Abstract
US Latinos, a growing, aging population, are disproportionately burdened by cognitive decline and dementia. Identification of modifiable risk factors is needed for interventions aimed at reducing risk. Broad sociocultural context may illuminate complex etiology among culturally diverse Latinos. Among 1,418 older (≥60 years), low–socioeconomic position (SEP) Latinos (predominantly of Mexican descent) in Sacramento, California, we examined whether US acculturation was associated with cognitive performance, cognitive decline, and dementia/ cognitive impairment without dementia over a 10-year period and whether education modified the associations (Sacramento Area Latino Study on Aging, 1998–2008). Analyses used linear mixed models, competing-risk regression, and inverse probability of censoring weights for attrition. Participants with high US acculturation had better cognitive performance (0.21 fewer cognitive errors at grand-mean-centered age 70 years) than those with low acculturation after adjustment for sociodemographic factors, practice effects, and survey language. Results may have been driven by cultural language use rather than identity factors (e.g., ethnic identity, interactions). Rate of cognitive decline and risk of dementia/cognitive impairment without dementia did not differ by acculturation, regardless of education (β = 0.00 (standard error, 0.00) and hazard ratio = 0.81 (95% confidence interval: 0.49, 1.35), respectively). High US acculturation was associated with better cognitive performance among these older, low-SEP Latinos. Acculturation may benefit cognition when SEP is low. Future studies should incorporate extended longitudinal assessments among more diverse groups.
Keywords: acculturation, cognition, cognitive dysfunction, dementia, education, Hispanic Americans, social determinants of health
Abbreviations
- ARSMA-II
Acculturation Rating Scale for Mexican Americans–Version II
- CI
confidence interval
- CIND
cognitive impairment, no dementia
- HR
hazard ratio
- IPCW
inverse probability of censoring weights
- IQCODE
Informant Questionnaire on Cognitive Decline in the Elderly
- 3MSE
Modified Mini-Mental State Examination
- SALSA
Sacramento Area Latino Study on Aging
- SE
standard error
- SENAS
Spanish and English Neuropsychological Assessment Scales
- SEP
socioeconomic position
- SEVLT
Spanish English Verbal Learning Test
Latinos are 1.5 times as likely to have Alzheimer disease and related dementias as non-Hispanic Whites, and are twice as likely to have cognitive impairment (1–4). However, cognitive outcomes vary among Latino subgroups (5, 6): For example, the odds of cognitive impairment among Mexican Americans are 2–5 times those among non-Hispanic Whites (7, 8). US Latinos are disproportionately burdened by modifiable socioeconomic and health-related dementia risk factors (e.g., low educational level, diabetes), which are shaped by broad social determinants like acculturation (6, 9).
Acculturation is cultural change after exposure to culturally dissimilar people, groups, and social influences; culture is comprised of language, attitudes, beliefs, behaviors, and interactions (10). Nativity initiates the acculturation process, and longer duration of residence in a new country and common language use create opportunities for greater cultural exposure and community integration (10, 11). Importantly, these factors are sometimes treated as proxies for acculturation, but individually they do not capture the full acculturative process or its downstream health pathways (10).
Acculturation shapes health via social and behavioral pathways like daily activities, dietary choices, and health-care access (9). Negative acculturation theory posits that US acculturation worsens health, but positive associations are also known (9, 12, 13). For example, high US acculturation is associated with increased alcohol consumption and smoking and a poorer diet, but also with greater health-care access, economic and educational opportunities, and exercise (12–14). Understanding the relationship between acculturation and cognition may provide greater insight into risk differentials among US Latinos, and broad cultural links may guide intervention efforts aimed at identifying modifiable targets.
Research examining associations between acculturation proxies and cognitive outcomes has produced inconsistent results (7, 15–20). Still, 2 longitudinal studies carried out among Mexican Americans identified a higher risk of cognitive impairment among foreign-born participants than the US-born (16, 17) and better cognitive outcomes among persons with longer durations of residence in the United States (21, 22). Education has received limited exploration in acculturation-cognition research, despite extensive links to both, and a greater focus on the role of education may provide greater insight into the association between acculturation and cognition (10, 12, 13, 23–27).
We examined how a validated measure of US acculturation was associated with cognitive performance and with dementia/cognitive impairment, no dementia (CIND) over a period of 10 years among older, low–socioeconomic position (SEP) Latinos. On the basis of prior cognitive research with acculturation proxies and in contrast with negative acculturation theory, we hypothesized that 1) participants who were less acculturated toward the United States would have higher dementia/CIND risk and accelerated cognitive decline, and 2) the cognitive impact of low acculturation would be more severe for less educated persons.
METHODS
Study population
Participants were drawn from the Sacramento Area Latino Study on Aging (SALSA), a 10-year longitudinal cohort study of 1,789 older (aged ≥60 years), community-dwelling Latinos (predominantly of Mexican descent) in Sacramento, California (28). Baseline age ranged from 60 years to 101 years (1998–1999). Home visits occurred every 12–13 months until 2008, for a maximum of 7 follow-up visits. Interviewer-administered surveys in English or Spanish collected health, lifestyle, and sociodemographic data. Clinical and cognitive assessments were completed. Informed consent was obtained from all participants, and study procedures were approved by institutional review boards. Additional details have been previously published (28, 29). Average annual attrition was 5% (28, 30). Participants lacking acculturation or cognition data (n = 11), those with limited follow-up (<2 visits; n = 253), and those with baseline dementia/CIND (n = 95) were excluded, which left 1,430 participants for unweighted supplemental analyses. We created inverse probability of censoring weights (IPCW) to account for attrition, and 12 participants lacked data on covariates, which left 1,418 eligible participants for weighted analyses.
Measures
Acculturation.
All acculturation measures were assessed at baseline using the validated Acculturation Rating Scale for Mexican Americans–Version II (ARSMA-II), a 30-item multidimensional measure that captures information on language, ethnic identity, and ethnic interactions (31, 32). ARSMA-II has 2 acculturation scales: Anglo, herein referred to as “US,” and Mexican. Points for each question are averaged within each scale, and the Mexican score is then subtracted from the US score to obtain an overall mean score. The US and Mexican subscales of ARSMA-II have strong internal reliability (Cronbach’s α: α = 0.83 and α = 0.88, respectively) and test-retest reliability at 1-week intervals (ρ = 0.94 and ρ = 0.96, respectively), as well as strong concurrent validity with the original ARSMA (ρ = 0.89) (31, 32). We modified cutpoints for dichotomous total US acculturation: ≥0 indicates “high” and <0 indicates “low” (i.e., acculturated toward non-US birth/ancestral country) (31). We combined the small bicultural sample (score = 0; <1%) with persons with high US acculturation (score > 0) because our population was US-based; therefore, exposure to US culture was likely stronger (33).
Language is a driver of acculturation (10). For an acculturation sensitivity assessment, we parsed apart the ARSMA-II measures into cultural language use/preference measures and identity measures and created 2 separate exposures to determine whether language drove cognitive associations. Language use and preference, herein called “language,” was measured with questions on interpersonal communications and media. Identity was measured with questions on social interaction, ethnic identity, and cultural practice and traditions. We calculated individual high/low scores for language- and identity-related acculturation as we did for total US acculturation. Participants scoring as bicultural for language and identity were few (<6% and <1%, respectively).
Bilingualism may benefit cognition via enhanced cognitive reserve (19, 34). Despite a small sample size, we conducted a bicultural language sensitivity assessment for the relationship between a 3-level (high, bicultural, and low) language-related US acculturation exposure and cognitive performance. As for total acculturation, ARSMA-II language questions were scored and high, bicultural, and low scores were designated >0, 0, and <0, respectively.
Cognitive performance.
Cognitive performance was assessed using the Modified Mini-Mental State Examination (3MSE), a 100-point global test validated and field-tested in English and Spanish (35). Higher scores indicated better performance. The 3MSE shows better reliability, test-retest properties, sensitivity, and specificity than the Mini-Mental State Examination and has fewer ceiling effects (35, 36). With repeated measures, we examined cognitive decline over a period of 10 years. Errors were calculated for each assessment and log-transformed for normal distribution (log(101 − 3MSE score)) (37, 38). More errors indicated worse cognition and, over time, decline.
Dementia/CIND.
Dementia/CIND was diagnosed in 3 stages. First, the 3MSE and the Spanish English Verbal Learning Test (SEVLT), a 15-point verbal memory recall test with five 15-word trials, were administered. The SEVLT has been validated in English and Spanish, and the final trial score is usually taken (39, 40). If participants scored less than the 20th percentile on either test or if their scores declined by more than 8 3MSE points or more than 3 SEVLT points from the previous assessment, they were referred for further testing. Second, the Spanish and English Neuropsychological Assessment Scales (SENAS) (41) and the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) (42) were administered. Participants were referred for more testing if they scored as follows: ≥3.40 points on the IQCODE and <10th percentile on ≥1 SENAS tests; <10th percentile on ≥4 SENAS tests; or >4.0 points on the IQCODE. Third, neurologists and neuropsychologists used the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, the National Institute of Neurological and Communicative Disorders and Stroke, and the Alzheimer’s Disease and Related Disorders Association to diagnose dementia/CIND. Demented participants then underwent magnetic resonance imaging and laboratory testing.
Potential confounders.
We considered the following types of factors as confounders in directed acyclic graphs (43): sociodemographic (age, sex, nativity, survey language, migration age, duration of US residence, marital status, education, lifetime occupation, employment), lifestyle (diet, physical activity, smoking, alcohol, sleep), and health (self-reported health, depression, body mass index (weight (kg)/height (m)2), insurance status). Final adjustment excluded variables identified as mediators.
Effect measure modifier.
We examined education as a modifier of acculturation-cognition associations. We dichotomized education (<12 years, “low”; ≥12 years, “high”) on the basis of the distribution of education in the study population and previous research among SALSA and similar populations (33, 44, 45).
Statistical analysis
Main analyses.
Analyses were conducted in SAS 9.4 (SAS Institute, Inc., Cary, North Carolina).
For cognitive performance and decline, we used linear mixed models to produce β coefficients and 95% confidence intervals (46). A higher β coefficient indicated more errors (a lower cognitive score) and, for slope over time, accelerated decline. We used an unstructured correlation structure for within-subject associations and a random intercept (baseline cognitive performance) and slope (linear rate of cognitive change). For incident dementia/CIND, we used competing-risk regression models to produce hazard ratios and 95% confidence intervals and to account for the competing risk of death (47). Participants were observed from study entry to the date of dementia/CIND diagnosis (event of interest), death (competing event), or censoring (last contact date). Time was operationalized as grand-mean-centered visit age (70 years) for both analyses.
We adjusted for 3 sets of confounders. All models included baseline age (43, 48); cognitive performance analyses adjusted for practice effects with first- and second-assessment indicators (49). Model 1 additionally accounted for sex and marital status for demographic adjustment. Model 2 additionally adjusted for education to explore the role of confounding (33, 44, 45). Model 3 additionally adjusted for survey language to account for cultural bias in cognitive testing among persons with greater exposure to US culture and English (50, 51). Modification analyses were conducted within high/low education strata.
We used IPCW for attrition across study visits that was not due to mortality (52, 53). Numerator and denominator models adjusted for visit, quadratic visit, and US acculturation, and denominator models additionally adjusted for age, sex, education, survey language, cognitive score, self-rated health, diabetes, and depression. The IPCW weight mean was 0.99 (standard deviation, 0.36), with a range of 0.27–7.78. Web Table 1 (available at https://doi.org/10.1093/aje/kwaa088) displays unweighted and weighted characteristics by attrition.
Sensitivity assessments.
First, in primary analyses, we divided total acculturation into 2 separate dimensions of language-related and identity-related acculturation, treating each as a dichotomous exposure. Second, in primary analyses, we evaluated the 3-level language acculturation exposure measure to investigate whether bicultural language use may drive beneficial associations with cognitive decline. Third, in supplemental assessments, we examined 2 additional sets of adjustment covariates: 1) adjusting for acculturation proxies to isolate the ARSMA-II exposure, though these factors are highly interrelated, and 2) adjusting for health insurance status given its role in dementia diagnosis, though the direction of association from acculturation is debatable. Fourth, in supplemental assessments, we excluded bicultural total acculturation participants from all cognitive analyses to ensure that they did not drive results.
RESULTS
Table 1 displays descriptive characteristics overall and by total US acculturation and education strata for 1,418 participants. The median age of participants was 68 years; 60.1% were female, and 49.7% were US-born. The median duration of education was 6 years. Levels of total, language-related, and identity-related US acculturation were high for 37.0%, 47.9%, and 17.2% of participants, respectively. The median 3MSE score at baseline was 89, and 10.6% of participants had incident dementia/CIND. During the study, 282 participants (20%) died (data not shown); among those who were free of dementia/CIND (n = 1,276), death was a competing risk for 228 participants (18%).
Table 1.
IPCW-Weighted Sociodemographic and Health Characteristics of Participants, Overall and by Total US Acculturation and Educational Level, Sacramento Area Latino Study on Aging, Sacramento, California, 1998–2008
| Characteristic a | Overall | Total US Acculturation | Educational Level b | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low | High | Low | High | |||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | |
| All participants | 1,418 | 100.0 | 896 | 63.0 | 522 | 37.0 | 959 | 72.0 | 459 | 28.0 |
| Age, yearsc | 68.1 (64.1–73.1) | 68.2 (64.1–73.2) | 67.8 (64.0–72.6) | 68.5 (64.2–73.6) | 66.8 (63.7–71.5) | |||||
| Female sex (vs. male) | 824 | 60.1 | 539 | 62.3 | 285 | 56.2 | 579 | 62.7 | 245 | 53.4 |
| US nativity (vs. non-US birthd) | 719 | 49.7 | 252 | 26.1 | 467 | 90.1 | 364 | 38.1 | 355 | 79.7 |
| Age at migration, yearsc,e | 30.0 (20.0–47.1) | 32.0 (21.0–48.0) | 2.0 (1.0–12.0) | 32.0 (20.8–48.2) | 21.0 (7.6.–30.0) | |||||
| Marriage/domestic partnership (vs. none) | 851 | 60.8 | 544 | 62.2 | 307 | 58.3 | 573 | 60.8 | 278 | 60.6 |
| Missing data | 1 | 1 | 0 | 1 | ||||||
| High educational level (vs. low) | 459 | 28.0 | 141 | 12.0 | 318 | 55.2 | 0 | 0.0 | 459 | 100.0 |
| Duration of education, yearsc | 6.0 (3.0–12.0) | 7.0 (4.0–12.0) | 12.0 (9.0–14.0) | 4.0 (1.0–8.0) | 13.0 (12.0–15.0) | |||||
| Major lifetime occupation | ||||||||||
| Nonmanual | 321 | 20.9 | 116 | 11.7 | 205 | 36.7 | 72 | 7.4 | 249 | 56.2 |
| Manual | 839 | 60.5 | 600 | 67.6 | 239 | 48.2 | 689 | 70.9 | 150 | 33.1 |
| Otherf | 242 | 18.7 | 171 | 20.7 | 71 | 15.1 | 192 | 21.7 | 50 | 10.8 |
| Missing data | 16 | 9 | 7 | 6 | 10 | |||||
| Gross household income,dollars/month | ||||||||||
| <1,000 | 579 | 24.7 | 475 | 57.1 | 104 | 21.8 | 496 | 54.4 | 83 | 17.3 |
| 1,000–1,999 | 455 | 31.3 | 276 | 29.6 | 179 | 34.4 | 325 | 32.6 | 130 | 28.0 |
| ≥2,000 | 365 | 44.0 | 131 | 13.4 | 234 | 43.9 | 124 | 13.0 | 241 | 54.7 |
| Missing data | 19 | 14 | 5 | 14 | 5 | |||||
| English survey language (vs. Spanish) | 641 | 45.0 | 162 | 17.4 | 479 | 92.2 | 275 | 30.3 | 366 | 83.0 |
| Health insurance coverage (vs. none) | 1,296 | 89.5 | 788 | 85.1 | 508 | 96.9 | 853 | 86.8 | 443 | 96.3 |
| Missing data | 2 | 1 | 1 | 2 | 0 | |||||
| Self-rated health of good or better (vs. less than good) | 765 | 52.8 | 413 | 45.3 | 352 | 65.7 | 429 | 44.6 | 336 | 73.9 |
| Body mass indexg | ||||||||||
| <25 | 243 | 17.2 | 144 | 16.3 | 99 | 18.8 | 162 | 17.1 | 81 | 17.6 |
| 25–29 | 524 | 38.5 | 336 | 39.8 | 188 | 36.5 | 351 | 38.0 | 173 | 39.8 |
| ≥30 | 591 | 44.3 | 366 | 44.0 | 225 | 44.7 | 401 | 44.9 | 190 | 42.6 |
| Missing data | 60 | 50 | 10 | 45 | 15 | |||||
| Any alcohol consumption(vs. none)h | 815 | 56.1 | 470 | 50.6 | 345 | 65.4 | 500 | 51.2 | 315 | 68.7 |
| Smoking status | ||||||||||
| Never smoker | 645 | 46.2 | 409 | 46.9 | 236 | 45.0 | 422 | 45.3 | 223 | 48.4 |
| Former smoker | 614 | 41.9 | 383 | 40.7 | 231 | 43.9 | 421 | 41.8 | 193 | 42.2 |
| Current smoker | 159 | 11.9 | 104 | 12.4 | 55 | 11.1 | 116 | 12.9 | 43 | 9.4 |
| Overall fatigue in past month (vs. none) | ||||||||||
| Baseline | 391 | 28.3 | 246 | 28.5 | 145 | 28.0 | 274 | 29.4 | 117 | 25.4 |
| Ever during study period | 682 | 47.9 | 433 | 48.3 | 249 | 47.2 | 474 | 49.6 | 208 | 43.6 |
| Restless sleep in past week(vs. none) | ||||||||||
| Baseline | 322 | 21.8 | 243 | 26.1 | 79 | 14.5 | 249 | 24.2 | 73 | 15.6 |
| Ever during study period | 755 | 53.0 | 534 | 59.1 | 221 | 42.5 | 567 | 58.5 | 188 | 38.8 |
| High level of depressivesymptoms (vs. low)i | ||||||||||
| Baseline | 337 | 23.8 | 259 | 29.0 | 78 | 15.1 | 280 | 28.4 | 57 | 11.9 |
| Ever during study period | 788 | 56.4 | 543 | 61.2 | 245 | 48.1 | 596 | 62.6 | 192 | 40.3 |
| Diabetes diagnosis (vs. none) | ||||||||||
| Baseline | 438 | 31.8 | 270 | 30.9 | 168 | 33.3 | 301 | 32.5 | 137 | 30.1 |
| Ever during study period | 645 | 46.5 | 404 | 46.2 | 241 | 46.9 | 443 | 47.7 | 202 | 43.3 |
| High US acculturation (vs. low)j | ||||||||||
| Total acculturation | 522 | 37.0 | 0 | 0.0 | 522 | 100.0 | 204 | 23.0 | 318 | 72.9 |
| Language-relatedacculturation | 691 | 47.9 | 177 | 18.4 | 514 | 98.3 | 304 | 32.6 | 387 | 87.4 |
| Identity-related acculturation | 247 | 17.2 | 8 | 0.7 | 239 | 45.3 | 88 | 9.9 | 159 | 35.9 |
| 3MSE score (raw score)c | 89.0 (81.0–94.0) | 85.0 (78.0–91.0) | 93.0 (88.0–97.0) | 86.0 (79.0–91.0) | 95.0 (91.0–97.0) | |||||
| Incident dementia/CIND diagnosis (vs. none) | 142 | 10.6 | 103 | 12.1 | 39 | 7.9 | 117 | 12.5 | 25 | 5.6 |
Abbreviations: CIND, cognitive impairment, no dementia; GED, General Educational Development; IPCW, inverse probability of censoring weights; 3MSE, Modified Mini-Mental State Examination.
a Information was collected at baseline unless otherwise stated.
b Educational level was dichotomized: high, ≥12 years/high school/GED; low, <12 years/high school/GED.
c Values are expressed as median (interquartile range).
d Country of non-US birth: Mexico, 88.8%; other, 11.2%.
e Migration age was restricted to 721 non-US-born participants.
f Includes participants categorized as unemployed or housewives.
g Weight (kg)/height (m)2.
h Beer, wine, or liquor.
i 20-item Center for Epidemiologic Studies Depression Scale score ≥16 = high.
j Assessed by means of the Acculturation Rating Scale for Mexican Americans–Version II.
Total US acculturation
Cognitive performance and decline.
Overall. In fully adjusted models, participants with a high level of acculturation made 0.21 fewer cognitive errors at age 70 years (better performance at the grand-mean-centered age) than those with low acculturation (model 3: acculturation β = −0.21 (standard error (SE), 0.05)) (Table 2, Figure 1A). Rate of decline did not differ by acculturation (model 3: acculturation × age β = 0.00 (SE, 0.00)).
Table 2.
IPCW-Weighted Changes in Cognitive Assessment Scores (β (Standard Error)) According to Total US Acculturation, Overall and by Educational Levela, Sacramento Area Latino Study on Aging, Sacramento, California, 1998–2008
| Variable | Model | |||
|---|---|---|---|---|
| Crude | Model 1 b | Model 2 c | Model 3 d | |
| Overall (n = 1,418) | ||||
| High US acculturation (vs. low) | −0.61 (0.04)e | −0.59 (0.04)e | −0.33 (0.04)e | −0.21 (0.05)e |
| Age (per year) | 0.03 (0.00)e | 0.09 (0.00)e | 0.09 (0.00)e | 0.09 (0.00)e |
| High US acculturation × age | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Low educational level (n = 959) | ||||
| High US acculturation | −0.41 (0.05)e | −0.41 (0.05)e | −0.21 (0.06)e | |
| Age | 0.03 (0.00)e | 0.08 (0.01)e | 0.08 (0.01)e | |
| High US acculturation × age | −0.00 (0.01) | −0.00 (0.01) | −0.00 (0.01) | |
| High educational level (n = 459) | ||||
| High US acculturation | −0.19 (0.06)e | −0.16 (0.06)e | −0.20 (0.07)e | |
| Age | 0.04 (0.01)e | 0.12 (0.01)e | 0.12 (0.01)e | |
| High US acculturation × age | −0.00 (0.01) | 0.00 (0.01) | −0.00 (0.01) | |
Abbreviations: GED, General Educational Development; IPCW, inverse probability of censoring weights.
a Educational level was dichotomized: high, ≥12 years/high school/GED; low, <12 years/high school/GED.
b Adjusted for baseline age, practice effects, sex, and marital status.
c Adjusted for baseline age, practice effects, sex, marital status, and education.
d Adjusted for baseline age, practice effects, sex, marital status, survey language, and, in overall models, education.
e P ≤ 0.05 (2-sided).
Figure 1.
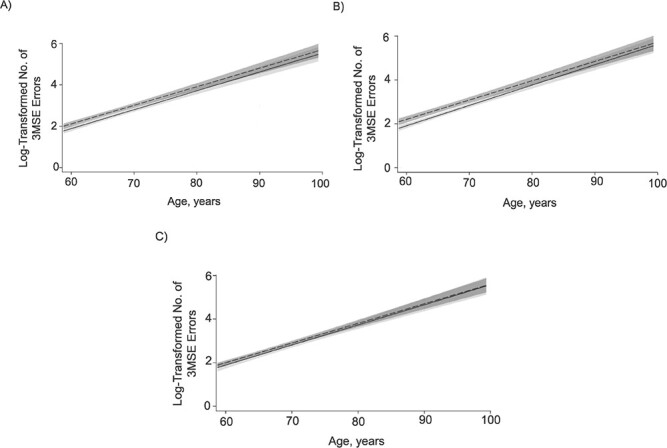
IPCW-weighted and adjusted changes in cognitive assessment scores by level of total (A), language-related (B), and identity-related (C) US acculturation (n = 1,418), Sacramento Area Latino Study on Aging, Sacramento, California, 1998–2008. Dashed lines, low acculturation; solid lines, high acculturation. The lines correspond to β coefficients, and the shaded areas show 95% confidence intervals. Results were adjusted for baseline age, sex, marital status, survey language, and education. IPCW, inverse probability of censoring weights; 3MSE, Modified Mini-Mental State Examination.
By education. For both education strata, cognitive performance was better among high-acculturation participants than among low-acculturation participants, with similar magnitudes (model 3: for low education, acculturation β = −0.21 (SE, 0.06); for high education, β = −0.20 (SE, 0.07)), and decline did not vary.
Incident dementia/CIND.
Overall. In models that adjusted for age, sex, and marital status, high acculturation wasassociated with reduced dementia/CIND risk (model 1: hazard ratio (HR) = 0.62, 95% confidence interval (CI): 0.44, 0.89) (Table 3). After additional adjustment for education and language, the association became null, potentially because of limited statistical power (model 2: HR = 0.75 (95% CI: 0.51, 1.10); model 3: HR = 0.81 (95% CI: 0.49, 1.35)).
Table 3.
IPCW-Weighted Risk of Incident Dementia/CIND According to Total US Acculturation (High vs. Low), Overall and by Educational Level, Sacramento Area Latino Study on Aging, Sacramento, California, 1998–2008
| Model | Overall (n = 1,418) | Educational Level a | ||||
|---|---|---|---|---|---|---|
| Low (n = 959) | High (n = 459) | |||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Crude | 0.64b | 0.45, 0.91 | 0.75 | 0.49, 1.15 | 0.73 | 0.30, 1.79 |
| Model 1c | 0.62b | 0.44, 0.89 | 0.74 | 0.49, 1.14 | 0.73 | 0.30, 1.80 |
| Model 2d | 0.75 | 0.51, 1.10 | ||||
| Model 3e | 0.81 | 0.49, 1.35 | 0.91 | 0.51, 1.63 | 0.48 | 0.18, 1.30 |
Abbreviations: CI, confidence interval; CIND, cognitive impairment, no dementia; GED, General Educational Development; HR, hazard ratio; IPCW, inverse probability of censoring weights.
a Educational level was dichotomized: high, ≥12 years/high school/GED; low, <12 years/high school/GED.
b P ≤ 0.05 (2-sided).
c Adjusted for baseline age, sex, and marital status.
d Adjusted for baseline age, sex, marital status, and education.
e Adjusted for baseline age, sex, marital status, survey language, and, in overall models, education.
By education.ducation did not modify the association between total acculturation and incident dementia/CIND, but fully adjusted effect estimates suggested that statistical power was limited (model 3: for low education, HR = 0.91 (95% CI: 0.51, 1.63); for high education, HR = 0.48 (95% CI: 0.18, 1.30)).
Sensitivity assessment for language-related and identity-related US acculturation
Cognitive performance and decline.
Language-related acculturation results were comparable to total acculturation results for overall models (Figure 1B) but not for educational strata (Table 4). Cognition at age 70 years was better with high language acculturation than with low language acculturation among low-education participants, but cognition did not differ by language acculturation for high-education participants (model 3: acculturation β = −0.25 (SE, 0.07) and β = −0.11 (SE, 0.11), respectively). Identity-related acculturation results differed from those for total acculturation and language acculturation for overall models (Figure 1C) and educational strata. Overall and for low-education participants, high identity acculturation was not associated with cognition at age 70 years (model 3: acculturation β = −0.09 (SE, 0.05) and β = −0.02 (SE, 0.08), respectively). However, for persons with a high level of education, high identity acculturation was associated with better cognitive performance at age 70 years than for those with low education (model 3: acculturation β = −0.15 (SE, 0.06)).
Table 4.
IPCW-Weighted Changes in Cognitive Assessment Scores (β (Standard Error)) According to Language-Related and Identity-Related US Acculturation, Overall and by Educational Levela, Sacramento Area Latino Study on Aging, Sacramento, California, 1998–2008
| Variable | Acculturation Variable and Model | |||||||
|---|---|---|---|---|---|---|---|---|
| Language-Related Acculturation | Identity-Related Acculturation | |||||||
| Crude | Model 1 b | Model 2 c | Model 3 d | Crude | Model 1 b | Model 2 c | Model 3 d | |
| Overall (n = 1,418) | ||||||||
| High US acculturation (vs. low) | −0.62 (0.03)e | −0.61 (0.03)e | −0.34 (0.04)e | −0.25 (0.06)e | −0.49 (0.05)e | −0.47 (0.05)e | −0.20 (0.05)e | −0.09 (0.05) |
| Age (per year) | 0.03 (0.00)e | 0.09 (0.01)e | 0.09 (0.01)e | 0.09 (0.01)e | 0.03 (0.00)e | 0.09 (0.01)e | 0.09 (0.00)e | 0.09 (0.00)e |
| High US acculturation × age | 0.01 (0.00)e | 0.01 (0.00)e | 0.01 (0.00) | 0.00 (0.00) | 0.00 (0.01) | 0.00 (0.01) | 0.00 (0.01) | 0.00 (0.01) |
| Low educational level (n = 959) | ||||||||
| High US acculturation | −0.41 (0.04)e | −0.40 (0.04)e | −0.25 (0.07)e | −0.28 (0.07)e | −0.27 (0.07)e | −0.02 (0.08) | ||
| Age | 0.03 (0.00)e | 0.08 (0.01)e | 0.08 (0.01)e | 0.03 (0.00)e | 0.08 (0.01)e | 0.08 (0.01)e | ||
| High US acculturation × age | 0.00 (0.00) | 0.00 (0.01) | 0.00 (0.01) | 0.00 (0.01) | −0.00 (0.01) | 0.00 (0.01) | ||
| High educational level (n = 459) | ||||||||
| High US acculturation | −0.11 (0.08) | −0.10 (0.08) | −0.11 (0.11) | −0.17 (0.06)e | −0.15 (0.06)e | −0.15 (0.06)e | ||
| Age | 0.03 (0.01)e | 0.12 (0.01)e | 0.12 (0.01)e | 0.04 (0.01)e | 0.12 (0.01)e | 0.12 (0.01)e | ||
| High US acculturation × age | 0.00 (0.01) | 0.00 (0.01) | 0.00 (0.01) | −0.00 (0.01) | −0.00 (0.01) | −0.00 (0.01) | ||
Abbreviations: GED, General Educational Development; IPCW, inverse probability of censoring weights.
a Educational level was dichotomized: high, ≥12 years/high school/GED; low, <12 years/high school/GED.
b Adjusted for baseline age, practice effects, sex, and marital status.
c Adjusted for baseline age, practice effects, sex, marital status, and education.
d Adjusted for baseline age, practice effects, sex, marital status, survey language, and, in overall models, education.
e P ≤ 0.05 (2-sided).
Incident dementia/CIND.
As with total acculturation, neither language-related acculturation nor identity-related acculturation was associated with dementia/CIND (Table 5). Education was not a modifier.
Table 5.
IPCW-Weighted Risk of Incident Dementia/CIND According to Language-Related or Identity-Related US Acculturation, Overall and by Educational Levela, Sacramento Area Latino Study on Aging, Sacramento, California, 1998–2008
| Acculturation Variable and Model | Overall (n = 1,418) | Educational Level a | ||||
|---|---|---|---|---|---|---|
| Low (n = 959) | High (n = 459) | |||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| High language-related US acculturation (vs. low) | ||||||
| Crude | 0.69b | 0.50, 0.95 | 0.80 | 0.55, 1.15 | 1.03 | 0.29, 3.71 |
| Model 1c | 0.63b | 0.45, 0.89 | 0.73 | 0.50, 1.08 | 1.00 | 0.28, 3.63 |
| Model 2d | 0.76 | 0.53, 1.08 | ||||
| Model 3e | 0.81 | 0.51, 1.30 | 0.85 | 0.53, 1.38 | 0.51 | 0.07, 3.89 |
| High identity-related US acculturation (vs. low) | ||||||
| Crude | 0.58b | 0.35, 0.95 | 0.81 | 0.46, 1.45 | 0.41 | 0.15, 1.12 |
| Model 1c | 0.62 | 0.37, 1.01 | 0.84 | 0.47, 1.52 | 0.43 | 0.16, 1.21 |
| Model 2d | 0.72 | 0.43, 1.22 | ||||
| Model 3e | 0.79 | 0.46, 1.37 | 1.02 | 0.54, 1.92 | 0.37 | 0.13, 1.07 |
Abbreviations: CI, confidence interval; CIND, cognitive impairment, no dementia; GED, General Educational Development; HR, hazard ratio; IPCW, inverse probability of censoring weights.
a Educational level was dichotomized: high, ≥12 years/high school/GED; low, <12 years/high school/GED.
b P ≤ 0.05 (2-sided).
c Adjusted for baseline age, sex, and marital status.
d Adjusted for baseline age, sex, marital status, and education.
e Adjusted for baseline age, sex, marital status, survey language, and, in overall models, education.
Sensitivity assessment for bicultural language-related US acculturation: cognitive performance and decline
Prevalences of high, bicultural, and low language-related acculturation were 43.3% (n = 614), 5.4% (n = 77), and 51.3% (n = 727), respectively (data not shown). Overall, participants with high language acculturation had better cognitive performance at age 70 years than participants with low language acculturation (model 3: acculturation β = −0.29 (SE, 0.06)) (Table 6). In comparison with low language acculturation, we did not detect an association between bicultural language acculturation and cognitive performance. Cognitive decline also did not vary.
Table 6.
IPCW-Weighted Changes in Cognitive Assessment Scores (β (Standard Error)) According to a 3-Level Measure of Language-Related US Acculturation (n = 1,418), Sacramento Area Latino Study on Aging, Sacramento, California, 1998–2008
| Variable | Model | |||
|---|---|---|---|---|
| Crude | Model 1 a | Model 2 b | Model 3 c | |
| US acculturation | ||||
| Bicultural (vs. low) | −0.40 (0.08)d | −0.40 (0.08)d | −0.18 (0.07)d | −0.14 (0.08) |
| High (vs. low) | −0.65 (0.04)d | −0.63 (0.04)d | −0.37 (0.04)d | −0.29 (0.06)d |
| Age (per year) | 0.03 (0.00)d | 0.09 (0.01)d | 0.09 (0.01)d | 0.09 (0.01)d |
| US acculturation × age | ||||
| Bicultural (vs. low) | 0.02 (0.01)d | 0.02 (0.01)d | 0.02 (0.01)d | 0.02 (0.01) |
| High (vs. low) | 0.01 (0.00) | 0.01 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
Abbreviations: IPCW, inverse probability of censoring weights.
a Adjusted for baseline age, practice effects, sex, and marital status.
b Adjusted for baseline age, practice effects, sex, marital status, and education.
c Adjusted for baseline age, practice effects, sex, marital status, education, and survey language.
d P ≤ 0.05 (2-sided).
Supplemental sensitivity assessments
Remaining sensitivity assessments for unweighted analyses (Web Tables 2–6), additional sets of adjustment covariates (Web Tables 7 and 8), and exclusion of bicultural total acculturation participants (Web Tables 9 and 10) did not meaningfully alter our results or conclusions.
DISCUSSION
To our knowledge, this was the first population-based longitudinal study to examine associations between multidimensional US acculturation, cognitive performance and decline, and incident dementia/CIND. Supporting prior cognitive research in Latinos and in contrast with the negative acculturation hypothesis, high-US-acculturation participants had better cognitive performance than those with low acculturation (i.e., cultural orientation toward another birth/ancestral country). Cognitive decline and dementia/CIND risk did not vary by acculturation, regardless of education. High language-related acculturation may have stronger beneficial associations with cognitive performance than identity-related acculturation (e.g., self-identity, traditions, social interactions), signifying that language use is salient for cognitive testing scores. Overall, among these older, low-SEP US Latinos, high acculturation was associated with better cognitive performance but not with cognitive decline or dementia/CIND risk.
Cognitive decline did not vary by acculturation, but acculturative differences in cognitive performance were present at study onset (median age, 68 years). Generally, high US acculturation has been linked to poor cardiovascular health and determinants (1, 6, 54, 55), which are key in the etiology of cognitive decline and dementia (38, 54, 56). However, the association between US acculturation and cardiovascular health may be reversed for older Latinos (57, 58). In previous SALSA research, López et al. (57) identified a beneficial association between high US acculturation and some cardiovascular factors (e.g., blood pressure, cholesterol, physical activity), which may partially explain our findings. Moreover, predictors of poor cognition like depression, stress, and poor sleep are more common with low acculturation among older Latinos and SALSA participants (29, 59–67), highlighting other potential mediating pathways. For example, given their lower education, income, and English use, socioeconomic and acculturative stressors were probably more prevalent among SALSA participants with low US acculturation (68, 69).
Acculturation and late-life cognition are shaped across the life course: For example, cognitive decline begins at 20–30 years of age (9, 70, 71). Further, risk factors linked to acculturation (e.g., SEP, chronic conditions) are determinants of life-course cognitive trajectories even in early and midlife (72). Similarly, differences in decline by acculturation for SALSA may have occurred before study onset, which would explain why we only observed established differences in cognitive performance. While acculturation was not associated with cognitive decline in this work, our findings indicate that downstream pathways of low acculturation should be examined as potential drivers of decline in future research.
Education, commonly established in early to midlife, informs social determinants and trajectories of acculturation and cognition (10, 12, 13, 23–27). Education and acculturation in SALSA were closely linked: 55% of high-acculturation participants had a high level of education, as compared with 12% of low-acculturation participants; and 23% of low-education participants (median duration of education, 4 years) had high acculturation, as compared with 73% of high-education participants (median duration of education, 13 years). Cognitive scores at study onset were also better among high-education participants. We expected these differences, since greater acculturation (e.g., English fluency) facilitates social advantages like excelling within educational systems (10, 13, 73). High education is also associated with enhanced cognitive reserve and other positive health outcomes (e.g., access to health care) (23–27). Yet a cognitive advantage among high-acculturation participants persisted across educational strata, even when adjusting for nativity and migration age in supplemental analyses, which should partially account for educational content differences.
High US acculturation was not predictive of dementia/CIND risk when adjusting for demographic factors, education, and survey language, regardless of acculturation type (language-related or identity-related). However, small sample sizes may have limited our power to detect associations, as estimates suggested reduced dementia/CIND risk for high US acculturation. Still, differing results between cognitive performance and dementia/CIND may highlight the importance of cognitive reserve in the expression of clinical dementia. Education shapes cognitive outcomes via multiple pathways (23–27), but high cognitive reserve is posited to offset expression of dementia’s physical brain degeneration (23). Whether acculturation shapes dementia/CIND risk independently of education should be explored further in larger populations.
Language-related acculturation, rather than identity-related acculturation (e.g., traditions, interactions), may drive acculturative differences in cognitive performance and scoring. In the same vein, bilingualism has been hypothesized to enhance cognitive reserve, but the literature is inconsistent, including null findings for cognitive trajectories in SALSA (19, 34). We explored this further in a bicultural language supplemental sensitivity assessment, despite the small sample size. Cognitive performance was better for participants with high language acculturation than for those with low language acculturation, providing confidence that beneficial associations were not attributable to bicultural language use. However, estimates for bicultural language acculturation also suggested a beneficial association. To further interrogate cognitive differences by acculturation subtypes and bicultural language use, larger, more diverse populations and validated approaches for acculturation subtypes are needed, given our modified approach (31).
SEP was low overall in our study population (e.g., a median of 6 years of education and a household income less than $2,000/month for 56% of participants). When SEP is low, high US acculturation may be beneficial for health outcomes (57, 74, 75). Factors like improved health-care access, which is especially important for older populations as chronic disease becomes more common, and stronger social networks may serve as underlying pathways (6, 12, 57, 76–78). However, the mediating dynamics of downstream acculturation pathways require further exploration.
Our study had limitations. First, we used a modified ARSMA-II approach and were unable to fully assess biculturalism given the sample size. However, in a supplemental sensitivity assessment, we excluded persons with bicultural acculturation, which gave confidence to our findings. Second, attrition was a concern, but IPCW accounted for this dropout (52, 53). Third, survivor bias and depletion of exposed (i.e., susceptible) individuals were concerns in our older study population (79, 80). Depletion can lead to a reversal of association (81), but findings were supported by previous literature (16, 17). Fourth, our binary high/low treatment of education may have led to residual confounding, but we based the cutpoint on sample size, population distributions, and previous research (33, 44, 45).
Fifth, we were limited in terms of power to detect associations for dementia/CIND. Sixth, as noted, there are known biases in cognitive testing with higher acculturation and education, but we attempted to account for these biases with covariate adjustment. Moreover, the 3MSE is a brief, global cognitive screening instrument, and we could not draw conclusions about specific cognitive domains. Finally, our study population comprised predominantly low-SEP, Mexican-descent participants, and the ARSMA-II was created for Mexican Americans; therefore, results may not be generalizable to Latinos overall or to other subgroups. However, it is reasonable to hypothesize that populations and individuals with comparable acculturative experiences and immigration patterns could have similar cognitive outcomes.
Our study also had strengths. First, earlier studies mainly used proxy measures of acculturation (e.g., language use, nativity). We employed a validated scale to characterize the complex multifaceted acculturation process (31). Second, we completed multiple sensitivity assessments to further parse apart the complex acculturation process: 1) use of cultural language and identity as separate exposures, 2) assessment of bicultural language acculturation, and 3) exclusion of bicultural total acculturation participants. Third, we accounted for socioeconomic context by examining modification by education to assess the joint sociocultural pathways that shape cognition. Fourth, we used IPCW to account for selection bias. Fifth, we accounted for the competing risk of death in dementia/CIND analyses (47). Sixth, we developed a rigorous methodological approach with multiple sociocultural and clinical measures, including repeated measures of global cognition and thorough multistage diagnosis of incident dementia/CIND.
In conclusion, in this study, participants with high US acculturation had better cognitive performance than those with low US acculturation, which may be explained by cultural language use rather than factors related to identity (e.g., traditions, interactions). The findings do not support a negative acculturation hypothesis for cognitive outcomes but do support previous research that identified worse cognitive outcomes among foreign-born Mexican Americans, an acculturation proxy. Cognitive decline and dementia/CIND risk did not vary by acculturation, regardless of education, though null dementia/CIND findings may be attributable to limited power. Future studies should incorporate extended longitudinal assessments among more diverse Latino groups. If results are replicated, modifiable pathways between high US acculturation and improved health and cognition (e.g., alcohol use, diabetes) should be examined with formal mediation analyses. Identification of novel intervention points (e.g., language proficiency, health-care access) would serve to guide and advance the reduction of poor cognitive outcomes among older Latinos.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina (Erline E. Martinez-Miller, Whitney R. Robinson, Christy L. Avery, Allison E. Aiello); Department of Population and Data Sciences, University of Texas Southwestern Medical Center, Dallas, Texas (Erline E. Martinez-Miller); Social & Scientific Systems, Durham, North Carolina (Erline E. Martinez-Miller); Department of Sociology, Lineberger Comprehensive Cancer Center, Carolina Population Center, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina (Yang C. Yang); Department of Epidemiology and Biostatistics, School of Medicine, University of California, San Francisco, San Francisco, California (Mary N. Haan); and Department of Psychiatry, School of Medicine, University of California, San Francisco, San Francisco, California (Aric A. Prather).
This work was supported by the National Institute on Aging (grants R01AG01297 and R01AG057800), the National Institute of Diabetes and Digestive and Kidney Diseases (grant R01DK087864), and the Center for Integrative Approaches to Health Disparities, National Institute on Minority Health and Health Disparities (grant P60MD002249), of the National Institutes of Health; the Carolina Population Center (grant P2CHD050924); and the Cancer Prevention and Research Institute of Texas (grant RP160157).
We thank members of the Aiello Research Group and staff at the University of California, San Francisco, for their assistance with data management and analysis.
This work was presented in poster form at the 52nd Annual Meeting of the Society for Epidemiologic Research, Minneapolis, Minnesota, June 18–21, 2019.
Conflict of interest: none declared.
REFERENCES
- 1. Alzheimer’s Association . 2018 Alzheimer’s disease facts and figures. Alzheimers Dement. 2018;14(3):367–429. [Google Scholar]
- 2. Alzheimer’s Association . 2010 Alzheimer’s disease facts and figures. Alzheimers Dement. 2010;6(2):158–194. [DOI] [PubMed] [Google Scholar]
- 3. Garcia MA, Downer B, Chiu C-T, et al. Racial/ethnic and nativity differences in cognitive life expectancies among older adults in the United States. Gerontologist. 2019;59(2):281–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States. Washington, DC: US Census Bureau; 2014. (Current Population Reports no. P25-1140). [Google Scholar]
- 5. Mehta KM, Yeo GW. Systematic review of dementia prevalence and incidence in United States race/ethnic populations. Alzheimers Dement. 2017;13(1):72–83. [DOI] [PubMed] [Google Scholar]
- 6. Vega IE, Cabrera LY, Wygant CM, et al. Alzheimer’s disease in the Latino community: intersection of genetics and social determinants of health. J Alzheimers Dis. 2017;58(4):979–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weden MM, Miles JNV, Friedman E, et al. The Hispanic paradox: race/ethnicity and nativity, immigrant enclave residence and cognitive impairment among older US adults. J Am Geriatr Soc. 2017;65(5):1085–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Flores A, López G, Radford J. 2015, Hispanic Population in the United States Statistical Portrait. Washington, DC: Pew Research Center; 2017. [Google Scholar]
- 9. Abraído-Lanza AF, Echeverría SE, Flórez KR. Latino immigrants, acculturation, and health: promising new directions in research. Annu Rev Public Health. 2016;37:219–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: a systematic review of public health studies with Hispanic populations in the United States. Soc Sci Med. 2009;69(7):983–991. [DOI] [PubMed] [Google Scholar]
- 11. Murray KE, Klonoff EA, Garcini LM, et al. Assessing acculturation over time: a four-year prospective study of Asian American young adults. Asian Am J Psychol. 2014;5(3):252–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fox M, Thayer Z, Wadhwa PD. Acculturation and health: the moderating role of socio-cultural context. Am Anthropol. 2017;119(3):405–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lara M, Gamboa C, Kahramanian MI, et al. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abraído-Lanza AF, Armbrister AN, Florez KR, et al. Toward a theory-driven model of acculturation in public health research. Am J Public Health. 2006;96(8):1342–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Xu H, Zhang Y, Wu B. Association between migration and cognitive status among middle-aged and older adults: a systematic review. BMC Geriatr. 2017;17:Article 184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Downer B, Garcia MA, Saenz J, et al. The role of education in the relationship between age of migration to the United States and risk of cognitive impairment among older Mexican Americans. Res Aging. 2018;40(5):411–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Garcia MA, Reyes AM, Downer B, et al. Age of migration and the incidence of cognitive impairment: a cohort study of elder Mexican-Americans. Innov Aging. 2017;1(3):igx037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guzmán-Vélez E, Tranel D. Does bilingualism contribute to cognitive reserve? Cognitive and neural perspectives. Neuropsychology. 2015;29(1):139–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mungas D, Early DR, Glymour MM, et al. Education, bilingualism, and cognitive trajectories: Sacramento Area Latino Aging Study (SALSA). Neuropsychology. 2018;32(1):77–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Moon H, Badana ANS, Hwang SY, et al. Dementia prevalence in older adults: variation by race/ethnicity and immigrant status. Am J Geriatr Psychiatry. 2019;27(3):241–250. [DOI] [PubMed] [Google Scholar]
- 21. Simpao MP, Espino DV, Palmer RF, et al. Association between acculturation and structural assimilation and Mini-Mental State Examination-assessed cognitive impairment in older Mexican Americans: findings from the San Antonio Longitudinal Study of Aging. J Am Geriatr Soc. 2005;53(7):1234–1239. [DOI] [PubMed] [Google Scholar]
- 22. Tang F, Chi I, Zhang W, et al. Activity engagement and cognitive function: findings from a community-dwelling U.S. Chinese aging population study. Gerontol Geriatr Med. 2018;4:2333721418778180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Meng X, D’Arcy C. Education and dementia in the context of the cognitive reserve hypothesis: a systematic review with meta-analyses and qualitative analyses. PLoS One. 2012;7(6):e38268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sharp ES, Gatz M. Relationship between education and dementia: an updated systematic review. Alzheimer Dis Assoc Disord. 2011;25(4):289–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Xu W, Tan L, Wang HF, et al. Education and risk of dementia: dose-response meta-analysis of prospective cohort studies. Mol Neurobiol. 2016;53(5):3113–3123. [DOI] [PubMed] [Google Scholar]
- 26. White L. Educational attainment and mid-life stress as risk factors for dementia in late life. Brain. 2010;133(8):2180–2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jefferson AL, Gibbons LE, Rentz DM, et al. A life course model of cognitive activities, socioeconomic status, education, reading ability, and cognition. J Am Geriatr Soc. 2011;59(8):1403–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Haan MN, Mungas DM, Gonzalez HM, et al. Prevalence of dementia in older Latinos: the influence of type 2 diabetes mellitus, stroke and genetic factors. J Am Geriatr Soc. 2003;51(2):169–177. [DOI] [PubMed] [Google Scholar]
- 29. González HM, Haan MN, Hinton L. Acculturation and the prevalence of depression in older Mexican Americans: baseline results of the Sacramento Area Latino Study on Aging. J Am Geriatr Soc. 2001;49(7):948–953. [DOI] [PubMed] [Google Scholar]
- 30. Haan MN, Lee A, Odden MC, et al. Gender differences in the combined effects of cardiovascular disease and osteoarthritis on progression to functional impairment in older Mexican Americans. J Gerontol A Biol Sci Med Sci. 2016;71(8):1089–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cuellar I, Arnold B, Maldonado R. Acculturation Rating Scale for Mexican Americans-II: a revision of the original ARSMA scale. Hisp J Behav Sci. 1995;17(3):275–304. [Google Scholar]
- 32. Jimenez DE, Gray HL, Cucciare M, et al. Using the revised Acculturation Rating Scale for Mexican Americans (ARSMA-II) with older adults. Hispanic Health Care Int. 2010;8(1):14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ward JB, Haan MN, Garcia ME, et al. Intergenerational education mobility and depressive symptoms in a population of Mexican origin. Ann Epidemiol. 2016;26(7):461–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Noort M, Struys E, Bosch P, et al. Does the bilingual advantage in cognitive control exist and if so, what are its modulating factors? A systematic review. Behav Sci (Basel). 2019;9(3):Article 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Teng EL, Chui HC. The Modified Mini-Mental State (3MS) Examination. J Clin Psychiatry. 1987;48(8):314–318. [PubMed] [Google Scholar]
- 36. Tombaugh TN. Test-retest reliable coefficients and 5-year change scores for the MMSE and 3MS. Arch Clin Neuropsychol. 2005;20(4):485–503. [DOI] [PubMed] [Google Scholar]
- 37. Zeki Al Hazzouri A, Haan MN, Whitmer RA, et al. Central obesity, leptin and cognitive decline: the Sacramento Area Latino Study on Aging. Dement Geriatr Cogn Disord. 2012;33(6):400–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zeki Al Hazzouri A, Haan MN, Neuhaus JM, et al. Cardiovascular risk score, cognitive decline, and dementia in older Mexican Americans: the role of sex and education. J Am Heart Assoc. 2013;2(2):e004978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. González HM, Mungas D, Haan MN. A semantic verbal fluency test for English- and Spanish-speaking older Mexican-Americans. Arch Clin Neuropsychol. 2005;20(2):199–208. [DOI] [PubMed] [Google Scholar]
- 40. González HM, Mungas D, Haan MN. A verbal learning and memory test for English- and Spanish-speaking older Mexican-American adults. Clin Neuropsychol. 2002;16(4):439–451. [DOI] [PubMed] [Google Scholar]
- 41. Mungas D, Reed BR, Haan MN, et al. Spanish and English Neuropsychological Assessment Scales: relationship to demographics, language, cognition, and independent function. Neuropsychology. 2005;19(4):466–475. [DOI] [PubMed] [Google Scholar]
- 42. Quinn TJ, Fearon P, Noel-Storr AH, et al. Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) for the diagnosis of dementia within community dwelling populations. Cochrane Database Syst Rev. 2014;(4):CD010079. [DOI] [PubMed] [Google Scholar]
- 43. Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79(3):340–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zeki Al Hazzouri A, Haan MN, Robinson WR, et al. Associations of intergenerational education with metabolic health in U.S. Latinos. Obesity (Silver Spring). 2015;23(5):1097–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Albrecht SS, Gordon-Larsen P. Socioeconomic gradients in body mass index (BMI) in US immigrants during the transition to adulthood: examining the roles of parental education and intergenerational educational mobility. J Epidemiol Community Health. 2014;68(9):842–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kwok OM, Underhill AT, Berry JW, et al. Analyzing longitudinal data with multilevel models: an example with individuals living with lower extremity intra-articular fractures. Rehabil Psychol. 2008;53(3):370–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. [Google Scholar]
- 48. Pencina MJ, Larson MG, D’Agostino RB. Choice of time scale and its effect on significance of predictors in longitudinal studies. Stat Med. 2007;26(6):1343–1359. [DOI] [PubMed] [Google Scholar]
- 49. Goldberg TE, Harvey PD, Wesnes KA, et al. Practice effects due to serial cognitive assessment: implications for preclinical Alzheimer’s disease randomized controlled trials. Alzheimers Dement (Amst). 2015;1(1):103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Byrd DA, Sanchez D, Manly JJ. Neuropsychological test performance among Caribbean-born and U.S.-born African American elderly: the role of age, education and reading level. J Clin Exp Neuropsychol. 2005;27(8):1056–1069. [DOI] [PubMed] [Google Scholar]
- 51. Dilworth-Anderson P, Hendrie HC, Manly JJ, et al. Diagnosis and assessment of Alzheimer’s disease in diverse populations. Alzheimers Dement. 2008;4(4):305–309. [DOI] [PubMed] [Google Scholar]
- 52. Buchanan AL, Hudgens MG, Cole SR, et al. Worth the weight: using inverse probability weighted Cox models in AIDS research. AIDS Res Hum Retroviruses. 2014;30(12):1170–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Cole SR, Hernan MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Baumgart M, Snyder HM, Carrillo MC, et al. Summary of the evidence on modifiable risk factors for cognitive decline and dementia: a population-based perspective. Alzheimers Dement. 2015;11(6):718–726. [DOI] [PubMed] [Google Scholar]
- 55. Beydoun MA, Beydoun HA, Gamaldo AA, et al. Epidemiologic studies of modifiable factors associated with cognition and dementia: systematic review and meta-analysis. BMC Public Health. 2014;14:Article 643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bruijn RF, Ikram MA. Cardiovascular risk factors and future risk of Alzheimer’s disease. BMC Med. 2014;12:Article 130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. López L, Peralta CA, Lee A, et al. Impact of acculturation on cardiovascular risk factors among elderly Mexican Americans. Ann Epidemiol. 2014;24(10):714–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Rodriguez F, Hastings KG, Hu J, et al. Nativity status and cardiovascular disease mortality among Hispanic adults. J Am Heart Assoc. 2017;6(12):e007207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Herbert J, Lucassen PJ. Depression as a risk factor for Alzheimer’s disease: genes, steroids, cytokines and neurogenesis—what do we need to know? Front Neuroendocrinol. 2016;41:153–171. [DOI] [PubMed] [Google Scholar]
- 60. Richard E, Reitz C, Honig LH, et al. Late-life depression, mild cognitive impairment, and dementia. JAMA Neurol. 2013;70(3):374–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Skogen JC, Bergh S, Stewart R, et al. Midlife mental distress and risk for dementia up to 27 years later: the Nord-Trondelag Health Study (HUNT) in linkage with a dementia registry in Norway. BMC Geriatr. 2015;15:Article 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Johansson L, Guo X, Waern M, et al. Midlife psychological stress and risk of dementia: a 35-year longitudinal population study. Brain. 2010;133(8):2217–2224. [DOI] [PubMed] [Google Scholar]
- 63. Torres L, Driscoll MW, Voell M. Discrimination, acculturation, acculturative stress, and Latino psychological distress: a moderated mediational model. Cultur Divers Ethnic Minor Psychol. 2012;18(1):17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Torres L. Predicting levels of Latino depression: acculturation, acculturative stress, and coping. Cultur Divers Ethnic Minor Psychol. 2010;16(2):256–263. [DOI] [PubMed] [Google Scholar]
- 65. Chiriboga DA, Black SA, Aranda M, et al. Stress and depressive symptoms among Mexican American elders. J Gerontol B Psychol Sci Soc Sci. 2002;57(6):P559–P568. [DOI] [PubMed] [Google Scholar]
- 66. Martinez-Miller EE, Prather AA, Robinson WR, et al. US acculturation and poor sleep among an intergenerational cohort of adult Latinos in Sacramento, California. Sleep. 2019;42(3):zsy246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Dzierzewski JM, Dautovich N, Ravyts S. Sleep and cognition in older adults. Sleep Med Clin. 2018;13(1):93–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Baum A, Garofalo JP, Yali AM. Socioeconomic status and chronic stress. Does stress account for SES effects on health? Ann N Y Acad Sci. 1999;896:131–144. [DOI] [PubMed] [Google Scholar]
- 69. Lueck K, Wilson MD. Acculturative stress in Latino immigrants: the impact of social, socio-psychological and migration-related factors. Int J Intercult Relat. 2011;35(2):186–195. [Google Scholar]
- 70. Fox M, Entringer S, Buss C, et al. Intergenerational transmission of the effects of acculturation on health in Hispanic Americans: a fetal programming perspective. Am J Public Health. 2015;105(suppl 3):S409–S423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Salthouse TA. When does age-related cognitive decline begin? Neurobiol Aging. 2009;30(4):507–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Hughes TF, Ganguli M. Modifiable midlife risk factors for late-life cognitive impairment and dementia. Curr Psychiatry Rev. 2009;5(2):73–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Riosmena F, Everett BG, Rogers RG, et al. Negative acculturation and nothing more? Cumulative disadvantage and mortality during the immigrant adaptation process among Latinos in the United States. Int Migr Rev. 2015;49(2):443–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Espinosa de Los Monteros K, Gallo LC, Elder JP, et al. Individual and area-based indicators of acculturation and the metabolic syndrome among low-income Mexican American women living in a border region. Am J Public Health. 2008;98(11):1979–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Padilla R, Steiner JF, Havranek EP, et al. A comparison of different measures of acculturation with cardiovascular risk factors in Latinos with hypertension. J Immigr Minor Health. 2011;13(2):284–292. [DOI] [PubMed] [Google Scholar]
- 76. Siddiqi A, Zuberi D, Nguyen QC. The role of health insurance in explaining immigrant versus non-immigrant disparities in access to health care: comparing the United States to Canada. Soc Sci Med. 2009;69(10):1452–1459. [DOI] [PubMed] [Google Scholar]
- 77. Bauldry S, Szaflarski M. Immigrant-based disparities in mental health care utilization. Socius. 2017;3:10.1177/2378023116685718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Boustani M, Peterson B, Hanson L, et al. Screening for dementia in primary care: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;138(11):927–937. [DOI] [PubMed] [Google Scholar]
- 79. Glymour MM. Invited commentary: when bad genes look good—APOE*E4, cognitive decline, and diagnostic thresholds. Am J Epidemiol. 2007;165(11):1239–1246. [DOI] [PubMed] [Google Scholar]
- 80. Hernan MA, Alonso A, Logroscino G. Cigarette smoking and dementia: potential selection bias in the elderly. Epidemiology. 2008;19(3):448–450. [DOI] [PubMed] [Google Scholar]
- 81. Weuve J, Proust-Lima C, Power MC, et al. Guidelines for reporting methodological challenges and evaluating potential bias in dementia research. Alzheimers Dement. 2015;11(9):1098–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


