Abstract
Infections caused by Aspergillus species are being increasingly reported. Aspergillus flavus is the second most common species within this genus causing invasive infections in humans, and isolates showing azole resistance have been recently described. A. flavus has three cyp51-related genes (cyp51A, cyp51B, and cyp51C) encoding 14-α sterol demethylase-like enzymes which are the target of azole drugs. In order to study triazole drug resistance in A. flavus, three strains showing reduced azole susceptibility and 17 azole susceptible isolates were compared. The three cyp51-related genes were amplified and sequenced. A comparison of the deduced Cyp51A, Cyp51B, and Cyp51C protein sequences with other protein sequences from orthologous genes in different filamentous fungi led to a protein identity that ranged from 50% to 80%. Cyp51A and Cyp51C presented several synonymous and non-synonymous point mutations among both susceptible and non-susceptible strains. However, two amino acid mutations were present only in two resistant isolates: one strain harbored a P214L substitution in Cyp51A, and another a H349R in Cyp51C that also showed an increase of cyp51A and cyp51C gene expression compared to the susceptible strain ATCC2004304. Isolates that showed reduced in vitro susceptibility to clinical azoles exhibited a different susceptibility profile to demethylation inhibitors (DMIs). Although P214L substitution might contribute to azole resistance, the role of H349R substitution together with changes in gene expression remains unclear.
Keywords: Aspergillus flavus, Cyp51s, azole resistance mechanisms, azole drugs, DMIs fungicides
1. Introduction
Aspergillus spp. are opportunistic fungi that cause both allergic and invasive syndromes. The genus Aspergillus contains approximately 175 species, but only a few of them have been associated with human disease [1]. The primary route of infection is characterized by the inhalation of conidia which, due to their small size, easily reach the pulmonary alveoli and cause local and invasive infections [2]. Among the wide range of aspergillosis manifestations, invasive aspergillosis (IA) is the most severe one and is linked to high morbidity and mortality rates in immunocompromised patients [3,4,5]. Besides the risk of immunosuppressed patients to Aspergillus infections, sporadic cases of invasive aspergillosis on immunocompetent hosts have also been reported [6,7].
In general, aspergillosis is mainly caused by Aspergillus fumigatus, followed by A. flavus, Aspergillus terreus, Aspergillus niger and Aspergillus nidulans [8]. A. flavus has a wide environmental distribution favored by the formation of conidia that are highly tolerant to adverse conditions and is considered an important pathogen that is responsible for several diseases in humans [9]. In Spain, the FILPOP study reported A. fumigatus as the most frequently isolated species (48.5%), followed by A. flavus (8.4%), A. terreus (8.1%), Aspergillus tubingensis (6.8%), and A. niger (6.5%) [10]. An updated study in 2018 showed an increase in the frequency of isolation of A. fumigatus (52.74%), followed by A. niger (5.27%), A. flavus (5.07%), and A. terreus (4.67%) [11]. These species distribution can vary from country to country. For instance, A. flavus is more prevalent in Asia, Africa and the Middle East and it is considered the most frequent species causing aspergillosis in those areas [12]. Moreover, outbreaks associated with A. flavus appear to be produced by single or closely related strains, in contrast to those associated with A. fumigatus [9].
The first-line antifungal treatment against aspergillosis is broad-spectrum azole drugs, although polyenes and echinocandins are also included as alternative or salvage therapy, respectively [13]. Triazole drugs target the 14-α sterol demethylase (Cyp51), an enzyme that plays a key role in the ergosterol biosynthesis pathway [14]. However, the treatment of Aspergillus infections has recently become increasingly complicated because some species are developing resistance to antifungal drugs worldwide [15]. In A. fumigatus, the development of azole resistance has been mainly attributed to two different routes: (i) an in vivo or in-host acquisition that can happen after prolonged azole therapy and (ii) an acquisition in the environmental setting due to use of demethylation inhibitors (DMIs) fungicides which have a similar structure to clinical azoles implying cross-resistance between both of them [16,17]. Besides the clinical use of antifungals to treat A. flavus in human infections, the use of azoles in agriculture raises the concern about A. flavus azole resistance related to the use of this class of antifungals in the fields since it is also an important crop associated pathogen [18]. Fungicides are traditionally used to avoid food contaminations, such as A. flavus and other fungi that can be harmful for humans due to their ability to produce large amounts of mycotoxins [19].
In contrast to A. fumigatus, information regarding antifungal resistance mechanisms in A. flavus is relatively scarce. A. fumigatus has two Cyp51 isoenzymes, Cyp51A and Cyp51B [20]. Azole resistance in this fungus has been associated with the presence of several cyp51A point mutations and variations in the promoter [16]. An interesting difference between A. flavus and other Aspergillus species is the existence of a third Cyp51 protein, the Cyp51C [21]. Recently, A. flavus isolates with in vitro azole resistance have been described and azole resistance mechanisms in these strains are being analyzed. To date, different A. flavus Cyp51 point mutations have been described [22,23,24,25,26], however their role in azole resistance cannot be assumed since most of them were eventually described in azole susceptible strains. To date, only one point mutation (Y319H) in A. flavus Cyp51C seems to be related to azole resistance although it needs further confirmation [25].
The objective of this work was to sequence the three Cyp51 paralogues in several azole susceptible and resistant A. flavus clinical strains and to analyze the expression of the three genes during fungal growth. We also analyzed if the specific mutations found in each Cyp51 protein could be responsible for their resistance phenotype to azole drugs. The susceptibility of these A. flavus strains to different imidazoles and triazoles commonly used in crop protection was also tested and the hypothetical link between the development of resistance in agriculture and in the clinical setting for A. flavus isolates is discussed.
2. Materials and Methods
2.1. Strains and Molecular Identification
Twenty A. flavus isolates obtained from clinical samples were analyzed (Table 1). Fourteen strains belonged to the Mycology Reference Laboratory collection (CM) and six strains were obtained from the Hospital Universitario Central de Asturias (TP). Sample origin and year of isolation of all the A. flavus isolates are displayed in Supplementary Table S1. A. flavus ATCC2004304 was used as reference strain. Conidia from each strain were cultured in GYEP liquid medium (0.3% yeast extract, 1% peptone; Difco, Soria Melguizo, Madrid, Spain) with 2% glucose (Sigma-Aldrich Química, Madrid, Spain) for 24 h at 37 °C. After mechanical disruption of the mycelium by vortex-mixing with glass beads, genomic DNA of isolates was extracted using the phenol-chloroform method [27]. Molecular identification was performed by PCR amplifying and sequencing ITS1-5.8S-ITS2 regions and a portion of the β-tubulin gene [28].
Table 1.
Antifungal susceptibility profile of A. flavus isolates for various antifungal drugs. AmB, amphotericin B; ITC, itraconazole; VRC, voriconazole; POS, posaconazole; ISV, isavuconazole. In bold the A. flavus azole resistant strains. * Marked strains were previously tested in a preceding work [36].
| Strains | MICs Ranges (mg/L) | ||||
|---|---|---|---|---|---|
| AmB | ITC | VRC | POS | ISV | |
| ATCC2004304 | 1 | 0.5 | 2 | 0.125 | 1 |
| CM7668 * | 0.5 | >8 | 0.25 | 1–2 | 0.5 |
| CM8087 | 8–>16 | 4–8 | 8 | 0.5 | 8 |
| CM9165 | 1 | 0.25 | 0.5 | 0.125 | 0.25 |
| CM9174 | 2 | 0.5–1 | 1–4 | 0.125–0.25 | 2–4 |
| CM9189 | 1 | 0.5 | 1 | 0.25 | 1 |
| CM9195 | 1 | 0.25 | 1 | 0.125 | 1 |
| CM9228 | 1 | 0.5 | 0.5 | 0.25 | 2 |
| CM9267 | 2 | 0.5 | 1 | 0.25 | 1 |
| CM9298 | 1 | 0.5 | 1 | 0.125 | 1 |
| CM9326 * | 1–2 | 4–8 | 8 | 1–2 | >8 |
| CM9329 | 2 | 0.5 | 1 | 0.25 | 1 |
| CM9331 | 1 | 0.5 | 1 | 0.25 | 2 |
| CM9684 | 0.5 | 1 | >8 | 0.25 | 2 |
| TP642 | 1 | 1 | 2 | 0.25 | 2 |
| TP968 | 1 | 1–2 | 4 | 0.5–1 | 4 |
| TP992 | 1 | 0.5 | 2 | 0.25 | 1 |
| TP1004 | 1 | 1 | 4 | 0.5 | 4 |
| TP1115 | 1 | 1 | 4 | 0.5 | 4 |
| TP1179 | 1 | 1 | 4 | 0.5 | 4 |
Note: isolates with ITC MIC > 1 mg/L were considered resistant and selected for futher studies.
2.2. Antifungal Susceptibility Testing (AFST)
Microdilution testing was performed according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) standard methodology [29,30]. A. fumigatus ATCC2004305 and A. flavus ATCC2004304 were used as quality control strains. Antifungal agents used in the study were amphotericin B (AmB) (Sigma-Aldrich Química, Madrid, Spain), itraconazole (ITC) (Janssen Pharmaceutica, Madrid, Spain), voriconazole (VRC) (Pfizer SA, Madrid, Spain), posaconazole (POS) (Schering-Plough Research Institute, Kenilworth, NJ, USA), isavuconazole (ISV) (Basilea Pharmaceutica, Basel, Switzerland), terbinafine (TBR) (Novartis, Basel, Switzerland), caspofungin (Merck & Co., Inc., Rahway, NJ, USA), micafungin (Astellas Pharma, Inc., Tokyo, Japan), and anidulafungin (Pfizer SA, Madrid, Spain). The final concentrations tested ranged from 0.03 to 16 mg/L for amphotericin B, terbinafine, and caspofungin; from 0.015 to 8 mg/L for itraconazole, voriconazole, and posaconazole; from 0.008 to 4 mg/L for anidulafungin; and from 0.004 to 2 mg/L for micafungin. Microdilution plates were incubated at 35 °C for 48 h in a humid atmosphere. Visual readings were performed at 24 and 48 h with the help of a mirror. The endpoint for amphotericin B, itraconazole, voriconazole, posaconazole, isavuconazole, and terbinafine was the antifungal concentration that produced a complete inhibition of visual growth at 24 and 48 h (MIC). For the echinocandins, the endpoint was the antifungal concentration that produced a visible change in the morphology of the hyphae compared with the growth control well (minimum effective concentration (MEC)). EUCAST has set breakpoints for the interpretation of antifungal susceptibility testing results, although they have only been set for itraconazole and isavuconazole for A. flavus strains (MICs of ≤1 μg/mL susceptible and >1–2 Resistant). EUCAST breakpoint values set for other antifungals for A. fumigatus strains were used as a reference but taking into account that the epidemiological cut-off values (ECOFFs) [31] established for A. flavus strains are one dilution higher than for A. fumigatus: 0.5 mg/L for posaconazole (POS), and 4 mg/L for voriconazole (VRC). Strains were selected for further study if they were ITC resistant (ITC MIC >1 mg/L).
2.3. Susceptibility Testing to 14-α Sterol Demethylase Inhibitors (DMIs)
Two imidazole drugs, prochloraz and imazalil, and five triazole drugs, metconazole, tebuconazole, epoxiconazole, difenoconazole, bromuconazole and myclobutanil (Sigma-Aldrich Quimica SA, Madrid, Spain), that belong to the 14-α sterol demethylation inhibitors (DMIs) and are frequently used to protect crops, were tested following the EUCAST methodology. The final concentrations of each azole drug tested ranged from 0.06 to 32 mg/L. The plates were incubated at 35 °C for 48 h in a humid atmosphere. Visual readings were performed at 24 and 48 h with the help of a mirror. The endpoint for all of them was the antifungal concentration that produced a complete inhibition of visual growth at 24 and 48 h (MIC).
2.4. PCR Amplification and Sequence Analysis of the cyp51A, cyp51B and cyp51C Genes
The cyp51A, cyp51B and cyp51C genes, including their promoter region, were amplified and sequenced using the primers described in Supplementary Table S2. PCR conditions for amplification of each cyp51 gene were described before [32] although the annealing temperature varied depending on the primer combination. Specific conditions for cyp51A amplification were 1 cycle of 5 min at 94 °C and then 35 cycles of 30 s at 94 °C, 45 s at 54 °C for F1 and R1, 55 °C for F2 and R2, F3 and R3, F4 and R4, 2 min at 72 °C and, finally, 5 min at 72 °C. Specific conditions for cyp51B amplification were 1 cycle of 5 min at 94 °C and then 35 cycles of 30 s at 94 °C, 45 s at 60 °C for F1, and R4, 2 min at 72 °C and, finally, 5 min at 72°C. The parameters used for cyp51C amplification were 1 cycle of 5 min at 94 °C and then 35 cycles of 30 s at 94 °C, 45 s at 58 °C for 1_F and 2_R, 54 °C for 3_F and 4_R, 52 °C for 5_F and 6_R, 54 °C for 7_F and 8_R, 2 min at 72 °C and, finally, 5 min at 72 °C. To exclude the possibility that any change identified in the sequences was due to PCR-induced errors, each isolate was independently analyzed twice.
2.5. RNA Isolation, Reverse Transcription and Quantitative PCR (RT-qPCR)
The A. flavus inocula were added to 100 mL of minimal medium broth [33] reaching a final concentration of 106/mL total conidia and grown 18 h at 150 rpm at 37 °C. Then, mycelium was harvested using a funnel and miracloth paper (CalbiochemR, Merck Millipore, Spain). Mycelial samples were blot dried, frozen in liquid nitrogen, and ground to powder using a pestle and a mortar. RNA was isolated from mycelial powder by using an RNeasy plant minikit (Qiagen, Madrid, Spain) and following manufacturer’s instructions. cDNA was obtained through reverse transcription using the commercial ImProm-IITM Reverse Transcription System kit (Promega, Madison, WI, USA). The PCR reaction mixture was prepared following manufacturer’s instructions (1μg of cellular RNA, 1 µg/mL of the primers (dT), 4.5 µL of RNase-free water, 4 µL of reaction buffer ImProm-II (5×), 4 µL of MgCl2, 1 µL of dNTPs, 0.5 µL of the ribonucleases inhibitor, rRNasin® (Promega, Madison, WI, USA), and 1 µL of reverse transcriptase, ImProm-IITM (Promega, Madison, WI, USA), in a total volume of 20 µL. The reverse transcription was performed in a GeneAmp PCR System 9700 (Applied Biosystems, Foster City, CA, USA) by using the following program parameters: 5 min at 25 °C, 60 min at 42 °C, and 15 min at 70 °C. cDNA was diluted in RNase-free water (1:5) for qPCR.
Quantitative PCR (qPCR) was performed to determine the differences in relative expression of cyp51 genes between azole resistant and azole susceptible A. flavus isolates. The A. flavus β-tubulin gene was used as housekeeping gene. Specific primers for the qPCR (Supplementary Table S2) were designed and PCR conditions were standardized and optimized for each primer pair. After cDNA synthesis, qPCR mixtures were carried out with SensiMix SYBR-Hi carboxy-X-rhodamine (Bioline, Barcelona, Spain). The PCR conditions were 10 min at 95 °C and 40 cycles of 10 s at 95 °C, 5 s at 58 °C, and 30 s at 72 °C. Each assay was conducted in triplicates with RNA isolated from two biological replicas. Fold changes of gene expression were calculated using the 2(−ΔCt) method for individual time points and normalized to the β-tubulin gene [34]. Fold changes in gene expression were calculated relative to cyp51A of the ATCC20044304 strain.
2.6. Sequence Computer Analysis
All sequence analyses were carried out using DNAstar software package, DNASTAR™ Lasergene Genomics Suite Software, (DNASTAR, Inc., Madison, WI, USA). Nucleotide sequences were analyzed using EditSeq and SeqMan and the amino acid sequences of the putative 14-α demethylase Cyp51A, Cyp51B, and Cyp51C proteins were deduced from nucleotide sequences using SeqBuilder.
2.7. Phylogenetic Analysis
Phylogenetic trees were obtained by maximum likelihood analysis [35] using InfoQuestTH FP software, version 4.5 (Bio-Rad laboratories Inc, Hercules, CA, USA). Deduced proteins sequence of Cyp51A A. flavus NRRL3357(NCBI accession number XP_002375123); A. flavus AF70=MYA-384/AF70, (NCBI accession number KOC13200); Aspergillus oryzae RIB40 (NCBI accession number XP_001819419), Cyp51B (A. flavus NRRL3357 (NCBI accession number XP_002379130); A. flavus AF70 (NCBI accession number KOC13803) and A. oryzae RIB40 (NCBI accession number XP_001822241) and Cyp51C A. flavus NRRL3357(NCBI accession number XP_002383931); A. flavus AF70, (NCBI accession number KOC15064) and A. oryzae RIB40 (NCBI accession number XP_001824687) were compared with the amino acid sequences derived from Cyp51 proteins from other filamentous fungi, including other Aspergillus species, Penicillium spp., Fusarium spp., and other plant pathogens: A. fumigatus AfCyp51A; (NCBI accession number AAK73659); A. fumigatus AfCyp51B (NCBI accession number AAK73660); A. terreus AtCyp51A (NCBI accession number EAU33678); A. terreus AtCyp51B (NCBI accession number EAU36124); Fusarium graminearum FgCyp51A (NCBI accession number ESU09049); FgCyp51B (NCBI accession number EWZ31250) and FgCyp51C NCBI accession number ESU17718); Fusarium oxysporum FoCyp51A (NCBI accession number RKK94077), FoCyp51B (NCBI accession number EWY82136) and FoCyp51C (NCBI accession number EWY82136); Penicillium italicum PiCyp51 (NCBI accession number CAA89824); Penicillium digitatum PdCyp51 (NCBI accession number CAD277993); Oculimacula yallundae OyCyp51 (NCBI accession number AAG44831); Oculimacula acuformis OaCyp51 (NCBI accession number AAF18468); Neurospora crassa NcCyp51 (NCBI accession number EAA34813.); Erysiphe necátor EnCyp51 (NCBI accession number AAD55135).
3. Results
3.1. Antifungal Susceptibility Testing
Using the EUCAST methodology, all A. flavus strains but three were susceptible to azole drugs tested, showing some strain-dependent variations (Table 1). Three strains (CM7668, CM8087 and CM9326) were considered resistant to azole drugs with three different susceptibility profiles. There were no major differences in susceptibility to amphotericin B (AmB) except for one strain (CM8087) that could be considered AmB resistant. No differences were found in susceptibility to either echinocandins or terbinafine (results not shown).
3.2. Susceptibility Testing to 14-α Sterol Demethylase Inhibitors (DMIs) Fungicides
A. flavus susceptibility to each DMI antifungal drug is presented in Table 2. All strains but three exhibited MIC values to DMI fungicides similar to those of the A. flavus wild type strain (ATCC2004304), which is considered as a reference strain for EUCAST antifungal susceptibility testing. Two strains (CM8087 and CM9326) had higher MIC values to all imidazole and triazole drugs and one strain (CM7668) could be considered as hyper-susceptible to all DMIs.
Table 2.
Antifungal susceptibility profile of A. flavus isolates to imidazole and triazole demethylase inhibitors (DMIs). In bold the A. flavus azole resistant strains.
| A. flavus strains | MICs Ranges (mg/L) | |||||||
|---|---|---|---|---|---|---|---|---|
| Imidazole | Triazole | |||||||
| Imazalil | Prochloraz | Metconazole | Tebuconazole | Epoxiconazole | Bromuconazole | Difenoconazole | Myclobutanil | |
| ATCC2004304 | 1–2 | 2–4 | 4–8 | 8 | 8–16 | 4–16 | 8–>32 | >32 |
| CM7668 | 0.25 | 1 | 1 | 1 | 0.5–1 | 0.25–1 | 0.5–1 | 4 |
| CM8087 | 16 | >32 | >32 | >32 | >32 | >32 | >32 | >32 |
| CM9165 | 2 | 1 | 8 | 8 | 8 | 8 | 16 | >32 |
| CM9174 | 4 | 2 | 16 | 16 | 32 | 8 | 16 | >32 |
| CM9189 | 2 | 1 | 8 | 8 | 8 | 8 | 16 | >32 |
| CM9195 | 2 | 1 | 8 | 4 | 8 | 8 | 16 | >32 |
| CM9228 | 2 | 1 | 8 | 4 | 8 | 8 | 16 | 32 |
| CM9267 | 2 | 2 | 8 | 8 | 8 | 16 | 16 | >32 |
| CM9298 | 2 | 2 | 8 | 4 | 8 | 8 | 16 | >32 |
| CM9326 | 32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 |
| CM9329 | 1 | 1 | 4 | 4 | 8 | 8 | 16 | 32 |
| CM9331 | 2 | 1 | 8 | 8 | 16 | 8 | 32 | >32 |
| CM9684 | 8 | 2–4 | 16 | 16 | 16–>32 | 32–>32 | 16–>16 | >32 |
| TP642 | 8 | 8 | 16 | 16 | >32 | 32 | >32 | >32 |
| TP968 | 8 | 32 | 16 | 32 | >32 | 16 | 32 | >32 |
| TP992 | 2 | 2 | 8 | 4 | 16 | 8 | >32 | >32 |
| TP1004 | 8 | 8 | 16 | 16 | >32 | >32 | >32 | >32 |
| TP1115 | 8 | 8 | 16 | 16 | >32 | >32 | >32 | >32 |
| TP1179 | 8 | 8 | 16 | 32 | >32 | >32 | >32 | >32 |
3.3. Sequence Analysis of cyp51A, cyp51B and cyp51C Genes
The three Cyp51 paralogues possess a different number of introns with different sizes. The GeneBank accession Numbers of all A. flavus cyp51A, cyp51B and cyp51C sequences are displayed in Supplementary Table S3.
3.3.1. Aspergillus flavus Cyp51A
Gene cyp51A is 1591 bp long, with one intron of 67 bp (from base 194 to base 260) and that translates into 507 aa. The cyp51A sequences from strain ATCC2004304, A. flavus NRRL3357 (GenBank: XM_002375082.1), A. flavus AF70, and A. oryzae RIB40, were used as reference for comparison. The first 18 bp (atgatcttctcacgcagc) encoding six amino acid (MIFSRS) were excluded from the A. flavus NRRL3357 sequence because they did not match the other sequences (AF70 or RIB40). Changes in the cyp51A full coding sequence and derived amino acid sequences are displayed in Table 3. Several synonymous and non-synonymous point mutations were found among both susceptible and non-susceptible strains. One azole resistant strain (CM7668) harbored a c641t base change, resulting in a P214L point mutation that was only present in this strain, previously described in a recent work [36].
Table 3.
Aspergillus flavus Cyp51A analysis. The sequence of A. flavus NRRL3357 type strain was used as Reference. In bold the A. flavus azole resistant strains.
| Strains | A * | Aspergillus flavus Cyp51A | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| c132t | c165t | c342t | g390a | t546c | g595a | c641t | t723c | c738t | t907c | t927c | g966t | a985g | c1065t | t1164c | c1368t | g1371a | ||
| F44 | P55 | G114 | K130 | F182 | A199T | P214L 1 | Y241 | N246 | L303 | P309 | K322N | T329A | H355 | P388 | N456 | L456 | ||
| CM7668 | R | c165t | g390a | t546c | c641t | t1164c | ||||||||||||
| CM8087 | R | c165t | g390a | t546c | a985g | t1164c | ||||||||||||
| CM8098 | S | c165t | g390a | t546c | a985g | t1164c | ||||||||||||
| CM9165 | S | c165t | t546c | t723c | t1164c | |||||||||||||
| CM9174 | S | c165t | g390a | t546c | a985g | t1164c | ||||||||||||
| CM9189 | S | c165t | g390a | t546c | t1164c | |||||||||||||
| CM9195 | S | c165t | g390a | t546c | t1164c | |||||||||||||
| CM9228 | S | t546c | t907c | g966t | t1164c | |||||||||||||
| CM9267 | S | c165t | g390a | t546c | t1164c | |||||||||||||
| CM9298 | S | c132t | c165t | c342t | g390a | t546c | t927c | t1164c | c1368t | |||||||||
| CM9326 | R | c165t | g390a | t546c | t1164c | |||||||||||||
| CM9329 | S | c165t | g390a | t546c | t1164c | |||||||||||||
| CM9331 | S | c165t | g390a | t546c | t1164c | |||||||||||||
| CM9684 | S | c165t | g390a | t546c | a985g | t1164c | ||||||||||||
| TPH642 | S | c165t | g390a | t546c | t1164c | |||||||||||||
| TPH968 | S | c165t | g390a | t546c | t1164c | |||||||||||||
| TPH992 | S | c165t | g390a | t546c | t1164c | |||||||||||||
| TPH1004 | S | c165t | g390a | t546c | t1164c | |||||||||||||
| TPH1115 | S | c165t | g390a | t546c | t1164c | |||||||||||||
| TPH1179 | S | c165t | g390a | t546c | t1164c | |||||||||||||
| ATCC2004304 | S | c165t | g390a | t546c | g595a | c1065t | t1164c | c1368t | g1371a | |||||||||
| A. oryzae RIB40 | - | c165t | g390a | t546c | g595a | c1065t | t1164c | c1368t | g1371a | |||||||||
| A. flavus AF70 | - | c165t | g390a | t546c | c738t | t1164c | c1368t | |||||||||||
| Protein | F44 | P55 | G114 | K130 | F182 | A199T | P214L 1 | Y241 | N246 | L303 | P309 | K322N | T329A | H355 | P388 | N456 | L456 | |
* A, azole drugs profile, S susceptible, R Resistant. 1 This mutation was previously described in a recent work [36].
3.3.2. Aspergillus flavus Cyp51B
Gene cyp51B is 1740 bp long, with three introns: the first one of 54 bp (from base 247 to base 300), the second one of 58 bp (from base 499 to base 556) and the last one of 53 bp (from base 1616 to base 1668) that translates into 524 aa. Cyp51B sequences from strain ATCC2004304, A. flavus NRRL3357, A. flavus AF70 and A. oryzae RIB40 were used as reference sequences. Changes in the cyp51B full coding sequence and derived amino acid sequences are displayed in Table 4. This protein only harbored four synonymous mutations and showed a fully conserved amino acid sequence in all azole susceptible and resistant A. flavus strains.
Table 4.
Aspergillus flavus Cyp51B analysis. The sequence of A. flavus NRRL3357 was used as reference. In bold the A. flavus azole resistant strains.
| Strains | A * | Aspergillus flavus Cyp51B | |||
|---|---|---|---|---|---|
| c237t | c498t | t699c | a799g | ||
| C79 | I166 | N233 | K267 | ||
| CM7668 | R | ||||
| CM8087 | R | ||||
| CM9165 | S | c237t | c498t | a799g | |
| CM9174 | S | ||||
| CM9189 | S | c498t | |||
| CM9195 | S | c498t | |||
| CM9228 | S | c498t | |||
| CM9267 | S | ||||
| CM9298 | S | c498t | |||
| CM9326 | R | c498t | |||
| CM9329 | S | ||||
| CM9331 | S | c498t | |||
| CM9684 | S | t699c | |||
| TPH642 | S | ||||
| TPH968 | S | ||||
| TPH992 | S | ||||
| TPH1004 | S | ||||
| TPH1115 | S | ||||
| TPH1179 | S | ||||
| ATCC2004304 | S | ||||
| A. oryzae RIB40 | - | ||||
| A. flavus AF70 | - | c498t | a799g | ||
| Protein | C79 | I166 | N233 | K267 | |
* A, azole drugs profile, S susceptible, R, Resistant.
3.3.3. Aspergillus flavus Cyp51C
Gene cyp51C is 1612 bp long, with one 70 bp intron (from base 197 to base 266) and translates into 513 aa. Cyp51C sequences from strain ATCC2004304, A. flavus NRRL3357, A. flavus AF70 and A. oryzae RIB40 were used as reference. Changes in the cyp51C full coding sequence and derived amino acid sequences are displayed in Table 5. Several synonymous and non-synonymous point mutations were found among both susceptible and non-susceptible strains. One azole resistant strain (CM9326) showed an a1046g base change resulting in a H349R point mutation that was only present in this strain, previously described in a recent work [36].
Table 5.
Aspergillus flavus Cyp51C analysis. The sequence of A. flavus NRRL3357 (Type strain) was used as Reference. In bold the A. flavus azole resistant strains.
| Strains | A * | Aspergillus flavus Cyp51C | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| t161c | c174g | t718g | c748t | g760a | a761g | c826a | a853g | t876g | t894a | g915a | c978t | a1044g | a1046g | c1158t | g1196t | a1263g | a1267g | a1455g | ||
| M54T | G58G | S240A | R250ST | D254N | D254G | P276T | I285V | A292A | S298S | M305I | L326 | L348 | H349R 1 | S386 | S399I | E421 | N423D | V485V | ||
| CM7668 | R | t161c | c174g | t718g | a761g | c978t | a1044g | c1158t | a1263g | a1267g | ||||||||||
| CM8087 | R | t161c | c174g | t718g | ||||||||||||||||
| CM9165 | S | t161c | c174g | t718g | ||||||||||||||||
| CM9174 | S | t161c | c174g | t718g | ||||||||||||||||
| CM9189 | S | t161c | c174g | t718g | a761g | c826a | a853g | t876g | t894a | c1158t | a1263g | a1267g | ||||||||
| CM9195 | S | t161c | c174g | t718g | a761g | c978t | a1044g | c1158t | a1263g | a1267g | ||||||||||
| CM9228 | S | t161c | c174g | t718g | c748t | g1196t | ||||||||||||||
| CM9267 | S | t161c | c174g | t718g | a761g | c978t | a1044g | c1158t | a1263g | a1267g | ||||||||||
| CM9298 | S | t161c | c174g | t718g | a761g | c978t | a1044g | c1158t | a1263g | a1267g | ||||||||||
| CM9326 | R | t161c | c174g | t718g | a1046g | |||||||||||||||
| CM9329 | S | t161c | c174g | t718g | a761g | c978t | a1044g | c1158t | a1263g | a1267g | ||||||||||
| CM9331 | S | t161c | c174g | t718g | g760a | c826a | a853g | t876g | t894a | c1158t | a1263g | a1267g | ||||||||
| CM9684 | S | t161c | c174g | t718g | ||||||||||||||||
| TPH642 | S | t161c | c174g | t718g | a761g | c978t | a1044g | c1158t | a1263g | a1267g | ||||||||||
| TPH968 | S | t161c | c174g | t718g | a761g | c978t | a1044g | c1158t | a1263g | a1267g | ||||||||||
| TPH992 | S | t161c | c174g | t718g | a761g | c978t | a1044g | c1158t | a1263g | a1267g | ||||||||||
| TPH1004 | S | t161c | c174g | t718g | a761g | c978t | a1044g | c1158t | a1263g | a1267g | ||||||||||
| TPH1115 | S | t161c | c174g | t718g | a761g | c978t | a1044g | c1158t | a1263g | a1267g | ||||||||||
| TPH1179 | S | t161c | c174g | t718g | a761g | c978t | a1044g | c1158t | a1263g | a1267g | ||||||||||
| ATCC ** | S | t161c | c174g | t718g | g760a | a853g | t876g | t894a | c1158t | a1455g | ||||||||||
| RIB40 *** | - | t161c | c174g | t718g | ||||||||||||||||
| AF70 | - | t161c | c174g | t718g | g760a | g915a | c1158t | a1263g | a1267g | |||||||||||
| Protein | M54T | G58G | S240A | R250ST | D254N | D254G | P276T | I285V | A292A | S298S | M305I | L326 | L348 | H349R 1 | S386 | S399I | E421 | N423D | V485V | |
* A, azole drugs profile, S susceptible, R, Resistant. ** Reference strain A. flavus ATCC2004304. *** A. oryzae. 1 This mutation was previously described in a recent work [36].
3.4. Aspergillus flavus cyp51 Genes Expression
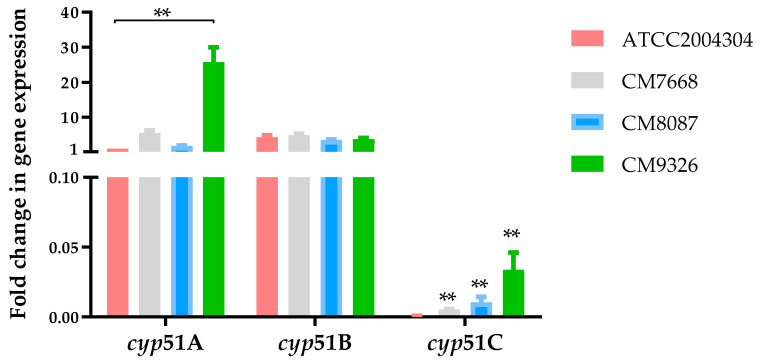
RT-PCR amplification was initially conducted to show that all cyp51 genes were expressed during hyphal growth (Supplementary Figure S1). Then, a quantitative PCR (qPCR) was performed to determine differences in relative expression of cyp51 genes between azole resistant (CM7668, CM8087 and CM9326) and the azole susceptible A. flavus ATCC2004304 strains (Figure 1). The expression of cyp51A was relatively similar between the strain ATCC2004304 and CM7668 and CM8087 strains. However, a significant increase of cyp51A expression was observed in the CM9326 isolate (p < 0.001). No differences of gene expression for the cyp51B were observed between all four isolates. Notably, the cyp51C gene was less expressed among all the strains (fold change of gene expression <500) compared to cyp51A or cyp51B. Although cyp51Cwas expressed in very low levels, we observed a significant increase of gene expression for all strains relative to the ATCC2004304 (Figure 1).
Figure 1.
Fold change in gene expression of cyp51A, cyp51B and cyp51C in the ATCC2004304, CM7668, CM8087 and CM9326 A. flavus strains. Gene expression values are represented as bar plots with mean +SD. P-values were calculated using the Mann–Whitney U test, p-values of statistical tests are shown within the graphs. ** p < 0.001.
3.5. Sequence Analysis: Alignments and Similarity
The deduced 507 amino-acid protein encoded by the 1521-bp coding sequence of A. flavus cyp51A gene was compared to the known complete amino acid sequences of different fungal Cyp51 proteins including Aspergillus species, Penicillium spp., Fusarium spp., and other plant pathogens. The strongest identities were shown with A. terreus Cyp51A (80.59%), A. fumigatus Cyp51A (77.60%), A. flavus Cyp51C (77%), Penicillium spp. Cyp51 (70%), Fusarium spp. Cyp51s (68 %), and A. flavus Cyp51B (58%). Homology with other plant pathogens, such as N. crassa, O. yallundae, O. acuformis, E. necátor, Venturia inaequalis, and Venturia nashicola, was around 58%.
The deduced 524 amino-acid protein encoded by the coding sequence of A. flavus cyp51B gene was compared to the known complete amino acid sequences of fungal Cyp51s. A strong identity was shown with A. terreus Cyp51B (84%), A. fumigatus Cyp51B (84%), P. italicum Cyp51 (78%), Fusarium spp. Cyp51s (63%), A. flavus Cyp51A (58%), and A. flavus Cyp51C (57%), while a range between 59% and 61% was shown with N.crassa, O. yallundae, O. acuformis, E. necátor, V. inaequalis, and V. nashicola.
The deduced 513-amino-acid protein encoded by the coding sequence A. flavus cyp51C gene was compared to the known complete amino acid sequences of fungal Cyp51s. A strong identity was shown with A. fumigatus Cyp51A (78%), A. flavus Cyp51A (77.56%), A. terreus Cyp51A (74.71%), Penicillium spp. Cyp51 (68%), Fusarium spp. Cyp51s (66%), A. flavus Cyp51B (60%), and A. fumigatus Cyp51B (60%). Identity to other plant pathogens ranged between 55% and 57%.
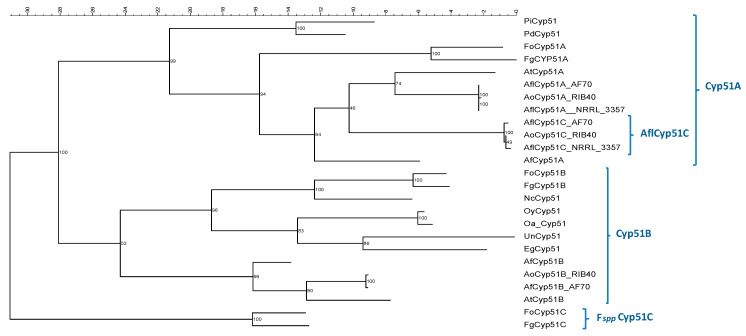
3.6. Phylogenetic Analysis
The phylogenetic tree derived from the comparison of Cyp51′s protein sequences from A. flavus with those from other Aspergillus spp. and other fungal pathogens is shown in Figure 2. Well defined clusters could be detected for the Cyp51B-derived proteins and for the Cyp51A-derived proteins. However, the A. flavus Cyp51C sequences fall in a sub-cluster within the Cyp51A cluster. Interestingly, Fusarium spp. Cyp51C formed an independent cluster from Cyp51A or Cyp51B proteins.
Figure 2.
Phylogenetic tree obtained by maximum likelihood analysis. The bootstrap consensus tree was inferred from 2000 replicates to represent the phylogeny. The deduced amino acid sequence of the A. flavus Cyp51A, Cyp51B and Cyp51C; A. oryzae Cyp51A, Cyp51B and Cyp51C; A. fumigatus AfCyp51A and AfCyp51B; A. terreus AtCyp51A and AtCyp51B; F. graminearum FgCyp51A, FgCyp51B and FgCyp51C; F. oxysporum FoCyp51A, FoCyp51B and FoCyp51C; P. italicum PiCyp51 and P. digitatum PdCyp51; O. yallundae OyCyp51 and O. acuformis OaCyp51; N. crassa NcCyp51; E. graminis EgCyp51; and U. necátor UnCyp51.
4. Discussion
The emergence of A. fumigatus azole resistance is becoming an important issue worldwide [16]. Less frequently, cases of azole resistance in A. flavus have started to be described, originating a similar concern as A. flavus is the second most common Aspergillus spp., causing invasive infections in immunocompromised patients and the most frequent isolated species in some regions of the globe [12]. The extensive and prolonged use of azole drugs in immunocompromised patients has been reported as the main cause of the selection of azole resistant A. fumigatus strains [37]. Moreover, the agricultural industry uses pesticides, mainly azole fungicides, to optimize food production, and several studies have suggested an environmental route of A. fumigatus azole resistance through the exposure to azole fungicides in agriculture [38]. Although a similar phenomenon has never been described for A. flavus, this is an important issue because A. flavus produces aflatoxin which contaminates food and livestock feed resulting in significant annual crop losses internationally [39]. For this reason, fungicides, including azole fungicides (DMIs), are commonly used for crop protection [40,41]. Therefore, both the antifungal clinical use to treat A. flavus human infections and the use of azoles in agriculture raise the concern about A. flavus azole resistance emergence. Regardless of the route of development of azole resistance, the undesirable consequence of that event would be treatment failure [42].
Azole susceptibility in clinical and environmental A. flavus strains has been evaluated in several studies, although percentages of azole resistance are quite variable depending on the country and the study [12]. This variability could be due to the criteria used to establish susceptibility or resistance. According to EUCAST [31], A. flavus clinical breakpoints to azoles have only been established for itraconazole (ITC) (isolates are considered resistant with ITC MIC > 1 mg/L) and isavuconazole (ISV) (isolates are considered resistant with ISV MIC > 2 mg/L). ECOFFs are used for the rest of antifungals, and in general they are considered one step higher than for A. fumigatus: 0.5 mg/L for posaconazole (POS), and 4 mg/L for voriconazole (VRC). We considered azole resistance only if resistance to ITC was present. Considering these criteria in our study, only three of the A. flavus strains showed a reduced in vitro susceptibility to ITC. However, their susceptibility profile was quite different: the CM7668 strain was resistant to ITC and POS but not to VRC or ISV; strain CM9326 was resistant to all azole drugs and strain CM8087 was resistant to all azoles as well as Amphotericin B (AmB) (Table 1). Because azole resistance development has also been related to the use of DMIs in the field, we tested the most frequently used drugs to protect crops: imidazoles and triazoles (Table 2). Cross resistance between clinical azoles and DMIs was shown in the strains CM8087 and CM9326, which had elevated MICs to all the DMIs evaluated. However, the strain CM7668 showed lower MICs for all DMIs tested. This result indicates that different azole resistance mechanisms might be operating in these strains.
Following what has been established for A. fumigatus, one of the most studied species regarding amino acid substitutions in Cyp51 proteins, we studied the Cyp51 proteins in A. flavus. A key difference between A. flavus and other Aspergillus species is the existence of a third paralog in A. flavus, named cyp51C [24]. In contrast, other Aspergillus spp. and most filamentous fungi possess two Cyp51 proteins, Cyp51A and Cyp51B, although some species have only one [43]. Phylogenetic analysis shows that Cyp51B enzymes and all Cyp51s of those species with only one enzyme form a clear sub-group in the phylogenetic tree (Figure 2). Another subgroup contains all Cyp51As and includes A. flavus Cyp51C. This Cyp51C is relatively similar to A. flavus Cyp51A (77%) and it has been described in previous phylogenetic studies as a second Cyp51A [43]. The existence of this third paralog in A. flavus could explain why A. flavus has higher MICs to all azole drugs, compared to A. fumigatus, as the inhibition of the three enzymes would be needed. Recent studies have shown that Fusarium spp. also have three Cyp51 paralogues (Cyp51A, -B, and -C), with Cyp51C being unique to the genus [44,45]. However, Fusarium spp. Cyp51C represents a complete different subgroup in the phylogenetic tree (Figure 2) [43]. In fact, it has recently been demonstrated that Fusarium graminearum Cyp51C does not encode a 14-α sterol demethylase [44].
In order to study azole drug resistance in A. flavus, the three genes encoding 14-α sterol demethylase enzymes (cyp51A, cyp51B, and cyp51C genes) were sequenced in all A. flavus strains included in this study and their deduced amino acid sequences were compared. We used the sequence of the A. flavus type strain (NRRL3357) as the reference sequence, because it was the first strain with the whole genome sequence [46]. Sequences from A. flavus (AF70) and A. oryzae (RIB40) were also included to see if the differences found between the sequences of the different Cyp51s in all the A. flavus clinical strains could correspond to very closely related species, such as A. oryzae, or different A. flavus morphotypes [47]. However, that was not the case. Several amino acid replacements were detected in Cyp51A and Cyp51C but none were found in Cyp51B. Previous studies have described different mutations in all three genes: cyp51A, cyp51B, and cyp51C. The initial studies [23] focused on mutations in Cyp51A and Cyp51B in spontaneous mutant strains obtained after voriconazole exposure. Although different mutations in both proteins were found (Y132N, K197N, D282E, M288L, and T469S in Cyp51A, and two combined mutations H399P/D411N and T454P/T486P in Cyp51B), these substitutions have been recently found in different A. flavus isolates regardless of their susceptibility to azoles, which makes their implication in drug resistance highly unlikely. Similarly, our Cyp51B results showed no amino acid changes in any of the A. flavus isolates, except for a few polymorphisms responsible for synonymous mutations (Table 4).
Cyp51A turns out to be highly polymorphic with several synonymous and non-synonymous point mutations (A199T, K332N, and T329A) that were found among azole susceptible and non-susceptible strains, therefore excluding their possible implication in azole resistance. However, one strain (CM7668) resistant only to ITC and POS harbored a c641t base change resulting in a P214L point mutation that was only present in this strain. This mutation is located at the equivalent position of P216L in A. fumigatus Cyp51A, a mutation that has been confirmed to be linked to azole resistance by gene replacement [48]. The amino acid P216 is a conserved amino acid within the fungal kingdom Cyp51s. Its role in azole resistance has been explored in Cyp51 homology models and results suggest that the alteration of this residue could be affecting the antifungal-enzyme interaction [49]. A previous homology model proved the interaction of P216L with POS but not with VRC, indicating that mutations in this region might play a role in POS resistance [49]. A. fumigatus strains with P216L mutation are resistant to itraconazole and posaconazole but not to voriconazole [50,51]. This peculiar azole susceptibility pattern is similar to the azole susceptibility phenotype exhibited by our A. flavus isolate which carries a P214L alteration. The location of the P214L substitution in Cyp51A of A. flavus strain CM7668, together with the similarity to the A. fumigatus azole susceptibility profile of strains with the P216L Cyp51A mutation, as well as the protein homology studies, highly suggest that this mutation is responsible for the azole resistance shown by this strain. Also, the hypersusceptibility to DMIs shown by this strain (Table 2) seems to indicate that the P214L mutation was not selected in the environment. A limitation of the present study was that clinical data were not collected and we cannot know if the patient was previously treated with ITC or POS, information which would be interesting in the study of the resistance mechanisms. Due to this lack of data, it is impossible to know if the development of azole resistance is related to an in-host acquisition or if this occurred before. However, previous reports A. fumigatus Cyp51A P214L mutated in patients treated with ITC will support this in vivo selection after ITC or POS treatment [48].
The other very polymorphic gene was A. flavus cyp51C with several synonymous and non-synonymous point mutations that were found among both susceptible and non-susceptible strains, and therefore excluding their possible implication in azole resistance. Several mutations found in this study were previously described in other studies, such as M54T, S240A, D254N, I285V, and N423D [24,25,26], while other substitutions are novel, including D254G, P276T, S399I, and a mutation responsible for a stop codon (R250ST). However, one strain (CM9326) resistant to all azole drugs harbored an a1064g base change resulting in a H349R point mutation that was only present in this strain (Table 5). How this mutation could be connected with the interaction of the azole drugs and the enzyme Cyp51C remains unclear. To date, only one point mutation (Y319H) in A. flavus Cyp51C suggests a relation to azole resistance although its role still needs further confirmation [25,26]. In fact, studies of homology modeling and molecular dynamic simulations showed its distant location from the iron porphyrin complex and its lack of effect on the docking of the azoles at the binding site and therefore its doubtful relevance in azole resistance [52].
Gene expression analysis (Figure 1) showed that cyp51A and cyp51B are predominantly expressed among all the strains compared to cyp51C, suggesting that 14-α sterol demethylase activity can be mainly attributed to Cyp51A and Cyp51B. These findings are supported by recent studies of the basal expressions of A. flavus cyp51s showed that cyp51A and cyp51B expression levels were greater than that of cyp51C, with an extremely low gene expression that can be strain-dependent [52]. Interestingly, the CM9326 strain showed higher gene expression levels of cyp51A and cyp51C than the reference strain ATCC2004304. Since the expression of cyp51C is at minimal detectable levels for all the strains, these results suggest an association between the cyp51A gene expression and the CM9326 azole resistance phenotype. Further experiments would be necessary to explore the role of the Cyp51C Y319H mutation in azole resistance alone or in combination with the cyp51A gene expression. Currently, one limitation of this study is that genetic manipulation of A. flavus is not fully developed yet, hence we cannot prove the implication of the Cyp51C Y319H mutation or increased Cyp51A expression in azole resistance.
One A. flavus strain (CM8087) with a susceptibility profile of resistance to all azoles did not show any amino acid change in any of the three enzymes, or their expression, that could explain or suggest an azole resistant mechanism. Other mechanisms, such as the upregulation of azole target (Cyp51s) or multidrug efflux transporters (ABC (ATP-binding cassette)/MFS (major facilitator superfamily)) that could lead to decreased drug concentrations within the fungal cell are starting to be explored [53]. The cyp51A, cyp51B, or cyp51C expression levels in A. flavus do not seem to be related to VRC resistance. In fact, the expression profiles of these genes barely vary among WT and non-WT strains, even after exposure to azoles [54]. Moreover, some studies on basal and voriconazole-induced expression of various efflux pump genes showed low basal expression irrespective of the azole susceptibility of the isolate [54]. Only a possible role of the multidrug efflux pump Cdr1B overexpression in A. flavus azole has been recently proposed [54]. Additionally, this strain (CM8087) was also resistant to AmB and therefore a different resistant mechanism would be expected. Further experiments will be needed to explore other resistance mechanisms that could explain this particular susceptibility profile. Cross resistance between azoles and AmB has been better analyzed in yeast. For instance, in Candida tropicalis, a bypass in the ergosterol biosynthesis pathway may develop as a result of mutations in sterol Δ5,6-desaturase (ERG3) together with Erg11/Cyp51 mutations, resulting in cross resistance to azoles and AmB [55]. In general, the ergosterol biosynthesis pathway is more complex in filamentous fungi and in particular, it has not been studied in A. flavus yet. Although, to date, it would be difficult to search for this kind of resistance mechanism in A. flavus, this possibility deserves consideration in further research.
5. Conclusions
In conclusion, antifungal resistance mechanisms in A. flavus isolates can be relevant in the clinical and in the environmental setting. The results of this study suggest that these mechanisms can be associated to A. flavus Cyp51A or Cyp51C mutations or are related to an increase of cyp51A gene expression. However, the role of these genes variations and their contribution to antifungal resistance needs to be further investigated.
Supplementary Materials
The following are available online at https://www.mdpi.com/2073-4425/11/10/1217/s1, Table S1: Clinical Aspergillus flavus isolates: sample origin and year of isolation. Table S2: Primers used for Aspergillus flavus cyp51A, cyp51B and cyp51C DNA amplification and sequencing and RT-PCR from RNA. Table S3: GenBank Accession Numbers of all A. flavus cyp51A, cyp51B and cyp51C. Figure S1: Aspergillus flavus cyp51 genes expression.
Author Contributions
E.M. conceived and designed the experiments. J.L., I.G.-J. and O.R.-M. performed the experiments. E.M., A.A.-I., L.A.-F. and T.P. analyzed the data. J.L., I.G.-J., L.A.-F. and E.M. drafted the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Fondo de Investigacion Sanitaria (FIS PI18CIII/00045) and also by Plan Nacional de I+D+i 2013–2016 and Instituto de Salud Carlos III, Subdirección General de Redes y Centros de Investigación Cooperativa, Ministerio de Economía, Industria y Competitividad, Spanish Network for Research in Infectious Diseases (REIPI RD16/CIII/0004/0003), co-financed by European Development Regional Fund ERDF “A way to achieve Europe”, Operative program Intelligent Growth 2014-2020. J.L. holds a predoctoral fellowship from the Fondo de Investigación Sanitaria (F17CIII/00037).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Richardson M., Lass-Flörl C. Changing epidemiology of systemic fungal infections. Clin. Microbiol. Infect. 2008;14:5–24. doi: 10.1111/j.1469-0691.2008.01978.x. [DOI] [PubMed] [Google Scholar]
- 2.Paulussen C., Hallsworth J.E., Álvarez-Pérez S., Nierman W.C., Hamill P.G., Blain D., Rediers H., Lievens B. Ecology of aspergillosis: Insights into the pathogenic potency of Aspergillus fumigatus and some other Aspergillus species. Microb. Biotechnol. 2017;10:296–322. doi: 10.1111/1751-7915.12367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Low C.Y., Rotstein C. Emerging fungal infections in immunocompromised patients. F1000 Med. Rep. 2011;3:14. doi: 10.3410/M3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nivoix Y., Velten M., Letscher-Bru V., Moghaddam A., Natarajan-Amé S., Fohrer C., Lioure B., Bilger K., Lutun P., Marcellin L., et al. Factors Associated with Overall and Attributable Mortality in Invasive Aspergillosis. Clin. Infect. Dis. 2008;47:1176–1184. doi: 10.1086/592255. [DOI] [PubMed] [Google Scholar]
- 5.Taccone F.S., Van den Abeele A.M., Bulpa P., Misset B., Meersseman W., Cardoso T., Paiva J.A., Blasco-Navalpotro M., De Laere E., Dimopoulos G., et al. AspICU Study Investigators. Epidemiology of invasive aspergillosis in critically ill patients: Clinical presentation, underlying conditions, and outcomes. Crit. Care. 2015;19:7. doi: 10.1186/s13054-014-0722-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Samarakoon P., Soubani A. Invasive pulmonary aspergillosis in patients with COPD: A report of five cases and systematic review of the literature. Chron. Respir. Dis. 2008;5:19–27. doi: 10.1177/1479972307085637. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Giraldo A.M., Mora B.L., Loaiza-Castaño J.M., Cedano J.A., Rosso F. Invasive fungal infection by Aspergillus flavus in immunocompetent hosts: A case series and literature review. Med. Mycol. Case Rep. 2018;23:12–15. doi: 10.1016/j.mmcr.2018.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krishnan S., Manavathu E.K., Chandrasekar P.H. Aspergillus flavus: An emerging non-fumigatus Aspergillus species of significance. Mycoses. 2009;52:206–222. doi: 10.1111/j.1439-0507.2008.01642.x. [DOI] [PubMed] [Google Scholar]
- 9.Hedayati M., Pasqualotto A.C., Warn P.A., Bowyer P., Denning D.W. Aspergillus flavus: Human pathogen, allergen and mycotoxin producer. Microbiology. 2007;153:1677–1692. doi: 10.1099/mic.0.2007/007641-0. [DOI] [PubMed] [Google Scholar]
- 10.Alastruey-Izquierdo A., Mellado E., Peláez T., Pemán J., Zapico S., Alvarez M., Rodríguez-Tudela J.L., Cuenca-Estrella M., FILPOP Study Group Population-based survey of filamentous fungi and antifungal resistance in Spain (FILPOP Study) Antimicrob. Agents Chemother. 2013;57:3380–3387. doi: 10.1128/AAC.00383-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alastruey-Izquierdo A., Alcazar-Fuoli L., Rivero-Menéndez O., Ayats J., Castro C., García-Rodríguez J., Goterris-Bonet L., Ibáñez-Martínez E., Linares-Sicilia M.J., Martin-Gomez M.T., et al. The FILPOP2 Project from GEMICOMED (SEIMC) and REIPI. Molecular Identification and Susceptibility Testing of Molds Isolated in a Prospective Surveillance of Triazole Resistance in Spain (FILPOP2 Study) Antimicrob. Agents Chemother. 2018;62:e00358-18. doi: 10.1128/AAC.00358-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rudramurthy S.M., Paul R.A., Chakrabarti A., Mouton J.W., Meis J.F. Invasive Aspergillosis by Aspergillus flavus: Epidemiology, Diagnosis, Antifungal Resistance, and Management. J. Fungi. 2019;5:55. doi: 10.3390/jof5030055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ullmann A.J., Aguado J.M., Arikan-Akdagli S., Denning D.W., Groll A.H., Lagrou K., Lass-Flörl C., Lewis R.E., Munoz P., Verweij P.E., et al. Diagnosis and Management of Aspergillus Diseases: Executive Summary of the 2017 ESCMID-ECMM-ERS Guideline. Clin. Microbiol. Infect. 2018;24:e1–e38. doi: 10.1016/j.cmi.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 14.Lepesheva G.I., Waterman M.R. Sterol 14alpha-demethylase cytochrome P450 (CYP51), a P450 in all biological kingdoms. Biochim. Biophys. Acta. 2007;1770:467–477. doi: 10.1016/j.bbagen.2006.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chowdhary A., Sharma C., Meis J.F. Azole-Resistant Aspergillosis: Epidemiology, Molecular Mechanisms, and Treatment. J. Infect. Dis. 2017;216:S436–S444. doi: 10.1093/infdis/jix210. [DOI] [PubMed] [Google Scholar]
- 16.Garcia-Rubio R., Cuenca-Estrella M., Mellado E. Triazole Resistance in Aspergillus Species: An Emerging Problem. Drugs. 2017;77:599–613. doi: 10.1007/s40265-017-0714-4. [DOI] [PubMed] [Google Scholar]
- 17.Zhang J., van den Heuvel J., Debets A.J.M., Verweij P.E., Melchers W.J.G., Zwaan B.J., Schoustra S.E. Evolution of cross-resistance to medical triazoles in Aspergillus fumigatus through selection pressure of environmental fungicides. Proc. Biol. Sci. 2017;284:20170635. doi: 10.1098/rspb.2017.0635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klich M.A. Aspergillus flavus: The major producer of aflatoxin. Mol. Plant. Pathol. 2007;8:713–722. doi: 10.1111/j.1364-3703.2007.00436.x. [DOI] [PubMed] [Google Scholar]
- 19.Varga J., Frisvad J.C., Samson R.A. Two new aflatoxin producing species, and an overview of Aspergillus section Flavi. Stud. Mycol. 2011;69:57–80. doi: 10.3114/sim.2011.69.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mellado E., Diaz-Guerra T.M., Cuenca-Estrella M., Rodriguez-Tudela J.L. Identification of two different 14-a sterol demethylase-related genes (cyp51A and cyp51B) in Aspergillus fumigatus and other Aspergillus species. J. Clin. Microbiol. 2001;39:2431–2438. doi: 10.1128/JCM.39.7.2431-2438.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang J., Li L., Lv Q., Yan L., Wang Y., Jiang Y. The Fungal CYP51s: Their Functions, Structures, Related Drug Resistance, and Inhibitors. Front. Microbiol. 2019;10:691. doi: 10.3389/fmicb.2019.00691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choi M.J., Won E.J., Joo M.Y., Park Y.J., Kim S.H., Shin M.G., Shin J.H. Microsatellite typing and resistance mechanism analysis of voriconazole-resistant Aspergillus flavus isolates in South Korean hospitals. Antimicrob. Agents Chemother. 2019;63:e01610-18. doi: 10.1128/AAC.01610-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krishnan-Natesan S., Chandrasekar P.H., Alangaden G.J., Manavathu E.K. Molecular characterisation of cyp51A and cyp51B genes coding for P450 14α-lanosterol demethylases A (CYP51Ap) and B (CYP51Bp) from voriconazole-resistant laboratory isolates of Aspergillus flavus. Int. J. Antimicrob. Agents. 2008;32:519–524. doi: 10.1016/j.ijantimicag.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 24.Liu W., Sun Y., Chen W., Liu W., Wan Z., Bu D., Li R. The T788G mutation in the cyp51C gene confers voriconazole resistance in Aspergillus flavus causing aspergillosis. Antimicrob. Agents Chemother. 2012;56:2598–2603. doi: 10.1128/AAC.05477-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paul R.A., Rudramurthy S.M., Meis J.F., Mouton J.W., Chakrabarti A. A Novel Y319H Substitution in CYP51C Associated with Azole Resistance in Aspergillus flavus. Antimicrob. Agents Chemother. 2015;59:6615–6619. doi: 10.1128/AAC.00637-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sharma C., Kumar R., Kumar N., Masih A., Gupta D., Chowdhary A. Investigation of Multiple Resistance Mechanisms in Voriconazole-Resistant Aspergillus flavus Clinical Isolates from a Chest Hospital Surveillance in Delhi, India. Antimicrob. Agents Chemother. 2018;62:e01928-17. doi: 10.1128/AAC.01928-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang C.M., Cohen J., Holden D.W. An Aspergillus fumigatus alkaline protease mutant constructed by gene disruption is deficient in extracellular elastase activity. Mol. Microbiol. 1992;6:1663–1671. doi: 10.1111/j.1365-2958.1992.tb00891.x. [DOI] [PubMed] [Google Scholar]
- 28.Alcazar-Fuoli L., Mellado E., Alastruey-Izquierdo A., Cuenca-Estrella M., Rodriguez-Tudela J.L. Aspergillus section Fumigati: Antifungal susceptibility patterns and sequence-based identification. Antimicrob. Agents Chemother. 2008;52:1244–1251. doi: 10.1128/AAC.00942-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arendrup M.C., Cuenca-Estrella M., Lass-Flörl C., Hope W.W. European Committee on Antimicrobial Susceptibility Testing Subcommittee on Antifungal Susceptibility Testing (EUCAST-AFST). EUCAST technical note on Aspergillus and amphotericin B, itraconazole, and posaconazole. Clin. Microbiol. Infect. 2012;18:248–250. doi: 10.1111/j.1469-0691.2012.03890.x. [DOI] [PubMed] [Google Scholar]
- 30.Arendrup M.C., Cuenca-Estrella M., Lass-Flörl C., Hope W.W. Breakpoints for antifungal agents: An update from EUCAST focussing on echinocandins against Candida spp. and triazoles against Aspergillus spp. Drug Resist. Updat. 2013;16:81–95. doi: 10.1016/j.drup.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 31.The European Committee on Antimicrobial Susceptibility Testing Breakpoint Tables for Interpretation of MICs for Antifungal Agents, Version 10.0. [(accessed on 16 April 2020)];2020 Available online: http://www.eucast.org/astoffungi/clinicalbreakpointsforantifungals/
- 32.Diaz-Guerra T.M., Mellado E., Cuenca-Estrella M., Rodriguez-Tudela J.L. A point mutation in the 14alpha-sterol demethylase gene cyp51A contributes to itraconazole resistance in Aspergillus fumigatus. Antimicrob. Agents Chemother. 2003;47:1120–1124. doi: 10.1128/AAC.47.3.1120-1124.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cove D.J. The induction and repression of nitrate reductase in the fungus Aspergillus nidulans. Biochim. Biophys. Acta. 1966;113:51–56. doi: 10.1016/S0926-6593(66)80120-0. [DOI] [PubMed] [Google Scholar]
- 34.Schmittgen T.D., Livak K.J. Analyzing real-time PCR data by the comparative C(T) method. Nat. Protoc. 2008;3:1101–1108. doi: 10.1038/nprot.2008.73. [DOI] [PubMed] [Google Scholar]
- 35.Hess J., Goldman N. Addressing inter-gene heterogeneity in maximum likelihood phylogenomic analysis: Yeasts revisited. PLoS ONE. 2011;6:e22783. doi: 10.1371/journal.pone.0022783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rivero-Menendez O., Soto-Debran J.C., Medina N., Lucio J., Mellado E., Alastruey-Izquierdo A. Molecular Identification, Antifungal Susceptibility Testing, and Mechanisms of Azole Resistance in Aspergillus Species Received within a Surveillance Program on Antifungal Resistance in Spain. Antimicrob. Agents Chemother. 2019;63:e00865-19. doi: 10.1128/AAC.00865-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tashiro M., Izumikawa K., Hirano K., Ide S., Mihara T., Hosogaya N., Takazono T., Morinaga Y., Nakamura S., Kurihara S., et al. Correlation between triazole treatment history and susceptibility in clinically isolated Aspergillus fumigatus. Antimicrob. Agents Chemother. 2012;56:4870–4875. doi: 10.1128/AAC.00514-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Berger S., El Chazli Y., Babu A.F., Coste A.T. Azole Resistance in Aspergillus fumigatus: A Consequence of Antifungal Use in Agriculture? Front. Microbiol. 2017;8:1024. doi: 10.3389/fmicb.2017.01024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nierman W.C., Yu J., Fedorova-Abrams N.D., Losada L., Cleveland T.E., Bhatnagar E., Bennett J.W., Dean R., Payne G.A. Genome Sequence of Aspergillus flavus NRRL 3357, a Strain That Causes Aflatoxin Contamination of Food and Feed. Genome Announc. 2015;3:e00168-15. doi: 10.1128/genomeA.00168-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chowdhary A., Kathuria S., Xu J., Meis J.F. Emergence of Azole-Resistant Aspergillus fumigatus Strains due to Agricultural Azole Use Creates an Increasing Threat to Human Health. PLoS Pathog. 2013;9:e1003633. doi: 10.1371/annotation/4ffcf1da-b180-4149-834c-9c723c5dbf9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hollomon D. Does Agricultural Use of Azole Fungicides Contribute to Resistance in the Human Pathogen Aspergillus fumigatus? Pest. Manag. Sci. 2017;73:1987–1993. doi: 10.1002/ps.4607. [DOI] [PubMed] [Google Scholar]
- 42.Verweij P.E., Chowdhary A., Melchers W.J., Meis J.F. Azole Resistance in Aspergillus fumigatus: Can We Retain the Clinical Use of Mold-Active Antifungal Azoles? Clin. Infect. Dis. 2016;62:362–368. doi: 10.1093/cid/civ885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hawkins N.J., Cools H.J., Sierotzki H., Shaw M.W., Knogge W., Kelly S.L., Kelly D.E., Fraaije B.A. Paralog re-emergence: A novel, historically contingent mechanism in the evolution of antimicrobial resistance. Mol. Biol. Evol. 2014;7:1793–1802. doi: 10.1093/molbev/msu134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fan J., Urban M., Parker J.E., Brewer H.C., Kelly S.L., Hammond-Kosack K.E., Fraaije B.A., Liu X., Cools H.J. Characterization of the sterol 14α-demethylases of Fusarium graminearum identifies a novel genus-specific CYP51 function. New Phytol. 2013;198:821–835. doi: 10.1111/nph.12193. [DOI] [PubMed] [Google Scholar]
- 45.Zheng B., Yan L., Liang W., Yang Q. Paralogous Cyp51s Mediate the Differential Sensitivity of Fusarium Oxysporum to Sterol Demethylation Inhibitors. Pest. Manag. Sci. 2019;75:396–404. doi: 10.1002/ps.5127. [DOI] [PubMed] [Google Scholar]
- 46.Payne G.A., Nierman W.C., Wortman J.R., Pritchard B.L., Brown D., Dean R.A., Bhatnagar D., Cleveland T.E., Machida M., Yu J. Whole genome comparison of Aspergillus flavus and A. oryzae. Med. Mycol. 2006;44:S9–S11. doi: 10.1080/13693780600835716. [DOI] [PubMed] [Google Scholar]
- 47.Gilbert M.K., Mack B.M., Moore G.G., Downey D.L., Lebar M.D., Joardar V., Losada L., Yu J., Nierman W.C., Bhatnagar D. Whole genome comparison of Aspergillus flavus L-morphotype strain NRRL 3357 (type) and S-morphotype strain AF70. PLoS ONE. 2018;13:e0199169. doi: 10.1371/journal.pone.0199169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Camps S.M., van der Linden J.W., Li Y., Kuijper E.J., van Dissel J.T., Verweij P.E., Melchers W.J. Rapid induction of multiple resistance mechanisms in Aspergillus fumigatus during azole therapy: A case study and review of the literature. Antimicrob. Agents Chemother. 2012;56:10–16. doi: 10.1128/AAC.05088-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xiao L., Madison V., Chau A.S., Loebenberg D., Palermo R.E., McNicholas P.M. Three-dimensional models of wild-type and mutated forms of cytochrome P450 14alpha-sterol demethylases from Aspergillus fumigatus and Candida albicans provide insights into posaconazole binding. Antimicrob. Agents Chemother. 2004;48:568–574. doi: 10.1128/AAC.48.2.568-574.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dabas Y., Xess I., Bakshi S., Mahapatra M., Seth R. Emergence of Azole-Resistant Aspergillus fumigatus from Immunocompromised Hosts in India. Antimicrob. Agents Chemother. 2018;62:e02264-17. doi: 10.1128/AAC.02264-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ballard E., Melchers W.J.G., Zoll J., Brown A.J.P., Verweij P.E., Warris A. In-host microevolution of Aspergillus fumigatus: A phenotypic and genotypic analysis. Fungal Genet. Biol. 2018;113:1–13. doi: 10.1016/j.fgb.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rudramurthy S.M., Seyedmousavi S., Dhaliwal M., Chakrabarti A., Meis J.F., Mouton J.W. Pharmacodynamics of Voriconazole against Wild-Type and Azole-Resistant Aspergillus flavus Isolates in a Nonneutropenic Murine Model of Disseminated Aspergillosis. Antimicrob. Agents Chemother. 2016;61:e01491-16. doi: 10.1128/AAC.01491-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Paul R.A., Rudramurthy S.M., Dhaliwal M., Singh P., Ghosh A.K., Kaur H., Varma S., Agarwal R., Chakrabarti A. Magnitude of voriconazole resistance in clinical and environmental isolates of Aspergillus flavus and investigation into the role of multidrug efflux pumps. Antimicrob. Agents Chemother. 2018;62:e01022-18. doi: 10.1128/AAC.01022-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pérez-Cantero A., López-Fernández L., Guarro J., Capilla J. Azole resistance mechanisms in Aspergillus: Update and recent advances. Int. J. Antimicrob. Agents. 2020;55:105807. doi: 10.1016/j.ijantimicag.2019.09.011. [DOI] [PubMed] [Google Scholar]
- 55.Forastiero A., Mesa-Arango A.C., Alastruey-Izquierdo A., Alcazar-Fuoli L., Bernal-Martinez L., Pelaez T., Lopez J.F., Grimalt J.O., Gomez-Lopez A., Cuesta I., et al. Candida tropicalis antifungal cross-resistance is related to different azole target (Erg11p) modifications. Antimicrob. Agents Chemother. 2013;57:4769–4781. doi: 10.1128/AAC.00477-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.