Abstract
Simple Summary
Cancer stem cells (CSCs) have been shown to be the main cause of therapy resistance and cancer recurrence. An analysis of their biological properties has revealed that CSCs have a particular metabolism that differs from non-CSCs to maintain their stemness properties. In this review, we analyze the flexible metabolic mechanisms of CSCs and highlight the new therapeutics that target CSC metabolism.
Abstract
Numerous findings have indicated that CSCs, which are present at a low frequency inside primary tumors, are the main cause of therapy resistance and cancer recurrence. Although various therapeutic methods targeting CSCs have been attempted for eliminating cancer cells completely, the complicated characteristics of CSCs have hampered such attempts. In analyzing the biological properties of CSCs, it was revealed that CSCs have a peculiar metabolism that is distinct from non-CSCs to maintain their stemness properties. The CSC metabolism involves not only the catabolic and anabolic pathways, but also intracellular signaling, gene expression, and redox balance. In addition, CSCs can reprogram their metabolism to flexibly respond to environmental changes. In this review, we focus on the flexible metabolic mechanisms of CSCs, and highlight the new therapeutics that target CSC metabolism.
Keywords: cancer stem cells, glucose metabolism, mitochondrial metabolism, redox homeostasis, ROS, metastasis
1. Introduction
Over the years, as the biological properties of cancers become clearer, various therapies have been developed to target them. For example, therapeutic agents that target the vigorous cell growth of cancer cells, DNA replication inhibitors, and cell division inhibitors have shown dramatic effects for tumor regression [1,2,3,4,5]. However, while many therapeutic agents have transient effects, tumors often become refractory and repopulate by acquiring treatment resistance [1,3,5]. Cancer stem cells (CSCs) or tumor-initiating cells, which represent a small population of cells existing inside cancer tissues, are responsible for treatment resistance and the recurrence of cancers [6,7,8,9,10,11,12]. Since the discovery of CSCs in leukemia cells about 30 years ago [7], CSC research has been conducted in various hematological and solid tumors [12]. CSCs can generate cancer cells with different characteristics by dividing unevenly while maintaining a poorly differentiated state [9,11]. It is considered that such pluripotency and self-renewal ability are the reasons for the heterogeneity in cancer tissues, and the cause of treatment resistance and recurrence [8].
A number of molecular markers have been identified to isolate CSCs from primary tumors and experimental tumor models. Although there are molecular markers that are common between tumors of various tissues, such as CD44 and aldehyde dehydrogenase (ALDH), most CSCs express tissue-specific molecular markers [12]. However, emerging evidence suggests that the phenotype of CSCs originating from a tissue is not always constant, but changes in a context-dependent manner. For example, it has been shown that multiple CSC populations with different growth and metastatic traits are present simultaneously within the same tumor [13,14]. At present, the metabolic mechanism of cancer cells is attracting attention as a predisposing factor underlying the diversity of CSCs [15,16,17,18,19,20]. One hundred years ago, when it was discovered that the glucose metabolism of cancer cells was different from that of normal cells, the quantities and categories of metabolites that could be analyzed were limited [21]. However, with the progress of metabolomics and isotope tracing technology in the recent years, it is now possible to investigate not only changes in quantity, but also the details of the flux of metabolites and metabolic heterogeneities within tumors [22,23]. In this review, we describe the details of tumor metabolism revealed in recent studies and discuss the therapeutic potential of the CSC-specific metabolic machinery.
2. Tumor Metabolism
The specialized metabolism of tumors was first revealed by Warburg et al. in 1927 [21]. They discovered that cancer cells have a high dependence on glucose, and this property of cancer cells is still being applied in tumor imaging techniques, such as positron emission tomography [24,25]. Over the years, cancer metabolism and the Warburg effect have been treated synonymously, but recent studies have revealed that the Warburg effect is only one aspect of the metabolic mechanisms of tumors [26,27,28,29]. Each tumor activates different metabolic pathways in response to gene mutations and changes in the microenvironment [26,27,28,29].
2.1. Glucose Metabolism
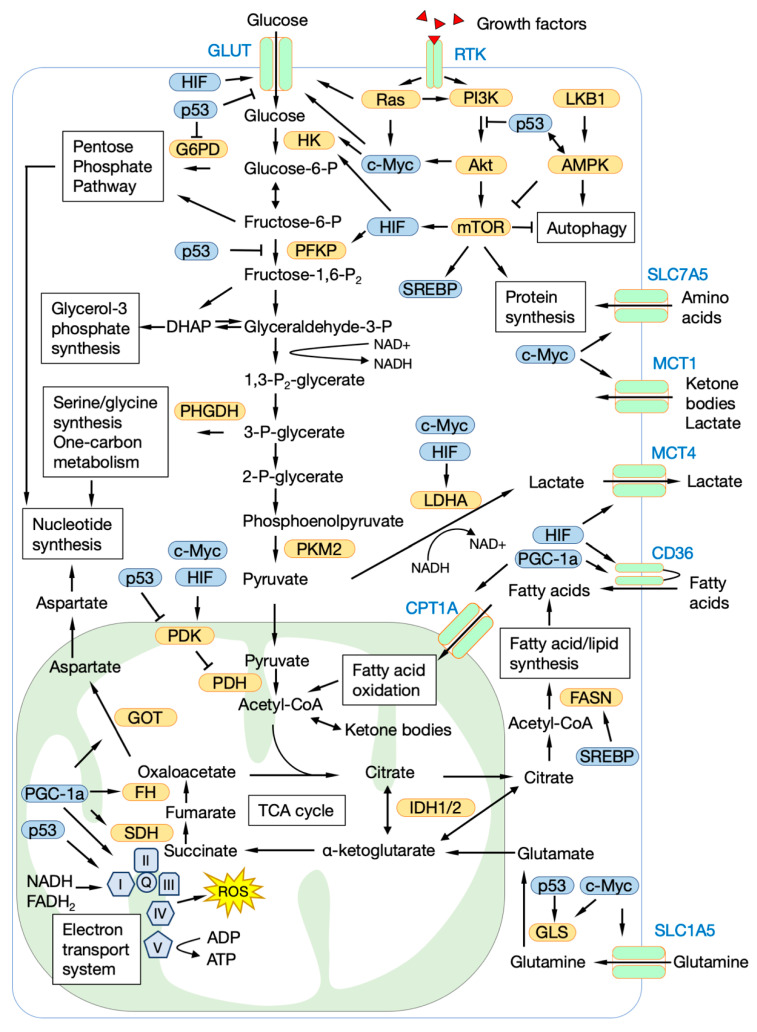
In typical glycolysis, 1 mole of glucose is converted to 2 moles of pyruvate by 10 enzymes. Under normal oxygen conditions, the 2 moles of pyruvate are completely oxidized through the mitochondrial tricarboxylic acid (TCA) cycle, and 30 or 32 moles of ATP are produced by the electron transport system (ETS). However, even when there is sufficient oxygen and the mitochondria are functioning normally, cancer cells excrete most of the pyruvate as lactate [21,24,25]. Although this is energetically inefficient, it can be advantageous for cancer cells, because glycolytic intermediates, which are generated in the pre-stage of lactate secretion, are linked to various other metabolic pathways that produce biogenic substances required for cell growth (Figure 1). The pentose phosphate pathway (PPP) is an important pathway for supplying ribose, which is a material for nucleic acids, and NADPH, which plays an important role in maintaining intracellular redox balance [30]. Dihydroxyacetone phosphate, which is produced by the degradation of fructose bisphosphate, is reduced to glycerol-3 phosphate, and becomes a material for cell membranes [22]. 3-Phosphoglycerate is metabolized to serine, then undergoes one-carbon metabolism to become a material for nucleic acids and glutathione (GSH), or is metabolized to S-adenosylmethionine, which is a methyl group donor for proteins and DNA [31,32]. To accelerate glycolysis, cancer cells convert NADH generated in the metabolic process into NAD+ by using it for the reduction of pyruvate without transporting it to the ETS [24]. Lactate produced by the reduction of pyruvate is excreted extracellularly, and it becomes an energy source for other cancer cells and stromal cells [33,34]. Lactate also promotes the metastasis of cancer cells and suppresses the function of immune cells by acidifying the tumor microenvironment [33,34,35].
Figure 1.
The central carbon metabolism map in cancer cells. GLUT, glucose transporter; RTK, receptor tyrosine kinase; MCT, monocarboxylate transporter; SLC7A5, solute carrier family 7 member 5; SLC1A5, solute carrier family 1 member 5; HK, hexokinase; G6PD, glucose-6-phosphate dehydrogenase; PFKP, phosphofructokinase platelet; PHGDH, phosphoglycerate dehydrogenase; PKM2, pyruvate kinase M2; LDHA, lactate dehydrogenase A; PI3K, phosphatidylinositol-3 kinase; LKB1, Liver kinase B1; AMPK, AMP-activated protein kinase; mTOR, mammalian target of rapamycin; FASN, fatty acid synthase; GLS, glutaminase; PDK1, pyruvate dehydrogenase kinase 1; PDH, pyruvate dehydrogenase; IDH, isocitrate dehydrogenase; SDH, succinate dehydrogenase; FH, fumarate hydratase; GOT, glutamic-oxaloacetic transaminase; I-X, electron transport chain complex I-X; PGC-1a, peroxisome proliferator-activated receptor gamma coactivator 1-alpha; HIF, hypoxia inducible factor; SREBP, sterol regulatory element binding transcription factor.
Many transporters and enzymes involve in glucose uptake and metabolism, e.g., glucose transporters (GLUTs), monocarboxylate transporters, hexokinase 2, lactate dehydrogenase A, and pyruvate dehydrogenase kinase 1, and transcription factors that regulate their expression, e.g., hypoxia inducible factor-1 alpha (HIF-1α) and c-myc, are overexpressed in various cancers [36,37,38,39,40,41,42]. Similarly, it is well-known that in various cancers, gene mutations and dysregulation occur in Kras/mitogen-activated protein kinase (MAPK) and phosphatidylinositol-3 kinase (PI3K)/Akt/mTOR, which are signal transduction pathways related to glycolysis control [26,43]. It is also known that the tumor suppressor gene p53 has a role in suppressing glycolysis by inhibiting GLUTs expression and phosphofructokinase activity [44,45,46,47,48,49], whereas mutant p53 conversely promotes glucose uptake and glycolysis [48,49].
2.2. Mitochondrial Metabolism and Oxidative Phosphorylation
Similar to glycolysis, various metabolites produced by mitochondrial metabolism, including the TCA cycle, are required for building cellular components and energy production [50,51,52]. Acetyl-CoA produced by the degradation of citrate is a material for fatty acid synthesis and an acetyl group donor for the histone acetylation reaction [50,51,52]. Oxaloacetate is converted to aspartate by glutamate-oxaloacetate transaminase, and the aspartate also serves as a material for nucleic acids [53]. The main fuel of the TCA cycle is acetyl-CoA that is derived from glucose, but when there are insufficient amounts of available glucose or under conditions of hypoxia, glutamine, other branched-chain amino acids, and acetyl-CoA produced by the β-oxidation of fatty acids are used as fuel in the TCA cycle [28,37,54].
Compared to normal tissues, glycolysis is activated in most cancer cells, but the cancer cells still produce the ATP required for growth and survival via the mitochondrial oxidative phosphorylation (OXPHOS) system [55]. The ETS reaction is essential for generating the proton-driving force necessary for synthesizing large amounts of ATP, and at the same time, the reaction causes the production of reactive oxygen species (ROS), which are harmful to cells. Therefore, mitochondria are equipped with numerous ROS defense mechanisms, and many of them are upregulated in cancer cells [50,51,52]. While excessive amounts of ROS are harmful to cancer cells, it is known that an appropriate amount of ROS plays an important role in signal transduction and the differentiation of cancer cells [52,56]. The various effects of ROS on the phenotype of CSCs will be described later.
Peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α), which plays a central role in mitochondrial biosynthesis, is overexpressed in various cancers [57,58]. PGC-1α has been reported to induce cancer growth and distant metastasis in a mitochondrial metabolism-dependent manner [59,60]. c-Myc is known to be involved in mitochondrial biosynthesis and the regulation of the expression of glycolysis-related genes [61]. It has been shown that cancer cells overexpressing c-myc have increased mitochondrial masses and activated OXPHOS [61,62].
It has been reported that mutations of genes encoding enzymes involved in mitochondrial metabolism affect the phenotype of cancer cells. A mutation of isocitrate dehydrogenase 1 and 2 found in glioma produces D-2-hydroxy-glutarate from α-ketoglutarate, which results in the inhibition of DNA and histone methyltransferases, and causes epigenetic dysregulation [55,63,64]. Mutations in succinate dehydrogenase and fumarate hydratase inhibit prolyl hydroxylase activity by accumulating succinate and fumarate in cells, and suppress HIF-1α degradation [55,65].
2.3. Amino Acids, Lipids and Other Fuels
Glucose is a raw material that makes up various biological substances, but it contains only carbon, hydrogen, and oxygen. Since glutamine plays an important role as a source of nitrogen in amino acids and nucleic acids, it is known that many cancer cells have a high dependence on glutamine [66,67,68,69,70]. Glutamine uptake and metabolism in cancer cells is regulated by PI3K, Kras, and c-myc [26,43,66,67,71,72,73,74,75]. Tryptophan is an important amino acid for the activation of immune cells, but cancer cells overexpress the tryptophan-metabolizing enzyme IDO, which suppresses immune cell function by depleting tryptophan in the tumor microenvironment [66]. In addition, it has been reported that kynurenine produced by the catabolism of tryptophan enhances the resistance of CSCs to radiation [76]. Acute lymphocytic leukemia is known to have a high dependence on asparagine [66,67,77]. The treatment method of using L-asparaginase to degrade and deplete asparagine in the tumor microenvironment has shown a high therapeutic effect on acute lymphocytic leukemia in children [66,67,77,78].
A large amount of lipids, a component of biological membranes, is required for the rapid cell division of cancer cells. Therefore, the overexpression of fatty acid synthetase and sterol regulatory element-binding protein, which are involved in lipid and cholesterol synthesis, is observed in cancer cells [79]. In addition, it has been reported that the CD36 receptor, which regulates the uptake of lipids, promotes the growth and metastasis of cancer cells [80,81,82]. Synthesized or incorporated lipids are used not only as a component for biological membranes, but also for energy production by fatty acid oxidation (FAO) when other nutrients are depleted [79,83].
It has been suggested that common hexoses other than glucose, such as galactose and fructose, are also involved in the growth and metastasis of cancer cells. Galactose has been shown to induce OXPHOS-dependent metabolism and suppress the growth and metastasis of cancer cells [84,85,86]. On the other hand, fructose has been shown to promote liver metastasis in colon cancer and breast cancer [87]. It has also been shown that aldolase B involved in fructose metabolism promotes the liver metastasis of cancer cells but does not promote metastasis to other organs [87].
2.4. Tumor Microenvironments
Stromal cells surrounding tumors, such as endothelial cells, fibroblasts, adipocytes, and immune cells, also support tumor survival and growth [27,55]. It has been shown that these normal cells regulate the growth of cancer cells by secreting growth factors and cytokines, and they actively exchange metabolites, such as lactate and ketone bodies that are generated by aerobic glycolysis, with cancer cells [27,55,88]. Adipocytes also support the survival of cancer cells by supplying fatty acids and glutamine to the tumor microenvironment [77,89].
It is considered that the supply of oxygen and nutrients from existing blood vessels to cancer cells is insufficient for the rapid growth of tumors. Hypoxia induces the reprogramming of glycolysis-dependent metabolism in cancer cells by stabilizing HIFs and increasing the expression of glycolysis-associated genes [37,40]. On the other hand, the chronic deprivation of nutrients induces the metabolism of cancer cells to switch from anabolic to catabolic. For example, metabolic stress activates the p53 and, Liver kinase B1-AMPK cascade, and induces OXPHOS, FAO, and autophagy [90,91]. Although these tumor suppressor genes were originally believed to function in suppressing the cell growth of cancer cells, they are now considered to have a function in preventing cancer cells from undergoing apoptosis during periods of energy deficiency [90,91]. Therefore, it is considered that cancer cells with mutations in these tumor suppressor genes are highly susceptible to the inhibition of specific metabolism pathways and the direct restriction of calories [92,93,94].
Interactions with the extracellular matrix also affect the metabolism of cancer cells. For example, hyaluronic acids in the extracellular matrix induce glycolysis metabolism and epithelial-mesenchymal transition (EMT) in cancer cells through CD44 and receptor tyrosine kinase [95,96,97,98]. On the other hand, it has been shown that mitochondria-related genes, such as the gene for PGC-1α, are upregulated, and OXPHOS is activated in cancer cells that are detached from the extracellular matrix and circulate in blood [60]. The antioxidant system is enhanced in circulating cancer cells in order to remove the increased amounts of ROS resulting from the activation of OXPHOS [99]. In addition, to prevent cell death due to the ROS, some cancer cells create a hypoxic environment by clustering, and induce mitophagy and glycolytic metabolism [84]. Thus, the metabolic reprogramming of cancer cells found in the blood circulation plays an important role in determining the metastatic target and the formation of metastatic foci [100,101,102].
3. The Concept of CSCs
Numerous studies have suggested that CSCs are responsible for treatment resistance and cancer recurrence and metastasis [6,7,8,9,10,11,12]. CSCs show very similar phenotypes to normal stem cells, suggesting that there are two possibilities for the development of CSCs, i.e., they are produced due to oncogenic mutations in normal stem cells or progenitor cells with stem cell characteristics, or they are produced when differentiated cancer cells acquire stem cell traits, just like how induced pluripotent stem cells are generated [10]. Like normal stem cells, CSCs usually undergo very slow cell division or remain quiescent in the G0 phase, so they are highly resistant to common anti-cancer drugs that target the vigorous growth of cancer cells [8,10]. In addition, it has been suggested that CSCs contribute to the formation of the heterogeneity in tumors by producing progenitor cells of different differentiation levels via asymmetric division [8,9,10].
There are various methods for identifying and examining CSCs, including: methods for examining the expression of a specific cell surface marker; methods for examining drug resistance ability, such as the function of ABC transporters; methods for measuring specific enzyme activities, such as endogenous protease or ALDH; methods for examining in vitro spheroid-forming ability; and methods for examining tumorigenicity using mouse models [12,103].
CSC traits are controlled by various pluripotent transcription factors, including Oct4, Sox2, Nanog, Klf4, and c-myc, and their upstream signal transduction pathways, including the Wnt, Notch, Hedgehog, Ras/MAPK, Jak/Stat, and PI3K/Akt/mTOR pathways, as well as the characteristics of the complex microenvironment surrounding the tumor, including conditions of hypoxia, stromal cells, growth factors, and the extracellular matrix [6,11,12,97]. In addition to these, it has been revealed in recent years that CSC-specific metabolic mechanisms play an important role in exerting stem cell traits, and they have been attracting attention as new CSC-specific therapeutic targets [15,16,17,18,19,20].
4. Metabolism of CSCs
Attempts to identify and inhibit CSC-specific metabolic traits could well lead to the development of therapeutics to eradicate CSCs. To achieve this goal, many researchers are investigating the metabolic phenotypes of CSCs derived from various tissues [15,16,17,18,19,20]. However, there are conflicting hypotheses about whether CSCs depend on glycolysis, mitochondrial metabolism, or other metabolic pathways for maintaining stem cell traits [17,18,20]. In addition, CSC-specific metabolism is responsible for maintaining intracellular redox homeostasis by regulating metabolic balance and synthesizing antioxidants [17,18].
4.1. Glycolysis in CSCs
Previous studies have revealed that somatic stem cells, embryonic stem cells, and induced pluripotent stem cells have increased glycolysis activity in order to maintain their stem cell traits [104,105,106,107]. Similarly, in CSCs, such as in breast cancer [108,109,110], lung cancer [111], hepatocellular carcinoma [112,113], glioma [114], ovarian cancer [115], prostate cancer [116], and nasopharyngeal carcinoma [117,118], it has been reported that glycolysis plays an important role in acquiring stem cell properties. For example, CSCs from side-population cells and spheroids overexpress various genes for glycolysis-related factors, such as GLUTs, monocarboxylate transporters, hexokinases, and pyruvate dehydrogenase kinase 1, when compared to non-CSCs [108,110,111,113,118]. In addition, the suppression of the expression or functional inhibition of those glycolysis-related genes markedly reduces the CSC population and attenuates the tumor growth in mouse models [108,109,111,114]. Moreover, the fact that most of the glycolysis-related genes are regulated by HIF-1α could explain why hypoxia stimulation induces CSC traits in differentiated cancer cells in many tumors [114,119,120,121].
Glycolysis-dependent metabolic reprogramming also plays an important role in treatment resistance and metastatic ability, which are important hallmarks of CSCs. Several studies have shown that the inhibition of the glycolysis pathway suppresses the expression of ABC transporter genes in CSCs [122,123]. Nakano et al. have shown that metabolic reprogramming from glycolysis to OXPHOS suppresses the expression of ABC transporter genes by inhibiting the acetylation modification of histone H3 K27 near the promoter of ABC transporter genes [122]. Interestingly, the activation of OXPHOS suppressed the expression of the ABC transporter genes in cells with wild-type p53, while it increased the expression of ABC transporter genes in cancer cells with mutant-p53 [123].
Snail, a key mediator of EMT in cancer cells, is known to induce glycolysis-dependent metabolism by suppressing the expression of the gluconeogenesis-related gene FBP1 in breast cancer [109,124]. On the other hand, recent studies have shown that Snail can switch the metabolic pathway of glucose to PPP by suppressing the expression of phosphofructokinase, platelet [125], suggesting that the role of Snail in glycolysis varies depending on the situation. Moreover, it has been suggested that the switch from OXPHOS to glycolysis-dependent metabolism is required for EMT in several types of cancer cells and for liver metastasis in breast cancer and colorectal cancer cells [87,102,126,127].
4.2. Mitochondrial OXPHOS in CSCs
Previous studies have reported that the mitochondria OXPHOS is activated in CSCs in breast cancer [62], lung cancer [128], glioma [129], ovarian cancer [130], pancreatic cancer [131,132], and leukemia [133]. CD133+ cells in pancreatic cancer and glioma have significantly increased gene expression levels of enzymes involved in the TCA cycle and OXPHOS when compared to CD133- cells [129,132]. In many OXPHOS-dependent CSCs, the upregulation of mitochondrial biosynthesis-related genes was observed along with an increase in the numbers and masses of the mitochondria, an increase in the membrane potential of the mitochondria, and the elongation of cristae [62,128,129,130,131,132]. It has been suggested that the characteristics of mitochondria common to CSCs may serve as a new CSC selection marker [134,135,136,137]. Lee et al. have demonstrated that c-myc and mitochondrial protein Mcl1 cooperate to activate OXPHOS in breast cancer CSCs, thereby promoting drug resistance and tumor formation [62]. FAO has also been shown to activate OXPHOS in CSCs by supplying acetyl-CoA in the TCA cycle [89,130,138]. Han et al. demonstrated that carnitine palmitoyltransferase 1A and 2, which are FAO rate-limiting enzymes, enhance the tolerance to radiation of breast cancer cells by enhancing ATP production by FAO [138]. Furthermore, Citrate, which is generated from FAO-derived acetyl-CoA, is oxidized to α-ketoglutarate or pyruvate in cytoplasm and produces cytosolic NADPH [83]. Since PPP-derived NADPH is reduced under glucose-deficient conditions, FAO activation in CSCs can compensate for the lack of NADPH and inhibit ROS-induced apoptosis [83,139].
Whether cancer cells can survive while circulating in the blood is an important factor that determines the success or failure of distant metastasis. Many studies have reported that OXPHOS is activated in circulating cancer cells with the overexpression of PGC-1α [60,100,101]. However, it has been suggested that PGC-1α promotes lung and bone metastasis in breast cancer [59,60,100,101], while suppressing liver metastasis [59].
4.3. Metabolic Heterogeneity in CSCs
Even when targeting CSCs derived from the same type of tumor, the observed metabolic phenotypes of CSCs differ in each experiment. Several studies have shown that differences in in vitro and in vivo microenvironments have a significant impact on the metabolic phenotypes of cancer cells [140,141]. The in vivo interactions with the extracellular matrix and the exchange of metabolites and signal transduction substances with stromal cells are important factors for maintaining stem cell traits [6,11,120]. When selecting CSCs from tumors, flow cytometry is often used to analyze the expression of cell surface or endogenous markers, such as CD44, CD133, and ALDH [12]. When cancer cells are taken out from a complicated microenvironment, it is difficult to think that those cancer cells can maintain the metabolic state originally exhibited in the tumor for a long period of time. In addition, conventional cell culture systems use culture media that contain nutrients, such as glucose and glutamine, at levels that exceed those found in physiological conditions, so there is a risk that cancer cells may shift to a metabolic system that depends on those nutrients [140,142]. Therefore, to more accurately elucidate the metabolism of CSCs, it may be necessary to perform quick analyses in fresh cells immediately after they are taken from the body, or to culture CSCs under conditions close to the original environment. Although it is difficult to reproduce the original tumor microenvironment in vitro, organoid culture technology may enable the development of an effective method to reproduce the heterogeneous structure of tumors [143,144,145].
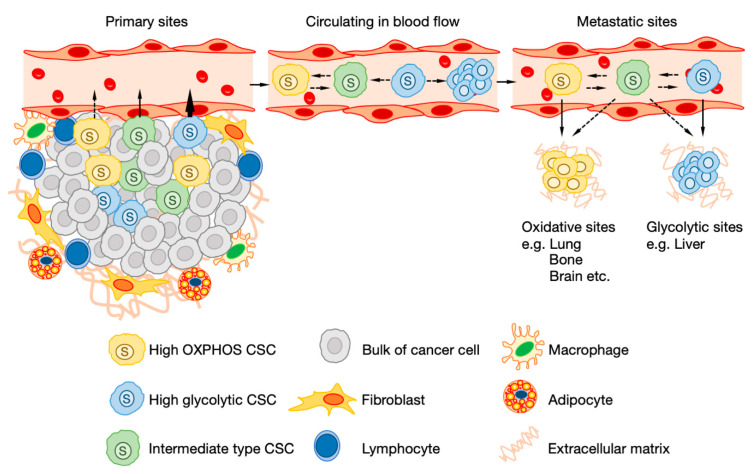
Recent studies have suggested that CSCs contained in the same tumor have non-uniform metabolic phenotypes, and that CSCs with different metabolic phenotypes can coexist (Figure 2) [13,14,132,146]. For example, since many CSCs of pancreatic cancer depend on OXPHOS, OXPHOS-dependent CSCs die when the mitochondria are inhibited [132]. However, in some CSCs, both OXPHOS and glycolysis are activated, so even if OXPHOS is inhibited, glycolysis can be enhanced, and the CSCs can avoid cell death [132]. Luo et al. also showed that there are two types of CSCs in breast cancer, i.e., CD44-positive CSCs and ALDH-positive CSCs [14]. It was shown that in CD44-positive CSCs, the cell cycle is at a quiescent stage and glycolysis is activated, while in ALDH-positive CSCs, cell division proceeds and OXPHOS is activated [13,14]. These results indicate that CSCs do not solely depend on either the glycolysis pathway or the OXPHOS pathway but can flexibly regulate the balance between the strengths and weaknesses of each metabolic pathway depending on the surrounding environment and the stage of differentiation.
Figure 2.
The metabolic heterogeneity and flexibility of cancer stem cells (CSCs). The metabolic phenotypes of each CSC are very heterogeneous even within the same tumor. High glycolytic CSCs have more invasive ability compared to high oxidative phosphorylation (OXPHOS) CSCs. Circulating cancer stem cells are dependent on OXPHOS or have a higher metabolic capacity. Glycolytic CSCs reprogram metabolism to OXPHOS-dependent manner or maintains glycolytic metabolism by forming clusters during circulating. Eventually, CSCs metastasize to organs that are compatible with metabolic phenotypes.
4.4. Redox Homeostasis in CSCs
To eliminate ROS caused by various internal and external factors, such as increased OXPHOS, radiotherapy, and chemotherapy, CSCs have a potent antioxidant system [14,18,147,148]. The transcription factor Nrf2 is known to be a master regulator of redox homeostasis in normal stem cells and CSCs [14,18,148]. Under basic conditions, ubiquitination by Keap1 suppresses the expression of Nrf2, but ROS stimulation inhibits the interaction between Keap1 and Nrf2, which activates the Nrf2-dependent antioxidant system [149]. In addition, oncogenes, such as Kras and c-myc, have been shown to increase the transcriptional levels of Nrf2 [56,150]. Nrf2 both directly and indirectly regulates the expression of genes related to antioxidant defense, such as the genes for superoxide dismutase, GSH peroxidase, glutamate-cysteine ligase catalytic subunit, glutamate-cysteine ligase modifier subunit, and thioredoxin (Trx), and genes related to drug metabolism, such as the genes for ALDH and ABC transporters [148,149,150,151]. The cysteine/glutamate antiporter (System Xc-) consisting of xCT and 4F2hc plays an important role in the synthesis of GSH, a major intracellular antioxidant [152]. Nrf2 has been shown to promote GSH synthesis by directly controlling the transcription of xCT [153,154]. In addition to activating the antioxidant system, Nrf2 regulates redox homeostasis by reprogramming the metabolism of CSCs [155,156,157,158]. Chang et al. demonstrated that the overexpression of Nrf2 weakens OXPHOS activity and reduces ROS production by inducing the expression of glycolysis-related and non-oxidative PPP-related genes [155]. ROS inhibition by metabolic reprogramming is also observed in other CSCs. It has been shown that the NANOG gene suppresses OXPHOS-derived ROS generation and induces CSC traits by changing the metabolic mechanism of liver cancer CSCs in a glycolysis- and FAO-dependent manner [112]. In addition, Liu et al. have demonstrated that the selective mitophagy of dysfunctional mitochondria induces NANOG gene expression by suppressing p53 gene expression [159].
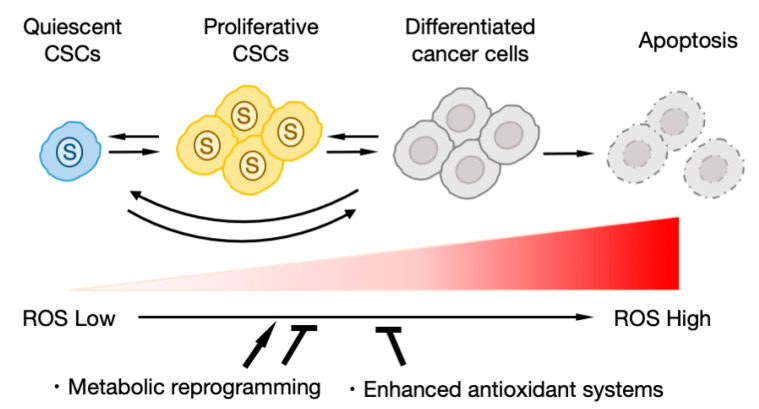
In contrast, it has been suggested that ROS may promote CSC proliferation and metabolic reprogramming in some tumors [56,62,114,160,161]. Lee et al. demonstrated that c-Myc/Mcl1-overexpressing breast cancer CSCs generate ROS upon the activation of OXPHOS, and that the stabilization of HIF-1α by accumulating ROS is important for maintaining CSC traits [62]. Similarly, in glioma CSCs, the overexpression of HIF-1α associated with increased ROS production was shown to induce CSC traits [114]. Moreover, common to both experiments, the removal of ROS or the suppression of HIF-1α was shown to significantly inhibit CSC traits [62,114]. It is also known that ROS regulate signal transduction that is important for cell proliferation and survival, such as the PI3K/Akt/mTOR, MAPK cascade, Notch, and Wnt/b-catenin pathways [56,161].
On the other hand, it has been suggested that the role of ROS differ depending on the stage of cell differentiation (Figure 3). Normal hematopoietic stem cells (HSCs) in a dormant state have reduced ROS production due to the activation of glycolysis and suppression of OXPHOS [105,161,162]. When it becomes necessary to supplement the blood, the HSCs activate OXPHOS with ROS production to promote cell growth [105,161,162]. Therefore, artificially inhibiting glycolysis or inducing the production of ROS reduces the number of HSCs in the dormant state [105,161,162]. OXPHOS-dependent metabolic reprogramming has also been observed during normal tissue regeneration [163]. Similar to normal tissues and stem cells, when ROS production is increased, the number of resting cells decrease and cell division is promoted among CSCs in leukemia [133], breast cancer [14], and head and neck cancer [155]. Lagadinou et al. revealed that quiescent leukemia stem cells overexpress Bcl-2 to suppress ROS production [133]. It has been shown that the inhibition of Bcl-2 selectively eliminates ROS-low quiescent leukemia stem cells but has little effect on ROS-high differentiated leukemia cells [133]. These results strongly suggest that for the tumor to maintain the CSC population, it is necessary to maintain an appropriate amount of ROS by modulating the balance of metabolic activity and the antioxidant system.
Figure 3.
The redox regulation and differentiation of CSCs. Quiescent CSCs maintain low-level reactive oxygen species (ROS) by glycolysis-dependent metabolism or enhanced antioxidant systems. ROS accumulation associated with OXPHOS activation induces CSC proliferation and differentiation.
5. Therapeutic Strategies for Targeting CSC Metabolism
Basically, dormant CSCs are considered to have strong resistance to conventional chemotherapy and radiation therapy that target active cell proliferation [8,10]. However, a treatment targeting CSC-specific metabolism may be able to selectively eliminate even dormant CSCs by depleting the energy or metabolites required for the survival of CSCs [15,16,17,18,19,20]. In addition, the inhibition of CSC-specific metabolism has been reported to increase the sensitivity to conventional chemotherapy [15,16,17,18,19,20]. Furthermore, since the importance of CSC-specific metabolism has been clarified by previous studies, it has been suggested that not only conventional chemotherapy, but also diet therapy is important in reducing the risk of cancer malignancy and a poor prognosis [20].
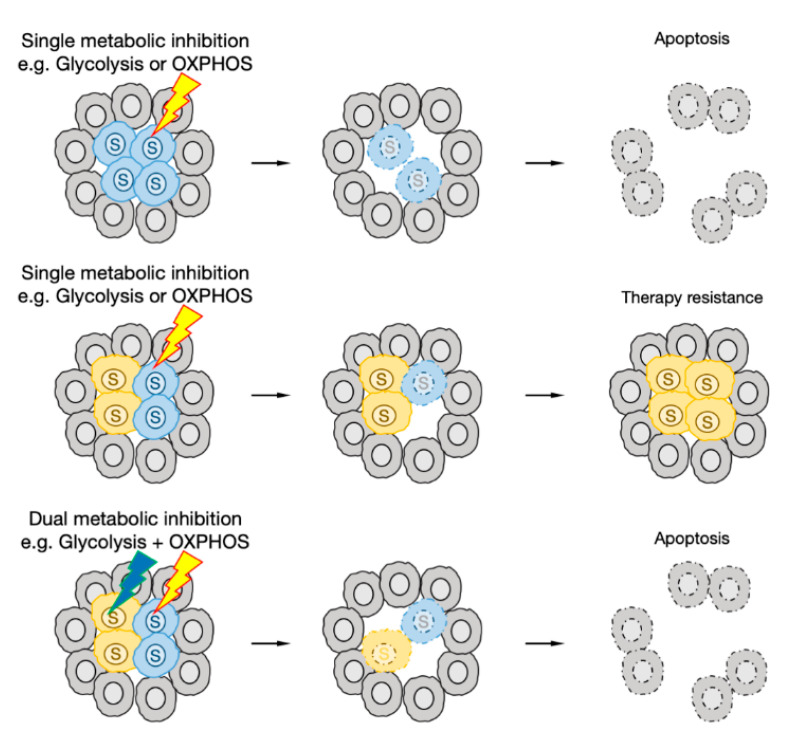
The mitochondrial metabolism of CSCs is currently attracting attention as an effective therapeutic target [17,19,20,50,55]. In addition to OXPHOS, mitochondria are the center of various metabolic pathways that provide essential cellular components, such as amino acids, including glutamine, fatty acids, and ketone bodies through the TCA cycle [50,51,52,55]. It has also been shown that mitochondria function normally even in glycolysis-dependent cancer cells, and that glutamine metabolism and FAO are activated [50,51,52,54,55]. In vitro and in vivo experiments have shown that inhibitors of mitochondrial OXPHOS, such as metformin, phenformin, and menadione, suppress CSC traits [132,163,164,165,166,167]. Also, since mitochondria are derived from a prokaryote that originally parasitized eukaryotic cells, it is known that its function can be inhibited by treatment with various antibiotics [17,18,19,20,168,169,170]. It has been shown that tetracycline antibiotics, such as doxycycline, specifically inhibit CSC traits by inhibiting mitochondrial biosynthesis, but they do not exert toxicity on normal cells or the bulk of the cancer [168,169,170]. On the other hand, the inhibition of glycolysis has been shown to be effective against some CSCs, but in many cases, it induces the resistance of cancer cells to therapy [108,110,171].
The metabolic state of CSCs in tumors is very heterogeneous, and the metabolism of each CSC is flexible enough to adapt to metabolic changes. Therefore, in most cases, even if a single metabolic pathway is inhibited, it is extremely difficult to uniformly eliminate all CSCs. However, the simultaneous inhibition of multiple metabolic pathways may prevent resistance acquisition and eliminate CSCs more efficiently (Figure 4). Since metformin is already approved by the U.S. Food and Drug Administration (FDA) as an anti-diabetic drug, its combined effect with a wide range of metabolism inhibitors is being tested [68,132,172,173,174,175]. In addition to the ETS, metformin is known to inhibit mTORC1 activity indirectly or directly [176,177]. mTORC1 has a central role in the metabolic regulation of cancer cells, so metformin may enhance the effects of other metabolic inhibitors by inhibiting the metabolic reprograming of CSCs. The glutaminase inhibitors BPTES and CB839 strongly inhibit the growth of glutamine-addicted tumors even when used alone, but they have been shown to be more potent when combined with other metabolic inhibitors or conventional chemotherapy [68,69,70,171,178,179]. The FAO inhibitor etomoxir also enhanced the therapeutic effect of conventional chemotherapy in several types of cancers in vivo [138,180,181]. The selective Nrf2 inhibitor trigonelline, the xCT inhibitor sulfasalazine, the GSH inhibitor buthionine sulfoximine, and the Trx inhibitor auranofin induce cell death by accumulating ROS in CSCs. When the GSH pathway is inhibited, Trx expression is increased to compensate for it, indicating that the inhibition of both GSH and Trx at the same time can eliminate CSCs more efficiently than the inhibition of GSH or Trx alone [182,183,184,185].
Figure 4.
Therapeutic strategies targeting the metabolism of CSCs. If CSCs depend on a particular metabolism, a single metabolic inhibitor can effectively eliminate the tumor. When multiple CSCs with distinct metabolic phenotypes are present in the same tumor, it is necessary to simultaneously inhibit multiple metabolic pathways to eliminate the tumor.
It is known that the activation of aerobic glycolysis in cancer cells leads to glucose depletion in the microenvironment and acidification due to lactate over-secretion, thereby impairing immune cell function [33,34,186]. In contrast, the activation of mitochondrial OXPHOS in cancer cells may promote immune responses [187]. Harel et al. conducted a detailed analysis of the metabolic phenotypes of melanoma patients who underwent cancer immunotherapy, and the tumors of patients showing a therapeutic effect had significantly increased expression levels of genes related to mitochondrial OXPHOS when compared to those of the non-responders [187]. Furthermore, they found that the expression of OXPHOS-related genes restored the antigen-presenting function of cancer cells [187]. Therefore, glycolysis inhibition or OXPHOS activation can be expected to enhance the effect of cancer immunotherapy by simultaneously activating the antigen-presenting function of cancer cells and the function of immune cells [187,188].
Previous studies have suggested that calorie restriction and diet therapy may reduce the incidence and progression of cancer [189]. However, little is known about the effects of these external factors on CSCs. At the least, experiments using model mice have suggested that overeating after calorie restriction promotes the proliferation of CSCs and distant metastases [190]. On the other hand, some food-derived ingredients, e.g., eicosapentaenoic acids and docosahexaenoic acids, which are omega-3 polyunsaturated fatty acids, and vitamin C, have a therapeutic effect on CSCs [191,192,193,194]. However, there have been no reported clinical cases in which these components were effective for tumor regression. Ketogenic diets are expected to reduce the risk of the malignant transformation of cancer, but conflicting results on the suppression/promotion of tumor growth have been obtained even within the same tumor types [195]. In addition, Martinez-Outschoorn et al. reported that ketone bodies induce stemness properties in breast cancer cells [196]. Similar to how cancer cells acquire resistance to certain metabolic inhibitors, the continual intake of biased diets may induce CSCs to adapt to the biased environment, which may increase the risk of cancer malignancy.
Both in vitro and in vivo experiments have demonstrated that the inhibition of metabolism may induce a reduction in the CSC population and tumor regression, but many of the metabolic pathways activated in cancer cells are also activated in various tissues, organs, normal stem cells, and the like. Therefore, as with general anticancer agents, many metabolic inhibitors have serious side effects, such as acidosis by the treatment of anti-diabetic drugs [94,197,198]. To reduce the side effects, it is necessary to accurately determine the effects of the metabolic inhibitors on cancer cells and normal cells, and to identify and establish highly selective methods of eliminating cancer cells.
6. Conclusions
In light of the technological progress and great efforts of researchers in recent years, the importance of CSCs and their metabolic regulation that underlie tumor heterogeneity have gradually been revealed. Numerous studies have revealed that each CSC has a distinct metabolic mechanism that differs from that of non-CSCs, and CSC-specific metabolism is therefore an attractive target for cancer therapy. However, the simultaneous presence of multiple CSCs with distinct metabolic phenotypes, even within same tumor types, and the metabolic flexibility of CSCs make the development of effective treatments difficult. If the various metabolic pathways are obstructed in a blind way, it causes serious side effects in normal tissues. As such, it is necessary to efficiently identify and target the specific metabolic vulnerabilities of each type of CSC. Although there are critical factors that play central roles, the activity of each metabolic pathway is regulated by complex interactions between many factors. For example, even if we focus only on glycolysis, the pathway is not isolated, and at each reaction step, different enzymes regulate the reactions and the metabolites may flow into or out of different metabolic pathways. Within such a complicated metabolic system, it is very difficult to identify potential targets in CSCs. However, recent studies have attempted to identify such targets by systematically linking the metabolic profiles of tumors with genome-wide transcriptome and proteomics analysis [142,199,200,201]. In the near future, by accumulating such research data, it is expected that the identification of the metabolic vulnerabilities of each tumor will be possible, which will enable the development of more efficient diagnostic techniques and therapies.
Author Contributions
A.T. wrote the manuscript with support from H.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Bukowski K., Kciuk M., Kontek R. Mechanisms of multidrug resistance in cancer chemotherapy. Int. J. Mol. Sci. 2020;21:3233. doi: 10.3390/ijms21093233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hevener K.E., Verstak T.A., Lutat K.E., Riggsbee D.L., Mooney J.W. Recent developments in topoisomerase-targeted cancer chemotherapy. Acta Pharm. Sin. B. 2018;8:844–861. doi: 10.1016/j.apsb.2018.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luqmani Y.A. Mechanisms of drug resistance in cancer chemotherapy. Med. Princ. Pract. 2005;14:35–48. doi: 10.1159/000086183. [DOI] [PubMed] [Google Scholar]
- 4.Ubhi T., Brown G.W. Exploiting DNA replication stress for cancer treatment. Cancer Res. 2019;79:1730–1739. doi: 10.1158/0008-5472.CAN-18-3631. [DOI] [PubMed] [Google Scholar]
- 5.Wang J., Seebacher N., Shi H., Kan Q., Duan Z. Novel strategies to prevent the development of multidrug resistance (MDR) in cancer. Oncotarget. 2017;8:84559–84571. doi: 10.18632/oncotarget.19187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Batlle E., Clevers H. Cancer stem cells revisited. Nat. Med. 2017;23:1124–1134. doi: 10.1038/nm.4409. [DOI] [PubMed] [Google Scholar]
- 7.Lapidot T., Sirard C., Vormoor J., Murdoch B., Hoang T., Caceres-Cortes J., Minden M., Paterson B., Caligiuri M.A., Dick J.E. A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature. 1994;367:645–648. doi: 10.1038/367645a0. [DOI] [PubMed] [Google Scholar]
- 8.Lytle N.K., Barber A.G., Reya T. Stem cell fate in cancer growth, progression and therapy resistance. Nat. Rev. Cancer. 2018;18:669–680. doi: 10.1038/s41568-018-0056-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meacham C.E., Morrison S.J. Tumour heterogeneity and cancer cell plasticity. Nature. 2013;501:328–337. doi: 10.1038/nature12624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Plaks V., Kong N., Werb Z. The cancer stem cell niche: How essential is the niche in regulating stemness of tumor cells? Cell Stem Cell. 2015;16:225–238. doi: 10.1016/j.stem.2015.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prager B.C., Xie Q., Bao S., Rich J.N. Cancer Stem Cells: The Architects of the Tumor Ecosystem. Cell Stem Cell. 2019;24:41–53. doi: 10.1016/j.stem.2018.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang L., Shi P., Zhao G., Xu J., Peng W., Zhang J., Zhang G., Wang X., Dong Z., Chen F., et al. Targeting cancer stem cell pathways for cancer therapy. Signal Transduct. Target. Ther. 2020;5:8. doi: 10.1038/s41392-020-0110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu S., Cong Y., Wang D., Sun Y., Deng L., Liu Y., Martin-Trevino R., Shang L., McDermott S.P., Landis M.D., et al. Breast cancer stem cells transition between epithelial and mesenchymal states reflective of their normal counterparts. Stem Cell Rep. 2014;2:78–91. doi: 10.1016/j.stemcr.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luo M., Shang L., Brooks M.D., Jiagge E., Zhu Y., Buschhaus J.M., Conley S., Fath M.A., Davis A., Gheordunescu E., et al. Targeting Breast Cancer Stem Cell State Equilibrium through Modulation of Redox Signaling. Cell Metab. 2018;28:69–86.e6. doi: 10.1016/j.cmet.2018.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chae Y.C., Kim J.H. Cancer stem cell metabolism: Target for cancer therapy. BMB Rep. 2018;51:319–326. doi: 10.5483/BMBRep.2018.51.7.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dando I., Dalla Pozza E., Biondani G., Cordani M., Palmieri M., Donadelli M. The metabolic landscape of cancer stem cells. IUBMB Life. 2015;67:687–693. doi: 10.1002/iub.1426. [DOI] [PubMed] [Google Scholar]
- 17.De Francesco E.M., Sotgia F., Lisanti M.P. Cancer stem cells (CSCs): Metabolic strategies for their identification and eradication. Biochem. J. 2018;475:1611–1634. doi: 10.1042/BCJ20170164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jagust P., De Luxán-Delgado B., Parejo-Alonso B., Sancho P. Metabolism-based therapeutic strategies targeting cancer stem cells. Front. Pharmacol. 2019;10:1–26. doi: 10.3389/fphar.2019.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sancho P., Barneda D., Heeschen C. Hallmarks of cancer stem cell metabolism. Br. J. Cancer. 2016;114:1305–1312. doi: 10.1038/bjc.2016.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Snyder V., Reed-Newman T.C., Arnold L., Thomas S.M., Anant S. Cancer stem cell metabolism and potential therapeutic targets. Front. Oncol. 2018;8:1–9. doi: 10.3389/fonc.2018.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Warburg O., Wild F., Ngelein E. The metabolism of tumours in the body. J. Gen. Physiol. 1927;8:519–530. doi: 10.1085/jgp.8.6.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh J., Suh E.H., Sharma G., Khemtong C., Sherry A.D., Kovacs Z. Probing carbohydrate metabolism using hyperpolarized 13C-labeled molecules. NMR Biomed. 2019;32:1–23. doi: 10.1002/nbm.4018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hensley C.T., Faubert B., Yuan Q., Lev-Cohain N., Jin E., Kim J., Jiang L., Ko B., Skelton R., Loudat L., et al. Metabolic Heterogeneity in Human Lung Tumors. Cell. 2016;164:681–694. doi: 10.1016/j.cell.2015.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vander Heiden M.G., Cantley L.C., Thompson C.B. Understanding the Warburg Effect: The Metabolic Requirements of Cell Proliferation. Science. 2009;324:1029–1033. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koppenol W.H., Bounds P.L., Dang C.V. Otto Warburg’s contributions to current concepts of cancer metabolism. Nat. Rev. Cancer. 2011;11:325–337. doi: 10.1038/nrc3038. [DOI] [PubMed] [Google Scholar]
- 26.Cairns R.A., Harris I.S., Mak T.W. Regulation of cancer cell metabolism. Nat. Rev. Cancer. 2011;11:85–95. doi: 10.1038/nrc2981. [DOI] [PubMed] [Google Scholar]
- 27.Pavlova N.N., Thompson C.B. The Emerging Hallmarks of Cancer Metabolism. Cell Metab. 2016;23:27–47. doi: 10.1016/j.cmet.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DeBerardinis R.J., Chandel N.S. Fundamentals of cancer metabolism. Sci. Adv. 2016;2:e1600200. doi: 10.1126/sciadv.1600200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ward P.S., Thompson C.B. Metabolic Reprogramming: A Cancer Hallmark Even Warburg Did Not Anticipate. Cancer Cell. 2012;21:297–308. doi: 10.1016/j.ccr.2012.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patra K.C., Hay N. The pentose phosphate pathway and cancer. Trends Biochem. Sci. 2014;39:347–354. doi: 10.1016/j.tibs.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ducker G.S., Rabinowitz J.D. One-Carbon Metabolism in Health and Disease. Cell Metab. 2017;25:27–42. doi: 10.1016/j.cmet.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reid M.A., Allen A.E., Liu S., Liberti M.V., Liu P., Liu X., Dai Z., Gao X., Wang Q., Liu Y., et al. Serine synthesis through PHGDH coordinates nucleotide levels by maintaining central carbon metabolism. Nat. Commun. 2018;9:1–11. doi: 10.1038/s41467-018-07868-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hirschhaeuser F., Sattler U.G.A., Mueller-Klieser W. Lactate: A metabolic key player in cancer. Cancer Res. 2011;71:6921–6925. doi: 10.1158/0008-5472.CAN-11-1457. [DOI] [PubMed] [Google Scholar]
- 34.Parks S.K., Mueller-Klieser W., Pouysségur J. Lactate and Acidity in the Cancer Microenvironment. Annu. Rev. Cancer Biol. 2020;4:141–158. doi: 10.1146/annurev-cancerbio-030419-033556. [DOI] [Google Scholar]
- 35.Li X., Zhang Z., Zhang Y., Cao Y., Wei H., Wu Z. Upregulation of lactate-inducible snail protein suppresses oncogene-mediated senescence through p16 INK4a inactivation. J. Exp. Clin. Cancer Res. 2018;37:1–13. doi: 10.1186/s13046-018-0701-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Doherty J.R., Yang C., Scott K.E.N., Cameron M.D., Fallahi M., Li W., Hall M.A., Amelio A.L., Mishra J.K., Li F., et al. Blocking lactate export by inhibiting the myc target MCT1 disables glycolysis and glutathione synthesis. Cancer Res. 2014;74:908–920. doi: 10.1158/0008-5472.CAN-13-2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eales K.L., Hollinshead K.E.R., Tennant D.A. Hypoxia and metabolic adaptation of cancer cells. Oncogenesis. 2016;5:e190. doi: 10.1038/oncsis.2015.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gan L., Xiu R., Ren P., Yue M., Su H., Guo G., Xiao D., Yu J., Jiang H., Liu H., et al. Metabolic targeting of oncogene MYC by selective activation of the proton-coupled monocarboxylate family of transporters. Oncogene. 2016;35:3037–3048. doi: 10.1038/onc.2015.360. [DOI] [PubMed] [Google Scholar]
- 39.He T.L., Zhang Y.J., Jiang H., Li X.H., Zhu H., Zheng K.L. The c-Myc–LDHA axis positively regulates aerobic glycolysis and promotes tumor progression in pancreatic cancer. Med. Oncol. 2015;32:1–8. doi: 10.1007/s12032-015-0633-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim J., Gao P., Liu Y.-C., Semenza G.L., Dang C.V. Hypoxia-Inducible Factor 1 and Dysregulated c-Myc Cooperatively Induce Vascular Endothelial Growth Factor and Metabolic Switches Hexokinase 2 and Pyruvate Dehydrogenase Kinase 1. Mol. Cell. Biol. 2007;27:7381–7393. doi: 10.1128/MCB.00440-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miller D.M., Thomas S.D., Islam A., Muench D., Sedoris K. c-Myc and cancer metabolism. Clin. Cancer Res. 2012;18:5546–5553. doi: 10.1158/1078-0432.CCR-12-0977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Park S.J., Smith C.P., Wilbur R.R., Cain C.P., Kallu S.R., Valasapalli S., Sahoo A., Guda M.R., Tsung A.J., Velpula K.K. An overview of MCT1 and MCT4 in GBM: Small molecule transporters with large implications. Am. J. Cancer Res. 2018;8:1967–1976. [PMC free article] [PubMed] [Google Scholar]
- 43.Pupo E., Avanzato D., Middonti E., Bussolino F., Lanzetti L. KRAS-driven metabolic rewiring reveals novel actionable targets in cancer. Front. Oncol. 2019;9:1–9. doi: 10.3389/fonc.2019.00848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bensaad K., Tsuruta A., Selak M.A., Vidal M.N.C., Nakano K., Bartrons R., Gottlieb E., Vousden K.H. TIGAR, a p53-Inducible Regulator of Glycolysis and Apoptosis. Cell. 2006;126:107–120. doi: 10.1016/j.cell.2006.05.036. [DOI] [PubMed] [Google Scholar]
- 45.Contractor T., Harris C.R. p53 negatively regulates transcription of the pyruvate dehydrogenase kinase Pdk2. Cancer Res. 2012;72:560–567. doi: 10.1158/0008-5472.CAN-11-1215. [DOI] [PubMed] [Google Scholar]
- 46.Jiang P., Du W., Wang X., Mancuso A., Gao X., Wu M., Yang X. P53 regulates biosynthesis through direct inactivation of glucose-6-phosphate dehydrogenase. Nat. Cell Biol. 2011;13:310–316. doi: 10.1038/ncb2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang L., Xiong H., Wu F., Zhang Y., Wang J., Zhao L., Guo X., Chang L.J., Zhang Y., You M.J., et al. Hexokinase 2-Mediated Warburg Effect Is Required for PTEN- and p53-Deficiency-Driven Prostate Cancer Growth. Cell Rep. 2014;8:1461–1474. doi: 10.1016/j.celrep.2014.07.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yamamoto S., Iwakuma T. Regulators of oncogenic mutant TP53 gain of function. Cancers. 2019;11:4. doi: 10.3390/cancers11010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang C., Liu J., Liang Y., Wu R., Zhao Y., Hong X., Lin M., Yu H., Liu L., Levine A.J., et al. Tumour-associated mutant p53 drives the Warburg effect. Nat. Commun. 2013;4 doi: 10.1038/ncomms3935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ghosh P., Vidal C., Dey S., Zhang L. Mitochondria targeting as an effective strategy for cancer therapy. Int. J. Mol. Sci. 2020;21:3363. doi: 10.3390/ijms21093363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vyas S., Zaganjor E., Haigis M.C. Mitochondria and Cancer. Cell. 2016;166:555–566. doi: 10.1016/j.cell.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wallace D.C. Mitochondria and cancer. Nat. Rev. Cancer. 2012;12:685–698. doi: 10.1038/nrc3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cantor J.R., Sabatini D.M. Cancer cell metabolism: One hallmark, many faces. Cancer Discov. 2012;2:881–898. doi: 10.1158/2159-8290.CD-12-0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fan J., Kamphorst J.J., Mathew R., Chung M.K., White E., Shlomi T., Rabinowitz J.D. Glutamine-driven oxidative phosphorylation is a major ATP source in transformed mammalian cells in both normoxia and hypoxia. Mol. Syst. Biol. 2013;9:1–11. doi: 10.1038/msb.2013.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jia D., Park J., Jung K., Levine H., Kaipparettu B. Elucidating the Metabolic Plasticity of Cancer: Mitochondrial Reprogramming and Hybrid Metabolic States. Cells. 2018;7:21. doi: 10.3390/cells7030021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Raza M.H., Siraj S., Arshad A., Waheed U., Aldakheel F., Alduraywish S., Arshad M. ROS-modulated therapeutic approaches in cancer treatment. J. Cancer Res. Clin. Oncol. 2017;143:1789–1809. doi: 10.1007/s00432-017-2464-9. [DOI] [PubMed] [Google Scholar]
- 57.Mastropasqua F., Girolimetti G., Shoshan M. PGC1α: Friend or foe in cancer? Genes. 2018;9:48. doi: 10.3390/genes9010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tan Z., Luo X., Xiao L., Tang M., Bode A.M., Dong Z., Cao Y. The role of PGC1α in cancer metabolism and its therapeutic implications. Mol. Cancer Ther. 2016;15:774–782. doi: 10.1158/1535-7163.MCT-15-0621. [DOI] [PubMed] [Google Scholar]
- 59.Andrzejewski S., Klimcakova E., Johnson R.M., Tabariès S., Annis M.G., McGuirk S., Northey J.J., Chénard V., Sriram U., Papadopoli D.J., et al. PGC-1α Promotes Breast Cancer Metastasis and Confers Bioenergetic Flexibility against Metabolic Drugs. Cell Metab. 2017;26:778–787.e5. doi: 10.1016/j.cmet.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 60.Lebleu V.S., O’Connell J.T., Gonzalez Herrera K.N., Wikman H., Pantel K., Haigis M.C., De Carvalho F.M., Damascena A., Domingos Chinen L.T., Rocha R.M., et al. PGC-1α mediates mitochondrial biogenesis and oxidative phosphorylation in cancer cells to promote metastasis. Nat. Cell Biol. 2014;16:992–1003. doi: 10.1038/ncb3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li F., Wang Y., Zeller K.I., Potter J.J., Wonsey D.R., O’Donnell K.A., Kim J., Yustein J.T., Lee L.A., Dang C.V. Myc Stimulates Nuclearly Encoded Mitochondrial Genes and Mitochondrial Biogenesis. Mol. Cell. Biol. 2005;25:6225–6234. doi: 10.1128/MCB.25.14.6225-6234.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee K.M., Giltnane J.M., Balko J.M., Schwarz L.J., Guerrero-Zotano A.L., Hutchinson K.E., Nixon M.J., Estrada M.V., Sánchez V., Sanders M.E., et al. MYC and MCL1 Cooperatively Promote Chemotherapy-Resistant Breast Cancer Stem Cells via Regulation of Mitochondrial Oxidative Phosphorylation. Cell Metab. 2017;26:633–647.e7. doi: 10.1016/j.cmet.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dang L., White D.W., Gross S., Bennett B.D., Bittinger M.A., Driggers E.M., Fantin V.R., Jang H.G., Jin S., Keenan M.C., et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009;462:739–744. doi: 10.1038/nature08617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lu C., Ward P.S., Kapoor G.S., Rohle D., Turcan S., Abdel-Wahab O., Edwards C.R., Khanin R., Figueroa M.E., Melnick A., et al. IDH mutation impairs histone demethylation and results in a block to cell differentiation. Nature. 2012;483:474–478. doi: 10.1038/nature10860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.King A., Selak M.A., Gottlieb E. Succinate dehydrogenase and fumarate hydratase: Linking mitochondrial dysfunction and cancer. Oncogene. 2006;25:4675–4682. doi: 10.1038/sj.onc.1209594. [DOI] [PubMed] [Google Scholar]
- 66.Lieu E.L., Nguyen T., Rhyne S., Kim J. Amino acids in cancer. Exp. Mol. Med. 2020;52:15–30. doi: 10.1038/s12276-020-0375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vettore L., Westbrook R.L., Tennant D.A. New aspects of amino acid metabolism in cancer. Br. J. Cancer. 2020;122:150–156. doi: 10.1038/s41416-019-0620-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Elgogary A., Xu Q., Poore B., Alt J., Zimmermann S.C., Zhao L., Fu J., Chen B., Xia S., Liu Y., et al. Combination therapy with BPTES nanoparticles and metformin targets the metabolic heterogeneity of pancreatic cancer. Proc. Natl. Acad. Sci. USA. 2016;113:E5328–E5336. doi: 10.1073/pnas.1611406113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lee P., Malik D., Perkons N., Huangyang P., Khare S., Rhoades S., Gong Y.Y., Burrows M., Finan J.M., Nissim I., et al. Targeting glutamine metabolism slows soft tissue sarcoma growth. Nat. Commun. 2020;11 doi: 10.1038/s41467-020-14374-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Momcilovic M., Bailey S.T., Lee J.T., Fishbein M.C., Braas D., Go J., Graeber T.G., Parlati F., Demo S., Li R., et al. The GSK3 Signaling Axis Regulates Adaptive Glutamine Metabolism in Lung Squamous Cell Carcinoma. Cancer Cell. 2018;33:905–921. doi: 10.1016/j.ccell.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Van Geldermalsen M., Wang Q., Nagarajah R., Marshall A.D., Thoeng A., Gao D., Ritchie W., Feng Y., Bailey C.G., Deng N., et al. ASCT2/SLC1A5 controls glutamine uptake and tumour growth in triple-negative basal-like breast cancer. Oncogene. 2016;35:3201–3208. doi: 10.1038/onc.2015.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Scalise M., Pochini L., Console L., Losso M.A., Indiveri C. The Human SLC1A5 (ASCT2) amino acid transporter: From function to structure and role in cell biology. Front. Cell Dev. Biol. 2018;6:1–17. doi: 10.3389/fcell.2018.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hayashi K., Jutabha P., Endou H., Anzai N. c-Myc is crucial for the expression of LAT1 in MIA Paca-2 human pancreatic cancer cells. Oncol. Rep. 2012;28:862–866. doi: 10.3892/or.2012.1878. [DOI] [PubMed] [Google Scholar]
- 74.Gao P., Tchernyshyov I., Chang T.C., Lee Y.S., Kita K., Ochi T., Zeller K.I., De Marzo A.M., Van Eyk J.E., Mendell J.T., et al. C-Myc suppression of miR-23a/b enhances mitochondrial glutaminase expression and glutamine metabolism. Nature. 2009;458:762–765. doi: 10.1038/nature07823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chen Z., Wang Y., Warden C., Chen S. Cross-talk between ER and HER2 regulates c-MYC-mediated glutamine metabolism in aromatase inhibitor resistant breast cancer cells. J. Steroid Biochem. Mol. Biol. 2015;149:118–127. doi: 10.1016/j.jsbmb.2015.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Low H.Y., Lee Y.C., Lee Y.J., Wang H.L., Chen Y.I., Chien P.J., Li S.T., Chang W.W. Reciprocal regulation between indoleamine 2,3-dioxigenase 1 and notch1 involved in radiation response of cervical cancer stem cells. Cancers. 2020;12:1547. doi: 10.3390/cancers12061547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ehsanipour E.A., Sheng X., Behan J.W., Wang X., Butturini A., Avramis V.I., Mittelman S.D. Adipocytes cause leukemia cell resistance to l-asparaginase via release of glutamine. Cancer Res. 2013;73:2998–3006. doi: 10.1158/0008-5472.CAN-12-4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Richards N.G.J., Kilberg M.S. Asparagine Synthetase Chemotherapy. Annu. Rev. Biochem. 2006;75:629–654. doi: 10.1146/annurev.biochem.75.103004.142520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Koundouros N., Poulogiannis G. Reprogramming of fatty acid metabolism in cancer. Br. J. Cancer. 2020;122:4–22. doi: 10.1038/s41416-019-0650-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nath A., Li I., Roberts L.R., Chan C. Elevated free fatty acid uptake via CD36 promotes epithelial-mesenchymal transition in hepatocellular carcinoma. Sci. Rep. 2015;5:1–19. doi: 10.1038/srep14752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pascual G., Avgustinova A., Mejetta S., Martín M., Castellanos A., Attolini C.S.O., Berenguer A., Prats N., Toll A., Hueto J.A., et al. Targeting metastasis-initiating cells through the fatty acid receptor CD36. Nature. 2017;541:41–45. doi: 10.1038/nature20791. [DOI] [PubMed] [Google Scholar]
- 82.Van der Mijn J.C., Fu L., Khani F., Zhang T., Molina A.M., Barbieri C.E., Chen Q., Gross S.S., Gudas L.J., Nanus D.M. Combined Metabolomics and Genome-Wide Transcriptomics Analyses Show Multiple HIF1α-Induced Changes in Lipid Metabolism in Early Stage Clear Cell Renal Cell Carcinoma. Transl. Oncol. 2020;13:177–185. doi: 10.1016/j.tranon.2019.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Carracedo A., Cantley L.C., Pandolfi P.P. Cancer metabolism: Fatty acid oxidation in the limelight. Nat. Rev. Cancer. 2013;13:227–232. doi: 10.1038/nrc3483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Labuschagne C.F., Cheung E.C., Blagih J., Domart M.C., Vousden K.H. Cell Clustering Promotes a Metabolic Switch that Supports Metastatic Colonization. Cell Metab. 2019;30:720–734.e5. doi: 10.1016/j.cmet.2019.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Li N., He Y., Wang L., Mo C., Zhang J., Zhang W., Li J., Liao Z., Tang X., Xiao H. D-galactose induces necroptotic cell death in neuroblastoma cell lines. J. Cell. Biochem. 2011;112:3834–3844. doi: 10.1002/jcb.23314. [DOI] [PubMed] [Google Scholar]
- 86.Shiratori R., Furuichi K., Yamaguchi M., Miyazaki N., Aoki H., Chibana H., Ito K., Aoki S. Glycolytic suppression dramatically changes the intracellular metabolic profile of multiple cancer cell lines in a mitochondrial metabolism-dependent manner. Sci. Rep. 2019;9:1–15. doi: 10.1038/s41598-019-55296-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bu P., Chen K.Y., Xiang K., Johnson C., Crown S.B., Rakhilin N., Ai Y., Wang L., Xi R., Astapova I., et al. Aldolase B-Mediated Fructose Metabolism Drives Metabolic Reprogramming of Colon Cancer Liver Metastasis. Cell Metab. 2018;27:1249–1262.e4. doi: 10.1016/j.cmet.2018.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chen W.J., Ho C.C., Chang Y.L., Chen H.Y., Lin C.A., Ling T.Y., Yu S.L., Yuan S.S., Louisa Chen Y.J., Lin C.Y., et al. Cancer-associated fibroblasts regulate the plasticity of lung cancer stemness via paracrine signalling. Nat. Commun. 2014;5 doi: 10.1038/ncomms4472. [DOI] [PubMed] [Google Scholar]
- 89.Woolthuis C.M., Stranahan A.W., Park C.Y., Minhajuddin M., Gasparetto M., Stevens B., Pei S., Jordan C.T. Leukemic Stem Cells Evade Chemotherapy by Metabolic Adaptation to an Adipose Tissue Niche. Cell Stem Cell. 2016;19:23–37. doi: 10.1016/j.stem.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Flöter J., Kaymak I., Schulze A. Regulation of metabolic activity by p53. Metabolites. 2017;7:21. doi: 10.3390/metabo7020021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ren Y., Shen H.M. Critical role of AMPK in redox regulation under glucose starvation. Redox Biol. 2019;25:101154. doi: 10.1016/j.redox.2019.101154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Buzzai M., Jones R.G., Amaravadi R.K., Lum J.J., DeBerardinis R.J., Zhao F., Viollet B., Thompson C.B. Systemic treatment with the antidiabetic drug metformin selectively impairs p53-deficient tumor cell growth. Cancer Res. 2007;67:6745–6752. doi: 10.1158/0008-5472.CAN-06-4447. [DOI] [PubMed] [Google Scholar]
- 93.Maddocks O.D.K., Berkers C.R., Mason S.M., Zheng L., Blyth K., Gottlieb E., Vousden K.H. Serine starvation induces stress and p53-dependent metabolic remodelling in cancer cells. Nature. 2013;493:542–546. doi: 10.1038/nature11743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shackelford D.B., Abt E., Gerken L., Vasquez D.S., Seki A., Leblanc M., Wei L., Fishbein M.C., Czernin J., Mischel P.S., et al. LKB1 Inactivation Dictates Therapeutic Response of Non-Small Cell Lung Cancer to the Metabolism Drug Phenformin. Cancer Cell. 2013;23:143–158. doi: 10.1016/j.ccr.2012.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nam K.S., Sunhwa O.H., Shin I. Ablation of CD44 induces glycolysis-To-oxidative phosphorylation transition via modulation of the c-Src-Akt-LKB1-AMPKα pathway. Biochem. J. 2016;473:3013–3030. doi: 10.1042/BCJ20160613. [DOI] [PubMed] [Google Scholar]
- 96.Sullivan W.J., Mullen P.J., Schmid E.W., Flores A., Momcilovic M., Sharpley M.S., Jelinek D., Whiteley A.E., Maxwell M.B., Wilde B.R., et al. Extracellular Matrix Remodeling Regulates Glucose Metabolism through TXNIP Destabilization. Cell. 2018;175:117–132.e21. doi: 10.1016/j.cell.2018.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Nallanthighal S., Heiserman J.P., Cheon D.-J. The Role of the Extracellular Matrix in Cancer Stemness. Front. Cell Dev. Biol. 2019;7:1–14. doi: 10.3389/fcell.2019.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chanmee T., Ontong P., Kimata K., Itano N. Key roles of hyaluronan and its CD44 receptor in the stemness and survival of cancer stem cells. Front. Oncol. 2015;5:1–11. doi: 10.3389/fonc.2015.00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Schafer Z.T., Grassian A.R., Song L., Jiang Z., Gerhart-Hines Z., Irie H.Y., Gao S., Puigserver P., Brugge J.S. Antioxidant and oncogene rescue of metabolic defects caused by loss of matrix attachment. Nature. 2009;461:109–113. doi: 10.1038/nature08268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.McGuirk S., Audet-Delage Y., St-Pierre J. Metabolic Fitness and Plasticity in Cancer Progression. Trends Cancer. 2020;6:49–61. doi: 10.1016/j.trecan.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 101.Lehúede C., Dupuy F., Rabinovitch R., Jones R.G., Siegel P.M. Metabolic plasticity as a determinant of tumor growth and metastasis. Cancer Res. 2016;76:5201–5208. doi: 10.1158/0008-5472.CAN-16-0266. [DOI] [PubMed] [Google Scholar]
- 102.Bhattacharya D., Scimè A. Metabolic Regulation of Epithelial to Mesenchymal Transition: Implications for Endocrine Cancer. Front. Endocrinol. 2019;10:1–9. doi: 10.3389/fendo.2019.00773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Vlashi E., Lagadec C., Vergnes L., Reue K., Frohnen P., Chan M., Alhiyari Y., Dratver M.B., Pajonk F. Metabolic differences in breast cancer stem cells and differentiated progeny. Breast Cancer Res. Treat. 2014;146:525–534. doi: 10.1007/s10549-014-3051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Folmes C.D.L., Nelson T.J., Martinez-Fernandez A., Arrell D.K., Lindor J.Z., Dzeja P.P., Ikeda Y., Perez-Terzic C., Terzic A. Somatic oxidative bioenergetics transitions into pluripotency-dependent glycolysis to facilitate nuclear reprogramming. Cell Metab. 2011;14:264–271. doi: 10.1016/j.cmet.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ito K., Suda T. Metabolic requirements for the maintenance of self-renewing stem cells. Nat. Rev. Mol. Cell Biol. 2014;15:243–256. doi: 10.1038/nrm3772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Varum S., Rodrigues A.S., Moura M.B., Momcilovic O., Easley C.A., IV, Ramalho-Santos J., van Houten B., Schatten G. Energy metabolism in human pluripotent stem cells and their differentiated counterparts. PLoS ONE. 2011;6:e20914. doi: 10.1371/journal.pone.0020914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wu J., Ocampo A., Belmonte J.C.I. Cellular Metabolism and Induced Pluripotency. Cell. 2016;166:1371–1385. doi: 10.1016/j.cell.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 108.Peng F., Wang J.H., Fan W.J., Meng Y.T., Li M.M., Li T.T., Cui B., Wang H.F., Zhao Y., An F., et al. Glycolysis gatekeeper PDK1 reprograms breast cancer stem cells under hypoxia. Oncogene. 2018;37:1062–1074. doi: 10.1038/onc.2017.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Dong C., Yuan T., Wu Y., Wang Y., Fan T.W.M., Miriyala S., Lin Y., Yao J., Shi J., Kang T., et al. Loss of FBP1 by snail-mediated repression provides metabolic advantages in basal-like breast cancer. Cancer Cell. 2013;23:316–331. doi: 10.1016/j.ccr.2013.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ciavardelli D., Rossi C., Barcaroli D., Volpe S., Consalvo A., Zucchelli M., De Cola A., Scavo E., Carollo R., D’Agostino D., et al. Breast cancer stem cells rely on fermentative glycolysis and are sensitive to 2-deoxyglucose treatment. Cell Death Dis. 2014;5:1–12. doi: 10.1038/cddis.2014.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Liu P.P., Liao J., Tang Z.J., Wu W.J., Yang J., Zeng Z.L., Hu Y., Wang P., Ju H.Q., Xu R.H., et al. Metabolic regulation of cancer cell side population by glucose through activation of the Akt pathway. Cell Death Differ. 2014;21:124–135. doi: 10.1038/cdd.2013.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chen C.L., Uthaya Kumar D.B., Punj V., Xu J., Sher L., Tahara S.M., Hess S., Machida K. NANOG Metabolically Reprograms Tumor-Initiating Stem-like Cells through Tumorigenic Changes in Oxidative Phosphorylation and Fatty Acid Metabolism. Cell Metab. 2016;23:206–219. doi: 10.1016/j.cmet.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hur W., Ryu J.Y., Kim H.U., Hong S.W., Lee E.B., Lee S.Y., Yoon S.K. Systems approach to characterize the metabolism of liver cancer stem cells expressing CD133. Sci. Rep. 2017;7:1–11. doi: 10.1038/srep45557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhou Y., Zhou Y., Shingu T., Feng L., Chen Z., Ogasawara M., Keating M.J., Kondo S., Huang P. Metabolic alterations in highly tumorigenic glioblastoma cells: Preference for hypoxia and high dependency on glycolysis. J. Biol. Chem. 2011;286:32843–32853. doi: 10.1074/jbc.M111.260935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Liao J., Qian F., Tchabo N., Mhawech-Fauceglia P., Beck A., Qian Z., Wang X., Huss W.J., Lele S.B., Morrison C.D., et al. Ovarian cancer spheroid cells with stem cell-like properties contribute to tumor generation, metastasis and chemotherapy resistance through hypoxia-resistant metabolism. PLoS ONE. 2014;9:1–13. doi: 10.1371/journal.pone.0084941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Li X., Lu J., Kan Q., Li X., Fan Q., Li Y., Huang R., Slipicevic A., Dong H.P., Eide L., et al. Metabolic reprogramming is associated with flavopiridol resistance in prostate cancer DU145 cells. Sci. Rep. 2017;7:5081. doi: 10.1038/s41598-017-05086-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lin C.H., Hung P.H., Chen Y.J. CD44 is associated with the aggressive phenotype of nasopharyngeal carcinoma through redox regulation. Int. J. Mol. Sci. 2013;14:13266–13281. doi: 10.3390/ijms140713266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Shen Y.-A., Wang C.-Y., Hsieh Y.-T., Chen Y.-J., Wei Y.-H. Metabolic reprogramming orchestrates cancer stem cell properties in nasopharyngeal carcinoma. Cell Cycle. 2015;14:86–98. doi: 10.4161/15384101.2014.974419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Heddleston J.M., Li Z., Lathia J.D., Bao S., Hjelmeland A.B., Rich J.N. Hypoxia inducible factors in cancer stem cells. Br. J. Cancer. 2010;102:789–795. doi: 10.1038/sj.bjc.6605551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Qiu G.Z., Jin M.Z., Dai J.X., Sun W., Feng J.H., Jin W.L. Reprogramming of the Tumor in the Hypoxic Niche: The Emerging Concept and Associated Therapeutic Strategies. Trends Pharmacol. Sci. 2017;38:669–686. doi: 10.1016/j.tips.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 121.Semenza G.L. Hypoxia-inducible factors: Coupling glucose metabolism and redox regulation with induction of the breast cancer stem cell phenotype. EMBO J. 2017;36:252–259. doi: 10.15252/embj.201695204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Nakano A., Tsuji D., Miki H., Cui Q., El Sayed S.M., Ikegame A., Oda A., Amou H., Nakamura S., Harada T., et al. Glycolysis inhibition inactivates ABC transporters to restore drug sensitivity in malignant cells. PLoS ONE. 2011;6:1–10. doi: 10.1371/journal.pone.0027222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Belkahla S., Khan A.U.H., Gitenay D., Alexia C., Gondeau C., Vo D.N., Orecchioni S., Talarico G., Bertolini F., Cartron G., et al. Changes in metabolism affect expression of ABC transporters through ERK5 and depending on p53 status. Oncotarget. 2018;9:1114–1129. doi: 10.18632/oncotarget.23305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yu J., Li J., Chen Y., Cao W., Lu Y., Yang J., Xing E. Snail Enhances Glycolysis in the Epithelial-Mesenchymal Transition Process by Targeting FBP1 in Gastric Cancer. Cell. Physiol. Biochem. 2017;43:31–38. doi: 10.1159/000480314. [DOI] [PubMed] [Google Scholar]
- 125.Kim N.H., Cha Y.H., Lee J., Lee S.H., Yang J.H., Yun J.S., Cho E.S., Zhang X., Nam M., Kim N., et al. Snail reprograms glucose metabolism by repressing phosphofructokinase PFKP allowing cancer cell survival under metabolic stress. Nat. Commun. 2017;8 doi: 10.1038/ncomms14374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Dupuy F., Tabariès S., Andrzejewski S., Dong Z., Blagih J., Annis M.G., Omeroglu A., Gao D., Leung S., Amir E., et al. PDK1-dependent metabolic reprogramming dictates metastatic potential in breast cancer. Cell Metab. 2015;22:577–589. doi: 10.1016/j.cmet.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 127.Gaude E., Frezza C. Tissue-specific and convergent metabolic transformation of cancer correlates with metastatic potential and patient survival. Nat. Commun. 2016;7:1–9. doi: 10.1038/ncomms13041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gao C., Shen Y., Jin F., Miao Y., Qiu X. Cancer stem cells in small cell lung cancer cell line H446: Higher dependency on oxidative phosphorylation and mitochondrial substrate-level phosphorylation than non-stem cancer cells. PLoS ONE. 2016;11:1–16. doi: 10.1371/journal.pone.0154576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Janiszewska M., Suvà M.L., Riggi N., Houtkooper R.H., Auwerx J., Clément-Schatlo V., Radovanovic I., Rheinbay E., Provero P., Stamenkovic I. Imp2 controls oxidative phosphorylation and is crucial for preservin glioblastoma cancer stem cells. Genes Dev. 2012;26:1926–1944. doi: 10.1101/gad.188292.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Pastò A., Bellio C., Pilotto G., Ciminale V., Silic-Benussi M., Guzzo G., Rasola A., Frasson C., Nardo G., Zulato E., et al. Cancer stem cells from epithelial ovarian cancer patients privilege oxidative phosphorylation, and resist glucose deprivation. Oncotarget. 2014;5:4305–4319. doi: 10.18632/oncotarget.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Viale A., Pettazzoni P., Lyssiotis C.A., Ying H., Sánchez N., Marchesini M., Carugo A., Green T., Seth S., Giuliani V., et al. Oncogene ablation-resistant pancreatic cancer cells depend on mitochondrial function. Nature. 2014;514:628–632. doi: 10.1038/nature13611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sancho P., Burgos-Ramos E., Tavera A., Bou Kheir T., Jagust P., Schoenhals M., Barneda D., Sellers K., Campos-Olivas R., Graña O., et al. MYC/PGC-1α balance determines the metabolic phenotype and plasticity of pancreatic cancer stem cells. Cell Metab. 2015;22:590–605. doi: 10.1016/j.cmet.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 133.Lagadinou E.D., Sach A., Callahan K., Rossi R.M., Neering S.J., Minhajuddin M., Ashton J.M., Pei S., Grose V., O’Dwyer K.M., et al. BCL-2 inhibition targets oxidative phosphorylation and selectively eradicates quiescent human leukemia stem cells. Cell Stem Cell. 2013;12:329–341. doi: 10.1016/j.stem.2012.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bonuccelli G., De Francesco E.M., de Boer R., Tanowitz H.B., Lisanti M.P. NADH autofluorescence, a new metabolic biomarker for cancer stem cells: Identification of Vitamin C and CAPE as natural products targeting “stemness”. Oncotarget. 2017;8:20667–20678. doi: 10.18632/oncotarget.15400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Farnie G., Sotgia F., Lisanti M.P. High mitochondrial mass identifies a sub-population of stem-like cancer cells that are chemo-resistant. Oncotarget. 2015;6:30472–30486. doi: 10.18632/oncotarget.5401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lamb R., Bonuccelli G., Ozsvári B., Peiris-Pagès M., Fiorillo M., Smith D.L., Bevilacqua G., Mazzanti C.M., McDonnell L.A., Naccarato A.G., et al. Mitochondrial mass, a new metabolic biomarker for stem-like cancer cells: Understanding WNT/FGF-driven anabolic signaling. Oncotarget. 2015;6:30453–30471. doi: 10.18632/oncotarget.5852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ye X.Q., Wang G.H., Huang G.J., Bian X.W., Qian G.S., Yu S.C. Heterogeneity of Mitochondrial Membrane Potential: A Novel Tool to Isolate and Identify Cancer Stem Cells from a Tumor Mass? Stem Cell Rev. Rep. 2011;7:153–160. doi: 10.1007/s12015-010-9122-9. [DOI] [PubMed] [Google Scholar]
- 138.Han S., Wei R., Zhang X., Jiang N., Fan M., Huang J.H., Xie B., Zhang L., Miao W., Butler A.C.P., et al. CPT1A/2-Mediated FAO Enhancement—A Metabolic Target in Radioresistant Breast Cancer. Front. Oncol. 2019;9:1–15. doi: 10.3389/fonc.2019.01201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Li X., Wang Z., Zheng Y., Guan Y., Yang P., Chen X., Peng C., He J., Ai Y., Wu S., et al. Nuclear Receptor Nur77 Facilitates Melanoma Cell Survival under Metabolic Stress by Protecting Fatty Acid Oxidation. Mol. Cell. 2018;69:480–492.e7. doi: 10.1016/j.molcel.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 140.Muir A., Danai L.V., Vander Heiden M.G. Microenvironmental regulation of cancer cell metabolism: Implications for experimental design and translational studies. DMM Dis. Model. Mech. 2018;11 doi: 10.1242/dmm.035758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Davidson S.M., Papagiannakopoulos T., Olenchock B.A., Heyman J.E., Keibler M.A., Luengo A., Bauer M.R., Jha A.K., O’Brien J.P., Pierce K.A., et al. Environment impacts the metabolic dependencies of ras-driven non-small cell lung cancer. Cell Metab. 2016;23:517–528. doi: 10.1016/j.cmet.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lagziel S., Lee W.D., Shlomi T. Inferring cancer dependencies on metabolic genes from large-scale genetic screens. BMC Biol. 2019;17:1–11. doi: 10.1186/s12915-019-0654-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Cruz-Gil S., Sánchez-Martínez R., Wagner-Reguero S., Stange D., Schölch S., Pape K., de Molina A.R. A more physiological approach to lipid metabolism alterations in cancer: CRC-like organoids assessment. PLoS ONE. 2019;14 doi: 10.1371/journal.pone.0219944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Okkelman I.A., Neto N., Papkovsky D.B., Monaghan M.G., Dmitriev R.I. A deeper understanding of intestinal organoid metabolism revealed by combining fluorescence lifetime imaging microscopy (FLIM) and extracellular flux analyses. Redox Biol. 2020;30:101420. doi: 10.1016/j.redox.2019.101420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sharick J.T., Walsh C.M., Sprackling C.M., Pasch C.A., Pham D.L., Esbona K., Choudhary A., Garcia-Valera R., Burkard M.E., McGregor S.M., et al. Metabolic Heterogeneity in Patient Tumor-Derived Organoids by Primary Site and Drug Treatment. Front. Oncol. 2020;10:1–17. doi: 10.3389/fonc.2020.00553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Anderson A.S., Roberts P.C., Frisard M.I., Hulver M.W., Schmelz E.M. Ovarian tumor-initiating cells display a flexible metabolism. Exp. Cell Res. 2014;328:44–57. doi: 10.1016/j.yexcr.2014.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Diehn M., Cho R.W., Lobo N.A., Kalisky T., Dorie M.J., Kulp A.N., Qian D., Lam J.S., Ailles L.E., Wong M., et al. Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature. 2009;458:780–783. doi: 10.1038/nature07733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Ryoo I.G., Lee S.H., Kwak M.K. Redox Modulating NRF2: A Potential Mediator of Cancer Stem Cell Resistance. Oxid. Med. Cell. Longev. 2016;2016 doi: 10.1155/2016/2428153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tonelli C., Chio I.I.C., Tuveson D.A. Transcriptional Regulation by Nrf2. Antioxid. Redox Signal. 2018;29:1727–1745. doi: 10.1089/ars.2017.7342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Denicola G.M., Karreth F.A., Humpton T.J., Gopinathan A., Wei C., Frese K., Mangal D., Yu K.H., Yeo C.J., Calhoun E.S., et al. Oncogene-induced Nrf2 transcription promotes ROS detoxification and tumorigenesis. Nature. 2011;475:106–110. doi: 10.1038/nature10189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Duong H.Q., You K.S., Oh S., Kwak S.J., Seong Y.S. Silencing of NRF2 reduces the expression of ALDH1A1 and ALDH3A1 and sensitizes to 5-FU in pancreatic cancer cells. Antioxidants. 2017;6:52. doi: 10.3390/antiox6030052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ishimoto T., Nagano O., Yae T., Tamada M., Motohara T., Oshima H., Oshima M., Ikeda T., Asaba R., Yagi H., et al. CD44 Variant Regulates Redox Status in Cancer Cells by Stabilizing the xCT Subunit of System xc- and Thereby Promotes Tumor Growth. Cancer Cell. 2011;19:387–400. doi: 10.1016/j.ccr.2011.01.038. [DOI] [PubMed] [Google Scholar]
- 153.Fan Z., Wirth A.-K., Chen D., Wruck C.J., Rauh M., Buchfelder M., Savaskan N. Nrf2-Keap1 pathway promotes cell proliferation and diminishes ferroptosis. Oncogenesis. 2017;6:e371. doi: 10.1038/oncsis.2017.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Habib E., Linher-Melville K., Lin H.X., Singh G. Expression of xCT and activity of system xc- are regulated by NRF2 in human breast cancer cells in response to oxidative stress. Redox Biol. 2015;5:33–42. doi: 10.1016/j.redox.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Chang C.W., Chen Y.S., Tsay Y.G., Han C.L., Chen Y.J., Yang C.C., Hung K.F., Lin C.H., Huang T.Y., Kao S.Y., et al. ROS-independent ER stress-mediated NRF2 activation promotes warburg effect to maintain stemness-associated properties of cancer-initiating cells. Cell Death Dis. 2018;9:194. doi: 10.1038/s41419-017-0250-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hawkins K.E., Joy S., Delhove J.M.K.M., Kotiadis V.N., Fernandez E., Fitzpatrick L.M., Whiteford J.R., King P.J., Bolanos J.P., Duchen M.R., et al. NRF2 Orchestrates the Metabolic Shift during Induced Pluripotent Stem Cell Reprogramming. Cell Rep. 2016;14:1883–1891. doi: 10.1016/j.celrep.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Mitsuishi Y., Taguchi K., Kawatani Y., Shibata T., Nukiwa T., Aburatani H., Yamamoto M., Motohashi H. Nrf2 Redirects Glucose and Glutamine into Anabolic Pathways in Metabolic Reprogramming. Cancer Cell. 2012;22:66–79. doi: 10.1016/j.ccr.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 158.Zhang H.S., Zhang Z.G., Du G.Y., Sun H.L., Liu H.Y., Zhou Z., Gou X.M., Wu X.H., Yu X.Y., Huang Y.H. Nrf2 promotes breast cancer cell migration via up-regulation of G6PD/HIF-1α/Notch1 axis. J. Cell. Mol. Med. 2019;23:3451–3463. doi: 10.1111/jcmm.14241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Liu K., Lee J., Kim J.Y., Wang L., Tian Y., Chan S.T., Cho C., Machida K., Chen D., Ou J.H.J. Mitophagy Controls the Activities of Tumor Suppressor p53 to Regulate Hepatic Cancer Stem Cells. Mol. Cell. 2017;68:281–292.e5. doi: 10.1016/j.molcel.2017.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wang C., Shao L., Pan C., Ye J., Ding Z., Wu J., Du Q., Ren Y., Zhu C. Elevated level of mitochondrial reactive oxygen species via fatty acid β-oxidation in cancer stem cells promotes cancer metastasis by inducing epithelial-mesenchymal transition. Stem Cell Res. Ther. 2019;10:1–16. doi: 10.1186/s13287-019-1265-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kobayashi C.I., Suda T. Regulation of reactive oxygen species in stem cells and cancer stem cells. J. Cell. Physiol. 2012;227:421–430. doi: 10.1002/jcp.22764. [DOI] [PubMed] [Google Scholar]
- 162.Chen C., Liu Y., Liu R., Ikenoue T., Guan K.L., Liu Y., Zheng P. TSC-mTOR maintains quiescence and function of hematopoietic stem cells by repressing mitochondrial biogenesis and reactive oxygen species. J. Exp. Med. 2008;205:2397–2408. doi: 10.1084/jem.20081297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Shyh-Chang N., Zhu H., Yvanka De Soysa T., Shinoda G., Seligson M.T., Tsanov K.M., Nguyen L., Asara J.M., Cantley L.C., Daley G.Q. Lin28 enhances tissue repair by reprogramming cellular metabolism. Cell. 2013;155:778. doi: 10.1016/j.cell.2013.09.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Brown J.R., Chan D.K., Shank J.J., Griffith K.A., Fan H., Szulawski R., Yang K., Reynolds R.K., Johnston C., McLean K., et al. Phase II clinical trial of metformin as a cancer stem cell-targeting agent in ovarian cancer. JCI Insight. 2020;5:12. doi: 10.1172/jci.insight.133247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ivanova D., Zhelev Z., Getsov P., Nikolova B., Aoki I., Higashi T., Bakalova R. Vitamin K: Redox-modulation, prevention of mitochondrial dysfunction and anticancer effect. Redox Biol. 2018;16:352–358. doi: 10.1016/j.redox.2018.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Shank J.J., Yang K., Ghannam J., Cabrera L., Johnston C.J., Reynolds R.K., Buckanovich R.J. Metformin targets ovarian cancer stem cells in vitro and in vivo. Gynecol. Oncol. 2012;127:390–397. doi: 10.1016/j.ygyno.2012.07.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Shi P., Liu W., Tala T., Wang H., Li F., Zhang H., Wu Y., Kong Y., Zhou Z., Wang C., et al. Metformin suppresses triple-negative breast cancer stem cells by targeting KLF5 for degradation. Cell Discov. 2017;3 doi: 10.1038/celldisc.2017.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Zhang L., Xu L., Zhang F., Vlashi E. Doxycycline inhibits the cancer stem cell phenotype and epithelial-to-mesenchymal transition in breast cancer. Cell Cycle. 2017;16:737–745. doi: 10.1080/15384101.2016.1241929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Lamb R., Ozsvari B., Lisanti C.L., Tanowitz H.B., Howell A., Martinez-Outschoorn U.E., Sotgia F., Lisanti M.P. Antibiotics that target mitochondria effectively eradicate cancer stem cells, across multiple tumor types: Treating cancer like an infectious disease. Oncotarget. 2015;6:4569–4584. doi: 10.18632/oncotarget.3174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Matsumoto T., Uchiumi T., Monji K., Yagi M., Setoyama D., Amamoto R., Matsushima Y., Shiota M., Eto M., Kang D. Doxycycline induces apoptosis via ER stress selectively to cells with a cancer stem cell-like properties: Importance of stem cell plasticity. Oncogenesis. 2017;6:1–10. doi: 10.1038/s41389-017-0009-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Pusapati R.V., Daemen A., Wilson C., Sandoval W., Gao M., Haley B., Baudy A.R., Hatzivassiliou G., Evangelista M., Settleman J. mTORC1-Dependent Metabolic Reprogramming Underlies Escape from Glycolysis Addiction in Cancer Cells. Cancer Cell. 2016;29:548–562. doi: 10.1016/j.ccell.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 172.Cheong J.H., Park E.S., Liang J., Dennison J.B., Tsavachidou D., Nguyen-Charles C., Cheng K.W., Hall H., Zhang D., Lu Y., et al. Dual inhibition of tumor energy pathway by 2-deoxyglucose and metformin is effective against a broad spectrum of preclinical cancer models. Mol. Cancer Ther. 2011;10:2350–2362. doi: 10.1158/1535-7163.MCT-11-0497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Deng J., Peng M., Wang Z., Zhou S., Xiao D., Deng J., Yang X., Peng J., Yang X. Novel application of metformin combined with targeted drugs on anticancer treatment. Cancer Sci. 2019;110:23–30. doi: 10.1111/cas.13849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Iliopoulos D., Hirsch H.A., Struhl K. Metformin decreases the dose of chemotherapy for prolonging tumor remission in mouse xenografts involving multiple cancer cell types. Cancer Res. 2011;71:3196–3201. doi: 10.1158/0008-5472.CAN-10-3471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Issaq S.H., Teicher B.A., Monks A. Bioenergetic properties of human sarcoma cells help define sensitivity to metabolic inhibitors. Cell Cycle. 2014;13:1152–1161. doi: 10.4161/cc.28010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Wang Y., Xu W., Yan Z., Zhao W., Mi J., Li J., Yan H. Metformin induces autophagy and G0/G1 phase cell cycle arrest in myeloma by targeting the AMPK/mTORC1 and mTORC2 pathways. J. Exp. Clin. Cancer Res. 2018;37:1–12. doi: 10.1186/s13046-018-0731-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Howell J.J., Hellberg K., Turner M., Talbott G., Kolar M.J., Ross D.S., Hoxhaj G., Saghatelian A., Shaw R.J., Manning B.D. Metformin Inhibits Hepatic mTORC1 Signaling via Dose-Dependent Mechanisms Involving AMPK and the TSC Complex. Cell Metab. 2017;25:463–471. doi: 10.1016/j.cmet.2016.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Boysen G., Jamshidi-Parsian A., Davis M.A., Siegel E.R., Simecka C.M., Kore R.A., Dings R.P.M., Griffin R.J. Glutaminase inhibitor CB-839 increases radiation sensitivity of lung tumor cells and human lung tumor xenografts in mice. Int. J. Radiat. Biol. 2019;95:436–442. doi: 10.1080/09553002.2018.1558299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Li D., Fu Z., Chen R., Zhao X., Zhou Y., Zeng B., Yu M., Zhou Q., Lin Q., Gao W., et al. Inhibition of glutamine metabolism counteracts pancreatic cancer stem cell features and sensitizes cells to radiotherapy. Oncotarget. 2015;6:31151–31163. doi: 10.18632/oncotarget.5150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Samudio I., Harmancey R., Fiegl M., Kantarjian H., Konopleva M., Korchin B., Kaluarachchi K., Bornmann W., Duvvuri S., Taegtmeyer H., et al. Pharmacologic inhibition of fatty acid oxidation sensitizes human leukemia cells to apoptosis induction. J. Clin. Investig. 2010;120:142–156. doi: 10.1172/JCI38942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Choi H.J., Jhe Y.L., Kim J., Lim J.Y., Lee J.E., Shin M.K., Cheong J.H. FoxM1-dependent and fatty acid oxidation-mediated ROS modulation is a cell-intrinsic drug resistance mechanism in cancer stem-like cells. Redox Biol. 2020;36:101589. doi: 10.1016/j.redox.2020.101589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Harris I.S., Treloar A.E., Inoue S., Sasaki M., Gorrini C., Lee K.C., Yung K.Y., Brenner D., Knobbe-Thomsen C.B., Cox M.A., et al. Glutathione and Thioredoxin Antioxidant Pathways Synergize to Drive Cancer Initiation and Progression. Cancer Cell. 2015;27:211–222. doi: 10.1016/j.ccell.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 183.Arlt A., Sebens S., Krebs S., Geismann C., Grossmann M., Kruse M.L., Schreiber S., Schäfer H. Inhibition of the Nrf2 transcription factor by the alkaloid trigonelline renders pancreatic cancer cells more susceptible to apoptosis through decreased proteasomal gene expression and proteasome activity. Oncogene. 2013;32:4825–4835. doi: 10.1038/onc.2012.493. [DOI] [PubMed] [Google Scholar]
- 184.Rodman S.N., Spence J.M., Ronnfeldt T.J., Zhu Y., Solst S.R., O’Neill R.A., Allen B.G., Guan X., Spitz D.R., Fath M.A. Enhancement of Radiation Response in Breast Cancer Stem Cells by Inhibition of Thioredoxin- and Glutathione-Dependent Metabolism. Radiat. Res. 2016;186:385–395. doi: 10.1667/RR14463.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Tanaka G., Inoue K., Shimizu T., Akimoto K., Kubota K. Dual pharmacological inhibition of glutathione and thioredoxin systems synergizes to kill colorectal carcinoma stem cells. Cancer Med. 2016;5:2544–2557. doi: 10.1002/cam4.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Kouidhi S., Ayed F.B., Elgaaied A.B. Targeting tumor metabolism: A new challenge to improve immunotherapy. Front. Immunol. 2018;9:1–11. doi: 10.3389/fimmu.2018.00353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Harel M., Ortenberg R., Varanasi S.K., Mangalhara K.C., Mardamshina M., Markovits E., Baruch E.N., Tripple V., Arama-Chayoth M., Greenberg E., et al. Proteomics of Melanoma Response to Immunotherapy Reveals Mitochondrial Dependence. Cell. 2019;179:236–250.e18. doi: 10.1016/j.cell.2019.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Cascone T., McKenzie J.A., Mbofung R.M., Punt S., Wang Z., Xu C., Williams L.J., Wang Z., Bristow C.A., Carugo A., et al. Increased Tumor Glycolysis Characterizes Immune Resistance to Adoptive T Cell Therapy. Cell Metab. 2018;27:977–987.e4. doi: 10.1016/j.cmet.2018.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Meynet O., Ricci J.E. Caloric restriction and cancer: Molecular mechanisms and clinical implications. Trends Mol. Med. 2014;20:419–427. doi: 10.1016/j.molmed.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 190.Kusuoka O., Fujiwara-Tani R., Nakashima C., Fujii K., Ohmori H., Mori T., Kishi S., Miyagawa Y., Goto K., Kawahara I., et al. Intermittent calorie restriction enhances epithelial-mesenchymal transition through the alteration of energy metabolism in a mouse tumor model. Int. J. Oncol. 2018;52:413–423. doi: 10.3892/ijo.2017.4229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.De Francesco E.M., Ózsvári B., Sotgia F., Lisanti M.P. Dodecyl-TPP Targets Mitochondria and Potently Eradicates Cancer Stem Cells (CSCs): Synergy with FDA-Approved Drugs and Natural Compounds (Vitamin C and Berberine) Front. Oncol. 2019;9 doi: 10.3389/fonc.2019.00615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.De Francesco E.M., Bonuccelli G., Maggiolini M., Sotgia F., Lisanti M.P. Vitamin C and Doxycycline: A synthetic lethal combination therapy targeting metabolic flexibility in cancer stem cells (CSCs) Oncotarget. 2017;8:67269–67286. doi: 10.18632/oncotarget.18428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.De Carlo F., Witte T.R., Hardman W.E., Claudio P.P. Omega-3 Eicosapentaenoic Acid Decreases CD133 Colon Cancer Stem-Like Cell Marker Expression While Increasing Sensitivity to Chemotherapy. PLoS ONE. 2013;8:1–12. doi: 10.1371/journal.pone.0069760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Hegde S., Kaushal N., Ravindra K.C., Chiaro C., Hafer K.T., Gandhi U.H., Thompson J.T., Van Den Heuvel J.P., Kennett M.J., Hankey P., et al. Δ12-prostaglandin J3, an omega-3 fatty acid-derived metabolite, selectively ablates leukemia stem cells in mice. Blood. 2011;118:6909–6919. doi: 10.1182/blood-2010-11-317750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Weber D.D., Aminazdeh-Gohari S., Kofler B. Ketogenic diet in cancer therapy. Aging. 2018;10:164–165. doi: 10.18632/aging.101382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Martinez-Outschoorn U.E., Prisco M., Ertel A., Tsirigos A., Lin Z., Pavlides S., Wang C., Flomenberg N., Knudsen E.S., Howell A., et al. Ketones and lactate increase cancer cell “stemness”, driving recurrence, metastasis and poor clinical outcome in breast cancer: Achieving personalized medicine via metabolo-genomics. Cell Cycle. 2011;10:1271–1286. doi: 10.4161/cc.10.8.15330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Crofford O.B. Metformin. N. Engl. J. Med. 1995;333:588–589. doi: 10.1056/NEJM199508313330910. [DOI] [PubMed] [Google Scholar]
- 198.Owen M.R., Doran E., Halestrap A.P. Evidence that metformin exerts its anti-diabetic effects through inhibition of complex 1 of the mitochondrial respiratory chain. Biochem. J. 2000;348:607–614. doi: 10.1042/bj3480607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Ortmayr K., Dubuis S., Zampieri M. Metabolic profiling of cancer cells reveals genome-wide crosstalk between transcriptional regulators and metabolism. Nat. Commun. 2019;10 doi: 10.1038/s41467-019-09695-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Sinkala M., Mulder N., Patrick Martin D. Metabolic gene alterations impact the clinical aggressiveness and drug responses of 32 human cancers. Commun. Biol. 2019;2:1–14. doi: 10.1038/s42003-019-0666-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Zhang C., Aldrees M., Arif M., Li X., Mardinoglu A., Aziz M.A. Elucidating the Reprograming of Colorectal Cancer Metabolism Using Genome-Scale Metabolic Modeling. Front. Oncol. 2019;9 doi: 10.3389/fonc.2019.00681. [DOI] [PMC free article] [PubMed] [Google Scholar]