Abstract
Women and children bear substantial morbidity and mortality as a result of armed conflicts. This Series paper focuses on the direct (due to violence) and indirect health effects of armed conflict on women and children (including adolescents) worldwide. We estimate that nearly 36 million children and 16 million women were displaced in 2017, on the basis of international databases of refugees and internally displaced populations. From geospatial analyses we estimate that the number of non-displaced women and children living dangerously close to armed conflict (within 50 km) increased from 185 million women and 250 million children in 2000, to 265 million women and 368 million children in 2017. Women’s and children’s mortality risk from non-violent causes increases substantially in response to nearby conflict, with more intense and more chronic conflicts leading to greater mortality increases. More than 10 million deaths in children younger than 5 years can be attributed to conflict between 1995 and 2015 globally. Women of reproductive ages living near high intensity conflicts have three times higher mortality than do women in peaceful settings. Current research provides fragmentary evidence about how armed conflict indirectly affects the survival chances of women and children through malnutrition, physical injuries, infectious diseases, poor mental health, and poor sexual and reproductive health, but major systematic evidence is sparse, hampering the design and implementation of essential interventions for mitigating the harms of armed conflicts.
Introduction
Reducing the frequency and intensity of armed conflicts is an explicit goal and a common theme of the 2030 Sustainable Development Goals. 1 The destructiveness of armed conflict presents persistent setbacks to the development and flourishing of human societies. 2 This Series paper focuses on the direct (due to violence) and indirect health effects of armed conflict on women and children (including adolescents), which are populations with unique vulnerabilities and risks that may be increased during periods of conflict.
We surveyed the evidence for the adverse health effects experienced by women and children exposed to armed conflict, acknowledging that every conflict-affected region, every conflict, and every affected community is different from all others, while also sharing common features. Information documenting the health consequences of armed conflict among affected populations is often weak, and data specifically about women and children are even more limited.
The attribution of adverse effects to a conflict—other than battle-related deaths of combatants and civilians (ie, conflict’s indirect effects)—is methodologically complex. Additionally, the context for conflict is changing, further complicating efforts to infer consistent effects across time and geography. 3 In this Series paper, we provide new estimates of the numbers of women and children affected by armed conflict, first for displaced and then for nondisplaced populations. We then estimate the indirect mortality effects of conflicts by extending previous analyses of infant and child mortality and summarising findings on mortality from conflict among women of childbearing age. Finally, we review and reflect on the current evidence of the non-fatal adverse effects of conflicts, such as malnutrition and injuries among women and children, and highlight knowledge gaps and research priorities.
Populations affected by armed conflict
Attempts to define and estimate the size of the populations affected by conflict are an intuitive starting point for estimating the bounds of the health burden from armed conflict. The populations affected by conflict can be conceptualised in different ways depending on the effects that are assessed. Unless noted otherwise, we define populations affected as women (≥18 years) and children (0–18 years) who are either forcibly displaced— including refugees, asylum seekers, and internally displaced people—or not displaced but living at increased risk of direct or indirect mortality and morbidity from nearby armed conflicts.
To gauge the populations affected, we started with a standard conceptualisation of armed conflict. The Uppsala Conflict Data Program (UCDP) has been collecting data about conflict, violence, and peacemaking for research purposes, with data going back to 1946. The programme categorises data about conflict events and fatalities in state-based conflict (in which a government is engaged in armed conflict against combatant groups such as another government or rebel group); non-state conflict (violence between non-state groups such as rebel groups, and no government is involved); and one-sided conflict (a government perpetrates violence against non-combatants, mostly civilians). In this Series paper, we consider the effects on women and children’s health irrespective of the type of conflict. We define armed conflict as any of the conflict types in the UCDP: use of force which results in at least 25 battle-related deaths per year in a specific country. 4
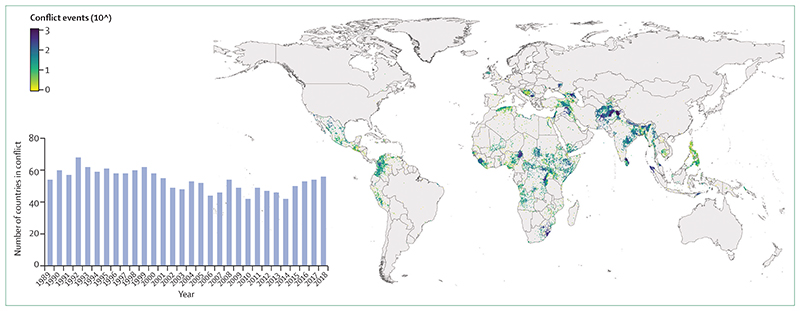
Direct combat-related deaths in the UCDP are separated for combatants and non-combatants, but not by sex or age. Figure 1 shows the number of countries in which armed conflict (of any type) has occurred from 1989 to 2018, and the spatial distribution of armed conflict events, indicating that conflict is concentrated in parts of the world that are generally considered to be less developed (Africa, central Asia, and south Asia). Every year over the past three decades, armed conflict has occurred in between a quarter and a third of the world’s countries, without clear time trends. Some studies posit that the post-World War 2 era is among the most peaceful in human history, and that armed conflict has declined steadily since the end of World War 2. 5 Although the evidence for inter-state conflicts shows meaningful and unambiguous decline since 1946, the patterns in intrastate conflicts, most notably in Africa, the Middle East, and parts of Asia and Latin America, suggest stable or intensified (and often protracted) fighting in the past three decades. 3,6,7
Figure 1. Geographical distribution of armed conflict events, 1989-2018, shown in log10 scale.
Inset shows the number of countries in conflict in each year. Data are from the Uppsala Conflict Data Program.
Women and children displaced by armed conflict
Refugee statistics have to be interpreted cautiously because definitions and data collection methods often vary between countries and agencies. 8 According to data compiled by the UN High Commissioner for Refugees (UNHCR) the number of refugees, defined as forcibly displaced people who cross an international border and who cannot return home safely, has almost doubled during the past decade, from 10·5 million in 2008 to 20·4 million by the end of 2018. Two-thirds of the refugees originated from five countries: Syria (6·7 million), Afghanistan (2·7 million), South Sudan (2·3 million), Myanmar (1·1 million) and Somalia (0·9 million). Additionally, there were 3·1 million asylum seekers in 2017. Another 5·5 million Palestinian refugees are under the mandate of the UN Relief and Works Agency, rather than the UNHCR, bringing the total number of refugees globally to 25·9 million in 2018. Venezuela has a rapidly growing number of international migrants and refugees, exceeding 4 million in the course of 2019 according to the UNHCR, as a result of the country’s economic and political instability. Notably, displacement is a complex process, and these estimates are approximations that cannot accurately capture mixed displacement patterns and distinguish forced displacement due to conflict from other causes, such as droughts.
Armed conflicts also lead to displacement of populations that do not cross international borders, and therefore remain uncounted by the UNHCR. Based on data from the Internal Displacement Monitoring Centre, the number of internally displaced people due to conflict and violence increased from approximately 25 million in 2009–10, to 45·7 million in 2019, of whom almost 21 million (46%) were women and girls. 9,10 Two-thirds of internally displaced people were based in six countries: Syria, Colombia, Democratic Republic of the Congo, Yemen, Afghanistan, and Somalia. The quality of statistics on internally displaced people is often poor because of challenges in counting mobile populations, differences in statistical definitions (eg, on nomads or children born to internally displaced people), poor measurement of so-called end events (eg, return migration, urban settlement, death), and incentives to both under-report and over-report. 11
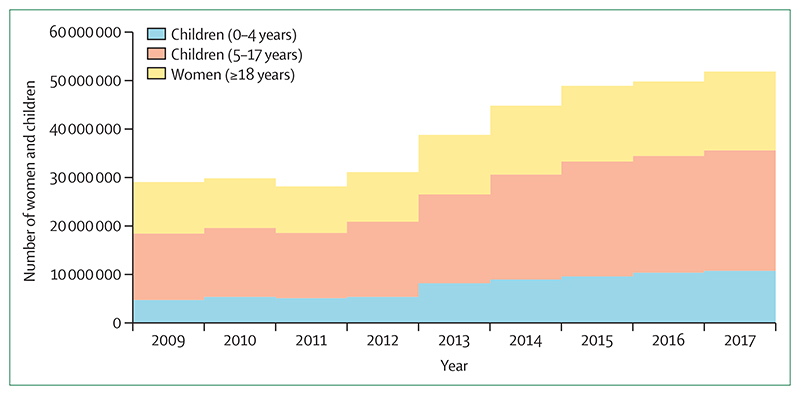
Most forcibly displaced people in the world are women and children. Since 2009, the UNHCR has published data about the age and sex distribution of internally displaced and refugee populations. Between 2009 and 2017, the number of displaced people for whom age and sex data were available increased from 12 million to 27 million. The proportion of displaced people who were children increased gradually since 2009, reaching 52·6% in 2017. The proportion of displaced people who were women decreased gradually, from 26·5% in 2009 to 23·6% in 2017, similar to the proportion of displaced men aged 18 years or older (23·8%).
Applying the age–sex distribution from available data to all displaced populations, we can estimate the number of women and children displaced by armed conflicts. We used regional age–sex distributions and applied these to the regional numbers of displaced people from the UNHCR and Internal Displacement Monitoring Centre databases. For the Palestinian refugee population, we used the age–sex distribution for the state of Palestine as reported by the UN Population Division. 12 In 2009, an estimated 18·5 million children and 10·6 million women were displaced (figure 2). By 2017, there was an increase in both the numbers of displaced children (35·7 million, 1·4% of all children worldwide) and women (16·2 million, 0·6% of all women worldwide; appendix pp 2–3).
Figure 2. Estimated number of children and women displaced by conflict, 2009-17.
Non-displaced women and children affected by conflict
Women and children can be affected by conflict even without being displaced from their homes. Populations that do not move away from nearby conflict—often poor and vulnerable groups—are at increased risk of morbidity and mortality from direct violence and from the deterioration of local conditions. In 2012, there were an estimated 149 million non-displaced people affected by conflict globally. 13 A more recent estimate indicated that approximately 420 million children younger than 18 years were living in areas affected by conflict in 2017. 14
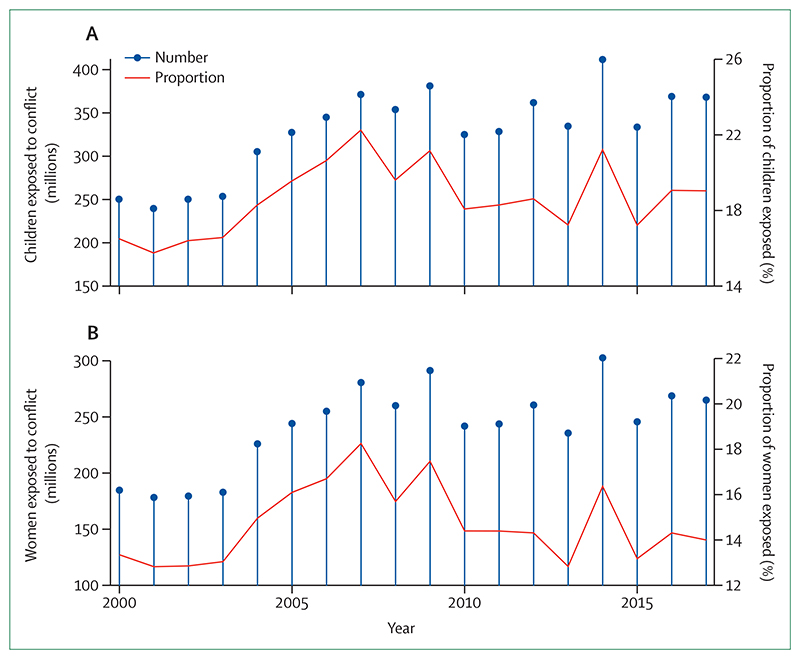
Figure 3 presents the estimated time trend of the conflict-affected non-displaced population sizes from 2000 to 2017, based on the geospatial methods described in the appendix (pp 4–5). We estimate that the number of non-displaced women and children living dangerously close to armed conflict (ie, within 50 km) increased from 185 million women (6·1% of women globally) and 250 million children (11·3% of children globally) in 2000, to 265 million women (7·3%) and 368 million children (16·1%) in 2017, a total of more than 630 million. The greater increase in the global share of children affected by conflict (4·8% increase) compared with women (1·2% increase) could be accounted for by a greater concentration of conflicts in countries with higher fertility.
Figure 3. Women and children exposed to conflict within 50 km.
The number and proportion of children (<18 years; panel A) and women (aged 18-49 years; panel B) living within 50 km of conflict in Africa, Asia (including the Middle East), and the Americas (Latin America and the Caribbean). The denominator is the total age-matched population in those three world regions.
These estimates of non-displaced populations deserve several additional observations. First, the number of women and children living in conflict-affected areas has been gradually growing since 2000, due to the confluence of population growth, urbanisation of conflicts (putting more people at risk), and the persistence of conflicts. 3 The spike observed in 2014 (figure 3) is the result of more intense fighting in Afghanistan, Iraq, Nigeria, Pakistan, and Somalia in that year. Syria has had between 7 million and 9·5 million non-displaced women and children affected every year since 2011, and therefore contributes substantially to the total over time, but not to the spike in the trend. Second, although the estimates vary from year to year, the combined total of conflict-affected women and children did not decrease below 350 million over the 18-year period examined. Third, every year, between a fifth and a sixth of all women and children living in Africa, Asia, and the Americas are affected by nearby armed conflict events. Fourth, underlying population data are often based on estimates that might not fully account for displacement because of armed conflict. In that case, the estimates of the affected non-displaced populations might represent an upper bound on the true numbers. This potential bias is, however, relatively small since the size of the affected non-displaced population is more than ten times larger than that of the displaced population (estimated 633 million, compared with 52 million displaced women and children). Lastly, countries in Asia and Africa are home to the greatest number of affected populations due to a combination of population size and conflict density. In 2017, women and children in Pakistan, Nigeria, and India accounted for about a third of the global total affected by conflict.
Mortality
The burden of mortality that is attributable to armed conflict has been a topic of substantial debate (panel). 26 Considerable uncertainty surrounds estimates of direct and indirect deaths associated with armed conflict. Some have argued that the overlap of conflict-prone countries and high child and maternal mortality is evidence of high mortality toll of conflicts. However, the correspondence between countries with many deaths and many conflicts does not reflect the fact that conflicts are a marker of generalised under-development, which in turn is associated with other conditions related to elevated mortality among women and children.
Panel: Divergent estimates of direct and indirect mortality due to conflicts.
The measurement of the number of deaths among women, children, and adolescents due to conflicts is complex. During active conflict, measurement of casualties due to violence is often limited and subject to much speculation. Global efforts to collect data about violent events and fatalities, such as the Uppsala Conflict Data Program or the Armed Conflict Location & Event Data, are crucial, but they collect only information that is available in news media or field reports and generally do not contain information about indirect mortality or specific population characteristics. A dataset from the Violation Documentation Center that documents violent deaths in Syria was used to estimate that 70% of all violent deaths were civilians. 15 The proportions of civilians who were women and children increased during 2011–16. By 2016, 23·3% of violent deaths were children and 13·8% were adult women.
The estimation of death and disease related to conflict from causes other than violence—often referred to as indirect harms, such as from the breakdown of health services, food security, water supply, and shelter—is even more difficult than direct counts, because it requires high quality measurements as well as a counterfactual (death and disease from the same causes in the absence of conflict) based on assumptions about morbidity and mortality in the absence of conflict. Most estimates of civilian casualties suggest that indirect mortality is considerably higher than direct mortality. Indirect mortality has been estimated to be associated with at least 75% of total excess mortality in 11 of 15 armed conflicts. 16
Household surveys before, during, and after a conflict are often the primary source of estimation of excess mortality. National Demographic and Health Surveys (DHS) are a useful source because they provide retrospective mortality data (birth and sibling survival histories), provided that the potential exclusion of the most insecure areas in the survey is taken into account. A DHS-based comparison of mortality trends in children younger than 5 years in 13 conflict-affected countries in sub-Saharan Africa during 1990–2016 with sub-regional trends showed that, during the active conflict phase, the median annual rate of reduction in child mortality was 1·1% slower in the affected countries in comparison with regional trends. 17 In the first 5 years after conflict cessation, the annual rate of reduction was 1·7% faster in conflict-affected countries compared with sub-regional trends.
Special national surveys have been used to estimate excess mortality in several conflicts, such as those in the Democratic Republic of the Congo, Afghanistan, and Iraq, often resulting in much debate about the methods and results. 18–21 Large numbers of small-scale surveys, generally conducted by non-government organisations involved in the response, are frequently conducted in crisis situations but might give a biased picture of overall mortality trends.
In South Sudan, data from 210 local household surveys conducted during the conflict were used to estimate excess mortality during the period December, 2013–April, 2018. Mortality was estimated at 382 000 including 190 000 deaths due to violence. 22 Among the violent deaths, 10·6% were children and 7·9% were women. A synthesis of 63 local surveys in Darfur region in Sudan showed almost 300 000 excess deaths during 2004–08, of which about 80% were not related to violence and greatly affected child survival. 23
A detailed discussion of the multiple methodological issues and limitations related to national and local surveys, as well as other modes of mortality data collection during and after armed conflicts, is beyond the scope of this paper and is discussed in detail elsewhere. 24,25
A 2018 estimate of the mortality consequences of armed conflicts on infants and children younger than 5 years (under-5s) in Africa was made by aggregating, across 35 African countries, the observed mortality rates during periods of conflict, and comparing them with the observed mortality rates in the same region during periods free of conflict. 27 The results suggest that, from 1995 to 2015, an infant exposed to armed conflict in their first year of life had a 7·7% higher chance of dying before reaching age 1 year than expected in that region without armed conflict. This corresponded with 3·1–3·5 million infants (and 4·9–5·5 million children younger than 5 years) whose deaths were attributable to armed conflict over this period in Africa.
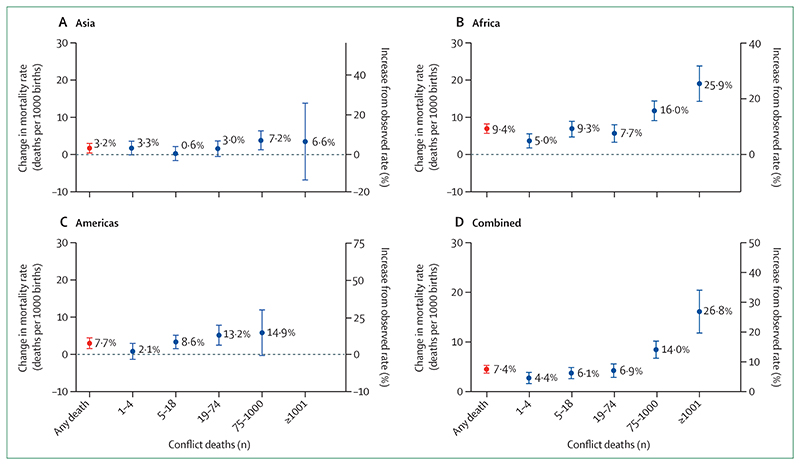
In this paper, we extend the scope of that analysis to consider an additional 18 countries in Asia and 11 countries in the Americas for which we also have georeferenced child survival data from the Demographic and Health Surveys (DHS).
The patterns in the three regions of the world are similar. Figure 4 presents the results of data from the 64 countries (35 in Africa, 18 in Asia, and 11 in the Americas) that represent more than 93% of all conflict events recorded in the UCDP during 1995–2015. The regional pooled effect sizes range from a 3·2% increase in the expected probability of dying before reaching age 1 year in Asia, to 9·4% in Africa, with a combined effect of 7·4%. When we apply this region-specific effect size to the observed number of births within 50 km of conflicts, there is a cumulative total of 6·7–7·5 million infants and 10·1–11·2 million children younger than 5 years whose deaths can be attributable to conflict from 1995 to 2015. This translates into 5·7–6·3% of all infant and child deaths during that period, based on the total number of deaths provided by the UN Interagency Group on Child Mortality Estimation. 28
Figure 4. Increase in risk of mortality in the first year of life for infants born within 50 km of armed conflict.
The figure shows the increase in risk of mortality from having any nearby conflict (red bar), and the mortality risk from conflicts of increasing intensity (blue bars). Observed rate is the population average mortality rate. Error bars are 95% CI. Data for this analysis comes from 4·72 million births between 1995 and 2015 recorded in all Demographic and Health Surveys with cluster coordinates in 64 countries in the Americas, Africa, and Asia. Syria, Yemen, or South Sudan are not included in the mortality risk increase estimations (they were not geocoded in the Uppsala Conflict Data Program or Demographic and Health Surveys were not available), which might bias the effects downward. Compared with the original analysis,27 the effect size in Africa is higher (9·4%, vs 7·7% in the original analysis). Although these differences are not statistically significant, they are notable and result from additional Demographic and Health Surveys that were not available at the time of the 2018 analysis, and combined modelling that included data from Asia and the Americas.
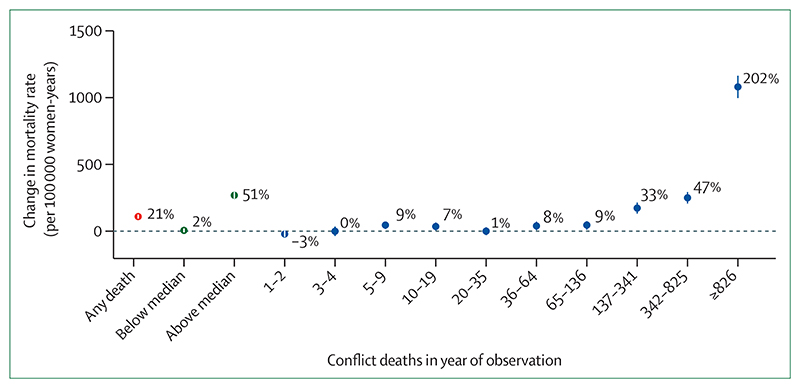
In a separate analysis, we examined the effect of armed conflict on mortality among women of childbearing age (15–49 years), using data about the survival of the sisters of the respondents in DHS surveys (appendix pp 6–8). 29 Figure 5 shows the increase in the probability of a woman of childbearing age dying when exposed to armed conflict within 50 km (proxied by the index sister’s place of residence), compared with years without conflict in the area.
Figure 5. Relationship of mortality among women of childbearing age and armed conflict within 50 km in Africa.
The pooled effect of exposure to any conflict (in red), and the changing effect with exposure to conflicts below or above medial intensity (in green), and increasing deciles of conflict intensity (in blue) for the sample from Africa is based on 19·3 million women-years of observation in 33 African countries.Mortality and location of women was taken from index woman information in Demographic and Health Surveys. 29
The overall relationship is a 21% (95% CI 18·2–23·9) increase in the risk of death among women of childbearing age in Africa. However, the shape of the mortality response to conflict is different from that for infants: conflict confers no appreciable risk when the nearby conflict was of relatively low intensity, and there is a steep rise in the risk from conflicts with an intensity greater than the median number of battle-related deaths. In Africa, the risk of dying among women in the vicinity of conflicts at the top decile in terms of conflict-related deaths was more than three times higher than during non-conflict periods. Nearly all conflicts with intensity in the top decile were concentrated in a few countries: Rwanda, Burundi, Democratic Republic of the Congo, Liberia, and Sierra Leone accounted for most of those events, and only 92 491 (4%) out of 2·25 million women in our sample were exposed to such conflicts.
Malnutrition
Famines, characterised by widespread acute malnutrition and high mortality, have been associated with political instability, disastrous economic strategies of totalitarian regimes, and climatic factors. 30 As the global frequency of famines and associated mortality have been decreasing over time, protracted armed conflicts have become an increasingly important driver of food insecurity, hunger, and malnutrition in populations. 31 Conflicts, by themselves or in combination with natural disasters and decisions made about food supplies and rationing, can lead to a decrease in food availability, social disruption, higher food prices, and eventually hunger. Often, excess mortality is caused by starvation and especially by concomitant diseases such as measles, typhoid fever, and cholera, particularly in children.
Since 1990, eight famines with estimated mortality exceeding 50 000 deaths have been recorded and all, except in North Korea, were associated with conflicts. 32 As of January, 2019, the Famine Early Warning Systems network identified four countries with populations with acute food insecurity and emergency situations (Afghanistan, Nigeria, South Sudan, and Yemen), all of which are countries with extensive recent history of armed conflicts. 33
Small-scale cross-sectional household surveys are the main source of data for malnutrition during conflicts. Wasting prevalence in under-5s (weight for height below two standard deviations from the WHO reference population), with the presence of oedema, has become one of the key indicators of the severity of a crisis. 34 Large numbers of local surveys using the Standardized Monitoring and Assessment of Relief and Transitions (SMART) methods are conducted to monitor nutritional status. A database that compiled survey data from complex emergencies identified 3309 SMART surveys conducted between 2000 and 2013. 35 All local survey results have to be interpreted cautiously and take into account the specifics of each setting, because sampling issues and data quality problems are common. 36 Seasonality and issues related to population displacement also affect survey findings. 37
An analysis of national surveys in sub-Saharan Africa showed that conflict-affected countries had higher levels of wasting in under-5s than the sub-regional averages for the same year during the conflict phase (1·0% higher), but had lower prevalence in surveys conducted 0–4 years (1·2% lower) and 5–9 years (2·2% lower) after the end of the conflict. 17
Stunted growth in under-5s is indicative of chronic malnutrition and can affect future health and development outcomes. Children who resided in conflict-affected areas during the Ethiopia–Eritrea war in 1999–2000 experienced higher levels of stunting than did other children living outside the conflict-affected areas in those countries. 38,39 A similar effect of conflict on stunting was observed in Burundi. 40 In a geospatial analysis of all national surveys in sub-Saharan Africa done during 1995–2005, stunting in children born near a conflict was 2·9% higher than the 34·4% average prevalence. 27
Non-fatal physical injuries and disabilities
Even though physical trauma is a strikingly visible direct consequence of explosives and gunfire, burden estimates are surprisingly scarce. Weapons that are commonly implicated in physical injuries include firearms and explosive devices such as mines, artillery shells, bombs, and improvised explosive devices. Explosive devices can cause injury either at the time of intended detonation, or as unexploded remnants and ordnance that cause injuries after the acute conflict event. Injuries sustained by remnants of war are borne predominantly by non-combatant civilians, including women and children. A systematic review 41 suggested that most injuries from the remnants of war are caused
in the course of daily economic necessities, such as transportation for work or household duties. In that review, between 22% and 55% (median 38%) of landmine casualties were children younger than 18 years, and 0–31% were in women and girls. Although the overall burden of physical injuries was unclear, the frequency of injuries decreased in most studies included in the systematic review, possibly because of improved ordnance (with less unexploded ordnance), and reduced use of landmines. The most common type of injury was a limb amputation, reported in 20–83% of victims. 41 Surveys of traumatic brain injuries among refugees and internally displaced people suggest those are similarly caused by landmines and explosive devices, and are further associated with mental health concerns. 42
Some single-conflict studies attempt enumeration of physical injuries, and include injuries sustained by both combatants and non-combatants. 43,44 However, composite evidence about the burden of conflict-related physical injuries is lacking at this time.
Acute and infectious illnesses
Infectious disease outbreaks are often a feature of waraffected regions, stemming from reduced capacity to prevent infectious disease outbreaks, to control infection spread, and to address infections once they are recognised. 45 Population displacement often forces people into living conditions that include crowding and mixing with large groups of other displaced individuals, in camps or elsewhere. These crowded conditions promote the spread of infections. A systematic review found that incidence and prevalence of active tuberculosis was twice that of the reference population in crisis-affected populations. 46 Measles and hepatitis B outbreaks—diseases transmitted most readily among children—are relatively common among displaced populations from Yemen and Syria. 47,48 Cholera outbreaks have occurred in refugee camps close to conflict zones, such as in Yemen, Democratic Republic of the Congo, and Somalia. 49,50
Reports of widespread rape and sexual violence in conflict settings have prompted investigations into the effects of conflict on HIV. A systematic review 51 of data from seven conflict-affected African countries did not find increased prevalence of HIV in conflict settings or in refugee camps compared with reference populations, but it could not assess the effects of conflict on HIV incidence. Rape and sexual violence remain widely recognised war-related behaviours, but their effects on the transmission of infectious diseases, especially among women, are unknown. 52,53
Armed conflicts also pose a threat for emerging infectious diseases by eroding surveillance and disease control systems. Fundamental disease control measures such as vaccinations, sanitation, and safe drinking water all come under threat in conflict settings. The erosion of conditions that enable control of multiple infectious diseases suggest that the effects can be widespread. Efforts to eradicate poliovirus have been successful in most parts of the world, except for regular outbreaks in war-torn regions such as northern Nigeria, eastern Democratic Republic of the Congo, Syria, and Afghanistan. 54 However, challenging environments, including attacks on health workers, mean that vaccination and eradication campaigns repeatedly fail to achieve sufficient coverage in conflict-affected regions, especially in northern Nigeria and central Asia. 55,56 Although the burden of polio is modest—a handful of wild poliovirus cases are detected each year—billions of USD are invested into reaching populations living in conflict-affected areas to maintain current gains and prevent disease recrudescence. The response to the 2018–20 Ebola virus outbreak in conflict-afflicted North Kivu, Democratic Republic of the Congo, is fraught with pitfalls, a striking illustration of how immediate and lingering effects of armed conflict hinder response to re-emerging infectious diseases and create conditions for their rapid spread. 57
Finally, destruction of clean water and sanitation facilities, especially in refugee and displaced populations, imposes unique risks. The bombing of water facilities in Yemen has enabled a cholera outbreak affecting more than 500 000 people, mostly children. 50 Hepatitis B and E outbreaks are also associated with refugee camps. Hepatitis E, in particular, can be lethal to pregnant women, and recent outbreaks have been documented among refugees in South Sudan and Ethiopia. 58 In post-conflict northern Uganda, hepatitis B prevalence was 2–2·5 times higher than the national average. 59
Chronic and non-communicable diseases (NCDs)
Chronic conditions are increasingly important in conflict settings because of the general rise in the prevalence of NCDs in low-income countries, the spread of conflicts to middle-income countries where NCDs are often the leading cause of death, and the protracted and urban nature of current conflicts. 60,61
The evidence on effects of armed conflict on the incidence, severity, and case fatality of NCDs is limited, in terms of both immediate and long-term effects. 61,62 In theory, protracted conflicts can have unpredictable effects on major behavioural risk factors for NCDs, because they can lead to increased or decreased tobacco use, alcohol consumption, poor diet, and lack of physical exercise. The economic, social, logistical, and mental health events surrounding armed conflict might lead to stressors associated with, for example, cancer, respiratory diseases, or risk factors such as hypertension. Although stress can exacerbate NCD risk factors, the evidence for armed conflicts exacerbating NCDs through this pathway, especially among women and children, is weak. 63
Poor access to health services and lack of continuity of care in conflict settings can result in disruption to the effective care of cardiovascular and cerebrovascular conditions, diabetes, chronic respiratory diseases, cancers, and other NCDs. The increases in targeted attacks on health facilities and health workers in conflict settings further complicate the provision of health services, affecting all ages and both sexes.
Mental health
Women and children affected by armed conflicts are exposed to increased levels of traumatic experiences, which include direct exposure to violence, disruption of family structure, and social disintegration. Many people are affected by displacement, including prolonged confinement to refugee camps. The trends towards protracted complex conflicts in often urban settings with greater effects on civilians are likely to lead to greater exposure to traumatic experiences for all civilians. 3
Exposure to armed conflicts is associated with increased prevalence of anxiety disorders, such as post-traumatic stress disorder, and depression among children, 64,65 adolescents, 66 and women, 67 both during and after conflicts. The quantification of the effects of warfare exposure on mental health is complex, not only because the results on the prevalence and risk factors for mental disorders can vary widely between conflicts but also because of methodological issues related to the measurement of population mental health in general, and in conflict settings in particular. It has been estimated that the average prevalence of anxiety disorders and major depression among conflict-affected populations is two to four times as high as global prevalence estimates, with a large effect of conflict exposure on women’s mental health. 67 Several studies have reported greater effect of conflicts on women than men, 68,69 often associated with gender-based violence. 70
The mental health burden among children and adolescents has been documented among child soldiers 71 and among those exposed to conflict. Inter-generational effects of armed conflicts are also a major concern, due to, for instance, increased levels of family violence and breakdown of family structures. 72 Sexual and domestic violence have been documented as further precipitating factors of mental health problems in children and adolescents. 73 Caregiver mental health issues such as maternal depression and post-traumatic stress are associated with poorer psychosocial outcomes of conflict-affected children. 74 However, there are major data gaps on the effect of conflict on, for instance, depression among children and adolescents. 75
Sexual and reproductive health
Conflict and displacement leave women and children vulnerable to sexual violence, early marriage, harassment, isolation, and exploitation. 8 A review of 19 studies 76 estimated that 21% of displaced women experienced sexual violence, which is possibly an underestimate because of social stigma, poor law enforcement systems, and inadequate services. There was considerable variation in reports of sexual violence between conflicts, and the overall extent is difficult to document given the lack of standardised definitions (and definitions that may be influenced by cultural factors). 77 Intimate partners are the most common perpetrators in general and there is some evidence of increased risk of intimate partner violence during conflicts. 78 Sexual and gender-based violence has major effects on physical and mental health, including injuries from rape, HIV, reproductive health problems, and social isolation. 79,80 Previous analyses have also shown that maternal mortality is increased by 11% on average and 28% in relatively more intense conflicts, compared with conflict-free periods. 29
Fertility in conflict settings might decrease because of demographic changes (reduced frequency of marriages and spousal separation) and biological effects (reduced fecundity or increased abortion). 31 Conversely, reduced access to modern contraceptives and increased sexual violence might increase the number of unintended pregnancies and abortions. Studies have shown a decrease in fertility during the active phase of conflict. For instance, in Cambodia, fertility decreased by about a third from pre-civil war levels during 1975–79. 81 In Angola, Ethiopia, and Eritrea, decreases in fertility were observed in relation to conflicts. 82–84 Common reasons for these fertility decreases were the separation of spouses, reductions in marriage, lower fecundity, and increased risk of spontaneous abortion, especially when famine coexisted. In virtually all of these settings, the decrease in fertility was temporary and a post-conflict rebound of fertility occurred.
A systematic review 85 of adolescent marriage and fertility patterns during conflicts concluded that both increases and decreases in numbers of adolescent marriage have been observed. There was an increase in adolescent marriages during the active phase of conflicts in Palestine, Syria (among refugees in Jordan), Mali, Nepal, and Tajikistan, whereas in other settings (Cambodia, Eritrea, Ethiopia, and Lebanon) adolescent marriage rates decreased. For instance, data from the Jordanian Population and Health Surveys from 2010 and 2015 indicate that the percentage of Syrian girls (<18 years) being married in Jordan increased from 33% in 2010 to 44% in 2015. 86
There is little scientific evidence on the extent to which the demand for family planning methods is affected during conflict, and to what extent this affects fertility in protracted conflicts with large numbers of refugees. The availability of modern family planning in conflicts is often low, and unmet need for family planning tends to be high in conflict settings. 87,88 There is ample evidence of reduced access to maternal and newborn health services, especially for the poorest and least educated women. 89,90
Conclusion
Ample but incomplete evidence exists of the devastating effects of armed conflict on the health of women and children. Our estimate of the number of women and children affected by conflict—more than 630 million in 2017, including over 50 million women and children displaced by conflict—is, at more than 8% of the world’s population, strikingly large. The number of women and children affected by conflict has increased since 2000, partly due to population growth, a stable-to-increasing number of armed conflicts, the urbanisation of conflict, and a growing number of refugees and internally displaced people. The underlying data for estimating displaced and non-displaced population sizes contain uncertainties, although the increasing counts are unambiguous.
Armed conflict increases indirect mortality among children and women. Armed conflict within 50 km of a place of residence increases the risk of death among children and women of childbearing age in a dose– response relationship with conflict intensity. Exposure to conflicts in the highest quartile of intensity increases infants’ risk of death by more than 25%, and the risk of death in women of childbearing age by three times in Africa. As with our estimates of the size of the population affected by conflict, our retrospective computations of mortality consequences from armed conflict are limited by data availability and by the quality of data on exposure to conflict and on mortality recalled through surveys.
Food security is threatened during conflict, and increases in the number of children affected by acute malnutrition are widely documented. Modern-day famines are restricted to countries in conflict. Increased levels of chronic malnutrition in children are also common and more pronounced among children living in the proximity of severe conflict.
Less evidence exists for the effect of conflicts on morbidity from infectious diseases. Eroded water and sanitation capabilities, crowding, mobility, and breakdown of immunisation services putatively increases the risk of contagions. Visible local effects (eg, cholera and typhoid fever) and global effects (eg, polio virus and Ebola virus disease outbreaks) are common concerns in conflict-affected areas. The evidence on NCDs remains limited, but effects on mental health, especially post-traumatic stress disorder, depression, and anxiety disorders have been widely documented. Sexual violence against women and children is common, with variability between conflicts and major challenges in obtaining reliable populationbased data. Data about adolescents, in particular, is sparse to non-existent.
In most conflict-affected areas, data about the health of women and children are inadequate. Although challenges to data collection using traditional surveillance tools are intuitive, such data are urgently needed for contextspecific programming and policy making to mitigate the health consequences of armed conflict on women and children, especially in the context of the changing nature of conflicts.
Supplementary Material
Key messages.
The effects of armed conflicts on the health and mortality of women and children far exceed the effects on those directly affected by the violence in conflicts.
The number of women and children affected by armed conflict has grown steadily since 2000, due to a combination of increasing population sizes, urbanisation of many conflicts, and a steady rate of conflict events around the world. In 2017, at least 630 million women and children—10% of women and 16% of children worldwide— were either displaced by conflict or resided dangerously close to armed conflict events.
Women’s and children’s mortality risk from non-violent causes increases substantially in response to nearby conflict, with more intense and more chronic conflicts leading to greater mortality increases. More than 10 million deaths in children under the age of 5 years, globally, can be attributed to conflict between 1995 and 2015.
The ways in which health can be affected by conflict are protean but systematic evidence is sparse. Existing evidence links conflict to malnutrition, physical injuries, acute and infectious diseases, poor mental health, and poor sexual and reproductive health. However, aside from malnutrition, the evidence is typically localised and of low to moderate quality. Data on adolescents are sparse to non-existent.
Clearer information on the indirect health effects of armed conflicts, including their duration and extent, could greatly aid in the design and implementation of essential interventions for mitigating the harms of armed conflicts.
Acknowledgements
The analysis was supported by a grant from the Centre for Global Child Health at the Hospital for Sick Children, which was partly supported by the Countdown to 2030 for Women’s, Children’s and Adolescents’ Health. The BRANCH consortium (Bridging Research & Action in Conflict Settings for the Health of Women & Children) provided general support for coordinating and convening the authors. No other specific funding was provided for this work.
Footnotes
Contributors
EB and TB were involved in conceptualising the manuscript, collecting the data, and drafting the initial and revised drafts. NA helped with extracting and preparing the information on displaced populations, and in all draft revisions. AL helped with bounding the manuscript scope, with collecting data on adolescents, and in all draft revisions. EBM drafted the initial section on mental health effects of conflict, and in all subsequent draft revisions. EAO was involved in conceptualising and scoping the initial drafts, and in all draft revisions. PHW was instrumental to the conceptual framework in this paper and the Series as a whole, to formulating the principal health impact domains, and to revising the manuscript. SH-N is the geospatial analyst who estimated the number of non-displaced women and children living near armed conflicts, and he carefully edited the methodological portions of the manuscript. REB and ZAB were important for formulating the approach to this paper and in all drafting stages. All authors read and approved the final version of the manuscript.
Declaration of interests
ZAB reports grants from the International Development Research Centre, the Norwegian Agency for Development Cooperation, the Bill & Melinda Gates Foundation, UNICEF, and the Family Larsson-Rosenquist Foundation. All other authors declare no competing interests.
Contributor Information
Eran Bendavid, Center for Population Health Sciences, Division of Primary Care and Population Health, Department of Medicine.
Ties Boerma, Stanford University, CA, USA; Center for Global Public Health, University of Manitoba, Winnipeg, MB, Canada.
Nadia Akseer, Centre for Global Child Health, Hospital for Sick Children SickKids), Toronto, ON, Canada; The Institute for International Programs, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA.
Ana Langer, Women and Health Initiative, Harvard T H Chan School of Public Health, Boston, MA, USA.
Espoir Bwenge Malembaka, Ecole Régionale de Santé Publique, Faculté de Médecine, Université Catholique de Bukavu, Bukavu, DR Congo.
Emelda A Okiro, Population Health Unit, Kenya Medical Research Institute— Wellcome Trust Research Programme, Nairobi, Kenya; Centre for Tropical Medicine and Global Health, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK.
Paul H Wise, Department of Pediatrics.
Sam Heft-Neal, and Center on Food Security and the Environment.
Robert E Black, The Institute for International Programs, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA.
Zulfiqar A Bhutta, Centre for Global Child Health, Hospital for Sick Children SickKids), Toronto, ON, Canada; Centre of Excellence in Women and Child Health and Institute for Global Health and Development, The Aga Khan University, Karachi, Pakistan.
BRANCH Consortium Steering Committee members:
Canada, Pakistan, Switzerland, and USA
References
- 1.UN. Transforming our world: the 2030 Agenda for Sustainable Development. Sustainable Development Knowledge Platform; [accessed Dec 10, 2020]. https://sustainabledevelopment.un.org/post2015/transformingourworld . [Google Scholar]
- 2.Collier P. The bottom billion: why the poorest countries are failing and what can be done about it. Oxford University Press; Oxford: 2008. [Google Scholar]
- 3.Wise PH, Shiel A, Southard N, et al. The political and security dimensions of the humanitarian health response to violent crime. Lancet. 2021 doi: 10.1016/S0140-6736(21)00130-6. published online Jan 24. [DOI] [PubMed] [Google Scholar]
- 4.Uppsala University. UCDP definitions. [accessed Dec 10, 2020]. http://www.pcr.uu.se/research/
- 5.Pinker S. The better angels of our nature: why violence has declined. Viking; New York, NY: 2011. [Google Scholar]
- 6.Wallensteen P. In: Transformations of conflict studies. Stohl M, Lichbach MI, Grabosky P, editors. Routledge; New York, NY: 2017. Wars, civil wars and armed conflict Pattern, trends and analytic paradigms in states and peoples in conflict; pp. 253–75. [Google Scholar]
- 7.Pettersson T, Wallensteen P. Armed conflicts 1946–2014. J Peace Res. 2015;52:536–50. [Google Scholar]
- 8.World Bank. Forcibly displaced: toward a development approach supporting refugees, the internally displaced, and their hosts. 2017. [accessed Dec 10, 2020]. http://documents.worldbank.org/curated/en/104161500277314152/Forcibly-displaced-toward-a-development-approach-supporting-refugees-the-internally-displaced-and-their-hosts .
- 9.Internal Displacement Monitoring Centre. Global Report on Internal Displacement 2019. 2019. May, [accessed Dec 10, 2020]. https://www.internal-displacement.org/global-report/grid2019/
- 10.Internal Displacement Centre. Women and girls in internal displacement. 2020. Mar, [accessed Dec 10, 2020]. https://www.internal-displacement.org/publications/women-and-girls-in-internal-displacement .
- 11.Sarzin ZI. Stocktaking of global forced displacement data. The World Bank; 2017. [accessed Dec 10, 2020]. https://openknowledge.worldbank.org/handle/10986/26183 . [Google Scholar]
- 12.UN Population Division. World Population Prospects: the 2017 revision. UN Department of Social and Economic Affairs; New York, NY: 2017. [Google Scholar]
- 13.Centre for Research on the Epidemiology of Disasters. People affected by conflict: humanitarian needs in numbers. [accessed Dec 10, 2020]. https://www. cred.be/node/1329 .
- 14.Save the Children. Stop the War on Children: protecting children in 21st century conflict. [accessed Dec 10, 2020]. https://www.stopwaronchildren.org/report.pdf .
- 15.Guha-Sapir D, Schlüter B, Rodriguez-Llanes JM, Lillywhite L, Hicks MH. Patterns of civilian and child deaths due to war-related violence in Syria: a comparative analysis from the Violation Documentation Center dataset, 2011–16. Lancet Glob Health. 2018;6:e103–10. doi: 10.1016/S2214-109X(17)30469-2. [DOI] [PubMed] [Google Scholar]
- 16.Wise PH. The epidemiologic challenge to the conduct of just war: confronting indirect civilian casualties of war. Daedalus. 2017;146:139–54. [Google Scholar]
- 17.Boerma T, Tappis H, Saad-Haddad G, et al. Armed conflicts and national trends in reproductive, maternal, newborn and child health in sub-Saharan Africa: what can national health surveys tell us? BMJ Glob Health. 2019;4(suppl 4):e001300. doi: 10.1136/bmjgh-2018-001300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coghlan B, Brennan RJ, Ngoy P, et al. Mortality in the Democratic Republic of Congo: a nationwide survey. Lancet. 2006;367:44–51. doi: 10.1016/S0140-6736(06)67923-3. [DOI] [PubMed] [Google Scholar]
- 19.Hagopian A, Flaxman AD, Takaro TK, et al. Mortality in Iraq associated with the 2003–2011 war and occupation: findings from a national cluster sample survey by the University Collaborative Iraq Mortality Study. PLoS Med. 2013;10:e1001533. doi: 10.1371/journal.pmed.1001533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Afghanistan mortality survey. 2011. [accessed Dec 10, 2020]. https://www.usaid.gov/sites/default/files/documents/1871/Mortality%20Survey%202010.pdf .
- 21.Spagat M, Dougherty J. Conflict deaths in Iraq: a methodological critique of the ORB Survey estimate. Survey Res Methods. 2010;4:3–15. [Google Scholar]
- 22.Checchi F, Testa A, Warsame A, Quach L, Burns R. Estimates of crisis-attributable mortality in South Sudan, December 2013–April 2018: a statistical analysis. 2018. Sep, [accessed Dec 10, 2020]. https://reliefweb.int/report/south-sudan/estimates-crisis-attributable-mortality-south-sudan-december-2013-april-2018 .
- 23.De Gomme O, Guha-Sapir D. Patterns of mortality rates in Darfur conflict. Lancet. 2010;375:294–300. doi: 10.1016/S0140-6736(09)61967-X. [DOI] [PubMed] [Google Scholar]
- 24.Checchi F, Warsame A, Treacy-Wong V, et al. Public health information in crisis-affected populations: a review of methods and their use for advocacy and action. Lancet. 2017;390:2297–23. doi: 10.1016/S0140-6736(17)30702-X. [DOI] [PubMed] [Google Scholar]
- 25.Checchi F. Estimation of population mortality in crisis-affected populations: guidance for humanitarian coordination mechanisms. 2018. [accessed April 29, 2020]. https://www.who.int/health-cluster/resources/publications/LSHTM-Mortality-Estimation-Options-oct2018.pdf .
- 26.Nordenstedt H, Rosling H. Chasing 60% of maternal deaths in the post-fact era. Lancet. 2016;388:1864–65. doi: 10.1016/S0140-6736(16)31793-7. [DOI] [PubMed] [Google Scholar]
- 27.Wagner Z, Heft-Neal S, Bhutta ZA, Black RE, Burke M, Bendavid E. Armed conflict and child mortality in Africa: a geospatial analysis. Lancet. 2018;392:857–65. doi: 10.1016/S0140-6736(18)31437-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.UN Interagency Group on Child Mortality Estimation and UNICEF. Child mortality estimates. [accessed Dec 10, 2020]. https://childmortality.org/#datasets .
- 29.Wagner Z, Heft-Neal S, Wise PH, et al. Women and children living in areas of armed conflict in Africa: a geospatial analysis of mortality and orphanhood. Lancet Glob Health. 2019;7:e1622–31. doi: 10.1016/S2214-109X(19)30407-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gráda CÓ. Famine: a short history. Princeton University Press; Princeton, NJ: 2010. [Google Scholar]
- 31.Newman JL. Famine demography: perspectives from the past and present. 2002. [accessed Dec 10, 2020]. https://onlinelibrary.wiley.com/doi/abs/10.1002/psp.300 .
- 32.World Peace Foundation. Famine trends dataset, tables and graphs. [accessed Dec 10, 2020]. https://sites.tufts.edu/wpf/famine/
- 33.Famine Early Warning System Network. Hunger-related mortality likely as IPC phase 4 outcomes and large-scale assistance needs persist. [accessed Dec 10, 2020]. https://fews.net/sites/default/files/Food_assistance_peak_needs_2019.pdf .
- 34.Young H, Borrel A, Holland D, Salama P. Public nutrition in complex emergencies. Lancet. 2004;364:1899–909. doi: 10.1016/S0140-6736(04)17447-3. [DOI] [PubMed] [Google Scholar]
- 35.Altare C, Guha-Sapir D. The Complex Emergency Database: a global repository of small-scale surveys on nutrition, health and mortality. PLoS One. 2014;9:e109022. doi: 10.1371/journal.pone.0109022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prudhon C, Spiegel PB. A review of methodology and analysis of nutrition and mortality surveys conducted in humanitarian emergencies from October 1993 to April 2004. Emerg Themes Epidemiol. 2007;4:10. doi: 10.1186/1742-7622-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mason JB, White JM, Heron L, Carter J, Wilkinson C, Spiegel P. Child acute malnutrition and mortality in populations affected by displacement in the Horn of Africa, 1997–2009. Int J Environ Res Public Health. 2012;9:791–806. doi: 10.3390/ijerph9030791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Akresh R, De Walque D. Armed conflict and schooling: evidence from the 1994 Rwandan genocide. World Bank Washington; Washington, DC: 2008. [Google Scholar]
- 39.Akresh R, Lucchetti L, Thirumurthy H. Wars and child health: evidence from the Eritrean–Ethiopian conflict. J Dev Econ. 2012;99:330–40. doi: 10.1016/j.jdeveco.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bundervoet T, Verwimp P, Akresh R. Health and civil war in rural Burundi. J Hum Resour. 2009;44:536–63. [Google Scholar]
- 41.Frost A, Boyle P, Autier P, et al. The effect of explosive remnants of war on global public health: a systematic mixed-studies review using narrative synthesis. Lancet Public Health. 2017;2:e286–96. doi: 10.1016/S2468-2667(17)30099-3. [DOI] [PubMed] [Google Scholar]
- 42.McPherson JI. Traumatic brain injury among refugees and asylum seekers. Disabil Rehabil. 2019;41:1238–42. doi: 10.1080/09638288.2017.1422038. [DOI] [PubMed] [Google Scholar]
- 43.Salamati P, Razavi SM, Shokraneh F, et al. Mortality and injuries among Iranians in Iraq-Iran war: a systematic review. Arch Iran Med. 2013;16:542–50. [PubMed] [Google Scholar]
- 44.Iraq Family Health Survey Study Group. Violence-related mortality in Iraq from 2002 to 2006. N Engl J Med. 2008;358:484–93. doi: 10.1056/NEJMsa0707782. [DOI] [PubMed] [Google Scholar]
- 45.Wise PH, Barry M. Civil war & the global threat of pandemics. Daedalus. 2017;146:71–84. [Google Scholar]
- 46.Kimbrough W, Saliba V, Dahab M, Haskew C, Checchi F. The burden of tuberculosis in crisis-affected populations: a systematic review. Lancet Infect Dis. 2012;12:950–65. doi: 10.1016/S1473-3099(12)70225-6. [DOI] [PubMed] [Google Scholar]
- 47.Eiset AH, Wejse C. Review of infectious diseases in refugees and asylum seekers—current status and going forward. Public Health Rev. 2017;38:22. doi: 10.1186/s40985-017-0065-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sharara SL, Kanj SS. War and infectious diseases: challenges of the Syrian civil war. PLoS Pathog. 2014;10:e1004438. doi: 10.1371/journal.ppat.1004438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Griffith DC, Kelly-Hope LA, Miller MA. Review of reported cholera outbreaks worldwide, 1995–2005. Am J Trop Med Hyg. 2006;75:973–77. [PubMed] [Google Scholar]
- 50.Qadri F, Islam T, Clemens JD. Cholera in Yemen—an old foe rearing its ugly head. N Engl J Med. 2017;377:2005–07. doi: 10.1056/NEJMp1712099. [DOI] [PubMed] [Google Scholar]
- 51.Spiegel PB, Bennedsen AR, Claass J, et al. Prevalence of HIV infection in conflict-affected and displaced people in seven sub-Saharan African countries: a systematic review. Lancet. 2007;369:2187–95. doi: 10.1016/S0140-6736(07)61015-0. [DOI] [PubMed] [Google Scholar]
- 52.Rubin R. For Nobel Peace Prize winner Dr Denis Mukwege, his patients motivate and inspire. JAMA. 2019;321:19–21. doi: 10.1001/jama.2018.18199. [DOI] [PubMed] [Google Scholar]
- 53.Omare D, Kanekar A. Determinants of HIV/AIDS in armed conflict populations. J Public Health Afr. 2011;2:e9. doi: 10.4081/jphia.2011.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Garon JR, Orenstein WA. Overcoming barriers to polio eradication in conflict areas. Lancet Infect Dis. 2015;15:1122–24. doi: 10.1016/S1473-3099(15)00008-0. [DOI] [PubMed] [Google Scholar]
- 55.Bhutta ZA. Conflict and polio: winning the polio wars. JAMA. 2013;310:905–06. doi: 10.1001/jama.2013.276583. [DOI] [PubMed] [Google Scholar]
- 56.Ado JM, Etsano A, Shuaib F, et al. Progress toward poliomyelitis eradication in Nigeria. J Infect Dis. 2014;210(suppl 1):S40–49. doi: 10.1093/infdis/jiu318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Claude KM, Underschultz J, Hawkes MT. Ebola virus epidemic in war-torn eastern DR Congo. Lancet. 2018;392:1399–401. doi: 10.1016/S0140-6736(18)32419-X. [DOI] [PubMed] [Google Scholar]
- 58.Abera WK. Outbreak investigation of suspected hepatitis E among South Sudan refugees, Gambella regional state, Ethiopia, July 2014. Int J Infect Dis. 2016;45:428. [Google Scholar]
- 59.Ochola E, Ocama P, Orach CG, et al. High burden of hepatitis B infection in Northern Uganda: results of a population-based survey. BMC Public Health. 2013;13:727. doi: 10.1186/1471-2458-13-727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Spiegel PB, Checchi F, Colombo S, Paik E. Health-care needs of people affected by conflict: future trends and changing frameworks. Lancet. 2010;375:341–45. doi: 10.1016/S0140-6736(09)61873-0. [DOI] [PubMed] [Google Scholar]
- 61.Levy BS, Sidel VW. Documenting the effects of armed conflict on population health. Annu Rev Public Health. 2016;37:205–18. doi: 10.1146/annurev-publhealth-032315-021913. [DOI] [PubMed] [Google Scholar]
- 62.Levy BS, Sidel VW. Health effects of combat: a life-course perspective. Annu Rev Public Health. 2009;30:123–36. doi: 10.1146/annurev.publhealth.031308.100147. [DOI] [PubMed] [Google Scholar]
- 63.Demaio A, Jamieson J, Horn R, de Courten M, Tellier S. Non-communicable diseases in emergencies: a call to action. PLoS Curr. 2013;5:ecurrents.dis.53e08b951d59ff913ab8b9bb51c4d0de. doi: 10.1371/currents.dis.53e08b951d59ff913ab8b9bb51c4d0de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Attanayake V, McKay R, Joffres M, Singh S, Burkle F, Jr, Mills E. Prevalence of mental disorders among children exposed to war: a systematic review of 7,920 children. Med Confl Surviv. 25:4–19. doi: 10.1080/13623690802568913. [DOI] [PubMed] [Google Scholar]
- 65.Slone M, Mann S. Effects of war, terrorism and armed conflict on young children: a systematic review. Child Psychiatry Hum Dev. 2016;47:950–65. doi: 10.1007/s10578-016-0626-7. [DOI] [PubMed] [Google Scholar]
- 66.Dimitry L. A systematic review on the mental health of children and adolescents in areas of armed conflict in the Middle East. Child Care Health Dev. 2012;38:153–61. doi: 10.1111/j.1365-2214.2011.01246.x. [DOI] [PubMed] [Google Scholar]
- 67.Charlson F, Ommeren van M, Flaxman A, Cornett J, Whiteford H, Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet. 2019;394:240–48. doi: 10.1016/S0140-6736(19)30934-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rugema L, Mogren I, Ntaganira J, Krantz G. Traumatic episodes and mental health effects in young men and women in Rwanda, 17 years after the genocide. BMJ Open. 2015;5:e006778. doi: 10.1136/bmjopen-2014-006778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Silove D, Liddell B, Rees S, et al. Effects of recurrent violence on post-traumatic stress disorder and severe distress in conflict-affected Timor-Leste: a 6-year longitudinal study. Lancet Glob Health. 2014;2:e293–300. doi: 10.1016/S2214-109X(14)70196-2. [DOI] [PubMed] [Google Scholar]
- 70.Dossa NI, Zunzunegui MV, Hatem M, Fraser WD. Mental health disorders among women victims of conflict-related sexual violence in the Democratic Republic of Congo. J Interpers Violence. 2015;30:2199–220. doi: 10.1177/0886260514552447. [DOI] [PubMed] [Google Scholar]
- 71.Kohrt BA, Jordans MJD, Tol WA, et al. Comparison of mental health between former child soldiers and children never conscripted by armed groups in Nepal. JAMA. 2008;300:691–702. doi: 10.1001/jama.300.6.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Devakumar D, Birch M, Osrin D, Sondorp E, Wells JC. The intergenerational effects of war on the health of children. BMC Med. 2014;12:57. doi: 10.1186/1741-7015-12-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lokuge K, Shah T, Pintaldi G, et al. Mental health services for children exposed to armed conflict: Médecins Sans Frontières’ experience in the Democratic Republic of Congo, Iraq and the occupied Palestinian territory. Paediatr Int Child Health. 2013;33:259–72. doi: 10.1179/2046905513Y.0000000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Betancourt T, Khan KT. The mental health of children affected by armed conflict: protective processes and pathways to resilience. Int Rev Psychiatry. 2008;20:317–28. doi: 10.1080/09540260802090363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dardas LA, Bailey DE, Jr, Simmons LA. Adolescent depression in the Arab region: a systematic literature review. Issues Ment Health Nurs. 2016;37:569–85. doi: 10.1080/01612840.2016.1177760. [DOI] [PubMed] [Google Scholar]
- 76.Vu A, Adam A, Wirtz A, et al. The prevalence of sexual violence among female refugees in complex humanitarian emergencies: a systematic review and meta-analysis. PLoS Curr. 2014;6:ecurrents.dis.835f10778fd80ae031aac12d3b533ca7. doi: 10.1371/currents.dis.835f10778fd80ae031aac12d3b533ca7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Messner N, Woods A, Petty A, et al. Qualitative evidence of crimes against humanity: the August 2017 attacks on the Rohingya in northern Rakhine State, Myanmar. Confl Health. 2019;13:41. doi: 10.1186/s13031-019-0227-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C. Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. Lancet. 2008;371:1165–72. doi: 10.1016/S0140-6736(08)60522-X. [DOI] [PubMed] [Google Scholar]
- 79.Spangaro J, Adogu C, Ranmuthugala G, Davies GP, Steinacker L, Zwi A. What evidence exists for initiatives to reduce risk and incidence of sexual violence in armed conflict and other humanitarian crises? A systematic review. PLoS One. 2013;8:e62600. doi: 10.1371/journal.pone.0062600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Stark L, Ager A. A systematic review of prevalence studies of genderbased violence in complex emergencies. Trauma Violence Abuse. 2011;12:127–34. doi: 10.1177/1524838011404252. [DOI] [PubMed] [Google Scholar]
- 81.de Walque D. The socio-demographic legacy of the Khmer Rouge period in Cambodia. Popul Stud (Camb) 2006;60:223–31. doi: 10.1080/00324720600684767. [DOI] [PubMed] [Google Scholar]
- 82.Agadjanian V, Prata N. War, peace, and fertility in Angola. Demography. 2002;39:215–31. doi: 10.1353/dem.2002.0013. [DOI] [PubMed] [Google Scholar]
- 83.Lindstrom DP, Berhanu B. The impact of war famine, and economic decline on marital fertility in Ethiopia. Demography. 1999;36:247–61. [PubMed] [Google Scholar]
- 84.Blanc AK. The role of conflict in the rapid fertility decline in Eritrea and prospects for the future. Stud Fam Plann. 2004;35:236–45. doi: 10.1111/j.0039-3665.2004.00028.x. [DOI] [PubMed] [Google Scholar]
- 85.Neal S, Stone N, Ingham R. The impact of armed conflict on adolescent transitions: a systematic review of quantitative research on age of sexual debut, first marriage and first birth in young women under the age of 20 years. BMC Public Health. 2016;16:225. doi: 10.1186/s12889-016-2868-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hikmat R. Child marriage in Jordan policy brief. [accessed Dec 18, 2020]. https://reliefweb.int/report/jordan/policy-brief-child-marriage-jordan-2017 .
- 87.McGinn T, Austin J, Anfinson K, et al. Family planning in conflict: results of cross-sectional baseline surveys in three African countries. Confl Health. 2011;5:11. doi: 10.1186/1752-1505-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ivanova O, Rai M, Kemigisha E. A systematic review of sexual and reproductive health knowledge, experiences and access to services among refugee, migrant and displaced girls and young women in Africa. Int J Environ Res Public Health. 2018;15:1583. doi: 10.3390/ijerph15081583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gopalan SS, Das A, Howard N. Maternal and neonatal service usage and determinants in fragile and conflict-affected situations: a systematic review of Asia and the Middle-East. BMC Womens Health. 2017;17:20. doi: 10.1186/s12905-017-0379-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Akseer N, Wright J, Tasic H, et al. Women, children and adolescents in conflict countries: an assessment of inequalities in intervention coverage and survival. BMJ Glob Health. 2020;5:e002214. doi: 10.1136/bmjgh-2019-002214. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.