Abstract
Aim
Shared decision making for adults with severe mental illness has increasingly attracted attention. However, this concept has not been comprehensively clarified. This review aimed to clarify a concept of shared decision making for adults with severe mental illness such as schizophrenia, depression, and bipolar disorder, and propose an adequate definition.
Methods
Rodgers' evolutionary concept analysis was used. MEDLINE, PsychINFO, and CINAHL were searched for articles written in English and published between 2010 and November 2019. The search terms were “psychiatr*” or “mental” or “schizophren*” or “depression” or “bipolar disorder”, combined with “shared decision making”. In total, 70 articles met the inclusion criteria. An inductive approach was used to identify themes and sub‐themes related to shared decision making for adults with severe mental illness. Surrogate terms and a definition of the concept were also described.
Results
Four key attributes were identified: user–professional relationship, communication process, user‐friendly visualization, and broader stakeholder approach. Communication process was the densest attribute, which consisted of five phases: goal sharing, information sharing, deliberation, mutual agreement, and follow‐up. The antecedents as prominent predisposing factors were long‐term complex illness, power imbalance, global trend, users' desire, concerns, and stigma. The consequences included decision‐related outcomes, users' changes, professionals' changes, and enhanced relationship.
Conclusions
Shared decision making for adults with severe mental illness is a communication process, involving both user‐friendly visualization techniques and broader stakeholders. The process may overcome traditional power imbalance and encourage changes among both users and professionals that could enhance the dyadic relationship.
Keywords: bipolar disorder, depression, review, schizophrenia, shared decision making
1. INTRODUCTION
The treatment and rehabilitation of people with severe mental illness (SMI) such as schizophrenia, depression, and bipolar disorder, have progressed toward recovery‐oriented care rather than simply symptom relief. Recovery is a way of living a meaningful life even with limitations caused by mental illness, overcoming the challenges of the disability (Deegan, 1988). The recovery weighs control being placed in the hands of the service users and not in those of the health professionals (Jacobson, 2001). Accordingly, recovery‐oriented care craves for the collaborative nature of interactions between people with SMI and health professionals (Duncan, Best, & Hagen, 2010).
In this regard, instead of a paternalistic decision‐making model, where the health professionals take the initiative, shared decision making (SDM) has been increasingly promoted in the mental health field as an ideal model. SDM is an ethical imperative (Drake & Deegan, 2009) and has started to be seen as a key element in the delivery of user‐centered care (Barry & Edgman‐Levitan, 2012). SDM leads to a central part of the recovery paradigm described above, which originates from the service user's right to autonomy and self‐determination (Storm & Edwards, 2013). It may reduce medical care costs by reducing hospital admissions among people with SMI (Cosh et al., 2017). It can also decrease the costs associated with the use of unnecessary or unwanted prescriptions (Latimer, Bond, & Drake, 2011). Several studies have found that most adults with SMI wanted to be involved in decision making (Park et al., 2014; Velligan, Roberts, Sierra, Fredrick, & Roach, 2016), and are able to participate (Aoki, Furuno, Watanabe, & Kayama, 2019a; Aoki et al., 2019b; Duncan et al., 2010; LeBlanc et al., 2015).
Hence, SDM has now been adopted at the national policy level in many Western countries (van Hoof et al., 2015) and has extended to Asian and African countries (Singh, 2015; Stein, 2014). Interventions or training programs to promote SDM for adults with SMI have been developed in both outpatient and inpatient settings. They involve various stakeholders such as clinicians, nurses, social workers, and peer supporters. The decisions involved are also diverse, and include treatment, medication, care plans, and community care after discharge from hospital.
However, despite the growing reports in the literature, a theoretical concept of SDM in the mental health field has not been explored thus fur, and no concept analysis of SDM for adults with SMI has been performed. The absence of a clear concept of SDM for people with SMI has made it harder to understand the needs and roles of health professionals in the process. This situation has caused confusion and in turn made collaboration between service users and health professionals more difficult. Describing and defining the concept of SDM for adults with SMI could therefore provide appropriate guidance for health professionals including nurses.
Given the above, SDM for adults with SMI was viewed an appropriate term for more verification using the concept analysis methodology.
This review aimed to describe the findings of an evolutionary concept analysis of the term SDM in the mental health field, particularly adults with SMI.
2. METHODS
Rodgers' (2000) evolutionary method was used for this review. This evolutionary method is particularly appropriate because of the changes in the concept of SDM over the last few decades, its dynamic nature and its adaptability to different settings and situations. This meant it was necessary to use a method that would allow comparison of changes over time, and the use of SDM for SMI in different studies. As SDM for adults with SMI has been increasingly recognized and widely implemented in various settings, we focused on how it is used, as well as clarified and defined its concept in context. This review followed six steps: (a) identify the concept of interest; (b) select the appropriate realm (sample and setting) for data collection; (c) collect data relevant for identification of (i) attributes, (ii) the concept's contextual basis (antecedents and consequences), and (iii) surrogate terms; (d) analyze data regarding the above components; (e) identify an example of the concept if appropriate; and (f) describe the implications, hypotheses, and future development opportunities (Rodgers, 2000).
2.1. Data sources
A systematic search was conducted using the terms “psychiatr*” or “mental” or “schizophren*” or “depression” or “bipolar disorder” combined with “shared decision making” as key words within the titles or abstracts in the online databases such as MEDLINE, PsychINFO, and CINAHL.
2.2. Data selection
The inclusion criteria were:
empirical studies among adults with SMI (schizophrenia, depression, and/or bipolar disorder) and/or health professionals caring for adults with SMI;
articles that focused on SDM between adults with SMI and health professionals; and
English articles published from 2010 to November 2019.
This period was selected to ensure a contemporary analysis of this concept.
The exclusion criteria were:
review articles, discussion articles, and protocol articles;
articles casually citing “SDM”;
studies that excluded adults with SMI; and
studies among parents or guardians of children with SMI.
We excluded parents or guardians of children with SMI to avoid confusion between surrogate and own decision making, because surrogate decision making might have different elements.
The initial search strategy revealed 1,185 articles. This was reduced to 497 articles when duplicates were removed, limited to articles in mental health settings. The abstracts of 497 articles were examined and the relevance to SDM for adults with SMI was assessed. Review articles, discussion articles, and protocol articles were excluded. Articles regarding SDM for people with other mental illnesses except SMI or children with mental health problems were also removed. Following this assessment, 89 articles were retained. An additional hand‐searched article relevant to SDM for adults with SMI was included. The full text of these 90 articles was obtained, and each paper was read once to examine the general subject of the work and its relevance. As a result, some articles casually citing the term were excluded before the analysis. In total, 70 articles met the inclusion criteria and were included in the concept analysis (Appendix 1). Figure 1 illustrates the flowchart of article selection.
FIGURE 1.
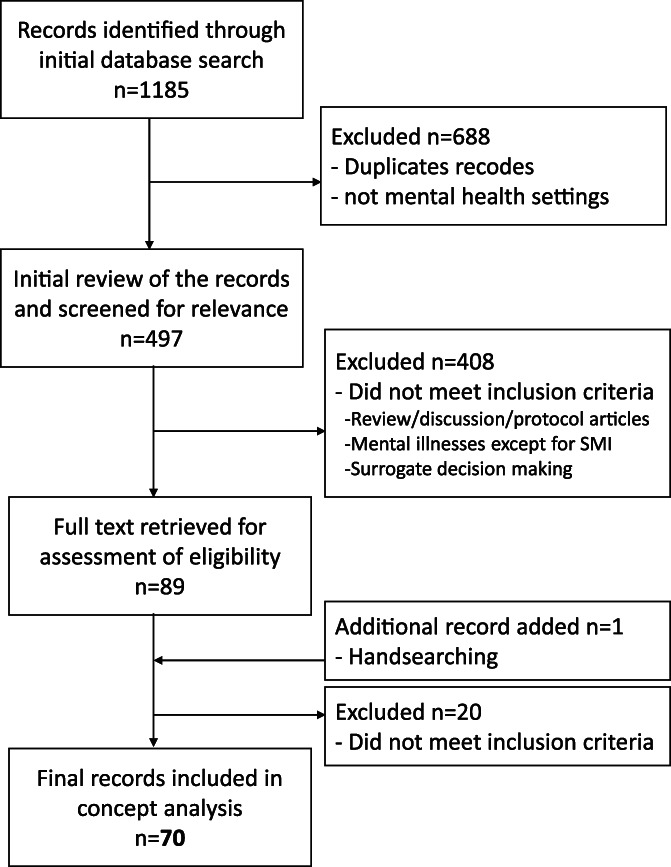
Flow chart of article selection
2.3. Data analysis
The coding procedure was conducted by adopting the Rodgers' (2000) evolutionary method. First, the articles were read and examined to gain the essence of this concept. Thereafter, they were reviewed once again for systematic data extraction and assuring their validity. Second, the extracted data were divided into categories using thematic analysis to determine attributes, antecedents, or consequences. Data that express this concept ideas through other words were extracted as surrogate terms. To ensure the validity and reliability of the analysis, the process of the analysis was supervised by a nursing researcher experienced in this method of analysis.
3. RESULTS
3.1. Attributes
3.1.1. User–professional relationship
The relationship between the service users and health professionals served a foundation attribute to cultivate SDM in the mental health field. SDM in mental health care values the philosophy of partnering with the service users (Hamera, Pallikkathayil, Baker, & White, 2010). In particular, the relationship with collaborative attitude as equals is central to SDM (Alegria et al., 2018; Chong, Aslani, & Chen, 2013b; Eliacin, Salyers, Kukla, & Matthias, 2015; Hamera et al., 2010; Kreyenbuhl et al., 2016; Matthias, Fukui, & Salyers, 2017; Mikesell, Bromley, Young, Vona, & Zima, 2016; Stead, Morant, & Ramon, 2017; Paudel, Sharma, Joshi, & Randall, 2018; Woltmann & Whitley, 2010; Zisman‐Ilani et al., 2019). The health professionals work to build an alliance with the service users for the success of SDM (Paudel et al., 2018). Other valued characteristics of the user–professional relationship are openness, honesty, and transparency, not selectively and discriminative when sharing decision making with the service users (Chong, Aslani, & Chen, 2013ab; De Las Cuevas et al., 2011; Hamann et al., 2016; Mahone et al., 2011; Martin, Perlman, & Bieling, 2015; Mikesell et al., 2016; Nott, Mcintosh, Taube, & Taylor, 2018; Schön, Grim, Wallin, Rosenberg, & Svedberg, 2018; Stead et al., 2017).
3.1.2. Communication process
Communication process was the densest attribute, which consisted of the following five phases: goal sharing, information sharing, deliberation, mutual agreement, and follow‐up.
Goal sharing
Goal sharing was described as the initial phase of the communication process. The goal for the decision is not granted by the health professionals unilaterally, but set together with the service users through discussion (Matthias et al., 2017). It is the user's own goal, which is individual recovery‐oriented (Matthias et al., 2017; Paudel et al., 2018; Woltmann, Wilkniss, Teachout, McHugo, & Drake, 2011; Yamaguchi et al., 2017). Thereafter, both parties share the service user's identified personal goal (Finnerty et al., 2019; Paudel et al., 2018; Yamaguchi et al., 2017).
Information sharing
The next phase of the communication process was information sharing that emerged as a multidimensional concept described below. Table 1 shows articles that contributed on information sharing and the related sub‐themes.
TABLE 1.
Attributes of shared decision making for adults with severe mental illness
| Themes | Sub‐themes | Article |
|---|---|---|
| User–provider relationship | ||
| Partnership /collaboration | Alegria, Chongb, Mikesell, Schön, Eliacin, Stead, Hamera, Kreyenbuhl, Matthias2017, Paudel, Perestelo, Woltmann2010, Zisman‐ilani | |
| Alliance | Paudel | |
| Openness /honesty/transparency | Chonga,b, De las Cuevas2011, Hamann2016, Mahone, Martin, Mikesell, Nott, Schön, Stead | |
| Communication process | ||
| Goal sharing | Aokia, Bonfils, Schön, Finnerty2019, Fukui2015, Goscha, Grim, Luken, Stead, Kreyenbuhl, Matthias2017, Paudel, Sather, Solberg, Woltmann2010,2011, Yamaguchi, Zaini | |
| Information sharing | ||
| Description of condition | Alegria, Aokia,b, Chonga,b, Eliacin, Finnerty2019, Fukui2014, Goscha, Grim, Hamann2016, Martin, Metz2018, Patel, Paudel, Raue, Van der Krieke, Zaini | |
| Psychoeducation | Chongb, Raue, Van der Krieke | |
| Options | Alegria, Aokia,b, Brooks, Chongb, Finnerty2019, Fukui2014, Goscha, Hamann2016, Kivelitz, Klausen, Mahone, Matthias2017, Park, Patel, Paudel, Schön, Shepherd, Stead, Velligan, Zaini, Zisman‐ilani | |
| Modules | Chongb, Goscha, Hamera, Kivelitz, LeBlanc, Martin, Patel, Raue, Stead, Van der Krieke, Zaini, Zisman‐ilani | |
| Pros and cons | Aokia,b, Chonga, Ehrlich, Eliacin, Fukui2014,2015, Grim, Hamann2016, Hamera, Kivelitz, LeBlanc, Luken, Mahone, Martin, Matthias2017, Nott, Paudel, Perestelo, Ramon, Raue, Shepherd, Stead, Van der Krieke, Velligan, Verwijimeren, Zaini, Zisman‐ilani | |
| Research evidence | Finnerty2018, Fukui2015, Kreyenbuhl, LeBlanc, Perestelo, Verwijimeren | |
| Costs | Hamera, Raue, Zaini | |
| Uncertainties | Campbell, De las Cuevas2011, Fukui2014,2015 | |
| Impact of daily life | Aokia,b, Fukui2015, Grim, Hamera, Kivelitz, Klausen, LeBlanc, Mahone, Matthias2017, Metz2018, Patel, Ramon, Yamaguchi, Zaini | |
| Users' views | ||
| Wants/expectations/needs | Chonga, Eliacin, Giacco, Goscha, Grim, Klausen, Lovell, Metz2018, Mikesell, Paudel, Sather, Schön, Shepherd, Van der Krieke, Woltmann2011 | |
| Opinions | Chonga, Giacco, Ishi, Klingaman, Matthias2012, Paudel, Sather, Woltmann2011 | |
| Preferences/values | Alegria, Aokia,b, Brooks, Campbell, Chonga, Eliacin, Finnerty2018,2019, Fukui2014,2015, Giacco, Goscha, Grim, Hamann2011,2016, Kreyenbuhl, LeBlanc, Mahone, Matthias2012,2014, Metz2018, Mikesell, Patel, Paudel, Ramon, Raue, Sather, Schön, Shepherd, Solberg, Stead, Stein, Van der Krieke, Woltmann2010,2011, Yamaguchi, Younas, Zaini, Zisman‐ilani | |
| Past experiences | Aljumah, Eliacin, Goscha, Grim, Hamann2016, Klausen, Kreyenbuhl, Mahone, Mikesell, Ramon, Raue, Sather, Stead, Van der Krieke, Zaini, Zisman‐ilani | |
| Concerns/doubts | Alegria, Aokib, Bonfils, Chonga, Ehrlich, Fukui2015, Goscha, Grim, Hamann2016, Hamera, Luken, Matthias2012, Patel, Ramon, Raue, Stead, Stein, Van der Krieke, Yamaguchi | |
| Self‐help resources | ||
| Personal wellness strategies | Stead, Hamera, Paudel, Finnerty2019, Goscha, Grim, Yamaguchi, Campbell | |
| Relapse prevention | Paudel, Finnerty2019 | |
| Professionals' views | ||
| Recommendations | Aokia,b, Chonga, Grim, Hamera, Patel, Shepherd, Van der Krieke | |
| Clinical expertise | Fukui2015, Luken, Mikesell, Stead | |
| Previous experiences | Kreyenbuhl, Stead, Van der Krieke, Zaini | |
| Peers' recovery experiences | Ali, Aokia, Bonfils, Campbell, Finnerty2019, Goscha, Metz2018, Paudel, Stead, Yamaguchi | |
| Deliberation | ||
| Reviewing | Aokia,b, Eliacin, Goscha, Grim, Hamann2016, Patel, Paudel, Perestelo, Raue, Sather, Schön, Shepherd, Van der Krieke, Woltmann2010, Zisman‐ilani | |
| Preparation for encounters | Aokia,b, Bonfils, Goscha, Grim, Hamann2016, Metz2018, Schön, Van der Krieke | |
| Mutual agreement | Alegria, Aokia,b, Chonga, De las Cuevas2011, Eliacin, Fukui2014, Goscha, Grim, Hamann2016, Ishi, Klingaman, Mahone, Matthias2012,2014, Park, Paudel, Perestelo, Shepherd, Woltmann2010,2011, Yamaguchi, Zisman‐ilani | |
| Follow‐up | Goscha, Grim, Luken, Matthias2012, Paudel, Ramon, Schön, Shepherd | |
| User‐friendly visualization | ||
| Ali, Aokia,b, Campbell, Chongb, Grim, Kivelitz, Martin, Metz2018, Schön, Stead, Van der Krieke, Velligan, Woltmann2010,2011, Wright‐Berryman, Zaini | ||
| Using support tools | Ali, Aljumah, Aokia,b, Bonfils, Campbell, Chongb, Finnerty2018,2019, Goscha, Grim, LeBlanc, Lovell, Luken, Martin, Metz2018, Mikesell, Ramon, Raue, Sather, Schön, Stead, Stein, Van der Krieke, Woltmann2010,2011, Yamaguchi, Zisman‐ilani | |
| Broader stakeholder approach | ||
| Interprofessional collaboration | Aljumah, Chonga,b, Giacco, Ishi, Paudel, Sather, Stead, Younas, Zaini, Zisman‐ilani | |
| Involving carers | Aokia,b, Chongb, Eliacin, Giacco, Grim, Hamann2016, Kivelitz, Klausen, Shepherd, Stead, Velligan | |
Description of condition
In the beginning, the service users' current condition was shared. The health professionals inform the psychiatric diagnosis to the service users. Information about symptoms and related behaviors are shared. Such information regarding illnesses is often provided by psychoeducation. Furthermore, description of condition involves the user's problem formulation by deciding the current problem, and identifying the how and why of the problem.
Options
Options were the most frequently discussed in the information sharing phase. All available options for the service user's current condition or problems are offered. The options are treatment options, care plan options, or rehabilitation options depending on the setting. The service users and health professionals explore the options by discussing modules, pros and cons, research evidence, costs, and uncertainties of each option.
Impact on daily life
How the service user's condition or proposed available options would impact on their daily life was explored. The service users and health professionals discuss how those things impact on the service user's personal circumstances, including social functioning and lifestyle.
Users' views
Several aspects of the service users' subjective views were shared. Those are individual treatment/care wants and expectations including informational needs, own opinions, preferences/values containing what is the most important to the user. Past experiences of the service users were also shared. Moreover, the service users voice concerns or doubts about health conditions, treatment options, or their future.
Self‐help resources
The reference about self‐help resources of the service users was also discussed. This includes personal wellness strategies such as developing coping skills to relieve symptoms, awareness of warning signs, and acquiring environmental support systems for relapse prevention.
Professionals' views
The health professionals' views were contributed as well. The professionals add recommendations giving their clinical expertise with some examples of previous experiences that are related to the illness and its treatment.
Peers' recovery experiences
In many articles, not only health professionals' views but also peer specialists' perspectives based on their own recovery experiences were introduced as reference opinions.
Deliberation
The third phase of the communication process was the deliberation.
Reviewing
The service users and health professionals review together the information shared thus far (Goscha & Rapp, 2015; Zisman‐Ilani et al., 2019). For deeper understanding, the health professionals offer the users sufficient time to ponder that information in more detail, and even gather extra information, at home without any stress or pressure (Schön et al., 2018).
Preparation for encounters
During the deliberation, the users can prepare for further encounters on the decision‐making process (Aoki et al., 2019ab; Bonfils et al., 2018; Goscha & Rapp, 2015; Grim, Rosenberg, Svedberg, & Schön, 2016; Hamann et al., 2016; Metz et al., 2018; Schön et al., 2018; van der Krieke et al., 2013).
Mutual agreement
The fourth phase of the communication process was the mutual agreement. The service users and health professionals discuss and finally arrive at a consensus about diagnostic decisions and further treatment plans (Perestelo‐Perez et al., 2017). They make decisions together, and collaboratively agree on the decision (Grim et al., 2016).
Follow‐up
Being offered follow‐up encounters was described as the important phase. This is because questions or worries of the service users might arise after the decision (Schön et al., 2018). The health professionals follow the progress of the users to monitor how long a decision remains in effect and the possibilities for revising the decision (Grim et al., 2016). Continuous evaluation and adaptation are needed (Grim et al., 2016).
3.1.3. User‐friendly visualization
The attribute of user‐friendly visualization was mainly derived from the information sharing phase of the communication process. When explaining the diagnosis and related options, the health professionals are devoid of medical jargon (Grim et al., 2016), rather they are familiar with plain language, simple statistics, and narrative stories in consideration of the users' different literacy and recovery levels (Martin et al., 2015; Velligan et al., 2016; Zaini et al., 2018). Tailor‐made verbal information is essential (Chong et al., 2013b), and combination with visible information is also important (Grim et al., 2016). The health professionals incorporate readily understood graphs and icons including personalized graphics about their mental health conditions in their written summaries (Metz et al., 2018). For the service users, getting information visually facilitates not only ease of understanding but also opportunity to review it at home (Aoki et al., 2019a). The service users can print the checkbox form and take it with them to further encounters (van der Krieke et al., 2013). In that context, much of the reports in the literature have used various types of decision aids (booklets, web‐based online instruments, tablet and smartphone) as support tools to facilitate the decision‐making process.
3.1.4. Broader stakeholder approach
In many articles, broader stakeholders had important roles during the SDM process (e.g., health professionals, formal/informal carers). For a shared decision to be carried out, all health professionals who are in the clinical team should be informed and they should contribute as needed (Giacco, Mavromara, Gamblen, Conneely, & Priebe, 2018). Interprofessional collaboration consisting of different professions (e.g., psychiatrists, nurses, psychologists, pharmacists, social workers, occupational therapists) is perceived to facilitate SDM by addressing time constraints, allowing more opportunities for the users to discuss their concerns and opinions (Chong et al., 2013a). Nurses can serve as a bridge between the user and the psychiatrist, translating technical information and helping them as a decision coach, to further clarify the user's preferences and values (Aoki et al., 2019b; Paudel et al., 2018; Raue et al., 2019). Furthermore, engaging the involvement of loved ones as other potential carers, such as family members, and providing them information about mental illness and treatments are identified as facilitators to the SDM process (Chong et al., 2013b). The family members can provide valuable input about the service users' experiences with treatments (Eliacin et al., 2015).
3.2. Antecedents
Six antecedents and five related sub‐themes were extracted (Appendix 2).
3.2.1. Long‐term and complex illness
The first antecedent was characteristic to this targeted population on the premise. SMI is a long‐term complex disorder fluctuating over time and often recurring (Grim et al., 2016; Hamann et al., 2016; Lukens, Solomon, & Sorenson, 2013). Subsequently, as treatment decisions are also complex and are frequently made (Fukuiet al., 2014; Grim et al., 2016), it is important to consider symptom severity and the phase of the mental health disturbance during the decision‐making process (Luciano et al., 2019). Lukens et al. (2013) insist that success in long‐term care is dependent upon active user involvement because it is the user and not the health professional who is most responsible for making the decision.
3.2.2. Power imbalance
This antecedent was ascribed as the traditional relationship between the service users and health professionals in the mental health field. An inevitable and very real power structure exists between the users and health professionals (Fukui et al., 2014). Mental health services have a history showing that health professionals have been hesitant about patient's active involvement in decision making (Ishii et al., 2017). It is crucial to be aware of hierarchies and disparities of power in any decision‐making process (Stacey et al., 2016). SDM implies giving up decisional power (Hamann et al., 2012) and aims to change the traditional power asymmetry by strengthening the exchange of information and the decisional position of the users (Hamann, Bühner, & Rüsch, 2017a). Mikesell et al. (2016) suggest that the service users can treat the professionals' expertise and knowledge as superior, but they do not have to perceive it as such, just because of the professionals' authority.
3.2.3. Global trend
Several global trends which challenge traditional professionals' authority were emphasized in many articles. First, the active participation of the users in the decision‐making process has been increasingly advocated (Klausen, Blix, Karlsson, Haugsgjerd, & Lorem, 2017; Perestelo‐Perez et al., 2017). Government policies in many countries are currently more interested in promoting user‐centered healthcare (Chong et al., 2013b; Klingaman et al., 2015; Sather, Iversen, Svindseth, Crawford, & Vasset, 2019; Younas, Bradley, Holmes, Sud, & Maidment, 2016). Second, in recent years, every part of mental health care is being committed to recovery, increasing emphasis of the users' roles as active participants (Mahone et al., 2011). SDM in the mental health field is conceptually congruent with this recovery movement, as it is considered to be a central component of the recovery‐oriented system (Park et al., 2014). Third, information technology can offer the users more involvement in self‐understanding and self‐care of their mental illnesses (Woltmann et al., 2011). Compared with the past, the users have a greater access to information regarding their diseases and treatments (Hamera et al., 2010). The internet is no longer a rare resource for finding general information based on research evidence, in addition to the experience‐based knowledge of others (Grim et al., 2016).
3.2.4. Users' desire
Besides the global trend above, many articles reported that the service users themselves have a considerable desire to participate in decision making about their own treatment. Being offered options and being asked one's views about treatments for mental illness are nearly universally preferred (Park et al., 2014). Few users endorse a paternalistic, professional‐driven, decision‐making style (Woltmann & Whitley, 2010). Inpatients are no exception. Involuntary hospital users also wish to be involved in decisions within the hospital (Giacco et al., 2018). The service users are willing to be part of their care and learn more how to manage their own health problems (Sather et al., 2019). Furthermore, they want to share responsibility for deciding what the best treatment/care is (De Las Cuevas, Peñate, & de Rivera, 2014).
3.2.5. Concerns
Despite the positive global trend and service users' desire, the concerns regarding SDM peculiar to SMI were also identified. First, the health professionals' concerns were raised about the capacity of users with SMI to participate in decision making. Lack of cognitive ability associated with illnesses was frequently proposed as concerns to engaging the users in SDM. Whether the users would be able to communicate effectively with health professionals was described (An, Kim, & Kim, 2017). Second, time constraints were raised. SDM tends to be perceived of as a time‐consuming method (Schön et al., 2018). Particularly, outpatients' services have many users to visit in a very short time (Zaini et al., 2018). This may make it difficult to prioritize time for implementing new methods (Schön et al., 2018).
3.2.6. Stigma
Several articles pointed out stigma associated with mental illness. Many mental health service users feel the stigma associated with their diagnosis (Klausen et al., 2017; Lovell, Bee, & Brooks, 2018). This negatively influences the users' attitudes on SDM (Chong et al., 2013b). When the users suffer from self‐stigma and shame, then their behaviors may become less participatory and less critical during the communication with the health professionals (Hamann et al., 2017a). The health professionals' perception of the stigma associated with mental health services also exists within themselves or the healthcare system itself (Chong et al., 2013b).
3.3. Consequences
Four consequences and 12 related sub‐themes were extracted (Appendix 3).
3.3.1. Decision‐making related outcomes
One of the widely cited consequences was decision making‐related outcomes. SDM could activate the service users to take great engagement in decision making, motivating them to be involved in the decision‐making process (Hamann et al., 2011). Thereby, SDM led the users with SMI to less conflict (Metz et al., 2019; Perestelo‐Perez et al., 2017), more satisfaction (LeBlanc et al., 2015; Woltmann et al., 2011), and being more responsible for their decisions and actions (Hamann et al., 2011). SDM did not extend time required for decision‐making consultation/encounters (Aoki et al., 2019b; Bonfils et al., 2018; LeBlanc et al., 2015).
3.3.2. Users' changes
Several changes of the service users were identified through the SDM process. First, the service users became more knowledgeable about mental illnesses, treatment options, rehabilitation services, and themselves (LeBlanc et al., 2015; Perestelo‐Perez et al., 2017; Woltmann et al., 2011). Second, SDM could boost the service users' behaviors in persisting on the chosen treatment/care (Hamann et al., 2011; Ishii et al., 2017; Raue et al., 2019). Third, the service users could feel empowered and more self‐respect (Hamann, Parchmann, & Sassenberg, 2017b; Lovell et al., 2018), and then became less dependent on the health providers (Lukens et al., 2013). Rather, they implemented active self‐management of illnesses while developing strategies to cope and take charge of their life with SMI (Matthias, Salyers, Rollins, & Frankel, 2012; Matthias et al., 2017). Fourth, SDM could promote the service users' wellness (Goscha & Rapp, 2015; Ramon, Morant, Stead, & Perry, 2017). Not many but some studies reported that SDM could improve the users' condition and some symptoms (Zaini et al., 2018; Metz et al., 2019).
3.3.3. Professionals' changes
The health professionals also changed in some aspects. SDM contributed to becoming more aware of the health professionals' own communication patterns with the service users (Schön et al., 2018). The health professionals became more aware of the users' views including concerns and worries (Woltmann et al., 2011). Furthermore, they gained confidence to open dialogs about mental illnesses and related options with the service users (Ramon et al., 2017).
3.3.4. Enhanced relationship
Besides each party's changes described above, the user–provider relationship was also enhanced. SDM led the service users to view the relationship with their psychiatrists as improved and reliable as it could increase the effectiveness of communication between two parties (Goscha & Rapp, 2015; Yamaguchi et al., 2017). The service users and health professionals moved toward more equal and collaborative discussion (Ramon et al., 2017). SDM could help to demonstrate an equalization of decision‐making power (Grim et al., 2016; Hamann et al., 2011). It could also build trust and strengthen the therapeutic relationship between the user and professional (Martin et al., 2015; Matthias et al., 2014).
The attributes, antecedents and consequences emerging from this review are summarized in Figure 2.
FIGURE 2.
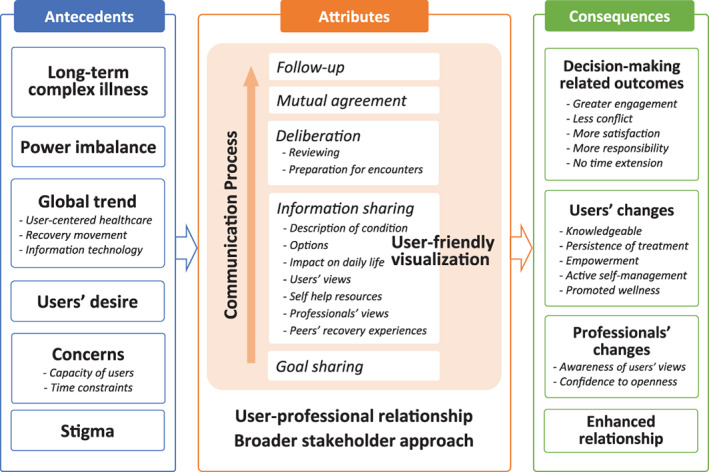
Concept model of shared decision making for adults with severe mental illness
3.4. Surrogate terms
Surrogate terms of SDM for adults with SMI included “concordance” (Ali, Smith, Mican, & Brown, 2015; De Las Cuevas et al., 2011), “patient involvement in decision‐making” (Giacco et al., 2018; Hamann et al., 2016; McCabe, Khanom, Bailey, & Priebe, 2013) “consumer involvement in decision‐making” (Chong et al., 2013a; Matthias et al., 2017; McCabe et al., 2013), and “involvement in care planning” (Lovell et al., 2018) to describe SDM about care and treatment between users and professionals. “Recovery‐oriented care” (Paudel et al., 2018; Schön et al., 2018), “consumer‐oriented approach” (Hamann et al., 2017a), and “patient‐centered approach” (Shepherd, Shorthouse, & Gask, 2014) were also surrogate terms for SDM for adults with SMI to describe respect for users' preferences, autonomy, and active management.
4. DISCUSSION
4.1. Theoretical definition
Shared decision making for adults with SMI is a communication process based on a user–professional relationship in various settings. It is delivered through sharing goals and information to reach agreement, including follow‐up. The process can be promoted by involving user‐friendly visualization techniques and broader stakeholders. SDM for adults with SMI may overcome traditional power imbalances and bring about changes among both users and professionals that could enhance the dyadic relationship.
4.2. Traits of SDM for adults with SMI
Charles, Gafni, and Whelan (1997) defined an SDM model that has the most widely recognized core features in the medical field. This model involves at least two participants – physician and patient (Charles et al., 1997). Both parties share information, take steps to build a consensus about the preferred treatment, and reach an agreement on the treatment to implement (Charles et al., 1997). Although the SDM literature in the mental health field has been developing in alliance with the Charles model similar to other somatic areas, this concept analysis could provide two worthwhile findings that would be helpful to understand the theoretical principles of SDM, which are peculiar to people with SMI. Especially, multidimensional concepts emerging from the information‐sharing phase are noteworthy. First, even in treatment decision‐making where medication options are proposed, it appears to be important to share their self‐help resources for symptom relief or relapse prevention. Individuals with SMI are developing their own wellness activities using their strengths to cope with long‐term complex illnesses. Martin et al. (2015) suggest that the service users' strengths could be integrated into treatment discussions. Next, although providing the line of research evidence regarding treatment options is emphasized when conducting SDM in somatic areas (Légaré et al., 2018), recovery experiences of others would be helpful for people with SMI during the SDM process. Along with an interprofessional approach that could promote eliciting the service users' frank and honest views, giving a chance to access narrative stories of people with similar conditions might be useful.
4.3. Overcoming barriers to SDM for adults with SMI
Several antecedents that might become barriers to implement SDM in the mental health field appeared, but there were also attributes that could overcome these barriers. First, despite the concerns about users' capacity to participate in the decision‐making process, this review found the feasibility of SDM for adults with SMI, giving practical examples including those in acute wards (An et al., 2017; Hamann et al., 2011, 2017; Ishii et al., 2017; Kivelitz et al., 2018; Stacey et al., 2016; Velligan et al., 2016; Zisman‐Ilani et al., 2019). Using user‐friendly visualization could be a bridge to allay such concerns and worries about the users' capacity. As the antecedent shows, SMI is a long‐term complex disease and faces various decisions depending on the illness severity or individual life stage. On each occasion, it is crucial for the health professionals to ensure that the users' abilities are properly assessed. Otherwise, the decisions that should be in the users' hands might be driven by the health professionals following the traditional hierarchy. Second, contrary to the time constraints assumed, the consequences have identified no time extension thus far. As Chong et al. (2013a) suggest, interprofessional collaboration could work for alleviating this matter related to busy outpatient services. Third, stigma may also become a barrier to implement SDM. As the attribute shows, SDM requires understanding of their own current condition. People must overcome their debilitating self‐stigmatization to face their own mental illness (Corrigan & Watson, 2002). It is considered that the greater the stigma, the more difficult it is to overcome the debilitating effect of one's own self‐stigmatization. Health professionals who support the decision‐making processes of adults with SMI need to assume that the service users are struggling with stigma and must listen carefully to their feelings while simultaneously sharing their own goals as a partner (Amador, 2012). Moreover, behaviors and efforts to create a stigma‐free society are also needed.
SDM for adults with SMI may be able to overcome those barriers and bring about changes that could enhance the user–professional relationship.
5. LIMITATIONS
This review included only papers written in English; therefore, possible relevant reports in other languages were excluded.
6. CONCLUSIONS
SDM for adults with SMI is a communication process involving user‐friendly visualization techniques and broader stakeholders. The process may overcome traditional power imbalance and bring about changes to both users and professionals that could enhance the dyadic relationship. The findings may be useful for understanding the theoretical structure for the current usage of this term. The results are helpful in carrying out treatment/care decision making in line with the service users' values.
CONFLICT OF INTEREST
Y.A. has received the Japan Society for the Promotion of Science‐in‐Aid for Scientific Research and lecture fees from MSD.
AUTHOR CONTRIBUTIONS
Y.A. designed this study, carried out the literature search, drafted the manuscript, and approved the final manuscript.
Supporting information
Appendix S1: Supporting Information
Appendix S2: Supporting Information
Appendix S3: Supporting Information
ACKNOWLEDGMENTS
I would like to thank Professor Junko Tashiro of St. Luke's International University for her valuable comments. I greatly appreciate Dr. Edward Barroga (https://orcid.org/0000-0002-8920-2607), Medical Editor and Professor of Academic Writing at St. Luke's International University for editing the manuscript.
Aoki Y. Shared decision making for adults with severe mental illness: A concept analysis. Jpn J Nurs Sci. 2020;17:e12365 10.1111/jjns.12365
REFERENCES
*Studies included in this concept analysis
- * Alegria, M. , Nakash, O. , Johnson, K. , Ault‐Brutus, A. , Carson, N. , Fillbrunn, M. , … Shrout, P. E. (2018). USA effectiveness of the DECIDE interventions on shared decision making and perceived quality of care in behavioral health with multicultural patients: A randomized clinical trial. JAMA Psychiatry, 75(4), 325–335. 10.1001/jamapsychiatry.2017.4585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Ali, S. , Smith, T. L. , Mican, L. , & Brown, C. (2015). Psychiatric providers' willingness to participate in shared decision making when prescribing psychotropics. The Journal of Pharmacy Technology, 31(5), 212–218. 10.1177/8755122515578288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Aljumah, K. , & Hassali, M. A. (2015). Impact of pharmacist intervention on adherence and measurable patient outcomes among depressed patients: A randomised controlled study. BMC Psychiatry, 15, 219 10.1186/s12888-015-0605-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amador, X. (2012). I am not sick, I don't need help! How to help someone with mental illness accept treatment. 10th anniversary Ed. New York, NY: Vida Press. [Google Scholar]
- * An, S. Y. , Kim, G. H. , & Kim, J. Y. (2017). Effectiveness of shared decision‐making training program in people with schizophrenia in South Korea. Perspectives in Psychiatric Care, 53(2), 111–118. 10.1111/ppc.12144 [DOI] [PubMed] [Google Scholar]
- * Aoki, Y. , Furuno, T. , Watanabe, K. , & Kayama, M. (2019a). Psychiatric outpatients' experiences with shared decision‐making: A qualitative descriptive study. Journal of Communication in Healthcare, 12(2), 102–111. 10.1080/17538068.2019.1612212 [DOI] [Google Scholar]
- * Aoki, Y. , Takaesu, Y. , Inoue, M. , Furuno, T. , Kobayashi, Y. , Chiba, H. , … Watanabe, K. (2019b). Seven‐day shared decision making for outpatients with first episode of mood disorders among university students: A randomized controlled trial. Psychiatry Research, 281, 112531 10.1016/j.psychres.2019.112531 [DOI] [PubMed] [Google Scholar]
- Barry, M. J. , & Edgman‐Levitan, S. (2012). Shared decision making ‐ pinnacle of patient‐centered care. The New England Journal of Medicine, 366(9), 780–781. 10.1056/NEJMp1109283 [DOI] [PubMed] [Google Scholar]
- * Bonfils, K. A. , Dreison, K. C. , Luther, L. , Fukui, S. , Dempsey, A. E. , Rapp, C. A. , & Salyers, M. P. (2018). Implementing CommonGround in a community mental health center: Lessons in a computerized decision support system. Psychiatric Rehabilitation Journal, 41(3), 216–223. 10.1037/prj0000225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Brooks, H. , Harris, K. , Bee, P. , Lovell, K. , Rogers, A. , & Drake, R. (2017). Exploring the potential implementation of a tool to enhance shared decision making (SDM) in mental health services in the United Kingdom: A qualitative exploration of the views of service users, carers and professionals. International Journal of Mental Health Systems, 11, 42 10.1186/s13033-017-0149-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Campbell, S. R. , Holter, M. C. , Manthey, T. J. , & Rapp, C. A. (2014). The effect of CommonGround software and decision support center. American Journal of Psychiatric Rehabilitation, 17(2), 166–180. 10.1080/15487768.2014.916126 [DOI] [Google Scholar]
- Charles, C. , Gafni, A. , & Whelan, T. (1997). Shared decision‐making in the medical encounter: What does it mean? (or it takes at least two to tango). Social Science & Medicine, 44(5), 681–692. [DOI] [PubMed] [Google Scholar]
- * Chong, W. W. , Aslani, P. , & Chen, T. F. (2013a). Multiple perspectives on shared decision‐making and interprofessional collaboration in mental healthcare. Journal of Interprofessional Care, 27(3), 223–230. 10.3109/13561820.2013.767225 [DOI] [PubMed] [Google Scholar]
- * Chong, W. W. , Aslani, P. , & Chen, T. F. (2013b). Shared decision‐making and interprofessional collaboration in mental healthcare: A qualitative study exploring perceptions of barriers and facilitators. Journal of Interprofessional Care, 27(5), 373–379. 10.3109/13561820.2013.785503 [DOI] [PubMed] [Google Scholar]
- Corrigan, P. W. , & Watson, A. C. (2002). Understanding the impact of stigma on people with mental illness. World Psychiatry, 1(1), 16–20. [PMC free article] [PubMed] [Google Scholar]
- Cosh, S. , Zenter, N. , Ay, E. S. , Loos, S. , Slade, M. , De Rosa, C. , & Puschner, B. (2017). Clinical decision making and mental health service use among persons with severe mental illness across Europe. Psychiatric Services, 68(9), 970–974. 10.1176/appi.ps.201600114 [DOI] [PubMed] [Google Scholar]
- Deegan, P. (1988). Recovery: The lived experience of rehabilitation. Psychosocial Rehabilitation Journal, 9(4), 11–19. [Google Scholar]
- * De Las Cuevas, C. , Peñate, W. , & de Rivera, L. (2014). To what extent is treatment adherence of psychiatric patients influenced by their participation in shared decision making? Patient Preference and Adherence, 8, 1547–1553. 10.2147/PPA.S73029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * De Las Cuevas, C. , Rivero, A. , Perestelo‐Perez, L. , Gonzalez, M. , Perez, J. , & Peñate, W. (2011). Psychiatric patients' attitudes towards concordance and shared decision making. Patient Education and Counseling, 85(3), e245–e250. 10.1016/j.pec.2011.02.015 [DOI] [PubMed] [Google Scholar]
- Drake, R. E. , & Deegan, P. E. (2009). Shared decision making is an ethical imperative. Psychiatric Services, 60(8), 1007 10.1176/appi.ps.60.8.1007 [DOI] [PubMed] [Google Scholar]
- Duncan, E. , Best, C. , & Hagen, S. (2010). Shared decision making interventions for people with mental health conditions. Cochrane Database of Systematic Reviews, 20(1), CD007297 10.1002/14651858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Ehrlich, C. , & Dannapfel, P. (2017). Shared decision making: People with severe mental illness experiences of involvement in the care of their physical health. Mental Health & Prevention, 5, 21–26. 10.1016/j.mhp.2016.12.002 [DOI] [Google Scholar]
- * Eliacin, J. , Salyers, M. P. , Kukla, M. , & Matthias, M. S. (2015). Factors influencing patients' preferences and perceived involvement in shared decision‐making in mental health care. Journal of Mental Health, 24(1), 24–28. 10.3109/09638237.2014.954695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Finnerty, M. , Austin, E. , Chen, Q. , Layman, D. , Kealey, E. , Ng‐Mak, D. , … Hoagwood, K. (2019). Implementation and use of a client‐facing web‐based shared decision‐making system (MyCHOIS‐CommonGround) in two specialty mental health clinics. Community Mental Health Journal, 55(4), 641–650. 10.1007/s10597-018-0341-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Finnerty, M. T. , Layman, D. M. , Chen, Q. , Leckman‐Westin, E. , Bermeo, N. , Ng‐Mak, D. S. , … Hoagwood, K. E. (2018). Use of a web‐based shared decision‐making program: Impact on ongoing treatment engagement and antipsychotic adherence. Psychiatric Services, 69(12), 1215–1221. 10.1176/appi.ps.201800130 [DOI] [PubMed] [Google Scholar]
- * Fukui, S. , Matthias, M. S. , & Salyers, M. P. (2015). Core domains of shared decision‐making during psychiatric visits: Scientific and preference‐based discussions. Administration and Policy in Mental Health and Mental Health Services Research, 42(1), 40–46. 10.1007/s10488-014-0539-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Fukui, S. , Salyers, M. P. , Matthias, M. S. , Collins, L. , Thompson, J. , Coffman, M. , & Torrey, W. C. (2014). Predictors of shared decision making and level of agreement between consumers and providers in psychiatric care. Community Mental Health Journal, 50(4), 375–382. 10.1007/s10597-012-9584-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Giacco, D. , Mavromara, L. , Gamblen, J. , Conneely, M. , & Priebe, S. (2018). Shared decision‐making with involuntary hospital patients: A qualitative study of barriers and facilitators. BJPsych Open, 4(3), 113–118. 10.1192/bjo.2018.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Goscha, R. , & Rapp, C. (2015). Exploring the experiences of client involvement in medication decisions using a shared decision making model: Results of a qualitative study. Community Mental Health Journal, 51(3), 267–274. 10.1007/s10597-014-9759-y [DOI] [PubMed] [Google Scholar]
- * Grim, K. , Rosenberg, D. , Svedberg, P. , & Schön, U. K. (2016). Shared decision‐making in mental health care: A user perspective on decisional needs in community‐based services. International Journal of Qualitative Studies on Health and Well‐Being, 11, 30563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Hamann, J. , Bühner, M. , & Rüsch, N. (2017a). Self‐stigma and consumer participation in shared decision making in mental health services. Psychiatric Services, 68(8), 783–788. 10.1176/appi.ps.201600282 [DOI] [PubMed] [Google Scholar]
- * Hamann, J. , Kohl, S. , McCabe, R. , Bühner, M. , Mendel, R. , Albus, M. , & Bernd, J. (2016). What can patients do to facilitate shared decision making? A qualitative study of patients with depression or schizophrenia and psychiatrists. Social Psychiatry and Psychiatric Epidemiology, 51(4), 617–625. 10.1007/s00127-015-1089-z [DOI] [PubMed] [Google Scholar]
- * Hamann, J. , Mendel, R. , Bühner, M. , Kissling, W. , Cohen, R. , Knipfer, E. , & Eckstein, H. H. (2012). How should patients behave to facilitate shared decision making: The doctors' view. Health Expectations, 15(4), 360–366. 10.1111/j.1369-7625.2011.00682.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Hamann, J. , Mendel, R. , Meier, A. , Asani, F. , Pausch, E. , Leucht, S. , & Kissling, W. (2011). “How to speak to your psychiatrist”: Shared decision‐making training for inpatients with schizophrenia. Psychiatric Services, 62(10), 1218–1221. 10.1176/ps.62.10 [DOI] [PubMed] [Google Scholar]
- * Hamann, J. , Parchmann, A. , & Sassenberg, N. (2017b). Training patients with schizophrenia to share decisions with their psychiatrists: A randomized‐controlled trial. Social Psychiatry and Psychiatric Epidemiology, 52(2), 175–182. 10.1007/s00127-016-1327-z [DOI] [PubMed] [Google Scholar]
- * Hamera, E. , Pallikkathayil, L. , Baker, D. , & White, D. (2010). Descriptive study of shared decision making about lifestyle modifications with individuals who have psychiatric disabilities. Journal of the American Psychiatric Nurses Association, 16(5), 280–287. 10.1177/1078390310384863 [DOI] [PubMed] [Google Scholar]
- * Ishii, M. , Okumura, Y. , Sugiyama, N. , Hasegawa, H. , Noda, T. , Hirayasu, Y. , & Ito, H. (2017). Feasibility and efficacy of shared decision making for first‐admission schizophrenia: A randomized clinical trial. BMC Psychiatry, 17(1), 52 10.1186/s12888-017-1218-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson, N. (2001). What is recovery? A conceptual model and explication. Psychiatric Services, 52(4), 482–485. [DOI] [PubMed] [Google Scholar]
- * Kivelitz, L. , Härter, M. , Mohr, J. , Melchior, H. , Goetzmann, L. , Warnke, M. H. , … Dirmaier, J. (2018). Choosing the appropriate treatment setting: Which information and decision‐making needs do adult inpatients with mental disorders have? A qualitative interview study. Patient Preference and Adherence, 12, 823–833. 10.2147/PPA.S164160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Klausen, R. K. , Blix, B. H. , Karlsson, M. , Haugsgjerd, S. , & Lorem, G. F. (2017). Shared decision making from the service users' perspective: A narrative study from community mental health centers in northern Norway. Social Work in Mental Health, 15(3), 354–371. 10.1080/15332985.2016.1222981 [DOI] [Google Scholar]
- * Klingaman, E. A. , Medoff, D. R. , Park, S. G. , Brown, C. H. , Fang, L. , Dixon, L. B. , … Kreyenbuhl, J. A. (2015). Consumer satisfaction with psychiatric services: The role of shared decision making and the therapeutic relationship. Psychiatric Rehabilitation Journal, 38(3), 242–248. 10.1037/prj0000114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Kreyenbuhl, J. A. , Medoff, D. R. , McEvoy, J. P. , Smith, T. E. , Hackman, A. L. , Nossel, I. R. , … Buchanan, R. W. (2016). The RAISE connection program: Psychopharmacological treatment of people with a first episode of schizophrenia. Psychiatric Services, 67(12), 1300–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latimer, E. A. , Bond, G. R. , & Drake, R. E. (2011). Economic approaches to improving access to evidence‐based and recovery‐oriented services for people with severe mental illness. The Canadian Journal of Psychiatry, 56(9), 523–529. 10.1177/070674371105600903 [DOI] [PubMed] [Google Scholar]
- * LeBlanc, A. , Herrin, J. , Williams, M. D. , Inselman, J. W. , Branda, M. E. , Shah, N. D. , … Montori, V. M. (2015). Shared decision making for antidepressants in primary care: A cluster randomized trial. JAMA Internal Medicine, 175(11), 1761–1770. 10.1001/jamainternmed [DOI] [PMC free article] [PubMed] [Google Scholar]
- Légaré, F. , Adekpedjou, R. , Stacey, D. , Turcotte, S. , Kryworuchko, J. , Graham, I. D. , … Donner‐Banzhoff, N. (2018). Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane Database of Systematic Reviews, 7, CD006732 10.1002/14651858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Lovell, K. , Bee, P. , & Brooks, H. (2018). Embedding shared decision‐making in the care of patients with severe and enduring mental health problems: The EQUIP pragmatic cluster randomised trial. PLoS One, 13(8), e0201533 10.1371/journal.pone.0201533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Luciano, M. , Sampogna, G. , Del Vecchio, V. , Loos, S. , Slade, M. , Clarke, E. , … CEDAR Study Group . (2019). When does shared decision making is adopted in psychiatric clinical practice? Results from a European multicentric study. European Archives of Psychiatry and Clinical Neuroscience. 10.1007/s00406-019-01031-y [DOI] [PubMed] [Google Scholar]
- * Lukens, J. M. , Solomon, P. , & Sorenson, S. B. (2013). Shared decision making for clients with mental illness: A randomized factorial survey. Research on Social Work Practice, 23(6), 694–705. 10.1177/1049731513489734 [DOI] [Google Scholar]
- * Mahone, I. H. , Farrell, S. , Hinton, I. , Johnson, R. , Moody, D. , Rifkin, K. , … Region Ten CSB/UVA School of Nursing Partnership . (2011). Shared decision making in mental health treatment: Qualitative findings from stakeholder focus groups. Archives of Psychiatric Nursing, 25(6), e27–e36. 10.1016/j.apnu.2011.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Martin, L. , Perlman, C. , & Bieling, P. (2015). Using the RAI‐MH to support shared decision‐making in mental healthcare. Healthcare Management Forum, 28(4), 163–166. 10.1177/0840470415581231 [DOI] [PubMed] [Google Scholar]
- * Matthias, M. S. , Fukui, S. , Kukla, M. , Eliacin, J. , Bonfils, K. A. , Firmin, R. L. , … Salyers, M. P. (2014). Consumer and relationship factors associated with shared decision making in mental health consultations. Psychiatric Services, 65(12), 1488–1491. 10.1176/appi.ps.201300563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Matthias, M. S. , Fukui, S. , & Salyers, M. P. (2017). What factors are associated with consumer initiation of shared decision making in mental health visits? Administration and Policy in Mental Health and Mental Health Services Research, 44(1), 133–140. 10.1007/s10488-015-0688-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Matthias, M. S. , Salyers, M. P. , Rollins, A. L. , & Frankel, R. M. (2012). Decision making in recovery‐oriented mental health care. Psychiatric Rehabilitation Journal, 35(4), 305–314. 10.2975/35.4.2012.305.314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * McCabe, R. , Khanom, H. , Bailey, P. , & Priebe, S. (2013). Shared decision‐making in ongoing outpatient psychiatric treatment. Patient Education and Counseling, 91(3), 326–328. 10.1016/j.pec.2012.12.020 [DOI] [PubMed] [Google Scholar]
- * Metz, M. , Elfeddali, I. , Veerbeek, M. , de Beurs, E. , Beekman, A. , & van der Feltz‐Cornelis, C. (2018). Effectiveness of a multi‐facetted blended eHealth intervention during intake supporting patients and clinicians in shared decision making: A cluster randomised controlled trial in a specialist mental health outpatient setting. PLoS One, 13(6), e0199795 10.1371/journal.pone.0199795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Metz, M. J. , Veerbeek, M. A. , Twisk, J. W. R. , van der Feltz‐Cornelis, C. M. , de Beurs, E. , & Beekman, A. T. F. (2019). Shared decision‐making in mental health care using routine outcome monitoring: Results of a cluster randomised‐controlled trial. Social Psychiatry and Psychiatric Epidemiology, 54(2), 209–219. 10.1007/s00127-018-1589-8 [DOI] [PubMed] [Google Scholar]
- * Mikesell, L. , Bromley, E. , Young, A. S. , Vona, P. , & Zima, B. (2016). Integrating client and clinician perspectives on psychotropic medication decisions: Developing a communication‐centered epistemic model of shared decision making for mental health contexts. Health Communication, 31(6), 707–717. 10.1080/10410236.2014.993296 [DOI] [PubMed] [Google Scholar]
- * Nott, J. , Mcintosh, A. , Taube, C. , & Taylor, M. (2018). Shared decision‐making in psychiatry: A study of patient attitudes. Australasian Psychiatry, 26(5), 478–481. 10.1177/1039856218758562 [DOI] [PubMed] [Google Scholar]
- * Park, S. G. , Derman, M. , Dixon, L. B. , Brown, C. H. , Klingaman, E. A. , Fang, L. J. , … Kreyenbuhl, J. (2014). Factors associated with shared decision‐making preferences among veterans with serious mental illness. Psychiatric Services, 65(12), 1409–1413. 10.1176/appi.ps.201400131 [DOI] [PubMed] [Google Scholar]
- * Patel, S. R. , Schnall, R. , Little, V. , Lewis‐Fernández, R. , & Pincus, H. A. (2014). Primary care professional's perspectives on treatment decision making for depression with African Americans and Latinos in primary care practice. Journal of Immigrant and Minority Health, 16(6), 1262–1270. 10.1007/s10903-013-9903-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Paudel, S. , Sharma, N. , Joshi, A. , & Randall, M. (2018). Development of a shared decision making model in a community mental health center. Community Mental Health Journal, 54(1), 1–6. 10.1007/s10597-017-0134-7 [DOI] [PubMed] [Google Scholar]
- * Perestelo‐Perez, L. , Rivero‐Santana, A. , Sanchez‐Afonso, J. A. , Perez‐Ramos, J. , Castellano‐Fuentes, C. L. , Sepucha, K. , & Serrano‐Aguilar, P. (2017). Effectiveness of a decision aid for patients with depression: A randomized controlled trial. Health Expectations, 20(5), 1096–1105. 10.1111/hex.12553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Ramon, S. , Morant, N. , Stead, U. , & Perry, B. (2017). Shared decision‐making for psychiatric medication: A mixed‐methods evaluation of a UKtraining programme for service users and clinicians. International Journal of Social Psychiatry, 63(8), 763–772. 10.1177/0020764017733764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Raue, P. J. , Schulberg, H. C. , Bruce, M. L. , Banerjee, S. , Artis, A. , Espejo, M. , … Romero, S. (2019). Effectiveness of shared decision‐making for elderly depressed minority primary care patients. The American Journal of Geriatric Psychiatry, 27(8), 883–893. 10.1016/j.jagp.2019.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers B. L. (Ed.). (2000). Concept analysis: An evolutionary view. Philadelphia, PA: Saunders. [Google Scholar]
- * Sather, E. W. , Iversen, V. C. , Svindseth, M. F. , Crawford, P. , & Vasset, F. (2019). Patients' perspectives on care pathways and informed shared decision making in the transition between psychiatric hospitalization and the community. Journal of Evaluation in Clinical Practice, 25(6), 1131–1141. 10.1111/jep.13206 [DOI] [PubMed] [Google Scholar]
- * Schön, U. K. , Grim, K. , Wallin, L. , Rosenberg, D. , & Svedberg, P. (2018). Psychiatric service staff perceptions of implementing a shared decision‐making tool: A process evaluation study. International Journal of Qualitative Studies on Health and Well‐Being, 13(1), 1421352 10.1080/17482631.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Shepherd, A. , Shorthouse, O. , & Gask, L. (2014). Consultant psychiatrists' experiences of and attitudes towards shared decision making in antipsychotic prescribing, a qualitative study. BMC Psychiatry, 14, 127 10.1186/1471-244X-14-127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, O. P. (2015). National mental health policy of India: New pathways new hope—A journey on enchanted path. Eastern Journal of Psychiatry, 18(2), 1–2. [Google Scholar]
- * Solberg, L. I. , Crain, A. L. , Rubenstein, L. , Unützer, J. , Whitebird, R. R. , & Beck, A. (2014). How much shared decision making occurs in usual primary care of depression? Journal of the American Board of Family Medicine, 27(2), 199–208. 10.3122/jabfm.2014.02.130164 [DOI] [PubMed] [Google Scholar]
- * Stacey, G. , Felton, A. , Morgan, A. , Stickley, T. , Willis, M. , Diamond, B. , … Dumenya, J. (2016). A critical narrative analysis of shared decision‐making in acute inpatient mental health care. Journal of Interprofessional Care, 30(1), 35–41. 10.3109/13561820.2015.1064878 [DOI] [PubMed] [Google Scholar]
- * Stead, U. , Morant, N. , & Ramon, S. (2017). Shared decision‐making in medication management: Development of a training intervention. BJPsych Bulletin, 41(4), 221–227. 10.1192/pb.bp.116.053819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein, D. J. (2014). A new mental health policy for South Africa. South African Medical Journal, 104(2), 115–116. 10.7196/SAMJ.7938 [DOI] [PubMed] [Google Scholar]
- * Stein, B. D. , Kogan, J. N. , Mihalyo, M. J. , Schuster, J. , Deegan, P. E. , Sorbero, M. J. , & Drake, R. E. (2013). Use of a computerized medication shared decision making tool in community mental health settings: Impact on psychotropic medication adherence. Community Mental Health Journal, 49(2), 185–192. 10.1007/s10597-012-9528-8 [DOI] [PubMed] [Google Scholar]
- Storm, M. , & Edwards, A. (2013). Models of user involvement in the mental health context: Intentions and implementation challenges. Psychiatric Quarterly, 84(3), 313–327. 10.1007/s11126-012-9247-x [DOI] [PubMed] [Google Scholar]
- * van der Krieke, L. , Emerencia, A. C. , Boonstra, N. , Wunderink, L. , de Jonge, P. , & Sytema, S. (2013). A web‐based tool to support shared decision making for people with a psychotic disorder: Randomized controlled trial and process evaluation. Journal of Medical Internet Research, 15(10), e216 10.2196/jmir.2851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hoof, F. , Knispel, A. , Aagaard, J. , Schneider, J. , Beeley, C. , & Keet, R. (2015). The role of national policies and mental health care systems in the development of community care and community support: An international analysis. Journal of Mental Health, 24(4), 202–207. 10.3109/09638237.2015.1036973 [DOI] [PubMed] [Google Scholar]
- * Velligan, D. I. , Roberts, D. L. , Sierra, C. , Fredrick, M. M. , & Roach, M. J. (2016). What patients with severe mental illness transitioning from hospital to community have to say about care and shared decision‐making. Issues in Mental Health Nursing, 37(6), 400–405. 10.3109/01612840.2015.1132289 [DOI] [PubMed] [Google Scholar]
- * Verwijmeren, D. , & Grootens, L. P. (2018). Shared decision making in pharmacotherapy decisions, perceived by patients with bipolar disorder. International Journal of Bipolar Disorders, 6, 21 10.1186/s40345-018-0129-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Woltmann, E. M. , & Whitley, R. (2010). Shared decision making in public mental health care: Perspectives from consumers living with severe mental illness. Psychiatric Rehabilitation Journal, 34(1), 29–36. 10.2975/34.1.2010.29.36 [DOI] [PubMed] [Google Scholar]
- * Woltmann, E. M. , Wilkniss, S. M. , Teachout, A. , McHugo, G. J. , & Drake, R. E. (2011). Trial of an electronic decision support system to facilitate shared decision making in community mental health. Psychiatric Services, 62(1), 54–60. 10.1176/ps.62.1.pss6201_0054 [DOI] [PubMed] [Google Scholar]
- * Wright‐Berryman, J. L. , & Cremering, A. (2017). Physical health decision making and decision aid preferences of individuals with severe mental illness. Social Work in Mental Health, 15(6), 651–662. 10.1080/15332985.2017.1279584 [DOI] [Google Scholar]
- * Yamaguchi, S. , Taneda, A. , Matsunaga, A. , Sasaki, N. , Mizuno, M. , Sawada, Y. , … Ito, J. (2017). Efficacy of a peer‐led, recovery‐oriented shared decision‐making system: A pilot randomized controlled trial. Psychiatric Services, 68(12), 1307–1311. 10.1176/appi.ps.201600544 [DOI] [PubMed] [Google Scholar]
- * Younas, M. , Bradley, E. , Holmes, N. , Sud, D. , & Maidment, I. D. (2016). Mental health pharmacists views on shared decision‐making for antipsychotics in serious mental illness. International Journal of Clinical Pharmacy, 38(5), 1191–1199. 10.1007/s11096-016-0352-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Zaini, S. , Manivanna Bharathy, H. A. , Sulaiman, A. H. , Singh Gill, J. , Ong Hui, K. , Zaman Huri, H. , … Chong Guan, N. (2018). Development of a strategic tool for shared decision‐making in the use of antidepressants among patients with major depressive disorder: A focus group study. International Journal of Environmental Research and Public Health, 15(7), E1402 10.3390/ijerph15071402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Zisman‐Ilani, Y. , Roe, D. , Elwyn, G. , Kupermintz, H. , Patya, N. , Peleg, I. , & Karnieli‐Miller, O. (2019). Shared decision making for psychiatric rehabilitation services before discharge from psychiatric hospitals. Health Communication, 34(6), 631–637. 10.1080/10410236.2018.1431018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting Information
Appendix S2: Supporting Information
Appendix S3: Supporting Information


