Abstract
Purpose:
To evaluate the effect of COVID-19 pandemic and national lockdown on patient care at a tertiary-care ophthalmology institute.
Methods:
Records of all the patients who presented from March 25th to May 3rd, 2020 were scanned to evaluate the details regarding the presenting complaints, diagnosis, advised treatment and surgical interventions.
Results:
The number of outpatient department visits, retinal laser procedures, intravitreal injections and cataract surgeries during this lockdown decreased by 96.5%, 96.5%, 98.7% and 99.7% respectively compared from the corresponding time last year. Around 38.8% patients could be triaged as non-emergency cases based on history alone while 59.5% patients could be triaged as non-emergency cases after examination. Only eighty-four patients opted for video-consultation from April 15th to May 3rd, 2020. Nine patients presented with perforated corneal ulcer, but could not undergo penetrating keratoplasty due to the lack to available donor corneal tissue. One of these patients had to undergo evisceration due to disease progression. Two patients with open globe injury presented late after trauma and had to undergo enucleation. Around 9% patients could not undergo the advised urgent procedure due to logistical issues related to the lockdown.
Conclusion:
A significant number of patients could not get adequate treatment during the lockdown period. Hospitals need to build capacity to cater to the expected patient surge post-COVID-19-era, especially those requiring immediate in-person attention. A large number of patients can be classified as non-emergency cases. These patients need to be encouraged to follow-up via video-consultation to carve adequate in-person time for the high-risk patients.
Keywords: COVID-19, emergency, eye banking, lockdown, surge, video consultation
The coronavirus disease (COVID-19) pandemic caused by the highly contagious virus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused mayhem across the world. The Government of India imposed a country-wide total lockdown of all non-essential services in order to restrain the rapid spread of the disease. The first two phases of this lockdown extended from March 25th to April 14th, 2020 and from April 15th to May 3rd, 2020 respectively.[1,2,3,4]
In this critical situation, the health-care sector is expected to be the forerunner and safely guide the rest of the country though this natural calamity. The health-care providers have the responsibility of not only providing adequate care to the patients but also protecting themselves from falling prey to this potentially deadly disease. These unprecedented circumstances have posed a number of challenges for all health-care workers (HCW), including those involved in non-COVID-19 related field like ophthalmology, in terms of providing patient care. The policy of social distancing to prevent the spread of the disease has crippled the ability of hospital to deal with large number of patients.[5] Patients presenting with non-emergency conditions further strain the already limited resources. The delay in presentation to the hospital due to lockdown and fear of infection, can lead to progression of the disease, further intensifying the difficulties.[6] The All India Ophthalmological Society (AIOS) provided guidelines to assist the ophthalmology fraternity regarding the optimum strategies to cater to patients without increasing the chances of exposure for both the patients and the HCWs.[7]
This study was performed to evaluate the effect of COVID-19 pandemic and national lockdown on patient care at a tertiary-care ophthalmology institute.
Methods
This retrospective study was conducted at a tertiary care dedicated ophthalmic hospital in Tamil Nadu, without any associated multi speciality hospital. This hospital not only caters to the various districts within the state but also to the surrounding states of Andhra Pradesh, Kerala and Telangana. The study was performed after obtaining an approval from the Institutional Review Board and adhered to the tenets of the Declaration of Helsinki. An informed consent was taken from the patient(s) or their attendant(s) in case the patient(s) underwent any procedure. Records of all the patients taking treatment at the institute from March 25th to May 3rd, 2020 were evaluated with the help of electronic medical record (EMR).
All the guidelines and precautions advised by AIOS were strictly followed by all the HCWs at all times. These included postponing of the scheduled appointments for all elective procedures; adequate personal protection equipment (PPE) for on-duty staff; reduction of the workforce; entry point screening and triaging of patients; regular sanitization of furniture; recommended social distancing norms in waiting halls, outpatient department (OPD) and inpatient department (IPD); and adequate channelization of the patient flow to minimise crowding and the time spent by patients in the hospital. The patients were urged to contact the hospital regarding ocular complaints using video and audio-based teleconsultations instead of coming to the hospitals.
Since the hospital is not associated with any multi-speciality hospital, HCWs from our institution were not diverted for the management of COVID-19 patients. In spite of the hospital facing grave financial strain, there were no job lay-offs. Hence, there was enough man-power for providing adequate care for the incoming patients.
The electronic medical records of the patients who presented to the centre during this lockdown period were scanned to retrieve data regarding their presenting complaints, final diagnosis, treatment advised and surgical interventions. We graded the patients as non emergency or emergency, based on the triage provided by the AIOS.[2,7] We also tried to understand if a detailed in-person examination was needed for evaluation of these patients or a video-consultation was sufficient. We also made a note of the cases where there was an unprecedented delay in undergoing the advised intervention, caused by difficulties directly related to the lockdown.
Statistical analysis
The data were entered into a Microsoft Excel spreadsheet and statistical analysis was performed with STATA statistical software, Version 14.0 (StataCorp, College Station, Texas, USA). Continuous variables were expressed as mean (±standard deviation) or median (Range). Chi-square test/Fisher's exact test was used to assess the association of categorical variables.
Results
The total number of OPD visits during this period were 3434 (average, 85.8 visits per day). On the contrary, total number of OPD visits during the corresponding period last year was 102,262 (average, 2556.6 visits per day). Thus, the OPD volume decreased by 96.6% [Fig. 1]. The mean age of the presenting patients was 38.7 ± 20.6 years (Range, 1 month to 95 years). The proportion of females presenting during this lockdown and during corresponding period last year was 40.8% and 48.2% (P < 0.001). The proportion of patients ≤60 years age during this lockdown and during corresponding period last year were 84.7% and 67.4% (P < 0.001) [Table 1].
Figure 1.
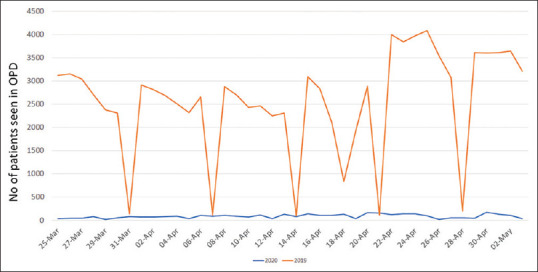
Comparison of the number of patients presenting to the hospital during COVID-19 lockdown and during corresponding time interval in the previous year
Table 1.
Comparison of demographics of patients presenting to the hospital during COVID-19 lockdown with corresponding period last year
| Age group (in years) | COVID-19 lockdown (25.3.2020-02.05.2020) | Corresponding period last year (25.3.2019-02.05.2019) | P (Total 1 vs Total 2) | ||||
|---|---|---|---|---|---|---|---|
| Male | Female | Total 1 | Male | Female | Total 2 | ||
| ≤15 | 338 | 229 | 567 (16.5%) | 5153 | 3908 | 9061 (8.9%) | 0.01 |
| 16-40 | 720 | 494 | 1214 (35.3%) | 9806 | 9465 | 19271 (18.8%) | |
| 41-50 | 308 | 223 | 531 (15.5%) | 8171 | 8388 | 16559 (16.2%) | |
| 51-60 | 361 | 236 | 597 (17.4%) | 11337 | 12734 | 24071 (23.5%) | |
| 61-70 | 188 | 157 | 345 (10.0%) | 12491 | 11253 | 23744 (23.2%) | |
| 71-80 | 100 | 58 | 158 (4.6%) | 5182 | 3159 | 8341 (8.2%) | |
| >80 | 19 | 3 | 22 (0.6%) | 859 | 356 | 1215 (1.2%) | |
| Total | 2034 | 1400 | 3434 | 52999 | 49263 | 102262 | |
The most common presenting complaints were red eye (n = 1277), ocular pain (n = 989), ocular irritation (n = 711), discharge (n = 500) and mechanical trauma to the eye (n = 463). The most common indication for which patients presented to the hospital were infective conjunctivitis (n = 593), closed globe injury (n = 361), allergic conjunctivitis (n = 293), dry eye (n = 214) and corneal or conjunctival foreign body (n = 157).
After a careful history-taking, 1334 patients (38.8%) could be triaged as non-emergency or non-urgency cases [Table 2]. Similarly, 2042 patients (59.5%) could be triaged as non-emergency or non-urgency cases after ocular examination, [Table 3]. Some patients who had non-emergency conditions like infective conjunctivitis (n = 58), allergic conjunctivitis (n = 17), routine surgical follow-up (n = 16), dry eye (n = 9), episcleritis (n = 7), conjunctival or corneal foreign body (n = 6), chalazion (n = 3), stable glaucoma (n = 2) and headache (n = 1) presented to the hospital more than once during this lockdown period. Eighty-four patients sought advise through video-consultation from April 15 to May 2. All the calls were attended by ophthalmologists and not by tele-counsellors. All the patients wanted to visit the hospital de novo for consultation.
Table 2.
Number of patients triaged as non-ocular emergency or urgency cases based on history alone
| Complaints | Number of patients |
|---|---|
| Eye irritation | 711 (20.70%) |
| Routine surgical follow-up (last 3 months) | 412 (12.00%) |
| Gradual decrease of vision | 80 (2.33%) |
| Headache | 69 (2.01%) |
| Want new spectacles | 38 (1.11%) |
| Routine or yearly follow up | 8 (0.23%) |
| Want cataract surgery | 7 (0.20%) |
| Come for Silicon oil removal | 4 (0.12%) |
| Diabetic retinopathy screening | 2 (0.06%) |
| Routine hydrochloroquine retinopathy screening | 1 (0.03%) |
| Deviation of eye | 1 (0.03%) |
| Removal of canalicular stent | 1 (0.03%) |
| Total | 1334 (38.84%) |
Table 3.
Number of patients triaged as non-ocular emergency or urgency cases after examination
| Diagnosis | Number of patients |
|---|---|
| Infective conjunctivitis | 593 (17.3%) |
| Routine surgical follow-up (last 3 months) | 412 (12.0%) |
| Allergic conjunctivitis | 293 (8.5%) |
| Dry eye | 214 (6.2%) |
| Refractive error | 96 (2.8%) |
| Episcleritis | 76 (2.2%) |
| Headache due to non-serious cause | 63 (1.8%) |
| Chalazion | 61 (1.8%) |
| Follow-up case of glaucoma (stable) | 55 (1.6%) |
| Immature cataract | 45 (1.3%) |
| Pingecula/Pterygium | 41 (1.2%) |
| Stable NPDR or vascular occlusion or PDR s/p PRP without ME | 39 (1.1%) |
| Subconjunctival haemorrhage | 36 (1.0%) |
| Macular hole, retinal dystrophy, IJT, CNVM | 8 (0.2%) |
| Central serous chrorioretinopathy | 5 (0.1%) |
| Stable thyroid eye disease | 5 (0.1%) |
| Total | 2042 (59.5%) |
NPDR: Non-proliferative diabetic retinopathy, PRP: Panretinal photocoagulation, ME: Macular edema; IJT: Idiopathic juxtafoveal telangiectasia, CNVM: Choroidal neovascular membrane
All elective surgeries were postponed during the lockdown period. Emergency intervention was advised for 194 patients, all of whom had an imminent risk of visual loss. The emergency interventions performed included laser barrage for peripheral retinal breaks (n = 3), laser peripheral iridotomy for acute angle closure attack (n = 11), panretinal photocoagulation sessions (PRP) for proliferative diabetic retinopathy (n = 47), intravitreal anti-vascular endothelial growth factor (VEGF) injections for retinal conditions (n = 15) and surgical interventions (n = 93) [Table 4]. The indication for anti-VEGF injection were neovascular glaucoma (n = 7), single-eyed patients with active choroidal neovascular membrane (CNVM) in one eye and scarred CNVM in the other (n = 3), ischemic central retinal vein occlusion (n = 2), aggressive posterior retinopathy of prematurity (APROP, n = 2) and diabetic macular edema (n = 1). On the contrary, 1435 retinal laser procedures, 1160 intravitreal injections and 3316 cataract surgeries were performed during the corresponding period last year. Hence, the number of retinal laser procedures, intravitreal injections and cataract surgeries fell by 96.5%, 98.7% and 99.7% respectively.
Table 4.
Indications for which patients underwent an urgent surgery during COVID-19 lockdown in view of imminent visual loss
| Indication for surgery | Number of patients |
|---|---|
| Open globe injury | 41 |
| Rhegmatogenous retinal detachment | 16 |
| Lens-related glaucoma | 10 |
| Endophthalmitis | 8 |
| Lid tear | 4 |
| Conjunctival tear | 4 |
| Intractable or advanced glaucoma | 5 |
| Peripheral perforated corneal ulcer (Amniotic membrane transplant) | 1 |
| Multiple corneal foreign body (under general anaesthesia) | 1 |
| Perforated corneal ulcer with spontaneous evisceration | 1 |
| Painful blind eye | 1 |
| Retinoblastoma | 1 |
However, because of the logistical issues directly related to lockdown, several patients could not receive the advised emergency treatment. Nine patients presented with perforated corneal ulcer, but could not undergo penetrating keratoplasty due to the lack to available donor cornea tissue. One of these patients had to undergo evisceration. Two patients with open globe injury presented late after trauma and had to undergo enucleation. Some patients could not undergo urgent procedures due to logistical and financial issues. These included three patients (1.5%) who did not undergo cataract surgery for lens-related glaucoma, seven patients (3.6%) who did not come back for PRP completion and seven patients (3.6%) who did not undergo intravitreal anti-VEGF injections.
During the entry point screening, none of the patients presenting to the centre gave any history or showed any signs of COVID-19 disease. None of the HCWs at the institute developed any symptoms suggestive of COVID-19 disease during or after this period, till the last date of manuscript preparation.
Discussion
The lockdown measures imposed to curb the growth of COVID-19 pandemic brought the whole country to a standstill as all the public transport services were stopped and free movement of public for non-essential work was restricted. With the announcement of lockdown, our hospital also gave out official notification in all the regional dailies requesting patients to visit the hospital only in case of an ocular emergency. Public showed a good compliance to the lockdown guidelines as the OPD load in our hospital decreased to nearly 3.5% of its load during the corresponding time previous year. Other authors have also reported a similar decrease in the number of patients presenting to ODP, depending upon the region and profile of the institute.[8,9] The reduced OPD and surgical volume not only posed a major financial challenge for the institution, but also increased the chances of high-risk patients not receiving adequate treatment.
There were a number of interesting patterns in the health care seeking behavior of the patients during this lockdown. A gender-bias was noted as a significantly lower proportion of females presented to the hospital during this lockdown period compared from the corresponding period last year. This may be due to higher probability of females remaining involved with their children, who stayed mostly at home due to shutdown of schools. Similarly, a statistically higher proportion of young patients presented during this lockdown compared to the corresponding period last year. This may be due to elective cataract surgeries being postponed as well as the awareness that elderly people are at higher risk of getting infected. Pellegrini et al. also reported similar observations i.e., higher mean age and intensified male gender-bias among patients presenting during lockdown compared to the previous year.[8] Another peculiar observation was a high proportion of people presenting with red eye. Shetty et al. reported similar observation with nearly 60% teleophthalmology consultations done for red eye. They attributed this to the use of alcohol-based sanitizers and termed the entity as sanitizer aerosol-driven ocular surface disease (SADOSD).[10] Also, reports suggesting red eye as the first feature of COVID-19 may have provoked patients to seek ophthalmologists' advise.[11,12]
More than one-third patients presenting to our hospital during the period were triaged as non-emergency cases based on their history alone. After an examination, nearly 60% patients could be triaged as non-emergency cases. Similarly, Pellegrini et al. reported that nearly 57% cases presenting during lockdown were unlikely to be emergency cases.[8] Some of these patients even presented multiple times during the lockdown period. A large majority of these multiple-visit patients came for routine post-surgical examination. These non-emergency patients could have avoided hospital visits and instead sought consultation via video-calls as recommended to them. However, only 84 patients sought opinion through video-calls. Video-consultations were provided free of cost as a pilot project to check out its feasibility. However, the consultations were not recorded on the EMR. In future, we plan to connect this modality with EMR and assess its efficacy in the management of patients with various diseases. In this time of health emergency when social distancing norms have to be followed, we need to focus on identifying this set of low risk patients and encourage them to follow up with the help of video consultations.
Videos consultations allow for a thorough history taking as well as gross examination of the ocular adnexa and anterior segment. Williams et al. at the University of Pittsburgh reported that only 25%, 35% and 41% of the new, follow-up and post-op patients respectively needed in-person visit to the hospital, while others could be triaged for either a video visit or a rescheduled appointment after 3-6 months.[13] Kang et al. reported that video consultations were useful for follow-up and post-operative patients, as well as to accurately triaging the new patients in their oculoplasty clinic. The patients treated via these video consultations were also satisfied with the ease, safety and efficiency of the system.[14]
The most common indications for surgery at our centre during this lockdown were open-globe injury (OGI), rhegmatogenous retinal detachment (RRD) and lens-related glaucoma. Similarly, Tang et al. reported that majority of surgery at their centre in Hong Kong were done for RRD, OGI and glaucoma.[15] Du et al. reported the most common indication for surgery at their centre in China was glaucoma.[16] Although majority of the indicated emergency surgeries were performed at our institute without any delay, penetrating keratoplasty could not be done due to unavailability of the donor corneal tissue. Eye banking has faced a major setback during this pandemic due to confusion regarding guidelines related to tissue harvesting. It is expected to take a few more months before eye banking can resume its normal functioning. Availability of artificial corneas and 3D-bioprinted corneas may have proved to be of immense importance during this health emergency, however, these are still under research.[17,18]
The inability of patients to reach the hospital for timely treatment has been another big problem during this health emergency. A number of patients could not undergo an urgent procedure due to logistical and financial issues directly related to the lockdown. The number of patients undergoing intravitreal injections for freshly diagnosed diseases as well as those on treat and extend regimen have reduced drastically compared from last year. The patients undergoing laser treatment for peripheral tears as well as retinal vascular pathologies have also dwindled. In the absence of timely intervention, such patients are expected to follow the natural course of their respective diseases, resulting in progression to advanced stages. The number of elective surgeries has also reduced drastically, thus adding on to the back log. In nut shell, two major problems are expected to crop up due to this COVID-19 pandemic. Firstly, there may be a huge surge in the number of patients presenting to the hospitals. Secondly, a large chunk of patients may present with advanced eye diseases unamenable to treatment.
The functioning of hospitals has to be changed to prevent the health-care system from crumpling. Hospitals need to work on capacity-building in order to cater to the expected surge in the OPD as well as surgical volume, without compromising the safety of the patient as well as the eye-care quality. Provisions have to be made to make sure that the patients with high-risk diseases receive immediate in-person attention. As seen from the results of our study, a large majority of patients can be triaged as low-risk patients. These patients need to be quickly identified and encouraged to seek virtual consultation, especially for follow-up and post-operative visits. Provisions should be made to elevate these video-consultations at par with the in-person visits in terms of proper medical record maintenance and consultation fees. Although, these virtual-consultation are limited by their inability to perform visual acuity, detailed ocular examination and other investigations, they are sufficient for gross examination and triage. Concerns regarding medical and medicolegal repercussion in case of diagnostic errors in the absence of a traditional exam have to be addressed. Both the patients as well as doctors need to be educated regarding the importance of these video consultations. Practising trial video-consultation calls with the patients who have come to the hospital for examination will help alleviate the anxiety on both the sides.
Conclusion
A significant number of patients could not get adequate treatment during the lockdown period. The battle with COVID-19 is expected to continue for a long time. We have to prepare ourselves for not only the ongoing pandemic but also to deal with its aftermath by building capacity to cater to the expected patient surge. This time should be efficiently utilised to prepare for the future, making adequate arrangements for delivering safe and efficient health-care to the high-risk patients, without ignoring the needs of non-emergency cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: Results of a survey. Indian J Ophthalmol. 2020;68:725–30. doi: 10.4103/ijo.IJO_797_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sengupta S, Honavar SG, Sachdev MS, Sharma N, Kumar A, Ram J, et al. All India Ophthalmological Society - Indian Journal of Ophthalmology consensus statement on preferred practices during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:711–24. doi: 10.4103/ijo.IJO_871_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khanna RC, Cicinelli MV, Gilbert SS, Honavar SG, Murthy GSV. COVID-19 pandemic: Lessons learned and future directions. Indian J Ophthalmol. 2020;68:703–10. doi: 10.4103/ijo.IJO_843_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sachdev MS, Tamilarasan S. Survival tool kit for ophthalmic practices during difficult times: Build your resilience in the face of crisis. Indian J Ophthalmol. 2020;68:679–82. doi: 10.4103/ijo.IJO_861_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Honavar SG. Navigating the new normal in ophthalmology. Indian J Ophthalmol. 2020;68:957–8. doi: 10.4103/ijo.IJO_1649_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4:e10–1. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Honavar SG, Sharma N Sachdev MS for the Governing Council of the All India Ophthalmological Society. AIOS-Operational-Guidelines-COVID19. [Last accessed on 2020 May 24]. Available from: https://aiosorg/pdf/AIOSOperational-Guidelines-COVID19pdf .
- 8.Pellegrini M, Roda M, Lupardi E, Di Geronimo N, Giannaccare G, Schiavi C. The impact of COVID-19 pandemic on ophthalmological emergency department visits. Acta Ophthalmol. doi: 10.1111/aos.14489. doi: 101111/aos 14489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moravvej Z, Soltani-Moghadam R, Ahmadian Yazdi A, Shahraki K. COVID-19 pandemic: Ophthalmic practice and precautions in a tertiary eye hospital in Iran. Infect Control Hosp Epidemiol. 2020:1–2. doi: 10.1017/ice.2020.164. doi: 101017/ice2020164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shetty R, Jayadev C, Chabra A, Maheshwari S, D'Souza S, Khamar P, et al. Sanitizer aerosol-driven ocular surface disease (SADOSD)-A COVID-19 repercussion.? Indian J Ophthalmol. 2020;68:981–3. doi: 10.4103/ijo.IJO_1308_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yu AY, Tu R, Shao X, Pan A, Zhou K, Huang J. A comprehensive Chinese experience against SARS-CoV-2 in ophthalmology. Eye Vis (Lond) 2020;7:19. doi: 10.1186/s40662-020-00187-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar K, Prakash AA, Gangasagara SB, Rathod SBL, Ravi K, Rangaiah A, et al. Presence of viral RNA of SARS-CoV-2 in conjunctival swab specimens of COVID-19 patients. Indian J Ophthalmol. 2020;68:1015–7. doi: 10.4103/ijo.IJO_1287_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams AM, Kalra G, Commiskey PW, Bowers EMR, Rudolph BR, Pitcher MD, et al. Ophthalmology practice during the Coronavirus disease 2019 pandemic: The University of Pittsburgh experience in promoting clinic safety and embracing video visits. Ophthalmol Ther. 2020:1–9. doi: 10.1007/s40123-020-00255-9. doi: 10.1007/s40123-020-00255-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang S, Thomas PBM, Sim DA, Parker RT, Daniel C, Uddin JM. Oculoplastic video-based telemedicine consultations: Covid-19 and beyond. Eye (Lond) 2020;34:1193–5. doi: 10.1038/s41433-020-0953-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tang EWH, Wong DHT, Chan YYY, Li KKW. Emergency ophthalmic surgeries during COVID-19-A Hong Kong perspective. Graefes Arch Clin Exp Ophthalmol. 2020:1–2. doi: 10.1007/s00417-020-04768-8. doi: 101007/s00417-020-04768-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Du H, Zhang M, Zhang H, Sun X. Practical experience on emergency ophthalmic surgery during the prevalence of COVID-19. Graefes Arch Clin Exp Ophthalmol. 2020:1–3. doi: 10.1007/s00417-020-04692-x. doi: 101007/s00417-020-04692-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sommer AC, Blumenthal EZ. Implementations of 3D printing in ophthalmology. Graefes Arch Clin Exp Ophthalmol. 2019;257:1815–22. doi: 10.1007/s00417-019-04312-3. [DOI] [PubMed] [Google Scholar]
- 18.Zhang B, Xue Q, Li J, Ma L, Yao Y, Ye H, et al. 3D bioprinting for artificial cornea: Challenges and perspectives. Med Eng Phys. 2019;71:68–78. doi: 10.1016/j.medengphy.2019.05.002. [DOI] [PubMed] [Google Scholar]


