Abstract
Tuberculosis (TB) caused by Mycobacterium tuberculosis is one of the most lethal infectious diseases with estimates of approximately 1.4 million human deaths in 2018. M. tuberculosis has a well-established ability to circumvent the host immune system to ensure its intracellular survival and persistence in the host. Mechanisms include subversion of expression of key microRNAs (miRNAs) involved in the regulation of host innate and adaptive immune response against M. tuberculosis. Several studies have reported differential expression of miRNAs during active TB and latent tuberculosis infection (LTBI), suggesting their potential use as biomarkers of disease progression and response to anti-TB therapy. This review focused on the miRNAs involved in TB pathogenesis and on the mechanism through which miRNAs induced during TB modulate cell antimicrobial responses. An attentive study of the recent literature identifies a group of miRNAs, which are differentially expressed in active TB vs. LTBI or vs. treated TB and can be proposed as candidate biomarkers.
Keywords: microRNA, tuberculosis, diagnosis, biomarker, pathogenesis, latent infection, disease progression, response to therapy, innate immunity, apoptosis, autophagy
1. Introduction
Tuberculosis (TB), caused by Mycobacterium tuberculosis, is one of the most lethal infectious diseases worldwide [1]. The latest estimates indicate that approximately one fourth of all people worldwide have been infected by M. tuberculosis and that TB causes 1.4 million deaths every year [2].
A key pathogenic feature of M. tuberculosis is its ability to survive for a long time in the human host, inside macrophages in tubercle granulomas [3]. Macrophages are key components of the host innate immune response against M. tuberculosis that can eliminate mycobacteria through different mechanism, such as induction of apoptosis, immune-inflammatory responses, and phagocytic activity [4]. However, the pathogen can counteract host antimicrobial mechanisms to ensure survival and persistence. In most M. tuberculosis infections, the host immune response is able to arrest bacterial growth and clear the microorganisms or induce a status of latent tuberculosis infection (LTBI). However, about 5–15% of LTBI progress to active TB with pulmonary and/or extra pulmonary involvement [5]. Active TB generally manifests soon after infection, but, in some cases, it may occur even years after primary infection, because of reduced immune response, thus indicating the importance of innate and adaptive immunity in M. tuberculosis control [6] (Figure 1).
Figure 1.
Tuberculosis pathogenesis and disease progression. Mycobacterium tuberculosis infection initiates with inhalation of droplets that carry bacteria and their uptake by alveolar macrophages. Innate immune responses characterize the initial phase of infection, with recruitment of inflammatory cells in the lung. Bacterial dissemination to the draining lymph node leads to T cell priming and expansion of antigen-specific T cells. Recruitment of activated macrophages, neutrophils, T cells, and B cells in the lung leads to granuloma formation, which contains M. tuberculosis in a latent status. However, in about 10% of infected individuals, M. tuberculosis escapes immune control and granulomas are disrupted, with release of infectious bacteria.
Bacteria, including M. tuberculosis, have evolved several strategies to evade host innate immunity and to survive inside host immune cells. M. tuberculosis can modulate several cellular processes such as phagosome–lysosome fusion in macrophages, apoptosis, autophagy, inflammation, innate immune response, MHC class II expression, and antigen presentation by MHC class I in dendritic cells (DCs) [7]. Mechanisms of immune evasion include dysregulation of the host microRNAs (miRNAs) that are involved in control of these biological processes [8,9].
MiRNAs are small non-coding RNAs, typically 18–24 nucleotides in length, which are involved in the regulation of gene expression at post-transcriptional level and influence many biological processes including the immune response. To perform their regulatory functions, miRNAs bind to complementary sequences in the 3′-untranslated region of mRNA targets leading to transcript degradation or translational inhibition [10]. The human genome encodes about two thousands potentially functional miRNAs and each miRNA may suppress multiple genes, while one mRNA can be targeted by multiple miRNAs. Specific anomalies of miRNA expression have been associated with several diseases, including infectious diseases, and investigated as potential diagnostic markers or therapeutic tools [11,12]. Several studies highlighted changes in the levels of circulating miRNAs in patients with TB and identified miRNA signatures that could discriminate between patients with active TB and those with LTBI [13]. The development of new diagnostic and prognostic biomarkers would be particularly useful for screening M. tuberculosis infection and disease, for which current methods are still unsatisfactory. In fact, direct diagnosis of M. tuberculosis infection by molecular testing and bacterial culture has low sensitivity and long turnaround time, respectively, while indirect diagnosis by tuberculin skin test or interferon gamma (IFNγ) release assay (IGRA) is not able to differentiate LTBI from active TB or to identify patients at risk of disease progression [13,14].
Recent review articles highlighted the relevant role of host miRNAs in the immune response to M. tuberculosis infection, their potential as TB biomarkers [15,16] and as targets or tools for therapeutic interventions [17]. However, methodological variability and technical hurdles in miRNA profiling represent important limitations for comparisons of results among studies, as excellently discussed by Ruiz-Tangle and colleagues [18]. With the aim to pursue the effort at identifying potential diagnostic and prognostic miRNA biomarkers, we present here an updated and comprehensive review of basic and clinical studies that identified miRNAs involved in TB pathogenesis, escape from host antimicrobial response, and associated with TB progression or response to anti-TB therapy.
2. MicroRNAs in Tuberculosis Pathogenesis
Several studies reported altered expression profiles of circulating and cellular miRNAs in patients with active TB vs. those with LTBI or healthy controls [19]. Differentially expressed miRNAs were further investigated to identify their role within the innate immune response during M. tuberculosis infection. In vitro and in vivo experiments confirmed the involvement of miRNAs in modulating gene expression in the major target cells of M. tuberculosis, like macrophages, DCs, natural killer (NK) and T cells [20]. M. tuberculosis can induce or inhibit miRNA expression in order to escape the immune response. Triggering the apoptotic pathway, induction of autophagy, stimulation of IFNγ and tumor necrosis factor alpha (TNFα) secretion are some of the mechanisms adopted by the host cells during bacterial infection. For example, among miRNAs that are upregulated in TB patients, miR-146a-5p, miR-21-5p, miR-99b-5p and miR-132-5p negatively regulate host inflammatory pathways triggered by Toll-like receptor (TLR) signaling in myeloid cells, thus promoting M. tuberculosis survival [21]. Other miRNAs that are upregulated in M. tuberculosis-infected macrophages, like miR-27a-5p, miR-33, miR-125-5p and miR-144-5p, inhibit autophagosome formation and M. tuberculosis killing by macrophages [22,23]. MiR-29a-3p and miR-125-5p, both upregulated in infected macrophages, directly target IFNγ and TNFα, hence suppressing the immune response to intracellular M. tuberculosis [24,25]. Cell apoptosis and inflammasome induction are other mechanisms of defense against intracellular pathogens, which are regulated by M. tuberculosis-modulated host miRNAs, like miR-325-3p and miR-20b-5p [26,27]. On the other hand, some miRNAs, like miR-155-5p and let-7f, which are modulated in the course of M. tuberculosis infection, play a key role in the activation of host innate and adaptive immunity and clearance of bacteria [28,29,30].
The following paragraphs briefly describe the most studied miRNAs involved in TB pathogenesis and evasion of host innate immunity, as summarized in Table 1.
Table 1.
Summary of the role of microRNAs (miRNAs) in tuberculosis (TB) pathogenesis.
| Function | Upregulated in TB | Dowregulated in TB |
|---|---|---|
| Inhibition of innate immunity | miR-26-5p, miR-132-3p, miR-155-5p | miR-29-3p |
| Suppression of inflammation | miR-21-5p, miR-27b-3p, miR-99b-5p, miR-125-5p, miR-146a-5p, miR-223-3p | let-7f, miR-20b-5p miR-142-3p |
| Inhibition of phagosome maturation and autophagy | miR-33 locus, miR-27a-5p, miR-144-5p, miR-889-5p | |
| Apoptosis inhibition | miR-155-5p, miR-325-3p |
3. Modulation of Innate and Adaptive Immunity
The innate immune response that leads to M. tuberculosis infection control initiates with pathogen recognition and uptake by resident lung macrophages, which results in cytokine and chemokine production, expression of immune receptors, and initiation of host defense mechanisms, such as the production of antimicrobial molecules and reactive oxygen species [31]. Recognition of M. tuberculosis occurs through different pattern recognition receptors and associated molecules, like TLR2, TLR9, the adaptor molecule MYD88, DC-SIGN, and NLRP3. Stimulation of these pattern recognition receptors induces the expression of pro-inflammatory cytokines, chemokines and cell adhesion receptors that induce immune cell mobilization and activation [32]. Besides lung macrophages, DCs, NK cells, neutrophils and other immune cells contribute to the early innate response against M. tuberculosis, which can be effective in preventing infection. However, in most cases, M. tuberculosis is able to survive and proliferate in infected macrophages, which require activation by antigen-specific T cells to kill the pathogen. Actually, the role of innate immunity in the early stage of M. tuberculosis infection is to establish a suitable condition for induction of adaptive T cell response. The adaptive immune response to M. tuberculosis is characterized by production of IFNγ and chemokines by antigen-specific T cells, which facilitate recruitment of further T cells and trigger the phagocytic activity against intracellular bacteria of macrophages [32].
3.1. MiR-155-5p Inhibits Host Innate Immunity and Promotes M. tuberculosis Clearance
MiR-155-5p is a key regulatory factor in the innate immunity. Its expression is increased in M. tuberculosis-infected macrophages [29] and DCs [30] and in the lungs and liver of mice with M. tuberculosis infection [28,33]. Overexpression of miR-155-5p promotes the survival of infected macrophages and intracellular bacterial replication during the early innate response to M. tuberculosis infection, but promotes M. tuberculosis control during the chronic phase of infection [29,34]. In fact, macrophages from miR-155−/− knock out mice control M. tuberculosis growth better than wild type macrophages by increasing cellular apoptosis. Accordingly, after low-dose aerosol infection, miR-155−/− mice exhibit enhanced control of M. tuberculosis during the early stage of infection, when macrophage function is critical, and this is associated with increased cellular apoptosis in the lungs. However, during the chronic phase of infection, miR-155−/− mice have a higher load of M. tuberculosis and increased inflammatory damage in their lungs and associated mortality than wild-type mice [28,29]. In addition, miR-155−/− mice show a decreased number of antigen-specific CD4+ and CD8+ T cells during chronic M. tuberculosis infection and a reduced production of protective cytokines, such as IFNγ and TNFα, by T cells [28,29]. During M. tuberculosis infection, both in T cells and in macrophages, upregulation of miR-155-5p directly inhibits expression of SHIP1 [25,29], an inositol phosphatase that promotes cell apoptosis through the modification of the PI3K/Akt signaling pathway. Mir-155-5p expression is also induced in M. bovis BCG-infected macrophages via TLR2, NF-κB and JNK signaling pathway [35,36]. In infected macrophages, miR-155-5p inhibits expression of his target SHIP1, leading to increased ROS production [36].
In summary, upregulation of miR-155-5p during M. tuberculosis infection, despite inhibiting innate immunity during the early phases of infection, exerts a protective role against TB by promoting the survival of both infected macrophages and DCs, allowing their activation and hence recruitment of T cells, which play a key role in the ultimate control of M. tuberculosis through their effector functions [29,30].
3.2. MiR-29a-3p Targets IFNγ and Is Downregulated in Experimental Mycobacterial Infection
Production of IFNγ by CD4 T cells is considered a major determinant of TB immunity, although it is not the sole effector mechanisms that contributes to CD4 T cells-mediated protective immunity [37]. During intracellular bacterial infection, miR-29a-3p expression inversely correlates with IFNγ production [38]. In particular, miR-29a-3p is downregulated while IFNγ mRNA levels are higher in CD4+ or CD8+ T cells from M. bovis BCG-infected mice than in those from the uninfected controls [34]. Experiments showed that IFNγ mRNA is a direct target of miR-29a-3p and that miR-29a-3p suppresses immune responses to intracellular pathogens by targeting IFNγ [38]. However, data on the association between miR-29a-3p and IFNγ in humans are contrasting. Lower levels of miR-21-5p, miR-26a-5p, miR-29a-3p, and miR-142-3p were found in CD4+ T cells from children with active TB than from those with LTBI [39]. At variance, analysis of M. tuberculosis-specific IFNγ-expressing T cells in children with TB versus healthy controls did not show any correlation between miR-29a-3p and IFNγ expression [40]. Moreover, suppression of miR-29a-3p in primary human T cells by antagomirs indicated no effect on IFNγ expression after in vitro activation [39].
3.3. Targeting IFNγ Signaling by MiR-26a-5p
Similarly, miR-26a-5p and miR-132-3p can attenuate host immune responses and macrophage activation by IFNγ [41]. These two miRNAs, which are up-regulated upon M. tuberculosis infection, directly target the transcriptional coactivator p300, a component of the IFNγ signaling cascade [41]. However, opposite results were obtained by another study [42], which reported decreased miR-26a-5p expression in macrophages infected with M. tuberculosis and in the lungs, spleen, and lymph nodes of M. tuberculosis-infected mice, while miR-26a-5p overexpression led to reduced M. tuberculosis survival in macrophages. MiR-26a-5p downregulation was associated with increased expression of the transcription factor KLF4, which was validated as a new target for miR-26a-5p [42]. KLF4 was demonstrated to drive macrophage polarization towards M2 phenotype, characterized by production of arginase and inhibition of autophagy, and to inhibit trafficking of M. tuberculosis to lysosomes [42].
4. Suppression of Inflammatory Signaling Pathways
Strong immune responses against M. tuberculosis are required for TB control, but they need to be strictly regulated. In fact, excessive inflammation induced by Th1 cells may compromise the acquired immune responses and become detrimental for the host, while a poor inflammatory response may allow uncontrolled bacteria growth [31]. In this context, anti-inflammatory regulatory T cells are an important component of the immune response to M. tuberculosis infection, as they counterbalance the protective but pro-inflammatory immune response mediated by Th1 cells [43].
4.1. MiR-21-5p, An Anti-Inflammatory MiRNA Upregulated in Mycobacterial Infections
Like in M. tuberculosis infection, the spectrum of clinical manifestations of leprosy depends on the interactions between the host immune response and the invading M. leprae pathogen at the site of disease. Few skin lesions with involvement of local peripheral nerves characterize the mild form of leprosy, called tuberculoid leprosy, while multiple lesions infiltrating nearly all the skin with extensive peripheral nerve involvement characterize the severe progressive disease, called lepromatous leprosy. Skin lesions of tuberculoid leprosy are characterized by innate and adaptive immune responses mediated by T helper type 1 (Th1) cytokines and macrophages programmed to express the vitamin D–dependent antimicrobial pathway, while the immune response in skin lesions of lepromatous leprosy is typically mediated by Th2 cytokines and macrophages with phagocytic activity [44,45].
Comparative analysis of skin lesions of subjects with lepromatous versus tuberculoid disease identified a set of 13 differentially expressed miRNAs, including the top ranking miR-21-5p, miR-24-5p, and miR-146a-5p with significantly higher expression in lepromatous than in tuberculoid disease [46]. Experimental validation studies showed that miR-21-5p is induced in human monocytes infected with M. leprae or treated with phenolic glycolipid-I (PGL-I), a virulence factor from the M. leprae envelope [46]. In addition, M. leprae infection of macrophages upregulates miR-21-5p at the site of infection [46]. MiR-21-5p and other miRNAs associated with lepromatous disease directly target genes involved in host defense mechanisms, such as CYP27B1 and IL1B of the vitamin D antimicrobial pathway, and, indirectly, induce interleukin 10 (IL-10) production and inhibit antimicrobial gene expression [46]. In addition, miR-21-5p overexpression in monocytes blocks TLR2/TLR1-induced antimicrobial activity against M. tuberculosis, while its silencing restores the antimicrobial activity [46].
Expression of miR-21-5p is also upregulated in lung macrophages obtained from mice after vaccination with M. bovis BCG and in macrophages and DCs infected ex vivo with M. bovis BCG [47]. In this infection model, miR-21-5p suppresses host Th1 response by targeting IL-12 and promotes DC apoptosis by targeting Bcl-2 [47].
A recent study showed that M. tuberculosis infection of macrophages is associated with inhibition of host glycolysis [48], and this is dependent on the repression of the phosphofructokinase muscle (PFK-M) isoform by miR-21-5p [48]. At variance, M. tuberculosis infection of macrophages obtained from miR-21-5p-deficient mice induces lactate production, suggestive of increased glycolysis [48]. In miR-21-5p-deficient macrophages, bacterial intracellular growth is reduced in comparison with wild type macrophages, and this is paralleled by increased production of pro-inflammatory mediators with anti-bacterial activity [48]. Thus, upregulation of miR-21-5p represents a strategy adopted by mycobacteria to evade the host antimicrobial responses and to ensure intracellular survival and replication. On the other hand, IFNγ production by activated macrophages downregulates miR-21-5p, hence augmenting PFK-M expression and macrophage glycolysis [48].
4.2. Let-7 Family, Anti-Inflammatory MiRNAs Downregulated in TB
MiRNAs of the let-7 family are downregulated in M. tuberculosis infected macrophages at the transcriptional level in a way dependent on the M. tuberculosis early secreted antigenic target 6-kDa protein (ESAT-6), a secreted effector that can modulate host immune responses and promote M. tuberculosis escape from the phagosome [49]. Transfection of macrophages with let-7 family mimics showed that let-7f is the most effective in attenuating M. tuberculosis survival in macrophages, while treatment with let-7f inhibitor augments M. tuberculosis survival [49]. In the context of M. tuberculosis infection, the deubiquitinating enzyme A20, also known as TNFα-induced protein 3 (TNFAIP3), is a relevant direct target for let-7f and, accordingly, its expression increases while let-7f levels decrease with progression of M. tuberculosis infection in mice [49]. A20 is involved in the maintenance of immune homeostasis as feedback inhibitor of the NF-κB pathway through deubiquitination of TRAF-6 and A20-deficient mice are characterized by severe inflammation and premature death [50]. In M. tuberculosis-infected macrophages, A20 reduces the production of pro-inflammatory cytokines, chemokines and NO by decreasing NF-κB activity, thus promoting M. tuberculosis survival [49].
4.3. MiR-125-5p Suppresses TNFα Production and Autophagy Activation
M. tuberculosis up-regulates miR-155-5p and miR-125b-5p expression in macrophages through its envelope component lipomannan [24,25] and ESAT-6 [34,51]. In comparison with the nonvirulent M. smegmatis, M. tuberculosis induces lower levels of miR-155-5p and higher levels of miR-125b-5p [24]. Since miR-125b-5p directly targets TNFA [24,25], the imbalance between these miRNAs leads to lower production of TNFα by macrophages, thereby reducing host inflammatory response [25]. Moreover, miR-125a-3p targets the UV radiation resistance-associated gene UVRAG, which plays an essential role in the initiation of autophagy through an association of UVRAG with the Beclin 1/Bcl-2/PI(3)KC3 multiprotein complex [24]. Taken together, these data indicate that miR-125a-3p promotes M. tuberculosis immune escape by inhibiting innate host defenses and activation of autophagy [24].
4.4. MiR-146a-5p, Upregulated by Mycobacteria, Targets TRAF6 and Decreases NO Production
MiR-146a-5p is upregulated in M. bovis BCG-infected macrophages both in vitro and in vivo, in which it promotes mycobacteria survival, without affecting phagocytosis [36,52]. In infected macrophages, miR-146a-5p attenuates the activation of NF-κB and mitogen-activated protein kinases signaling pathways, which in turn suppresses the inducible NO synthase (iNOS) expression and NO generation. Mechanistically, these effects are due to miR-146a-5p direct targeting of TNF receptor-associated factor 6 (TRAF6) [52]. In fact, silencing TRAF6 decreased iNOS expression and NO production in M. bovis BCG-infected macrophages, while overexpression of TRAF6 reversed miR-146a-5p-mediated inhibition of NO production and clearance of mycobacteria [52].
4.5. MiR-223-3p, Overexpressed in TB, Mitigates Excessive Inflammation
Active M. tuberculosis infection induces infiltration of neutrophils and macrophages in the lung where they contribute to local inflammation [20]. MiR-223-3p, which plays a relevant role in myeloid cells biology and is enriched in neutrophils and macrophages [53], is abundantly expressed in blood and lung parenchyma in human and murine TB [54,55,56]. In myeloid cells, miR-223-3p controls NF-κB activity and negatively regulates cytokine release in TB [22,54]. Direct targets of miR-223-3p are represented by the chemokine C-X-C motif ligand 2 (CXCL2), C-C motif ligand 3 (CCL3), and IL-6 [54]. Notably, miR-223-3p knock-out mice fail to control pulmonary TB due to an increased amount of aberrant neutrophils migration and exacerbated inflammation [54]. Thus, miR-223-3p is able to control excessive inflammation in TB by regulating leukocyte chemotaxis and NF-kB activity.
4.6. MiR-27b-3p and MiR-99b-5p Prevent Excessive Inflammation in TB
In macrophages, M. tuberculosis infection upregulates expression of the miR-23b/miR-27b/miR-24-1 cluster [57]. Among these miRNAs, miR-27b-3p is induced by the TLR-2/MyD88/NF-kB signaling pathway and suppresses the production of pro-inflammatory factors and NF-kB activity, thereby providing a negative feedback loop to prevent excessive inflammation during M. tuberculosis infection [58]. In addition, miR-27b-3p increases p53-dependent cell apoptosis and the production of reactive oxygen species, while decreasing bacterial burden [58]. In macrophages, the Bcl-2–associated athanogene 2 (Bag2) was identified as direct target of miR-27b-3p, which can reverse miR-27b-3p–mediated inhibition of the production of pro-inflammatory factors and apoptosis induction [58].
MiR-99b-5p is another miRNA capable of modulating host immunity after M. tuberculosis infection by controlling TNFα production. Interestingly, miR-99b-5p is significantly up-regulated in M. tuberculosis-infected DCs and macrophages [59]. Inhibition of miR-99b-5p expression leads to reduced bacterial growth in DCs and up-regulation of pro-inflammatory cytokines such as IL-6, IL-12, and IL-1β [59].
4.7. MiR-142-3p, An Anti-Inflammatory MiRNA Downregulated in TB
MiR-142-3p, downregulated in CD4 T cells and peripheral blood from TB patients [39] and in M. bovis-infected macrophages [60], negatively regulates the expression of inflammatory cytokines, like NF-κB, TNF-α, and IL-6, in part by targeting the IRAK1 gene [60].
5. Inhibition of Phagosome Maturation and Autophagy
Inhibition of phagosome acidification, phagosome–lysosome fusion, ESAT-6 secretion system 1 (ESX1)-dependent escape from the phagosome, and inhibition of autophagy are a key pathogenic mechanisms of M. tuberculosis to ensure survival and persistence in the host [61]. M. tuberculosis has evolved different virulence mechanisms to evade macrophage killing. For example, the cell wall component lipoarabinomannan suppresses the process of fusion between phagosomes and lysosomes and autophagy. Different miRNAs modulated upon M. tuberculosis infection target the autophagy process and phagolysosome maturation.
5.1. MiR-33 Locus MiRNAs Target Autophagy Effectors
The miR-33 locus consists of two intronic miRNAs miR-33a-5p and miR-33b-5p and the respective passenger strands miR33a-3p and miR-33-3p, which co-regulate a set of genes involved in cellular cholesterol export and fatty acid oxidation [62,63]. These miRNAs are upregulated in macrophages upon M. tuberculosis infection or treatment with mycobacterial cell wall constituents via an NF-κB-dependent mechanism [23]. In infected macrophages, expression of the miR-33 locus contributes to the formation of fatty-acid-rich lipid bodies, which serve as source of nutrients for intracellular mycobacteria and to the inhibition of autophagy pathways, lysosomal function and fatty acid oxidation, though direct targeting of several genes encoding autophagy effectors (such as ATG5, ATG12, LC3B, and LAMP1) [23]. Another target of miR-33a-5p was identified in the kinase AMPK (adenosine 5′ monophosphate-activated protein kinase), which activates the transcription factors FOXO3 and TFEB, both promoting the expression of genes involved in the biogenesis and function of autophagosomes and lysosomes [23]. Silencing of miR-33 in macrophages was demonstrated to enhance M. tuberculosis clearance via the autophagy pathway, thus highlighting a mechanism exploited by M. tuberculosis to enable intracellular survival and persistence in the host [23].
5.2. MiR-27a-5p Downregulates Culcium Signaling and Autophagosome Formation
Expression profiling of miRNAs showed that miR-27a-5p is abundantly expressed in active TB patients, M. tuberculosis-infected mice and infected murine primary macrophages, where it promotes bacterial survival through inhibition autophagosome formation [22]. Notably, miR-27a-5p knockout mice infected with M. tuberculosis have less histological damage and inflammatory infiltrates in their lungs than wild type mice, thus indicating that miR-27a-5p confers susceptibility to M. tuberculosis infection [22]. To investigate the feasibility of miR-27a-5p suppression as a therapeutic strategy for TB, mice were infected with M. tuberculosis via the aerosol route and then intraperitoneally injected with a miR-27a-5p antagomir solution. Indeed, treatment resulted in suppression of miR-2a-5p expression in the lung and spleen and significant reduction of bacterial load and tissue damage in the lungs [22]. A key target of miR-27a-5p in TB pathogenesis is CACNA2D3, a component of a voltage-dependent calcium transporter located in the endoplasmic reticulum [22]. Targeting of this transporter leads to the downregulation of Ca2+ signaling and, as a consequence, to the inhibition of autophagosome formation and xenophagy, hence promoting the intracellular survival of M. tuberculosis [22].
5.3. MiR-144-5p Inhibits Phagosome Maturation and T Cell Function
MiR-144-5p is overexpressed in the blood, PBMCs, and sputum of active TB patients and its levels decrease after anti-tuberculosis therapy [64,65]. In vitro, it is upregulated in human monocyte-derived macrophages after M. tuberculosis infection [66]. MiR-144-3p directly binds the 3′UTR region of DRAM2 mRNA (DNA damage regulated autophagy modulator 2), which encodes a transmembrane lysosomal protein that interacts with key components of the autophagy machinery [21]. In PBMCs of patients with active TB, miR-144-5p is mainly expressed by T cells. Forced miR-144-5p overexpression in T cells decreases cell proliferation and reduces IFNγ and TNFα secretion upon TCR stimulation [65]. All together, these data suggest that miR-144-5p upregulation in macrophages and T cells during M. tuberculosis infection represents another mechanism to circumvent anti-tuberculosis immunity through inhibition of phagosome maturation and T cell function.
5.4. MiR-155-5p Promotes M. tuberculosis Killing Through Autophagy
MiR-155-5p inhibits the survival of intracellular mycobacteria through different mechanisms, including promoting phagosome maturation and autophagy induction [33]. In infected macrophages, miR-155-5p targets the negative regulator of autophagy Rheb (Ras homologue enriched in brain), which inhibits autophagy via mTOR [33]. At variance, in M. tuberculosis-infected DCs, miR-155-5p targets ATG3, an E2-ubiquitin-like-conjugating enzyme with an essential role in autophagosome formation, thereby suppressing autophagy in DCs [30].
5.5. MiR-889-5p, Overexpressed in LTBI, Inhibits Autophagy
MiRNA profiling in PBMCs from rheumatoid arthritis patients with LTBI identified miR-889-5p as the top ranking overexpressed miRNA compared with patients without infection [67]. The levels of circulating miR-889-5p were confirmed to be significantly higher in patients with LTBI and to decrease after prophylactic therapy [67]. MiR-889-5p directly targets the cytokine TWEAK (TNF-like weak inducer of apoptosis), whose expression increases in macrophages and PBMCs upon infection with M. tuberculosis or exposure to heat-killed M. tuberculosis [67]. An in vitro model of human TB granuloma showed TWEAK upregulation during the early phase of infection, followed by a decline an increased expression of miR-889-5p with the development of a granuloma-like structure, representative of a LTBI status [67]. Upon entry to latency, elevated miR-889-5p levels are associated with TNFα and granuloma formation/maintenance [67]. In macrophages, TWEAK induces autophagy and promotes autophagosome maturation through activation of AMP-activated protein kinase. In macrophages infected with M. bovis BCG, miR-889-5p overexpression inhibits autophagy and maintains mycobacterial survival in granulomas. Treatment of these granuloma-like structures with adalimumab, an anti-TNF-α monoclonal antibody, reduces levels of both TNF-α and miR-889-5p and causes granuloma destruction and LTBI reactivation [67]. As expected, TWEAK levels are low in LTBI patients and increased after prophylactic therapy [67]. Interestingly, in one LTBI patient receiving adalimumab therapy, circulating TWEAK levels increased at the time of LTBI reactivation and returned to baseline values after anti-TB therapy [67].
6. Subversion of Macrophage Death Pathways
Apoptosis of infected macrophages is a strong innate host defense tool against intracellular pathogens, including mycobacteria, as apoptotic vesicles containing bacterial antigens are taken by other phagocytes or DCs. Then, DCs can efficiently present bacterial antigens to naïve T cells, leading to their activation. Virulent M. tuberculosis inhibits apoptosis and triggers necrosis of host macrophages to evade bacterial killing and innate immunity and to delay the initiation of adaptive immunity [68]. Necrosis is induced when M. tuberculosis escapes from the phagosome and diffuses into the cytosol of macrophages. Necrosis leads to cell lysis and extracellular dissemination of mycobacteria, which can infect other macrophages that have been recruited to the lung. Pyroptosis, a form of necrosis that requires caspase 1 and inflammasome activation, occurs in infected macrophages, when the plasma membrane is damaged by M. tuberculosis ESX-1 secretion system or after phagosome rupture. This damage causes activation of NLRP3-dependent IL-1β release and pyroptosis, which facilitates the spread of bacteria to neighboring cells [69].
6.1. MiR-20b-5p, Downregulated in M. tuberculosis Infection, Inhibits Inflammasome Activation and Promotes Apoptosis
Macrophages isolated from TB patients have decreased miR-20b-5p level, while NLRP3 inflammasome, a central regulator in the inflammatory process and pyroptosis, is activated [27]. In particular, low miR-20b-5p expression and activated NLRP3/caspase-1/IL-1β pathway were observed in a TB mouse model stably infected with M. tuberculosis [27]. In these mice, intravenous injection of miR-20b-5p mimic deactivated the NLRP3/caspase-1/IL-1β pathway and alleviated the inflammatory response. Moreover, transfection of miR-20b-5p in macrophages from TB mice induced M1 to M2 polarization via the NLRP3/caspase-1/IL-1β pathway [27]. MiR-20b-5p resulted downregulated also in a murine macrophage cell line infected by M. tuberculosis [70]. In vitro transfection of these macrophages with miR-20b-5p mimics and a miR-20b-5p inhibitor demonstrated that inhibition of miR-20b-5p promotes M. tuberculosis intracellular survival through attenuation of cell apoptosis [70]. The mechanisms of inflammasome inhibition and apoptosis induction by miR-20b-5p are conceivably the direct targeting of NLRP3 [27] and Mcl-1 [70], a negative regulator of cell apoptosis, respectively.
6.2. MiR-325-3p, Upregulated in M. tuberculosis Infection, Inhibits Apoptosis
MiR-325-3p is upregulated in experimental M. tuberculosis infection in mice and macrophages and in patients with LTBI [26]. MiR-325-3p upregulation occurs also after exposure of macrophages to gamma-irradiated M. tuberculosis but not after infection with M. bovis BCG, which lacks the RD1 genomic region of pathogenicity [26]. Macrophages with silenced miR-325-3p and miR-325-deficient mice show resistance to M. tuberculosis, thus indicating that miR-325-3p promotes M. tuberculosis persistence and latency in the host. MiR-325-3p directly targets LNX1, which encodes an E3 ubiquitin ligase of the serine/threonine protein kinase NEK6. In macrophages, M. tuberculosis leads to LNX1 downregulation and hence NEK6 accumulation, which in turn inhibits apoptosis through activation of STAT3 signaling [26]. Conversely, suppression of the NEK6/STAT3 pathway reduces bacterial burden and improves survival of M. tuberculosis infected mice [26].
6.3. MiR-155-5p Modulates Apoptosis
MiR-155-5p role in the modulation of apoptosis is controversial. In fact, validated targets of miR-155-5p in M. tuberculosis-infected macrophages include: PKI-α, a negative regulator of PKA signaling, whose activation triggers pro-apoptotic genes [35]; the suppressor of cytokine signaling-1 (SOCS1), whose suppression leads to increased IL-6 and TNFα production and apoptosis induction [51]; and forkhead box O3 (FOXO3), which is involved in cell cycle regulation, innate immune response, and resistance to cell apoptosis [71].
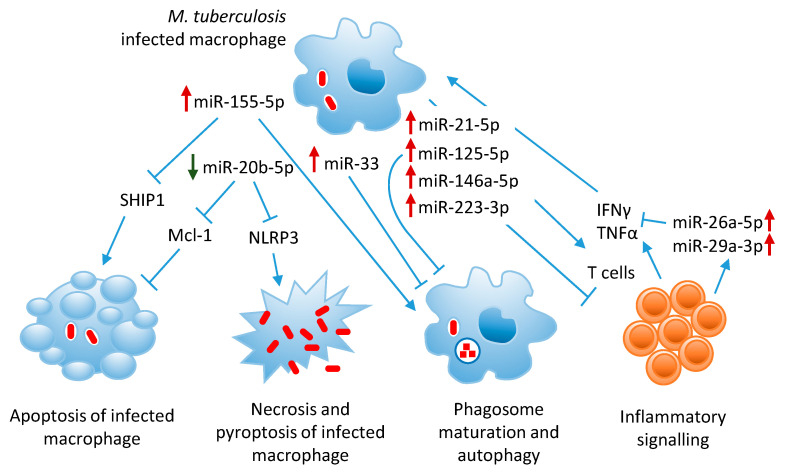
The role of the most relevant miRNAs involved in TB pathogenesis is summarized in Figure 2.
Figure 2.
Graphical representation of miRNA regulation of host immune responses against M. tuberculosis infection. MicroRNAs that are up-regulated or down-regulated during M. tuberculosis infection are indicated with red and green arrows, respectively.
7. Biomarker Discovery Studies
Diagnosis of M. tuberculosis infection and the distinction between active TB and LTBI remain challenging. In addition, currently available tests do not allow predicting which cases of LTBI have higher risk to progress to overt disease during their lifetime. Approaches for the diagnosis of TB include screening tests, based on the evaluation of host immunity, for detecting M. tuberculosis infection in wide populations and more accurate methods, based on direct pathogen detection in clinical samples, for the identification and monitoring of subjects with active TB. A correct strategic approach in the use of screening methods is crucial for both efficiency and sustainability of downstream diagnostics, and for the administration of preventive therapies especially for population groups in whom direct detection of M. tuberculosis in blood or sputum might be problematic (i.e., in children) or in settings where excessively elaborate or expensive methods are hardly sustainable. To date, screening methods rely mainly on tuberculin skin tests and/or IGRA, both lacking the ability to distinguish between active TB or LTBI. Since only about 10% of LTBI subjects will develop active disease, the predictive power of such tests may not be optimal. Screening methods based on disease biomarkers (typically quantified in blood samples) could be of help in detecting subjects with higher probability of progressing into active TB, or who are in early stages of disease [72,73].
Aiming to meet these requirements, several clinical studies have identified molecular signatures, generally applied to PCR assays in blood, which have proven to be effective when tested on prospective cohorts. Such studies make use of gene (or protein) expression screening methods (microarrays, RT-PCR arrays, RNA-sequencing) to detect consistent alterations associated with specific clinical features, typically comparing groups of TB patients with LTBI or healthy subjects, and validating a short-list of selected candidate markers in follow-up studies of TB-exposed groups to predict which subjects will develop pulmonary disease. Many different signatures have been proposed, showing higher sensitivity and specificity than the currently used screening tests [74,75,76,77,78,79,80,81]. Moreover, with a similar approach, signatures of genes or proteins whose expression varies in response to TB therapy have been proposed to provide help in follow-up clinical evaluation of treated patients, or to support prognostic evaluation of newly diagnosed TB cases [74,82].
As for cancer and other diseases, miRNAs have been taken into consideration as a possible source for such biomarkers, and many discovery studies have been published, either as screenings in subjects-vs-controls cohorts or aiming at validating miRNAs identified in experimental studies [83].
As overviewed in the previous paragraphs, M. tuberculosis infection can cause a dysregulation in the expression of genes (including miRNAs) involved in several physiological pathways (immunity, inflammation, autophagy and apoptosis) which could be potentially used as diagnostic and prognostic biomarkers of disease and response to therapy. Several research groups have tried to identify well-defined miRNA signatures that could be analyzed in easily accessible specimens, with particular focus on circulating miRNAs, which are detected in blood (PBMCs or serum/plasma). The desirable miRNA signature should specifically identify subjects with M. tuberculosis infection, and possibly distinguish an active infection (i.e., pulmonary and/or extra-pulmonary tuberculosis) from LTBI. In the next paragraphs, some relevant screening studies performed on serum/plasma or blood cells with different design strategies are briefly reviewed. Data from these and other studies published in the last 10 years are summarized in Table 2 (studies on whole blood, plasma or serum) and in Table 3 (studies on blood cells).
Table 2.
Summary of studies on miRNA biomarker discovery in blood samples from TB subjects and controls.
| Cases No. (Category) |
Controls No. (Category) |
Country | Samples | Method for Screening | Method for Validation | Up-Regulated in TB | Down-Regulated in TB | Ref. | Year |
|---|---|---|---|---|---|---|---|---|---|
| 8 (TB), 21 (LTBI) | 6 treated TB, 14 HC | Brazil | blood | RNA-Seq (Illumina) | qRT-PCR | miR-589-5p | miR-196b-5p, let-7a-5p | [84] | 2020 |
| 60 (TB), 60 (LTBI) | 60 HC | China | exosomes from serum | RNA-Seq (Illumina) | qRT-PCR | miR-1246, miR-2110, miR-370-3p, miR-28-3p, miR-193b-5p | miR-3675-5p | [85] | 2019 |
| 84 (TB), 35 (LTBI) | 42 HC | Cameroon | plasma | literature (miRNA selection) | qRT-PCR | miR-29a-3p, miR-361-5p (vs LTBI); miR-155-5p (vs HC) | [86] | 2019 | |
| 15 (TB), 22 (extra-pulmonary TB) | 15 HC | India | serum | RNA-Seq (Ion Torrent) | qRT-PCR | miR-146a-5p (TB), miR-125b-5p (EPTB) | [87] | 2019 | |
| 246 (TB) | 105 HC | China | exosomes from plasma | Microarray (Affymetrix) | qRT-PCR | miR-20a-5p, miR-20b-5p, miR-26a-5p, miR-106a-5p, miR-191-5p, miR-486-5p | [88] | 2019 | |
| 25 (TB) | 25 HC | Iran | exosomes from serum | literature (miRNA selection) | qRT-PCR | miR-484, miR-425-5p, miR-96-3p | [89] | 2019 | |
| 100 (TB) | 89 treated TB, 100 HC | China | plasma | miRNA PCR panel (Exiqon) | qRT-PCR | miR-29a-3p, miR-99b-5p (vs HC), miR-29a-3p, miR-99b-5p, miR-26a-5p (vs treated) | miR-21-5p, miR-146a-5p, miR-652-5p | [90] | 2018 |
| 54 (TB) | 54 HC | South Africa, Uganda | serum | qRT-PCR | qRT-PCR | miR-21-5p, miR-484 | miR-148b-3p | [91] | 2018 |
| 53 (TB) | 53 treated TB, 53 HC | China | serum | RNA-Seq (Illumina) | qRT-PCR | miR-21-5p, miR-92a-3p, miR-148b-3p (vs treated) | miR-125a-5p (vs treated) | [92] | 2017 |
| 178 (TB) | 95 HC | China | plasma | RNA-Seq (Illumina) | qRT-PCR | miR-22-3p, miR-320a-5p, miR-769-5p | [93] | 2017 | |
| 60 (TB), 32 (MDR-TB) | 60 HC | China | serum | RNA-Seq (Illumina) | qRT-PCR | miR-424-5p, miR-4433b-5p (MDR vs. DS); miR-199b-5p, miR-424-5p (vs HC) | [94] | 2016 | |
| 124 (TB) | 117 HC | China | serum and sputum | literature (miRNA selection) | qRT-PCR | miR-144-3p | [64] | 2016 | |
| 30 (TB), 19 (MDR-TB) | 10 treated TB, 30 HC | India | serum | literature (miRNA selection) | qRT-PCR | miR-16-5p, miR-155-5p | [95] | 2016 | |
| 73 (TB) | 69 HC | China | blood | available microarray dataset | none | miR-132-3p, miR-155-5p | [96] | 2016 | |
| 10 (TB), 13 (LTBI) | 11 HC | China | plasma | Microarray (Agilent) | qRT-PCR | let-7b-5p, miR-30b-5p | [97] | 2016 | |
| 11 (TB) | 10 HC | China | serum | available microarray dataset | miRNA PCR panel (TaqMan) | miR-1249-5p | list of 11 miRNAs | [98] | 2015 |
| 34 (TB, 17 HIV co-infected) | 30 treated TB (14 HIV co-infected) | South Africa | plasma | miRNA PCR panel (MIHS-106Z arrays) | qRT-PCR | miR-29a-3p, miR-17-3p, miR-133a | [99] | 2015 | |
| 17 (TB), 17 (LTBI) | 16 HC | Spain | blood | Microarray (Agilent) | qRT-PCR | miR-194-5p, miR-21-5p, miR-29c-3p (vs HC and LTBI) | miR-150-5p (vs HC and LTBI) | [100] | 2015 |
| 110 (TB) | 48 HC | China | serum | literature (miRNA selection) | qRT-PCR | miR-183-5p | [101] | 2015 | |
| 15 (TB), 14 (LTBI) | 68 HC | China | serum | RNA-Seq (Illumina) | qRT-PCR | miR-196b-5p, miR-376c-3p | [102] | 2014 | |
| 29 (TB) | 37 HC | Egypt | serum | literature (miRNA selection) | miRNA PCR Panel (miScript) | miR-197-3p | [103] | 2013 | |
| 108 (TB) | 88 HC | China | serum | RNA-Seq (Illumina) | qRT-PCR | miR-378a-5p, miR-483-5p, miR-22-3p, miR-29c-3p | miR-101-3p, miR-320b | [104] | 2013 |
| 269 (TB, 73 HIV co-infected), 109 (LTBI) | 105 HC | Italy, Tanzania, Uganda | serum | miRNA PCR panel (TaqMan), pooling of samples | qRT-PCR in a subset of individual samples | list of 12 miRNAs (e.g., miR-148a, miR-192, miR-193a-5p, miR-451, miR-590-5p, miR-885-5p) | let-7e-5p | [105] | 2013 |
| 8 (TB) | 8 HC | Germany | serum | Microarray (Agilent) | none | list of 17 miRNAs | miR-574-5p, miR-768-3p, miR-940 | [106] | 2012 |
| 30 (TB) | 65 HC | China | serum | miRNA PCR panels (TaqMan) | qRT-PCR | miR-361-5p, miR-889, miR-576-3p, miR-210, miR-26a-5p, miR-432-5p, miR-134 | [107] | 2012 | |
| 75 (TB) | 55 HC | China | serum | Microarray (Exiqon) | qRT-PCR | miR-93-3p, miR-29a-3p | miR-3125 | [108] | 2011 |
Table 3.
Summary of miRNA biomarker discovery studies in blood cells (in vivo or ex vivo) from TB subjects and controls.
| Subjects No. (Category) |
Controls No. (Category) |
Country | Samples | Method for Screening | Method for Validation | Up-Regulated in TB | Down-Regulated in TB | Ref. | Year |
|---|---|---|---|---|---|---|---|---|---|
| 30 (TB), 35 (LTBI) | 35 HC | China | PBMCs | available microarray dataset | qRT-PCR | miR-212-3p | [109] | 2019 | |
| 3 (TB) | 3 HC | China | PBMCs | small RNA-seq | none | list of 18 miRNAs | list of 23 miRNAs | [110] | 2018 |
| 12 (TB) | 12 HC | South Africa | PBMCs | literature (miRNA selection) | qRT-PCR | miR-320a-3p, miR-204-5p, miR-331-3p, miR-147b, miR-210-3p | miR-197-3p, miR-99b-5p, miR-191-5p | [111] | 2018 |
| 21 (TB) | 21 treated TB | Mexico | PBMCs | literature (miRNA selection) | qRT-PCR | miR-29a-3p, miR-326 | [112] | 2017 | |
| 9 (TB) | 9 HC | Argentina | PBMCs | literature (miRNA selection) | qRT-PCR | miR-29a-3p, miR-30c-5p, miR-181a-5p, miR-181b-5p | [113] | 2017 | |
| 122 (TB) | 130 HC | China | PBMCs, CSF | literature (miRNA selection) | qRT-PCR | miR-29a-3p | [114] | 2017 | |
| 28 (TB) | 24 HC | China | PBMCs | Microarray (Agilent) | qRT-PCR | miR-29b-3p | miR-1-3p, miR-155-5p, miR-31-5p, miR-146a-5p, miR-10a-5p, miR-125b-5p, miR-150-5p | [115] | 2016 |
| 3 (TB), 4 (LTBI) | 3 HC | Hong Kong-China | Macrophages ex vivo | miRNA PCR panel (TaqMan) | none | miR-16-5p, miR-137, miR-140-3p, miR-193a-3p, miR-501-5p, miR-598 | miR-95 | [116] | 2015 |
| 65 (TB) | 60 HC | China | PBMCs | literature (miRNA selection) | qRT-PCR | miR-31 | [117] | 2015 | |
| 30 (TB), 28 (LTBI) | 30 HC | China | CD4 + T cells | Microarray (Exiqon) | qRT-PCR | miR-451a, miR-340-5p, miR-136-5p, miR-29b-3p | miR-4292 | [118] | 2013 |
| 22 (TB), 14 (LTBI) | 19 HC | Germany | CD4 + T cells | literature (miRNA selection) | qRT-PCR | miR-21-5p, miR-26a-5p, miR-29a-3p, miR-142-3p | [39] | 2013 | |
| 24 (TB) | 20 HC | Argentina | PBMCs | literature (miRNA selection) | qRT-PCR | miR-424-5p | miR-146a-5p | [119] | 2012 |
| 29 (TB), 29 (LTBI) | 18 HC | China | PBMCs | Microarray (Agilent) | qRT-PCR | miR-424-5p, miR-365a-3p (vs HC); miR-424-5p, miR-365a-3p, miR-144-3p, miR-223-3p, miR-451a (vs LTB) | [120] | 2011 | |
| 21 (TB) | 19 HC | China | PBMCs induced with PPD | Microarray (Agilent) | qRT-PCR | miR-155-5p, miR-155-3p | [112] | 2011 |
7.1. Biomarkers of Active Tuberculosis
The starting step in the definition of miRNAs as effective biomarkers in TB diagnosis is the establishment of a consistent signature of differential miRNA expression in samples from active TB cases compared to healthy controls. During the last decade, several studies with this design have been performed to identify TB-associated miRNA signatures in serum/plasma and blood cells (Table 2 and Table 3). Though serum and plasma are usually preferred as starting material for diagnostic screenings, many researchers used cells (PBMCs or specific cell subsets) for discovery studies on miRNA expression. Studies that performed miRNA profiling by broad-spectrum unbiased methods, like miRNA microarray analysis or small RNA sequencing by next-generation sequencing techniques, should generate more reliable results than studies based on the investigation of a panel of candidate miRNAs. However, screenings by small RNA-sequencing or miRNA microarrays have been generally applied to relatively small groups of subjects (usually less than 10 subjects), and then the identified candidates were validated by targeted assays, like qRT-PCR, in larger groups of subjects. This approach might present limitations for the robustness and reproducibility of results. At variance, several other studies performed only qRT-PCR to validate candidate miRNA biomarkers identified from available datasets or based on the role of the candidate miRNA in TB pathogenesis [111,113,114,117,119].
Unfortunately, poor consensus arises from the results of these screenings, as very few miRNAs are present in the proposed signature of two or more studies. Probably this is due to the different screening methods (various RNA-sequencing and microarrays platforms) or to heterogeneity of cohorts (including size and ethnicity). RNA isolation methods can also influence heavily the results, as is the case of studies that were performed with protocols that specifically recover RNA from blood exosome vesicles [87,88]. Since many miRNAs are abundant in exosomes, this approach can be of particular interest, although the results obtained by the two studies on exosome vesicles-associated miRNAs do not agree [87,88].
Nonetheless, notwithstanding the heterogeneity of the results, some miRNAs have been recurrently identified as candidate biomarkers of TB in more than one study. Among these candidate miRNAs, miR-26a-5p, and miR-29a-3p were identified by different studies as significantly overexpressed in patients with active TB vs. healthy controls [86,88,90,108,109,115]. These are relevant miRNAs in TB pathogenesis, since, as previously discussed, both directly or indirectly target IFNγ, thus suppressing host innate and adaptive immune response against intracellular pathogens. Other anti-inflammatory miRNA, miR-21-5p, and miR-146a-5p, which are overexpressed in active TB patients, are promising diagnostic biomarker to differentiate between active TB and latent infection or an healthy condition [87,92,101]. MiR-155-5p, overexpressed in TB patients and candidate biomarker of active TB, plays a key role in host defense against M. tuberculosis [86,96,112].
7.2. MiRNAs in Latent vs. Active Tuberculosis
Since the currently available tests do not effectively discriminate between LTBI and active TB, a biomarker with a significant difference in expression between the two conditions would be very useful. Several studies of miRNA expression profiling in serum/plasma [86,90,97,102] or in blood cells [33,39,109,116,118] have been performed in cohorts which included subjects with LTBI along with active TB infection and healthy controls. In some of these studies, significant miRNA signatures were identified that could actually discriminate active TB from LTBI. A study on PBMCs used miRNA-specific microarrays to obtain a short-list of candidates that were validated by qRT-PCR [33]. Interestingly, five miRNAs (miR-424-5p, miR-365a-3p, miR-144-3p, miR-223-3p, and miR-451a-5p) with high expression in PBMCs were upregulated in active TB vs. LTBI, with target predictions suggesting a possible role in hematopoiesis. The same experimental setup was used in another study that identified overexpression of miR-194-5p, miR-21-5p, miR-29c-3p and the downregulation of miR-150-5p in the active TB group compared with both LTBI and HC groups [100]. By using qRT-PCR, miR-29a-3p overexpression was confirmed to be a valuable candidate biomarker to discriminate between active TB and LTBI in a cohort of subjects from Cameroon [86]. In this cohort, expression levels of miRNAs was similar in subjects co-infected with HIV and in those without HIV infection [86]. A recent study in China, which analyzed miRNA expression profile by RNA-sequencing in serum exosomes, found overexpression of miR-1246, miR-2110, miR-370-3p, miR-28-3p, miR-193b-5p and downregulation of miR-3675-5p in active TB, but also identified a set of miRNAs exclusively expressed in latent TB [85]. No validation experiments in a second cohort of patients were performed.
7.3. Prognostic Biomarkers of Risk of Progression to Tuberculosis and Response to Therapy
Prospective studies have been performed with the aim to identify prognostic miRNA signatures associated with the risk of progression from LTBI to active TB or predictive of response to anti-TB therapies.
As an example of the first aim, a recent study [91] identified in a cohort of subjects in South Africa and Uganda, developing active TB in a 2 years follow up, a significant miRNA signature of disease-progression (i.e., overexpression of miR-21-5p, miR-484 and downregulation of miR-148b-3p).
As for the second aim, the identification of a miRNA signature with diagnostic value can help in evaluating follow-up subjects during treatment. Theoretical expectations are that miRNAs deregulated at diagnosis can revert to baseline values if therapy is successful. A study in an Indian cohort [95] showed that miR-16-5p and miR-155-5p worked as diagnostic biomarkers in patients with acute TB, while levels were low in healthy controls and in TB patients who successfully completed therapy. These miRNA, though, were selected on literature basis and not after an experimental screening. Other miRNAs (miR-99b-5p, miR-29a-3p, miR-26a-5p) were identified as being downregulated in subjects undergoing successful TB treatment in a large Chinese cohort tested by two different qRT-PCR protocols [90]. At variance, another Chinese study with a similar design and therapeutic regimen, but with a different screening method (i.e., small RNA-sequencing) obtained different results. In this case, treated subjects had downregulated miR-21-5p, miR-92a-3p, miR-148b-3p, and overexpressed miR-125a-5p [92]. Possibly, the reason of such heterogeneous reports could be due to differences in screening methods, thus emphasizing the importance of standardization of protocols to provide more consistent findings. A recent report from Brazil [84], which used small RNA-seq of whole blood from subjects with active TB, latent TB and isoniazide-treated latent TB, identified three miRNAs (let-7a-5p, miR-196b-5p, miR-589-5p) and the small nucleolar RNA SNORD104 as a highly sensitive (100%) classifier to discriminate TB from non-TB groups. However, no highly accurate biomarker were found for the discrimination between TB and LTBI [84]. Interestingly, expression of the four small RNAs changed as expected in a LTBI patient who progressed to active TB (i.e., downregulation for let-7a-5p, miR-196b-5p, and SNORD104, but upregulation for miR-589-5p) and tended to normalize in two patients with active TB for whom whole blood samples were available after completion of therapy [84]. In addition, these small RNAs had similar expression profiles in peripheral whole blood in active TB patients and in PBMCs infected ex vivo with M. tuberculosis [84].
Another study investigated the levels of circulating small RNAs in a group of 34 patients with active TB (including 17 with HIV-1 co-infection) who were treated with standard 6-month drug regimen for pulmonary TB [99]. Comparison of small RNA levels before and after completion of therapy showed a significant decrease of plasma small RNA levels after effective treatment, which was independent of HIV-1 co-infection [99]. No single miRNAs nor combination of small RNAs were significantly associated with successful TB treatment, even though there was a trend towards a decrease of miR-17-3p, miR-29a-3p, miR-133a, and SNORD61 in those who responded to therapy (n = 30) compared with those who did not (n = 4) [99].
8. Conclusions
Tuberculosis remains one of the most relevant health emergencies worldwide, with estimates of 1.4 million fatalities in 2018. Despite great advances in diagnosis and therapy, the large proportion of infected subjects in populations, especially in low-income countries, requires the development of new screening methods capable of detecting high-risk conditions with easily manageable assays.
With this aim, the search for ideal biomarkers for detection in blood (or other non-invasive samples) has found miRNAs as potentially ideal candidates. MiRNAs are indeed strictly involved in the pathogenesis pathways of TB, and in particular in the regulation of immune responses related to the switch between latent and active infection. Moreover, many of them are present in detectable amounts in plasma or serum, and can easily be quantified by PCR-based methods.
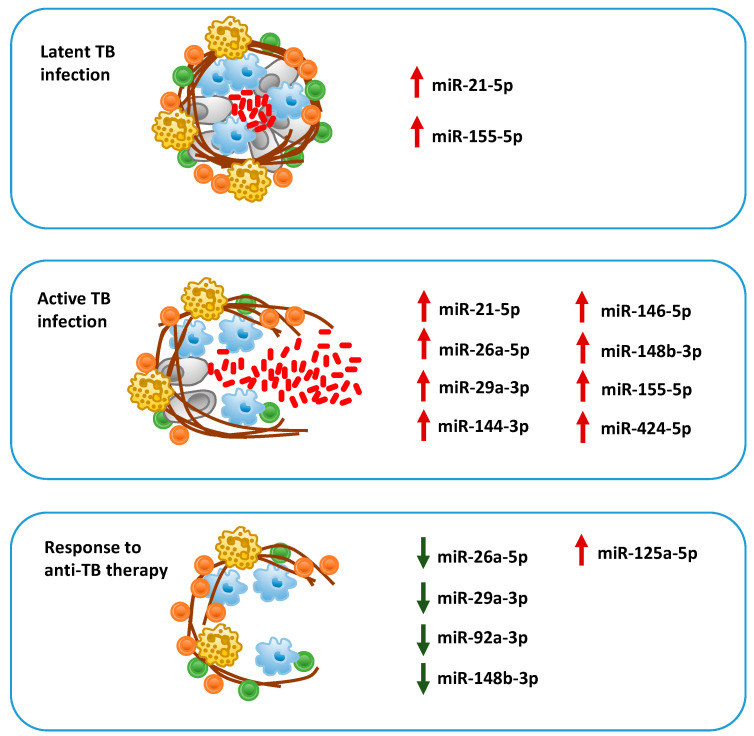
Several studies in recent years have focused on selecting short-lists (signatures) of miRNAs whose expression in consistently related to the development of active TB or to a differential response to therapies. Their common aim is introducing in diagnostic routine screening assays with significant predictive power, improving the accuracy of currently used assays based mainly on tuberculin skin test of IGRA. On the other hand, many research groups are working to establish functional relations between miRNAs expression in differential conditions and their actual biological effect, molecular biology and bioinformatics methods to validate their biological targets and understand their role in TB pathogenesis. This review, in particular, identified some promising candidates, like miR-155-5p, miR-146a-5p, miR-26a-5p, miR-29a-3p, mir-21-5p, mir-144-3p, and miR-424-5p, which can discriminate among active TB from LTBI and healthy condition and predict response to anti-TB therapy (Figure 3). Taken together, these two arms of the general effort of the scientific community are expected to provide in the next future a new generation of screening assays based on miRNAs. These diagnostic tools need to adhere to quality requirements of specificity and sensitivity, but as well to have biological relevance in TB pathogenesis.
Figure 3.
Graphical representation of circulating miRNAs, which are significantly up-regulated (red arrow) or down-regulated (green arrow) in subjects with latent tuberculosis (TB) infection, active TB, or who responded to anti-TB therapy, and have been proposed as candidate biomarkers.
Author Contributions
Conceptualization, L.B., R.M., and S.V.; data curation, L.B.; A.S., E.P., and S.R.; writing—original draft preparation, A.S. and E.P.; writing—review and editing, L.B.; visualization, L.B.; supervision, L.B.; project administration, R.M.; funding acquisition, S.V. All authors have read and agreed to the published version of the manuscript.
Funding
This study received financial support from the European Commission’s Horizon 2020 research and innovation program under grant agreement No 825931 (ARREST-TB).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Dye C., Williams B.G. The population dynamics and control of tuberculosis. Science. 2010;328:856–861. doi: 10.1126/science.1185449. [DOI] [PubMed] [Google Scholar]
- 2.WHO . Global Tuberculosis Report 2019. World Health Organization; Geneva, Switzerland: 2019. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 3.Pai M., Behr M.A., Dowdy D., Dheda K., Divangahi M., Boehme C.C., Ginsberg A., Swaminathan S., Spigelman M., Getahun H., et al. Tuberculosis. Nat. Rev. Dis. Primers. 2016;2:16076. doi: 10.1038/nrdp.2016.76. [DOI] [PubMed] [Google Scholar]
- 4.Simmons J.D., Stein C.M., Seshadri C., Campo M., Alter G., Fortune S., Schurr E., Wallis R.S., Churchyard G., Mayanja-Kizza H., et al. Immunological mechanisms of human resistance to persistent Mycobacterium tuberculosis infection. Nat. Immun. 1996;64:683–690. doi: 10.1038/s41577-018-0025-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith I. Mycobacterium tuberculosis pathogenesis and molecular determinants of virulence. Clin. Microbiol. Rev. 2003;16:463–496. doi: 10.1128/CMR.16.3.463-496.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Natarajan K., Kundu M., Sharma P., Basu J. Innate immune responses to M. tuberculosis infection. Tuberculosis. 2011;91:427–431. doi: 10.1016/j.tube.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Ahmad S. Pathogenesis, immunology, and diagnosis of latent Mycobacterium tuberculosis infection. Clin. Dev. Immunol. 2011:814943. doi: 10.1155/2011/814943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Das K., Garnica O., Dhandayuthapani S. Modulation of host miRNAs by intracellular bacterial pathogens. Front. Cell. Infect. Microbiol. 2016;6:79. doi: 10.3389/fcimb.2016.00079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maudet C., Mano M., Eulalio A. MicroRNAs in the interaction between host and bacterial pathogens. FEBS Lett. 2014;588:4140–4147. doi: 10.1016/j.febslet.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Pillai R.S., Bhattacharyya S.N., Filipowicz W. Repression of protein synthesis by miRNAs: How many mechanisms? Trends Cell. Biol. 2007;17:118–126. doi: 10.1016/j.tcb.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 11.Hammond S.M. An overview of microRNAs. Adv. Drug Deliv. Rev. 2015;87:3–14. doi: 10.1016/j.addr.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tribolet L., Kerr E., Cowled C., Bean A.G.D., Stewart C.R., Dearnley M., Farr R.J. MicroRNA biomarkers for infectious diseases: From basic research to biosensing. Front. Microbiol. 2020;11:1197. doi: 10.3389/fmicb.2020.01197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walzl G., McNerney R., du Plessis N., Bates M., McHugh T.D., Chegou N.N., Zumla A. Tuberculosis: Advances and challenges in development of new diagnostics and biomarkers. Lancet Infect. Dis. 2018;18:e199–e210. doi: 10.1016/S1473-3099(18)30111-7. [DOI] [PubMed] [Google Scholar]
- 14.Lalvani A., Berrocal-Almanza L.C., Halliday A. Predicting progression to active tuberculosis: A rate-limiting step on the path to elimination. PLoS Med. 2019;16:e1002814. doi: 10.1371/journal.pmed.1002814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang T., Ge B. miRNAs in immune responses to Mycobacterium tuberculosis infection. Cancer Lett. 2018;431:22–30. doi: 10.1016/j.canlet.2018.05.028. [DOI] [PubMed] [Google Scholar]
- 16.Behrouzi A., Alimohammadi M., Nafari A.H., Yousefi M.-H., Riazi Rad F., Vaziri F., Siadat S.D. The role of host miRNAs on Mycobacterium tuberculosis. ExRNA. 2019;1:40. doi: 10.1186/s41544-019-0040-y. [DOI] [Google Scholar]
- 17.Sabir N., Hussain T., Shah S.Z.A., Peramo A., Zhao D., Zhou X. miRNAs in tuberculosis: New avenues for diagnosis and host-directed therapy. Front. Microbiol. 2018;9:602. doi: 10.3389/fmicb.2018.00602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruiz-Tagle C., Naves R., Balcells M.E. Unraveling the role of microRNAs in Mycobacterium tuberculosis infection and disease: Advances and pitfalls. Infect. Immun. 2020;88:e00649-19. doi: 10.1128/IAI.00649-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harapan H., Fitra F., Ichsan I., Mulyadi M., Miotto P., Hasan N.A., Calado M., Cirillo D.M. The roles of microRNAs on tuberculosis infection: Meaning or myth? Tuberculosis. 2013;93:596–605. doi: 10.1016/j.tube.2013.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Philips J.A., Ernst J.D. Tuberculosis pathogenesis and immunity. Annu. Rev. Pathol. 2012;7:353–384. doi: 10.1146/annurev-pathol-011811-132458. [DOI] [PubMed] [Google Scholar]
- 21.Kim J.K., Kim T.S., Basu J., Jo E.K. MicroRNA in innate immunity and autophagy during mycobacterial infection. Cell. Microbiol. 2017;19 doi: 10.1111/cmi.12687. [DOI] [PubMed] [Google Scholar]
- 22.Liu F., Chen J., Wang P., Li H., Zhou Y., Liu H., Liu Z., Zheng R., Wang L., Yang H., et al. MicroRNA-27a controls the intracellular survival of Mycobacterium tuberculosis by regulating calcium-associated autophagy. Nat. Commun. 2018;9:4295. doi: 10.1038/s41467-018-06836-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ouimet M., Koster S., Sakowski E., Ramkhelawon B., van Solingen C., Oldebeken S., Karunakaran D., Portal-Celhay C., Sheedy F.J., Dutta Ray T., et al. Mycobacterium tuberculosis induces the miR-33 locus to reprogram autophagy and host lipid metabolism. Nat. Immunol. 2016;17:677–686. doi: 10.1038/ni.3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim J.K., Yuk J.M., Kim S.Y., Kim T.S., Jin H.S., Yang C.S., Jo E.K. MicroRNA-125a inhibits autophagy activation and antimicrobial responses during mycobacterial infection. J. Immunol. 2015;194:5355–5365. doi: 10.4049/jimmunol.1402557. [DOI] [PubMed] [Google Scholar]
- 25.Rajaram M.V., Ni B., Morris J.D., Brooks M.N., Carlson T.K., Bakthavachalu B., Schoenberg D.R., Torrelles J.B., Schlesinger L.S. Mycobacterium tuberculosis lipomannan blocks TNF biosynthesis by regulating macrophage MAPK-activated protein kinase 2 (MK2) and microRNA miR-125b. Proc. Natl. Acad. Sci. USA. 2011;108:17408–17413. doi: 10.1073/pnas.1112660108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fu B., Xue W., Zhang H., Zhang R., Feldman K., Zhao Q., Zhang S., Shi L., Pavani K.C., Nian W., et al. MicroRNA-325-3p facilitates immune escape of Mycobacterium tuberculosis through targeting LNX1 via NEK6 accumulation to promote anti-apoptotic STAT3 signaling. mBio. 2020;11:e00557-20. doi: 10.1128/mBio.00557-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lou J., Wang Y., Zhang Z., Qiu W. MiR-20b inhibits Mycobacterium tuberculosis induced inflammation in the lung of mice through targeting NLRP3. Exp. Cell Res. 2017;358:120–128. doi: 10.1016/j.yexcr.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 28.Iwai H., Funatogawa K., Matsumura K., Kato-Miyazawa M., Kirikae F., Kiga K., Sasakawa C., Miyoshi-Akiyama T., Kirikae T. MicroRNA-155 knockout mice are susceptible to M. tuberculosis infection. Tuberculosis. 2015;95:246–250. doi: 10.1016/j.tube.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 29.Rothchild A.C., Sissons J.R., Shafiani S., Plaisier C., Min D., Mai D., Gilchrist M., Peschon J., Larson R.P., Bergthaler A., et al. MiR-155–regulated molecular network orchestrates cell fate in the innate and adaptive immune response to Mycobacterium tuberculosis. Proc. Natl. Acad. Sci. USA. 2016;113:E6172–E6181. doi: 10.1073/pnas.1608255113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Etna M.P., Sinigaglia A., Grassi A., Giacomini E., Romagnoli A., Pardini M., Severa M., Cruciani M., Rizzo F., Anastasiadou E., et al. Mycobacterium tuberculosis-induced miR-155 subverts autophagy by targeting ATG3 in human dendritic cells. PLoS Pathog. 2018;14:e1006790. doi: 10.1371/journal.ppat.1006790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Orme I.M., Robinson R.T., Cooper A.M. The balance between protective and pathogenic immune responses in the TB-infected lung. Nat. Immunol. 2015;16:57–63. doi: 10.1038/ni.3048. [DOI] [PubMed] [Google Scholar]
- 32.Ernst A.D. The immunological life cycle of tuberculosis. Nat. Rev. Immunol. 2012;12:581–591. doi: 10.1038/nri3259. [DOI] [PubMed] [Google Scholar]
- 33.Wang J., Yang K., Zhou L., Wu M., Wu Y., Zhu M., Lai X., Chen T., Feng L., Li M., et al. MicroRNA-155 promotes autophagy to eliminate intracellular mycobacteria by targeting Rheb. PLoS Pathog. 2013;9:e1003697. doi: 10.1371/journal.ppat.1003697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kumar R., Halder P., Sahu S.K., Kumar M., Kumari M., Jana K., Ghosh Z., Sharma P., Kundu M., Basu J. Identification of a novel role of ESAT-6-dependent miR-155 induction during infection of macrophages with Mycobacterium tuberculosis. Cell Microbiol. 2012;14:1620–1631. doi: 10.1111/j.1462-5822.2012.01827.x. [DOI] [PubMed] [Google Scholar]
- 35.Ghorpade D.S., Leyland R., Kurowska-Stolarska M., Patil S.A., Balaji K.N. MicroRNA-155 is required for Mycobacterium bovis BCG-mediated apoptosis of macrophages. Mol. Cell. Biol. 2012;32:2239–2253. doi: 10.1128/MCB.06597-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang J., Wu M., Wen J., Yang K., Li M., Zhan X., Feng L., Li M., Huang X. MicroRNA-155 induction by Mycobacterium bovis BCG enhances ROS production through targeting SHIP1. Mol. Immunol. 2014;62:29–36. doi: 10.1016/j.molimm.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 37.Ernst J.D. Mechanisms of M. tuberculosis immune evasion as challenges to TB vaccine design. Cell Host Microbe. 2018;24:34–42. doi: 10.1016/j.chom.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ma F., Xu S., Liu X., Zhang Q., Xu X., Liu M., Hua M., Li N., Yao H., Cao X. The microRNA miR-29 controls innate and adaptive immune responses to intracellular bacterial infection by targeting interferon-γ. Nat. Immunol. 2011;12:861–869. doi: 10.1038/ni.2073. [DOI] [PubMed] [Google Scholar]
- 39.Kleinsteuber K., Heesch K., Schattling S., Kohns M., Sander-Jülch C., Walzl G., Hesseling A., Mayatepek E., Fleischer B., Marx F.M., et al. Decreased expression of miR-21, miR-26a, miR-29a, and miR-142-3p in CD4+ T cells and peripheral blood from tuberculosis patients. PLoS ONE. 2013;8:e61609. doi: 10.1371/journal.pone.0061609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Afum-Adjei Awuah A., Ueberberg B., Owusu-Dabo E., Frempong M., Jacobsen M. Dynamics of T-cell IFN-γ and miR-29a expression during active pulmonary tuberculosis. Int. Immunol. 2014;26:579–582. doi: 10.1093/intimm/dxu068. [DOI] [PubMed] [Google Scholar]
- 41.Ni B., Rajaram M.V., Lafuse W.P., Landes M.B., Schlesinger L.S. Mycobacterium tuberculosis decreases human macrophage IFN-γ responsiveness through miR-132 and miR-26a. J. Immunol. 2014;193:4537–4547. doi: 10.4049/jimmunol.1400124. [DOI] [PubMed] [Google Scholar]
- 42.Sahu S.K., Kumar M., Chakraborty S., Banerjee S.K., Kumar R., Gupta P., Jana K., Gupta U.D., Ghosh Z., Kundu M., et al. MicroRNA26a (miR-26a)/KLF4 and CREB-C/EBPβ-regulate innate immune signaling, the polarization of macrophages and the trafficking of Mycobacterium tuberculosis to lysosomes during infection. PLoS Pathog. 2017;13:e1006410. doi: 10.1371/journal.ppat.1006410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cardona P., Cardona P.J. Regulatory T cells in Mycobacterium tuberculosis infection. Front. Immunol. 2019;10:2139. doi: 10.3389/fimmu.2019.02139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yamamura M., Uyemura K., Deans R.J., Weinberg T., Rea H., Bloom B.R., Modlin R.L. Defining protective responses to pathogens: Cytokine profiles in leprosy lesions. Science. 1991;254:277–279. doi: 10.1126/science.1925582. [DOI] [PubMed] [Google Scholar]
- 45.Montoya D., Cruz D., Teles R.M., Lee D.J., Ochoa M.T., Krutzik S.R., Chun R., Schenk M., Zhang X., Ferguson B.G., et al. Divergence of macrophage phagocytic and antimicrobial programs in leprosy. Cell Host Microbe. 2009;6:343–353. doi: 10.1016/j.chom.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu P.T., Wheelwright M., Teles R., Komisopoulou E., Edfeldt K., Ferguson B., Mehta M.D., Vazirnia A., Rea T.H., Sarno E.N., et al. MicroRNA-21 targets the vitamin D–dependent antimicrobial pathway in leprosy. Nat. Med. 2012;18:267–273. doi: 10.1038/nm.2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wu Z., Lu H., Sheng J., Li L. Inductive microRNA-21 impairs anti-mycobacterial responses by targeting IL-12 and Bcl-2. FEBS Lett. 2012;586:2459–2467. doi: 10.1016/j.febslet.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 48.Hackett E.E., Charles-Messance H., O’Leary S.M., Gleeson L.E., Muñoz-Wolf N., Case S., Wedderburn A., Johnston D.G.W., Williams M.A., Smyth A., et al. Mycobacterium tuberculosis limits host glycolysis and IL-1β by restriction of PFK-M via microRNA-21. Cell Rep. 2020;30:124–136.e4. doi: 10.1016/j.celrep.2019.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kumar M., Kumar Sahu S., Kumar R., Subuddhi A., Kumar Maji R., Jana K., Gupta P., Raffetseder J., Lerm M., Ghosh Z., et al. MicroRNA let-7 modulates the immune response to Mycobacterium tuberculosis infection via control of A20, an inhibitor of the NF-kB pathway. Cell Host Microbe. 2015;17:345–356. doi: 10.1016/j.chom.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 50.Vereecke L., Beyaert R., van Loo G. The ubiquitin-editing enzyme A20 (TNFAIP3) is a central regulator of immunopathology. Trends Immunol. 2009;30:383–391. doi: 10.1016/j.it.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 51.Yang S., Li F., Jia S., Zhang K., Jiang W., Shang Y., Chang K., Deng S., Chen M. Early secreted antigen ESAT-6 of Mycobacterium tuberculosis promotes apoptosis of macrophages via targeting the microRNA155–SOCS1 interaction. Cell. Physiol. Biochem. 2015;35:1276–1288. doi: 10.1159/000373950. [DOI] [PubMed] [Google Scholar]
- 52.Li M., Wang J., Fang Y., Gong S., Li M., Wu M., Lai X., Zeng G., Wang Y., Yang K., et al. microRNA-146a promotes mycobacterial survival in macrophages through suppressing nitric oxide production. Sci. Rep. 2016;6:23351. doi: 10.1038/srep23351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johnnidis J.B., Harris M.H., Wheeler R.T., Stehling-Sun S., Lam M.H., Kirak O., Brummelkamp T.R., Fleming M.D., Camargo F.D. Regulation of progenitor cell proliferation and granulocyte function by microRNA-223. Nature. 2008;451:1125–1129. doi: 10.1038/nature06607. [DOI] [PubMed] [Google Scholar]
- 54.Dorhoi A., Iannaccone M., Farinacci M., Faé K.C., Schreiber J., Moura-Alves P., Nouailles G., Mollenkopf H.J., Oberbeck-Müller D., Jörg S., et al. MicroRNA-223 controls susceptibility to tuberculosis by regulating lung neutrophil recruitment. J. Clin. Investig. 2013;123:4836–4848. doi: 10.1172/JCI67604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li T., Morgan M.J., Choksi S., Zhang Y., Kim Y.S., Liu Z.G. MicroRNAs modulate the noncanonical transcription factor NF-kappaB pathway by regulating expression of the kinase IKKalpha during macrophage differentiation. Nat. Immunol. 2010;11:799–805. doi: 10.1038/ni.1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu Y., Wang R., Jiang J., Yang B., Cao Z., Cheng X. MiR-223 is upregulated in monocytes from patients with tuberculosis and regulates function of monocyte-derived macrophages. Mol. Immunol. 2015;67:475–481. doi: 10.1016/j.molimm.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 57.Wu Y., Guo Z., Yao K., Miao Y., Liang S., Liu F., Wang Y., Zhang Y. The transcriptional foundations of Sp110-mediated macrophage (RAW264.7) resistance to Mycobacterium tuberculosis H37Ra. Sci. Rep. 2016;6:22041. doi: 10.1038/srep22041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liang S., Song Z., Wu Y., Gao Y., Gao M., Liu F., Wang F., Zhang Y. MicroRNA-27b modulates inflammatory response and apoptosis during Mycobacterium tuberculosis infection. J. Immunol. 2018;200:3506–3518. doi: 10.4049/jimmunol.1701448. [DOI] [PubMed] [Google Scholar]
- 59.Singh Y., Kaul V., Mehra A., Chatterjee S., Tousif S., Dwivedi V.P., Suar M., Van Kaer L., Bishai W.R., Das G. Mycobacterium tuberculosis controls microRNA-99b (miR-99b) expression in infected murine dendritic cells to modulate host immunity. J. Biol. Chem. 2013;288:5056–5061. doi: 10.1074/jbc.C112.439778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xu G., Zhang Z., Wei J., Zhang Y., Zhang Y., Guo L., Liu X. MicroR-142-3p down-regulates IRAK-1 in response to Mycobacterium bovis BCG infection in macrophages. Tuberculosis. 2013;93:606–611. doi: 10.1016/j.tube.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 61.Zhai W., Wu F., Zhang Y., Fu Y., Liu Z. The immune escape mechanisms of Mycobacterium tuberculosis. Int. J. Mol. Sci. 2019;20:340. doi: 10.3390/ijms20020340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Najafi-Shoushtari S.H., Kristo F., Li Y., Shioda T., Cohen D.E., Gerszten R.E., Näär A.M. MicroRNA-33 and the SREBP host genes cooperate to control cholesterol homeostasis. Science. 2010;328:1566–1569. doi: 10.1126/science.1189123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rayner K.J., Suárez Y., Dávalos A., Parathath S., Fitzgerald M.L., Tamehiro N., Fisher E.A., Moore K.J., Fernández-Hernando C. MiR-33 contributes to the regulation of cholesterol homeostasis. Science. 2010;328:1570–1573. doi: 10.1126/science.1189862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lv Y., Guo S., Li X.G., Chi J.Y., Qu Y.Q., Zhong H.L. Sputum and serum microRNA-144 levels in patients with tuberculosis before and after treatment. Int. J. Infect. Dis. 2016;43:68–73. doi: 10.1016/j.ijid.2015.12.014. [DOI] [PubMed] [Google Scholar]
- 65.Liu Y., Wang X., Jiang J., Cao Z., Yang B., Cheng X. Modulation of T cell cytokine production by miR-144* with elevated expression in patients with pulmonary tuberculosis. Mol. Immunol. 2011;48:1084–1090. doi: 10.1016/j.molimm.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 66.Kim J.K., Lee H.M., Park K.S., Shin D.M., Kim T.S., Kim Y.S., Suh H.W., Kim S.Y., Kim I.S., Kim J.M., et al. MIR144* inhibits antimicrobial responses against Mycobacterium tuberculosis in human monocytes and macrophages by targeting the autophagy protein DRAM2. Autophagy. 2017;13:423–441. doi: 10.1080/15548627.2016.1241922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen D.-Y., Chen Y.-M., Lin C.-F., Lo C.-M., Liu H.-J., Liao T.-L. MicroRNA-889 inhibits autophagy to maintain mycobacterial survival in patients with latent tuberculosis infection by targeting TWEAK. mBio. 2020;11:e03045-19. doi: 10.1128/mBio.03045-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Behar S.M., Divangahi M., Remold H.G. Evasion of innate immunity by M. tuberculosis: Is death an exit strategy? Nat. Rev. Microbiol. 2010;8:668–674. doi: 10.1038/nrmicro2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Beckwith K.S., Beckwith M.S., Ullmann S., Sætra R.S., Kim H., Marstad A., Åsberg S.E., Strand T.A., Haug M., Niederweis M., et al. Plasma membrane damage causes NLRP3 activation and pyroptosis during Mycobacterium tuberculosis infection. Nat. Commun. 2020;11:2270. doi: 10.1038/s41467-020-16143-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhang D., Yi Z., Fu Y. Downregulation of miR-20b-5p facilitates Mycobacterium tuberculosis survival in RAW 264.7 macrophages via attenuating the cell apoptosis by Mcl-1 upregulation. J. Cell. Biochem. 2019;120:5889–5896. doi: 10.1002/jcb.27874. [DOI] [PubMed] [Google Scholar]
- 71.Huang J., Jiao J., Xu W., Zhao H., Zhang C., Shi Y., Xiao Z. MiR-155 is upregulated in patients with active tuberculosis and inhibits apoptosis of monocytes by targeting FOXO3. Mol. Med. Rep. 2015;12:7102–7108. doi: 10.3892/mmr.2015.4250. [DOI] [PubMed] [Google Scholar]
- 72.Fiore-Gartland A., Carpp L.N., Naidoo K., Thompson E., Zak D.E., Self S., Churchyard G., Walzl G., Penn-Nicholson A., Scriba T.J., et al. Considerations for biomarker-targeted intervention strategies for tuberculosis disease prevention. Tuberculosis. 2018;109:61–68. doi: 10.1016/j.tube.2017.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Levin M., Kaforou M. Predicting active tuberculosis progression by RNA analysis. Lancet. 2016;387:2268–2270. doi: 10.1016/S0140-6736(16)00165-3. [DOI] [PubMed] [Google Scholar]
- 74.Sigal G.B., Segal M.R., Mathew A., Jarlsberg L., Wang M., Barbero S., Small N., Haynesworth K., Davis J.L., Weiner M., et al. Biomarkers of tuberculosis severity and treatment effect: A directed screen of 70 host markers in a randomized clinical trial. EBioMedicine. 2017;25:112–121. doi: 10.1016/j.ebiom.2017.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Anderson S.T., Kaforou M., Brent A.J., Wright V.J., Banwell C.M., Chagaluka G., Crampin A.C., Dockrell H.M., French N., Hamilton M.S., et al. Diagnosis of childhood tuberculosis and host RNA expression in Africa. N. Engl. J. Med. 2014;370:1712–1723. doi: 10.1056/NEJMoa1303657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Leong S., Zhao Y., Joseph N.M., Hochberg N.S., Sarkar S., Pleskunas J., Hom D., Lakshminarayanan S., Horsburgh C.R., Jr., Roy G., et al. Existing blood transcriptional classifiers accurately discriminate active tuberculosis from latent infection in individuals from south India. Tuberculosis. 2018;109:41–51. doi: 10.1016/j.tube.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 77.Maertzdorf J., McEwen G., Weiner J., 3rd, Tian S., Lader E., Schriek U., Mayanja-Kizza H., Ota M., Kenneth J., Kaufmann S.H. Concise gene signature for point-of-care classification of tuberculosis. EMBO Mol. Med. 2016;8:86–95. doi: 10.15252/emmm.201505790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sambarey A., Devaprasad A., Mohan A., Ahmed A., Nayak S., Swaminathan S., D’Souza G., Jesuraj A., Dhar C., Babu S., et al. Unbiased identification of blood-based biomarkers for pulmonary tuberculosis by modeling and mining molecular interaction networks. EBioMedicine. 2017;15:112–126. doi: 10.1016/j.ebiom.2016.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Suliman S., Thompson E., Sutherland J., Weiner J., 3rd, Ota M.O.C., Shankar S., Penn-Nicholson A., Thiel B., Erasmus M., Maertzdorf J., et al. Four-Gene Pan-African Blood Signature Predicts Progression to Tuberculosis. Am. J. Respir. Crit. Care Med. 2018 doi: 10.1164/rccm.201711-2340OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sweeney T.E., Braviak L., Tato C.M., Khatri P. Genome-wide expression for diagnosis of pulmonary tuberculosis: A multicohort analysis. Lancet Respir. Med. 2016;4:213–224. doi: 10.1016/S2213-2600(16)00048-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zak D.E., Penn-Nicholson A., Scriba T.J., Thompson E., Suliman S., Amon L.M., Mahomed H., Erasmus M., Whatney W., Hussey G.D., et al. A blood RNA signature for tuberculosis disease risk: A prospective cohort study. Lancet. 2016;387:2312–2322. doi: 10.1016/S0140-6736(15)01316-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Thompson E.G., Du Y., Malherbe S.T., Shankar S., Braun J., Valvo J., Ronacher K., Tromp G., Tabb D.L., Alland D., et al. Host blood RNA signatures predict the outcome of tuberculosis treatment. Tuberculosis. 2017;107:48–58. doi: 10.1016/j.tube.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pedersen J.L., Bokil N.J., Saunders B.M. Developing new TB biomarkers, are miRNA the answer? Tuberculosis. 2019;118:101860. doi: 10.1016/j.tube.2019.101860. [DOI] [PubMed] [Google Scholar]
- 84.de Araujo L.S., Ribeiro-Alves M., Leal-Calvo T., Leung J., Durán V., Samir M., Talbot S., Tallam A., Mello F.C.Q., Geffers R., et al. Reprogramming of small noncoding RNA populations in peripheral blood reveals host biomarkers for latent and active Mycobacterium tuberculosis infection. mBio. 2019;10:e01037-19. doi: 10.1128/mBio.01037-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lyu L., Zhang X., Li C., Yang T., Wang J., Pan L., Jia H., Li Z., Sun Q., Yue L., et al. Small RNA profiles of serum exosomes derived from individuals with latent and active tuberculosis. Front. Microbiol. 2019;10:1174. doi: 10.3389/fmicb.2019.01174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ndzi E.N., Nkenfou C.N., Mekue L.M., Zentilin L., Tamgue O., Pefura E.W.Y., Kuiaté J.R., Giacca M., Ndjolo A. MicroRNA hsa-miR-29a-3p is a plasma biomarker for the differential diagnosis and monitoring of tuberculosis. Tuberculosis. 2019;114:69–76. doi: 10.1016/j.tube.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 87.Chakrabarty S., Kumar A., Raviprasad K., Mallya S., Satyamoorthy K., Chawla K. Host and MTB genome encoded miRNA markers for diagnosis of tuberculosis. Tuberculosis. 2019;116:37–43. doi: 10.1016/j.tube.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 88.Hu X., Liao S., Bai H., Wu L., Wang M., Wu Q., Zhou J., Jiao L., Chen X., Zhou Y., et al. Integrating exosomal microRNAs and electronic health data improved tuberculosis diagnosis. EBioMedicine. 2019;40:564–573. doi: 10.1016/j.ebiom.2019.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Alipoor S.D., Tabarsi P., Varahram M., Movassaghi M., Dizaji M.K., Folkerts G., Garssen J., Adcock I.M., Mortaz E. Serum exosomal miRNAs are associated with active pulmonary tuberculosis. Dis. Markers. 2019;2019:1907426. doi: 10.1155/2019/1907426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Barry S.E., Ellis M., Yang Y., Guan G., Wang X., Britton W.J., Saunders B.M. Identification of a plasma microRNA profile in untreated pulmonary tuberculosis patients that is modulated by anti-mycobacterial therapy. J. Infect. 2018;77:341–348. doi: 10.1016/j.jinf.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 91.Duffy F.J., Thompson E., Downing K., Suliman S., Mayanja-Kizza H., Boom W.H., Thiel B., Weiner J., III, Kaufmann S.H.E., Dover D., et al. A serum circulating miRNA signature for short-term risk of progression to active tuberculosis among household contacts. Front. Immunol. 2018;9:661. doi: 10.3389/fimmu.2018.00661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang C., Yang S., Liu C.M., Jiang T.T., Chen Z.L., Tu H.H., Mao L.G., Li Z.J., Li J.C. Screening and identification of four serum miRNAs as novel potential biomarkers for cured pulmonary tuberculosis. Tuberculosis. 2018;108:26–34. doi: 10.1016/j.tube.2017.08.010. [DOI] [PubMed] [Google Scholar]
- 93.Cui J.Y., Liang H.W., Pan X.L., Li D., Jiao N., Liu Y.H., Fu J., He X.Y., Sun G.X., Zhang C.L., et al. Characterization of a novel panel of plasma microRNAs that discriminates between Mycobacterium tuberculosis infection and healthy individuals. PLoS ONE. 2017;12:e0184113. doi: 10.1371/journal.pone.0184113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang C., Liu C.M., Wei L.L., Shi L.Y., Pan Z.F., Mao L.G., Wan X.C., Ping Z.P., Jiang T.T., Chen Z.L., et al. A Group of novel serum diagnostic biomarkers for multidrug-resistant tuberculosis by iTRAQ-2D LC-MS/MS and Solexa sequencing. Int. J. Biol. Sci. 2016;12:246–256. doi: 10.7150/ijbs.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wagh V., Urhekar A., Modi D. Levels of microRNA miR-16 and miR-155 are altered in serum of patients with tuberculosis and associate with responses to therapy. Tuberculosis. 2017;102:24–30. doi: 10.1016/j.tube.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 96.Zheng M.L., Zhou N.K., Luo C.H. MiRNA-155 and miRNA-132 as potential diagnostic biomarkers for pulmonary tuberculosis: A preliminary study. Microb. Pathog. 2016;100:78–83. doi: 10.1016/j.micpath.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 97.Xin H., Yang Y., Liu J., Li X., Li M., Feng B., Li Z., Zhang H., Li H., Shen F., et al. Association between tuberculosis and circulating microRNA hsa-let-7b and hsa-miR-30b: A pilot study in a Chinese population. Tuberculosis. 2016;99:63–69. doi: 10.1016/j.tube.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 98.Xu Z., Zhou A., Ni J., Zhang Q., Wang Y., Lu J., Wu W., Karakousis P.C., Lu S., Yao Y. Differential expression of miRNAs and their relation to active tuberculosis. Tuberculosis. 2015;95:395–403. doi: 10.1016/j.tube.2015.02.043. [DOI] [PubMed] [Google Scholar]
- 99.Honeyborne I., Lipman M.C., Eckold C., Evangelopoulos D., Gillespie S.H., Pym A., McHugh T.D. Effective anti-tuberculosis therapy correlates with plasma small RNA. Eur. Respir. J. 2015;45:1741–1744. doi: 10.1183/09031936.00221214. [DOI] [PubMed] [Google Scholar]
- 100.Latorre I., Leidinger P., Backes C., Domínguez J., de Souza-Galvão M.L., Maldonado J., Prat C., Ruiz-Manzano J., Sánchez F., Casas I., et al. A novel whole-blood miRNA signature for a rapid diagnosis of pulmonary tuberculosis. Eur. Respir. J. 2015;45:1173–1176. doi: 10.1183/09031936.00221514. [DOI] [PubMed] [Google Scholar]
- 101.Zhang C., Wang Q., Xi X., Jiao J., Xu W., Huang J., Lai Z. High serum miR-183 level is associated with the bioactivity of macrophage derived from tuberculosis patients. Int. J. Clin. Exp. Pathol. 2015;8:655–659. [PMC free article] [PubMed] [Google Scholar]
- 102.Zhang H., Sun Z., Wei W., Liu Z., Fleming J., Zhang S., Lin N., Wang M., Chen M., Xu Y., et al. Identification of Serum microRNA Biomarkers for Tuberculosis Using RNA-seq. PLoS ONE. 2014;9:e88909. doi: 10.1371/journal.pone.0088909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Abd-El-Fattah A.A., Sadik N.A., Shaker O.G., Aboulftouh M.L. Differential microRNAs expression in serum of patients with lung cancer, pulmonary tuberculosis, and pneumonia. Cell Biochem. Biophys. 2013;67:875–884. doi: 10.1007/s12013-013-9575-y. [DOI] [PubMed] [Google Scholar]
- 104.Zhang X., Guo J., Fan S., Li Y., Wei L., Yang X., Jiang T., Chen Z., Wang C., Liu J., et al. Screening and identification of six serum microRNAs as novel potential combination biomarkers for pulmonary tuberculosis diagnosis. PLoS ONE. 2013;8:e81076. doi: 10.1371/journal.pone.0081076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Miotto P., Mwangoka G., Valente I.C., Norbis L., Sotgiu G., Bosu R., Ambrosi A., Codecasa L.R., Goletti D., Matteelli A., et al. MiRNA signatures in sera of patients with active pulmonary tuberculosis. PLoS ONE. 2013;8:e80149. doi: 10.1371/journal.pone.0080149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Maertzdorf J., Weiner J., Mollenkopf H.J., TBornotTB Network. Bauer T., Prasse A., Müller-Quernheim J., Kaufmann S.H. Common patterns and disease-related signatures in tuberculosis and sarcoidosis. Proc. Natl. Acad. Sci. USA. 2012;109:7853–7858. doi: 10.1073/pnas.1121072109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Qi Y., Cui L., Ge Y., Shi Z., Zhao K., Guo X., Yang D., Yu H., Cui L., Shan Y., et al. Altered serum microRNAs as biomarkers for the early diagnosis of pulmonary tuberculosis infection. BMC Infect. Dis. 2012;12:384. doi: 10.1186/1471-2334-12-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Fu Y., Yi Z., Wu X., Li J., Xu F. Circulating microRNAs in patients with active pulmonary tuberculosis. J. Clin. Microbiol. 2011;49:4246–4251. doi: 10.1128/JCM.05459-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lin Y., Zhang Y., Yu H., Tian R., Wang G., Li F. Identification of unique key genes and miRNAs in latent tuberculosis infection by network analysis. Mol. Immunol. 2019;112:103–114. doi: 10.1016/j.molimm.2019.04.032. [DOI] [PubMed] [Google Scholar]
- 110.Zhang X., Zhu M., Hu X. Integrated miRNA and mRNA expression profiling to identify mRNA targets of dysregulated miRNAs in pulmonary tuberculosis. Epigenomics. 2018;10:1051–1069. doi: 10.2217/epi-2018-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.van Rensburg I.C., du Toit L., Walzl G., du Plessis N., Loxton A.G. Decreased neutrophil–associated miRNA and increased B-cell associated miRNA expression during tuberculosis. Gene. 2018;655:35–41. doi: 10.1016/j.gene.2018.02.052. [DOI] [PubMed] [Google Scholar]
- 112.Corral-Fernández N.E., Cortes-García J.D., Bruno R.S., Romano-Moreno S., Medellín-Garibay S.E., Magaña-Aquino M., Salazar-González R.A., González-Amaro R., Portales-Pérez D.P. Analysis of transcription factors, microRNAs and cytokines involved in T lymphocyte differentiation in patients with tuberculosis after directly observed treatment short-course. Tuberculosis. 2017;105:1–8. doi: 10.1016/j.tube.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 113.Spinelli S.V., Fernández R.D.V., Zoff L., Bongiovanni B., Díaz A., D’Attilio L., Santucci N., Alvarez T., Marchesini M.M., Bogue C., et al. MiR-30c is specifically repressed in patients with active pulmonary tuberculosis. Tuberculosis. 2017;105:73–79. doi: 10.1016/j.tube.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 114.Pan D., Pan M., Xu Y.M. Mir-29a expressions in peripheral blood mononuclear cell and cerebrospinal fluid: Diagnostic value in patients with pediatric tuberculous meningitis. Brain Res. Bull. 2017;130:231–235. doi: 10.1016/j.brainresbull.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 115.Zhou M., Yu G., Yang X., Zhu C., Zhang Z., Zhan X. Circulating microRNAs as biomarkers for the early diagnosis of childhood tuberculosis infection. Mol. Med. Rep. 2016;13:4620–4626. doi: 10.3892/mmr.2016.5097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zheng L., Leung E., Lee N., Lui G., To K.F., Chan R.C., Ip M. Differential microRNA expression in human macrophages with Mycobacterium tuberculosis infection of Beijing/W and Non-Beijing/W strain types. PLoS ONE. 2015;10:e0126018. doi: 10.1371/journal.pone.0126018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wang J.X., Xu J., Han Y.F., Zhu Y.B., Zhang W.J. Diagnostic values of microRNA-31 in peripheral blood mononuclear cells for pediatric pulmonary tuberculosis in Chinese patients. Genet. Mol. Res. 2015;14:17235–17243. doi: 10.4238/2015.December.16.23. [DOI] [PubMed] [Google Scholar]
- 118.Fu Y., Yi Z., Li J., Li R. Deregulated microRNAs in CD4+ T cells from individuals with latent tuberculosis versus active tuberculosis. J. Cell. Mol. Med. 2014;18:503–513. doi: 10.1111/jcmm.12205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Spinelli S.V., Diaz A., D’Attilio L., Marchesini M.M., Bogue C., Bay M.L., Bottasso O.A. Altered microRNA expression levels in mononuclear cells of patients with pulmonary and pleural tuberculosis and their relation with components of the immune response. Mol. Immunol. 2013;53:265–269. doi: 10.1016/j.molimm.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 120.Wang C., Yang S., Sun G., Tang X., Lu S., Neyrolles O., Gao Q. Comparative miRNA expression profiles in individuals with latent and active tuberculosis. PLoS ONE. 2011;6:e25832. doi: 10.1371/journal.pone.0025832. [DOI] [PMC free article] [PubMed] [Google Scholar]