Abstract
The development of stimuli-responsive nanomedicines with tunable cargo release is gathering an increased applicability in bone regeneration and precision biomedicine. Yet, the formulation of nanocarriers that explore skeletal-specific stimuli remains remarkably challenging to materialize due to several endogenous and disease-specific barriers that must be considered during particle design stages. Such anatomo-physiological constrains ultimately hinder nanocarriers bioavailability in target bone tissues and impact the overall therapeutic outcome. This review aims to showcase and critically discuss the hurdles encountered upon responsive nanocarriers delivery in the context of skeletal diseases or tissue regeneration scenarios. Such focus is complemented with an in-depth and up-to-date analysis of advances in the development of stimuli-responsive, bone-focused delivery systems. In a holistic perspective, a deeper knowledge of human osteology combined with advances in materials functionalization via simple precision-chemistry is envisioned to incite the manufacture of stimuli-triggered nanomedicines with more realistic potential for clinical translation.
1. Introduction
The continuous improvement in humans life-expectancy in the past decades has contributed for an increased incidence of numerous skeletal diseases and age-related bone abnormalities such as osteoporosis, osteoarthritis, osteomyelitis or bone cancer [1]. Regardless of several decades of scientific and medical progress, still no definitive treatment options exist for any of these pathologies [2].
Currently available treatment options for such disorders rely mostly on pharmacological-based therapeutics that are administered under various regimes according to each individuals disease progression status [3]. Despite their recognizable therapeutic benefits, these approaches are still undermined by deleterious side effects that affect patients general health and daily quality of life. This issue is clearly evident for various therapies that are currently employed in the clinics [4]. For example, the administration of FDA-approved recombinant parathyroid hormone (PTH) is limited to severe cases of osteoporosis and for a maximum period of 2 years, owing to the increased risk of developing osteosarcoma as a side effect [5]. Likewise, the oral administration of antiresorptive bisphosphonates has been reported to induce gastric ulcer and osteonecrosis of the jaw [6,7]. In the case of bone diseases that require immediate treatment such as osteosarcoma, the access of systemically administered pharmaceutics to the tumor is also physically hindered due to the existence of a denser osteoid. Such limitation adds on to the common side-effects underlying chemotherapeutics systemic administration [8].
The challenge of administering bioactive molecules to diseased bone tissues lies in attaining an optimal compromise between: (i) pharmacokinetic/pharmacodynamic (PK/PD) parameters, (ii) the administered dose, (iii) the existence of off-target side-effects (e.g., nephrotoxicity, cardiotoxicity, etc), (iv) the overall treatment efficacy and, more importantly, (v) the short or long-term therapeutic outcome.
To overcome such issues, the development of advanced nanosized carriers formulated for delivery of bone therapeutics via different administration routes has been extensively explored in the past decade [9–12]. Such nanocarriers have so far been engineered to modify drugs pharmacokinetics to improve their local concentration, whilst reducing unspecific tissue partitioning. Ensuing nanoformulated bone therapeutics bioavailability following minimally intravenous administration is a crucial parameter to address during pre-clinical design stages, especially considering that some bone sections are poorly perfused and that its highly hierarchic structure naturally restricts particles access [13]. Numerous in vitro and in vivo studies highlight the potential of nanocarriers for delivery of bioactive molecules to treat different bone disorders, but so far, very few have managed to actually reach clinical trials. One example is the Phase II trial (NCT03140657 – currently at recruitment stage), which aims to evaluate the use of nanoformulated curcumin for the treatment of patients diagnosed with Ankylosing spondylitis. Other interesting clinical trial focusing on bone regeneration was recently completed in China Medical Hospital (NCT01323894). This study involved the use of stem cells transfected with hydroxyapatite-based nanoparticles as a strategy to improve human mesenchymal/stromal stem cells (hMSCs) osteoblastogenesis. It is important to highlight that both trials employ pristine nanoparticles with no specific selectivity for bone tissue or bone tissue progenitor cells. In fact, as the knowledge on the complexity of bone disease/remodeling dynamics deepens, there is an ever-increasing notion that simply relying on increased drug accumulation in bone tissues and passive diffusion from nanocarriers may not be enough to achieve a selective and clinically significant therapeutic effect [14,15].
The functionalization of nanocarriers with bone targeting moieties is particularly valuable for improving accumulation in bone-specific cells or in dynamic bone disease scenarios. Among the different molecules explored to date, bisphosphonates, aptamers and peptides (e.g., aspartate-based oligopeptides), have been the most used to functionalize nanocarriers surface and endow them with bone-targeting properties [16–18]. Interestingly, some of these peptides are capable of minimizing particle aggregation in biological media, while others possess inherent osteogenic properties [17,19]. The latter could be interesting to formulate bone nanotherapeutics that take advantage of drug-peptide combination therapies as means to achieve a synergistic osteo-regenerative effect.
Apart from the desirable increase in nanomedicines bone selectivity, the controlled release of therapeutics is also a major aspect that is yet to be fully controlled in vivo.
Stimuli-responsive nanocarriers have been investigated in the last years as an approach to circumvent the characteristic burst-type release profile of nano-formulated therapeutics or the residual release during parenteral administration. To achieve this control, these so-termed smart delivery systems, can be precisely tailored to respond to internal, external, or physiological triggering conditions as means to promote a fine tuning of bioactive molecules release [20]. Specifically, stimuli-responsive nanocarriers have been engineered to respond to triggers such as: (i) pH gradients, (ii) redox conditions; (iii) light; (iv) ultrasound (v) magnetic fields; (vi) temperature or (vii) enzymes [20]. The majority of these have significant potential to be used in the context of bone regeneration or skeletal diseases. In fact, the progression of some chronic bone disorders is characterized by changes in the biological microenvironment, resulting in pathophysiological-induced shifts (e.g., pH, enzymes, temperature) that can activate nanotherapeutics release.
From this standpoint, this review aims to showcase state-of-the-art stimuli-responsive nanocarriers applied in bone-related therapies, as well as their unique designs and properties. The different biological barriers encountered during nanosized particles systemic delivery is also addressed in a disease-specific mode as this should be a determinant factor during pre-clinical design and testing stages. As an overarching concept the loading of osteo-regenerative/resorptive drugs or bone chemotherapeutics within nanocarriers, combined with the inclusion of sensitive stimuli-responsive linkages should enhance their efficacy while minimizing off-target cytotoxic effects.
2. Biological barriers to nanocarrier-mediated delivery of bone therapeutics
Upon parenteral administration, the accumulation of pristine or targeted stimuli-responsive delivery systems in bone is hindered by its unique anatomic structure. In essence, mature bone is a complex calcified tissue primarily composed of: 50-70 % mineral hydroxyapatite (HA), 20 - 40 % collagen matrix, 5-10 % water and 1-5 % lipidic contents [14]. Hierarchically, it consists of: (i) cortical bone, a compact shell with rapid tissue turnover that is comprised of well-aligned Haversian systems, also termed Osteons, which run in parallel along the structure, and (ii) cancellous (trabecular) bone, a highly porous core that consists of an intertwined microarchitecture with bone marrow-filled free spaces. Both these structures represent 80 % and 20 % of total bone mass, respectively [21–23]. The Osteon is particularly interesting as it harbors nerves and arterial/venous blood vessels. In this system, Haversian canals run longitudinally and Volkmann canals branch out radially, endowing the entire osteon with an intricate vascular network [24]. The osteon is also comprised by concentric lamellae with embedded osteocytes, interconnected through canaliculi channels with approximately 100 - 300 nm in diameter [25,26]. From a therapeutic perspective, such may be an important size threshold for successful delivery of nanomedicines to osteocyte cells in different disease scenarios.
Since bone is a highly complex and dynamic tissue from both an anatomical and physiological level, the question arises as how are nanoparticles capable of accumulating within the bone matrix and be internalized in deregulated bone cells.
Recently, several reports have been detailing nanocarriers in vivo fate and focusing on major biological barriers or tissue accumulation issues encountered upon parenteral administration [27][28,29]. However, the barriers encountered upon particles intravenous administration and during accumulation in bone tissues have been poorly described so far. Such is evident both in the context of non-malignant bone diseases and in bone regeneration scenarios. Having a fundamental knowledge about skeletal anatomo-physiological barriers is paramount to design more effective bone-specific nanotherapeutics.
There are several biological barriers that may hinder nanocarriers delivery via systemic route to different tissues including bone. In an overview, following intravenous injection, nanotherapeutics must first travel in the bloodstream for sufficient time to promote accumulation in bones, either by probabilistic passive accumulation, or by active targeting to cell-specific moieties. The latter could be achieved by designing nanocarriers targeted to specific bone cell receptors such as Periostin, or neighboring extracellular matrix components (reviewed in detail elsewhere [4,30,31]). To achieve sufficient circulation time for accumulation in the desired tissues, nanocarriers must also be formulated to avoid opsonisation and sequestration by the components of the reticuloendothelial system (RES) including phagocytic cells of the liver (e.g., Kupffer cells), spleen (e.g., Splenocytes), as well as kidney excretion (< ~5 nm) (reviewed in detail in [27]).
Once in the vicinity of skeletal tissues, nanocarriers are transported by the nutrient arteries that penetrate the bone cortex and give rise to cortical capillaries that connect to the medullar vascular capillaries. These capillaries form a dense blood network inside the bone marrow. While vessels in cortical bone are characterized by a continuous lining of endothelial cells with no phago-endocytic activity, the microvascular bed in bone marrow sinusoids possesses phago-endocytic activity and several intercellular gaps often appearing to have an incomplete basement membrane [24,32].
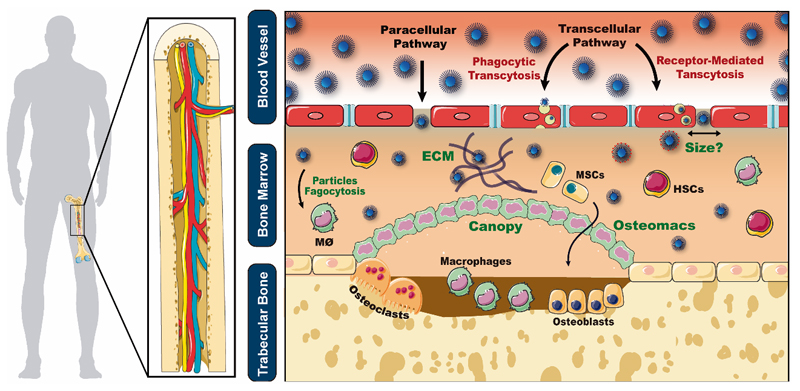
Upon reaching the bone marrow vessels, nanocarriers can then transverse it by extravasating either via (i) intercellular gaps (paracellular pathway), or (ii) by phago-endocytic uptake throughout the endothelium (transcellular pathway) [33] (Figure 1).
Figure 1.
Schematics of nanocarriers biological barriers and routes of extravasation from the sinusoidal vasculature into the extravascular space. Green text represents major barriers to nanocarrier delivery to bone cells (bone marrow ECM, macrophage-mediated phagocytosis, unknown fenestration size, bone canopy and its osteomacs - generally present in bone remodeling/regeneration stages).
In general, the mechanisms of accumulation across the marrow-blood vessel barrier have been poorly explored so far and further insights on their influence in nanotherapeutics accumulation are necessary for improving their potential.
To better understand and explore nanoparticle accumulation in bone through the paracellular pathway two main aspects must be discussed. First, the existence of different types of gaps throughout the endothelium of bone marrow capillaries is unclear. In a detailed review performed by Sarin, the bone marrow endothelium is described as non-fenestrated, except when hematopoietic cells are traversing through it and creating transient openings [32]. The author suggests that the primary route of biomacromolecules transport to marrow interstitial space is via phago-endocytic uptake (molecules > 5 nm) and macula occludens inter-endothelial junctions (lipid-insoluble molecules ≤ 5 nm in diameter) [32]. Other reports define bone marrow capillaries as being discontinuous/sinusoidal, with large sinusoidal gaps between endothelium cells, but with no diaphragm [34]. Therefore, it seems that there is some ambiguity regarding the classification of this particular set of capillaries. Providing further insights on these structures could aid in the design of the next-generation of nanotherapeutics.
The presence of diaphragms and their role in the extravasation of nanoparticles via these intercellular spaces is also not yet clear. The possible presence of diaphragms in marrow fenestrae likely reduces flexibility/permeability and may further constrain therapeutics transport. In comparison with other preferential particle accumulation organs such as the liver, the boundaries of hepatic open fenestrae lack a considerable amount of glycocalyx matrix fibers rendering these fenestrae less restrictive [32]. It is unknown whether this pattern of glycocalyx is similar in marrow fenestrae [32]. Overall, the presence of the diaphragm in fenestrae and adjacent patterning of glycocalyx matrix fibers could play a role in delineating the physiologic upper limit of pore size and affect particles accumulation. The type of capillaries also varies between red (hematopoietic) and yellow (fatty) bone marrow. While vessels in red marrow are characterized by flat reticulum cells with many diaphragmed fenestrations and no basal membrane, in yellow bone marrow the vessels are closed and continuous, akin to those present in other tissues such as the muscle [35]. Interestingly, this may help explain the biodistribution pattern that Sou and co-workers observed after intravenous administration of bone marrow-specific liposomes (216 ± 21 nm) in non-human primates [36]. Besides achieving 70 % of the administered dose accumulated in the bone marrow, these researchers observed that liposomes biodistribution in rhesus monkeys was similar to that of the pattern of red marrow in humans. Because red marrow is highly irrigated with sinusoid capillaries, one can hypothesize that this reflects the importance of sinusoids in nanocarriers bone marrow accumulation.
The second aspect that must be considered in the paracellular accumulation pathway is the exact marrow fenestrae dimension in humans, particularly in non-malignant disease, since this is currently unknown to the best of our knowledge. The reported size fenestrae ranges in the literature are extrapolated from a multitude of studies performed only in animal models and should be updated with robust information from human studies. The existing differences in bone vascular microarchitecture between species may impact the analysis of the biological performance of nanocarriers and impair their successful clinical translation in the long run. In fact, there is a clear disparity between the organization of cortical vascularization in long bones among species, with rodents lacking well-developed Harvesian remodeling systems when compared to larger mammals [37]. This type of remodeling is a significant source of cortical porosity and age-related bone loss, being thus important for therapeutics delivery in aged individuals [37]. Also, rodent marrow and cortical vasculature are thought to be in series, contrasting with parallel vascular networks in humans [24]. In other species, such as rabbit and marmoset (but not humans), perisinal macrophages populate the marrow stroma adjacent to bone sinus endothelium, often extending cytoplasmic processes into the lumen and monitoring circulation [38]. These perisinal macrophages are an active component of the marrow-blood barrier and play a key role in the uptake of triglyceride-rich macromolecules.
It is important to emphasize that these vascular and cellular barriers are altered in bone-specific diseases including bone cancer/metastasis, inflammation or during bone remodeling/regeneration processes. In bone regeneration scenarios, after transposing blood vessels and entering the marrow stroma/extravascular space nanocarriers encounter a complex bone extracellular matrix that hinders diffusion (Figure 1, ECM). Adding to this, nanotherapeutics need to subsequently overcome phagocytosis by macrophages and avoid unspecific uptake by hematopoietic/mesenchymal stem cells. The latter is particularly important to minimize potential toxicities to the hematopoietic niche and could lead to the development of many disorders such as leukemia. In bone remodeling areas and regeneration scenarios nanocarriers also need to overcome osteomac-based cellular canopy isolating bone remodeling pockets from marrow compartments and get internalized for example by target osteoblasts (Figure 1, canopy) via the various cellular uptake pathways (reviewed in detail by Hillaireau and co-workers [39]). All these events depend on the dynamics of bone blood perfusion as it will be discussed.
2.1. Influence of bone physiological blood flow on nanocarriers accumulation
Skeletal perfusion is a fundamental parameter following nanocarriers parenteral administration and influences bone therapeutics accumulation dynamics. Interestingly, the values of blood flow vary significantly amongst different skeletal regions. For instance, trabecular bone experiences approximately 4-fold increased blood perfusion when compared to cortical bone [25]. This vascular diversity should result in different exposures to nanocarriers. Several pathological conditions have been associated with impaired blood flow and subsequent bone loss, such as osteonecrosis, postmenopausal-osteoporosis (in both women and ovariectomized mice) and glucocorticoid-induced osteoporosis, which may be linked with increased conversion of the more vascularized red marrow to yellow marrow [37,40,41]. The vessels in fatty bone marrow are closed and less vascularized than those of the red marrow [42], such can limit nanoparticle extravasation. Patients suffering from myelodysplastic syndromes also present an abnormal expansion of sinusoidal compartments. Nanotherapeutics could potentially benefit from facilitated access across the bone-marrow barrier in these scenarios akin to what is normally proposed by the enhanced permeability and retention (EPR) effect in cancer [43]. However, the latter should be addressed carefully as this phenomenon is quite variable from patient to patient and its true impact in therapeutics accumulation is yet to be fully elucidated in a clinical setting [44,45]. Strategies to augment the EPR through vascular modulators (e.g., nitric oxide, bradykinin [46]) have been investigated so far for cancer with some promising pre-clinical in vivo data [47]. To the best of our knowledge such has not been explored for other bone disorders that could benefit from this strategy. One can postulate that dynamic studies addressing this may provide important insights to increase the performance of disease-specific nanocarriers.
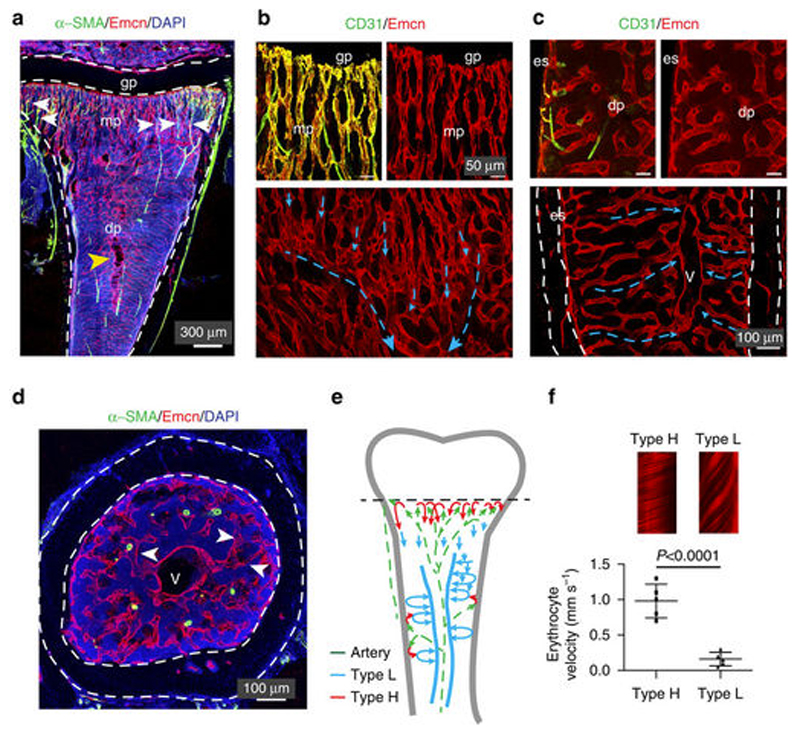
A recent study performed by Ramasamy and co-workers is one of the few that investigated the fundaments of blood flow dynamics in bone by using in vivo fluorescence intravital imaging. The reported results indicate that blood velocity in type H capillaries is about 6-fold higher than that of sinusoidal type L vessels (Figure 2) [41]. However, it is worth noting that this set of data pertains to 4-week-old mice tibial vasculature and thus could lead to importance differences in blood flow in more matured animals.
Figure 2.
Fluorescence microscopy imaging of 4-week-old tibial C57BL/6J mice vasculature. (A) Immunostaining of smooth muscle actin containing arteries (α-SMA positive cells, green channel), Endomucin (Emcn, red channel) and cell nuclei (DAPI, blue channel). mp- represents metaphyseal plate; gp- represents growth plate. White arrows indicate α-SMA cells connection to metaphyseal H-type vessels. (B, C) Confocal images proximal to the growth plate (b, top panel) or to diaphysis (c, top). CD31+ and Emcn-arteries terminate in type H vessels in metaphysis (CD31+ and Emcn+) and endosteum (es). No interaction with L-type vessels in diaphysis was observed. Blue arrows indicate blood flow from metaphyseal vessel columns (B) and endosteum (C), respectively. (D) Transversal tibial sections where sinusoidal L-type vessels (arrowheads) connect to the large central vein (v). Dashed lines represent compact bone. From these images, it is clear that CD31+ Emnc-arteries containing multiple smooth muscle cells cross the diaphysis. (E) Schematics of arterial (green arrows), H-type (red arrows) and sinusoidal/venous blood flow (blue arrows) of murin long bones. (F) Erythrocytes velocity data demonstrating the differences between type H and type L vessels. Adapted from [41] under Creative Commons Attribution 4.0 International License.
Considering that osteoporosis and aging diminish bone perfusion, associated with the reduction of type H capillaries, these aspects must be taken into consideration during particles pre-clinical design and investigation of optimal dose/treatment regime. Age-induced increase in vascular stiffness and calcification of muscle vessels has also shown to contribute to an impaired vascular function in humans [48]. Such is corroborated by ultrasound doppler data that indicates a 30 % lower femoral artery blood flow in aged human male patients (average of 64 years) in comparison with those of young men in their mid-twenties [49]. It is therefore clear that bone vascular complexity and the blood-marrow interface pose significant barriers for nanotherapeutics delivery. To overcome these barriers various particles physicochemical parameters should be optimized, including surface charge, shape and size. The latter is one of the most important aspects that needs to be considered to improve therapeutics pharmacokinetics and performance in the bone blood-marrow microenvironment.
2.2. Nanocarriers size-dependent bone accumulation
Regarding nanocarriers size-dependent bone accumulation there are some literature reports that suggest optimal bone delivery for nanocarriers under 80 nm, motivated by the detailed work of Howlett and co-workers on avian tibia microstructures [50]. It is important to emphasize that up-to-date there is a scarcity in human and non-human primate studies regarding this topic [50]. Considering the disparity between the physiological upper limit of pore size in human hepatic sinusoids (180 nm) versus rodents (280 nm), one could expect that bone microvasculature could also be slightly different across mammals [32]. In fact, differences between avian and mammalian erythropoiesis could convey important differences in the organization of the bone sinusoids traversing the marrow. In mammals erythropoiesis is extravascular, whereas in birds is intravascular and involves no marrow-blood barrier [51]. More studies on the ultrastructure of bone microvasculature across species are necessary to shed light into the optimal design of nanocarriers.
The size of rabbit bone marrow fenestrae was reported to range from 85 nm to 150 nm [52]. This is supported by the work of Porter and colleagues, that studied the accumulation of poloxamer 407-coated polystyrene particles (sizes of 60, 150 and 250 nm) in rabbit femoral bone marrow [53]. The obtained results indicate that nanoparticles with sizes of 150 nm and below, effectively avoided liver and spleen clearance and were predominantly located within bone marrow sinus endothelial cells after 24 h. Such was evident by the formation of dense bodies consisting of particle clusters. Importantly, in this study no evidence of transcytosis to the marrow extravascular space was observed [53]. However, it was also not clear if the 250 nm nanoparticles were not efficiently accumulated in bone due to size limitations of the nanocarrier or due to increased RES uptake in spleen and liver, as these particles had less density of stealth polymer coating when compared to smaller formulations. Bone marrow targeting by these poloxamer 407-coated nanoparticles is a phenomenon reportedly only in rabbit-based animal models [38]. This observation is not related to the exclusive perisinal macrophage population present in rabbit marrow, because the authors claimed that these macrophages were unable to interact with the poloxamer particles, perhaps due to the steric barrier provided by the hydrophilic moieties of poloxamer-407. Not only does this emphasizes the key role of nanocarrier composition in marrow uptake, but reinforces the differences between different animal models. Conversely, non-targeted liposomal formulations of several sizes (136-318 nm) were unable to significantly accumulate in rabbit bone marrow in a biodistribution study following intravenous administration [52]. Another study performed by Mann and colleagues exploited the unique expression of E-selectin in bone marrow endothelium by using nanoparticle-loaded, E-selectin functionalized, porous silica microcarriers administrated intravenously in mice [54]. Remarkably, the targeted microparticles (~1.6 µm) were capable of delivering paclitaxel-loaded nanoliposomes (25-35 nm) within bone marrow endothelium, as demonstrated by fluorescence microscopy analysis [54]. Some studies also suggest that nanocarrier dosage could play a role in bone marrow uptake. When administering liposomal dosages above 50 mg/kg in rabbits, the bone marrow appears to be the first tissue to become saturated, followed by increased uptake in the liver and spleen [52]. These reports further highlight the importance of fully characterizing nanocarriers surface chemistry and targeting moieties type and density; since these parameters play key roles in the outcomes of biodistribution studies [55,56]. Ideally, it is important to also evaluate nanocarriers protein ‘hard’ and ‘soft’ corona and its influence in in vivo particles targeting performance [34]. The sole functionalization of stimuli-responsive nanocarriers with osteotropic bone moieties may not confer bone selectivity if the bound protein corona temporarily or permanently shields these linkers, as it was already observed for transferrin-functionalized nanoparticles [57,58].
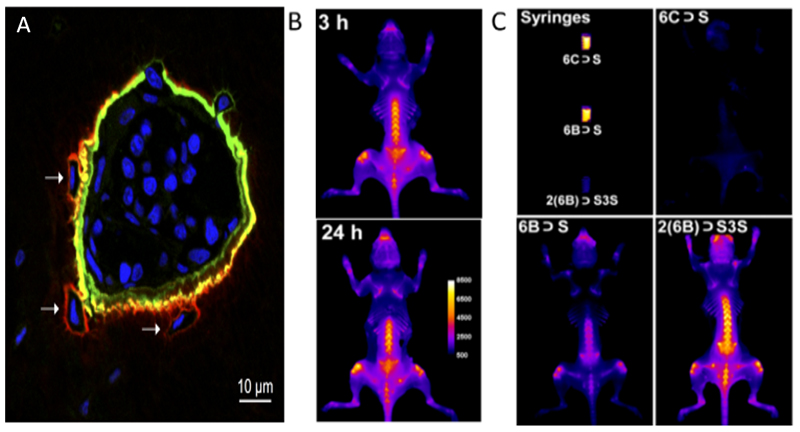
On this topic some emerging imaging technologies could prove useful in clarifying nanocarriers bone accumulation. Sun and his team developed a bone imaging toolkit containing several clinically relevant fluorescent probes, which could be useful for further investigation of bone physio-pharmacology (Figure 3A) [59]. Using a different strategy, Peck and colleagues exploited synthavidin technology to design highly biocompatible pre-assembled probes with affinity for high turnover living bone regions [60]. Notably this probe maintained high stability even after 24 h past administration (Figure 3B). The probe does suffer from squaraine self-quenching in aqueous solutions, but binding to bone surfaces inhibits this effect, an exciting observation that may be useful in the future for improving signal/noise ratio (Figure 3C).
Figure 3.
Advanced bone imaging technologies. (A) Pocket of bone marrow surrounded by fluorescently labelled bone matrix (red - low HA affinity probe; green - high HA affinity probe) with DAPI (blue) stained nuclei. Adapted from [59] with permission from the American Chemical Society. (B) Evidence of probe high stability on living mice skeleton. (C) Fluorescence enhancement caused by probe unfolding when binding to bone. Adapted from [60] with permission from the American Chemical Society.
The advances in disease-specific imaging and cell tracking techniques in bone tissues are expected to contribute for a more robust pre-clinical validation of nanotherapeutics. These techniques will be particularly valuable to follow the release of drugs and biomacromolecules from stimuli-responsive nanocarriers in complex in vivo environments. Such follow-up remains a challenging aspect in the assessment of smart delivery systems biological performance. In the following section, we will present and discuss up-to-date reports on stimuli-sensitive nanocarriers that exploit different stimuli in an attempt to achieve a therapeutically relevant release of bioactive molecules.
3. Stimuli-responsive Nanocarriers for the delivery of Bioactive Molecules to Bone Tissues
Bone is one of the most dynamic tissues being in constant adsorption/remodeling during lifetime. Naturally, a myriad of biomolecular cues and hotspot microenvironments render bone an interesting organ in which to explore stimuli-responsive delivery at both homeostatic or pathological scenarios. The latter is particularly interesting since during the onset and progression of different bone disorders many of skeletal microenvironment hallmarks and cellular functions become profoundly deregulated. Each of these disease-specific features represent unique barriers, but also unique opportunities for nanocarrier-mediated stimuli-responsive release of therapeutics. To date several types of non-responsive nanocarriers have been explored for bone therapeutics delivery, reviewed in detail elsewhere [30]. Yet, the majority is unable to achieve a realistic spatiotemporally controlled release of their payload at the target site. This is observed for various types of cargo including small molecule drugs, nucleic acids or proteins (e.g., bone morphogenetic proteins).
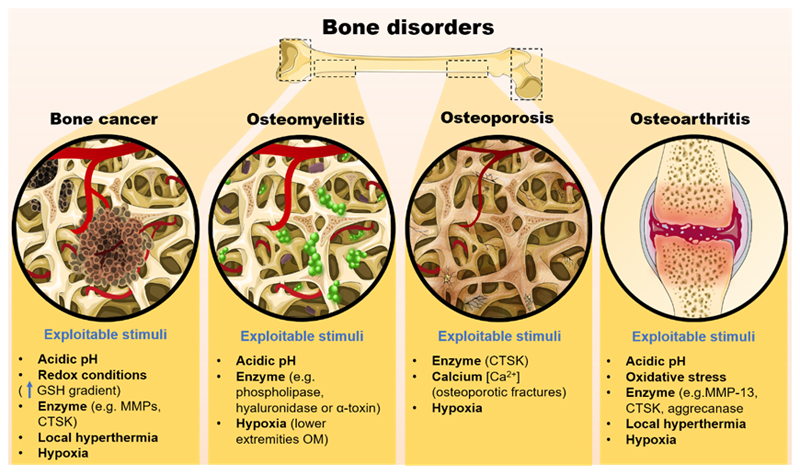
In general, there are several interesting biological characteristics within bone tissues and alterations found in different skeletal pathologies that can be exploited for stimuli-responsive delivery of bone therapeutics (Figure 4).
Figure 4.
Schematics of different stimuli that can be explored to promote the release of therapeutics from nanocarriers engineered for different bone-specific disorders.
In the context of bone regeneration scenarios, the existence of specific enzymes involved in the bone remodeling process, such as cathepsin K, certain matrix metalloproteinases (e.g., MMPs -2, -9, -13, -14 and -16), vacuolar H+ ATPase (an osteoclastic enzyme that contains a unique 116-kD subunit which may also be exploited for specific targeting), are valuable triggers to be exploited. Tartrate-resistant acid phosphatase (TRAP), normally present within the bone milieu is also an interesting endogenous target for stimuli-responsive delivery [1,61,62].
On the other hand, certain bone disorders are characterized by specific biological modifications in the bone vicinity that could trigger cargo release. For example, an hallmark of osteomyelitis is the reduction in local pH due to bacterial infection [63]. On the other hand, in osteoarthritis there is a slight localized temperature increase (~2 – 3 ºC), due to joint inflammation [64]. In osteolytic cancer there is a markedly decreased pH due to exaggerated osteoclastic activity that can be explored as trigger, amongst other more common exploitations in cancers such as redox-based stimuli within the tumor microenvironment [65,66]. In this context, the following subchapters highlight the different strategies currently being explored for the design of stimuli-responsive nanocarriers aimed to be used for different bone disorders.
3.1. Enzyme-responsive nanocarriers
Enzyme-responsive nanocarriers take advantage of intrinsic enzymatic activity at the target tissues. Such stimuli can be explored in certain pathologies or during tissue remodeling/repair where enzyme activity can be upregulated, thus making it an interesting biological trigger to promote the release of bioactive molecules from nanocarriers at specific sites [20]. Typically, the most commonly explored instances of enzyme-responsive delivery take advantage of altered expression profiles of proteases, phospholipases and oxireductases underlying various scenarios such as wound healing, infectious pathogens, neurodegeneration, diabetes or tumor invasion [67]. Particularly in the bone milieu, cathepsin K (CTSK) is one of the most valuable enzyme-based stimuli to be explored.
CTSK production is associated with the bone remodeling dynamics, particularly bone catabolism. In this process, osteoclasts (multinucleated cells responsible for resorbing bone), are localized within the resorption lacunae, an acidic sealed area (pH~4), where these cells release CTSK and HCl to digest the collagenous organic matrix and hydroxyapatite (HA) crystals, respectively. Apart from osteoclast-mediated expression, breast cancer skeletal metastases are also known to overexpress this specific proteinase [68]. Also, CTSK expression has been reported in fibrotic lung tissues [69]. Hence during pre-clinical analysis of CTSK-responsive nanocarriers aimed for bone therapies, one should take into consideration possible unspecific particle accumulation in these organs and undesired drug release. Directing CTSK-responsive particles to target skeletal tissues is therefore crucial to maximize their efficacy and reduce side-effects.
Various researchers have explored the incorporation of specific peptides as CTSK-cleavable linkers in the design of stimuli-responsive nanocarriers for delivery to osteoclastic bone resorbing zones, including those occurring in osteoporosis.
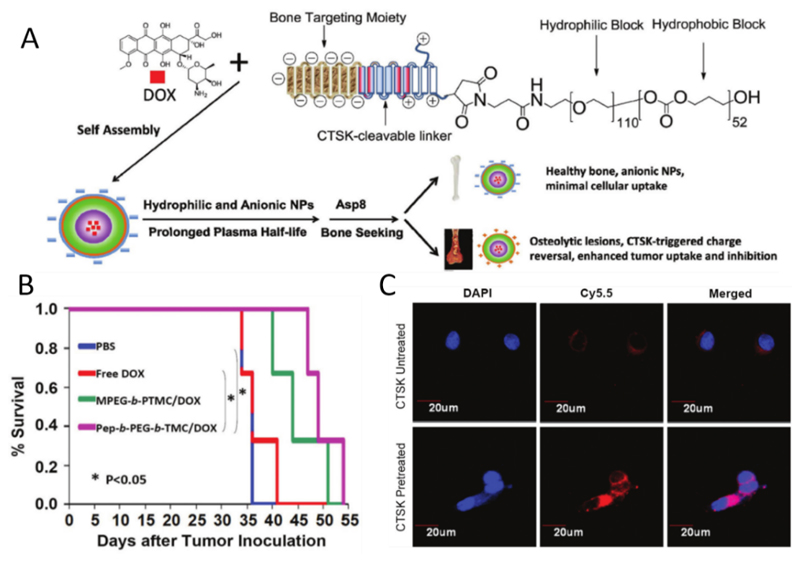
Peptide sequences that are CTSK substrates such as the GGP-Nle, GGGMGPSGPWGGK and HPGGPQ have been extensively employed for enzyme-responsive delivery in various studies [70–72]. Clearly, there are immediately two ways to exploit this cleavage-dependent delivery: (i) incorporating sensitive moieties in polymeric nanocarrier backbone, eliciting its disruption upon enzyme exposure; (ii) or attaching the drug to the nanocarrier through CTSK sensitive linkers, prompting drug release from nanoparticles via enzyme cleavage. The latter approach has been used with success in a study by Pan and co-workers which showed the induction of bone formation in vivo in ovariectomized Sprague-Dawley rats after administration of prostaglandin E1 attached to a Asp8-HPMA copolymer via a CTSK-sensitive oligopeptide sequence (GGP-Nle) [70]. Also, a particularly elegant approach by Wang and co-workers exploited the CTSK-mediated cleavage to increase the cellular uptake of charge-shifting nanocarriers and improve chemotherapeutics delivery to bone metastasis [72]. In this study, PEG and poly(trimethylene carbonate) diblock copolymer (PEG-b-PTMC) were synthesized via ring-opening polymerization of trimethylene carbonate (TMC) and then PEG blocks were functionalized with a chimeric peptide, prior to doxorubicin (DOX) anti-cancer drug loading. This multifunctional peptide consisted of three components: i) the exposed anionic aspartate repetitions (Asp8), responsible for bone targeting; ii) the CTSK substrate (HPGGPQ) sequence linking the two adjacent domains; and iii) the cationic residue linked to the surface of the diblock copolymer, responsible for increasing cellular uptake upon CSTK-cleavage (Figure 5). This hybrid biomaterial was able to self-assemble into micelles in aqueous solution via dialysis under mild conditions (size: 75 ± 10 nm, ζ-potential −18.5 ± 1.9 mV).
Figure 5.
Mechanism of action of CTSK-triggered charge reversal micelles for targeted in vivo bone metastasis treatment. Kaplan–Meier survival curves of mice following tumor injection and treatment. Adapted from [72] with permission from Royal Society of Chemistry.
The negatively charged micelles then experience a charge-reversal upon reaching osteolytic lesion sites overexpressing CTSK, due to enzymatic cleavage of the anionic block, which exposes the cationic moiety and triggers a charge reversal from negative to positive (-18.5 mV to +15.2 mV), markedly increasing in vitro cellular uptake in MCF-7 breast cancer cells after 30 min incubation with CTSK, when compared to absence of CTSK conditions (Figure 5C). Interestingly, following intravenous injection, these enzyme-sensitive polymeric micelles prolonged the survival of 4TGM1 mice bearing bone metastatic myeloma in comparison to free DOX and non-responsive formulations. In addition, serum IgG 2b levels were the lowest for the CTSK-responsive nanomicelles, which correlates with reduced tumor burden across all controls.
Another enzyme-based trigger mechanism that can be explored relies on extracellular matrix-degrading enzymes, specifically matrix metalloproteinases (MMPs). These zinc-dependent proteinases are actively implicated in bone remodeling and are also involved in bone cancer dissemination via degradation of the extracellular matrix [73]. Osteoclasts are known to express various MMPs, including MMP-14, MMP-12 and MMP-9[74], while osteoblasts are reported to express MMP-13 [75]. Regarding MMP-9, some reports describe the formulation of smart nanocarriers endowed with MMP-9 sensitivity, however these are yet to be applied for bone-specific delivery [76,77]. Since MMP-9 is highly expressed in regenerating bone tissues (e.g., upon fracture), the stimuli-responsive carriers could enhancing bone regeneration when loaded with appropriate osteoinductive/pro-regenerative factors [78]. In the context of bone malignancies, Liu and his team developed MMP-7-sensitive photodynamic molecular beacons that achieved tumor reduction in a vertebral model of osteolytic bone metastasis [79].
Hyaluronic acid-based nanocarriers may also be explored for stimuli-responsive release in a disease-specific mode since hyaluronidase is present in some bone disorders. This enzyme is secreted by Staphylococcus aureus, the main bacterial pathogen for osteomyelitis. The infectious microenvironment of osteomyelitis is characterized by a marked reduction in local pH, as well as the local presence of specific glycosidases, phosphatases, lipases and toxins, all inherent to the excessive proliferation of infecting bacteria [63,80]. To treat this disease, Baier and co-workers developed biocompatible hyaluronic acid-based nanocapsules (size: 320 nm, ζ-potential: -17 mV) carrying polyhexanide, a known antimicrobial agent. The obtained results indicate that enzyme-responsive formulations had significantly lower minimal inhibitory concentration against S. aureus and Methicillin-resistant S. aureus (ATCC 29213 and 43300) when compared to non-hyaluronidase degradable nanocarriers [81]. As evidenced by Baier, taking advantage of microorganisms hyaluronidase secretion to trigger the release of encapsulated antibiotics is a valuable strategy to eradicate bacterial infections not only in bone but also in other tissues.
Despite being valuable examples, more information regarding the kinetics of enzymes under/over-expression in each patient and at each disease progression stage is necessary. Adding to this, fundamental in vitro studies regarding the efficacy of enzyme-based release at very low colony forming units (CFUs) should also be addressed, as the quantity of produced enzymes could be insufficient to prompt bioactive molecules release. Such research is envisioned to aid in the determination of the optimal enzyme-sensitive nanocarriers administration regime and the adaptation of therapy to each patient and bacterial strain in a more personalized mode.
3.2. Thermo-responsive nanocarriers
Thermo-responsive nanocarriers frequently comprise a thermolabile moiety such as the extensively explored material poly(N-isopropyl acrylamide) (PNIPAM) or temperature-sensitive lipids such as dipalmitoyl phosphatidylcholine and lysolipids [20,33]. Temperature sensitivity is correlated with materials ability to change their properties with temperature, often in a nonlinear and sharp mode. The low critical solution temperature (LCST) of different materials used for nanocarriers assembly is as key parameter to tailor the temperature-mediated release profile of these delivery systems. Owing to their biological characteristics, healthy humans have thermoregulatory mechanisms that guarantee constant body temperature over time. However, some pathophysiological scenarios, including inflammation and tumors are characterized by higher temperatures than healthy tissues [82]. This thermal difference between cancer and normal tissues has been extensively explored for developing thermo-responsive nanocarriers with application in cancer treatment, as shown below. However, because not all tumors behave equally in locally increased temperature this selective delivery could be further improved by externally heating the tumor site either through ultrasound, alternating magnetic fields or temperature-controlled water sacks [20,33]. Yet, we should carefully address the validity of such approaches in the context of tumors, since the overexpression of heat-shock proteins (e.g., Hsp-70, HSP-90 [83]) may further contribute for cells thermal resistance along time and counteract the cytotoxic effect of released chemotherapeutics. Some combinatorial strategies for silencing HSPs and releasing cytotoxic drugs have been under development to circumvent this resistance mechanism [84].
For the particular case of bone tissues, Staruch and co-workers were able to achieve magnetic resonance imaging (MRI)-guided drug deposition in bone through the administration of thermo-responsive liposomes containing DOX (ThermoDox®) [85]. Focused ultrasound heating after liposomal administration in New Zealand white rabbits resulted in 8.2 and 16.8-fold increased DOX concentration in bone marrow and bone adjacent muscles, respectively, in comparison with non-heated tissues. On a similar note, Song and colleagues developed thermo-responsive pamidronate (PA)-functionalized liposomes containing DOX for treatment of bone tumor metastases [86]. These liposomes exhibited a strong binding affinity to hydroxyapatite and a complete release of DOX was observed within 10 min at 42 ºC. Blank liposomes showed relatively low cytotoxicity to A549 cells, regardless of PA-functionalization. However, it is important to underline that in this study, the heating effect on cell viability with blank liposomes was not explored. For DOX concentrations over 5 µM, PA-functionalized liposomes clearly showed higher cytotoxicity than non-targeted liposomes. Pre-heating PA-coated liposomes at 42 ºC prior to in vitro administration induced higher cytotoxicity than the same formulation at 37 ºC, validating the superior therapeutic effect of the thermo-sensitive liposomes.
Apart from increased temperature in bone cancers, other bone diseases such as osteoarthritis present at late stages significant joint inflammation, resulting in a mild increase on local temperature [64]. Such environment can also be exploited with thermo-responsive nanocarriers for improving therapeutics spatiotemporal delivery and the overall therapeutic outcome. Current studies on osteoarthritis, such as that of Poh and colleagues exploit (N,N′-bis(acryloyl)cystamine) disulfide crosslinked PEGylated poly(N-isopropylacrylamide-2-acrylamido-2-methyl-1-propanesulfonate) nanoparticles to load the anti-inflammatory peptide KAFAKLAARLYRKALARQLGVAA (KAFAK) (size: 223 ± 9.7 nm, ζ-potential: -3.81 ± 2.01 mV). Particles formulation was promoted through temperature and disulfide crosslinking assembly, while drug loading was achieved through passive diffusion below the LCST. Such particles then rely on intracellular stimuli (pH and redox) for therapeutics spatiotemporally controlled release [87]. In the context of bone disorders, the KAFAK peptide delivery is promising for osteoarthritis due to its suppression of TNF-α and IL-6 production. Despite being already an interesting system, the performance of these nanocarriers could be further improved by external heating so as to enhance the delivery at intended joints or inflamed areas in the knee [88]. In addition, it is well known that osteoarthritis progression is related with increased oxidative stress. For example, previously reported citrate-based thermo-responsive nanocarriers with intrinsic antioxidant properties could be used in the future to improve osteoarthritis treatment [89].
From the available body of literature, it is clear that there are still significant challenges to be overcome in the development of bone-specific thermo-responsive nanocarriers to achieve maximum therapeutic efficacy in vivo. This is particularly challenging for scenarios where there is no significant increase of internal temperature, thus requiring external heating as stimuli. In this context, one of the most important aspects is the ability to assure an externally focused heating to bone disease sites without affecting neighboring healthy tissues.
3.3. Ultrasound-responsive nanocarriers
Ultrasound is based on the use of low or high intensity acoustic energy and is widely used in clinic for non-invasive biomedical imaging [90]. Ultrasound-responsive systems have been widely explored for delivery of bioactive therapeutics, typically by exploiting liposomal and micellar nanocarriers [91]. In the context of drug delivery, this external stimulus induces cavitation of microbubble contrast agents (small gas bubbles) loaded within nanocarriers hydrophobic reservoirs. The incidence of ultrasound leads to expansion and can ultimately fragment carriers structure.
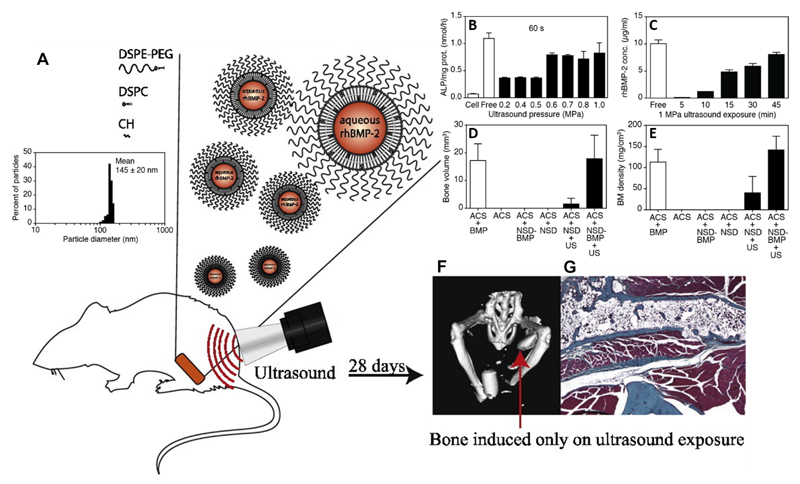
Echogenic liposomes have been previously designed to allow multiple stimuli-responsiveness and enhance the release of bioactive molecules. Nahire and co-workers developed MMP-9 responsive echogenic liposomes comprised of 1-palmitoyl-2-oleoyl- sn-glycero-3-phosphocholine with a triple-helical lipopeptide (size: 190 ± 35 nm) [92]. In this study an increased payload release from liposomes upon simultaneous application of diagnostic-used ultrasound frequency (3 MHz) was obtained. More recently, Crasto and her team developed PEGylated liposomes (size: 145 ± 20 nm) that released recombinant human BMP-2 (rhBMP-2) upon ultrasound exposure (1 MHz) (Figure 6) [93]. Such ultrasound-responsive liposomes exhibited rhBMP-2 release correlated with exposure time and ultrasound pressure, which lead to increased C2C12 cellular expression of alkaline phosphatase (ALP) (Figure 6B and 6C). Moreover, these nanocarriers for sonodisruptable delivery (NSD) were embedded within an absorbable collagen sponge (ACS) for a proof-of-concept comparison with the clinical standard of rhBMP-2 delivered via ACS implants. Indeed, µCT data showed that the ACS-NSD groups carrying rhBMP-2 elicited an increase in bone volume and mineral density (BM) comparable to the ACS-BMP groups (Figure 6D and 6E). By using this strategy, the researchers were able to increase localized bone matrix formation in a Swiss Webster mice muscle pouch model, representing the first in vivo validation of ultrasound-triggered delivery of rhBMP-2 and consequently have issued a patent on this technology [94].
Figure 6.
Ultrasound-responsive liposomes characterization. (A) Dynamic light scattering analysis of PEGylated nanoliposomes loaded with rhBMP-2; (B) ALP assay in C2C12 cellsfollowing rhBMP-2 released from nanoparticles for sonodisruptable delivery containing rhBMP-2 (NSD-BMP) exposed to increasing ultrasound pressures for 60 s (N=3, n=2); Free refers to an assayed amount of soluble rhBMP-2 predicted to be contained within NSD-BMP-2 of the same sample size. (C) Evaluation of ultrasound exposure in rhBMP-2 release profile, i.e, ultrasound duration dependence of rhBMP-2 release from NSD-BMP in phantom tissue (5–45 min at 1 MPa), quantified by ELISA (N=3, n=2); (D) Bone volume data acquired from µCT; ACS + BMP, standard rhBMP-2 implant (no ultrasound), ACS, implant sponge only (no rhBMP-2, no ultrasound), ACS + NSD- BMP, NSD-BMP nanocomplexes with rhBMP-2 payload applied to ACS implant (no ultrasound), ACS + NSD, nanoparticles without rhBMP-2 payload, on ACS implant (no ultrasound), ACS + NSD + US, nanoparticles without rhBMP-2 payload, on ACS implant (ultrasound applied 24 h after implantation surgery), ACS + NSD-BMP + US, nanocomplexes with rhBMP-2 payload applied to ACS implant (ultrasound applied 24 h after implantation surgery) (E) Bone mineral density analysis of different formulations. ACS – represents collagen implant. NSD – PEGylated nanoliposomes; NSD-BMP- PEGylated nanoliposomes loaded with rhBMP-2. US- ultrasound (applied 24 h following surgery). (F) µCT reconstruction, group subjected to ultrasound exposure. This induced bone formation by using the ACS+NSD-BMP formulation. (G) Masson’s trichrome staining of perifemoral section showing the extent of bone induction by using ACS implant with NSD-BMP formulations and administering ultrasound 24 h post-surgery. Adapted from [93] with permission from Elsevier.
Despite achieving promising results, it must be emphasized that this study involved liposome impregnation within a collagen sponge, a delivery route that is invasive and may entail further surgery-associated problems. Apart from standard ultrasound stimulation, low intensity pulsed ultrasound stimulation (LIPUS) is also valuable in the scope of bone disorders with recent reports from different researchers emphasizing the ability to enhance bone regeneration during fracture healing and callus distraction [95]. In addition to its pro-osteogenic potential, Nagao and his team recently investigated the anti-inflammatory effects of LIPUS on MC3T3-E1 mouse calvarial cell line, where it was discovered that LIPUS was able to suppress the nuclear translocation of NF-kB activation induced by lipopolysaccharide, while also inhibiting the upregulation of toll-like receptor 4 and inflammatory cytokine IL-1 [96]. Moreover, this effect was found to be mediated by an increased expression of mechanosensitive angiotensin receptor type I upon LIPUS application. We thus hypothesize that this stimulus could potentially be used in the future as a tool to treat inflammatory bone diseases such as periodontitis or osteoarthritis. Combining LIPUS with ultrasound-responsive nanocarriers, could be a valuable strategy to design a stimuli-responsive nanomedicine-based therapeutic approach where not only drug release could be spatiotemporally controlled, but also where the triggering stimuli itself has therapeutic activity. Despite being a promising approach for the future, it should be taken into account that LIPUS potential for bone therapy may vary with a multitude of factors, ranging from medical history of previous treatments, site of application, type of fracture or nature of bone loss, treatment regime and patients age [97].
3.4. Magnetic-responsive nanocarriers
Magnetic-responsive nanoparticles respond to magnetic fields and find application in various areas including bioimaging namely through magnetic resonance imaging (MRI) and as guidance systems that allow cell or particle magnetic guidance. In this approach, magnetic forces are used to move nanocarriers towards the intended anatomical sites [20]. Then, the locally increased drug concentration due to nanocarrier retention is expected to translate into sustained doses released within the therapeutic window. However, this strategy is always dependent on the passive release of therapeutics from carriers. Moreover, because this guidance requires a localized magnetic force, this approach is not very promising for the treatment of systemic bone disorders such as osteoporosis, that logically require a widespread delivery to bone tissues. Nevertheless, magnetic delivery systems may be valuable to direct chemotherapeutics toward target osteosarcoma tumor hotspots and achieve localized malignant cells ablation [98]. In the context of bone regeneration, particles can be directed to localized defects such as fractures and be used to deliver bioactive molecules that prompt regeneration and the development of fully functional tissue [99]. The design of magnetic-responsive drug release by nanocarriers is of uttermost importance and highly desirable to control the therapeutic effect overtime. Magnetic-responsive nanocarriers span beyond the scope of simply being magnetically guided, since external alternating magnetic fields (AMFs) can be used to disrupt their colloidal structure, thus providing the possibility to spatiotemporally control drug release in an on-demand mode [100].
An extensive literature analysis revealed that so far only cationic magnetic liposomes were explored for magnetic on-demand drug delivery in bone, namely in mouse and hamster osteosarcoma models, both with successful outcomes [101,102]. These examples take advantage of magnetically-induced temperature increase. Typically, the diffusion of loaded drugs from liposomal carriers core increases with bilayer permeability, which in turn is generally dictated by lipids melting temperature (Tm). The value of Tm can be tailored depending on the lipid composition, and by tuning the high-frequency AMF pulses. This promotes lipid bilayer disruption by surpassing the intrinsic Tm and thereby prompts cargo release [103,104]. Despite being an attractive design, the application of these smart-release systems in bone regeneration or other bone disorders is still scarce when compared to its use in cancer therapy, where there are numerous studies upholding its potential. This could be due to bone characteristic anatomic location since its localized deep within the body, constituting a major biophysical barrier that is responsible for a rapid drop in magnetic field strength with increasing depth. Moreover, the before mentioned intertwining bone vasculature poses a major barrier in nanocarriers guidance [105]. To overcome the former barrier, recently, a magnetic spatial localization strategy has been developed in which magnetic field density can be focused at a distance from the pole. This may overcome magnetic attenuation and be used for both magnetic guidance and on-demand magnetic-mediated therapeutics release [106].
3.5. pH-responsive nanocarriers
Therapeutics delivery from nanocarriers via pH stimuli can be explored mainly in two different modes. The first one involves the design of nanocarriers with a pH-sensitive release profile resulting from existence of carboxylic acids or amines (including tertiary amines) within the nanocarrier backbone/structure [14,107]. Changes in the medium pH then results in different protonation/deprotonation states of these ionizable groups and to a shift in nanocarriers properties. This behavior can thus be explored for spatiotemporally controlled delivery of entrapped drugs within polymeric nanocarriers in specific microenvironments. The second alternative involves drug attachment to pH-sensitive moieties such as polyketals, acetals or hydrazide linkers that act as anchoring spots for binding the drug to the nanocarrier until pH-mediated hydrolysis occurs [10,90,108].
To date nanocarriers pH-sensitivity has been mainly explored for cancer therapy due to the characteristic acidic pH in tumors microenvironment (pH 6.5-7.2) [109,110]. This characteristic acidity is further accentuated in osteolytic cancers (e.g., bone Ewing’s sarcoma), due to an excessive osteoclastic activity that acts in concert with cancer cells to further contribute to bone tumors acidity [66]. Owing to these exploitable features it becomes clear why a significant body of literature involves the development of pH-responsive carriers for cancer therapy. On this topic, some interesting multifunctional pH-responsive delivery systems have been recently developed. Ferreira and colleagues prepared alendronate (AL)-coated liposomes for pH-responsive release of DOX in female nude BALB/c mice bearing bone metastases established through injection of MDA-MB-231 breast cancer cells on mice tibia [111]. The presence of 1,2-dioleoylglycero-3-phosphatidylethanolamine (DOPE) and cholesteryl hemisuccinate (CHEMS) lipids endowed the liposome with pH sensitivity, whereas AL-targeting moiety was responsible for nanocarriers active binding to hydroxyapatite. The liposome sizes ranged from 150 to 185 nm and exhibited a sharp DOX release at pH=5 when compared to pH=7.4, highlighting the pH-responsiveness of the formulation. Furthermore, encapsulated DOX maintained its cytotoxicity with a significant dose-dependent effect against the MDA-MB-231 cell line, while also markedly reducing drug cardiac uptake. Biodistribution studies indicated a 4-fold increase in chemotherapeutics accumulation in tumor tissues when compared to that of the free drug.
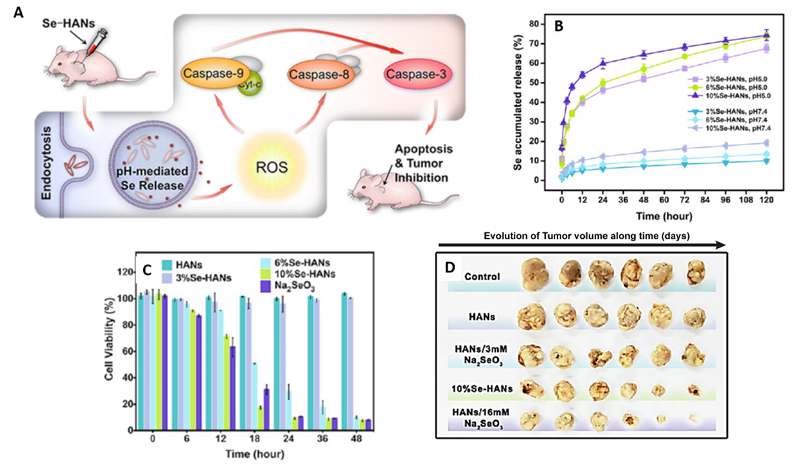
In a different approach, Wang and his team developed biodegradable and pH-responsive selenium-doped hydroxyapatite nanoparticles (Se-HANs) for the treatment of osteosarcoma (Figure 7 A) [112]. These rod-shaped HANs (size: 78.55 ± 0.20 nm, ζ-potential of -37.13 ± 0.63 mV) elicited 4 to 5-fold increase in selenium release under acidic conditions (pH=5) when compared to that obtained at physiological conditions (Figure 7 B). As evidenced by FITC-labeled nanocarriers the amount of encapsulated selenium significantly affected Se-HANs degradation in the lysosome, with higher selenium content resulting in a faster, pH-mediated degradation. In vitro results in human MNNG/HOS osteosarcoma cells, showed that the 10 % Se-HANs formulation had the highest cytotoxic effect on osteosarcoma cells, with their administration resulting in 83 % cell death after 18h. This cytotoxic activity was found to be associated with the intracellular generation of reactive oxygen species (ROS) mediated by the selenium cargo. More importantly, Se-HANs induced tumor apoptosis and reduced systemic toxicity in vivo, in a BALB/c nude mice osteosarcoma model. Following nanocarriers intratumoral administration 2- and 3-fold reduction in tumor weight and volume was obtained. Additionally, serum biochemical analysis of nanocarrier injected mice found that 10% Se-HANs had the lowest systemic toxicity when compared to a mixture of equal selenium content (HANs / 16 mM Na2SeO3), suggesting a controlled release profile at local tumor and reduced leakage at normal tissues. However, further studies involving nanocarriers parenteral delivery could be performed to fully characterize the biological performance of these carriers.
Figure 7.
(A) In vivo treatment of mice-bearing osteosarcoma with pH-responsive release of selenium-doped hydroxyapatite nanoparticles (Se-HANs) HANs. Internalized Se-HANs by nonspecific endocytosis are rapidly degraded in acidic lysosomes to release selenium. (B) Selenium release from Se-HANs exhibited a pH-responsive release profile at pH = 5.0 versus pH = 7.4. (C) CCK-8 assay of MNNG/HOS osteosarcoma cells showed that viability was highly associated with selenium content and degradation of Se-HANs. (D) In vivo evaluation of anti-osteosarcoma activity of Se-HANs after intratumoral injection on a xenograft osteosarcoma model. Compounds with higher selenium content, including 10%Se-HANs and HANs/16 mM Na2SeO3 exhibited efficient inhibition of tumor growth as evidenced by the reduction of tumor size (left). Adapted from [112] with permission from the American Chemical Society.
Exploring pH-responsiveness to elicit improved nanocarrier cytotoxicity may also be valuable for bone therapy, particularly in bone cancer. Alpaslan and colleagues showcased the potential of dextran-coated cerium oxide nanoparticles (nanoceria) (size: 45 nm (pH=7) and 29 nm (pH=6), ζ-potential: 16.68 ± 3.98 mV (pH=6)), which exhibit antioxidant activity at physiological pH values, but shifts to an oxidizing profile at slightly acidic pH conditions [113]. These nanoceria allow for a selective increase in ROS generation in osteosarcoma microenvironment. In this study, nanoceria particles incubated at pH=6 showed maximum cytotoxicity against osteosarcoma MG-63 cells. In healthy osteoblasts in vitro cultures (pH=6) no significant ROS generation was observed at any nanoceria concentration, thus confirming the proposed ROS-dependent cancer-killing mechanism. After 5 days at pH=6, the osteosarcoma IC50 value was found to be 100 µg/mL, as opposed to 500 µg/mL for normal osteoblasts [113]. In addition, nanoceria particles maintain their selective cancer-killing effect even at physiological pH, being observed that after a 5-day treatment, the IC50 values for healthy osteoblasts were well above 1000 µg/mL, in contrast with IC50 values of 250 µg/mL for MG-63 osteosarcoma cells.
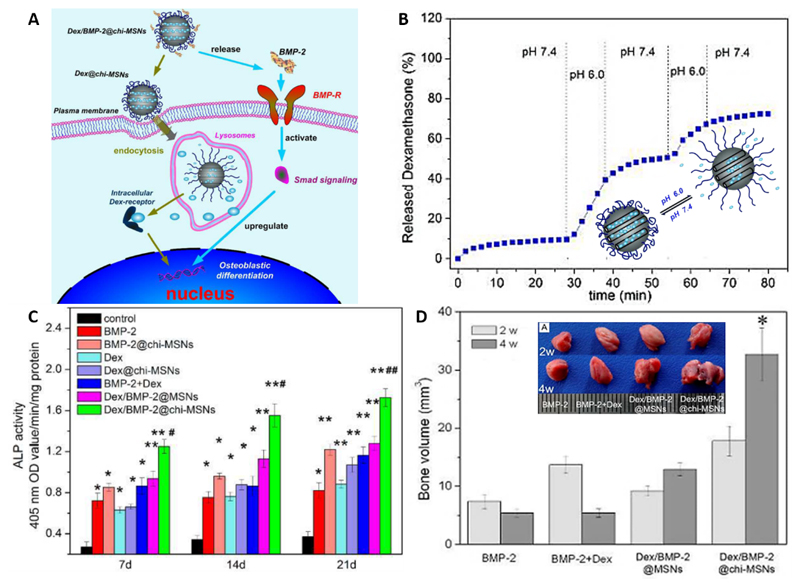
In the context of tissue engineering and regenerative medicine, Gan and co-workers developed pH-responsive chitosan-capped MCM-41 mesoporous silica nanoparticles (chi-MSNs) (size: 130 nm, ζ-potential: +22.5 mV) for delivery of BMP-2 and dexamethasone (Dex) to enhance bone regeneration (Figure 8) [114]. Chitosan (CS) functionalization of MSNs surface endowed the nanocarrier with pH-responsiveness due to CS primary amine protonation states at different pH (pka~6.5). In this sense, CS functioned as a nanovalve for controlled release of MCM-41 mesopores-loaded Dex upon intracellular uptake. Dex release followed a pH-responsive behavior, achieving 85% release within 60 min at pH=6.0, while almost no Dex was released at physiological pH conditions (pH=7.4). In addition, the outer chitosan layer also functioned as a matrix for BMP-2 incorporation, with results showing that BMP-2 release profile is unaffected by the culture medium pH, resulting in an immediate release under physiological conditions (80% BMP-2 release after 6 h). On one hand, this is beneficial as BMP-2 requires binding to specific cell-surface receptors, but on the other hand, because BMPs have low bioavailability, this release profile is not the most adequate for systemic administration, which is why the authors opted for the implantation with Gelfoam® (Absorbable gelatin sponge). Nevertheless, this nanocarrier has shown particular promise in promoting in vitro osteogenesis, with the combinatorial effect of Dex/BMP-2 dual-loaded chi-MSNs exhibiting significantly higher ALP activity of rat bone mesenchymal stem cells (BMSCs) than single Dex or BMP-2 MSNs loaded formulations. Moreover, alizarin red S staining further confirmed that BMSCs incubated with Dex/BMP-2@chi-MSNs have greater mineralization nodules when compared to controls. The in vivo osteogenic capacity of this formulation was evaluated via ectopic bone formation in a male mice thigh muscle pouch model. By using 3D µCT analysis the authors demonstrate that after 4 weeks there is an increase in tissue mineral density of both dual-loaded formulations when compared to the free therapeutics control groups.
Figure 8.
Physicochemical characterization and biological performance of silica-based pH-responsive nanocarriers. (A) Schematic diagram of Dex/BMP-2@chi-MSNs on osteoblast differentiation. First, BMP-2 is quickly released and then activates the downstream Smad signaling by binding to specific cell surface BMP receptors. Secondly, Dex is delivered intracellularly through a pH-responsive release within lysosomes. (B) The capping effect of chitosan in the pH-responsive release of Dex from chi-MSNs. (C) Effect of different nanocarriers formulations bMSCs ALP activity cultured (D) In vivo ectopic bone formation induced by BMP-2 and Dex with different implants after 2 and 4 weeks post-implantation. Quantitative analysis of regenerated bone volume from 3D µCT images. Adapted from [114] with reprint permission from Royal Society of Chemistry.
Even though such nanovehicle has not been formulated for minimally invasive intravenous administration, this example highlights the potential of pH-responsive delivery of pharmaceuticals for bone regeneration, an area where parenteral routes of administration have been poorly explored so far.
Apart from the former examples, there are also other bone disorders for which pH-responsive nanocarriers could be valuable as on-demand delivery systems. In osteomyelitis, the production of acid by osteoclasts and infecting bacteria metabolism tends to reduce the pH in the site of inflammation [63]. Such acidic environment, could allow for selective release of bioactive molecules (e.g., antibiotics) in the affected bone milieu.
To treat bone bacterial infections, Ferreira and co-workers developed a pH-responsive liposomal theranostic platform (DOPE, CHEMS, PEG2K-DSPE) containing technetium-99m-labeled ceftizoxime, a 3rd generation cephalosporin antibiotic. The liposomal carriers (size: 169.1 ± 8.4 nm, ζ potential: 2.2 ± 1.1 mV) were able to accumulate in bone infected foci in a male Wistar rat model of acute osteomyelitis following intravenous administration [115]. These liposomes undergo structural destabilization in acidic medium, locally releasing the radiotracer and thereby allowing accurate infection imaging and treatment. The obtained results indicate that the radioactivity level in the infected tibia was 1.5-fold higher than in healthy tibia. Although this study demonstrated the positive effect of such theranostic liposomes, from the perspective of clinical application the use of radiotracers could entail some restrictions due to their known toxicity. With the advent of multimodal imaging technologies and non-radioactive probes such concept could be further investigated.
More recently, AL-coated PEG-poly(lactic acid-co-glycolic acid) (PLGA) micelles were used for bone-targeted delivery of the antibiotic vancomycin [116]. These micellar carriers showed faster vancomycin release profiles at pH=5.0 when compared to that obtained under physiological conditions. Interestingly, the binding affinity to hydroxyapatite was unaffected by external pH and therefore these micelles may constitute a suitable nanocarrier for stimuli-responsive treatment of osteomyelitis. However, it is important to emphasize that for early stage osteomyelitis, the acidic environment may not be sufficient to be used as a drug release trigger, thus limiting drugs therapeutic efficacy before disease progression.
Such could be overcome by engineering highly sensitive pH-responsive systems as those recently developed by Sethuraman and co-workers. These researchers produced a two component pH-mediated charge-shifting nanocarrier comprised by: (i) PLA-b-PEG diblock copolymers conjugated to TAT cell penetrating peptide and (ii) pH-sensitive diblock copolymer poly(L-cystine bisamide-g-sulfadiazine)-b-PEG (PCBS23K-b-PEG5K) [117]. At physiological pH, sulfadiazine is negatively charged and shields the TAT-micelle by electrostatic interactions. Upon a decrease in pH, sulfadiazine becomes neutral and detaches from the TAT-micelle, exposing TAT for interaction with nearby cells, while the PCBS moiety is degraded by glutathione. This polymeric micelle markedly enhanced DOX cytotoxicity within 0.2 pH units below of pH 7.2 [117]. This remarkably sensitive block may be an interesting design tweak for improving stimuli sensitivity during the initial onset of osteomyelitis.
3.6. Redox-responsive nanocarriers
Redox-sensitive nanocarriers are very interesting due to their ability to respond to oxidative-reductive environments including those dependent on glutathione (GSH), thioredoxin, or human serum albumin (HAS-SH) concentration [118,119]. Redox-responsive nanocarriers are designed to disassemble in the cytosol and release their bioactive cargo. Such is an important aspect for skeletal disorders considering that some bioactive therapeutics for bone cells have intracellular molecular targets [14,120]. Human cells intracellular compartments contain a high GSH concentration (2-10 mM), which is about 103-fold higher than that found in the extracellular matrix and blood plasma (2-20 µM) [121]. However, some studies suggest that reductive conditions may already be present at the endosome during receptor-mediated endocytosis [122]. This difference in redox-potential inside cells is typically exploited by designing nanocarriers containing reduction-sensitive linkers that are cleaved upon cellular uptake, thus releasing cargo only in intracellular conditions. The disulfide bond is the most commonly used redox-sensitive linker. However, the library of redox-responsible chemical modifications that can be imprinted in nanocarriers structure is increasing with other responsive moieties such as diseleinide, ditellurium [123] and maleimide-arylthiol bonds gaining increased attention in recent years [124,125]. Such chemical imprinting of redox-responsive moieties in nanocarriers structure can be achieved by three main ways: (i) grafting of bioreducible linkers on the repeating monomers of polymeric backbones, which readily prompt nanocarrier intracellular disintegration; (ii) grafting disulfide bonds as terminal crosslinkers between different polymer blocks in copolymer-based nanocarriers, that can lead to micelles disassembly [125] and (iii) precision chemical modification of polymer monomeric units with redox-responsive moieties linked to drugs (polymer-drug conjugate), which upon the stimulus are promptly released. These strategies have been extensively used for formulation of redox-responsive polymeric micelles for delivery of pharmaceutics under redox-conditions, either through core or shell disulfide-based crosslinking, which can greatly improve polymeric micelles stability [126]. However, it is important to emphasize that few redox-responsive carriers have been used for the treatment of bone diseases other than cancer.
For treatment of osteosarcoma, Maciel and colleagues designed a facile method for preparing redox-responsive alginate nanogels by crosslinking with cystamine through mini-emulsion [127]. Then, cytotoxic drug loading was achieved by incorporating DOX in aqueous solution with nanogels, resulting in high encapsulation efficiency (95.2 ± 4.7%). These biocompatible nanogels significantly increased DOX intracellular concentration and enhanced cytotoxicity in osteosarcoma cells (CAL-72). Another interesting approach for bone cancer is that proposed by Yao and co-workers which designed glutathione-responsive self-assembled micelles (size: 169.8 nm, ζ-potential: +20.23 mV) based on disulfide crosslinked stearyl cationic polypeptide copolymers containing arginine and histidine for co-delivery of DOX and microRNA-34a to androgen-independent prostate cancer cells both in vitro and in vivo [128]. These micelles reduced anthracycline cardiotoxicity and promoted a synergistic anti-tumoral effect upon drug-gene co-delivery (DOX/microRNA-34a). In particular, because microRNA-34a has shown an important role in myeloid and bone-related cancers (namely myeloma, leukemia, osteosarcoma and Ewing’s sarcoma), it might be interesting to pursue further studies in bone with these micelles [129].
For the treatment of osteoarthritis, other researchers developed PEGylated poly(N-isopropylacrylamide-2-acrylamido-2-methyl-1-propanesulfonate) nanoparticles with a disulfide crosslinker (N, N’-bis(acryloyl)cystamine) (NGPEGSS)) for delivery of the anti-inflammatory peptide KAFAK to an ex vivo model [130]. These disulfide nanocarriers exhibited enhanced extracellular stability and improved KAFAK loading, as well as enhanced release under reducing conditions. Strikingly, they selectively infiltrate inflamed cartilage and were internalized by chondrocytes, which are recognized as a hard to transfect cell type. The KAFAK-loaded NGPEGSS nanoparticles were able to significantly decrease cytokine IL-6 production over time both in chondrocytes and macrophages, demonstrating its potential to act as an intra-articular injectable nanocarrier for the treatment of osteoarthritis [87,130].
It is without doubt that the unique reversibility and responsiveness of disulfide linkages as a ubiquitous stimulus contributed to the engineering of redox-responsive nanocarriers with efficient on-demand release of therapeutics for various bone diseases. Yet, to fulfil their potential for clinical translation some aspects such as the effect of cell surface thiols in their cellular uptake and intracellular trafficking of such carriers should be further investigated and optimized [121].
5. Conclusion and Perspectives
From an in-depth analysis of available literature reports focusing on stimuli-responsive nanocarriers it is clear that their overwhelming majority aims for bone cancer treatment and takes advantage of cancer-specific stimuli (e.g., redox, pH, temperature). The motivation for such focus stems mostly from tumors increasing prevalence, but also from the relative understanding of their major hallmarks and microvasculature [55,82,110,131,132].
Apart from this pathology, non-regenerating acute bone injuries (e.g., critical size fractures), bone diseases (e.g., osteomyelitis, osteoporosis) and joint degeneration problems (e.g., osteoarthritis) are increasing in incidence and the development of more effective treatments tailored for these disorders is evermore required in a clinical setting. However, the translation of stimuli-responsive nanocarriers into clinical practice remains highly challenging.
To date, few stimuli-responsive nanocarriers reached clinical stages across all areas, an aspect that is particularly evident for bone disorders. This could be in part assigned to insufficient nanocarriers bioavailability and selectivity to bone tissues. But can be mainly attributed to our poor understanding of more fundamental aspects regarding the unique biological barriers posed by the skeletal architecture. An increased information of how intravenously administered nanocarriers can reach bone tissues and what optimal characteristics in terms of size, shape, surface charge and blood stability they should possess is fundamental and should receive a renewed focus. Intravenous administration is in fact highly attractive when compared to localized delivery via micro- or macro-sized implants, that while interesting for some bone disorders, do not warrant enough coverage to reach every bone tissue in a similar manner [10], a major aspect in osteoporosis. Furthermore, the procedures for implant introduction are costly, laborious and highly invasive, not to mention the possible complications or infections arising from surgery.
In a critical perspective, it is clear that a stimuli-mediated control over therapeutics release provides significant advances over the current shortcomings regarding premature leakage and burst release, yet, future generations of responsive carriers must be rationally engineered. Achieving a balance between complexity and biological performance is an underlying issue in the drug delivery field since the trend in the past years has been to develop perhaps overengineered stimuli-responsive multifunctional carriers in detriment of more simple systems as recently emphasized [133]. Such trend could be restrictive in the context of cost-effectiveness and realistic industrial production.
Yet, the design of more complex, multifunctional carriers could have an added benefit in the context of bone pathologies/injuries that feature more than one physicochemical/biochemical features as compared with healthy bone. Hence, the manufacture of dual/multi-stimuli responsive systems (pH+temperatute, pH+redox, light+pH, etc) could offer synergistic non-linear responses that could enhance the therapeutic outcome of such nanobiomaterials [134]. Envisioning future advances, the next-generation of such systems could combine also physical and morphological properties such as shape, topography and mechanical properties which are known to influence cellular behavior and carriers biological performance [135].
Alongside with this, in the design of multifunctional carriers aimed for parenteral delivery different strategies other than the widely used PEGylation as shielding mechanism should be encouraged and pursued, particularly following the myriad of recent reports highlighting some pitfalls in such approach [136]. In fact, with the latest developments regarding alternatives to endow nanocarriers with stealth character we will for sure assist to the proposal of smarter nanocarriers for systemic bone treatments. However, parallel efforts should be done in order to comply with regulatory guidelines to seriously consider the final application of such systems.
We envision that having an open mindset on these fundamental challenges could contribute for the formulation of responsive nanocarriers with more potential for future commercialization and realistic clinical application.
Acknowledgments
The authors would like to acknowledge the support of the European Research Council grant agreement ERC-2014-ADG-669858 for project ATLAS. The authors also acknowledge the financial support by the Portuguese Foundation for Science and Technology (FCT) through a Post-doctoral grant (SFRH/BPD/119983/2016, Vítor Gaspar). The authors also acknowledge Servier Medical Art (www.servier.com), for providing image vectors for Figure 1 and 4, licensed under the Creative Commons Attribution 3.0 Unported License (http://creativecommons.org/license/by/3.0/).
References
- [1].Rodan GA, Martin TJ. Therapeutic Approaches to Bone Diseases. Science (80-. ) 2000;289:1508–1514. doi: 10.1126/science.289.5484.1508. [DOI] [PubMed] [Google Scholar]
- [2].Gu W, Wu C, Chen J, Xiao Y. Nanotechnology in the targeted drug delivery for bone diseases and bone regeneration. Int J Nanomedicine. 2013;8:2305–2317. doi: 10.2147/IJN.S44393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Feurer E, Chapurlat R. Emerging drugs for osteoporosis. Expert Opin Emerg Drugs. 2014;19:385–395. doi: 10.1517/14728214.2014.936377. [DOI] [PubMed] [Google Scholar]
- [4].Carbone EJ, Rajpura K, Allen BN, Cheng E, Ulery BD, Lo KWH. Osteotropic nanoscale drug delivery systems based on small molecule bone-targeting moieties. Nanomedicine Nanotechnology, Biol Med. 2017;13:37–47. doi: 10.1016/j.nano.2016.08.015. [DOI] [PubMed] [Google Scholar]
- [5].Vahle JL, Sato M, Long GG, Young JK, Francis PC, Engelhardt Ja, Westmore MS, Linda Y, Nold JB. Skeletal changes in rats given daily subcutaneous injections of recombinant human parathyroid hormone (1-34) for 2 years and relevance to human safety. Toxicol Pathol. 2002;30:312–321. doi: 10.1080/01926230252929882. [DOI] [PubMed] [Google Scholar]
- [6].Nase JB, Suzuki JB. Osteonecrosis of the jaw and oral bisphosphonate treatment. J Am Dent Assoc. 2006;137:1115–1119. doi: 10.14219/jada.archive.2006.0350. [DOI] [PubMed] [Google Scholar]
- [7].Graham DY. What the gastroenterologist should know about the gastrointestinal safety profiles of bisphosphonates. Dig Dis Sci. 2002;47:1665–1678. doi: 10.1023/a:1016495221567. [DOI] [PubMed] [Google Scholar]
- [8].Luetke A, Meyers PA, Lewis I, Juergens H. Osteosarcoma treatment - Where do we stand? A state of the art review. Cancer Treat Rev. 2014;40:523–532. doi: 10.1016/j.ctrv.2013.11.006. [DOI] [PubMed] [Google Scholar]
- [9].Farokhi M, Mottaghitalab F, Shokrgozar MA, Ou KL, Mao C, Hosseinkhani H. Importance of dual delivery systems for bone tissue engineering. J Control Release. 2016;225:152–169. doi: 10.1016/j.jconrel.2016.01.033. [DOI] [PubMed] [Google Scholar]
- [10].Newman MR, Benoit DSW. Local and targeted drug delivery for bone regeneration. Curr Opin Biotechnol. 2016;40:125–132. doi: 10.1016/j.copbio.2016.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Balmayor ER. Targeted delivery as key for the success of small osteoinductive molecules. Adv Drug Deliv Rev. 2015;94:13–27. doi: 10.1016/j.addr.2015.04.022. [DOI] [PubMed] [Google Scholar]
- [12].Kim Y-H, Tabata Y. Dual-controlled release system of drugs for bone regeneration. Adv Drug Deliv Rev. 2015;94:28–40. doi: 10.1016/j.addr.2015.06.003. [DOI] [PubMed] [Google Scholar]
- [13].Basha G, Ordobadi M, Scott WR, Cottle A, Liu Y, Wang H, Cullis PR. Lipid Nanoparticle Delivery of siRNA to Osteocytes Leads to Effective Silencing of SOST and Inhibition of Sclerostin In Vivo. Mol Ther Acids. 2016;5:e363. doi: 10.1038/mtna.2016.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Alencastre IS, Sousa DM, Alves CJ, Leitão L, Neto E, Aguiar P, Lamghari M. Delivery of pharmaceutics to bone: Nanotechnologies, high-throughput processing and in silico mathematical models. Eur Cells Mater. 2016;31:355–381. doi: 10.22203/eCM.v031a23. [DOI] [PubMed] [Google Scholar]
- [15].Yang L, Webster TJ. Nanotechnology controlled drug delivery for treating bone diseases. Expert Opin Drug Deliv. 2009;6:851–64. doi: 10.1517/17425240903044935. [DOI] [PubMed] [Google Scholar]
- [16].Hirabayashi H, Fujisaki J. Bone-Specific Drug Delivery Systems Approaches via Chemical Modification of. Clin Pharmacokinet. 2003;42:1319–1330. doi: 10.2165/00003088-200342150-00002. [DOI] [PubMed] [Google Scholar]
- [17].Aoki K, Alles N, Soysa N, Ohya K. Peptide-based delivery to bone. Adv Drug Deliv Rev. 2012;64:1220–1238. doi: 10.1016/j.addr.2012.05.017. [DOI] [PubMed] [Google Scholar]
- [18].Dang L, Liu J, Li F, Wang L, Li D, Guo B, He X, Jiang F, Liang C, Liu B, Badshah S, et al. Targeted Delivery Systems for Molecular Therapy in Skeletal Disorders. Int J Mol Sci. 2016;17:428. doi: 10.3390/ijms17030428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Nowinski AK, White AD, Keefe AJ, Jiang S. Biologically inspired stealth peptide-capped gold nanoparticles. Langmuir. 2014;30:1864–1870. doi: 10.1021/la404980g. [DOI] [PubMed] [Google Scholar]
- [20].Mura S, Nicolas J, Couvreur P. Stimuli-responsive nanocarriers for drug delivery. Nat Mater. 2013;12:991–1003. doi: 10.1038/nmat3776. [DOI] [PubMed] [Google Scholar]
- [21].Yi H, Rehman F Ur, Zhao C, Liu B, He N. Recent advances in nano scaffolds for bone repair. Bone Res. 2016;4 doi: 10.1038/boneres.2016.50. 16050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Cheng CW, Solorio LD, Alsberg E. Decellularized tissue and cell-derived extracellular matrices as scaffolds for orthopaedic tissue engineering. Biotechnol Adv. 2014;32:462–484. doi: 10.1016/j.biotechadv.2013.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Clarke B. Normal Bone Anatomy and Physiology. Clin J Am Soc Nephrol. 2008;3:S131–S139. doi: 10.2215/CJN.04151206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Cowin SC, Cardoso L. Blood and interstitial flow in the hierarchical pore space architecture of bone tissue. J Biomech. 2015;48:842–854. doi: 10.1016/j.jbiomech.2014.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].McCarthy I. The physiology of bone blood flow: a review. J Bone Joint Surg Am. 2006;88–A:4–9. doi: 10.2106/JBJS.F.00890. [DOI] [PubMed] [Google Scholar]
- [26].Cowin SC, Gailani G, Benalla M. Hierarchical poroelasticity: movement of interstitial fluid between porosity levels in bones. Philos Trans A Math Phys Eng Sci. 2009;367:3401–44. doi: 10.1098/rsta.2009.0099. [DOI] [PubMed] [Google Scholar]
- [27].Blanco E, Shen H, Ferrari M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat Biotechnol. 2015;33:941–951. doi: 10.1038/nbt.3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kim SM, Faix PH, Schnitzer JE. Overcoming key biological barriers to cancer drug delivery and efficacy. J Control Release. 2017 doi: 10.1016/j.jconrel.2017.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Moros M, Mitchell SG, Grazu V. The fate of nanocarriers as nanomedicines in vivo: important considerations and biological barriers to overcome. Curr Med Chem. 2013;20:2759–2778. doi: 10.2174/0929867311320220003. [DOI] [PubMed] [Google Scholar]
- [30].Cheng H, Chawla A, Yang Y, Li Y, Zhang J, Jang HL, Khademhosseini A. Development of nanomaterials for bone-targeted drug delivery. Drug Discov Today. 2017 doi: 10.1016/j.drudis.2017.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Cobo T, Viloria CG, Solares L, Fontanil T, González-Chamorro E, De Carlos F, Cobo J, Cal S, Obaya AJ. Role of periostin in adhesion and migration of bone remodeling cells. PLoS One. 2016;11:1–19. doi: 10.1371/journal.pone.0147837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Sarin H. Physiologic upper limits of pore size of different blood capillary types and another perspective on the dual pore theory of microvascular permeability. J Angiogenes Res. 2010;2:1–19. doi: 10.1186/2040-2384-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Torchilin VP. Multifunctional, stimuli-sensitive nanoparticulate systems for drug delivery. Nat Rev Drug Discov. 2014;13:813–827. doi: 10.1038/nrd4333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Setyawati MI, Tay CY, Docter D, Stauber RH, Leong DT. Understanding and exploiting nanoparticles’ intimacy with the blood vessel and blood. Chem Soc Rev. 2015;44:8174–99. doi: 10.1039/c5cs00499c. [DOI] [PubMed] [Google Scholar]
- [35].Williams EA, Fitzgerald RH, Jr, Kelly PJ. Physiol Pharmacol Microcirc. Academic Press; 1984. 8 - Microcirculation of Bone; pp. 267–323. A2 - Mortillaro, Nicholas A. BT - The Physiology and Pharmacology of the Microcirculation. [DOI] [Google Scholar]
- [36].Sou K, Goins B, Leland MM, Tsuchida E, Phillips WT. Bone marrow-targeted liposomal carriers: a feasibility study in nonhuman primates. Nanomedicine (Lond) 2010;5:41–9. doi: 10.2217/nnm.09.78. [DOI] [PubMed] [Google Scholar]
- [37].Lafage-Proust M-H, Roche B, Langer M, Cleret D, Vanden Bossche A, Olivier T, Vico L. Assessment of bone vascularization and its role in bone remodeling. Bonekey Rep. 2015;4:662. doi: 10.1038/bonekey.2015.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Moghimi SM. Exploiting bone marrow microvascular structure for drug delivery and future therapies. Adv Drug Deliv Rev. 1995;17:61–73. [Google Scholar]
- [39].Hillaireau H, Couvreur P. Nanocarriers’ entry into the cell: relevance to drug delivery. Cell Mol Life Sci. 2009;66:2873–2896. doi: 10.1007/s00018-009-0053-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Weinstein RS. Glucocorticoid-Induced Osteoporosis and Osteonecrosis. Endocrinol Metab Clin North Am. 2012;41:595–611. doi: 10.1016/j.ecl.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Ramasamy SK, Kusumbe AP, Schiller M, Zeuschner D, Bixel MG, Milia C, Gamrekelashvili J, Limbourg A, Medvinsky A, Santoro MM, Limbourg FP, et al. Blood flow controls bone vascular function and osteogenesis. Nat Commun. 2016;7 doi: 10.1038/ncomms13601. 13601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Griffith JF, Yeung DK, Tsang PH, Choi KC, Kwok TC, Ahuja AT, Leung KS, Leung PC. Compromised Bone Marrow Perfusion in Osteoporosis. J Bone Miner Res. 2008;23:1068–1075. doi: 10.1359/jbmr.080233. [DOI] [PubMed] [Google Scholar]
- [43].Ewalt MD, Gratzinger D. Selective quantitation of microvessel density reveals sinusoidal expansion in myelodysplastic syndromes. Leuk Lymphoma. 2016;57:2923–2926. doi: 10.3109/10428194.2016.1170829. [DOI] [PubMed] [Google Scholar]
- [44].Maeda H. Toward a full understanding of the EPR effect in primary and metastatic tumors as well as issues related to its heterogeneity. Adv Drug Deliv Rev. 2015;91:3–6. doi: 10.1016/j.addr.2015.01.002. [DOI] [PubMed] [Google Scholar]
- [45].Danhier F. To exploit the tumor microenvironment: Since the EPR effect fails in the clinic, what is the future of nanomedicine? J Control Release. 2016;244:108–121. doi: 10.1016/j.jconrel.2016.11.015. [DOI] [PubMed] [Google Scholar]
- [46].Maeda H, Tsukigawa K, Fang J. A Retrospective 30 Years After Discovery of the Enhanced Permeability and Retention Effect of Solid Tumors: Next-Generation Chemotherapeutics and Photodynamic Therapy—Problems, Solutions, and Prospects. Microcirculation. 2016;23:173–182. doi: 10.1111/micc.12228. [DOI] [PubMed] [Google Scholar]
- [47].Kinoshita R, Ishima Y, Chuang VTG, Nakamura H, Fang J, Watanabe H, Shimizu T, Okuhira K, Ishida T, Maeda H. Improved anticancer effects of albumin-bound paclitaxel nanoparticle via augmentation of EPR effect and albumin-protein interactions using S-nitrosated human serum albumin dimer. Biomaterials. 2017;140:162–169. doi: 10.1016/j.biomaterials.2017.06.021. [DOI] [PubMed] [Google Scholar]
- [48].Marenzana M, Arnett TR. The Key Role of the Blood Supply to Bone. Bone Res. 2013;1:203–215. doi: 10.4248/BR201303001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Dinenno FA, Tanaka H, Stauffer BL, Seals DR. Reductions in basal limb blood flow and vascular conductance with human ageing: role for augmented α-adrenergic vasoconstriction. J Physiol. 2001;536:977–983. doi: 10.1111/j.1469-7793.2001.00977.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Howlett CR, Dickson M, Sheridan AK. The fine structure of the proximal growth plate of the avian tibia: vascular supply. Anat J. 1984;139(Pt 1):115–32. [PMC free article] [PubMed] [Google Scholar]
- [51].Tavassoli M. The marrow-blood barrier. Br J Haematol. 1979;41:297–302. doi: 10.1111/j.1365-2141.1979.tb05862.x. [DOI] [PubMed] [Google Scholar]
- [52].Sou K, Goins B, Oyajobi BO, Travi BL, Phillips WT. Bone marrow-targeted liposomal carriers. Expert Opin Drug Deliv. 2011;8:317–28. doi: 10.1517/17425247.2011.553218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Porter CJ, Moghimi SM, Illum L, Davis SS. The polyoxyethylene / polyoxypropylene selectively redirects intravenously injected microspheres to sinusoidal endothelial cells of rabbit bone marrow. FEBS Lett. 1992;305:62–66. doi: 10.1016/0014-5793(92)80655-z. [DOI] [PubMed] [Google Scholar]
- [54].Mann AP, Tanaka T, Somasunderam A, Liu X, Gorenstein DG, Ferrari M. E-selectin-targeted porous silicon particle for nanoparticle delivery to the bone marrow. Adv Mater. 2011;23:278–282. doi: 10.1002/adma.201101541. [DOI] [PubMed] [Google Scholar]
- [55].Albanese A, Tang PS, Chan WCW. The Effect of Nanoparticle Size, Shape, and Surface Chemistry on Biological Systems. Annu Rev Biomed Eng. 2012;14:1–16. doi: 10.1146/annurev-bioeng-071811-150124. [DOI] [PubMed] [Google Scholar]
- [56].He C, Hu Y, Yin L, Tang C, Yin C. Effects of particle size and surface charge on cellular uptake and biodistribution of polymeric nanoparticles. Biomaterials. 2010;31:3657–3666. doi: 10.1016/j.biomaterials.2010.01.065. [DOI] [PubMed] [Google Scholar]
- [57].Salvati A, Pitek AS, Monopoli MP, Prapainop K, Bombelli FB, Hristov DR, Kelly PM, Aberg C, Mahon E, Dawson KA. Transferrin-functionalized nanoparticles lose their targeting capabilities when a biomolecule corona adsorbs on the surface. Nat Nano. 2013;8:137–143. doi: 10.1038/nnano.2012.237. [DOI] [PubMed] [Google Scholar]
- [58].Milani S, Baldelli Bombelli F, Pitek AS, Dawson KA, Rädler J. Reversible versus Irreversible Binding of Transferrin to Polystyrene Nanoparticles: Soft and Hard Corona. ACS Nano. 2012;6:2532–2541. doi: 10.1021/nn204951s. [DOI] [PubMed] [Google Scholar]
- [59].Sun S, BŁazewska KM, Kadina AP, Kashemirov BA, Duan X, Triffitt JT, Dunford JE, Russell RGG, Ebetino FH, Roelofs AJ, Coxon FP, et al. Fluorescent Bisphosphonate and Carboxyphosphonate Probes: A Versatile Imaging Toolkit for Applications in Bone Biology and Biomedicine. Bioconjug Chem. 2016;27:329–340. doi: 10.1021/acs.bioconjchem.5b00369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Peck EM, Battles PM, Rice DR, Roland FM, Norquest KA, Smith BD. Pre-Assembly of Near-Infrared Fluorescent Multivalent Molecular Probes for Biological Imaging. Bioconjug Chem. 2016;27:1400–1410. doi: 10.1021/acs.bioconjchem.6b00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Hayman AR. Tartrate-resistant acid phosphatase (TRAP) and the osteoclast/immune cell dichotomy. Autoimmunity. 2008;41:218–23. doi: 10.1080/08916930701694667. [DOI] [PubMed] [Google Scholar]
- [62].Paiva KBS, Granjeiro JM. Bone tissue remodeling and development: Focus on matrix metalloproteinase functions. Arch Biochem Biophys. 2014;561:74–87. doi: 10.1016/j.abb.2014.07.034. [DOI] [PubMed] [Google Scholar]
- [63].Uskokovic V. Nanostructured platforms for the sustained and local delivery of antibiotics in the treatment of osteomyelitis. Crit Rev Ther Drug Carrier Syst. 2015;32:1–59. doi: 10.1615/critrevtherdrugcarriersyst.2014010920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Tsai PF, Richards K, Tatom I. The association between knee temperature and pain in elders with osteoarthritis of the knee: A pilot study. J Adv Nurs. 2003;42:373–381. doi: 10.1046/j.1365-2648.2003.02629.x. [DOI] [PubMed] [Google Scholar]
- [65].Upreti M, Jyoti A, Sethi P. Tumor microenvironment and nanotherapeutics. Transl Cancer Res. 2013;2:309–319. doi: 10.3978/j.issn.2218-676X.2013.08.11. Tumor. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Yoneda T, Hiasa M, Nagata Y, Okui T, White FA. Acidic microenvironment and bone pain in cancer-colonized bone. Bonekey Rep. 2015;4:690. doi: 10.1038/bonekey.2015.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Hu Q, Katti PS, Gu Z. Enzyme-responsive nanomaterials for controlled drug delivery. Nanoscale. 2014;6:12273–12286. doi: 10.1039/c4nr04249b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Le Gall C, Bellahcène A, Bonnelye E, Gasser Ja, Castronovo V, Green J, Zimmermann J, Clézardin P. A cathepsin K inhibitor reduces breast cancer induced osteolysis and skeletal tumor burden. Cancer Res. 2007;67:9894–9902. doi: 10.1158/0008-5472.CAN-06-3940. [DOI] [PubMed] [Google Scholar]
- [69].Bühling F, Röcken C, Brasch F, Hartig R, Yasuda Y, Saftig P, Brömme D, Welte T. Pivotal Role of Cathepsin K in Lung Fibrosis. Am J Pathol. 2004;164:2203–2216. doi: 10.1016/S0002-9440(10)63777-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Pan H, Sima M, Miller SC, Kopečková P, Yang J, Kopeček J. Efficiency of high molecular weight backbone degradable HPMA copolymer-Prostaglandin E1 conjugate in promotion of bone formation in ovariectomized rats. Biomaterials. 2013;34:6528–6538. doi: 10.1016/j.biomaterials.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Hsu CW, Olabisi RM, Olmsted-Davis EA, Davis AR, West JL. Cathepsin K-sensitive poly(ethylene glycol) hydrogels for degradation in response to bone resorption. J Biomed Mater Res - Part A. 2011;98 A:53–62. doi: 10.1002/jbm.a.33076. [DOI] [PubMed] [Google Scholar]
- [72].Wang X, Yang Y, Jia H, Jia W, Miller S, Bowman B, Feng J, Zhan F. Peptide Decoration of Nanovehicles to Achieve Active Targeting and Pathology-Responsive Cellular Uptake for Bone Metastasis Chemotherapy. Biomater Sci. 2014;2:961–971. doi: 10.1039/C4BM00020J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Lynch CC. Matrix metalloproteinases as master regulators of the vicious cycle of bone metastasis. Bone. 2011;48:44–53. doi: 10.1016/j.bone.2010.06.007. [DOI] [PubMed] [Google Scholar]
- [74].Hou P, Troen T, Ovejero MC, Kirkegaard T, Andersen TL, Byrjalsen I, Ferreras M, Sato T, Shapiro SD, Foged NT, Delaissé J-M. Matrix metalloproteinase-12 (MMP-12) in osteoclasts: new lesson on the involvement of MMPs in bone resorption. Bone. 2017;34:37–47. doi: 10.1016/j.bone.2003.08.011. [DOI] [PubMed] [Google Scholar]
- [75].Raggatt LJ, Partridge NC. Cellular and molecular mechanisms of bone remodeling. J Biol Chem. 2010;285:25103–25108. doi: 10.1074/jbc.R109.041087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Sarkar N, Banerjee J, Hanson AJ, Elegbede AI, Rosendahl T, Krueger AB, Banerjee AL, Tobwala S, Wang R, Lu X, Mallik S, et al. Matrix metalloproteinase-assisted triggered release of liposomal contents. Bioconjug Chem. 2008;19:57–64. doi: 10.1021/bc070081p. [DOI] [PubMed] [Google Scholar]
- [77].Kulkarni PS, Haldar MK, Nahire RR, Katti P, Ambre AH, Muhonen WW, Shabb JB, Padi SKR, Singh RK, Borowicz PP. MMP-9 responsive PEG cleavable nanovesicles for efficient delivery of chemotherapeutics to pancreatic cancer. Mol Pharm. 2014;11:2390–2399. doi: 10.1021/mp500108p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Page-McCaw A, Ewald AJ, Werb Z. Matrix metalloproteinases and the regulation of tissue remodelling. Nat Rev Mol Cell Biol. 2007;8:221–33. doi: 10.1038/nrm2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Liu TW, Akens MK, Chen J, Wilson BC, Zheng G. Matrix metalloproteinase-based photodynamic molecular beacons for targeted destruction of bone metastases in vivo. Photochem Photobiol Sci. 2016;15:375–381. doi: 10.1039/c5pp00414d. [DOI] [PubMed] [Google Scholar]
- [80].Hatzenbuehler J, Pulling TJ. Diagnosis and Management of Osteomyelitis. Am Fam Physician. 2011;84:1027–1033. [PubMed] [Google Scholar]
- [81].Baier G, Cavallaro A, Vasilev K, Mailander V, Musyanovych A, Landfester K. Enzyme Responsive Hyaluronic Acid Nanocapsules Containing Polyhexanide and Their Exposure to Bacteria To Prevent Infection. Biomacromolecules. 2013;14:1103–1112. doi: 10.1021/bm302003m. [DOI] [PubMed] [Google Scholar]
- [82].Danhier F, Feron O, Préat V. To exploit the tumor microenvironment: Passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J Control Release. 2010;148:135–146. doi: 10.1016/j.jconrel.2010.08.027. [DOI] [PubMed] [Google Scholar]
- [83].Calderwood SK, Gong J. Heat Shock Proteins Promote Cancer: It’s a Protection Racket. Trends Biochem Sci. 2016;41:311–323. doi: 10.1016/j.tibs.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Liu D, Ma L, An Y, Li Y, Liu Y, Wang L, Guo J, Wang J, Zhou J. Thermoresponsive Nanogel-Encapsulated PEDOT and HSP70 Inhibitor for Improving the Depth of the Photothermal Therapeutic Effect. Adv Funct Mater. 2016;26:4749–4759. doi: 10.1002/adfm.201600031. [DOI] [Google Scholar]
- [85].Staruch R, Chopra R, Hynynen K. Hyperthermia in Bone Generated with MR Imaging-controlled Focused Ultrasound: Control Strategies and Drug Delivery. Radiology. 2012;263:117–127. doi: 10.1148/radiol.11111189. [DOI] [PubMed] [Google Scholar]
- [86].Song H, Zhang J, Liu X, Deng T, Yao P, Zhou S, Yan W. Development of drug loaded nanoparticles binding to hydroxyapatite based on a bisphosphonate modified nonionic surfactant. J Nanomater. 2015;2015:680–7. doi: 10.1155/2015/393968. [DOI] [Google Scholar]
- [87].Poh S, Lin JB, Panitch A. Release of Anti-inflammatory Peptides from Thermosensitive Nanoparticles with Degradable Cross-Links Suppresses Pro-inflammatory Cytokine Production. Biomacromolecules. 2015;16:1191–1200. doi: 10.1021/bm501849p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Cetin N, Aytar A, Atalay A, Akman MN. Comparing hot pack, short-wave diathermy, ultrasound, and TENS on isokinetic strength, pain, and functional status of women with osteoarthritic knees: a single-blind, randomized, controlled trial. Am J Phys Med Rehabil. 2008;87:443–451. doi: 10.1097/PHM.0b013e318174e467. [DOI] [PubMed] [Google Scholar]
- [89].Yang J, Van Lith R, Baler K, Hoshi RA, Ameer GA. A thermoresponsive biodegradable polymer with intrinsic antioxidant properties. Biomacromolecules. 2014;15:3942–3952. doi: 10.1021/bm5010004. [DOI] [PubMed] [Google Scholar]
- [90].Fleige E, Quadir MA, Haag R. Stimuli-responsive polymeric nanocarriers for the controlled transport of active compounds: Concepts and applications. Adv Drug Deliv Rev. 2012;64:866–884. doi: 10.1016/j.addr.2012.01.020. [DOI] [PubMed] [Google Scholar]
- [91].Zardad A-Z, Choonara Y, du Toit L, Kumar P, Mabrouk M, Kondiah P, Pillay V. A Review of Thermo- and Ultrasound-Responsive Polymeric Systems for Delivery of Chemotherapeutic Agents. Polymers (Basel) 2016;8:359. doi: 10.3390/polym8100359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Nahire R, Paul S, Scott MD, Singh RK, Muhonen WW, Shabb J, Gange KN, Srivastava DK, Sarkar K, Mallik S. Ultrasound enhanced matrix metalloproteinase-9 triggered release of contents from echogenic liposomes. Mol Pharm. 2012;9:2554–2564. doi: 10.1021/mp300165s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Crasto GJ, Kartner N, Reznik N, Spatafora MV, Chen H, Williams R, Burns PN, Clokie C, Manolson MF, Peel SAF. Controlled bone formation using ultrasound-triggered release of BMP-2 from liposomes. J Control Release. 2016 doi: 10.1016/j.jconrel.2016.09.032. [DOI] [PubMed] [Google Scholar]
- [94].Crasto GJ, Chen H, Kartner N, Reznik N, Peel SAF. Ultrasound triggered delivery of growth factors from liposomes for tissue regeneration. 2016 [Google Scholar]
- [95].Sawant S, Shegokar R. A2 - Grumezescu, Alexandru Mihai BT - Nanobiomaterials in Hard Tissue Engineering. William Andrew Publishing; 2016. Chapter 5 - Bone scaffolds: What’s new in nanoparticle drug delivery research? pp. 155–187. [DOI] [Google Scholar]
- [96].Nagao M, Tanabe N, Manaka S, Naito M, Nakai K, Takayama T, Kawato T, Torigoe G, Sekino J, Tsukune N, Maeno M, et al. LIPUS suppressed LPS-induced IL-1α through the inhibition of NF-κB nuclear translocation via AT1-PLCβ pathway in MC3T3-E1. J Cell Physiol. 2017 doi: 10.1002/jcp.25777. [DOI] [PubMed] [Google Scholar]
- [97].Puts R, Albers J, Kadow-Romacker A, Geissler S, Raum K. Influence of Donor Age and Stimulation Intensity on Osteogenic Differentiation of Rat Mesenchymal Stromal Cells in Response to Focused Low-Intensity Pulsed Ultrasound. Ultrasound Med Biol. 2016;42:2965–2974. doi: 10.1016/j.ultrasmedbio.2016.08.012. [DOI] [PubMed] [Google Scholar]
- [98].Li X-S, Li W-Q, Wang W-B. Using targeted magnetic arsenic trioxide nanoparticles for osteosarcoma treatment. Cancer Biother Radiopharm. 2007;22:772–8. doi: 10.1089/cbr.2007.352. [DOI] [PubMed] [Google Scholar]
- [99].Matsuo T, Sugita T, Kubo T, Yasunaga Y, Ochi M, Murakami T. Injectable magnetic liposomes as a novel carrier of recombinant human BMP-2 for bone formation in a rat bone-defect model. J Biomed Mater Res A. 2003;66:747–54. doi: 10.1002/jbm.a.10002. [DOI] [PubMed] [Google Scholar]
- [100].Guisasola E, Baeza A, Talelli M, Arcos D, Moros M, La Fuente JMD, Vallet-regí M, Guisasola E, Baeza A, Talelli M, Arcos D, et al. Magnetic-responsive Release Controlled by Hot Spot Effect Magnetic-responsive Release Controlled by Hot Spot Effect. Langmuir. 2015;31:12777–12782. doi: 10.1021/acs.langmuir.5b03470. [DOI] [PubMed] [Google Scholar]
- [101].Shido Y, Nishida Y, Suzuki Y, Kobayashi T, Ishiguro N. Targeted hyperthermia using magnetite cationic liposomes and an alternating magnetic field in a mouse osteosarcoma model. J Bone Joint Surg Br. 2010;92:580–585. doi: 10.1302/0301-620X.92B4.22814. [DOI] [PubMed] [Google Scholar]
- [102].Matsuoka F, Shinkai M, Honda H, Kubo T, Sugita T, Kobayashi T. Hyperthermia using magnetite cationic liposomes for hamster osteosarcoma. Biomagn Res Technol. 2004;2:3. doi: 10.1186/1477-044X-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Amstad E, Kohlbrecher J, Müller E, Schweizer T, Textor M, Reimhult E. Triggered release from liposomes through magnetic actuation of iron oxide nanoparticle containing membranes. Nano Lett. 2011;11:1664–1670. doi: 10.1021/nl2001499. [DOI] [PubMed] [Google Scholar]
- [104].Kraft JC, Freeling JP, Wang Z, Ho RJY. Emerging research and clinical development trends of liposome and lipid nanoparticle drug delivery systems. J Pharm Sci. 2014;103:29–52. doi: 10.1002/jps.23773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].McBain SC, Yiu HHP, Dobson J. Magnetic nanoparticles for gene and drug delivery. Int J Nanomedicine. 2008;3:169–180. doi: 10.2147/ijn.s1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Huang Z, Pei N, Wang Y, Xie X, Sun A, Shen L, Zhang S, Liu X, Zou Y, Qian J, Ge J. Deep magnetic capture of magnetically loaded cells for spatially targeted therapeutics. Biomaterials. 2010;31:2130–2140. doi: 10.1016/j.biomaterials.2009.11.062. [DOI] [PubMed] [Google Scholar]
- [107].Kanamala M, Wilson WR, Yang M, Palmer BD, Wu Z. Mechanisms and biomaterials in pH-responsive tumour targeted drug delivery: a review. Biomaterials. 2016;85:152–167. doi: 10.1016/j.biomaterials.2016.01.061. [DOI] [PubMed] [Google Scholar]
- [108].Pang X, Jiang Y, Xiao Q, Leung AW, Hua H, Xu C. pH-responsive polymer–drug conjugates: design and progress. J Control Release. 2016;222:116–129. doi: 10.1016/j.jconrel.2015.12.024. [DOI] [PubMed] [Google Scholar]
- [109].Schmaljohann D. Thermo- and pH-responsive polymers in drug delivery. Adv Drug Deliv Rev. 2006;58:1655–1670. doi: 10.1016/j.addr.2006.09.020. [DOI] [PubMed] [Google Scholar]
- [110].Torchilin V. Tumor delivery of macromolecular drugs based on the EPR effect. Adv Drug Deliv Rev. 2011;63:131–135. doi: 10.1016/j.addr.2010.03.011. [DOI] [PubMed] [Google Scholar]
- [111].Ferreira D dos S, Faria SD, de Lopes SCA, Teixeira CS, Malachias A, Magalhães-Paniago R, de Souza Filho JD, Oliveira de Jesus Pinto BL, Guimarães AR, Caravan P, et al. Development of a bone-targeted pH-sensitive liposomal formulation containing doxorubicin: Physicochemical characterization, cytotoxicity, and biodistribution evaluation in a mouse model of bone metastasis. Int J Nanomedicine. 2016;11:3737–3751. doi: 10.2147/IJN.S109966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Wang Y, Wang J, Hao H, Cai M, Wang S, Ma J, Li Y, Mao C, Zhang S. In Vitro and in Vivo Mechanism of Bone Tumor Inhibition by Selenium-Doped Bone Mineral Nanoparticles. ACS Nano. 2016;10:9927–9937. doi: 10.1021/acsnano.6b03835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Alpaslan E, Yazici H, Golshan NH, Ziemer KS, Webster TJ. pH-Dependent Activity of Dextran-Coated Cerium Oxide Nanoparticles on Prohibiting Osteosarcoma Cell Proliferation. ACS Biomater Sci Eng. 2015;1:1096–1103. doi: 10.1021/acsbiomaterials.5b00194. [DOI] [PubMed] [Google Scholar]
- [114].Gan Q, Zhu J, Yuan Y, Liu H, Qian J, Li Y, Liu C. A dual-delivery system of pH-responsive chitosan-functionalized mesoporous silica nanoparticles bearing BMP-2 and dexamethasone for enhanced bone regeneration. J Mater Chem B. 2015;3:2056–2066. doi: 10.1039/c4tb01897d. [DOI] [PubMed] [Google Scholar]
- [115].Ferreira SMZMD, Domingos GP, Ferreira DDS, Rocha TGR, Serakides R, De Faria Rezende CM, Cardoso VN, Fernandes SOA, Oliveira MC. Technetium-99m-labeled ceftizoxime loaded long-circulating and pH-sensitive liposomes used to identify osteomyelitis. Bioorganic Med Chem Lett. 2012;22:4605–4608. doi: 10.1016/j.bmcl.2012.05.105. [DOI] [PubMed] [Google Scholar]
- [116].C Y, Q C, L M, L J, H G, T G, Y Y, Z C, J Q. Alendronate-decorated biodegradable polymeric micelles for potential bone-targeted delivery of vancomycin. J Biomater Sci Polym Ed. 2015;26:629–643. doi: 10.1080/09205063.2015.1053170. [DOI] [PubMed] [Google Scholar]
- [117].Sethuraman VA, Lee MC, Bae YH. A biodegradable pH-sensitive micelle system for targeting acidic solid tumors. Pharm Res. 2008;25:657–666. doi: 10.1007/s11095-007-9480-4. [DOI] [PubMed] [Google Scholar]
- [118].Wu C, Wang S, Bruelisauer L, Leroux J, Gauthier MA. Broad control of disulfide stability through microenvironmental effects and analysis in complex redox environments. Biomacromolecules. 2013;14:2383–2388. doi: 10.1021/bm400501c. [DOI] [PubMed] [Google Scholar]
- [119].Turell L, Radi R, Alvarez B. Free Radical Biology and Medicine The thiol pool in human plasma : The central contribution of albumin to redox processes. Free Radic Biol Med. 2013;65:244–253. doi: 10.1016/j.freeradbiomed.2013.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [120].Drake MT, Clarke BL, Khosla S. Bisphosphonates : Mechanism of Action and Role in Clinical Practice. Mayo Clin Proc. 2008;83:1032–1045. doi: 10.4065/83.9.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Cheng R, Feng F, Meng F, Deng C, Feijen J, Zhong Z. Glutathione-responsive nano-vehicles as a promising platform for targeted intracellular drug and gene delivery. J Control Release. 2011;152:2–12. doi: 10.1016/j.jconrel.2011.01.030. [DOI] [PubMed] [Google Scholar]
- [122].Yang Y, Chen H, Vlahov IR, Cheng J-X, Low PS. Evaluation of disulfide reduction during receptor-mediated endocytosis by using FRET imaging. Proc Natl Acad Sci U S A. 2006;103:13872–13877. doi: 10.1073/pnas.0601455103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Zhang X, Han L, Liu M, Wang K, Tao L, Wan Q, Wei Y. Recent progress and advances in redox-responsive polymers as controlled delivery nanoplatforms. Mater Chem Front. 2017;1:807–822. [Google Scholar]
- [124].Baldwin AD, Kiick KL. Reversible maleimide–thiol adducts yield glutathione-sensitive poly(ethylene glycol)–heparin hydrogels. Polym Chem. 2012;4:133–143. doi: 10.1039/C2PY20576A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [125].Sun H, Meng F, Cheng R, Deng C, Zhong Z. Reduction-responsive polymeric micelles and vesicles for triggered intracellular drug release. Antioxid Redox Signal. 2014;21:755–67. doi: 10.1089/ars.2013.5733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [126].Talelli M, Barz M, Rijcken CJF, Kiessling F, Hennink WE, Lammers T. Core-crosslinked polymeric micelles: Principles, preparation, biomedical applications and clinical translation. Nano Today. 2015;10:93–117. doi: 10.1016/j.nantod.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127].Maciel D, Figueira P, Xiao S, Hu D, Shi X, Rodrigues J, Tomás H, Li Y. Redox-responsive alginate nanogels with enhanced anticancer cytotoxicity. Biomacromolecules. 2013;14:3140–3146. doi: 10.1021/bm400768m. [DOI] [PubMed] [Google Scholar]
- [128].Yao C, Liu J, Wu X, Tai Z, Gao Y, Zhu Q, Li J, Zhang L, Hu C, Gu F, Gao J, et al. Reducible self-assembling cationic polypeptide-based micelles mediate co-delivery of doxorubicin and microRNA-34a for androgen-independent prostate cancer therapy. J Control Release. 2016;232:203–214. doi: 10.1016/j.jconrel.2016.04.034. [DOI] [PubMed] [Google Scholar]
- [129].Li XJ, Ren ZJ, Tang JH. MicroRNA-34a: a potential therapeutic target in human cancer. Cell Death Dis. 2014;5:e1327. doi: 10.1038/cddis.2014.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [130].Lin JB, Poh S, Panitch A. Controlled release of anti-inflammatory peptides from reducible thermosensitive nanoparticles suppresses cartilage inflammation. Nanomedicine. 2016;12:2095–2100. doi: 10.1016/j.nano.2016.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [131].Flavahan WA, Gaskell E, Bernstein BE. Epigenetic plasticity and the hallmarks of cancer. Science (80-. ) 2017;357:el2380. doi: 10.1126/science.aal2380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [132].Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- [133].Leroux J. Drug Delivery: Too Much Complexity, Not Enough Reproducibility? Angew Chemie Int Ed. 2017 doi: 10.1002/anie.201709002. [DOI] [PubMed] [Google Scholar]
- [134].Mano JF. Stimuli-Responsive Polymeric Systems for Biomedical Applications. Adv Eng Mater. 2008;10:515–527. doi: 10.1002/adem.200700355. [DOI] [Google Scholar]
- [135].Lima AC, Alvarez-Lorenzo C, Mano JF. Design Advances in Particulate Systems for Biomedical Applications. Adv Healthc Mater. 2016;5:1687–1723. doi: 10.1002/adhm.201600219. [DOI] [PubMed] [Google Scholar]
- [136].Anchordoquy TJ, Simberg D. Watching the gorilla and questioning delivery dogma. J Control Release Off J Control Release Soc. 2017;262:87. doi: 10.1016/j.jconrel.2017.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]