Abstract
The present study: (1) tested whether a structure of common mental disorders within the hierarchical taxonomy of psychopathology was invariant from late childhood to adolescence in a sample of Mexican-origin youth, (2) examined the developmental course of psychopathology at different levels of the hierarchy, and (3) tested the degree to which changes in psychopathology were associated with changes in the Big Five personality domains. Results were consistent with the longitudinal hierarchical invariance of common mental disorders from age 12 to 17 (n = 674). Further, initial levels of conscientiousness, agreeableness, and emotional stability were positively associated with lower initial levels of a higher-order factor of psychopathology, and increases in extraversion and decreases in neuroticism were associated with decreases in a higher-order factor of psychopathology, which captured the general tendency for externalizing, internalizing, and attention-hyperactivity-related dimensions of psychopathology to correlate. Results of the present study indicate that a hierarchicial model of common mental disorders extends to Mexican-origin youth and that developmental change in Big Five personality are related to developmental change in psychopathology.
General Scientific Summary
A hierarchical model of common mental disorders has been documented in previous studes. The present study find that this model extends to Mexican-origin youth. Moreover, results indicate that neuroticism is a developmental risk factor for a general factor of psychopathology.
Hierarchical Taxonomy of Psychopathology.
An established body of research indicates that individual differences in psychopathology are organized in a hierarchical fashion, calling into question traditional nosologies that view psychiatric disorders as binary and categorically distinct (Lahey et al, 2017). At the top of the hierarchy is a single common factor, which captures the broad tendency to experience psychiatric symptoms across diagnostic demarcations (Carragher, Krueger, Eaton & Slade, 2015; Kim & Eaton, 2015). Internalizing and externalizing factors are more specific subordinate factors that capture patterns of comorbidity among subsets of more closely related disorders (e.g., anxiety and depression for internalizing, and conduct problems and substance-use for externalizing). Then, there is variance that is unique to individual symptom dimensions, including unsystematic measurement error. Thus, as with other human individual differences, including personality (Chang, Connelly, & Geeza, 2012; DeYoung & Krueger, 2018; Tackett et al., 2012; van der Linden, Nijenhuis, & Bakker, 2010) and cognitive abilities (Carroll, 2003), patterns of comorbidity among psychiatric symptoms can be understood within a hierarchical taxonomy (Kotov et al., 2017).
Although many studies of the hierarchical structure of psychopathology have focused on adults, a multitude of studies have shown that such patterns of comorbidity are not limited to adulthood but apply to adolescence and childhood as well (Brandes, Herzhoff, Smack, & Tackett, 2019; Castellanos-Ryan et al., 2016; De Bolle, Beyers, De Clercq, & De Fruyt, 2012; Sterba, Egger, & Angold, 2007; Harden et al., 2019; Lahey et al., 2015; Trosper, Whitton, Brown, & Pincus, 2012). In fact, internalizing, externalizing, and general factors of psychopathology have been shown to account for patterns of psychiatric comorbidity in children as young as 3 years old (Olino, Dougherty, Bufferd, Carlson, & Klein, 2014). In support of the criterion validity of latent factors of psychopathology in youth, studies have evinced statistically significant relations with childhood temperament and effortful control (Olino et al., 2014, Shields, Reardon, Brandes, & Tackett, 2019), academic performance (Lahey et al., 2015), and intelligence and executive functions (Harden et al., 2019; Shields et al., 2019). Additionally, moderate and statistically significant correlations between parent- and youth-reports provides evidence for the convergent validity of general and subordinate factors of psychopathology in adolescence (Harden et al., 2019).
Of course, the number and nature of first-order factors depends not only on the true underlying structure of psychopathology, but also on the number and type of psychiatric symptoms that are measured in a given study. When additional problems, such as those associated with obsessive compulsive disorder, mania, and schizophrenia are measured, then a latent factor representing common variation among thought disorders emerges (Caspi et al., 2014). When panic disorder and different phobias are measured, in addition to other common internalizing and externalizing symptoms, then internalizing tends to split into factors representing fear- and distress-related components (Krueger, 1999; Kim & Eaton, 2015; Lahey et al., 2017). When ADHD-related symptoms are extensively assessed, then an attention-related factor emerges (Harden et al., 2019). In other studies, as few as two and as many as nine latent factors have emerged to capture patterns of covariation among symptoms of mental disorders (Lahey et al., 2008; Murray et al. 2016).
In addition to understanding comorbidity among symptoms of common mental disorders, previously categorized as Axis-I disorders, there have also been efforts to include personality disorders when modeling psychiatric comorbidity within a hierarchical taxonomy (e.g., Kotov et al., 2011; Markon, 2010; Røysamb et al., 2011; Widiger et al., 2019; Wright & Simms, 2015). Importantly, when both common mental disorders, personality disorders, and pathological trait dimensions are included in the same study, five latent factors have emerged to account for patterns of comorbidity, which bear a resemblance to the Big Five domains of personality (Wright & Simms, 2015). These findings suggest that domains of basic psychological function and dysfunction may share a common structure and reinforce the appeal of adopting a dimensional perspective on psychopathology.
Dimensional Perspective on Psychopathology.
Psychiatric disorders capture individual differences in behavior, cognition, and emotion that cause significant distress and impairment in life functioning. Personality traits capture individual differences in behavior, cognition, and emotion that span the continuum from functional and healthy to dysfunctional and ill. Consequently, as captured by observations of “the fuzziness of the distinction between dispositions and psychopathology” (Lahey et al., 2017, p. 160), the boundaries between personality and psychopathology are not always clear. A dimensional perspective, however, embraces the lack of clear boundaries between personality and psychopathology with the intent of leveraging knowledge of common developmental processes to understand when, how, and why the development of personality goes awry and, in turn, leads to the expression of psychiatric symptoms (DeYoung & Krueger, 2018; Krueger & Tackett, 2003; Miller, Lynam, Widiger, & Leukefeld, 2001). Thus, a dimensional perspective does not view mental disorders as binary or categorically distinct from healthy domains of functioning. Instead, psychiatric symptoms are conceptualized as extreme or pernicious manifestations and combinations of otherwise healthy cognitions, emotions, and behaviors.
Big Five Personality & Psychopathology.
The Big Five model is the most widely accepted model of normal range variation in personality, positing five broad dimensions to account for individual differences in human behavior, cognition, and emotion: extraversion, agreeableness, conscientiousness, neuroticism, and openness/intellect (John & Soto, in press, Handbook of Personality, 4th edition). Importantly, there is evidence that the Big Five model captures individual differences in youth, even in children as young as 3-to-5 years old (Tackett et al., 2012; Soto & Tackett, 2015). Concurrent associations between levels of Big Five traits and individual psychiatric disorders are also well documented, as are associations between the Big Five and internalizing and externalizing psychopathology in childhood (Decuyper et al., 2009; Kotov et al., 2010; Malouff, Thorsteinsson, & Schutte, 2005; Ruiz, Pincus, & Schinka, 2008; Samuel & Widiger, 2008; Saulsman & Page, 2004).
Studies of Big Five traits and psychopathology indicate that internalizing and externalizing are both negatively associated with conscientiousness and agreeableness in childhood and adolescence (Malouff et al., 2005; De Bolle et al., 2012). Conscientiousness and agreeableness are also negatively associated with symptoms of ADHD (De Pauw & Mervielde, 2011; Miller, Miller, Newcorn, & Halperin, 2008; Nigg et al., 2002). Moreover, conscientiousness is negatively associated with individual substance use, mood, anxiety, and stress-related disorders in adulthood (e.g. major depressive disorder, dysthymic disorder, generalized anxiety, PTSD, specific phobias, social phobias, and panic disorder), while agreeableness is usually not significantly associated with these individual disorders in adulthood (Kotov, Gamez, Schmidt, & Watson, 2010). However, in adolescence, agreeableness is negatively associated with a general factor of psychopathology (Castellanos-Ryan et al., 2016).
The associations between extraversion and some (but not all) mood, anxiety, and stress-related disorders is negative, and associations between extraversion and broad dimensions of internalizing and externalizing tend to be negative and positive, respectively, though these associations appear to be specific to distinct subfactors of extraversion (Kotov et al., 2010; Malouff et al., 2005; Watson et al., 2019). Openness/intellect is usually unrelated to psychopathology, other than disorders involving mania (Barnett et al., 2011; Tackett, Quilty, Sellbom, Rector, & Bagby, 2008), but when divided into its two major subfactors (openness to experience and intellect), openness to experience is positively associated with thought disorders (DeYoung, 2015; Samuel & Widiger, 2008).
Finally, neuroticism is a robust positive correlate of individual substance-use, mood, anxiety, and stress-related disorders in adulthood (Kotov et al., 2010). Neuroticism is also positively associated with internalizing and externalizing dimensions of psychopathology in childhood, though the association with internalizing tends to be much stronger—to the point where internalizing can be difficult to distinguish from neuroticism statistically (Griffith et al., 2009; Malouff et al., 2005). Particularly germane, there is also evidence for strong overlap between the general factor of psychopathology and neuroticism in youth (Brandes et al., 2019; Castellanos-Ryan et al., 2016; Olino et al., 2014; Tackett et al., 2012)
Longitudinal Links Between Personality & Psychopathology.
Although concurrent overlap between the Big Five and psychopathology is well established, longitudinal patterns of co-development have received less attention. Despite the relative paucity of studies that have examined the development of psychopathology and how it relates to the development of personality traits, understanding the developmental dynamics of personality has begun to shed light on internalizing and externalizing psychopathology. For example, longitudinal research has demonstrated that mean levels of disinhibited traits change over adolescent development (Harden & Tucker-Drob, 2011), which maps onto the rise in externalizing behavior that occurs during adolescence. Notably, there is evidence that changes in disinhibited traits are associated with changes in externalizing behaviors, including delinquency and substance use (Atherton, Lawson, Ferrer, & Robins, in press; Mann et al., 2018; Quinn & Harden, 2013). However, the extent to which such developmental links generalize to other personality traits and latent dimension of psychopathology remains unclear.
A large body of research has also examined prospective associations between neuroticism and internalizing problems. For example, a meta-analysis found that longitudinal links between neuroticism and symptoms of anxiety and depression were moderate, even after accounting for variance associated with symptoms at baseline (Jeronimus, Kotov, Riese, & Ormel, 2016). Further, this meta-analysis indicates that the prospective association between neuroticism and later internalizing problems is only slightly larger across short, compared to long, intervals of time. In adolescence, there is also evidence that decreases in extraversion and conscientiousness predict later internalizing and externalizing problems, respectively, and increases in neuroticism predict later internalizing and externalizing problems (van den Akker, Dekovic, & Prinzie, 2010). In turn, externalizing problems have been shown to predict future levels of neuroticism in childhood (Shiner, Masten, & Tellegen, 2002), and internalizing and externalizing problems have been shown to predict future levels of conscientiousness in late childhood and adolescence (De Bolle et al., 2012). There is also evidence that externalizing problems predict future levels of extraversion in adolescence (De Bolle et al., 2012). However, what these studies do not reveal is the extent to which differences in within-individual change in the Big Five are associated with within-individual change in latent psychopathology at different levels of generality and specificity when psychopathology is modeled in a hierarchical fashion.
Motivations for the Present Study.
An empirically-grounded understanding of psychiatric nosology and how it relates to common personality traits has been limited by an overreliance on cross-sectional studies. Additionally, the vast majority of research on transdiagnostic patterns of comorbidity has relied on samples from WEIRD populations with little-to-no racial/ethnic diversity (Western, Educated, and from Industrialized, Rich, and Democratic countries; Henrich, Heine, & Norenzayan, 2010; Jones, 2010), restricting the generalizability of findings. Further, little is known about the developmental dynamics of the hierarchical structure of psychopathology during critical periods such as childhood and adolescence. In particular, it remains unknown whether the measurement, expression, and co-occurrence of psychiatric symptoms differs for Mexican-origin youth, both within and across diagnoses.
Previous studies on the measurement invariance of assessment scales for youth psychopathology have yielded only mixed support for cross-cultural similarity (Stevanovic et al., 2017). A meta-analysis of cross-cultural studies using the Minnesota Multiphasic Personality Inventory (MMPI & MMPI-2) found that ethnic minority groups score higher on some scales and lower on others (Hall, Bansal, & Lopez, 1999). Moreover, Mexican-origin families experience a unique suite of hardships associated with immigration, including poverty, acculturation-related stress, discrimination, and restricted access to health services, which may contribute to the onset and exacerbation of psychiatric symptoms (Torres, Santiago, Walts, & Richards, 2018). As clusters of co-occurring symptoms are often the target of clinical interventions, establishing whether, how, and when patterns of comorbidity change for Mexican-origin youth has high potential impact on the prevention and treatment of psychopathology for this at-risk population. To address these limitations, the present study examines measurement and structural invariance of common mental disorders at different levels of transdiagnostic specificity in a large sample of Mexican-origin youth assessed annually from age 10 to 17. Moreover, we examine associations between changes in Big Five personality and changes in general and subordinate factors of psychopathology.
There are additional reasons that pursuing a developmental perspective on transdiagnostic liability may be especially fruitful. Adolescence is a period of development accompanied by critical biological change (Sisk & Foster, 2004; Sisk & Zehr, 2005) and marked by the onset of many common psychiatric disorders (Paus, Keshavan, & Giedd, 2008), including substance use disorders. Thus, with the onset of substance use and related psychosocial problems in adolescence, the co-occurrence of psychiatric symptoms may be different, compared to childhood and adulthood. Internalizing and externalizing disorders are also known to exhibit heterotypic continuity across the lifespan (Cicchetti & Rogosh, 2002; Kagan, 1980); that is, although internalizing and externalizing symptoms are relatively stable, there are changes in the way symptoms are expressed over the course of development. Given changing symptoms (e.g., somatic complaints and temper-tantrums are common early in development but less common later on), patterns of comorbidity may change as well.
Finally, the effects of biological sex on psychopathology and personality are well documented, in both nationally-representative and clinical samples (Bongers, Koot, Van Der Ende, & Verhulst, 2004; Costello et al., 2003; Del Giudice, Booth, & Irwing, 2012; Kessler et la., 1994; Newman et al., 1996; McLean, Asnaani, Litz, & Hofmann, 2001; Salk, Hyde, & Abramson, 2017; Schmitt et al., 2008; Steel et al., 2015; Vesga-López et al., 2008; Wasserman, McReynolds, Ko, Katz, & Carpenter, 2005). Therefore, to ensure that estimates of developmental covariation between personality and psychopathology are not confounded by sex differences, when estimating growth models of personality and psychopathology, self-reported biological sex was introduced as an exogenous covariate of intercept and slope factors.
Method
Sample
Data came from the California Families Project, a longitudinal study of 674 Mexican-origin youth (50% female) and their parents. The institutional review board at University of California, Davis approved all study procedures (Protocol # 217484–21). Participants were recruited at random using rosters from school districts in Sacramento and Woodland, California. Inclusion criteria for participation included being in 5th grade at the onset of the study, being of Mexican origin, and living with one’s biological mother. Approximately 2/3 of parents (63% of mothers and 65% of fathers) had less than a high school education, and the median household income at the onset of the study was between $30,000 and $35,000 (range = less than $5,000 to greater than $95,000).
Data were collected annually from 5th grade to 12th grade (age 10 to 17), but the present study used data from 7th through 12th grade (age 12 to 17) to examine the co-development of personality and psychopathology, when both symptom-counts for DSM-defined psychiatric disorders and self-reports of Big Five personality were available. Retention rates were high across the duration of the study. Of the original 674 families enrolled in the study, roughly 89% to 92% were retained from waves 3 through 8. Missing data for symptom-counts and measures of Big Five personality were handled using pair-wise deletion, which is the default for Mplus when estimating models with ordinal or categorical dependent variables, resulting in a final analytic sample of n = 646 adolescents to test for longitudinal invariance of a hierarchical structure of common mental disorders and to estimate growth trajectories of psychopathology.
Measures
Psychiatric Symptoms.
Annually from age 10 to 17, the National Institute of Mental Health (NIMH) Diagnostic Interview Schedule for Children-IV (DISC-IV) was administered to youth. The DISC-IV is a semi-structured interview that measures mental health problems for children and adolescents according to DSM-IV and ICD-10 symptom criteria (Shaffer et al., 2000). The DISC-IV has been validated in clinical and community populations, in both English and Spanish (Costello, Edelbrock, & Costello, 1985; Schwab-Stone et al., 1996; Shaffer et al., 2000; translated into Spanish by Bravo, Woodbury-Farina, Canino, & Rubio-Stipec, 1993). For the present study, we used symptom-counts for the following disorders, with symptoms coded as being present or not in the past year: major depressive disorder (MDD), generalized anxiety disorder (GAD), post-traumatic stress disorder (PTSD), inattention and hyperactivity facets of attention-deficit-hyperactivity disorder (ADHD), defiance and emotion dysregulation facets of oppositional defiance disorder (ODD), conduct disorder (CD), and marijuana-use. Symptom-counts were calculated by summing the number of symptoms at each wave to create composite scores.
All interviewers were bilingual and had obtained a B.A./B.S. or higher degree in social sciences or two or more years of experience in survey research, public relations, or community organizations. Interviewers received 45 hours of training to ensure strict adherence to the interview protocol and procedures, including didactic presentations, written materials, modeling, role-playing and practice interviews with families similar to those recruited for the study. Interviewer training also included discussion of at-risk situations in the home and of referral processes if a child or parent was at-risk for abuse, neglect, or suicide. In addition, biweekly meetings were held with interviewers throughout data collection to monitor their work, address potential problems, and reinforce protocol and procedures.
Big Five Personality Traits.
Annually from age 12 to 17, Big Five personality traits were measured using youth responses to the Ten Item Personality Inventory (TIPI; Gosling, Rentfrow, & Swann, 2003), which measures each Big Five trait using two items. The mean of the two items is then calculated to create a composite score. Despite its short length, a number of studies have provided support for the validity and reliability of the TIPI, in both English and Spanish (Ehrhart et al., 2009; Muck, Hell, & Gosling, 2007; Romero, Villar, Gómez-Fraguela, & López-Romero, 2012; Renau, Oberst, Gosling, Rusiñol, & Chamarro, 2013). For example, in a large sample of Spanish-speaking participants, the TIPI exhibited “acceptable psychometric properties for measuring the Big Five in terms of test–retest reliability, self–other agreement, factor structure, convergence with the NEO-PI-R and correlations with relevant criteria” (p. 289, Romero et al., 2012). Given that only two items are used to measure each of the Big Five scales, low internal consistency is a common limitation of the TIPI (Romero et al., 2012) because measures of internal consistency, like Cronbach’s alpha, are highly sensitive to the number of items in the scale (the fewer items, the lower Cronbach’s alpha). However, low-to-moderate internal consistency is desired when measuring a broad construct with a brief measure (Kline, 1986). In such cases, high internal consistency can indicate redundancy in the content of items or a limited rather than a broad focus.
Analytic Procedures
Data were prepared for analysis and descriptive statistics were calculated using R version 3.4.2. Inferential analyses were conducted using Mplus version 8.0 (Muthén & Muthén, 1998–2017). First, we examined whether there were systematic differences for participants with and without missing data. Specifically, using Welch paired t-tests and Wilcoxon paired signed-rank tests, we compared individuals who did and did not participate at the last wave of data collection on assessments of the Big Five and psychopathology assessed at the first wave of data collection. No statistically significant differences were observed (ps > .05).
As would be expected in a non-referred community sample, the distributions of symptoms-counts were highly censored (i.e., zero-inflated). Consequently, prior to conducting further analyses, symptom-counts were transformed into ordered-categorical responses, based on the assumption that ordinal responses provide a coarsened index of an underlying continuous distribution of liability (Rijsdijk & Sham, 2002; Falconer, 1965). The highest number of categorical responses was retained, such that the observed frequencies of each response were approximately equal to or greater than the total number of response categories. This retained as many ordered categories as possible while ensuring sufficient frequencies in each category to estimate threshold parameters, yielding four categories to differentiate between adolescents with different levels of psychopathology: (0) = no symptoms, (1) = one or two symptoms, (2) = three or four symptoms, (3) = five or more symptoms.
In all models, transformed symptom-counts were treated as ordinal indicators using the ‘CATEGORICAL’ option in Mplus, scales scores of Big Five domains were treated as continuous variables, and structural equation models with ordinal indicators were estimated using robust weighted least squares (i.e. WLSMV; Flora & Curran, 2004; Muthén & Muthén, 1998–2017). Descriptive statistics for non-transformed variables and the distributions of transformed variables are reported in the supplemental materials (see Tables S1-S3). To help protect against type-I errors, a conservative threshold was adopted for evaluating the statistical significance of parameter estimates (α = .005; Benjamin et al., 2018), as well as other proposed solutions for improving statistical inference, like focusing on the size and precision of estimated effects (Ioannidis, 2018). Hence, to help ease the interpretation of the relations between personality and psychopathology, intercept-intercept and slope-slope covariances were rescaled as correlations and reported with 95% confidence intervals.
Results
Longitudinal Measurement Invariance.
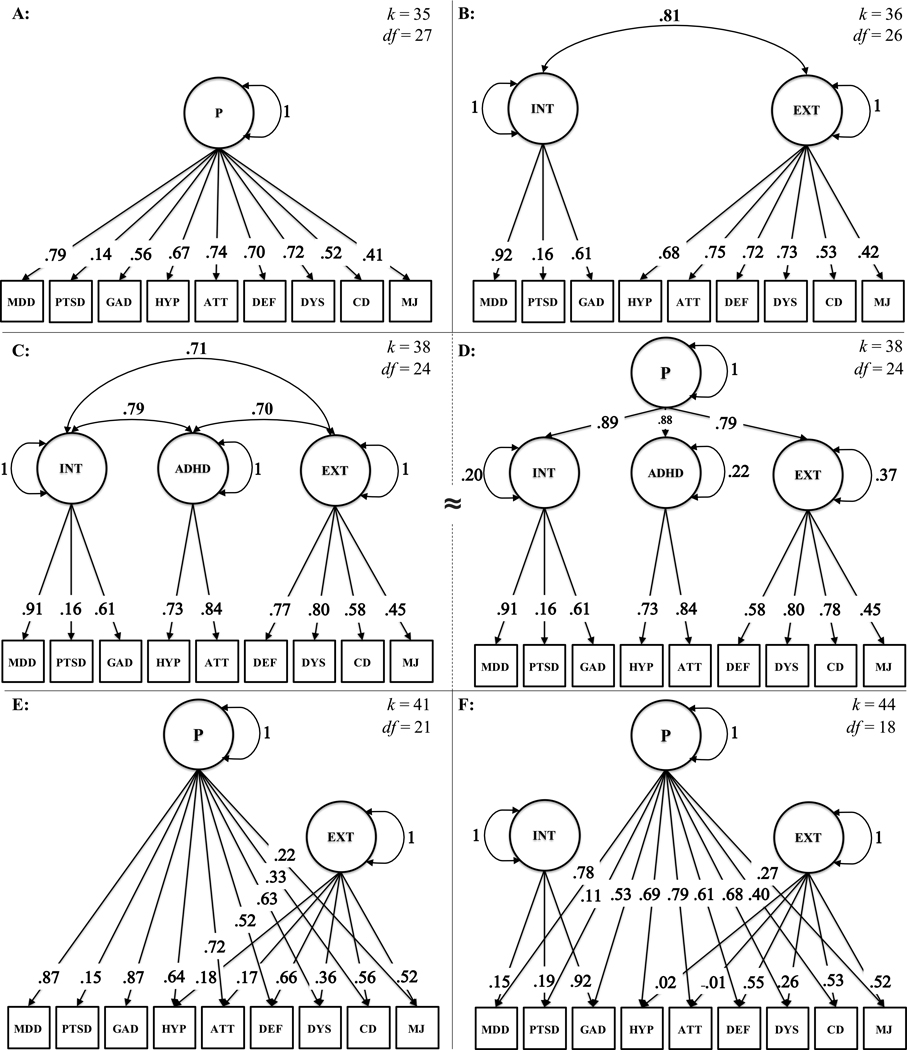
Before examining growth trajectories at different levels of a hierarchical structure of psychopathology, a series of confirmatory factor analysis models were used to test for longitudinal invariance. Detailed descriptions of these models are provided in the supplemental materials, including fit statistics and model comparisons (see Tables S7 & S8). Depicted in Figure 1, one-factor, two-factor, and three-factor models were fit to the data. Note, the correlated three-factor and higher-order models have the same degrees of freedom and fit statistics because the higher-order factor is just-identified (see cells C & D of Figure 1). However, the higher-order model may represent an appropriate interpretative framework when subordinate factors are theoretically salient, and the higher-order factor represents the tendency for these factors to intercorrelate (Markon, 2019). Thus, the higher-order model provides an appropriate interpretative framework for capturing the general tendency for different dimensions of psychopathology to intercorrelate.
Figure 1. Path Diagrams of Cross-Sectional Models of Psychiatric Symptoms.
Notes. Parameter estimates at reported from cross-sectional models at age 17 years. k = number of freely estimated parameters. df = model degrees of freedom. MDD = major depressive disorder. PTSD = post-traumatic stress disorder. GAD = generalized anxiety disorder. HYP = hyperactivity-related symptoms of attention-deficit hyperactivity disorder (ADHD). ATT = attention-related symptoms of ADHD. DEF = defiance-related symptoms of oppositional defiance disorder (ODD). DYS = emotion dysregulation-related symptoms of ODD. CD = conduct disorder symptoms. MJ = marijuana use. INT = Internalizing. EXT = Externalizing. P = Psychopathology.
An alternative approach is the bifactor model, which has been used in previous studies to model the hierarchical structure of psychopathology (Caspi et al., 2014; Kim & Eaton, 2015; Lahey et al., 2017; Murray et al., 2016). Examples of bifactor models are depicted on the bottom of Figure 1. In the present study, bifactor models were compared to alternative models with caution because simulation studies have revealed critical limitations in comparing bi-factor to higher-order and correlated factor solutions (Murray & Johnson, 2013; Morgan, Hodge, Wells, & Watkins, 2015). For example, model comparisons tend to be biased in favor of a bifactor model when there is complexity in the data that is unaccounted for, which is quite common when conducting confirmatory analyses (Murray & Johnson, 2013). Model comparisons also favor the bifactor model even when simulated samples are generated from a different model (Morgan, Hodge, Wells, & Watkins, 2015), particularly when indicators are positively skewed, like counts of psychiatric symptoms (Green et al., In Press). Moreover, bifactor models of psychopathology symptoms can yield latent factors that are unstable and difficult to interpret (Watts, Porre, & Waldman, In Press).
With respect to a hierarchical structure of psychopathology, compared to the more parsimonious higher-order model, the bifactor model posits a related yet distinct interpretative framework for the general and subordinate factors. Unlike the higher-order model, for which the general factor represents the tendency for the dimensions of psychopathology to intercorrelate, the general factor in the bifactor model is theoretically primary to latent internalizing, externalizing, and other subordinate factors, which represent residual variance in psychiatric symptoms that are not explained by the general factor (Markon, 2019). Therefore, with the bifactor model, internalizing and externalizing factors of psychopathology are orthogonal to each other and the bifactor, and capture distinct dimensions of covariation among psychiatric symptoms. Consequently, to capture the general tendency for dimensions of psychopathology to intercorrelate (i.e. to operationalize a general factor of comorbidity), the higher-order model may provide a more appropriate interpretative framework. Nevertheless, given the prominence of the bifactor model in previous studies of the hierarchical structure of psychopathology, the bifactor models depicted in Figure 1 were estimated and included in model comparisons.
Fit statistics unambiguously favored a bifactor model (cell D of Figure 1) at ages 10, 14, and 15 years, but a three-factor model was preferred at ages 12 and 17 years. Fit statistics were discrepant at ages 11, 13, and 16 years1, leading to an equivocal decision regarding the best-fitting model. However, the bi-factor models produced a non-positive definite residual covariance matrix, specifically a negative residual variance for one or more indicators of psychopathology at ages 10, 13, and 17 years. Therefore, the bifactor model was neither carried forward to test for longitudinal invariance nor to estimate growth models. Comparing one, two, and three factor models, at least two of three fit statistics were consistent with the persistence of a three-factor solution from age 11 to 17. On the other hand, at age 10, fit statistics unambiguously preferred a two-factor solution. Therefore, a three-factor model was selected as the best-fitting model from age 11 to 17 and carried forward to test for longitudinal invariance.
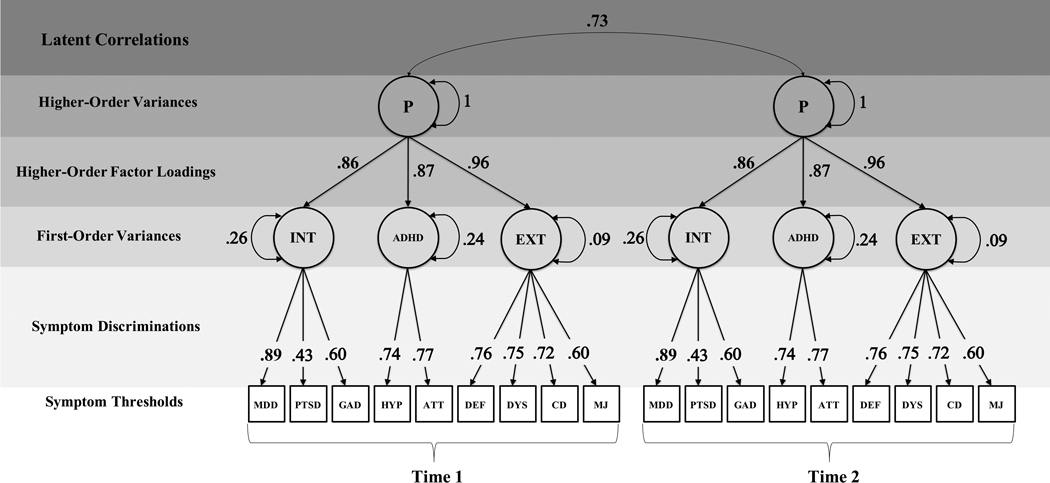
Figure 2 depicts a path diagram of a restrictive model that assumes full longitudinal measurement invariance. This model was compared to a series of less restrictive models that allowed measurement and structural parameters to be freely estimated across measurement occasion (see supplemental materials). Despite some discrepancies across fit statistics, model comparisons were consistent with the longitudinal invariance of a three-factor high-order model from ages 12 to 17. Although fit statistics provided comparatively strong support for the invariance of structural parameters, there was weaker support for the invariance of measurement parameters, especially thresholds for symptom-counts. This suggests that age-related differences in how frequently symptoms are endorsed may not be fully accounted for by age-related differences in the underlying factors. Nevertheless, according to root mean squared error of approximation (RMSEA = .043), a model that freely estimated latent correlations but otherwise assumed full measurement and structural invariance met traditional standards for good model fit (Hu & Bentler, 1999). Although, the comparative fit index (CFI) for this model was below these standards (CFI = .871), it may be argued that RMSEA should be preferred over CFI “in confirmatory contexts, when researchers wish to determine whether a given model fits well enough to yield interpretable parameters” (Rigdon, 1996, p. 378). In addition, small distortions from simple structure have been shown to produce misfit in incremental fit indexes, like CFI, but not RMSEA (Beauducel & Wittmann, 2005). In light of these considerations, the three-factor higher-order model was carried forward for subsequent analyses.
Figure 2. Path Diagram of the Longitudinal Higher-Order Model of Psychopathology.
Notes. The longitudinal baseline model was fit to data at seven measurement occasions (age 11 to 17 years) but only two occasions are depicted to ease visualization. Parameters are freely estimated but constrained to equality over time to reflect longitudinal invariance. MDD = major depressive disorder. PTSD = post-traumatic stress disorder. GAD = generalized anxiety disorder. HYP = hyperactivity-related symptoms of ADHD. ATT. = attention-related symptoms of ADHD. DEF = defiance-related symptoms of ODD. DYS = emotion-dysregulation-related symptoms of ODD. CD = conduct disorder symptoms. MJ = marijuana use. INT = Internalizing. EXT = Externalizing.
In this model, the standardized factor loadings of symptom-counts onto their respective factors were moderate to high (range of λ = .43 to .89, ps < .001). Standardized loadings onto the higher-order factor were high (λs = .86, .87, & .96, ps < .001), indicating a high degree of covariation among latent internalizing, ADHD, and externalizing factors. Indeed, the higher-order factor explained approximately 70–90% of the variance in internalizing factors (R2 = .74, 95% C.I. = .69 to .89), approximately 70–80% of the variance in ADHD factors (R2 = .76, 95% C.I. = .68 to .79), and approximately 85–95% of the variance in externalizing factors (R2 = .91, 95% C.I. = .86 to .96). Nevertheless, there was significant residual variance in internalizing (σ2I = .26, SE = .03, p < .001), ADHD (σ2A = .24, SE = .03, p < .001), and externalizing factors (σ2A = .09, SE = .03, p = .001), after accounting for variance shared with the higher-order factor, which was itself relatively stable across adolescence (range of rs = .42 to .94, ps < .001). The longitudinal stability of the higher-order factor from one year to the next was high (range of rs = .73 to .93, ps < .001), and the stability of the higher-order factor was moderate-to-high over longer intervals of time, specifically 2 to 7 years (range of rs = .42 to .75, ps < .001).
Growth Models.
A series of latent growth models were fit separately to each Big Five trait and latent internalizing, ADHD, externalizing, and higher-order factors. For each construct, an intercept-only model was fit to the data, which implies no growth. This model served as a baseline for comparing alterative models, including linear, quadratic, and latent-basis growth models. Growth models of the Big Five were fit to observed variables while growth models of psychopathology were fit to latent variables. Thus, developmental changes in psychopathology factors were modeled using curve of factors models (CUFFs; McArdle, 1988), whereby a latent factor at each measurement occasion was regressed on intercept and slope factors to characterize initial-levels and changes over time. To examine within-individual changes in the general tendency for latent factors of psychopathology to correlate, the higher-order factor was regressed on intercept and slope factors. Next, a CUFFs model of the higher-order factor was compared to a factor of curves model (FOCUS; Atherton et al., in press; McArdle, 1988), which tests whether common intercept and slope factors can account for associations among the latent intercepts and slopes of internalizing, ADHD, and externalizing factors. A more detailed description of growth curve models is provided in the supplemental materials, including the use of fit statistics, model comparisons, and path diagrams of the higher-order CUFFs and FOCUS models.
Given the statistically significant residual variance in latent factors of psychopathology after accounting for the higher-order factor, a series of bivariate curves of factors models were used to estimate the growth trajectories of internalizing, ADHD, and externalizing factors, while accounting for the higher-order factor. As estimates of standardized residual variance were relatively low after accounting for the higher-order factor (range of σ2 = .09 to .26) and free of unsystematic measurement error, after specifying growth factors, the residual variances of internalizing, ADHD, and externalizing factors were fixed to zero. Consequently, in these models, all of the variance in factors of psychopathology were explained by the higher-order factor, combined with intercept and slope factors for the narrower factors, which capture variation in initial-levels and within-individual changes in psychopathology after accounting for the higher-order factor. In addition, the covariances between intercept and slopes were freely estimated within-domain. In contrast, to reflect the independence of the higher-order and residual factors of psychopathology, the cross-domain covariances between the growth factors for the higher-order and subordinate factors were fixed to zero.
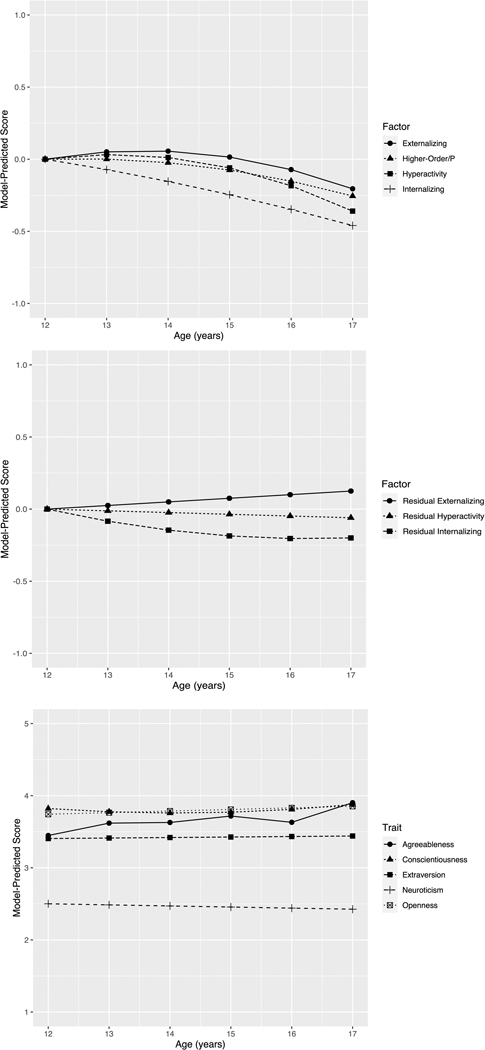
Trajectories of Psychopathology.
Results of growth models are reported in Table 1. Change in model chi-squared (ps < .001) and RMSEA (range = .047 to .067) indicated that a quadratic model was preferred over alternative solutions for internalizing, ADHD, externalizing, and the higher-order factor of psychopathology. On average, internalizing psychopathology was predicted to decrease from age 12 to 17. There was also significant variance in initial-levels of internalizing, rates of linear change, and rates of quadratic change. Initial-levels of internalizing were not significantly associated with linear or quadratic rates of change in internalizing (covintercept-linear = −.036, SE = .023, p = .116; covintercept-quadratic = −.001, SE = .004, p = .838). On average, ADHD psychopathology was predicted to increase slightly from age 12 to 13, before decreasing from age 13 to 17. There was also variance in initial-levels of ADHD and rates of linear change. Initial-levels of ADHD were not significantly associated with linear or quadratic rates of change in ADHD (covintercept-linear = −.054, SE = .029, p = .057; covintercept-quadratic = .003, SE = .005, p = .568).
Table 1.
Estimated Growth Parameters for Big Five Personality and Latent Psychopathology
| Intercept | Linear Slope | Quadratic Slope | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| σ2 | SE | M | SEM | σ2 | SE | M | SEM | σ2 | SE | |
| Agreeableness | .158** | .026 | .066** | .007 | .004* | .002 | - | - | - | - |
| Neuroticism | .197** | .027 | −.032** | .007 | .008** | .002 | - | - | - | - |
| Openness/Intellect | .153** | .024 | .022** | .006 | .003 | .002 | - | - | - | - |
| Extraversion | .253** | .031 | .007 | .008 | .011** | .002 | - | - | - | - |
| Conscientiousness | .259** | .042 | −.059* | .023 | .088** | .042 | .014** | .004 | .003** | .001 |
| Higher-Order Factor | .249** | .025 | .014 | .016 | .050** | .009 | −.013** | .003 | .002** | .000 |
| Internalizing | .424** | .036 | −.067* | .025 | .084** | .022 | −.005 | .005 | .002** | .001 |
| ADHD | .484** | .004 | .058 | .031 | .077** | .032 | −.026** | .006 | .002 | .001 |
| Externalizing | .642** | .044 | .074* | .028 | .145** | .026 | −.023** | .005 | .004** | .001 |
| Residual Internalizing | .115** | .022 | −.095** | .020 | .023 | .015 | .011** | .004 | .001 | .000 |
| Residual ADHD | .151** | .027 | −.012 | .009 | .008** | .003 | - | - | - | - |
| Residual Externalizing | .223** | .024 | .025** | .008 | .011** | .002 | - | - | - | - |
Note. σ2 = variance. SE = standard error. M = mean. SEM = standard error of the mean. One and two asterisks denote estimates that were statistically significant at p(two-tailed) < .05 and p(two-tailed) < .005.
Externalizing psychopathology was predicted to increase from age 12 to 14, before declining from age 14 to 17. There was statistically significant variance in initial-levels of externalizing, rates of linear change, and rates of quadratic change. Initial-levels of externalizing were significantly associated with rates of linear change in externalizing (covintercept-linear = −105, SE = .027, p < .001; covintercept-quadratic = .007, SE = .005, p = .118), such that adolescents with higher levels of externalizing at age 12, on average, increased less rapidly from age 12 to 14. Finally, the higher-order factor, which captured the tendency for latent factors of psychopathology to correlate, remained relatively unchanged from age 12 to 13, before decreasing from age 13 to 17. However, there was statistically significant variation in initial-levels of the higher-order factor, rates of linear change, and rates of quadratic change.
The CUFFs model of the higher-order factor (χ2 = 3514.82, df = 1429, p < .001, RMSEA = .048, CFI = .874) was compared to the FOCUS model (χ2 = 3025.25, df = 1417, p < .001, RMSEA = .042, CFI = .903). Standardized loadings on the common intercept factor were high (λs = .93, .87, .97, ps < .001), as well as the loadings on the common slope factor (range of λs = .98 to 1.0). In fact, the variances of lower-order quadratic growth factors were fixed to zero, as there was no residual variance in these factors after estimating a common factor of quadratic curves. Both models showed good fit to the data, but compared to the CUFFs model, the FOCUS model showed significant improvement in fit (Δχ2 = 374.42, df = 12, p < .001)2. Therefore, when examining the developmental covariation between personality and the higher-order factor of psychopathology, change in personality was estimated using traditional growth models and change in psychopathology was estimated using both CUFFs and FOCUS models. This way the results of bivariate models can be compared across the two approaches.
After accounting for variance captured by the higher-order factor, the average level of residual internalizing was predicted to decrease from age 12 to 15 years and then begin to stabilize from 15 to 17 years. There was significant variance in initial-levels of residual internalizing that was independent from the high-order factor, but variation in rates of change were not significantly different than zero, and initial-levels of residual internalizing were not significantly associated with rates of change in residual internalizing (covintercept-linear = −.006, SE = .015, p = .706; covintercept-quadratic = −.001, SE = .003, p = .693).
After accounting for the higher-order factor, the average level of ADHD psychopathology was predicted to decrease very slightly from age 12 to 17 years, although the average rate of change was not significantly different than zero. However, there was significant variance in initial-levels of residual ADHD psychopathology that was independent from the higher-order factor, as well as rates of change. Initial-levels of residual ADHD psychopathology were not significantly associated with rates of change in ADHD psychopathology (covintercept-linear = −.016, SE = .007, p = .026).
Finally, residual externalizing psychopathology that was independent of the higher-order factor was predicted to increase slightly across adolescence. There was also statistically significant variation in rates of change, and initial-levels of residual externalizing were negatively associated with rates of change (covintercept-linear = −.020, SE = .006, p = .001), such that adolescents with higher-levels of residual externalizing at baseline, on average, exhibited less rapid rates of change in residual externalizing across adolescence. Figure 3 plots the average estimated growth trajectories for latent psychopathology factors (top panel), as well as the growth trajectories for the variance in psychopathology factors after accounting for the higher-order factor (middle panel).
Figure 3. Average Growth Trajectories of Latent Psychopathology Factors and Big Five Personality.
Note. Growth trajectories of psychopathology factors were estimated from linear and quadratic CUFFs models. Growth trajectories estimated from best-fitting growth models.
Trajectories of Big Five Personality Traits.
Before examining the developmental co-occurrence of the Big Five and psychopathology, univariate growth models of the Big Five were estimated. Model fit statistics and nested comparisons for growth models of the Big Five are reported in supplemental materials. For openness/intellect, extraversion, and neuroticism, Δχ2 indicated that a linear growth model was preferred over alternative models. On the other hand, Δχ2 indicated that a quadratic and latent-basis model were preferred for conscientiousness and agreeableness, respectively. The estimated growth trajectories for Big Five personality traits are plotted on the bottom panel of Figure 3.
On average, the Big Five showed little to no growth across adolescence. Mean-levels of openness/intellect increased only slightly from age 12 to 17, while mean-levels of extraversion remained nearly unchanged. However, there was significant variation in initial-levels of extraversion and significant variation in rates of linear change. For openness/intellect, there was significant variation in initial-levels, but not rates of change. Initial-levels of extraversion were associated with changes in extraversion (covintercept-linear = −.020, SE = .007, p = .004), such that adolescents with higher levels of extraversion at age 12, on average, increased less rapidly in extraversion across adolescence. A similar result was observed for openness/intellect. On average, adolescents with higher levels of openness/intellect at age 12 increased less rapidly in openness/intellect across adolescence (covintercept-linear = −.012, SE = .006, p = .028). However, these intercept-slope associations did not reach a conservative threshold for statistical significance (i.e. ps > .005).
Compared to extraversion and openness/intellect, the growth trajectory of neuroticism was in the opposite direction, declining very slightly from age 12 to 17. There was variation in initial-levels of neuroticism and rates of change. Individuals with higher levels of neuroticism at age 12 tended to decrease more slowly in neuroticism across adolescence (covintercept-linear = −.015, SE = .006, p = .023), but this association did not meet a conservative threshold for statistical significance. Conscientiousness remained largely unchanged, but, on average, declined very slightly from age 12 to 14, before inclining very slightly from age 14 to 17. There was variation in levels of conscientiousness at age 12, as well as variation in linear and quadratic rates of change. Initial-levels of conscientiousness were significantly and negatively associated with linear rates of change in conscientiousness (covintercept-linear = −.082, SE = .028, p = .003; covintercept-quadratic = .010, SE = .004, p = .019). Finally, agreeableness increased slightly from age 12 to 17 and in a non-linear fashion. There was variation in levels of agreeableness at age 12. However, variation in non-linear trajectories of agreeableness was not significantly different than zero, and initial-levels of agreeableness were not significantly associated with changes in agreeableness.
Bivariate and Multivariate Growth Models.
Bivariate growth models were used to estimate longitudinal covariation between psychopathology and the Big Five. In bivariate models, the best-fitting growth models from the previous step were carried forward, and associations between the growth factors of the Big Five and latent psychopathology factors were estimated in pairwise combinations. In these models, the correlation between the slope(s) of a personality trait and the curves of latent psychopathology factors were freely estimated.3 These correlations test whether interindividual differences in within-individual change in the Big Five are associated with interindividual differences in within-individual change in psychopathology. Correlations between the intercepts of the Big Five and the intercepts of latent psychopathology factors were also freely estimated, which test whether initial-levels of personality at age 12 were associated with initial-levels of psychopathology. Correlations between growth factors are reported in Tables 2 and 3. One and two asterisks denote correlations that were statistically significant at p < .05 and p < .005, respectively, and exact p-values (> .001) are reported in the text, which represent the probability of the estimated correlation, if the null hypothesis is true.
Table 2.
Correlations Between the Growth Factors of the Big Five and Latent Psychopathology
| Factor: | Higher-Order Factor | ||||||
|---|---|---|---|---|---|---|---|
| Big Five | Correlation: | Intercept-Intercept | Slope-Linear | Slope-Quadratic | |||
| Personality: | Estimate: | Point | Interval | Point | Interval | Point | Interval |
| Openness/Intellect | −.018 | [−.119 to .083] | −.241 | [−.533 to .050] | .224 | [−.092 to .541] | |
| Conscientiousness | −.162** | [−.242 to −.082] | −.003 | [−.047 to .041] | −.045 | [−.103 to .014] | |
| Extraversion | .068 | [−.025 to .160] | −.290** | [−.470 to −.109] | .189 | [−.008 to .386] | |
| Agreeableness | −.206** | [−.305 to −.108] | .052 | [−.169 to .274] | −.027 | [−.267 to .214] | |
| Neuroticism | .458** | [.371 to .546] | .288** | [.092 to .484] | −.322** | [−.536 to −.108] | |
| Factor: | Internalizing | ||||||
| Big Five | Correlation: | Intercept-Intercept | Slope-Linear | Slope-Quadratic | |||
| Personality: | Estimate: | Point | Interval | Point | Interval | Point | Interval |
| Openness/Intellect | −.039 | [−.146 to .068] | −.081 | [−.400 to .238] | −.006 | [−.375 to .363] | |
| Conscientiousness | −.085* | [−.167 to −.003] | −.021 | [−.071 to .030] | −.017 | [−.084 to .051] | |
| Extraversion | −.041 | [−.138 to .056] | −.226 | [−.431 to −.022] | .061 | [−.180 to .301] | |
| Agreeableness | −.151** | [−.254 to −.048] | .220 | [−.063 to .503] | −.222 | [−.541 to .097] | |
| Neuroticism | .430** | [.334 to .525] | .160 | [−.059 to .380] | −.124 | [−.376 to .128] | |
| Factor: | ADHD | ||||||
| Big Five | Correlation: | Intercept-Intercept | Slope-Linear | Slope-Quadratic | |||
| Personality: | Estimate: | Point | Interval | Point | Interval | Point | Interval |
| Openness/Intellect | .007 | [−.100 to .113] | −.408 | [−.862, .046] | .482 | [−.054 to 1.00] | |
| Conscientiousness | −.246** | [−334 to −.157] | .030 | [−.027 to .087] | −.089* | [−.171 to −.007] | |
| Extraversion | .080 | [−.022 to .182] | −.249 | [−.510 to .012] | .188 | [−.105 to .481] | |
| Agreeableness | −.199** | [−.299 to −.099] | .103 | [−.201 to .407] | −.035 | [−.376 to .306] | |
| Neuroticism | .371** | [.273 to .468] | .363* | [.077 to .649] | −.436* | [−.780 to −.091] | |
| Factor: | Externalizing | ||||||
| Big Five | Correlation: | Intercept-Intercept | Slope-Linear | Slope-Quadratic | |||
| Personality: | Estimate: | Point | Interval | Point | Interval | Point | Interval |
| Openness/Intellect | −.012 | [−.112 to .088] | −.212 | [−.494 to .069] | .214 | [−114 to .541] | |
| Conscientiousness | −.124** | [−.203 to −.044] | −.011 | [−.056 to .034] | −.025 | [−.089 to .038] | |
| Extraversion | .127* | [.036 to .219] | −.283** | [−.463 to −.103] | .241* | [.028 to .453] | |
| Agreeableness | −.208** | [−.310 to −.106] | −.115 | [−.366 to .136] | .151 | [−.152 to .454] | |
| Neuroticism | .424** | [.332 to .516] | .253* | [.068 to .439] | −.328** | [−.545 to −.112] | |
Note. Point estimates report zero-order correlations between growth factors. Interval estimates report 95% confidence intervals for point estimates. Intercept-Intercept denotes correlations between the intercepts of personality and psychopathology. Slope-Linear denotes correlations between either a linear slope or latent-basis slope of personality and a linear slope of psychopathology. Slope-Quadratic denotes correlations between linear, quadratic, or latent-basis slopes of personality and a quadratic slope of psychopathology. One and two asterisks denote estimates that were statistically significant at p(two-tailed) < .05 and p(two-tailed) < .005.
Table 3.
Correlations Between the Growth Factors of the Big Five and Residual Variance in Latent Psychopathology After Accounting for the Higher-Order Factor
| Factor: | Residual Internalizing | ||||||
|---|---|---|---|---|---|---|---|
| Big Five | Correlation: | Intercept-Intercept | Slope-Linear | Slope-Quadratic | |||
| Personality: | Estimate: | Point | Interval | Point | Interval | Point | Interval |
| Openness/Intellect | −.065 | [−.190 to .060] | .242 | [−.227 to .710] | −.426 | [−1.08 to .227] | |
| Conscientiousness | .086 | [−.016 to .188] | −.039 | [−.117 to .039] | .047 | [−.064 to .158] | |
| Extraversion | −.221** | [−.341to −.101] | .002 | [−.294 to .297] | −.199 | [−.610 to .211] | |
| Agreeableness | .035 | [−.086 to .156] | .390 | [−.036 to .816] | −.460 | [−1.02 to .103] | |
| Neuroticism | .134* | [.019 to .248] | −.124 | [−.447 to .199] | .286 | [−.172 to .743] | |
| Factor: | Residual ADHD | ||||||
| Big Five | Correlation: | Intercept-Intercept | Slope-Linear | Slope-Quadratic | |||
| Personality: | Estimate: | Point | Interval | Point | Interval | Point | Interval |
| Openness/Intellect | .009 | [−.100 to .119] | .166 | [−.155 to .487] | - | - | |
| Conscientiousness | −.238** | [−.337 to −.138] | .158 | [−.071 to .386] | −.185 | [−.444 to .074] | |
| Extraversion | .042 | [−.075 to .159] | .138 | [−.075 to .351] | - | - | |
| Agreeableness | −.054 | [−.163 to .055] | .170 | [−.084 to .425] | - | - | |
| Neuroticism | −.009 | [−.109 to .090] | −.074 | [−.262 to .115] | - | - | |
| Factor: | Residual Externalizing | ||||||
| Big Five | Correlation: | Intercept-Intercept | Slope-Linear | Slope-Quadratic | |||
| Personality: | Estimate: | Point | Interval | Point | Interval | Point | Interval |
| Openness/Intellect | .003 | [−.092 to .097] | −.074 | [−.331 to .183] | - | - | |
| Conscientiousness | .016 | [−.061 to .094] | −.140 | [−.304 to .025] | .135 | [−.045 to .314] | |
| Extraversion | .155** | [.061 to .250] | −.041 | [−.212 to .103] | - | - | |
| Agreeableness | −.145** | [−.240 to −.049] | −.131 | [−.331 to .070] | - | - | |
| Neuroticism | .223** | [.131 to .315] | −.043 | [−.208 to .122] | - | - | |
Note. Point estimates report zero-order correlations between growth factors. Interval estimates report 95% confidence intervals for point estimates. Intercept-Intercept denotes correlations between the intercepts of personality and psychopathology. Slope-Linear denotes correlations between either a linear slope or latent-basis slope of personality and a linear slope of psychopathology. Slope-Quadratic denotes correlations between linear, quadratic, or latent-basis slopes of personality and a quadratic slope of psychopathology. One and two asterisks denote estimates that were statistically significant at p(two-tailed) < .05 and p(two-tailed) < .005.
Openness/Intellect & Psychopathology.
Initial-levels of openness/intellect were not significantly associated with initial-levels of internalizing (p = .471), ADHD (p = .901), externalizing (p = .812), or a higher-order factor of psychopathology (p = .728). Similarly, changes in openness/intellect were not significantly associated with changes in internalizing (pslope-linear = .618, pslope-quadratic = .974), changes in ADHD (pslope-linear =.038, pslope-quadratic = .974), changes in externalizing (pslope-linear = .113, pslope-quadratic = .169), or changes in a higher-order factor of psychopathology (pslope-linear = .085; pslope-quadratic = .145). After accounting for the higher-order factor, initial-levels of residual internalizing were not significantly associated with initial-levels of openness/intellect (p = .308), similar to associations with initial-levels of residual externalizing (p = .955) and residual ADHD (p = .867). Changes in openness/intellect were not significantly associated with changes in residual internalizing (pslope-linear = .312; pslope-quadratic = .201), changes in residual externalizing (pslope-linear =.038), or changes in residual ADHD (pslope-linear = .311).
Conscientiousness & Psychopathology.
Initial-levels of conscientiousness were not significantly associated with initial-levels of internalizing (p = .042) but were negatively associated with initial-levels of ADHD (p < .001), initial-levels of externalizing (p = .002), and initial-levels of the higher-order factor of psychopathology (p < . 001). Changes in conscientiousness were not associated with changes in internalizing (pslope-linear = .426; pslope-quadratic = .630), changes in ADHD (pslope-linear = . 309; pslope-quadratic = .034), changes in externalizing (pslope-linear = .632; pslope-quadratic = .426), or changes in the higher-order factor (pslope-linear = .892; pslope-quadratic = .135). After accounting for the higher-order factor of psychopathology, initial-levels of residual internalizing were not significantly associated with initial-levels of conscientiousness (p = .098) or initial-levels of residual externalizing (p = .675). However, initial-levels of conscientiousness were negatively associated with initial-levels of residual ADHD (p < .001). Changes in conscientiousness were not significantly associated with changes in residual internalizing (pslope-linear = .327; pslope-quadratic = .407), changes in residual externalizing (pslope-linear = .095), or changes in residual ADHD (pslope-linear = .176).
Extraversion & Psychopathology.
Initial-levels of extraversion were not significantly associated with initial-levels of internalizing (p = .408), ADHD (p = .128), or initial-levels of the higher-order factor of psychopathology (p = .153). However, initial-levels of extraversion were marginally and positively associated with initial-levels of externalizing (p = .008). Within-individual changes in extraversion were not significantly associated with changes in internalizing (pslope-linear = .029; pslope-quadratic = .662) or changes in ADHD (pslope-linear = .046; pslope-quadratic = .191). However, rates of change in extraversion were significantly associated with rates of change in externalizing (pslope-linear = .001; pslope-quadratic =.020), as well as rates of change in the higher-order factor of psychopathology (pslope-linear = .001; pslope-quadratic = .059). After accounting for the higher-order factor, initial-levels of residual internalizing were negatively associated with initial-levels of extraversion (p < .001). On the other hand, initial-levels of residual externalizing were positively associated with initial-level of extraversion (p = .001). Initial-levels of extraversion were not significantly associated with initial-levels of residual ADHD (p = .485). Changes in extraversion were not significantly associated with changes in residual internalizing (pslope-linear = .992; pslope-quadratic = .341), changes in residual externalizing (pslope-linear = .642) or changes in residual ADHD (pslope-linear = .203).
Agreeableness & Psychopathology.
Initial-levels of agreeableness were negatively associated with initial-levels of internalizing (p = .005), ADHD (p < .001), externalizing (p < .001), and higher-order psychopathology (p < .001). On the other hand, changes in agreeableness were not significantly associated with changes in psychopathology, including changes in internalizing (pslope-linear = .111, pslope-quadratic = .159), changes in ADHD (pslope-linear = .494; pslope-quadratic = .839), changes in externalizing (pslope-linear = .352; pslope-quadratic = .303), and changes in higher-order psychopathology (pslope-linear = .642; pslope-quadratic = .829). After accounting for the higher-order factor, initial-levels of residual internalizing were not significantly associated with initial-levels of agreeableness (p = .570) or initial-level of residual ADHD (p = .332). However, initial-levels of agreeableness were negatively associated with initial-levels of residual externalizing (p < .001), such that adolescents with high levels of externalizing at age 12, independent of the tendency for dimensions of psychopathology to correlate, on average, had lower levels of agreeableness at age 12. Changes in agreeableness were not significantly associated with changes in residual internalizing (pslope-linear = .073; pslope-quadratic = .110), changes in residual externalizing (pslope-linear = .202), or changes in residual ADHD (pslope-linear = .190).
Neuroticism & Psychopathology.
Initial-levels of neuroticism were positively associated with initial-levels of psychopathology, including internalizing, ADHD, externalizing, and higher-order factors psychopathology (ps < .001). Changes in neuroticism were not significantly associated with changes in internalizing (pslope-linear = .145; pslope-quadratic = .326) but were marginally associated with changes in ADHD (pslope-linear = .008; pslope-quadratic = .006) and externalizing (pslope-linear = .008; pslope-quadratic = .003). Finally, changes in neuroticism were significantly associated with changes in the higher-order factor of psychopathology (pslope-linear = .004; pslope-quadratic = .003). After accounting for the higher-order factor, the association between initial-levels of residual internalizing and neuroticism did not meet a conservative threshold for statistical significance (p =.023). Moreover, initial-levels of neuroticism were not significantly associated with initial-levels of residual ADHD (p = .859). However, initial-levels of neuroticism were significantly and positively associated with initial-levels of residual externalizing (p < .001). Changes in neuroticism were not significantly associated with changes in residual internalizing (pslope-linear = .453; pslope-quadratic = .222), changes in residual externalizing (pslope-linear = .611), or changes in residual ADHD (pslope-linear = .445).
Effects of Biological Sex.
Next, self-reported biological sex (coded female = 1, male = 0) was introduced to univariate and bivariate growth curve models as a time-invariant covariate of intercept and slope factors. The regression of intercept and slope factors on biological sex tests whether being female, as opposed to male, is associated with initial-levels or rates of change in psychopathology or the Big Five. As a consequence of regressing growth factors on biological sex, intercept-intercept and slope-slope correlations between psychopathology and the Big Five are partial, as opposed to zero-order, helping to ensure that associations are not confounded by sex differences. The standardized effects of biological sex on the growth factors of psychopathology and the Big Five are reported in Table 4 (i.e. STDY; Muthén & Muthén, 1998–2017), which are interpreted as the predicted difference in standard deviation units due to being female, as opposed to male. Exact p-values (> .001) are reported in the text, which represent that probability of the observed sex difference assuming the null hypothesis is true (i.e. there is no difference between females and males).
Table 4.
Effects of Biological Sex on the Growth Factors of Big Five Personality and Psychopathology
| βintercept | βlinear | βquadratic | |
|---|---|---|---|
| Agreeableness | .395**(.137 to .654) | −.018 (−.411 to .374) | - |
| Neuroticism | .282* (.046 to .518) | .135 (−.180 to .451) | - |
| Openness/Intellect | .168 (−.084 to .419) | −.099 (−.543 to .345) | - |
| Extraversion | −.124 (−.349 to .100) | .034 (−.243 to .311) | - |
| Conscientiousness | .371**(.129 to .613) | −.093 (−.398 to .212) | .032 (−.266 to .330) |
| Higher-Order Factor | .223*(.036 to .411) | .492** (.219 to .765) | −.541**(−.841 to −.241) |
| Internalizing | .304**(.101 to .506) | .655** (.324 to .987) | −.647**(−1.02 to −.277) |
| ADHD | −.043 (−.261 to .176) | .722**(.269 to 1.174) | −.814**(−1.35 to −.277) |
| Externalizing | .286**(.092 to .481) | .117 (−.166 to .400) | −.205 (−.528 to .118) |
| Residual Internalizing | .248 (−.012 to .508) | .601*(.104 to 1.097) | −.474 (−1.020 to .072) |
| Residual ADHD | −.416**(−.682 to −.151) | −.053 (−.433 to .327) | - |
| Residual Externalizing | .179 (−.035 to .393) | −.293*(−.575 to −.010) | - |
Note. Sex was coded 1 = female and 0 = male. Standardized (STDY) coefficients are reported. One and two asterisks denote estimates that were statistically significant at p(two-tailed) < .05 and p(two-tailed) < .005.
With respect to psychopathology, biological sex was a relatively strong predictor of initial-levels and rates of change in adolescence. For example, being female was associated with higher-initial levels of internalizing (p = .004) and externalizing (p = .005). Being female was also associated with rates of change in internalizing (plinear < .001; pquadratic < .001), ADHD (plinear = .001; pquadratic < .001), and higher-order psychopathology (plinear = .001; pquadratic < .001). On the other hand, biological sex was not significantly associated with initial-levels of ADHD and higher-order psychopathology or changes in externalizing. After accounting for the higher-order factor of psychopathology, biological sex was neither a significant predictor of initial-levels of residual internalizing and externalizing nor rates of change in residual internalizing and externalizing. However, biological sex was a significant predictor of initial-levels of residual ADHD (p = .002), but not a significant predictor of rates of change in residual ADHD.
With respect to the Big Five, being female was associated with higher initial-levels of agreeableness (p = .003) and higher initial-levels of conscientiousness at age 12 (p = .002). Despite the fact that biological sex was associated with initial-levels and rates of change in dimensions of psychopathology and personality, the intercept-intercept and slope-slope associations that were estimated in bivariate growth models remained largely unchanged after including biological sex as a covariate of growth factors. However, there was one exception. The slope-slope association between neuroticism and the higher-order factor was similar in magnitude (.251 versus .288), but only marginally significant after accounting for the effects of biological sex on growth factors (rlinear-linear = .251 [.056 to .446], p = .013; rlinear-quadratic = −.283 [−0.497, −.069], p = .011). A comprehensive comparison of zero-order and partial correlations between growth factors (controlling for biological sex) are reported in the supplemental materials.
Discussion
Structure of Common Mental Disorders in Mexican-Origin Youth.
The results of the present study demonstrate longitudinal invariance of a hierarchical structure of common mental disorders in Mexican-origin youth from age 11 to 17. This implies that patterns of comorbidity among symptoms of common mental disorders remain largely unchanged from 11 to 17 years old. As minimizing the severity and prevalence of co-occurring symptoms is often the target of clinical interventions, the present study suggests that these targets remain relatively unchanged for Mexican-origin youth from late childhood through adolescence. On the other hand, results also suggest that the boundaries between ADHD-related symptoms and externalizing problems are not clearly defined at age 10, such that attention-related symptoms of ADHD are just as closely related to the symptoms of externalizing disorders than hyperactivity-related symptoms of ADHD. In other words, results suggest that the differentiation of ADHD symptoms from the co-occurrence of other externalizing problems is not clear at age 10 but emerges more clearly in adolescence. As a consequence, clinicians should recognize that the differential expression of ADHD from externalizing may not be clear in younger children but, rather, should emerge as individuals develop from late childhood through adolescence.
With initiation of substance use in adolescence, one might predict a subsequent change in patterns of symptom expression and comorbidity (Carragher et al., 2015). In the current study, at age 12 and 13 less than 1% and 2% of youth reported marijuana use problems, compared to 10% by age 17, approximating the prevalence rate of substance use disorders among adolescents in the US (~11%; Merikangas et al., 2010). Thus, reflecting the heterotypic continuity of externalizing psychopathology, symptoms of marijuana use problems were included as an indicator of externalizing psychopathology from age 14 to 17, but not from age 10 to 13. The finding of partial longitudinal invariance, therefore, may be considered especially striking given the emergence of this novel source of variation in adolescent symptomatology. Nevertheless, results suggest that, before and after the emergence of marijuana use problems, the patterns of comorbidity among the symptoms of other psychiatric disorders persist. Therefore, whether marijuana use contributes to, exacerbates, or covaries with other psychiatric symptoms, the emergence of such problems in adolescence does not seem to have a large impact on transdiagnostic patterns of comorbidity, that is, at least among the symptoms of common mental disorders that were measured in the current study.
Similar to previous studies of the hierarchical structure of psychopathology, three latent factors were needed to account for patterns of comorbidity among symptoms of psychiatric disorders, including internalizing, externalizing, and ADHD-related factors. In addition, these factors were moderately-to-highly correlated, such that much of the common variance among these dimensions of psychopathology were explained by a general high-order factor. These results demonstrate that patterns of comorbidity for Mexican-origin youth in the U.S. do not differ profoundly from the patterns of comorbidity that have been observed in other racial/ethnic groups.
However, it should be noted that a bifactor model, which has been used in previous studies to model the hierarchical structure of psychopathology, yielded inadmissible estimates in cross-sectional models (i.e. Heywood cases). This finding may be interpreted in at least two ways. Note that the bifactor model is highly complex and estimates almost as many parameters as an exploratory factor analysis model. Consequently, combined with the statistical reservations that were previously discussed, one may conclude that the exploratory nature of the bifactor model capitalized on sampling variability and overfit the data, yielding results that are difficult to interpret. On the other hand, one might argue that the Heywood cases produced by the bifactor model, specifically negative residual variances, indicate that after the bifactor accounted for shared variance among symptoms of common mental disorders, distinct dimensions of covariations were less pronounced for Mexican-origin youth, compared to other racial/ethnic groups. However, drawing conclusions from models that yield estimates that, by definition, cannot correspond with reality should be considered dubious and warrants caution. Studies of the hierarchical structure of psychopathology should focus not only on model comparisons using fit statistics to determine the best-fitting hierarchical model, but also on the comparative interpretability of estimated parameters.
Developmental Trajectories of Psychopathology & Personality.
Results of the present study also shed light on divergent developmental trajectories of common mental disorders at varying levels of generality and specificity in a hierarchical structure of psychopathology. Internalizing psychopathology decreased from age 12 to 17, and ADHD and externalizing psychopathology increased slightly from age 12 to 14 before decreasing. Finally, a higher-order factor of psychopathology showed no mean change from age 12 to 13 before decreasing to age 17. After accounting for a higher-order factor, which captures the general tendency for dimensions of psychopathology to correlate, internalizing psychopathology decreased slightly from age 12 to 15 years, before beginning to stabilize from 15 to 17 years. On average, there was little change in ADHD-related psychopathology after accounting for the higher-order factor, but mean-levels decreased very slightly from age 12 to 17 years. Finally, residual externalizing psychopathology that was independent from the higher-order factor was predicted to increase slightly from age 12 to 17 years.
These results highlight the value of disentangling overlapping from unique sources of variation when modeling the development of psychopathology. Without accounting for the higher-order factor, the developmental trajectories of internalizing, externalizing, and ADHD-related psychopathology closely mirrored one another, as well as the developmental trajectory of the higher-order factor. This is due, in part, to the strong degree of overlap between factors of psychopathology, which can be gleaned from the high factor loadings on the general higher-order factor. After accounting for the general factor, the residual or unique components of subordinate factors exhibited only slight change but greater developmental divergence across adolescence.
The present study documented inter-individual differences in rates of change in psychopathology. However, compared to the amount of variation in initial-levels of psychopathology at age 12, average change in psychopathology was small in magnitude from age 12 to 17, regardless of the level of the hierarchy or dimension of psychopathology in question. This finding is consistent with the relatively high rank-order stability of the high-order factor observed in the present study. Taken together, these results imply that although psychopathology changes for some adolescents from age 12 to 17, on average, these changes are relatively small compared to the differences in psychopathology that exist between adolescents at age 12, such that the rank-order of individuals experiencing symptoms across diagnostic categories remains relatively stable. Similarly, the developmental trajectories of the Big Five personality traits were largely stable across adolescence, such that the Big Five exhibited very little mean-level change. However, similarly to psychopathology, there was variation in initial-levels and rates of change for the Big Five. This indicates that youth not only exhibit differences in the Big Five at 12 years of age but also differences in rates of change during adolescence.
Developmental Co-occurrence of Psychopathology & Personality.
The general patterns of associations between initial-levels of Big Five traits and initial-levels of psychopathology at age 12 were largely consistent with previous studies (Malouff et al., 2005). For example, previous studies have found that neuroticism is a robust correlate of psychopathology, including internalizing and externalizing in childhood (Malouff et al., 2005), while openness/intellect is unrelated to psychopathology, other than disorders involving mania (Barnett et al., 2011; Tackett, Quilty, Sellbom, Rector, & Bagby, 2008). In the present study, openness/intellect was not significantly associated with initial-levels or rates of change in psychopathology, but initial-levels of neuroticism at age 12 were positively associated with initial-levels of internalizing, externalizing, ADHD, and the higher-order factor of psychopathology. The negative correlations between conscientiousness and agreeableness with initial-levels of psychopathology were also consistent with the results of previous studies (Malouff et al., 2005). After accounting for the higher-order factor, initial-levels of conscientiousness were negatively correlated with ADHD, while initial-levels of agreeableness were negatively correlated with externalizing. Controlling for the higher-order factor, neuroticism was positively correlated with internalizing and externalizing factors, while extraversion was positively and negatively correlated with externalizing and internalizing, respectively.
Neuroticism was the strongest correlate of all dimensions of psychopathology, except for the residual ADHD factor when controlling for the higher-order factor. Moreover, rates of change in neuroticism were correlated with rates of change in ADHD, externalizing, and the general higher-order factor. These findings support and extend previous work that has conceptualized neuroticism as a prominent risk factors for psychopathology (Brandes et al., 2019; Tackett et al., 2012). Thus, not only is neuroticism a relatively stable risk factor for psychopathology, partly undergirded by genetic factors (Tackett et al., 2012), but it is also a developmental risk factor, as changes in neuroticism dovetailed with changes in psychopathology from late childhood through adolescence.
Even though the present study recruited non-WEIRD participants, specifically a sample of Mexican-origin youth from predominately low-income families, results of the current study provide evidence that many of the associations that exist between normal-range personality traits and dimensions of psychopathology are largely consistent with other populations. However, one exception is the relation between extraversion and psychopathology. In the current study, the correlation between initial-levels of extraversion and initial-levels of externalizing was positive and approached a conservative threshold for statistical significance, and changes in extraversion were associated with rates of change in externalizing. Whereas in a previous meta-analysis, the concurrent association between extraversion and childhood externalizing was positive, but not significantly different than zero (Malouff et al., 2005). Future studies should test whether these associations replicate and, if so, test potential mediators that may explain this cultural difference in relations between personality and psychopathology.
Changes in extraversion were associated with changes in externalizing and the higher-order factor of psychopathology. In addition, changes in neuroticism were associated with changes in the higher-order factor of psychopathology, such that adolescents who decreased more rapidly in neuroticism from age 12 to 17 tended to decrease more rapidly in the general higher-order factor. Put differently, adolescents who showed greater decreases in neuroticism tended to show steeper arch-shaped trajectories of higher-order psychopathology. However, for neuroticism, the extension of this protective association to more specific first-order factors of psychopathology should be interpretted with caution, as neither linear nor quadratic slopes met a conservative threshold for statistical significance. Consequently, results of the present study suggest that levels of neuroticism in late childhood and change in neuroticism from late childhood through adolescence may be considered markers of general psychopathology.
Compared to a previous study of the developmental dynamics of personality and psychopathology in adults (Wright, Hopwood, & Zanarini, 2015), the strength of associations between personality and psychopathology documented in the present study are comparatively small. There are many possible explanations for these differences in effect size, including differences in the measurement of personality and psychopathology (e.g. common mental disorders vs. borderline personality pathology; c.f. Wright, Hopwood, & Zanarini, 2015), as well as cultural and socioeconomic differences. There is also evidence that the magnitude of individual differences in personality increases across development, such that children become less alike as they progress through adolescences (Mõttus et al., 2019; Mõttus, Soto, & Slobodskaya, 2017). All else being equal, as the homogeneity of a variable increases, the magnitude of its correlation with another variable decreases (Bates, Zhang, Dufek, & Chen, 1996). This is why it is important for researchers to avoid range restriction to ensure sufficient heterogeneity when estimating correlations (Bland & Altman, 2011). Consequently, it seems likely that these differences in effect size are do, at least partly, to differences in variance that exist for personality at different times across the lifespan.
Effects of Biological Sex
Consistent with previous studies, females exhibited higher initial-levels of internalizing psychopathology compared to males, as well as higher initial levels of agreeableness and conscientiousness. However, in the present study, females also had higher levels of externalizing psychopathology, which stands in contrast to studies that have reported higher levels of externalizing disorders in males (Newman et al., 1996). An examination of sex differences in observed symptom-counts (see Table S5 in the supplemental materials) suggests that, in the current study, the latent sex difference in levels of externalizing were likely undergirded by the emotion-dysregulation and defiance-related facets of oppositional defiance disorder. Compared to males, females had higher levels of defiance-related symptoms at age 13 and 14 and marginally higher defiance-related symptoms at age 12, 15, and 17. Females also had higher levels of emotion-dysregulation from ages 13 to 17, and marginally higher levels at age 11.
Although these sex differences may come as a surprise, a recent meta-analysis of sex differences in emotion expression found that boys expressed more externalizing emotions than girls in early and middle childhood, but girls expressed more externalizing emotions than boys in adolescence (Chaplin & Aldao, 2013). A meta-analysis of ODD in middle childhood (age 6 to 13) also found that the prevalence of ODD symptoms was higher in males than females, but only in Western cultures (Demmer et al., 2017). In contrast to participants in the current study, samples from Western cultures usually do not include Mexican-origin youth. Thus, these meta-analyses may suggest that the age and ethnic origin of participants played a role in what, at first glance, may seem to be a peculiar finding. Note, however, that the sources of sex differences in initial-levels do not necessarily explain sex differences in within-individual changes. Therefore, future cross-cultural studies of developmental psychopathology stand to benefit from replicating and probing these findings further. Importantly, the links between personality traits and psychopathology that were observed in the present study remained largely unchanged after controlling for biological sex.
Nonetheless, after accounting for variation associated with biological sex, the slope-slope correlations between neuroticism and the higher-order factor met only a traditional threshold for statistical significance (i.e. p < .05). However, in the present study, the estimated effect sizes of developmental links between the Big Five domains and dimensions of psychopathology were similar across different statistical approaches (i.e., CUFFs & FOCUS models and sensitivity analyses reported in supplemental materials) and after controlling for the effects of biological sex on initial-levels and within-individual changes. Such dynamic links between variation in common personality traits and symptoms of psychiatric disorders is consistent with dimensional perspectives of psychopathology, which view psychiatric symptoms as dysfunction or problematic manifestations of otherwise healthy cognitions, emotions, and behaviors (Krueger & Tackett, 2003; Miller, Lynam, Widiger, & Leukefeld, 2001).
Limitations and Future Directions.
Relying on a brief measure of Big Five personality traits is one limitation of the present study. Although we found that extraversion and neuroticism were developmental correlates of a higher-order factor of psychopathology, the present study does not shed light on whether changes in more specific facets of personality dovetail with changes in individual psychiatric disorders or a broad tendency to experience symptoms across multiple disorders. Although the present study analyzed developmental change from the end of childhood through late adolescence, which is a critical period of development for hormonal, neurobiological, and social change, future research should examine whether changes in extraversion and neuroticism are developmental correlates of psychopathology earlier and later in life. It also remains unknown whether the dynamic links between personality and higher-order psychopathology will extend to clinical samples, where psychiatric symptoms are more frequent and have a greater impact on life functioning.
The current study also focused on the measurement of common mental disorders, previously classified as Axis-I disorders, to the exclusion of personality disorders. It stands to reason that the developmental co-occurrence between normal-range personality and dimensions of psychopathology would be larger if those dimensions included individual differences in personality pathology. The current study also does not address occasion-to-occasion associations across domains of healthy and pathological functioning. With the assessment of comparable constructs, future studies stand to benefit from examining both associations between growth parameters, as well as the direct links across constructs over time. This may be achieved by estimating bivariate trait-state-error models or using other comparable analytic techniques.
Despite these limitations, the present study contributes to research on the hierarchical taxonomy of psychopathology as well as the developmental dynamics of personality and psychopathology. Results indicate that a structure of common mental disorders within the hierarchical taxonomy of psychopathology extends to Mexican-origin youth and is largely invariant from late childhood through adolescence. Further, initial levels of conscientiousness and agreeableness were positively associated with lower initial-levels of ADHD, externalizing, and a higher-order factor of psychopathology. Higher initial-levels of agreeableness were also associated with lower initial-levels of internalizing psychopathology. Higher initial-levels of neuroticism were associated with higher initial-levels of internalizing, ADHD, externalizing, and a higher-order factor of psychopathology. Changes in extraversion and neuroticism were associated with changes in a higher-order factor of psychopathology. Extraversion was also a developmental correlate of externalizing psychopathology, and neuroticism was a developmental correlate of externalizing and ADHD psychopathology.
Supplementary Material
Acknowledgments
F.D.M. was supported by a grant from the John Templeton Foundation, through the Genetics and Human Agency project. R.F.K was partially supported by the National Institutes of Health (R01AG053217, U19AG051426, and R21AA025689). The California Families Project was supported by a grant from the National Institute on Drug Abuse and the National Institute on Alcohol Abuse and Alcoholism (DA017902) awarded to R.W.R. and R.D.C.
Footnotes
RMSEA favored a bifactor model at ages 11 and 13 years , and a three-factor solution at 16 years. CFI favored a three-factor solution at ages 11 and 13 years but favored a bi-factor solution at 16 years.
When comparing the fit of growth models, change in model degrees of freedom (Δdf) were small, relative to Δdf when comparing measurement invariance models. Therefore, we did not rely on ΔRMSEA, ΔCFI, and RDR to compare growth models, as these fit statistics are recommended specifically for comparing measurement invariance models.
For openness/intellect, extraversion, and neuroticism, the linear slopes of personality traits were allowed to covary with the linear and quadratic curves of factors of psychopathology. For agreeableness, the latent-basis slope was allowed to covary with linear and quadratic curves of factors, and the linear and quadratic slopes of conscientiousness were allowed to covary with the linear and quadratic curves of factors, respectively.
References
- Atherton OE, Lawson KM, Ferrer E, & Robins RW (in press). The role of effortful control in the development of ADHD, ODD, and CD symptoms. Journal of Personality and Social Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett JH, Huang J, Perlis RH, Young MM, Rosenbaum JF, Nierenberg AA, … Smoller JW (2011). Personality and bipolar disorder: Dissecting state and trait associations between mood and personality. Psychological Medicine, 41, 1593–1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates BT, Zhang, Dufek JS, & Chen FC (1996). The effects of sample size and variability on the correlation coefficient. Medicine and Science in Sports and Exercise, 28(3), 386–391. [DOI] [PubMed] [Google Scholar]
- Beauducel A, & Wittmann WW (2005). Simulation study on fit indexes in CFA based on data with slightly distorted simple structure. Structural Equation Modeling, 12(1), 41–75. [Google Scholar]
- Benjamin DJ, Berger JO, Johannesson M, Nosek BA, Wagenmakers EJ, Berk R, …& Cesarini D. (2018). Redefine Statistical Significance. Nature Human Behaviour, 2(1), 6–10. [DOI] [PubMed] [Google Scholar]
- Bland JM, & Altman DG (2011). Correlation in restricted ranges of data. The British Medical Journal (BMJ) 342, d556. [DOI] [PubMed] [Google Scholar]
- Bongers IL, Koot HM, Van Der Ende J, & Verhulst FC (2004). Developmental trajectories of externalizing behaviors in childhood and adolescence. Child Development, 75(5), 1523–1537. [DOI] [PubMed] [Google Scholar]
- Brandes CM, Herzhoff K, Smack AJ, & Tackett JL (2019). The p factor and the n factor: Associations between the general factors of psychopathology and neuroticism in children. Clinical Psychological Science, 7(6), 1266–1284. [Google Scholar]
- Bravo M, Woodbury-Farina M, Canino GJ, & Rubio-Stipec M. (1993). The Spanish translation and cultural adaptation of the Diagnostic Interview Schedule for Children (DISC) in Puerto Rico. Culture, Medicine, & Psychiatry, 17(3), 329–344. [DOI] [PubMed] [Google Scholar]
- Browne MW, & Du Toit SH (1992). Automated fitting of nonstandard models. Multivariate Behavioral Research, 27(2), 269–300. [DOI] [PubMed] [Google Scholar]
- Byrne BM, Shavelson RJ, & Muthén B. (1989). Testing for the equivalence of factor covariance and mean structures: the issue of partial measurement invariance. Psychological Bulletin, 105(3), 456–466. [Google Scholar]
- Carroll JB (2003). The higher-stratum structure of cognitive abilities: Current evidence supports g and about ten broad factors. The scientific study of general intelligence (pp. 5–21). [Google Scholar]
- Carragher N, Krueger RF, Eaton NR, & Slade T. (2015). Disorders without borders: current and future directions in the meta-structure of mental disorders. Social Psychiatry and Psychiatric Epidemiology, 50(3), 339–350. [DOI] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, … & Moffitt TE (2014). The p factor: one general psychopathology factor in the structure of psychiatric disorders?. Clinical Psychological Science, 2(2), 119–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos-Ryan N, Brière FN, O’Leary-Barrett M, Banaschewski T, Bokde A, Bromberg U, … The IMAGEN Consortium. (2016). The structure of psychopathology in adolescence and its common personality and cognitive correlates. Journal of Abnormal Psychology, 125(8), 1039–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaplin TM, & Aldao A. (2013). Gender differences in emotion expression in children: A meta-analytic review. Psychological Bulletin, 139(4), 735–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang L, Connelly BS, & Geeza AA (2012). Separating method factors and higher order traits of the Big Five: A meta-analytic multitrait–multimethod approach. Journal of Personality and Social Psychology, 102(2), 408–426. [DOI] [PubMed] [Google Scholar]
- Chen FF (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 464–504. [Google Scholar]
- Cheung GW, & Rensvold RB (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural equation modeling, 9(2), 233–255. [Google Scholar]
- Cicchetti D, & Rogosch FA (2002). A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology, 70, 6–20. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Edelbrock CS, & Costello AJ (1985). Validity of the NIMH diagnostic interview schedule for children: A comparison between psychiatric and pediatric referrals. Journal of Abnormal Child Psychology, 13, 579–595. DOI: 10.1007/BF00923143 [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, & Angold A. (2003). Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry, 60(8), 837–844 [DOI] [PubMed] [Google Scholar]
- De Bolle M, Beyers W, De Clercq B, & De Fruyt F. (2012). General personality and psychopathology in referred and nonreferred children and adolescents: An investigation of continuity, pathoplasty, and complication models. Journal of Abnormal Psychology, 121(4), 958–970. [DOI] [PubMed] [Google Scholar]
- Decuyper M, De Pauw S, De Fruyt F, De Bolle M, & De Clercq BJ (2009). A meta‐analysis of psychopathy‐, antisocial PD‐and FFM associations. European Journal of Personality, 23(7), 531–565. [Google Scholar]
- Del Giudice M, Booth T, & Irwing P. (2012). The distance between Mars and Venus: Measuring global sex differences in personality. PloS one, 7(1), e29265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demmer DH, Hooley M, Sheen J, McGillivray JA, & Lum JA (2017). Sex differences in the prevalence of oppositional defiant disorder during middle childhood: a meta-analysis. Journal of Abnormal Child Psychology, 45(2), 313–325. [DOI] [PubMed] [Google Scholar]
- De Pauw SS, & Mervielde I. (2011). The role of temperament and personality in problem behaviors of children with ADHD. Journal of Abnormal Child Psychology, 39(2), 277–291. [DOI] [PubMed] [Google Scholar]
- DeYoung CG (2015). Openness/Intellect: A dimension of personality reflecting cognitive exploration In Cooper ML & Larsen RJ (Eds.), The APA handbook of personality and social psychology: Personality processes and individual differences (Vol. 4, pp. 369–399). Washington, DC: American Psychological Association. [Google Scholar]
- DeYoung CG, & Krueger RF (2018). A cybernetic theory of psychopathology. Psychological Inquiry. [Google Scholar]
- Ehrhart MG, Ehrhart KH, Roesch SC, Chung-Herrera BG, Nadler K, & Bradshaw K. (2009). Testing the latent factor structure and construct validity of the Ten-Item Personality Inventory. Personality and Individual Differences, 47(8), 900–905. [Google Scholar]
- Falconer DS (1965). The inheritance of liability to certain diseases, estimated from the incidence among relatives. Annals of Human Genetics, 29(1), 51–76. [Google Scholar]
- Flora DB, & Curran PJ (2004). An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychological Methods, 9(4), 466–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene AL, Eaton NR, Li K, Forbes MK, Krueger RF, Markon KE, … & Fried EI. (In Press). Are fit indices used to test psychopathology structure biased? A simulation study. Journal of abnormal psychology. [DOI] [PubMed] [Google Scholar]
- Griffith JW, Zinbarg RE, Craske MG, Mineka S, Rose RD, Waters AM, & Sutton JM (2010). Neuroticism as a common dimension in the internalizing disorders. Psychological Medicine, 40(7), 1125–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosling SD, Rentfrow PJ, & Swann WB Jr (2003). A very brief measure of the Big-Five personality domains. Journal of Research in Personality, 37(6), 504–528. [Google Scholar]
- Hall GCN, Bansal A, & Lopez IR (1999). Ethnicity and psychopathology: A meta-analytic review of 31 years of comparative MMPI/MMPI-2 research. Psychological Assessment, 11(2), 186–197. [Google Scholar]
- Harden KP, Engelhardt LE, Mann FD, Patterson MW, Grotzinger AD, Savicki SL, … & Tucker-Drob EM (2019). Genetic Associations Between Executive Functions and a General Factor of Psychopathology. Journal of the American Academy of Child & Adolescent Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harden KP, & Tucker-Drob EM (2011). Individual differences in the development of sensation seeking and impulsivity during adolescence: Further evidence for a dual systems model. Developmental Psychology, 47(3), 739–746. [DOI] [PubMed] [Google Scholar]
- Henrich J, Heine SJ, & Norenzayan A. (2010). Most people are not WEIRD. Nature, 466 (7302), 29. [DOI] [PubMed] [Google Scholar]
- Hildebrandt A, Wilhelm O, & Robitzsch A. (2009). Complementary and competing factor analytic approaches for the investigation of measurement invariance. Review of Psychology, 16(2), 87–102. [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal, 6(1), 1–55. [Google Scholar]
- Ioannidis JP (2018). The proposal to lower p value thresholds to. 005. The Journal of the American Medical Association, 319(14), 1429–1430. [DOI] [PubMed] [Google Scholar]
- John OP, Naumann LP, & Soto CJ (2008). Paradigm shift to the integrative big five trait taxonomy. Handbook of Personality: Theory and Research, 3, 114–158. [Google Scholar]
- Jones D. (2010). A WEIRD view of human nature skews psychologists’ studies. Science, 326, (5986), 1627. [DOI] [PubMed] [Google Scholar]
- Jeronimus BF, Kotov R, Riese H, & Ormel J. (2016). Neuroticism’s prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: a meta-analysis on 59 longitudinal/prospective studies with 443313 participants. Psychological Medicine, 46(14), 2883–2906. [DOI] [PubMed] [Google Scholar]
- Kagan J. (1980). Perspectives on continuity In Brim OG. & Kagan J (Eds.), Constancy and change in human development (pp. 26–74). Cambridge, MA, US: Harvard University Press [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, … & Kendler KS (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General psychiatry, 51(1), 8–19. [DOI] [PubMed] [Google Scholar]
- Kim H, & Eaton NR (2015). The hierarchical structure of common mental disorders: Connecting multiple levels of comorbidity, bifactor models, and predictive validity. Journal of Abnormal Psychology, 124(4), 1064–1078. [DOI] [PubMed] [Google Scholar]
- Kline P. (1986). A handbook of test construction: Introduction to psychometric design. New York: Methuen. [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, … & Eaton NR (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. [DOI] [PubMed] [Google Scholar]
- Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, & Zimmerman M. (2011). New dimensions in the quantitative classification of mental illness. Archives of General Psychiatry, 68(10), 1003–1011. [DOI] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, & Watson D. (2010). Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychological Bulletin, 136(5), 768–821. [DOI] [PubMed] [Google Scholar]
- Krueger RF (1999). The structure of common mental disorders. Archives of General Psychiatry, 56(10), 921–926. [DOI] [PubMed] [Google Scholar]
- Krueger RF, & Tackett JL (2003). Personality and psychopathology: Working toward the bigger picture. Journal of Personality Disorders, 17(2: Special issue), 109–128. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, & Zald DH (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin, 143(2), 142–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Keenan K, Stepp SD, Loeber R, & Hipwell AE (2015). Criterion validity of the general factor of psychopathology in a prospective study of girls. Journal of Child Psychology and Psychiatry, 56(4), 415–422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Van Hulle C, Urbano RC, Krueger RF, Applegate B, … & Waldman ID (2008). Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. Journal of Abnormal Child Psychology, 36(2), 187–206. [DOI] [PubMed] [Google Scholar]
- Malouff JM, Thorsteinsson EB, & Schutte NS (2005). The relationship between the five-factor model of personality and symptoms of clinical disorders: A meta-analysis. Journal of Psychopathology and Behavioral Assessment, 27(2), 101–114. [Google Scholar]
- Mann FD, Paul SL, Tackett JL, Tucker-Drob EM, & Harden KP (2018). Personality risk for antisocial behavior: Testing the intersections between callous–unemotional traits, sensation seeking, and impulse control in adolescence. Development and Psychopathology, 30(1), 267–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markon KE (2010). Modeling psychopathology structure: A symptom-level analysis of Axis I and II disorders. Psychological medicine, 40(2), 273–288. [DOI] [PubMed] [Google Scholar]
- Markon KE (2019). Bifactor and hierarchical models: Specification, inference, and interpretation. Annual review of clinical psychology, 15, 51–69. [DOI] [PubMed] [Google Scholar]
- Markus KA (2019) Re: Configural Invariance - bad model fit. Email Correspondence from SEMNET on Dec 13, 2019, 9:35 AM. [Google Scholar]
- McArdle JJ (1988). Dynamic but structural equation modeling of repeated measures data In Handbook of multivariate experimental psychology (pp. 561–614). Springer, Boston, MA. [Google Scholar]
- McLean CP, Asnaani A, Litz BT, & Hofmann SG (2011). Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research, 45(8), 1027–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, … & Swendsen J. (2010). Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller CJ, Miller SR, Newcorn JH, & Halperin JM (2008). Personality characteristics associated with persistent ADHD in late adolescence. Journal of Abnormal Child Psychology, 36(2), 165–173. [DOI] [PubMed] [Google Scholar]
- Miller JD, Lyman DR, Widiger TA, & Leukefeld C. (2001). Personality disorders as extreme variants of common personality dimensions: Can the five factor model adequately represent psychopathy? Journal of Personality, 69(2), 253–276. [DOI] [PubMed] [Google Scholar]
- Morgan GB, Hodge KJ, Wells KE, & Watkins MW (2015). Are fit indices biased in favor of bi-factor models in cognitive ability research?: A comparison of fit in correlated factors, higher-order, and bi-factor models via Monte Carlo simulations. Journal of Intelligence, 3(1), 2–20. [Google Scholar]
- Mõttus R, Briley DA, Zheng A, Mann FD, Engelhardt LE, Tackett JL, Harden KP, & Tucker-Drob EM (2019). Kids becoming less alike: A behavioral genetic analysis of developmental increases in personality variance from childhood to adolescence. Journal of Personality and Social Psychology, 117(3), 635–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mõttus R, Soto CJ, & Slobodskaya HR (2017). Are all kids alike? The magnitude of individual differences in personality characteristics tends to increase from early childhood to early adolescence. European Journal of Personality, 31(4), 313–328. [Google Scholar]
- Muck PM, Hell B, & Gosling SD (2007). Construct validation of a short five-factor model instrument. European Journal of Psychological Assessment, 23(3), 166–175. [Google Scholar]
- Murray AL, Eisner M, & Ribeaud D. (2016). The development of the general factor of psychopathology ‘p factor’ through childhood and adolescence. Journal of Abnormal Child Psychology, 44(8), 1573–1586. [DOI] [PubMed] [Google Scholar]
- Murray AL, & Johnson W. (2013). The limitations of model fit in comparing the bi-factor versus higher-order models of human cognitive ability structure. Intelligence, 41(5), 407–422. [Google Scholar]
- Muthén LK, & Muthén B (1998–2017). Mplus. The comprehensive modelling program for applied researchers: User’s guide, 5. [Google Scholar]
- Newman DL, Moffitt TE, Caspi A, Magdol L, Silva PA, & Stanton WR (1996). Psychiatric disorder in a birth cohort of young adults: prevalence, comorbidity, clinical significance, and new case incidence from ages 11 to 21. Journal of consulting and clinical psychology, 64(3), 552–562. [PubMed] [Google Scholar]
- Nigg J, Blaskey L, Huang-Pollock C, & John O. (2002). ADHD symptoms and personality traits: Is ADHD an extreme personality trait?. The ADHD Report, 10(5), 6–11. [Google Scholar]
- Olino TM, Dougherty LR, Bufferd SJ, Carlson GA, & Klein DN (2014). Testing models of psychopathology in preschool-aged children using a structured interview-based assessment. Journal of abnormal child psychology, 42(7), 1201–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paus T, Keshavan M, & Giedd JN (2008). Why do many psychiatric disorders emerge during adolescence?. Nature Reviews Neuroscience, 9(12), 947–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn PD, & Harden KP (2013). Differential changes in impulsivity and sensation seeking and the escalation of substance use from adolescence to early adulthood. Development and Psychopathology, 25(1), 223–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renau V, Oberst U, Gosling S, Rusiñol J, & Chamarro A. (2013). Translation and validation of the ten-item-personality inventory into Spanish and Catalan. Aloma: Revista de Psicologia, Ciències de l’Educació i de l’Esport, 31(2). [Google Scholar]
- Rigdon EE (1996). CFI versus RMSEA: A comparison of two fit indexes for structural equation modeling. Structural Equation Modeling: A Multidisciplinary Journal, 3(4), 369–379. [Google Scholar]
- Rijsdijk FV, & Sham PC (2002). Analytic approaches to twin data using structural equation models. Briefings in Bioinformatics, 3(2), 119–133. [DOI] [PubMed] [Google Scholar]
- Romero E, Villar P, Gómez-Fraguela JA, & López-Romero L. (2012). Measuring personality traits with ultra-short scales: A study of the Ten Item Personality Inventory (TIPI) in a Spanish sample. Personality and Individual Differences, 53(3), 289–293. [Google Scholar]
- Røysamb E, Kendler KS, Tambs K, Ørstavik RE, Neale MC, Aggen SH, Torgersen S, & Reichborn-Kjennerud T. (2011). The joint structure of DSM-IV Axis I and Axis II disorders. Journal of Abnormal Psychology, 120(1), 198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz MA, Pincus AL, & Schinka JA (2008). Externalizing pathology and the five-factor model: A meta-analysis of personality traits associated with antisocial personality disorder, substance use disorder, and their co-occurrence. Journal of personality disorders, 22(4), 365–388. [DOI] [PubMed] [Google Scholar]
- Samuel DB, & Widiger TA (2008). A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: A facet level analysis. Clinical Psychology Review, 28(8), 1326–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salk RH, Hyde JS, & Abramson LY (2017). Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological Bulletin, 143(8), 783–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saulsman LM, & Page AC (2004). The five-factor model and personality disorder empirical literature: A meta-analytic review. Clinical psychology review, 23(8), 1055–1085. [DOI] [PubMed] [Google Scholar]
- Schmitt DP, Realo A, Voracek M, & Allik J. (2008). Why can’t a man be more like a woman? Sex differences in Big Five personality traits across 55 cultures. Journal of Personality and Social Psychology, 94(1), 168. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone M, Shaffer D, Dulcan M, Jensen P, Fisher P, Bird H, Goodman S, Lahey B, Lichtman J, Canino G, Rubio-Stipec, & Rae D. (1996). Criterion validity of the NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC 2.3). Journal of the American Academy of Child & Adolescent Psychiatry 35, 878–888. [DOI] [PubMed] [Google Scholar]
- Samejima F. (2016). Graded response models In: Jvd Linden W. In Handbook of Item Response Theory (pp. 123–136). CRC Press; Boca Raton, FL. [Google Scholar]
- Shaffer D, Fisher P, Lucas C, Dulcan M, & Schwab-Stone M. (2000). NIMH Diagnostic Interview Schedule for Children version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry 39, 28–38. [DOI] [PubMed] [Google Scholar]
- Shields AN, Reardon KW, Brandes CM, & Tackett JL (2019). The p factor in children: Relationships with executive functions and effortful control. Journal of Research in Personality, 82, 103853. [Google Scholar]
- Shiner RL, Masten AS, & Tellegen A. (2002). A developmental perspective on personality in emerging adulthood: Childhood antecedents and concurrent adaptation. Journal of Personality and Social Psychology, 83(5), 1165–1177. [PubMed] [Google Scholar]
- Sisk CL, & Foster DL (2004). The neural basis of puberty and adolescence. Nature neuroscience, 7(10), 1040–1047. [DOI] [PubMed] [Google Scholar]
- Sisk CL, & Zehr JL (2005). Pubertal hormones organize the adolescent brain and behavior. Frontiers in neuroendocrinology, 26(3–4), 163–174. [DOI] [PubMed] [Google Scholar]
- Soto CJ, & Tackett JL (2015). Personality traits in childhood and adolescence: Structure, development, and outcomes. Current Directions in Psychological Science, 24(5), 358–362. [Google Scholar]
- Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, & Silove D. (2014). The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. International Journal of Epidemiology, 43(2), 476–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterba S, Egger HL, & Angold A. (2007). Diagnostic specificity and nonspecificity in the dimensions of preschool psychopathology. Journal of Child Psychology and Psychiatry, 48(10), 1005–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevanovic D, Jafari P, Knez R, Franic T, Atilola O, Davidovic N, … & Lakic A. (2017). Can we really use available scales for child and adolescent psychopathology across cultures? A systematic review of cross-cultural measurement invariance data. Transcultural Psychiatry, 54(1), 125–152. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Lahey BB, van Hulle C, Waldman I, Krueger RF, & Rathouz PJ (2013). Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. Journal of Abnormal Psychology, 122(4), 1142–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tackett JL, Slobodskaya HR, Mar RA, Deal J, Halverson CF Jr, Baker SR, … & Besevegis E. (2012). The hierarchical structure of childhood personality in five countries: Continuity from early childhood to early adolescence. Journal of Personality, 80(4), 847–879. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Quilty LC, Sellbom M, Rector N, & Bagby RM (2008). Additional evidence for a quantitative hierarchical model of mood and anxiety disorders for DSM–5: The context of personality structure. Journal of Abnormal Psychology, 117, 812–825. doi: 10.1037/a0013795 [DOI] [PubMed] [Google Scholar]
- Torres SA, Santiago CD, Walts KK, & Richards MH (2018). Immigration policy, practices, and procedures: The impact on the mental health of Mexican and Central American youth and families. American Psychologist, 73(7), 843–854. [DOI] [PubMed] [Google Scholar]
- Trosper SE, Whitton SW, Brown TA, & Pincus DB (2012). Understanding the latent structure of the emotional disorders in children and adolescents. Journal of abnormal child psychology, 40(4), 621–632. [DOI] [PubMed] [Google Scholar]
- van den Akker AL, Dekovic M, & Prinzie P. (2010). Transitioning to adolescence: How changes in child personality and overreactive parenting predict adolescent adjustment problems. Development and Psychopathology, 22, 151–163 [DOI] [PubMed] [Google Scholar]
- Van der Linden D, te Nijenhuis J, & Bakker AB (2010). The general factor of personality: A meta-analysis of Big Five intercorrelations and a criterion-related validity study. Journal of Research in Personality, 44(3), 315–327. [Google Scholar]
- Vesga-López O, Schneier F, Wang S, Heimberg R, Liu SM, Hasin DS, & Blanco C. (2008). Gender differences in generalized anxiety disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). The Journal of Clinical Psychiatry, 69(10), 1606–1616. [PMC free article] [PubMed] [Google Scholar]
- Wasserman GA, McReynolds LS, Ko SJ, Katz LM, & Carpenter JR (2005). Gender differences in psychiatric disorders at juvenile probation intake. American Journal of Public Health, 95(1), 131–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Ellickson-Larew S, Stanton K, Levin-Aspenson HF, Khoo S, Stasik-O’Brien SM, & Clark LA (2019). Aspects of extraversion and their associations with psychopathology. Journal of Abnormal Psychology, 128(8), 777–794. [DOI] [PubMed] [Google Scholar]
- Watts AL, Porre HE, & Waldman ID (In Press) Riskier Tests of the Validity of the Bifactor Model of Psychopathology. Clinical Psychological Science. [Google Scholar]
- Widiger TA, Sellbom M, Chmielewski M, Clark LA, DeYoung CG, Kotov R, … & Samuel DB (2019). Personality in a hierarchical model of psychopathology. Clinical Psychological Science, 7(1), 77–92. [Google Scholar]
- Wright AGC, Hopwood CJ, & Zanarini MC (2015). Associations between changes in normal personality traits and borderline personality disorder symptoms over 16 years. Personality Disorders: Theory, Research, and Treatment, 6(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AG, & Simms LJ (2015). A metastructural model of mental disorders and pathological personality traits. Psychological Medicine, 45(11), 2309–2319. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.