During the COVID-19 pandemic, various social distancing measures were implemented to reduce transmission of the virus. The effect of easing these measures on SARS-CoV-2 transmission is uncertain. This study, which involved an agent-based simulation model, considers the effect of implementing and easing social distancing measures at different levels of adherence on the total number of COVID-19 cases in 3 urban communities.
Visual Abstract. Predicting COVID-19 Trends Over Time.
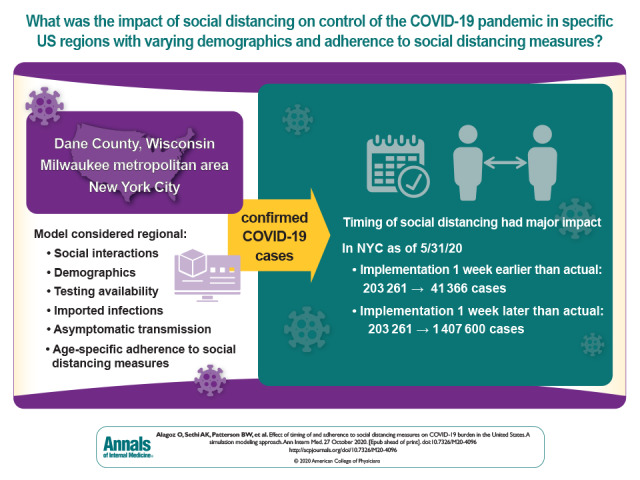
During the COVID-19 pandemic, various social distancing measures were implemented to reduce transmission of the virus. The effect of easing these measures on SARS-CoV-2 transmission is uncertain. This study, which involved an agent-based simulation model, considers the effect of implementing and easing social distancing measures at different levels of adherence on the total number of COVID-19 cases in 3 urban communities.
Abstract
Background:
Across the United States, various social distancing measures were implemented to control the spread of coronavirus disease 2019 (COVID-19). However, the effectiveness of such measures for specific regions with varying population demographic characteristics and different levels of adherence to social distancing is uncertain.
Objective:
To determine the effect of social distancing measures in unique regions.
Design:
An agent-based simulation model.
Setting:
Agent-based model applied to Dane County, Wisconsin; the Milwaukee metropolitan (metro) area; and New York City (NYC).
Patients:
Synthetic population at different ages.
Intervention:
Different times for implementing and easing social distancing measures at different levels of adherence.
Measurements:
The model represented the social network and interactions among persons in a region, considering population demographic characteristics, limited testing availability, “imported” infections, asymptomatic disease transmission, and age-specific adherence to social distancing measures. The primary outcome was the total number of confirmed COVID-19 cases.
Results:
The timing of and adherence to social distancing had a major effect on COVID-19 occurrence. In NYC, implementing social distancing measures 1 week earlier would have reduced the total number of confirmed cases from 203 261 to 41 366 as of 31 May 2020, whereas a 1-week delay could have increased the number of confirmed cases to 1 407 600. A delay in implementation had a differential effect on the number of cases in the Milwaukee metro area versus Dane County, indicating that the effect of social distancing measures varies even within the same state.
Limitation:
The effect of weather conditions on transmission dynamics was not considered.
Conclusion:
The timing of implementing and easing social distancing measures has major effects on the number of COVID-19 cases.
Primary Funding Source:
National Institute of Allergy and Infectious Diseases.
The novel coronavirus disease 2019 (COVID-19) pandemic poses unprecedented challenges for communities and policymakers. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19, is spread mainly through infectious respiratory droplets and, in closed, crowded spaces, by aerosols, but evolving knowledge of transmission dynamics makes it challenging to tailor disease control measures to specific communities. In the absence of an effective vaccine, nonpharmaceutical interventions, such as social distancing and other measures that reduce the number of close contacts during which transmission may occur, are the primary means of reducing the spread of COVID-19. These include closing schools and businesses, requiring facial coverings, and canceling large-scale events. When these measures are implemented and followed, daily counts of new COVID-19 cases decrease (“flattening the curve”) (1).
The negative economic and societal consequences of social distancing warrant a “dialing back” of such policies when it is safe to do so. However, the effect of easing social distancing on the transmission of SARS-CoV-2 is unclear. A set of indicators have been proposed by the current administration to guide communities on when they may consider easing rigorous, mandated social distancing (2). However, these lagging indicators, such as hospitals having the capacity to “treat patients without crisis care,” are not ideal because once the number of new infections increases to a level at which the health care system becomes burdened by the resulting hospitalizations, reimplementation of mandated social distancing is less effective at mitigation than earlier implementation (2). The ability to predict the effect of easing of social distancing is important to provide leading indicators for the right time to do this for a particular community.
Mathematical modeling of SARS-CoV-2 transmission dynamics using the best information available allows scientists to forecast the effect of social distancing on the COVID-19 pandemic. In particular, agent-based models—a class of computational models that can simulate the actions and interactions of autonomous agents, such as humans—provide a flexible and simulation-based method to better represent transmission dynamics in a complex system. Although other models are available, including those providing predictions for every U.S. state, these models have several limitations that limit their generalizability (3–7). For example, they assume a closed population and ignore “imported” infections, they do not accurately consider imperfect adherence levels to the dynamic social distancing measures, and most do not incorporate the effect of limited testing capacity into the number of confirmed cases (3–6).
We present an agent-based model that represents the social network and interactions among persons in a region, considering local population demographic characteristics, population density, the daily number of contacts in the absence of social distancing measures, and adherence to social distancing measures. Our model, the COVID-19 Agent-based simulation Model (COVAM), allows transmission from asymptomatic patients, accounts for imported cases during the early days of the pandemic, and considers the possibility that some patients with mild to moderate symptoms never receive confirmatory testing for COVID-19. This study shows how COVAM can inform decision making on how social distancing measures may be adjusted to control the spread of SARS-CoV-2 and prevent a return to exponential growth in COVID-19 cases in 3 unique urban communities.
Methods
Persons in COVAM have unique attributes, such as age, and interact with each other in ways that transmit SARS-CoV-2. We use a time step of 1 simulated day to update the status of these persons and to represent interactions. We assume all persons in the model are susceptible to COVID-19 at the beginning of the simulation—that is, no vaccine is available, and there is no preexisting immunity. Details of the modeling approach and parameter estimation are provided in section A of the Supplement and are briefly summarized here.
All persons in COVAM are categorized into 1 of 8 possible states representing their COVID-19 status (Figure 1). We consider transmission by exposed patients during the last several days of the incubation period and allow some to never be tested positive for COVID-19 even when they have mild symptoms, which reflects limited testing capacity and variation in sensitivity of the diagnostic tests in the earlier days of the pandemic in the United States (8–12).
Figure 1. Progression of COVID-19 in persons in COVAM.
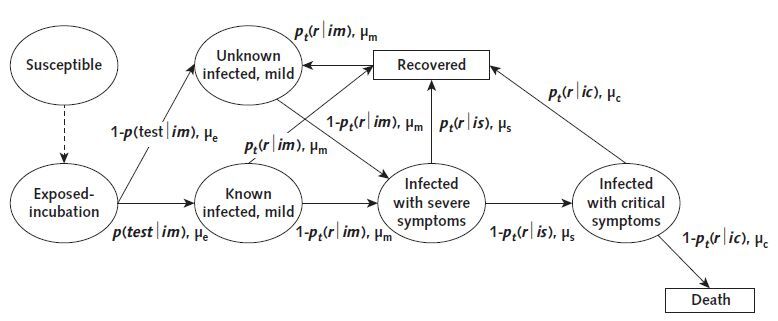
Ovals and rectangles represent the transient and absorbing states, respectively, that a person could be in; arrows show possible transitions among various states; and values on arrows represent the probability and mean duration of transitioning from one state to another. The notation used in the figure is described in Appendix Table. COVAM = COVID-19 Agent-based simulation Model; COVID-19 = coronavirus disease 2019.
The simulation starts with 1 (or more) exposed person. At the beginning of each day, the contagious person randomly interacts with other persons in the community. For each interaction, there is a possibility that the contagious person exposes the susceptible persons to SARS-CoV-2.
Input Parameters
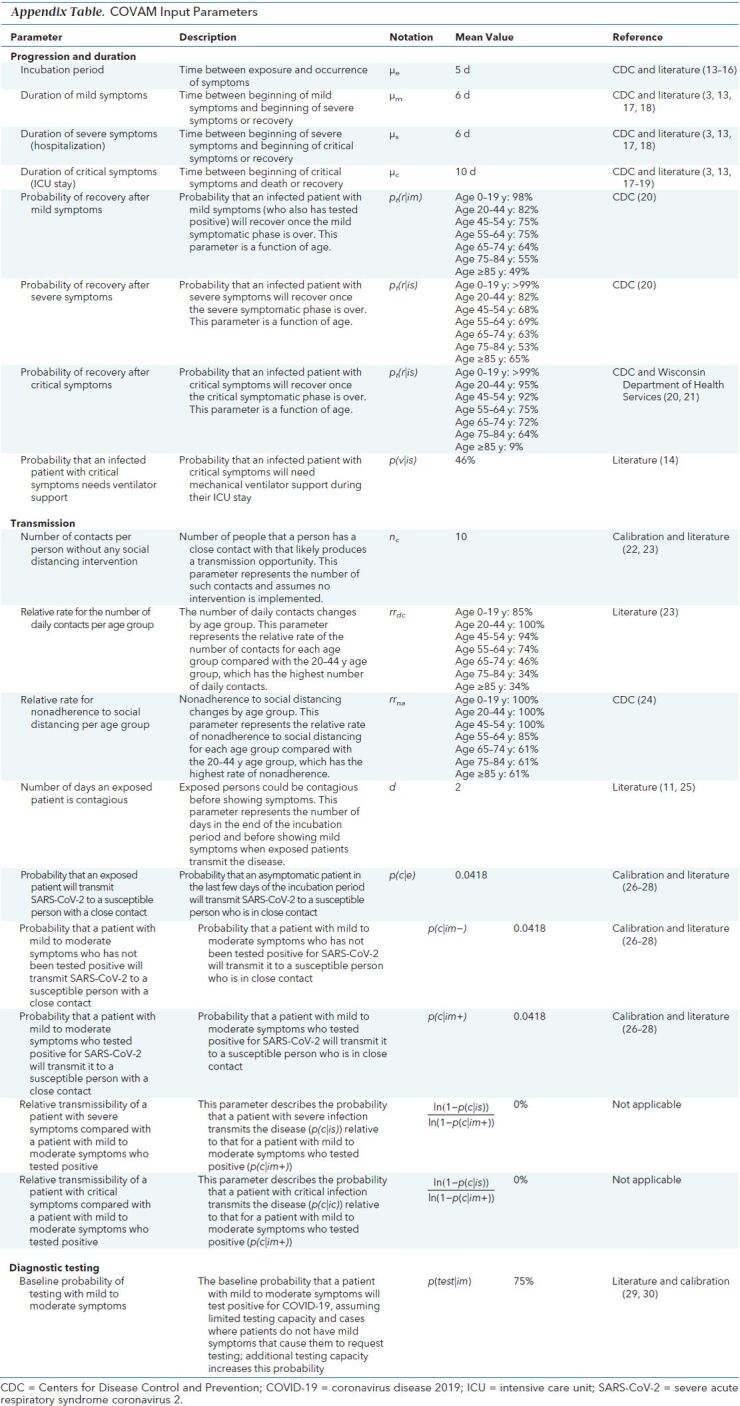
To maximize model generalizability, we derived input parameter estimates from relevant results in peer-reviewed literature and used data from Dane County, Wisconsin, to calibrate several parameters (Appendix Table [13–30]). There are 2 sets of parameters governing the transmissibility of SARS-CoV-2 in COVAM. The first is the number of close contacts per day without any intervention, which represents the social network effect and is independent of the respiratory agent that is transmitted. This parameter depends on population density and age group and is estimated using the literature and calibration, as explained below. The second parameter is the probability that contagious, exposed patients transmit SARS-CoV-2 to a susceptible person when a close contact occurs. The theoretical basic reproductive number (R0) corresponding to these parameter estimates was 3.34 for Dane County without any social distancing measures, which was within the range of R0 values reported in the literature (1.5 to 6.5) (26, 27).
Appendix Table. COVAM Input Parameters.
Adherence to Social Distancing Measures
The effectiveness of social distancing measures depends on how closely a population follows them and the type of measures that are implemented at different times. For example, in New York, mass gathering restrictions started on 12 March 2020, initial business closures were recommended on 16 March, educational facilities were closed on 18 March, and nonessential services closed and a statewide stay-at-home order was issued on 22 March (5). In COVAM, adherence to social distancing is represented by adjusting the number of contacts per person using cellphone mobility data published by several sources (31–34). For instance, the estimated average number of daily close contacts per person in New York City (NYC) is 20; therefore, a 70% adherence level reduces the number of such contacts to 6 per person per day, leading to slower transmission. The number of close contacts and adherence to social distancing change by age group because social distancing literature and COVID-19–specific studies show that younger persons are more likely to have more contacts and lower adherence to social distancing measures than older persons (23, 24, 35–37). It is important to note that adherence to social distancing measures in COVAM is a proxy for several behaviors that reduce the transmissibility of SARS-CoV-2, including infrequent travel, keeping at least 6 feet apart during person-to-person interactions, frequent handwashing, and wearing masks.
Calibration and Validation
We used a simple calibration procedure using earlier surveillance data from Dane County to fine-tune several input parameters that involve uncertainty (Appendix Table). We used the reported COVID-19 data from Dane County until 15 May 2020 to test whether our initial parameter estimates replicated the number of cases accurately. After this date, we modified the structure of the model to incorporate the age-specific number of close contacts and age-specific adherence inputs. We did not change any of the parameters after 31 July 2020 and compared the model's projections with the actual number of cases after this date.
Application to Dane County
The input parameters used for the computational experiments for Dane County are presented in Table 1. Briefly, we incorporated the population demographic characteristics in terms of age groups, the number of persons imported into Dane County, and adherence to social distancing measures. The model has the ability to add different numbers of imported cases daily; however, we kept the number of initial imported cases the same to prevent overfitting. We considered that adherence to social distancing measures in Dane County decreased on 14 May 2020 because the Wisconsin Supreme Court struck down the governor's stay-at-home order on this date (39).
Table 1. Input Parameters Used to Apply COVAM to Dane County, Milwaukee Metro Area, and New York City.
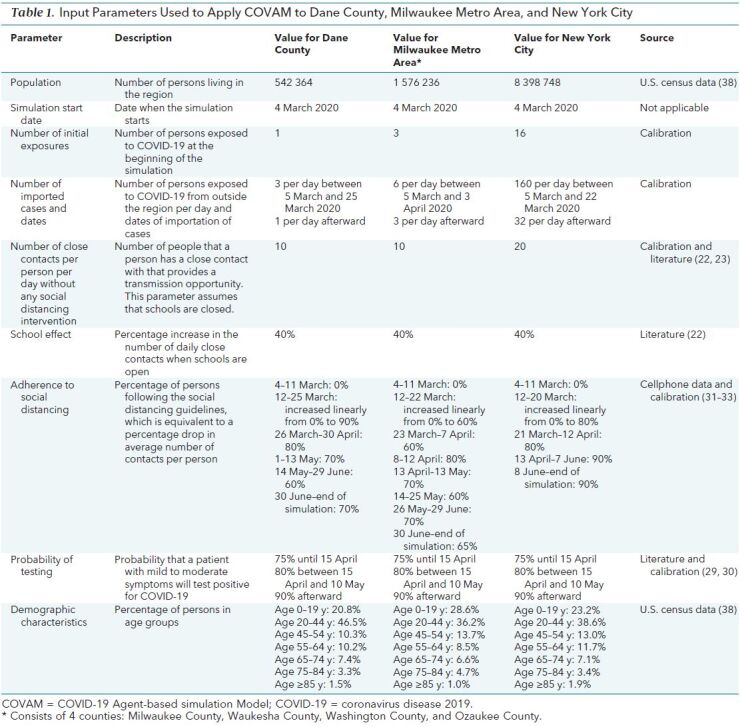
Application to Milwaukee Metropolitan Area
We adapted COVAM to Milwaukee to cross-validate our model and test its predictive accuracy. The population density of the Milwaukee metropolitan (metro) region is approximately 3 times that of Dane County (1341 vs. 438 per square mile) (38). Therefore, the Milwaukee metro area also provided a useful comparator region for COVAM to test whether the effect of timing and adherence to social distancing measures on COVID-19 differed between regions within the same state. Our objective was to modify as few parameters as possible to prevent overfitting. We used the same simulation settings as those in Dane County, except for 4 changes (Table 1): the epidemic was initiated with 3 exposed patients instead of 1; 6 imported cases were added to account for the larger population; demographic characteristics were adjusted using Milwaukee population data; and the adherence input was adjusted proportionately to cellphone mobility data, which indicated lower adherence in Milwaukee (31–33).
Application to NYC
New York City was among the first epicenters of the COVID-19 pandemic in the United States. Thus, the relative maturity of the epidemic in NYC made it a good test case to evaluate COVAM's predictive accuracy for later stages of the pandemic. As before, to maximize generalizability and avoid overfitting, we used the same simulation settings as those in Dane County, except for 4 changes (Table 1): 160 imported cases were added between 5 March and 22 March 2020 and 32 imported cases were added after 22 March to account for the greater number of visitors and daily commuters to NYC; demographic characteristics were adjusted using NYC population data; adherence to social distancing measures was adjusted because cellphone data showed higher adherence in NYC than in Dane County (31–33, 40); and the number of contacts per person per day was set to 20 because of substantially higher population density (27 755 vs. 438 per square mile) and reports from the social network analysis literature that population density increases the number of close contacts (41, 42).
Policy Analyses
We used COVAM to evaluate the effect of 3 aspects of social distancing. First, to evaluate the effect of adherence, we compared a scenario in which social distancing was not implemented with scenarios in which it was implemented at the beginning of the simulation and adherence was consistently at 25%, 50%, 75%, and 90%. Second, to evaluate the effect of timing of implementation, we tested scenarios in which social distancing was implemented 1 week earlier and 1 to 4 weeks later than the actual date. Finally, to evaluate the effect of the timing of easing of social distancing, we tested scenarios in which measures were eased on different dates (this was done only for NYC, where social distancing measures were eased on 8 June 2020). We assumed that after the measures were eased, adherence decreased by 5, 10, and 15 percentage points because of heightened community awareness. In NYC, a decrease of 5 percentage points reduced adherence from 90% to 85% after social distancing measures were eased.
We did both a parametric and a structural sensitivity analysis for NYC. Our parametric sensitivity analysis tested the effect of uncertainty in 3 input parameters: probability of testing, transmission rates, and number of imported cases. Our structural sensitivity analysis evaluated 3 different scenarios: hospital transmission was allowed; the number of daily close contacts differed for persons with and without known infection status; and the number of daily contacts varied widely to represent superspreader events. In all of these sensitivity analyses, we recalibrated model parameters and reevaluated all of the scenarios. We ran 100 replications for each experiment and report only mean values because the SEs were very low.
Role of the Funding Source
The National Institute of Allergy and Infectious Diseases funded this research but had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Results
In COVAM, the observed number of COVID-19 cases, and thus SARS-CoV-2 transmission dynamics, was accurately replicated in the short term over time in Dane County, Milwaukee, and NYC (Supplement Figure 1). Our first set of experiments showed that adherence to social distancing has a substantial effect on the cumulative number of cases (Supplement Figure and Supplement Table 1). For example, compared with 50% adherence, no social distancing other than closing schools increased the total number of cases from 56 433 to 487 501 in NYC in just 26 days (by 31 March).
Figure 2 presents the change in the number of cases when social distancing measures were implemented earlier or later than the actual date. We found that even a 1-week delay in implementation would have had a major effect on the total number of confirmed infections over time in each region. For example, implementing the measures 1 week earlier in NYC could have reduced the number of cases by 80%, from 203 261 to 41 366 by 31 May, whereas a 1-week delay could have increased the number of confirmed cases by almost 7-fold, to 1 407 600 (Figure 2; Supplement Table 2). The effect of implementing social distancing measures depends highly on the region because each has different levels of adherence and transmission (Supplement Table 2). For example, implementing the measures 1 week later in Dane County could have increased the number of cases by 36% as of 31 July (4239 to 5785), whereas the same scenario in NYC could have increased the number of cases by 539% (224 194 to 1 432 960). Compared with Dane County, in the Milwaukee metro area, a delay in implementation had a differential effect on the number of cases.
Figure 2. Comparison of total number of confirmed cases time for implementation of social distancing at different dates in Dane County (.
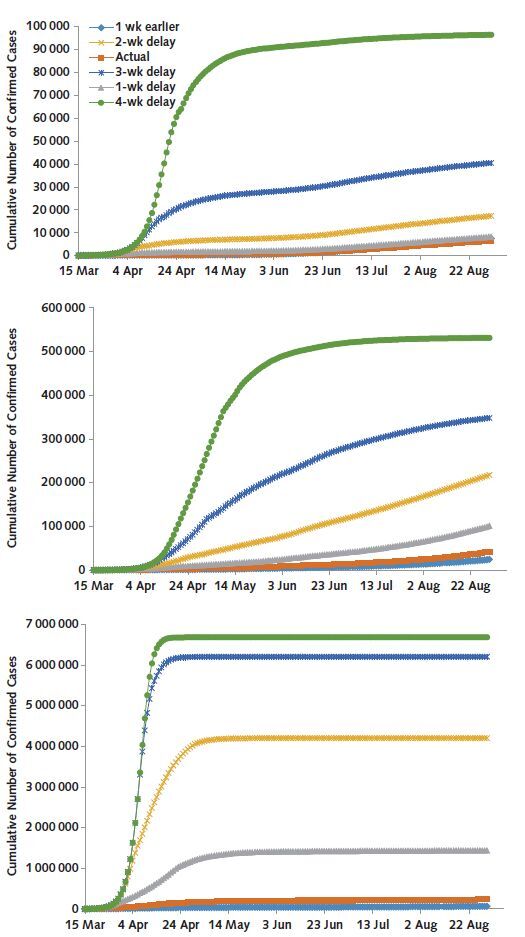
top ), Milwaukee metropolitan area ( middle ), and New York City ( bottom ).
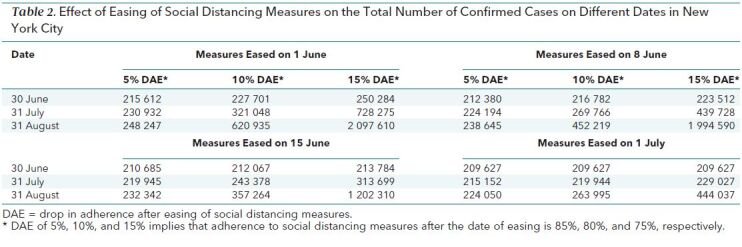
Earlier easing of the social distancing measures would have had major detrimental effects on the total number of COVID-19 cases in NYC, especially when there was a significant decrease in adherence after easing (Table 2). Easing of the measures on 1 June instead of the actual date (8 June) and a decrease in adherence of 5 percentage points would have increased the total number of confirmed cases from 224 194 to 230 932 as of 31 July. If adherence had decreased by 15 percentage points after social distancing measures were eased on 8 June, the number of cases could have increased from 224 194 to 439 728 by 31 July (Table 2), showing the importance of personal behaviors that prevent transmission of SARS-CoV-2, such as face mask use after the measures are eased. The decrease in adherence after easing has a more pronounced effect on the number of cases than the date of easing (Table 2).
Table 2. Effect of Easing of Social Distancing Measures on the Total Number of Confirmed Cases on Different Dates in New York City.
The sensitivity analyses showed that the overall trends in base-case runs would still hold (Supplement Figures 3 to 18 and Supplement Tables 3 to 24).
Discussion
In this study, we used agent-based simulation modeling to estimate the effect of the timing of implementation and easing of social distancing measures and adherence to them in 3 urban communities. We found that the timing of implementation of social distancing and adherence had a large effect on the number of cases that varied widely by region. The effect in NYC was large compared with Dane County and the Milwaukee metro area. This finding shows the importance of considering implementation of reopening policies at the regional level, as the results in Dane County and the Milwaukee metro area differed considerably despite being in the same state. We also found that maintaining a high level of adherence after easing of social distancing measures has a major effect on the number of cases, implying that cities and regions should strongly encourage the community to maintain behaviors that reduce the transmissibility of SARS-CoV-2, such as wearing masks. COVAM's accuracy in predicting the current outbreak and ability to estimate the effect of easing social distancing measures at the regional level shows its unique value for informing current and future policies. Our findings show that one-size-fits-all strategies are suboptimal and that context- and region-specific policies are needed when considering implementing and easing social distancing measures.
Our findings are consistent with those of other studies that focused on the effect of social distancing measures on COVID-19 burden. One study found that a reduction of 75% in nonhousehold contacts would be needed to handle the peak hospitalization demand in the Austin, Texas, metro area (43). In contrast, our model estimated that 70%, 70%, and 85% adherence to social distancing measures in Dane County, Milwaukee, and NYC, respectively, would be needed to keep the pandemic in a steady state. Another study reported that 57% of infections in the United States as of 3 May 2020 could have been avoided if social distancing measures had been implemented just 1 week earlier (44). We found that implementing social distancing measures 1 week earlier would have reduced the number of infections by 46%, 52%, and 80% in Dane County, Milwaukee, and NYC, respectively, as of 15 May 2020.
Some opponents of social distancing policies cite achievement of herd immunity as a reason for easing current measures (45). However, herd immunity is possible only if infection with SARS-CoV-2 results in lasting immunity, which is unknown at this time. Moreover, the correlates of protective immunity to SARS-CoV-2 have yet to be identified (45). In the absence of these data, social distancing is the most effective tool to prevent further spread of SARS-CoV-2. To date, social distancing measures and adherence to them have halted exponential growth in daily case counts of COVID-19. However, SARS-CoV-2 continues to spread, and many U.S. cities and urban communities have yet to return to pre–exponential growth levels of transmission. COVAM showed that premature easing of social distancing measures and low adherence to them could result in a rapid return to exponential growth of COVID-19 cases in communities.
Closing schools and businesses has major adverse economic and health consequences. Despite acknowledging the growing evidence that children and adolescents play a role in disease transmission, the American Academy of Pediatrics notes the importance of in-school learning and the negative effects that school closures had on children in the spring of 2020 (46). These include social isolation, worsening of mental and physical health, and learning deficits without adequate resources. Business closures caused substantial job losses in many sectors and led to major issues in the supply chain of essential items, including medical supplies (47). Precautions to control the COVID-19 pandemic have led to worse health outcomes for other diseases as well. For example, a recent commentary by the director of the National Cancer Institute noted that reduced screening and delays in diagnosis due to the COVID-19 pandemic are expected to lead to almost 10 000 excess deaths from breast and colorectal cancer in the United States over the next decade (48). It is critical that local decision makers determine region-specific policies that weigh the competing risks for COVID-19 transmission and negative economic, health, and social effects of business and school closures.
Our study has limitations, most of which are due to limited data and uncertainty about SARS-CoV-2. We made simplifying assumptions, such as that asymptomatic patients transmit the disease at the same rate as symptomatic patients and weather does not affect SARS-CoV-2 transmissibility, whereas several studies suggest otherwise (49, 50). Furthermore, COVAM uses adherence to social distancing as a proxy for several factors contributing to disease transmission, including fewer close contacts because of limited travel and precautions that prevent transmission during a close contact, such as wearing masks. Therefore, COVAM may not accurately estimate the effect of personal precautions on transmission.
There are also limitations related to the modeling approach. Our calibration procedure used a simple trial–error approach, as opposed to a full-scale calibration in which all plausible combinations of the input parameter values are tested (51). Owing to the computational intensity of a more formal and detailed calibration procedure, our calibration may not have identified the best parameter combinations. As with any other modeling technique, agent-based modeling has limitations, including greater computational needs compared with more commonly used compartmental models because of modeling of probabilistic events, as well as more complex development given that agent-based models typically require stylistic programming to represent events more realistically.
In conclusion, our model shows that delayed implementation of, lower adherence to, and premature easing of social distancing generally resulted in increased cases of COVID-19 in urban areas of the United States. However, the magnitude of effect varied substantially by region. These findings highlight the importance of region-specific considerations, and ideally modeling, as inputs to making policy decisions for a given region.
Supplementary Material
Footnotes
This article was published at Annals.org on 27 October 2020
References
- 1. Davies NG, Kucharski AJ, Eggo RM, et al; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 working group. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health. 2020;5:e375-e385. [PMID: 32502389] doi:10.1016/S2468-2667(20)30133-X [DOI] [PMC free article] [PubMed]
- 2. The White House. Guidelines for opening up America again. Accessed at www.whitehouse.gov/openingamerica on 29 April 2020.
- 3.Modeling COVID-19 spread vs healthcare capacity. Accessed at https://alhill.shinyapps.io/COVID19seir on 2 April 2020.
- 4. Predictive Healthcare at Penn Medicine. COVID-19 hospital impact model for epidemics (CHIME). Accessed at https://penn-chime.phl.io on 2 April 2020.
- 5. Institute for Health Metrics and Evaluation. COVID-19 projections. Accessed at https://covid19.healthdata.org/united-states-of-america on 26 April 2020.
- 6. Jewell NP, Lewnard JA, Jewell BL. Predictive mathematical models of the COVID-19 pandemic: underlying principles and value of projections. JAMA. 2020;323:1893-1894. [PMID: 32297897] doi:10.1001/jama.2020.6585 [DOI] [PubMed]
- 7. Jewell NP, Lewnard JA, Jewell BL. Caution warranted: using the Institute for Health Metrics and Evaluation model for predicting the course of the COVID-19 pandemic [Editorial]. Ann Intern Med. 2020;173:226-227. [PMID: 32289150] doi:10.7326/M20-1565 [DOI] [PMC free article] [PubMed]
- 8. Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany [Letter]. N Engl J Med. 2020;382:970-971. [PMID: 32003551] doi:10.1056/NEJMc2001468 [DOI] [PMC free article] [PubMed]
- 9. Nishiura H, Linton NM, Akhmetzhanov AR. Serial interval of novel coronavirus (COVID-19) infections. Int J Infect Dis. 2020;93:284-286. [PMID: 32145466] doi:10.1016/j.ijid.2020.02.060 [DOI] [PMC free article] [PubMed]
- 10. Du Z, Xu X, Wu Y, et al. Serial interval of COVID-19 among publicly reported confirmed cases. Emerg Infect Dis. 2020;26:1341-1343. [PMID: 32191173] doi:10.3201/eid2606.200357 [DOI] [PMC free article] [PubMed]
- 11. Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science. 2020;368:489-493. [PMID: 32179701] doi:10.1126/science.abb3221 [DOI] [PMC free article] [PubMed]
- 12. Rhoads DD, Cherian SS, Roman K, et al. Comparison of Abbott ID Now, DiaSorin Simplexa, and CDC FDA emergency use authorization methods for the detection of SARS-CoV-2 from nasopharyngeal and nasal swabs from individuals diagnosed with COVID-19 [Letter]. J Clin Microbiol. 2020;58. [PMID: 32303564] doi:10.1128/JCM.00760-20 [DOI] [PMC free article] [PubMed]
- 13. Centers for Disease Control and Prevention. Interim clinical guidance for management of patients with confirmed coronavirus disease (COVID-19). Accessed at www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html#Asymptomatic on 2 April 2020.
- 14. Guan WJ, Ni ZY, Hu Y, et al; China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [PMID: 32109013] doi:10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed]
- 15. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199-1207. [PMID: 31995857] doi:10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed]
- 16. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577-582. [PMID: 32150748] doi:10.7326/M20-0504 [DOI] [PMC free article] [PubMed]
- 17. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [PMID: 32031570] doi:10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed]
- 18. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [PMID: 31986264] doi:10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed]
- 19. Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle region—case series. N Engl J Med. 2020;382:2012-2022. [PMID: 32227758] doi:10.1056/NEJMoa2004500 [DOI] [PMC free article] [PubMed]
- 20. CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343-346. [PMID: 32214079] doi:10.15585/mmwr.mm6912e2 [DOI] [PMC free article] [PubMed]
- 21. Wisconsin Department of Health Services. COVID-19: Wisconsin summary data. Accessed at www.dhs.wisconsin.gov/covid-19/data.htm on 12 August 2020.
- 22. Lee BY, Brown ST, Cooley P, et al. Simulating school closure strategies to mitigate an influenza epidemic. J Public Health Manag Pract. 2010;16:252-61. [PMID: 20035236] doi:10.1097/PHH.0b013e3181ce594e [DOI] [PMC free article] [PubMed]
- 23. Del Valle SY, Hyman JM, Hethcote HW, et al. Mixing patterns between age groups in social networks. Social Networks. 2007;29:539-554. doi:10.1016/j.socnet.2007.04.005
- 24. Czeisler MÉ, Tynan MA, Howard ME, et al. Public attitudes, behaviors, and beliefs related to COVID-19, stay-at-home orders, nonessential business closures, and public health guidance—United States, New York City, and Los Angeles, May 5-12, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:751-758. [PMID: 32555138] doi:10.15585/mmwr.mm6924e1 [DOI] [PMC free article] [PubMed]
- 25. He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672-675. [PMID: 32296168] doi:10.1038/s41591-020-0869-5 [DOI] [PubMed]
- 26. Liu Y, Gayle AA, Wilder-Smith A, et al. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med. 2020;27. [PMID: 32052846] doi:10.1093/jtm/taaa021 [DOI] [PMC free article] [PubMed]
- 27. Imai N, Cori A, Dorigatti I, et al. Report 3: transmissibility of 2019-nCoV. Imperial College London (25-01-2020). Accessed at www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-transmissibility-25-01-2020.pdf on 30 April 2020.
- 28. Pedersen MG, Meneghini M. Quantifying undetected COVID-19 cases and effects of containment measures in Italy. ResearchGate. Accessed at www.researchgate.net/publication/339915690_Quantifying_undetected_COVID-19_cases_and_effects_of_containment_measures_in_Italy_Predicting_phase_2_dynamics on 30 April 2020.
- 29. Crisanti A, Cassone A. In one Italian town, we showed mass testing could eradicate the coronavirus. The Guardian. 20 March 2020. Accessed at www.theguardian.com/commentisfree/2020/mar/20/eradicated-coronavirus-mass-testing-covid-19-italy-vo on 30 April 2020.
- 30. Hu Z, Song C, Xu C, et al. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020;63:706-711. [PMID: 32146694] doi:10.1007/s11427-020-1661-4 [DOI] [PMC free article] [PubMed]
- 31. Unacast. Social distancing scoreboard. Accessed at www.unacast.com/covid19/social-distancing-scoreboard on 10 August 2020.
- 32. GeoDS Lab @ UW-Madison. Mapping mobility changes in response to COVID-19 Accessed at https://geods.geography.wisc.edu/covid19/physical-distancing on 10 August 2020.
- 33. Google. COVID-19 community mobility report. Accessed at www.google.com/covid19/mobility on 10 August 2020.
- 34. Gao S, Rao J, Kang Y, et al. Mobile phone location data reveal the effect and geographic variation of social distancing on the spread of the COVID-19 epidemic. JAMA Open Network. 2020. [Forthcoming].
- 35. Mossong J, Hens N, Jit M, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 2008;5:e74. [PMID: 18366252] doi:10.1371/journal.pmed.0050074 [DOI] [PMC free article] [PubMed]
- 36. Canning D, Karra M, Dayalu R, et al. The association between age, COVID-19 symptoms, and social distancing behavior in the United States. medRxiv. Preprint posted online 23 April 2020. doi:10.1101/2020.04.19.20065219
- 37. Pedersen MJ, Favero N. Social distancing during the COVID-19 pandemic: who are the present and future non-compliers? Public Adm Rev. 2020. [PMID: 32836442] doi:10.1111/puar.13240 [DOI] [PMC free article] [PubMed]
- 38. United States Census Bureau. Age and sex table. Accessed at https://data.census.gov/cedsci on 18 August 2020.
- 39.Wisconsin Legislature v. Andrea Palm. Wisconsin Supreme Court (Wis. 2020) 2020:No. 2020AP000765-OA.
- 40. Feng Z, Hill AN, Smith PJ, et al. An elaboration of theory about preventing outbreaks in homogeneous populations to include heterogeneity or preferential mixing. J Theor Biol. 2015;386:177-87. [PMID: 26375548] doi:10.1016/j.jtbi.2015.09.006 [DOI] [PMC free article] [PubMed]
- 41. Xu B, Tian H, Sabel CE, et al. Impacts of road traffic network and socioeconomic factors on the diffusion of 2009 pandemic influenza A (H1N1) in mainland China. Int J Environ Res Public Health. 2019;16. [PMID: 30959783] doi:10.3390/ijerph16071223 [DOI] [PMC free article] [PubMed]
- 42. Mei S, Chen B, Zhu Y, et al. Simulating city-level airborne infectious diseases. Comput Environ Urban Syst. 2015;51:97-105. doi:10.1016/j.compenvurbsys.2014.12.002
- 43. Wang X, Pasco RF, Du Z, et al. Impact of social distancing measures on COVID-19 healthcare demand in central Texas. medRxiv. Preprint posted online 22 April 2020. doi:10.1101/2020.04.16.20068403 [DOI] [PMC free article] [PubMed]
- 44. Pei S, Kandula S, Shaman J. Differential effects of intervention timing on COVID-19 spread in the United States. medRxiv. Preprint posted online 29 May 2020. doi:10.1101/2020.05.15.20103655 [DOI] [PMC free article] [PubMed]
- 45. Altmann DM, Douek DC, Boyton RJ. What policy makers need to know about COVID-19 protective immunity. Lancet. 2020;395:1527-1529. [PMID: 32353328] doi:10.1016/S0140-6736(20)30985-5 [DOI] [PMC free article] [PubMed]
- 46. American Academy of Pediatrics. COVID-19 planning considerations: guidance for school re-entry. Accessed at https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-planning-considerations-return-to-in-person-education-in-schools on 7 July 2020.
- 47. Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185-193. [PMID: 32305533] doi:10.1016/j.ijsu.2020.04.018 [DOI] [PMC free article] [PubMed]
- 48. Sharpless NE. COVID-19 and cancer [Editorial]. Science. 2020;368:1290. [PMID: 32554570] doi:10.1126/science.abd3377 [DOI] [PubMed]
- 49. Araujo MB, Naimi B. Spread of SARS-CoV-2 coronavirus likely to be constrained by climate. medRxiv. Preprint posted online 7 April 2020. doi:10.1101/2020.03.12.20034728
- 50. Luo W, Majumder MS, Liu D, et al. The role of absolute humidity on transmission rates of the COVID-19 outbreak. medRxiv. Preprint posted online 17 February 2020. doi:10.1101/2020.02.12.20022467
- 51. Barker AK, Alagoz O, Safdar N. Interventions to reduce the incidence of hospital-onset Clostridium difficile infection: an agent-based modeling approach to evaluate clinical effectiveness in adult acute care hospitals. Clin Infect Dis. 2018;66:1192-1203. [PMID: 29112710] doi:10.1093/cid/cix962 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


