SYRINGE SERVICE PROGRAMS
The term “syringe service program” (SSP), also referred to as “needle exchanges” or “needle and syringe programs,” is inclusive of any setting that provides needles, syringes, and other supplies intended for injection of drugs.2 SSPs were first established in Europe in the 1980s during the human immunodeficiency virus (HIV)/AIDS epidemic.3 Since then, as evidence has mounted supporting their value, SSPs have been implemented worldwide.4
Most SSPs offer free or low-cost harm reduction services such naloxone rescue kits, education, infectious disease screening and vaccination, wound care, and recovery resources.5–7 Identifying and screening for infectious diseases at SSPs or through SSP outreach work has resulted in successful linkage to care.8 Onsite clinical care for HIV and hepatitis C (HCV) is less common, but can exist.9 Since many people who inject drugs (PWID) avoid health care settings, but may be willing to engage with SSPs, integrated testing and outreach has strong potential to identify otherwise undiagnosed infectious diseases.7 Mobile SSP units, based out of vehicles that can travel to several locations, are also poised to further geographically expand screening.2
In the United States, the political and funding environment for SSPs has been largely unfavorable, although recent high-profile HIV outbreaks have spurred some policy changes.10,11 Services vary significantly in scope and scale and are often limited by regulations and funding.12–15 Policy needs to evolve to allow for expansion, innovation, and research on SSP delivery models such as mobile delivery models and peer sharing networks.6
Evidence of Syringe Service Programs Benefit in Infectious Disease Prevention
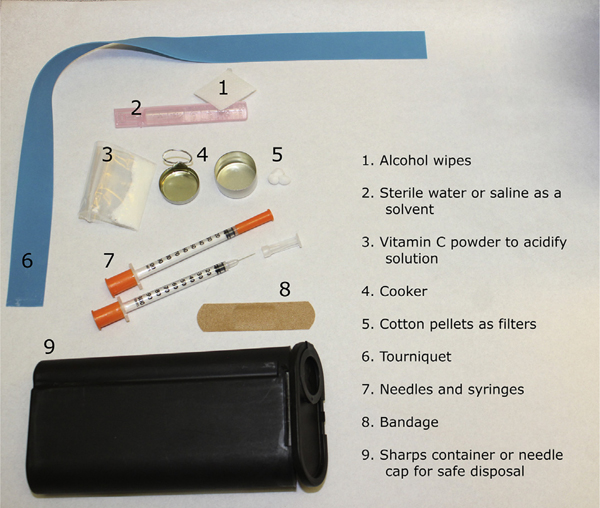
A critical component of SSPs is the promotion of safe injection practices through supply distribution and education. An understanding of these supplies, their proper use, and risk reduction is important for communicating effectively with PWID. Items that may be available at SSPs are shown in Fig. 1 and are summarized in Table 1.
Fig. 1.
Drug preparation equipment.
Table 1.
Summary of equipment for drug preparation process
| Street Examples95 | Recommended Supplies | Purpose96–104 |
|---|---|---|
| No skin cleanser, tap water, soap and water, hand sanitizer, cloth/tissue, alcoholic beverage | Alcohol wipes | Clean hands and skin at injection site before injection |
| Spoons, bottle caps | Cookers | Sterile metal cup in which to heat up/dissolve drug powder into solvent |
| Tap or bottle water, pond or puddle water, spit, toilet water | Sterile water or saline | Solvent for drug solution |
| Lemon juice, vinegar, kettle descaler | Vitamin C | Acidify solution to help dissolve crack cocaine and “black tar” heroin |
| Cigarettes, cotton balls, cotton tipped swabs, tampons, lint | Dental/cotton pellets | Catch particulates as the drug solution is drawn up into the syringe; can decrease bacterial loads |
| Reused needles | New needles | Injecting into vein |
| Socks, belts, gloves, condoms | Tourniquets | Prepare vein for injection |
| Reused syringes | Syringes | Injecting into vein |
| Reused needles/syringes, trash, street | Sharps containers | Safe storage, return syringes and needles to SSP for exchange if available |
| No wound care | Wound care supplies: band- aids, gauze, gloves, bandage wraps, tape, ointments | Protect open wounds |
| No preventive services | Fentanyl test strips, condoms, naloxone kits, PrEP | Reduce overdoses, reduce sexually transmitted infections |
Abbreviation: PrEP, pre-exposure prophylaxis for HIV prevention.
Although it can be challenging to study the effect of SSPs in the real-world setting, SSPs have clearly reduced high-risk injection behaviors such as equipment sharing, reuse, and high injection frequency.15 This risk reduction can extend beyond SSP users to their peer network.
In terms of injection drug use (IDU)-associated infections, there is strong evidence that SSPs decrease HIV and its associated costs.15,16 Implementation of SSPs in conjunction with other harm reduction measures in the midst of HIV outbreaks have proven effective measures to curb ongoing transmission.17 Although pre-exposure prophylaxis (PrEP) for HIV prevention uptake has been low among PWID, SSPs can be a channel for increasing PrEP awareness and use18
The quality of evidence is more limited than for HIV, but SSPs can also potentially play a role in decreasing other IDU-associated infections. HCV can remain on drug equipment surfaces for several days; not surprisingly, because they distribute clean equipment, SSPs can decrease HCV risk.19,20 Distance from SSP can increase HCV risk, whereas frequent SSP use decreases HCV risk.21,22 Although not well-studied, infrequent SSP use has been linked to HBV.16,23 Additionally, decreasing injection risk behaviors among SSP users suggests promise in reducing skin and soft tissue infections (SSTI), which are prevalent among PWID.7
Regulations Surrounding Syringe Service Programs in the United States
Despite the proven and potential benefits, SSPs remain somewhat controversial in the United States owing to the “war on drugs” ideology and the misconception that substance use disorders (SUD) represent a moral failing, as well as the fear that SSPs might lead to drug use initiation.10,24 At the time of inaugural SSP development in the 1980s, one notable barrier was the 1988 ban on the use of federal funding for SSP programs until they could be proven safe and effective.10,24
As evidence on the benefits of SSPs mounted, over the decades there were several attempts to lift the funding ban.24 After the HIV outbreak in Scott County, Indiana, brought national attention to the event and SSPs were included in the public health response, the federal ban was removed again in 2015 to allow for the use of federal funds to support SSP operations in areas or jurisdictions deemed at risk for outbreaks, excepting the actual purchase of needles and syringes.10 This change has facilitated SSP expansion.25 However, SSPs have been slow to spread to vulnerable areas, reflecting continuing stigma as well as hurdles posed by state and local drug paraphernalia laws.26 By 2015, many states had updated policies to allow for licensed SSPs, but today there are still several states that prohibit them.11 Other regulations also affect the number of syringes that can be distributed or exchanged, for example, requiring a used syringe to be collected for each clean syringe dispensed (ie, 1-for-1 syringe exchange).27 Overall, in the United States there continues to be a complicated regulatory landscape that hinders adequate access to sterile injection supplies.
In contrast, other countries including Canada, Australia, and many European Union nations are permissive and supportive of SSPs, with costs shared by national and local governments and even international organizations.4,28 Many countries have also explored the use of safe injection facilities, which is discussed further in the next section.
Summary
SSPs can decrease IDU-associated infections
SSPs vary in availability of preventative services, such as vaccinations and PrEP, however PWID have shown interest in these important services.
Despite evidence showing the benefits of SSPs, in the United States several regulatory barriers exist that prevent SSP expansion
SUPERVISED INJECTION FACILITIES
Individuals can bring preowned drugs to supervised injection facilities (SIFs), which are safe environments to inject drugs. SIFs are also sometimes referred to as medically supervised injection centers, safe injection facilities, supervised consumption facilities, drug consumption rooms, or overdose prevention sites. Facility staff members do not directly assist in injecting or handling any drugs preowned by the individual, but they are present to provide sterile injection equipment, answer questions on safe injection techniques, administer first aid when needed, and monitor for overdose.
SIFs were first started in the 1970s and have been operating in Europe, Australia, and Canada for decades,29 but no legally authorized facilities exist in the United States to date. Insite, the first SIF in North America, was opened in Vancouver, Canada in 2003, as a response to the devastating epidemics of HIV and drug overdose deaths and was legally sanctioned in 2011. Mobile and in-hospital SIFs also exist in some countries.30,31 In the United States, SIFs have faced opposition; however, SIFs in Canada and Australia have undergone numerous evaluations showing that they have multiple health and community benefits.32,33 SIF benefits and barriers are discussed further in this section.33–38
Benefits of Supervised Injection Facilities
Reduce morbidity and mortality
A cohort study that compared mortality before and after Insite was opened in Vancouver, British Columbia, showed a decrease in overdose death by 35%.34 Another study found that the number of deaths averted by Insite ranged from 1.9 to 11.7 deaths per year.35 SIFs have reported thousands of witnessed overdoses; however, no deaths have been reported thus far.37,39 Notably, a study from Sydney, Australia, also reported a 67% decrease in the number of ambulance calls for overdose reversal in a SIF neighborhood.36,39
Reduce infections
In addition to monitoring for overdoses, SIFs provide clients education on safe injection techniques, provide vaccinations, and conduct screening and treatment for sexually transmitted infections.40 PWID who use SIFs frequently practice safer injection, and there have been significant decreases in prolonged hospitalizations for IDUassociated infections.41,42 Modeling studies have shown that SIFs can decrease incident HIV and HCV infections43 and the costs incurred to provide lifelong HIV care and expensive HCV treatment.37,38,41,42,44–46
Reduce cost
Studies have shown that SIFs are cost effective. One cost-effectiveness analysis showed that a SIF was associated with an incremental net savings of almost $14 million and 920 life-years gained over a 10-year period.43 There are expected cost savings from averted HIV and HCV, decreased skin and soft tissue infections, averted overdose deaths, and increased uptake of medications for opioid use disorder (MOUD).43,45–48
Reduce drug use and increase treatment uptake
Studies in Vancouver have shown that SIF users reported less frequent reuse of syringes, and in 1 study, 57% of clients entered MOUD treatment programs.49,50 SIFs can also facilitate referrals to the hospital for earlier intervention.41,42
Decrease public injecting and increase public safety
Observational studies have reported beneficial effects of SIFs for PWID and neighborhoods. PWID who used SIFs are less likely to report needle sharing (71%), to dispose of syringes unsafely (56%), and to inject in public places. By decreasing fatal drug overdoses in the streets and reducing public drug use, public safety is maintained.37,50–52
Barriers to Safe Injection Facilities
The barriers to opening SIFs in the United States arise from the public and legal issues that are presented in Table 2. SIF opponents report concerns that SIFs are morally or legally wrong and will promote drug use and increase crime rates; however, these fears are unsubstantiated.33,53 In October 2019, a federal judge ruled that the bid of a nonprofit group, Safehouse, to open a SIF in Philadelphia did not violate federal law. Its opening, however, was halted in the setting of opposition.54
Table 2.
Supervised injection facilities in the United States
| Barriers | Arguments and Evidence to Support SIFs |
|---|---|
| Legal: Legality complicated owing to federal and state government involvement. The US forbids: Possession of controlled substances Making places available for unlawful distribution or use of a controlled substance.27 | CSA* meant to address drug purchasing and consumption (colloquially known as the “Crack House Statute”)27
CSA not meant to influence public health interventions/infringe on state public health authority27 |
| Public opinion: Although evidence support SIFs, establishing SIFs can be challenging in the setting of public opposition | PWID need public support98
SIFs are public health interventions that can reduce mortality, morbidity, and IDU-associated infections37,44,48,99 SIFs reduce public injecting, crime and increase public safety50–52 |
| Funding: SIFs may require significant startup and operating costs. Obtaining federal, state and local funding, in addition to outside donations, can be difficult owing to the legal controversies. | Cost saving100,101 Life saving, lead to early medical interventions, and should be publicly funded42 |
Abbreviation: CSA, Controlled Substance Act.
Summary
SIFs are safe indoor spaces where PWID can inject their preowned drugs in the presence of trained staff
SIFs decrease morbidity and mortality, while increasing treatment uptake and public safety
The status of SIFs in the United States remains uncertain, although in 2019 a federal judge ruled that opening a SIF in Philadelphia would not violate federal law
INTEGRATING HARM REDUCTION INTO CLINICAL PRACTICE
Particularly in the setting of increasing stimulant use, harm reduction is an essential component to preventing IDU-associated infections. In addition to reviewing evidence-based harm reduction strategies to integrate into clinical practice, this section reviews the concept of low barrier programs and opportunities for providers to advocate for harm reduction policies.
Overdose Prevention
Naloxone is a cost-effective, rapidly acting opioid antagonist to reverse drug overdoses, and it is particularly effective when distributed directly to PWID.55,56 In some states, standing orders for naloxone exist; that is, the ability for a person at risk of overdose and/or a potential bystander to purchase naloxone without a prescription.57 Although anyone with prescribing authority is able to prescribe naloxone to patients at risk for overdose, state laws vary in terms of prescriptions for third parties (ie, potential bystanders).58
Barriers to obtaining naloxone, such as stigma, inconvenience, cost, and lack of syringe service or community programs, have been reported.58,59 Given these barriers, providers should prescribe naloxone. Despite its effectiveness, the uptake of prescribing naloxone has been suboptimal, often owing to a lack of provider training, lack of time, and/or concerns for “enabling” drug use.60,61 Strategies to improve naloxone prescribing include partnering with community organizations who can deliver naloxone education to providers,62,63 obtaining political and institutional support to streamline naloxone education and prescribing,64,65 and the use of existing online resources (ie, naloxone training videos).58,66 These strategies can help providers to improve their prescribing self-efficacy and to integrate naloxone prescribing into practice. In addition, providers should counsel patients on how to recognize the signs and symptoms of an overdose.
Counseling strategies to prevent overdoses are summarized in Table 4. In addition, fentanyl test strip technology, initially developed as a tool for detecting fentanyl in the urine, has been used by many PWID to detect fentanyl in their street drugs.67 Although use of fentanyl test strips has been associated with overdose safety,68 there are still some fentanyl test strip limitations, including an inability to quantify fentanyl and difficulty interpreting results.67
Table 4.
Counseling points for overdose prevention
| Mixing drugs | Use 1 drug at a time Minimize use of each drug Avoid mixing drugs with alcohol |
| Quality of drug | Test a small amount of drug first (“test shot”) Purchase from same distributor Be cautious when switching between pills, know what you are using |
| Overdose plan | Do not use alone Keep door unlocked and/or slightly open Call a friend to check in Have naloxone ready |
| Mode of administration | Injecting and smoking increase overdose risk If using alone or concerns for decreased tolerance, snort if possible |
From National Harm Reduction Coalition. Overdose Prevention Tips. Available at: https://harmreduction.org/wp-content/uploads/2012/11/HRC_ODprevention_worksheet9.pdf. Accessed March 2 2020; with permission106.
Safe Injection Techniques
Safe injection techniques can reduce complications from IDU-associated infections. Provider strategies to begin these discussions include: (1) an awareness of safe injection techniques, (2) a nonjudgmental manner, (3) an awareness of local resources and regulations (SSPs, mobile units, and local policies like pharmacist dispensing), and (4) the willingness to explore the patient barriers to accessing harm reduction services.
There are multiple steps in the drug preparation process, and specific counseling points for each step are summarized in Table 3.69,70 Asking open-ended questions (eg, “Can you walk me through how you usually inject?”) can help to begin these conversations. By understanding specific injection practices, providers can then make individualized suggestions to minimize infection risk.71 Other factors, such as stigma and a lack of access to housing and/or SSPs or pharmacies may influence injection practices, so these issues should also be addressed.72
Table 3.
Summary of drug preparation steps and safe injection counseling points
| Drug Preparation Step | Counseling Points69,70,102–106 |
|---|---|
| Injection site preparation | Wash hands before and after injection Use alcohol pads, gauze pads, and bandages at injection site Clean other surfaces blood may have touched (ie, tourniquets) To minimize SSTIs, avoid “skip popping” (injecting subcutaneously) or “muscle popping” (injecting intramuscularly) if unable to find veins Avoid major arteries and small veins Rotate injection sites |
| N/S | Avoid reusing N/S Although often done to recover residual drug, avoid licking needles If no clean N/S available, wash with full-strength bleach for >2 min |
| Filters | Cigarette or other filters that require manual manipulation increase infection risk Consider small, preformed pellets Use new filters with each injection |
| Cookers | Cooking drugs can decrease bacterial burden. Avoid reusing or sharing cookers |
| Dissolving drug | Use sterile water when possible |
| Acidifiers (used if injecting solids such as base heroin or crack cocaine) | Use vitamin C packets to minimize risk of fungal infections and vein damage Avoid excessive use (ie, entire vitamin C packet) owing to risk of vein damage Consider adding small amount of sodium bicarbonate to buffer solution at the end of drug preparation process105 |
| Environment | Take your time; find a clean, safe space Avoid injecting alone To decrease overdose risk, inject yourself, rather than having someone else do it |
Abbreviations: N/S, sterile needles and syringes; SSTIs, skin and soft tissue infections.
In Canada, providers have been successful in providing clean drug equipment for their patients; however, in the United States, state laws vary in terms of (1) possession of drug equipment, such as the number of needles/syringes an individual can carry and (2) provider ability to prescribe needles, syringes, and other supplies. Providers should also seek guidance from institutional or practice legal counsel to understand their scopes or practice. Provision of supplies can not only help to ensure access to clean supplies, but also help to develop a therapeutic relationship with patients.73
Other Preventative Measures: Vaccinations and Pre-exposure Prophylaxis for Human Immunodeficiency Virus Infection
Vaccinations
Hepatitis A, B, Td, and Tdap vaccines are indicated for PWID. Viral hepatitis vaccines may be given without serologic confirmation. PCV13 and PPSV23 vaccines should also be offered to PWID who report tobacco or alcohol use. Other age-appropriate vaccines should be given per national guidelines.74,75
Pre-exposure prophylaxis
PWID are at risk for acquiring HIV infection; however, PrEP uptake for PWID has been relatively low.76 Oral tenofovir disoproxil fumarate/emtricitabine and oral tenofovir alafenamide fumarate/emtricitabine taken once daily are both approved by the US Food and Drug Administration for PrEP, although oral tenofovir alafenamide fumarate/emtricitabine has not been studied in people at risk for HIV through receptive vaginal sex and there are cost concerns.77 Although not yet approved by the US Food and Drug Administration, long-acting injectable formulations of PrEP may be future options.78
In addition to increasing provider knowledge and training around PrEP prescribing,79 strategies such as developing electronic medical record-based algorithms to alert providers of potential PrEP candidates, colocating PrEP and other services, and creating pharmacist-led PrEP programs through collaborative practice agreements are feasible and acceptable approaches to integrating PrEP prescribing into clinical practice.80–82
Low barrier programs
Low barrier programs incorporate a harm reduction approach of meeting patients with SUD “where they are at.” They can increase engagement in care, as well as improve patient–provider relationships and patient outcomes. These programs are flexible and meet the needs of individual patients, for example, maintaining SUD program participation even in the setting of continued drug use.83 Although they may offer counseling services, low barrier programs do not require counseling. This harm reduction, patient-centered approach could also minimize infectious complications of IDU.84 A lack of confidence has been cited as a provider barrier to providers offering SUD treatment85; however, there are several resources such as warmlines86 and telemedicine programs for provider-to-provider consultation to help providers integrate SUD treatment into their practices.87
Prescribing heroin or fentanyl
In the United States, heroin cannot be prescribed. However, in other countries, prescribing heroin (also known as “supervised injectable heroin” or “heroin-assisted treatment”) with optional oral methadone had benefits for people “refractory” to MOUD. Because the heroin is quality controlled (ie, of a known potency) and dosed at intervals based on patient response, this approach has been adopted to minimize overdose risk and engage PWID in care.88
In Canada, in PWID who are also refractory to MOUD, there is also some evidence on treating OUD with prescribed transdermal fentanyl, which creates stable, long-acting drug levels.89 Although diversion and safety are valid concerns, transdermal fentanyl could prove to be another harm reduction approach to mitigate the downstream infectious complications of injecting fentanyl.89
Advocacy and partnering with the community
Medicaid expansion has been associated with increased naloxone availability and improved health outcomes.90,91 In addition, Good Samaritan laws can protect people from prosecution if they help to reverse an overdose.92 Providers can play an important role in advocating for Medicaid expansion and Good Samaritan laws in states where these policies have not yet been adopted. In addition, partnering with the community is key to help promoting best practices around harm reduction.93,94 Finally, especially in areas where harm reduction services are scarce or prohibited, providers can partner with community organizations to advocate for SSPs, SIFs, and other policies like eliminating 1-for-1syringe exchange and decriminalization of drug paraphernalia and syringe possession.
Summary
Naloxone prescribing can be integrated into clinical practice
Discussing safe injection techniques, offering vaccinations, and PrEP for HIV prevention are some evidence based-strategies for preventing IDU-associated infections
Low barrier programs can improve engagement in care and patient outcomes
Advocacy is crucial for promoting harm reduction
DISCUSSION
Harm reduction is grounded in social justice and aimed at meeting people where they are at. By integrating a harm reduction approach into practice, providers can help to mitigate the infectious complications of drug use. In addition to interacting with patients in a nonjudgmental manner and with compassion, providers should work with patients to develop practical strategies to minimize infectious consequences associated with drug use. By openly discussing safe injection techniques and access to harm reduction services such as SSPs, naloxone, and other drug equipment, providers can empower PWID to use more safely. Moreover, advocating for policies that increase access to harm reduction services, such as SIFs and elimination of 1for-1 syringe exchanges, can help to ensure that PWID are able to access lifesaving prevention and treatment services.
KEY POINTS.
Harm reduction is a social justice movement and encompasses nonjudgmental strategies to mitigate negative consequences from ongoing drug use.
Syringe service programs and supervised infection facilities are evidence-based strategies to prevent injection drug use-associated infections and overdoses.
Clinicians can integrate harm reduction strategies into their practice and work with community partners to advocate for the health and safety of people who inject drugs.
WHAT IS HARM REDUCTION?
Harm reduction encompasses practical strategies, programs, and policies to help mitigate the negative consequences of drug use. Grounded in social justice, harm reduction is based on several principles and includes treating people who use drugs with respect and compassion. Harm reduction is a pragmatic approach where providers can offer people a range of options to reduce harm and individualize care plans to protect their health, while respecting the autonomy of people who use drugs.1
Acknowledgments
This work was supported by grant U54 GM115516 from the National Institutes of Health for the Northern New England Clinical and Translational Research network.
Footnotes
DISCLOSURE
The authors have no financial disclosures or conflicts of interest to report.
REFERENCES
- 1.Coalition HR. Principles of harm reduction. Available at: https://harmreduction.org/about-us/principles-of-harm-reduction/. Accessed March 10, 2020.
- 2.National Alliance of State and Territorial AIDS directors, Urban Coalition for HIV/AIDS Prevention Services. Syringe services program (SSP) development and implementation guidelines for state and local health departments. 2012. [Google Scholar]
- 3.Chu Z, Xu J, Reilly KH, et al. HIV related high risk behaviors and willingness to participate in HIV vaccine trials among China MSM by computer assisted self-interviewing survey. Biomed Res Int 2013;2013:493128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gay Man’s Health Crisis. Syringe exchange programs around the world: the global context. 2009. Available at: https://www.gmhc.org/files/editor/file/gmhc_intl_seps.pdf. Accessed June 2020.
- 5.Guardino V, Des Jarlais, Arasteh K, et al. Syringe exchange programs — United States, 2008. MMWR Morb Mortal Wkly Rep 2010;59(45):1488–91. [PubMed] [Google Scholar]
- 6.Des Jarlais DC, McKnight C, Goldblatt C, et al. Doing harm reduction better: syringe exchange in the United States. Addiction 2009;104(9):1441–6. [DOI] [PubMed] [Google Scholar]
- 7.Summers PJ, Hellman JL, MacLean MR, et al. Negative experiences of pain and withdrawal create barriers to abscess care for people who inject heroin. A mixed methods analysis. Drug Alcohol Depend 2018;190:200–8. [DOI] [PubMed] [Google Scholar]
- 8.Tookes H, Bartholomew TS, Geary S, et al. Rapid Identification and Investigation of an HIV Risk Network Among People Who Inject Drugs -Miami, FL, 2018. AIDS Behav 2020;24(1):246–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Behrends CN, Nugent AV, Des Jarlais DC, et al. Availability of HIV and HCV On-Site Testing and Treatment at Syringe Service Programs in the United States. J Acquir Immun Defic Syndr 2018;79(2):e76–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weinmeyer R Needle Exchange Programs’ Status in US Politics. AMA J Ethics 2016;18(3):252–7. [DOI] [PubMed] [Google Scholar]
- 11.Burris S Syringe Distribution Laws. Available at: http://lawatlas.org/datasets/syringe-policies-laws-regulating-non-retail-distribution-of-drug-parapherna. Accessed February 14, 2020.
- 12.Teshale EH, Asher A, Aslam MV, et al. Estimated cost of comprehensive syringe service program in the United States. PLoS One 2019;14(4):e0216205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Des Jarlais DC, Nugent A, Solberg A, et al. Syringe Service Programs for Persons Who Inject Drugs in Urban, Suburban, and Rural Areas - United States, 2013. MMWR Morb Mortal Wkly Rep 2015;64(48):1337–41. [DOI] [PubMed] [Google Scholar]
- 14.Phillips KT, Altman JK, Corsi KF, et al. Development of a risk reduction intervention to reduce bacterial and viral infections for injection drug users. Subst Use Misuse 2013;48(1–2):54–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MacArthur GJ, van Velzen E, Palmateer N, et al. Interventions to prevent HIV and Hepatitis C in people who inject drugs: a review of reviews to assess evidence of effectiveness. Int J Drug Policy 2014;25(1):34–52. [DOI] [PubMed] [Google Scholar]
- 16.Fernandes RM, Cary M, Duarte G, et al. Effectiveness of needle and syringe Programmes in people who inject drugs - An overview of systematic reviews. BMC Public Health 2017;17(1):309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruiz MS, O’Rourke A, Allen ST, et al. Using Interrupted Time Series Analysis to Measure the Impact of Legalized Syringe Exchange on HIV Diagnoses in Baltimore and Philadelphia. J Acquir Immun Defic Syndr 2019;82(Suppl 2):S148–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allen ST, O’Rourke A, White RH, et al. Barriers and facilitators to PrEP use among people who inject drugs in rural Appalachia: a qualitative study. AIDS Behav 2019;24(6):1942–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Doerrbecker J, Behrendt P, Mateu-Gelabert P, et al. Transmission of hepatitis C virus among people who inject drugs: viral stability and association with drug preparation equipment. J Infect Dis 2013;207(2):281–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Palmateer NE, Taylor A, Goldberg DJ, et al. Rapid decline in HCV incidence among people who inject drugs associated with national scale-up in coverage of a combination of harm reduction interventions. PLoS One 2014;9(8):e104515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Canary L, Hariri S, Campbell C, et al. Geographic Disparities in Access to Syringe Services Programs Among Young Persons With Hepatitis C Virus Infection in the United States. Clin Infect Dis 2017;65(3):514–7. [DOI] [PubMed] [Google Scholar]
- 22.Platt L, Minozzi S, Reed J, et al. Needle and syringe programmes and opioid substitution therapy for preventing HCV transmission among people who inject drugs: findings from a Cochrane Review and meta-analysis. Addiction 2018; 113(3):545–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hagan H, Jarlais DC, Friedman SR, et al. Reduced risk of hepatitis B and hepatitis C among injection drug users in the Tacoma syringe exchange program. Am J Public Health 1995;85(11):1531–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Des Jarlais DC. Harm reduction in the USA: the research perspective and an archive to David Purchase. Harm Reduct J 2017;14(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.SEP locations. 2020. Available at: https://www.nasen.org/map/. Accessed March 9, 2020.
- 26.Davis CS, Carr DH, Samuels EA. Paraphernalia Laws, Criminalizing Possession and Distribution of Items Used to Consume Illicit Drugs, and Injection-Related Harm. Am J Public Health 2019;109(11):1564–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beletsky L, Davis CS, Anderson E, et al. The law (and politics) of safe injection facilities in the United States. Am J Public Health 2008;98(2):231–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abuse CCoS. Needle exchange programs (NEPs) FAQs 2004. [Google Scholar]
- 29.Dolan K, Kimber J, Fry C, et al. Drug consumption facilities in Europe and the establishment of supervised injecting centres in Australia. Drug Alcohol Rev 2000;19(3):337–46. [Google Scholar]
- 30.Mema SC, Frosst G, Bridgeman J, et al. Mobile supervised consumption services in Rural British Columbia: lessons learned. Harm Reduct J 2019;16(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mertz E, Bartko K. Edmonton supervised consumption site opening at Royal Alexandra Hospital April 2. 2018. Available at: https://globalnews.ca/news/4107666/royal-alexandra-hospital-safe-injection-supervised-consumption-site/. Accessed March 10, 2020.
- 32.Hyshka E, Strathdee S, Wood E, et al. Needle exchange and the HIV epidemic in Vancouver: lessons learned from 15 years of research. Int J Drug Policy 2012; 23(4):261–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hedrich D, Kerr T, Dubois- A. Drug Consumption Facilities in Europe and Beyond Harm Reduction: Evidence, Impacts and Challenges: European Monitoring Centre for Drugs and Drug Addiction. 2010. Available at: https://www.emcdda.europa.eu/system/files/publications/555/EMCDDA-monograph10harm_reduction_final_205049.pdf. Accessed June 2020.
- 34.Marshall BD, Milloy MJ, Wood E, et al. Reduction in overdose mortality after the opening of North America’s first medically supervised safer injecting facility: a retrospective population-based study. Lancet 2011;377(9775):1429–37. [DOI] [PubMed] [Google Scholar]
- 35.Milloy MJ, Kerr T, Tyndall M, et al. Estimated drug overdose deaths averted by North America’s first medically-supervised safer injection facility. PLoS One 2008;3(10):e3351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Salmon AM, van Beek I, Amin J, et al. The impact of a supervised injecting facility on ambulance call-outs in Sydney, Australia. Addiction 2010;105(4): 676–83. [DOI] [PubMed] [Google Scholar]
- 37.Kilmer B, Taylor J, Caulkins JP, et al. Considering heroin-assisted treatment and supervised drug consumption sites in the United States. Santa Monica, CA:: RAND; 2018. [Google Scholar]
- 38.Kerr T, Tyndall MW, Lai C, et al. Drug-related overdoses within a medically supervised safer injection facility. Int J Drug Policy 2006;17(5):436–41. [Google Scholar]
- 39.Darke S, Ross J, Hall W. Overdose among heroin users in Sydney, Australia: I. Prevalence and correlates of non-fatal overdose. Addiction 1996;91(3):405–11. [PubMed] [Google Scholar]
- 40.Belackova V, Ritter A, Shanahan M, et al. Assessing the concordance between illicit drug laws on the books and drug law enforcement: comparison of three states on the continuum from “decriminalised” to “punitive”. Int J Drug Policy 2017;41:148–57. [DOI] [PubMed] [Google Scholar]
- 41.Lloyd-Smith E, Wood E, Zhang R, et al. Determinants of hospitalization for a cutaneous injection-related infection among injection drug users: a cohort study. BMC Public Health 2010;10:327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Palepu A, Tyndall MW, Leon H, et al. Hospital utilization and costs in a cohort of injection drug users. CMAJ 2001;165(4):415–20. [PMC free article] [PubMed] [Google Scholar]
- 43.Bayoumi AM, Zaric GS. The cost-effectiveness of Vancouver’s supervised injection facility. CMAJ 2008;179(11):1143–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pinkerton SD. How many HIV infections are prevented by Vancouver Canada’s supervised injection facility? Int J Drug Policy 2011;22(3):179–83. [DOI] [PubMed] [Google Scholar]
- 45.Andresen MA, Boyd N. A cost-benefit and cost-effectiveness analysis of Vancouver’s supervised injection facility. Int J Drug Policy 2010;21(1):70–6. [DOI] [PubMed] [Google Scholar]
- 46.Kerr T, Tyndall M, Li K, et al. Safer injection facility use and syringe sharing in injection drug users. Lancet 2005;366(9482):316–8. [DOI] [PubMed] [Google Scholar]
- 47.Kennedy MC, Karamouzian M, Kerr T. Public health and public order outcomes associated with supervised drug consumption facilities: a systematic review. Curr HIV/AIDS Rep 2017;14(5):161–83. [DOI] [PubMed] [Google Scholar]
- 48.Irwin A, Jozaghi E, Bluthenthal RN, et al. A cost-benefit analysis of a potential supervised injection facility in San Francisco, California, USA. J Drug Issues 2017;47(2):164–84. [Google Scholar]
- 49.Wood E, Tyndall MW, Qui Z, et al. Service uptake and characteristics of injection drug users utilizing North America’s first medically supervised safer injecting facility. Am J Public Health 2006;96(5):770–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stoltz J-A, Wood E, Small W, et al. Changes in injecting practices associated with the use of a medically supervised safer injection facility. J Public Health 2007;29(1):35–9. [DOI] [PubMed] [Google Scholar]
- 51.Broadhead RS, Kerr TH, Grund J-PC, et al. Safer injection facilities in North America: their place in public policy and health initiatives. J Drug Issues 2002;32(1):329–55. [Google Scholar]
- 52.Wood E, Tyndall MW, Lai C, et al. Impact of a medically supervised safer injecting facility on drug dealing and other drug-related crime. Substance Abuse Treat Prev Policy 2006;1:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kerr T, Stoltz JA, Tyndall M, et al. Impact of a medically supervised safer injection facility on community drug use patterns: a before and after study. BMJ 2006;332(7535):220–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Feldman N, Blumgart J. Safehouse hits pause on plan to open supervised injection site in South Phill. 2020. Available at: https://whyy.org/articles/safehousehits-pause-on-plan-to-open-supervised-injection-site-in-south-philly/. Accessed March 4, 2020.
- 55.Coffin PO, Sullivan SD. Cost-effectiveness of distributing naloxone to heroin users for lay overdose reversal in Russian cities. J Med Econ 2013;16(8): 1051–60. [DOI] [PubMed] [Google Scholar]
- 56.Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ 2013;346:f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Prescribing Naloxone And Pharmacy Access To Naloxone In MA. Available at: http://masstapp.edc.org/prescribing-naloxone-and-pharmacy-access-naloxonema. Accessed March 10, 2020.
- 58.Lim JK, Bratberg JP, Davis CS, et al. Prescribe to prevent: overdose prevention and naloxone rescue kits for prescribers and pharmacists. J Addict Med 2016; 10(5):300–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Drainoni ML, Koppelman EA, Feldman JA, et al. Why is it so hard to implement change? A qualitative examination of barriers and facilitators to distribution of naloxone for overdose prevention in a safety net environment. BMC Res Notes 2016;9(1):465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Coffin PO, Behar E, Rowe C, et al. Nonrandomized intervention study of naloxone coprescription for primary care patients receiving long-term opioid therapy for pain. Ann Intern Med 2016;165(4):245–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kispert D, Carwile JL, Silvia KB, et al. Differences in Naloxone Prescribing by Patient Age, Ethnicity, and Clinic Location Among Patients at High-Risk of Opioid Overdose. J Gen Intern Med 2020;35(5):1603–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mueller SR, Walley AY, Calcaterra SL, et al. A review of opioid overdose prevention and naloxone prescribing: implications for translating community programming into clinical practice. Subs Abus 2015;36(2):240–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Albert S, Brason FW 2nd, Sanford CK, et al. Project Lazarus: community-based overdose prevention in rural North Carolina. Pain Med 2011;12(Suppl 2): S77–85. [DOI] [PubMed] [Google Scholar]
- 64.Beletsky L, Ruthazer R, Macalino GE, et al. Physicians’ knowledge of and willingness to prescribe naloxone to reverse accidental opiate overdose: challenges and opportunities. J Urban Health 2007;84(1):126–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jawa R, Luu T, Bachman M, et al. Rapid naloxone administration workshop for health care providers at an academic medical center. MedEdPORTAL 2020;16: 10892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Substance Abuse and Mental Health Services Administration. SAMHSA Opioid Overdose Prevention Toolkit. HHS Publication No. (SMA) 18–4742. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2018. [Google Scholar]
- 67.Harm Reduction Coalition. Fentanyl test strip pilot: San Francisco (CA): 2018. Available at: https://harmreduction.org/issue-area/overdose-prevention-issuearea/fentanyl-test-strip-pilot/. Accessed March 2, 2020. [Google Scholar]
- 68.Peiper NC, Clarke SD, Vincent LB, et al. Fentanyl test strips as an opioid overdose prevention strategy: findings from a syringe services program in the South-eastern United States. Int J Drug Policy 2019;63:122–8. [DOI] [PubMed] [Google Scholar]
- 69.Thakarar K, Weinstein ZM, Walley AY. Optimising health and safety of people who inject drugs during transition from acute to outpatient care: narrative review with clinical checklist. Postgrad Med J 2016;92(1088):356–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Seval N, Eaton E, Springer SA. Beyond antibiotics: a practical guide for the infectious disease physician to treat opioid use disorder in the setting of associated infectious diseases. Open Forum Infect Dis 2020;7(1):ofz539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Phillips KT, Anderson BJ, Herman DS, et al. Risk factors associated with skin and soft tissue infections among hospitalized people who inject drugs. J Addict Med 2017;11(6):461–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rhodes T Risk environments and drug harms: a social science for harm reduction approach. Int J Drug Policy 2009;20(3):193–201. [DOI] [PubMed] [Google Scholar]
- 73.Keyes KM, Cerda M, Brady JE, et al. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health 2014;104(2):e52–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Belani H, Chorba T, Fletcher F, et al. Centers for Disease Control and Prevention. Integrated prevention services for HIV infection, viral hepatitis, sexually transmitted diseases, and tuberculosis for persons who use drugs illicitly: summary guidance from CDC and the U.S. Department of Health and Human Services. MMWR Recomm Rep 2012;61(RR-5):1–40. [PubMed] [Google Scholar]
- 75.Rockwell PG. ACIP Approves 2020 Adult and Childhood/Adolescent Immunization Schedules. Am Fam Physician 2020;101(4):251–2. [PubMed] [Google Scholar]
- 76.Taylor JL, Walley AY, Bazzi AR. Stuck in the window with you: HIV exposure prophylaxis in the highest risk people who inject drugs. Subs Abus 2019;40(4): 441–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Krakower DS, Daskalakis DC, Feinberg J, et al. Tenofovir alafenamide for HIV preexposure prophylaxis: what can we DISCOVER about its true value? Ann Intern Med 2020;172:281–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Marshall BDL, Goedel WC, King MRF, et al. Potential effectiveness of long-acting injectable pre-exposure prophylaxis for HIV prevention in men who have sex with men: a modelling study. Lancet HIV 2018;5(9):e498–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Christian ECW, Thakarar K. Examining PrEP knowledge and prescribing likelihood among medical residents before and after PrEP education. Open Forum Infect Dis 2018;5(suppl_1):S403. [Google Scholar]
- 80.Krakower DS, Gruber S, Hsu K, et al. Development and validation of an automated HIV prediction algorithm to identify candidates for pre-exposure prophylaxis: a modelling study. Lancet HIV 2019;6(10):e696–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Havens JP, Scarsi KK, Sayles H, et al. Acceptability and feasibility of a pharmacist-led HIV pre-exposure prophylaxis (PrEP) program in the Midwestern United States. Open Forum Infect Dis 2019;6(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Uyei J, Fiellin DA, Buchelli M, et al. Effects of naloxone distribution alone or in combination with addiction treatment with or without pre-exposure prophylaxis for HIV prevention in people who inject drugs: a cost-effectiveness modelling study. Lancet Public Health 2017;2(3):e133–40. [DOI] [PubMed] [Google Scholar]
- 83.Martin SA, Chiodo LM, Bosse JD, et al. The next stage of buprenorphine care for opioid use disorder. Ann Intern Med 2019;170(11):821–2. [DOI] [PubMed] [Google Scholar]
- 84.National Academies of Sciences E, and Medicine. Opportunities to improve opioid use disorder and infectious disease services: integrating responses to a dual epidemic. Washington, DC: The National Academies Press; 2020. [PubMed] [Google Scholar]
- 85.Andrilla CHA, Coulthard C, Patterson DG. Prescribing practices of rural physicians waivered to prescribe buprenorphine. Am J Prev Med 2018;54(6 Suppl 3):S208–14. [DOI] [PubMed] [Google Scholar]
- 86.Egan JE, Casadonte P, Gartenmann T, et al. The Physician Clinical Support System-Buprenorphine (PCSS-B): a novel project to expand/improve buprenorphine treatment. J Gen Intern Med 2010;25(9):936–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Talal AH, Andrews P, McLeod A, et al. Integrated, co-located, telemedicine-based treatment approaches for hepatitis C virus management in opioid use disorder patients on methadone. Clin Infect Dis 2019;69(2):323–31. [DOI] [PubMed] [Google Scholar]
- 88.Kilmer B, Taylor J, Caulkins JP, et al. Considering heroin-assisted treatment and supervised drug consumption sites in the United States. Santa Monica, CA: RAND Corporation; 2018. [Google Scholar]
- 89.Bardwell G, Wood E, Brar R. Fentanyl assisted treatment: a possible role in the opioid overdose epidemic? Substance Abuse Treat Prev Policy 2019;14(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sohn M, Talbert JC, Delcher C, et al. Association between state Medicaid expansion status and naloxone prescription dispensing. Health Serv Res 2020;55(2):239–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kravitz-Wirtz N, Davis CS, Ponicki WR, et al. Association of Medicaid Expansion With Opioid Overdose Mortality in the United States. JAMA Netw Open 2020; 3(1):e1919066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jakubowski A, Kunins HV, Huxley-Reicher Z, et al. Knowledge of the 911 Good Samaritan Law and 911-calling behavior of overdose witnesses. Subs Abus 2018;39(2):233–8. [DOI] [PubMed] [Google Scholar]
- 93.Associated Press. MMC research leads to toolkit for naloxone education. Portland Press Herald; 2019. Available at: https://www.pressherald.com/2019/10/31/researchers-naxolone-underprescribed-to-high-risk-patients/. Accessed June 2020 [Google Scholar]
- 94.Davis C, Chang S, Carr D, et al. Legal interventions to reduce overdose mortality: naloxone access and overdose good Samaritan laws 2014. Network for Public Health Law; Available at: https://www.networkforphl.org/wp-content/uploads/2020/01/legal-interventions-to-reduce-overdose.pdf. Accessed June 2020. [Google Scholar]
- 95.Bradford D, Jawa R, Wright J. Safer shooting: a harm reduction curriculum for patient centered advocacy in the treatment of people who inject drugs. Paper presented at: AMERSA; Boston, November 7, 2019. [Google Scholar]
- 96.Scott J, Winfield A, Kennedy E, et al. Laboratory study of the effects of citric and ascorbic acids on injections prepared with brown heroin. Int J Drug Policy 2000; 11(6):417–22. [DOI] [PubMed] [Google Scholar]
- 97.Ng H, Patel RP, Bruno R, et al. Filtration of crushed tablet suspensions has potential to reduce infection incidence in people who inject drugs. Drug Alcohol Rev 2015;34(1):67–73. [DOI] [PubMed] [Google Scholar]
- 98.Cruz MF, Patra J, Fischer B, et al. Public opinion towards supervised injection facilities and heroin-assisted treatment in Ontario, Canada. Int J Drug Policy 2007;18(1):54–61. [DOI] [PubMed] [Google Scholar]
- 99.Lloyd-Smith E, Wood E, Zhang R, et al. Risk factors for developing a cutaneous injection-related infection among injection drug users: a cohort study. BMC Public Health 2008;8:405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hood JE, Behrends CN, Irwin A, et al. The projected costs and benefits of a supervised injection facility in Seattle, WA, USA. Int J Drug Policy 2019;67:9–18. [DOI] [PubMed] [Google Scholar]
- 101.Irwin A, Jozaghi E, Weir BW, et al. Mitigating the heroin crisis in Baltimore, MD, USA: a cost-benefit analysis of a hypothetical supervised injection facility. Harm Reduct J 2017;14(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ciccarone D, Harris M. Fire in the vein: heroin acidity and its proximal effect on users’ health. Int J Drug Policy 2015;26(11):1103–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Coalition HR. A Safety Manual For Injection Drug Users. 2015. Available at: https://harmreduction.org/wp-content/uploads/2011/12/getting-off-right.pdf. Accessed Mar 4, 2020.
- 104.Harris M, Scott J, Wright T, et al. Injecting-related health harms and overuse of acidifiers among people who inject heroin and crack cocaine in London: a mixed-methods study. Harm Reduct J 2019;16(1):60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Harris M The ‘do-it-yourself’ New Zealand injecting scene: implications for harm reduction. Int J Drug Policy 2013;24(4):281–3. [DOI] [PubMed] [Google Scholar]
- 106.Coalition HR. Overdose Prevention Tips. Available at: https://harmreduction.org/wp-content/uploads/2012/11/HRC_ODprevention_worksheet9.pdf. Accessed March 2 2020.