 10.1242/jcs.120907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shibue T., Brooks M.W., Inan M.F., Reinhardt F., Weinberg R.A. The outgrowth of micrometastases is enabled by the formation of filopodium-like protrusions. Cancer Discov. 2012;2:706–721. doi: 10.1158/2159-8290.CD-11-0239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sood A.K., Coffin J.E., Schneider G.B., Fletcher M.S., DeYoung B.R., Gruman L.M., Gershenson D.M., Schaller M.D., Hendrix M.J. Biological significance of focal adhesion kinase in ovarian cancer: Role in migration and invasion. Am. J. Pathol. 2004;165:1087–1095. doi: 10.1016/S0002-9440(10)63370-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhao J., Guan J.L. Signal transduction by focal adhesion kinase in cancer. Cancer Metastasis Rev. 2009;28:35–49. doi: 10.1007/s10555-008-9165-4. [DOI] [PubMed] [Google Scholar]
- 81.Lin K.T., Yeh Y.M., Chuang C.M., Yang S.Y., Chang J.W., Sun S.P., Wang Y.S., Chao K.C., Wang L.H. Glucocorticoids mediate induction of microRNA-708 to suppress ovarian cancer metastasis through targeting Rap1B. Nat. Commun. 2015;6:5917. doi: 10.1038/ncomms6917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mei J., Huang Y., Hao L., Liu Y., Yan T., Qiu T., Xu R., Xu B., Xiao Z., Jiang X., et al. DAAM1-mediated migration and invasion of ovarian cancer cells are suppressed by miR-208a-5p. Pathol. Res. Pract. 2019;215:152452. doi: 10.1016/j.prp.2019.152452. [DOI] [PubMed] [Google Scholar]
- 83.Chen P., Zeng M., Zhao Y., Fang X. Upregulation of Limk1 caused by microRNA-138 loss aggravates the metastasis of ovarian cancer by activation of Limk1/cofilin signaling. Oncol. Rep. 2014;32:2070–2076. doi: 10.3892/or.2014.3461. [DOI] [PubMed] [Google Scholar]
- 84.Prunier C., Prudent R., Kapur R., Sadoul K., Lafanechere L. LIM kinases: Cofilin and beyond. Oncotarget. 2017;8:41749–41763. doi: 10.18632/oncotarget.16978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wang L., Mezencev R., Svajdler M., Benigno B.B., McDonald J.F. Ectopic over-expression of miR-429 induces mesenchymal-to-epithelial transition (MET) and increased drug sensitivity in metastasizing ovarian cancer cells. Gynecol. Oncol. 2014;134:96–103. doi: 10.1016/j.ygyno.2014.04.055. [DOI] [PubMed] [Google Scholar]
- 86.Luo X., Dong Z., Chen Y., Yang L., Lai D. Enrichment of ovarian cancer stem-like cells is associated with epithelial to mesenchymal transition through an miRNA-activated AKT pathway. Cell Prolif. 2013;46:436–446. doi: 10.1111/cpr.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Persad S., Dedhar S. The role of integrin-linked kinase (ILK) in cancer progression. Cancer Metastasis Rev. 2003;22:375–384. doi: 10.1023/A:1023777013659. [DOI] [PubMed] [Google Scholar]
- 88.Scheau C., Badarau I.A., Costache R., Caruntu C., Mihai G.L., Didilescu A.C., Constantin C., Neagu M. The Role of Matrix Metalloproteinases in the Epithelial-Mesenchymal Transition of Hepatocellular Carcinoma. Anal. Cell Pathol. (Amst.) 2019;2019:9423907. doi: 10.1155/2019/9423907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jin H., Yu Y., Zhang T., Zhou X., Zhou J., Jia L., Wu Y., Zhou B.P., Feng Y. Snail is critical for tumor growth and metastasis of ovarian carcinoma. Int. J. Cancer. 2010;126:2102–2111. doi: 10.1002/ijc.24901. [DOI] [PubMed] [Google Scholar]
- 90.Paoli P., Giannoni E., Chiarugi P. Anoikis molecular pathways and its role in cancer progression. Biochim. Biophys. Acta. 2013;1833:3481–3498. doi: 10.1016/j.bbamcr.2013.06.026. [DOI] [PubMed] [Google Scholar]
- 91.Braga E.A., Fridman M.V., Kushlinskii N.E. Molecular Mechanisms of Ovarian Carcinoma Metastasis: Key Genes and Regulatory MicroRNAs. Biochemistry. 2017;82:529–541. doi: 10.1134/S0006297917050017. [DOI] [PubMed] [Google Scholar]
- 92.Semenza G.L. Hypoxia-inducible factors: Mediators of cancer progression and targets for cancer therapy. Trends Pharmacol. Sci. 2012;33:207–214. doi: 10.1016/j.tips.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Keith B., Johnson R.S., Simon M.C. HIF1alpha and HIF2alpha: Sibling rivalry in hypoxic tumour growth and progression. Nat. Rev. Cancer. 2011;12:9–22. doi: 10.1038/nrc3183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Joshi H.P., Subramanian I.V., Schnettler E.K., Ghosh G., Rupaimoole R., Evans C., Saluja M., Jing Y., Cristina I., Roy S., et al. Dynamin 2 along with microRNA-199a reciprocally regulate hypoxia-inducible factors and ovarian cancer metastasis. Proc. Natl. Acad. Sci. USA. 2014;111:5331–5336. doi: 10.1073/pnas.1317242111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Schietke R., Warnecke C., Wacker I., Schodel J., Mole D.R., Campean V., Amann K., Goppelt-Struebe M., Behrens J., Eckardt K.U., et al. The lysyl oxidases LOX and LOXL2 are necessary and sufficient to repress E-cadherin in hypoxia: Insights into cellular transformation processes mediated by HIF-1. J. Biol. Chem. 2010;285:6658–6669. doi: 10.1074/jbc.M109.042424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bindra R.S., Gibson S.L., Meng A., Westermark U., Jasin M., Pierce A.J., Bristow R.G., Classon M.K., Glazer P.M. Hypoxia-induced down-regulation of BRCA1 expression by E2Fs. Cancer Res. 2005;65:11597–11604. doi: 10.1158/0008-5472.CAN-05-2119. [DOI] [PubMed] [Google Scholar]
- 97.Boussios S., Karihtala P., Moschetta M., Karathanasi A., Sadauskaite A., Rassy E., Pavlidis N. Combined Strategies with Poly (ADP-Ribose) Polymerase (PARP) Inhibitors for the Treatment of Ovarian Cancer: A Literature Review. Diagnostics. 2019;9:87. doi: 10.3390/diagnostics9030087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Balkwill F. Cancer and the chemokine network. Nat. Rev. Cancer. 2004;4:540–550. doi: 10.1038/nrc1388. [DOI] [PubMed] [Google Scholar]
- 99.Lv Y., Lei Y., Hu Y., Ding W., Zhang C., Fang C. miR-448 negatively regulates ovarian cancer cell growth and metastasis by targeting CXCL12. Clin. Transl. Oncol. 2015;17:903–909. doi: 10.1007/s12094-015-1325-8. [DOI] [PubMed] [Google Scholar]
- 100.Casey R.C., Skubitz A.P. CD44 and beta1 integrins mediate ovarian carcinoma cell migration toward extracellular matrix proteins. Clin. Exp. Metastasis. 2000;18:67–75. doi: 10.1023/A:1026519016213. [DOI] [PubMed] [Google Scholar]
- 101.Santoiemma P.P., Powell D.J., Jr. Tumor infiltrating lymphocytes in ovarian cancer. Cancer Biol. Ther. 2015;16:807–820. doi: 10.1080/15384047.2015.1040960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhou J., Li X., Wu X., Zhang T., Zhu Q., Wang X., Wang H., Wang K., Lin Y., Wang X. Exosomes Released from Tumor-Associated Macrophages Transfer miRNAs That Induce a Treg/Th17 Cell Imbalance in Epithelial Ovarian Cancer. Cancer Immunol. Res. 2018;6:1578–1592. doi: 10.1158/2326-6066.CIR-17-0479. [DOI] [PubMed] [Google Scholar]
- 103.Wang X., Zhu Q., Lin Y., Wu L., Wu X., Wang K., He Q., Xu C., Wan X., Wang X. Crosstalk between TEMs and endothelial cells modulates angiogenesis and metastasis via IGF1-IGF1R signalling in epithelial ovarian cancer. Br. J. Cancer. 2017;117:1371–1382. doi: 10.1038/bjc.2017.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Mantovani A., Sozzani S., Locati M., Allavena P., Sica A. Macrophage polarization: Tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends. Immunol. 2002;23:549–555. doi: 10.1016/S1471-4906(02)02302-5. [DOI] [PubMed] [Google Scholar]
- 105.Jiang B., Zhu S.J., Xiao S.S., Xue M. MiR-217 Inhibits M2-Like Macrophage Polarization by Suppressing Secretion of Interleukin-6 in Ovarian Cancer. Inflammation. 2019;42:1517–1529. doi: 10.1007/s10753-019-01004-2. [DOI] [PubMed] [Google Scholar]
- 106.Xie J., Liu M., Li Y., Nie Y., Mi Q., Zhao S. Ovarian tumor-associated microRNA-20a decreases natural killer cell cytotoxicity by downregulating MICA/B expression. Cell Mol. Immunol. 2014;11:495–502. doi: 10.1038/cmi.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ghadially H., Brown L., Lloyd C., Lewis L., Lewis A., Dillon J., Sainson R., Jovanovic J., Tigue N.J., Bannister D., et al. MHC class I chain-related protein A and B (MICA and MICB) are predominantly expressed intracellularly in tumour and normal tissue. Br. J. Cancer. 2017;116:1208–1217. doi: 10.1038/bjc.2017.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Nam J.W., Rissland O.S., Koppstein D., Abreu-Goodger C., Jan C.H., Agarwal V., Yildirim M.A., Rodriguez A., Bartel D.P. Global analyses of the effect of different cellular contexts on microRNA targeting. Mol. Cell. 2014;53:1031–1043. doi: 10.1016/j.molcel.2014.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.He M., Liu Y., Wang X., Zhang M.Q., Hannon G.J., Huang Z.J. Cell-type-based analysis of microRNA profiles in the mouse brain. Neuron. 2012;73:35–48. doi: 10.1016/j.neuron.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Parikh A., Lee C., Joseph P., Marchini S., Baccarini A., Kolev V., Romualdi C., Fruscio R., Shah H., Wang F., et al. microRNA-181a has a critical role in ovarian cancer progression through the regulation of the epithelial-mesenchymal transition. Nat. Commun. 2014;5:2977. doi: 10.1038/ncomms3977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chen Z., Zhu J., Zhu Y., Wang J. MicroRNA-616 promotes the progression of ovarian cancer by targeting TIMP2. Oncol. Rep. 2018;39:2960–2968. doi: 10.3892/or.2018.6368. [DOI] [PubMed] [Google Scholar]
- 112.Salem M., O’Brien J.A., Bernaudo S., Shawer H., Ye G., Brkic J., Amleh A., Vanderhyden B.C., Refky B., Yang B.B., et al. miR-590-3p Promotes Ovarian Cancer Growth and Metastasis via a Novel FOXA2-Versican Pathway. Cancer Res. 2018;78:4175–4190. doi: 10.1158/0008-5472.CAN-17-3014. [DOI] [PubMed] [Google Scholar]
- 113.Ying X., Wei K., Lin Z., Cui Y., Ding J., Chen Y., Xu B. MicroRNA-125b Suppresses Ovarian Cancer Progression via Suppression of the Epithelial-Mesenchymal Transition Pathway by Targeting the SET Protein. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2016;39:501–510. doi: 10.1159/000445642. [DOI] [PubMed] [Google Scholar]
- 114.Pan L., Meng Q., Li H., Liang K., Li B. LINC00339 promotes cell proliferation, migration, and invasion of ovarian cancer cells via miR-148a-3p/ROCK1 axes. Biomed. Pharmacother. 2019;120:109423. doi: 10.1016/j.biopha.2019.109423. [DOI] [PubMed] [Google Scholar]
- 115.Yan H., Li H., Li P., Li X., Lin J., Zhu L., Silva M.A., Wang X., Wang P., Zhang Z. Long noncoding RNA MLK7-AS1 promotes ovarian cancer cells progression by modulating miR-375/YAP1 axis. J. Exp. Clin. Cancer Res. CR. 2018;37:237. doi: 10.1186/s13046-018-0910-4. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 116.Loginov V.I., Pronina I.V., Burdennyy A.M., Filippova E.A., Kazubskaya T.P., Kushlinsky D.N., Utkin D.O., Khodyrev D.S., Kushlinskii N.E., Dmitriev A.A., et al. Novel miRNA genes deregulated by aberrant methylation in ovarian carcinoma are involved in metastasis. Gene. 2018;662:28–36. doi: 10.1016/j.gene.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 117.Zhang H., Wang Q., Zhao Q., Di W. MiR-124 inhibits the migration and invasion of ovarian cancer cells by targeting SphK1. J. Ovarian Res. 2013;6:84. doi: 10.1186/1757-2215-6-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Xiaohong Z., Lichun F., Na X., Kejian Z., Xiaolan X., Shaosheng W. MiR-203 promotes the growth and migration of ovarian cancer cells by enhancing glycolytic pathway. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2016;37:14989–14997. doi: 10.1007/s13277-016-5415-1. [DOI] [PubMed] [Google Scholar]
- 119.Zhao G., Guo Y., Chen Z., Wang Y., Yang C., Dudas A., Du Z., Liu W., Zou Y., Szabo E., et al. miR-203 Functions as a Tumor Suppressor by Inhibiting Epithelial to Mesenchymal Transition in Ovarian Cancer. J. Cancer Sci. Ther. 2015;7:34–43. doi: 10.4172/1948-5956.1000322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Iorio M.V., Visone R., Di Leva G., Donati V., Petrocca F., Casalini P., Taccioli C., Volinia S., Liu C.G., Alder H., et al. MicroRNA signatures in human ovarian cancer. Cancer Res. 2007;67:8699–8707. doi: 10.1158/0008-5472.CAN-07-1936. [DOI] [PubMed] [Google Scholar]
- 121.Zhang X., Guo G., Wang G., Zhao J., Wang B., Yu X., Ding Y. Profile of differentially expressed miRNAs in high-grade serous carcinoma and clear cell ovarian carcinoma, and the expression of miR-510 in ovarian carcinoma. Mol. Med. Rep. 2015;12:8021–8031. doi: 10.3892/mmr.2015.4485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ye G., Bernaudo S., Peng C. Advances in Ovarian Cancer Management. Future Medicine Ltd.; London, UK: 2012. Etiology and overview. [DOI] [Google Scholar]
- 123.Braicu O.L., Budisan L., Buiga R., Jurj A., Achimas-Cadariu P., Pop L.A., Braicu C., Irimie A., Berindan-Neagoe I. miRNA expression profiling in formalin-fixed paraffin-embedded endometriosis and ovarian cancer samples. Onco Targets Ther. 2017;10:4225–4238. doi: 10.2147/OTT.S137107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Feng W., Dean D.C., Hornicek F.J., Shi H., Duan Z. Exosomes promote pre-metastatic niche formation in ovarian cancer. Mol. Cancer. 2019;18:124. doi: 10.1186/s12943-019-1049-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Yang L., Wei Q.M., Zhang X.W., Sheng Q., Yan X.T. MiR-376a promotion of proliferation and metastases in ovarian cancer: Potential role as a biomarker. Life Sci. 2017;173:62–67. doi: 10.1016/j.lfs.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 126.Zuberi M., Mir R., Das J., Ahmad I., Javid J., Yadav P., Masroor M., Ahmad S., Ray P.C., Saxena A. Expression of serum miR-200a, miR-200b, and miR-200c as candidate biomarkers in epithelial ovarian cancer and their association with clinicopathological features. Clin. Transl. Oncol. 2015;17:779–787. doi: 10.1007/s12094-015-1303-1. [DOI] [PubMed] [Google Scholar]
- 127.Langhe R., Norris L., Saadeh F.A., Blackshields G., Varley R., Harrison A., Gleeson N., Spillane C., Martin C., O’Donnell D.M., et al. A novel serum microRNA panel to discriminate benign from malignant ovarian disease. Cancer Lett. 2015;356:628–636. doi: 10.1016/j.canlet.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 128.Zuberi M., Khan I., Gandhi G., Ray P.C., Saxena A. The conglomeration of diagnostic, prognostic and therapeutic potential of serum miR-199a and its association with clinicopathological features in epithelial ovarian cancer. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2016;37:11259–11266. doi: 10.1007/s13277-016-4993-2. [DOI] [PubMed] [Google Scholar]
- 129.Li Y., Liu C., Liao Y., Wang W., Hu B., Lu X., Cui J. Characterizing the landscape of peritoneal exosomal microRNAs in patients with ovarian cancer by high-throughput sequencing. Oncol. Lett. 2019;17:539–547. doi: 10.3892/ol.2018.9558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhang J., Liu W., Shen F., Ma X., Liu X., Tian F., Zeng W., Xi X., Lin Y. The activation of microRNA-520h-associated TGF-beta1/c-Myb/Smad7 axis promotes epithelial ovarian cancer progression. Cell Death Dis. 2018;9:884. doi: 10.1038/s41419-018-0946-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lin J., Zhang L., Huang H., Huang Y., Huang L., Wang J., Huang S., He L., Zhou Y., Jia W., et al. MiR-26b/KPNA2 axis inhibits epithelial ovarian carcinoma proliferation and metastasis through downregulating OCT4. Oncotarget. 2015;6:23793–23806. doi: 10.18632/oncotarget.4363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lu J., Zhang W., Ding Y., Li X., Song J. Expression of miR-26b in ovarian carcinoma tissues and its correlation with clinicopathology. Oncol. Lett. 2019;17:4417–4422. doi: 10.3892/ol.2019.10117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Vang S., Wu H.T., Fischer A., Miller D.H., MacLaughlan S., Douglass E., Comisar L., Steinhoff M., Collins C., Smith P.J., et al. Identification of ovarian cancer metastatic miRNAs. PLoS ONE. 2013;8:e58226. doi: 10.1371/journal.pone.0058226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wahab N.A., Othman Z., Nasri N.W.M., Mokhtar M.H., Ibrahim S.F., Hamid A.A., Raja Ali R.A., Mokhtar N.M. Inhibition of miR-141 and miR-200a Increase DLC-1 and ZEB2 Expression, Enhance Migration and Invasion in Metastatic Serous Ovarian Cancer. Int. J. Environ. Res. Public Health. 2020;17:2766. doi: 10.3390/ijerph17082766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.McMillen B.D., Aponte M.M., Liu Z., Helenowski I.B., Scholtens D.M., Buttin B.M., Wei J.J. Expression analysis of MIR182 and its associated target genes in advanced ovarian carcinoma. Mod. Pathol. 2012;25:1644–1653. doi: 10.1038/modpathol.2012.118. [DOI] [PubMed] [Google Scholar]
- 136.Liu Z., Liu J., Segura M.F., Shao C., Lee P., Gong Y., Hernando E., Wei J.J. MiR-182 overexpression in tumourigenesis of high-grade serous ovarian carcinoma. J. Pathol. 2012;228:204–215. doi: 10.1002/path.4000. [DOI] [PubMed] [Google Scholar]
- 137.Srivastava A.K., Banerjee A., Cui T., Han C., Cai S., Liu L., Wu D., Cui R., Li Z., Zhang X., et al. Inhibition of miR-328-3p Impairs Cancer Stem Cell Function and Prevents Metastasis in Ovarian Cancer. Cancer Res. 2019;79:2314–2326. doi: 10.1158/0008-5472.CAN-18-3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Wang Y., Zhang X., Tang W., Lin Z., Xu L., Dong R., Li Y., Li J., Zhang Z., Li X., et al. miR-130a upregulates mTOR pathway by targeting TSC1 and is transactivated by NF-kappaB in high-grade serous ovarian carcinoma. Cell Death Differ. 2017;24:2089–2100. doi: 10.1038/cdd.2017.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Liu F., Zhang G., Lv S., Wen X., Liu P. miRNA-301b-3p accelerates migration and invasion of high-grade ovarian serous tumor via targeting CPEB3/EGFR axis. J. Cell Biochem. 2019;120:12618–12627. doi: 10.1002/jcb.28528. [DOI] [PubMed] [Google Scholar]
- 140.Lou Y., Yang X., Wang F., Cui Z., Huang Y. MicroRNA-21 promotes the cell proliferation, invasion and migration abilities in ovarian epithelial carcinomas through inhibiting the expression of PTEN protein. Int. J. Mol. Med. 2010;26:819–827. doi: 10.3892/ijmm_00000530. [DOI] [PubMed] [Google Scholar]
- 141.Su N., Qiu H., Chen Y., Yang T., Yan Q., Wan X. miR-205 promotes tumor proliferation and invasion through targeting ESRRG in endometrial carcinoma. Oncol. Rep. 2013;29:2297–2302. doi: 10.3892/or.2013.2400. [DOI] [PubMed] [Google Scholar]
- 142.Wei Z., Liu Y., Wang Y., Zhang Y., Luo Q., Man X., Wei F., Yu X. Downregulation of Foxo3 and TRIM31 by miR-551b in side population promotes cell proliferation, invasion, and drug resistance of ovarian cancer. Med. Oncol. (Northwood Lond. Engl.) 2016;33:126. doi: 10.1007/s12032-016-0842-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Chaluvally-Raghavan P., Jeong K.J., Pradeep S., Silva A.M., Yu S., Liu W., Moss T., Rodriguez-Aguayo C., Zhang D., Ram P., et al. Direct Upregulation of STAT3 by MicroRNA-551b-3p Deregulates Growth and Metastasis of Ovarian Cancer. Cell Rep. 2016;15:1493–1504. doi: 10.1016/j.celrep.2016.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Han X., Zhang Y., Wang D., Fu X., Li M., Wang A. Upregulation of microRNA-18b induces phosphatase and tensin homolog to accelerate the migration and invasion abilities of ovarian cancer. Oncol. Lett. 2017;14:5631–5637. doi: 10.3892/ol.2017.6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Liu D.T., Yao H.R., Li Y.Y., Song Y.Y., Su M.Y. MicroRNA-19b promotes the migration and invasion of ovarian cancer cells by inhibiting the PTEN/AKT signaling pathway. Oncol. Lett. 2018;16:559–565. doi: 10.3892/ol.2018.8695. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 146.Zhuang R.J., Bai X.X., Liu W. MicroRNA-23a depletion promotes apoptosis of ovarian cancer stem cell and inhibits cell migration by targeting DLG2. Cancer Biol. Ther. 2019;20:897–911. doi: 10.1080/15384047.2019.1579960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Xia Y., Gao Y. MicroRNA-181b promotes ovarian cancer cell growth and invasion by targeting LATS2. Biochem. Biophys. Res. Commun. 2014;447:446–451. doi: 10.1016/j.bbrc.2014.04.027. [DOI] [PubMed] [Google Scholar]
- 148.Wang A., Jin C., Li H., Qin Q., Li L. LncRNA ADAMTS9-AS2 regulates ovarian cancer progression by targeting miR-182-5p/FOXF2 signaling pathway. Int. J. Biol. Macromol. 2018;120:1705–1713. doi: 10.1016/j.ijbiomac.2018.09.179. [DOI] [PubMed] [Google Scholar]
- 149.Liang T., Li L., Cheng Y., Ren C., Zhang G. MicroRNA-194 promotes the growth, migration, and invasion of ovarian carcinoma cells by targeting protein tyrosine phosphatase nonreceptor type 12. Onco. Targets Ther. 2016;9:4307–4315. doi: 10.2147/OTT.S90976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Fan Y., Fan J., Huang L., Ye M., Huang Z., Wang Y., Li Q., Huang J. Increased expression of microRNA-196a predicts poor prognosis in human ovarian carcinoma. Int. J. Clin Exp. Pathol. 2015;8:4132–4137. [PMC free article] [PubMed] [Google Scholar]
- 151.Wei J., Zhang L., Li J., Zhu S., Tai M., Mason C.W., Chapman J.A., Reynolds E.A., Weiner C.P., Zhou H.H. MicroRNA-205 promotes cell invasion by repressing TCF21 in human ovarian cancer. J. Ovarian Res. 2017;10:33. doi: 10.1186/s13048-017-0328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Chu P., Liang A., Jiang A., Zong L. miR-205 regulates the proliferation and invasion of ovarian cancer cells via suppressing PTEN/SMAD4 expression. Oncol. Lett. 2018;15:7571–7578. doi: 10.3892/ol.2018.8313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Li J., Hu K., Gong G., Zhu D., Wang Y., Liu H., Wu X. Upregulation of MiR-205 transcriptionally suppresses SMAD4 and PTEN and contributes to human ovarian cancer progression. Sci. Rep. 2017;7:41330. doi: 10.1038/srep41330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Liu H., Pan Y., Han X., Liu J., Li R. MicroRNA-216a promotes the metastasis and epithelial-mesenchymal transition of ovarian cancer by suppressing the PTEN/AKT pathway. Onco. Targets Ther. 2017;10:2701–2709. doi: 10.2147/OTT.S114318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Zhao W., Han T., Li B., Ma Q., Yang P., Li H. miR-552 promotes ovarian cancer progression by regulating PTEN pathway. J. Ovarian Res. 2019;12:121. doi: 10.1186/s13048-019-0589-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Rupaimoole R., Ivan C., Yang D., Gharpure K.M., Wu S.Y., Pecot C.V., Previs R.A., Nagaraja A.S., Armaiz-Pena G.N., McGuire M., et al. Hypoxia-upregulated microRNA-630 targets Dicer, leading to increased tumor progression. Oncogene. 2016;35:4312–4320. doi: 10.1038/onc.2015.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Ying X., Li-ya Q., Feng Z., Yin W., Ji-hong L. MiR-939 promotes the proliferation of human ovarian cancer cells by repressing APC2 expression. Biomed. Pharmacother. 2015;71:64–69. doi: 10.1016/j.biopha.2015.02.020. [DOI] [PubMed] [Google Scholar]
- 158.Tang M., Jiang L., Lin Y., Wu X., Wang K., He Q., Wang X., Li W. Platelet microparticle-mediated transfer of miR-939 to epithelial ovarian cancer cells promotes epithelial to mesenchymal transition. Oncotarget. 2017;8:97464–97475. doi: 10.18632/oncotarget.22136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Salem M., Shan Y., Bernaudo S., Peng C. miR-590-3p Targets Cyclin G2 and FOXO3 to Promote Ovarian Cancer Cell Proliferation, Invasion, and Spheroid Formation. Int. J. Mol. Sci. 2019;20:1810. doi: 10.3390/ijms20081810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Zhou J., Gong G., Tan H., Dai F., Zhu X., Chen Y., Wang J., Liu Y., Chen P., Wu X., et al. Urinary microRNA-30a-5p is a potential biomarker for ovarian serous adenocarcinoma. Oncol. Rep. 2015;33:2915–2923. doi: 10.3892/or.2015.3937. [DOI] [PubMed] [Google Scholar]
- 161.Dong R., Liu X., Zhang Q., Jiang Z., Li Y., Wei Y., Li Y., Yang Q., Liu J., Wei J.J., et al. miR-145 inhibits tumor growth and metastasis by targeting metadherin in high-grade serous ovarian carcinoma. Oncotarget. 2014;5:10816–10829. doi: 10.18632/oncotarget.2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Lam S.S., Ip C.K., Mak A.S., Wong A.S. A novel p70 S6 kinase-microRNA biogenesis axis mediates multicellular spheroid formation in ovarian cancer progression. Oncotarget. 2016;7:38064–38077. doi: 10.18632/oncotarget.9345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kim T.H., Song J.Y., Park H., Jeong J.Y., Kwon A.Y., Heo J.H., Kang H., Kim G., An H.J. miR-145, targeting high-mobility group A2, is a powerful predictor of patient outcome in ovarian carcinoma. Cancer Lett. 2015;356:937–945. doi: 10.1016/j.canlet.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 164.Pan Y., Robertson G., Pedersen L., Lim E., Hernandez-Herrera A., Rowat A.C., Patil S.L., Chan C.K., Wen Y., Zhang X., et al. miR-509-3p is clinically significant and strongly attenuates cellular migration and multi-cellular spheroids in ovarian cancer. Oncotarget. 2016;7:25930–25948. doi: 10.18632/oncotarget.8412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wang Y., Yan S., Liu X., Zhang W., Li Y., Dong R., Zhang Q., Yang Q., Yuan C., Shen K., et al. miR-1236-3p represses the cell migration and invasion abilities by targeting ZEB1 in high-grade serous ovarian carcinoma. Oncol. Rep. 2014;31:1905–1910. doi: 10.3892/or.2014.3046. [DOI] [PubMed] [Google Scholar]
- 166.Zhang P., Zhu J., Zheng Y., Zhang H., Sun H., Gao S. miRNA-574-3p inhibits metastasis and chemoresistance of epithelial ovarian cancer (EOC) by negatively regulating epidermal growth factor receptor (EGFR) Am. J. Transl. Res. 2019;11:4151–4165. [PMC free article] [PubMed] [Google Scholar]
- 167.Liang H., Zhao X., Wang C., Sun J., Chen Y., Wang G., Fang L., Yang R., Yu M., Gu Y., et al. Systematic analyses reveal long non-coding RNA (PTAF)-mediated promotion of EMT and invasion-metastasis in serous ovarian cancer. Mol. Cancer. 2018;17:96. doi: 10.1186/s12943-018-0844-7. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 168.Liang H., Yu T., Han Y., Jiang H., Wang C., You T., Zhao X., Shan H., Yang R., Yang L., et al. LncRNA PTAR promotes EMT and invasion-metastasis in serous ovarian cancer by competitively binding miR-101-3p to regulate ZEB1 expression. Mol. Cancer. 2018;17:119. doi: 10.1186/s12943-018-0870-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Liang H., Yu M., Yang R., Zhang L., Zhang L., Zhu D., Luo H., Hong Y., Yu T., Sun J., et al. A PTAL-miR-101-FN1 Axis Promotes EMT and Invasion-Metastasis in Serous Ovarian Cancer. Mol. Ther. Oncolytics. 2020;16:53–62. doi: 10.1016/j.omto.2019.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Gong C., Yang Z., Wu F., Han L., Liu Y., Gong W. miR-17 inhibits ovarian cancer cell peritoneal metastasis by targeting ITGA5 and ITGB1. Oncol. Rep. 2016;36:2177–2183. doi: 10.3892/or.2016.4985. [DOI] [PubMed] [Google Scholar]
- 171.Chen S., Chen X., Xiu Y.L., Sun K.X., Zhao Y. Inhibition of Ovarian Epithelial Carcinoma Tumorigenesis and Progression by microRNA 106b Mediated through the RhoC Pathway. PLoS ONE. 2015;10:e0125714. doi: 10.1371/journal.pone.0125714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Yan J., Jiang J.Y., Meng X.N., Xiu Y.L., Zong Z.H. MiR-23b targets cyclin G1 and suppresses ovarian cancer tumorigenesis and progression. J. Exp. Clin. Cancer Res. CR. 2016;35:31. doi: 10.1186/s13046-016-0307-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Xu H., Mao H.L., Zhao X.R., Li Y., Liu P.S. MiR-29c-3p, a target miRNA of LINC01296, accelerates tumor malignancy: Therapeutic potential of a LINC01296/miR-29c-3p axis in ovarian cancer. J. Ovarian Res. 2020;13:31. doi: 10.1186/s13048-020-00631-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zhang R.R., Wang L.M., Shen J.J. Overexpression of miR-32 inhibits the proliferation and metastasis of ovarian cancer cells by targeting BTLA. Eur. Rev. Med. Pharmacol. Sci. 2020;24:4671–4678. doi: 10.26355/eurrev_202005_21154. [DOI] [PubMed] [Google Scholar]
- 175.Dong P., Xiong Y., Watari H., Hanley S.J., Konno Y., Ihira K., Yamada T., Kudo M., Yue J., Sakuragi N. MiR-137 and miR-34a directly target Snail and inhibit EMT, invasion and sphere-forming ability of ovarian cancer cells. J. Exp. Clin. Cancer Res. CR. 2016;35:132. doi: 10.1186/s13046-016-0415-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Peng D.X., Luo M., Qiu L.W., He Y.L., Wang X.F. Prognostic implications of microRNA-100 and its functional roles in human epithelial ovarian cancer. Oncol. Rep. 2012;27:1238–1244. doi: 10.3892/or.2012.1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Yuan L., Li S., Zhou Q., Wang D., Zou D., Shu J., Huang Y. MiR-124 inhibits invasion and induces apoptosis of ovarian cancer cells by targeting programmed cell death 6. Oncol. Lett. 2017;14:7311–7317. doi: 10.3892/ol.2017.7157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Cao Y., Shi H., Ren F., Jia Y., Zhang R. Long non-coding RNA CCAT1 promotes metastasis and poor prognosis in epithelial ovarian cancer. Exp. Cell Res. 2017;359:185–194. doi: 10.1016/j.yexcr.2017.07.030. [DOI] [PubMed] [Google Scholar]
- 179.Luo J., Zhou J., Cheng Q., Zhou C., Ding Z. Role of microRNA-133a in epithelial ovarian cancer pathogenesis and progression. Oncol. Lett. 2014;7:1043–1048. doi: 10.3892/ol.2014.1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Zhang Y., Dun Y., Zhou S., Huang X.H. LncRNA HOXD-AS1 promotes epithelial ovarian cancer cells proliferation and invasion by targeting miR-133a-3p and activating Wnt/beta-catenin signaling pathway. Biomed. Pharmacother. 2017;96:1216–1221. doi: 10.1016/j.biopha.2017.11.096. [DOI] [PubMed] [Google Scholar]
- 181.Yang L., Hou J., Cui X.H., Suo L.N., Lv Y.W. MiR-133b regulates the expression of CTGF in epithelial-mesenchymal transition of ovarian cancer. Eur. Rev. Med. Pharmacol. Sci. 2017;21:5602–5609. doi: 10.26355/eurrev_201712_14001. [DOI] [PubMed] [Google Scholar]
- 182.Tang W., Jiang Y., Mu X., Xu L., Cheng W., Wang X. MiR-135a functions as a tumor suppressor in epithelial ovarian cancer and regulates HOXA10 expression. Cell Signal. 2014;26:1420–1426. doi: 10.1016/j.cellsig.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 183.Duan S., Dong X., Hai J., Jiang J., Wang W., Yang J., Zhang W., Chen C. MicroRNA-135a-3p is downregulated and serves as a tumour suppressor in ovarian cancer by targeting CCR2. Biomed. Pharmacother. 2018;107:712–720. doi: 10.1016/j.biopha.2018.08.044. [DOI] [PubMed] [Google Scholar]
- 184.Yeh Y.M., Chuang C.M., Chao K.C., Wang L.H. MicroRNA-138 suppresses ovarian cancer cell invasion and metastasis by targeting SOX4 and HIF-1alpha. Int. J. Cancer. 2013;133:867–878. doi: 10.1002/ijc.28086. [DOI] [PubMed] [Google Scholar]
- 185.Qu M., Zhu Y., Jin M. MicroRNA-138 inhibits SOX12 expression and the proliferation, invasion and migration of ovarian cancer cells. Exp. Ther. Med. 2018;16:1629–1638. doi: 10.3892/etm.2018.6375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Liu J., Jin S., Wang R. MicroRNA139 suppressed tumor cell proliferation, migration and invasion by directly targeting HDGF in epithelial ovarian cancer. Mol. Med. Rep. 2017;16:3379–3386. doi: 10.3892/mmr.2017.6956. [DOI] [PubMed] [Google Scholar]
- 187.Xue F., Li Q.R., Xu Y.H., Zhou H.B. MicroRNA-139-3p Inhibits the Growth and Metastasis of Ovarian Cancer by Inhibiting ELAVL1. Onco Targets Ther. 2019;12:8935–8945. doi: 10.2147/OTT.S210739. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 188.Wang Y., Li J., Xu C., Zhang X. MicroRNA-139-5p Inhibits Cell Proliferation and Invasion by Targeting RHO-Associated Coiled-Coil-Containing Protein Kinase 2 in Ovarian Cancer. Oncol. Res. 2018;26:411–420. doi: 10.3727/096504017X14974343584989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Liu X., Li Y., Wen J., Qi T., Wang Y. Long non-coding RNA TTN-AS1 promotes tumorigenesis of ovarian cancer through modulating the miR-139-5p/ROCK2 axis. Biomed. Pharmacother. 2020;125:109882. doi: 10.1016/j.biopha.2020.109882. [DOI] [PubMed] [Google Scholar]
- 190.Zhou J., Zhang X., Li W., Chen Y. MicroRNA-145-5p regulates the proliferation of epithelial ovarian cancer cells via targeting SMAD4. J. Ovarian Res. 2020;13:54. doi: 10.1186/s13048-020-00656-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Li L.W., Xiao H.Q., Ma R., Yang M., Li W., Lou G. miR-152 is involved in the proliferation and metastasis of ovarian cancer through repression of ERBB3. Int. J. Mol. Med. 2018;41:1529–1535. doi: 10.3892/ijmm.2017.3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Jin M., Yang Z., Ye W., Xu H., Hua X. MicroRNA-150 predicts a favorable prognosis in patients with epithelial ovarian cancer, and inhibits cell invasion and metastasis by suppressing transcriptional repressor ZEB1. PLoS ONE. 2014;9:e103965. doi: 10.1371/journal.pone.0103965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Zhu X., Shen H., Yin X., Long L., Xie C., Liu Y., Hui L., Lin X., Fang Y., Cao Y., et al. miR-186 regulation of Twist1 and ovarian cancer sensitivity to cisplatin. Oncogene. 2016;35:323–332. doi: 10.1038/onc.2015.84. [DOI] [PubMed] [Google Scholar]
- 194.Mitra A.K., Chiang C.Y., Tiwari P., Tomar S., Watters K.M., Peter M.E., Lengyel E. Microenvironment-induced downregulation of miR-193b drives ovarian cancer metastasis. Oncogene. 2015;34:5923–5932. doi: 10.1038/onc.2015.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Li H., Xu Y., Qiu W., Zhao D., Zhang Y. Tissue miR-193b as a Novel Biomarker for Patients with Ovarian Cancer. Med. Sci. Monit. 2015;21:3929–3934. doi: 10.12659/MSM.895407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Yu H.Y., Pan S.S. MiR-202-5p suppressed cell proliferation, migration and invasion in ovarian cancer via regulating HOXB2. Eur. Rev. Med. Pharmacol. Sci. 2020;24:2256–2263. doi: 10.26355/eurrev_202003_20491. [DOI] [PubMed] [Google Scholar]
- 197.Dai C., Xie Y., Zhuang X., Yuan Z. MiR-206 inhibits epithelial ovarian cancer cells growth and invasion via blocking c-Met/AKT/mTOR signaling pathway. Biomed. Pharmacother. 2018;104:763–770. doi: 10.1016/j.biopha.2018.05.077. [DOI] [PubMed] [Google Scholar]
- 198.Chang L., Guo R., Yuan Z., Shi H., Zhang D. LncRNA HOTAIR Regulates CCND1 and CCND2 Expression by Sponging miR-206 in Ovarian Cancer. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2018;49:1289–1303. doi: 10.1159/000493408. [DOI] [PubMed] [Google Scholar]
- 199.Lin Y., Jin Y., Xu T., Zhou S., Cui M. MicroRNA-215 targets NOB1 and inhibits growth and invasion of epithelial ovarian cancer. Am. J. Transl. Res. 2017;9:466–477. [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 200.Li J., Li D., Zhang W. Tumor suppressor role of miR-217 in human epithelial ovarian cancer by targeting IGF1R. Oncol. Rep. 2016;35:1671–1679. doi: 10.3892/or.2015.4498. [DOI] [PubMed] [Google Scholar]
- 201.Li N., Wang L., Tan G., Guo Z., Liu L., Yang M., He J. MicroRNA-218 inhibits proliferation and invasion in ovarian cancer by targeting Runx2. Oncotarget. 2017;8:91530–91541. doi: 10.18632/oncotarget.21069. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 202.Wei C., Zhang X., He S., Liu B., Han H., Sun X. MicroRNA-219-5p inhibits the proliferation, migration, and invasion of epithelial ovarian cancer cells by targeting the Twist/Wnt/beta-catenin signaling pathway. Gene. 2017;637:25–32. doi: 10.1016/j.gene.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 203.Xing F., Song Z., He Y. MiR-219-5p inhibits growth and metastasis of ovarian cancer cells by targeting HMGA2. Biol. Res. 2018;51:50. doi: 10.1186/s40659-018-0199-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Cao J., Cai J., Huang D., Han Q., Chen Y., Yang Q., Yang C., Kuang Y., Li D., Wang Z. miR-335 represents an independent prognostic marker in epithelial ovarian cancer. Am. J. Clin. Pathol. 2014;141:437–442. doi: 10.1309/AJCPLYTZGB54ISZC. [DOI] [PubMed] [Google Scholar]
- 205.Zhang R., Shi H., Ren F., Liu Z., Ji P., Zhang W., Wang W. Down-regulation of miR-338-3p and Up-regulation of MACC1 Indicated Poor Prognosis of Epithelial Ovarian Cancer Patients. J. Cancer. 2019;10:1385–1392. doi: 10.7150/jca.29502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Wen C., Liu X., Ma H., Zhang W., Li H. miR3383p suppresses tumor growth of ovarian epithelial carcinoma by targeting Runx2. Int. J. Oncol. 2015;46:2277–2285. doi: 10.3892/ijo.2015.2929. [DOI] [PubMed] [Google Scholar]
- 207.Huang Z., Li Q., Luo K., Zhang Q., Geng J., Zhou X., Xu Y., Qian M., Zhang J.A., Ji L., et al. miR-340-FHL2 axis inhibits cell growth and metastasis in ovarian cancer. Cell Death Dis. 2019;10:372. doi: 10.1038/s41419-019-1604-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Li P., Sun Y., Liu Q. MicroRNA-340 Induces Apoptosis and Inhibits Metastasis of Ovarian Cancer Cells by Inactivation of NF-x03BA;B1. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2016;38:1915–1927. doi: 10.1159/000445553. [DOI] [PubMed] [Google Scholar]
- 209.Lin Y., Xu T., Zhou S., Cui M. MicroRNA-363 inhibits ovarian cancer progression by inhibiting NOB1. Oncotarget. 2017;8:101649–101658. doi: 10.18632/oncotarget.21417. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 210.Wang Y., Xu C., Wang Y., Zhang X. MicroRNA-365 inhibits ovarian cancer progression by targeting Wnt5a. Am. J. Cancer Res. 2017;7:1096–1106. [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 211.Zhang Y., Zhao F.J., Chen L.L., Wang L.Q., Nephew K.P., Wu Y.L., Zhang S. MiR-373 targeting of the Rab22a oncogene suppresses tumor invasion and metastasis in ovarian cancer. Oncotarget. 2014;5:12291–12303. doi: 10.18632/oncotarget.2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Zhang Z., Cheng J., Wu Y., Qiu J., Sun Y., Tong X. LncRNA HOTAIR controls the expression of Rab22a by sponging miR-373 in ovarian cancer. Mol. Med. Rep. 2016;14:2465–2472. doi: 10.3892/mmr.2016.5572. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 213.Yu R., Cai L., Chi Y., Ding X., Wu X. miR377 targets CUL4A and regulates metastatic capability in ovarian cancer. Int. J. Mol. Med. 2018;41:3147–3156. doi: 10.3892/ijmm.2018.3540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Yang A., Wang X., Yu C., Jin Z., Wei L., Cao J., Wang Q., Zhang M., Zhang L., Zhang L., et al. microRNA-494 is a potential prognostic marker and inhibits cellular proliferation, migration and invasion by targeting SIRT1 in epithelial ovarian cancer. Oncol. Lett. 2017;14:3177–3184. doi: 10.3892/ol.2017.6501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Liu W., Yang Y.J., An Q. LINC00963 Promotes Ovarian Cancer Proliferation, Migration and EMT via the miR-378g /CHI3L1 Axis. Cancer Manag. Res. 2020;12:463–473. doi: 10.2147/CMAR.S229083. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 216.Ye W., Ni Z., Yicheng S., Pan H., Huang Y., Xiong Y., Liu T. Anisomycin inhibits angiogenesis in ovarian cancer by attenuating the molecular sponge effect of the lncRNAMeg3/miR421/PDGFRA axis. Int. J. Oncol. 2019;55:1296–1312. doi: 10.3892/ijo.2019.4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Muys B.R., Sousa J.F., Placa J.R., de Araujo L.F., Sarshad A.A., Anastasakis D.G., Wang X., Li X.L., de Molfetta G.A., Ramao A., et al. miR-450a Acts as a Tumor Suppressor in Ovarian Cancer by Regulating Energy Metabolism. Cancer Res. 2019;79:3294–3305. doi: 10.1158/0008-5472.CAN-19-0490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Xu L., Li H., Su L., Lu Q., Liu Z. MicroRNA455 inhibits cell proliferation and invasion of epithelial ovarian cancer by directly targeting Notch1. Mol. Med. Rep. 2017;16:9777–9785. doi: 10.3892/mmr.2017.7790. [DOI] [PubMed] [Google Scholar]
- 219.Jiang H.W., Li L., Jiang P., Wang Y.F. MicroRNA-489 targets XIAP to inhibit the biological progression of ovarian cancer via regulating PI3K/Akt signaling pathway and epithelial-to-mesenchymal transition. Eur. Rev. Med. Pharmacol. Sci. 2020;24:4113–4122. doi: 10.26355/eurrev_202004_20990. [DOI] [PubMed] [Google Scholar]
- 220.Wang W., Ren F., Wu Q., Jiang D., Li H., Peng Z., Wang J., Shi H. MicroRNA-497 inhibition of ovarian cancer cell migration and invasion through targeting of SMAD specific E3 ubiquitin protein ligase 1. Biochem. Biophys. Res. Commun. 2014;449:432–437. doi: 10.1016/j.bbrc.2014.05.053. [DOI] [PubMed] [Google Scholar]
- 221.Park G.B., Kim D. MicroRNA-503-5p Inhibits the CD97-Mediated JAK2/STAT3 Pathway in Metastatic or Paclitaxel-Resistant Ovarian Cancer Cells. Neoplasia. 2019;21:206–215. doi: 10.1016/j.neo.2018.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Yang D., Sun Y., Hu L., Zheng H., Ji P., Pecot C.V., Zhao Y., Reynolds S., Cheng H., Rupaimoole R., et al. Integrated analyses identify a master microRNA regulatory network for the mesenchymal subtype in serous ovarian cancer. Cancer Cell. 2013;23:186–199. doi: 10.1016/j.ccr.2012.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Wei H., Tang Q.L., Zhang K., Sun J.J., Ding R.F. miR-532-5p is a prognostic marker and suppresses cells proliferation and invasion by targeting TWIST1 in epithelial ovarian cancer. Eur. Rev. Med. Pharmacol. Sci. 2018;22:5842–5850. doi: 10.26355/eurrev_201809_15911. [DOI] [PubMed] [Google Scholar]
- 224.Sun X., Cui M., Zhang A., Tong L., Wang K., Li K., Wang X., Sun Z., Zhang H. MiR-548c impairs migration and invasion of endometrial and ovarian cancer cells via downregulation of Twist. J. Exp. Clin. Cancer Res. CR. 2016;35:10. doi: 10.1186/s13046-016-0288-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Yang L., Ma H.L. MiRNA-584 suppresses the progression of ovarian cancer by negatively regulating LPIN1. Eur. Rev. Med. Pharmacol. Sci. 2020;24:1062–1071. doi: 10.26355/eurrev_202002_20156. [DOI] [PubMed] [Google Scholar]
- 226.Wang J., Ding W., Xu Y., Tao E., Mo M., Xu W., Cai X., Chen X., Yuan J., Wu X. Long non-coding RNA RHPN1-AS1 promotes tumorigenesis and metastasis of ovarian cancer by acting as a ceRNA against miR-596 and upregulating LETM1. Aging (Albany NY) 2020;12:4558–4572. doi: 10.18632/aging.102911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Yu H., Xu Y., Zhang D., Liu G. Long noncoding RNA LUCAT1 promotes malignancy of ovarian cancer through regulation of miR-612/HOXA13 pathway. Biochem Biophys. Res. Commun. 2018;503:2095–2100. doi: 10.1016/j.bbrc.2018.07.165. [DOI] [PubMed] [Google Scholar]
- 228.Duan M., Fang M., Wang C., Wang H., Li M. LncRNA EMX2OS Induces Proliferation, Invasion and Sphere Formation of Ovarian Cancer Cells via Regulating the miR-654-3p/AKT3/PD-L1 Axis. Cancer Manag. Res. 2020;12:2141–2154. doi: 10.2147/CMAR.S229013. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 229.Liu J., Jiang Y., Wan Y., Zhou S., Thapa S., Cheng W. MicroRNA665 suppresses the growth and migration of ovarian cancer cells by targeting HOXA10. Mol. Med. Rep. 2018;18:2661–2668. doi: 10.3892/mmr.2018.9252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Xia B., Lin M., Dong W., Chen H., Li B., Zhang X., Hou Y., Lou G. Upregulation of miR-874-3p and miR-874-5p inhibits epithelial ovarian cancer malignancy via SIK2. J. Biochem. Mol. Toxicol. 2018;32:e22168. doi: 10.1002/jbt.22168. [DOI] [PubMed] [Google Scholar]
- 231.Li C., Yu S., Wu S., Ni Y., Pan Z. MicroRNA-936 targets FGF2 to inhibit epithelial ovarian cancer aggressiveness by deactivating the PI3K/Akt pathway. Onco Targets Ther. 2019;12:5311–5322. doi: 10.2147/OTT.S213231. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 232.Dasari S., Pandhiri T., Grassi T., Visscher D.W., Multinu F., Agarwal K., Mariani A., Shridhar V., Mitra A.K. Signals from the Metastatic Niche Regulate Early and Advanced Ovarian Cancer Metastasis through miR-4454 Downregulation. Mol. Cancer Res. MCR. 2020;18:1202–1217. doi: 10.1158/1541-7786.MCR-19-1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Liu L., Ning Y., Yi J., Yuan J., Fang W., Lin Z., Zeng Z. miR-6089/MYH9/beta-catenin/c-Jun negative feedback loop inhibits ovarian cancer carcinogenesis and progression. Biomed. Pharmacother. 2020;125:109865. doi: 10.1016/j.biopha.2020.109865. [DOI] [PubMed] [Google Scholar]
- 234.Kanlikilicer P., Rashed M.H., Bayraktar R., Mitra R., Ivan C., Aslan B., Zhang X., Filant J., Silva A.M., Rodriguez-Aguayo C., et al. Ubiquitous Release of Exosomal Tumor Suppressor miR-6126 from Ovarian Cancer Cells. Cancer Res. 2016;76:7194–7207. doi: 10.1158/0008-5472.CAN-16-0714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Yang J., Li G., Zhang K. MiR-125a regulates ovarian cancer proliferation and invasion by repressing GALNT14 expression. Biomed. Pharmacother. 2016;80:381–387. doi: 10.1016/j.biopha.2015.12.027. [DOI] [PubMed] [Google Scholar]
- 236.Cowden Dahl K.D., Dahl R., Kruichak J.N., Hudson L.G. The epidermal growth factor receptor responsive miR-125a represses mesenchymal morphology in ovarian cancer cells. Neoplasia. 2009;11:1208–1215. doi: 10.1593/neo.09942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Yang L., Zhang X., Ma Y., Zhao X., Li B., Wang H. Ascites promotes cell migration through the repression of miR-125b in ovarian cancer. Oncotarget. 2017;8:51008–51015. doi: 10.18632/oncotarget.16846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Zuberi M., Khan I., Mir R., Gandhi G., Ray P.C., Saxena A. Utility of Serum miR-125b as a Diagnostic and Prognostic Indicator and Its Alliance with a Panel of Tumor Suppressor Genes in Epithelial Ovarian Cancer. PLoS ONE. 2016;11:e0153902. doi: 10.1371/journal.pone.0153902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Wei L.Q., Liang H.T., Qin D.C., Jin H.F., Zhao Y., She M.C. MiR-212 exerts suppressive effect on SKOV3 ovarian cancer cells through targeting HBEGF. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2014;35:12427–12434. doi: 10.1007/s13277-014-2560-2. [DOI] [PubMed] [Google Scholar]
- 240.Duan Y., Dong Y., Dang R., Hu Z., Yang Y., Hu Y., Cheng J. MiR-122 inhibits epithelial mesenchymal transition by regulating P4HA1 in ovarian cancer cells. Cell Biol. Int. 2018;42:1564–1574. doi: 10.1002/cbin.11052. [DOI] [PubMed] [Google Scholar]
- 241.Gong L., Wang C., Gao Y., Wang J. Decreased expression of microRNA-148a predicts poor prognosis in ovarian cancer and associates with tumor growth and metastasis. Biomed. Pharmacother. 2016;83:58–63. doi: 10.1016/j.biopha.2016.05.049. [DOI] [PubMed] [Google Scholar]
- 242.Zhou B., Xu H., Xia M., Sun C., Li N., Guo E., Guo L., Shan W., Lu H., Wu Y., et al. Overexpressed miR-9 promotes tumor metastasis via targeting E-cadherin in serous ovarian cancer. Front. Med. 2017;11:214–222. doi: 10.1007/s11684-017-0518-7. [DOI] [PubMed] [Google Scholar]
- 243.Laios A., O’Toole S., Flavin R., Martin C., Kelly L., Ring M., Finn S.P., Barrett C., Loda M., Gleeson N., et al. Potential role of miR-9 and miR-223 in recurrent ovarian cancer. Mol. Cancer. 2008;7:35. doi: 10.1186/1476-4598-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Tang H., Yao L., Tao X., Yu Y., Chen M., Zhang R., Xu C. miR-9 functions as a tumor suppressor in ovarian serous carcinoma by targeting TLN1. Int. J. Mol. Med. 2013;32:381–388. doi: 10.3892/ijmm.2013.1400. [DOI] [PubMed] [Google Scholar]
- 245.Mak C.S., Yung M.M., Hui L.M., Leung L.L., Liang R., Chen K., Liu S.S., Qin Y., Leung T.H., Lee K.F., et al. MicroRNA-141 enhances anoikis resistance in metastatic progression of ovarian cancer through targeting KLF12/Sp1/survivin axis. Mol. Cancer. 2017;16:11. doi: 10.1186/s12943-017-0582-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Mateescu B., Batista L., Cardon M., Gruosso T., de Feraudy Y., Mariani O., Nicolas A., Meyniel J.P., Cottu P., Sastre-Garau X., et al. miR-141 and miR-200a act on ovarian tumorigenesis by controlling oxidative stress response. Nat. Med. 2011;17:1627–1635. doi: 10.1038/nm.2512. [DOI] [PubMed] [Google Scholar]
- 247.Ye Q., Lei L., Shao L., Shi J., Jia J., Tong X. MicroRNA141 inhibits epithelialmesenchymal transition, and ovarian cancer cell migration and invasion. Mol. Med. Rep. 2017;16:6743–6749. doi: 10.3892/mmr.2017.7482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Suo H.B., Zhang K.C., Zhao J. MiR-200a promotes cell invasion and migration of ovarian carcinoma by targeting PTEN. Eur. Rev. Med. Pharmacol. Sci. 2018;22:4080–4089. doi: 10.26355/eurrev_201807_15398. [DOI] [PubMed] [Google Scholar]
- 249.Pecot C.V., Rupaimoole R., Yang D., Akbani R., Ivan C., Lu C., Wu S., Han H.D., Shah M.Y., Rodriguez-Aguayo C., et al. Tumour angiogenesis regulation by the miR-200 family. Nat. Commun. 2013;4:2427. doi: 10.1038/ncomms3427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Sun Q., Zou X., Zhang T., Shen J., Yin Y., Xiang J. The role of miR-200a in vasculogenic mimicry and its clinical significance in ovarian cancer. Gynecol. Oncol. 2014;132:730–738. doi: 10.1016/j.ygyno.2014.01.047. [DOI] [PubMed] [Google Scholar]
- 251.Nam E.J., Yoon H., Kim S.W., Kim H., Kim Y.T., Kim J.H., Kim J.W., Kim S. MicroRNA expression profiles in serous ovarian carcinoma. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2008;14:2690–2695. doi: 10.1158/1078-0432.CCR-07-1731. [DOI] [PubMed] [Google Scholar]
- 252.Lu Y.M., Shang C., Ou Y.L., Yin D., Li Y.N., Li X., Wang N., Zhang S.L. miR-200c modulates ovarian cancer cell metastasis potential by targeting zinc finger E-box-binding homeobox 2 (ZEB2) expression. Med. Oncol. (Northwood Lond. Engl.) 2014;31:134. doi: 10.1007/s12032-014-0134-1. [DOI] [PubMed] [Google Scholar]
- 253.Cochrane D.R., Spoelstra N.S., Howe E.N., Nordeen S.K., Richer J.K. MicroRNA-200c mitigates invasiveness and restores sensitivity to microtubule-targeting chemotherapeutic agents. Mol. Cancer Ther. 2009;8:1055–1066. doi: 10.1158/1535-7163.MCT-08-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Wang B., Li X., Zhao G., Yan H., Dong P., Watari H., Sims M., Li W., Pfeffer L.M., Guo Y., et al. miR-203 inhibits ovarian tumor metastasis by targeting BIRC5 and attenuating the TGFbeta pathway. J. Exp. Clin. Cancer Res. CR. 2018;37:235. doi: 10.1186/s13046-018-0906-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Zhang L., Huang J., Yang N., Greshock J., Megraw M.S., Giannakakis A., Liang S., Naylor T.L., Barchetti A., Ward M.R., et al. microRNAs exhibit high frequency genomic alterations in human cancer. Proc. Natl. Acad. Sci. USA. 2006;103:9136–9141. doi: 10.1073/pnas.0508889103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Hirata Y., Murai N., Yanaihara N., Saito M., Saito M., Urashima M., Murakami Y., Matsufuji S., Okamoto A. MicroRNA-21 is a candidate driver gene for 17q23-25 amplification in ovarian clear cell carcinoma. BMC Cancer. 2014;14:799. doi: 10.1186/1471-2407-14-799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Filippova E.A., Loginov V.I., Burdennyi A.M., Braga E.A., Pronina I.V., Kazubskaya T.P., Kushlinskii D.N., Utkin D.O., Fridman M.V., Khodyrev D.S., et al. Hypermethylated Genes of MicroRNA in Ovarian Carcinoma: Metastasis Prediction Marker Systems. Bull. Exp. Biol. Med. 2019;167:79–83. doi: 10.1007/s10517-019-04465-5. [DOI] [PubMed] [Google Scholar]
- 258.Braga E.A., Loginov V.I., Filippova E.A., Burdennyi A.M., Pronina I.V., Kazubskaya T.P., Khodyrev D.S., Utkin D.O., Kushlinskii D.N., Adamyan L.V., et al. Diagnostic Value of a Group of MicroRNA Genes Hypermethylated in Ovarian Carcinoma. Bull. Exp. Biol. Med. 2018;166:253–256. doi: 10.1007/s10517-018-4326-0. [DOI] [PubMed] [Google Scholar]
- 259.Hermeking H. MicroRNAs in the p53 network: Micromanagement of tumour suppression. Nat. Rev. Cancer. 2012;12:613–626. doi: 10.1038/nrc3318. [DOI] [PubMed] [Google Scholar]
- 260.Welponer H., Tsibulak I., Wieser V., Degasper C., Shivalingaiah G., Wenzel S., Sprung S., Marth C., Hackl H., Fiegl H., et al. The miR-34 family and its clinical significance in ovarian cancer. J. Cancer. 2020;11:1446–1456. doi: 10.7150/jca.33831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Tian M., Tian D., Qiao X., Li J., Zhang L. Modulation of Myb-induced NF-kB -STAT3 signaling and resulting cisplatin resistance in ovarian cancer by dietary factors. J. Cell. Physiol. 2019;234:21126–21134. doi: 10.1002/jcp.28715. [DOI] [PubMed] [Google Scholar]
- 262.Luo S., Wang J., Ma Y., Yao Z., Pan H. PPARgamma inhibits ovarian cancer cells proliferation through upregulation of miR-125b. Biochem. Biophys. Res. Commun. 2015;462:85–90. doi: 10.1016/j.bbrc.2015.04.023. [DOI] [PubMed] [Google Scholar]
- 263.Vignati S., Albertini V., Rinaldi A., Kwee I., Riva C., Oldrini R., Capella C., Bertoni F., Carbone G.M., Catapano C.V. Cellular and molecular consequences of peroxisome proliferator-activated receptor-gamma activation in ovarian cancer cells. Neoplasia. 2006;8:851–861. doi: 10.1593/neo.06433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Kim S., Lee J.J., Heo D.S. PPARgamma ligands induce growth inhibition and apoptosis through p63 and p73 in human ovarian cancer cells. Biochem. Biophys. Res. Commun. 2011;406:389–395. doi: 10.1016/j.bbrc.2011.02.052. [DOI] [PubMed] [Google Scholar]
- 265.Zeineldin R., Muller C.Y., Stack M.S., Hudson L.G. Targeting the EGF receptor for ovarian cancer therapy. J. Oncol. 2010;2010:414676. doi: 10.1155/2010/414676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Merritt W.M., Lin Y.G., Han L.Y., Kamat A.A., Spannuth W.A., Schmandt R., Urbauer D., Pennacchio L.A., Cheng J.F., Nick A.M., et al. Dicer, Drosha, and outcomes in patients with ovarian cancer. N. Engl. J. Med. 2008;359:2641–2650. doi: 10.1056/NEJMoa0803785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Mori M., Triboulet R., Mohseni M., Schlegelmilch K., Shrestha K., Camargo F.D., Gregory R.I. Hippo signaling regulates microprocessor and links cell-density-dependent miRNA biogenesis to cancer. Cell. 2014;156:893–906. doi: 10.1016/j.cell.2013.12.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Suzuki H.I., Yamagata K., Sugimoto K., Iwamoto T., Kato S., Miyazono K. Modulation of microRNA processing by p53. Nature. 2009;460:529–533. doi: 10.1038/nature08199. [DOI] [PubMed] [Google Scholar]
- 269.Han C., Liu Y., Wan G., Choi H.J., Zhao L., Ivan C., He X., Sood A.K., Zhang X., Lu X. The RNA-binding protein DDX1 promotes primary microRNA maturation and inhibits ovarian tumor progression. Cell Rep. 2014;8:1447–1460. doi: 10.1016/j.celrep.2014.07.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Peng S., Kuang Z., Sheng C., Zhang Y., Xu H., Cheng Q. Association of microRNA-196a-2 gene polymorphism with gastric cancer risk in a Chinese population. Dig. Dis. Sci. 2010;55:2288–2293. doi: 10.1007/s10620-009-1007-x. [DOI] [PubMed] [Google Scholar]
- 271.Christensen B.C., Avissar-Whiting M., Ouellet L.G., Butler R.A., Nelson H.H., McClean M.D., Marsit C.J., Kelsey K.T. Mature microRNA sequence polymorphism in MIR196A2 is associated with risk and prognosis of head and neck cancer. Clin. Cancer Res. Off. 2010;16:3713–3720. doi: 10.1158/1078-0432.CCR-10-0657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Hoffman A.E., Zheng T., Yi C., Leaderer D., Weidhaas J., Slack F., Zhang Y., Paranjape T., Zhu Y. microRNA miR-196a-2 and breast cancer: A genetic and epigenetic association study and functional analysis. Cancer Res. 2009;69:5970–5977. doi: 10.1158/0008-5472.CAN-09-0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Song Z.S., Wu Y., Zhao H.G., Liu C.X., Cai H.Y., Guo B.Z., Xie Y.A., Shi H.R. Association between the rs11614913 variant of miRNA-196a-2 and the risk of epithelial ovarian cancer. Oncol. Lett. 2016;11:194–200. doi: 10.3892/ol.2015.3877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Lukacs J., Soltesz B., Penyige A., Nagy B., Poka R. Identification of miR-146a and miR-196a-2 single nucleotide polymorphisms at patients with high-grade serous ovarian cancer. J. Biotechnol. 2019;297:54–57. doi: 10.1016/j.jbiotec.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 275.Liu R., Martin T.A., Jordan N.J., Ruge F., Ye L., Jiang W.G. Metastasis suppressor 1 expression in human ovarian cancer: The impact on cellular migration and metastasis. Int. J. Oncol. 2015;47:1429–1439. doi: 10.3892/ijo.2015.3121. [DOI] [PubMed] [Google Scholar]
- 276.Georgescu M.M. PTEN Tumor Suppressor Network in PI3K-Akt Pathway Control. Genes Cancer. 2010;1:1170–1177. doi: 10.1177/1947601911407325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Niu K., Shen W., Zhang Y., Zhao Y., Lu Y. MiR-205 promotes motility of ovarian cancer cells via targeting ZEB1. Gene. 2015;574:330–336. doi: 10.1016/j.gene.2015.08.017. [DOI] [PubMed] [Google Scholar]
- 278.Li J., Li L., Li Z., Gong G., Chen P., Liu H., Wang J., Liu Y., Wu X. The role of miR-205 in the VEGF-mediated promotion of human ovarian cancer cell invasion. Gynecol. Oncol. 2015;137:125–133. doi: 10.1016/j.ygyno.2015.01.531. [DOI] [PubMed] [Google Scholar]
- 279.Ghoneum A., Said N. PI3K-AKT-mTOR and NFkappaB Pathways in Ovarian Cancer: Implications for Targeted Therapeutics. Cancers. 2019;11:949. doi: 10.3390/cancers11070949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Xu G., Bernaudo S., Fu G., Lee D.Y., Yang B.B., Peng C. Cyclin G2 is degraded through the ubiquitin-proteasome pathway and mediates the antiproliferative effect of activin receptor-like kinase 7. Mol. Biol. Cell. 2008;19:4968–4979. doi: 10.1091/mbc.e08-03-0259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Bernaudo S., Salem M., Qi X., Zhou W., Zhang C., Yang W., Rosman D., Deng Z., Ye G., Yang B.B., et al. Cyclin G2 inhibits epithelial-to-mesenchymal transition by disrupting Wnt/beta-catenin signaling. Oncogene. 2016;35:4816–4827. doi: 10.1038/onc.2016.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Fu G., Peng C. Nodal enhances the activity of FoxO3a and its synergistic interaction with Smads to regulate cyclin G2 transcription in ovarian cancer cells. Oncogene. 2011;30:3953–3966. doi: 10.1038/onc.2011.127. [DOI] [PubMed] [Google Scholar]
- 283.Zhang Y., Chen Q. Relationship between matrix metalloproteinases and the occurrence and development of ovarian cancer. Braz. J. Med. Biol. Res. 2017;50:e6104. doi: 10.1590/1414-431x20176104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Yang Z., Jin P., Xu S., Zhang T., Yang X., Li X., Wei X., Sun C., Chen G., Ma D., et al. Dicer reprograms stromal fibroblasts to a pro-inflammatory and tumor-promoting phenotype in ovarian cancer. Cancer Lett. 2018;415:20–29. doi: 10.1016/j.canlet.2017.11.026. [DOI] [PubMed] [Google Scholar]
- 285.Stone R.L., Nick A.M., McNeish I.A., Balkwill F., Han H.D., Bottsford-Miller J., Rupairmoole R., Armaiz-Pena G.N., Pecot C.V., Coward J., et al. Paraneoplastic thrombocytosis in ovarian cancer. N. Engl. J. Med. 2012;366:610–618. doi: 10.1056/NEJMoa1110352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Liang R., Chen X., Chen L., Wan F., Chen K., Sun Y., Zhu X. STAT3 signaling in ovarian cancer: A potential therapeutic target. J. Cancer. 2020;11:837–848. doi: 10.7150/jca.35011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Hill L., Browne G., Tulchinsky E. ZEB/miR-200 feedback loop: At the crossroads of signal transduction in cancer. Int. J. Cancer. 2013;132:745–754. doi: 10.1002/ijc.27708. [DOI] [PubMed] [Google Scholar]
- 288.Eichler W., Hamann J., Aust G. Expression characteristics of the human CD97 antigen. Tissue Antigens. 1997;50:429–438. doi: 10.1111/j.1399-0039.1997.tb02897.x. [DOI] [PubMed] [Google Scholar]
- 289.Yona S., Lin H.H., Siu W.O., Gordon S., Stacey M. Adhesion-GPCRs: Emerging roles for novel receptors. Trends Biochem. Sci. 2008;33:491–500. doi: 10.1016/j.tibs.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 290.Li J., Zhou B.P. Activation of beta-catenin and Akt pathways by Twist are critical for the maintenance of EMT associated cancer stem cell-like characters. BMC Cancer. 2011;11:49. doi: 10.1186/1471-2407-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Pan Y., Tong J.H.M., Lung R.W.M., Kang W., Kwan J.S.H., Chak W.P., Tin K.Y., Chung L.Y., Wu F., Ng S.S.M., et al. RASAL2 promotes tumor progression through LATS2/YAP1 axis of hippo signaling pathway in colorectal cancer. Mol. Cancer. 2018;17:102. doi: 10.1186/s12943-018-0853-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Li S., Yu Z., Chen S.S., Li F., Lei C.Y., Chen X.X., Bao J.M., Luo Y., Lin G.Z., Pang S.Y., et al. The YAP1 oncogene contributes to bladder cancer cell proliferation and migration by regulating the H19 long noncoding RNA. Urol. Oncol. 2015;33:427.e1–427.e10. doi: 10.1016/j.urolonc.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 293.Guo C., Wang X., Liang L. LATS2-mediated YAP1 phosphorylation is involved in HCC tumorigenesis. Int. J. Clin. Exp. Pathol. 2015;8:1690–1697. [PMC free article] [PubMed] [Google Scholar]
- 294.Lu Q., Longo F.M., Zhou H., Massa S.M., Chen Y.H. Signaling through Rho GTPase pathway as viable drug target. Curr. Med. Chem. 2009;16:1355–1365. doi: 10.2174/092986709787846569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Ghosh D., Bagley A.F., Na Y.J., Birrer M.J., Bhatia S.N., Belcher A.M. Deep, noninvasive imaging and surgical guidance of submillimeter tumors using targeted M13-stabilized single-walled carbon nanotubes. Proc. Natl. Acad. Sci. USA. 2014;111:13948–13953. doi: 10.1073/pnas.1400821111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Lessan K., Aguiar D.J., Oegema T., Siebenson L., Skubitz A.P. CD44 and beta1 integrin mediate ovarian carcinoma cell adhesion to peritoneal mesothelial cells. Am. J. Pathol. 1999;154:1525–1537. doi: 10.1016/S0002-9440(10)65406-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Morgan M.R., Byron A., Humphries M.J., Bass M.D. Giving off mixed signals--distinct functions of alpha5beta1 and alphavbeta3 integrins in regulating cell behaviour. IUBMB Life. 2009;61:731–738. doi: 10.1002/iub.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Iwanicki M.P., Davidowitz R.A., Ng M.R., Besser A., Muranen T., Merritt M., Danuser G., Ince T.A., Brugge J.S. Ovarian cancer spheroids use myosin-generated force to clear the mesothelium. Cancer Discov. 2011;1:144–157. doi: 10.1158/2159-8274.CD-11-0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Abate-Shen C. Deregulated homeobox gene expression in cancer: Cause or consequence? Nat. Rev. Cancer. 2002;2:777–785. doi: 10.1038/nrc907. [DOI] [PubMed] [Google Scholar]
- 300.Li B., Jin H., Yu Y., Gu C., Zhou X., Zhao N., Feng Y. HOXA10 is overexpressed in human ovarian clear cell adenocarcinoma and correlates with poor survival. Int. J. Gynecol. Cancer. 2009;19:1347–1352. doi: 10.1111/IGC.0b013e3181a83f1d. [DOI] [PubMed] [Google Scholar]
- 301.Seeber L.M., Horree N., Vooijs M.A., Heintz A.P., van der Wall E., Verheijen R.H., van Diest P.J. The role of hypoxia inducible factor-1alpha in gynecological cancer. Crit. Rev. Oncol. Hematol. 2011;78:173–184. doi: 10.1016/j.critrevonc.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 302.Markert E.K., Levine A.J., Vazquez A. Proliferation and tissue remodeling in cancer: The hallmarks revisited. Cell Death Dis. 2012;3:e397. doi: 10.1038/cddis.2012.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Hu X., Macdonald D.M., Huettner P.C., Feng Z., El Naqa I.M., Schwarz J.K., Mutch D.G., Grigsby P.W., Powell S.N., Wang X. A miR-200 microRNA cluster as prognostic marker in advanced ovarian cancer. Gynecol. Oncol. 2009;114:457–464. doi: 10.1016/j.ygyno.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 304.van Jaarsveld M.T., Helleman J., Boersma A.W., van Kuijk P.F., van Ijcken W.F., Despierre E., Vergote I., Mathijssen R.H., Berns E.M., Verweij J., et al. miR-141 regulates KEAP1 and modulates cisplatin sensitivity in ovarian cancer cells. Oncogene. 2013;32:4284–4293. doi: 10.1038/onc.2012.433. [DOI] [PubMed] [Google Scholar]
- 305.Chen J.L., Chen F., Zhang T.T., Liu N.F. Suppression of SIK1 by miR-141 in human ovarian cancer cell lines and tissues. Int. J. Mol. Med. 2016;37:1601–1610. doi: 10.3892/ijmm.2016.2553. [DOI] [PubMed] [Google Scholar]
- 306.Zheng H., Kang Y. Multilayer control of the EMT master regulators. Oncogene. 2014;33:1755–1763. doi: 10.1038/onc.2013.128. [DOI] [PubMed] [Google Scholar]
- 307.Dykxhoorn D.M. MicroRNAs and metastasis: Little RNAs go a long way. Cancer Res. 2010;70:6401–6406. doi: 10.1158/0008-5472.CAN-10-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Olson P., Lu J., Zhang H., Shai A., Chun M.G., Wang Y., Libutti S.K., Nakakura E.K., Golub T.R., Hanahan D. MicroRNA dynamics in the stages of tumorigenesis correlate with hallmark capabilities of cancer. Genes Dev. 2009;23:2152–2165. doi: 10.1101/gad.1820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Imai T., Horiuchi A., Shiozawa T., Osada R., Kikuchi N., Ohira S., Oka K., Konishi I. Elevated expression of E-cadherin and alpha-, beta-, and gamma-catenins in metastatic lesions compared with primary epithelial ovarian carcinomas. Hum. Pathol. 2004;35:1469–1476. doi: 10.1016/j.humpath.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 310.Nowek K., Wiemer E.A.C., Jongen-Lavrencic M. The versatile nature of miR-9/9(*) in human cancer. Oncotarget. 2018;9:20838–20854. doi: 10.18632/oncotarget.24889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Gang W., Tanjun W., Yong H., Jiajun Q., Yi Z., Hao H. Inhibition of miR-9 decreases osteosarcoma cell proliferation. Bosn. J. Basic Med. Sci. 2020;20:218–225. doi: 10.17305/bjbms.2019.4434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Hersi H.M., Raulf N., Gaken J., Folarin N., Tavassoli M. MicroRNA-9 inhibits growth and invasion of head and neck cancer cells and is a predictive biomarker of response to plerixafor, an inhibitor of its target CXCR4. Mol. Oncol. 2018;12:2023–2041. doi: 10.1002/1878-0261.12352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Dochez V., Caillon H., Vaucel E., Dimet J., Winer N., Ducarme G. Biomarkers and algorithms for diagnosis of ovarian cancer: CA125, HE4, RMI and ROMA, a review. J. Ovarian Res. 2019;12:28. doi: 10.1186/s13048-019-0503-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Wu S.G., Chang T.H., Liu Y.N., Shih J.Y. MicroRNA in Lung Cancer Metastasis. Cancers. 2019;11:265. doi: 10.3390/cancers11020265. [DOI] [PMC free article] [PubMed] [Google Scholar]