Abstract
Objectives
Modelling and assessing the loss of geographical accessibility is key to support disaster response and rehabilitation of the healthcare system. The aim of this study was therefore to estimate postdisaster travel times to functional health facilities and analyse losses in accessibility coverage after Cyclones Idai and Kenneth in Mozambique in 2019.
Setting
We modelled travel time of vulnerable population to the nearest functional health facility in two cyclone-affected regions in Mozambique. Modelling was done using AccessMod V.5.6.30, where roads, rivers, lakes, flood extent, topography and land cover datasets were overlaid with health facility coordinates and high-resolution population data to obtain accessibility coverage estimates under different travel scenarios.
Outcome measures
Travel time to functional health facilities and accessibility coverage estimates were used to identify spatial differences between predisaster and postdisaster geographical accessibility.
Results
We found that accessibility coverage decreased in the cyclone-affected districts, as a result of reduced travel speeds, barriers to movement, road constraints and non-functional health facilities. In Idai-affected districts, accessibility coverage decreased from 78.8% to 52.5%, implying that 136 941 children under 5 years of age were no longer able to reach the nearest facility within 2 hours travel time. In Kenneth-affected districts, accessibility coverage decreased from 82.2% to 71.5%, corresponding to 14 330 children under 5 years of age having to travel >2 hours to reach the nearest facility. Damage to transport networks and reduced travel speeds resulted in the most substantial accessibility coverage losses in both Idai-affected and Kenneth-affected districts.
Conclusions
Postdisaster accessibility modelling can increase our understanding of spatial differences in geographical access to care in the direct aftermath of a disaster and can inform targeting and prioritisation of limited resources. Our results reflect opportunities for integrating accessibility modelling in early disaster response, and to inform discussions on health system recovery, mitigation and preparedness.
Keywords: international health services, organisation of health services, geographical mapping, risk management
Strengths and limitations of this study.
This is the first study presenting the applicability of postdisaster geographical accessibility modelling.
The approach enables quantification of disaster impacts on geographical healthcare accessibility to prioritise postdisaster interventions and to build resilience for future disasters.
To account for uncertainty of the assumed travel speeds, we considered −20% and +20% intervals on motorised travel speeds.
Data from various sources and administrative levels were combined to represent the postcyclone situation as realistically as possible, but since data gathering was ongoing, it was expected that some data were incomplete or not fully processed at the time of usage.
Our accessibility modelling assumes that patients always travel to the nearest health facility; however, literature has shown that patients sometimes bypass health facilities in search of higher-quality care in Mozambique.
Introduction
Geographical proximity to health facilities is a crucial aspect of accessibility, utilisation and the provision of health services to populations in need.1 Road networks and natural barriers (such as rivers, water bodies and flooded areas) are important factors that determine the geographical (ie, physical) accessibility of a population to the network of functional health facilities. During natural disasters, roads and health facilities are often damaged, yet healthcare demand rises substantially at the same time due to injuries and increased communicable disease risks.2 3 The interplay between the disruption of health infrastructure, transport network and the rise in healthcare demand is known to disable a large portion of the population’s access to care they need in the aftermath of a disaster.3 4 This is especially the case in already medically underserved regions, where the event can lead to new health disparities or exacerbate existing ones.2
In March and April 2019, two cyclones made landfall in Mozambique. This was the first time in history that two strong cyclones hit Mozambique consecutively in the same season.5 On 14 March 2019, tropical Cyclone Idai made landfall in Beira. Followed by a week of heavy rains and winds, the storm ended on 21 March 2019.6 In the middle of the humanitarian emergency response for Cyclone Idai, a second cyclone hit Northern Mozambique. Cyclone Kenneth, a category 4 cyclone and the strongest recorded cyclone on the African continent, made landfall in Pemba, Cabo Delgado on 25 April 2019.7 8 The two cyclones combined had a death toll of 648, with 603 fatalities due to Idai and 45 deaths caused by Kenneth, and left over 2.2 million people in need of humanitarian assistance.5 The cyclones’ destruction isolated entire communities for weeks due to flood waters, destroyed telecommunication networks and caused extensive road damage.9 10 In addition, stagnant waters, inability in accessing safe water and sanitation and overcrowding in temporary accommodation led to a cholera outbreak and a significant increase in malaria cases.5 8 11 12 Major damage to 113 health facilities was reported after both cyclones, causing severe disruption in health service provision and restricting the population’s access to adequate healthcare.13 14 Although many humanitarian actors have estimated substantial losses in healthcare accessibility and availability,5 9 10 13 15 the quantitative impact of Cyclones Idai and Kenneth on geographical accessibility to healthcare remains unknown. Modelling geographical accessibility and population coverage by means of travel time to health facilities can give important insights for targeting humanitarian action and preparing for future disasters in a coordinated manner.16
Currently, quantitative postdisaster accessibility assessments are not a part of standardised response guidelines, preventing coordinated and centralised decision making on temporary facility location to serve beneficiaries in the most optimal way.16 Guidelines for a postdisaster needs assessment from WHO,17 advise on a comparison between baseline and postdisaster accessibility through the evaluation of key indicators. However, the suggested key indicators reflect rather static measures of accessibility, such as hospital beds per 10 000 population or number of damaged health facilities.17
Yet, international efforts to support humanitarian responses on the ground accelerate postdisaster data gathering, enabling a more realistic quantification of accessibility to healthcare by means of health facility damages, loss of road access and barriers to movement such as flood waters.18 Guidance on assessing loss in geographical accessibility while considering spatial barriers remains abstract or even lacking in disaster management frameworks. Meanwhile, geographical accessibility models hold actionable information and have the potential to quantify gaps and overlaps in (temporary) service provisioning, enabling coordinated, targeted and centralised decision making for humanitarian action,16 enhancing both financial and operational efficiency.19 20
This study therefore presents a data processing and spatial accessibility modelling method to assess postdisaster accessibility to health facilities and analyse accessibility coverage losses as a result of Cyclones Idai and Kenneth in Mozambique. The approach enables quantification of disaster impacts on geographical healthcare accessibility to prioritise postdisaster interventions and to build resilience for future disasters. This is the first study presenting the applicability of postdisaster geographical accessibility modelling.
Methods
Overall methodology
In this study, accessibility is measured as the travel time to health facilities and accessibility coverage (ie, coverage) is defined as the estimated number or percentage of people covered or located within a travel time catchment area.21 To model accessibility to health facilities, we consider topography, road networks, constraints to movement (eg, rivers, lakes and flood extent), target population distribution and the locations of functional health facilities. We accessed and prepared multiple data layers (table 1) assembled in the aftermath of Cyclones Idai and Kenneth, between April and September 2019. A total of three scenarios were prepared, representing (1) pre-Idai and pre-Kenneth (before March 2019), (2) post-Idai (up to 1 week postcyclone) and (3) post-Kenneth (up to 1 week postcyclone) situations. We modelled population travel time to the nearest health facility and accessibility coverage for two cyclone-affected regions.
Table 1.
Overview of data layers and data sources
| Layer name | Source | Source date* | Download date | Type | Original resolution |
| Administrative boundaries | INE & UN-OCHA ROSEA (HDX)55 | 02.04.19 | 31.07.19 | Polygons | – |
| Cyclone trajectory (Idai/Kenneth) |
GDACS56 57 | 15.03.19/ 25.04.19 |
08.03.20 | Polygons | – |
| Land cover | Copernicus25 | 15.11.18 | 31.07.19 | Raster | 100 m |
| Elevation | SRTM CGIAR54 | 25.11.18 | 20.09.19 | Raster | 30 m |
| Rivers and lakes | DNGRH | 12.8.19 | 19.9.19 | Polygons | – |
| Primary streams | DNGRH | 12.8.19 | 19.9.19 | Lines | – |
| Flood extent, Idai | UNOSAT/Sentinel-1 (HDX)28 | 19.03.19 | 31.07.19 | Polygons | – |
| Flood extent, Kenneth | Copernicus EMSR354 (INGC Geonode)29 | 02.05.19 | 31.07.19 | Polygons | – |
| Roads | OpenStreetMap (INGC Geonode)58 | 25.11.18 | 07.08.19 | Lines | – |
| Road damages (Idai/Kenneth) | LOG-WFP59 60 | 19.03.19/ 03.05.19 |
23.09.19 | PDF file | – |
| Health facilities | SIS-MA (HDX)35 | 31.12.17 | 08.08.19 | Points | – |
| Health facilities damages | Provided by WHO-Mozambique | Represents health facility status 48 hours until 1 week postcyclone | 17.09.19 | Points | – |
| Population density | Facebook/CIESIN population density32 | 01.10.18 | 06.08.19 | Raster | 30 m |
*Source date represents the imagery acquisition date for the flood extents and the release date for all other data.
CIESIN, Centre for International Earth Science Information Network; DNGRH, National Directorate for Water Resource Management; GDACS, Global Disaster Alert and Coordination System; HDX, Humanitarian Data Exchange; INE, National Institute for Statistics Mozambique; INGC, National Institute for Disaster Management Mozambique; LOG-WFP, Logistics Cluster World Food Programme; UN-OCHA ROSEA, United Nations Office for the Coordination of Humanitarian Affairs Southern and Eastern Africa; SIS-MA, Ministry of Health Mozambique; SRTM, Shuttle Radar Topography Mission; UNOSAT, United Nations Operational Satellite Applications Programme.
Data sources and preparation
The projection, resolution and alignment of geospatial data were processed using Quantum Geographical Information System (V.3.4)22 and, to a limited extent, R (V.3.5.2).23 As indicated in table 1, most data layers were retrieved from open data platforms. All rasters and shapefiles were saved in the projection system of Mozambique, that is, UTM-37S (EPSG:32 737). The data preparation process is briefly described in this section and is fully detailed in online supplemental file 1.
bmjopen-2020-039138supp001.pdf (444.6KB, pdf)
Elevation data were obtained from the Shuttle Radar Topography Mission in tiles at a resolution of 30 m and mosaiced to cover the whole country.24 Slopes were derived from it and were accounted for when modelling walking movements.
Land cover data were downloaded for the whole African continent at 100 m resolution from Copernicus Global Land Service25 and were clipped to the extent of Mozambique. As analyses were carried out at 30 m resolution, the land cover raster was resampled at a resolution of 30 m, using nearest neighbour interpolation.
The precyclone road network dataset was retrieved from Open Street Map (OSM) through the Geonode Platform of the National Institute for Disaster Management Mozambique, and linked to the road damage information as indicated by the Logistics Cluster of the World Food Programme (LOG-WFP).26 27 Historical postcyclone status of roads and road segments were manually digitised from PDF maps provided by LOG-WFP. The maps were cross-referenced with the OSM road network layer, to include postcyclone road damage status, that is, (1) open, (2) restricted and (3) closed. Road damages as a consequence of Cyclones Idai and Kenneth were taken from maps dated 19 March and 3 May 2019, respectively (table 1).26 27 Information on road type and damage were combined in order to obtain unique road type-damage combinations (online supplemental file 2).
Information on rivers and lake layout were obtained as shapefiles from the National Directorate for Water Resource Management. Only primary rivers and lakes were considered as barriers to movement, under the informed assumption that smaller rivers and streams were passable by the population. This assumption was checked for several instances against background satellite imagery. Flood extents for Idai (on 19 March 2019) and Kenneth (on 2 May 2019) were sourced as shapefiles from Sentinel-1 and Copernicus EMSR354, respectively.28 29 The flood extents were visually inspected and found to be largest on those two dates, and thus represent the biggest constraints for healthcare access. All flooded areas were treated under two scenarios: 1) as being impassable, under the assumption that people avoid traversing flood water to prevent further injury, 2) as being passable by foot at an average walking speed of 1.5 km/hour. In the first scenario, health facilities located on flood extents were always treated as inaccessible since they are located on barriers.
While cyclones impact entire populations, the burden disproportionately affects children and women.30 It is estimated that for Cyclones Idai and Kenneth >50% of the affected population were children, and with flood waters rising above 6 m, their movements to safety and healthcare were particularly limited.5 Moreover, children under 5 years of age represent the age group used as benchmark for child survival targets in both the Millennium Development Goals and the Sustainable Development Goals.31 In this context and through the collaborative work with UNICEF, this analysis aimed at informing the impact of the disasters on the burden for specific child health services that target children under 5 years of age (eg, immunisation).
High-resolution population density estimates for children under 5 years of age were obtained from the Facebook Connectivity Lab and Center for International Earth Science Information Network (CIESIN)32 with a 30 m resolution. Although several gridded populations datasets are available, the Facebook CIESIN dataset was assumed to have the most realistic reallocation of population to settlements.33 In addition, other frequently used high-resolution gridded population datasets, such as WorldPop,34 use distances from roads and villages as covariates, and this can produce collinearity when used in conjunction with accessibility models. Population density was used to run zonal statistics on the cyclone-affected districts. In this step, the total population per district is summed and the estimated absolute number of children under 5 years of age that are able to reach a facility in a predefined travel time catchment are calculated.
Additionally, geographic coordinates of all villages (ie, communities) in Idai-affected districts were obtained from UNICEF Mozambique, which had gathered this information through a community mapping initiative conducted by health officials, 6–8 months before Cyclone Idai made landfall. These community locations were used to extract precyclone and postcyclone travel time for each community to the nearest functional health centre. Unfortunately, geographic coordinates of villages in Kenneth-affected districts were not available at the time of study.
The geographic coordinates of all health facilities were sourced from the health management information system, Ministry of Health in Mozambique.35 Data cleaning was undertaken in cases where the geographic coordinates for health facilities were located outside the international border of Mozambique or for coordinates falling on barriers to movement (online supplemental file 1). Information on damaged health facilities was provided in tabular format by WHO. The health system in Mozambique comprises four levels: the primary level consists of urban and rural health centres, the secondary level consists of general, rural and district hospitals, the tertiary level comprises provincial capital hospitals and quaternary facilities comprise the central and specialised hospitals.36 Health facilities of all levels were included in the model.
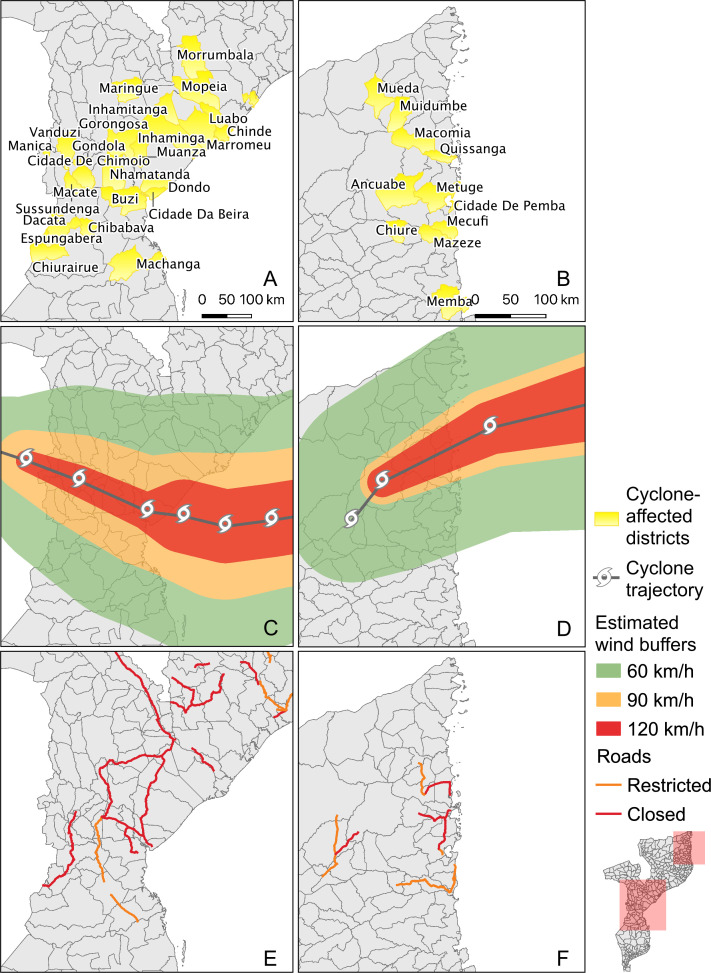
Districts that were most affected by Cyclones Idai and Kenneth (‘cyclone-affected districts’, thereafter) were identified in close collaboration with UNICEF and humanitarian responders. All statistics presented below were calculated for these identified districts, with 26 such districts in the Idai-affected region and 11 districts in the Kenneth-affected region (figure 1A, B). Storm trajectories of both cyclones and road damages in both districts are also presented (figure 1C-F).
Figure 1.
Cyclone-affected districts, cyclone trajectory and road damages. (A) Idai-affected districts. (B) Kenneth-affected districts. (C) Idai cyclone trajectory*. (D) Kenneth cyclone trajectory*. (E) Road damages in Idai-affected districts. (F) Road damages in Kenneth-affected districts. *Cyclone paths as reported on Global Disaster Alert and Coordination System.
Geographical accessibility modelling
To model travel times and accessibility coverages, we used AccessMod 5 (V.5.6.30), in particular the ‘accessibility’ and ‘zonal statistics’ modules.21 37 AccessMod models geographical accessibility using terrain-based least-cost path distance calculation. This open-source software has been successfully applied in many different settings, among which accessibility and referral assessments of health facility networks, optimisation modelling of health programmes in obstetric and neonatal care (EmONC),38 primary health care,39 emergency care,40 referral times41 and treatment of fever cases.42
Using the ‘merge land cover’ module in AccessMod, we overlaid the roads, rivers, lakes, flood extent and land cover datasets to obtain a single 30 m resolution raster dataset, to which different travel scenarios were applied.
The travel scenarios (presented in online supplemental file 2) were derived using local information as model inputs on precyclone and postcyclone travel speeds and travel modes. Both scenarios were developed in close collaboration with UNICEF Mozambique, with focus on geographical accessibility to functional health facilities for the target population of children under 5 years of age. Postcyclone travel speeds were adjusted for wet weather conditions as heavy rains persisted in the direct aftermath of both cyclones. During the postcyclone situation, restricted and closed roads that were not inundated were assumed to be unpassable by any vehicle, but they were perceived to be accessible by foot. All land cover classes outside of the road network and the barriers were considered as passable. We assumed a functional bridge where a road segment crossed a river.
To account for uncertainty of the assumed travel speeds, we also considered both precyclone and postcyclone motorised travel speeds with a 20% slower and 20% faster speed, as adapted from Ouma et al.40 Accessibility coverage of the network of health centres was calculated at the 2 hour maximum travel time limit. This limit was deemed appropriate to capture the extent of effective access, and is often used in health accessibility studies, notably in maternal health.38
Patients and the public involvement
There was no patient or public involvement in this study. Health facility functionality status was shared in tabular format by WHO. All other geospatial data were publicly available.
Results
All statistics mentioned in the results are estimates of children covered by functional health facilities based on our accessibility model.
Precyclone accessibility
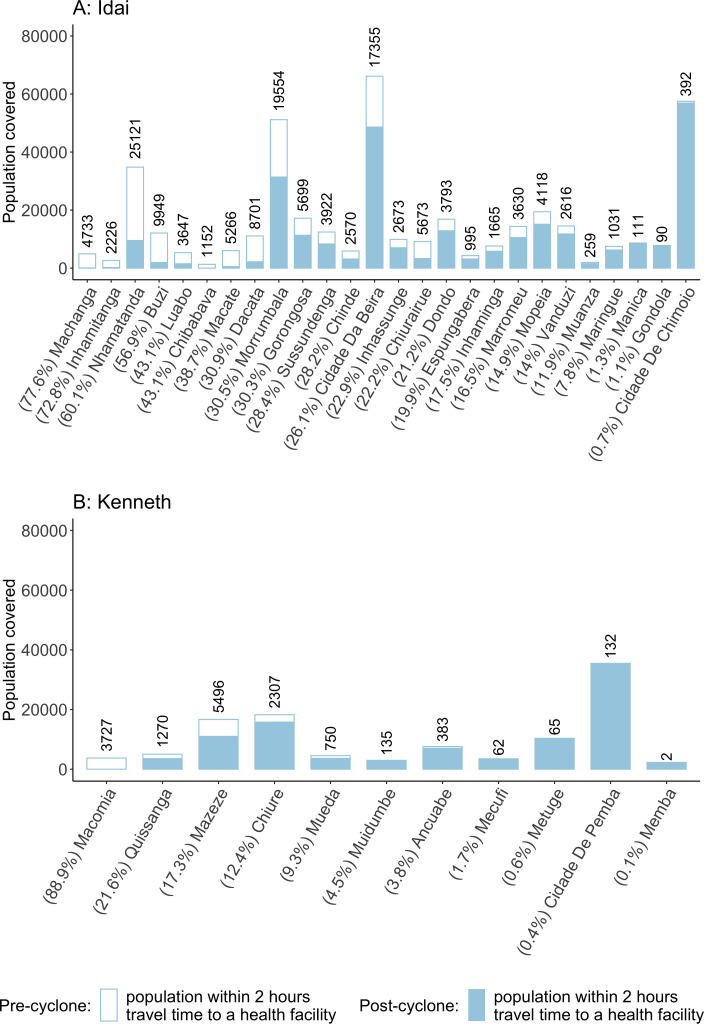
Precyclone coverage in Idai-affected districts (figure 2A) was highest in Cidade De Chimoio and Cidade Da Beira, with 99.8% and 99.5% of all children under 5 years of age covered within the 2-hour catchment limit, respectively (online supplemental file 3). However, this coverage ranged from 35.8% to 99.8% in all Idai-affected districts (online supplemental file 3). Absolute precyclone coverage was also highest in Cidade De Chimoio and Cidade Da Beira, where 57 476 and 66 135 children were within 2 hours travel time from a health facility (figure 2). In Kenneth-affected districts (figure 2B), precyclone coverage was highest in Cidade De Pemba, where 100% of the children under 5 years of age were expected to be able to reach a health facility within 2 hours travel time (online supplemental file 4). The lowest pre-cyclone coverage was seen in Mazeze, where only 52.6% of children under 5 were within 2 hours travel time from a health facility (online supplemental file 4). Absolute precyclone coverage in Kenneth-affected districts was highest in Cidade De Pemba (n=35 467 children) and Chiure (n=18 257 children) (figure 2). Precyclone travel time rasters for the cyclone-affected areas were mapped (figures 3A and 4A).
Figure 2.
Absolute and relative reduction in accessibility coverage precyclone and postcyclone Idai (A) and Kenneth (B). Labels on top of bars indicate absolute reduction in accessibility coverage of children under 5 years of age. Labels under districts indicate relative reduction in accessibility coverage. Maximum limits of the bars indicate the absolute precyclone coverage within 2 hours travel time. Limits of the blue filled bar indicate the absolute postcyclone coverage. The x-axis is ordered according to relative reduction in population coverage.
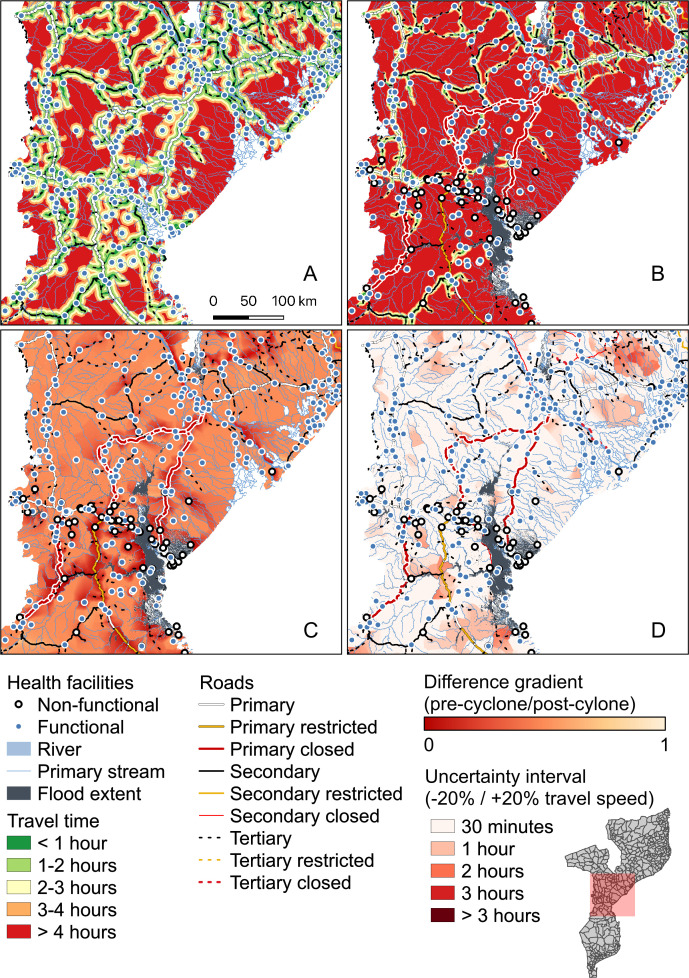
Figure 3.
Accessibility modelling results for Idai districts. Precyclone travel time raster (A). Postcyclone travel time raster (B). Difference ratio raster between precyclone and postcyclone travel time (C). Uncertainty raster, as a result of the difference between −20% and +20% travel speed accessibility (D).
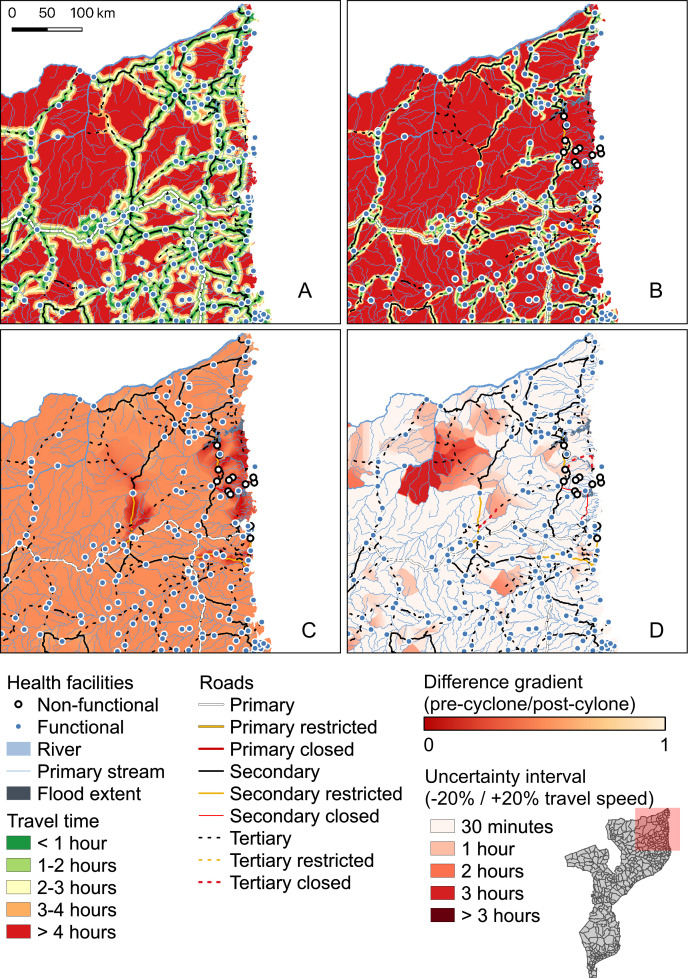
Figure 4.
Accessibility modelling results in Kenneth districts. Precyclone travel time raster (A). Postcyclone travel time raster (B). Difference ratio raster between precyclone and postcyclone travel time (C). Uncertainty raster, as a result of the difference between −20% and +20% travel speed accessibility (D).
Losses in accessibility coverage
Geographical accessibility to healthcare decreased in the cyclone-affected districts, as a result of reduced travel speeds, road constraints and non-functional health facilities (figures 3B and 4B). Ratios of precyclone and postcyclone travel time rasters are mapped for Idai-affected districts, with ratios close to 1 indicating similar travel times precyclone and postcyclone, and ratios closer to 0 indicating large precyclone and postcyclone accessibility differences (figure 3C). The same results for Kenneth-affected districts are presented (figure 4C). Regions shown in red indicate localities with relatively large differences between precyclone and postcyclone travel times (figure 3C). In the Idai-affected region, especially in the districts surrounding the flood water and closed roads, accessibility is severely impacted. In Idai-affected districts, the percentage of children under 5 years of age covered within 2 hours travel time generally decreased from 78.8% to 52.5%, implying that 136 941 previously covered children under 5 years of age lost timely access to healthcare (table 2).
Table 2.
Overview of precyclone and postcyclone accessibility coverage in Idai-affected and Kenneth-affected districts
| Cyclone | Travel time | Precyclone | Postcyclone | ||||
| Children <5 covered (no.) | Children <5 covered (%) | Children <5 covered (no.) | Children <5 covered (%) | Children <5 coverage loss (no.) | Children <5 coverage loss (%) | ||
| Idai | 30 min | 298 432 | 57.3 | 153 842 | 29.5 | 144 591 | 27.7 |
| 1 hour | 346 409 | 66.5 | 206 610 | 39.6 | 139 799 | 26.8 | |
| 2 hours | 410 696 | 78.8 | 273 755 | 52.5 | 136 941 | 26.3 | |
| Kenneth | 30 min | 131 120 | 72.0 | 63 953 | 48.8 | 30 415 | 23.2 |
| 1 hour | 99 056 | 73.8 | 86 997 | 64.8 | 12 060 | 9.0 | |
| 2 hours | 110 348 | 82.2 | 96 019 | 71.5 | 14 330 | 10.7 | |
The largest relative accessibility coverage decline, within 2 hours travel time, was observed in Machanga, where 77.6% of the previously covered population was no longer able to access a facility under 2 hours in the aftermath of Idai (figure 2). In terms of absolute coverage, Nhamatanda was the most affected district, with a coverage loss of 25 121 children under 5 years of age, followed by Morrumbala (n=19 554 children), Cidade Da Beira (n=17 355 children) and Bùzi (n=9949 children) (figure 2). Uncertainty modelling, by accounting for 20% slower and 20% faster motorised travel speeds,40 indicated localities with travel time differences up to 3 hours comparing slower and faster travel speeds (figures 3D and 4D). This information indicates where our travel time assumptions have the largest effect on accessibility and coverage losses and where this may be either underestimated or overestimated, which can help guide resource allocation for decreasing this uncertainty.
Relative accessibility coverage in all Kenneth-affected districts decreased from 82.2% to 71.5%, corresponding to 14 330 children having lost access to the nearest facility within 2 hours travel time (table 2). The most affected district in terms of relative coverage loss was Macomia, where 88.9% of the children that were covered precyclone lost access (online supplemental file 3 and 4). Mazeze was the most affected district in terms of absolute coverage loss, as 5496 children lost access in the aftermath of Cyclone Kenneth, followed by Macomia (n=3727 children), Chiure (n=2307 children), Quissanga (n=1270 children) and Mueda (n=750 children) (figure 2).
Since flood waters slowly receded in the days/weeks after the cyclones, we ran an additional scenario where flood waters were passable at a 1.5 km/hour walking speed. Considering this scenario, absolute coverage losses for Idai-affected districts within 2 hours travel time were highest in Morrumbala (n=29 566 children), Nhamatanda (n=25 758 children), Dacata (n=8914 children) and Bùzi (n=8757 children). In Kenneth-affected districts, Mazeze (n=6167 children), Chiure (n=4684 children) and Macomia (n=3727 children) had the highest coverage losses in 2-hour catchments under the passable scenario.
Travel time in affected communities
The most affected villages in Idai-affected districts, in terms of reduced accessibility to the nearest health facility, were communities located in Bùzi and Muanza districts in Sofala province. Mucinemo in Bùzi district was found to have a precyclone travel time of 1.3 hours to the nearest health facility. However, this travel time upsurged to 63.6 hours in the direct aftermath of Cyclone Idai (online supplemental file 5 and 6). Generally, the six most affected communities in terms of accessibility in Idai-affected districts all had a precyclone travel time between 1 hour and 3 hours, while all postcyclone travel times increased to over 55 hours (online supplemental file 5 and 6). Overall, postcyclone accessibility ranged from some minutes up to 78 hours, with the highest travel time found in Chipota, in Muanza district.
Health facility closures
The effects of non-functioning health facilities were isolated by comparing two separate scenarios: (1) a postcyclone scenario where all health facilities were considered functional and (2) a postcyclone scenario where modified functionality status was considered. By comparing these precyclone and postcyclone scenarios, the coverage losses caused by the transportation-specific disruptions (ie, adjusted travel speeds and road constraints) could be isolated from the reduction in coverage due to the damage to health facilities (ie, non-functional health facilities), providing a way to assess the likely impact of future programmes aimed at reinforcing health facilities for disasters. In order to make these comparisons in this specific example, both scenarios were run under the assumption that flood waters were fully passable. In all other instances throughout the paper, flood waters were considered impassable. In case all health facilities remained functional in Idai-affected districts (ie, disruption was due to transportation only), the overall coverage within 2 hours travel time would decrease from 79.3% to 57.7%, a difference of 21.6% (n=112 538 children). Damage to health facilities caused an additional coverage decline of 5.3% (n=27 840 children) in Idai-affected districts. However, hospital closures did not evenly affect all districts. In 17 out of 26 Idai-affected districts, hospital closures had no additional effect on accessibility. However, in the remaining nine Idai-affected districts, hospital closures were responsible for an additional 1.9%–59.7% coverage loss within 2 hours catchment. Health facility closures in Machanga affected the relative coverage the most, with 59.7% coverage loss (n=3642 children) caused by non-functionality of three out of six health facilities. Absolute coverage losses as an effect of non-functional health facilities were highest in Nhamatanda, where 12 946 (31.0%) children under 5 years of age lost access due to health facility closures. In Nhamatanda, 9 out of 16 health facilities became unfunctional as a consequence of Cyclone Idai. Health facility closures did not have an additional effect on postcyclone accessibility in Kenneth-affected districts.
Discussion
Accessibility coverage decreased and travel times substantially increased in the direct aftermath of the cyclones. Damage to transport networks and reduced travel speeds resulted in the most substantial accessibility coverage losses in both Idai-affected and Kenneth-affected districts. In Kenneth-affected districts, it was found that hospital closures did not have an additional effect on postcyclone accessibility; this is likely caused by the fact that flood extents and hospital closures were of much smaller magnitudes in the Kenneth-affected region than in the Idai-affected region.
In a postdisaster setting, access to healthcare is essential for effective response and recovery.43 The results of our study can be implemented beyond the response phase of the cyclones. Although the emphasis of the results is on identification of decreased accessibility coverage directly after the cyclones, the information presented here also provides a platform for discussing health system recovery, mitigation and preparedness.44
Early identification of underserved districts in the response phase can help reduce the impacts caused by health service interruption, through targeted deployment of medical services in districts with the largest accessibility coverage losses and lowest baseline accessibility.45 Information on accessibility coverage losses per cyclone-affected district can support decision-making in the prioritisation and planning of these medical services, by targeting where the deployment of medical services reaches the highest number of people. Growing access to open data and postdisaster information enables prompt accessibility modelling in the aftermath of a natural disaster and the growing ability to quickly assemble these data provides an opportunity to integrate accessibility modelling in the early response phase of a natural disaster, so resources can be allocated in an informed way and health impacts can be reduced. In this specific study, all data for an initial postcyclone accessibility study became available between 1 week and 1 month postdisaster (table 1). This allows for an accessibility analysis in the early stages of a disaster response. Generally, data on flood extents and road damages, acquired from satellite imagery, were downloadable within 1 week postdisaster. Whereas information that had to be ground validated, such as health facility functionality, became available approximately 1 month postdisaster.
Furthermore, the extensive damages to the road network will continue to limit movements of the population, further complicating physical accessibility.5 Our results indicate that road damages are responsible for a relatively large loss of accessibility. This calls for a concerted effort between road and health authorities when prioritising reconstruction efforts. It was estimated by WHO that damages to (health) infrastructure translated into 200 000 people living >5 km from a functioning health facility.46 However, our results, which provide a more realistic representation of accessibility, by accounting for topography, barriers to movement and population distribution, suggest this figure is an underestimate. We estimated that as a result of the damage to infrastructure and barriers to movement, 314 591 children under 5 years of age live further than 1 hour travelling from a functioning health facility.
Fourteen per cent of all health facilities in Idai-affected and Kenneth-affected districts have been damaged or fully destroyed, although more health facilities were temporarily impacted in service provisioning due to flooding, electricity constraints or damage to equipment.14 47 While it is critical to restore access to essential health services as soon as possible, WHO reported that the reconstruction of all destructed and damaged facilities may take up to 5 years14. To restore baseline accessibility, the establishment of mobile outreach units, deployment of community health workers (CHWs), together with the reconstruction of damaged facilities should be implemented. However, under the umbrella of Building Back Better, rebuilding more resilient facilities and infrastructure, that are able to withstand future hazards under the ‘Hospitals Safe from Disasters’ approach, are needed to prevent similar impacts in future disasters.46 47 The results presented here show the importance of joint efforts to reduce both impacts on health facilities and the existing road network. However, resources are limited, and efficient financial planning is needed to outline health system investment plans.5 11 The results of our accessibility modelling can be used to prioritise health facility reconstruction for facilities with highest accessibility coverages. Cyclone Idai for instance, caused the destruction of the only tertiary hospital in four affected provinces that serves an estimated 12 million people.43 Targeting hospitals with coverage numbers like these, to be strengthened for future disaster impacts and to support them in providing continuity of care in the aftermath of future disasters can help reduce health losses.48
Due to the persisting health system disruption, humanitarian responders have identified the need to deploy CHWs and mobile outreach services to cover accessibility losses caused by the cyclones and to extend the reach of existing functional services.43 49 These study findings can assist policymakers in identifying and prioritising severely impacted districts and communities and regions where deployment of CHWs can make a difference. Online supplemental file 3-6 present the most affected communities in terms of increased travel time and coverage losses postcyclone. These analyses can be routinely updated to assess the effect of health system recovery on accessibility.
The districts that were most affected by Cyclones Idai and Kenneth were historically, and are in the future, also prone to disasters due to their topography (ie, due to their location as low-lying coastal cities in the cyclone belt near the Indian Ocean).43 46 Ideally, accessibility modelling could be applied to simulate the effects of historical disasters on accessibility, as indicated in online supplemental file 5 and 6, so targeted preventive measures can be taken for future disasters. Postdisaster accessibility modelling can help identify weak spots in geographical accessibility to the health system and helps to distinguish pre-existing accessibility gaps (figures 3A and 4A) from accessibility coverage losses as a result of disasters (figures 3B and 4B). This information is essential in health system recovery, strengthening and preparing for future disasters.
Limitations and uncertainties of this study were primarily linked to the data. While the occurrence of natural disasters generally accelerates data availability in affected countries, there also are challenges of data quality, consistency and format.50 In this study, data from various sources were combined to represent the postcyclone situation as realistically as possible. But since data gathering was ongoing, it was expected that some data were incomplete or not fully processed at the time of usage. Health facility coordinates had duplicate occurrences in the database and health facility damages were solely indicated by name, which resulted in manual spatial merging. Co-occurrences of rivers that were indicated as floods were seen in the flood extent layer, minimally overestimating actual flood extents in some parts of the affected regions. Besides postdisaster data uncertainty, predisaster spatial data were also checked against background satellite imagery. The hydrography of primary rivers stored in the data was found not to be fully representative for actual hydrography in some regions. This could be a consequence of digitising against a less granular spatial resolution.51 In some cases, passages and bridges were detected on satellite background imagery where the OpenStreetMap road layer did not present presence of roads. In places where hydrography was potentially overestimated and not all roads are mapped, isolated land pockets were created in the merged land cover. When modelling accessibility in these land pockets, the population is assumed to be fully isolated from healthcare. In general, we would advise on a more rigorous and sustainable data management during and after humanitarian emergency operations to ensure the applicability of spatiotemporal data analyses to quantify disaster impacts.
Next to data uncertainties, travel scenarios present a source of uncertainty as assumptions on travel speeds and modes are uniformly generalised across regions. In addition, we assumed that roads indicated as being restricted or closed were considered only passable by foot if they were not inundated. However, some of the restricted roads were in fact passable by 4×4 vehicles. Other means of transport (eg, bicycle, motorcycle) may also have been used in some places, which would increase accessibility to health centres. Since car ownership and access to motorised transport by the target population was expected to be very low, especially postcyclone, it was decided to run the accessibility model for restricted and closed roads only by means of walking.
Our accessibility modelling assumes that patients always travel to the nearest health facility. However, literature has shown that patients sometimes bypass health facilities in search of higher quality care in Mozambique.52 53 Previous research, has shown that 30.8% of pregnant women bypassed the nearest health facility in search of better prenatal care.52 Our results can therefore present slight underestimations of actual travel times.
Despite some of the limitations, the results presented here provide important initial information for postcyclone health system recovery which can be expanded through future research. Since postdisaster needs continuously change based on the nature of the event (eg, receding flood waters, reconstruction efforts and deployment of temporary medical services), following studies should also be focused on the ability to dynamically model accessibility based on these changes, so accessibility can be continuously monitored and humanitarian service delivery can be updated accordingly in disaster-affected districts. Additionally, it would be interesting to assess the effect of CHW deployment and mobile outreach communities on improved accessibility and accessibility coverage estimates, to quantify the effect of these interventions.
Postdisaster accessibility modelling can increase our understanding of spatial differences in healthcare needs in the direct aftermath of a disaster and can help target limited resources efficiently. Currently, there is no standardised approach in the humanitarian programme cycle to assess postdisaster accessibility losses against baseline accessibility.17 The lack of a standardised methodology to spatially assess disaster impacts on accessibility can result in uncoordinated decision making for temporary health facility locations, introducing duplication probability, and complicates prioritisation in recovery efforts. The results in this paper reflect the importance of incorporating accessibility modelling in early disaster response, and provide a platform for discussing health system recovery, mitigation and preparedness.
Supplementary Material
Acknowledgments
The authors would like to thank Michelle Schmitz and Peter Macharia for useful comments on an earlier version of the manuscript.
Footnotes
Contributors: FH: conceptualisation, methodology, formal analysis, writing, editing, visualisation, supervision. NeR: data sharing, methodology, writing, editing, validation. MM: writing, editing. RP: methodology, writing, editing. NiR: conceptualisation, methodology, writing, editing, validation, supervision.
Funding: This study was partly funded by UNICEF.
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request. Most data used in this study are openly accessible through the indicated data sources in Table 1. Other data are available on request.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Delamater PL, Messina JP, Shortridge AM, et al. Measuring geographic access to health care: raster and network-based methods. Int J Health Geogr 2012;11:15. 10.1186/1476-072X-11-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davis JR, Wilson S, Brock-Martin A, et al. The impact of disasters on populations with health and health care disparities. Disaster Med Public Health Prep 2010;4:30–8. 10.1017/S1935789300002391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abbas HB, Routray JK. A semi-quantitative risk assessment model of primary health care service interruption during flood: case study of aroma locality, Kassala state of Sudan. International Journal of Disaster Risk Reduction 2013;6:118–28. 10.1016/j.ijdrr.2013.10.002 [DOI] [Google Scholar]
- 4.Makanga PT, Schuurman N, Sacoor C, et al. Seasonal variation in geographical access to maternal health services in regions of southern Mozambique. Int J Health Geogr 2017;16:1. 10.1186/s12942-016-0074-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United Nations Office of Coordinated Humanitarian Affairs Humanitarian reponse plan (2018-2019): revised following Cyclones Idai and Kenneth. may, 2019. [Google Scholar]
- 6.Chen WH, Azman AS. Mitigating cholera in the aftermath of cyclone Idai. Am J Trop Med Hyg 2019;101:tpmd190285–962. 10.4269/ajtmh.19-0285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization Relatório dA Situação Nacional 11: 04 de Outubro de 2019, Período abrangido 9 a 22 de Setembro de 2019, 2019. Available: https://www.afro.who.int/sites/default/files/2019-10/National_SitRep%2011_MOZ_9%20a%2022%20de%20Setembro%202019_PORT.pdf
- 8.Cambaza E, Mongo E, Anapakala E, et al. Outbreak of cholera due to cyclone Kenneth in northern Mozambique, 2019. Int J Environ Res Public Health 2019;16:2925 10.3390/ijerph16162925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Willcock G. After Cyclones Idai and Kenneth, Recovery in Mozambique Continues: Reliefweb; 2019 [updated 17 May, 2019. Available: https://reliefweb.int/report/mozambique/after-cyclones-idai-and-kenneth-recovery-mozambique-continues [Accessed 16 Oct 2019].
- 10.UNICEF Cyclone response mid-year sitrep #12: March-July 2019, 2019. [Google Scholar]
- 11.Devi S. Cyclone Idai: 1 month later, devastation persists. Lancet 2019;393:1585. 10.1016/S0140-6736(19)30892-X [DOI] [PubMed] [Google Scholar]
- 12.Kahn R, Mahmud AS, Schroeder A, et al. Rapid forecasting of cholera risk in Mozambique: translational challenges and opportunities. Prehosp Disaster Med 2019;34:557–62. 10.1017/S1049023X19004783 [DOI] [PubMed] [Google Scholar]
- 13.Santos E. Mozambique: The recovery from Cyclone Idai continues, but health needs remain [Report], 2019. Available: https://reliefweb.int/report/mozambique/mozambique-recovery-cyclone-idai-continues-health-needs-remain
- 14.World Health Organization Cyclone Idai - events as they happen 2019, 2019. Available: https://www.who.int/emergencies/cyclone-idai/events-as-they-happen [Accessed 16 Oct 2019].
- 15.Tropical Cyclones Idai and Kenneth International Federation of the red cross. Mozambique, 2019. [Google Scholar]
- 16.Muggy L, Heier Stamm JL. Dynamic, robust models to quantify the impact of decentralization in post-disaster health care facility location decisions. Oper Res Health Care 2017;12:43–59. 10.1016/j.orhc.2017.01.002 [DOI] [Google Scholar]
- 17.World Health Organization Post-Disaster needs assessments guidelines, 2014. [Google Scholar]
- 18.Humanitarian Data Exchange Mozambique, 2019. Available: https://data.humdata.org/event/idai [Accessed 25 April 2019].
- 19.Tapia AH, Maldonado E, Ngamassi Tchouakeu Louis‐Marie, et al. Coordinating humanitarian information. Info Technology & People 2012;25:240–58. 10.1108/09593841211254312 [DOI] [Google Scholar]
- 20.Thévenaz C, Resodihardjo SL. All the best laid plans…conditions impeding proper emergency response. International Journal of Production Economics 2010;126:7–21. 10.1016/j.ijpe.2009.09.009 [DOI] [Google Scholar]
- 21.Ray N, Ebener S. AccessMod 3.0: computing geographic coverage and accessibility to health care services using anisotropic movement of patients. Int J Health Geogr 2008;7:63. 10.1186/1476-072X-7-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.QGIS geographic information system [program] 2019.
- 23.R Foundation for Statistical Computing R: A Language and Environment for Statistical Computing [program]. 5 version. Vienna, Austria, 2018. [Google Scholar]
- 24.Jarvis A, Reuter H, Nelson A, et al. Hole-field seamless SRTM data, International centre for tropical agriculture (CIAT), 2008. Available: http://srtmcsicgiarorg
- 25.Buchhorn M, Smets B, Bertels L, et al. Copernicus Global Land Service: Land Cover 100m, epoch “2015”, Globe. 2019. Version V2.0.2. [Data set]. Available: https://lcviewer.vito.be/download [Accessed 31 Jul 2019].
- 26.LOG-WFP Mozambique: access constraints as of 19 March 2019, 2019. Available: https://logcluster.org/map/mozambique-access-constraints-map-19-march-2019
- 27.LOG-WFP Mozambique - Cabo Delgado: Access constraints map 3 May 2019, 2019. Available: https://logcluster.org/map/mozambique-cabo-delgado-access-constraints-map-3-may-2019
- 28.UN Operational Satellite Applications Programme (UNOSAT) UNOSAT Geospatial Data on Floods in Mozambique - March 2019, 2019. Available: https://data.humdata.org/dataset/unosat-analysis-on-floods-in-mozambique-march-2019 [Accessed 31 Jul 2019].
- 29.Copernicus EMSR354 Tc Kenneth Copernicus EMSR354 flood extent 20190502, 2019. Available: https://geonode.ingc.gov.mz/layers/geonode:emsr354_observedeventmerged_20190502 [Accessed 31Jul 2019].
- 30.UNICEF Strategy for health (2016–2030. New York: United Nations Children’s Fund, 2015. [Google Scholar]
- 31.Golding N, Burstein R, Longbottom J, et al. Mapping under-5 and neonatal mortality in Africa, 2000–15: a baseline analysis for the sustainable development goals. The Lancet 2017;390:2171–82. 10.1016/S0140-6736(17)31758-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Facebook Connectivity Lab and Center for International Earth Science Information Network - CIESIN - Columbia University High resolution settlement layer (HRSL), 2019. Available: https://data.humdata.org/dataset/highresolutionpopulationdensitymaps-moz [Accessed 6 Aug 2019].
- 33.Thematic Research Network on Data and Statistics (TReNDS) Leaving no one of the MAP: a guide for gridded population data for sustainable development, 2020. Available: https://static1.squarespace.com/static/5b4f63e14eddec374f416232/t/5eb2b65ec575060f0adb1feb/1588770424043/Leaving+no+one+off+the+map-4.pdf
- 34.Tatem AJ. WorldPop, open data for spatial demography. Sci Data 2017;4:1–4. 10.1038/sdata.2017.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.SIS-MA MMoH Mozambique - Health facilities, 2019. Available: https://data.humdata.org/dataset/mozambique-health-facilities [Accessed 17 Sept 2019].
- 36.Dos Anjos Luis A, Cabral P. Geographic accessibility to primary healthcare centers in Mozambique. Int J Equity Health 2016;15:173. 10.1186/s12939-016-0455-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization Health economics: GeoAccess, 2019. Available: https://www.who.int/choice/geoaccess/en/ [Accessed 15 Mar 2019].
- 38.Ebener S, Stenberg K, Brun M, et al. Proposing standardised geographical indicators of physical access to emergency obstetric and newborn care in low-income and middle-income countries. BMJ Glob Health 2019;4:e000778. 10.1136/bmjgh-2018-000778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huerta Munoz U, Källestål C. Geographical accessibility and spatial coverage modeling of the primary health care network in the Western Province of Rwanda. Int J Health Geogr 2012;11:40. 10.1186/1476-072X-11-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ouma PO, Maina J, Thuranira PN, et al. Access to emergency hospital care provided by the public sector in sub-Saharan Africa in 2015: a geocoded inventory and spatial analysis. Lancet Glob Health 2018;6:e342–50. 10.1016/S2214-109X(17)30488-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schmitz MM, Serbanescu F, Arnott GE, et al. Referral transit time between sending and first-line receiving health facilities: a geographical analysis in Tanzania. BMJ Glob Health 2019;4:e001568. 10.1136/bmjgh-2019-001568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alegana VA, Wright JA, Pentrina U, et al. Spatial modelling of healthcare utilisation for treatment of fever in Namibia. Int J Health Geogr 2012;11:6. 10.1186/1476-072X-11-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moitinho de Almeida M, Guha-Sapir D. Why Mozambique’s cyclones tell us disaster preparedness needs health at its core: The BMJ opinion, 2019. Available: https://blogs.bmj.com/bmj/2019/05/10/mozambiques-cyclones-disaster-preparedness-needs-health-core/?utm_source=twitter&utm_medium=hootsuite&utm_term=&utm_content=&utm_campaign=editors [Accessed 17 Dec 2019].
- 44.Khan H, Vasilescu LG, Khan A. Disaster management cycle-a theoretical approach. Journal of Management and Marketing 2008;6:43–50. [Google Scholar]
- 45.Liu A, Sullivan S, Khan M, et al. Community health workers in global health: scale and scalability. Mt Sinai J Med 2011;78:419–35. 10.1002/msj.20260 [DOI] [PubMed] [Google Scholar]
- 46.Reliefweb As post-cyclone resettlement, 200 000 people lack access to health services in Mozambique, 2019. [Google Scholar]
- 47.World Health Organization Hospitals safe from disasters: reduce risk, protect health facilities, save lives, 2007. [Google Scholar]
- 48.World Health Organization Natural disasters: protecting the public’s health. Natural disasters: protecting the public’s health, 2000. [Google Scholar]
- 49.UNICEF One year after cyclone Idai, 2.5 million people in Mozambique remain in need of humanitarian assistance: UNICEF prepares for more frequent and ferocious disasters as a result of the climate crisis, 2020. Available: https://www.unicef.org/mozambique/en/press-releases/one-year-after-cyclone-idai-25-million-people-mozambique-remain-need-humanitarian [Accessed 16 March 2020].
- 50.Altay N, Labonte M. Challenges in humanitarian information management and exchange: evidence from Haiti. Disasters 2014;38:S50–72. 10.1111/disa.12052 [DOI] [PubMed] [Google Scholar]
- 51.Nelson T, Wulder M, Niemann KO. Spatial resolution implications of digitizing aerial photography for environmental applications. The Imaging Science Journal 2001;49:223–32. 10.1080/13682199.2001.11784386 [DOI] [Google Scholar]
- 52.Yao J, Agadjanian V. Bypassing health facilities in rural Mozambique: spatial, institutional, and individual determinants. BMC Health Serv Res 2018;18:1006. 10.1186/s12913-018-3834-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Keyes EB, Parker C, Zissette S, et al. Geographic access to emergency obstetric services: a model incorporating patient bypassing using data from Mozambique. BMJ Glob Health 2019;4:e000772. 10.1136/bmjgh-2018-000772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.U.S. Geological Survey (USGS) Shuttle Radar Topography Mission 1 Arc-Second Global: SRTM1N22W016V3. 2000. [Data set]. [Available from]. Available: https://search.earthdata.nasa.gov/search [Accessed : 20 Sept, 2019].
- 55.Instituto Nacional de Estatistica United nations office for coordination of humanitarian Affairs regional office for southern and eastern Africa. Mozambique administrative level shapefiles, 2019. Available: https://data.humdata.org/dataset/mozambique-administrative-levels-0-3 [Accessed 07 Jul 2019].
- 56.Global Disaster Alert and Coordination System Overall red alert tropical cyclone for IDAI-19, 2019. Available: https://www.gdacs.org/resources.aspx?eventid=1000552&episodeid=24&eventtype=TC [Accessed March 2020].
- 57.Global Disaster Alert and Coordination System Overall red alert tropical cyclone for KENNETH-19, 2019. Available: https://www.gdacs.org/report.aspx?eventtype=TC&eventid=1000559&episodeid=12 [Accessed March 2020].
- 58.OpenStreetMap Osm roads (daily extract), 2018. Available: https://geonode.ingc.gov.mz/layers/geonode:osm_roads [Accessed 07 Aug 2019].
- 59.World Food Program Mozambique: access constraints as of 19 March, 2019. Available: https://logcluster.org/sites/default/files/maps/moz_op_accessconstraints_a3p_20190319.pdf [Accessed 23 Sept 2019].
- 60.World Food Program Mozambique - Cabo Delgado - Access Constraints Map, 2019. Available: https://logcluster.org/map/mozambique-cabo-delgado-access-constraints-map-3-may-2019 [Accessed 23 Sept 2019].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-039138supp001.pdf (444.6KB, pdf)