Abstract
To assess efficacy and safety of Thulium laser enucleation of prostate (ThuLEP) for benign prostatic hyperplasia. It is a systemic review based on a comprehensive search of PubMed, Cochrane, and Google scholar databases from inception to 31 March 2020. All studies in English evaluating ThuLEP as well as those comparing it with Transurethral resection of prostate (TURP) and Holmium Laser enucleation of prostate (HoLEP) were enrolled. The primary outcome was to evaluate operative, postoperative, and functional outcomes (IPSS, QoL, Qmax, PVR) in patients undergoing ThuLEP. Secondary outcome was to compare operative, postoperative, and functional outcomes with TURP and HoLEP in comparative studies. Fourteen studies with a total of 2,562 patients were included in this review. 2,034 underwent ThuLEP, 349 underwent TURP, and remaining 139 had HoLEP. We found that ThuLEP is safe as well as efficacious in all age groups as well as across all prostate sizes and with all four functional outcomes (IPSS, QoL, Qmax, PVR) revealing marked improvement at 3, 6, 12, and 24 months. Compared to TURP and HoLEP, Thulep is non-inferior in terms of operative and functional outcomes and, in fact, is associated with lesser catheterization duration as well as shorter hospital stay. Further, Thulium fiber laser (TFL) has advantages of being light weight, having high frequency, less fiber degradation, and less energy consumption, making it cost effective for operational and maintenance purpose. ThuLEP is a safe, efficacious, and cost-effective procedure for BPE.
Keywords: Enucleation, holmium, LASER, prostate, thulium, transurethral resection
Introduction
Benign prostatic enlargement (BPE) often leads to urinary obstruction often referred to as Benign Prostatic Obstruction (BPO). The symptom complex developing as a result of this enlargement is termed as Lower Urinary Tract Symptoms (LUTS). LUTS is the most common urological problem among men, affecting about a third of men over age 50.[1,2] In addition to LUTS, these patients can have other symptoms as well, including retention of urine (acute and chronic), visible or non-visible hematuria, infections in urinary tract, stone formation in bladder, bladder wall weakness and damage, kidney dysfunction, and issues with continence.[3] For standardization of symptoms, International Prostate Symptom Score (IPSS) index is commonly used.[4] There is no ideal treatment, each patient’s treatment is determined by factors, such as IPSS, BPE complications, and most importantly patient preferences. Research has revealed that majority of BPE patients receive pharmacological management in the form alpha blockers, 5-Alpha reductase inhibitors (5-ARIs), and other medications.[5] However, there is good population of men who end up having surgical interventions. Transurethral resection has been the reference “gold standard,” but due to its complications and issues with larger volume prostates, many alternatives have been developed and assessed.[6] In order to overcome these issues, many alternative procedures have been evolved, which have been able to reduce complications, shorten hospital stay, and accelerate patient recovery without compromising efficacy. The new methods are broadly divided into three types according to their treatment principles: resection methods (resection of prostate tissue piece by piece), vaporization methods (vaporization of excessive prostate tissue), and enucleation methods (peeling the enlarged prostate from the prostate capsule).[7] Among these new treatments, enucleation methods have shown better Qmax and IPSS values than vaporization and resection methods.[7]
Lasers have been used in BPE treatment from last 15 years, recent advances in technology, more clinical experience, and more advanced devices have challenged the supremacy of TURP.[8] Among lasers, HoLEP has equivalent outcomes to TURP and open prostatectomy with reduced complications. With refinements in technique and better learning, HoLEP is often considered as a true gold standard for surgical management of BPH.[6] The Ho:YAG laser is a non-continuous pulsed laser with pulse duration of 350 ms. Energy is produced at a wavelength of 2,140 nm with prostatic tissue penetration of about 0.4 mm. In 2005, the high-power Thulium laser was introduced in treatment of prostatic hyperplasia.[9]
This literature review will focus on critical analysis of Thulium Laser Enucleation of prostate (Thulep) for BPE. Firstly, this study looked into outcomes of ThuLEP procedure, including demographic characteristics, pre-operative, operative and post-operative variables, evaluating functional outcomes along with long term safety and durability. Secondly, this study compared outcomes of ThuLEP with HoLEP (Holmium Laser Enucleation of Prostate) and TURP in comparative studies to decrease bias. Further, it is important to mention that in our study, only ThuLEP procedures were taken into consideration unlike some other reviews, which have combined the usage of ThuLEP and Thulium Laser Vapoenucleation of prostate (ThuVEP).[10] To the best of our knowledge, as such, this is the first review that discusses ThuLEP exclusively.
Methodology
Search strategy and selection criteria
PubMed, Cochrane, and Google scholar databases from inception to 31 March 2020. We searched with terms “BPH,” “prostatic hyperplasia,” “benign prostatic hyperplasia,” “prostate enucleation,” “Thulium laser,” “Holmium laser,” “transurethral resection of prostate”.
143 articles matched initial search. After removing duplicates, 28 were excluded (language other than English, abstract-only studies) while 53 were screened. Further, SQR3 (Survey, Question, Read, Recite, and Review) technique was used and 14 relevant articles were selected.[11] Figure 1 represents the PRISMA Flow chart.
Figure 1.
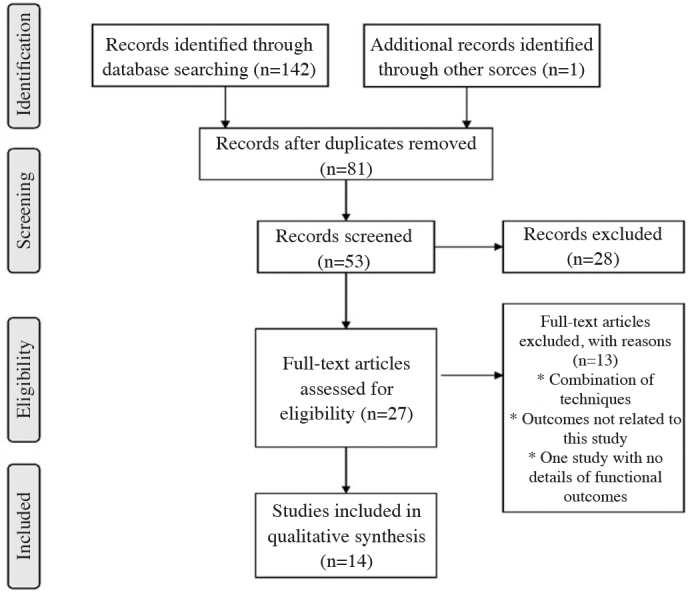
Preferred Reporting items for Systemic reviews and Meta-analyses flow sheet for study selction
Outcome measures
The outcome measures for analysis included:
Patient characteristics (age, high-risk patients),
Operative characteristics (prostate volumes, surgical operative times, enucleated tissues weight, and enucleation time),
Post-operative characteristics (pain, catheterization duration, and hospital stay), and
Functional outcomes (Qmax, IPSS, QOL, PSA, and PVR).
Data extraction
During the first stage, pre-operative data included age of patient in years, prostate volume in mL, IPSS, Qmax in mL/sec, post-void residual (PVR) in ml, prostate-specific agent (PSA) in ng/mL, and hemoglobin in g/dL, and these data were collected and tabulated into two groups.
First group included eight ThuLEP only studies (Non-comparative), Table 1.[12–19} Second group included six Comparative studies only, Table 2.[20–25] It is important to note that out of these six comparative studies, only in four studies patients were randomized. In one study, matching pair analysis was used and in another patient inclusion and exclusion criterion was used for grouping of patients.
Table 1.
Pre-operative characteristics from Thulium-only studies
| Study | Number of patients | Age in years | Prostate volume in ml | IPSS | QOL | Qmax (mL/sec) | PVR in mL | PSA (ng/mL) | Hb | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Chang et al.[12] (Retrospective) | 125 | 71.85 | 106.8 | 27.9 | - | 9.9 | 329.7 | 4.5 | - |
| 2 | Raghuvanshi and Vartak[13] (Prospective) | 109 | 70 | 120.5 | 30 | - | - | - | 1.85 | 11.75 |
| 3 | Saredi et al.[14] (Prospective) | 100 | 70 | 59 | 26 | 4 | 8.8 | 70 | 4.16 | 14.6 |
| 4 | Castellani et al.[15] (Prospective) | 412 | 69.8 | 58 | 26 | 4.4 | 8.1 | - | 2.9 | - |
| 5 | Raber et al.[16] (Prospective) | 139 | 67.8 | 66.9 | 21.2 | 4.4 | 9.6 | 131 | 4.5 | - |
| 6 | Vartak and Salvi[17] (Prospective) | 236 | 72.5 | 70 | 21 | - | 11.2 | - | 3.8 | - |
| 7 | Rausch et al.[18] (Prospective) | 234 | 72.88 | 84.8 | - | - | 10.17 | - | 7.29 | - |
| 8 | Iacono et al.[19] (Prospective) | 148 | 68.2 | 108.8 | 21.1 | 4.38 | - | - | 9.53 | - |
Hb: Hemoglobin; IPSS: International Prostate Symptom Score; PVR: Post-Void residual; PSA: Prostate Specific Antigen; ThuLEP: Thulium Laser enucleation of Prostate; QoL: Quality of Life; Qmax: Maximum Flow rate
Table 2.
Pre-operative details from comparative studies (ThuLEP vs HoLEP)
| Study | Procedure Type | Number of patients | Age in years | Prostate volume in mL | IPSS | QOL | Qmax (mL/sec) | PVR in mL | PSA (ng/mL) | Hb | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 9 | Pirola et al.[20] (Retrospective) | ThuLEP | 117 | 70 | 75 | 20 | 5 | 7 | 90 | 3.8 | 13.5 |
| HoLEP | 117 | 70 | 75 | 21 | 5 | 7 | 130.5 | 5.4 | 14 | ||
|
| |||||||||||
| 10 | Zhang et al.[21] (Prospective) | ThuLEP | 71 | 74.2 | 45 | 24.6 | - | 7 | 64.6 | - | - |
| HoLEP | 62 | 74.2 | 45 | 22.8 | - | 7 | 64.6 | - | - | ||
| Pre-operative details from comparative studies (ThuLEP vs TURP) | |||||||||||
|
| |||||||||||
| 11 | Hou et al.[22] (Retrospective) | ThuLEP | 135 | 70 | 53.5 | 25.5 | 4.8 | 7.8 | 125 | 5.7 | - |
| TURP | 141 | 68 | 48.4 | 24.6 | 4.6 | 10 | 118 | 4.8 | - | ||
|
| |||||||||||
| 12 | Bozzini et al.[23] (Prospective) | ThuLEP | 102 | 72.5 | 89.7 | 19.7 | - | 7.5 | 120 | 3.2 | 14.2 |
| TURP | 106 | 70.7 | 81.9 | 18.6 | - | 6.9 | 112.9 | 3.6 | 14.7 | ||
|
| |||||||||||
| 13 | Swinarski et al.[24] (Prospective) | ThuLEP | 54 | 68.3 | 62.03 | 20.38 | 4.7 | 7.73 | 166.2 | 3.37 | 14.2 |
| TURP | 54 | 69.3 | 66.5 | 20.85 | 4.9 | 8.57 | 152 | 3.73 | 14.4 | ||
|
| |||||||||||
| 14 | Xia et al.[25] (Prospective) | ThuLEP | 52 | 68.9 | 59.2 | 20.8 | 4.7 | 8.0 | 93.1 | - | - |
| TURP | 48 | 69.3 | 55.1 | 20.8 | 4.5 | 8.3 | 85 | - | - | ||
Hb: Hemoglobin; HOLEP: Holmium laser enucleation of prostate; IPSS: International Prostate Symptom Score; PVR: Post-Void residual; PSA: Prostate Specific Antigen; ThuLEP: Thulium Laser enucleation of Prostate; TURP: Transurethral Resection of Prostate; QoL: Quality of Life; Qmax: Maximum Flow rate
This was followed by extracting intra-operative details, including total surgical time in minutes, enucleation time in minutes, morcellation time in minutes, and enucleated adenoma weight in grams. Post-operative parameters included hospital stay, catheterization time, prostate volume in mL, IPSS, Qmax in mL/sec, PVR in mL, PSA in ng/mL, Hemoglobin drop in g/dL, and overall complications. These details are summarized in Tables 3 and 4 (a, b).[12–25]
Table 3.
Intra- and post-operative details from Thulium-only studies
| Study | Total surgical time (minutes) | Enucleation time/Morcellation time (minutes) | Enucleation Weight in grams | Hospital Catheterization in days | Stay in days | IPSS | QoL | Qmax In mL/sec | PVR mL | PSA in (ng/mL) | Hb drop g/dL | Complication rate | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Chang et al.[12] (Retrospective) | - | - | - | - | - | 7.35 | - | 17.92 | 48.22 | - | - | CD-24 %, Mortality=0.8% |
| 2 | Raghuvanshi and Vartak[13] (Prospective) | 62.5 | 35/27.5 | - | 1 | 2.5 | - | - | - | - | - | 0.9 | 41% including one death |
| 3 | Saredi et al.[14] (Prospective) | 56.5 | 21.5/15 | - | 1 | 1 | 3 | 1 | 19 | - | 1 | 1.4 | CD-14% |
| 4 | Castellani et al.[15] (Retrospective) | 55 | - | - | 2 | 3 | 4 | 0.9 | 13.2 | - | 1 | - | CD-14.1 % |
| 5 | Raber et al.[16] (Prospective) | 63.7 | - | 23.8 | 1.5 | - | 3.6 | 1.8 | 31.2 | - | 1.2 | 1.9 | CD-3.6% |
| 6 | Vartak and Salvi[17] (Prospective) | 86.5 | 53/33.5 | - | 1.05 | 1.18 | 4.2 | - | 21 | - | 1.3 | 0.8 | Superficial bladder injury (7.6%), Stricture (3.8%), Bladder neck contracture (1.2%) |
| 7 | Rausch et al.[18] (Prospective) | 102.54 | - | 53.68 | 6.5 | 5.1 | 1.07 | 23.27 | 12.40 | - | - | CD-19.8% | |
| 8 | Iacono et al.[19] | 70.03 | 50.34/18.23 | 2.04 | 2.15 | 3.90 | - | 28.67 | - | 0.94 | 1.27 | UTI (12.8%), Irritating symptoms (6.7%, Recatheterization (2.7%) |
CD-Clavien Dindo classification of post-operative complications[26], Hb: Hemoglobin; HOLEP: Holmium laser enucleation of prostate; IPSS: International Prostate Symptom Score; PVR: Post-Void residual; PSA: Prostate Specific Antigen; ThuLEP: Thulium Laser enucleation of Prostate; TURP: Transurethral Resection of Prostate; QoL: Quality of Life; Qmax: Maximum Flow rate
Table 4a.
Intra- and post -operative details from comparative studies (ThuLEP vs HoLEP)
| Study | Procedure type | Total surgical time (minutes) | Enucleation time/Morcellation time (minutes) | Enucleation Weight in grams | Catheterization in days | Hospital stay in days | IPSS | QoL | Qmax In mL/sec | PVR in mL | PSA (ng/mL) | Hb drop g/dL | Complication rate | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10 | Pirola et al.[20] (Retrospective) | ThuLEP | 82.7 | 70.5/12.0 | 45.6 | 1 | 1 | 3.8 | 0.36 | 20.43 | 11.83 | 2.6 | 0.5 | 20% |
| HoLEP | 90 | 75.5/11.5 | 44 | 1 | 2 | 4.8 | 1 | 23 | 29.83 | 2.0 | 0.9 | 26% | ||
|
| ||||||||||||||
| 11 | Zhang et al.[21] (Prospective) | ThuLEP | 37.6 | - | 37.6 | 2.4 | - | 9.0 | 1.8 | 21.75 | 16.25 | - | 0.5 | - |
| HoLEP | 40.4 | - | 40.4 | 2.5 | - | 9.5 | 1.8 | 19.75 | 18.00 | - | 0.5 | - | ||
|
| ||||||||||||||
| Table 4b. Intra- and post-operative details from comparative studies (ThuLEP vs TURP) | ||||||||||||||
|
| ||||||||||||||
| 12 | Hou et al.[22] (Retrospective) | ThuLEP | 79.3 | - | 24.99 | - | 4.2 | 4.06 | 1.4 | 14.76 | - | - | - | 11.99 % |
| TURP | 62.4 | - | 23.03 | - | 4.3 | 3.9 | 1.3 | 15.1 | - | - | - | 5.0% | ||
|
| ||||||||||||||
| 13 | Bozzini et al.[23] (Prospective) | ThuLEP | 53.69 | - | 51.13 | 1.3 | 1.7 | 5.8 | - | 22.14 | 31.2 | - | .45 | 17.2% |
| TURP | 61.66 | - | 48.84 | 4.8 | 5.2 | 5.7 | - | 19.87 | 39.8 | - | 2.8 | 24.3% | ||
|
| ||||||||||||||
| 14 | Swinarski et al.[24] (Prospective) | ThuLEP | 102.2 | 74.2/28.1 | 24.8 | 2.1 | 3.6 | 7.5 | 1.7 | 22.44 | 29.9 | - | 0.95 | - |
| TURP | 74.2 | 34.8 | 2.0 | 3.5 | 7.8 | 1.4 | 24.9 | 32.4 | - | 1.8 | - | |||
|
| ||||||||||||||
| 15 | Xia et al.[25] (Prospective) | ThuLEP | 46.3 | - | 21.2 | 1.9 | 4.8 | 4.7 | 1.2 | 24.0 | 14.1 | 0.92 | UTI (3.9%) Ret. Ejaculation (55%) | |
| TURP | 50.4 | - | 34.8 | 3.6 | 6.7 | 4.7 | 1.1 | 23.3 | 15.0 | 1.46 | UTI (8.3%) Ret. Ejaculation (965%) | |||
Hb: Hemoglobin; HOLEP: Holmium laser enucleation of prostate; IPSS: International Prostate Symptom Score; PVR: Post-Void residual; PSA: Prostate Specific Antigen; ThuLEP: Thulium Laser enucleation of Prostate; TURP: Transurethral Resection of Prostate; QoL: Quality of Life; Qmax: Maximum Flow rate
Results
Based on primary outcomes, the results from patients who underwent ThuLEP procedure for BPH are as under:
Age: This review found that mean age of patients was around 70 years. However, many studies have revealed ThuLEP is safe in elderly population even in the range of 90 years as well.[12,13,22]
High-Risk Patients: ThuLEP can be used in patients having high risk American Society of Anaesthesiologists (ASA) grades for surgery. In one study, 109 patients with ASA Grade 3 or 4, in age group of 60 and 70 years, having comorbidities, such as ischemic heart diseases, hypertension, and diabetes mellitus, underwent ThuLEP with good results.[14]
Prostate Volumes: In this review, we found ThuLEP has been safely used in prostates with volumes of 70 mL on an average. However, a recent study has found, in 125 patients with volumes of more than 80 mL, that ThuLEP is safe as well as efficacious.[12]
Operative times: Operative times of ThuLEP was around 75 minutes in our review. On an average enucleation time was about 50.75 and morcellation time being 20.72 minutes. It is anticipated that enucleation can be better with TFL as compared with Ho:YAG as laser fiber as it is continuous in former rather than pulsed. However, there was still visible variation in duration of surgeries in different studies, the two main factors responsible for time duration included previous exposure to laser enucleation techniques and, secondly, less experienced surgeons taking more time for enucleation.[14]
Enucleated Tissue: Enucleated adenoma weight was on an average around 35 grams.
Post-operative pain: A recent study has established that ThuLEP is far more tolerated and needed minimal analgesia in post-op period compared with other procedures; study found that the TURP group required oral analgesics for more than 1 week after surgery (12.2% vs 4.4%, p=0.039).[22]
Catheterization Time and Hospital stay: For ThuLEP procedures average Catheterization timing was 1.5 days. This is quite an important factor as it often determines safe discharge of the patient from the hospital. The average hospital stay in hospital was 2.8 days for ThuLEP patients.
Functional outcomes: Functional outcomes after calculating averages are summarized in Figure 2. The main reason was variability in studies in their follow up. In some studies, it was 4–6 weeks and in others as far as 24 months. The reasons for variation are 2-fold origin of study determining length of follow up based on local guidelines and practices and secondly determined by the main aim of study. All four parameters IPSS, QoL, Qmax, and PVR show improvement till 12 months and then values usually plateau. This is seen in terms of means as well as values obtained in studies carried for 24 months.[15,18]
Complications: We found lot of variation in reporting of complications. On Clavein Dindo reporting most studies reported Grade 3 being maximum[26]. Most common complications included urinary tract infections, irritating symptoms, and re-catheterization. One study reported death of a patient due to myocardial infarction 1-week post-surgery.[13]
Cost: Regarding cost effectiveness, although there are no comparative trails available but there are multiple factors that make ThuLEP a cost-effective procedure. If we look at acquisition costs, TFL fiber cost is about 400 Pounds each, which is comparable to other Laser systems, however, in contrast to them, it can be used many times and amounts to negligible running costs.[27] Similarly, energy consumption is 9 times less than Holep and less maintenance of components decreases cost further.[28] Also less intra-operative morbidity and early post- operative recovery, helps in early hospital discharge, and subsequently leads to a decreased cost.[29]
Figure 2.

Functional outcomes after ThuLEP
IPSS: International Prostate Symptom Score; PVR: Post-Void residual; PSA: Prostate Specific Antigen; QoL: Quality of Life; Qmax: Maximum Flow rate
Secondary outcomes included comparison with TURP and HoLEP. Table 5 summarizes mean values for all studies for purpose of comparison. Graphical comparison is represented in Figures 3, 4.
Table 5.
Summarized results for all three types of surgeries
| ThuLEP | TURP | HOLEP | |
|---|---|---|---|
| Patients | 2034 | 349 | 179 |
| Age | 70.49 | 69.3 | 72.1 |
| Preoperative | |||
| ThuLEP | TURP | HOLEP | |
| Prostate volume | 75.64 | 62.9 | 60.0 |
| IPSS | 23.39 | 21.21 | 21.9 |
| QoL | 4.54 | 4.6 | 5.0 |
| Qmax | 8.56 | 8.4 | 7.0 |
| PVR | 132.1 | 116.9 | 97.5 |
| PSA | 4.55 | 4.04 | 5.4 |
| Hb | 13.65 | 14.55 | 14.0 |
| Operative | |||
| Total surgical time | 69.12 | 62.16 | 65.2 |
| Enucleation time | 50.75 | - | 75.5 |
| Morcellation time | 20.72 | - | 11.5 |
| Enucleated adenoma weight | 35.35 | 35.36 | 42.2 |
| Post-operative | |||
| ThuLEP | TURP | HoLEP | |
| Catheterization time (days) | 1.57 | 3.4 | 1.75 |
| Hospital stay (days) | 2.8 | 4.9 | 2.0 |
| IPSS | 5.07 | 5.5 | 7.15 |
| Qol | 1.24 | 1.26 | 1.08 |
| Qmax (mL/sec) | 21.52 | 21.04 | 21.37 |
| PVR (mL) | 23.41 | 29.06 | 23.9 |
| PSA (ng/mL) | 1.34 | - | 2.0 |
| Hb drop (g/dL) | 0.95 | 2.0 | 0.7 |
Hb: Hemoglobin; HOLEP: Holmium laser enucleation of prostate; IPSS: International Prostate Symptom Score; PVR: Post-Void residual; PSA: Prostate Specific Antigen; ThuLEP: Thulium Laser enucleation of Prostate; TURP: Transurethral Resection of Prostate; QoL: Quality of Life; Qmax: Maximum Flow rate
Figure 3.

Pre-operative comparison
Hb: Hemoglobin; HOLEP: Holmium laser enucleation of prostate; IPSS: International Prostate Symptom Score; PVR: Post-Void residual; PSA: Prostate Specific Antigen; ThuLEP: Thulium Laser enucleation of Prostate; TURP: Transurethral Resection of Prostate; QoL: Quality of Life; Qmax: Maximum Flow rate
Figure 4.

Post-operative comparison
Hb: Hemoglobin; HOLEP: Holmium laser enucleation of prostate; IPSS: International Prostate Symptom Score; PVR: Post-Void residual; PSA: Prostate Specific Antigen; ThuLEP: Thulium Laser enucleation of Prostate; TURP: Transurethral Resection of Prostate; QoL: Quality of Life; Qmax: Maximum Flow rate
Discussion
Lasers have become an essential tool in the armamentarium for urologists. Lately, Thulium laser has been making in roads and replacing Ho:YAG laser. Although both Holmium and Thulium lasers use water as chromophore, the fiber in Thulium Fiber Laser (TFL) is diode pumped, which gives it the capability of operating in either a pulsed mode or a continuous wave mode at around 2000 nm. The continuous wave mode is more suitable for haemostasis and coagulation of tissue, whereas the pulsed mode is more suited for lithotripsy.[30] The continuous mode causes rapid and improved vaporization thereby ensuring smooth tissue incisions compared to those of the holmium laser. This helps surgeons to accurately remove the adenoma at the level of the surgical capsule by easily distinguishing adenoma.[31] Further with shallow depth of penetration of 0.25 mm, it causes minimal damage to surrounding tissues. This helps in prevention of many post-operative complications, including post-operative dysuria noticed with other lasers.[32] The other advantages of TFL is that its diameter is about 50 mm compared to minimum 200 mm in Ho:YAG, this results in advantages in irrigation, scope deflection, and (in) direct effects on accessibility, visibility, efficiency, and surgical time, as well as offering future miniaturization possibilities.[33] Further, TFL fibers do not degrade easily and have 4 times more absorption coefficient and results in higher ablation efficiency.[34] The TFL machine itself is seven times smaller and eight times lighter than a high-power Ho:YAG laser system( 35–45 kg to 250–300 kg) and consumes nine times less energy as its frequency can reach upto 2,200 Hertz (Hz) compared with Ho:YAG, which can reach a maximum of 80–100 Hz. Maintenance is expected to be very low due to the durability of its components.[15]
Our review revealed that ThuLEP is safe for all age groups as well as for all prostate sizes. Comparing it with TURP and HoLEP we established it is non-inferior to both these standard procedures intra-operatively in terms of tissue enucleation and overall surgical duration. The results from our review regarding improvement in functional outcomes and complications are somewhat similar to a previous review in which all forms of Thulium laser procedures for BPH (enucleation, resection, and vaporization) were compared with TURP, BiTURP, and Holmium.[10] In one study comparing ThuLep with TURP, a higher proportion of patients in the TURP group required oral analgesics for more than 1 week after surgery (12.2% vs 4.4%, p=0.039).[25] In our review, the mean catheterization timing for ThuLEP was 1.5 days, which was lower compared with HoLEP at 1.75 days and 3.4 days for TURP. This often gets reflected in early discharge from hospital. It is estimated that such outcomes can bring down cost from conventional surgeries by about 27%.[16]
Regarding cost effectiveness, although there are no comparative trails available but there are multiple factors that make ThuLEP a cost-effective procedure as has been explained and highlighted earlier in results section. Another added benefit is that ThuLep is easy in terms of the learning curve as compared with HoLep, which needs 40–60 cases on an average to become proficient.[35] The first important reason for this that the thulium laser allows for instant conversion to vaporization with the same end-fire fiber, a technique that more urologists are comfortable with.[36] The second reason is that compared to HoLEP, ThuLEP vaporizes more tissue, makes a wider incision and plane between adenoma, and the capsule is always clearly visible.[19]
This review has many limitations, the primary goals of different studies were variable and as such there was quite variability in patient characteristics. Further, the outcome measurements were calculated in different methods and authors had to often calculate averages for outcome measurements. In addition, there was often non-uniformity in reporting complications. Some studies had reported complications using Clavien Dindo classification, while as others had enlisted in percentages.[26]
In conclusion, ThuLep is safe, efficacious, and cost-effective alternative to TURP and HoLEP in all age groups and prostate sizes. To establish its permanent position in management of BPE, more comparative trials will be necessary in future.
Main Points.
ThuLEP is a safe and efficacious alternative to HoLEP and TURP for all age groups and prostate sizes.
Thulep is non-inferior in terms of operative and functional outcomes and, in fact, is associated with better post-operative results in terms of lesser catheterization duration as well as shorter hospital stay.
All four functional outcomes (IPSS, QoL, Qmax, PVR) revealed marked improvement at 3, 6, 12, and 24 months.
Thulium fiber laser (TFL) has advantages of being light weight, having high frequency, less degradation, and less energy consumption making it cost effective for operational and maintenance purpose.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – M.W., S.M.; Design – M.W., S.M.; Supervision – S.M., S.S.; Resources – M.W., T.B.; Materials – M.W.; Data Collection and/or Processing – M.W.; Analysis and/or Interpretation – S.M., S.S., T.B.; Literature Search – M.W., T.B.; Writing Manuscript – M.W.; Critical Review – S.M., Other – S.S., T.B.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Chapple CR. Lower urinary tract symptoms suggestive of benign prostatic obstruction--Triumph: design and implementation. Eur Urol. 2001;39(Suppl 3):31–6. doi: 10.1159/000052565. [DOI] [PubMed] [Google Scholar]
- 2.Wei JT, Calhoun E, Jacobsen SJ. Urologic diseases in America project: benign prostatic hyperplasia. J Urol. 2005;173:1256–61. doi: 10.1097/01.ju.0000155709.37840.fe. [DOI] [PubMed] [Google Scholar]
- 3.Speakman M, Cheng X. Management of the complications of BPH/BOO. Indian J Urol. 2014;30:208. doi: 10.4103/0970-1591.127856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barry M, Cantor A, Roehrborn C. Relationships Among Participant International Prostate Symptom Score, Benign Prostatic Hyperplasia Impact Index Changes and Global Ratings of Change in a Trial of Phytotherapy in Men with Lower Urinary Tract Symptoms. J Urol. 2013;189:987–92. doi: 10.1016/j.juro.2012.08.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Asseldonk Barkin, Elterman Medical therapy for benign prostatic hyperplasia: a review. Can J Urol. 2015;22(Suppl 1):7–17. [PubMed] [Google Scholar]
- 6.Vincent M, Gilling P. HoLEP has come of age. World J Urol. 2014;33:487–93. doi: 10.1007/s00345-014-1443-x. [DOI] [PubMed] [Google Scholar]
- 7.Huang S, Tsai C, Tseng C, Shih M, Yeh Y, Chien K, et al. Comparative efficacy and safety of new surgical treatments for benign prostatic hyperplasia: systematic review and network meta-analysis. BMJ. 2019:l5919. doi: 10.1136/bmj.l5919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gravas S, Bachmann A, Reich O, Roehrborn C, Gilling P, De La Rosette J. Critical review of lasers in benign prostatic hyperplasia (BPH) BJU Int. 2011;107:1030–43. doi: 10.1111/j.1464-410X.2010.09954.x. [DOI] [PubMed] [Google Scholar]
- 9.Shu-Jie X. Two-micron (thulium) laser resection of the prostate-tangerine technique: a new method for BPH treatment. Asian J Androl. 2009;11:277–81. doi: 10.1038/aja.2009.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barbalat Y, Velez M, Sayegh C, Chung D. Evidence of the efficacy and safety of the thulium laser in the treatment of men with benign prostatic obstruction. Ther Adv Urol. 2016;8:181–91. doi: 10.1177/1756287216632429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coughlan M, Cronin P. Health and Social Care. 1st. SAGE; 2013. Doing a literature review in nursing. [Google Scholar]
- 12.Chang C, Lin T, Huang J. Safety and effectiveness of high-power thulium laser enucleation of the prostate in patients with glands larger than 80mL. BMC Urol. 2019;19:8. doi: 10.1186/s12894-019-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raghuvanshi K, Vartak K. Outcome of thulium laser enucleation of prostate surgery in high-risk patients with benign prostatic hyperplasia. Urol Ann. 2019;11:358–62. doi: 10.4103/UA.UA_175_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saredi G, Pirola G, Ambrosini F, Barbieri S, Berti L, Pacchetti A, et al. Feasibility of en bloc thulium laser enucleation of the prostate in a large case series. Are results enhanced by experience? Asian J Urol. 2019;6:339–45. doi: 10.1016/j.ajur.2019.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castellani D, Pirola G, Gasparri L, Pucci M, Di Rosa M, Carcano G, et al. Are Outcomes of Thulium Laser Enucleation of the Prostate Different in Men Aged 75 and Over? A Propensity Score Analysis. Urology. 2019;132:170–6. doi: 10.1016/j.urology.2019.06.025. [DOI] [PubMed] [Google Scholar]
- 16.Raber M, Buchholz N, Vercesi A, Hendawi N, Inneo V, Di Paola G, et al. Thulium laser enucleation of the prostate (ThuLEP): Results, complications, and risk factors in 139 consecutive cases. Arab J Urol. 2018;16:411–6. doi: 10.1016/j.aju.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vartak K, Salvi P. Thulium laser enucleation of the prostate is a safe and a highly effective modality for the treatment of benign prostatic hyperplasia - Our experience of 236 patients. Urol Ann. 2016;8:76–80. doi: 10.4103/0974-7796.171494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rausch S, Heider T, Bedke J, Kruck S, Schwentner C, Fischer K, et al. Analysis of Early Morbidity and Functional Outcome of Thulium: Yttrium-Aluminum-Garnet Laser Enucleation for Benign Prostate Enlargement: Patient Age and Prostate Size Determine Adverse Surgical Outcome. Urology. 2015;85:182–8. doi: 10.1016/j.urology.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 19.Iacono F, Prezioso D, Di Lauro G, Romeo G, Ruffo A, Illiano E, et al. Efficacy and safety profile of a novel technique, ThuLEP (Thulium laser enucleation of the prostate) for the treatment of benign prostate hypertrophy. Our experience on 148 patients. BMC Surg. 2012;12(Suppl 1):S21. doi: 10.1186/1471-2482-12-S1-S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pirola G, Saredi G, Codas Duarte R, Bernard L, Pacchetti A, Berti L, et al. Holmium laser versus thulium laser enucleation of the prostate: a matched-pair analysis from two centers. Ther Adv Urol. 2018;10:223–33. doi: 10.1177/1756287218779784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang F, Shao Q, Herrmann T, Tian Y, Zhang Y. Thulium Laser Versus Holmium Laser Transurethral Enucleation of the Prostate: 18-Month Follow-up Data of a Single Center. Urology. 2012;79:869–74. doi: 10.1016/j.urology.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 22.Hou CP, Lin YH, Juang HH, Chang PL, Chen CI, Yang PS, et al. Clinical outcome of transurethral enucleation of the prostate using the 120-W thulium Laser (Vela™ XL) compared to bipolar transurethral resection of the prostate (TURP) in aging male. Aging. 2020;12:1888–98. doi: 10.18632/aging.102720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bozzini G, Seveso M, Melegari S, de Francesco O, Buffi N, Guazzoni G, et al. Thulium laser enucleation (ThuLEP) versus transurethral resection of the prostate in saline (TURis): A randomized prospective trial to compare intra and early postoperative outcomes. Actas Urol Esp. 2017;41:309–15. doi: 10.1016/j.acuro.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 24.Świniarski P, Stępień S, Dudzic W, Kęsy S, Blewniewski M, Różański W. BPH Thulium laser enucleation of the prostate (TmLEP) vs. transurethral resection of the prostate (TURP): evaluation of early results. Cent European J Urol. 2012;65:130–4. doi: 10.5173/ceju.2012.03.art6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xia S, Zhuo J, Sun X, Han B, Shao Y, Zhang Y. Thulium Laser versus Standard Transurethral Resection of the Prostate: A Randomized Prospective Trial. Eur Urol. 2008;53:382–90. doi: 10.1016/j.eururo.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 26.Clavien P, Barkun J, de Oliveira M, Vauthey J, Dindo D, Schulick R, et al. The Clavien-Dindo Classification of Surgical Complications. Ann Surg. 2009;250:187–96. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 27.Szlauer R, Götschl R, Razmaria A, Paras L, Schmeller N. Endoscopic Vaporesection of the Prostate Using the Continuous-Wave 2-μm Thulium Laser: Outcome and Demonstration of the Surgical Technique. Eur Urol. 2009;55:368–75. doi: 10.1016/j.eururo.2008.10.034. [DOI] [PubMed] [Google Scholar]
- 28.Bach T, Herrmann T, Haecker A, Michel M, Gross A. Thulium:yttrium-aluminium-garnet laser prostatectomy in men with refractory urinary retention. BJU Int. 2009;104:361–4. doi: 10.1111/j.1464-410X.2009.08412.x. [DOI] [PubMed] [Google Scholar]
- 29.Carmignani L, Macchi A, Ratti D, Finkelberg E, Casellato S, Maruccia S, et al. One day surgery in the treatment of benign prostatic enlargement with thulium laser: A single institution experience. Korean J Urol. 2015;56:365–9. doi: 10.4111/kju.2015.56.5.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hardy L, Wilson C, Irby P, Fried N. Thulium fiber laser lithotripsy in an in vitro ureter model. J Biomed Opt. 2014;19:128001. doi: 10.1117/1.JBO.19.12.128001. [DOI] [PubMed] [Google Scholar]
- 31.Chang CH, Lin TP, Huang JY. Safety and effectiveness of high-power thulium laser enucleation of the prostate in patients with glands larger than 80mL. BMC Urol. 2019;19:8. doi: 10.1186/s12894-019-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rieken M, Ebinger Mundorff N, Bonkat G, Wyler S, Bachmann A. Complications of laser prostatectomy: a review of recent data. World J Urol. 2010;28:53–62. doi: 10.1007/s00345-009-0504-z. [DOI] [PubMed] [Google Scholar]
- 33.Kronenberg P, Traxer O. The laser of the future: reality and expectations about the new thulium fiber laser-a systematic review. Transl Androl Urol. 2019;8(Suppl 4):S398–S417. doi: 10.21037/tau.2019.08.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilson C, Hardy L, Irby P, Fried N. Microscopic analysis of laser-induced proximal fiber tip damage during holmium:YAG and thulium fiber laser lithotripsy. Optical Engineering. 2016;55:046102. doi: 10.1117/1.OE.55.4.046102. [DOI] [Google Scholar]
- 35.Brunckhorst O, Ahmed K, Nehikhare O, Marra G, Challacombe B, Popert R. Evaluation of the Learning Curve for Holmium Laser Enucleation of the Prostate Using Multiple Outcome Measures. Urology. 2015;86:824–9. doi: 10.1016/j.urology.2015.07.021. [DOI] [PubMed] [Google Scholar]
- 36.Gross AJ, Netsch C, Knipper S, Hölzel J, Bach T. Complications and Early Postoperative Outcome in 1080 Patients After Thulium Vapoenucleation of the Prostate: Results at a Single Institution. Eur Urol. 2013;63:859–67. doi: 10.1016/j.eururo.2012.11.048. [DOI] [PubMed] [Google Scholar]


