Abstract
Background:
The fundamental principles of healthcare practices and policies are derived from good quality research. Doctors collectively are a source of vast sums of invaluable information. This information if effectively utilized can improve and strengthen the healthcare system. Our study provides a comprehensive overview of the ecosystem of an Indian medical researcher.
Objectives:
To understand (1) the obstacles faced by medical professionals (2) the challenges encountered at various steps (3) the gaps in research knowledge and (4) the means to rectify them.
Method:
Doctors from medical schools, hospitals, and in private practices were approached. Data were collected through online and physical questionnaire. Data were analyzed and studied.
Results:
The total number of participants in this study is 212. Case reports (51.9%) and case-control studies (51.14%) are the most frequently conducted types of research. Lack of access to research journals (43.9%) and absence of proper guidance or mentorship (37.39%) are the commonly faced challenges among individuals who have pursued research, whereas busy schedule is the top-cited reason for not pursuing research (34.24%) and discontinuing research (57.4%). Coordinating time schedule with mentees is a challenge for mentors (49.2%). Doctors also face the greatest difficulty (48.12%) and delay (47.4%) in the publication process. On the other hand, personal interest (60.15%) and job requirement (46.61%) are the top facilitators for research. A small percentage has or knows someone that has plagiarized (21.32%) or falsified data (33.49%). Most of the doctors agree that research experience should be a mandatory part of undergrad training (81.6%).
Conclusion:
We believe interest, impact and importance of research can be the best developed and emphasized in the training years. Institutional support, adequate mentorship and an uplifting research environment can go a long way in motivating the doctors and tackling the challenges they face.
Keywords: Barriers, challenges, data falsification, mentorship, motivators, plagiarism, research
Introduction
A novel approach, clearly defined objectives, methodical analysis and intelligible scientific writing are some of the attributes of a good quality research study.[1] Only results from such studies can contribute to identifying patterns and trends in health and disease and can consistently add to the knowledge pool. Furthermore, research is vital to ensure the optimization of healthcare practices, policies, delivery as well as standardization of treatment protocols and long-term interventions. This, in turn, leads to overall sustainable development of the nation.
Various geographical, cultural, genetic and dietary differences make populations distinct from one another. These differences should be taken into account while tailoring medical recommendations to a population. Sound research of substantial quality and quantity, privy to these subtleties, can uplift the nation to a better state of physical and mental wellbeing.
On literature review, there has been one such study from AIIMS in India, which shows that difficulties related to statistical analysis, lack of support from the institution, shortage of time, lack of interest in research, high workload, budget difficulties, social responsibilities and lack of resources, hinders research.[2] No similar study is available from South India.
Our aim, via this study, is to address inefficiencies in the research processes that can be corrected and to recognize facilitators that can be strengthened. We have attempted to not oversimplify the multi-dimensional medical research ecosystem in India but to lay a foundation upon which further studies can be based on.
Materials and Methods
Study type
A cross-sectional' study using the postal/questionnaire method.[3]
Study population and data collection
The study sample was collected using purposeful sampling due to the absence of prior studies and the inability to calculate theoretical saturation owing primarily to the vast scope of the questions posed and the postal/questionnaire format used. We have attempted to overcome this by increasing the sample size ensuring that theme saturation was obtained.
Ethical clearance
Obtained from Father Muller Medical College Institutional Ethics Committee, Mangalore. Reference no: FMMCIEC/CCM/4092018. Ethical committee clearance obtained on 17.07.2018.
Eligibility Criteria
Inclusion criteria: Graduates of Bachelor of Medicine and Bachelor of Surgery (MBBS)
Exclusion criteria: Students studying MBBS.
Data collection
Data was collected via both online and physical questionnaire. The questionnaire focused on obtaining qualitative data. The study was designed to maintain the anonymity of the participant. For the purposes of the study, a paper was defined as a completed, published or not published work that included case reports, case series, cross-sectional studies, cohort studies, case-control studies, randomized control trials, meta-analysis or reviews. The questionnaire was designed to focus on whether a participant had written a paper and factors that facilitated or acted as a barrier to writing a paper. The questionnaire also focused on other facets of research such as falsification of data, plagiarism, mentoring and the use of technology in research.
Doctors from medical schools, hospitals, and private practice were approached. They were selected based on convenience and accessibility. The online questionnaire permitted a small amount of non-discriminant snowballing sampling.
Responses were entered into Microsoft Excel and data compiling and analysis was carried out.
Results
Total population
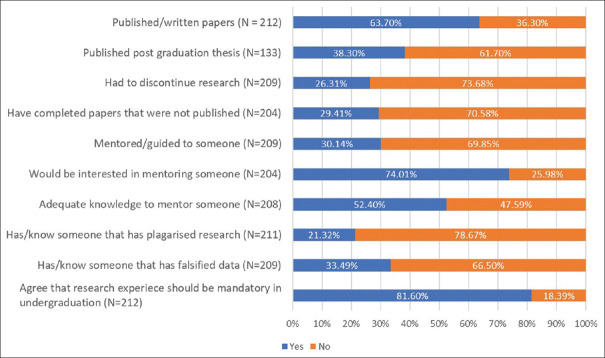
There were total 212 responses of which 63.7% (135) of doctors have written or published at least one paper and 36.3% (77) have not.
The responses to the questionnaire were collected from various institutions; 80% of which were collected from Bangalore City and the rest were either from the state of Karnataka or unknown. 33% of responses were from medical colleges, 37% from hospitals, and the remaining 30% were from unknown institutions. Of the people that answered the questionnaire, 58% were males and 42% were females. The socio-demographic characteristics of our patient population have been listed in Table 1.
Table 1.
Socio-demographics
| 1. City | Frequency | Percentage |
|---|---|---|
| a. Bangalore City | 170 | 80.18 |
| b. Other cities in Karnataka or unknown | 67 | 19.81 |
| 2. Gender | ||
| a. Male | 123 | 58.1 |
| b. Female | 89 | 41.9 |
| 3. Institution | ||
| a. Medical Colleges | 70 | 33.01 |
| b. Hospitals | 78 | 36.79 |
| c. Unknown | 64 | 30.18 |
| 4. Subspecialty | ||
| a. Clinical | 107 | 50.47 |
| b. Non clinical | 51 | 24.05 |
| c. Post MBBS | 54 | 25.47 |
In the study population, the mean number of years since graduation was 12.73 years, with 49.5% of the population having graduated less than 10 years ago. 50.5% were specialized in clinical fields, 24% in non-clinical fields and 25% were graduates.
Participants that have written one or more papers
Of the participants that have written a paper (135), the average number of years since their last publication was 2.53 years with SD of 3.91 years; 53% were women and 47% were men (χ2 = 0.089). The average number of papers written by male participants was 7.6 papers compared to the 5.85 papers written by female participants (p > 0.05). The mean number of papers written by those who have worked in a medical college is 8.31 papers while those that have not are 3.14 papers (p < 0.05). 47.69% of participants (n = 130) published the majority of their papers while working in a medical college; 30.76% as postgraduates and 13.84% as students.
The descriptive statistics, that is, mean, median, mode, SD of the total number of papers published is 6.67, 3.00, 1.00, 9.36; of papers published in journals is 6.11, 3.00, 1.0, 9.64; of papers indexed in PubMed is 2.64, 1, 0.0, 4.97, respectively.
38.3% of the doctors have published their postgraduate thesis paper.
In the following questions, participants were allowed to pick multiple, all, no options or give their reasons; therefore, each option is represented as a percentage of the number of people that could have picked it. The most common options are described below.
The following multiple-choice questions have been summarized in Tables 2 and 3: (i) types of research done by the participants; (ii) reasons for pursuing research; (iii) research processes causing the greatest difficulty and delay; (iv) challenges faced while doing research; and (v) if doctors used advances in technology such as video calling, online shared documents, etc., to work with their research team.
Table 2.
Participants that have written one or more papers
| 1. What are the types of research that you have done? * (131 responses of 135 participants) | Frequency | Percentage |
| a. Case report | 68 | 51.90 |
| b. Cross-sectional study | 67 | 51.14 |
| c. Case series | 43 | 32.82 |
| d. Case control | 35 | 26.71 |
| e. Cohort | 19 | 14.50 |
| f. Randomized Control Trial | 17 | 12.97 |
| g. Meta-analysis | 9 | 6.87 |
| 2. What are your reasons for pursuing research? * (133 responses of 135 participants) | Frequency | Percentage |
| a. Personal interest | 80 | 60.15 |
| b. Mandatory job requirement/requirement for promotion | 62 | 46.61 |
| c. To improve knowledge of field | 56 | 41.35 |
| d. To present in conferences and CMEs | 49 | 36.84 |
| e. Requirement for completion of degree | 40 | 30.07 |
| f. For recognition/acclaim | 27 | 20.30 |
| g. To become a prominent doctor in the field of study | 10 | 7.51 |
| h. To pursue career abroad/education abroad | 9 | 6.76 |
| 3. How much do you use advances in technology (video calling, online shared documents) for working with your research team? (132 responses of 135 participants) | Frequency | Percentage |
| a. Not at all | 7 | 5.3 |
| b. Don’t know how to use it | 32 | 24.2 |
| c. Use it but not comfortable using it | 61 | 46.2 |
| d. Use it and comfortable using it | 29 | 22 |
Table 3.
Challenges faced by participants that have written one or more papers
| 1. Which of the following processes did you face the greatest…? * (133 responses of 135 participants) | …Difficulty in? Frequency (%) | …Delay in? Frequency (%) |
| a. Publication process | 64 (48.12) | 67 (47.40) |
| b. Data collection | 52 (39.09) | 53 (39.25) |
| c. Statistical analysis | 49 (36.48) | 20 (14.81) |
| d. Writing up the paper | 45 (33.83) | 53 (39.25) |
| e. Conception of idea | 24 (18.04) | 15 (11.11) |
| 2. What are the challenges you faced while doing research? * (123 responses of 135 participants) | Frequency | Percentage |
| I. Challenges of knowledge | ||
| a. Difficulty performing statistics | 38 | 30.89 |
| b. Inadequate knowledge of research methodology | 35 | 28.45 |
| c. Inability to identify potential research topics | 21 | 17.07 |
| d. Deficit in skill set for collection of data | 13 | 10.56 |
| II. Challenges of support | ||
| e. Lack of access to journals for literature review and references | 54 | 43.90 |
| f. Lack of proper guidance/dedicated mentor | 46 | 37.39 |
| g. Insufficient or absence of funding | 46 | 47.49 |
| h. Lack of a team | 33 | 26.82 |
| i. Lack of support/encouragement in work place/institution | 32 | 26.01 |
| j. Unaware of means to obtain funding | 22 | 17.88 |
| k. Inadequate dedication from members of the team | 13 | 10.56 |
| III. Other challenges | ||
| l. Lack of access to statistical software like SPSS | 21 | 17.07 |
| m. Social responsibilities | 29 | 23.57 |
| n. Loss of interest/motivation | 25 | 20.32 |
Participants that have not written any papers
The multiple choice questions listing the reasons for not pursuing research has been summarized in Table 4.
Table 4.
Participants that have not written any papers
| If you have not pursued research, why not? * (73 responses of 77 participants) | Frequency | Percentage |
|---|---|---|
| a. Busy schedule | 25 | 34.24 |
| b. Did not come across opportunities | 24 | 32.87 |
| c. Never obtained any adequate/training for research | 24 | 32.87 |
| d. No knowledge regarding research methodology | 21 | 28.76 |
| e. Did not receive support/encouragement | 13 | 17.80 |
| f. Research is expensive | 10 | 13.61 |
| g. Absence of a guide | 10 | 13.61 |
| h. Not interested | 8 | 10.95 |
| i. No other colleague/friend interested in doing research | 7 | 9.58 |
| j. Research is only meant to be done in medical colleges | 2 | 2.73 |
| k. Inability to obtain ethical clearance | 1 | 1.36 |
| l. Research does affect my medical practice in a significant manner | 1 | 1.36 |
Questions relevant to both groups
Questions detailing thr following: (i) reasons for discontinuing research, (ii) reasons for failure to publish completed papers, (iii) early correctional steps that could have contributed maximally towards pursuing research, and (iv) challenges faced as a mentor has been summarized in Tables 5 and 6.
Table 5.
Mentorship and its challenges
| Have you ever mentored someone in research? What challenges did you face? | Frequency | Percentage |
|---|---|---|
| a. Yes | 63 | 30.14 |
| b. No | 146 | 69.85 |
| Challenges* (60 responses of 60 participants) | ||
| a. Coordinating time schedules | 31 | 49.20 |
| b. Maintaining mentee’s focus and interest | 25 | 39.68 |
| c. Mentee had difficulty with statistics | 20 | 31.74 |
| d. Mentee’s busy schedule | 19 | 30.15 |
| e. Mentee had difficulty with data collection | 18 | 28.57 |
| f. Mentee’s poor knowledge of research | 15 | 23.80 |
| g. Inability of mentee to choose appropriate research topic | 15 | 23.80 |
| h. Gaps in your knowledge | 13 | 20.63 |
Table 6.
Discontinued or unpublished research and correctional steps
| 1. Have you discontinued research? If yes, why? | Frequency | Percentage |
| a. Yes | 55 | 26.31 |
| b. No | 154 | 74.68 |
| Reasons* (54 responses of 55 participants) | ||
| a. Busy schedule | 31 | 57.40 |
| b. Poor quality data collection | 23 | 42.59 |
| c. Difficulty coordinating tasks with co-authors | 19 | 35.18 |
| d. Inadequate dedication from members of the team | 19 | 35.18 |
| e. Lack of support/encouragement | 18 | 33.33 |
| f. Loss of interest in completing the study | 8 | 14.81 |
| g. Difficulty performing statistics | 7 | 12.96 |
| h. Improper literature review | 7 | 12.96 |
| i. Discontinued funding | 5 | 9.25 |
| 3. Do you have completed unpublished papers? Why? | Frequency | Percentage |
| a. Yes | 60 | 29.41 |
| b. No | 144 | 70.58 |
| Responses* (56 responses of 60 participants) | ||
| a. Paper not accepted in esteemed journals | 18 | 32.14 |
| b. Similar study already done | 16 | 28.57 |
| c. Quality of paper not satisfactory | 14 | 25 |
| d. Multiple rejections | 12 | 21.42 |
| e. Lack of funds | 11 | 19.64 |
| f. Improper methodology | 5 | 8.92 |
| 4. Which of the following correctional steps if done early, would have contributed maximally towards starting research? *(199 responses of 212 participants) | Frequency | Percentage |
| a. Mandatory research project in under-graduation | 125 | 62.81 |
| b. Mandatory research training in under-graduation | 120 | 60.30 |
| c. Compulsory research facility | 110 | 55.27 |
| d. Greater value for research in job placements | 95 | 47.73 |
Questions enumerating (i) participant's interest in mentoring, (ii) participant's knowledge to mentor, (iii) if the participant has or knows someone that has plagiarized or falsified data, and lastly, (iv) if research experience should be a mandatory part of undergraduate experience has been summarized in Figure 1.
Figure 1.
Graphical representation of questions applicable to both groups
Discussion
Participants who have written one or more papers
I. Gender
In our study population, more papers were written and published by male doctors compared to females (p > 0.05). This corroborates with the overall global statistics of fewer papers being published by women. Studies have shown that women publish less and are less likely to be the first authors in published papers.[4] This can be attributed to several factors such as women experiencing greater work exhaustion, lack of control over work time and pace as well as inadequate institutional support for research compared to their male counterparts. In addition, women are financially disadvantaged owing to the uneven distribution of grants between male and female researchers.[5] Statistics specific to India are not available.
II. Place of work
Our data showed a higher number of publications by those who at one point worked in medical colleges (p < 0.05). Job promotions, recognition of academic advancements, funding and support available in medical colleges are some of the reasons, we believe, contributed to this finding.
III. Publication statistics
It is essential that physicians not only read published articles to update themselves but also to publish high-quality papers themselves.[6] Focusing on the number of publications alone would be an unhealthy and skewed view of the reality of “academic productivism” but it was the most easily available data (better options would be impact factor, number of citations, h-index, and g-index).[7]
An attempt was made to improve this view by compounding it with publications in PubMed as a stand-in for evaluation of quality. While most studies that were written were published, there was a drastic drop in papers published in journals indexed in PubMed. This raises the concern of medical researchers focusing on quantity over quality thereby hindering the progress of healthcare research.[8]
This is mirrored at a global level where India ranks 12th in the total number of publications worldwide but with citation per document of only 9.95 and h-index of 336 (c.f. the average number of citations per document and h-index of the first 10 countries are 21.29 and 758.8, respectively).[9]
IV. Evidence-based medicine
The hierarchy of evidence is the core principle of evidence-based medicine. The hierarchy is as follows (from bottom to top): case series/cross-sectional studies (level IV) < case-controlled studies/cohort studies/non-randomized experimental trial (level III) < pseudo-randomized controlled trials (level II) < systematic review (level I).[10] In our study, the two most common types of papers written were case reports and cross-sectional studies, both belonging to the lowest level of the hierarchy. Higher the level of the study design, the more rigorous the methodology and the more likely it is that the results can be applied to the general population.
V. Delays and difficulty in the research and publication process
The publication process includes the steps of submission of the manuscript, first check by editor in chief, subsequent checks by assistant editor, editor, and managing editor followed by a review by reviewers, revisions, and ultimately the final nod of approval for publication.[11] This is a thorough and long process with each paper going back and forth multiple times. In the era of online submissions and communications, any delay can, understandably, be a source of frustration and anxiety for the authors. This is reflected in our data where up to 50% of the individuals face the greatest difficulty as well as a delay in the publication process. The authors should strive to adhere to the guidelines of the journal, approach a journal suited to their study and ensure their write up is grammatically sound in order to avoid unnecessary delays.[12]
Difficulty and delay in data collection were also faced by a sizeable proportion of the participants. This can be tackled by effective communication with the participants, building trust, having uninterrupted funds, open-minded approach, preparedness and compensation when needed.[13]
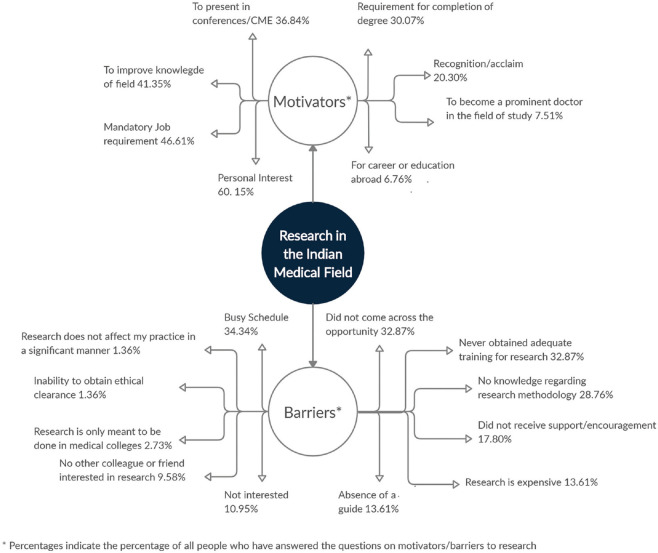
VI. Reasons for pursuing research
In our study, personal interest is the main reason for pursuing research, followed by papers being written for job requirements or for promotions at the workplace [Figure 2]. Focusing on higher objectives such as adding to the knowledge pool or striving for excellence in their respective fields will lead to betterment in the quality of research. We believe this drive to pursue research can be instilled in individuals (as demonstrated by a Swedish cohort study over a 12-year period by Helena Mortenius et al. where oral [seminars, conferences] written [research bulletins, scientific reports] and digital media evoked a significant interest in research and development among healthcare professionals at a primary healthcare center).[14] Furthermore, the responsibility each individual bears towards research together with its significance and benefits should be emphasized early on in the researcher's career.
Figure 2.
Pictorial representation of the motivators and barriers to research in the Indian medical field
VII. Challenges faced while doing research
-
(a)
Challenges of knowledge: We believe that with the clinical practice being the primary focus of the medical environment in India, doctors rarely develop or hone their research skill set. In our study, lack of access to journals for literature review and references, difficulty performing statistics, inadequate knowledge of research methodology, inability to identify research topics and deficiency in skill set for collection of data were the most commonly faced challenges [Figure 2]. Institutions should develop programs aimed at training physicians/students in research in addition to providing support and encouragement in their pursuits. Literature review in PubMed brings forth only a few articles that emphasize the gaps in research related knowledge.[2,15,16] Further studies are necessary to address these core issues and resolve them.
-
(b)
Challenges of support: The right support leads to a better research environment which in turn leads to a better support system resulting in a positive and constructive cycle. In addition, researchers themselves play an influential role in their colleagues, encouraging them to get involved in research as well.[14] Lack of proper mentors, insufficient funding points towards foundational problems in the research environment of doctors.
-
(c)
Other challenges: Social responsibilities, loss of interest/motivation. Challenges of inadequacy in medical recording keeping and data retrieval further compound the hassles faced by a researcher to conduct clinical studies.[17] (Note: This factor was not evaluated in our study.)
VIII. Using advances in technology (video calling, online shared documents) for working with your research team
Although 68.2% of participants who have done research have used technology to share documents and help ease communication, only 22% are comfortable using technology. In literature review, multiple studies have focused on using technology to improve communication between the clinician and patients for the purpose of better medical care as well as follow-up of patients enrolled in clinical trials.[18,19] However, studies on the use of technology to assist working with the research team are lacking. We believe that the use of online resources reduces the traditional need for a common location to work. It also makes work hours flexible and improves communication between researchers resulting in a more efficient research team. It also helps address distance as a hindrance for interinstitutional, interstate and international studies.
Participants that have not written any papers
Most common reasons cited for not writing papers were busy schedule, not being able to identify opportunities for research, inadequate training for research, lack of knowledge of research methodology, and lack of support and encouragement. These reasons are corrigible either by ensuring adequate training of the medical researcher or by policy changes at the level of the institution. Focusing on correcting these deficiencies will result in more doctors participating in research as evidenced by trends found in other studies on barriers to research.[20]
Questions relevant to both groups
I. Research discontinuation or failure to publish
In our study, 26% of the participants have discontinued research (busy schedule being the most frequently picked choice followed by poor quality data collection) and 29.41% of the participants have failed to publish completed papers (rejection of manuscripts in esteemed journals and similar studies being done previously being frequent reasons). We believe that prematurely terminated research projects lead to monetary losses, futile labor and time. Many reasons can be avoided if thorough planning is undertaken at the start of the study.[21,22] Rejections can be disheartening especially since long hours are spent in writing and perfecting the manuscript. Oftentimes, incorrect journal selection can be a reason for non-acceptance. Inadequacies in the manuscript, if present, should be corrected or the paper redrafted to improve its standards. Suggestions should be taken positively to avoid feeling discouraged.[21,23]
II. Mentorship
A mentor is defined as “that person directly responsible for the professional development of a research trainee”.[24] They not only serve as role models but influence and hone the skills of their mentees through guidance, advice, critique and more.[25] While the right mentor can inspire, the wrong one can be equally detrimental to the growth of his/her student. The challenges encountered in a mentor-mentee relationship can arise from misaligned priorities, lack of communication, absence of mutual respect and understanding, mentor's inadequate knowledge and ability to fill in the mentee's knowledge gaps.[24,26] The latter is further demonstrated by the fact that three-quarters of the study group are interested in mentoring someone in their pursuit of research despite the results of the succeeding question where more than half of the study population does not have the adequate knowledge to mentor someone. Academic expertise together with communication and organization skills are essential qualities to take on the role of a mentor.[27] We believe that recognizing and addressing these at the onset can forestall unfruitful mentor-mentee relationships.
III. Plagiarism and data falsification
Plagiarism or the act of copy pasting information from another's work and passing it off as one's own without citation, has been aptly described as a 'menace' and an 'epidemic' that is in urgent need of curtailment.[28] In all, 21% of our study population have claimed to have or to have known someone that has indulged in plagiarism. Falsification of data including statistics and images, like plagiarism, comes under the umbrella of scientific misconduct; 33% of our study group has or knows someone that has falsified data. Notwithstanding the reasons for their occurrence, plagiarism and data distortion of any form is condemnable, jeopardizing the credibility of the author, the research and the journal. The rise of scientific misconduct in India hurts the integrity of the entire research body on a global platform.[28] Anti-plagiarism technologies, penalties, transparent institutional processes, training in scientific writing and the importance of unadulterated research emphasized at undergraduate and postgraduate levels are some of the steps to curb these wrongdoings.[29,30]
IV. Undergraduate training in research
In all, 81% of our study population agreed that research experience should be a mandatory part of undergraduate training. We believe that this would not only incline students towards purposeful research but also enhance their competency, increase their awareness and draw attention to the importance of translating clinical medicine into research and vice versa. The students would possess an overview of the entire research process, statistics, scientific writing and publication. In addition, medical students need to be encouraged to nurture an inquisitive and questioning mind through which they can identify and develop research topics. The deficits in research, their correction as well as the need and benefits of integration of research experience into the medical curricula is reiterated in several papers.[31,32]
A note on the role of primary care doctors
Primary care in India is a growing field with one of the largest collection of doctors who work at the grass root level. While the ability to produce good quality research will show benefits throughout the medical field, we believe that the field of primary care will bear the most fruit. Such a large population of doctors is an untapped source of data and research. Primary care researchers will be able to gather a sample that is representative of the entire population. Increased funding should be directed towards research in primary care as they are the first line of contact for patients. More and more primary care physicians should be encouraged to participate in national level research as its results can lead to improve care throughout the country.
Conclusion
According to the World Health Organization, “High-quality research is essential to achieve its constitutional objective, namely, “the attainment by all peoples of the highest possible level of health”. Research and the evidence that research yields are critical elements for improving global health and health equity, as well as economic development.” This can made possible by every healthcare provider who is, wittingly or unwittingly, a researcher, producing data, identifying trends, implementing and testing solutions until an effective one is found. Therefore, gaining an understanding of the ecosystem of a medical researcher helps strengthen it. We believe that interest, impact and importance of research can be the best developed and emphasized in the training years. Institutional support, adequate mentorship and an uplifting research environment can go a long way in motivating the doctors and tackling the challenges they face.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.de Oliveira DM, Buckeridge MS, Dos Santos WD. Ten simple rules for developing a successful research proposal in Brazil. PLoS Comput Biol. 2017;13:e1005289. doi: 10.1371/journal.pcbi.1005289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alamdari A, Venkatesh S, Roozbehi A, Kannan A. Health research barriers in the faculties of two medical institutions in India. J Multidiscip Healthc. 2012;5:187–94. doi: 10.2147/JMDH.S27841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beckett C, Clegg S. Qualitative data from a postal questionnaire: Questioning the presumption of the value of presence. Int J Soc Res Methodol. 2007;10:307–17. [Google Scholar]
- 4.West JD, Jacquet J, King MM, Correll SJ, Bergstrom CT. The role of gender in scholarly authorship. PLoS One. 2013;8:e66212. doi: 10.1371/journal.pone.0066212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fridner A, Norell A, Škesson G, Gustafsson Sendén M, Tevik Løvseth L, Schenck-Gustafsson K. Possible reasons why female physicians publish fewer scientific articles than male physicians-A cross-sectional study. BMC Med Educ. 2015;15:67. doi: 10.1186/s12909-015-0347-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marusic M. Why physicians should publish, how easy it is, and how important it is in clinical work. Arch Oncol. 2003;11:59–64. [Google Scholar]
- 7.Sahel JA. Quality versus quantity: Assessing individual research performance. Sci Transl Med. 2011;3:84cm13. doi: 10.1126/scitranslmed.3002249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomaz SM, Mormul RP. Misinterpretation of 'slow science' and 'academic productivism' may obstruct science in developing countries. Braz J Biol. 2014;74(3 Suppl 1):S1–2. doi: 10.1590/1519-6984.03013. [DOI] [PubMed] [Google Scholar]
- 9.Scimago institutions ranking. Scimago institution and country rank. [Last accessed on 2019 Feb 15]. Available from: https://wwwscimagojrcom/countryrankphparea=2700 .
- 10.National Health and Medical Research Council. NHMRC Levels of Evidence and Grades for Recommendations for Developers of Clinical Practice Guidelines. 2009. Retrieved 2020 June 21. Available from: https://wwwmjacomau/sites/default/files/NHMRClevelsofevidence2008-09pdf .
- 11.Ali PA, Watson R. Peer review and the publication process. Nurs Open. 2016;3:193–202. doi: 10.1002/nop2.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cornelius JL. Reviewing the review process: Identifying sources of delay. Australas Med J. 2012;5:26–9. doi: 10.4066/AMJ.2012.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holden RJ, McDougald Scott AM, Hoonakker PL, Hundt AS, Carayon P. Data collection challenges in community settings: Insights from two field studies of patients with chronic disease. Qual Life Res. 2014;24:1043–55. doi: 10.1007/s11136-014-0780-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morténius H. Creating an interest in research and development as a means of reducing the gap between theory and practice in primary care: An interventional study based on strategic communication. Int J Environ Res Public Health. 2014;11:8689–708. doi: 10.3390/ijerph110908689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kyaw Soe HH, Than NN, Lwin H, Nu Htay MNN, Phyu KL, Abas AL. Knowledge, attitudes, and barriers toward research: The perspectives of undergraduate medical and dental students. J Educ Health Promot. 2018;7:23. doi: 10.4103/jehp.jehp_61_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chellaiyan VG, Manoharan A, Jasmine M, Liaquathali F. Medical research: Perception and barriers to its practice among medical school students of Chennai. J Educ Health Promot. 2019;8:134. doi: 10.4103/jehp.jehp_464_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bali A, Bali D, Iyer N, Iyer M. Management of medical records: Facts and figures for surgeons. J Maxillofac Oral Surg. 2011;10:199–202. doi: 10.1007/s12663-011-0219-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Almario CV. The effect of digital health technology on patient care and research. Gastroenterol Hepatol (N Y) 2017;13:437–9. [PMC free article] [PubMed] [Google Scholar]
- 19.Forum on Neuroscience and Nervous System Disorders; Board on Health Sciences Policy; Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine. Neuroscience Trials of the Future: Proceedings of a Workshop. Washington (DC): National Academies Press (US); 2016. Aug 19, p. 4. Transforming Clinical Trials with Technology. Available from: https://www.ncbi.nlm.nih.gov/books/NBK379506/ [PubMed] [Google Scholar]
- 20.Canadian Plastic Surgery Research Collaborative (CPSRC) Barriers and attitudes to research among residents in plastic and reconstructive surgery: A national multicenter cross-sectional study. J Surg Educ. 2017;74:1094–104. doi: 10.1016/j.jsurg.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Ali J. Manuscript rejection: Causes and remedies. J Young Pharm. 2010;2:3–6. doi: 10.4103/0975-1483.62205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kasenda B, Von Elm E, You J, Blümle A, Tomonaga Y, Saccilotto R, et al. Prevalence, characteristics, and publication of discontinued randomized trials. JAMA. 2014;311:1045–51. doi: 10.1001/jama.2014.1361. [DOI] [PubMed] [Google Scholar]
- 23.Dhammi IK, Rehan-Ul-Haq Rejection of manuscripts: Problems and solutions. Indian J Orthop. 2018;52:97–9. doi: 10.4103/ortho.IJOrtho_68_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Academy of Sciences (US), National Academy of Engineering (US) and Institute of Medicine (US) Panel on Scientific Responsibility and the Conduct of Research. Responsible Science: Ensuring the Integrity of the Research Process. II. Washington (DC): National Academies Press (US); 1993. p. 3. Mentorship and the Research Training Experience. Available from: https://www.ncbi.nlm.nih.gov/books/NBK236193/ [Google Scholar]
- 25.Toklu HZ, Fuller JC. Mentor-mentee relationship: A win-win contract in graduate medical education. Cureus. 2017;9:e1908. doi: 10.7759/cureus.1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Straus SE, Johnson MO, Marquez C, Feldman MD. Characteristics of successful and failed mentoring relationships: A qualitative study across two academic health centers. Acad Med. 2013;88:82–9. doi: 10.1097/ACM.0b013e31827647a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gandhi M, Johnson M. Creating more effective mentors: Mentoring the mentor. AIDS Behav. 2016;20(Suppl 2):294–303. doi: 10.1007/s10461-016-1364-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Debnath J. Plagiarism: A silent epidemic in scientific writing-Reasons, recognition and remedies. Med J Armed Forces India. 2016;72:164–7. doi: 10.1016/j.mjafi.2016.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Juyal D, Thawani V, Thaledi S. Rise of academic plagiarism in India: Reasons, solutions and resolution. Lung India. 2015;32:542–3. doi: 10.4103/0970-2113.164151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Das N. Intentional or unintentional, it is never alright to plagiarize: A note on how Indian universities are advised to handle plagiarism. Perspect Clin Res. 2018;9:56–7. doi: 10.4103/picr.PICR_140_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abu-Zaid A, Alkattan K. Integration of scientific research training into undergraduate medical education: A reminder call. Med Educ Online. 2013;18:22832. doi: 10.3402/meo.v18i0.22832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bilal M, Haseeb A, Mari A, Ahmed S, Sher Khan MA, Saad M. Knowledge, attitudes, and barriers toward research among medical students of Karachi. Cureus. 2019;11:e5599. doi: 10.7759/cureus.5599. [DOI] [PMC free article] [PubMed] [Google Scholar]