Abstract
Background:
This study will appraise the impact of pelvic floor ultrasound (PFU) in diagnosis of postpartum pelvic floor dysfunction (PPPFD).
Methods:
Studies that report the impact of PFU in diagnosis of PPPFD will be examined in Cochrane Library, MEDLINE, EMBASE, PSYCINFO, Scopus, Web of Science, Allied and Complementary Medicine Database, CNKI, and WANGFANG up to June 1, 2020. Grey literature sources will also be searched. All potential case-controlled studies (CCSs) exploring the impact of PFU in diagnosis of PPPFD will be considered for inclusion in this study. Data will be extracted from eligible CCSs for data pooling and meta-analysis. Whenever necessary, we will also perform summary effect size, heterogeneity across studies, study quality assessment, and reporting bias.
Results:
The present study will estimate pooled outcome effects regarding the impact of PFU in diagnosis of PPPFD.
Conclusion:
This study may provide robust evidence to judge the impact of PFU on PPPFD
Systematic review registration:
PROSPERO CRD42020187623.
Keywords: impact, pelvic floor dysfunction, pelvic floor ultrasound, postpartum
1. Introduction
Pelvic floor dysfunction (PFD) is a common disorder that affects ability to control and coordinate pelvic floor muscles.[1–4] It constitutes a spectrum of pathologies[5] and is associated with stress urinary incontinence (SUI), bowel incontinence, pelvic pain, sexual dysfunction, constipation, and pelvic organ prolapse (POP),[6–9] which significantly affect quality of life for patients with PFD.[10–12] It has been estimated that its prevalence varies from 23.7% to 46.2% of women experience at least 1 PFD,[13,14] and its prevalence in females over 40 years old is between 30% and 50%.[15] Its incidence is reported about 58.70% with about 48.3% for POP and 8.7% for SUI.[16] PFD commonly affects women of all ages, but there is a higher risk for pregnancy women after delivery with PFD, also known as postpartum pelvic floor dysfunction (PPPFD).[17–23] Thus, it is very important to diagnose this condition at early stage.
Pelvic floor ultrasound (PFU) is responsible for diagnosis of PPPFD, and a variety of studies have reported the impact of PFU for diagnosis of PPPFD.[24–27] However, little is known about the impact of PFU in diagnosis of PPPFD at evidence-based medicine level. Thus, in order to better understand this issue, we will conduct a systematic review to address the impact of PFU in diagnosis of PPPFD.
2. Methods
2.1. Study registration
This study has been registered on PROSPERO with CRD42020187623. It has been reported following the guideline of Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocol statement.[28]
2.2. Inclusion criteria for study selection
2.2.1. Type of studies
The present study will include case-controlled studies (CCSs) that assessed the impact of PFU in diagnosis of PPPFD.
2.2.2. Type of participants
All adult female patients (over 18 years old) who were diagnosed as PPPFD will be included in this study, regardless educational background, economic status, and severity of PPPFD.
2.2.3. Type of index test
Index test: PFU is used in detecting patients with PPPFD. However, we will exclude combination of PFU and other tests.
Reference test: patients who were detected by magnetic resonance imaging or computed tomography-proven PPPFD will be considered as comparators.
2.2.4. Outcome measurements
Outcomes are sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio.
2.3. Data sources and search strategy
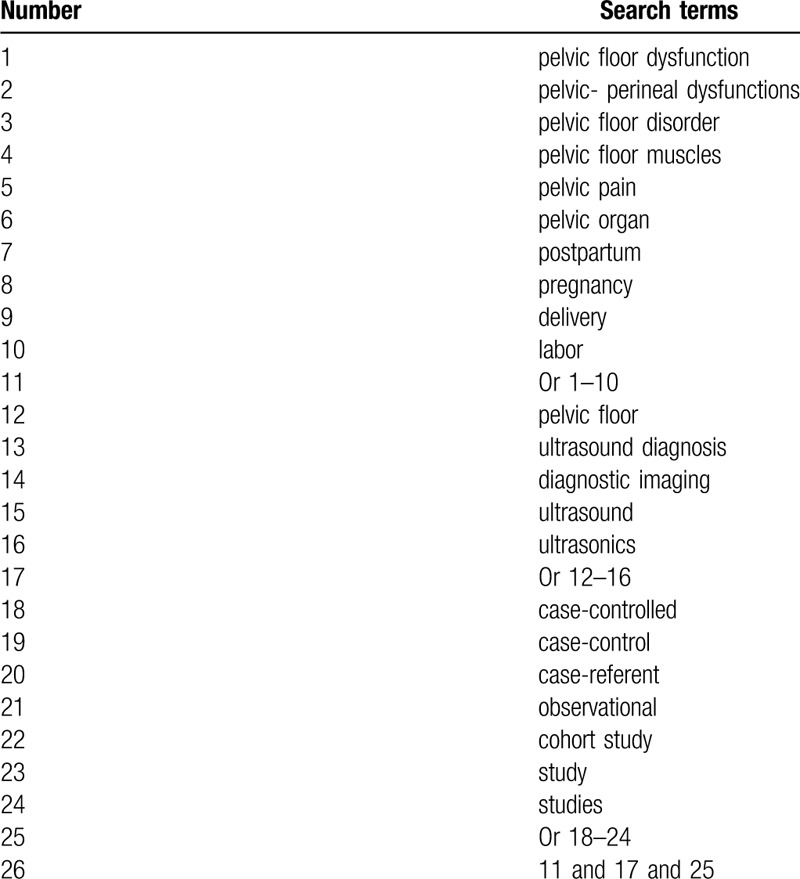
With the help of an academic librarian, this study will carry out a systematic literature search to find out studies that assess the impact of PFU in diagnosis of PPPFD. We will comprehensively search citations in Cochrane Library, MEDLINE, EMBASE, PSYCINFO, Scopus, Web of Science, Allied and Complementary Medicine Database, CNKI and WANGFANG up to June 1, 2020. In addition, grey literature sources, such as conference abstracts, thesis, and dissertation will be searched. All CCSs focusing on the impact of PFU in diagnosis of PPPFD will be included. We will provide search strategy of MEDLINE in Table 1. We will adapt similar search strategies to other electronic databases.
Table 1.
Search strategy applied in MEDLINE database.
2.4. Data collection and analysis
2.4.1. Study selection
Two authors will scan titles and abstracts of studies retrieved utilizing the search strategy from electronic databases and grey literatures. All unconnected studies will be removed. Then, full text of potential studies will be retrieved for inclusion against all inclusion criteria. Any conflicts will be clarified through discussion with a third author. We will summarize study selection in a flow diagram.
2.4.2. Data extraction
Two independent authors will extract data from all eligible studies utilizing data extraction sheet. It includes general information of included studies and patients (such as authors, title, time of publication, country, etc), sample size, inclusion and exclusion criteria, study quality, index and reference tests, and outcomes. Any disagreements will be resolved by a third author through discussion. If any missing or unclear information is identified, we will contact primary authors to request them.
2.5. Quality assessment
All eligible CCSs will be assessed by 2 independent authors using Quality Assessment of Diagnostic Accuracy Studies tool.[29] Any opposition between 2 authors will be cleared up by a third author through discussion.
2.6. Statistical analysis
This study will apply RevMan V.5.3 software (London, UK) and Stata V.12.0 software (StataCorp; USA) to perform data analysis. We will summarize specific characteristics and study findings in tables. We will estimate outcome as descriptive statistics and 95% confidence intervals, and will perform plots of descriptive forest and summary receiver operating characteristic. Heterogeneity will be checked by I2 statistic. I2 ≤ 50% suggests low heterogeneity, and Mantel-Haenszel fixed-effects model will be used, while I2 > 50% indicates significant heterogeneity, and Mantel-Haenszel random-effects model will be applied. If there is low heterogeneity, we will conduct meta-analysis based on the sufficient eligible studies on the same outcome indicator. If there is substantial heterogeneity, we will carry out subgroup analysis to examine its possible sources.
2.7. Subgroup analysis
This study will perform subgroup analysis according to the different study characteristics, study qualities, and outcomes.
2.8. Sensitivity analysis
This study will conduct sensitivity analysis to examine stability of study findings by removing low quality studies.
2.9. Reporting bias
This study will test reporting bias using funnel plots and associated regression tests.[30,31]
2.10. Ethics and dissemination
This study will only extract data from published studies, thus no ethic approval is required. It will be published in a relevant peer-reviewed journal.
3. Discussion
Although many studies have reported the impact of PFU in diagnosis on PPPFD, no systematic review or/and meta-analysis is conducted to explore the impact of PFU in detection of PPPFD. Thus, this is the first systematic review to comprehensively search and summarize most recent evidence on the impact of PFU in diagnosis of PPPFD, and to synthesize the effect estimates from all included studies. The findings of this study will inform clinical practice and further studies focusing on the impact of PFU in diagnosis of PPPFD.
Author contributions
Conceptualization: Tian-you Xin, Xiao-hui Wang.
Data curation: Fan-bo Wang, Rong Rong, Jing-jun Xu, Xiao-hui Wang.
Formal analysis: Rong Rong, Guang Yang, Tian-you Xin.
Funding acquisition: Xiao-hui Wang.
Investigation: Xiao-hui Wang.
Methodology: Fan-bo Wang, Rong Rong, Guang Yang, Tian-you Xin.
Project administration: Xiao-hui Wang.
Resources: Fan-bo Wang, Rong Rong, Jing-jun Xu, Guang Yang, Hai-bo Tang.
Software: Fan-bo Wang, Rong Rong, Jing-jun Xu, Guang Yang, Hai-bo Tang.
Supervision: Xiao-hui Wang.
Validation: Fan-bo Wang, Rong Rong, Guang Yang, Xiao-hui Wang, Hai-bo Tang.
Visualization: Fan-bo Wang, Jing-jun Xu, Tian-you Xin, Xiao-hui Wang.
Writing – original draft: Fan-bo Wang, Rong Rong, Guang Yang, Tian-you Xin, Xiao-hui Wang.
Writing – review & editing: Fan-bo Wang, Rong Rong, Jing-jun Xu, Xiao-hui Wang, Hai-bo Tang.
Footnotes
Abbreviations: CCSs = case-controlled studies, CIs = confidence intervals, PFU = pelvic floor ultrasound, POP = pelvic organ prolapse, PPPFD = postpartum pelvic floor dysfunction, SUI = stress urinary incontinence.
How to cite this article: Wang Fb, Rong R, Xu Jj, Yang G, Xin Ty, Wang Xh, Tang Hb. Impact of pelvic floor ultrasound in diagnosis of postpartum pelvic floor dysfunction: A protocol of systematic review. Medicine. 2020;99:32(e21582).
F-bW and R-rY have contributed equally to this study.
This study is partly supported by the 2019 Heilongjiang Provincial Colleges and Universities Basic Research Business Expenses Research Project (2019-KYYWF-1352). The funder did not take part in any parts of this study.
The authors have no conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Dietz HP. Female pelvic floor dysfunction--an imaging perspective. Nat Rev Gastroenterol Hepatol 2011;9:113–21. [DOI] [PubMed] [Google Scholar]
- [2].Mallett VT, Bump RC. The epidemiology of female pelvic floor dysfunction. Curr Opin Obstet Gynecol 1994;6:308–12. [PubMed] [Google Scholar]
- [3].Bump RC, Norton PA. Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am 1998;25:723–46. [DOI] [PubMed] [Google Scholar]
- [4].Sung VW, Hampton BS. Epidemiology of pelvic floor dysfunction. Obstet Gynecol Clin North Am 2009;36:421–43. [DOI] [PubMed] [Google Scholar]
- [5].Turner CE, Young JM, Solomon MJ, et al. Incidence and etiology of pelvic floor dysfunction and mode of delivery: an overview. Dis Colon Rectum 2009;52:1186–95. [DOI] [PubMed] [Google Scholar]
- [6].Gao L, Ding S, Ding Y, et al. Symptom distribution of female pelvic floor dysfunction patients with constipation as chief complaint. Zhonghua Wei Chang Wai Ke Za Zhi 2018;21:798–802. [PubMed] [Google Scholar]
- [7].Ramage L, Georgiou P, Qiu S, et al. Can we correlate pelvic floor dysfunction severity on MR defecography with patient-reported symptom severity? Updates Surg 2018;70:467–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Haylen BT, Maher CF, Barber MD, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Neurourol Urodyn 2016;35:137–68. [DOI] [PubMed] [Google Scholar]
- [9].DeLancey JO. The anatomy of the pelvic floor. Curr Opin Obstet Gynecol 1994;6:313–6. [PubMed] [Google Scholar]
- [10].Zhu Q, Shu H, Dai Z. Effect of pelvic floor dysfunction on sexual function and quality of life in Chinese women of different ages: an observational study. Geriatr Gerontol Int 2019;19:299–304. [DOI] [PubMed] [Google Scholar]
- [11].Ascanelli S, Morganti L, Martinello R, et al. Combined rectal and gynecologic surgery in complex pelvic floor dysfunction: clinical outcomes and quality of life of patients treated by a multidisciplinary group. Minerva Chir 2018;73:345–7. [DOI] [PubMed] [Google Scholar]
- [12].Frota IPR, Rocha ABO, Neto JAV, et al. Pelvic floor muscle function and quality of life in postmenopausal women with and without pelvic floor dysfunction. Acta Obstet Gynecol Scand 2018;97:552–9. [DOI] [PubMed] [Google Scholar]
- [13].MacLennan AH, Taylor AW, Wilson DH, et al. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. Br J Obstet Gynaecol 2000;107:1460–70. [DOI] [PubMed] [Google Scholar]
- [14].Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA 2008;300:1311–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lawrence JM, Lukacz ES, Nager CW, et al. Prevalence and co-occurrence of pelvic floor disorders in community-dwelling women. Obstet Gynecol 2008;111:678–85. [DOI] [PubMed] [Google Scholar]
- [16].Su Y, Li D, Han Y, et al. The screening of pelvic floor disordersamong women attending health examination in Zhongshan city. Guangdong Med J 2014;35:1405–7. [Google Scholar]
- [17].Chen GD. Pelvic floor dysfunction in aging women. Taiwan J Obstet Gynecol 2007;46:374–8. [DOI] [PubMed] [Google Scholar]
- [18].Harvey MA. Pelvic floor exercises during and after pregnancy: a systematic review of their role in preventing pelvic floor dysfunction. J Obstet Gynaecol Can 2003;25:487–98. [DOI] [PubMed] [Google Scholar]
- [19].Rørtveit G, Hannestad YS. Association between mode of delivery and pelvic floor dysfunction. Tidsskr Nor Laegeforen 2014;134:1848–52. [DOI] [PubMed] [Google Scholar]
- [20].Zuchelo LTS, Bezerra IMP, Da Silva ATM, et al. Questionnaires to evaluate pelvic floor dysfunction in the postpartum period: a systematic review. Int J Womens Health 2018;10:409–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Chen Z, Huang H, Chen QY. Effect of modified Buzhong Yiqi decoction combined with pelvic floor muscle exercise-biofeedback-electrical stimulation on early stage postpartum pelvic floor dysfunction. Zhongguo Zhong Yao Za Zhi 2018;43:2391–5. [DOI] [PubMed] [Google Scholar]
- [22].Sun Z, Zhu L, Lang J, et al. Postpartum pelvic floor rehabilitation on prevention of female pelvic floor dysfunction: a multicenter prospective randomized controlled study. Zhonghua Fu Chan Ke Za Zhi 2015;50:420–7. [PubMed] [Google Scholar]
- [23].Pregazzi R, Sartore A, Bortoli P, et al. Immediate postpartum perineal examination as a predictor of puerperal pelvic floor dysfunction. Obstet Gynecol 2002;99:581–4. [DOI] [PubMed] [Google Scholar]
- [24].Leombroni M, Buca D, Liberati M, et al. Post-partum pelvic floor dysfunction assessed on 3D rotational ultrasound: a prospective study on women with first- and second-degree perineal tears and episiotomy. J Matern Fetal Neonatal Med 2019;1–1. ahead of print. [DOI] [PubMed] [Google Scholar]
- [25].Laterza RM, Schrutka L, Umek W, et al. Pelvic floor dysfunction after levator trauma 1-year postpartum: a prospective case-control study. Int Urogynecol J 2015;26:41–7. [DOI] [PubMed] [Google Scholar]
- [26].van Delft K, Sultan AH, Thakar R, et al. The relationship between postpartum levator ani muscle avulsion and signs and symptoms of pelvic floor dysfunction. BJOG 2014;121:1164–71. [DOI] [PubMed] [Google Scholar]
- [27].Rogers RG, Leeman LM, Borders N, et al. Contribution of the second stage of labour to pelvic floor dysfunction: a prospective cohort comparison of nulliparous women. BJOG 2014;121:1145–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Shamseer L, Moher D, Clarke M, et al. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P): elaboration and explanation. BMJ 2015;349:g7647. [DOI] [PubMed] [Google Scholar]
- [29].Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529–36. [DOI] [PubMed] [Google Scholar]
- [30].Sutton AJ, Duval SJ, Tweedie RL, et al. Empirical assessment of effect of publication bias on meta-analyses. BMJ 2000;320:1574–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]


