Summary
Background
Lower incomes are associated with poorer mental health and wellbeing, but the extent to which income has a causal effect is debated. We aimed to synthesise evidence from studies measuring the impact of changes in individual and household income on mental health and wellbeing outcomes in working-age adults (aged 16–64 years).
Methods
For this systematic review and meta-analysis, we searched MEDLINE, Embase, Web of Science, PsycINFO, ASSIA, EconLit, and RePEc on Feb 5, 2020, for randomised controlled trials (RCTs) and quantitative non-randomised studies. We had no date limits for our search. We included English-language studies measuring effects of individual or household income change on any mental health or wellbeing outcome. We used Cochrane risk of bias (RoB) tools. We conducted three-level random-effects meta-analyses, and explored heterogeneity using meta-regression and stratified analyses. Synthesis without meta-analysis was based on effect direction. Critical RoB studies were excluded from primary analyses. Certainty of evidence was assessed using Grading of Recommendations Assessment, Development and Evaluation (GRADE). This study is registered with PROSPERO, CRD42020168379.
Findings
Of 16 521 citations screened, 136 were narratively synthesised (12·5% RCTs) and 86 meta-analysed. RoB was high: 30·1% were rated critical and 47·1% serious or high. A binary income increase lifting individuals out of poverty was associated with 0·13 SD improvement in mental health measures (95% CI 0·07 to 0·20; n=42 128; 18 studies), considerably larger than other income increases (0·01 SD improvement, 0·002 to 0·019; n=216 509, 14 studies). For wellbeing, increases out of poverty were associated with 0·38 SD improvement (0·09 to 0·66; n=101 350, 8 studies) versus 0·16 for other income increases (0·07 to 0·25; n=62 619, 11 studies). Income decreases from any source were associated with 0·21 SD worsening of mental health measures (–0·30 to –0·13; n=227 804, 11 studies). Effect sizes were larger in low-income and middle-income settings and in higher RoB studies. Heterogeneity was high (I2=79-87%). GRADE certainty was low or very low.
Interpretation
Income changes probably impact mental health, particularly where they move individuals out of poverty, although effect sizes are modest and certainty low. Effects are larger for wellbeing outcomes, and potentially for income losses. To best support population mental health, welfare policies need to reach the most socioeconomically disadvantaged.
Funding
Wellcome Trust, Medical Research Council, Chief Scientist Office, and European Research Council.
Introduction
Poor mental health is a leading global cause of disability linked with worsened social and physical health outcomes.1–4 Social conditions are thought to be important in driving mental health burden and increasing health inequalities.5 Income could be particularly important, with those on lower incomes less able to access health-promoting goods and services and maintain a feeling of control or security over their lives.6–8 Crucially, income is also amenable to policy intervention.9,10
Low income is demonstrably correlated with poor mental health, but it is less clear whether changing someone’s income will improve their mental health.11,12 Those with poor mental health are more likely to experience subsequent income losses, indicating potential for reverse causation or health selection.13 Additionally, poor mental health and income changes have common causes (eg, job loss) that introduce potential for confounding.14 There is evidence that income source and setting might influence any potential causal relationship, with more convincing evidence of effects on mental health for those on low incomes, in low-income countries, or where money is from a policy intervention rather than one-off events like lottery wins.15–19
Governments have the ability to redistribute incomes through taxation or welfare policies, potentially influencing mental health and health inequalities, especially in the working-age population which is particularly influenced by such policy levers (eg, via income taxation or unemployment benefits).20–22 There have been narrative reviews considering the impact of income changes on adult mental health,23 but previous quantitative evidence syntheses have focused on specific exposures or are restricted to low-income or middle-income settings.24,25 Using tools designed to aid in the interpretation of potential threats to causal inference, we aimed to quantify the impact of any changes in individual or household incomes on mental health outcomes for working-age adults, considering whether the source or size of income change was important, and whether any beneficial or detrimental impacts varied by socioeconomic background or setting.
Methods
Overview
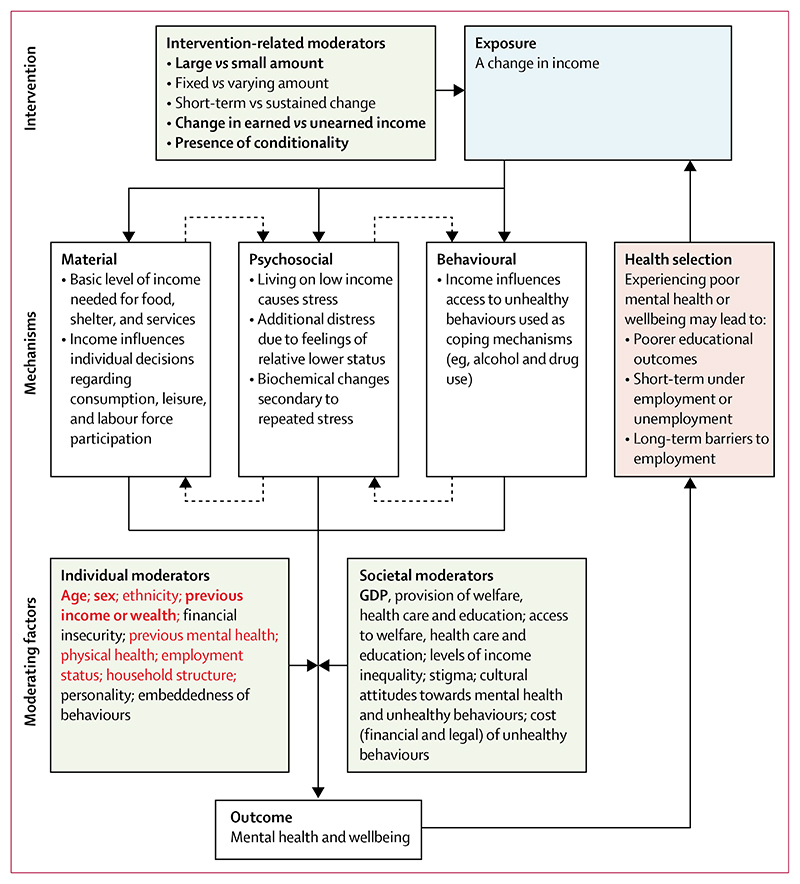
We did a systematic review and meta-analysis as per Preferred Reporting Items for Systematic review and Meta-Analysis (PRISMA) and Synthesis Without Meta-analysis (SWiM) in systematic reviews: reporting guidance.26,27 This study is registered with PROSPERO, CRD42020168379.28 A logic model was developed drawing on a systematic review of theory by Benzeval and colleagues13 and advice from subject experts (figure 1; further background in protocol28), which was used to identify important confounders and effect modifiers to explore in subgroup analysis. Protocol deviations are reported in the appendix (p 2).
Figure 1. Logic model indicating theory of change for income and mental health.
Variables considered as important potential confounders in this study are indicated in red and were selected a priori by the researchers on the basis of variables that were viewed as key confounders in the literature. Variables considered important potential effect modifiers for exploration in this study are indicated in bold; these were selected based on assumptions regarding their likely importance and anticipated data availability. GDP=gross domestic product.
Literature search
Searches of peer-reviewed and relevant grey literature (eg, economics working papers and academic theses) were done using MEDLINE, Embase, Web of Science, PsycINFO, ASSIA, EconLIT, and RePEc on Feb 5, 2020, using a strategy developed with an information specialist (appendix p 14). No date limits were applied to the search. Search terms included “mental health”, depression, anxiety, “anxiety disorder”, wellbeing, “quality of life”, “life satisfaction”, “psychological distress” AND income [or synonym] NEAR change [or synonym]. See the appendix for full details on the search terms (appendix p 14). Our population of interest was working-age adults (aged 16–64 years). Exposure or intervention of interest was change in household or individual income from any source, compared to no equivalent income change. All mental health (eg, depression or anxiety) or wellbeing (eg, life satisfaction or happiness) outcomes were eligible for inclusion (details on classification are in the appendix p 2). We included randomised and non-randomised quantitative studies, with the latter category including any non-randomised study design (eg, case-control, cohort, or natural experiment studies) provided comparison was made between an exposed and unexposed group. References were de-duplicated in Endnote (version X9) and imported to Covidence for screening.
Study selection
All titles or abstracts and full-text papers were independently screened by RMT and a second reviewer (EI, AKP, MS, AL, AP, or SVK), with conflicts resolved by consensus or discussion with a third reviewer (SVK or HT). Non-English-language studies were excluded at the full-text stage. Reference lists of relevant systematic reviews and included studies were screened for additional studies. Where eligible studies contained overlapping or duplicate data, a set of decision rules considered alignment with our PECO (ie, population, exposure, comparator, and outcome) and risk of bias (RoB; appendix p 2).
Data extraction and RoB assessment
Data were extracted in Excel (version 2202) by RMT and checked by a second reviewer (EI, AKP, MS, AL, AP, or SVK). RoB assessment was done independently at the datapoint or outcome level by RMT and the same second reviewer using the Cochrane Collaboration RoB-2 tool for randomised studies29 and Risk of Bias in Non-randomised Studies of Interventions (ROBINS-I) for non-randomised studies.30 A low ROBINS-I rating is considered comparable to a well-conducted randomised controlled trial (RCT) in assessing intervention effect; omitting any key confounder automatically merits at least a serious rating. Conflicts were resolved by consensus. Non-randomised studies rated critical were excluded from primary synthesis as per ROBINS-I guidance but explored in a sensitivity analysis. Further detail on extracted items, decision rules, and RoB assessment, including selection of prespecified key confounders, is available in the appendix (pp 3, 6).
Data synthesis
Synthesis without meta-analysis (SWiM)
We synthesised findings from all studies within the SWiM. Direction of effect was coded as beneficial or harmful for both outcome domains separately at study level, with findings categorised as inconsistent if less than 70% of extracted datapoints reported one effect direction.31 As per Cochrane guidance, statistical significance was not taken into account during this classification.32 Modified effect direction plots displayed findings stratified by RoB and are presented in the appendix (p 96). Sign tests assessed evidence of effect (excluding studies at critical RoB or with inconsistent findings) and χ2 tests assessed differences in effect by RoB, study design (RCT vs non-randomised studies), or income change source.
Primary meta-analyses
We did random-effects meta-analyses, with mental health and wellbeing measures analysed separately. Heterogeneity was explored using the I2 statistic. Where two or more datapoints from one study were included in the same analysis (eg, sex-stratified results), three-level meta-analyses accounted for dependence of effect sizes.33 We used the restricted maximum likelihood estimator to estimate between-study variance.34 In our primary meta-analyses, we combined estimates from RCTs and non-randomised studies, as they provide contrasting strengths and weaknesses for our research question; however, we also did a subgroup analysis analysing them separately.
Continuous exposures of log (income) were analysed separately from binary exposures of income increases or decreases because the income–health relationship is thought to be curvilinear, with decreasing marginal returns at higher levels.35 Binary exposure datapoints were transformed to standardised mean difference (SMD) for synthesis, combining continuous and dichotomous outcomes as per Cochrane guidelines.36 Continuous exposure datapoints were transformed to standardised beta coefficients or odds ratios (ORs) for continuous and binary outcomes, respectively (appendix p 4).
Where more than ten studies were included in the meta-analysis, meta-regression explored heterogeneity by: characteristics of income change (increases vs decreases, small vs large changes, or movement across a poverty threshold), type of income change (source of transfer, earned vs unearned, if accompanied by conditionality), type of outcome measure (self-report vs validated tools or administrative data), and individual or setting (socioeconomic position [SEP], high-income country [HIC] vs low-income and middle-income country [LMIC]). Statistical analysis was done using the meta package (version 4·19-0) in RStudio.37
Subgroup analyses
Additionally, we stratified meta-analyses by sex, study design (RCT vs non-randomised studies), RoB (low or moderate vs serious vs critical), movement across a poverty threshold, participant SEP (as defined within the study), HIC versus LMIC, and whether non-working-age participants were included. Analyses stratified by poverty movements and SEP generated similar results due to data overlap; only the former are discussed in the Results section (all plots are available in the appendix p 97). Publication bias or small study effect was assessed using funnel plots and Egger’s test.
Certainty assessment
Certainty of evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system.38 This combines information on five domains: risk of bias, imprecision, inconsistency (including statistical heterogeneity), indirectness (assessing how closely available data reflect the research question), and publication bias. Key outcomes reported were: the impact of income changes on grouped mental health outcomes and the impact of income changes on grouped wellbeing outcomes. A planned key outcome on the impact of changes in unearned income was not reported (appendix p 2). A condensed GRADE summary of findings (table) is presented, with additional details provided in the appendix (p 93).
Table. Condensed summary of findings and certainty of evidence (as per GRADE).
| Number of participants (number of studies) | Effect estimate (95% CI) | Certainty of evidence | |
|---|---|---|---|
| Income changes and grouped mental health outcomes | |||
| Any income change (effect direction) | 922 428 (54) | 88·9% (77·4 to 95·8) of studies report beneficial effect of income on mental health | Low* |
| 10% income increase | 1510 666 (9) | Standardised β 0·003 (0·0003 to 0·005) | Low* |
| Crossing poverty or subsistence threshold | 42 128 (18) | SMD 0·13 (0·07 to 0·20) | Low† |
| Income decrease (mixed amounts) | 227 804 (11) | SMD –0·21 (–0·30 to – 0·13) | Very low‡ |
| Income changes and grouped wellbeing outcomes | |||
| Any income change (effect direction) | 311 219 (40) | 95·0% (83·1 to 99·4) of studies report beneficial effect of income on wellbeing | Low* |
| 10% income increase | 105 326 (9) | Standardised β 0·003 (0·002 to 0·005) | Very low‡ |
| Crossing poverty or subsistence threshold | 101 350 (8) | SMD 0·38 (0·09 to 0·66) | Low* |
| Income decrease (mixed amounts) | Insufficient evidence§ |
GRADE=Grading of Recommendations Assessment, Development and Evaluation. SMD=standardised mean difference. For full GRADE results, see the appendix (p 93).
Downgraded by 2 levels for inconsistency and risk of bias of included studies.
Downgraded by 2 levels for inconsistency and indirectness of evidence.
Downgraded by 3 levels for inconsistency, risk of bias of included studies, and publication bias.
Insufficient numbers of studies identified to investigate this planned GRADE outcome.
No ethics approval was requested, as the research solely extracted non-disclosive data from previously published studies in which informed consent was obtained by the primary investigators.28
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Of 16 521 articles screened, 136 studies were eligible for inclusion (PRISMA flowchart, appendix p 18).18,19,39–172 90 studies reported mental health outcomes (230 datapoints) and 65 reported wellbeing outcomes (146 datapoints). Studies excluded at the full-text stage are detailed in the appendix (p 69). Only 17 included studies were RCTs (12·5%; appendix p 28), all of which examined the effect of a binary income increase. Most included studies were from HICs (72·1%), with 26·5% from the USA.
Most studies (61·0%) reported on income changes without specifying their size, but 30·1% specifically reported effects of large income changes (>20% change, or described as large by study authors), and 8·8% small income changes. A sizeable minority (37·5%) focused on income changes in low SEP populations, with 20·6% measuring the effect of moves across a meaningful poverty or subsistence threshold (either explicitly reported as such or representing a large change in an exclusively low SEP population; appendix p 6). Income change source was not reported in 46·3% of studies, typically where income fluctuations were measured over time in panel data. Known sources were: welfare policies influencing income alone such as cash transfers (16·9%); disasters (7·4%); taxation or wage policies (6·6%); welfare policies with additional components beyond income (5·9%); lottery wins (5·1%); and income changes due to illness or caring responsibilities, salary changes, benefit advice services, or cash transfers from other sources (all <5%). Time horizons ranged from 0 to 288 months, with 12 months the most common interval between intervention and outcome (mean 34·3; median 14·5 [IQR 12–36]).
Risk of bias of the 136 included studies was high: 4·8% were rated low, 18·4% moderate or some concerns, 47·1% serious or high, and 30·1% critical (appendix p 63). 68 non-critical studies were included in primary meta-analyses, with an additional 18 critical RoB studies explored in sensitivity meta-analyses.
The effect direction in all 90 studies considering mental health outcomes is shown in an effect direction plot in the appendix (p 96). After excluding studies with inconsistent findings and at critical RoB, 88·9% reported a beneficial effect of income, where either an income increase was associated with improvement in mental health or an income decrease was associated with worsening of mental health (95% CI 77·4–95·8, n=54, p<0·0001). There was no evidence of difference in this percentage by RoB (p=0·55), study design (p=0·77), or income source (p=0·84).
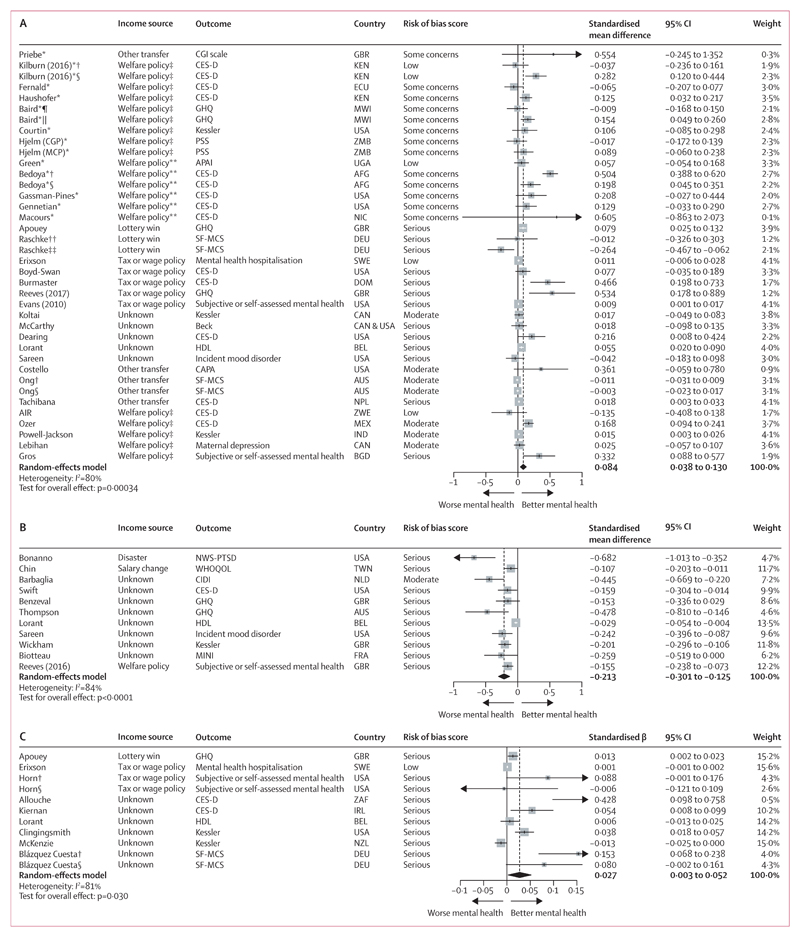
On meta-analysis, a binary income increase was associated with a 0·084 SD improvement in mental health measures (95% CI 0·038 to 0·130, I2=80%, indicating high heterogeneity). This was based on 32 studies analysing 258 637 people (figure 2A), with most exposures influencing unearned income and 40·6% of studies (n=13) rated serious RoB. Eight RCTs and five non-randomised studies (40·6% of all studies) included at least one important co-intervention for those exposed that could influence mental health, such as education, training, or work incentives (appendix p 28). Meta-regression suggested effect sizes were larger where income changes moved individuals across a poverty threshold (β 0·11, 95% CI 0·03 to 0·19) or targeted those of low SEP (0·08, –0·01 to 0·17]), or in LMICs (0·07, −0·02 to 0·15; appendix p 91). Considering income source, only welfare policies not solely targeting income had differential, slightly larger effects (β 0·18, 95% CI 0·02 to 0·34). In stratified analyses (appendix pp 97–104), effect sizes were strikingly larger for poverty transitions (SMD 0·134, 95% CI 0·070 to 0·198 vs 0·011, 0·002 to 0·019 for other income changes; p<0·00017 for test of differences), as well as in LMICs (SMD 0·122, 95% CI 0·041 to 0·203 vs 0·030, 0·007–0·053 in HICs; p=0·033). Critical RoB studies reported effect sizes six times larger than other studies: SMD 0·507 (95% CI 0·163 to 0·851) versus 0·087 for both low or moderate RoB (0·030 to 0·144) and serious RoB (–0·001 to 0·175; p=0·061; appendix p 99). Effect sizes also appeared larger in RCTs than in non-randomised studies (SMD 0·130, 95% CI 0·047 to 0·213 vs 0·043, 0·012 to 0·074; p=0·054) and for studies that only included those of working age (0·118, 0·056 to 0·181 vs 0·035, –0·016 to 0·087; p=0·044). There were no important sex differences (appendix p 97).
Figure 2. Forest plots for meta-analyses of studies reporting the effect of a binary income increase (A; n=32) and decrease (B; n=11) on a mental health outcome and of a continuous log (income) change on a mental health outcome (C; n=9).
In A, number of people=258 637 and number of observations=1 756 078. In B, number of people=227 804 and number of observations=281 728. In C, number of people=1 510 221 and number of observations=3 036 715. In all panels, studies are sorted in order of trial status (randomised controlled trial or non-randomised study), income source, outcome, and risk of bias score. AFG=Afghanistan. APAI=Acholi Psychosocial Assessment Instrument. AUS=Australia. Beck=Beck depression inventory. BEL=Belgium. BGD=Bangladesh. CAN=Canada. CAPA=Child and Adolescent Psychiatric Assessment. CES-D=Center for Epidemiological Studies-Depression scale. CGI=Clinical Global Impression. CGP=Zambia child grant programme. CIDI=Composite International Diagnostic Interview. DEU=Germany. DOM=Dominican Republic. ECU=Ecuador. FRA=France. GBR=Great Britain. GHQ=General Health Questionnaire. HDL=Health and Daily Living Form. IND=India. IRL=Ireland. KEN=Kenya. Kessler=Kessler Psychological Distress scales. MCP=Zambia multiple category cash transfer programme. MEX=Mexico. MINI=Mini International Neuropsychiatric Interview. MWI=Malawi. NLD=Netherlands. NIC=Nicaragua. NPL=Nepal. NWS-PTSD=National Women’s Study-Post-traumatic Stress Disorder module. NZL=New Zealand. PSS=Perceived Stress Scale. SF-MCS=Mental Component Summary of Short Form Survey. SWE=Sweden. TWN=Taiwan. UGA=Uganda. WHOQOL=psychological domain of abbreviated WHO Quality of Life tool. ZAF=South Africa. ZMB=Zambia. ZWE=Zimbabwe. *Study was a randomised controlled trial. †Sex-stratified results for women. ‡Welfare policy only affected income. §Sex-stratified results for men. ¶Stratified results for school dropouts. ||Stratified results for school attenders. **Welfare policy influenced income and other factors. ††Stratified results for those of high educational attainment. ‡‡Stratified results for those of low educational attainment.
A binary income decrease was associated with a 0·213 SD worsening of mental health measures (95% CI –0·301 to –0·125; I2=84%), two and a half times the magnitude for income increases. This was based on eleven non-randomised studies analysing 227 804 people (figure 2B), with income source mostly unknown, and all but one rated serious RoB. Meta-regression suggested larger effect sizes where the income change was due to a disaster (β –0·48, 95% CI –0·88 to –0·07), although only one study reported this exposure;61 no other differences were seen by income source. In stratified analyses (appendix pp 105–107) effect sizes were again larger in critical (SMD –0·346, 95% CI –0·449 to –0·244]) than in serious RoB studies (–0·185, –0·264 to –0·107; p=0·012). There was no evidence of important sex or age differences.
The pooled standardised β for a log (income) change on continuous mental health outcomes was 0·027 (95% CI 0·003 to 0·052; I2=81%), indicating a 10% income increase would be associated with a 0·003 SD improvement in mental health. This was based on nine non-randomised studies analysing 1 510 221 people (figure 2C), with income source again mostly unknown and all but one study rated serious RoB. Two low RoB Swedish lottery studies unfortunately could not be included in the synthesis as income was not log-transformed within their modelling, but they also reported a small beneficial effect of winning on mental health.18,19 On stratification (appendix p 107–109) there was some evidence effects were larger in women (SMD 0·090, 95% CI 0·031 to 0·149) than men (0·047, –0·035 to 0·129), although this was based on few studies. There was no clear evidence of important SEP or age differences.
The pooled effect for five non-randomised studies considering the effect of log (income) change on binary mental health measures was OR 0·967 (95% CI 0·919–1·016; I2=53%), with sex-stratified analysis finding no clear differences (appendix p 119).
For the wellbeing outcome domain, the effect direction in all 64 studies considering wellbeing outcomes is shown in an effect direction plot in the appendix (p 96). After excluding those with inconsistent findings and at critical RoB, 95·0% reported a beneficial effect (95% CI 83·1–99·4, n=40, sign test p<0·0001). On χ2 testing there was no evidence of differences by RoB (p=0·63), study design (p=0·68), or income source (p=0·92).
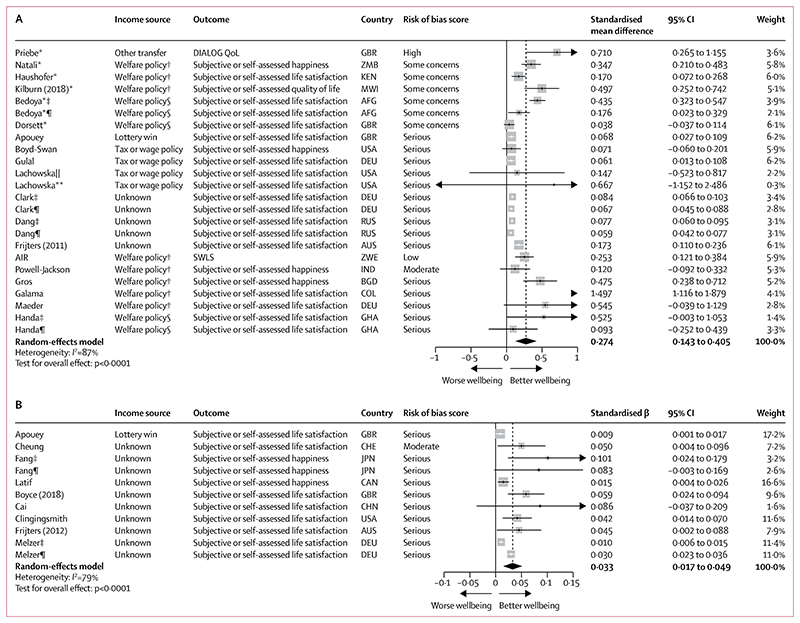
On meta-analysis, a binary income increase was associated with a 0·274 SD improvement in wellbeing measures (95% CI 0·143 to 0·405; I2=87%), three times that seen for mental health. This was based on 19 studies analysing 163 969 people (figure 3A), with most exposures originating from unearned income as in figure 2A, and 63·2% of studies (n=12) rated serious RoB. Three RCTs and three non-randomised studies (31·6% of all studies) had important co-interventions (appendix p 28). On meta-regression, only welfare policies affecting solely income potentially had larger effects (β 0·33, 95% CI –0·01 to 0·68). In stratified analyses (appendix p 110–116), effect sizes were larger for poverty transitions (SMD 0·377, 95% CI 0·093 to 0·661 vs 0·160, 0·069 to 0·252]; p=0·16) and in LMICs (0·371, 0·153 to 0·589 vs 0·087, 0·052 to 0·122; p=0·012). Studies at serious rather than low or moderate RoB reported slightly larger effects (0·315, 0·089 to 0·540 vs 0·245, 0·137 to 0·353; p=0·83) but estimates were imprecise. Effect sizes for women were larger than for men (0·195, 0·080 to 0·309 vs 0·063, 0·050 to 0·077; p<0·0046). There was no evidence of important differences when stratifying by study design or age.
Figure 3. Forest plots for meta-analyses of studies reporting the effect of a binary income increase on a wellbeing outcome (A; n=19) and a continuous log (income) change on a wellbeing outcome (B; n=9).
In A, number of people=163 969 and number of observations=885 981. In B, number of people=105 326 and number of observations=567 356. In both panels, studies are sorted in order of trial status (randomised controlled trial or non-randomised study), income source, outcome, and risk of bias score. AFG=Afghanistan. AIR=American Institutes for Research. AUS=Australia. BGD=Bangladesh. CHE=Switzerland. CHN=China. COL=Columbia. DEU=Germany. DIALOG QoL=DIALOG quality of life scale. GBR=Great Britain. GHA=Ghana. IND=India. JPN=Japan. KEN=Kenya. MWI=Malawi. RUS=Russia. SWLS=Diener’s Satisfaction with Life Scale. ZMB=Zambia. ZWE=Zimbabwe. *Study was a randomised controlled trial. †Welfare policy only affected income. ‡Sex-stratified results for women. §Welfare policy influenced by income and other factors. ¶Sex-stratified results for men. ||Stratified results for those on medium income. **Stratified results for those on low income.
There were insufficient non-critical RoB studies considering the impact of a binary income decrease on wellbeing outcomes to perform meta-analysis (n=3). However, in a sensitivity analysis including critical RoB studies (appendix p 117), the effect size was slightly larger in critical RoB studies (SMD –0·278, 95% CI –0·378 to –0·178 vs –0·195, –0·317 to –0·073; p=0·30) with wide CIs.
The pooled standardised β for a log (income) change on continuous wellbeing outcomes was 0·033 (95% CI 0·017–0·049; I2=79%), indicating a 10% income increase would be associated with a 0·003 SD improvement in wellbeing, a similar effect magnitude as for mental health. This was based on nine non-randomised studies analysing 105 326 people (figure 3B), with income source again unknown in most cases and all but one study rated serious RoB (88·9%). Again, a low RoB lottery study could not be included in meta-analysis but also reported a small significant effect of lottery wins on life satisfaction.19 There was no clear evidence of important age or sex differences (appendix pp 117–118).
For common outcome measures, we used variance or SDs reported in other included studies to facilitate data transformations where these were not reported for the study sample (n=7;46,47,82,92,97,100,139 appendix p 5). To ensure this did not introduce bias we re-ran meta-analyses excluding these studies, and there was no change to the overall pattern of the findings (appendix pp 120–123).
Funnel plots and Egger’s test results indicated some evidence of publication bias or small study effect in our primary meta-analyses (appendix pp 123–125). This was particularly striking for studies considering income decreases and mental health outcomes (p<0·0001), and continuous income changes and wellbeing outcomes (p=0·027).
Overall, the evidence base showed substantial limitations when assessed according to the GRADE criteria (table and appendix p 93).38 We report with low certainty that income changes have beneficial effects on mental health and wellbeing (ie, an income increase is associated with improvement while an income decrease is associated with worsening). Our estimates of effect size for key outcomes were subject to low or very low certainty.
Discussion
Our comprehensive systematic review and meta-analysis, covering a broad range of income change sources, contexts, and settings, found that income has beneficial effects on mental health and wellbeing: income increases resulted in a 0·08 SD (95% CI 0·04 to 0·13) improvement in mental health measures and 0·27 SD (0·14 to 0·41) improvement in wellbeing measures. In stratified analyses, effects were up to 13 times larger where increases moved individuals out of poverty, and up to four times larger for those in LMICs. There was no consistent evidence that effect size was influenced by income source. Effects from studies reporting continuous income were smaller than those considering binary income changes, possibly because these could not incorporate any threshold effect of poverty. Effects might be larger for income decreases, which were associated with a 0·21 SD worsening of mental health measures (95% CI –0·30 to –0·13). Certainty for all key outcomes was low or very low due to high heterogeneity, considerable risk of bias, unmeasured confounding, and inclusion of cointerventions such as conditionality or non-monetary benefits.
The relationship between income and mental health has been subject to detailed study over many decades. However, previous evidence syntheses have been subject to limitations. Cooper and Stewart23 published a narrative review in 2015 concluding income has a positive effect on mental health, but did not attempt to quantify this relationship or explore why effects diverge across the literature. A more recent non-systematic review by Ridley and colleagues25 examined the effect of anti-poverty interventions on mental health, reporting a similar effect size to our own (SMD 0·09) despite excluding non-randomised studies. McGuire and colleagues24 in their meta-analysis focus on cash transfers in LMICs and do not assess certainty, but also report similar effect sizes. The added value of our study is in summarising evidence from a broader range of exposures, considering how effects differ by exposure characteristics and between groups, and robustly assessing RoB and certainty of the evidence base to aid in causal interpretation, providing meta-analysed effect estimates showing a small if uncertain effect of income change on mental health.
The larger effect sizes found in our study for income increases targeting the most socioeconomically disadvantaged were not unexpected.15,23 It is difficult to determine which of the three most consistent effect modifiers we identified (poverty transitions, lower SEP, or LMIC setting) is most important, due to considerable overlap of studies falling into two or three of these categories. Our finding of a larger effect size for wellbeing outcomes was in keeping with those of McGuire and colleagues;24 we do note that most studies reported single subjective wellbeing items (eg, life satisfaction or happiness), which are arguably more biased than multi-dimensional wellbeing measures.173,174
Existing literature on loss aversion suggests financial losses could have greater effects on mental health than financial gains,63 although evidence is inconsistent.175 The very low certainty we report in this finding due to potential publication bias does not resolve this debate, nor will it be easy to settle since reducing incomes cannot be ethically tested in trials. Here, future research might need to rely on natural experiment approaches, ideally with pre-registered analysis plans to ensure dissemination of negative findings.176 Triangulation across methodologies could help overcome the limitations and trade-offs required by each individual approach to determining causal inference, in particular where this draws on cross-disciplinary learning.177
Finally, to contextualise our results within wider literature on common mental health interventions, in comparable meta-analyses on treatments for mental ill health pooled effect sizes for antidepressant usage and cognitive behavioural therapy (CBT) were SMD 0·30 and SMD 0·53, respectively.178,179 This implies that, based on our findings, income-based interventions that move people above the poverty line might be roughly half as effective in improving mental health as antidepressants and a quarter as effective as CBT. Given that, in contrast with our included studies, these treatments are primarily studied in individuals at high-risk rather than general population samples, the potential impacts of anti-poverty interventions at a population mental health level could be substantial.
Our study has important strengths. To our knowledge, this is the first review to quantitatively summarise the totality of the evidence base on income changes and mental health or wellbeing. We closely followed gold standard Cochrane guidance on conducting and reporting systematic reviews of interventions. Using ROBINS-I we were able to include non-randomised studies and rigorously assess these against the same standard for threats to causal interpretation as RCTs. We pre-registered our study protocol and made only minimal changes (appendix p 2). Our decisions about key confounding variables and stratified analyses were informed by a comprehensive literature review and preparation of a logic model (figure 1), ensuring our assumptions about proposed causal mechanisms were clear.
However, some important limitations remain. First, some relevant economics working papers might have been missed by our search methods despite efforts to avoid this. Second, the heterogeneity of included studies is very high. Combining RCTs and non-randomised studies in the same meta-analyses (which is not standard practice) could have contributed to this, although we did not find marked differences in heterogeneity when stratifying by study design. We feel on balance the benefits of including non-randomised studies (which often evaluate real-world, large-scale natural policy experiments) probably outweighed potential drawbacks. Third, although ideally synthesis of income change exposures would be expressed in terms of absolute or relative change, data availability and reporting meant we were unable to do this with our binary exposures. Our sensitivity analyses considering effects of small versus large changes and poverty transitions explored some heterogeneity by intervention size, but possibly not all. Excluding non-English language texts is also a limitation, although we note only 12 records were excluded solely for this reason (PRISMA flowchart; appendix p 18). Finally, although not unanticipated, the relatively high RoB of included studies means caution should be taken in interpretation, as shown by our GRADE certainty assessments.
In terms of policy implications, our findings add to the evidence base supporting income supplementation as a means to improve mental health and wellbeing, especially when targeted at those in poverty or in LMICs. Although effect sizes are small, they are comparable with common individual-level interventions such as antidepressants or CBT. Our findings also suggest a particularly detrimental effect of income decreases, indicating policy makers wishing to protect population mental health should mitigate against societal or economic changes that could erode income. Decision makers and policy modellers might benefit from use of our results when calculating potential mental health impacts of future policies that will change incomes.
Future intervention studies of cash transfers should consider including more robust, multi-dimensional measures of wellbeing. There is a need for studies reporting the impact of income change on a continuous scale that consider the question in a causal or counterfactual way, as well as studies considering longitudinal effects of living on a low income. The low certainty of our GRADE assessments highlights both that non-randomised studies considering this topic area frequently do not appropriately adjust for known key confounding variables (particularly past mental health), and that RCTs often include cointerventions which create difficulties in measuring the effect of income alone. To improve certainty in future estimates, researchers should consider how best to reduce these threats to causal inference during study planning.
Given our focus on individual-level exposures and outcomes, future systematic reviews considering the quantitative impact of relative income or community-level outcomes would be welcome, as would further analyses considering whether and how the benefits of income are augmented when accompanied by co-interventions. Finally, in our logic model (figure 1) we identified some potential effect modifiers (eg, ethnicity and income inequality) we were unable to explore in detail in our synthesis due to lack of data; future research on this topic could benefit from use of our logic model when planning analyses to prespecify potentially important variables for stratification.
Our findings suggest that income probably does have a causal effect on mental health and wellbeing despite weaknesses in the evidence base, and this relationship is stronger for those in poverty or in LMICs. To be most supportive of population mental health and reduce inequalities, policy makers should design income and welfare policies that provide an adequate financial safety net for the most socioeconomically disadvantaged. There would be considerable value in future research investigating the mechanisms linking income and health, and the incorporation of these findings into intervention planning and evaluation.
Supplementary Material
Research in context.
Evidence before this study
Those on low incomes are known to have poorer mental health and wellbeing than those who are wealthier. However, there is debate in the literature around the extent to which this represents a causal relationship, rather than being solely the result of confounding or reverse causation. Before conducting this study, we searched MEDLINE, Google Scholar, and PROSPERO to identify existing or planned English-language systematic and non-systematic reviews of the relationship between income and health outcomes in adults, with no date limits; we repeated these scoping searches on Nov 24, 2021. Search terms included health, “mental health”, depression, anxiety, wellbeing AND income (or synonym). Existing reviews have either suggested a potential association between income changes and mental health without attempting to quantify this potential relationship or considering risk of bias within the literature, or have focused on narrow definitions of exposures in restricted settings.
Added value of this study
In this systematic review and meta-analysis, integrating Cochrane risk of bias tools designed to assist in interpretating threats to causality, income changes were associated with small but consistent effects on subsequent mental health and wellbeing outcomes in working-age adults (aged 16–64 years). Effect sizes were largest where increases crossed a poverty threshold. To our knowledge, this is the first comprehensive systematic review to quantify effect sizes through meta-analysis and rigorously assess causality and certainty of evidence across the breadth of literature on this topic.
Implication of all the available evidence
Income changes probably have a causal effect on the mental health of working-age adults, although certainty in the effect size is low due to heterogeneity and risk of bias. Welfare policy makers wishing to improve public mental health should prioritise lifting individuals out of poverty.
Acknowledgments
This work was supported by the Wellcome Trust (218105/Z/19/Z and 205412/Z/16/Z), NHS Research Scotland (SCAF/15/02), the Medical Research Council (MC_UU_00022/2), the Chief Scientist Office (SPHSU17), and the European Research Council (949582). The authors gratefully acknowledge the assistance of Valerie Wells in designing and implementing the literature search, Rod Taylor in providing guidance on statistical synthesis, and Michele Hilton Boon in providing guidance on usage of GRADE, and warmly thank the project advisory group members for providing feedback on the protocol and provisional findings. We also thank Guido Schwarzer, creator of the R meta package, for his helpful responses and package updates in relation to our modelling requirements.
Footnotes
See Online for appendix
Contributors
RMT, SVK, AP, AL, and HT drafted the study protocol. GM and AR provided critical feedback on the protocol as part of the project’s advisory group. RMT did the literature searches, and EI, AKP, MS, SVK, AP, AL, and HT contributed to the screening process and selection of included studies. RMT initially extracted data and did risk of bias assessments; these data were subsequently verified by a second reviewer (either EI, AKP, MS, SVK, AP, or AL) who also completed independent risk of bias scores. RMT completed the data analysis, and all authors had access to the data. All authors critically reviewed and approved the manuscript.
Declaration of interests
We declare no competing interests.
For the study protocol see https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=168379
For the GitHub repository see https://github.com/rachelmthomson/thomson-income-mh-sr
Contributor Information
Prof Gerry McCartney, School of Social and Political Sciences, University of Glasgow, Glasgow, UK; Public Health Scotland, Edinburgh, UK.
Aaron Reeves, Department of Social Policy and Intervention, University of Oxford, Oxford, UK.
Prof S Vittal Katikireddi, MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, Glasgow, UK; Public Health Scotland, Edinburgh, UK.
Data sharing
The study protocol is published on PROSPERO. All extracted data used for analysis and analytic code are available in a public GitHub repository. Template data forms and copies of the totality of data extracted from included studies are available from the corresponding author on reasonable request.
References
- 1.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3:171–78. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- 2.Organisation for Economic Co-operation and Development. Sick on the Job? Myths and realities about mental health and work. OECD Publishing; Paris: 2012. [Google Scholar]
- 3.Cohen BE, Edmondson D, Kronish IM. State of the art review: depression, stress, anxiety, and cardiovascular disease. Am J Hypertens. 2015;28:1295–302. doi: 10.1093/ajh/hpv047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thornicroft G. Premature death among people with mental illness. BMJ. 2013;346:969. doi: 10.1136/bmj.f2969. [DOI] [PubMed] [Google Scholar]
- 5.Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 6.Subramanian SV, Belli P, Kawachi I. The macroeconomic determinants of health. Annu Rev Public Health. 2002;23:287–302. doi: 10.1146/annurev.publhealth.23.100901.140540. [DOI] [PubMed] [Google Scholar]
- 7.Kiely KM, Leach LS, Olesen SC, Butterworth P. How financial hardship is associated with the onset of mental health problems over time. Soc Psychiatry Psychiatr Epidemiol. 2015;50:909–18. doi: 10.1007/s00127-015-1027-0. [DOI] [PubMed] [Google Scholar]
- 8.Marmot M, Wilkinson RG. Psychosocial and material pathways in the relation between income and health: a response to Lynch. BMJ. 2001;322:1233–36. doi: 10.1136/bmj.322.7296.1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piketty T. Capital and ideology. Harvard University Press; Cambridge, MA: 2020. [Google Scholar]
- 10.Hills J. Good times, bad times: the welfare myth of them and us, revised edn. Policy Press; Bristol: 2017. [Google Scholar]
- 11.Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. 2013;90:24–31. doi: 10.1016/j.socscimed.2013.04.026. [DOI] [PubMed] [Google Scholar]
- 12.Mackenbach JP. Re-thinking health inequalities. Eur J Public Health. 2020;30:615. doi: 10.1093/eurpub/ckaa001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benzeval M, Bond L, Campbell M, et al. How does money influence health? MRC/CSO Social and Public Health Sciences Unit; York: 2014. [Google Scholar]
- 14.Gunasekara FI, Carter K, Blakely T. Change in income and change in self-rated health: systematic review of studies using repeated measures to control for confounding bias. Soc Sci Med. 2011;72:193–201. doi: 10.1016/j.socscimed.2010.10.029. [DOI] [PubMed] [Google Scholar]
- 15.Owusu-Addo E, Renzaho AMN, Smith BJ. The impact of cash transfers on social determinants of health and health inequalities in sub-Saharan Africa: a systematic review. Health Policy Plan. 2018;33:675–96. doi: 10.1093/heapol/czy020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lucas PJ, McIntosh K, Petticrew M, Roberts H, Shiell A. Financial benefits for child health and well-being in low income or socially disadvantaged families in developed world countries. Cochrane Database Syst Rev. 2008;2:CD006358. doi: 10.1002/14651858.CD006358.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pega F, Liu SY, Walter S, Pabayo R, Saith R, Lhachimi SK. Unconditional cash transfers for reducing poverty and vulnerabilities: effect on use of health services and health outcomes in low-and middle-income countries. Cochrane Database Syst Rev. 2017;11:CD011135. doi: 10.1002/14651858.CD011135.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cesarini D, Lindqvist E, Ostling R, Wallace B. Wealth, health, and child development: evidence from administrative data on Swedish lottery players. Q J Econ. 2016;131:687–738. [Google Scholar]
- 19.Lindqvist E, Ostling R, Cesarini D. Long-run effects of lottery wealth on psychological well-being. 2018. [accessed Dec 2, 2021]. https://www.nber.org/system/files/working_papers/w24667/w24667.pdf .
- 20.Thomson RM, Niedzwiedz CL, Katikireddi SV. Trends in gender and socioeconomic inequalities in mental health following the Great Recession and subsequent austerity policies: a repeat crosssectional analysis of the Health Surveys for England. BMJ Open. 2018;8:e022924. doi: 10.1136/bmjopen-2018-022924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beckfield J, Krieger N. Epi + demos + cracy: linking political systems and priorities to the magnitude of health inequities-evidence, gaps, and a research agenda. Epidemiol Rev. 2009;31:152–77. doi: 10.1093/epirev/mxp002. [DOI] [PubMed] [Google Scholar]
- 22.McCartney G, Hearty W, Arnot J, Popham F, Cumbers A, McMaster R. Impact of political economy on population health: a systematic review of reviews. Am J Public Health. 2019;109:e1–12. doi: 10.2105/AJPH.2019.305001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooper K, Stewart K. Does money in adulthood affect adult outcomes. Joseph Rowntree Foundation; York: 2015. [Google Scholar]
- 24.McGuire J, Kaiser C, Bach-Mortensen AM. A systematic review and meta-analysis of the impact of cash transfers on subjective wellbeing and mental health in low-and middle-income countries. Nat Hum Behav. 2022;6:359–70. doi: 10.1038/s41562-021-01252-z. [DOI] [PubMed] [Google Scholar]
- 25.Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: causal evidence and mechanisms. Science. 2020;370:eaay0214. doi: 10.1126/science.aay0214. [DOI] [PubMed] [Google Scholar]
- 26.Moher D, Shamseer L, Clarke M, et al. Preferred Reporting Items for Systematic review and Meta-analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campbell M, McKenzie JE, Sowden A, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890. doi: 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thomson RM, Shimonovich M, Igelström E, et al. How do changes in individual or household income impact on mental health for working-age adults? A protocol for a systematic review and metaanalysis. 2020. [accessed Dec 2, 2021]. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020168379 .
- 29.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 30.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boon MH, Thomson H. The effect direction plot revisited: application of the 2019 Cochrane handbook guidance on alternative synthesis methods. Res Synth Methods. 2021;12:29–33. doi: 10.1002/jrsm.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McKenzie JE, Brennan SE. Cochrane handbook for systematic reviews of interventions (version 6.2) 2021. Dec 2, Chapter 12: synthesizing and presenting findings using other methods. https://training.cochrane.org/handbook/current/chapter-12 . [Google Scholar]
- 33.Van den Noortgate W, López-López JA, Marín-Martínez F, Sánchez-Meca J. Three-level meta-analysis of dependent effect sizes. Behav Res Methods. 2013;45:576–94. doi: 10.3758/s13428-012-0261-6. [DOI] [PubMed] [Google Scholar]
- 34.Veroniki AA, Jackson D, Viechtbauer W, et al. Methods to estimate the between-study variance and its uncertainty in meta-analysis. Res Synth Methods. 2016;7:55–79. doi: 10.1002/jrsm.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mackenbach JP, Martikainen P, Looman CW, Dalstra JA, Kunst AE, Lahelma E. The shape of the relationship between income and selfassessed health: an international study. Int J Epidemiol. 2005;34:286–93. doi: 10.1093/ije/dyh338. [DOI] [PubMed] [Google Scholar]
- 36.Deeks J, Higgins J, Altman D. Cochrane handbook for systematic reviews of interventions (version 6.2) 2021. [accessed Dec 2, 2021]. Chapter 10: analysing data and undertaking meta-analyses. https://training.cochrane.org/handbook/current/chapter-10 . [Google Scholar]
- 37.Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–60. doi: 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–26. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abbott S, Hobby L. Welfare benefits advice in primary care: evidence of improvements in health. Public Health. 2000;114:324–27. doi: 10.1038/sj.ph.1900680. [DOI] [PubMed] [Google Scholar]
- 40.Abbott S, Hobby L, Cotter S. What is the impact on individual health of services in general practice settings which offer welfare benefits advice? Health Soc Care Community. 2006;14:1–8. doi: 10.1111/j.1365-2524.2005.00582.x. [DOI] [PubMed] [Google Scholar]
- 41.Abel GA, Albelda R, Khera N, et al. Financial hardship and patient-reported outcomes after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2016;22:1504–10. doi: 10.1016/j.bbmt.2016.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adams H, Bell AR, Tamal MEH. Temporal dimensions of reported life satisfaction in a low-income, agricultural environment. Ecol Soc. 2019;24:29 [Google Scholar]
- 43.Adeola FO. Mental health psychosocial distress sequelae of Katrina: an empirical study of survivors. Hum Ecol Rev. 2009;16:195–210. [Google Scholar]
- 44.Allouche M. Psychological well-being and the dynamics of poverty. 2019. [accessed Dec 2, 2021]. https://www.proquest.com/docview/2306306964/EC7057764A7D4A8BPQ/1 .
- 45.Ambrey CL, Fleming CM. The causal effect of income on life satisfaction and the implications for valuing non-market goods. Econ Lett. 2014;123:131–34. [Google Scholar]
- 46.American Institutes for Research. 12-month impact report for Zimbabwe’s harmonised social cash transfer programmes. American Institutes for Research Washington; Washington, DC: 2014. [Google Scholar]
- 47.Apouey B, Clark AE. Winning big but feeling no better? The effect of lottery prizes on physical and mental health. Health Econ. 2015;24:516–38. doi: 10.1002/hec.3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Arata CM, Picou JS, Johnson GD, McNally TS. Coping with technological disaster: an application of the conservation of resources model to the Exxon Valdez oil spill. J Trauma Stress. 2000;13:23–39. doi: 10.1023/A:1007764729337. [DOI] [PubMed] [Google Scholar]
- 49.Araya R, Lewis G, Rojas G, Fritsch R. Education and income: which is more important for mental health? J Epidemiol Community Health. 2003;57:501–05. doi: 10.1136/jech.57.7.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Asadullah MN, Chaudhury N. Subjective well-being and relative poverty in rural Bangladesh. J Econ Psychol. 2012;33:940–50. [Google Scholar]
- 51.Assari S, Preiser B, Kelly M. Education and income predict future emotional well-being of whites but not blacks: a ten-year cohort. Brain Sci. 2018;8:e122. doi: 10.3390/brainsci8070122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Baird S, de Hoop J, Ozler B. Income shocks and adolescent mental health. J Hum Resour. 2013;48:370–403. [Google Scholar]
- 53.Barbaglia MG, ten Have M, Dorsselaer S, Alonso J, de Graaf R. Negative socioeconomic changes and mental disorders:a longitudinal study. J Epidemiol Community Health. 2015;69:55–62. doi: 10.1136/jech-2014-204184. [DOI] [PubMed] [Google Scholar]
- 54.Becchetti L, Castriota S. The effects of a calamity on income and wellbeing of poor microfinance borrowers: the case of the 2004 tsunami shock. J Dev Stud. 2010;46:211–33. [Google Scholar]
- 55.Bedoya Arguelles G, Coville A, Haushofer J, Isaqzadeh MR, Shapiro J. No household left behind: Afghanistan targeting the ultra poor impact evaluation. 2019. [accessed Dec 2, 2021]. https://openknowledge.worldbank.org/bitstream/handle/10986/31867/WPS8877.pdf .
- 56.Benzeval M, Judge K. Income and health: the time dimension. Soc Sci Med. 2001;52:1371–90. doi: 10.1016/s0277-9536(00)00244-6. [DOI] [PubMed] [Google Scholar]
- 57.Biotteau AL, Bonnet C, Cambois E. Risk of major depressive episodes after separation: the gender-specific contribution of the income and support lost through union dissolution. Eur J Popul. 2018;35:519–42. doi: 10.1007/s10680-018-9488-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bland SH, O’Leary ES, Farinaro E, Jossa F, Trevisan M. Long-term psychological effects of natural disasters. Psychosom Med. 1996;58:18–24. doi: 10.1097/00006842-199601000-00004. [DOI] [PubMed] [Google Scholar]
- 59.Blázquez Cuesta M, Budria S. Does income deprivation affect people’s mental well-being? 2013. [accessed Dec 2, 2021]. https://www.bde.es/f/webbde/SES/Secciones/Publicaciones/PublicacionesSeriadas/DocumentosTrabajo/13/Fich/dt1312e.pdf .
- 60.Bolden L, Wicks MN. Predictors of mental health, subjective burden, and rewards in family caregivers of patients with chronic liver disease. Arch Psychiatr Nurs. 2010;24:89–103. doi: 10.1016/j.apnu.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 61.Bonanno GA, Galea S, Bucciarelli A, Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J Consult Clin Psychol. 2007;75:671–82. doi: 10.1037/0022-006X.75.5.671. [DOI] [PubMed] [Google Scholar]
- 62.Boyce CJ, Delaney L, Wood AM. The Great Recession and subjective well-being: how did the life satisfaction of people living in the United Kingdom change following the financial crisis? PLoS One. 2018;13:e0201215. doi: 10.1371/journal.pone.0201215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Boyce CJ, Wood AM, Banks J, Clark AE, Brown GD. Money, wellbeing, and loss aversion: does an income loss have a greater effect on well-being than an equivalent income gain? Psychol Sci. 2013;24:2557–62. doi: 10.1177/0956797613496436. [DOI] [PubMed] [Google Scholar]
- 64.Boyce W, Raja S, Patranabish RG, Bekoe T, Deme-der D, Gallupe O. Occupation, poverty and mental health improvement in Ghana. Alter (Paris) 2009;3:233–44. [Google Scholar]
- 65.Boyd-Swan C, Herbst CM, Ifcher J, Zarghamee H. The earned income tax credit, mental health, and happiness. J Econ Behav Organ. 2016;126:18–38. [Google Scholar]
- 66.Brenner MH, Andreeva E, Theorell T, et al. Organizational downsizing and depressive symptoms in the European recession: the experience of workers in France, Hungary, Sweden and the United Kingdom. PLoS One. 2014;9:e97063. doi: 10.1371/journal.pone.0097063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brickman P, Coates D, Janoff-Bulman R. Lottery winners and accident victims: is happiness relative? J Pers Soc Psychol. 1978;36:917–27. doi: 10.1037//0022-3514.36.8.917. [DOI] [PubMed] [Google Scholar]
- 68.Brock AM, O’Sullivan P. From wife to widow. Role transition in the elderly. J Psychosoc Nurs Ment Health Serv. 1985;23:6–12. doi: 10.3928/0279-3695-19851201-04. [DOI] [PubMed] [Google Scholar]
- 69.Burke RJ. Reemployment on a poorer job after a plant closing. Psychol Rep. 1986;58:559–70. [Google Scholar]
- 70.Burmaster KB, Landefeld JC, Rehkopf DH, et al. Impact of a private sector living wage intervention on depressive symptoms among apparel workers in the Dominican Republic: a quasi-experimental study. BMJ Open. 2015;5:e007336. doi: 10.1136/bmjopen-2014-007336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Buttke D, Vagi S, Schnall A, et al. Community Assessment for Public Health Emergency Response (CASPER) one year following the Gulf Coast oil spill: Alabama and Mississippi, 2011. Prehosp Disaster Med. 2012;27:496–502. doi: 10.1017/S1049023X12001380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cai S, Park A. Permanent income and subjective well-being. J Econ Behav Organ. 2016;130:298–319. [Google Scholar]
- 73.Casey P, Goolsby S, Berkowitz C, et al. Maternal depression, changing public assistance, food security, and child health status. Pediatrics. 2004;113:298–304. doi: 10.1542/peds.113.2.298. [DOI] [PubMed] [Google Scholar]
- 74.Cheung F, Lucas RE. When does money matter most? Examining the association between income and life satisfaction over the life course. Psychol Aging. 2015;30:120–35. doi: 10.1037/a0038682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chou FH, Chou P, Su TT, et al. Quality of life and related risk factors in a Taiwanese village population 21 months after an earthquake. Aust N Z J Psychiatry. 2004;38:358–64. doi: 10.1080/j.1440-1614.2004.01364.x. [DOI] [PubMed] [Google Scholar]
- 76.Chin WS, Guo YL, Liao SC, et al. Quality of life at 6 years after occupational injury. Qual Life Res. 2018;27:609–18. doi: 10.1007/s11136-017-1772-5. [DOI] [PubMed] [Google Scholar]
- 77.Chrostek P. An empirical investigation into the determinants and persistence of happiness and life evaluation. J Happiness Stud. 2016;17:413–30. [Google Scholar]
- 78.Clark AE, D’Ambrosio C, Ghislandi S. Adaptation to poverty in long-run panel data. Rev Econ Stat. 2016;98:591–600. doi: 10.1162/REST_a_00544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Clingingsmith D. Negative emotions, income, and welfare: causal estimates from the PSID. J Econ Behav Organ. 2016;130:1–19. [Google Scholar]
- 80.Coley RL, Lombardi CM. Low-income women’s employment experiences and their financial, personal, and family well-being. J Fam Psychol. 2014;28:88–97. doi: 10.1037/a0034998. [DOI] [PubMed] [Google Scholar]
- 81.Costello EJ, Erkanli A, Copeland W, Angold A. Association of family income supplements in adolescence with development of psychiatric and substance use disorders in adulthood among an American Indian population. JAMA. 2010;303:1954–60. doi: 10.1001/jama.2010.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Courtin E, Muennig P, Verma N, et al. Conditional cash transfers and health of low-income families in the US: evaluating the family rewards experiment. Health Aff (Millwood) 2018;37:438–46. doi: 10.1377/hlthaff.2017.1271. [DOI] [PubMed] [Google Scholar]
- 83.Daley A. Income and the mental health of Canadian mothers: evidence from the Universal Child Care Benefit. SSM Popul Health. 2017;3:674–83. doi: 10.1016/j.ssmph.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dang H-AH, Lokshin MM, Abanokova K. Did the poor adapt to their circumstances? Evidence from long-run Russian panel data. Econ Bull. 2019;39:2258–74. [Google Scholar]
- 85.Dearing E, Taylor BA, McCartney K. Implications of family income dynamics for women’s depressive symptoms during the first 3 years after childbirth. Am J Public Health. 2004;94:1372–77. doi: 10.2105/ajph.94.8.1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Diener E, Sandvik E, Seidlitz L, Diener M. The relationship between income and subjective well-being-relative or absolute. Soc Indic Res. 1993;28:195–223. [Google Scholar]
- 87.Dolan P, Lordan G. Moving up and sliding down: an empirical assessment of the effect of social mobility on subjective wellbeing. 2013. [accessed Dec 2, 2021]. https://cep.lse.ac.uk/pubs/download/dp1190.pdf .
- 88.Dorsett R, Oswald AJ. Human well-being and in-work benefits:a randomized controlled trial. 2014. [accessed Dec 2, 2021]. https://warwick.ac.uk/fac/soc/economics/research/centres/cage/manage/publications/182-2014_oswald.pdf .
- 89.Elwell-Sutton T, Folb N, Clark A, Fairall LR, Lund C, Bachmann MO. Socioeconomic position and depression in South African adults with long-term health conditions: a longitudinal study of causal pathways. Epidemiol Psychiatr Sci. 2019;28:199–209. doi: 10.1017/S2045796017000427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Erixson O. Health responses to a wealth shock: evidence from a Swedish tax reform. J Popul Econ. 2017;30:1281–336. [Google Scholar]
- 91.Evans S, Huxley P. Adaptation, response-shift and quality of life ratings in mentally well and unwell groups. Qual Life Res. 2005;14:1719–32. doi: 10.1007/s11136-005-1742-1. [DOI] [PubMed] [Google Scholar]
- 92.Evans WN, Garthwaite CL. Giving mom a break: the impact of higher EITc payments on maternal health. 2010. [accessed Dec 2, 2021]. https://www.nber.org/system/files/working_papers/w16296/w16296.pdf .
- 93.Fang Z, Niimi Y. Do losses bite more than gains? Evidence from a panel quantile regression analysis of subjective well-being in Japan. 2015. [accessed Dec 2, 2021]. http://www.agi.or.jp/workingpapers/WP2015-18.pdf .
- 94.Feeny S, McDonald L, Posso A. Are poor people less happy? Findings from Melanesia. World Dev. 2014;64:448–59. [Google Scholar]
- 95.Fenn B, Noura G, Sibson V, Dolan C, Shoham J. The role of unconditional cash transfers during a nutritional emergency in Maradi region, Niger: a pre-post intervention observational study. Public Health Nutr. 2015;18:343–51. doi: 10.1017/S1368980014000378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fernald LC, Hidrobo M. Effect of Ecuador’s cash transfer program (Bono de Desarrollo Humano) on child development in infants and toddlers: a randomized effectiveness trial. Soc Sci Med. 2011;72:1437–46. doi: 10.1016/j.socscimed.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 97.Frijters P, Johnston DW, Shields MA. Life satisfaction dynamics with quarterly life event data. Scand J Econ. 2011;113:190–211. [Google Scholar]
- 98.Frijters P, Johnston DW, Shields MA. The optimality of tax transfers: what does life satisfaction data tell us? J Happiness Stud. 2012;13:821–32. [Google Scholar]
- 99.Galama TJ, Morgan R, Saavedra JE. Wealthier, happier and more self-sufficient: when anti-poverty programs improve economic and subjective wellbeing at a reduced cost to taxpayers. 2017. [accessed Dec 2, 2021]. https://www.nber.org/system/files/working_papers/w24090/w24090.pdf .
- 100.Gassman-Pines A, Yoshikawa H. Five-year effects of an anti-poverty program on marriage among never-married mothers. J Policy Anal Manage. 2006;25:11–30. [Google Scholar]
- 101.Gennetian LA, Miller C. Children and welfare reform: a view from an experimental welfare program in Minnesota. Child Dev. 2002;73:601–20. doi: 10.1111/1467-8624.00426. [DOI] [PubMed] [Google Scholar]
- 102.Grattan LM, Brumback B, Roberts SM, Buckingham-Howes S, Toben AC, Morris G. “Bouncing back” after the Deepwater Horizon oil spill. Disaster Prev Manag. 2017;26:122–33. [Google Scholar]
- 103.Green EP, Blattman C, Jamison J, Annan J. Does poverty alleviation decrease depression symptoms in post-conflict settings? A cluster-randomized trial of microenterprise assistance in northern Uganda. Glob Ment Health (Camb) 2016;3:e7. doi: 10.1017/gmh.2015.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gros C, Bailey M, Schwager S, et al. Household-level effects of providing forecast-based cash in anticipation of extreme weather events: quasi-experimental evidence from humanitarian interventions in the 2017 floods in Bangladesh. Int J Disaster Risk Reduct. 2019;41:101275 [Google Scholar]
- 105.Gulal F, Ayaita A. The impact of minimum wages on well-being: evidence from a quasi-experiment in Germany. J Happiness Stud. 2019;21:2669–92. [Google Scholar]
- 106.Handa S, Park M, Darko RO, Osei-Akoto I, Davis B, Daidone S. Carolina Population Center. University of North Carolina; Chapel Hill, NC: 2014. Livelihood empowerment against poverty program impact evaluation. [Google Scholar]
- 107.Hanly P, Maguire R, Hyland P, Sharp L. Examining the role of subjective and objective burden in carer health-related quality of life: the case of colorectal cancer. Support Care Cancer. 2015;23:1941–49. doi: 10.1007/s00520-014-2551-2. [DOI] [PubMed] [Google Scholar]
- 108.Hasan H. Does happiness adapt to increase in income? Evidence from Pakistan socio-economic survey (1998-2001) Pak Dev Rev. 2016;55:113–22. [Google Scholar]
- 109.Haushofer J, Shapiro J. The short-term impact of unconditional cash transfers to the poor: experimental evidence from Kenya. Q J Econ. 2016;131:1973–2042. doi: 10.1093/qje/qjw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hilton JM, Kopera-Frye K. Loss and depression in cohabiting and noncohabiting custodial single parents. Fam J (Alex Va) 2006;14:28–40. [Google Scholar]
- 111.Hjelm L, Handa S, de Hoop J, Palermo T. Poverty and perceived stress: evidence from two unconditional cash transfer programs in Zambia. Soc Sci Med. 2017;177:110–17. doi: 10.1016/j.socscimed.2017.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Horn BP, Maclean JC, Strain MRDO. Minimum wage increases influence worker health? Econ Inq. 2017;55:1986–2007. [Google Scholar]
- 113.Huang Y, Wong H, Tan NT. Associations between economic loss, financial strain and the psychological status of Wenchuan earthquake survivors. Disasters. 2015;39:795–810. doi: 10.1111/disa.12126. [DOI] [PubMed] [Google Scholar]
- 114.Ishiguro A, Inoue M, Fisher J, Inoue M, Matsumoto S, Yamaoka K. Gender-based risk and protective factors for psychological distress in the midterm recovery period following the Great East Japan Earthquake. Disaster Med Public Health Prep. 2019;13:487–96. doi: 10.1017/dmp.2018.80. [DOI] [PubMed] [Google Scholar]
- 115.Jalal CS, Frongillo EA, Warren AM. Food insecurity mediates the effect of a poverty-alleviation program on psychosocial health among the ultra-poor in Bangladesh. J Nutr. 2015;145:1934–41. doi: 10.3945/jn.115.210799. [DOI] [PubMed] [Google Scholar]
- 116.Junna L, Moustgaard H, Tarkiainen L, Martikainen P. The association between income and psychotropic drug purchases: individual fixed effects analysis of annual longitudinal data in 2003-2013. Epidemiology. 2019;30:221–29. doi: 10.1097/EDE.0000000000000956. [DOI] [PubMed] [Google Scholar]
- 117.Kendall GE, Nguyen H, Ong R. The association between income, wealth, economic security perception, and health: a longitudinal Australian study. Health Sociol Rev. 2019;28:20–38. [Google Scholar]
- 118.Kiernan F. The Great Recession and mental health: the effect of income loss on the psychological health of young mothers. 2018. [accessed Dec 2, 2021]. https://www.ucd.ie/geary/static/publications/workingpapers/gearywp201821.pdf .
- 119.Kikuchi H, Mifune N, Niino M, et al. Structural equation modeling of factors contributing to quality of life in Japanese patients with multiple sclerosis. BMC Neurol. 2013 doi: 10.1186/1471-2377-13-10. published online Jan 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kilburn K, Handa S, Angeles G, Tsoka M, Mvula P. Paying for happiness: experimental results from a large cash transfer program in Malawi. J Policy Anal Manage. 2018;37:331–56. doi: 10.1002/pam.22044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kilburn K, Thirumurthy H, Halpern CT, Pettifor A, Handa S. Effects of a large-scale unconditional cash transfer program on mental health outcomes of young people in Kenya. J Adolesc Health. 2016;58:223–29. doi: 10.1016/j.jadohealth.2015.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Klein J, Lüdecke D, Hofreuter-Gätgens K, Fisch M, Graefen M, von dem Knesebeck O. Income and health-related quality of life among prostate cancer patients over a one-year period after radical prostatectomy: a linear mixed model analysis. Qual Life Res. 2017;26:2363–73. doi: 10.1007/s11136-017-1582-9. [DOI] [PubMed] [Google Scholar]
- 123.Koltai J, Bierman A, Schieman S. Financial circumstances, mastery, and mental health: taking unobserved time-stable influences into account. Soc Sci Med. 2018;202:108–16. doi: 10.1016/j.socscimed.2018.01.019. [DOI] [PubMed] [Google Scholar]
- 124.Krauss A, Graham C. Subjective wellbeing in Colombia: some insights on vulnerability, job security, and relative incomes. 2013. [accessed Dec 2, 2021]. https://openknowledge.worldbank.org/bitstream/handle/10986/16887/WPS6672.pdf .
- 125.Kuhn P, Kooreman P, Soetevent A, Kapteyn A. The effects of lottery prizes on winners and their neighbors: evidence from the Dutch postcode lottery. Am Econ Rev. 2011;101:2226–47. [Google Scholar]
- 126.Lachowska M. The effect of income on subjective well-being evidence from the 2008 economic stimulus tax rebates. J Hum Resour. 2017;52:37–17. [Google Scholar]
- 127.Lafave HG, de Souza HR, Prince PN, Atchison KE, Gerber GJ. Partnerships for people with serious mental illness who live below the poverty line. Psychiatr Serv. 1995;46:1071–73. doi: 10.1176/ps.46.10.1071. [DOI] [PubMed] [Google Scholar]
- 128.Lam JA, Rosenheck RA. Correlates of improvement in quality of life among homeless persons with serious mental illness. Psychiatr Serv. 2000;51:116–18. doi: 10.1176/ps.51.1.116. [DOI] [PubMed] [Google Scholar]
- 129.Latif E. Happiness adaptation to income: evidence from Canada. Econ Bull. 2015;35:1477–87. [Google Scholar]
- 130.Lebihan L, Mao Takongmo C-O. The impact of universal child benefits on family health and behaviours. Res Econ. 2018;72:415–27. [Google Scholar]
- 131.Lindahl M. Estimating the effect of income on health and mortality using lottery prizes as an exogenous source of variation in income. J Hum Resour. 2005;40:144–68. [Google Scholar]
- 132.Lorant V, Croux C, Weich S, Deliège D, Mackenbach J, Ansseau M. Depression and socio-economic risk factors: 7-year longitudinal population study. Br J Psychiatry. 2007;190:293–98. doi: 10.1192/bjp.bp.105.020040. [DOI] [PubMed] [Google Scholar]
- 133.Lorenz FO, Elder GH, Jr, Bao WN, Wickrama KAS, Conger RD. After farming: emotional health trajectories of farm, nonfarm, and displaced farm couples. Rural Sociol. 2000;65:50–71. [Google Scholar]
- 134.Macours K, Schady N, Vakis R. Cash transfers, behavioral changes, and cognitive development in early childhood: evidence from a randomized experiment. Am Econ J Appl Econ. 2012;4:247–73. [Google Scholar]
- 135.Maeder M. Earnings-related parental leave benefits and subjective well-being of young mothers: evidence from a German parental leave reform: Bavarian Graduate Program in Economics. 2014. [accessed Dec 2, 2021]. https://www.bgpe.de/texte/DP/148_Maeder.pdf .
- 136.Markussen T, Ngo Q-T. Economic and non-economic returns to communist party membership in Vietnam. World Dev. 2019;122:370–84. [Google Scholar]
- 137.McCarthy B, Carter A, Jansson M, Benoit C, Finnigan R. Poverty, material hardship, and mental health among workers in three frontline service occupations. J Poverty. 2018;22:334–54. [Google Scholar]
- 138.McKenzie SK, Imlach Gunasekara F, Richardson K, Carter K. Do changes in socioeconomic factors lead to changes in mental health? Findings from three waves of a population based panel study. J Epidemiol Community Health. 2014;68:253–60. doi: 10.1136/jech-2013-203013. [DOI] [PubMed] [Google Scholar]
- 139.Melzer SM, Muffels RJ. Migrants’ pursuit of happiness: an analysis of the effects of adaptation, social comparison and economic integration on subjective well-being on the basis of German panel data for 1990-2014. Migr Stud. 2017;5:190–215. [Google Scholar]
- 140.Milligan K, Stabile M. Do child tax benefits affect the wellbeing of children? Evidence from Canadian Child Benefit Expansions. 2008. [accessed Dec 2, 2021]. https://www.nber.org/system/files/working_papers/w14624/w14624.pdf .
- 141.Mohanty MS. What determines happiness? Income or attitude: evidence from the U.S. longitudinal data. J Neuroscience Psychology Econ. 2014;7:80–102. [Google Scholar]
- 142.Natali L, Handa S, Peterman A, Seidenfeld D, Tembo G. Does money buy happiness? Evidence from an unconditional cash transfer in Zambia. SSM Popul Health. 2018;4:225–35. doi: 10.1016/j.ssmph.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.North RJ, Holahan CJ, Moos RH, Cronkite RC. Family support, family income, and happiness: a 10-year perspective. J Fam Psychol. 2008;22:475–83. doi: 10.1037/0893-3200.22.3.475. [DOI] [PubMed] [Google Scholar]
- 144.Ong R, Nguyen T, Kendall G. The impact of intergenerational financial transfers on health and wellbeing outcomes: a longitudinal study. Soc Sci Med. 2018;214:179–86. doi: 10.1016/j.socscimed.2018.08.028. [DOI] [PubMed] [Google Scholar]
- 145.Oshio T, Umeda M, Fujii M. The association between income dynamics and subjective well-being: evidence from career income records in Japan. 2012. [accessed Dec 2, 2021]. https://www.nber.org/system/files/working_papers/w14624/w14624.pdf .
- 146.Ozer EJ, Fernald LCH, Weber A, Flynn EP, VanderWeele TJ. Does alleviating poverty affect mothers’ depressive symptoms? A quasi-experimental investigation of Mexico’s Oportunidades programme. Int J Epidemiol. 2011;40:1565–76. doi: 10.1093/ije/dyr103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Plagerson S, Patel V, Harpham T, Kielmann K, Mathee A. Does money matter for mental health? Evidence from the Child Support Grants in Johannesburg, South Africa. Glob Public Health. 2011;6:760–76. doi: 10.1080/17441692.2010.516267. [DOI] [PubMed] [Google Scholar]
- 148.Powell-Jackson T, Pereira SK, Dutt V, Tougher S, Haldar K, Kumar P. Cash transfers, maternal depression and emotional wellbeing: quasi-experimental evidence from India’s Janani Suraksha Yojana programme. Soc Sci Med. 2016;162:210–18. doi: 10.1016/j.socscimed.2016.06.034. [DOI] [PubMed] [Google Scholar]
- 149.Priebe S, Yeeles K, Bremner S, et al. Effectiveness of financial incentives to improve adherence to maintenance treatment with antipsychotics: cluster randomised controlled trial. BMJ. 2013;347:f5847. doi: 10.1136/bmj.f5847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Proto E, Rustichini A. Life satisfaction, income and personality. J Econ Psychol. 2015;48:17–32. [Google Scholar]
- 151.Radey M, McWey L, Cui M. Psychological distress among low-income mothers: the role of public and private safety nets. Women Health. 2020;60:692–706. doi: 10.1080/03630242.2019.1700586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Raschke C. Unexpected windfalls, education, and mental health: evidence from lottery winners in Germany. Appl Econ. 2019;51:207–18. [Google Scholar]
- 153.Reeve J, James F, McNeill R, Brown P, Cameron L, Mills S. Functional and psychological outcomes following burn injury: reduced income and hidden emotions are predictors of greater distress. J Burn Care Res. 2011;32:468–74. doi: 10.1097/BCR.0b013e3182223c46. [DOI] [PubMed] [Google Scholar]
- 154.Reeves A, Clair A, McKee M, Stuckler D. Reductions in the United Kingdom’s government housing benefit and symptoms of depression in low-income households. Am J Epidemiol. 2016;184:421–29. doi: 10.1093/aje/kww055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Reeves A, McKee M, Mackenbach J, Whitehead M, Stuckler D. Introduction of a national minimum wage reduced depressive symptoms in low-wage workers: a quasi-natural experiment in the UK. Health Econ. 2017;26:639–55. doi: 10.1002/hec.3336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Robert G, Martinez JM, García AM, Benavides FG, Ronda E. From the boom to the crisis: changes in employment conditions of immigrants in Spain and their effects on mental health. Eur J Public Health. 2014;24:404–09. doi: 10.1093/eurpub/cku020. [DOI] [PubMed] [Google Scholar]
- 157.Rogers SJ, DeBoer DD. Changes in wives’ income: effects on marital happiness, psychological well-being, and the risk of divorce. J Marriage Fam. 2001;63:458–72. [Google Scholar]
- 158.Roh YH, Chang JY, Kim MU, Nam SK. The effects of income and skill utilization on the underemployed’s self-esteem, mental health, and life satisfaction. J Employ Couns. 2014;51:125–41. [Google Scholar]
- 159.Rosenheck RA, Dausey DJ, Frisman L, Kasprow W. Outcomes after initial receipt of social security benefits among homeless veterans with mental illness. Psychiatr Serv. 2000;51:1549–54. doi: 10.1176/appi.ps.51.12.1549. [DOI] [PubMed] [Google Scholar]
- 160.Sareen J, Afifi TO, McMillan KA, Asmundson GJ. Relationship between household income and mental disorders: findings from a population-based longitudinal study. Arch Gen Psychiatry. 2011;68:419–27. doi: 10.1001/archgenpsychiatry.2011.15. [DOI] [PubMed] [Google Scholar]
- 161.Schöllgen I, Kersten N, Rose U. Income trajectories and subjective well-being: linking administrative records and survey data. Int J Environ Res Public Health. 2019;16:e4779. doi: 10.3390/ijerph16234779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Schyns P. Income and satisfaction in Russia. J Happiness Stud. 2001;2:173–204. [Google Scholar]
- 163.Sekulova F, van den Bergh J. Climate change, income and happiness: an empirical study for Barcelona. Glob Environ Change. 2013;23:1467–75. [Google Scholar]
- 164.Swift SL, Elfassy T, Bailey Z, et al. Association of negative financial shocks during the Great Recession with depressive symptoms and substance use in the USA: the CARDIA study. J Epidemiol Community Health. 2020;74:995–1001. doi: 10.1136/jech-2020-213917. [DOI] [PubMed] [Google Scholar]
- 165.Tachibana T, Goto R, Sakurai T, Rayamajhi S, Adhikari A, Dow WH. Do remittances alleviate negative impacts of disaster on mental health? A case of the 2015 Nepal earthquake. Soc Sci Med. 2019;238:112460. doi: 10.1016/j.socscimed.2019.112460. [DOI] [PubMed] [Google Scholar]
- 166.Thoits P, Hannan M. Income and psychological distress: the impact of an income-maintenance experiment. J Health Soc Behav. 1979;20:120–38. [PubMed] [Google Scholar]
- 167.Thompson S, Hartel G, Manderson L, Woelz-Stirling N, Kelaher M. The mental health status of Filipinas in Queensland. Aust N Z J Psychiatry. 2002;36:674–80. doi: 10.1046/j.1440-1614.2002.01070.x. [DOI] [PubMed] [Google Scholar]
- 168.Turvey C, Stromquist A, Kelly K, Zwerling C, Merchant J. Financial loss and suicidal ideation in a rural community sample. Acta Psychiatr Scand. 2002;106:373–80. doi: 10.1034/j.1600-0447.2002.02340.x. [DOI] [PubMed] [Google Scholar]
- 169.Wickham S, Whitehead M, Taylor-Robinson D, Barr B. The effect of a transition into poverty on child and maternal mental health:a longitudinal analysis of the UK Millennium Cohort Study. Lancet Public Health. 2017;2:e141–48. doi: 10.1016/S2468-2667(17)30011-7. [DOI] [PubMed] [Google Scholar]
- 170.Wong H, Ye S. Impact of enforcing a statutory minimum wage on work and quality of life of vulnerable groups in Hong Kong. Int J Soc Welf. 2015;24:223–35. [Google Scholar]
- 171.Yun YH, Rhee YS, Kang IO, et al. Economic burdens and quality of life of family caregivers of cancer patients. Oncology. 2005;68:107–14. doi: 10.1159/000085703. [DOI] [PubMed] [Google Scholar]
- 172.Zimmerman FJ, Katon W. Socioeconomic status, depression disparities, and financial strain: what lies behind the incomedepression relationship? Health Econ. 2005;14:1197–215. doi: 10.1002/hec.1011. [DOI] [PubMed] [Google Scholar]
- 173.Kahneman D, Krueger AB. Developments in the measurement of subjective well-being. J Econ Perspect. 2006;20:3–24. [Google Scholar]
- 174.Ruggeri K, Garcia-Garzon E, Maguire Á, Matz S, Huppert FA. Well-being is more than happiness and life satisfaction:a multidimensional analysis of 21 countries. Health Qual Life Outcomes. 2020;18:192. doi: 10.1186/s12955-020-01423-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kromydas T, Thomson RM, Pulford A, Green MJ, Katikireddi SV. Which is most important for mental health: money, poverty, or paid work? A fixed-effects analysis of the UK household longitudinal study. SSM Popul Health. 2021;15:100909. doi: 10.1016/j.ssmph.2021.100909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Craig P, Katikireddi SV, Leyland A, Popham F. Natural experiments: an overview of methods, approaches, and contributions to public health intervention research. Annu Rev Public Health. 2017;38:39–56. doi: 10.1146/annurev-publhealth-031816-044327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Matthay EC, Hagan E, Gottlieb LM, et al. Alternative causal inference methods in population health research: evaluating tradeoffs and triangulating evidence. SSM Popul Health. 2019;10:100526. doi: 10.1016/j.ssmph.2019.100526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391:1357–66. doi: 10.1016/S0140-6736(17)32802-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Cuijpers P, Berking M, Andersson G, Quigley L, Kleiboer A, Dobson KS. A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Can J Psychiatry. 2013;58:376–85. doi: 10.1177/070674371305800702. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The study protocol is published on PROSPERO. All extracted data used for analysis and analytic code are available in a public GitHub repository. Template data forms and copies of the totality of data extracted from included studies are available from the corresponding author on reasonable request.