Abstract
Approximately, one in three physicians is experiencing burnout at any given time. This may not only interfere with own wellbeing but also with the quality of delivered care. This narrative review discusses several aspects of the burnout syndrome: prevalence, symptoms, etiopathogenesis, diagnosis, impact, and strategies on how to deal with the problem.
Keywords: burnout, healthcare worker, prevalence, impact, symptoms, prevention
Never overestimate the strength of the torchbearer’s arm, for even the strongest arms grow weary.
AJ Darkholme, Rise of the Morningstar
Introduction
Burnout is a work-related stress syndrome resulting from chronic exposure to job stress. The term was introduced in the early 1970s by psychoanalyst Freudenberger and has subsequently been defined by Maslach et al as consisting of three qualitative dimensions which are emotional exhaustion, cynicism and depersonalization, reduced professional efficacy and personal accomplishment.1–4 Burnout can occur in any kind of profession.5
Healthcare workers, and especially perioperative clinicians seem to be at particular risk for burnout.6,7 This may have significant negative personal (substance abuse, broken relationships and even suicide),8,9 but also important professional consequences such as lower patient satisfaction,10−12 impaired quality of care,13,14 even up to medical errors,15–18 potentially ending up in malpractice suits with substantial costs for caregivers and hospitals.19
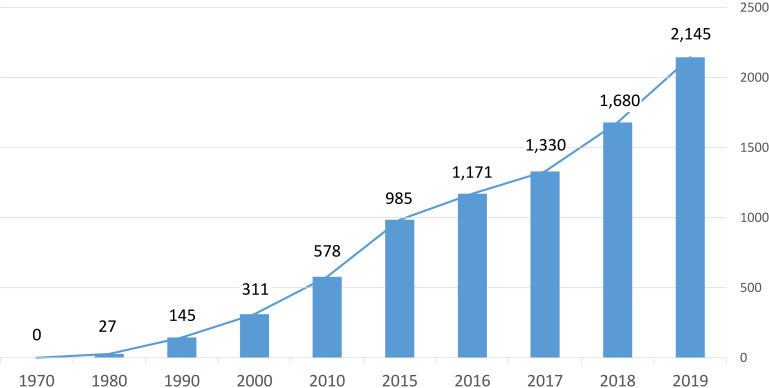
Therefore, alertness for the phenomenon with prompt recognition together with the development of adequate coping personal and organisational strategies is essential in dealing with this important problem in contemporary healthcare. The last 10 years have witnessed an increasing interest in the topic with an exponential growth in the number of papers published on the topic (Figure 1).
Figure 1.
Overview of the number of PubMed hits for the search term “burnout” between 1970 and 2019.
Prevalence
Because of the absence of a generally accepted definition of the syndrome of burnout, its multifactorial origin and the vagueness and subjectivity of the diagnostic criteria, it is difficult to get a clear and correct overview of the prevalence of burnout in a general population. Estimations report values up to 20% of the working population but the number is strongly dependent on the cut-off values to define severe burnout.20 Interestingly, the results of a Finnish study, looking at the relation between the level of burnout and socio-demographic factors found only small differences between the different population groups studied. There was a slightly higher incidence with increased age and some gender-specific features. For instance, in women burnout was related to education and socio-economic status while for men, a relation to marital status was observed.21
The reported incidence of burnout varies worldwide. For instance, in Europe, a difference is observed between the European Union countries (10%) and the non-European Union countries (17%). Within the European Union countries, the incidence of burnout ranges from 4.3% in Finland to 20.6% in Slovenia and within the non-European Union countries from 13% in Albania to 25% in Turkey.22 This study also indicated that burnout at the country level seemed positively related to the workload.
Burnout in Physicians
Burnout has been shown to occur in all kinds of jobs. However, the incidence seems to be higher in physicians. In a study comparing incidences of burnout between US physicians and a population control sample, Shanafelt et al observed an incidence of symptoms of burnout of 37.9% in physicians compared to 27.8% in the control population (p < 0.001).23 Physicians in specialties at the front line of care access such as family medicine, general internal medicine, and emergency medicine seem to be at greatest risk.
The 2020 Medscape National Physician Burnout and Suicide Report reported a burnout rate of about 43%,24 which remains quite similar to the 46% reported in 2015 and 39.8% in 2013. While most studies agree on the fact that there is no real gender effect in the incidence of burnout,25,26 the data from the Medscape National Physician Report indicate that women physicians reported more commonly symptoms of burnout (in 2015, 51% female vs 43% male and in 2020, 48% female vs 37% male).24 Interestingly, there seem to be gender differences in the presence of the different symptoms: exhaustion, depersonalization, and lack of efficacy. A study in general practitioners showed that exhaustion and fatigue occur equally in both sexes. On the other hand, the feeling of lack of efficacy seems more common in women. It seems that male physicians are less likely to doubt the quality of their work than women.26
It is difficult to have an exact estimation of the incidence of burnout in physicians. A recent systematic review including 182 studies published between 1991 and 2018 and involving 109,628 individuals in 45 countries observed a substantial variability in prevalence estimates of burnout among physicians, ranging from 0% to 80.5%. This appeared to be related to important differences in definitions of the syndrome and of the assessment methods applied. There were no relevant associations between burnout and demographic factors.27
Burnout in Anesthesiologists
The 2020 Medscape National Physician Burnout and Suicide Report ranked the incidence of burnout on 29 medical specialities. The top three medical specialisms for burnout are urology (54%), neurology (50%), and nephrology (49%). The lowest incidence of burnout is reported in general surgery (35%), psychiatry (35%), and orthopedics (34%). Anesthesiology comes on the 16th place with 41%, emergency medicine on place 14 with 43%, and critical care on place 10 with a reported incidence of burnout of 44%.24
During the last decade, several studies have been published specifically looking at burnout in the anesthesiology community. A recent systematic review identified a total of 167 papers on the topic, from which finally 17 were included to assess the prevalence and initiating factors for burnout.28 From this study, it appeared that the occurrence of burnout varied substantially among the different reports, ranging from 10% to 59%. It seems to occur in all career stages and is related to a stressful work situation. No specific relationship was observed between burnout and gender, or marital status. However, the authors underscore that the small number of studies included together with the large differences in their methodology and reporting approach make reliable conclusions difficult and warrant further research.28
Symptoms
Burnout has been defined as a syndrome of emotional exhaustion, depersonalization, and a sense of low personal accomplishment that leads to decreased effectiveness at work.29 Burnout seems to occur mainly in professions involving an interaction with people, such as physicians, nurses, social workers, and teachers but meanwhile, the syndrome has been described in other professions.30
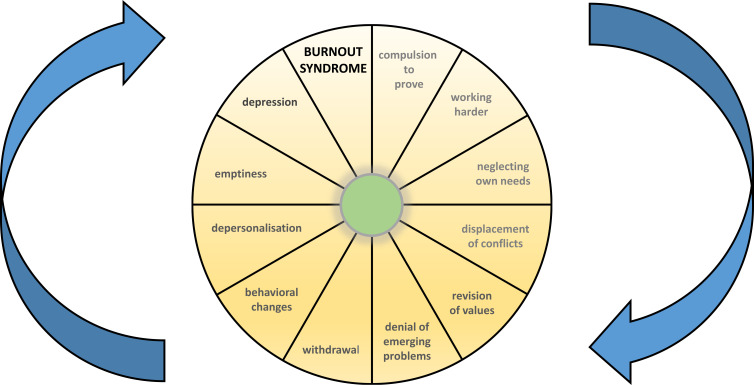
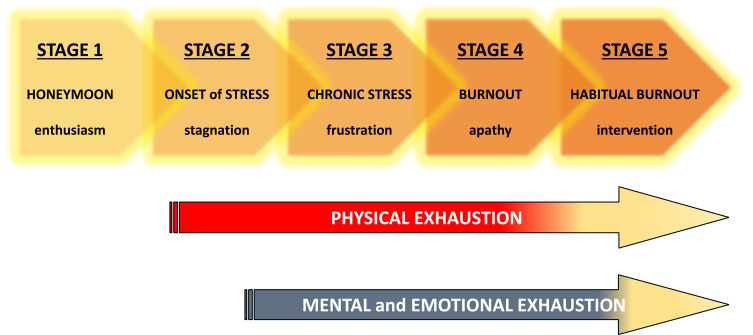
The symptomatology of burnout appears to be rather complex as the syndrome seems to develop in several consecutive stages. Initially, Freudenberger described its development in a 12-stage model31 (Figure 2). Later on, this model has been simplified, and currently, a 5-stage model is most frequently used (Figure 3). This 5-stage model starts with the honeymoon phase and is characterized by enthusiasm. However, inevitably, after time this becomes associated with experiencing the stresses of the job. If at this stage, no positive coping strategies are implemented, the process of burnout risks to become initiated. This is followed by a stage of stagnation characterized by the onset of stress. This second stage begins with an awareness of some days being more difficult than others. Life becomes limited to work and taking care of business, while family, social life and personal priorities are neglected and suffer and common stress symptoms appear, which affect the person emotionally, but also physically. Then a stage of chronic stress develops which leads to frustration. Individuals get the feeling of failure and a sense of powerlessness. Efforts do not visibly pay off and the impression or fact of not receiving enough acknowledgement leads to one feeling incompetent and inadequate. This then leads to the stage of apathy, where despair and disillusionment occur. People do not see a way out of the situation and become resigned and indifferent. The final stage is habitual burnout. Symptoms of burnout cause a significant physical or emotional problem and ultimately these may prompt one to look for help and intervention.
Figure 2.
12-stage model for the development of burnout as described by Freudenberger.31
Figure 3.
Simplified 5-stage model for the development of burnout which is most frequently used.
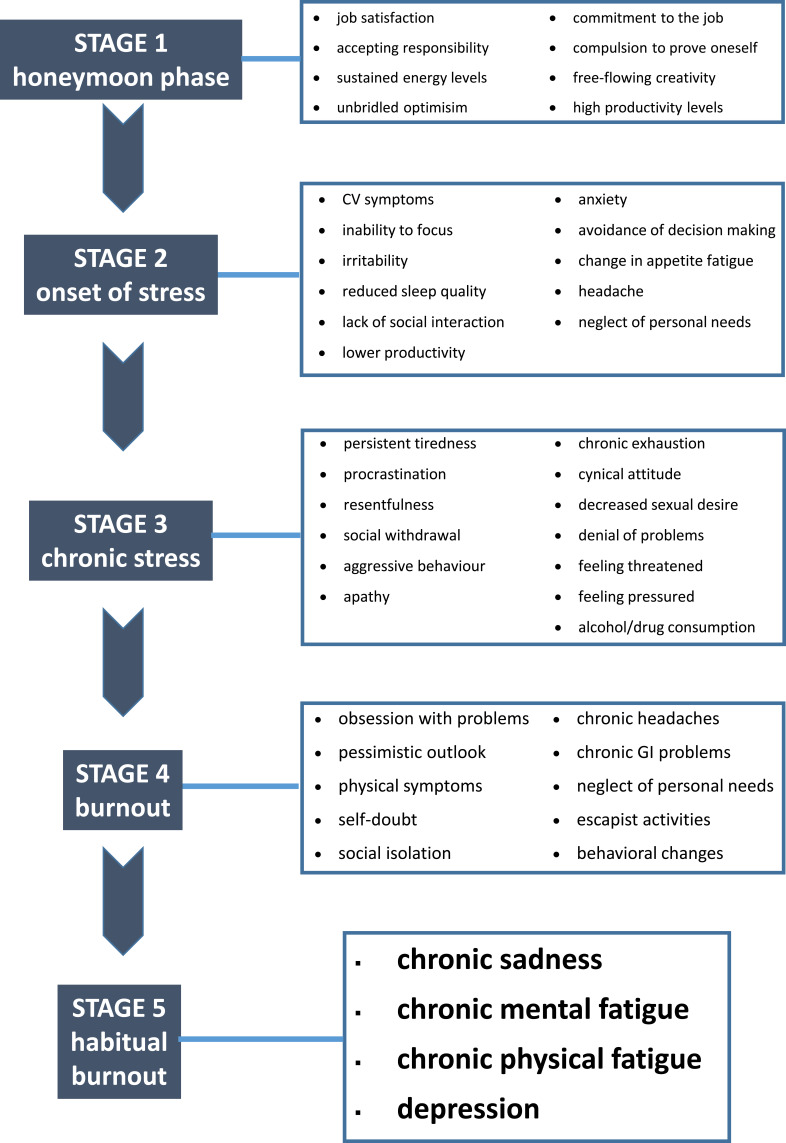
The list of symptoms is long and most of them are not very specific (Figure 4). Symptoms are related to the different stages of the syndrome and have been divided into different clusters.30 These include warning symptoms in the early phase (increased commitment to goals and exhaustion), followed by a phase of reduced commitment (towards patients and clients, towards others in general, towards work, towards increased demands), emotional reactions and blaming (depression, aggression), finally leading to reduction in cognitive performance, motivation, creativity, and judgement, flattening of emotional, social, and intellectual life, psychosomatic reactions and despair.
Figure 4.
Symptoms in the different stages of burnout.
Etiopathogenesis
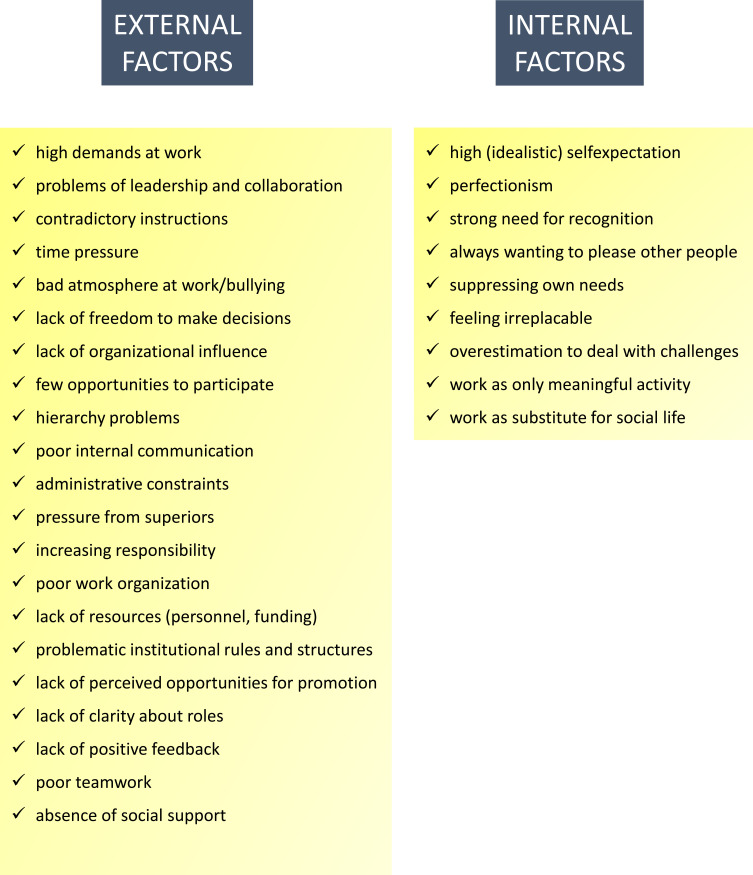
The etiopathogenesis of burnout is multifactorial. Different etiological factors are summarized in Figure 5. These factors have been taken into account in the development of the different psychological explanatory models for the etiopathogenesis of burnout. The job demand-control model focuses on the job task profile (job demand vs control),32 the effort-reward imbalance model focuses on the work contract (effort vs reward),33 and the organizational injustice model focuses on organizational justice (unfair procedures and their interactions).34
Figure 5.
External (environmental) and internal (personality-related) etiological factors for burnout.
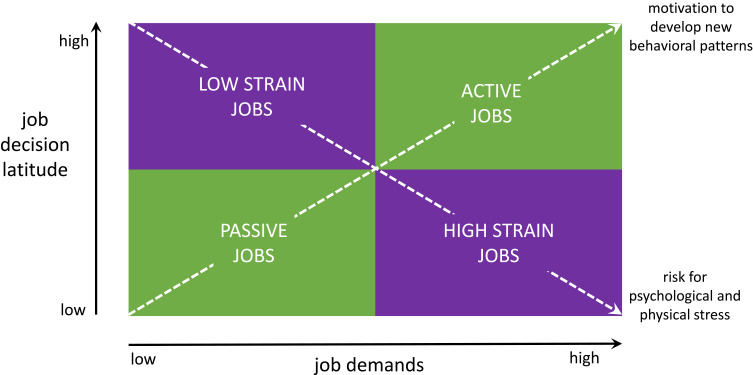
Job Demand-Control Model
The job demand-control model was introduced by Karasek in 1979 and focuses on the balance between the magnitude of the demands (height of strain) and the level of control (decision latitude) in a person’s work situation.32 The height of strain represents the requirements that are set at work which may cause for stress. This includes all aspects of the workload of a particular job such as work rate, availability, time pressure, travel time, difficulty of the tasks, etc. The decision latitude refers to the possibilities and freedom of an employee to organise and manage the workload. Based on these concepts a diagram has been proposed representing four different job situations, where both the stress imposed by the work situation and the personal attitude and engagement of the employee are incorporated. These are the low- and high strain jobs and the passive and active jobs (Figure 6).
Figure 6.
The job demand-control model, introduced by Karasek in 1979 focuses on the balance between the magnitude of the demands (height of strain) and the level of control (decision latitude) in a person’s work situation.32
The low strain job rectangle represents the combination of a job without important demanding tasks but with where the employee has some job decision latitude for instance some freedom to decide on own schedules and targets. This section represents a majority of the routine jobs. Persons in this category may progressively get bored in their work situation. A high strain job, on the contrary, refers to very demanding and/or complex jobs with little control about working conditions and targets by the employee. As a consequence, the risk of stress is very high.
Passive jobs are simple jobs but with very little decision latitude, typically repetitive production jobs. Such jobs present very little stress but also no substantial challenge to the employees. Active jobs, on the other end, represent highly demanding jobs but where the employees have a high level of decision latitude.
In fact this model focuses on the balance between the requirements of a job and the level of control the employee has in his/her professional situation.
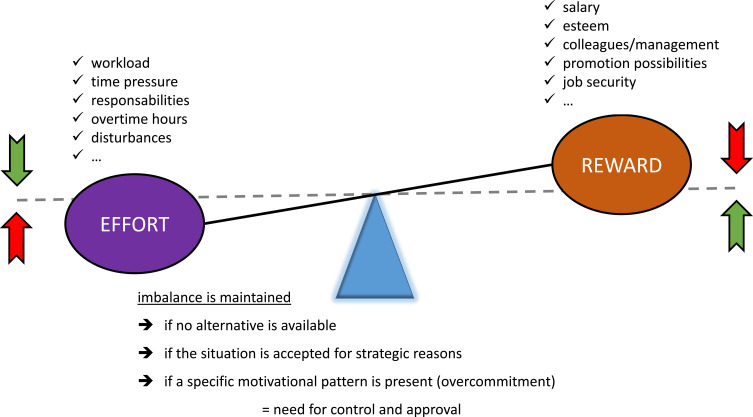
Effort-Reward Imbalance Model
Another theoretical explanatory model for the etiopathogenesis for burnout is the effort-reward imbalance model. It was proposed by Siegrist in 1996 and defines threatening job conditions as a mismatch between high demand (high workload) and low control over long-term rewards.35 An additional point in the model is the concept of overcommitment to the job, which may negatively impact the balance between effort and reward (Figure 7).
Figure 7.
The effort-reward imbalance model, proposed by Siegrist in 1996 defines threatening job conditions as a mismatch between high demand (high workload) and low control over long-term rewards.35
Organizational Injustice Model
A third model is the organizational injustice model. In 1987 Greenberg introduced the concept of organizational justice. This refers to how an employee judges the behavior of the organization.36,37 There are four components of organizational justice: distributive, procedural, interpersonal, and informational justice. Several models have been proposed to explain the structure of organizational justice perception including a two factor, a three factor, and a four factor model. It is beyond the scope of this review to discuss these. The interested reader is referred to specific articles on the topic.37–41
Other Proposed Models
Additional proposed models include the person-environment fit model, the job characteristics model, the diathesis stress model, and the job demands resource model.42–45 The multitude of explanatory models proposed indicates the complexity of the syndrome of burnout and no single model is capable of incorporating all the aspects of its etiopathogenesis. As a consequence, the different potential causative factors need to be explored when dealing with an individual case of burnout (Figure 5). An integration model of personality-related and environment-related etiological factors has been proposed by Fisher46 and has been considered plausible and practicable.30 In this model, the precondition for the development of burnout is a complementary interplay of factors in the employee’s personality and environmental triggering factors.47
Diagnosis
A health technology assessment report from 2010 commissioned by the German Institute for Medical Documentation and Information concluded that to date there is no standardized and generally valid procedure to diagnose the burnout syndrome.48 A number of screening tools are now available. The most frequently used is the Maslach Burnout Inventory (MBI).29 Others include the Tedium Measure (later renamed the Burnout Measure),49 the Shirom Melamed Burnout Questionnaire (SMBQ), the Oldenburg Burnout Inventory (OLBI), the Copenhagen Burnout Inventory (CBI), and the School Burnout Inventory (SBI).30,48 These different questionnaires are adapted for the specific population studied, in terms of language and culture and of specific occupations. They all share a similar approach of looking at burnout as a multi-dimensional construct consisting of the main three components, emotional exhaustion, depersonalization, and reduced personal accomplishment (or dissatisfaction with personal accomplishment). The problem is that all value for the diagnosis of burnout, and when such a value is used, it is determined arbitrarily. In addition, while the dimension emotional exhaustion appears to be a constant feature of burnout, this seems to be less the case for the dimensions depersonalization and personal accomplishment, which appear heterogeneous, thereby reducing the significance of the latter two dimensions.30,48
Following its publication in 1981,4 several new adapted versions of the MBI were progressively developed to fit different groups and different settings.29 There are currently five versions: Human Services Survey (MBI-HSS), Human Services Survey for Medical Personnel (MBI-HSS (MP)), Educators Survey (MBI-ES), General Survey (MBI-GS), and General Survey for Students (MBI-GS (S)). The questionnaires look at the different dimensions of burnout. The 9-item emotional exhaustion (EE) scale measures feelings of emotional overextension and exhaustion. The scale is used in the MBI-HSS, MBI-HSS (MP), and MBI-ES versions. The MBI-GS and MBI-GS (S) use a shorter 5-item version. The 5-item depersonalization scale assesses the degree of impersonal response towards the recipients of one’s care, treatment or service. This scale is used in the MBI-HSS, MBI-HSS (MP) and the MBI-ES versions. An 8-item personal accomplishment scale measures feelings of competence and achievement in one’s work and is used in the MBI-HSS, MBI-HSS (MP), and MBI-ES versions. The MBI-GS and MBI-GS (S) additionally score cynicism (indifference towards one’s work) on a 5-item scale and professional efficacy (feelings of competence and achievement) on a 6-item scale. All items are scored on a 7-level frequency scale: never (0), a few times a year or less (1), once a month or less (2), a few times a month (3), once a week (4), a few times a week (5), and every day (6).
Currently, none of the assessment tools for burnout provides instruments for differential diagnosis. In particular, the association between burnout and the chronic fatigue syndrome and burnout and depression is relevant, as all entities share quite some common symptoms and burnout is a risk factor for the development of depression.48
Burnout seems to be associated with musculoskeletal diseases among women and with cardiovascular diseases among men. These associations are not explained by sociodemographic factors, health behavior, or depression.49 Other studies have suggested that chronic burnout might be a risk factor for the onset of type 2 diabetes,50 and hyperlipidemia.51 The underlying neurobiological mechanisms for the physical effects of burnout are still unknown. Several studies have investigated the association between burnout and functioning of the hypothalamic-pituitary-adrenal axis, but the results are not consistent and the clinical implications of these findings remain to be established.52 Currently, there is no hard evidence for the clinical usefulness of any specific biomarker for burnout.53
Impact
Consequences of burnout are decreased job satisfaction,54 absenteeism,55 turnover in personnel,54,56 and cynicism.15,57 These effects at work frequently have repercussions on personal life such as feeling unhappy, anxiety, depression, isolation, substance abuse, frictional and broken relationships and divorce.58–66 Burnout in physicians may have more serious professional implications than in other professions. Indeed, physician burnout has been linked to suboptimal patient care [8] resulting in lower patient satisfaction,8−12 impaired quality of care.13,14 This may eventually lead up to medical errors,15–18 with potential malpractice suits and subsequent litigation, with substantial costs for caregivers and hospitals as a consequence.19
How to Deal with Burnout?
The complexity of the interaction between all the previously discussed external and internal factors in the development of burnout underscores the importance of a multifactorial approach in the prevention and the treatment of the syndrome. This means that both the work environment and the person’s own personality and attitude towards the work situation need to be addressed. This implies not only the implementation of measures at the level of the professional employers and work environment but also developing and implementing individual coping strategies.
Approaches to treating burnout syndrome should be guided by the severity of the symptoms. If these are minor and slight, measures such as changing life habits and optimizing work–life balance are recommended. These measures concentrate on three important pillars: relief from stressors, recuperation via relaxation and sport, and “return to reality” in terms of abandoning the ideas of perfection.30
Various wellness strategies can be applied by physicians in order to cope with the symptoms of burnout.6,15,67,68 A first strategy focuses on relationships. It refers to an understanding of the importance of spending quality time with family, friends and significant others. This strategy also includes actively developing connections with colleagues, to share and reflect with them on emotional and existential aspects of being a physician. A second element that seems to promote well-being in some people is religious belief and/or spiritual practice. This refers to a personal attentiveness to nurturing own spiritual aspects.68,69 It has been reported that up to 34% of persons mentioned this aspect to be important and even essential.15,68 A third element deals with work attitudes. This has two components. The first one refers to finding meaning and fulfillment in work, the second one to actively choosing and limiting the type of medical practice such as working part-time, being involved in education and/or research, managing schedule and discontinuing unfulfilling aspects of practice. A fourth strategy consists of self-care practices, in which an individual actively cultivates personal interests and self-awareness in addition to professional and family responsibilities. This also implies actively seeking professional help in case of personal physical and psychological problems or illness. Examples of such practices are, among others, exercise, self-expression activities, adequate nutrition and sleep, regular medical care, professional counseling, etc. Finally, the fifth component is adapting a specific life philosophy. This is developing a philosophical approach to life that is based on a positive outlook where one identifies own values and acts accordingly with emphasis on the balance between personal and professional life. It is likely that such strategies are also the designated tools to be implemented in the prevention of the development to burnout.
Although each individual is in the end responsible for his/her own wellness, organizational and institutional awareness, attention to and recognition of the problem can play a crucial role in promoting physicians’ well-being.6,70 Job characteristics and institutional factors that contribute to wellbeing include promoting autonomy,71–82 providing adequate office resources and support staff,83,84 and facilitating a collegial work environment.75,77 Giving physicians the ability to influence their work environment, to participate in organizational decisions that affect medical practice, and to have more control over their time schedules seem to have a substantial positive effect regardless of practice type.71–81 Efforts to minimize work-home interference by providing flexible scheduling, childcare adapted to irregular work hours, etc., are also important for increasing the employees’ well-being.59,81,84
If the symptoms of burnout are severe, psychotherapeutic interventions are recommended. There may also be a place for antidepressants, preferably combined with psychotherapy.30 There are several therapies for the treatment of burnout but all with unclear evidence. In 2012, a health technology assessment analyzed the usage and efficacy of different burnout therapies.85 In this systematic review, 17 papers were included. Thirteen of them (partly in combination with other techniques) deal with the efficacy of psychotherapy and psychosocial interventions for the reduction of burnout. In the majority of the studies, cognitive behaviour therapy seems to result in the improvement of emotional exhaustion. However, evidence is inconsistent for the efficacy of stress management and music therapy. Two studies on the efficacy of Qigong therapy do not deliver a distinct result and only one study shows the efficacy of the roots of Rhodiola Rosea. Physical therapy is examined separately in only one study and does not show a better result than standard therapy. Some authors report the effects of considerable natural recovery.
Conclusion
Burnout has become an important problem and a challenge for public health. Unfortunately, the syndrome still is not clearly defined and there is no consensus on the diagnosis.86
There is an agreement that burnout in medicine is harmful to the professional, the institution, and the patient. Risk situations should be identified and preventive measures should be implemented early to avoid future harm.87 Therefore, prospective, longitudinal studies are needed to further explore the causes of burnout and identify the specific instruments to measure physician’s well-being. We are also in need of additional prospective studies to identify individual and organizational interventions that can promote wellness and evaluate its effect on productivity, patient care, and patient satisfaction. Of note, well-being may depend on different variables and therefore studies specifically focusing on different subpopulations are needed.72,73,75,78,87–90 Staff working in critical care settings may be particularly affected.91 This situation may aggravate when the flow of critically ill patients starts to exceed available capacities, as is for instance the case with the recent COVID-19 pandemic.92
Also the efficacy of therapies for the treatment of burnout syndrome is insufficiently investigated. There is evidence from meta-analyses that organisational issues need to be addressed as well as individual ones,93,94 but the exact most effective strategies to apply in each individual remain to be established. Further studies are needed to evaluate the efficacy of the different therapeutic options.
Disclosure
The author reports no conflicts of interest in this work.
References
- 1.Freudenberger HJ. The staff burn-out syndrome in alternative institutions. Psychotherapy. 1975;12:73–82. [Google Scholar]
- 2.Freudenberger HJ. Burn-out: occupational hazard of the child care worker. Child Care Q. 1977;6:90–99. doi: 10.1007/BF01554695 [DOI] [Google Scholar]
- 3.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397 [DOI] [PubMed] [Google Scholar]
- 4.Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behav. 1981;2:99–113. doi: 10.1002/job.4030020205 [DOI] [Google Scholar]
- 5.Leiter MP, Schaufeli WB. Consistency of the burnout construct across occupations. Anxiety Stress Coping. 1996;9:229–243. doi: 10.1080/10615809608249404 [DOI] [Google Scholar]
- 6.Shanafelt T, Sloan J, Habermann T. The well-being of physicians. Am J Med. 2003;114:513–559. doi: 10.1016/S0002-9343(03)00117-7 [DOI] [PubMed] [Google Scholar]
- 7.Shanafelt T. Burnout in anesthesiology. A call to action. Anesthesiology. 2011;114:1–2. [DOI] [PubMed] [Google Scholar]
- 8.Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149:334–341. doi: 10.7326/0003-4819-149-5-200809020-00008 [DOI] [PubMed] [Google Scholar]
- 9.Shanafelt TD, Balch C, Dyrbye LN, et al. Suicidal ideation among American surgeons. Arch Surg. 2011;146:54–62. doi: 10.1001/archsurg.2010.292 [DOI] [PubMed] [Google Scholar]
- 10.DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians’ characteristics influence patients’ adherence to medical treatment: results from the Medical Outcomes Study. Health Psychol. 1993;12:93–102. doi: 10.1037/0278-6133.12.2.93 [DOI] [PubMed] [Google Scholar]
- 11.Linn LS, Brook RH, Clark VA, Davies AR, Fink A, Kosecoff J. Physician and patient satisfaction as factors related to the organization of internal medicine group practices. Med Care. 1985;23:1171–1178. doi: 10.1097/00005650-198510000-00006 [DOI] [PubMed] [Google Scholar]
- 12.Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15:122–128. doi: 10.1046/j.1525-1497.2000.02219.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grol R, Mokkink H, Smits A, et al. Work satisfaction of general practitioners and the quality of patient care. Fam Pract. 1985;2:128–135. doi: 10.1093/fampra/2.3.128 [DOI] [PubMed] [Google Scholar]
- 14.Melville A. Job satisfaction in general practice: implications for prescribing. Soc Sci Med Med Psychol Med Sociol. 1980;14A:495–499. [DOI] [PubMed] [Google Scholar]
- 15.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358:367. [DOI] [PubMed] [Google Scholar]
- 16.West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296:1071–1078. doi: 10.1001/jama.296.9.1071 [DOI] [PubMed] [Google Scholar]
- 17.Shanafelt TD, Balch C, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:1001–1002. doi: 10.1097/SLA.0b013e3181bfdab3 [DOI] [PubMed] [Google Scholar]
- 18.Firth-Cozens J, Greenhalgh J. Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44:1017–1022. doi: 10.1016/S0277-9536(96)00227-4 [DOI] [PubMed] [Google Scholar]
- 19.Jones JW, Barge BN, Steffy BD, Fay LM, Kunz LK, Wuebker LJ. Stress and medical malpractice: organizational risk assessment and intervention. J Appl Psychol. 1988;73:727–735. doi: 10.1037/0021-9010.73.4.727 [DOI] [PubMed] [Google Scholar]
- 20.Lindblom KM, Linton SJ, Fedeli C, Bryngelsson IL. Burnout in the working population: relations to psychosocial work factors. Int J Behav Med. 2006;13:51–59. doi: 10.1207/s15327558ijbm1301_7 [DOI] [PubMed] [Google Scholar]
- 21.Ahola K, Honkonen T, Isometsä E, et al. Burnout in the general population. Results from the Finnish Health 2000 Study. Soc Psychiatry Psychiatr Epidemiol. 2006;41:11–17. doi: 10.1007/s00127-005-0011-5 [DOI] [PubMed] [Google Scholar]
- 22.Schaufeli WB 2018. Burnout in Europe: relations with national economy, governance, and culture. Research Unit Occupational & Organizational Psychology and Professional Learning (internal report). KU Leuven, Belgium: Available from: https://www.wilmarschaufeli.nl/publications/Schaufeli/500.pdf. [Google Scholar]
- 23.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–1385. doi: 10.1001/archinternmed.2012.3199 [DOI] [PubMed] [Google Scholar]
- 24.Medscape National Physician Burnout & Suicide Report 2020. Available from: https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460. Accessed October15, 2020.
- 25.Shanafelt T. Enhancing Meaning in Work: A prescription for preventing physician burnout and promoting patient-centered care. JAMA. 2009;302:1338–1340. doi: 10.1001/jama.2009.1385 [DOI] [PubMed] [Google Scholar]
- 26.Houkes I, Winants Y. Development of Burnout over time and the causal order of the three dimensions of burnout among male and female GP’s. A three wave panel study. BMC Public Health. 2011;11:240. doi: 10.1186/1471-2458-11-240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of Burnout among physicians. a systematic review. JAMA. 2018;320:1131–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sanfilippo F, Noto A, Foresta G, et al. Incidence and factors associated with burnout in anesthesiology: a systematic review. Biomed Res Int. 2017;8648925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 30.Kaschka WP, Korczak D, Broich K. Burnout—a fashionable diagnosis. Dtsch Arztebl Int. 2011;108:781–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Freudenberger HJ. Counseling and dynamics: treating the end-stage person In: Jones JW, editor. The Burnout Syndrome. Park Ridge III: London House Press; 1982. [Google Scholar]
- 32.Karasek RA. Job demands, job decision latitude, and mental strain. Implications for job redesign. Adm Sci Q. 1979;24:285–308. doi: 10.2307/2392498 [DOI] [Google Scholar]
- 33.Siegrist J, Peter R. The effort-reward imbalance model In: Schnall P, Belkic K, Landsbergis P, Baker D, editors. The Workplace and Cardiovascular Disease. Occupational Medicine State of the Art Reviews. Vol. 15 2000:83–87. [Google Scholar]
- 34.Greenberg J. Organizational justice: yesterday, today, and tomorrow. J Manage. 1990;16:399–432. [Google Scholar]
- 35.Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1:27–41. doi: 10.1037/1076-8998.1.1.27 [DOI] [PubMed] [Google Scholar]
- 36.Elovainio M, Kivimäki M, Helkama K. Organizational justice evaluations, job control, and occupational strain. J Appl Psychol. 2001;86:418–424. doi: 10.1037/0021-9010.86.3.418 [DOI] [PubMed] [Google Scholar]
- 37.Colquitt JA. On the dimensionality of organizational justice: a construct validation of a measure. J Appl Psychol. 2001;86:386–400. doi: 10.1037/0021-9010.86.3.386 [DOI] [PubMed] [Google Scholar]
- 38.Liljegren M, Ekberg K. The associations between perceived distributive, procedural, and interactional organizational justice, self-rated health and burnout. Work. 2009;33:43–51. doi: 10.3233/WOR-2009-0842 [DOI] [PubMed] [Google Scholar]
- 39.Karriker JH, Williams ML. Organizational justice and organizational citizenship behavior: a mediated multifoci model. J Manage. 2009;35:112–135. [Google Scholar]
- 40.De Coninck JB. The effect of organizational justice, perceived organizational support, and perceived supervisor support on marketing employees’ level of trust. J Bus Res. 2010;63:1349–1355. doi: 10.1016/j.jbusres.2010.01.003 [DOI] [Google Scholar]
- 41.Yadav LK, Yadav N. Organizational justice: an analysis of approaches, dimensions and outcomes. NMIMS. 2016;31:14–31. [Google Scholar]
- 42.Ganster DC, Schaubroeck J. Work stress and employee health. J Manage. 1991;17:235–271. doi: 10.1177/014920639101700202 [DOI] [Google Scholar]
- 43.Mark GM, Smith AP. Stress models: a review and suggested new direction In: Houdmont, Leka, editors. Occupational Health Psychology. Vol. 3 Nottingham University Press; EA-OHP series. 2008;111–144. [Google Scholar]
- 44.Colligan TW, Colligan MSW, Higgins M. Workplace stress – etiology and consequences. J Workplace Behav Health. 2006;21:89–97. doi: 10.1300/J490v21n02_07 [DOI] [Google Scholar]
- 45.Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86(3):499–512. doi: 10.1037/0021-9010.86.3.499 [DOI] [PubMed] [Google Scholar]
- 46.Fischer HJ. A psychoanalytic view of burnout In: Farber BA, editor.Stress and Burnout in the Human Service Professions.New York, Pergamon;1983. [Google Scholar]
- 47.Burisch M. Das Burnout-Syndrom. 4th ed. Heidelberg: Springer; 2010. [Google Scholar]
- 48.Korczak D, Huber B, Kister C. Differential diagnosis of the burnout syndrome. GMS Health Technol Assess. 2010;6:1861–8863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Honkonen T, Ahola K, Pertovaara M, et al. The association between burnout and physical illness in the general population —results from the Finnish Health 2000 Study. J Psychosom Res. 2006;61:59–66. doi: 10.1016/j.jpsychores.2005.10.002 [DOI] [PubMed] [Google Scholar]
- 50.Melamed S, Shirom A, Toker S, Shapira I. Burnout and risk of type 2 diabetes: a prospective study of apparently healthy employed persons. Psychosom Med. 2006;68:863–869. doi: 10.1097/01.psy.0000242860.24009.f0 [DOI] [PubMed] [Google Scholar]
- 51.Shirom A, Westman M, Shamai O, Carel R. Effects of work overload and burnout on cholesterol and triglycerides levels: the moderating effects of emotional reactivity among male and female employees. J Occup Health Psychol. 1997;2:275–288. doi: 10.1037/1076-8998.2.4.275 [DOI] [PubMed] [Google Scholar]
- 52.Mommersteeg PMC, Heijnen CJ, Verbraak MJPM, van Doornen LJP. A longitudinal study on cortisol and complaint reduction in burnout. Psychoneuroendocrinology. 2006;31:793–804. doi: 10.1016/j.psyneuen.2006.03.003 [DOI] [PubMed] [Google Scholar]
- 53.Danhof-Pont MB, van Veen T, Zitman FG. Biomarkers in burnout: a systematic review. J Psychosom Res. 2011;70:505–524. doi: 10.1016/j.jpsychores.2010.10.012 [DOI] [PubMed] [Google Scholar]
- 54.Goldberg R, Boss RW, Chan L, et al. Burnout and its correlates in emergency physicians: four years’ experience with a wellness booth. Acad Emerg Med. 1996;3:1156–1164. doi: 10.1111/j.1553-2712.1996.tb03379.x [DOI] [PubMed] [Google Scholar]
- 55.Parker PA, Kulik JA. Burnout, self- and supervisor-rated job performance, and absenteeism among nurses. J Behav Med. 1995;18:581–599. doi: 10.1007/BF01857897 [DOI] [PubMed] [Google Scholar]
- 56.Doan-Wiggins L, Zun L, Cooper MA, Meyers DL, Chen EH. Practice satisfaction, occupational stress, and attrition of emergency physicians. Wellness Task Force, Illinois College of Emergency Physicians. Acad Emerg Med. 1995;2:556–563. [DOI] [PubMed] [Google Scholar]
- 57.Firth-Cozens J. Emotional distress in junior house officers. Br Med J. 1987;295(6597):533–536. doi: 10.1136/bmj.295.6597.533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Campbell DA Jr, Sonnad SS, Eckhauser FE, Campbell KK, Greenfield LJ. Burnout among American surgeons. Surgery. 2001;130:696–705. doi: 10.1067/msy.2001.116676 [DOI] [PubMed] [Google Scholar]
- 59.Geurts S, Rutte C, Peeters M. Antecedents and consequences of work-home interference among medical residents. Soc Sci Med. 1999;48:1135–1148. doi: 10.1016/S0277-9536(98)00425-0 [DOI] [PubMed] [Google Scholar]
- 60.Myers MF. The well-being of physician relationships. West J Med. 2001;174:30–33. doi: 10.1136/ewjm.174.1.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Colford JM Jr, McPhee SJ. The ravelled sleeve of care. Managing the stresses of residency training. JAMA. 1989;261:889–893. [PubMed] [Google Scholar]
- 62.Novack DH, Suchman AL, Clark W, Epstein RM, Najberg E, Kaplan C. Calibrating the physician. Personal awareness and effective patient care. Working Group on Promoting Physician Personal Awareness, American Academy on Physician and Patient. JAMA. 1997;278:502–509. [DOI] [PubMed] [Google Scholar]
- 63.Lewis CE, Prout DM, Chalmers EP, Leake B. How satisfying is the practice of internal medicine? A national survey. Ann Intern Med. 1991;114:1–5. doi: 10.7326/0003-4819-114-1-1 [DOI] [PubMed] [Google Scholar]
- 64.Smith JW, Denny WF, Witzke DB. Emotional impairment in internal medicine house staff. Results of a national survey. JAMA. 1986;255:1155–1158. [PubMed] [Google Scholar]
- 65.Hsu K, Marshall V. Prevalence of depression and distress in a large sample of Canadian residents, interns, and fellows. Am J Psychiatry. 1987;144:1561–1566. [DOI] [PubMed] [Google Scholar]
- 66.Gabbard GO, Menninger RW. The psychology of postponement in the medical marriage. JAMA. 1989;261:2378–2381. doi: 10.1001/jama.1989.03420160110032 [DOI] [PubMed] [Google Scholar]
- 67.Quill TE, Williamson PR. Healthy approaches to physician stress. Arch Intern Med. 1990;150:1857–1861. doi: 10.1001/archinte.1990.00390200057011 [DOI] [PubMed] [Google Scholar]
- 68.Weiner EL, Swain GR, Wolf B, Gottlieb M. A qualitative study of physicians’ own wellness-promotion practices. West J Med. 2001;174:19–23. doi: 10.1136/ewjm.174.1.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kash KM, Holland JC, Breitbart W, et al. Stress and burnout in oncology. Oncology (Huntingt). 2000;14:1621–1634, 1636–1637. [PubMed] [Google Scholar]
- 70.Revisions to selected Medical Staff Standards. Physician Health. Available from: http://www.jacwo.org. Accessed October15, 2020.
- 71.Cooper CL, Rout U, Faragher B. Mental health, job satisfaction, and job stress among general practitioners. Br Med J. 1989;298:366–370. doi: 10.1136/bmj.298.6670.366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ramirez AJ, Graham J, Richards MA, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer. 1995;71:1263–1269. doi: 10.1038/bjc.1995.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bachman KH. Freeborn DK. HMO physicians’ use of referrals. Soc Sci Med. 1999;48:547–557. doi: 10.1016/S0277-9536(98)00380-3 [DOI] [PubMed] [Google Scholar]
- 74.Deckard GJ, Hicks LL, Hamory BH. The occurrence and distribution of burnout among infectious diseases physicians. J Infect Dis. 1992;165:224–228. doi: 10.1093/infdis/165.2.224 [DOI] [PubMed] [Google Scholar]
- 75.Linzer M, Konrad TR, Douglas J, et al. Managed care, time pressure, and physician job satisfaction: results from the physician worklife study. J Gen Intern Med. 2000;15:441–450. doi: 10.1046/j.1525-1497.2000.05239.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Burdi MD, Baker LC. Market-level health maintenance organization activity and physician autonomy and satisfaction. Am J Manag Care. 1997;3:1357–1366. [PubMed] [Google Scholar]
- 77.Bates AS, Harris LE, Tierney WM, Wolinsky FD. Dimensions and correlates of physician work satisfaction in a midwestern city. Med Care. 1998;36:610–617. doi: 10.1097/00005650-199804000-00016 [DOI] [PubMed] [Google Scholar]
- 78.Frank E, McMurray JE, Linzer M, Elon L. Career satisfaction of US women physicians: results from the Women Physicians’ Health Study. Society of General Internal Medicine Career Satisfaction Study Group. Arch Intern Med. 1999;159:1417–1426. [DOI] [PubMed] [Google Scholar]
- 79.Arnetz BB. Physicians’ view of their work environment and organisation. Psychother Psychosom. 1997;66:155–162. doi: 10.1159/000289127 [DOI] [PubMed] [Google Scholar]
- 80.Stoddard JJ, Hargraves JL, Reed M, Vratil A. Managed care, professional autonomy, and income: effects on physician career satisfaction. J Gen Intern Med. 2001;16:675–684. doi: 10.1111/j.1525-1497.2001.01206.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Stamps PL. Physicians and organizations: an uneasy alliance or a welcome relief? J Fam Pract. 1995;41:27–32. [PubMed] [Google Scholar]
- 82.Landon BE, Rschovsky J, Blumenthal D. Changes in career satisfaction among primary care and specialist physicians, 1997–2001. JAMA. 2003;289:442–449. doi: 10.1001/jama.289.4.442 [DOI] [PubMed] [Google Scholar]
- 83.Freeborn DK. Satisfaction, commitment, and psychological wellbeing among HMO physicians. West J Med. 2001;174:13–18. doi: 10.1136/ewjm.174.1.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Linzer M, Visser MR, Oort FJ, Smets EM, McMurray JE, de Haes HC. Predicting and preventing physician burnout: results from the United States and the Netherlands. Am J Med. 2001;111:170–175. doi: 10.1016/S0002-9343(01)00814-2 [DOI] [PubMed] [Google Scholar]
- 85.Korczak D, Wastian M, Schneider M. Therapy of the burnout syndrome. GMS Health Technol Assess. 2012;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Heinemann LV, Heinemann T. Burnout Research: Emergence and Scientific Investigation of a Contested Diagnosis. SAGE Open; 2017:1–12. [Google Scholar]
- 87.De Hert S. Burnout among anesthesiologists: it’s time for action. J Cardiothor Vasc Anesth. 2018;32:2467–2468. doi: 10.1053/j.jvca.2018.06.010 [DOI] [PubMed] [Google Scholar]
- 88.Shanafelt T, Habermann T. Medical residents’ emotional wellbeing. JAMA. 2002;288:1846–1847. doi: 10.1001/jama.288.15.1846 [DOI] [PubMed] [Google Scholar]
- 89.Back AL, Wipf JE, Shanafelt T. Resident Burnout. Ann Intern Med. 2002;137:698–700; discussion 698–700. doi: 10.7326/0003-4819-137-8-200210150-00023 [DOI] [Google Scholar]
- 90.Clever LH. Who is sicker: patients–or residents? Residents’ distress and the care of patients. Ann Intern Med. 2002;136:391–393. doi: 10.7326/0003-4819-136-5-200203050-00012 [DOI] [PubMed] [Google Scholar]
- 91.Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. A critical care societies collaborative statement: burnout syndrome in critical care health-care professionals a call for action. Am J Respir Crit Care Med. 2016;194:106–113. doi: 10.1164/rccm.201604-0708ST [DOI] [PubMed] [Google Scholar]
- 92.Sasangohar F, Jones SL, Masud FN, Vahidy FS, Kash BA. Provider burnout and fatigue during the COVID-19 pandemic: lessons learned from a high-volume intensive care unit. Anesth Analg. 2020;131:106–111. doi: 10.1213/ANE.0000000000004866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272–2281. doi: 10.1016/S0140-6736(16)31279-X [DOI] [PubMed] [Google Scholar]
- 94.Kleinpell R, Moss M, Good VS, Gozal D, Sessler CN. The critical nature of addressing burnout prevention: results from the critical care societies collaborative’s national summit and survey on prevention and management of Burnout in the ICU. Crit Care Med. 2020;48:249–253. doi: 10.1097/CCM.0000000000003964 [DOI] [PMC free article] [PubMed] [Google Scholar]