Executive summary
With one billion people on the move or having moved in 2018, migration is a global reality, which has also become a political lightning rod. Although estimates indicate that the majority of global migration occurs within low-income and middle-income countries (LMICs), the most prominent dialogue focuses almost exclusively on migration from LMICs to high-income countries (HICs). Nowadays, populist discourse demonises the very same individuals who uphold economies, bolster social services, and contribute to health services in both origin and destination locations. Those in positions of political and economic power continue to restrict or publicly condemn migration to promote their own interests. Meanwhile nationalist movements assert so-called cultural sovereignty by delineating an us versus them rhetoric, creating a moral emergency.
In response to these issues, the UCL-Lancet Commission on Migration and Health was convened to articulate evidence-based approaches to inform public discourse and policy. The Commission undertook analyses and consulted widely, with diverse international evidence and expertise spanning sociology, politics, public health science, law, humanitarianism, and anthropology. The result of this work is a report that aims to be a call to action for civil society, health leaders, academics, and policy makers to maximise the benefits and reduce the costs of migration on health locally and globally. The outputs of our work relate to five overarching goals that we thread throughout the report.
First, we provide the latest evidence on migration and health outcomes. This evidence challenges common myths and highlights the diversity, dynamics, and benefits of modern migration and how it relates to population and individual health. Migrants generally contribute more to the wealth of host societies than they cost. Our Article shows that international migrants in HICs have, on average, lower mortality than the host country population. However, increased morbidity was found for some conditions and among certain subgroups of migrants, (eg, increased rates of mental illness in victims of trafficking and people fleeing conflict) and in populations left behind in the location of origin. Currently, in 2018, the full range of migrants’ health needs are difficult to assess because of poor quality data. We know very little, for example, about the health of undocumented migrants, people with disabilities, or lesbian, gay, bisexual, transsexual, or intersex (LGBTI) individuals who migrate or who are unable to move.
Second, we examine multisector determinants of health and consider the implication of the current sector-siloed approaches. The health of people who migrate depends greatly on structural and political factors that determine the impetus for migration, the conditions of their journey, and their destination. Discrimination, gender inequalities, and exclusion from health and social services repeatedly emerge as negative health influences for migrants that require cross-sector responses.
Third, we critically review key challenges to healthy migration. Population mobility provides economic, social, and cultural dividends for those who migrate and their host communities. Furthermore, the right to the highest attainable standard of health, regardless of location or migration status, is enshrined in numerous human rights instruments. However, national sovereignty concerns overshadow these benefits and legal norms. Attention to migration focuses largely on security concerns. When there is conjoining of the words health and migration, it is either focused on small subsets of society and policy, or negatively construed. International agreements, such as the UN Global Compact for Migration and the UN Global Compact on Refugees, represent an opportunity to ensure that international solidarity, unity of intent, and our shared humanity triumphs over nationalist and exclusionary policies, leading to concrete actions to protect the health of migrants.
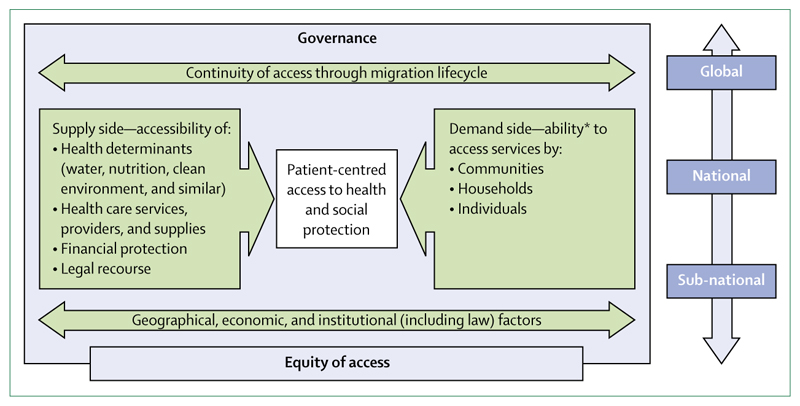
Fourth, we examine equity in access to health and health services and offer evidence-based solutions to improve the health of migrants. Migrants should be explicitly included in universal health coverage commitments. Ultimately, the cost of failing to be health-inclusive could be more expensive to national economies, health security, and global health than the modest investments required.
Finally, we look ahead to outline how our evidence can contribute to synergistic and equitable health, social, and economic policies, and feasible strategies to inform and inspire action by migrants, policy makers, and civil society. We conclude that migration should be treated as a central feature of 21st century health and development. Commitments to the health of migrating populations should be considered across all Sustainable Development Goals (SDGs) and in the implementation of the Global Compact for Migration and Global Compact on Refugees. This Commission offers recommendations that view population mobility as an asset to global health by showing the meaning and reality of good health for all. We present four key messages that provide a focus for future action.
Introduction
Nearly one-seventh of the world’s population is now living in a location different from the one in which they were born.1 A migrant is someone who has moved across an international border or within her or his own country away from their habitual place of residence. Migration is not a new phenomenon. People have migrated throughout human history and population mobility continues to benefit many individuals and communities, contributing to social and economic advancement globally.
Despite the long history of human migration, international dialogue has recently become more prominent, although only rarely has attention been paid to migration as a core determinant of health. When individuals migrate, they enter new environments that have different health risks.2 Studies indicate that morbidity patterns among migrants are diverse and dynamic because of numerous interacting influences, such as an individual’s pre-departure health, socioeconomic and environmental conditions, local disease patterns and risk behaviours, cultural norms and practices, and access to preventive or curative therapies throughout the migration process.3
Health outcomes in migrants are heterogeneous, but evidence consistently shows the disproportionate health, social, and economic burdens of forced migration.4 Despite widespread recognition of the numerous migration related health risks, mobile populations—even forced migrants who are fleeing for their lives—are often met with punitive border policies, arbitrary detention, abuse and extortion, and are commonly denied access to care. Governments that introduce immigration policies legalising exclusion and rights abuse frequently cite national security concerns to justify migration controls that extend beyond their own borders. These policies can go as far as criminalising migrant status, and deterring asylum seekers by detaining them; even separating children from their parents, as seen in US Government immigration policies in 2018.5 All too often, government policies prioritise the politics of xenophobia and racism over their responsibilities to act forcefully to counter them.
Our current global political economy is driven by high-income industrial powers that draw on natural and human resources in LMICs. Moreover, laws and regulations that encourage unrestricted trade in goods, services, and capital are simultaneously being used to control labour mobility to further the political and economic interests of the wealthy, while often leaving poor communities behind. Global trade and pro-business policies in lower-income countries have drained natural resources, contributed to environmental degradation, and pushed people into hazardous, exploitative work to meet consumer demands for cheap goods such as so-called fast fashion.6
International conventions are in place to guide policy to support safer and more inclusive migration and can be used to counter some of these negative forces. As for all human beings, migrants are equally entitled to universal human rights without discrimination. All migrants thus have the right to the "highest attainable standard of health" according to international law.7 All migrants are entitled to equal access to preventive, curative, and palliative health care.8 They also have rights to the underlying social, political, economic, and cultural determinants of physical and mental health, such as clean water and air and non-discriminatory treatment.8 Human rights treaties entitle migrants to due process of law in border practices and freedom from arbitrary detention and restrictions on movement. These rights do not merely impose legal obligations on governments but are essential preconditions for social and economic integration, prosperity, social cohesion in any society, and wellbeing in the modern world.9 The substantial gap between the international legal requirements guaranteeing the human rights of migrants and the implementation of these laws by states provides important context for this Commission report.
In 2016, at the UN General Assembly, the Global Compact for Safe, Orderly and Regular Migration, and a further Compact to respond to acute and chronic refugee situations were initiated in line with the 2030 Agenda for Sustainable Development target 10.7 (to facilitate safe, orderly, and responsible migration).10,11 Yet, these essential multilateral processes appear to be heading in a precarious direction, as exemplified by the US Government’s withdrawal from the Global Compact for Safe, Orderly and Regular Migration in 2017,12 the creation of potential internment camps termed migrant centres,13 and the reluctance of some EU countries to accept an equitable redistribution of migrants.
Our Commission’s journey
Worldwide mobility is our future—regardless of laws and walls. Our Commission was developed in light of the opportunity to realise the SDG commitments "to leave no one behind" and "to reach first those who are furthest behind",14 in the context of states’ guarantees to protect the human rights of migrants. We brought together 20 Commissioners with equal gender representation and wide geographical spread to generate transdisciplinary evidence, contemporary thought, and global expertise that draws on multiple scientific perspectives. To achieve this aim, Commissioners were drawn from a range of scientific backgrounds including sociology, policy, public health, law, humanitarianism, and anthropology.
We initially structured our work with working groups around key themes including health systems, labour migration, forced migration, vulnerabilities, law, human rights and politics, sociocultural factors and identity, and data and health outcomes. We undertook a series of rapid systematic reviews to identify key literature in each area and build on these, as well as two formal systematic reviews and meta-analyses that informed the Commission and are published in detail alongside the report.15,16 Our work was done over a 2-year period with two London based authors’ meetings and a week-long in-person review of the first draft of the Commission at the Rockefeller Foundation, Italy, in November, 2017, along with extensive collaborative work online and by phone.
The principles that underpin our report are equity and inclusion of migrants in access to health and health enhancing resources and opportunities. The Commission settled on five goals for in-depth examination, which provide a focus throughout the four sections of the final report. First, we review evidence on migration and health, challenge common myths, describe the composition and characteristics of population mobility, and assess uses and limitations of migrant categories. Second, we examine multisector determinants of health and consider the implication of current sector-siloed approaches, such as the dichotomous goals of the health sector versus the security sectors. Third, we critically review key challenges to healthy migration by analysing health and migration in relation to culture and identity, rights, legal issues, and environmental hazards and climate change. Fourth, we examine equity in access to health and health services and offer evidence-based solutions to improve the health of migrants. Fifth, we look ahead to consider how our evidence can contribute to synergistic, ethical policies and feasible strategies to inform and inspire action by governments, international agencies, and health professionals to promote health in global mobility.
To tackle this complex subject, we developed a Migration and Health Determinants framework to consider the interactions between migration and the individual, population, and global health (see appendix, supplementary figure 1). The framework highlights key factors influencing the health of mobile populations, including legal, social, and health structures and systems; service access and support; exposures and behaviours particular to migrants; and the epidemiological changes (positive and negative) related to population mobility. These health influences are generally relevant for each stage of a migration process. Our Commission thus offers evidence on how various factors might benefit or be detrimental to individual and population health throughout a journey—including at origin, transit, destination, and return.
Migration and health is a diverse topic with an extensive existing literature. Although we began with a broad and ambitious remit, it is not possible to cover all aspects of migration and health, nor give an overview of all groups of migrants and the conditions they experience. There are many other facets of migration and health that were beyond the specific remit or bounds of the five main goals of this Commission, but we plan to do more in the post-Commission phase in collaboration with others across sectors who are working in this space. Recognising the Lancet Series on Health in Humanitarian Crises, and the Syria Lancet Commission, we have not presented substantive amounts of reference to policy documents, examples of best practice, or deeper analysis in the field of refugee studies. We feel these areas, and wider collaboration on forced migration, will be key for the post-Commission phase in achieving further research, policy, and operational impact. In addition, although we cite on the ground case studies, we were unable to systematically explore grey literature or repositories of migration and health operational and interventional practice.
Section 1. The case for action: what do we know about migration and health
Migration is a dynamic process
Migration seldom involves a single long journey from one place to settle in another. The diversity and complexity of migration patterns include people travelling long and short distances, within and across borders, for temporary or permanent residency, and often undertaking the journey multiple times. A clear delineation or rigid categorisation of different types of migration is rarely possible. The categorisation process attempts to classify a large, heterogeneous population according to limited criteria, which are not generally suited to capture the complex social dynamics of human mobility or necessarily the perspectives or needs of the people who are moving. Terms such as voluntary or forced migration, and categories such as refugees, asylum seekers, and international and internal migrants can partly help to understand migration dynamics. These same terms can also be used to "other" and discriminate against migrants, as well as generally being administrative definitions used to classify migrants for protection, assistance, or research—rather than a true representation of individual circumstances. Legal categories are instrumental for migration control and management by states and international agencies providing support, but might not fully explain an individual’s circumstances. However, for the purposes of the evidence presented in this report, we often use existing definitions (see supplementary table 1 in appendix), which enable us to draw on up-to-date migration literature and data sources. At the same time, throughout the report we will highlight the complex drivers of migration and the difficulties and potential dangers of assigning singular or narrow definitions. Migrant categories are not necessarily objective or neutral; distinctions frequently reflect the assumptions, values, goals, and interests of the parties who assign these labels.
It is also difficult to categorise people in relation to their reasons for migrating. A myriad of negative drivers and positive aspirations (push or pull factors) exist that motivate people to migrate. Individuals, families, and groups often have mixed motives for migrating, and their reasons can change over the course of a single journey. For instance, people seeking safety from conflict can be classified as refugees, asylum seekers, undocumented migrants, or internally displaced persons. However, before and during transit, especially in protracted conflicts where aid resources are insufficient, migration decisions can also relate to livelihoods and employment. Distress migration or migration due to entrenched poverty, food insecurity, and household economic shock (eg, illness, debt), is common worldwide. Distress migration is linked to local unemployment, household financial crises, poor crop production, and in some instances, forced evictions. Evictions can be linked to rising real estate prices, large development projects, and land confiscation.
Regardless of migration motives, economic contributions, or people’s rights, populist rhetoric has morphed all people who move as migrants, condemning them, irrespective of whether they are refugees, asylum seekers, undocumented migrants, or low wage workers. The catch-all term of migrant obscures the net social, political, and economic benefits of migration for destination communities and obscures a migrant’s contribution to their place of origin, supporting families and supplementing development aid, which, in turn results in greater global health.
Health throughout the migration process
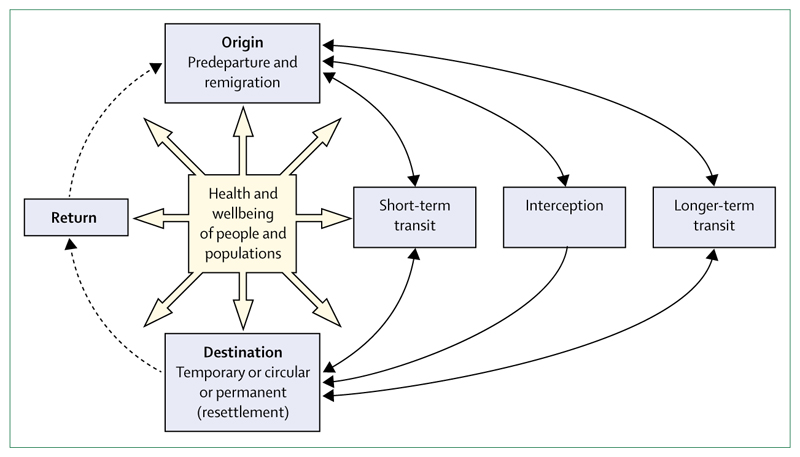
Migration trajectories involve various phases (figure 1) including, pre-departure circumstances at places of origin; short-term or long-term transit, which might involve interception by authorities, non-governmental groups, or criminal gangs; destination situations of long-term or short-term stay; and return to places of origin for resettlement or for temporary visits before remigration.3 In each phase of a person’s journey, potential health risks and possible health protective factors exist that can have a short-term or long-term effect on their wellbeing. As previously noted, the journeys are often diverse and rarely singular. It is common for labour migrants to undertake circular migration, transiting back and forth between their place of origin and destination, or remigrating to a new destination. When people are transiting between locations, their health and safety depends on the forms of transport (air travel, on foot across deserts, hidden in trucks) and the pathogenic or environmental exposures (malaria, tuberculosis, violence, heat exhaustion, dehydration) along the transit routes.17 Return migration also poses health risks and benefits. For instance, communities of origin could benefit from new skills or improved health behaviours gained by returning migrants,18 but conversely, individuals who are injured or disabled during their journey might return to locations with few services or support mechanisms. Importantly, policies to protect migrant and public health will be most effective if they take advantage of opportunities to address people’s health needs at the multiple phases of the migratory process.3 Maintaining the mental health and wellbeing of migrants and the families they might leave behind is particularly important. Even in the best possible conditions, migration is stressful and most people move in ways that are far from ideal; the stress of migration, travel conditions, and the causes that prompted migration in the first place, can all adversely affect mental health.
Figure 1. The migration cycle.
Migration, gender, and health
Both population mobility and the health implications of migration are highly gendered. That is, women, men, and sexual minorities are likely to encounter different health risks and protection opportunities at each phase of a migration journey—a journey they might have undertaken to flee gender-based violence. The risks begin before departure, when women and children could be at risk of violence and discrimination. Among those who are forcibly displaced, there is a particular risk of sexual violence, coercion, and sexual exploitation at all stages of their migration journey, such as accounts of the widespread rape of Rohingya women and girls forcibly displaced from Myanmar in 2016–17,19 or when moving along irregular and dangerous routes ending in official and unofficial detention centres as seen in the ongoing situation in Libya.20 Even when reaching zones of apparent safety, women and children have been exploited by humanitarian workers. This problem remains widespread suggesting that women and children might need protection from their so-called protectors.21 A systematic review of women and girls in conflict-affected settings indicated their extraordinary vulnerability to various forms of human trafficking and sexual exploitation, frequently occurring as underage or forced marriage and forced combatant sexual exploitation.22 Women and children are especially at risk when they migrate without the protection of family or social networks. Unaccompanied girls and boys who move in ways that are not readily detected by potential support mechanisms are particularly vulnerable to neglect, trafficking, abuse, and sexual exploitation. Examples include unaccompanied and separated children who resort to sex work to survive and shelter in parks and makeshift camps in Greece.23 Child marriages appear to increase among displaced populations,24 as parents are often forced to make impossible choices about their daughters based on their fear of sexual violence by armed forces or combatants and economic hardship.25 Sexual minorities might be among the most neglected and at-risk populations in circumstances of migration. The stigma associated with being LGBTI can subject individuals to bullying and abuse or force them to remain invisible. There appears to be little training for health and humanitarian aid professionals currently to meet the health needs of sexual minorities.
Challenging myths
In the current political climate, the term migrant raises a litany of myths and inaccurate stereotypes. While often used for political gain, falsehoods about migrants have frequently become publicly accepted. Here, we respond to common myths by offering data driven facts.
Are HICs being overwhelmed by migrants?
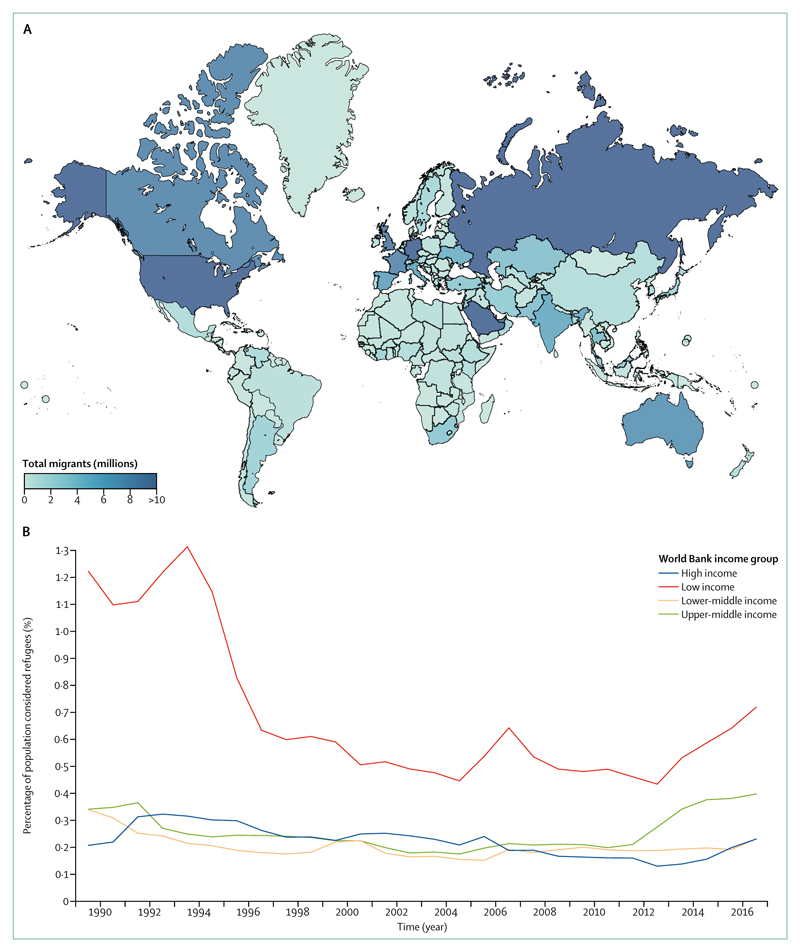
Discussions about migrants often centre around absolute numbers of migrants crossing international borders into HICs. This rhetoric tends to ignore findings that there has been little change in the percentage of the world’s international migrants, which has only risen from 2·9% to 3·4% from 1990 to 2017 globally, with diversity in geographical location of migrants (figure 2A). Although HICs have seen a greater rise in the percentage of migrants arriving from 7·6% to 13·4% (1990 to 2017), it is important to note that the percentage of the total population that were individuals who have been displaced and are currently living in HICs is considerably smaller than in LMICs. Furthermore, the figures for all international migrants in HICs include, for instance, students who pay for their education and often return to their countries of origin,28 and labour migrants who are net positive contributors to the economy. Previous waves of migration as a percentage of the global population (eg, Europeans colonising the Americas and Australasia) have been vastly greater in number than these recent trends. Similarly, the percentage of the world’s population that were refugees generally declined between 1990 and 2011. Subsequently, all countries saw an increase, but this was highest in LMICs (figure 2B). HICs had very little change in their refugee population, and it was low-income countries that had fluctuations from 1·3% to 0·4% (figure 2B). These data show that despite popular discourse to the contrary, changes in migration are more complex than the simple narrative of a rise in numbers. Overall, mobility patterns are highly regional and context specific, with less wealthy nations hosting disproportionate numbers of forcibly displaced populations.
Figure 2. International migration globally26.
(A) Global map of the total number of international migrants in 2015. (B) Percentage of population that were refugees by the World Bank Income group (1960-2017). Analysis done with data from the World Bank. Interactive online version available.27
Are migrants a burden on services?
Macroeconomic analysis on the effect of asylum seekers in Europe concluded that they have a positive effect on host countries’ economies.29 Nowadays, rather than burdening systems, migrants in HICs are more likely to bolster services by providing medical care, teaching children, caring for older people, and supporting understaffed services. Migration provides much needed high skilled and low skilled workers for economic growth. The way health-care markets are constructed, from both the supply and demand sides, is inextricably connected with human mobility. Hospitals, residential homes, child-care centres, and domestic and professional cleaning services are often staffed by migrants. Migrants constitute a considerable portion of the health-care workforce in many HICs and contribute to a substantial so-called brain gain in net-migrant receiving countries.30 For example, 37% of doctors in the UK gained their medical qualification in another country.31 Health-care workforce migration from poorer to wealthier countries has been the subject of extensive study. Health professionals migrate because of low remuneration, poor working conditions, work overload, and insufficient opportunities for professional advancement in their home countries.32 Higher-income countries reap the benefits. It is LMICs, such as Syria and Turkey, who host a higher proportion of displaced people, where it is challenging to deliver services for the poorest members of society. Although many migrants can access the labour markets, there are also many who might not have this same access with immediate and long-term consequences on livelihoods, social security, education, and health. Our systematic review and meta-analysis16 of global patterns of mortality however, provides evidence that international migrants, particularly those in HICs who are more likely to have actively chosen to migrate (such as economic, student, and family reunion migrants), are more likely to live longer compared with host populations across the majority of International Classification of Diseases (ICD)-10 categories.
Are fertility rates among migrants higher than among host populations?
Despite populist rhetoric that migrants have many more children than host populations, the growth and decline of migrant populations in a country is affected by birth and death rates and inward and outward migration from a country. Using large scale longitudinal data from six countries (France, Germany, Spain, Sweden, Switzerland, and UK), researchers found that migrants have lower first-birth rates than non-migrants with the exception of migrant Turkish women.33 Moreover, birth rates among migrants were barely at the level of population replacement (a total fertility rate below 2·1 births per woman) and often falling. Access to contraception also influences differences in fertility rates. Poor access to contraception among migrants is often related to inconsistent policies, guidelines, and provision of services. In the EU, migrants appear to have inadequate access to sexual and reproductive health care, including family planning services.34
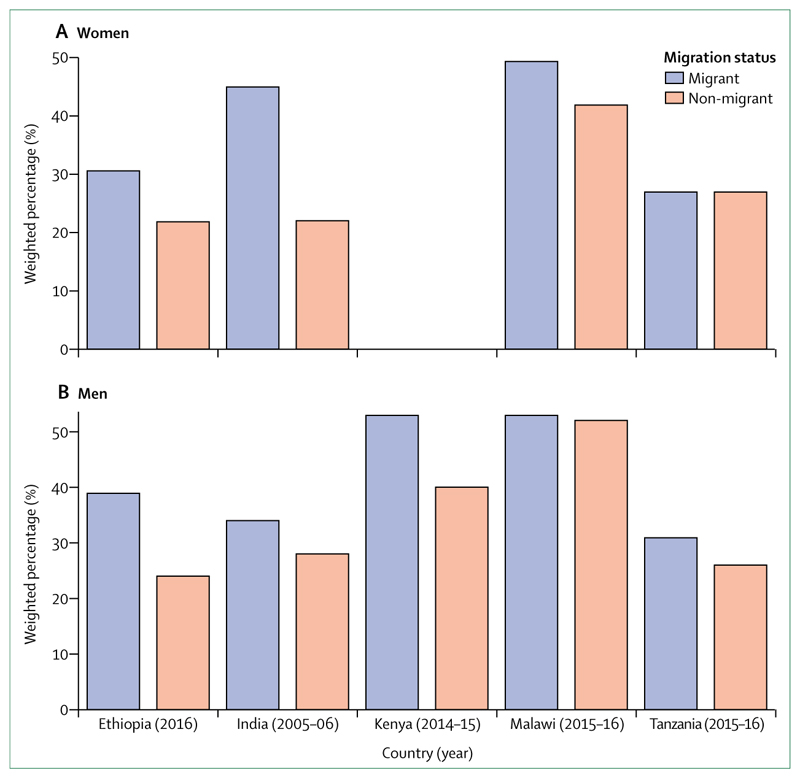
Evidence about fertility and its association with internal migration in LMICs is scarce. With Demographic and Health Survey data for the use of modern contraception by an individual’s migration category in five LMICs (Ethiopia, India, Kenya, Malawi, and Tanzania), we show that in each country internal migrants used modern contraception methods more often than non-migrants (figure 3). These results could be explained in substantial part by a person’s educational and socioeconomic status, supporting evidence that migrants have lower first-birth rates than non-migrants—and dispelling negative views about fertility among migrants. However, these data might not represent patterns among more marginalised groups such as undocumented migrants, refugees, asylum seekers, or displaced populations in humanitarian crisis situations. For these marginalised groups, in whom sexual assault is common, there is an even greater need for readily accessible sexual and reproductive health care.40
Figure 3. Weighted percentage of men and women using modern methods of contraception by migration status35–39.
No data available for Kenyan women.
Are migrants damaging economies?
An overwhelming consensus exists on the positive economic benefits of migration, which is insufficiently acknowledged. In settings that offer universal access to minimum economic benefits, there has been much debate as to whether migrants receive more in social assistance than they contribute in taxes. The evidence examining this issue generally suggests that migrants make greater overall contributions, except in countries with a high proportion of older migrants.41 In advanced economies, each 1% increase of migrants in the adult population increases the gross domestic product (GDP) per person by up to 2%.42 Migrants increase income per person and living standards through greater contributions to taxes, which are of greater economic worth than the social or welfare benefits they receive.41 Furthermore, in the EU and some other European countries, free movement has been shown to address imbalances in the labour market43 by serving as an equilibrating force through the provision of labour where and when needed. These benefits are not just accrued by the wealthiest in society. Moreover, the World Bank Group estimated that migrants sent a total sum of US$613 billion to their families at origin in 2017.44 Approximately three-quarters of these remittances were sent to LMICs—an amount more than three-times larger than official development assistance—and these remittance flows have been growing steadily since 1990.44 In countries such as Liberia, Nepal, and Tajikistan, up to one-third of GDP comes from international remittances. Globally, these sums of money are large and can transform the lives of non-migrants.44
Are migrants disease-carriers that pose risks to resident populations?
Suspicion against migrants as carriers of disease is probably the most pervasive and powerful myth related to migration and health throughout history.45 Although historical examples exist of the introduction of disease into new settings through human mobility (eg, the spread of infection from European colonial settlers), the risk of transmission from migrating populations to host populations is generally low. For example, studies on tuberculosis suggest that the risk of transmission is elevated within migrant households and migrant communities, but not in host populations.46,47 Nonetheless, several HICs screen migrants for tuberculosis as part of pre-migration visa application checks.48 Although tuberculosis screening systems could benefit individuals through early detection, screening is often stigmatising and can spur xenophobic media messages,49 despite the negligible risk of transmission in countries with functioning public and universal health systems.46 Migrant populations might come from countries with a high burden of disease50 and it is not uncommon for disease outbreaks to be found in situations of conflict, which can disrupt already weak public health systems. Illness and infection can also be acquired or spread via transit routes and transport means. For example, air travel can facilitate the rapid geographical spread of infections. However, even risk of air travel related outbreaks is low–modest if the destination setting has strong surveillance and inclusive public health services.51 These services are also crucial to prevent pandemics, whether associated with population movement or not.52 Epidemiological patterns and related risks are readily addressed by assessing the infectious disease burden among populations and with use of data to design targeted interventions to contain outbreaks and prevent new infections through immunisation. However, because of the prejudice and unfounded fear that can be generated by misuse of surveillance data, caution is required when releasing potentially stigmatising disease prevalence figures for public consumption. We revisit this issue throughout the report and discuss the misuse of data.
Composition of mobile populations
Understanding the health of people on the move requires clarity about who is moving, why, and where, and the potential positive and negative effects. Here, we offer an overview of international migrants, internal migrants, labour migrants, refugees, asylum seekers, internally displaced persons, and climate refugees (an emerging group that is likely to increase in number). Data will be presented with use of the most widely applied migration categories—despite our previously stated reservations about the weaknesses of these categories—reviewing numbers and their associated limitations, geographical distribution, age and sex characteristics, and key issues for each group.
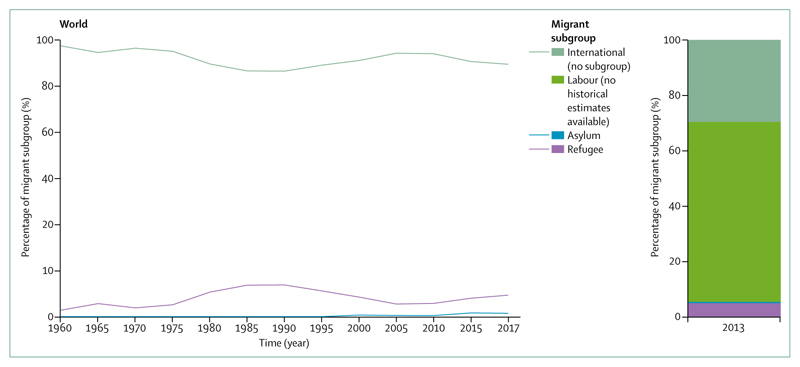
International migration
In 2017, there were an estimated 258 million international migrants, which accounted for 3·4% of the world’s population.53 Notably, most data for international migration between 1960 and 2017 did not classify migrants by subgroup. Estimates by the International Labour Organization indicate that labour migrants constituted 65% of all international migrants in 2013.54 However, 2013 was the only year for which global data were available on labour migration (figure 4). In 2017, Asia had the largest number of international migrants (80 million), closely followed by Europe (78 million), and North America (58 million).55 Globally, the largest number of international migrants were in the 30–34 age group and 48% were female.55 To date, data come primarily from population censuses, population registers, and nationally representative surveys, often with use of place of birth to establish international migrant status. For 47 countries, place of birth is not available so country of citizenship is used instead. This can potentially lead to overestimation of international migrant numbers. Conversely, these data can also underestimate migrant numbers by inappropriately excluding people born abroad with local citizenship. Data collection for international migration would benefit from better information on subgroups and categories of migrants with little data (eg, labour, undocumented, and trafficked) in order that these groups are not omitted from needs assessments and budget allocations for responses.
Figure 4. International migration by migrant subgroup26,54,55.
Percentage of all international migrants that were refugees, asylum seekers, and labour migrants, 1960–2017. Labour migration estimates only available for 2013. Refugee numbers are for those under the UN High Commissioner for Refugees’ mandate and therefore do not include individuals under the UN Relief and Works Agency for Palestine Refugees in the Near East’s mandate as data are not available back to 1960. Analysis done with data from UN High Commissioner for Refugees. Interactive online version available.27
Internal migration
Although international migration receives the most political and public attention, most movement globally is internal migration. In 2009, the number of people who moved across the major zonal demarcations within their countries was nearly four-times greater (740 million) than those who moved internationally.56 Approximately 40% of urban growth in Asia, Africa, and Latin America results from internal migration from rural to urban areas.57 In many LMICs, rural-rural internal migration to work in the agricultural sector still accounts for the largest number of people on the move.58 Previously, evidence suggested that internal migration was dominated by single men, however, recent trends show increases in women moving for work and to seek freedom from discriminatory social and cultural norms.59 From 2014 to 2050, the proportion of people living in urban areas, largely because of migration from rural areas, is expected to increase from 48% to 64% in Asia, and from 40% to 56% in Africa.57 Producing global estimates on internal migrants is methodologically challenging and routine data are rare.60
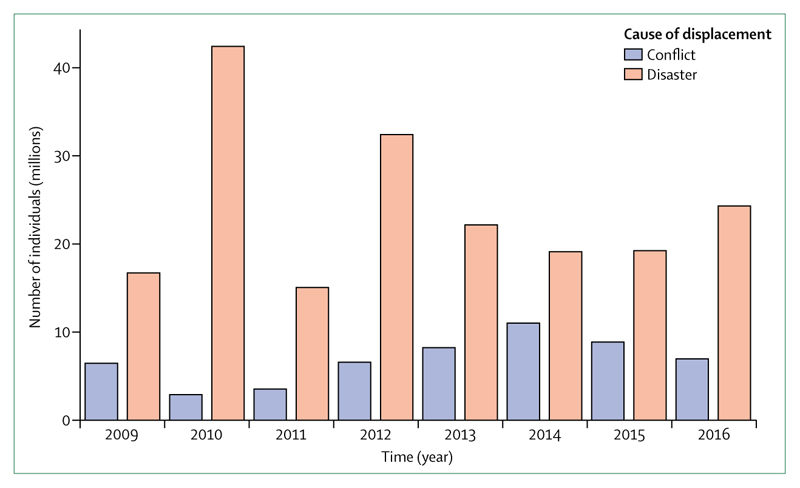
There are considerably more internally displaced persons because of conflict and natural disasters than asylum seekers and refugees globally. However, they also receive substantially less attention than asylum seekers and refugees, primarily because of the importance attached to national borders and citizenship, as well as the availability of better data collection for refugees. In 2017, there were 30·6 million newly internally displaced people associated with conflict and disaster.61 East Asia and Pacific was the region with the highest number of internally displaced people due to disasters and sub-Saharan Africa was the highest due to conflict and violence. Between 2008 and 2017, the number of individuals displaced because of conflict and violence was fewer than those resulting from disasters (figure 5).61
Figure 5. Total annual new displacements as a result of conflict and disasters globally61.
Interactive online version available.27
Labour migration
The International Labour Organization estimates suggest that in 2013 there were 150·3 million international migrant workers in the world.54 Although official figures indicate that the largest proportion of international labour migrants is in North America and northern, southern, and western Europe, these figures are perhaps misleading. Regional labour migration in LMICs often goes uncounted because of regional and bilateral labour and trade agreements, as well as undocumented or irregular border crossing.54,62 LMICs are estimated to host roughly 25% (37·9 million of 150·3 million) of total labour migrants globally.54,63 Moreover, it is important to note that these figures will be underestimates as they exclude undocumented international migration between neighbouring countries and workers in the informal economy. Among labour migrants globally, 2013 figures indicate that more migrant workers are male (56%) than female (44%).54 Women more commonly work in service jobs (74%) and less often in manufacturing and construction work (15%).54 Increases in the migration of women could be due in part to shifts in gender, social, and migration norms, and in other part by remittances they will receive,64 which create greater opportunity for women to migrate. Adolescent girls also migrate for work, driven by financial incentives,65,66 and hopes for greater freedom and empowerment. However, recognition is growing of the number of young women who end up in exploitative work.67 Comparative national data are very poor for the patterns and prevalence of internal labour migration, especially for harder to monitor forms, such as seasonal and often circular migration.
Forced migration
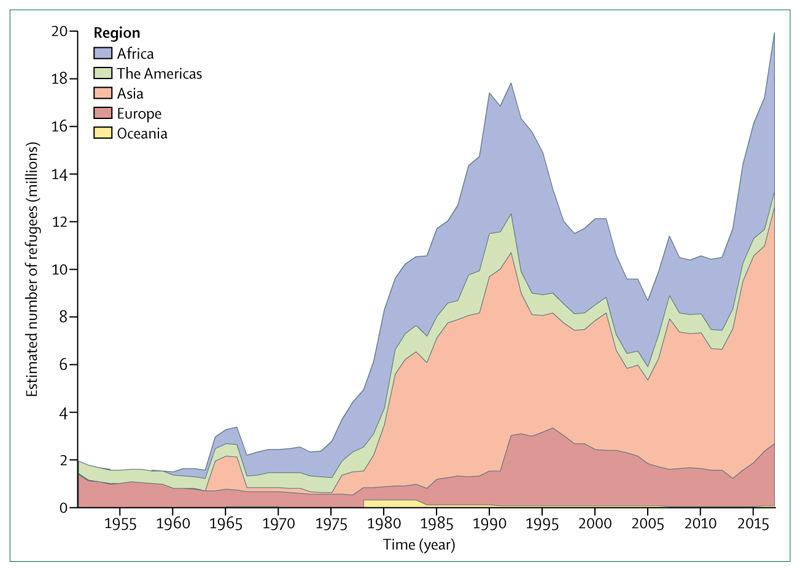
As of 2018, two billion people live in countries affected by civil unrest, violence, or ongoing conflict.68 In 2017 there were a total of 25·4 million refugees globally, with 19·9 million refugees under the UN High Commissioner for Refugees’ mandate and 5·4 million Palestinian refugees under the UN Relief and Works Agency’s mandate. Monitoring historical refugees numbers that fall under the UN High Commissioner for Refugees’ mandate reveals the percentage of international migrants who were refugees to have remained less than 11·4% following a peak in 1990 (figure 4). Consistent with the trend in percentage of refugees in relation to all international migrants, the number of refugees falling under the UN High Commissioner for Refugees’ mandate decreased from 17·8 million to a low of 8·7 million from 1992 to 2005, followed by an increase to 19·9 million in 2017 (figure 6). Africa had the highest percentage of refugees under 18 years in terms of the countries of origin and countries of asylum application in 2015 (see supplementary figure 2 in the appendix). Further details on the regional variation in the number of refugees are provided in the supplementary figures 3 and 4 in the appendix. Previously, most forcibly displaced people lived in camp-like settings, however, now refugees are more likely to live outside of camp settings in developing regions; 85% of the world’s refugees reside in developing regions and 58% live in urban areas, as reported in the 2017 Global Trends Report. Forced displacement from long-term conflicts, such as the Syrian conflict, have resulted in a protracted refugee situation for millions of refugees, who often reside in urban and peri-urban settings without formal refugee status. For example, less than one-fifth of refugees in Jordan live in camps.69
Figure 6. Estimated refugee numbers under the UN High Commissioner for Refugees’ mandate by region, 1951-2015.
Historical data in this figure do not include 5·4 million Palestinian refugees under the UN Relief and Works Agency for Palestine Refugees in the Near East’s mandate in 2017, as historical data for this group are not available. Interactive online version available.27
There were an estimated 1·9 million claims for asylum in 2017 and a total of 3·1 million asylum seekers whose refugee status was yet to be determined.70 The number of asylum-seekers with pending claims increased by 28% by the end of 2017, compared with 2016 according to the 2017 Global Trends Report. Asylum-seekers are increasingly experiencing longer periods with pending claims. There is enormous variation in the total number of asylum seekers by country of origin (see supplementary figure 5 in the appendix) reflecting proximity to source countries, and the proportion successfully securing refugee status. In other categories of forced migrants, the numbers of individuals who are undocumented and often the most vulnerable, are not available as they are often not in contact with authorities.
Resettlement is a considerable challenge. Refugees with acute health and medical needs are among the top priorities for consideration for resettlement referral by the UN High Commissioner for Refugees, and some resettlement countries expedite consideration of refugees facing acute health risks. In 2018, the UN High Commissioner for Refugees established that about 1·2 million refugees around the world needed resettlement.71
Human trafficking and modern slavery
Human trafficking, forced labour, and forced marriage, now referred to collectively as modern slavery, is estimated to affect 40·3 million people globally, according to 2017 estimates from the International Labour Organization.72 These new figures indicate that there were 25 million people in forced labour and highlight that there are also 15 million people in forced marriage. This number equates to 5·4 people for every 1000 individuals in the world.73 Regionally, Asia appears to have the largest number of modern slavery cases, with 62% of all enslaved people, followed by Africa at 23%. Women and girls are disproportionately affected, accounting for 71% of cases, as are children, with one in four individuals who are trafficked under the age of 18 years. Women and girls are commonly trafficked for sex work, domestic service, and as brides. Men and adolescent boys are more likely to be recruited, often deceptively, for various forms of strenuous manual labour, including commercial fishing and construction.74 Sexual minorities who are trafficked are often subjected to forced sex work.
Climate change refugees
Global climate change is driven by anthropogenic atmospheric and oceanic warming, and has global effects causing rising sea levels, shrinking of the cryosphere, and ocean acidification. Climate change has the potential to affect and disrupt well known drivers and mechanisms of migration in the future to an unknown but potentially striking degree. The Lancet Commission on Health and Climate Change,75 discusses the potential effects on migrants including the effect on urban health, extremes of heat, and the social effect of population redistribution as a result of only people from some demographics having the resources to move. A 2018 study suggested that by 2070, the combined effects of climate change and the vast expansion of irrigated agriculture could result in deadly heatwaves. Such heatwaves could make large parts of northern China, with a population of 400 million, uninhabitable.76 Climate change will also increase the frequency and intensity of hydrometeorological hazards.77
According to a 2018 report by the World Bank, climate change has the potential to force more than 143 million people to move within their country by 2050.78 The messages are that internal climate migration could be a reality, but not necessarily a crisis, and that migration can be a sensible climate change adaptation strategy if managed carefully and supported by good development policies and targeted investments. The effects of climate change on migration are largely uncertain because migration is driven by complex multicausal processes, which also include social, economic, political, and demographic dimensions. These dimensions impact on each other and can be driven by the effects of climate change. The uncertainty is compounded by the fact that refugees fleeing conflict, war, or persecution are protected by the 1951 Convention Relating to the Status of Refugees and its 1967 Protocol.79 By contrast, no international law recognises climate refugees, who are mostly seen as searching for better economic conditions. The World Bank report is confined to internal displacement, which limits its scope. For Bangladesh, a country considered to be at the front line for climate change effects, the World Bank projects that by 2050 there will be 13·3 million climate migrants (surpassing the number of other internal migrants).78 In panel 1, this projection is tested with use of detailed census data from 2001 to 2011. Migration attributed to hydrometeorological hazard risks from all causes are projected up to 2050, exceeding the World Bank figure of 13·3 million internal climate migrants. Therefore, as with northern China, the combination of global climate change and local anthropogenically driven environmental degradation could trigger substantial increases in migration. In our analysis, there was no automatic assumption for Bangladesh that climate change will cause mass migration, but rather that mass migration is occurring now and will increase, projected from current trends with large scale census data.
Panel 1. Projection for internal migrant numbers for Bangladesh by 2050.
The 2050 projection for internal migrants in Bangladesh was driven by hydrometeorological hazard risks under certain assumptions of social and political developments. Three different scenarios based on the combination of two development pathways and two climate trajectories were modelled by the World Bank.78 The modelling included three environmental variables: water stress, crop failure, and sea level rise, with a gravity model based on distance and attractiveness of the destination compared with the source area. The report defines climate migrants as people who have moved from their place of origin for at least 10 years and travelled over 14 kilometres within country because of climate change. The report aims to present a plausible range of outcomes rather than precise forecasts. The projection is based on a single model but has positive aspects such as the inclusion of socioeconomic factors, the choice of slow onset climate change variables, the use of whole globe decadal changes, and that downscaling can easily be achieved. The modelling was calibrated by the highest resolution population census data available at that time. The World Bank report projects that by 2050 there will be 13·3 million climate migrants in Bangladesh based on a pessimistic-realistic reference scenario with high emissions and unequal development.
To test the World Bank projection, the 2011 population and housing census data were collected from the Bangladesh Bureau of Statistics. This database was prepared from household surveying in Bangladesh with a questionnaire that covered the respondents’ household characteristics, demography, migration details, and economic activities among others. 50 districts of 64 in Bangladesh were identified as vulnerable to hydrometeorological hazard risks: flooding and river erosion (23 districts); cyclones and storm surges (19 districts); and drought and groundwater depletion (8 districts). Some districts are affected by multiple hazards. Subsequently, the total number of life-time (greater than 10 years) and inter-district migrants (travelled more than 14 kilometres away) was identified in each district. The migrants constitute about 9%, 12%, and 5% of district-wise total population categorised according to flooding and river erosion, cyclone and storm surge, and drought and groundwater depletion as reasons to migrate. They were then filtered by selecting only people migrating from rural areas, on the basis of an assumption that the adaptive capacity to climate change is lower in rural communities in Bangladesh because of a lack of development and poverty. They constitute about 8%, 11%, and 4% respectively. After applying these filters, it is possible to assess the number of internal migrants attributed to hydrometeorological hazard risks in Bangladesh and whether this figure is compatible with the local context. This assessment is made by analysing primary data collected through actual field surveying under the supervision of the Bangladesh Bureau of Statistics.
4·07 million internal migrants were identified for the period of 2001–11, migrating because of these hydrometeorological hazard risks. They represented about 4% of the country’s total population and 41% of the total migrant population of flooding hit districts, 42% of the total migrant population of cyclone hit districts, and 31% of the total migrant population of drought hit districts. By considering Bangladesh’s population growth rate (varying between 0·22–1·00%) and a similar scenario (without new climatic and development interventions) up to 2050, it can be estimated that the total number of internal migrants attributed to hydrometeorological hazard risks will be 19·4 million, which will surpass the World Bank projection of 13·3 million internal climate migrants by 2050. However, it cannot be confirmed that these hydrometeorological hazard risks (eg, river erosion and groundwater depletion), and their frequency and intensity are attributed to climate change.77 While our analysis of primary data suggests that a greater number of people will potentially be affected than the World Bank report projects, it does not validate their projections for internal climate migrants.
Political, cultural, environmental, and structural determinants of migration and health
Political determinants of health
Migration has become highly politicised, especially as some politicians try to curry electoral favour by migrant-blaming and undermining the welfare state. Stigmatising rhetoric has meant that the rights of migrants are under attack by the same structures and processes that are supposed to protect them. This occurs both in their country of origin, potentially leading some to move, and during their migration journey. The views, words, and actions of individuals in power both instigate discrimination and restrict access to education, work, justice, and health. The term fake news has recently been used to describe inaccurate information deliberately created or used to mislead. In a world of social media and populist discourse, fake news is used against migrants to undermine trust and divide communities. A previous Lancet Commission on Global Governance80 outlined the major influences and governance deficits that affect health and the power disparities governing health inequity. This previous Commission highlighted how the goals of the health sector, which are inclusive towards better health for all, commonly come into policy conflict with the interests of influential global actors such as states and transnational corporations who prioritise national security, sovereignty, and economic goals.80 When considering the health of migrants in light of the Global Governance report, the convergence of health and migration is situated at the heart of these opposing governance goals. For example, the Global Governance Commission highlighted democratic deficits, or the insufficient participation of civil society, health experts, and marginalised groups, in the decision making process.80 Migrants often experience exclusion, and despite their participation as workers, consumers, and investors in the economy, they are frequently left out of democratic processes. The previous Commission report80 also indicated that these democratic deficits are compounded by weak or absent government or public accountability mechanisms to fix the failings in this exclusionary system. Moreover, the authors point out the leadership vacuum on health, which is particularly true for migrant health.80 For instance, in the UN system, these global concerns cross thinly through many UN mandates with no clear leadership or coordination with all relevant external actors (eg, civil society, philanthropic organisations, the media, business, and academia). With these profound governance gaps, voices are few and far between to combat the highly charged political rhetoric that demonises migrants.
Culture, ethnicity, and identity
Understanding issues of culture, ethnicity, and identity is crucial for achieving equity in health, including migrant health.81 Past and present migration dynamics have contributed substantially to the cultural and ethnic diversity of many societies, highlighting the importance of the cultural dimensions of health and medical care. Culture can be outlined as a linked group of customs, practices, and beliefs jointly held by individuals, social networks, and groups. These factors help define who they are, where they stand in relation to those within and beyond the group, and give meaning and order to life. Anthropologists describe culture as “a process through which ordinary activities and conditions take on an emotional tone and a moral meaning for participants”;82 this definition includes perceptions, beliefs, and practices related to health, suffering, and disease. Culture is thus never static but evolves in relation to a range of social, economic, and political factors, and experiences of individuals and groups.
Both migration and culture are processes that define an individual’s identity and are dynamic in nature. Migration and living as a migrant in transit or in a host community entails multiple occasions and stimuli for cultural adaptation and change, on individual and collective levels. Identity can initially be based on one’s place of origin (eg, ethnicity, nationality). As a migrant, aspects of oneself are regularly reshaped as new identities emerge and new labels are imposed (eg, migrant, foreigner, undocumented). New locations raise challenges and individuals develop strategies to respond to opportunities or constraints, including how they care for their own health and that of their family, and how they interact with health systems. On arrival at a destination, assimilation and acculturation could alter their risk profile to mirror patterns of local residents or their fellow migrants. Independent of specific ethnicity or country of origin, this change in risk profile could mean higher morbidity due to the deleterious interaction of multiple adverse structural factors, including marginalisation, poverty, the effect of immigration laws and legal status, and poor access to care.83 Analysing the dominant discourse in host countries around migrants helps us to understand how these populations tend to be othered. The questioning by the general population and governments of the deservingness of some groups of migrants for health care has eventually supported actual practices and structures of exclusion.84 Such measures are both fuelled by and contribute to the anti-migration environments, which make individuals feel uncertain about their future, their safety, and the security of their family.
At all stages of the migration process, individuals and groups could be affected by the toxic consequences of social exclusion and discrimination on the grounds of ethnicity, race, nationality, or migrant status. For some migrants, ethnic discrimination or persecution is their reason to leave their place of origin. Subsequently, in transit or in receiving countries, migrants are often subject to pejorative discourses fed by cultural stereotypes and racism. The creation of group identity through distinct cultural artefacts, language, and an assumed common origin or history is an essential feature of culture. However, this diversity can be used as a tool for discrimination, which can be created or increased by individuals who seek to divide communities. Divisive discourse has detrimental consequences, including the impact of raising unfounded fears of increased infectious diseases, violence, and demands on health resources within the host group, a situation well known from past and recent history. Migrants’ burden of discrimination is often doubled as they carry group characteristics that might be associated with additional prejudice and exclusion, for example related to intersectionality with gender or disabilities.
Discrimination towards migrants is commonplace and often conflated with racism. Anti-migrant discrimination and racism overlap, sharing features of prejudice against the other, which are forms of xenophobia but distinct entities. Racism is based on the belief that one race or ethnicity is superior, justifying discriminatory actions. Anti-migrant discrimination is directed against migrants and tends to be a combination of prejudice against the other with fear over the loss of something to the migrant (eg, a job, a service). Crucially, discrimination against migrants is usually racism; that is, it is directed towards people who appear physically or culturally different. This racism can occur not only between the migrant and host community but also between one migrant group and another.85,86 Why is this distinction important? In political discourse, racism is usually socially prohibited and sometimes illegal. Discrimination against migrants, however, is considered acceptable for many and is commonly used in populist rhetoric. Anti-migrant language is a tool that provides the opportunity to divide populations on ethnic grounds to advance the majority view and to mobilise fear and hatred. For example, in September 2015, in an interview to Jornal Opção, the now elected Brazilian President Jair Bolsonaro described migrants from Bolivia, Haiti, Senegal, and Iran as "the scum of the world and their children are arriving in Brazil, as if we didn’t have enough problems to solve".87 When Viktor Orban, the Prime Minister of Hungary, was speaking about migrants in 2018 he stated that, "we do not want our own colour, traditions and national culture to be mixed with those of others".88 In the USA, anti-immigrant policies are associated with higher amounts of perceived discrimination in migrant and non-migrant Latino groups, providing a basis for the unequal treatment of both migrant and ethnic minority groups.89 A further study from the USA showed the effects on health; areas with higher anti-immigrant prejudice were associated with increased mortality generally among minority ethnic groups, but the migrants themselves had lower mortality.90 This could also have intergenerational consequences. A prominent raid against Latino migrants, in which 900 agents of the US Immigration and Customs Enforcement arrested 389 employees in a meat-processing plant in Iowa in 2008, was associated with subsequent poorer perinatal outcomes (increased risk of low birthweight) among members of the Latino community.91 An example from the UK is the so-called hostile environment towards migrants created by the Conservative government leading to migrants and British citizens being denied health care. This hostile environment was recently highlighted in the Windrush scandal in 2018, in which British citizens who came to the UK from the Caribbean more than 45 years ago were deported, denied re-entry, lost jobs and accommodation, and were denied rights and benefits.
The sociopolitical context that leads to inequalities in health creates an accumulation of disadvantage throughout the lifecycle, and potentially over generations. Migrant related discrimination is a profound determinant of health, especially mental health and social wellbeing. Studies have shown the substantial mental health implications of living in a state of persistent unpredictability and uncontrollability over one’s future.92 Fear of deportation, discrimination, and targeted condemnation can influence a migrant’s willingness to seek care and maintain follow-up appointments, including to receive medical test results and follow treatment regimens. Studies indicate that the wider consequences of discrimination are substantial. It is estimated that Australia lost 3·02% of GDP (AUS$37·9 billion) over the period 2001–11 as a result of individuals experiencing some form of racial discrimination.93
Various countries have implemented interventions to address discrimination. For example, Canadian schools have implemented cross-cultural youth leadership programmes and anti-racism courses to equip students and staff to deal more effectively with racism.94 In South Africa, the Roll Back Xenophobia programme used community radio to help combat negative stereotypes of migrants and promote social inclusivity.95 However, efforts to raise awareness of and support the needs of particularly at-risk migrant communities have an uphill battle against nationalist forces, exclusionary systems, parsimonious resourcing, and service-level biases.
Environmental influences and hazards
Extreme environmental events and ensuing disasters can cause displacement of populations. These could be naturally occurring hazards, such as tsunamis, floods, earthquakes, or volcanic eruptions; pandemics of infectious diseases; or conflict and disaster, all of which form a complex driver of both internal and international migration. Importantly, the most substantial components of risk in a disaster are the vulnerability and exposure, rather than the environmental hazard itself.96 In this context, vulnerability refers to the susceptibility of an individual or population to the adverse effect of the hazard; the components of which are physical, social, economic, or environmental. Although disasters can result in an increase in vulnerability, they are also a consequence of the underlying vulnerability of communities, infrastructure, and processes because of poor preparation and mitigation.
The increase in extreme weather events has been linked to anthropogenic climate change,75,97 but global disaster deaths have reduced as a proportion of the population. This reduction is attributed to progress in Disaster Risk Reduction actions98 reducing the vulnerability of communities, infrastructure, and health-care systems, and through the establishment of early warning systems. Reactive policies to a crisis that fail to address vulnerability can amplify the social, economic, and environmental drivers that turn natural hazards into large scale disasters.99 The majority of disaster deaths occur in fragile and conflict-affected states where Disaster Risk Reduction is almost absent.100 Disaster Risk Reduction aims to increase resilience and reduce the risk of disasters.
Large disasters typically cost between 0·2 and 10·0% of annual GDP depressing the economy101 and these costs could be considerably higher for the lowest income countries. Following the 2010 earthquake in Haiti, economic losses equalled GDP.102 Large disasters can exacerbate economically driven migration trends, in the medium to longer term from rural to urban areas103 and internationally.104 However, for localised disasters, where effective aid equals disaster losses, there might be no net migration.105 Evidence from a longitudinal study over 15 years in Indonesia showed that mostly permanent migration generally did not occur in response to disasters, with the exception of landslides.106 However, there is contrasting evidence from the Caribbean islands, which had substantial post-disaster international migration, and tsunami affected Japan where large numbers of local working-age people and families from the Tohoku coast have permanently relocated to Tokyo and other large cities.107 Rising sea levels are likely to cause permanent migration of coastal populations in developing countries with the lowest likelihood of protection (eg, coastal defences), however the people living in these settings have strong abilities and desires to make their own mobility decisions.108 Evidence also shows migration into disaster areas after the disaster in response to government programmes to create jobs or as a result of economic migrants filling the jobs of displaced people. These inward migrants have heightened susceptibility to environmental conditions owing to lower social capital and poorer disaster awareness.
Slow-onset changes in land use and availability due to sea level rise, coastal erosion, precipitation, or agricultural degradation and sector loss will influence the pre-existing economic drivers of permanent migration.109 These changes might be caused by human interference, for example overuse of land or deforestation that renders the land infertile. Drought is a common cause of migration. For example, the drought in Odisha, India in 2001 resulted in 60 000 people migrating, mostly to the adjoining state of Andhra Pradesh in search of employment.110 Migration involves substantial costs and the people with fewest resources have the least capacity to move away, and so are the most vulnerable to harm. Furthermore, environmental change has the potential to even further diminish people’s resources, exacerbating the vulnerability of a population. A resulting sub-section of the population, with the least ability to move, can become trapped.111 This non-migration influenced by environmental change is of great humanitarian concern.
It is essential for areas at high risk of natural disasters to develop strong Disaster Risk Reduction actions to mitigate future potential hazards and minimise mortality. An example of where Disaster Risk Reduction is important are the Rohingya settlements in Bangladesh. The Rohingya are the world’s largest stateless population, stripped of citizenship in 1982 by the government of Myanmar. In late August 2017, renewed violence by the military of Myanmar spurred a rapid mass exodus of Rohingya (655 000 people in 3 months) to the south-eastern region of Bangladesh.112 These locations, such as Cox’s Bazar and Bandarban, are very susceptible to cyclones, flash flooding, and rainfall-induced landslides. This risk coupled with the temporary, makeshift shelters often created by cutting into mud hillsides render the Rohingya highly vulnerable to environmental disasters. There is an urgent need to conduct multihazard vulnerability mapping of the refugee camp and surrounding areas, conduct mapping of human mobility patterns, improve drainage capacities of refugee settlement areas, develop evacuation and relocation processes, examine resilience of existing health-care centres to potential hazards, and generate a post-disaster plan.113
Education for migrant children and adolescents
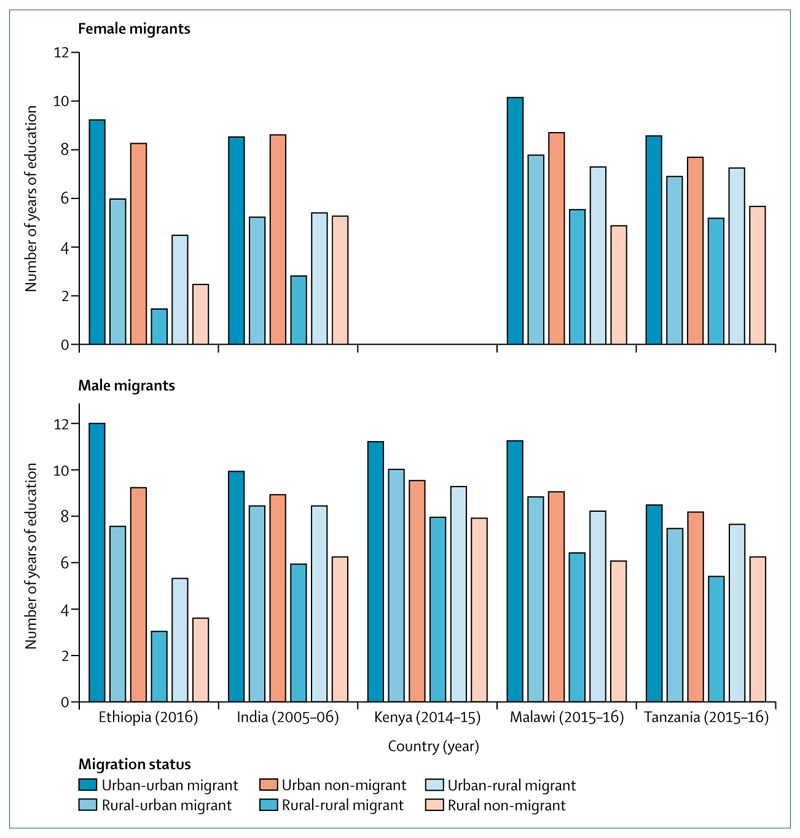
Education is essential for children and adolescents and is a determinant of future health and wellbeing. Education includes formal schooling, and acquisition of cognitive, social, and other soft skills that foster intellectual and social growth. Migration disrupts a child’s formal education, including difficulties accessing school. These difficulties have the potential to result in lost generations of educated adults, particularly for irregular child migrants and unaccompanied children. In a study of access to public schools in 28 developed and developing countries across the world, 40% of developed and 50% of developing countries did not allow immediate access to irregular migrant children.114 Migrant children might also be excluded from school in some countries because they have not undergone health screening,115 or they might miss school days because of their poor access to services to treat even simple illnesses. Migrant children in school can have poor educational attainment or decide to drop out because of language barriers, unsuitable materials, or teachers who are inadequately trained to support student integration. For migrant children with disabilities, obtaining an education can be especially challenging because few countries will prioritise adapting education and school structures or providing the necessary staff to ensure that children with disabilities can obtain a good education.116 Migrant students are more likely than native students to be placed in groups with lower curricular standards and lower average performance levels.117 An analysis of Demographic and Health Surveillance data from Ethiopia, India, Kenya, Malawi, and Tanzania on the association between mean number of years of education and internal migration status indicates that, on average, migrants have more years of education than non-migrants, with the exception of rural-rural migrants (figure 7). The differences in the educational attainment of female migrants and male migrants is notable among all groups, with males more likely to stay in school longer, especially among urban residents.
Figure 7. Weighted mean number of years of education by internal migration status35–39.
Internal migration in China is subjected to the Hukou system, which is a household registration system that establishes service entitlements by internal divisions on the basis of residency.118 These regulations can mean that internal Chinese migrants do not have access to their own public education system, or other services, because the child is not registered in the region that they live.119
However, where migration is managed well, children can integrate quickly into a new system with younger children assimilating particularly well. All children and adolescents, regardless of their status, should have access to education. According to the UN Convention on the Rights of the Child,120 states are responsible for making primary and secondary education available and accessible to all children, regardless of migration status. Primary education should be free and compulsory, and states should take progressive steps to make secondary education free as well. The UN Convention on the Rights of Persons with Disabilities121 also requires that governments ensure equal access to basic services including education for people with disabilities. A practical example of the inclusion of child migrants is the Reaching All Children with Education programme in Lebanon, which sought to integrate large numbers of migrant Syrian children into its public school system, while simultaneously improving access for Lebanese children.122 The programme increased the number of school places, waived fees, and provided education grants with encouraging results emerging.122
Health and safety of labour migrants
Migrant workers’ earnings can sustain households and influence entire economies. For some labour migrants (primarily highly skilled individuals with sufficient education, employment, financial, or citizenship credentials), migration poses few risks. In these circumstances, migration is generally advantageous for livelihoods, health, and wellbeing. However, the majority of labour migrants are less well situated, often originating from LMICs and seeking work in response to financial or safety needs.
Distress migration or economic migration puts migrant workers at particular risk of unsafe transit and pressures, sometimes with coercion to engage in unsafe work conditions. Low wage labour migration is closely linked to globalisation and supply and demand, especially for cheap labour. Migrant workers in these jobs are often among the most invisible of migrant populations. Not only are they likely to work in informal or even illegal sectors but they are also less likely to take part in the formal economy, engage with the local community, or use official resources. Their safety is also often hindered by poor social, economic, or legal status to assert their rights.
Labour migrants rarely migrate on their own without the assistance of labour intermediaries, which includes both formal agencies and informal migrant networks. Labour brokers have a fundamental role in linking individuals to jobs, however it is not unusual for recruiters to charge exorbitant fees, causing migrants to incur substantial debt. Recruitment agents, including from a migrant’s own social network, often facilitate third-party contractual arrangements, day labour, piece-work, and similar precarious employment and pay arrangements. These arrangements lead to long hours, exhaustion, and serious health hazards. For example, Bolivian migrant workers have been led to seek jobs in harsh working conditions in textile workshops in Argentina through their social networks.123
Although labour migration has served to advance global markets and offer greater livelihood opportunities, there is growing recognition of the often exploitative and hazardous nature of many work sectors and their adverse effects on health and wellbeing, particularly in emerging economies. The health and wellbeing of migrant workers is directly related to their working and living conditions and influenced by broader social conditions (table). Harmful labour situations are not uncommon for many migrants, especially individuals in low wage sectors. Employment destinations frequently involve hazardous working arrangements, dangerous tasks, and unsafe or unhygienic living conditions. For example, commercial fishing is considered to have some of the most hazardous work conditions—especially in situations of exploitation or so-called sea slavery. A study among trafficking survivors in the Thai fishing industry reported higher injury rates than non-trafficked fish industry workers. Additionally, in the fishing industry more trafficked workers were subjected to severe violence, compared with non-trafficked workers (table).124
Table.
Low wage labour sectors and associated occupational hazards among migrant workers (see appendix for full list of references)
| Examples of occupational hazards and harm | Migrant health study findings | |
|---|---|---|
| Sex work | Poor condom negotiation or use can cause sexually transmitted infections and unwanted pregnancy; sexual violence and confinement can cause anxiety disorders and depression | Migrant female sex workers in Benin, Ethiopia, and Kenya are at greater risk of HIV than non-migrant sex workers and higher risk of acute sexually transmitted infections in all settings |
| Construction | Work at heights can cause fatal falls and disabilities; heavy lifting can cause musculoskeletal problems; poor personal protective equipment can cause respiratory disease, dermatitis, and eye injury | In the USA, Latino construction workers were nearly twice (1·84, 95% CI 1·60-2·10) as likely to die from occupational injuries as their non-Latino counterparts |
| Manufacturing (eg, textiles) | Repeated bending and fixed postures can cause musculoskeletal damage and pain; sharp instruments can cause puncture wounds; dust particles can cause silicosis | In Malaysia, 64% of migrant workers had musculoskeletal pain caused or worsened by work compared with 28% of Malaysian non-migrant manufacturing workers |
| Commercial fishing | Environmental exposures (sun, cold, rain) can cause skin cancer, dehydration, frostbite; long hours and weeks with no break can cause exhaustion and pneumonia; unstable fishing vessels and inadequate life vests can cause drowning; fishing net and knife hazards can cause deep cuts and lost limbs | Survivors of trafficking working in the Thai fishing industry reported higher injury rates (47%) than non-trafficked fish industry workers (21%); 54% of trafficked fish industry workers experienced severe violence versus 10% of non-trafficked fish industry workers |
| Agriculture | Pesticide exposure can cause toxicity; environmental exposures (heat, cold, mosquitoes) can cause dehydration, kidney failure, headaches, and malaria; heavy lifting and bending can cause repetitive injury syndromes | In one greenhouse in Oman, 95% of workers were migrants; poor practices related to pesticide use resulted in numerous health problems, such as skin irritation (70%), headaches (39%), and vomiting (30%) |
| Domestic work | Physical, sexual, and verbal abuse, and social isolation can cause depression, anxiety, and suicide; extensive working hours and food deprivation can cause exhaustion; repeated lifting, bending, and reaching can cause musculoskeletal strain; chemical cleaning agents, cooking, ironing, and knives can cause skin damage and burns | A 2-year study in Kuwait found that hospital admission rates for domestic workers (93% from India, Philippines, and Sri Lanka) were 1·86 times higher than for Kuwaiti women (non-domestic worker control group); stress-related disorders were more common (49% vs 22%) in housemaids (of whom a majority are migrants) than Kuwaiti women |
| Mining and quarrying | Mercury extraction, lead exposure, and mineral dust can cause mercury poisoning (gold-mining), neurotoxic disorders, and pneumoconiosis; heavy lifting, falls, and falling rocks can cause fatalities, traumatic injuries, and disabilities; heavy equipment, long hours, and repetitive lifting can cause noise-induced hearing loss, long-term fatigue, and musculoskeletal injuries; remote locations can cause malaria and put individuals at risk of venomous snake bites | China’s Ministry of Health reports that 87% of occupational disease is pneumoconiosis (black lung disease), with a mortality higher than 20%; pneumoconiosis is a chronic lung disease that often affects miners, sandblasters, and metal grinders, occupations undertaken primarily by internal migrant workers |
| Forestry | Environmental exposures (heat, cold, mosquitoes) can cause dehydration, malaria, and infection with parasites; falls, sharp tools, and machinery can cause fatalities, broken bones, and lacerations; repetitive motions and long hours can cause pain, strains, and long-term fatigue | A study of Burmese migrants found 87 (83%) of 105 rubber plantation workers had a suspected case of malaria in the past year; workers had poor access to care because of their working hours and poor transportation |
| Leather and tanning | Chemical exposure (ie, chromium, benzene dyes, formaldehyde) can cause respiratory illness, ocular damage, cancer, ulcers, toxicity, dermatological diseases (rashes), and chronic or allergic bronchitis pulmonary tuberculosis | Higher morbidity rates were found in tannery workers (40%) than the control group (20%) in northern India |
| Brick kilns | Unsanitary environments and air pollution can cause bronchitis, asthma, silicosis, and respiratory toxicity; very high heat can cause burns and fatalities; high rates of child labour resulting in developmental problems for those children | Migrant brick kiln workers in south India had higher prevalence of chest symptoms (9%) versus general population rates (5%) related to occupational hazards and poor health-care access |
As for all migrants, health protections such as health entitlements or health insurance, occupational safety and health regulations, and reliable social support are often not easily accessible, particularly for low wage sectors and informal work. In addition to the common barriers to care for migrants, migrant workers worry about missing work to seek medical care. Especially when workers are paid by piecework or are struggling to pay off debts, missing work is very difficult. Moreover, if the medical recommendation for injuries or illness is rest and time off, day-wage workers are unlikely to heed this advice. In locations where there are regional accords for cross-border labour migration, it is still not unusual for workers to avoid seeking medical care for fear of being dismissed for injury, illness, or for missing work. Migrant workers might be covered by insurance in some instances. However, even individuals who are insured might not understand that they are insured or that they have the right to seek care without paying. For example, in a study of Bangladeshi domestic workers in Singapore,125 72% did not know if they had received information about company-paid insurance, and of those individuals that had received information, 68% did not receive it in their native language.
The diverse group that comprise labour migrants encounter major health risks often related to employment policies, which are inadequate to ensure worker health and safety. Most low wage sectors are poorly regulated or inspected for protections against occupational hazards and stressors, including fair wages, financial insecurity, poor psychosocial work environments, exploitation, and verbal or physical abuse.126,127
Migrant workers’ health has been included in international frameworks such as WHO Healthy Workplaces: a model for action: for employers, workers, policy makers and practitioners.128 However, migrants often do not qualify for medical subsidies and are frequently not covered by the health-care financing schemes that protect citizens.129 Where such entitlements do exist, work to date suggests that interventions should be directed towards improving migrant workers’ knowledge of workplace health and safety and about their health-care entitlements to improve their uptake.130 There have also been questions about whether the welfare state is a driver of migration. Research in the USA found little evidence for a link between welfare generosity and internal migration across states.131
Migrant workers’ human rights to health are often severely restricted. Three UN agencies jointly found that "migrant workers are among the most vulnerable workers in the world, often subject to exploitation, discrimination, and abuse, lacking access to mechanisms for remedy and redress and in constant fear of deportation".132 Only a small minority of migrant workers globally who sustain occupational injuries receive medical treatment.133 A report on the ten most notable human rights violations affecting global business included recruitment of migrants and refugees into forced labour, a near-absence of information on labour practices deep within the supply chain, and inadequate oversight of suppliers.134 From a human rights stand-point, the right to health requires states to ensure occupational health and safe working conditions in accordance with the International Labour Organization occupational health conventions 155 and 161, and regardless of immigration status. SDG 8, on decent work and economic growth, calls on governments to “protect labour rights and promote safe and secure working environments for all workers, including migrant workers…”,135 and the UN General Assembly has called for adequate workplace health and safety and protection against violence and exploitation of migrant workers.136 Nonetheless, states with substantial numbers of migrant workers often obstruct migrant worker freedoms and safety. For example, in the Gulf Cooperation Council member states, the kafala or sponsorship system restricts workers’ ability to change or leave their job without their employer’s permission, or challenge any unfair treatment by the employer (see access to health systems section and supplementary table 2 in the appendix).137 These restrictions have allowed private sector employers to pay exploitative wages, engage in unprotected hazardous work, and force workers to live in crowded, squalid, and unhygienic living quarters.
Section 2. Achieving safe and healthy migration
A strong case for action on migration and health exists, and evidence indicates that safeguarding the health of migrants will have positive effects for global wealth and population health. Countries have a moral and legal obligation to respect the human rights of migrants, although these obligations are not always respected by states. Over the past century, multilateral agencies and nation states have moved the migration and health agenda forward through various notable instruments and events (figure 8). One of the key challenges in progress on advancing the migrant health agenda is the cross-cutting nature of the migration health topic, which demands sustained multisectoral and intersectoral partnerships and policies for meaningful action. Policy developments at global, regional, and national levels since 2008, when the first World Health Assembly resolution 61.17 on the Health of Migrants was adopted, have shown evidence based practices on how to overcome such challenges. Successes have occurred through whole-of-government and whole-of-society approaches. Examples of these successes can be seen in national migration health policy development by countries such as Chile and Sri Lanka, multi-stakeholder coordination platforms including civil society and academia (eg, the Joint UN Initiative on Migration, Health and HIV in Asia and the Joint Initiative on the Health of Migrants and their families in Central America and Mexico), and implementation of comprehensive refugee responses (eg, in Uganda where provision of comprehensive health care to refugees is integrated within health facilities also serving host communities).
Figure 8. Historical evolution of the migration and health agenda: selected international instruments and events.
IOM=International Organization for Migration. OCHA=UN Nations Office for the Coordination of Humanitarian Affairs. UNGAHLD=UN General Assembly High-level Dialogue on International Migration and Development. WHA=World Health Assembly.
Most of these instruments include important principles supporting the health of migrants and propose several measures for consideration by member states and stakeholders to achieve health for all migrants. It is time for the health community to strongly advocate for all individuals who migrate to ensure safety and access to health for all and to hold governments accountable to the migration policy instruments and conventions.
In section 2, we review these policy instruments and conventions and the mechanisms by which states can be held accountable for a migrants’ right to health. We then explore how, in addition to these conventions, health services can be developed to protect and improve the health of migrants.
Strengthening respect for migrants’ rights
Migrants’ right to health
The right to the highest attainable health extends to all individuals who migrate, regardless of their circumstances of migration or their legal status. International human rights treaties, most notably the International Covenant on Economic, Social and Cultural Rights, guarantee “the right of everyone to the enjoyment of the highest attainable standard of physical and mental health”.78
States are obligated to respect the right to health by not interfering in its realisation, such as through policies that exclude some people from health programmes. They should also protect the right to health by ensuring that third parties do not interfere with this right, such as by discriminating against migrants. Also, states should fulfil the right by ensuring the provision of health services that meet essential elements of availability (economic, physical, and geographical, non-discriminatory accessibility, cultural, and other forms of acceptability) and adequate quality. However, these rights do not necessarily translate into entitlements and often states are implicit in this discrimination.138
For refugees, the Convention Relating to the Status of Refugees and its Protocol guarantees the right to “the same treatment with respect to public relief and assistance as is accorded their nationals” (Article 23), which has been interpreted to mean access to health services equivalent to the host population.139 However, health care for refugees is often poor because of inadequate resource allocation by front-line refugee-hosting countries and because states with large numbers of refugees, such as Jordan and Lebanon, are not signatories to this treaty. Difficulties can also arise for refugees resettling in non-signatory states where the law does not guarantee their right to access health care, social services, education, or employment.
For internally displaced persons and irregular migrants, access to health care is often severely restricted. Many states grant irregular migrants access only to emergency care, a practice that is both overtly discriminatory and is inconsistent with good public health practice for the host population and for migrants. In Europe, some states have shown that a humane response to migrant health is possible140 and expanded access to health services for migrants, especially for asylum seekers and children without regular documentation status. However, there remain major disparities in entitlements to access to health care on the basis of legal status (see supplementary table 3 in the appendix).
Ensuring limits to health-related restrictions on entry
According to UNAIDS, as of June 2015, 35 countries have imposed some form of travel restriction on people with HIV.141 Of these, five countries completely bar the entry of people who are HIV-positive, four countries require proof of HIV-negative status even for short-term stays, and 17 countries deport people who are found to be HIV-positive (see supplementary table 4 in the appendix). States impose other health-related restrictions on entry on the basis of infectious disease, communicable disease, drug dependency, mental illness, pregnancy,142 or cost of care, and permit deportation on these grounds (see supplementary table 5 in the appendix).
These restrictions on entry or deportation for diseases with low risk of casual transmission, such as HIV and AIDS, leprosy, and hepatitis C, are impermissible on both public health and human rights grounds.143,144 The policies violate migrants’ right to health and the ability of migrants with disabilities to enjoy the right to freedom of movement, choice of residence, and nationality on an equal basis with others.121,145 Linking health status to migration enforcement reinforces distrust of the health system and limits migrants’ ability to access health care on a non-discriminatory basis.8,146
In practice, health-related enforcement regimes can pressure health workers to act as immigration control agents. This practice violates their professional ethical requirements as practitioners, an issue that has been taken up by civil society organisations like Docs Not Cops in the UK. Deportation can interrupt medical treatment, and deportation on the grounds of pregnancy also violates women migrant workers’ rights to privacy, bodily autonomy, and reproductive choice; as well as their right to equal treatment, equal employment rights, and freedom of movement.7,8,145,147 Protection of the public is often invoked as a basis for these policies. However, if public health is invoked as a basis for denial of entry or deportation, the Siracusa principles relating to limitations on civil and political rights demand that the policy be necessary to protect public health, be based on evidence, be the least restrictive means available to accomplish the public health objective, and be applied without discrimination.8,148 Further, screening for highly contagious diseases should be done voluntarily and with informed consent, include pre-test and post-test counselling, and be confidential.149 Mass screening at entry for HIV, pregnancy, and disability is never permissible.149 Care should be taken that where pre-entry screening programmes operate, they do not represent a barrier to individuals seeking to migrate.
Several HICs impose residence restrictions on the basis of claims of high treatment costs, especially for migrants with particular chronic diseases or disabilities. For example, according to Australia’s Migration Act and Regulations grant, the Minister for Immigration and Border Protection can use their discretion to reject permanent residency applications if an applicant has a health condition for which treatment is “likely to result in significant health care and community service costs to the Australian community”.150 However, applicants for specific visas (including particular humanitarian, family, and skilled work visas) can apply for a waiver of the requirement.150,151 The five most common reasons for rejection on health grounds are intellectual impairment, functional impairment, HIV, cancer, and renal disease.152 As described earlier in relation to infectious diseases, these restrictions violate the rights of people with disabilities to liberty of movement and choice of residence.121 As such, the implementation of the law should be reasonable and proportionate to achieve a legitimate end. All too often, cost based restrictions are applied in an arbitrary manner across the board without individualised determinations. Also, they often do not adequately consider the potential economic, social, and cultural contributions that migrants with disabilities make to their host communities and countries, instead considering them only in terms of cost to the state.153
Protection of refugees and asylum seekers
The 1951 Refugee Convention and Protocol79 provides specific protections to refugees. Its centrepiece is Article 33, prohibiting non-refoulement, or the return of a refugee to a country where his or her life or freedom would be threatened on account of race, religion, nationality, membership in a particular social group, or political opinion. The Convention and Protocol also prohibit states from penalising refugees seeking protection for unauthorised entry or presence, whether through criminal prosecutions, arbitrary detention, or the imposition of other penalties, so long as they present themselves to authorities and show good cause for entry.79 States may not discriminate against refugees on account of race, religion, or country of origin. Equivalent protections apply to internally displaced persons, including freedom of movement and the right to leave a country and seek asylum elsewhere. Although 43 states have neither signed nor ratified the Convention and Protocol—including countries such as Bangladesh, Jordan, and Lebanon, which host sizeable refugee populations—these states are indirectly obligated to respect the principle of non-refoulement and other rights of asylum seekers and refugees through other relevant international instruments like the International Covenant on Civil and Political Rights.145
Among other rights guaranteed by the Convention, Article 17 requires receiving states to provide refugees with the same right to wage earning employment as nationals of a foreign state in the same circumstances, and the non-discrimination provisions of human rights laws do not permit distinctions in work based on nationality or migrant status. However, only half of the signatories to the Convention and Protocol grant refugees the right to work.154 As a result, refugees have to work unlawfully, if at all, which means they often encounter other rights violations and are at an increased risk of trafficking.
Gaining adherence to the requirements of the Refugee Convention and Protocol has been challenging, as a mechanism is not included for reviewing state compliance, so there is no or little accountability. Further, to avoid their duties to refugees and asylum seekers under the Convention, states often erect barriers to asylum seekers crossing into the country. These include providing incentives to neighbouring states to prevent asylum seekers travelling through those states from reaching the border, detaining asylum seekers for long periods of time, and criminalising unauthorised entry. Another strategy, adopted by the EU through the EU-Turkey deal, has been the return of refugees, who are fleeing the conflict in Syria, to Turkey; this has been on the grounds that Turkey is a safe third country. Yet, Turkey does not recognise all rights of Syrian refugees under the Convention. These barriers to entry often increase the health risks facing asylum seekers, leave them in difficult and dangerous situations, and push them to turn to irregular travel. The UN Global Compact on Refugees should address some of these concerns by strengthening support for immediate and ongoing refugee needs and offer incentives for good practice through assistance to national and local institutions and communities receiving refugees. However, the Compact on Refugees does not ensure strengthened enforcement or accountability.
Human rights of children in forced migration
Migration enforcement policies directed at adults, including detention and deportation, inevitably affect children.155 Children of parents who have been deported experience increased emotional and psychological symptoms.156 The UN Convention on the Rights of the Child120 guarantees civil, political, economic, social, and cultural rights to all children, irrespective of migration status or citizenship. The Convention requires that states act in the best interests of the child.120 Identifying the best interests of the child requires a comprehensive review of the child’s circumstances and ability to exercise basic rights, such as to education, health, and family unity. Children’s rights to life, survival, and development (Article 6) provide a framework for migrant and refugee children’s rights in host countries. States should ensure equal opportunity, access to services, and the chance for all children to thrive and reach their potential.120 As in other dimensions of international migration, however, national laws affecting child migrants often do not adhere to human rights requirements, treating children and adolescents as foreigners first, and often prioritising immigration enforcement policies over children’s rights.157
Immigration detention, human rights, and health
States are increasingly treating unauthorised border crossing as a criminal offence and detaining immigrants, regardless of circumstances. In 2018, the USA announced a zero tolerance policy for unauthorised border crossings, announcing that it would prosecute 100% of such crossings as crimes, regardless of whether the migrants included family groups with children. As a result, migrants have been arrested and jailed, and children, including very young children, have been separated from their parents.158
Evidence repeatedly shows the range of negative health consequences associated with detention, especially for children and adolescents. We systematically reviewed 38 peer-reviewed studies on the effects of immigration detention on health outcomes (Ramos et al, unpublished data). We found that most of the studies concerned male adults originating from Middle Eastern countries who were detained in Australia (38%) or the UK (22%). All studies showed negative health outcomes attributable to detention, especially mental health disorders. However, these studies are often limited by methodological constraints.
Detention poses clear violations of one of the most important international agreements, the International Covenant on Civil and Political Rights,145 which states that “everyone has the right to liberty and security of person. No one shall be subjected to arbitrary arrest or detention”. The 1951 Refugee Convention and Protocol79 established protections prohibiting penalising refugees because of entry without documented permission or presence and restrictions on movement other than those that are necessary, such as to verify identity or protect national security.159 Detention is only warranted when persuasive evidence exists that the individual poses a danger to the community, or is likely to flee to avoid further immigration proceedings, and must be of short duration.160 For children, the Convention on the Rights of the Child120 permits states to use detention “only as a measure of last resort and for the shortest appropriate period of time”.The UN Committee on the Rights of the Child found that immigration detention of children is never in the best interests of the child.161
However, throughout the world, detention of irregular migrants, including asylum seekers, is often used routinely, arbitrarily, and for an indefinite period.162 Conditions in detention facilities are often substandard, failing to meet needs for adequate food, clean water, health care, light, space, safety, and sanitation with consequences for health.163,164 Detainees, especially children, are commonly subjected to violent victimisation, including abuse and rape.165 Detention also impairs immigrants’ access to other human rights that can have profound and long-lasting effects on health, such as obtaining housing, education, employment, and pursuit of claims for asylum. Numerous human rights and health experts have called for gradual abolition of immigration detention because of its arbitrariness, detrimental effect on health, and flimsy justification.166
Gender, law, and health
As noted, health and migration are both highly gendered, affecting women, men, and sexual minorities differently. Discriminatory laws frequently sustain or foster health inequalities by gender, rather than protecting individuals, especially for women and girls and sexual minorities. For example, host countries are often governed by plural legal systems that severely limit women’s and girls’ rights to access contraception and abortion, avoid early marriage, and escape violence. Additionally, in humanitarian aid settings, implementing agencies often apply host country laws rather than international standards to determine the scope of access and rights of migrant women and girls. Examples of discriminatory laws in countries with very high numbers of displaced people are described in panel 2.
Panel 2. Gender, law, and health: a four-country analysis.
Rape, sexual servitude, child marriage, and sex trafficking lead to substantial risks of transmitted infections, poor maternal health outcomes, and enduring mental health problems. However, access to protections, medical treatment, and legal recourse, especially for women, are often dictated and constrained by laws and customs. An in-depth legal analysis of four countries in which migrants form a substantial portion of the population, Chad (519 968 total migrants), Jordan (3 112 026 total migrants), and especially in Lebanon (1 997 776 total migrants) and Turkey (2 964 916 total migrants), shows the highly gendered, and sometimes contradictory, nature of the laws and customs governing the rights and safety of women and girls (see supplementary table 6 in appendix). Among Syrian refugee communities, for example, rates of child marriage are high.167 Although many countries have established a legal minimum age of marriage, the practice of early and forced marriage prevails because of weak law enforcement, cumbersome marriage registration laws, and cultural norms. In Jordan, for example, the legal age of marriage is 18 years, yet children can be married with the approval of a Sharia court judge from age 15.168 Although Chad criminalises child marriage under the age of 18 years, the child marriage rate was 68% between 2004 and 2017.
Although countries might sign conventions and draft legislation against gender-based violence, migrant women are often unable to access justice because of cultural norms, language barriers, and poor legal representation. Countries often have plural legal systems that provide complete defences or reduced sentences for honour crimes. In Chad, for example, adultery is a criminal offence and murders committed because of adulterous behaviour are considered excusable. Women inhabiting migrant camps have faced months-long detentions on the grounds of adultery, while men rarely face punishment for rape and sexual assault.169 In both Jordan and Lebanon, perpetrators can avoid prosecution by marrying their victims170 as marital rape is not a crime in many host countries.
For unmarried and displaced adolescent girls, failing health systems, few providers, and poor domestic legal frameworks are substantial barriers to reproductive health service access. Individuals under the age of 18 years must obtain parental consent before receiving or undergoing any sort of medical treatment,171 including receiving contraceptives, in Jordan, Lebanon, and Turkey; in Jordan, spousal consent is also required.172 Migrant women also have poor access to abortion in the four countries reviewed. In Chad, Jordan, and Lebanon abortion is not legal in cases of rape.
Globally, intimate partner violence affects one in three women,173 and displacement appears to exacerbate conditions of abuse,173,174 triggered by destabilisation of gender norms and roles, men’s substance use, women’s separation from family, and rapid remarriages and forced marriages. Laws are often insufficient to protect women from sexual abuse. For example, among the migrant-recipient countries analysed, only Turkey has legislation against marital rape and only Chad allows termination to save the life of the mother, even in cases of rape. Countries are often reluctant to make commitments to protect women. Only Chad has signed and ratified without reservations the Convention on the Elimination of All Forms of Discrimination against Women147 and its accompanying Optional Protocols. Although international instruments such as these and the UN Convention on the Rights of the Child120 exist to protect women and children, implementation is often poor, especially during humanitarian crises. Dismantled or ineffective justice systems result in weak protections and responses for sexual and gender-based violence.175 Additionally, even when laws are in place, migrants who have a tenuous legal status or are not aware of their rights, are much less likely to benefit from health protections and medical treatment.
Some promising programmes and interventions exist to enhance gender justice for forcibly displaced people. For instance, the UN Development Programme, the UN Population Fund, and local partners launched a project to protect female migrants in refugee settlements in Iraq from exploitation, human trafficking, forced and underage marriages, and sexual and gender based violence.176 This project offers novel opportunities for female Syrian refugees to receive free and long-term legal assistance in addition to counselling and psychosocial support.176 The work of the Rights in Exile Programme, formerly known as the Fahamu Refugee Programme, is also notable for consolidating resources to support migrant legal aid advisers and advocates,177 and has gathered resources for legal advisers providing support for LGBTI migrants.178 Gender responsiveness, which focuses on respecting human rights, is referred to in 12 of the 23 objectives in the Global Compact for Migration.
Access to justice
Poor access to justice can lead to adverse health outcomes. People who migrate, for whatever reason, have the same rights to access justice as all other people under the International Covenant on Civil and Political Rights.145,179 Yet, migrants encounter numerous obstacles to justice systems, (eg, for violations of workplace rights and fair adjudication of asylum claims). Access to justice is frequently stymied by poor information, employer intimidation, lack of access to legal counsel, language barriers, and unfamiliarity with procedures. Individuals in refugee camps or settlements face difficulties accessing justice180 because camps are often located in remote areas where courts are absent, legal representation is scarce, and judicial systems might be weakened by civil unrest and war. Frequently, people are also unfamiliar with formal legal systems and further hindered by poor education, language barriers, and previous reliance on informal, local justice systems.181
Health services for mobile populations
Universal and equitable access to health care before, during, and after migration
One of the most promising measures to address health inequities is access to health care through universal health coverage. Migrants have a right to health and universal health coverage is a key strategy for the realisation of that right. Universal health coverage is a structural intervention under which “all people and communities can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship”.182 Making universal health coverage truly universal will promote SDG 3.8, which recommends “financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all”. Creating such systems that integrate migrant populations will benefit entire communities with better health access for all and positive gains for local populations. Therefore, this coverage should be championed by politicians and health-care leaders. To examine the potential role of this coverage to improve health in relation to global migration, we focus first on the health system and access for migrants, building on published work183 on transforming health systems towards SDG 3 targets and our conceptual model (see supplementary figure 6 in the appendix) to ensure healthy lives and promote wellbeing for all at all ages. We build on established health system analytic frameworks by addressing governance, health financing policy, health information systems, and the health workforce with a focus on migration.
Equitable access to health systems
A health system is the collection of people, institutions, and resources that aim to improve, protect, maintain, and restore health.184 How health systems are conceptualised and structured is primarily linked to nation states and their constituent units. Migration can create challenges for health systems due to people crossing between system boundaries. That is, health systems are generally delimited by geopolitical borders, which has made it difficult to assess how they might be strengthened to become migrant-inclusive. This difficulty is particularly found in situations of conflict that result in the spatial reorganisation of health systems within and across borders. These transformations can complicate the inclusion of displaced populations into health systems.185 Considerations for a health system that aims to be inclusive cover addressing heterogeneity in service delivery, ensuring cross-jurisdictional networking and interoperability, and protecting the rights of individuals and communities to access health services. Indeed, analysing health systems requires people-centred frame-works that are sensitive to individual and population care needs rather than determined by jurisdiction.
Level of access varies globally with published data providing some examples of good practice (see supplementary table 3 in the appendix). We did a secondary analysis of data from the Migrant Integration Policy Index (see supplementary panel 1 in the appendix), which complemented our analysis of access to health care in European countries (Law and human rights section). In our Migrant Integration Policy Index analysis, Italy received the highest rating of all countries, having a notably inclusive system that provides for asylum seekers and legal migrants under the same system as nationals. In Italy, undocumented migrants have access to wide health coverage, which is specified in the country’s law. Countries that scored poorly required migrants to pay for specific insurance when the national population was not required to, did not provide any exemptions for migrants, and detained undocumented migrants identified by health-care systems.
Drawing on the patient centred access framework by Levesque and colleagues,186 we developed a new people-centred health systems framework for migrants’ access to health and social protection (figure 9). Our framework is underpinned by concepts of equity to emphasise human rights and equal access to health care regardless of status. The framework explicitly defines health and social protection by highlighting both the supply side, or accessibility of services and determinants of health, such as water, nutrition, and sanitation; and the demand side, or the ability to access services. Both the demand and supply side are influenced by geographical, economic, and institutional factors, including law. These supply side and demand side factors exist within the broader context of how governance institutions define and protect the rights of people (including migrants and other marginalised groups equitably) to access and use health services and determinants.187 Guided by this framework, we reviewed the health system accessibility as it relates to migration.
Figure 9. A health systems framework for migrants’ access to health and social protection.
Factors on the supply side can affect demand and vice versa. Adapted from Levesque et al, 2013.186 *Social and cultural ability.
Overcoming barriers to health services
National regulations, private employer’s provision of health, or legal status coverage all interact with accessibility and create barriers to health services. Some countries, such as Kenya, have national treaties or constitutions that assert the right to health care for every person. Despite such legal protections, compared with Kenyan patients, migrants often continue to encounter obstacles including harassment, cost differentials, administrative issues, and language barriers.188 Differences between189 and even within190 countries in the rights of migrants to access health services are striking.
Unaffordable health services remain a substantial barrier for many migrants (eg, among Syrian refugees in Jordan, cessation of free access to health care is taking a negative toll on the health of refugees).191
Fear of deportation is of importance to undocumented migrants or unsuccessful asylum seekers, especially in locations where public health workers have a so-called duty to report undocumented migrants. These mandates contradict the fundamental ethics of health workers to do no harm, can hinder individual and public health, and result in further criminalisation of migration. Data from Doctors of the World’s European clinics suggest that the contradictions between health and immigration goals are considerable and growing across Europe.192 As a result, individuals with irregular status or who are displaced without a regular residence often avoid making themselves known to formal services.
Logistical challenges to provision of health services compound these hindrances, including transportation, job commitments, waiting times, or poor knowledge of how to navigate the medical system.193 Migrant workers who are paid by piecework or by the hour can rarely afford to sacrifice the time and income to seek medical care until it is urgent. To overcome these issues, health and social services might need to be taken closer to people, be available in more places, and be more mobile to achieve good access. As a result, various services have come to understand that medical care and health promotion campaigns need to be mobile to reach vulnerable migrant populations who are at the greatest risk of harm, which encorporates human rights approaches and equal access. Panel 3 outlines examples from the USA of mobile health services and other examples including mobile clinics such as the La Caravana de la Vida (The Life Caravan), which reaches artisanal gold miners in Madre de Dios, Peru.200
Panel 3. Health care for migrant and seasonal farmworkers in the USA: improving access and cultural competence.
A high proportion of migrant and seasonal farmworkers in the USA are uninsured or underinsured, due to both eligibility issues and very low incomes. It is estimated that at least 75% of farmworkers, and up to 90% of their children do not have health insurance.194 Many of these individuals do not qualify for government provided or subsidised insurance (eg, Medicaid) because they are undocumented.
There are positive examples of programmes that have been established to address the health needs of these populations. At a national level, the Health Resources and Services Administration funds 137 migrant health centres and 955 community health centres across the USA aimed at improving access to services for marginalised groups such as farm workers. This assistance includes a voucher programme enabling farmworkers to obtain care from community centres, and funding non-profit organisations such as Migrant Health Promotion, and Farmworker Health Services.194 However, a substantial gap in the literature exists in terms of robust assessments of the effectiveness or acceptability of such programmes. There are also numerous local programmes in the USA focused on accessible, culturally appropriate health assessments. Mobile outreach clinics for migrants exist for uninsured farmworkers who are considered to be working in a hazardous industry and are mostly foreign migrants. There are also clinics targeting farmworkers in the USA,195 and the Migrant Health Outreach programme (federally funded) mobile clinic for farmworkers staffed by nurses, which seems to be a successful approach.196 Outreach services offer the benefit of going to the locations where migrants are working, living, going to school, or to houses of worship,197 reducing many of the main access barriers. In the USA, for example, an estimated 1500 mobile clinics exist, receiving 5 million or more annual visits nationwide, which are becoming an integral component of the health-care system to serve vulnerable populations. Findings from a study on outreach to migrants and seasonal farmworkers in the USA shows that workers and their families make very restricted use of clinic-based services because of their mobility (constant residential changes), work hours, and poor knowledge of the US health system (almost 40% of the population is new each year). A majority prefer to seek care in Mexico, even individuals who have US health insurance; however, clinic outreach programmes are overcoming many of these barriers. Nevertheless, research suggests that mobile clinics for migrants have been more often disease-focused, to offer testing and treatment (eg, for HIV, especially for sex worker populations).197,198 Evening cluster clinics targeting migrant workers were considered by migrants themselves to be excellent or good.199 Six characteristics were believed to contribute to the successful delivery of health care and education through cluster clinics, including provision of both direct and referral services for this underserved population, comprehensive delivery of services in a single setting, collaborative delivery of services, access-driven delivery of services, delivery of culturally sensitive and linguistically appropriate services, and evidence-based service delivery. Free or mobile clinics and health and wellness programmes specially targeting migrant workers are relatively rare.
An understanding is emerging on the ways health needs in conflict-affected settings can be supported by telemedicine with digital health technology, such as cellular technology or cloud-based solutions.201 However, these technologies require rigorous assessment and monitoring during roll-out with particular attention paid to possible intervention induced inequalities. Implementation should be undertaken with evidence-based models, but if successful, such systems could help achieve SDG 3 indicators and foster better data collection among populations that are especially likely to be left behind.
Governance and leadership of universal health-care systems
Governance and leadership in the development of universal health-care systems that facilitate safe and successful migration processes have been absent until now. The current focus on provision of universal health coverage is therefore an exciting opportunity for this leadership vacuum to be filled. Such leadership commitment, as shown by the current WHO Director General, Tedros Adhanom Ghebreyesus, needs to be followed by concrete actions and be inclusive of migrants, in all countries and globally through better coordinated leadership across the UN system.
The importance of migrant health was emphasised by the World Health Assembly (resolutions 61.17 in 2008 and 70.15 in 2017). WHO Europe then created a “strategy and action plan for refugee and migrant health in the WHO European Region”.202 This document sets out various actions for inclusion of migrants into health systems. We specifically call for member states to take positive action in this respect, particularly through: appointing a government migration and health focal point that can engage multiple sectors; integrating migrants into existing national health structures and health systems; and providing inclusive health and social care that appropriately meet migrants’ needs.
These calls to action and strategic frameworks have not been implemented by many countries and more work is urgently needed to ensure existing policies and guidelines around migration and health are fully implemented. Exceptions to the lack of progress include how Switzerland has shown leadership in the provision of open health systems for all migrants, and countries such as China (panel 4) have made substantial progress in improving access for internal migrants.
Panel 4. Leadership in migrant population accessibility and affordability of health-care services.
China
Since the launch of the new round of medical reform in 2009, China has almost achieved full coverage of its medical insurance system for urban and rural residents, with a stable coverage rate of above 95% for the whole population. The medical insurance system mainly consists of three types of schemes, including urban employee basic medical insurance, urban resident basic medical insurance, and the new rural cooperative medical scheme. Among these, the number of people participating in the new rural cooperative medical scheme reached 670 million, with a coverage rate of 98·8%. However, despite the high coverage rate achieved, there is a definite difference among the coverage scope of the three medical insurance schemes, with a higher insurance level provided by urban employee basic medical insurance and urban resident basic medical insurance than by the new rural cooperative medical scheme. In addition, because the off-site medical expense settlement information system for new rural cooperative medical scheme has not been fully established, medical expenses of migrant populations cannot be directly deducted when they seek medical care in urban areas. Many migrants have to pay medical expenses first out of pocket then return to rural areas for reimbursement. Besides, the reimbursement review procedures are quite cumbersome and usually take a long time, resulting in a considerable number of migrants being without definite insurance security.
Faced with the demand of nearly 200 million migrants, in 2016, the Chinese Government distributed a relevant document on off-site medical expense settlement under basic medical insurance schemes. This document clarified the responsibility of all levels of government in ensuring the migrant population’s right to medical insurance and defined the unified management requirements for locations providing medical treatment. At the same time, the off-site medical expense settlement information system was established and improved. With distribution of social security cards, the migrant population can equally enjoy the convenient services of medical expense settlement across provinces. Through these policies and measures, the accessibility and affordability of health-care services for the migrant population have been greatly enhanced. Meanwhile, to promote the health of migrant workers working outside, the National Health and Family Planning Commission in migrant-sending areas also established a health education group on WeChat (a Chinese social media app), sending them health education messages and keeping track of their health status for better health management.
Switzerland
According to Peter Saladin, "similar to all other areas of corporate governance, diversity policies need assertiveness by the highest management level".203 The economist and former president of the H+ Swiss Hospital Association headed the Swiss Migrant-Friendly-Hospitals-project implemented in 2003–07, as part of the confederation’s strategy on migration and public health.204 According to the 2015 report of the Migration Integration Policy Index Health Strand, an international comparative study on health systems’ responsiveness to immigrants needs, the endeavour was successful. Switzerland scored second out of 38 nations, and has established a world-leading migration and health programme.205
On the political level, Switzerland chose to turn health into a priority area of its integration policy. Legal entitlements and access to coverage within the insurance based Swiss health-care system is nearly identical for nationals, legal migrants, asylum seekers, and undocumented migrants. Health-care providers are informed by the Federal Health Office or non-governmental organisations (eg, the Swiss Red Cross) about immigrant’s entitlements to health care and migrant patients are provided access to relevant health information in multiple languages.205 Data collection and funding for relevant migrant health data is well developed, as is training of health professionals in transcultural competencies. The actual adaptation and responsiveness of health services, however, varies between regions (cantons) and institutions. The implementation of federal policies and provisions depend on political and institutional structures, priorities, and leadership on the regional and local level. Interpreters and cultural mediators, for example, are available only at some health centres, mainly large and university hospitals. As costs are charged on hospital budgets, a negative incentive for use of interpreting services still exists. Specific services and support for undocumented migrants are also only available in a small number of cantons, and political and administrative barriers to the actual realisation of formally granted rights are still prevalent.
Financing universal health coverage for all stages in the migration journey
When a universal system does not exist, migrants are often unable to access even basic standards of health care for several reasons, one of the most important of which is cost. Well designed health financing systems can prevent any individual or family from experiencing catastrophic costs due to ill health, but this is unfortunately not the case in many countries. To address such issues, the 2005 World Health Assembly resolution 58.33 set out a series of statements with regards to sustainable health financing, universal coverage, and social health insurance, and urged member states to “ensure that health-financing systems include a method for prepayment of financial contributions for health care, with a view to sharing risk among the population and avoiding catastrophic health-care expenditure and impoverishment of individuals as a result.206 If implemented, policies such as those recommended by resolution 58.33 would ensure that no migrant is subject to financial hardship for health care. However, prepayments are particularly challenging for migrants, particularly if they become unexpectedly unwell shortly after, or during the migration process—a point at which any prepayment is unlikely to be sufficient to cover costs.
Several countries have managed to achieve impressive changes in coverage and financing of their health systems, including pro-poor pathways towards universal health coverage and specific coverage for labour migrants.207 These examples show how countries have managed to provide coverage with limited budgets, while being inclusive of migrants, but tend to focus on labour and other forms of documented migration. A systematic review identified six ways to improve coverage including adjusting eligibility criteria, improving awareness, reducing insurance costs to improve affordability, improving enrolment processes, strengthening delivery of health care, and improving the organisational delivery of insurance schemes.208
Health insurance schemes exist in many countries but do not cover migrants. A study of access to health services among migrants (including labour migrants) in the Greater Mekong Region (Cambodia, Lao, Myanmar, Thailand, and Vietnam)209 identified substantial diversity in the capacity of health systems to address the needs of migrant populations. Thailand, for example, has sought to improve migrant health coverage. This improvement has included developing migrant health programmes, migrant worker agreements, and the implementation of migrant health insurance schemes. In Vietnam, health coverage is provided to migrant workers. However, in the Greater Mekong Region overall, access to high quality health care remains very poor, particularly for migrant workers and especially individuals with insecure legal status.
In addition to health insurance and general taxation mechanisms to fund universal health coverage for documented migrants, innovative ways of financing might be particularly helpful for individuals who are undocumented and individuals temporarily transiting through a country. Several examples of such mechanisms exist. Foreign exchange transaction taxes have considerable potential for fundraising and are also a way of migrants indirectly financing the coverage themselves, given their likelihood of using such services. A new intergovernmental bond scheme administered either through a newly created global organisation similar to the Global Fund to Fight AIDs, Tuberculosis and Malaria or a regional entity should also be explored. Such mechanisms can also be administered through existing regional bodies where they exist such as the EU or African Union. Such a fund will allow nation states to provide care to settled and transient populations; this might be possible by drawing on funding from various sources including governmental donors, charitable sources, and taxation of or contributions from beneficiaries where they are able to work or wish to purchase additional cover. These forms of regional and global support and solidarity are necessary to enable less wealthy countries to make progress that will be to the benefit of host and destination populations.
Ensuring the provision of migration-appropriate health information systems
Health information systems are the cornerstone of efficient and effective health-care provision and are used for assessing needs, delivering care, assessing quality of services, and accounting and financing. At present, most health information systems do not collect routine information about the migratory status of individuals.210 Risks are associated with collecting this information (panel 5) although these are often outweighed by the wider overall benefits once mitigated. Health information systems that do not collect data for migration are unable to provide useful data to monitor differences in risk factors, morbidity, and mortality between migrant and non-migrant populations, an essential step in monitoring and improving equity of service provision to this group. When health information systems are misused, civil society, academia, and health-care workers—including through the creation of so-called sanctuary hospitals and sanctuary doctoring213—can play an important and essential role in standing up against the data misuse. Human rights law can reduce the risk as it requires respect for confidentiality and other protections against misuse of information. Finally, information governance and encryption procedures can be built into health information systems so that while data can be produced on migrants, they remain anonymous.
Panel 5. Inappropriate health data sharing for immigration enforcement in the UK.
On Jan 1, 2017, an MOU between the UK Home Office and NHS Digital was signed.211 The MOU formalised existing processes and data sharing that had occurred between NHS Digital and the Home Office.212 The MOU described how any data shared had to comply with the legal obligations under the Data Protection Act 1998, the Human Rights Act 1998, and the Health and Social Care Act 2012. Requests were used by the Home Office to track down migrants for the purposes of immigration enforcement.
On publication, the MOU generated substantial media interest, particularly as it became apparent that there had been an increasing use of these requests since 2010. The report led to a request for clarification about the issue from the Health Select committee, which received several responses from NHS Digital, the Home Office, the National Data Guardian, Public Health England, and the UK General Medical Council.212 In their responses, NHS Digital and the Department of Health outlined the basis by which the MOU had been written and the impact and equity considerations that had been reviewed. NHS Digital confirmed that no privacy impact statement had been undertaken, but that instead a public interest test was done in each individual tracing request.
In their response to the Health Select committee, Public Health England stated they were unable to find statistical evidence about the effect of knowledge of data sharing on deterring immigrants from accessing health-care treatment and agreed to undertake a full review within 2 years. However, in their testimony, Public Health England experts working in the field of communicable diseases stated that “sharing of personal information by NHS commissioners or healthcare providers, which has been provided to them by patients on an understanding of absolute confidentiality, with other government departments, law enforcement agencies or immigration enforcement authorities risks undermining public confidence in the public health system and could have unintended and serious consequences affecting the health of individuals and the risk to the public health of the wider community”.
The General Medical Council, the governing body for UK doctors, only permits clinicians to share patient information “if failure to disclose may expose others to a risk of death or serious harm“. Suspected immigration offences do not fall under this category. In the General Medical Council’s response to the committee, they stated that, “the memorandum of understanding sets out clearly the public interest in maintaining effective immigration controls. It does not however reflect the public interest in there being a confidential health system, or consider how those two public goods should be weighed against each other”.
The National Data Guardian, Dame Fiona Caldicott, also expressed her concerns about this issue stating, “any perception by the public that confidential data collected by the NHS is shared for a purpose that they had not anticipated or without appropriate controls may well lead to a loss of people’s trust" and that "trust would have been better maintained had there been more public debate about where the balance should be struck between the public interest in maintaining an effective immigration service and the public interest in a confidential health service before an agreement was made between NHS Digital, the Home Office, and the Department of Health. This would have allowed more scrutiny of the reasoning and factors which led to the policy position which has been taken”.
During a parliamentary debate in May, 2018, about new data protection regulations, a member of the UK parliament Conservative party and chair of Health Select committee, Dr Sarah Wollaston, tabled an amendment to end the data sharing arrangement between NHS Digital and the Home Office. During the debate, the Government announced a reversal of policy and accepted Dr Wollaston’s amendment, which substantially narrowed the scope of the MOU in order that it only covered sharing in cases in which a person was suspected of serious criminality.
MOU=memorandum of understanding. NHS=National Health Service.
The health-care providers of many refugees have developed bespoke information systems based on such a system’s ability to disaggregate populations by refugee status, enabling the monitoring of services, and humanitarian standards. It was therefore proposed that these systems remained separate and specific to the situation but would feed into the national infrastructure.214 Despite the advantages of such an approach, there are risks associated with developing a completely separate system for refugees and other migrants. Separate systems make comparisons between the host population and migrants much more challenging as the data collection processes and outcomes typically vary. Instead, national health information systems should be adapted, with only minor additions, to collect information on migrants that will provide public health and policy makers with better, more accurate data. A truly universal system requires joined up and universal health information systems. For these reasons we argue that wherever possible, these information systems should be adapted to include data for migration, rather than separate systems being used.
Cultural competence
The health sector cannot fully assess and support health needs, including health promotion, surveillance, and service provision, without understanding users’ backgrounds and perspectives and the mechanisms for exclusion. Approaches to tackle such challenges, however, need to be rooted in an understanding of the cultural context and its intersection with the environment. Yet too often, assumptions about the health risks and behaviours of individuals from cultural or ethnic minorities stem from misunderstandings, stereotypes, or racism, as described in section 1. These misjudgments and prejudice can obscure relevant individual, social, structural, economic, or political factors.82
Health-care provision should be culturally appropriate and sensitive to the individual’s understanding of health. Racism at social and institutional levels, as well as in the case of individual health providers, must be recognised, confronted, and avoided; this includes less obvious forms of racism enclosed in stereotype assumptions regarding health risks or health related concepts, beliefs and behaviours held by members of particular ethnic or migrant groups. The acceptability of health services for migrants depends on the ability and preparedness of health professionals to provide culturally informed care,215 which includes cultural humility: an understanding of and reflexivity about their own culture in order to foster non-paternalistic clinical encounters.216 To balance the awareness for culture with the need to address other relevant factors, and to avoid cultural stereotypes, structural competence (eg, training in medical education to understand the broader structural forces that influence health outcomes) is also needed.217 This need is reflected in an anthropological study of irregular Mexican farm workers in the USA, which showed that in contrast to the physician’s assumptions, the migrants’ culture was not the primary barrier to health access.218 Instead a range of structural issues, including farm schedules, economic pressure, absence of insurance coverage, and the mobility of farm workers determined use of local health resources.
Cultural competence is thus not just a technical skill that can be acquired through specific courses or training, although such training is an important starting point; it should be an ongoing commitment to "awareness of the cultural factors that influence another’s views and attitudes" regarding health and disease.81 Cultural competence supports the health-care provider in approaching the patients’ understanding of the illness, and how she or he “understands, feels, perceives, and responds to it”.82 This includes notions and practices commonly identified as traditional medicine, that for many reasons might be of great importance for the patient and his or her family and peers. Systematic reflection of the health providers’ own assumptions, beliefs, conventional understandings, and values regarding medicine, health, and their own culture or ethnic heritage is also essential. Understanding organisational culture, how medical institutions and professional groups function in particular settings (eg, non-governmental organisations providing humanitarian assistance), are also important factors to consider in providing effective health care for migrant populations.81
An additional domain when considering migrant health is the provision of adequate translation services and culturally appropriate health related support services to migrants to increase their understanding of health and how to access services.219 High quality interpretation and cultural mediation are among the most important factors in best practice delivery of health services to migrants.220 The use of family members as translators when a professional interpreter is not available is, by contrast, highly problematic. It is problematic for issues of confidentiality, quality of the translation, problems related to discussing sensitive topics, and the psychological burden (eg, for children when translating serious health issues for their parents). Moreover, it is important to consider that interpreters and individuals providing support services from the same country of origin or ethnicity might belong to socially and politically different parts of society, which can lead to associated challenges in effective provision of care.
Section 3. Burden of disease and migration
International migration and mortality
For many years, researchers pursued the theory of a healthy migrant effect, which has been described as "an empirically observed mortality advantage of migrants from certain countries of origin, relative to the majority population in the host countries, usually in the industrialised world".221 However, not surprisingly, this theory is now considered to be reductionist because it neglects the diversity and complexity of migration-related factors that influence people’s health and how these affect individuals at different stages of the life course.222 It also disregards that the health benefits of being a migrant tend to reduce over time.
To complement the Commission’s work, a systematic review and meta-analysis on mortality outcomes in migrants was undertaken.16 96 studies, mostly from research done in HICs, were included. The meta-analysis provides evidence of a mortality advantage of international migrants in high-income settings. There were only two ICD-10 categories for which there was evidence of increased standardised mortality ratios, infectious disease and external causes. As detailed in the Article,16 our results point to the need for improved data collection and reporting in migrant health research. The results of this analysis will be representative of international migrants in HICs, but not forced migrants in low-income and middle-income settings, for which better data is urgently required. Our systematic review16 highlights the heterogeneity of standardised mortality ratios by country of origin,223 which is consistent with other studies. Moreover, other evidence indicates the importance of age at migration, type of migrant, year of migration, social class, and policies towards promoting health in the receiving country.224
Internal migration and mortality
To explore internal migration and mortality, we did a case study with novel analysis of Health and Demographic Surveillance System data from sub-Saharan Africa (panel 6). Findings indicate that in half of the study sites, migrant mortality was 50% higher than non-migrants. These findings are strengthened by results from a study of internal migration and AIDS, tuberculosis, and non-communicable disease mortality in four Health and Demographic Surveillance System sites in South Africa and Kenya, which showed that in-migrants (from within the same country), and return-migrants even more so, had a higher mortality risk attributed to both non-communicable and infectious disease.227,228
Panel 6. Internal migration and mortality in sub-Saharan Africa.
Our analysis of all-cause mortality in 25 Health and Demographic Surveillance System sites in sub-Saharan Africa uses data representing a mix of rural and urban settlement types, from the International Network for the Demographic Evaluation of Populations and Their Health (INDEPTH) iShare platform.225 The datasets include individual level information on all movements into or out of a surveillance area for durations of more than 6 months. From these data, we can identify in-migrants (new residents) and return-migrants (former residents returning) to an area. After 5 years of residence, a migrant is considered a permanent resident, as previous analyses of the effect of duration following migration show that the mortality of migrants converges with that of permanent residents (non-migrants) after this length of time.226 For each migration category (non-migrant, in-migrant, return-migrant), premature mortality is estimated by the probability of mortality before 60 years of age if a person is alive at 15 years of age (45q15). The percentage difference in 45q15 between migrants and non-migrants was estimated by sex for each of the 25 Health and Demographic Surveillance System sites from the year 2000.
The analysis reveals that in sub-Saharan Africa, the distribution of the difference in premature adult mortality between migrants and non-migrants is substantial (ie, in half of the sites migrant mortality was 50% higher than non-migrant mortality). Differences in adult health probabilities (45q15) by migrant status in 25 sub-Saharan Africa Health and Demographic Surveillance Systems are presented in supplementary appendix figure 7. These analyses indicate that in half the sites, migrant mortality was 50% higher than non-migrant mortality.
These results suggest that internal migrants in the sub-Saharan Africa subdistricts have a health disadvantage relative to the resident, non-migrant population. A study of internal migration and AIDS, tuberculosis, and non-communicable disease mortality in four Health and Demographic Surveillance System sites in Kenya and South Africa affirmed these findings. In the Agincourt study population in rural South Africa, in-migrants and, even more so, return-migrants had a health disadvantage in terms of mortality risk attributed to both non-communicable and infectious disease.227,228 These findings suggest that relative to non-migrant mortality, the experience of migrants is demonstrably worse in many sub-Saharan settings, with poor access to health care a probable determinant along with poor social integration or inadequate living conditions. Further research into the circumstances at migrant destinations is a priority going forward.
The same method was used to examine child mortality (the probability of death in under 5 year olds) by migrant status, in which child migration status was considered independently of the migration status of their parents (see supplementary figure 8 in the appendix). The results present a striking contrast to that found in adults. Both in-migrant and return-migrant children of both sexes have lower all-cause mortality on average than non-migrant children. These results present an important direction for further research and challenge assumptions that determinants operate in the same way and have the same outcomes for adults and children.
Migration and morbidity across the life course
Here, we describe the health effects of migration on selected morbidity outcomes to show varying effects through the life course and in different migrant groups and, if available, we summarise evidence of effective interventions. Migrant health at different periods of life varies in important ways in comparison to non-migrants, and can lead to longer-term or intergenerational effects. There is paucity of evidence comparing migrant groups with the population in the location of origin and, unless otherwise stated, the studies relate to international migrants, with the comparison group being the host population. This paucity of evidence makes it difficult to ascertain whether migration itself improves or worsens health. The reality is that it would improve and worsen different risk factors for health at an individual and population level. The health risk profiles of migrants are determined by their pre-migration status and is a complex combination of biological and socioeconomic factors developed over their lives. Moving to a new location will change someone’s risk profile, with some determinants of health improving and others worsening. As people usually move to improve their lives, many risk factors will lessen, resulting in better overall health than they might have had in their previous location; however, a comparison to the host population only might make it appear that their morbidity is higher.
Perinatal health
An umbrella review (including 19 systematic reviews) of perinatal outcomes among migrants and refugee women compared with the host population generally found worse outcomes among migrants for maternal mortality, maternal mental health, preterm birth, and congenital anomalies.229 A meta-analysis of 18 million pregnancies in Europe showed that migrant populations had an increased risk of perinatal mortality (odds ratio [OR] 1·50, 95% CI 1·47–1·53), preterm birth (OR 1·24, 1·22–1·26), low birthweight (OR 1·43, 1·42–1·44), and congenital malformations (OR 1·61, 1·57–1·65). Importantly, these risks were significantly lower in countries with policies promoting social participation and active integration with the host population (Belgium, Denmark, the Netherlands, Norway, Sweden).230 In contrast to the umbrella review, a further large meta-analysis including more than 20 million pregnant women moving to high-income industrialised countries, found that children of migrants generally fared better in terms of perinatal outcomes. For subgroups of migrants from Asia and Africa, there were increased rates of preterm birth and mortality, but Latin American migrants were at a lower risk of preterm birth.231 The reasons for adverse birth outcomes included underlying conditions in the mother that could be exacerbated by migration, such as heart disease or HIV, poor access to and interaction with the health service, communication problems, socioeconomic deprivation, and the stress of migration.
Migration is also commonly associated with stressors that can have substantial effects on maternal mental health and post-partum depression. In a meta-analysis of perinatal mental disorders among women from LMICs living in HICs, 31% had symptoms of any depressive disorder and 17% had symptoms of major depressive disorder.232 Estimates suggest that within the first year after childbirth, the risk of post-partum depression is 1·4–2·2 times higher in immigrant versus non-immigrant women.233 Risk factors included a shorter period of residence, lower amounts of social support, difficulties adjusting to the new country, and perceived insufficient household income.229
Child and adolescent health
Children and adolescents who migrate generally adapt and integrate well into new environments. They do well especially when supported by families and when engaged in quality education with access to health services. The risk factors for health in the location of origin can be profound (eg, huge health benefits result from escaping trauma or conflict settings). Healthy development in infants, children, and adolescents occurs in the context of stable and caring relationships. The extent to which migration can alter these social determinants of health is immense and migration during sensitive developmental phases, especially when exposed to stressors, can determine later health outcomes and the health of the next generation. Migration can break up and alter family units, and loss of parents and carers can lead to emotional and psychological harm. However, migration can also bring families together and new family and social networks form over time. Maintenance of secure family structures and functions during the migration journey can help protect children and adolescents from some of the most adverse influences, while continued access to learning environments is essential for all children and adolescents. Migration can also disrupt the provision of health care such as immunisation schedules, threaten early childhood development, and limit access to schooling.234
Overall, far less evidence is available on adolescents compared with young children, despite adolescents constituting a larger proportion of migrants (figure 4). As children mature through adolescence (10–24 years) they become more directly exposed to social determinants of health beyond the family (eg, education, gender norms, racism). During puberty, brain maturation results in increased sensitivity to real and perceived differences related to migration. Beyond simply feeling different, the experience of stigma and social exclusion by bullying can contribute to emotional distress, anxiety and depression, and self-harm, including suicide.235 Some of these effects can be intergenerational. For example, migration of the mother as an adolescent or young adult was associated with lower sociability and problem-solving skills in her children at 4 years of age compared with children born in the country or children born to mothers who migrated when below the age of 12 years.236
Mental health
A systematic review of mental health outcomes in economic migrants found ambiguous results, varying by migrant group and host country.237 A meta-analysis of internal migration in China showed that migrant children have a greater risk of internalising (eg, depression, anxiety, loneliness) and externalising problems (eg, aggression, hyperactivity) in public schools, but not in migrant-specific schools.238 Among forcibly displaced children in HICs, higher rates of psychological morbidity have been recorded. Only a small number of studies have looked at migration itself with inconclusive results, but evidence shows that pre-migration factors, such as exposure to violence, were predictors of mental illness. Comparison studies with left-behind children are rare. Factors, such as support from families and friends and a positive school experience, can be protective. There is also evidence of increased mental illness239 and autism240 in second generation migrants, potentially mediated via epigenetic mechanisms and, in mental illness more generally, by their parents’ reactions to stress.
Nutrition
Rapid transitions associated with migration can lead to substantial changes in diet, exercise, and infectious disease exposure, all of which can affect nutritional status. Improving access to quality food by migrating would improve health, but changes in lifestyles, shrinking social networks, and the adoption of a diet high in fat, sugar, or processed foods can lead to obesity.241 Poor nutrition, particularly during fetal stages and infancy, coupled with rapid weight gain in a new environment can lead to an increased long-term risk of non-communicable diseases. In addition to under-nutrition, migration can lead to rapid weight gain, with evidence that timing of migration alters obesity rates.242 Children affected by migration can experience both being undernourished and overweight. For example, a Swedish study found an association between maternal migration and lower body-mass index in children less than 5 years old but higher body-mass index in older children.243 Apart from promoting breastfeeding, most other nutrition interventions vary according to the context and health outcome.244
Unaccompanied minors
Unaccompanied minors are typically 15–18 year olds who are “separated from both parents and other relatives and are not being cared for by an adult who, by law or custom, is responsible for doing so”.245 They are particularly at risk, both from the circumstances that have rendered them unaccompanied (eg, war, parental death) and the risks that can arise when offered less protection by close family. The group is diverse and includes victims of trafficking or modern slavery, individuals reuniting with family, and people seeking a better life. Less experienced than older adults, and generally impoverished, they are at great risk of exploitation. Unaccompanied minors can be subject to disputes over their age (panel 7). The younger the age of the unaccompanied minor, the greater the risks are to them. Unaccompanied young adults are also likely to be at greater risk than those protected by their immediate family. Health risks result from exposure to substances and unsafe sexual behaviours, and greater risk of early school completion and unsafe employment. Unaccompanied girls are particularly at risk of sexual violence and unwanted pregnancy.249 The accumulation of risks can result in complex health needs, especially mental health problems, which can then be compounded by issues around residency status.250
Panel 7. Age assessment, an unresolved challenge for unaccompanied minors and refugee children.
Although migration to Norway is not a new phenomenon, the number of refugees that came to Norway in 2015 was unprecedented. Over 30 000 sought asylum, of which 5000 were unaccompanied minors. This latter group is at increased risk of child trafficking, abuse, and violence, and requires guardianship and protection. However, instead of focusing on their rights and obligations to this group of children and adolescents, regrettably governments often seek to avoid these obligations.
Age determination has been a substantial challenge and source of debate among child rights groups and immigration officials. Though universally agreed definitions of a child exist, there are no agreed methods regarding the assessment to determine the age of a child. Unaccompanied minors often have no reliable information about their age or date of birth. Authorities deploy techniques and investigations that are, at best, approximations.246 The consequences of these approximations can be devastating for this group of children. In Norway, if the age assessment shows that someone is less than 18 years of age, they will be cared for by the Norwegian Child Welfare Services. The Child Welfare Services statutory obligation is "to ensure that children and youth who live in conditions that may be detrimental to their health and development receive the necessary assistance and care at the right time". In addition, non-resident minors are entitled to receive the same help from these services as any other Norwegian child. By contrast, if the assessments conclude that a person is over 18 years old, they will be treated as an ordinary adult asylum seeker, with few such rights.
Thus, unsurprisingly, the techniques to determine the age of a child are controversial. In Norway, the measurement of age by x-rays of the hand (bone age) and teeth are routinely used, despite long-standing dispute about these techniques. The x-rays assess ossification and presence of molar teeth and can be used to estimate age. However, they are not an accurate method and unnecessarily expose the adolescent to radiation. In response to the gravity of concerns expressed by the Norwegian Medical Association in the context of importance of these procedures, the responsibility for conducting these was transferred from the private sector to the Oslo University Hospital from January, 2017.
Age assessments, when necessary, should integrate clinical history and physical assessment, taking into account the person’s development (physical, cognitive, and emotional). A report on age assessments247 concluded that "there is evidence that radiography (x-rays) of bones and teeth, which is increasingly relied upon by immigration authorities, is imprecise, unethical and potentially unlawful, and should not be used for age assessment". Despite this report, x-rays are perpetuated as the gold standard. As this method of age assessment jeopardises the current and future situation of unaccompanied minors, many have no alternative but to resort to other even more dangerous choices of living. This might include living as undocumented minors on the streets of other European cities, exposing and endangering them to further perils. Moreover, substantial evidence suggests that even individuals over the legal age for mandatory support services and guardianship (ie, 16–24 years) have need of protection and support.248
Left-behind children
Children might be left behind when parents migrate, usually for work. Though there are no global estimates for the number of left-behind children, estimates indicate 61 million in China alone. The effects of parental migration on the health of left-behind children are mixed. In some settings there is evidence of a beneficial effect (eg, through receipt of remittances), but in others, children encounter adverse consequences. We undertook a systematic review of the literature in any language, including in Chinese, across key areas of child and adolescent mental and physical health.15 We identified 111 observational studies with outcomes for mental health, nutrition, infectious diseases, injuries, and key determinants of health. Most studies addressed children of internal migrants in China and showed no difference or worse outcomes in left-behind children or adolescents, compared with those of non-migrant parents. The meta-analyses showed an increased risk of anxiety (relative risk [RR] 1·85, 95% CI 1·36–2·53), depression (RR 1·52, 1·27–1·82), substance use (RR 1·24, 1·00–1·52), suicidal ideation (RR 1·70, 1·28–2-26), stunting (RR 1·12, 1·00–1·26), and wasting (RR 1·13, 1·02–1·24) among left-behind children and adolescents. No differences were found in the risk of being overweight or obese or experiencing abuse. In all the meta-analyses heterogeneity was high, however the results were robust to sensitivity analyses; removing low quality studies and subgroup analyses of internal and international migration showed little difference. Parental absence and lack of supervision can lead to unhealthy risk behaviours in left-behind adolescents. Given the very large population of left-behind children globally, the increased risk of mental disorders, substance use, and malnutrition represent a major concern.
Women, men, and sexual minority health
The health and morbidity patterns among adult migrants are associated with a combination of pre-existing factors, their new environment and lifestyles, and exposures during their journey. This combination of factors results in a great deal of variation in morbidity. Commonly, differences also exist between specific health conditions among recently migrated populations versus long-term residents. In this section, we review the latest evidence in this area.
Mental health
In general, prevalence rates of mental illness vary widely. First generation international migrants tend to have higher prevalence rates of depression, anxiety, and post-traumatic stress disorder compared with the host population, with an increased risk in asylum seekers and refugees.251 Men appear to have a higher risk than the host population for mood disorders (RR 1·29, 95% CI 1·06–1·56), but no difference has been observed between host and migrant women.239 Risks of psychosis and schizophrenia are consistently higher among migrants, approximately double the risk compared with the host population, and these effects are carried over into the next generation.252,253 The reasons for the differences in mental health outcomes and the variation between individuals and groups is multifaceted. They reflect real differences in precipitating risk factors, for example exposure to violence and traumatic events, time in the new setting, and, importantly, methodological variation. Discrimination is also implicated across a range of mental health outcomes including depression, psychological distress, anxiety, and wellbeing.254 Perceived discrimination has also been linked to specific types of physical health problems, like self-reported poor health and breast cancer, and potential risk factors for disease, such as obesity, hypertension, and substance use.255
Mixed results were found in mental health status in Chinese rural-urban internal migrants compared with urban non-migrants, but no difference or worsening mental health status was observed compared with rural residents. Social and economic exclusion were both important determinants of mental illness.256 Research on the mental health of migrants typically focuses on refugees, asylum seekers, and torture survivors. Systematic reviews and meta-analyses often indicate intersurvey variability. A review and meta-analysis of 181 surveys from 40 countries, comprising 81 866 refugees and people affected by torture and conflict found that the unadjusted weighted prevalence rate was 30·6% (range 0–99%) for post-traumatic stress disorder, and 30·8% (0–86%) for depression.257 Compared with labour migrants, refugees had approximately double the prevalence of depression and anxiety.258 Mental health interventions, including cognitive behavioural therapy259 and trauma-focused therapy260 have some efficacy in treating post-traumatic stress disorder, and community-based mental health services have been consistently shown to improve outcomes.261
Communicable diseases
Control measures for infectious diseases have long been established, including processes such as quarantine of visitors and animals at ports of entry. The true risk of transmission arising through migration is, however, a function of multiple factors. Risk varies according to the route of transmission of the pathogen, its transmissibility, the degree of mixing between the infectious and susceptible population, and the available control measures in place to mitigate transmission risks. Outbreaks of infectious diseases can be sustained by population movement. For example, during the west African Ebola outbreak, population movement within and between countries contributed to sustaining transmission.262 An important risk in relation to the spread of infections is the emergence and subsequent transmission of antimicrobial resistant strains that emerge in one part of the world and spread to other regions.263 However, the spread of such resistant pathogens is not due to migration, but driven by international travel and tourism and the movement of livestock.263 The public health burden of infectious disease in migrant populations remains high in many settings. Strong preventive services, including immunisation and screening programmes, and curative services to ensure early detection and treatment of infections in migrants are needed. Where screening programmes are established, they need to be evidence-based and culturally acceptable. Ultimately, the self-interest approach (improving global health security is designed to help the migrants but it is also good for the host population) is to strengthen global health security by supporting the establishment of sustainable health infrastructure and systems in all countries that are more mobility aware.
Physical disability
For people of any age with a range of disabilities (eg, individuals with mobility, visual, hearing, intellectual, or mental health impairments), the process of leaving home and travelling elsewhere can be physically challenging, stressful, and confusing, especially in times of crisis. These difficulties also often lead to later departure in times of economic stress or humanitarian disaster, placing them at additional risk. Furthermore, migration can disrupt existing social and medical support networks. People with disabilities are frequently and incorrectly assumed to be less able or competent, leading to an inability to find work or find enough work in a new community to cover their expenses or contribute to their households. Although the UN Convention on the Rights of Persons with Disabilities121 guarantees equal access across borders to all, people with disabilities experience discrimination during the immigration process, struggling to pass immigration tests and understanding oaths of alliance, or meeting minimum income requirements. People with disabilities in all societies are substantially more likely to be victims of violence.264
Non-communicable diseases
Increasingly people are moving with established non-communicable diseases and often combined with a double burden of communicable diseases. The interruption of care during transit—due to barriers to health access, documentation, absence of health-care providers, or disrupted health systems—prevents the continuous treatment necessary for the effective management of many chronic health conditions.265 The absence of effective prevention, screening, and continuity of care in migrant populations result in higher burdens of non-communicable disease morbidity and mortality. Evidence has shown that migrants undergo rapid changes in environmental risk factor profiles. When compared with the native Danish population, migrants from Africa, Asia, and the Middle East had 2·5 times the incidence of diabetes.266 This difference could be due to various factors such as poor health literacy and language barriers leading to difficulties accessing services, shift in socioeconomic status, decreased amounts of physical activity, and changes in diet. A systematic review of 37 studies of migrants to the EU found lower morbidity due to any malignancy in migrants compared with the host populations. For specific cancers some exceptions existed (eg, liver cancer), and incidence varied by the region migrants moved from.267 Consequently, more effective integration of non-communicable disease care into health systems and humanitarian responses is essential.
Tobacco and alcohol use
Although tobacco and alcohol use in migrants has been shown to be heterogeneous and context-dependent, various underlying risk factors were identified including unemployment, poor working conditions, language proficiency, level of integration, number of traumatic experiences, and community cohesion. Studies suggest that migrant smoking prevalence is dependent on the prevalence in the country of origin and in the host country. For example, Ghanaian migrants in Europe were more likely to smoke than both rural and urban dwellers in Ghana, but still smoked less than the host population.268 Several studies in HICs and for internal migrants in China have shown that migrants are less likely to smoke than non-migrants,269,270 while male migrants from Europe, North Africa, and the Middle East in Australia were found to smoke more than Australian born men.271 A study in Kazakhstan showed that international labour migrants reported higher rates of hazardous alcohol consumption compared with internal migrants and the host population.272 Conversely, in Peru, the prevalence and incidence of heavy drinking was the same for rural-urban internal migrants as their rural and urban counterparts.273
Occupational health outcomes in labour migrants
Rates of fatal and non-fatal injuries are higher in labour migrant populations compared with non-migrant populations. This difference is in part due to the type of employment (eg, construction, fishing, and metal-working); however, even within these sectors, occupational morbidity and mortality is higher among migrants than native-born workers (table).274 Occupational harms differ by sector and include injuries, exposure to weather or pesticides, respiratory conditions, depression and anxiety, and infectious diseases. As part of a new analysis done for this Commission (Hargreaves et al, unpublished data) we did a systematic review and meta-analysis focused on international labour migrants (originating from 24 LMICs). This analysis found a reported prevalence of 47% of migrants documenting at least one morbidity (7260 migrants, 95% CI 29–64, I2=99·7%), including predominantly musculoskeletal pain and dermatological conditions, and a prevalence of reported injury and accidents in 22% of migrants (3890 migrants, 95% CI 7–37, I2=99·4%).
However, other studies have shown no difference for migrant and non-migrant health in some sectors. In general, men are more likely than women to endure workplace injuries, illness, and fatalities.275 Migrant workers operating in many of the most hazardous work sectors might not be aware of, or have access to, occupational health and safety training or personal protective equipment.274
To date, few studies have explored the mental health of migrant workers. A review that compared labour migrants to refugees found that refugees had approximately double the prevalence of depression and anxiety. Importantly, the authors suggested that financial stress is a substantial risk factor and that a higher gross national product in the country of immigration was related to lower symptom prevalence of depression or anxiety (or both) in labour migrants but not in refugees.258 Examples of the consequences of financial pressures on mental health in trafficked migrants are described in panel 8.
Panel 8. Case study: labour trafficked migrants, mental health, and financial security.
A study among male, female, and child trafficking survivors in the Greater Mekong Subregion found that 48% encountered physical or sexual violence, 43% reported symptoms of depression, and 40% reported post-traumatic stress disorder.276 Employment is closely associated with mental health, with job insecurity and financial insecurity closely linked to anxiety and depression. Most data for employment and health come from high-income settings and studies on higher wage jobs, with very little research on migrant workers in low-income and middle-income countries. The study on trafficking, exploitation, and abuse in the Mekong276 documented forms of labour exploitation and health outcomes among men, women, and children using post-trafficking services in Cambodia, Thailand, and Vietnam. High rates of symptoms of depression and anxiety disorders, post-traumatic stress disorder, and suicidal ideation were found. These symptoms were associated with sexual and physical violence and threats during trafficking, poor living and working conditions, excessive overtime, and restricted freedom.
Being deprived of wages was also a major stressor for formerly trafficked people, many of whom felt guilt and shame from failing to fulfil income expectations. In the Study on Trafficking, Exploitation and Abuse in the Greater Mekong Subregion (STEAM), most trafficked migrants (62%) reported being cheated of their wages. Among the few who were paid for their work, domestic workers (US$0·40), agricultural workers ($0·70), and fish industry workers ($1·10) received the lowest daily wages. Unsurprisingly, domestic workers (76%) and fish industry workers (71%) more frequently expressed financial concerns. The majority (82%) of domestic workers reported depression, anxiety, or post-traumatic stress disorder symptoms (or combinations of the three), similar to individuals trafficked for construction work (79%). Individuals who had been cheated over their wages or had financial concerns were approximately 1·5 times more likely to be symptomatic of a mental health disorder.
Studies often overlook the significance of income security to a migrant’s psychological wellbeing because research on migrants’ mental health frequently focuses primarily on past events versus current stressors. Especially for those who migrated to improve their family’s economic circumstances and were unsuccessful, mental health support will need to include job training and placement or small business grants. Moreover, for migrants who have been exploited, cheated of their wages, or injured on the job, legal aid should be provided to help with wage recovery and compensation for abuses, and injuries, including long-term disability support.
Sexual and reproductive health
Addressing sexual and reproductive health needs can be particularly challenging because of the risks of sexual abuse and exploitation,277 especially among children and adolescents. Cultural practices can also increase health risk for girls and women, such as early or forced marriage,22 genital cutting, and historical and cultural norms, including unfamiliarity with or restricted use of gynaecological and obstetric care.
Sexual violence or threat of abuse exacerbates reproductive health problems and can deter women and young people from seeking care. Importantly, it is not uncommon for sexual abuse among boys to be overlooked, nor is it unusual for professionals to be ill-equipped to detect and treat men and boys who have been sexually abused. Traditional practices and beliefs can also be a point of contention, as new migrant populations call on local health services and social support organisations. Female genital mutilation or cutting is a human rights violation, with substantial mental and physical health implications. At least 200 million girls and women have been subjected to genital cutting in 30 countries.278 Health systems in locations where the practice is uncommon need to be able to manage the resulting morbidity in migrant women and girls. Health-care practitioners are well positioned to detect and address the negative effects of female genital mutilation or cutting among pregnant women. They can also help prevent the practice in girls in high risk families through provider training and guidelines, culturally appropriate information, and engagement with self-help groups for the communities concerned.279 Similarly, for migrant sexual minorities or LGBTI groups, appropriate and sensitive sexual services can be difficult to find. For example, in urban centres in China, approximately 70% of HIV infections are among rural Chinese residents, of whom 80% are 16–29 year old men, a portion of whom are so-called money boys or individuals who engage in transactional same-gender sex.280
Forcibly displaced women and adolescent girls might have facilitated access to much-needed sexual and reproductive health services if they enter well equipped humanitarian aid settings. Without such targeted services in place, migrant women and adolescent girls can be more vulnerable to poor sexual and reproductive health outcomes, including unwanted pregnancy, pregnancy complications, sexually transmitted infections, and unsafe termination options.281,282 Humanitarian aid agencies have established an agreed set of essential services to respond to reproductive health needs in humanitarian crises. The Minimal Initial Service Package includes preventing and managing the consequences of sexual violence, reducing HIV, and preventing maternal and neonate mortality and morbidity.283
Violence
Migration can be a movement away from physical or structural violence. For people fleeing from violence, whether by crossing an international border or moving within their own country, migration allows people to move away from circumstances in which their life and freedom were at risk.284 However, mobility and relocation can create substantial risk factors for various forms of gender-based violence, including rape, intimate partner violence, sexual exploitation, and human trafficking. Systematic reviews on health and human trafficking indicate that trafficking survivors are exposed to multiple physical and psychological abuses, sexual violence, confinement, occupational hazards, and poor living conditions.285 The physical, mental, social, and financial consequences of these extreme forms of exploitation are multiple, severe, and often enduring, especially psychological consequences.285 A meta-analysis of studies in humanitarian settings suggested that 21% of female refugees or displaced women in complex humanitarian emergencies experienced sexual violence, a probable underestimation.286 Despite the prevalence of gender-based violence in refugee populations, there is little evidence for the effectiveness of prevention programmes, interventions, and strategies.287
Mobility can increase or decrease these health and safety risks among LGBTI migrants, depending on the comparative amounts of discrimination and stigma in origin, transit, and destination locations. Research in LGBTI migrants suggests that these individuals are especially likely to have mental health disorders as a result of cultural or even state-sponsored persecution and violence. Many LGBTI migrants report emotional, physical, and sexual violence committed by their families, leaving them without a familial support network and even more susceptibility to violence upon migrating.288 Service providers in Nairobi have shown that LGBTI services for refugees need to be accessible and highly confidential to prevent further harassment or violence.289
Migrants with disabilities are substantially more likely to be victims of violence and are less likely to be able to report such violence. This can be because of barriers such as not being believed or an inaccessibility of reporting mechanisms. Additionally, a scarcity of employment options because of stigma, prejudice, less access to education, and less job-related skills training result in many people with disabilities being at increased risk of poverty and consequently increased risk of sexual violence and forced participation in prostitution and household slavery.290
Older people
Evidence is scarce on the health effects of migration on older people (generally aged older than 60 or 65 years, but variable by region), particularly from LMICs. Older people might have additional health risks due to multimorbidity, for example from interruptions to the continuity of care that contribute to clinical decompensation and declines in their health status. Despite lower mortality, morbidity is thought to be higher among older migrants. Analysis of population data from Belgium, England and Wales, and the Netherlands of healthy life expectancy at age 50 years (HLE50, expected number of remaining years in good health) found higher life expectancy in migrants compared with non-migrants, but HLE50 was lower. This difference was particularly so for migrants not from HICs (ie, not from Australia, Canada, Europe, Japan, New Zealand, or USA).291 Multicountry studies from across Europe show higher self-reported morbidity in older migrants compared with native people of the same age.292,293 A study from Sweden found an increased risk from 50% to 80% in cardiovascular determinants, such as physical activity, smoking, and body-mass index in older migrants.294
Studies of mental health in migrants across Europe found an increased risk of illness. Increased ORs of 1·6 in men295 for depression were found in older migrants, despite lower rates of other chronic diseases. Research in forced migrants also points to an increase in depression risk but evidence is insufficient to support this claim.296 The diagnosis and management of dementia is a particular concern among all migrants. With ageing populations, dementia is becoming more common globally. Migrant or ethnic minority populations receive diagnoses later and have differences in their management (eg, less medication and nursing home admission).297
Section 4. Knowledge to address future migration and health challenges
This Commission argues for a paradigm shift in research on migration and health, with a deliberate effort to enhance the funding mechanisms and networks supporting this change. Collaborative work is needed that links academia, policy, and front-line health and humanitarian workers. Research in migration and health has traditionally been difficult to do, partly because of the high mobility of migrants.298 In this section, we outline how we can generate better knowledge to meet the needs of people on the move through better data collection, research, research funding, and ethics (panel 9).
Panel 9. Research recommendations and priority research questions.
To address the health needs of migrants, high quality data collection for migration and health should:
Add migration related questions to regularly administered surveys such as Demographic and Health Surveys, health and population surveillance systems, and censuses
Examine the multiple interactions between migrant populations and between migrant and non-migrant groups
Include health outcomes of migrants that are more closely aligned with the drivers of migration and the geographical region of origin of migrants, internal migrants, and the interaction with aging to better understand health needs
In addition to comparisons with the host population, conduct research that makes comparisons with the population at origin to ascertain the consequences of migration on health, ideally with use of longitudinal data collection methods
To provide an evidence base for health-related drivers and outcomes of migration, it is essential to focus on the processes and implementation of migration and health research through:
Engagement with the population using participatory approaches to ensure that migration and health research meets their needs and does not result in harm
Undertaking research that responds to the population need, including through increased focus on the health effects across the lifecycle and genders
Analysis of best treatment regimens and modifications to these treatments required by mobile populations
Implementing evidence-based health interventions, with a focus on data collection, assessment of cost-effectiveness, and analysis of intervention impact and effectiveness
Increasing the evidence base describing the consequences of discrimination against migrants and racism, and ways to prevent this
Considering the health of migrant groups in all areas of research
To provide and use better data to reduce inequities, changes in the migrant health research process and methods are needed, through:
Use of globally accepted definitions to guide similar data collection and disaggregation, with a recognition that the categories used in human mobility and health are not static but fluid
Viewing the migrant population themselves as an asset and encouraging a participatory approach, in which migrants and local communities are included in research prioritisation, policy making, and the decision process
Including qualitative, adaptive, and context sensitive approaches to understand sociocultural factors of migration, the barriers to health care, and how the determinants of health might affect migrants differently
To provide evidence for health policy and systems research, the following questions should be considered:
What financing models are most effective in extending access equitably to migrants?
How can prevailing jurisdiction based health governance and citizen participation approaches be made more sensitive to the needs of migrants?
How can health-care providers be equipped with the necessary multicultural competencies for migrant care?
How can information systems be made more portable and interoperable while still preserving patient rights and privacy?
To produce ethical research, there should be incorporation of ethics, data protection, monitoring, and evaluation into all stages of the research process. The following questions should be considered:
Does the research meet the needs and priorities of the research population, and goals like equity, integration, health protection, and universal health coverage?
When defining the sample and the distinguishing categories of migrants, what are the sources of information that these definitions rely on and how do these categories resonate with the individual’s self-perception?
Does the research deal with the challenge to understand social boundaries by providing scientific evidence of differences between and homogeneity within social groups and populations?
To what extent does the research reflect social, structural, and political determinants of health and their implications on social gradients, historical power relations, and probably stigma?
To provide adequate funding and appropriate research, health funders should:
Make migration and health a priority research area
Ensure that funded research always endeavours to include migrants within it
Support capacity development among migration and health researchers and institutions in the Global South through specific funding initiatives and support of research networks
Meeting the health needs of a mobile world
Research undertaken in migration and health has to respond to the whole population need. This includes not only the migrants themselves but also the other groups affected by migration, such as families left in countries of origin and host communities. To enable this response, the migrant population themselves should be viewed as an asset and a participatory approach encouraged, in which migrants and local communities are included in all stages of the research process. Further, mixed methods and qualitative research, including anthropological and sociological work, is needed to understand sociocultural factors of the migration experience, how to reduce barriers to health care, and how the determinants of health might affect migrants differently, with gender analyses throughout. This should be done alongside systems level work to develop processes to mainstream and normalise migration.
We used data from our systematic review on mortality16 to systematically examine which disease areas have been the focus of historical research. Our data suggest that despite being the only ICD-10 disease categories with evidence of increased mortality, infectious and parasitic diseases was the fifth most studied group and external causes of mortality was the third most studied group in international migrants. These data also suggested that labour migrants have been understudied relative to the size of this population globally.
These data can be used to inform future funding priorities, but the current lack of evidence is compounded by the fact that migration has not been a priority among health funders. Review of the mission statements and strategies of the main global health funders (including the Global Fund, Gavi, the Vaccine Alliance, the World Bank, The Bill & Melinda Gates Foundation, the European Commission, United States Agency for International Development, United Kingdom’s Department for International Development, Wellcome Trust, Ford Foundation, Rockefeller Foundation, Medical Research Council, and National Institutes of Health) suggest that only two, the Global Fund and the European Commission, prioritise migrant health. Some funding streams exist that focus on research in humanitarian settings,299 but generally opportunities in migration and health are poor. Research funding agencies (eg, national government entities, charitable foundations, and multilateral funding organisations) should prioritise specific calls to address these gaps.
Data collection, technology, and innovation
Traditional cohort studies are important to understand the life course and intergenerational effects of migration. However, these are expensive and can be inefficient when studying populations with high levels of loss to follow-up. Existing studies have therefore had sub-national coverage on migrants who have already moved.300 One efficient way to produce health data for migrants might be the use of electronic health records with national coverage.301,302 However, in most countries, migrants are not identifiable within these datasets. Big data, such as that collected from wearable devices, mobile phones, the internet, and electronic health records has the potential to provide new sources of information on migration and health and improve uptake and follow-up rates for migrant populations.303 Progress in genomics, spatial models, and mathematical models, including mechanistic approaches that are driven by information from satellites, human behaviour data, and pathogen characteristics, will allow better elucidation of outbreaks and global mapping of infectious transmission.304,305
A difficulty in migration research is understanding internal migration flows with no border controls. A new method to map internal migrants is to use mobile phone data whereby each time a mobile phone is used, the location of the individual is logged. Anonymised mobile phone call detail record data can allow inferences about the movement patterns of individuals to be made, enabling tracking of the movement of populations at scale, even in remote areas. These data were used in 2016, when a monsoon in Nepal caused severe flooding and triggered a series of landslides. Using mobile phone call detail records, researchers were able to show that the monsoon resulted in large movements of people, examine the number of people who spent time outside their home area, identify where these areas of movement were, and identify individuals that were most affected.306
These new techniques are not without risks, ethical issues, and logistical problems. If personal health records or mobile data can be used to track where people have been, migrants might be reluctant to use them. In the case of the Dublin Regulation in the EU, this might mean that a migrant could be sent back to their first country of entry in Europe identified using such tracking technology. The acceptability of mobile health records therefore needs to be assessed further and any implementation of this method should undergo routine monitoring and assessment of the effects to include qualitative perspectives. Health professionals should recognise the need to protect the data and safeguards, including firewalls should be used to separate who can access the data. New technologies, such as the use of blockchains, can help to keep the data secure but might not be possible in low resource countries.
Intervention research
Although this Commission found ample evidence on differences in physical and mental health morbidity between migrants and host populations, information on specific interventions to improve the delivery of services or alter diagnosis and treatment pathways to better cater for migrants was scarce. To complement our understanding of health consequences, resources should be directed to find the best ways to improve health, from clinical and behavioural to health systems studies. Evidence on interventions outside the health system and focused on improving social, political, and economical determinants of health are also essential. Outside of the humanitarian setting and in populations who have previously migrated, robust interventions to improve the health of migrants are uncommon, particularly for neglected groups, such as older people left behind when their families migrate or LGBTI migrants. If evidence of effectiveness exists, for example talking-based therapies for post-traumatic stress disorder in refugees,259,260 data are needed on how to scale up and assess them. There might also be scope for adaptation and evaluation of interventions that work in other marginalised groups.
Understanding the best treatment regimens and modifications in mobile populations to ensure continuity of care is urgently needed. Advances in digital technology allow diagnosis and monitoring of treatment for infections to be undertaken remotely; removing the need for a clinic visit allows the prospect of remote-management and self-management for mobile populations.
In populations that have been traumatised by violence, either at the individual or community level, research on pathways to prevent or improve management of both physical and mental health are needed. Schools have been suggested as important sites for mental health intervention research for both child refugees and their families, although studies done thus far have been small and difficult to replicate.307 Moreover, intervention implementation should include routine monitoring and evaluation of programmes to strengthen migration health interventions long term.
Health policy and systems research
Our analysis of health systems and migration concludes that current thinking on health systems could well have a migration problem. Mainstream views of a health system tend to be of a jurisdiction defined by geopolitical boundaries within which services are provided, rather than—more appropriately and justly—a societal response to people’s needs regardless of their official status. Contemporary advances in trans-disciplinary health policy and systems research can partly address this problem. Health policy and systems research is concerned with answering evaluative, explanatory, and exploratory questions focused on bringing change in health systems and the policy processes that shape and underpin them.308 Multiple disciplines, such as economics, political science, sociology, anthropology, and public health, contribute towards this change. Of late, there has been a turn towards a people-centric approach to the design and process of reasearch, with the recognition that changes in health systems are not focused on one thing but are driven by different people at different levels of the system, including service users and communities.309 As such, health policy and systems research has the potential to include migration in relation to health system research questions. Under the umbrella question of how we can make existing real-world health systems more responsive to human mobility, thereby improving individual and population health outcomes, there is a range of valuable lines of inquiry. More qualitative research focusing on the experience of health care from the perspectives of migrant service users and providers can broaden and enrich our understanding of their needs in different settings. Finally, and essentially, implementation research on existing migration-friendly initiatives can help to identify bottlenecks and enablers, and which approaches work in which contexts and for whom, and translate those insights to other contexts. As we have described above, all aspects of migration and health are gendered and thus implementing gender analyses in all research is strongly recommended.
Research ethics
Migration should be an essential component of public health ethics, particularly in relation to social justice. Migration is a good example of when ethical issues related to health and determinants of health exist across state boundaries. Many important ethical issues exist, including the prioritisation of services, the detention and deportation of migrants, and the labelling of and discrimination against migrant groups. However, literature is scarce on migration and public health ethics beyond issues of access to health care.
Compliance with standards of research ethics is essential and can be particularly challenging in vulnerable and mobile populations. The social, cultural, legal, and political aspects of migration status are often associated with higher amounts of susceptibility. Because of this inferior social position of many migrants and the risks from encountering deprivation of rights and dignity, researchers have to be highly sensitive and responsive to unintended and possibly harmful consequences of their work. The particular vulnerability to abuse and discrimination of disadvantaged groups demands the inclusion of the social and historical contextualisation of research. Systematic reflection on ethical questions thus should be a part of all steps in the research process. When defining the research question, it is crucial to reflect on whether the research is likely to produce valuable data to improve living and health conditions. Data collection can cause fear and distrust in populations with experiences of exclusion and persecution, and trigger traumatising events in the case of victims and witnesses of torture, sexual abuse, and other types of violence. Communication of research results should be sensitive to the risk of directly or indirectly sustaining or promoting stereotypes and stigma. The principle of first do no harm thus applies to all steps of the research process, while issues of confidentiality and informed consent especially apply to data security and the risk of abuse of medical and personal data (eg, migration routes reflected in the medical record) by migration authorities. Little is known about whether migrants are willing to share their data and the perspectives they might have on this. Research activities should be sensitive to systematically include ethical reflection and accountability in the research process and be responsive to findings that encourage a reconsideration of research questions and methodological and moral challenges. Institutional review board approval is mandatory for all research activities, yet not sufficient, as it lacks the required flexibility and responsiveness. A key process to ensure that the research is fit for purpose is to engage with the public on migration and health. This engagement is in the design of the research, participatory methods in the conduct of the research, and in the dissemination and discussion of the results.
Conclusion
Migration should be urgently treated as a core determinant of health and wellbeing and addressed as a global health priority of the 21st century. Migration and global health are both defining issues of our time. How the world addresses human mobility will determine public health and social cohesion for decades to come. Our work for this Commission aimed to provide robust evidence on migration and health to examine the structures, systems, and contexts at the intersection of human mobility and individual and population health. By systematically presenting evidence on what is known about health and migration, it has been our intention to dispel populist myths about a perceived "other" and to suggest promising strategies for a highly mobile world. Amid international dialogues about safer, healthier migration, substantial gains can be achieved towards multiple SDGs by resisting the turbulence of nationalist xenophobic discourse.
In summary, our findings highlight that modern migration is a diverse and dynamic phenomenon, and the health of people who migrate generally reflects the circumstances of migration. Our evidence indicates that, with sufficient political will, the international community, states, and local providers have the knowledge and resources necessary to ensure that individuals who are most vulnerable to harm are not health-marginalised. But, at the same time, our findings suggest that attitudes, misperceptions, and cynical political motivations can hinder rights-based approaches to health for migrants, especially for people seeking safety and economic security for themselves and their family. We must ensure that a migrant’s equal right to health is respected and implemented.
Our multiple analyses also contradict myths about who is migrating where and the health burden of migration on recipient locations. Data for migration tell us that more people from LMICs are migrating within their own countries and region than across HIC borders, even if vocal political rhetoric implies otherwise. Additionally, migrants are, on average, healthier, better educated, and employed at higher rates than individuals in destination locations. However, many men and women who migrate are subjected to laws, restrictions, and discrimination that put them at risk of ill health. Particular mobile subgroups are especially likely to be exposed to migration-related harm and excluded from care, such as trafficking victims, irregular migrants, low wage workers, and asylum seekers. These highly vulnerable migrant subgroups are also frequently individuals who have been forced to move because of global economic and political forces well beyond their control. These global economic and political forces also apply to the populations left behind, when family members migrate for work or groups who are unable to flee from conflict areas or environmental dangers. The evidence indicates that through targeted rights-based laws; inclusive, migrant-friendly health systems; and mobile medical services, it is possible to reduce migration-related risks and increase peoples’ access and use of health services. Migration-informed laws, services, and public perceptions can increase determinants of good health. These determinants include social inclusion, safe employment with fair wages, good nutrition, decent housing and hygiene, and universally accessible health systems that do not result in potentially catastrophic costs for families.
Moreover, multiple opportunities exist to intervene to address health throughout the phases of a migrant’s journey. We believe that now is the time to call on our humanity and to take advantage of worldwide mobility to secure global health, especially for migrant groups who are most at risk of exclusion. We have the evidence, tools, and potential international political will via the UN Global Compact for Migration and the Global Compact on Refugees, and the SDGs.
The Commissioners have reviewed a mass of data collected by researchers from around the world. These data describe the scale and nature of migration and the many threats to the health of men and women and their families who are migrating. However, it is impossible to capture the entire distressing picture on the pages of a scientific journal. That would require the many individual accounts of tragedy, of children drowning in parents’ arms or dying by the wayside, or of individual heroism of people who risk their own lives to rescue them. For such stark realities, we can look to the few journalists and humanitarian organisations who have recorded these accounts, such as the now unforgettable picture of the lifeless body of Alan Kurdi being lifted from a Turkish beach. Anyone viewing these images should surely ask why the international community has done so little to live up to its commitments to advance the health of migrating populations, and especially individuals who have been forced to migrate. How can we explain this inertia?
There are no simple answers to these questions, but one indisputable reality is that, in the discourse on migration, health is far down the list of priorities. International meetings on migration are instead dominated by other considerations, such as domestic politics, national security, international trade, and commerce—especially when politicians ruthlessly exploit migration for their own purposes. These considerations almost always take precedence over the health needs of migrants. Indeed, if health is discussed at all, it is often unjustifiably framed as the migrant posing a threat to the population in the destination country, either as a vector for infections or a terrorist risk. Health and migration have competing, if not conflicting, policy goals. Health goals are inclusive (eg, better health for all, the Hippocratic oath) and international migration policy goals are exclusionary (secure borders, national trade). The other key challenges include financial issues and leadership.
Investing in the health of populations and individuals is generally an expensive long-term commitment, such as providing medical services over lifetimes. However, for state budgets, protecting borders and arranging deportation can seem a lesser investment for greater political gain often contrary to the more positive actual and perceived contributions of migrants by the public. Health leadership in the realm of migration policy making often seems to be considered as less important than other policy interests. Why are health leaders absent from the top table, engaging proactively in high level debates on migration? Instead, the health sector is often left to pick up the pieces of migration policies that leave the lives of migrants in tatters. Additionally, because the health sector will remain dedicated to these humanitarian ideals, policy makers can continue to prioritise security, exclusion, and trade, while discriminatory rhetoric reenforces the neglect and abuse of migrants. A second, much simpler question is why do some migrants have better health and health services than others? The answer is quite obviously related to the individual’s social and economic status and the power this wields. Therefore, perhaps the greatest challenge to achieving health equity for disadvantaged migrating populations will be promoting rights and empowerment that enable individuals to assert their own rights to health. The publication of the two UN Global Compacts with numerous references to health in the context of migration and for refugees presents an unprecedented opportunity that should be leveraged for specific action. Investments should be shifted towards empowering migrants through, for example, migrant worker insurance schemes or regional health and social accords. We present our recommendations for maximising the health of migrants in panel 10.
Panel 10. Recommendations.
The Commission makes the following recommendations that aim to maximise the health of people on the move and societies more broadly. We call for urgent action to raise migration and health on the political agenda in an objective and humane manner, increase multi-stakeholder action, and create robust accountability and monitoring mechanisms.
- Dedicate political capital, financial, and human resources to fulfil global commitments to secure healthy migration and improve the security and wellbeing of mobile groups, especially the most marginalised.
- States need to commit strong leadership to meet their commitments to the 2030 Sustainable Development Goals, and fulfil the health objectives of the Global Compact for Migration, the Global Compact on Refugees, and other relevant global agreements. We advocate for clarity in leadership at the global level and for support to national actors (public health workforce and civil society). We urge the Secretary General of the UN to appoint a Special Envoy on Migration and Health, regional bodies to appoint a regional representative, and national governments to have country-level focal points for migration and health.
- International and regional bodies need to use existing agreements, such as the Global Compacts and the WHO Action Plan, to prioritise the health, rights, and security of migrating populations. Decision makers should allocate sufficient funding to create equitable health protection mechanisms for mobile groups, such as joint health insurance or social safety net schemes, mutual health accords, and other mechanisms to integrate these groups into health systems.
- Multilateral funding organisations should have clear mechanisms to include migrants into national and regional proposals. Ultimately the inclusion of migrants into existing health systems, within the scope of universal health coverage, should improve such systems to benefit nationals and migrants.
- States and the international community should urgently develop policy links that recognise the integral connections between environmental conditions and anthropogenic climate change, migration, and health. Decision makers should join forces to predict and respond to the effects of climate change on population mobility. Investments are needed in sustainable health infrastructure models that respond to migrants’ health protection needs, including Disaster Risk Reduction mechanisms.
- States should go beyond rhetoric to tackle modern slavery by recognising the exploitation of migrant workers, especially in informal labour, and trafficking of individuals and families displaced by conflict, natural disasters, and environmental degradation.
- Re-balance policy making in migration, trade and environment, and foreign affairs to give greater prominence to health. Foster cross-sector, complementary decision making that integrates health considerations across policies and services that determine the health of migrants.
- International and regional bodies and states should create a prominent place for health representatives at high level policy making forums for migration-related sectors (eg, immigration, trade, labour, environment, security, education). Health leaders should assert their rights to participate in these policy forums. Conversely, high level representatives from other sectors should be encouraged to participate in similar health policy making forums.
- Health leaders and practitioners should fully engage in policy dialogues that affect migration, including the macroeconomic forces that affect population mobility. They should participate in multisector budgeting and programme planning for migrants.
- Migrants and their advocates should have a voice in strategies that affect their health and safety.
- Confront urgently, vigorously, and persistently divisive myths and discriminatory rhetoric about migrants.
- Political leaders and elected officials should resoundingly and consistently condemn misinformation and disinformation about migrants, especially xenophobia proffered by divisive and populist voices. Fact-checking, promoting truth, and vociferous objections should not be left to migrants and their advocates alone.
- Governments, international agencies, and civil society should stay ahead of developments in social media and digital technology to shut down anti-migrant abuse and promote fact-based portrayals of global migration, particularly the widespread reliance on migrants for economic development, health services, educational institutions, and cultural richness.
- Advocate for and improve the rights of migrants to ensure safe and healthy educational and working conditions that includes freedom of movement with no arbitrary arrest.
- States, regional bodies, and the international community should use policies, laws, and resources to improve the rights of migrants. States and businesses should ensure workplace health and safety measures, employment conditions, and implement inspections and monitoring tools targeted to protect migrant workers. Migrants should be assured easy-to-access, equitable health care and worker compensation entitlements. Transparent reporting using an agreed upon framework should occur.
- Policy makers should guarantee migrants’ rights and inclusion across sectors that affect the health of migrants, including workers, internally displaced people, asylum seekers, and refugees, and empower migrants to assert their rights to the underlying social, political, economic, and cultural determinants of physical and mental health.
- Social and health sector leaders and educational institutions should offer training to promote cultural competency, cultural mediation, and migrant-sensitive services, including outreach programmes for hard-to-reach individuals and groups.
- States should abolish arbitrary arrest and the detention of all migrants, especially children and adolescents. They should remove health restrictions on entry, stay, and residence and the deportation of individuals with specific health conditions. These measures should be codified in international agreements and included in national law.
- There is an urgent need to ensure adequate monitoring, evaluation, and research to support the implementation of the Global Compacts.
- States, coordinating with the global community and relevant local professionals (eg, health, refugee services, labour, civil society), should put into place robust monitoring frameworks and independent reporting mechanisms to ensure accountability in the delivery of the Global Compact for Migration and Global Compact on Refugees. Strategies should include transparent and easy to compare monitoring frameworks and mechanisms to report how regions and countries are adhering to the policy principles and implementation components on migration and health.
- The Commission, therefore, recommends that a Global Migration and Health Observatory is established to develop evidence-based indicators and measurement methods, and to ensure improved reporting, transparency, and accountability on the implementation of the Global Compact for Migration and the Global Compact on Refugees. The Observatory should also monitor the progressive inclusion of migrants within universal health coverage country plans and achievements.
- Specific recommendations for research are outlined in greater detail in panel 9 and were reached through a consensus approach by Commissioners.
The post-Commission phase
The Commission hopes to inspire action, building on the health and health determinant aspects of the Global Compact for Migration and Global Compact on Refugees, through various key initiatives. There is considerable momentum in the migration and health community to move from recommendations to action. We plan to engage at multiple levels of public life to raise the profile of migration and health. This engagement would be at the community level with the public, including migrants themselves and populations at all stages of the migration process. Secondly, we plan to support the establishment of an inclusive global mechanism that will bring together civil society with researchers, non-governmental bodies and charities, and multilateral organisations including WHO, International Organization for Migration, and the UN Refugee Agency to establish a distributed observatory to develop agreed indicators and a monitoring framework that has local, regional, and global reach. A distributed observatory is a model where several regional partners contribute to this global initiative following a common set of international agreed standards. The governance, reporting, and advocacy efforts will include the use of reports, media, and the arts to challenge elected officials and will support research to generate new evidence on implementating best practice. We expect the observatory to report annually and liaise with regional stakeholders for adapted versions of the report to allow local and interregional action on migration and health.
Supplementary Material
Key messages.
We call on nation states, multilateral agencies, non-governmental organisations, and civil society to positively and effectively address the health of migrants by improving leadership and accountability. First, we urge the UN to appoint a Special Envoy on Migration and Health and national governments to have a country-level focal point for migration and health. This would enable much needed coordination and also ensure that migrants are included in all decisions about their health. Second, we propose that a Global Migration and Health Observatory is established to develop evidence-based migration and health indicators to ensure better reporting, monitoring, transparency, and accountability on the implementation of the Global Compact for Migration and the Global Compact on Refugees.
International and regional bodies and states should re-balance policy making in migration to give greater prominence to health by inviting health representatives to high level policy making forums on migration. Health leaders and practitioners should fully engage in dialogues on the macroeconomic forces that affect population mobility and participate in multisector budgeting and programme planning for migrants.
Racism and prejudice should be confronted with a zero tolerance approach. Public leaders and elected officials have a political, social, and legal responsibility to oppose xenophobia and racism that fuels prejudice and exclusion of migrant populations. Health professionals’ and organisations’ awareness of racism and prejudice should be strengthened through regulatory and training bodies including accreditation, educational courses, and continuous professional development. Civil society organisations should hold leaders to account to ensure the implementation of these obligations.
Universal and equitable access to health services and to all determinants of the highest attainable standard of health within the scope of universal health coverage needs to be provided by governments to migrant populations, regardless of age, gender, or legal status. Solutions should include input from migrants and be specific to the diverse migrant populations. For those exposed to disaster or conflict, or both, mobility models and Disaster Risk Reduction systems should be integrated. Targeted interventions to improve the rights of migrant workers, their knowledge of workplace health and safety, and entitlement to health care are needed.
Acknowledgments
The funders of the Commission had no role in design, information, collection, analysis, interpretation, writing of the report, or the decision to submit the paper for publication. All authors had full access to all the data in the report and had final responsibility for the decision to submit for publication. We thank the Wellcome Trust, Rockefeller Foundation, UK National Institute for Health Research, the UCL Grand Challenges in Global Health, and the EU’s Health Programme (E-DETECT TB, 709624). Views expressed here are those of the authors only and their sole responsibility; they cannot be considered to reflect the views of the European Commission, the Consumers, Health, Agriculture and Food Executive Agency, any other body of the EU, or our other funders. We are also grateful to the following individuals for their contribution to various stages of the Commission and meetings: Catherine Kyobutungi (Commissioner until September 2017), Valentina Parisi, Victoria Rodulson, Kanokporn Kaojaroen, and Laura B Nellums. The INDEPTH Network collaboration acknowledges support from National Institutes of Health for the Migration and Health Follow-up Study. IA acknowledges funding from the National Institute for Health Research (SRF-2011-04-001; NF-SI-0616-10037), Medical Research Council, UK Department of Health, and the Wellcome Trust. DD received salary funding from the National Institute for Health Research. The views expressed are those of the authors and not necessarily those of the National Health Service, the National Institute for Health Research, or the Department of Health. RWA is supported by a Wellcome Trust Clinical Research Career Development Fellowship (206602/Z/17/Z).
Footnotes
Contributors
The UCL-Lancet Commission on Migration and Health has been an international collaboration spanning multiple continents. The Commission was chaired and led by IA, with support from the steering group (RWA, RB, DD, MO, and CZ). The Commission was coordinated by MO, with research assistance from RI for the first year and RB for the last year of the Commission work. The work for the Commission was undertaken in six subgroups and all commissioners met in person on three occasions: in London, UK (2016), London, UK (2017), and Bellagio, Italy (2017). The first draft of the manuscript was written by RWA and DD, the second draft was compiled by IA, DD, MO, and CZ. TM and LR provided sections on law; MK, NG, and BK provided sections on culture, society, and racism; AM and CZ provided sections on labour migration and trafficking; KS, DM, and PD provided sections on health systems; ST and RWA provided sections on data; PSa provided sections on the environment; MK provided sections on human rights; and NG provided sections on disabilities. All authors read and critiqued the manuscript and approved the final version of the report.
Declaration of interests
IA, DD, and RWA undertook paid consultancy work in support of the Doctors of the World 2017 Observatory report—Falling through the cracks: the failure of universal healthcare coverage in Europe. MO reports personal fees from WHO Regional Office for Europe, WHO Regional Office for the Eastern Mediterranean, Medecins Sans Frontieres, Operational Centre Brussels, outside the submitted work; and is a steering committee member for the Syria Public Health Network, which conducts research and policy work on public health issues in Syria and the region. All other authors declare no competing interests. The views and opinions expressed in this Article are those of the authors and do not necessarily reflect the views, official policy, or position of the International Organization for Migration, an organisation that is part of the UN system. The designations employed and the presentation of material throughout the article do not imply the expression of any opinion whatsoever on the part of the International Organization for Migration, concerning the legal status of any country, territory, city or area, or of its authorities, or concerning its frontiers or boundaries.
For the Lancet Series on Health in Humanitarian Crises see https://www.thelancet.com/series/health-in-humanitarian-crises
For the Syria Lancet Commission see https://www.thelancet.com/commissions/syria
For the UN High Commissioner for Refugees’ Operational Data Portal see https://data2.unhcr.org/en/situation
For the UN High Commissioner for Refugees Global Trends Report see http://www.unhcr.org/globaltrends2017/
For the UN High Commissioner for Refugees Global Trends Report see http://www.unhcr.org/globaltrends2017/
For the UN Convention on the Rights of the Child see https://www.ohchr.org/Documents/Professionallnterest/crc.pdf
For the UN Convention on the Rights of Persons with Disabilities see http://www.un.org/disabilities/documents/convention/convoptprot-e.pdf
Contributor Information
Prof Ibrahim Abubakar, Institute for Global Health.
Robert W Aldridge, Institute for Health Informatics.
Prof Mauricio L Barreto, University College London, London, UK; Centre for Data and Knowledge Integration for Health, Fundação Oswaldo Cruz, Salvador-Bahia, Brazil.
Poonam Dhavan, International Organization for Migration, Geneva, Switzerland.
Fouad M Fouad, Faculty of Health Sciences, American University of Beirut, Beirut, Lebanon.
Prof Nora Groce, Leonard Cheshire Centre, Institute of Epidemiology and Healthcare.
Prof Yan Guo, School of Public Health, Peking University, Beijing, China.
Sally Hargreaves, Institute of Infection and Immunity, St George’s, University of London, London, UK; International Health Unit, Section of Infectious Diseases and Immunity, Imperial College London, London, UK.
Michael Knipper, Institute for the History of Medicine, Justus Liebig University Giessen, Giessen, Germany.
Prof J Jaime Miranda, CRONICAS Center of Excellence in Chronic Diseases, Universidad Peruana Cayetano Heredia, Lima, Peru.
Prof Nyovani Madise, African Institute for Development Policy, Lilongwe, Malawi; Centre for Global Health, Population, Poverty and Policy, University of Southampton, Southampton, UK.
Prof Bernadette Kumar, Norwegian Centre for Minority Health Research, Oslo, Norway; Department of Community Medicine and Global Health, Institute of Health and Society, Faculty of Medicine, University of Oslo, Oslo, Norway.
Davide Mosca, International Organization for Migration, Geneva, Switzerland.
Prof Terry McGovern, Program on Global Health Justice and Governance, Mailman School of Public Health, Columbia University, New York, NY, USA.
Leonard Rubenstein, Center for Public Health and Human Rights; Johns Hopkins Bloomberg School of Public Health, and Berman Institute of Bioethics.
Prof Peter Sammonds, Institute for Risk and Disaster Reduction.
Prof Susan M Sawyer, Johns Hopkins University, Baltimore, MD, USA; Department of Paediatrics, University of Melbourne; University of Melbourne, Parkville, VIC, Australia; Centre for Adolescent Health, and Murdoch Children–s Research Institute, Royal Children–s Hospital, Parkville, VIC, Australia.
Kabir Sheikh, Public Health Foundation of India, Institutional Area Gurgaon, India; Nossal Institute of Global Health, University of Melbourne, Melbourne, VIC, Australia.
Prof Stephen Tollman, MRC/Wits Rural Public Health and Health Transitions Research Unit, School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa.
Prof Paul Spiegel, Department of International Health; Johns Hopkins Center for Humanitarian Health.
Prof Cathy Zimmerman, Gender, Violence and Health Centre, London School of Hygiene and Tropical Medicine, London, UK.
UCL-Lancet Commission on Migration and Health:
Mustafa Abbas, Eleanor Acer, Ayesha Ahmad, Bayes Ahmed, Seye Abimbola, Juan D Beltrán, Karl Blanchet, Philippe Bocquier, Fiona Samuels, Olga Byrne, Sonia Haerizadeh, Rita Issa, Mark Collinson, Carren Ginsburg, Ilan Kelman, Alys McAlpine, Nicola Pocock, Barbara Olshansky, Dandara Ramos, Katerina Stavrianaki, Michael White, and Suzanne Zhou
References
- 1.International Organization for Migration. [accessed June 25, 2018];World Migration Report. 2018 https://www.iom.int/wmr/world-migration-report-2018 .
- 2.Urquia ML, Gagnon AJ. Glossary: migration and health. [accessed Jan 15, 2018];2011 doi: 10.1136/jech.2010.109405. [DOI] [PubMed] [Google Scholar]
- 3.Zimmerman C, Kiss L, Hossain M. Migration and health: a framework for 21st century policy-making. PLoS Med. 2011;8:e1001034. doi: 10.1371/journal.pmed.1001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Major B, Dovidio JF, Link BG. The Oxford Handbook of Stigma, Discrimination, and Health. 2017. [accessed June 14, 2018]. https://books.google.com/books/about/The_Oxford_Handbook_of_Stigma_Discrimina.html?id=aOw9DwAAQBAJ .
- 5.Elliott P, Hennigan WJ. Exclusive: Navy document shows plan to erect ‘austere’ tent cities for immigrants. 2018. [accessed July 1, 2018]. http://time.com/5319334/navy-detainment-centers-zerol-tolerance-immigration-family-separation-policy/
- 6.McNeill L, Moore R. Sustainable fashion consumption and the fast fashion conundrum: fashionable consumers and attitudes to sustainability in clothing choice. Int J Consum Stud. 2015;39:212–22. [Google Scholar]
- 7.United Nations. Treaty Series. International Covenant on Economic, Social and Cultural Rights. OHCHR. 1976;993:3. [Google Scholar]
- 8.UN Committee on Economic, Social and Cultural Rights. General Comment 14, The right to the highest attainable standard of health. 2000. [accessed Jan 15, 2018]. http://www.refworld.org/pdfid/4538838d0.pdf .
- 9.Mann JM, Gostin L, Gruskin S, Brennan T, Lazzarini Z, Fineberg HV. Health and human rights. Health Hum Rights. 1994;1:6–23. [PubMed] [Google Scholar]
- 10.Compact for Migration. UN Refugees and Migrants. [accessed Jan 12, 2018]. http://refugeesmigrants.un.org/migration-compact .
- 11.New York Declaration for Refugees and Migrants: resolution adopted by the General Assembly, 3 October 2016, A/RES/71/1. United Nations General Assembly; 2016. [accessed Jan 15, 2018]. http://www.un.org/en/ga/search/view_doc.asp?symbol=A/RES/71/1 . [Google Scholar]
- 12.Tillerson R. Participation in the Global Compact on Migration. U.S. Department of State; 2017. [accessed Jan 12, 2018]. published online Dec 3. https://www.state.gov/secretary/20172018tillerson/remarks/2017/12/276190.html . [Google Scholar]
- 13.Henley JE. EU’s migrant centres could breach human rights, say campaigners. [accessed July 1, 2018];The Guardian. 2018 published online June 29. http://www.theguardian.com/world/2018/jun/29/eus-migrant-centres-could-breach-human-rights-say-campaigners . [Google Scholar]
- 14.UN Stats Division. [accessed Jan 15, 2018];The Sustainable Development Goals Report 2016: Leaving no one behind. 2016 https://unstats.un.org/sdgs/report/2016/leaving-no-one-behind .
- 15.Fellmeth G, Rose-Clarke K, Zhao C, et al. Health impacts of parental migration on left-behind children and adolescents: a systematic review and meta-analysis. Lancet. doi: 10.1016/S0140-6736(18)32558-3. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aldridge RW, Nellums LB, Bartlett S, et al. Global patterns of mortality in international migrants: a systematic review and meta-analysis. Lancet. doi: 10.1016/S0140-6736(18)32781-8. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lynch C, Roper C. The transit phase of migration: circulation of malaria and its multidrug-resistant forms in Africa. PLoS Med. 2011;8:e1001040. doi: 10.1371/journal.pmed.1001040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davies AA, Borland RM, Blake C, West HE. The dynamics of health and return migration. PLoS Med. 2011;8:e1001046. doi: 10.1371/journal.pmed.1001046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pocock NS, Mahmood SS, Zimmerman C, Orcutt M. Imminent health crises among the Rohingya people of Myanmar. BMJ. 2017;359:j5210. doi: 10.1136/bmj.j5210. [DOI] [PubMed] [Google Scholar]
- 20.United Nations Human Rights Office of the High Commission. ‘Detained and dehumanised‘ report on human rights abuses against migrants in Libya. [accessed June 28, 2018]. https://www.ohchr.org/Documents/Countries/LY/DetainedAndDehumanised_en.pdf .
- 21.UN Deputy Spokesperson. Sexual exploitation and abuse within the UN. United Nations; 2018. [accessed Sept 8, 2018]. published online July 30. https://www.un.org/preventing-sexual-exploitation-and-abuse/content/quarterly-updates. [Google Scholar]
- 22.McAlpine A, Hossain M, Zimmerman C. Sex trafficking and sexual exploitation in settings affected by armed conflicts in Africa, Asia and the Middle East: systematic review. BMC Int Health Hum Rights. 2016;16:34. doi: 10.1186/s12914-016-0107-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Freccero J, Biswas D, Whiting A, Alrabe K, Seelinger KT. Sexual exploitation of unaccompanied migrant and refugee boys in Greece: approaches to prevention. PLoS Med. 2017;14:e1002438. doi: 10.1371/journal.pmed.1002438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whitson A. ‘To protect her honour’: child marriage in emergencies–the fatal confusion between protecting girls and sexual violence. CARE; [accessed Jan 17, 2018]. http://insights.careinternational.org.uk/publications/to-protect-her-honour-child-marriage-in-emergencies-the-fatal-confusion-between-protecting-girls-and-sexual-violence . [Google Scholar]
- 25.Brides GN. Untying the knot: exploring early marriage in fragile states. World Vision; 2013. [accessed Jan 17, 2018]. https://www.girlsnotbrides.org/resource-centre/untying-the-knot-exploring-early-marriage-in-fragile-states/ [Google Scholar]
- 26.The World Bank. United Nations Population Division, Migrant stock; Population total; Refugees. 2012. [accessed Nov 1, 2018]. https://data.worldbank.org/
- 27.Orcutt M, Aldridge R, Devakumar D, Abubakar I. UCL-Lancet Commission on Migration and Health. 2018. [accessed Nov 14, 2018]. https://www.migrationandhealth.org/data . [DOI] [PubMed]
- 28.Migration Observatory. Immigration by category: workers, students, family members, asylum applicants—Migration Observatory. [accessed June 14, 2018]. http://www.migrationobservatory.ox.ac.uk/resources/briefings/immigration-by-category-workers-students-family-members-asylum-applicants/
- 29.d’Albis H, Boubtane E, Coulibaly D. Macroeconomic evidence suggests that asylum seekers are not a ‘burden’ for Western European countries. Science Advances. 2018;4:eaaq0883. doi: 10.1126/sciadv.aaq0883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Siyam A, Dal Poz MR, editors. Migration of health workers: WHO code of practice and the global economic crisis. 2014. [accessed Jan 17, 2018]. https://www.who.int/hrh/migration/14075_MigrationofHealth_Workers.pdf .
- 31.Baker C. [accessed Nov 6, 2018];NHS staff from overseas: statistics. House of Commons Library Briefing paper Number 7783. 2018 http://researchbriefings.parliament.uk/ResearchBriefing/Summary/CBP-7783 .
- 32.Okeke EN. Brain drain: Do economic conditions “push” doctors out of developing countries? Soc Sci Med. 2013;98:169–78. doi: 10.1016/j.socscimed.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 33.Kulu H, Hannemann T, Krapf S, Wolf K, Andersson G, Persson L. Country-specific case studies on fertility among the descendants of immigrants: Part 1. Families and Societies. 2015. [accessed Jan 15, 2018]. http://www.familiesandsocieties.eu/wp-content/uploads/2015/09/WP39HillEtAl2015Part1.pdf .
- 34.Keygnaert I, Guieu A, Ooms G, Vettenburg N, Temmerman M, Roelens K. Sexual and reproductive health of migrants: does the EU care? Health Policy. 2014;114:215–25. doi: 10.1016/j.healthpol.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 35.Central Statistical Agency Ethiopia and ICF. Ethiopia Demographic and Health Survey 2016. 2016. [accessed Oct 30, 2018]. https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf .
- 36.National Statistical Office. NSO/Malawi and ICF. Malawi Demographic and Health Survey 2015–16. 2017. [accessed Oct 30, 2018]. https://dhsprogram.com/pubs/pdf/FR319/FR319.pdf .
- 37.Kenya National Bureau of Statistics, Ministry of Health/Kenya, National AIDS Control Council/Kenya, Kenya Medical Research Institute, National Council for Population and Development/Kenya, and ICF International. Kenya Demographic and Health Survey 2014. 2015. [accessed Oct 30, 2018]. https://dhsprogram.com/pubs/pdf/fr308/fr308.pdf .
- 38.Ministry of Health, Community Development, Gender, Elderly and Children, Tanzania Mainland, Ministry of Health Zanzibar, National Bureau of Statistics Tanzania, Office of Chief Government Statistician Zanzibar, ICF. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Tanzania Demographic and Health Survey and Malaria Indicator Survey (TDHS-MIS) 2015-16. 2016. [accessed Oct 30, 2018]. https://dhsprogram.com/pubs/pdf/fr321/fr321.pdf .
- 39.Ministry of Health and Family Welfare Government of India. International Institute for Population Sciences India and Macro International. National Family Health Survey NFHS-3, 2005–06: India: Volume I. 2007. [accessed Oct 30, 2018]. https://dhsprogram.com/pubs/pdf/frind3/frind3-vol1andvol2.pdf .
- 40.Chynoweth SK. Advancing reproductive health on the humanitarian agenda: the 2012-2014 global review. Confl Health. 2015;9(suppl 1):11. doi: 10.1186/1752-1505-9-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Migration Policy Debates. Is migration good for the economy? Organisation for economic co-operation and development. 2014. [accessed Dec 17, 2017]. https://www.oecd.org/migration/OECD%20Migration%20Policy%20Debates%20Numero%202.pdf .
- 42.IMF Blog. Migrants Bring Economic Benefits for Advanced Economies. 2016. published online Oct 24 https://blogs.imf.org/2016/10/24/migrants-bring-economic-benefits-for-advanced-economies/
- 43.Jauer J, Liebig T, Martin JP, Puhani P. [accessed Jan 24, 2018];Migration as an adjustment mechanism in the crisis? A comparison of Europe and the United States. OECD Social, Employment and Migration Working Papers. 2014 https://www.oecd-ilibrary.org/social-issues-migration-health/migration-as-an-adjustment-mechanism-in-the-crisis-a-comparison-of-europe-and-the-united-states_5jzb8p51gvhl-en .
- 44.KNOMAD. Migration and development brief 29, migration and remittances: recent developments and outlook special topic: transit migration. 2018. [accessed June 25, 2018]. http://www.knomad.org/publication/migration-and-development-brief-29 .
- 45.Marks L, Worboys M, editors. Migrants, minorities and health. Historical and contemporary studies. Routledge; London/New York: 1999. [Google Scholar]
- 46.Aldridge RW, Zenner D, White PJ, et al. Tuberculosis in migrants moving from high-incidence to low-incidence countries: a population-based cohort study of 519 955 migrants screened before entry to England, Wales, and Northern Ireland. Lancet. 2016;388:2510–18. doi: 10.1016/S0140-6736(16)31008-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dahle UR, Eldholm V, Winje BA, Mannsåker T, Heldal E. Impact of immigration on the molecular epidemiology of Mycobacterium tuberculosis in a low-incidence country. Am J Respir Crit Care Med. 2007;176:930–35. doi: 10.1164/rccm.200702-187OC. [DOI] [PubMed] [Google Scholar]
- 48.Aldridge RW, Yates TA, Zenner D, White PJ, Abubakar I, Hayward AC. Prxntry screening programmes for tuberculosis in migrants to low-incidence countries: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14:1240–49. doi: 10.1016/S1473-3099(14)70966-1. [DOI] [PubMed] [Google Scholar]
- 49.Khan MS, Osei-Kofi A, Omar A, et al. Pathogens, prejudice, and politics: the role of the global health community in the European refugee crisis. Lancet Infect. 2016;16:e173–77. doi: 10.1016/S1473-3099(16)30134-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aldridge R, Devakumar D, Abubakar I. Doctors of the World: vulnerable people should not fear arrest when seeking healthcare. [accessed Jan 16, 2018];The BMJ Opinion. 2017 published online Nov 8. http://blogs.bmj.com/bmj/2017/11/08/doctors-of-the-world-vulnerable-people-should-not-fear-arrest-when-seeking-/ [Google Scholar]
- 51.Mass gatherings health—creating a public health legacy. Lancet. 2012;380:1. doi: 10.1016/S0140-6736(12)61108-8. The Lancet. [DOI] [PubMed] [Google Scholar]
- 52.Ihekweazu C, Abubakar I. Tackling viral haemorrhagic fever in Africa. Lancet. 2017;390:2612–14. doi: 10.1016/S0140-6736(17)32475-3. [DOI] [PubMed] [Google Scholar]
- 53.nited Nations, Department of Economic and Social Affairs, Population Division. [accessed July 4, 2018];International Migration Report 2017 Highlights (ST/ESA/SER.A/404) http://www.un.org/en/development/desa/population/migration/publications/migrationreport/docs/MigrationReport2017_Highlights.pdf .
- 54.International Labour Organization. ILO global estimates on migrant workers: results and methodology. 2015. [accessed Sept 23, 2017]. https://www.ilo.org/global/topics/labour-migration/publications/WCMS_436343/lang--en/index.htm .
- 55.United Nations, Department of Economic and Social Affairs, Population Division. [accessed Nov 1, 2018];International Migration Report 2017: Highlights. 2017 http://www.un.org/en/development/desa/population/migration/publications/migrationreport/docs/MigrationReport2017_Highlights.pdf .
- 56.UNDP. [accessed Nov 18, 2017];Human Development Report 2009: Overcoming barriers—human mobility and development. 2009 http://hdr.undp.org/sites/default/files/reports/269/hdr_2009_en_complete.pdf .
- 57.Farrell K. The rapid urban growth triad: a new conceptual framework for examining the urban transition in developing countries. Sustainability. 2017;9:1047. [Google Scholar]
- 58.Deshingkar P, Grimm S. Internal migration and development: a global perspective. Overseas Development Institute; 2005. [accessed Dec 18, 2017]. https://www.odi.org/resources/docs/68.pdf . [Google Scholar]
- 59.de Haan A. Migrants, livelihoods and rights: the relevance of migration in development policies. Social Development Department, University of Sussex; 2000. [accessed Dec 17, 2017]. https://books.google.com/books/about/Migrants_livelihoods_and_rights.html?hl=&id=ulhEAAAAYAAJ . [Google Scholar]
- 60.Division P. Cross-national comparisons of internal migration: an update on global patterns and trends, Technical Paper No. 2013/1. United Nations Department of Economic and Social Affairs; 2013. [accessed Dec 18, 2017]. http://www.un.org/en/development/desa/population/publications/pdf/technical/TP2013-1.pdf . [Google Scholar]
- 61.Internal Displacement Monitoring Centre and the Norwegian Refugee Council. [accessed Oct 29, 2018];Global Report on Internal Displacement. 2018 http://www.internal-displacement.org/sites/default/files/publications/documents/201805-final-GRID-2018_0.pdf .
- 62.Battistella G. The Palgrave Handbook of International Labour Migration. Palgrave Macmillan; London: 2015. Labour Migration in Asia and the Role of Bilateral Migration Agreements; pp. 299–324. [Google Scholar]
- 63.Terms KM. International Organization for Migration. 2015. [accessed Jan 15, 2018]. published online Jan 14 https://www.iom.int/key-migration-terms.
- 64.Hennebry J, Grass W, Mclaughlin J. Women migrant workers’ journey through the margins: labour, migration, and trafficking. UN Women; 2016. [accessed 24 Oct, 2018]. http://www.unwomen.org/en/digital-library/publications/2017/2/women-migrant-workers-journey-through-the-margins . [Google Scholar]
- 65.Temin M, Montgomery MR, Engebretsen S, Barker KM. Girls on the move: adolescent girls & migration in the developing world. Population Council; 2013. [accessed Jan 15, 2018]. http://www.popcouncil.org/research/girls-on-the-move-adolescent-girls-migration-in-the-developing-world . [Google Scholar]
- 66.International Labour Organization. Migrant children in child labour: a vulnerable group in need of attention. 2013. [accessed Nov 10, 2017]. published online April 26 http://www.ilo.org/ipecinfo/product/download.do?type=document&id=23755.
- 67.International Labour Organization. [accessed Jan 15, 2018];Report IV Addressing governance challenges in a changing labour migration landscape. 2017 http://www.ilo.org/ilc/ILCSessions/106/reports/reports-to-the-conference/WCMS_550269/lang-en/index.htm .
- 68.Fragility, Conflict and Violence. The World Bank; [accessed Jan 15, 2018]. http://www.worldbank.org/en/topic/fragilityconflictviolence/overview . [Google Scholar]
- 69.International Rescue Committee. In search of work - creating jobs for Syrian refugees. A case study of the Jordan Compact. 2017. [accessed Jan 18, 2018]. published online Feb 3 https://www.rescue-uk.org/report/search-work-creating-jobs-syrian-refugees-case-study-jordan-compact.
- 70.United Nations High Commissioner for Refugees. UNHCR Global Trends - Forced Displacement in 2017. [accessed July 4, 2018]. http://www.unhcr.org/statistics/unhcrstats/5b27be547/unhcr-global-trends-2017.html .
- 71.United Nations High Commissioner for Refugees. UNHCR Projected Global Resettlement Needs 2018. [accessed Jan 17, 2018]. http://www.unhcr.org/en-us/protection/resettlement/593a88f27/unhcr-projected-global-resettlement-needs-2018.html .
- 72.International Labour Organization. [accessed Nov 6, 2018];International Labour Report: Global estimates of modern slavery: forced labour and forced marriage. 2017 https://www.ilo.org/global/publications/books/WCMS_575479/lang--en/index.htm .
- 73.Alliance 87. Global estimates of modern slavery: forced labour and forced marriage. 2017. [accessed Jan 16, 2018]. http://www.alliance87.org/global_estimates_of_modern_slavery-forced_labour_and_forced_marriage.pdf .
- 74.Zimmerman C, Kiss L. Human trafficking and exploitation: a global health concern. PLoS Med. 2017;14:e1002437. doi: 10.1371/journal.pmed.1002437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Watts N, Adger WN, Agnolucci P, et al. Health and climate change: policy responses to protect public health. Lancet. 2015;386:1861–914. doi: 10.1016/S0140-6736(15)60854-6. [DOI] [PubMed] [Google Scholar]
- 76.Kang S, Eltahir EAB. North China Plain threatened by deadly heatwaves due to climate change and irrigation. Nat Commun. 2018;9:2894. doi: 10.1038/s41467-018-05252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. [accessed Oct 16, 2017];Intergovernmental Panel on Climate Change Climate Change 2014: Synthesis Report (Longer Report) 2014 https://reliefweb.int/report/world/climate-change-2014-synthesis-report .
- 78.Rigaud KK, de Sherbinin A, Jones B, et al. Groundswell: Preparing for Internal Climate Migration. Washington, DC: World Bank; 2018. [Google Scholar]
- 79.UN General Assembly, Convention Relating to the Status of Refugees. United Nations; 1951. Jul 28, [accessed Oct 26, 2018]. (Treaty Series). http://www.refworld.org/docid/3be01b964.html . [Google Scholar]
- 80.Ottersen OP, Dasgupta J, Blouin C, et al. The political origins of health inequity: prospects for change. Lancet. 2014;383:630–67. doi: 10.1016/S0140-6736(13)62407-1. [DOI] [PubMed] [Google Scholar]
- 81.Napier AD, Ancarno C, Butler B, et al. Culture and health. Lancet. 2014;384:1607–39. doi: 10.1016/S0140-6736(14)61603-2. [DOI] [PubMed] [Google Scholar]
- 82.Kleinman A, Benson P. Anthropology in the clinic: the problem of cultural competency and how to fix it. PLoS Med. 2006;3:e294. doi: 10.1371/journal.pmed.0030294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Willen SS, Knipper M, Abadía-Barrero CE, Davidovitch N. Syndemic vulnerability and the right to health. Lancet. 2017;389:964–77. doi: 10.1016/S0140-6736(17)30261-1. [DOI] [PubMed] [Google Scholar]
- 84.Willen SS. How is health-related “deservingness” reckoned? Perspectives from unauthorized im/migrants in Tel Aviv. Soc Sci Med. 2012;74:812–21. doi: 10.1016/j.socscimed.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 85.Bhopal R. Glossary of terms relating to ethnicity and race: for reflection and debate. J Epidemiol Community Health. 2004;58:441–5. doi: 10.1136/jech.2003.013466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fox JE, Mogilnicka M. Pathological integration, or, how East Europeans use racism to become British. Br J Sociol. 2017 doi: 10.1111/1468-4446.12337. published online Nov 30. [DOI] [PubMed] [Google Scholar]
- 87.Jornal Opção. Entrevista Bolsonaro Jornal Opção. 2015. [accessed Nov 1, 2018]. https://soundcloud.com/jornal-op-o-1/entrevista-bolsonaro .
- 88.Orbán Viktor. Prime Minister Viktor Orbán’s speech at the annual general meeting of the Association of Cities with County Rights Government. 2018. [accessed June 27, 2018]. http://www.kormany.hu/en/the-prime-minister/the-prime-minister-s-speeches/prime-minister-viktor-orban-s-speech-at-the-annual-general-meeting-of-the-association-of-cities-with-county-rights .
- 89.Almeida J, Biello KB, Pedraza F, Wintner S, Viruell-Fuentes E. The association between anti-immigrant policies and perceived discrimination among Latinos in the US: a multilevel analysis. SSM Popul Health. 2016;2:897–903. doi: 10.1016/j.ssmph.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Morey BN, Gee GC, Muennig P, Hatzenbuehler ML. Community-level prejudice and mortality among immigrant groups. Soc Sci Med. 2018;199:56–66. doi: 10.1016/j.socscimed.2017.04.020. [DOI] [PubMed] [Google Scholar]
- 91.Novak NL, Geronimus AT, Martinez-Cardoso AM. Change in birth outcomes among infants born to Latina mothers after a major immigration raid. Int J Epidemiol. 2017;46:839–49. doi: 10.1093/ije/dyw346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Momartin S, Stex Z, Coello M, Aroche J, Silove DM, Brooks R. A comparison of the mental health of refugees with temporary versus permanent protection visas. [Accessed June 14, 2018]; doi: 10.5694/j.1326-5377.2006.tb00610.x. [DOI] [PubMed] [Google Scholar]
- 93.Elias A, Paradies Y. Estimating the mental health costs of racial discrimination. BMC Public Health. 2016;16:1205. doi: 10.1186/s12889-016-3868-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Pauchulo AL. Anti-racism education in Canada: best practices—centre for race and culture. 2013. [accessed May 14, 2018]. https://cfrac.com/publications/anti-racism-education-in-canada-best-practices/
- 95.Muswede T. Approaches to ‘xenophobia’ interventions in Africa: common narratives through community radio in South Africa. The Journal for Transdisciplinary Research in Southern Africa. 2015;11:220–31. [Google Scholar]
- 96.O’Keefe P, Westgate K, Wisner B. Taking the naturalness out of natural disasters. Nature. 1976;260:566–67. [Google Scholar]
- 97.Watts N, Amann M, Ayeb-Karlsson S, et al. The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet. 2017 doi: 10.1016/S0140-6736(17)32464-9. published online Oct 30. [DOI] [PubMed] [Google Scholar]
- 98.Bahadur A, Simonet C. Disaster mortality, ODI Briefing. 2015. [accessed Oct 25, 2017]. https://www.odi.org/publications/9250-disaster-mortality .
- 99.Doel T, Thompson S, Dowrick T, Ahmad M, Clarkson M. Post-disaster recovery dilemmas: challenges in balancing short-term and long-term needs for vulnerability reduction. Environ Sci Policy. 2006;9:607–13. [Google Scholar]
- 100.Peters K. The next frontier for disaster risk reduction: tackling disasters in fragile and conflict-affected contexts. 2017. [accessed Oct 25, 2017]. http://repo.floodalliance.net/jspui/handle/44111/2502 .
- 101.Davis I, Alexander D. Recovery from disaster. Routledge; 2015. [accessed Oct 25, 2017]. https://www.routledge.com/Recovery-from-Disaster/Davis-Alexander/p/book/9780415611770 . [Google Scholar]
- 102.United Nations ESCAP. [accessed Jan 17, 2018];Asia Pacific Disaster Report 2010—Protecting Development Gains. 2010 http://www.unescap.org/publications/asia-pacific-disaster-report-2010-protecting-development-gains .
- 103.Beine M, Parsons C. [accessed Jan 17, 2018];Climatic factors as determinants of international migration. CESifo working paper: energy and climate economics. 2012 https://www.econstor.eu/bitstream/10419/55879/1/687925916.pdf .
- 104.Drabo A, Mbaye L. Climate change, natural disasters and migration: an empirical analysis in developing countries. Institute for the Study of Labor; 2011. [accessed Jan 17, 2018]. http://ftp.iza.org/dp5927.pdf . [Google Scholar]
- 105.Paul BK. Evidence against disaster-induced migration: the 2004 tornado in north-central Bangladesh. Disasters. 2005;29:370–85. doi: 10.1111/j.0361-3666.2005.00298.x. [DOI] [PubMed] [Google Scholar]
- 106.Bohra-Mishra P, Oppenheimer M, Hsiang SM. Nonlinear permanent migration response to climatic variations but minimal response to disasters. Proc Natl Acad Sci USA. 2014;111:9780–85. doi: 10.1073/pnas.1317166111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kelman I. Islandness within climate change narratives of small island developing states (SIDS) Island Studies J. 2018 published online May 15 http://discovery.ucl.ac.uk/1567002/ [Google Scholar]
- 108.Pomonis A, The Institution of Structural Engineers [accessed Aug 22, 2018];Recovery two years after the 2011 Tohoku earthquake and tsunami. A return mission report by EEFIT. https://www.istructe.org/getattachment/resources-centre/technical-topic-areas/eefit/eefit-reports/EEFIT-Japan-Recovery-Return-Mission-2013-Report-(1).pdf.aspx .
- 109.Barbieri AF, Domingues E, Queiroz BL, et al. Climate change and population migration in Brazil’s Northeast: scenarios for 2025–2050. Popul Environ. 2010;31:344–70. [Google Scholar]
- 110.Wandschneider T, Mishra P. The role of small rural towns in Bolangir District, India: a village-level perspective. University of Greenwich, Natural Resources Institute; 2003. [accessed Jan 17, 2018]. http://gala.gre.ac.uk/11672/1/Doc-0289.pdf . [Google Scholar]
- 111.Black R, Arnell NW, Adger WN, Thomas D, Geddes A. Migration, immobility and displacement outcomes following extreme events. Environ Sci Policy. 2013;27x [Google Scholar]
- 112.ReliefWeb. Situation Update ISCG. Rohingya Refugee Crisis, Cox’s Bazar. 2017. https://reliefweb.int/report/bangladesh/iscg-situation-update-rohingya-refugee-crisis-cox-s-bazar-21-december-2017 .
- 113.Ahmed B, Orcutt M, Sammonds P, et al. Humanitarian disaster for Rohingya refugees: impending natural hazards and worsening public health crises. Lancet Glob Health. 2018;6:e487–88. doi: 10.1016/S2214-109X(18)30125-6. [DOI] [PubMed] [Google Scholar]
- 114.Klugman J, Pereira IM. Assessment of national migration policies: human development research paper no. 48. United Nations Development Programme, Human Development Report Office; 2020. [accessed Jan 17, 2018]. http://hdr.undp.org/en/content/assessment-national-migration-policies . [Google Scholar]
- 115.Kalengayi FKN, Hurtig A-K, Nordstrand A, Ahlm C, Ahlberg BM. ‘It is a dilemma’: perspectives of nurse practitioners on health screening of newly arrived migrants. Glob Health Action. 2015;8:27903. doi: 10.3402/gha.v8.27903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.UNESCO. The right to education for persons with disabilities. 2015. [accessed June 14, 2018]. http://unesdoc.unesco.org/images/0023/002325/232592e.pdf .
- 117.Bartlett L. [accessed Jan 17, 2018];Access and quality of education for international migrant children. Education for all global monitoring report. 2020 http://unesdoc.unesco.org/images/0023/002324/232474e.pdf .
- 118.Gong P, Liang S, Carlton EJ, et al. Urbanisation and health in China. Lancet. 2012;379:843–52. doi: 10.1016/S0140-6736(11)61878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Fong HF. In: Routledge Handbook of Global Public Health in Asia. Griffiths SM, Tang JL, Yeoh EK, editors. 2014. Migration and health. Lessons from China; pp. 39–61. [Google Scholar]
- 120.United Nations. Convention on the Rights of the Child. 1990. [accessed Jan 16, 2018]. published online Sept 2 http://www.ohchr.org/Documents/ProfessionalInterest/crc.pdf.
- 121.United Nations. [accessed Jan 15, 2018];Article 18—Liberty of movement and nationality. Convention on the Rights of Persons with Disabilities. 18(1) https://www.un.org/development/desa/disabilities/convention-on-the-rights-of-persons-with-disabilities/article-18-liberty-of-movement-and-nationality.html . [Google Scholar]
- 122.UNICEF. Lebanon—refugees access to education. 2017. [accessed Jan 17, 2018]. https://weshare.unicef.org/Folder/2AMZIFIL5FQY .
- 123.Buller AM, Stoklosa H, Zimmerman C, Vaca V, Borland R. Labour exploitation, trafficking and migrant health: multi-country findings on the health risks and consequences of migrant and trafficked workers. International Organization for Migration; 2015. [accessed Sept 1, 2017]. https://publications.iom.int/books/labour-exploitation-trafficking-and-migrant-health-multi-country-findings-health-risks-and . [Google Scholar]
- 124.Chantavanich S, Laodumrongchai S, Harkins B, et al. Employment practices and working conditions in Thailand's fishing sector. ILO regional office for Asia and the Pacific; Bangkok, Thailand: 2013. [accessed Sept 1, 2017]. https://www.ilo.org/asia/publications/WCMS_220596/lang--en/index.htm . [Google Scholar]
- 125.Ang JW, Chia C, Koh CJ, et al. Healthcare-seeking behaviour, barriers and mental health of non-domestic migrant workers in Singapore. BMJ Glob Health. 2017;2:e000213. doi: 10.1136/bmjgh-2016-000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Malhotra R, Arambepola C, Tarun S, de Silva V, Kishore J, Østbye T. Health issues of female foreign domestic workers: a systematic review of the scientific and gray literature. Int J Occup Environ Health. 2013;19:261–777. doi: 10.1179/2049396713Y.0000000041. [DOI] [PubMed] [Google Scholar]
- 127.Hansen E, Donohoe M. Health issues of migrant and seasonal farmworkers. J Health Care Poor Underserved. 2003;14:153–64. doi: 10.1353/hpu.2010.0790. [DOI] [PubMed] [Google Scholar]
- 128.WHO. Healthy workplaces: a model for action for employers, workers, policy-makers and practitioners. 2010. [accessed Jan 17, 2018]. http://www.who.int/occupational_health/publications/healthy_workplaces_model_action.pdf .
- 129.Guinto RLLR, Curran UZ, Suphanchaimat R, Pocock NS. Universal health coverage in ‘One ASEAN’: are migrants included? Glob Health Action. 2015;8:25749. doi: 10.3402/gha.v8.25749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ramos AK, Carlo G, Grant KM, et al. A preliminary analysis of immigrant cattle feedyard worker perspectives on job-related safety training. Safety. 2018;4:37. [Google Scholar]
- 131.Levine PB, Zimmerman DJ. An empirical analysis of the welfare magnet debate using the NLSY. J Popul Econ. 1999;12:391–409. [Google Scholar]
- 132.International Organization for Migration, World Health Organization and Office of the High Commission for Human Rights. International migration, health and human rights. 2013. [accessed June 22, 2018]. http://www.ohchr.org/Documents/Issues/Migration/WHO_IOM_UNOHCHRPublication.pdf .
- 133.Benach J, Muntaner C, Delclos C, Menendez M, Ronquillo C. Migration and “low-skilled” workers in destination countries. PLoS Med. 2011;8:e1001043. doi: 10.1371/journal.pmed.1001043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Maplecroft V. Human rights outlook. 2016. [accessed June 22,2018]. https://maplecroft.com/portfolio/new-analysis/2016/02/15/human-rights-outlook-2016/
- 135.United Nations. Sustainable development goals—United Nations. United Nations Sustainable Development; [accessed June 22, 2018]. https://www.un.org/sustainabledevelopment/sustainable-development-goals/ [Google Scholar]
- 136.United Nations. United Nations Resolution adopted by the General Assembly on 17 December 2015. 2015. [accessed June 22, 2018]. http://www.un.org/en/development/desa/population/migration/generalassembly/docs/globalcompact/A_RES_70_147.pdf .
- 137.Alhasan H, Gulf Research Center Cambridge . Skillful Survivals: Irregular Migration to the Gulf. 2017. Irregular migration in Bahrain: legislation, policies, and practices; pp. 77–90. [Google Scholar]
- 138.El-Zein A, DeJong J, Fargues P, Salti N, Hanieh A, Lackner H. Who’s been left behind? Why sustainable development goals fail the Arab world. Lancet. 2016;388:207–10. doi: 10.1016/S0140-6736(15)01312-4. [DOI] [PubMed] [Google Scholar]
- 139.Pace P, editor. Migration and the right to health: a review of international law. International Migration Law; 2009. [accessed Jan 15, 2018]. http://publications.iom.int/system/files/pdf/iml_19.pdf . [Google Scholar]
- 140.Legido-Quigley H, Pajin L, Fanjul G, Urdaneta E, McKee M. Spain shows that a humane response to migrant health is possible in Europe. Lancet Public Health. 2018;3:e358. doi: 10.1016/S2468-2667(18)30133-6. [DOI] [PubMed] [Google Scholar]
- 141.UNAIDS. Lifting HIV-related restrictions on entry, stay and residence. [accessed Jan 15, 2018]. https://open.unaids.org/sites/default/files/documents/FINAL_TR_A3_press.pdf .
- 142.Human Rights Watch. Swept under the rug. Abuses against domestic workers around the world: V. Migrant domestic workers. [accessed Jan 15, 2018]. https://www.hrw.org/reports/2006/wrd0706/5.htm#_Toc139370 .
- 143.Sönmez S, Apostopoulos Y, Tran D, Rentrope S. Human rights and health disparities for migrant workers in the UAE. [accessed Jan 15, 2018];Health Hum Rights. 2011 13 https://www.hhrjournal.org/2013/08/human-rights-and-health-disparities-for-migrant-workers-in-the-uae . [PubMed] [Google Scholar]
- 144.Human Rights Watch. Deporting HIV-positive migrants threatens lives; global goals: need to ensure continuity of treatment and care across borders. 2009. [accessed Jan 15, 2018]. https://www.hrw.org/news/2009/09/23/deporting-hiv-positive-migrants-threatens-lives-global-goals .
- 145.United Nations. International Covenant on Civil and Political Rights. Vol. 999. United Nations; 1966. p. 171. (Treaty Series). [Google Scholar]
- 146.International Organization for Migration. International Migration. [accessed Jan 15, 2018];Health and Human Rights Report. 2013 https://www.iom.int/news/international-migration-health-and-human-rights-report .
- 147.Assembly UNG. Convention on the elimination of all forms of discrimination against women: CEDAW/C/TUN/3-4. 2000. [accessed Jan 15, 2018]. published online Aug 2. http://www.un.org/womenwatch/daw/cedaw/cedaw27/tun3-4.pdf.
- 148.United Nations. Siracusa principles on the limitation and derogation of provisions in the international covenant on civil and political rights. 1984. [accessed Jan 16, 2018]. http://icj.wpengine.netdna-cdn.com/wp-content/uploads/1984/07/Siracusa-principles-ICCPR-legal-submission-1985-eng.pdf .
- 149.Office of the High Commission for Human Rights. Recommended principles and guidelines on human rights at international borders. 2014. [accessed Jan 16, 2018]. http://www.globalmigrationgroup.org/system/files/OHCHR_Principles_and_Guidelines_on_Human_Rights_at_International_Borders_CRPA69.pdf .
- 150.Australian Government. Migration Regulations 1994, No. 268. https://www.legislation.gov.au/Details/F2016C01073/6d7be855-ba1a-4160-b359-a8d70b1ba871 .
- 151.Australian Government. [accessed Jan 16, 2018];Migration Act 1958, No. 62. 2013. https://www.legislation.gov.au/Details/C2013C00458 .
- 152.Australian Government. Significant costs and services in short supply. Australian Government Department of Immigration and Border Protection; [accessed Aug 23, 2017]. https://www.border.gov.au/Trav/Visa/Heal/overview-of-the-health-requirement/significant-costs-and-services-in-short-supply . [Google Scholar]
- 153.Kett M, Trani JF. Refugees Worldwide: Refugee health. Barbara, CA: Praeger Publishers; 2012. Refugees with disabilities: more vulnerable, more at risk; pp. 213–30. [Google Scholar]
- 154.Zetter R, Ruaudel H. Refugees’ right to work and access to labor markets–an assessment. Knomad Study; 2016. [accessed Jan 16, 2018]. http://www.knomad.org/sites/default/files/2017-03/KNOMAD%20Study%201%20Part%20I-%20Assessing%20Refugees%27%20Rights%20to%20Work_final.pdf . [Google Scholar]
- 155.Sinha A. Slavery by another name: ‘voluntary’ immigrant detainee labor and the thirteenth amendment. Stanford J Civ Rights Civ Lib. 2015;5 [Google Scholar]
- 156.Zayas LH, Aguilar-Gaxiola S, Yoon H, Rey GN. The distress of citizen-children with detained and deported parents. J Child Fam Stud. 2015;24:3213–23. doi: 10.1007/s10826-015-0124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.UNICEF. Judicial implementation of article 3 of the convention on the rights of the child in Europe: the case of migrant children including unaccompanied children. 2012. [accessed Jan 16, 2018]. http://www.refworld.org/docid/5135ae842.html .
- 158.The United States Department of Justice. Attorney general announces zero-tolerance policy for criminal illegal entry. 2018. [accessed June 14, 2018]. https://www.justice.gov/opa/pr/attorney-general-announces-zero-tolerance-policy-criminal-illegal-entry .
- 159.UN High Commissioner for Refugees. Detention of refugees and asylum-seekers. No. 44 (XXXVII) 1986. [accessed Jan 16, 2018]. http://www.unhcr.org/4aa764389.pdf .
- 160.United Nations. [accessed Jan 16, 2018];Special rapporteur on the rights of migrants Annual report of the United Nations High Commissioner for Human Rights and reports of the Office of the High Commissioner and the Secretary-General A/71/285 2016. 2016 https://reliefweb.int/report/world/human-rights-migrants-report-special-rapporteur-human-rights-migrants-a71285-enar-0 .
- 161.Committee on the Rights of the Child. The rights of all children in the context of international migration. 2012. [accessed Jan 16, 2018]. http://www2.ohchr.org/english/bodies/crc/docs/discussion2012/2012CRC_DGD-Childrens_Rights_InternationalMigration.pdf .
- 162.Assembly UNG. [accessed Jan 16, 2018];In safety and dignity: addressing large movements of refugees and migrants Report of the Secretary-General A/70/59. 2016 http://www.un.org/ga/search/view_doc.asp?symbol=A/70/59 .
- 163.Wales J, Rashid M. No longer a place of refuge: health consequences of mandatory detention for refugees. Can Fam Physician. 2013;59:609–11. [PMC free article] [PubMed] [Google Scholar]
- 164.United Nations High Commissioner for Refugees. UNHCR detention guidelines: guidelines on the applicable criteria and standards relating to the detention of asylum-seekers and alternatives to detention. [accessed Jan 16, 2018]. http://www.unhcr.org/publications/legal/505b10ee9/unhcr-detention-guidelines.html .
- 165.Kalt A, Hossain M, Kiss L, Zimmerman C. Asylum seekers, violence and health: a systematic review of research in high-income host countries. Am J Public Health. 2013;103:e30–42. doi: 10.2105/AJPH.2012.301136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Report of the Working Group on Arbitrary Detention A/HRC/13/50. UN Human Rights Council; 2010. [accessed Jan 16, 2018]. https://documents-dds-ny.un.org/doc/UNDOC/GEN/G10/108/72/PDF/G1010872.pdf?OpenElement . [Google Scholar]
- 167.Ghazal M. Child marriage on the rise among Syrian refugees. [accessed Jan 17, 2018];The Jordan Times. 2016 published online June 11. http://www.jordantimes.com/news/local/child-marriage-rise-among-syrian-refugees. [Google Scholar]
- 168.Amman Center for Human Rights. [accessed Jan 17, 2018];Jordan: NGO Report—On the implementation of the ICCPR. 2010 http://tbinternet.ohchr.org/Treaties/CCPR/Shared%20Documents/JOR/INT_CCPR_NGO_JOR_98_9263_E.pdf .
- 169.Leaning J, Bartels S, Mowafi H. Women, Migration, and Conflict. 2009. Sexual violence during war and forced migration; pp. 173–99. [Google Scholar]
- 170.Husseini R. Debate continues as Article 308 on way to Lower House’s vote. [accessed Jan 17, 2018];The Jordan Times. 2017 published online May 31. http://www.jordantimes.com/news/local/debate-continues-article-308-way-lower-houses-vote. [Google Scholar]
- 171.Gündüz RC, Halil H, Gürsoy C, et al. Refusal of medical treatment in the pediatric emergency service: analysis of reasons and aspects. Turk J Pediatr. 2014;56:638–42. [PubMed] [Google Scholar]
- 172.Gharaibeh MK, Oweis A, Shakhatreh FMN, Froelicher ES. Factors associated with contraceptive use among Jordanian muslim women: implications for health and social policy. J Int Womens Stud. 2011;12:168–84. [Google Scholar]
- 173.Devries KM, Mak JYT, García-Moreno C, et al. Global health. The global prevalence of intimate partner violence against women. Science. 2013;340:1527–28. doi: 10.1126/science.1240937. [DOI] [PubMed] [Google Scholar]
- 174.Wachter K, Horn R, Friis E, et al. Drivers of intimate partner violence against women in three refugee camps. Violence Against Women. 2018;24:286–306. doi: 10.1177/1077801216689163. [DOI] [PubMed] [Google Scholar]
- 175.Jacobs C, Flaam H, Fowlis M, Pangburn A. Justice needs, strategies, and mechanisms for the displaced: reviewing the evidence. Social Science Research Council; 2017. [accessed Sept 3, 2017]. https://www.ssrc.org/publications/view/justice-needs-strategies-and-mechanisms-for-the-displaced-reviewing-the-evidence/ [Google Scholar]
- 176.UNDP Arab States. Iraq: Syrian women and girls struggle to survive in camps. [accessed Jan 17, 2018]. http://www.arabstates.undp.org/content/rbas/en/home/ourwork/crisis-response/successstories/alone-in-iraq–syrian-women-and-girls-struggle-to-survive-in-ref.html .
- 177.Rights in Exile Programme. Refugee legal aid information for lawyers representing refugees globally. [accessed Jan 17, 2018]. http://www.refugeelegalaidinformation.org/
- 178.Forced Migration Review. Sexual orientation and gender identity and the protection of forced migrants. 2013. [accessed Jan 17, 2018]. http://www.fmreview.org/sites/fmr/files/FMRdownloads/en/fmr42full.pdf .
- 179.United Nations High Commissioner for Refugees. General comment no. 32, Article 14, Right to equality before courts and tribunals and to fair trial, CCPR/C/GC/32. Refworld; 2007. [accessed Jan 16, 2018]. http://www.refworld.org/docid/478b2b2f2.html . [Google Scholar]
- 180.Grove NJ, Zwi AB. Our health and theirs: forced migration, othering, and public health. Soc Sci Med. 2006;62:1931–42. doi: 10.1016/j.socscimed.2005.08.061. [DOI] [PubMed] [Google Scholar]
- 181.Jacobs C, Flaam H, Fowlis M, Pangburn A. Justice needs, strategies, and mechanisms for the displaced: reviewing the evidence. 2017. [accessed Sept 3, 2017]. http://webarchive.ssrc.org/working-papers/CPPF_Justice%20Needs_WorkingPaper.pdf .
- 182.WHO. What is universal coverage? 2018. [accessed June 14, 2018]. http://www.who.int/health_financing/universal_coverage_definition/en/
- 183.Stenberg K, Hanssen O, Edejer TT, et al. Financing transformative health systems towards achievement of the health Sustainable Development Goals: a model for projected resource needs in 67 low-income and middle-income countries. Lancet Glob Health. 2017;5:e875–87. doi: 10.1016/S2214-109X(17)30263-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.WHO. [accessed Jan 17, 2018];The world health report 2000—Health systems: improving performance. 2013 https://www.who.int/whr/2000/
- 185.Dewachi O, Skelton M, Nguyen VK, et al. Changing therapeutic geographies of the Iraqi and Syrian wars. Lancet. 2014;383:449–57. doi: 10.1016/S0140-6736(13)62299-0. [DOI] [PubMed] [Google Scholar]
- 186.Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. doi: 10.1186/1475-9276-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Dixit AK. Governance institutions and economic activity. Am Econ Rev. 2009;99:5–24. [Google Scholar]
- 188.Arnold C, Theede J, Gagnon A. A qualitative exploration of access to urban migrant healthcare in Nairobi, Kenya. Soc Sci Med. 2014;110:1–9. doi: 10.1016/j.socscimed.2014.03.019. [DOI] [PubMed] [Google Scholar]
- 189.Cuadra CB. Right of access to health care for undocumented migrants in EU: a comparative study of national policies. Eur J Public Health. 2012;22:267–71. doi: 10.1093/eurpub/ckr049. [DOI] [PubMed] [Google Scholar]
- 190.Miedema B, Hamilton R, Easley J. Climbing the walls: structural barriers to accessing primary care for refugee newcomers in Canada. Can Fam Physician. 2008;54:335–39. [PMC free article] [PubMed] [Google Scholar]
- 191.Doocy S, Lyles E, Akhu-Zaheya L, Burton A, Burnham G. Health service access and utilization among Syrian refugees in Jordan. Int J Equity Health. 2016;15:108. doi: 10.1186/s12939-016-0399-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Aldridge RW, Miller AK, Jakubowski B, Pereira L, Fille F, Noret I. [accessed Jan 17, 2018];Falling through the cracks: the failure of universal healthcare coverage in Europe, European Network to Reduce Vulnerabilities in Health Observatory Report. 2017 https://mdmeuroblog.files.wordpress.com/2014/01/observatory-report-2017-web-version.pdf .
- 193.Tsai TI, Lee SYD. Health literacy as the missing link in the provision of immigrant health care: a qualitative study of Southeast Asian immigrant women in Taiwan. Int J Nurs Stud. 2016;54:65–74. doi: 10.1016/j.ijnurstu.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 194.Arcury TA, Quandt SA. Delivery of health services to migrant and seasonal farmworkers. Annu Rev Public Health. 2007;28:34–63. doi: 10.1146/annurev.publhealth.27.021405.102106. [DOI] [PubMed] [Google Scholar]
- 195.Luque JS, Reyes-Ortiz C, Marella P, et al. Mobile farm clinic outreach to address health conditions among Latino migrant farmworkers in Georgia. J Agromed. 2012;17:386–97. doi: 10.1080/1059924X.2012.713837. [DOI] [PubMed] [Google Scholar]
- 196.Stein LM. Health care delivery to farmworkers in the Southwest: an innovative nursing clinic. J Am Acad Nurse Pract. 1993;5:119–24. doi: 10.1111/j.1745-7599.1993.tb00852.x. [DOI] [PubMed] [Google Scholar]
- 197.Thomas TA, Quandt SA. Delivery of health services to migrant and seasonal farmworkers. 2007. [accessed July 1, 2018]. https://www.annualreviews.org/doi/full/10.1146/annurev.publhealth.27.021405.102106?amp%3Bsearc= [DOI] [PubMed]
- 198.Conserve DF, Jennings L, Aguiar C, Shin G, Handler L, Maman S. Systematic review of mobile health behavioural interventions to improve uptake of HIV testing for vulnerable and key populations. J Telemed Telecare. 2017;23:347–59. doi: 10.1177/1357633X16639186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Heuer LJ, Hess C, Batson A. Cluster clinics for migrant Hispanic farmworkers with diabetes: perceptions, successes, and challenges. Rural Remote Health. 2006;6:469. [PubMed] [Google Scholar]
- 200.International Organization for Migration. ‘Caravan of Life’ documentary launched in Peru. 2015. [accessed July 1, 2018]. https://www.iom.int/news/caravan-life-documentary-launched-peru .
- 201.Asi YM, Williams C. The role of digital health in making progress toward Sustainable Development Goal (SDG) 3 in conflict-affected populations. Int J Med Inform. 2018;114:114–20. doi: 10.1016/j.ijmedinf.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 202.WHO Regional Office for Europe. Strategy and action plan for refugee and migrant health in the WHO European Region. [accessed Jan 17, 2018]. http://www.euro.who.int/__data/assets/pdf_file/0004/314725/66wd08e_MigrantHealthStrategyActionPlan_160424.pdf?ua=1 .
- 203.Coors M, Grützmann T, Peters T, et al. Der Umgang mit Fremdheit in Medizin und Pflege. Interkulturalität und Ethik. 2017. [accessed Jan 17, 2018]. published online May 22, http://www.edition-ruprecht.de/katalog/titel.php?id=399.
- 204.Saladin P, Bühlmann R. Switzerland Bundesamt für Gesundheit, H+ Swiss Hospital Association. Diversity and equality of opportunity: fundamentals for effective action in the microcosm of the health care institution. [accessed Jan 17, 2018]. http://www.ncbi.nlm.nih.gov/nlmcatalog/101485196 .
- 205.MIPEX 2015: Switzerland. Migration Integration Policy Index. [accessed Jan 17, 2018]. http://www.mipex.eu/switzerland .
- 206.WHO. WHA58. 33 Sustainable health financing, universal coverage and social health insurance. 2005. [accessed Jan 17, 2018]. http://apps.who.int/medicinedocs/documents/s21475en/s21475en.pdf .
- 207.Admasu K, Balcha T, Ghebreyesus TA. Pro-poor pathway towards universal health coverage: lessons from Ethiopia. J Glob Health. 2016;6:010305. doi: 10.7189/jogh.06.010305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Meng Q, Yuan B, Jia L, et al. Expanding health insurance coverage in vulnerable groups: a systematic review of options. Health Policy Plan. 2011;26:93–104. doi: 10.1093/heapol/czq038. [DOI] [PubMed] [Google Scholar]
- 209.McMichael C, Healy J. Health equity and migrants in the Greater Mekong Subregion. Glob Health Action. 2017;10:1271594. doi: 10.1080/16549716.2017.1271594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Rechel B, Mladovsky P, Ingleby D, Mackenbach JP, McKee M. Migration and health in an increasingly diverse Europe. Lancet. 2013;381:1235–45. doi: 10.1016/S0140-6736(12)62086-8. [DOI] [PubMed] [Google Scholar]
- 211.Department of Health and Social Care and Home Office. [accessed Jan 18, 2018];Information requests from the Home Office to NHS Digital: Memorandum of understanding (MOU) on processing information requests from the Home Office to NHS Digital for tracing immigration offenders. https://www.gov.uk/government/publications/information-requests-from-the-home-office-to-nhs-digital .
- 212.Health Committee. UK Parliament. Correspondence regarding Memorandum of Understanding (MoU) between NHS Digital, the Home Office and the Department of Health on data sharing. 2013. [accessed Jan 15, 2018]. https://www.parliament.uk/documents/commons-committees/Health/Correspondence/2016-17/Correspondence-Memorandum-Understanding-NHS-Digital-Home-Office-Department-Health-datasharing.pdf .
- 213.Saadi A, McKee M. Hospitals as places of sanctuary. BMJ. 2018;361:k2178. doi: 10.1136/bmj.k2178. [DOI] [PubMed] [Google Scholar]
- 214.Haskew C, Spiegel P, Tomczyk B, Cornier N, Hering H. A standardized health information system for refugee settings: rationale, challenges and the way forward. Bull World Health Organ. 2010;88:792–94. doi: 10.2471/BLT.09.074096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.WHO. A human rights-based approach to health. 2018. [accessed Jan 17, 2018]. https://www.who.int/hhr/news/hrba_to_health2.pdf .
- 216.Tervalon M, Murray-García J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved. 1998;9:117–25. doi: 10.1353/hpu.2010.0233. [DOI] [PubMed] [Google Scholar]
- 217.Metzl JM, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med. 2014;103:126–33. doi: 10.1016/j.socscimed.2013.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Holmes SM. The clinical gaze in the practice of migrant health: Mexican migrants in the United States. Soc Sci Med. 2012;74:873–81. doi: 10.1016/j.socscimed.2011.06.067. [DOI] [PubMed] [Google Scholar]
- 219.Simbiri KOA, Hausman A, Wadenya RO, Lidicker J. Access impediments to health care and social services between Anglophone and Francophone African immigrants living in Philadelphia with respect to HIV/AIDS. J Immigr Minor Health. 2010;12:569–79. doi: 10.1007/s10903-009-9229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Jensen NK, Nielsen SS, Krasnik A. Expert opinion on “best practices” in the delivery of health care services to immigrants in Denmark. Dan Med Bull. 2010;57:A4170. [PubMed] [Google Scholar]
- 221.Kirch W. Encyclopedia of Public Health. Vol. 2. Springer Science & Business Media; Dordrecht: 2008. [Google Scholar]
- 222.Spallek J, Zeeb H, Razum O. What do we have to know from migrants– past exposures to understand their health status? A life course approach. Emerg Themes Epidemiol. 2011;8:6. doi: 10.1186/1742-7622-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Marmot MG, Adelstein AM, Bulusu L. Lessons from the study of immigrant mortality. Lancet. 1984;1:1455–57. doi: 10.1016/s0140-6736(84)91943-3. [DOI] [PubMed] [Google Scholar]
- 224.Moullan Y, Jusot F. Why is the ‘healthy immigrant effect– different between European countries? Eur J Public Health. 2014;24(suppl 1):80–86. doi: 10.1093/eurpub/cku112. [DOI] [PubMed] [Google Scholar]
- 225.iSHARE Repository. INDEPTH Data Repository. 2013. [accessed Jan 15, 2018]. http://www.indepth-ishare.org/
- 226.Ginsburg C, Bocquier P, Béguy D, et al. Healthy or unhealthy migrants? Identifying internal migration effects on mortality in Africa using health and demographic surveillance systems of the INDEPTH network. Soc Sci Med. 2016;164:59–73. doi: 10.1016/j.socscimed.2016.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Ginsburg C, Bocquier P, Beguy D, et al. A multi-centre analysis of internal migration and cause specific mortality in Kenya and South Africa using health and demographic surveillance data of the INDEPTH network. 2017. [accessed Jan 15, 2018]. https://iussp.confex.com/iussp/ipc2017/meetingapp.cgi/Paper/2230 .
- 228.Ginsburg C, Bocquier P, Béguy D, et al. Association between internal migration and epidemic dynamics: an analysis of cause-specific mortality in Kenya and South Africa using health and demographic surveillance data. BMC Public Health. 2018;18:918. doi: 10.1186/s12889-018-5851-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Heslehurst N, Brown H, Pemu A, Coleman H, Rankin J. Perinatal health outcomes and care among asylum seekers and refugees: a systematic review of systematic reviews. BMC Med. 2018;16:89. doi: 10.1186/s12916-018-1064-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Bollini P, Pampallona S, Wanner P, Kupelnick B, et al. ROAM Collaboration Pregnancy outcome of migrant women and integration policy: a systematic review of the international literature. Soc Sci Med. 2009;68:452–61. doi: 10.1016/j.socscimed.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 231.Gagnon AJ, Zimbeck M, Zeitlin J, et al. ROAM Collaboration Migration to western industrialised countries and perinatal health: a systematic review. Soc Sci Med. 2009;69:934–46. doi: 10.1016/j.socscimed.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 232.Fellmeth G, Fazel M, Plugge E. Migration and perinatal mental health in women from low- and middle-income countries: a systematic review and meta-analysis. BJOG. 2017;124:742–52. doi: 10.1111/1471-0528.14184. [DOI] [PubMed] [Google Scholar]
- 233.Falah-Hassani K, Shiri R, Vigod S, Dennis C-L. Prevalence of postpartum depression among immigrant women: A systematic review and meta-analysis. J Psychiatr Res. 2015;70:67–82. doi: 10.1016/j.jpsychires.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 234.Mipatrini D, Stefanelli P, Severoni S, Rezza G. Vaccinations in migrants and refugees: a challenge for European health systems. A systematic review of current scientific evidence. Pathog Glob Health. 2017;111:59–68. doi: 10.1080/20477724.2017.1281374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Patton GC, Sawyer SM, Santelli JS, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387:2423–78. doi: 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Glick JE, Hanish LD, Yabiku ST, Bradley RH. Migration timing and parenting practices: contributions to social development in preschoolers with foreign-born and native-born mothers. Child Dev. 2012;83:1527–42. doi: 10.1111/j.1467-8624.2012.01789.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Stevens GWJM, Vollebergh WAM. Mental health in migrant children. J Child Psychol Psychiatry. 2008;49:276–94. doi: 10.1111/j.1469-7610.2007.01848.x. [DOI] [PubMed] [Google Scholar]
- 238.Sun X, Chen M, Chan KL. A meta-analysis of the impacts of internal migration on child health outcomes in China. BMC Public Health. 2016;16:66. doi: 10.1186/s12889-016-2738-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Mindlis I, Boffetta P. Mood disorders in first- and second-generation immigrants: systematic review and meta-analysis. Br J Psychiatry. 2017;210:182–89. doi: 10.1192/bjp.bp.116.181107. [DOI] [PubMed] [Google Scholar]
- 240.Crafa D, Warfa N, editors. Maternal migration and autism risk: systematic analysis. [accessed Jan 17, 2018];Int Rev Psychiatry. 2015 27:64–71. doi: 10.3109/09540261.2014.995601. [DOI] [PubMed] [Google Scholar]
- 241.Sanou D, O’Reilly E, Ngnie-Teta I, et al. Acculturation and nutritional health of immigrants in Canada: a scoping review. J Immigr Minor Health. 2014;16:24–34. doi: 10.1007/s10903-013-9823-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Dawson-Hahn E, Pak-Gorstein S, Matheson J, et al. Growth trajectories of refugee and nonrefugee children in the United Staes. Pediatrics. 2016;138:e20160953. doi: 10.1542/peds.2016-0953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Besharat Pour M, Bergström A, Bottai M, et al. Body mass index development from birth to early adolescence; effect of perinatal characteristics and maternal migration background in a Swedish cohort. PLoS One. 2014;9:e109519. doi: 10.1371/journal.pone.0109519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Victora CG, Bahl R, Barros AJD, Lancet Breastfeeding Series Group et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387:475–90. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 245.Alliance for Child Protection in Humanitarian Action. Field handbook on unaccompanied and separated children. [accessed June 26, 2018]. Inter-agency Working Group on Unaccompanied and Separated Children. https://www.iom.int/sites/default/files/HANDBOOK-WEB-2017-0322.pdf . [Google Scholar]
- 246.Commissioner for Human Rights. Methods for assessing the age of migrant children must be improved. [accessed June 14, 2018]. https://www.coe.int/en/web/commissioner/blog/-/asset_publisher/xZ32OPEoxOkq/content/methods-for-assessing-the-age-of-migrant-children-must-be-improv-1 .
- 247.Aynsley-Green A, Cole TJ, Crawley H, Lessof N, Boag LR, Wallace RMM. Medical, statistical, ethical and human rights considerations in the assessment of age in children and young people subject to immigration control. Br Med Bull. 2012;102:17–42. doi: 10.1093/bmb/lds014. [DOI] [PubMed] [Google Scholar]
- 248.Curry SR, Abrams LS. Housing and social support for youth aging out of foster care: state of the research literature and directions for future inquiry. Child Adolesc Social Work J. 2015;32:143–53. [Google Scholar]
- 249.Plan International. Weathering the storm: adolescent girls and climate change. 2011. [accessed Jan 15, 2018]. https://plan-international.org/publications/weathering-storm .
- 250.Fazel M, Reed RV, Panter-Brick C, Stein A. Mental health of displaced and refugee children resettled in high-income countries: risk and protective factors. Lancet. 2012;379:266–82. doi: 10.1016/S0140-6736(11)60051-2. [DOI] [PubMed] [Google Scholar]
- 251.Close C, Kouvonen A, Bosqui T, Patel K, O’Reilly D, Donnelly M. The mental health and wellbeing of first generation migrants: a systematic-narrative review of reviews. Global Health. 2016;12:47. doi: 10.1186/s12992-016-0187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Bourque F, van der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first- and second-generation immigrants. Psychol Med. 2011;41:897–910. doi: 10.1017/S0033291710001406. [DOI] [PubMed] [Google Scholar]
- 253.Cantor-Graae E, Selten J-P. Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry. 2005;162:12–24. doi: 10.1176/appi.ajp.162.1.12. [DOI] [PubMed] [Google Scholar]
- 254.Paradies Y, Ben J, Denson N, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10:e0138511. doi: 10.1371/journal.pone.0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135:531–54. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Li J, Rose N. Urban social exclusion and mental health of China2015’16s rural-urban migrants2015–16a review and call for research. Health Place. 2017;48:20–30. doi: 10.1016/j.healthplace.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 257.Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA. 2009;302:537–49. doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- 258.Lindert J, Ehrenstein OS, Priebe S, Mielck A, Brähler E. Depression and anxiety in labor migrants and refugees--a systematic review and meta-analysis. Soc Sci Med. 2009;69:246–57. doi: 10.1016/j.socscimed.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 259.Palic S, Elklit A. Psychosocial treatment of posttraumatic stress disorder in adult refugees: a systematic review of prospective treatment outcome studies and a critique. J Affect Disord. 2011;131:8–23. doi: 10.1016/j.jad.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 260.Nickerson A, Bryant RA, Silove D, Steel Z.> A critical review of psychological treatments of posttraumatic stress disorder in refugees. Clin Psychol Rev. 2011;31:399–417. doi: 10.1016/j.cpr.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 261.Williams ME, Thompson SC. The use of community-based interventions in reducing morbidity from the psychological impact of conflict-related trauma among refugee populations: a systematic review of the literature. J Immigr Minor Health. 2011;13:780–94. doi: 10.1007/s10903-010-9417-6. [DOI] [PubMed] [Google Scholar]
- 262.Omoleke SA, Mohammed I, Saidu Y. Ebola Viral Disease in West Africa: A Threat to Global Health, Economy and Political Stability. J Public Health Africa. 2016;7:534. doi: 10.4081/jphia.2016.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Holmes AH, Moore LSP, Sundsfjord A, et al. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet. 2016;387:176–87. doi: 10.1016/S0140-6736(15)00473-0. [DOI] [PubMed] [Google Scholar]
- 264.WHO, World Bank. [accessed Nov 1, 2018];World Report on Disability. 2011 https://www.who.int/disabilities/world_report/2011/report/en/
- 265.WHO: Regional Office for Europe. Migration and health: key issues. [accessed Jan 16, 2018]. http://www.euro.who.int/en/health-topics/health-determinants/migration-and-health/migrant-health-in-the-european-region/migration-and-health-key-issues .
- 266.Andersen GS, Kamper-Jørgensen Z, Carstensen B, Norredam M, Bygbjerg IC, Jørgensen ME. Diabetes among migrants in Denmark: Incidence, mortality, and prevalence based on a longitudinal register study of the entire Danish population. Diabetes Res Clin Pract. 2016;122:9–16. doi: 10.1016/j.diabres.2016.09.020. [DOI] [PubMed] [Google Scholar]
- 267.Arnold M, Razum O, Coebergh JW. Cancer risk diversity in non-western migrants to Europe: an overview of the literature. Eur J Cancer. 2010;46:2647–59. doi: 10.1016/j.ejca.2010.07.050. [DOI] [PubMed] [Google Scholar]
- 268.Brathwaite R, Addo J, Kunst AE, et al. Smoking prevalence differs by location of residence among Ghanaians in Africa and Europe: The RODAM study. PLoS One. 2017;12:e0177291. doi: 10.1371/journal.pone.0177291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Bosdriesz JR, Lichthart N, Witvliet MI, Busschers WB, Stronks K, Kunst AE. Smoking prevalence among migrants in the US compared to the US-born and the population in countries of origin. PLoS One. 2013;8:e58654. doi: 10.1371/journal.pone.0058654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Ji Y, Liu S, Zhao X, Jiang Y, Zeng Q, Chang C. Smoking and its determinants in Chinese internal migrants: nationally representative cross-sectional data analyses. Nicotine Tob Res. 2016;18:1719–26. doi: 10.1093/ntr/ntw101. [DOI] [PubMed] [Google Scholar]
- 271.Weber MF, Banks E, Sitas F. Smoking in migrants in New South Wales, Australia: report on data from over 100 000 participants in the 45 and up study. Drug Alcohol Rev. 2011;30:597–605. doi: 10.1111/j.1465-3362.2010.00247.x. [DOI] [PubMed] [Google Scholar]
- 272.El-Bassel N, Marotta PL. Alcohol and sexual risk behaviors among male central asian labor migrants and non-migrants in Kazakhstan: implications for HIV prevention. AIDS Behav. 2017;21(suppl 2):183–92. doi: 10.1007/s10461-017-1918-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Taype-Rondan A, Bernabe-Ortiz A, Alvarado GF, Gilman RH, Smeeth L, Miranda JJ. Smoking and heavy drinking patterns in rural, urban and rural-to-urban migrants: the PERU MIGRANT Study. BMC Public Health. 2017;17:165. doi: 10.1186/s12889-017-4080-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Schenker MB. A global perspective of migration and occupational health. Am J Ind Med. 2010;53:329–377. doi: 10.1002/ajim.20834. [DOI] [PubMed] [Google Scholar]
- 275.Stergiou-Kita M, Mansfield E, Bezo R, et al. Danger zone: Men, masculinity and occupational health and safety in high risk occupations. Saf Sci. 2015;80:213–20. doi: 10.1016/j.ssci.2015.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Kiss L, Pocock NS, Naisanguansri V, et al. Health of men, women, and children in post-trafficking services in Cambodia, Thailand, and Vietnam: an observational cross-sectional study. Lancet Glob Health. 2015;3:e154–61. doi: 10.1016/S2214-109X(15)70016-1. [DOI] [PubMed] [Google Scholar]
- 277.Mason-Jones AJ, Nicholson P. Structural violence and marginalisation. The sexual and reproductive health experiences of separated young people on the move. A rapid review with relevance to the European humanitarian crisis. Public Health. 2018;158:156–62. doi: 10.1016/j.puhe.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 278.UNICEF. Female genital mutilation and cutting. Monitoring the situation of children and women. [accessed Jan 15, 2018]. https://data.unicef.org/topic/child-protection/female-genital-mutilation-and-cutting/
- 279.Thierfelder C, Tanner M, Bodiang CMK. Female genital mutilation in the context of migration: experience of African women with the Swiss health care system. Eur J Public Health. 2005;15:86–90. doi: 10.1093/eurpub/cki120. [DOI] [PubMed] [Google Scholar]
- 280.Wong FY, Huang ZJ, He N, et al. HIV risks among gay- and non-gay-identified migrant money boys in Shanghai, China. AIDS Care. 2008;20:170–80. doi: 10.1080/09540120701534707. [DOI] [PubMed] [Google Scholar]
- 281.Austin J, Guy S, Lee-Jones L, McGinn T, Schlecht J. Reproductive health: a right for refugees and internally displaced persons. Reprod Health Matters. 2008;16:10–21. doi: 10.1016/S0968-8080(08)31351-2. [DOI] [PubMed] [Google Scholar]
- 282.Barbara G, Collini F, Cattaneo C, et al. Sexual violence and unwanted pregnancies in migrant women. Lancet Glob Health. 2017;5:e396–97. doi: 10.1016/S2214-109X(17)30075-X. [DOI] [PubMed] [Google Scholar]
- 283.WHO and the Inter-Agency Working Group for Reproductive Health. The Minimum Initial Service Package for reproductive health in crisis situations. [accessed Jan 15, 2018]. http://www.who.int/disasters/repo/7345.doc .
- 284.Bank A, Fröhlich C, Schneiker A. The political dynamics of human mobility: migration out of, as and into violence. Glob Policy. 2017;8:12–18. [Google Scholar]
- 285.Ottisova L, Hemmings S, Howard LM, Zimmerman C, Oram S. Prevalence and risk of violence and the mental, physical and sexual health problems associated with human trafficking: an updated systematic review. Epidemiol Psychiatr Sci. 2016;25:317–41. doi: 10.1017/S2045796016000135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Vu A, Adam A, Wirtz A, et al. The prevalence of sexual violence among female refugees in complex humanitarian emergencies: a systematic review and meta-analysis. PLoS Curr. 2014;6 doi: 10.1371/currents.dis.835f10778fd80ae031aac12d3b533ca7. ecurrents.dis.835f10778fd80ae031aac12d3b533ca7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Tappis H, Freeman J, Glass N, Doocy S. Effectiveness of interventions, programs and strategies for gender-based violence prevention in refugee populations: an integrative review. PLoS Curr. 2016;8 doi: 10.1371/currents.dis.3a465b66f9327676d61eb8120eaa5499. ecurrents.dis.3a465b66f9327676d61eb8120eaa5499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Forced Migration Review. Mental health challenges of LGBT forced migrants. [accessed Aug 22, 2018]. http://www.fmreview.org/sogi/shidlo-ahola.html?contrast=regular-contrast .
- 289.Breen D, Millo Y. Protection in the city: some good practice in Nairobi. Forced Migr Rev. 2013;42:54–56. [Google Scholar]
- 290.Groce N, Kett M, Lang R, Trani JF. Disability and poverty: the need for a more nuanced understanding of implications for development policy and practice. Third World Q. 2011;32:1493–513. [Google Scholar]
- 291.Reus-Pons M, Kibele EUB, Janssen F. Differences in healthy life expectancy between older migrants and non-migrants in three European countries over time. Int J Public Health. 2017;62:531–40. doi: 10.1007/s00038-017-0949-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Lanari D, Bussini O. International migration and health inequalities in later life. Ageing Soc. 2012;32:935–62. [Google Scholar]
- 293.Sole-Auro A, Crimmins EM. Health of immigrants in European countries. Int Migr Rev. 2008;42:861–76. doi: 10.1111/j.1747-7379.2008.00150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Pudaric S, Sundquist J, Johansson SE. Major risk factors for cardiovascular disease in elderly migrants in Sweden. Ethn Health. 2000;5:137–50. doi: 10.1080/713667448. [DOI] [PubMed] [Google Scholar]
- 295.Ladin K, Reinhold S. Mental health of aging immigrants and native-born men across 11 European countries. J Gerontol B Psychol Sci Soc Sci. 2013;68:298–309. doi: 10.1093/geronb/gbs163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Virgincar A, Doherty S, Siriwardhana C. The impact of forced migration on the mental health of the elderly: a scoping review. Int Psychogeriatr. 2016;28:889–96. doi: 10.1017/S1041610216000193. [DOI] [PubMed] [Google Scholar]
- 297.Sagbakken M, Kumar B, editors. Dementia, ethnic minorities and migrants. Norwegian Centre for Migration and Minority Health; 2017. [accessed Sept 3, 2017]. http://www.nakmi.no/publikasjoner/dokumenter/sagbakken-kumar- dementia-ethnic-minorities-and-migrants-nakmi-rapport-2-2017.pdf . [Google Scholar]
- 298.Migration SQR. Office for National Statistics; 2016. Dec, [accessed Jan17, 2018]. 2016 https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/internationalmigration/bulletins/migrationstatisticsquarterlyreport/dec2016. [Google Scholar]
- 299.Elrha. Research for Health in Humanitarian Crises. [accessed Aug 18, 2018]. http://www.elrha.org/r2hc/home/
- 300.Wright J, Small N, Raynor P, et al. Born in Bradford Scientific Collaborators Group Cohort profile: the born in Bradford multi-ethnic family cohort study. Int J Epidemiol. 2013;42:978–91. doi: 10.1093/ije/dys112. [DOI] [PubMed] [Google Scholar]
- 301.Bhaskaran K, Douglas I, Forbes H, dos-Santos-Silva I, Leon DA, Smeeth L. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5-24 million UK adults. Lancet. 2014;384:755–65. doi: 10.1016/S0140-6736(14)60892-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Pell J. Maximising the value of UK population cohorts: MRC strategic review of the largest UK population cohort studies. MRC; 2014. [accessed Jan 26, 2017]. http://www.mrc.ac.uk/news-events/publications/ [Google Scholar]
- 303.The Open University. Mapping Refugee Media Journeys. [accessed Jan 17, 2018]. http://www.open.ac.uk/ccig/research/projects/mapping-refugeemedia-journeys .
- 304.Pigott DM, Deshpande A, Letourneau I, et al. Local, national, and regional viral haemorrhagic fever pandemic potential in Africa: a multistage analysis. Lancet. 2017;390:2662–72. doi: 10.1016/S0140-6736(17)32092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Redding DW, Moses LM, Cunningham AA, Wood J, Jones KE. Environmental-mechanistic modelling of the impact of global change on human zoonotic disease emergence: a case study of Lassa fever. Methods Ecol Evol. 2016;7:646–55. [Google Scholar]
- 306.Worldpop. Nepal Floods. Population mobility, displacement and impacted areas based on analyses of anonymized mobile network data. 2016. [accessed Jan 17, 2018]. http://www.worldpop.org.uk/nepal/
- 307.Fazel M, Betancourt TS. Preventive mental health interventions for refugee children and adolescents in high-income settings. Lancet Child Adolesc Health. 2018;2:121–32. doi: 10.1016/S2352-4642(17)30147-5. [DOI] [PubMed] [Google Scholar]
- 308.WHO. Health policy and systems research; a methodology reader. [accessed Oct 1, 2017]. http://www.who.int/alliance-hpsr/alliancehpsr_reader.pdf .
- 309.Sheikh K, George A, Gilson L. People-centred science: strengthening the practice of health policy and systems research. Health Res Policy Syst. 2014;12:19. doi: 10.1186/1478-4505-12-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.