Abstract
Young people aged 10-24 years constitute 24% of the world’s population and investing in their health could yield a “triple benefit”: today, into adulthood, and for the next generation. However, in physical activity research this life stage is poorly understood with the evidence dominated by research in younger adolescents (10-14yr), school settings and high-income countries. Globally, 80% of adolescents are insufficiently active, and many engage in ≥2hrs of daily recreational screen time. This paper presents the most up-to-date global evidence on adolescent physical activity and discusses directions for identifying potential solutions to enhance physical activity levels in this population. Adolescent physical inactivity likely contributes to key global health problems, including cardio-metabolic and mental health disorders, but the evidence is methodologically weak. Evidence-based solutions focus on three key components of the adolescent physical activity system: (i) supportive schools, (ii) the social and digital environment, and (iii) multi-utility urban environments. Despite an increasing volume of research focused on adolescents, important knowledge gaps remain and efforts to improve adolescent physical activity surveillance, research, intervention implementation, and policy development are urgently needed.
Introduction
Young people aged 10-24 years constitute 24% of the world’s population.1 This includes, as per the Lancet Commission on Adolescent Health and Wellbeing,2 younger adolescents (10-14 years), older adolescents (15-19 years), and young adults (20-24 years), and will be referred to as such throughout this paper.3 Both the Lancet Commission2 and the Global Accelerated Action for the Health of Adolescents (AA-HA!)4 concluded that investing in adolescent health and wellbeing will yield a “triple benefit” – today, into adulthood, and for the next generation.2 While adolescence is generally considered a healthy period, many non-communicable diseases (NCDs) that manifest later are in part the result of modifiable risk behaviours established during this time, such as smoking, unhealthy diet patterns, and low levels of physical activity.5,6 There have been major global trends in adolescent health in recent decades.7 Notably, while a decrease in adolescent disease burden has been observed in many countries over the last 25 years, almost one in five (324 million [18%]) adolescents globally now have overweight or obesity7 and there is an increasing burden of adolescent mental health disorders (including depression and anxiety).8,9 It is estimated that 962·8 million adolescents (53% globally) now live in multi-burden countries, where they face a “triple burden” of health problems, including infectious diseases, injury and violence, and NCDs.7 Increased efforts to develop a better understanding of, and potential solutions to, health and well-being during adolescence are therefore encouraged.2,4,10,11 To support these efforts, The Lancet launched the “2020 Campaign on child and adolescent health”.12
Physical inactivity is associated with many NCDs and substantial economic costs on a global scale.13,14 It has been estimated to account for 5·3 million deaths per year,13 and to cost at least $54 billion in direct health care costs of which $31 billion is paid by the public sector.14 Although physical inactivity is recognized as a global pandemic,15 much of the evidence has come from studies among adults,13,16,17 when the effects on NCDs become apparent.18 Recent evidence, however, suggests marked increases in the prevalence of NCDs (e.g. type 2 diabetes)19 and NCD risk factors including hypertension20 and obesity21 in adolescence. Acknowledging the health risks of long-term neglect of adolescent health and wellbeing, the Lancet Commission on Adolescent Health and Wellbeing2 was launched in 2016, which proposed 12 headline to track progress in adolescent health. However, despite the known health risks of physical inactivity across the life course13,17,22 and alarmingly low levels of physical activity,23 no indicator related to physical activity was included. Therefore, physical activity appears to have low priority in adolescent health. It is crucial and timely to refocus the global prevention agenda in adolescence to include physical activity.
It is critical that we develop a better understanding of adolescent physical activity such that effective strategies can be implemented. The implementation of policies and interventions to promote physical activity has the potential to contribute to achieving many of the United Nations’ Sustainable Development Goals (SDGs) for 2030.24 The World Health Organization’s (WHO) Global Action Plan on Physical Activity 2018-203025 and an investigation in the current series26 demonstrate how the promotion of physical activity can help achieve multiple SDGs. Beyond its direct contribution to SDG-3 (good health and wellbeing),25 “co-benefits” of adolescent physical activity promotion include contributions to SDG-5 (gender equality) and, based on the increasing evidence linking physical activity to academic performance27,28 and the critical role of physical education in high quality education, SDG-4 (quality education). This paper provides an overview of up-to-date evidence on adolescent physical activity behaviours, including prevalence, determinants and consequences, and provides recommendations for action in research and practice. The term “physical activity behaviours” is used to capture both physical activity and sedentary behaviour; where evidence is specific to a type of behaviour this is indicated.
Adolescence and young adulthood: A period of transition
Adolescence is a key period of human development, as psychological and biological changes occur rapidly during this phase of life.4,6 Adolescence and young adulthood represent a significant transition in responsibilities and lifestyles in many cultures as young people shift from school settings to a variety of different pathways, including higher education, family, military, workforce, or unemployment. It is important to be mindful of the global variation in the timings of these pathways. For example, the proportion of adolescents globally not in educational settings is 15·9% in 12-14-year-olds and 36·3% in 15-17-year olds, but figures are as high as 36·6% and 57·8%, respectively, in Sub-Saharan Africa.29
In Western countries, young adulthood is characterized by great variability in demographics (income, housing, etc.), self-perceptions, identity exploration, and increased participation in risk behaviours.11,30 Globally, the age of achieving biological maturation is decreasing.31,32 At the same time, the age of attaining several “adult” milestones has risen in high-income countries (HICs) (e.g. age of first marriage,33 mother’s age at first birth,34 and age of completing education35). It is unclear if these social trends are mirrored, at least to some extent, in low-and-middle-income countries (LMICs), although global evidence suggests that the prevalence of early marriage36 and early childbearing37 have been declining over the past three decades. This expanding period of instability, key life transitions and increasing responsibilities represents an important period where decision-making autonomy increases and lifestyle habits, including physical activity, become established and entrenched, and thereby offers significant opportunities for interventions that can have life-long and inter-generational health implications.38–40
Are physical inactivity and sedentary behaviour problems in adolescence?
Physical activity
The WHO recommends that children and adolescents aged <18 years accumulate at least an average of 60 minutes per day of moderate-to-vigorous intensity physical activity, whereas people aged ≥18 years should accumulate at least 150-300 minutes of moderate-intensity physical activity or 75-150 minutes of vigorous-intensity physical activity per week, or an equivalent combination.41 Similar guidelines have been adopted by many countries across the WHO regions worldwide. The discrepancy reflects the different evidence bases used to develop public health guidelines. In adults, a major focus has been on the prevention of NCDs and premature mortality, while the focus in childhood and adolescence has been on improving fitness, developing coordination and movement control, and maintaining a healthy body weight. It appears unlikely that the dose of physical activity at which health benefits occur changes so dramatically at age 18 years but, as described later, the evidence base to inform quantitative health-related physical activity thresholds over this age range is sparse. This is an important area for future research.
This drastic shift in the recommended levels of physical activity for individuals aged 18 and above also impacts the ability to adequately monitor trends in physical activity compliance across the whole adolescent and young adult age range. For example, global surveillance data indicate that approximately 20% of under-18s, but 73% of adults (≥18 years), are classified as sufficiently active.42,43 Overall, global data availability is strongest for adolescents attending school. A recent analysis of data of 1·6 million students from 146 countries, territories, and areas,43 has provided an update on the physical activity prevalence data presented in the first Lancet Physical Activity series.23 Using self-reported data, it showed that in 2016, 81·0% of 11-17-year-olds were physically inactive, with a lower prevalence in boys compared to girls (77·6% vs. 84·7%, respectively). This constituted a slightly decreased prevalence of physical inactivity for boys (from 80·1% in 2001), but negligible change for girls (from 85·1% in 2001). There was no clear pattern according to country income group. Although within-country socio-economic differences could not be established, wider evidence suggests that these may operate differently across the globe: in HICs the association is equivocal, whereas in Brazil, for example, those from low socio-economic backgrounds have been shown to be more active overall.44,45 Sources of physical activity also differ, with work/household physical activity contributing more to overall adult physical activity in LMICs, and leisure physical activity contributing more in HICs.46 The collection of comparable and detailed physical activity data across countries is difficult, given, for example, country-level differences in seasonal variation and school attendance.
Monitoring absolute levels of activity, as opposed to guideline compliance, may provide a better representation of differences in physical activity across the adolescent and young adult age range. Although it can be estimated based on self-report measures, there is a growing list of countries and regions that have begun monitoring physical activity levels using pedometers and accelerometers (Panel 1). Figure 1 presents accelerometry data from American and European 10-24-year-olds. This shows that males are consistently more active than females, and a clear trend for decreasing physical activity with advancing age in early and late adolescence. Levels of physical activity, however, become more stable in young adulthood. This is supported by evidence that activity levels track reasonably well from adolescence into adulthood.47 Although the mechanisms through which tracking occurs are not well known (e.g., habit formation, early experience and skill development, or self-selection), it emphasises the importance of including a focus on adolescence in physical activity promotion for public health. Figure 1 also demonstrates the critical influence of the changing guidelines on our understanding of physical activity prevalence across adolescence and young adulthood; median values are generally below recommended levels for adolescents, but above recommended levels for adults.
Panel 1. Progress and challenges with physical activity surveillance in adolescents.
Increasing physical activity surveillance in adolescents
There has been a substantial increase in the number of countries with self-reported physical activity surveillance data for adolescents since the 2012 Lancet Physical Activity Series. Data from 105 countries were available for the 2012 report, compared to 120 countries in 2016, and 146 countries in the latest report.
-
Several countries are now integrating device-based measures of physical activity into their population surveillance systems. Some examples of device-based surveillance among adolescents include:
-
○
Canada has used accelerometers to measure physical activity in the Canadian Health Measures Survey annually since 2007.
-
○
The U.S. included accelerometers in the National Health and Nutrition Examination Survey in 2003-06 (waist worn), and again in 2011-14 (wrist worn).
-
○
Australia included pedometers in the Australian Health Survey in 2011-12.
-
○
Malta used accelerometers to measure physical activity in a nationally representative sample of adolescents in 2012.
-
○
Portugal used accelerometers to measure physical activity in a nationally representative sample of adolescents in 2006-08.
-
○
In Norway, accelerometers were used to measure physical activity in nationally representative samples of adolescents in three waves of data collection between 2005-2017.
-
○
Challenges and recommendations
The age span of 10 to 24 years encompasses two sets of aerobic physical activity guidelines (an average of 60 minutes daily up to age 17 years; 150 minutes per week for ages 18 years and over), making comparisons of proportions meeting guidelines problematic. There is no scientific reason why the dose of physical activity at which health benefits occur changes so dramatically at age 18. Strengthening the scientific evidence base upon which to identify quantitative health-related physical activity thresholds during the transition between adolescence and young adulthood is therefore an important area for future research.
Adolescent physical activity surveillance would benefit from the use of a combination of self-report and device-based assessment. This should consist of repeated cross-sectional surveys at a minimum every five years, conducted throughout the year to account for seasonal variations. Reporting of data should support the monitoring of progress towards reducing inequalities in participation in physical activity (such as by age, sex, geographical location and socio-economic status).
Current surveillance efforts rely on a variety of self-report questionnaires and devices, making comparison across countries and regions difficult. Moreover, collection of physical activity data across the entire year to account for seasonal variation is complicated by school attendance (versus not) which differs from country to country. Harmonisation of questionnaires and the development of algorithms to generate comparable estimates is paramount.
Data from low income countries continue to be scarce: only 8 (26%) out of 31 low-income countries contributed self-reported adolescent physical activity data to the latest report. Nationally representative device-based physical activity data are non-existent from low-income countries. Efforts should focus on improving surveillance globally.
The vast majority of self-reported surveillance data captures adolescents attending secondary school. Surveillance data of those not in schools is generally lacking, and methods to capture this population should be developed.
Physical activity surveillance should capture domain- and type-specific information to inform interventions. Data on specific aspects of adolescent physical activity, such as sports and walking or cycling for transport, are currently inconsistent and often not comparable across countries, yet important for physical activity promotion.
Surveillance of screen use has typically focussed on TV viewing and computer use. As the ways in which adolescents interact with screens is changing rapidly, surveys now need to incorporate more contemporary indicators capturing the multitude of ways in which adolescents use screens.
The use of different intensity cut-points across age when analysing device-based physical activity data makes comparisons across age and between studies difficult. Comparison between studies is further complicated by different wear protocol and data processing decisions, and we encourage the increased use and sharing of raw accelerometer data to enable such comparison.
Figure 1. Overall physical activity (expressed as total activity counts) from accelerometry in U.S. and European males and females from 10 to 24 years of age.
Note: Data for U.S. males (blue) and females (red) are smoothed 50th percentiles from NHANES 2003-2006. Data for European males (grey) and females (yellow) are age-specific median values from the Determinants of Diet and Physical Activity Knowledge Hub (DEDIPAC). Dotted lines indicate the estimated total activity counts associated with the adolescent guidelines (60 mins/day) and young adult guidelines (150 mins/week). See appendix 1 for methodological details.
Sedentary behaviour
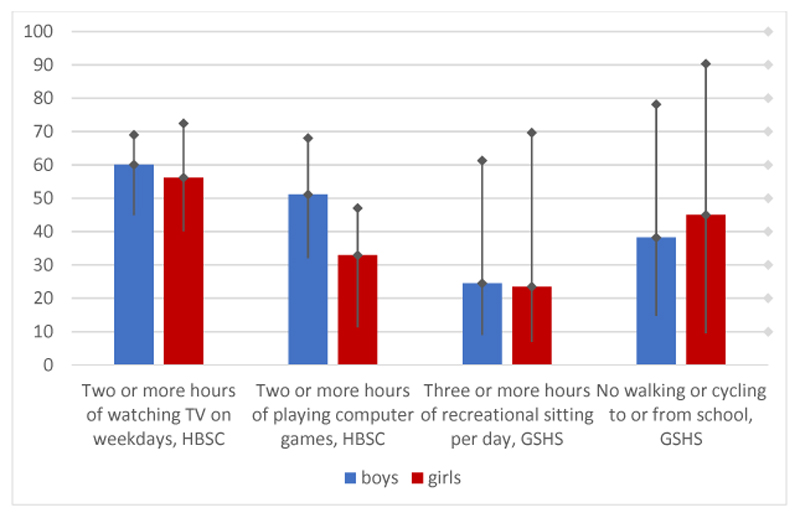
Over the past decade, time spent sitting and reclining while expanding little energy (sedentary behaviour) and engagement in specific sedentary activities (such as screen-based behaviours) have rapidly emerged as potential additional risk factors for adolescents’ health and well-being.48,49 The WHO does not provide quantitative guidelines for sedentary time.41 However, country-specific guidelines have been developed. For example, Australia and Canada recommend <2 hours recreational screen time per day for under-18s,50,51 and the UK recommends that all citizens “minimize the time spent sedentary”.52 These variations together with evidential uncertainties complicate global surveillance of sedentary behaviour. Self-reported global surveillance data on sedentary behaviour are available for adolescents in two large international school-based surveys: the Health Behaviour in School-Aged Children (HBSC) survey and the Global School-based Student Health Survey (GSHS) (details on methods and results: Appendix 2). Across the 97 countries with information on sitting in GSHS, 25% of boys and 24% of girls aged 13-15 years reported sitting for >3 hours per day in addition to sitting at school and for homework (Figure 2). Although the prevalence was similar across low-, lower-middle, and upper-middle income countries, it was twice as high for boys and girls from HICs as compared to all other income groups. Country prevalence ranged from 9% (Pakistan) to 61% (Kuwait) among boys, and from 7% (Pakistan) to 70% (Barbados) among girls.
Figure 2. Prevalence of watching TV (HBSC, 37 countries); playing computer games (HBSC, 38 countries); recreational sitting (GSHS, 97 countries); and no walking or cycling to or from school (GSHS, 73 countries).
Note: Data shows prevalence with minimum and maximum country values. HSBC data is from 2014, GSHS data from 2003-2017. See Appendix 2 for methodological details.
In recent years, the ways in which adolescents interact with screens has changed rapidly, posing a challenge for global surveillance of screen-based behaviour. For example, while TV viewing was the main source of US adolescents’ screen-time in the late 1970s, in 2016 it only represented 25% of their overall screen use.53 This indicates that TV viewing and computer use may no longer be appropriate metrics for sedentary behaviour surveillance and that we need more contemporary indicators capturing the multitude of ways in which adolescents use screens. Nevertheless, we drew on the most recent data on adolescent screen use from a range of countries to present prevalence. HBSC assessed TV use and playing computer/video games in up to 38 European countries (Appendix 2). The prevalence of 11-15-year-olds watching TV for ≥2 hours on weekdays was 60% for boys and 56% for girls (Figure 2). Country prevalence ranged from 45% (Switzerland) to 69% (United Kingdom, Wales) among boys, and from 40% (Switzerland) to 72% (Bulgaria) among girls. Prevalence of playing computer/video games for ≥2 hours on weekdays was 51% for boys and 33% for girls, ranging from 32% (Switzerland) to 68% (Denmark) for boys, and from 11% (Finland) to 47% (Netherlands) for girls. Prevalence of both behaviours was consistently higher for boys than girls, but was similar across country income groups. However, as with physical activity, the socio-economical patterning of screen use varies by country context, as demonstrated by a review identified in our umbrella review of correlates and determinants (Appendix 5).54 Specifically, whereas in HICs adolescents from high socioeconomic backgrounds are less likely to engage in high levels of screen-based behaviour, in LMICs it is the reverse. This demonstrates the importance of context in identifying problems and solutions.
Health consequences of adolescent physical activity behaviours
These high levels of adolescent inactivity and sedentary behaviour come with short- and long-term consequences for health and wellbeing. There is large variation in the consequences considered important to different stakeholders. Whereas evidence on reducing morbidity and health care cost may appeal to health professionals and policy makers, academic performance and mental health may be a priority for educators and parents, while wellbeing, social integration and having fun are more salient for adolescents.55 In order to instigate action at a variety of levels, high-quality evidence across this broad range of outcomes is required to achieve positive change at individual, population, and systems levels. For example, while evidence of the importance of physical activity for NCD prevention may help push physical activity promotion up the policy agenda, it is unlikely adolescents will change their behaviour for the benefit of distal health consequences. The more immediate benefits of physical activity are likely to be more relatable to adolescents.
The prevalence of obesity increases rapidly during adolescence and young adulthood.56 Its causes are complex and multifactorial, but evidence suggest prevention is critical as adolescents with overweight or obesity are unlikely to improve their weight status as they progress into young adulthood.57 Physical activity and sedentary behaviour are considered cornerstones for preventing unhealthy weight gain, with extensive review level evidence available.58 The magnitude of the associations between adolescent sedentary behaviours and adiposity are very small to small and there is limited evidence that the association is causal59 or independent from physical activity.60 Intuitively, higher levels of physical activity prevent gains in adiposity. However, the association is likely to be bi-directional (i.e. high body weight leading to lower physical activity levels).61 To understand and prevent a potentially vicious cycle of increasing body weight and decreasing activity behaviour and whether weight loss might lead to increases in activity, future research should establish a firm understanding of the causal association between physical activity (of different volumes and intensity) and unhealthy weight gain in adolescence.62
To establish the relationship between adolescent physical activity and less frequently studied later cardio-metabolic health outcomes, we systematically reviewed the literature assessing the prospective associations (where assessment of the physical activity behaviour preceded the outcome) with blood pressure, type 2 diabetes and the metabolic syndrome (Appendix 3 for details on methods and results). Only one study examined the association between physical activity in adolescence and type 2 diabetes in adulthood and found no association. Within adolescence and young adulthood (outcome measured at ≤24 years), the evidence for an association between physical activity and the metabolic syndrome and blood pressure was equivocal. The evidence was somewhat stronger for outcomes measured in adulthood (>24 years), with some evidence of a long-term negative association between physical activity and the metabolic syndrome, but not with blood pressure. Physical activity and sedentary behaviours during adolescence may be associated with some medium- and long-term cardio-metabolic health outcomes but the strength of the current evidence is generally low.
Mental health problems are a growing global public health concern in adolescence.8 Trial-based evidence suggests that physical activity appears to be a promising intervention for those experiencing depression.63 Many mental health problems have their origins in adolescence, and the role of physical inactivity in its development is poorly understood with a range of neurobiological, psychosocial and behavioural pathways hypothesised.64 Cross-sectional studies are problematic due to the hypothesised bi-directional association between mental health and physical activity, with evidence suggesting that mental health problems likely lead to decreases in physical activity and increases in sedentary behaviour.65 We reviewed the literature assessing prospective associations with anxiety and depression in generally healthy adolescents (Appendix 4 for details on methods and results). The results suggest that there is consistent evidence for a lack of prospective association between adolescent physical activity and later symptoms of depression and anxiety, but that the association with sedentary time is more equivocal. These findings may be due to the lack of measurement precision in both the outcome and exposure, and the small effect sizes expected in a generally healthy population. Indeed, a recent large-scale study in Lancet Psychiatry showed that an additional hour per day of accelerometer-assessed sedentary time in early adolescence was associated with an 8–11% increase in depression scores at age 18 years.49 Higher physical activity was negatively associated with later depressive symptoms. These positive findings need to be interpreted cautiously as the benefits may be difficult to achieve; compared to baseline levels, they would require a 14% decrease in sedentary time or a 57% increase in time spent in physical activity, whereas a 22% increase and no change were observed over the 4-year follow-up, respectively.
It is important to note that sedentary behaviour has predominantly been operationalised as engagement in ‘traditional’ screen-based behaviours. Given the radical shift in the way adolescents interact with screens, there is a need for an improved understanding of the generalisability of these research findings to the present generation. Moreover, a more sophisticated approach to studying screen-based behaviours and their impact on adolescent health and well-being may be warranted, including differentiating between ‘quantity’ and ‘quality’ of behaviours and their importance for health. Recent adult-based research suggests that mentally-passive sedentary behaviours (requiring minimal mental demands, e.g. TV-viewing, listening to music) are associated with a higher risk for depression, but not mentally-active behaviours (which increase mental demands, e.g. reading, video gaming).66 This suggests that not all minutes spent sedentary are equal, and importance of this for adolescent health requires further exploration.
In summary, physical activity behaviours in adolescence may be associated with some medium- and long-term health outcomes, but the evidence base is generally weak. These findings, however, should be interpreted in light of the various limitations of the available evidence: the overall scarcity and lack of global representation of evidence, self-reported exposures, small sample sizes due to attrition, and imperfectly measured or unmeasured confounders. Further high-quality research is urgently needed to strengthen the case for investment in adolescent physical activity behaviours to prevent health problems. This will require large sample sizes, device-based exposure measurement, follow-up within and beyond adolescence, appropriate assessment of confounders, and robust analytical approaches with pre-specified sub-group analyses to establish causality.
Inactive adolescents: correlates, determinants and potential solutions
For decades, research has been dedicated to understanding why some people are more active than others.67 Such inquiry regarding the correlates and determinants of physical activity behaviours aims to identify subpopulations at risk and understand the modifiable causes of inactivity to inform intervention efforts. Meanwhile, interventions have been tested around the world to identify potential solutions to physical inactivity, with variable success.68 Recently, physical inactivity has been recognised as a “wicked problem”, created and perpetuated by the complex system within which it occurs.69 As such, identifying solutions requires researchers not to ask whether an intervention ‘works’, but to identify if and how it contributes to reshaping a system favourably.70 This paradigm shift led the WHO to adopt a systems framework for their recent Global Physical Activity Action Plan,25 which aspires to create active societies, environments, people, and systems.71 Here, we aim to summarise the current literature on the correlates, determinants and interventions with an acknowledgement of the complexity of these issues and the biological and broader social and commercial determinants of health in which they operate and with which they interact. We focus on three key components of the adolescent physical activity system: (i) schools and educational settings, which are particularly important channels and locations for adolescent physical activity promotion, (ii) the social and digital environment, which offers both challenges and potential for behaviour change, and (iii) the urban environment, which is increasingly recognised as a critical and “upstream” strategy to tackling population-level physical inactivity.
The role of schools and other educational settings
Across the globe, schools are considered an important avenue to health promotion, reaching adolescents largely irrespective of their background characteristics. In recognition, WHO and UNESCO recently launched global standards to support their initiative “Making Every School a Health Promoting School”.72 School-based interventions also dominate the adolescent physical activity promotion literature. To better understand the opportunities and challenges this setting provides, we draw on the school-based evidence from our umbrella reviews on correlates and determinants of physical activity behaviours and on interventions to change physical activity behaviours (Panel 2; Appendix 5 and 6 for details on methods and results). Our umbrella review of correlates and determinants identified four reviews considering aspects of the school’s policy, social or physical environment.73–76 Together, this evidence suggests that the availability of within-school sports and activity in specific school areas was positively associated with overall adolescent physical activity. In contrast, access to sports equipment, adult supervision, overall teacher support, and quantity of physical education (PE) provision were not associated with adolescents’ physical activity levels. Of note, the most active PE classes were those that fostered a mastery climate (i.e., focusing on individual/team development rather than competition), were conducted outdoors and included team games. PE and after school sport provision are key vehicles for schools to contribute to physical activity promotion. The evidence suggests that the quality and content of these provisions, in addition to the absolute quantity, are critical. Specifically, offering within-school sports competitions and outdoor PE, and fostering of a mastery-focussed motivational climate in PE appear to be salient targets for schools.77 High quality sport and PE programs are needed to develop adolescents’ physical literacy78 and provide opportunities to develop lifelong physical activity skills to facilitate ‘physical activity independence’79 and long-term enjoyment, although they may not necessarily translate into higher overall activity in the short-term.80 It is important to note that this evidence is predominantly drawn from younger adolescent populations in HICs. PE is not typically mandated in senior school years,81 making it difficult for students to maintain physical activity while preparing for their final exams, whereas in LMICs there may be a need for provision of basic conditions (e.g. trained staff, materials and environments).
Panel 2. Informing solutions: progress in correlates and intervention research into adolescent physical activity behaviours.
In the first Lancet Physical Activity Series, Bauman et al and Heath et al summarised the global evidence on correlates of physical activity, and interventions to promote physical activity, respectively, including evidence on children and adolescents. For this paper on adolescent physical activity, we sought to identify the progress made since the initial publication. We conducted two complementary umbrella reviews addressing the research questions:
-
-
What are the correlates and determinants of physical activity in adolescence?
-
-
What is the effect of interventions to promote physical activity in adolescence?
Data for these reviews were identified by searches in December 2019 of Ovid Medline, Embase, PsycINFO, Web of Science, and Scopus using the search terms related to “adolescents”, “physical activity”, “systematic review”, in addition to terms for “correlates” or “interventions”, respectively (see Appendices 5 and 6 for full details). Only articles published from 2012 onwards, providing a (semi-)quantitative synthesis, and including 10-24-year-olds were included.
Correlates and determinants of adolescent physical activity behaviours
We identified 13 systematic reviews published since 2012. Most had a specific focus, such as an ecological domain of influence (e.g. interpersonal), location (e.g. school), country (e.g. United Arab Emirates), or population (e.g. North American Indigenous populations, Chinese). Across the reviews, 713 papers were included of which 19% reported on longitudinal studies, which constitutes a substantial increase in the proportion of longitudinal studies from 2012 (when 13.5% across the reviews included both cross-sectional and longitudinal evidence) and an improvement to the evidence base. A greater focus on modifiable factors indicates a clear shift from the evidence base in 2012, which was dominated by non-modifiable factors. Reviews included evidence from across the globe, but still predominately from Western-Europe, North America and Australia. Few studies were included from Africa (10 studies) or Central and South America (27 studies, of which 21 were from Brazil). The evidence shows that associations are likely to be context-specific, evidenced by a review showing that the association between socio-economic position and adolescent sedentary behaviour is negative in high-income countries, but positive in low-to-middle-income countries.52 Transferability of the current evidence base to understudied populations may therefore be limited. More research that aims to understand the context-specific drivers of physical inactivity is required to inform effective intervention development and implementation. Moreover, future research should adopt longitudinal designs, study older adolescent and young adult populations, investigate the relative importance of different factors to identify more targeted action, and focus attention on biological, environmental and policy-level influences (including commercial determinants of health) and how these interact with other correlates. This should include consideration of the diverse impacts of macro-environmental changes such as climate change across the globe.
Interventions to change adolescent physical activity behaviours
We identified 13 systematic reviews published since 2012. All but one predominantly included studies in early adolescence, with one review focussing on young adults at university/college. The evidence base was largely drawn from HICs, with limited representation of LMICs. Seven reviews focussed specifically on interventions in the school setting, with one additional review investigating the effectiveness of approaches set in universities/colleges, which was also the only review including studies in young adults. In general, previous interventions have had a minimal effect on adolescents’ physical activity, especially those that have used objective measures. Based on the evidence identified, we provide the following research recommendations. First, a shift in focus and innovative thinking is required to tackle physical activity behaviours beyond ‘early adolescence’. Solutions need to address the challenges faced by young people as they transition into higher education, employment, marriage and/or parenthood. Second, research on school and community-based interventions should focus more on mechanisms of change (mediation), implementation (i.e., adoption, dose delivered, reach, fidelity, and sustainability) and the determinants of implementation (e.g., feasibility, adaptability and acceptability).81 Poor implementation in original studies likely explains the lack of consistency in the effectiveness of different types of physical activity interventions targeting adolescents, and there is limited evidence on the extent to which interventions have been delivered as intended. Finally, researchers are encouraged to develop, implement and evaluate adolescent physical activity interventions in LMICs.
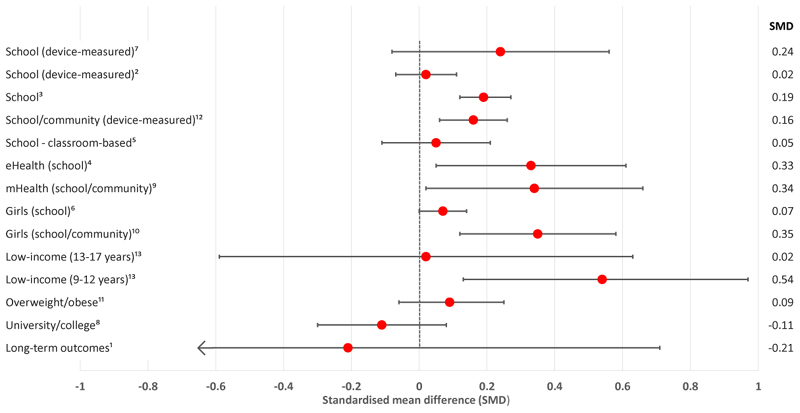
Overall, the intervention evidence included in our umbrella review suggests that physical activity promotion efforts in schools and universities/colleges have been largely unsuccessful in changing physical activity behaviours (Figure 3). Of concern, larger effect sizes were typically observed in studies using self-report measures compared to those utilising accelerometers, highlighting potential reporting bias. Emerging evidence has identified that poor implementation is a major barrier to the success of school-based interventions.82–85 This is potentially because ‘program drift’ and ‘voltage drop’ occur as interventions progress from efficacy to effectiveness to dissemination,86 and interdisciplinary research involving behavioural science, implementation science, education, and input from adolescents themselves is needed to optimise intervention effects. Multi-component interventions (i.e., comprehensive school-based physical activity programs)87,88 appear to be more successful than single component interventions, particularly for adolescent girls, and intra-curricular interventions (those delivered as part of the curriculum) have stronger effects than extra-curricular interventions. Curricular interventions are more closely aligned with teachers’ core responsibilities and potentially face fewer barriers to implementation. While there is a need to scale-up multi-component whole-of-school interventions, research should continue to identify implementation strategies and integrate approaches into the realities of the educational system. Although challenging, instigating changes at government policy level could maximize reach and change their mindset that promoting physical activity is incongruent with the educational system’s remit. Finally, there is a need for novel interventions targeting and attracting older adolescents and young adults in educational settings as these groups have been largely neglected in previous research.
Figure 3. Effects of interventions to promote physical activity or reduce sedentary behaviour in adolescents (standard mean differences from original systematic reviews).
Note: See Appendix 6 for review methods, detailed results, and references.
The challenges and opportunities of the social and digital environment
Adolescence is a period of growing independence, during which peers’ and friends’ social support becomes increasingly more influential compared to adults’ (parents, teachers). Our umbrella review identified three reviews specifically focussed on the role of social support in adolescent physical activity (Appendix 5).75,76,89 Together, they showed that social support from family and friends is positively associated with physical activity in early and late adolescence, although the effect sizes are small. The association with teacher support was equivocal. Parental support was studied in specific components, showing that encouragement and provision of instrumental support from both parents were positively associated, but the evidence was limited for parental co-participation in physical activity and parental modelling. Few studies investigated associations with friends’ support. This demonstrates the ongoing importance of parental social support in adolescence, which should be considered in future adolescent intervention efforts. Moreover, the importance of friends’ social networks and the opportunities this offers for interventions should be explored,90 as well the sources and types of social support relevant for young adults.
The digital revolution of the past decades has radically changed ways of living and communicating, especially in younger generations. In 2015, 95% of 15-year-olds globally had access to the internet at home91 and in Sub-Saharan Africa 63% of 18-29-year-olds own a smartphone.92 During this digital revolution, the global prevalence of physical inactivity in adolescents aged 11-17 years has remained relatively stable at around 80%,43 suggesting that increased digital media access and use may not be a key driver of adolescent physical inactivity. Instead, digital media may be replacing other traditional forms of sedentary behaviour: the percentage of US 16-17-year-olds who read a book/magazine daily declined from 60% in the late 1970s to 16% by 2016, and between 2010 and 2016 13-18-year olds significantly decreased their use of “legacy media” (books, magazines, newspapers, movies, and TV).53 As noted earlier, greater time spent in mentally-passive sedentary behaviours such as TV viewing may have negative consequences for mental health. This new digital reality provides opportunities for reaching the large proportion of adolescents and young adults not in formal education. Our interventions umbrella review (Appendix 6) identified two reviews focussed on the effectiveness of digitally delivered (eHealth/mHealth) physical activity promotion interventions.93,94 They demonstrate potential for changing adolescents' activity behaviours in the short-term, particularly when integrated with other intervention components (such as school-based environmental changes), and should be explored further. Critically, these should be sensitive to the social and environmental changes that are natural part of the adolescent transitionary period, tailored to the adolescent’s life stage (e.g. starting employment, parenthood), and be mindful of inequalities in mobile phone ownership, particularly in LMICs.95
Adolescents in urban environments
Currently 55.3% of the world’s population reside in urban environments and this is expected to increase.96 Improvements to urban environments to facilitate physical activity for transportation and recreation is a recommended strategy for physical activity promotion.15 Global research in adults has shown positive associations between objectively-ascertained urban environmental attributes and accelerometer-assessed physical activity, specifically for net residential density, intersection density, public transport density, and number of parks.97 Our umbrella review (Appendix 5) identified a dearth of review-level evidence on environmental influences on adolescents’ physical activity published since 2012. One review,98 including 19 studies in HICs, demonstrated positive effect sizes in both early and late adolescence for built environmental features promoting play (including sports and fitness), those promoting walking, and those promoting both activities. Larger effect sizes were observed for older adolescents, and for those environmental features that promoted both play and walking, suggesting that a multi-utility design of the urban environment is important, particularly as adolescents become older. As also noted by others,99 the evidence base is mainly cross-sectional and lacks evidence from LMICs where access to positive environments may be more strongly socio-economically patterned. To better inform policy and practice, research needs to move towards longitudinal designs and to consider impacts on adolescent behaviour in natural experimental evaluations of environmental interventions.
Active travel is an important contributor to adolescent physical activity,100,101 and promoting active travel is one of the opportunities identified in the Global Action Plan on Physical Activity 2018-2030. It also supports achievement of the Paris Agreement (i.e., net-zero emissions), suggested to result in 1.15 million fewer annual deaths due to increased active travel.102 Figure 2 presents the prevalence of active travel to school amongst 13-15-year-olds across 73 countries in the GSHS (also Appendix 2). An average of 38% of boys and 46% of girls reported never walking or cycling to school. While this prevalence increased slightly with country income, differences were very large between individual countries, ranging from 15% (Benin) to 78% (United Arab Emirates) among boys, and from 10% (Vietnam) to 90% (Niue) among girls, indicating substantial scope for improvement in many countries. National-level differences in the social, built and natural environment have likely contributed to this variability, although there is limited evidence exploring this. It is however also important to note that for many adolescents across the globe active transportation remains a necessity and not a choice. Moreover, travel patterns of those not in school have not been captured by this survey. In addition to capturing their travel patterns it may be especially important in LMICs to advance research on adolescents’ travel behaviours beyond school travel to other largely overlooked destinations (e.g., friends’ and relatives’ residence, shops/markets, work, household water collection points, etc.) that may be important contributors to overall activity levels.
Conclusions
Adolescence is a critical life stage in the development of healthy behaviours, but adolescent physical activity behaviours and their association with medium and long-term outcomes are poorly understood. Adolescents are not sufficiently active, and this is unequally distributed globally and within societies. A whole systems approach with radical change at social, environmental and systems levels through multidisciplinary and cross-sectorial collaboration is required to tackle this “wicked problem”. Although multi-component programmes, including tailored support for schools, are most likely to be successful, many adolescents across the globe are not in education and alternative strategies to reach this population are required (e.g. changes to the built environment or digital interventions). There is promising observational and interventional evidence on adolescent physical activity behaviours, yet major challenges with implementation remains and more studies from LMICs, those out of school, and older adolescents and young adults going through major life transitions are urgently needed to achieve the promise of the triple benefit of adolescent health promotion.
Supplementary Material
Key messages.
Physical activity levels are low and screen use is ubiquitous among adolescents across the globe. Within-country socioeconomic differences vary by country context: adolescents from high socio-economic backgrounds have better activity profiles than those from low socio-economic backgrounds in high-income countries (HIC), with the reverse true for low and middle-income countries (LMIC).
Adolescent physical inactivity likely contributes to key global health problems, including cardio-metabolic and mental health disorders, but the evidence is weak. Obesity and mental health problems may become auxiliary drivers of physical inactivity, further increasing the risk of morbidity and mortality.
Supportive social and built environments are key drivers of adolescent activity behaviour, and successful policy action should aim for directing change in these areas. Adolescents benefit from built environments that promote a range of activity behaviours (including active travel, play, and sport), and a supportive social environment in- and out-of-school. Access to supportive built environments is unequally distributed, particularly in LMICs.
Schools offer an effective avenue to increase physical activity among adolescents but school-based initiatives have had limited success overall and research involving older adolescents (15-19 years) is lacking. There is a need for sustained implementation of multi-component programmes, co-designed with adolescents. Such interventions require context-specific support for schools to ensure effective implementation and sustainability.
Many young people across the globe, particularly those aged 15-24 years, are not in educational settings and alternative strategies to reach this population are required. With wide-spread access to the internet and some evidence of effectiveness, the potential contribution of eHealth and mHealth approaches contextualised to adolescents’ needs and life circumstances should be explored.
The reasons to instigate change are different for decision-makers in health, policy, education, and among adolescents themselves. Understanding the myriad of benefits associated with physical activity, and tailoring messaging around the outcomes most salient to the specific audience will help drive change at multiple levels of a complex system.
Observational and interventional evidence on adolescent physical activity behaviours comes largely from HICs and younger adolescents (10-14 years). Increased knowledge from LMICs, those out of school, and older adolescents going through major life transitions (e.g. starting employment, parenthood) is urgently required to curb rapid rises in the health consequences of physical inactivity.
Panel 3. Best buys for increasing physical activity in adolescent populations.
Schools are ideally placed to provide younger and older adolescents with a dose of physical activity while equipping them with the necessary knowledge, skills and confidence to be active across the lifespan. Ideally, schools should implement multi-component interventions that include physical education, physical activity during school hours (e.g., active lunch and recess breaks, and classroom physical activity breaks), physical activity before and after school (e.g., active transportation to school and extra-curricular activities), staff involvement, and family and community engagement. Aligning with the recent WHO/UNESCO initiative on “Making Every School a Health Promoting School”,72 this whole-school approach is known as a comprehensive school-based physical activity programme (CSPAP) and is considered the ‘gold standard’ for increasing physical activity in youth.68,83
In general, school-based physical activity interventions targeting adolescents have been minimally successful. However, interventions involving all or multiple CSPAP components typically result in moderate effect sizes. An example is the Physical Activity 4 Everyone (PA4E1) program, implemented and evaluated in ten Australian secondary schools.84 PA4E1 included seven CSPAP components: enhanced physical education lessons, individualised student physical activity plans, enhanced school sport program, provision of programs and equipment during breaks, modified school policies to engage low-active students, after school community sport and fitness programs, and parental engagement. Intervention schools were supported to implement PA4E1 using six evidence-based implementation strategies. After two years, students in the intervention schools were engaging in an additional 7 minutes of moderate-to-vigorous physical activity per day, compared to those in the usual care control group. It is important to note that CSPAPs require substantial financial and logistical support, which may not be attainable in many LMICs and HICs.
Many adolescents across the globe are not in formal education, and there is an urgent need for non-school based approaches to physical activity promotion. There is emerging evidence for the efficacy of physical activity interventions involving eHealth (i.e., internet-based) and mHealth (i.e., mobile phone apps and text messaging) technology. Of note, combining eHealth/mHealth technology with traditional intervention strategies, such as school-based environmental change and/or education, appears to be more effective than technology only interventions. Considering the ubiquity of mobile devices and the high levels of internet access amongst adolescents globally, such approaches are likely to have extensive reach and should be explored more widely.
Acknowledgements
The work of EvS was supported by the Medical Research Council (MC_UU_12015/7) and undertaken under the auspices of the Centre for Diet and Activity Research (CEDAR), a UKCRC Public Health Research Centre of Excellence which is funded by the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the National Institute for Health Research, and the Wellcome Trust (MR/K023187/1). UE is supported by the Research Council of Norway (249932/F20). DRL is supported by an NHMRC Senior Research Fellowship (APP1154507). ICS is supported by the Brazilian National Research Council (CNPq). DD is supported by a Future Leader Fellowship from Heart Foundation Australia (#101234). PK is supported, in part, by the NIDDK Nutrition Obesity Research Center (National Institutes of Health; #2P30 DK072476), and the NIGMS Louisiana Clinical and Translational Science Center (National Institutes of Health; #U54 GM104940). EvS and DL act as consultants on a National Institutes of Health grant. RG is a staff member at WHO. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions, policy, or views of WHO.
We are thankful to the following people for their contribution to the work presented in this paper (in alphabetical order): Olivia Alliott, Mark Babic, Knut Eirik Dalene, Campbell Foubister, Qing He, Erin Hoare, Ying Huang, Erika Ikeda, Isla Kuhn, Rizka Maulida, Johan Ng, Miranda Smith, Jostein Steene Johannessen, Jakob Tarp, and Toaran Zeng.
Footnotes
Declaration of Interests
The other authors declared no conflicts of interest.
Author Contributions
EvS, UE, DD and PK conceptualised the paper, and EvS drafted the text with critical contributions from all authors. EvS, UE, and DL led the systematic reviews; ICS, AH, and ALO contributed to screening, data extraction, and synthesis. RG and PK led on collation and analysis of surveillance data.
References
- 1.United Nations Population Fund. World Population Dashboard. 2019. [accessed 29 Feb 2020]. https://www.unfpa.org/data/world-population-dashboard .
- 2.Patton GC, Sawyer SM, Santelli JS, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–78. doi: 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. 2018;2(3):223–8. doi: 10.1016/S2352-4642(18)30022-1. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organisation. Global Accelerated Action for the Health of Adolescents (AA-HA!): Guidance to Support Country Implementation. Geneva, Switzerland: 2017. [Google Scholar]
- 5.Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: a foundation for future health. Lancet. 2012;379(9826):1630–40. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organisation. Health for the World's Adolescents: A Second Chance in the Second Decade. Geneva, Switzerland: 2014. [Google Scholar]
- 7.Azzopardi PS, Hearps SJC, Francis KL, et al. Progress in adolescent health and wellbeing: tracking 12 headline indicators for 195 countries and territories, 1990-2016. Lancet. 2019;393(10176):1101–18. doi: 10.1016/S0140-6736(18)32427-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Erskine HE, Moffitt TE, Copeland WE, et al. A heavy burden on young minds: the global burden of mental and substance use disorders in children and youth. Psychol Med. 2015;45(7):1551–63. doi: 10.1017/S0033291714002888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kieling C, Baker-Henningham H, Belfer M, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378(9801):1515–25. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- 10.Patton GC, Coffey C, Cappa C, et al. Health of the world's adolescents: a synthesis of internationally comparable data. Lancet. 2012;379(9826):1665–75. doi: 10.1016/S0140-6736(12)60203-7. [DOI] [PubMed] [Google Scholar]
- 11.Arnett JJ, Zukauskiene R, Sugimura K. The new life stage of emerging adulthood at ages 18-29 years: implications for mental health. Lancet Psychiatry. 2014;1(7):569–76. doi: 10.1016/S2215-0366(14)00080-7. [DOI] [PubMed] [Google Scholar]
- 12.The Lancet. Join the Lancet 2020 Campaign on child and adolescent health. Lancet. 2020;395(10218):89. doi: 10.1016/S0140-6736(20)30002-7. [DOI] [PubMed] [Google Scholar]
- 13.Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–29. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ding D, Lawson KD, Kolbe-Alexander TL, et al. The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet. 2016;388(10051):1311–24. doi: 10.1016/S0140-6736(16)30383-X. [DOI] [PubMed] [Google Scholar]
- 15.Kohl HW, 3rd, Craig CL, Lambert EV, et al. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380(9838):294–305. doi: 10.1016/S0140-6736(12)60898-8. [DOI] [PubMed] [Google Scholar]
- 16.2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, D.C.: U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 17.Sallis JF, Bull F, Guthold R, et al. Progress in physical activity over the Olympic quadrennium. Lancet. 2016;388(10051):1325–36. doi: 10.1016/S0140-6736(16)30581-5. [DOI] [PubMed] [Google Scholar]
- 18.Gore FM, Bloem PJ, Patton GC, et al. Global burden of disease in young people aged 10-24 years: a systematic analysis. Lancet. 2011;377(9783):2093–102. doi: 10.1016/S0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- 19.Lascar N, Brown J, Pattison H, Barnett AH, Bailey CJ, Bellary S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 2018;6(1):69–80. doi: 10.1016/S2213-8587(17)30186-9. [DOI] [PubMed] [Google Scholar]
- 20.Song P, Zhang Y, Yu J, et al. Global Prevalence of Hypertension in Children: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019:1–10. doi: 10.1001/jamapediatrics.2019.3310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnson W, Li L, Kuh D, Hardy R. How Has the Age-Related Process of Overweight or Obesity Development Changed over Time? Co-ordinated Analyses of Individual Participant Data from Five United Kingdom Birth Cohorts. PLoS Med. 2015;12(5):e1001828. doi: 10.1371/journal.pmed.1001828. discussion e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302–10. doi: 10.1016/S0140-6736(16)30370-1. [DOI] [PubMed] [Google Scholar]
- 23.Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–57. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 24.United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. New York, United Nations: 2015. [Google Scholar]
- 25.World Health Organisation. Global action plan on physical activity 2018–2030: more active people for a healthier world. Geneva: 2018. [Google Scholar]
- 26.Salvo D, Garcia L, Reis R, et al. Physical activity promotion and the United Nations Sustainable Development Goals: Building Synergies to Maximize Impact. Lancet. doi: 10.1123/jpah.2021-0413. In submission. [DOI] [PubMed] [Google Scholar]
- 27.Alvarez-Bueno C, Pesce C, Cavero-Redondo I, Sanchez-Lopez M, Martinez-Hortelano JA, Martinez-Vizcaino V. The Effect of Physical Activity Interventions on Children's Cognition and Metacognition: A Systematic Review and Meta-Analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(9):729–38. doi: 10.1016/j.jaac.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 28.Singh AS, Saliasi E, van den Berg V, et al. Effects of physical activity interventions on cognitive and academic performance in children and adolescents: a novel combination of a systematic review and recommendations from an expert panel. Br J Sports Med. 2019;53(10):640–7. doi: 10.1136/bjsports-2017-098136. [DOI] [PubMed] [Google Scholar]
- 29.UNESCO Institute for Statistics. One in Five Children, Adolescents and Youth is Out of School (UN Fact Sheet No. 48) 2018 [Google Scholar]
- 30.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–80. [PubMed] [Google Scholar]
- 31.Ong KK, Ahmed ML, Dunger DB. Lessons from large population studies on timing and tempo of puberty (secular trends and relation to body size): the European trend. Mol Cell Endocrinol. 2006;254-255:8–12. doi: 10.1016/j.mce.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 32.Lee MH, Kim SH, Oh M, Lee KW, Park MJ. Age at menarche in Korean adolescents: trends and influencing factors. Reprod Health. 2016;13(1):121. doi: 10.1186/s12978-016-0240-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Census US. Table MS-2. Estmated Median Age at First Marriage: 1890 to Present. Source: U.S. Census Bureau, Current Population Survey, March and Annual Social and Economic Supplements. 2018. [accessed Jul 19 2018]. https://www.census.gov/data/tables/time-series/demo/families/marital.html .
- 34.Marin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: Final Data for 2016. Hyattsville, M.D.: 2018. [PubMed] [Google Scholar]
- 35.U.S. Census. Table A-2. Percent of People 25 Years and Over Who Have Completed High School or College, by Race, Hispanic Origin and Sex: Selected Years 1940 to 2017. 2018. [accessed July 19, 2018]. https://www.census.gov/data/tables/time-series/demo/educational-attainment/cps-historical-time-series.html .
- 36.Nguyen MC, Wodon Q. Global and Regional Trends in Child Marriage. The Review of Faith & International Affairs. 2015;13(3):6–11. [Google Scholar]
- 37.Decker MR, Kalamar A, Tuncalp O, Hindin MJ. Early adolescent childbearing in low- and middle-income countries: associations with income inequity, human development and gender equality. Health policy and planning. 2017;32(2):277–82. doi: 10.1093/heapol/czw121. [DOI] [PubMed] [Google Scholar]
- 38.Verplanken B, Roy D. Empowering interventions to promote sustainable lifestyles: testing the habit discontinuity hypothesis in a field experiment. J Environ Psychol. 2016;45:127–34. [Google Scholar]
- 39.Corder K, Winpenny EM, Foubister C, et al. Becoming a parent: A systematic review and meta-analysis of changes in BMI, diet, and physical activity. Obes Rev. 2020;21(4):e12959. doi: 10.1111/obr.12959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Winpenny EM, Smith M, Penney T, et al. Changes in physical activity, diet, and body weight across the education and employment transitions of early adulthood: A systematic review and meta-analysis. Obes Rev. 2020;21(4):e12962. doi: 10.1111/obr.12962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bull FC, Al-Asari S, Biddle S. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020 doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health. 2018;6(10):e1077–e86. doi: 10.1016/S2214-109X(18)30357-7. [DOI] [PubMed] [Google Scholar]
- 43.Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1.6 million participants. Lancet Child Adolesc Health. 2020;4(1):23–35. doi: 10.1016/S2352-4642(19)30323-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sherar LB, Griffin TP, Ekelund U, et al. Association between maternal education and objectively measured physical activity and sedentary time in adolescents. J Epidemiol Community Health. 2016;70(6):541–8. doi: 10.1136/jech-2015-205763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.da Silva IC, van Hees VT, Ramires VV, et al. Physical activity levels in three Brazilian birth cohorts as assessed with raw triaxial wrist accelerometry. International journal of epidemiology. 2014;43(6):1959–68. doi: 10.1093/ije/dyu203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Strain T, Wijndaele K, Garcia L, et al. Levels of domain-specific physical activity at work, in the household, for travel and for leisure among 327 789 adults from 104 countries. Br J Sports Med. 2020;54(24):1488–97. doi: 10.1136/bjsports-2020-102601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Telama R. Tracking of physical activity from childhood to adulthood: a review. Obes Facts. 2009;2(3):187–95. doi: 10.1159/000222244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carson V, Hunter S, Kuzik N, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: an update. Appl Physiol Nutr Metab. 2016;41(6 Suppl 3):S240–65. doi: 10.1139/apnm-2015-0630. [DOI] [PubMed] [Google Scholar]
- 49.Kandola A, Lewis G, Osborn DPJ, Stubbs B, Hayes JF. Depressive symptoms and objectively measured physical activity and sedentary behaviour throughout adolescence: a prospective cohort study. Lancet Psychiatry. 2020;7(3):262–71. doi: 10.1016/S2215-0366(20)30034-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Canadian Society for Exercise Physiology. Canadian 24-Hour Movement Guidelines: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. 2020. https://csepguidelines.ca/
- 51.Department of Health. Australia's Physical Activity and Sedentary Behaviour Guidelines and the Australian 24-Hour Movement Guidelines. 2019. https://www1.health.gov.au/internet/main/publishing.nsf/Content/health-pubhlth-strateg-phys-act-guidelines .
- 52.Department of Health and Social Care. UK Chief Medical Officers' Physical Activity Guidelines. 2019 [Google Scholar]
- 53.Twenge JM, Martin GM, Spitzberg BH. Trends in U.S. Adolescents’ media use, 1976–2016: The rise of digital media, the decline of TV, and the (near) demise of print. Psychology of Popular Media Culture. 2019;8(4):329–45. [Google Scholar]
- 54.Mielke GI, Brown WJ, Nunes BP, Silva ICM, Hallal PC. Socioeconomic Correlates of Sedentary Behavior in Adolescents: Systematic Review and Meta-Analysis. Sports Med. 2017;47(1):61–75. doi: 10.1007/s40279-016-0555-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Williamson C, Baker G, Mutrie N, Niven A, Kelly P. Get the message? A scoping review of physical activity messaging. Int J Behav Nutr Phys Act. 2020;17(1):51. doi: 10.1186/s12966-020-00954-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Patton GC, Coffey C, Carlin JB, et al. Overweight and obesity between adolescence and young adulthood: a 10-year prospective cohort study. J Adolesc Health. 2011;48(3):275–80. doi: 10.1016/j.jadohealth.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 58.Chaput JP, Willumsen J, Bull F, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5-17 years: summary of the evidence. Int J Behav Nutr Phys Act. 2020;17(1):141. doi: 10.1186/s12966-020-01037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Biddle SJ, Garcia Bengoechea E, Wiesner G. Sedentary behaviour and adiposity in youth: a systematic review of reviews and analysis of causality. Int J Behav Nutr Phys Act. 2017;14(1):43. doi: 10.1186/s12966-017-0497-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cliff DP, Hesketh KD, Vella SA, et al. Objectively measured sedentary behaviour and health and development in children and adolescents: systematic review and meta-analysis. Obes Rev. 2016;17(4):330–44. doi: 10.1111/obr.12371. [DOI] [PubMed] [Google Scholar]
- 61.Richmond RC, Davey Smith G, Ness AR, den Hoed M, McMahon G, Timpson NJ. Assessing causality in the association between child adiposity and physical activity levels: a Mendelian randomization analysis. PLoS Med. 2014;11(3):e1001618. doi: 10.1371/journal.pmed.1001618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lobstein T, Jackson-Leach R, Moodie ML, et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385(9986):2510–20. doi: 10.1016/S0140-6736(14)61746-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bailey AP, Hetrick SE, Rosenbaum S, Purcell R, Parker AG. Treating depression with physical activity in adolescents and young adults: a systematic review and meta-analysis of randomised controlled trials. Psychol Med. 2018;48(7):1068–83. doi: 10.1017/S0033291717002653. [DOI] [PubMed] [Google Scholar]
- 64.Lubans D, Richards J, Hillman C, et al. Physical Activity for Cognitive and Mental Health in Youth: A Systematic Review of Mechanisms. Pediatrics. 2016;138(3) doi: 10.1542/peds.2016-1642. [DOI] [PubMed] [Google Scholar]
- 65.Firth J, Siddiqi N, Koyanagi A, et al. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019;6(8):675–712. doi: 10.1016/S2215-0366(19)30132-4. [DOI] [PubMed] [Google Scholar]
- 66.Hallgren M, Owen N, Stubbs B, et al. Passive and mentally-active sedentary behaviors and incident major depressive disorder: A 13-year cohort study. J Affect Disord. 2018;241:579–85. doi: 10.1016/j.jad.2018.08.020. [DOI] [PubMed] [Google Scholar]
- 67.Varela AR, Pratt M, Harris J, et al. Mapping the historical development of physical activity and health research: A structured literature review and citation network analysis. Prev Med. 2018;111:466–72. doi: 10.1016/j.ypmed.2017.10.020. [DOI] [PubMed] [Google Scholar]
- 68.Heath GW, Parra DC, Sarmiento OL, et al. Evidence-based intervention in physical activity: lessons from around the world. Lancet. 2012;380(9838):272–81. doi: 10.1016/S0140-6736(12)60816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rutter H, Cavill N, Bauman A, Bull F. Systems approaches to global and national physical activity plans. Bull World Health Organ. 2019;97(162–165) doi: 10.2471/BLT.18.220533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rutter H, Savona N, Glonti K, et al. The need for a complex systems model of evidence for public health. Lancet. 2017;390(10112):2602–4. doi: 10.1016/S0140-6736(17)31267-9. [DOI] [PubMed] [Google Scholar]
- 71.ISPAH. ISPAH’s Eight Investments That Work for Physical Activity. 2020. https://www.ispah.org/resources/key-resources/8-investments/
- 72.Raniti M, Bennett K, De Nicolás Izquierdo C, et al. Global Standards and Indicators for Health Promoting Schools. 2020 [Google Scholar]
- 73.Morton KL, Atkin AJ, Corder K, Suhrcke M, van Sluijs EM. The school environment and adolescent physical activity and sedentary behaviour: a mixed-studies systematic review. Obes Rev. 2016;17(2):142–58. doi: 10.1111/obr.12352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhou Y, Wang L. Correlates of Physical Activity of Students in Secondary School Physical Education: A Systematic Review of Literature. Biomed Res Int. 2019;2019:4563484. doi: 10.1155/2019/4563484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Laird Y, Fawkner S, Kelly P, McNamee L, Niven A. The role of social support on physical activity behaviour in adolescent girls: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2016;13:14. doi: 10.1186/s12966-016-0405-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mendonça G, Cheng LA, Mélo EN, De Farias JC., Júnior Physical activity and social support in adolescents: A systematic review. Health Educ Res. 2014;29(5):822–39. doi: 10.1093/her/cyu017. [DOI] [PubMed] [Google Scholar]
- 77.Lubans DR, Lonsdale C, Cohen K, et al. Framework for the design and delivery of organized physical activity sessions for children and adolescents: rationale and description of the 'SAAFE' teaching principles. Int J Behav Nutr Phys Act. 2017;14(1):24. doi: 10.1186/s12966-017-0479-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Whitehead M. Definition of physical literacy and clarification of related issues. ICSSPE Bull J Sport Sci Phys Educ. 2013;65:28–33. [Google Scholar]
- 79.Hulteen RM, Smith JJ, Morgan PJ, et al. Global participation in sport and leisure-time physical activities: A systematic review and meta-analysis. Preventive medicine. 2017;95:14–25. doi: 10.1016/j.ypmed.2016.11.027. [DOI] [PubMed] [Google Scholar]
- 80.Ha AS, Lonsdale C, Lubans DR, Ng JYY. Increasing Students' Activity in Physical Education: Results of the Self-determined Exercise and Learning For FITness Trial. Medicine and science in sports and exercise. 2020;52(3):696–704. doi: 10.1249/MSS.0000000000002172. [DOI] [PubMed] [Google Scholar]
- 81.Beauchamp MR, Puterman E, Lubans DR. Physical Inactivity and Mental Health in Late Adolescence. JAMA Psychiatry. 2018;75(6):543–4. doi: 10.1001/jamapsychiatry.2018.0385. [DOI] [PubMed] [Google Scholar]
- 82.McCrabb S, Lane C, Hall A, et al. Scaling-up evidence-based obesity interventions: A systematic review assessing intervention adaptations and effectiveness and quantifying the scale-up penalty. Obes Rev. 2019;20(7):964–82. doi: 10.1111/obr.12845. [DOI] [PubMed] [Google Scholar]
- 83.Love R, Adams J, van Sluijs EMF. Are school-based physical activity interventions effective and equitable? A meta-analysis of cluster randomized controlled trials with accelerometer-assessed activity. Obes Rev. 2019;20(6):859–70. doi: 10.1111/obr.12823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cassar S, Salmon J, Timperio A, et al. Adoption, implementation and sustainability of school-based physical activity and sedentary behaviour interventions in real-world settings: a systematic review. Int J Behav Nutr Phys Act. 2019;16(1):120. doi: 10.1186/s12966-019-0876-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.McKay H, Naylor PJ, Lau E, et al. Implementation and scale-up of physical activity and behavioural nutrition interventions: an evaluation roadmap. Int J Behav Nutr Phys Act. 2019;16(1):102. doi: 10.1186/s12966-019-0868-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Beets MW, Weaver RG, Ioannidis JPA, et al. Identification and evaluation of risk of generalizability biases in pilot versus efficacy/effectiveness trials: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2020;17(1):19. doi: 10.1186/s12966-020-0918-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Centers for Disease Control and Prevention. Comprehensive School Physical Activity Programs: A Guide for Schools. Atlanta, GA: U.S. Department of Health and Human Services; 2013. [Google Scholar]
- 88.Sutherland RL, Campbell EM, Lubans DR, et al. The Physical Activity 4 Everyone Cluster Randomized Trial: 2-Year Outcomes of a School Physical Activity Intervention Among Adolescents. Am J Prev Med. 2016;51(2):195–205. doi: 10.1016/j.amepre.2016.02.020. [DOI] [PubMed] [Google Scholar]
- 89.Yao CA, Rhodes RE. Parental correlates in child and adolescent physical activity: a meta-analysis. Int. 2015;12:10. doi: 10.1186/s12966-015-0163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hunter RF, de la Haye K, Murray JM, et al. Social network interventions for health behaviours and outcomes: A systematic review and meta-analysis. PLoS Med. 2019;16(9):e1002890. doi: 10.1371/journal.pmed.1002890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.PISA. Results STUDENTS’ WELL-BEING VOLUME III, 2016. 2015 [Google Scholar]
- 92.Pew Research Center. Internet connectivity seen as having positive impact on life in Sub-Saharan Africa. 2018 [Google Scholar]
- 93.Shin Y, Kim SK, Lee M. Mobile phone interventions to improve adolescents' physical health: A systematic review and meta-analysis. Public Health Nurs. 2019;36(6):787–99. doi: 10.1111/phn.12655. [DOI] [PubMed] [Google Scholar]
- 94.Champion KE, Parmenter B, McGowan C, et al. Effectiveness of school-based eHealth interventions to prevent multiple lifestyle risk behaviours among adolescents: a systematic review and meta-analysis. The Lancet Digital Health. 2019;1(5):e206–e21. doi: 10.1016/S2589-7500(19)30088-3. [DOI] [PubMed] [Google Scholar]
- 95.LeFevre AE, Shah N, Bashingwa JJH, George AS, Mohan D. Does women's mobile phone ownership matter for health? Evidence from 15 countries. BMJ global health. 2020;5(5) doi: 10.1136/bmjgh-2020-002524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Department of Economic and Social Affairs. World Urbanization Prospects 2018. 2018. https://population.un.org/wup/
- 97.Sallis JF, Cerin E, Conway TL, et al. Physical activity in relation to urban environments in 14 cities worldwide: a cross-sectional study. Lancet. 2016;387(10034):2207–17. doi: 10.1016/S0140-6736(15)01284-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.McGrath LJ, Hopkins WG, Hinckson EA. Associations of objectively measured built-environment attributes with youth moderate-vigorous physical activity: a systematic review and meta-analysis. Sports Med. 2015;45(6):841–65. doi: 10.1007/s40279-015-0301-3. [DOI] [PubMed] [Google Scholar]
- 99.Ding D, Ramirez Varela A, Bauman AE, et al. Towards better evidence-informed global action: lessons learnt from the Lancet series and recent developments in physical activity and public health. Br J Sports Med. 2020;54(8):462–8. doi: 10.1136/bjsports-2019-101001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Larouche R, Saunders TJ, Faulkner G, Colley R, Tremblay M. Associations between active school transport and physical activity, body composition, and cardiovascular fitness: a systematic review of 68 studies. J Phys Act Health. 2014;11(1):206–27. doi: 10.1123/jpah.2011-0345. [DOI] [PubMed] [Google Scholar]
- 101.Peralta M, Henriques-Neto D, Bordado J, Loureiro N, Diz S, Marques A. Active Commuting to School and Physical Activity Levels among 11 to 16 Year-Old Adolescents from 63 Low- and Middle-Income Countries. Int J Environ Res Public Health. 2020;17(4) doi: 10.3390/ijerph17041276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hamilton I, Kennard H, McGushin A, et al. The public health implications of the Paris Agreement: a modelling study. Lancet Planet Health. 2021;5(2):e74–e83. doi: 10.1016/S2542-5196(20)30249-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.