Abstract
Objective:
The Centers for Medicare & Medicaid Services’ National Partnership to Improve Dementia Care in Nursing Homes focuses on but is not limited to long-term care (LTC) residents with dementia; the potential impact on residents with other diagnoses is unclear. We sought to determine whether resident subpopulations experienced changes in antipsychotic and mood stabilizer prescribing.
Design:
Repeated cross-sectional analysis of a 20% Medicare sample, 2011–2014.
Setting and Participant:
Fee-for-service Medicare beneficiaries with Part D coverage in LTC (n=562,485) and a secondary analysis limited to persons with depression or bipolar disorder (n=139,071).
Methods:
Main outcome was quarterly predicted probability of treatment with an antipsychotic or mood stabilizer.
Results:
From 2011–2014, the adjusted predicted probability (APP) of antipsychotic treatment fell from 0.120 (95% confidence interval [CI] 0.119–0.121) to 0.100 (95% CI 0.099–0.101; p<0.001). Use decreased for all age, sex, and racial/ethnic groups; the decline was larger for persons with dementia (p<0.001). The APP of mood stabilizer use grew from 0.140 (95% CI 0.139–0.141) to 0.185 (95% CI 0.184–0.186), growth slightly larger among persons without dementia (p<0.001). Among persons with depression or bipolar disorder, the APP of antipsychotic treatment increased from 0.081 (95% CI 0.079–0.082) to 0.087 (95% CI 0.085–0.088; p<0.001); APP of mood stabilizer treatment grew more, from 0.193 (95% CI 0.190–0.196) to 0.251 (0.248–0.253; p<0.001). Quetiapine was the most commonly prescribed antipsychotic. The most widely prescribed mood stabilizer was gabapentin, prescribed to 70.5% of those who received a mood stabilizer by the end of 2014.
Conclusions and Implications:
The likelihood of antipsychotic and mood stabilizer treatment did not decline for residents with depression or bipolar disorder, for whom such prescribing may be appropriate but who were not excluded from the Partnership’s antipsychotic quality measure. Growth in mood stabilizer use was widespread, and largely driven by growth in gabapentin prescribing.
Keywords: Geriatric psychiatry, psychotropic medications, long-term care
Brief Summary:
Following the CMS National Partnership to Improve Dementia Care, we found that reductions in antipsychotic prescribing were greatest among patients with dementia and not seen among patients with depression or bipolar disorder, where use may be appropriate.
INTRODUCTION
Psychotropic medication prescribing in long-term care (LTC) has been subject of significant regulatory focus in the U.S. since the Omnibus Budget Reconciliation Act (OBRA) of 1987.1 Attention increased further following a report from the U.S. Department of Health and Human Services Office of the Inspector General in 2011, which highlighted the largely off-label use of antipsychotic medications among LTC residents.2 Following the 2011 report, the Centers for Medicare and Medicaid Services’ (CMS) National Partnership to Improve Dementia Care (or, “the Partnership”) was introduced to improve dementia care, which was defined as reducing antipsychotic prescribing in LTC.3 To accomplish the desired reduction in antipsychotic prescribing, the Partnership emphasized non-pharmacologic treatment strategies through tools, trainings, and webinars. The antipsychotic measure used by the Partnership is also used in the publicly-reported Nursing Home Compare 5-star rating system.4
While antipsychotics cause a variety of side effects and adverse events, including increased risk of mortality when used to treat behavioral disturbances in patients with dementia, they remain the most evidence-based pharmacotherapy for agitation and psychosis.5 As antipsychotic prescribing in U.S. LTC settings has declined, use of antiepileptic medications (“mood stabilizers”) has risen.6 Mood stabilizers are used to treat bipolar disorder, though they are prescribed to patients with dementia to treat behavioral symptoms such as agitation and mood instability.7–9 Despite limited high-quality evidence to support use in dementia, valproic acid is the most common antipsychotic alternative among LTC clinicians and is not subject to quality reporting.10
Echoing concerns following the original OBRA legislation,11 there is concern among LTC clinicians that an over-correction may be underway due to the Partnership, where antipsychotics are being withheld from residents where use of these medications is appropriate. While the Partnership’s title includes “Dementia”, its antipsychotic prescribing quality measure is not limited to patients with dementia. The Partnership lists three exclusionary conditions for which treatment with an antipsychotic medication may be appropriate: schizophrenia, Tourette’s syndrome, and Huntington’s disease. However, the Partnership does not exclude residents with depression or bipolar disorder, even though some antipsychotics have been approved by the U.S. Food and Drug Administration (FDA) to treat these conditions. It is unclear if antipsychotic declines following the Partnership have been concentrated among residents with dementia—the intended target—or more widespread. Similarly, it is unknown if the rise in mood stabilizers has been limited to residents with dementia. Finally, it is unclear how prescribing of specific medications within these two classes has changed. This analysis uses Medicare data to examine: changes in LTC antipsychotic and mood stabilizer prescribing before and after the start of the Partnership; potentially unintended effects of the Partnership on treatment of residents with depression or bipolar disorders; and how use of specific agents has changed over time.
METHODS
Study Cohort.
Data were drawn from a 20% sample of Medicare beneficiaries from 2011–2014. We identified long-stay (>100 days) residents of nursing facilities based on place of service and current procedural terminology codes from physician visits in the Carrier (Physician/Supplier Part B file) and Outpatient files.12 Among these residents, we limited the sample to those with continuous fee-for-service and Medicare Part D coverage during the >100-day period that identified them as a long-stay resident. We used the same cohort exclusions that CMS applies for its antipsychotic monitoring: schizophrenia, Tourette’s syndrome, and Huntington’s disease. Residents with these conditions, identified using inpatient (Medicare Provider Analysis and Review file [MedPAR]) and outpatient files, were excluded from the primary analytic cohort (eTable 1). Encounters during the long-term stay-defining interval were used to identify these conditions. Residents contributed to a given quarterly denominator if they were at risk of the outcome (medication use) for at least one day during the quarter. That is, a long-stay resident remained in the cohort (i.e., denominator) until death or the end of the study period, whichever came first.
Because AP and mood stabilizer use among LTC residents with depression or bipolar disorder may be appropriate, we created a second cohort to examine if medication use among these residents was unintentionally reduced following the Partnership. For this analysis, we restricted the primary cohort to those with at least one diagnosis of depression or bipolar disorder but without dementia. If a resident was diagnosed with depression or bipolar disorder during the study (e.g., 2012 quarter 2), they contributed to the denominator beginning the quarter in which they were diagnosed.
Outcomes.
The outcomes of interest were antipsychotic and mood stabilizer use during a given quarter (eTable 2). Prescription fills were obtained from the Part D prescription drug event file. For residents in a given quarterly denominator, we determined if they had at least one day of antipsychotic or mood stabilizer supply in the quarter using the claim date and days’ supply fields. We attributed medication use to all possible quarters (e.g., a beneficiary with a 14-day prescription filled in the final week of quarter 1 contributed to the numerator for both quarters 1 and 2).
Demographic and Clinical Characteristics.
Age, gender, race/ethnicity, and state of residence were obtained from the Medicare Master Beneficiary Summary File. Presence of dementia, exclusion conditions, and clinical characteristics (i.e., the Elixhauser Index,13 delirium, Parkinson’s disease, post-traumatic stress disorder, personality disorder, and other anxiety disorders) were identified using the MedPAR and outpatient files (see eTable 1 for ICD-9-CM codes used).
Statistical Analysis.
We used multivariable logistic regression to model the odds of medication use over time by including time (quarter) in the model. The model was fit using generalized estimating equations with an autoregressive working correlation structure to account for the correlation among repeated observations on the same subject. We adjusted for patient demographics, Census Division, presence of dementia, and clinical characteristics that may be associated with psychotropic use, including individual Elixhauser conditions, delirium, Parkinson’s disease, post-traumatic stress disorder, personality disorder, other anxiety disorders.
Further, to examine if the odds of psychotropic use over time differed according to particular patient characteristics (e.g., age, race, sex, and dementia status), we fit a separate model for each characteristic and included its interaction with time (e.g., age*time). Interaction terms were tested using likelihood ratio tests. Lastly, we computed adjusted predicted probabilities of medication use overall and by specific characteristics (e.g., age) by setting all other variables to their average value over time. The same analyses were conducted for the second cohort—those without dementia and with depression or bipolar disorder—with dementia removed from the models.
Lastly, we examined which specific agents were increasing or decreasing over time by computing and plotting the percentage of users in a given medication class that used the specific agent during the quarter (e.g., percentage of antipsychotic users in given quarter that used quetiapine).
RESULTS
The cohort for the primary analysis included 562,485 long-stay nursing home residents with Medicare Part D from 2011–2014; 48.5% of residents during this time period had a diagnosis of dementia. Of the total sample, 39.8% (N=224,092) of residents had a diagnosis of depression either during study entry or during their long-term care stay; 3.3% (N=18,673) had a diagnosis of bipolar disorder. Of residents without dementia, 137,067 had depression and 12,513 had bipolar disorder (Table 1). The majority of residents overall were female (69.9%) and white (82.5%).
Table 1.
Characteristics of long-stay nursing home residents with Medicare Part D, 2011–2014, overall and for select subgroups
| Characteristic | Overall N=562,485 |
Dementia N=272,553 |
Depressiona N=137,067 |
Bipolara N=12,513 |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | |
| Age at NH entry, y (mean±S.D.) | 78.6 (12.1) | 82.3 (9.7) | 72.9 (13.5) | 61.8 (14.5) |
| Gender | ||||
| Male | 169,200 (30.1) | 75,780 (27.8) | 40,473 (29.5) | 4,298 (34.3) |
| Female | 393,285 (69.9) | 196,773 (72.2) | 96,594 (70.5) | 8,215 (65.7) |
| Race | ||||
| White | 464,053 (82.5) | 221,847 (81.4) | 115,750 (84.4) | 10,613 (84.8) |
| Black | 56,569 (10.1) | 29,288 (10.7) | 11,865 (8.7) | 1,076 (8.6) |
| Hispanic | 26,714 (4.7) | 14,366 (5.3) | 6,267 (4.6) | 564 (4.5) |
| Others | 15,149 (2.7) | 7,052 (2.6) | 3,185 (2.3) | 260 (2.1) |
| Clinical conditionsb | ||||
| Delirium | 91,970 (16.4) | 76,339 (28) | 10,090 (7.4) | 1,107 (8.8) |
| Parkinson | 22,475 (4) | 17,025 (6.2) | 3,086 (2.3) | 281 (2.2) |
| PTSD | 1,560 (0.3) | 460 (0.2) | 1,100 (0.8) | 382 (3.1) |
| Personality disorder | 1,397 (0.2) | 686 (0.3) | 623 (0.5) | 264 (2.1) |
| Other anxiety disorder | 72,961 (13) | 37,358 (13.7) | 26,869 (19.6) | 3,276 (26.2) |
| Dementia | 272,553 (48.5) | 272,553 (100.0) | – | – |
| Presence of select Elixhauser conditionsb | ||||
| Congestive Heart Failure | 142,804 (25.4) | 67,071 (24.6) | 37,890 (27.6) | 2,420 (19.3) |
| Hypertension Uncomplicated | 422,396 (75.1) | 203,167 (74.5) | 105,117 (76.7) | 8,160 (65.2) |
| Chronic Pulmonary Disease | 142,888 (25.4) | 60,008 (22) | 45,020 (32.8) | 4,279 (34.2) |
| Diabetes Uncomplicated | 193,243 (34.4) | 88,454 (32.5) | 53,405 (39) | 4,642 (37.1) |
| Renal Failure | 93,940 (16.7) | 40,467 (14.8) | 26,264 (19.2) | 1,916 (15.3) |
| Liver Disease | 18,291 (3.3) | 6,689 (2.5) | 6,628 (4.8) | 870 (7) |
| Obesity | 31,893 (5.7) | 7,939 (2.9) | 14,037 (10.2) | 1,622 (13) |
| Weight Loss | 48,398 (8.6) | 26,306 (9.7) | 12,530 (9.1) | 988 (7.9) |
| Alcohol Abuse | 6,479 (1.2) | 3,249 (1.2) | 2,187 (1.6) | 421 (3.4) |
| Drug Abuse | 3,087 (0.5) | 1,338 (0.5) | 1,426 (1) | 380 (3) |
| Psychoses | 45,026 (8) | 33,602 (12.3) | 7,886 (5.8) | 1,349 (10.8) |
| Total number of Elixhauser conditionsb | ||||
| 0 | 18,106 (3.2) | 8,230 (3) | 2,420 (1.8) | 491 (3.9) |
| 1–2 | 136,229 (24.2) | 66,300 (24.3) | 24,676 (18) | 2,709 (21.6) |
| 3–4 | 180,745 (32.1) | 91,220 (33.5) | 41,258 (30.1) | 3,656 (29.2) |
| 5–6 | 120,099 (21.4) | 58,166 (21.3) | 32,770 (23.9) | 2,762 (22.1) |
| 7–8 | 62,011 (11) | 28,888 (10.6) | 19,216 (14) | 1,583 (12.7) |
| ≥9 | 45,295 (8.1) | 19,749 (7.2) | 16,727 (12.2) | 1,312 (10.5) |
Excludes persons with dementia; columns are not mutually exclusive.
Presence determined from the resident’s date of entry into the cohort based on the 100-day period required to establish patient as a long-stay nursing home resident.
Antipsychotic and Mood Stabilizer Prescribing for Long-Stay Residents Overall
Among long-stay nursing home residents overall, the proportion prescribed an antipsychotic fell from 0.164 (95% confidence interval [CI] 0.162–0.165) to 0.115 (95% CI 0.114–0.116; eTable 3 and eFigure 1). Using the multivariable model accounting for cohort characteristics, the adjusted predicted probability (APP) of treatment fell from 0.120 (95% CI 0.119–0.121) to 0.100 (95% CI 0.099–0.101) from 2011–2014, a significant decrease over time (p<0.001; Table 2). While a small decline occurred among persons without dementia, the decrease in APP of antipsychotic treatment was larger for persons with dementia, falling from 0.174 (95% CI 0.172–0.176) to 0.136 (0.134–0.138) (p<0.001 for dementia × time interaction). Declines were slightly largely for those 75–84 and ≥85 (compared to those 65–74; p<0.001 for time × age group interaction) and slightly larger for Black and Hispanic compared to White residents (p<0.001 for time × race/ethnicity interaction).
Table 2.
Change in risk-adjusted probability of antipsychotic and mood stabilizer treatment among long-stay nursing home residents in the U.S. from the first quarter of 2011 to final quarter of 2014 (N = 562,485)
| Variable | Antipsychotics | Mood stabilizers | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2011, quarter 1 | 2014, quarter 4 | P-valuea | 2011, quarter 1 | 2014, quarter 4 | P-valuea | |||||
| Adjusted predicted probability | 95%CI | Adjusted predicted probability | 95%CI | Adjusted predicted probability | 95%CI | Adjusted predicted probability | 95%CI | |||
| Overall | 0.120 | (0.119–0.121) | 0.100 | (0.099–0.101) | <0.001 | 0.140 | (0.139–0.141) | 0.185 | (0.184–0.186) | <0.001 |
| Age | ||||||||||
| <75 (ref) | 0.130 | (0.128–0.132) | 0.118 | (0.116–0.120) | <0.001 | 0.177 | (0.175–0.179) | 0.234 | (0.232–0.237) | <0.001 |
| 75–84 | 0.118 | (0.116–0.119) | 0.094 | (0.093–0.096) | --b | 0.136 | (0.135–0.138) | 0.183 | (0.181–0.185) | -- |
| 85+ | 0.114 | (0.113–0.116) | 0.090 | (0.089–0.092) | --b | 0.119 | (0.118–0.120) | 0.152 | (0.150–0.153) | --b |
| Sex | ||||||||||
| Female (ref) | 0.115 | (0.114–0.116) | 0.095 | (0.094–0.096) | <0.001 | 0.140 | (0.138–0.141) | 0.186 | (0.185–0.188) | <0.001 |
| Male | 0.134 | (0.132–0.136) | 0.112 | (0.110–0.114) | -- | 0.141 | (0.139–0.143) | 0.181 | (0.179–0.183) | --b |
| Race/ethnicity | ||||||||||
| White (ref) | 0.121 | (0.120–0.122) | 0.102 | (0.101–0.103) | <0.001 | 0.143 | (0.141–0.144) | 0.187 | (0.186–0.189) | <0.001 |
| Black | 0.111 | (0.108–0.114) | 0.085 | (0.082–0.087) | --b | 0.130 | (0.127–0.133) | 0.177 | (0.173–0.180) | -- |
| Hispanic | 0.136 | (0.132–0.141) | 0.104 | (0.100–0.108) | --b | 0.130 | (0.126–0.135) | 0.172 | (0.167–0.177) | -- |
| Others | 0.102 | (0.096–0.108) | 0.082 | (0.077–0.087) | -- | 0.122 | (0.116–0.129) | 0.160 | (0.154–0.166) | -- |
| Dementia | ||||||||||
| No (ref) | 0.089 | (0.088–0.090) | 0.083 | (0.082–0.084) | <0.001 | 0.131 | (0.129–0.132) | 0.180 | (0.179–0.182) | <0.001 |
| Yes | 0.174 | (0.172–0.176) | 0.136 | (0.134–0.138) | --b | 0.154 | (0.152–0.156) | 0.191 | (0.190–0.193) | b |
Adjusted predicted probabilities of antipsychotic and mood stabilizer use in 2011Q1 and 2014Q4 for the overall cohort were obtained based on a model with time adjusting for age, gender, race, census division, the presence of dementia, the Elixhauser conditions, as well as additional clinical diagnoses (delirium, Parkinson’s disease, post-traumatic stress disorder, personality disorder, other anxiety disorders). For each characteristic-specific sub-cohort, the adjusted predicted probabilities were obtained using additional interaction terms of time (as a continuous variable) by the specific sub-cohort factor variables. For example, for sex sub-cohorts, the models for antipsychotic use and mood stabilizer use each included time by sex indicator of male × time, with female as the referent category.
P-value reflects significance test for time effect in the main model for the overall cohort and referent categories (e.g., p<0.001 for patients without dementia [reference] means that the probability of antipsychotic use for persons without dementia changed [decreased] with time).
p<0.001 (or c p<0.01) for a significant characteristic-by-time effect that differs from the referent sub-group category (e.g., for persons with dementia, the effect of time on likelihood of antipsychotic treatment was different than for persons without dementia [reference]).
Among long-stay nursing home residents overall, both the unadjusted proportion and APP of mood stabilizer treatment were higher than those of antipsychotic treatment. The APP of residents prescribed a mood stabilizer rose from 0.170 (95% CI 0.169–0.172) to 0.201 (95% CI 0.199–0.202; eTable 3 and eFigure 2). Using the multivariable model accounting for cohort characteristics, the APP of mood stabilizer treatment rose from 0.140 (95% CI 0.139–0.141) to 0.185 (95% CI 0.184–0.186) from 2011–2014, a significant increase over time (p<0.001; Table 2). The increase among persons without dementia was larger—the APP rose from 0.131 (95% CI 0.129–0.132) to 0.180 (0.179–0.182)—than for persons with dementia (p<0.001 for dementia × time interaction). Mood stabilizer use increased for all age, sex, and race/ethnicity groups, though was slightly smaller for the oldest residents (p<0.001 for age × time interaction for those ≥85) and for men (p<0.001 for age × sex interaction).
Antipsychotic and Mood Stabilizer Prescribing to Persons with Depression or Bipolar Disorder
Among long-stay nursing home residents with depression or bipolar disorder (excluding persons with dementia), antipsychotic prescribing was lower than among residents overall. The unadjusted proportion fell from 0.115 (95% CI 0.112–0.118) to 0.102 (95% CI 0.1–0.104; eTable 4 and eFigure 3). However, APP of antipsychotic treatment rose slightly from 0.081 (95% CI 0.079–0.082) to 0.087 (95% CI 0.085–0.088) from 2011–2014 (p<0.001; Table 3). There was a small decline in the APP of antipsychotic treatment among Hispanic residents, from 0.085 (95% CI 0.077–0.095) to 0.078 (95% CI 0.072–0.085; p<0.001 for race/ethnicity × time interaction). The APP of treatment rose for all other groups.
Table 3.
Change in risk-adjusted probability of antipsychotic and mood stabilizer treatment among long-stay nursing home residents in the U.S. with depression or bipolar disorder from the first quarter of 2011 to final quarter of 2014 (N = 139,071).
| Variable | Antipsychotics | Mood stabilizers | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2011Q1 | 2014Q4 | 2011Q1 | 2014Q4 | P-valuea | ||||||
| Adjusted predicted probability | 95%CI | Adjusted predicted probability | 95%CI | P-valuea | Adjusted predicted probability | 95%CI | Adjusted predicted probability | 95%CI | ||
| Overall | 0.081 | (0.079–0.082) | 0.087 | (0.085–0.088) | <0.001 | 0.193 | (0.190–0.196) | 0.251 | (0.248–0.253) | <0.001 |
| Age | ||||||||||
| <75 (ref) | 0.107 | (0.104–0.110) | 0.115 | (0.112–0.117) | <0.001 | 0.229 | (0.225–0.233) | 0.295 | (0.291–0.299) | <0.001 |
| 75–84 | 0.064 | (0.062–0.067) | 0.070 | (0.068–0.072) | -- | 0.169 | (0.165–0.173) | 0.230 | (0.226–0.234) | -- |
| 85+ | 0.054 | (0.051–0.057) | 0.058 | (0.056–0.060) | -- | 0.151 | (0.147–0.156) | 0.186 | (0.182–0.190) | --b |
| Sex | ||||||||||
| Female (ref) | 0.076 | (0.074–0.078) | 0.082 | (0.080–0.084) | <0.001 | 0.195 | (0.192–0.199) | 0.256 | (0.253–0.259) | <0.001 |
| Male | 0.094 | (0.090–0.097) | 0.100 | (0.097–0.103) | -- | 0.187 | (0.182–0.192) | 0.238 | (0.234–0.243) | -- |
| Race/ethnicity | ||||||||||
| White (ref) | 0.082 | (0.080–0.084) | 0.089 | (0.087–0.091) | <0.001 | 0.195 | (0.192–0.198) | 0.253 | (0.250–0.256) | <0.001 |
| Black | 0.070 | (0.064–0.076) | 0.074 | (0.070–0.079) | -- | 0.182 | (0.173–0.191) | 0.246 | (0.238–0.254) | -- |
| Hispanic | 0.085 | (0.077–0.095) | 0.078 | (0.072–0.085) | --b | 0.176 | (0.165–0.189) | 0.232 | (0.221–0.243) | -- |
| Others | 0.076 | (0.066–0.088) | 0.077 | (0.068–0.087) | -- | 0.187 | (0.170–0.206) | 0.225 | (0.210–0.240) | -- |
Adjusted predicted probabilities determined from logistic regression models adjusted for age, gender, race, census division, the Elixhauser conditions, as well as additional clinical diagnoses (delirium, Parkinson’s disease, post-traumatic stress disorder, personality disorder, other anxiety disorders). For each characteristic-specific sub-cohort, the adjusted predicted probabilities were obtained using additional interaction terms of time (as a continuous variable) by the specific sub-cohort factor variables. For example, for sex sub-cohorts, the models for antipsychotic use and mood stabilizer use each included time by sex indicator of male × time, with female as the referent category.
P-value reflects significance test for time effect in the main model for the overall cohort and referent categories (e.g., p<0.001 for residents <75 [reference] means that the probability of antipsychotic use by persons with depression or bipolar disorder changed [increased] with time).
p<0.001 (or c p<0.01) for a significant characteristic-by-time effect that differs from the referent sub-group category (e.g., in the case of age, the effect of time on likelihood of antipsychotic treatment was no different than those 75–84 or 85+ than for those <75 [reference]).
Among this cohort, the proportion prescribed a mood stabilizer rose from 0.233 (95% CI 0.229–0.237) to 0.264 (95% CI 0.262–0.267; eTable 4 and eFigure 4). The APP of mood stabilizer treatment rose from 0.193 (95% CI 0.190–0.196) to 0.251 (95% CI 0.248–0.253) from 2011–2014, a significant increase over time (p<0.001; Table 3). Mood stabilizer use increased for all age, sex, and race/ethnicity groups, though was slightly smaller for the oldest residents (p<0.001 for age × time interaction for those ≥85), growing only from 0.151 (95% CI 0.147–0.165) to 0.186 (95% CI 0.182–0.190).
Use of Specific Antipsychotics and Mood Stabilizers
Of all antipsychotic users, quetiapine was used most commonly. While the APP of receiving quetiapine declined slightly over time (Table 4), quetiapine accounted for an increasing share of antipsychotic prescribing overall. Compared to the start of 2011, the APP of quetiapine use decreased slightly from 0.049 (95% CI 0.048–0.049) to 0.043 (95% CI 0.043–0.044) by the end of 2014, but the percentage of persons prescribed antipsychotics on quetiapine grew from 42.5% to 45.6% (Figure 1a; eTable 5). When limiting the analysis to antipsychotic medications that were FDA approved for treatment of depressive episodes during the study period (e.g., aripiprazole, olanzapine/fluoxetine, quetiapine, and lurasidone), the APP of receiving these antipsychotics increased from 0.043 in 2011 to 0.049 by the end of 2014 (eTable 6).
Table 4:
Change in risk-adjusted probability of treatment with the most common antipsychotics and mood stabilizers among long-stay nursing home residents in the U.S., 2011–2014 (N = 562,485)
| 2011, quarter 1 | 2014, quarter 4 | ||||
|---|---|---|---|---|---|
| Adjusted predicted probability | 95%CI | Adjusted predicted probability | 95%CI | P-valuea | |
| Antipsychotics | |||||
| Quetiapine | 0.049 | (0.048–0.049) | 0.043 | (0.043–0.044) | <0.001 |
| Risperidone | 0.036 | (0.035–0.037) | 0.027 | (0.026–0.027) | <0.001 |
| Olanzapine | 0.016 | (0.015–0.016) | 0.012 | (0.012–0.013) | <0.001 |
| Other atypical APs | 0.012 | (0.011–0.012) | 0.011 | (0.011–0.011) | <0.001 |
| Conventional APs | 0.012 | (0.012–0.013) | 0.009 | (0.009–0.009) | <0.001 |
| Mood stabilizers | |||||
| Gabapentin | 0.086 | (0.085–0.086) | 0.126 | (0.125–0.127) | <0.001 |
| Valproate/derivatives | 0.028 | (0.028–0.029) | 0.030 | (0.030–0.031) | <0.001 |
| Carbamazepine | 0.006 | (0.006–0.007) | 0.006 | (0.005–0.006) | 0.0017 |
| Other | 0.011 | (0.010–0.011) | 0.014 | (0.013–0.014) | <0.001 |
Adjusted predicted probabilities were obtained based on separate models for each agent adjusting for age, gender, race, census division, the presence of dementia, the Elixhauser conditions, as well as additional clinical diagnoses (delirium, Parkinson’s disease, post-traumatic stress disorder, personality disorder, other anxiety disorders).
P-value reflects significance test for time effect for use of each individual agent.
Figure 1a and 1b.
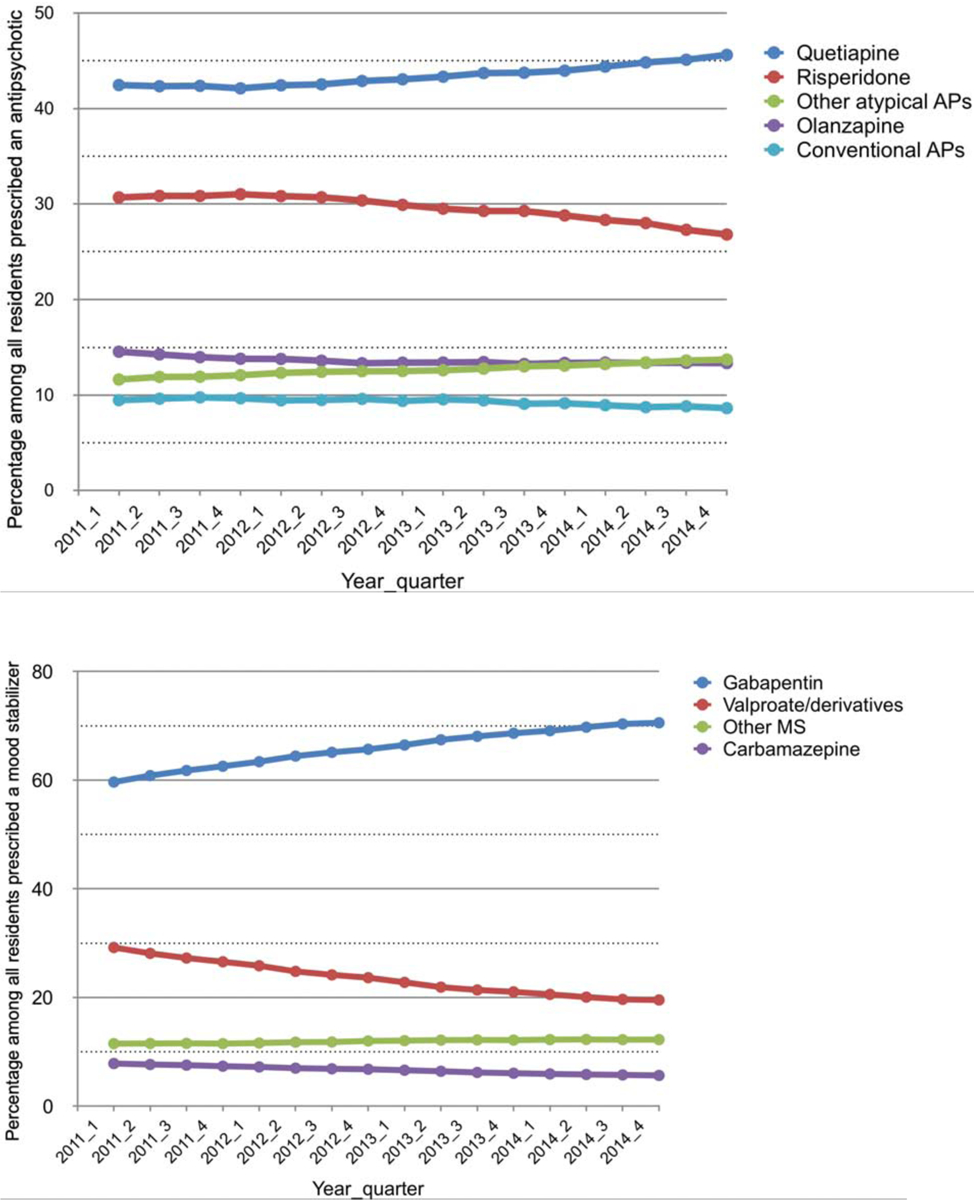
The most common antipsychotics (1a) and mood stabilizers (1b) prescribed to long-stay nursing home residents in the U.S. as a percentage of residents receiving each class, 2011–2014 (N=123,101 AP users [Figure 1a] and N=153,120 mood stabilizer users [Figure 1b]).
Gabapentin was the most commonly prescribed mood stabilizer to the overall cohort. Unlike antipsychotics, for whom the probability of treatment fell, the APP of gabapentin treatment grew from 0.086 (95% CI 0.085–0.086) to 0.126 (95% CI 0.125–0.127, p<0.001), a relative increase of nearly 50% (Table 4). Among those prescribed mood stabilizers, gabapentin was prescribed to 70.5% at the end of 2014 (Figure 1b; eTable 7). Among nursing home residents prescribed gabapentin, 91.2% had a diagnosis of chronic pain.
DISCUSSION
In this analysis of antipsychotic and mood stabilizer prescribing since the CMS National Partnership, we found that the overall likelihood of antipsychotic treatment declined for residents in LTC, with larger declines for residents with dementia. However, this was offset by an increase in the probability of mood stabilizer treatment for residents with dementia, which was of nearly identical size. The likelihood of antipsychotic treatment specifically among residents with depression or bipolar disorder—for whom antipsychotic use may be appropriate—did not decrease. Nearly half of residents prescribed an antipsychotic received quetiapine, while over 70% of residents prescribed mood stabilizers received gabapentin. Lastly, the prevalence rate of dementia, depression, and bipolar disorder among our sample of long-stay nursing home residents was 48.5%, 39.8%, and 3.3% respectively—which is consistent with previously published studies.14–16
Reductions in antipsychotic prescribing have been widespread. While the probability of treatment is still higher among persons with dementia, the relative decline was greater for residents with dementia, which was the intent of the Partnership. The rank order of specific agents being prescribed (e.g., quetiapine first) is consistent with what Breisacher et al. reported in long-term care from 2009–2010.17 While quetiapine generally has a lower associated mortality risk,18,19 it also has less evidence of benefit than other antipsychotics for treatment of behavioral symptoms.20,21
Even in 2011, before the Partnership began, mood stabilizer use exceeded antipsychotic prescribing. By the end of 2014 this gap had grown so that the probability of treatment with a mood stabilizer was nearly 10% higher in absolute terms than antipsychotic treatment. While declines in antipsychotic prescribing were more pronounced among residents with dementia, the growth in mood stabilizer use was more widespread, with large increases for both residents with and without dementia as well as among persons with depression or bipolar disorder. We anticipated that this class would be largely comprised of valproate, a widely used substitute for antipsychotics.10 However, valproate was a distant second among mood stabilizers, prescribed to just 20% of residents on mood stabilizers.
The growth in mood stabilizer use was dominated by gabapentin—the probability of a patient in LTC being prescribed this medication grew from 0.086 to 0.126 by the end of 2014, a relative increase of nearly 50%. The probability of gabapentin treatment was far higher than use of any other individual medication; the next-highest treatment probability was for quetiapine, at just 0.043 by the end of 2014. To our knowledge, this is the first analysis to describe the extent of gabapentin’s use in LTC. Use of mood stabilizers may have escaped close examination partly because they are not collected by the Minimum Data Set, the primary assessment completed for all nursing facility residents and used for the Partnership and the Nursing Home Compare quality rating system.
The outsize role of gabapentin perhaps should not have been surprising, given evidence of its growing use overall among non-LTC populations.22,23 While once considered with other mood stabilizers as an antipsychotic substitute,24,25 there is little evidence to support its use for behavioral symptoms in dementia, though it is routinely prescribed off-label by clinicians for symptoms such as anxiety, insomnia, and agitation.5 Johansen’s recent analysis demonstrated growth in use concentrated among those over 64, with a higher number of medical comorbidities, and those prescribed additional medications such as opioids or benzodiazepines. It may be that the gabapentin is being prescribed as an opioid alternative for pain. Among long-stay residents who received gabapentin in our analysis, 91% had a diagnosis of chronic pain. However, there is limited evidence to support the efficacy of gabapentin for this indication,26 reminiscent of the spread of its use for bipolar disorder, despite limited evidence.27
It is reassuring that the likelihood of antipsychotic treatment had not declined among persons with depression or bipolar disorders, for whom antipsychotic prescribing may be appropriate, at least by the end of 2014. Given the broad nature of the Partnership, including the fact that diagnosis-based exclusions from the antipsychotic quality measure were limited to just schizophrenia, Tourette’s syndrome, and Huntington’s disease, it was conceivable that antipsychotic prescribing may have declined for residents in whom it was clinically appropriate. Our analysis suggests that, at least through the end of 2014, treatment declines did not occur among residents with other psychiatric disorders.
There is limited longitudinal data with which to compare our findings. Two recent longitudinal studies of LTC residents with dementia in Canada found declines in antipsychotic prescribing of 6% but even larger growth in use of both sedative and non-sedative antidepressants and a small increase in mood stabilizer use (2%).28,29 These analyses did not consider mood stabilizers. Cross-sectional studies from Europe and Australia have generally found antidepressant use to be most common, followed by sedatives-anxiolytic/hypnotics and then antipsychotics, at levels similar to those found here.30–32 Mood stabilizer use was only considered in the Australian analysis, though gabapentin was not included.
Our analysis has several limitations. We derived our cohort of long-stay nursing home residents based on their Medicare claims rather than Minimum Data Set assessments, though this approach has high sensitivity (0.87) and specificity (0.96).12 Our sample is limited to those with continuous fee-for-service and Part D Medicare coverage and therefore does not include the growing population of Medicare Advantage beneficiaries nor non-Part D prescriptions. This analysis of prescription claims does not capture actual medication use and claims data do not include the prescribing indication. As such we are unable to determine whether these medications were prescribed for treatment of depression, bipolar disorder, behavioral disturbances in dementia, or other indication (e.g., gabapentin for treatment of pain). We were unable to assess physical restraint use, though reports from CMS demonstrate that use has substantially declined over the past two decades.33 Our analysis ends in 2014 and does not capture the most recent prescribing trends. Finally, administrative claims data do not capture use of non-pharmacologic treatment strategies, so we were not able to account for potential substitution of non-medication treatment strategies.
CONCLUSIONS AND IMPLICATIONS
Antipsychotic declines that occurred following the CMS National Partnership were widespread but were larger among residents with dementia. Importantly, the likelihood of antipsychotic treatment did not decline for residents with depression or bipolar disorder, for whom such prescribing would have been more appropriate but who were not excluded from the Partnership’s antipsychotic quality measure. The growth in mood stabilizer prescribing was even more widespread than the antipsychotic declines, included residents with dementia, and was largely driven by gabapentin prescribing. Regardless of whether the growth in this prescribing was for behavioral symptoms or other reasons (e.g., pain), growing use of this class merits cautious monitoring.
Supplementary Material
Acknowledgments:
Role of the Funder/Sponsor: The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Funding Source: This work was supported by The Patrick and Catherine Weldon Donaghue Medical Research Foundation and NIA P30AG024824.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures: The authors have none to disclose.
REFERENCES
- 1.Elon R, Pawlson LG. The impact of OBRA on medical practice within nursing facilities. J Am Geriatr Soc. 1992;40(9):958–963. [DOI] [PubMed] [Google Scholar]
- 2.Office of Inspector General, US Department of Health and Human Services. Medicare atpical antipsychotic drug claims for elderly nursing home residents. May 2011. https://oig.hhs.gov/oei/reports/oei-07-08-00150.pdf. Accessed on Aug 29, 2019.
- 3.Centers for Medicare and Medicaid Services. CMS announces partnership to improve dementia care in nursing homes. Available from: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-Releases/2012-Press-Releases-Items/2012-05-30.html. Accessed March 23, 2016.
- 4.Medicare.gov. “About Nursing Home Compare data.” https://www.medicare.gov/nursinghomecompare/Data/About.html. Accessed Oct 21,2019.
- 5.Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. BMJ. 2015;350:h369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maust DT, Kim HM, Chiang C, Kales HC. Association of the Centers for Medicare & Medicaid Services’ National Partnership to Improve Dementia Care With the Use of Antipsychotics and Other Psychotropics in Long-term Care in the United States From 2009 to 2014. JAMA Intern Med. 2018;178(5):640–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lott AD, McElroy SL, Keys MA. Valproate in the treatment of behavioral agitation in elderly patients with dementia. J Neuropsychiatry Clin Neurosci. 1995;7(3):314–319. [DOI] [PubMed] [Google Scholar]
- 8.Chambers CA, Bain J, Rosbottom R, Ballinger BR, Mclaren S. Carbamazepine in Senile Dementia and Overactivity - a Placebo Controlled Double-Blind Trial. Ircs Medical Science-Biochemistry. 1982;10(6):505–506. [Google Scholar]
- 9.Herrmann N, Lanctôt K, Myszak M. Effectiveness of gabapentin for the treatment of behavioral disorders in dementia. J Clin Psychopharmacol. 2000;20(1):90–93. [DOI] [PubMed] [Google Scholar]
- 10.Olivieri-Mui BL, Devlin JW, Ochoa A, Schenck D, Briesacher B. Perceptions vs. evidence: therapeutic substitutes for antipsychotics in patients with dementia in long-term care. Aging & Mental Health. 2018;22(4):544–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Colenda CC, Streim J, Greene JA, Meyers N, Beckwith E, Rabins P. The impact of OBRA ‘87 on psychiatric services in nursing homes - Joint testimony of the American Psychiatric Association and the American Association for Geriatric Psychiatry. Am J Geriatr Psychiatry. 1999;7(1):12–17. [PubMed] [Google Scholar]
- 12.Yun H, Kilgore ML, Curtis JR, et al. Identifying types of nursing facility stays using medicare claims data: an algorithm and validation. Health Services & Outcomes Research Methodology. 2010;10(1–2):100–110. [Google Scholar]
- 13.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical Care. 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 14.Magaziner J, German P, Zimmerman SI, et al. The prevalence of dementia in a statewide sample of new nursing home admissions aged 65 and older: diagnosis by expert panel. Epidemiology of Dementia in Nursing Homes Research Group. Gerontologist. 2000;40(6):663–672. [DOI] [PubMed] [Google Scholar]
- 15.Payne JL, Sheppard JM, Steinberg M, et al. Incidence, prevalence, and outcomes of depression in residents of a long-term care facility with dementia. Int J Geriatr Psychiatry. 2002;17(3):247–253. [DOI] [PubMed] [Google Scholar]
- 16.Grabowski DC, Aschbrenner KA, Feng Z, Mor V. Mental illness in nursing homes: variations across States. Health Aff. 2009;28(3):689–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Briesacher BA, Tjia J, Field T, Peterson D, Gurwitz JH. Antipsychotic use among nursing home residents. JAMA. 2013;309(5):440–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kales HC, Kim HM, Zivin K, et al. Risk of mortality among individual antipsychotics in patients with dementia. American Journal of Psychiatry. 2012;169(1):71–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huybrechts KF, Gerhard T, Crystal S, et al. Differential risk of death in older residents in nursing homes prescribed specific antipsychotic drugs: population based cohort study. BMJ. 2012;344:e977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yunusa I, Alsumali A, Garba AE, Regestein QR, Eguale T. Assessment of Reported Comparative Effectiveness and Safety of Atypical Antipsychotics in the Treatment of Behavioral and Psychological Symptoms of Dementia: A Network Meta-analysis. JAMA NetworkOopen. 2019;2(3):e190828–e190828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maher AR, Maglione M, Bagley S, et al. Efficacy and comparative effectiveness of atypical antipsychotic medications for off-label uses in adults: a systematic review and meta-analysis. JAMA. 2011;306(12):1359–1369. [DOI] [PubMed] [Google Scholar]
- 22.Johansen ME. Gabapentinoid use in the United States 2002 through 2015. JAMA Intern Med. 2018;178(2):292–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goodman CW, Brett AS. Gabapentin and pregabalin for pain—is increased prescribing a cause for concern? N Engl J Med. 2017;377(5):411–414. [DOI] [PubMed] [Google Scholar]
- 24.Gardner M, Ditmanson L, Garrett RW, Luu T, Meiling F. Anticonvulsant use in treating dementia-related agitation. J Pharm Pract. 2000;13(4):308–315. [Google Scholar]
- 25.Tariot PN, Schneider LS, Katz IR. Anticonvulsant and other non-neuroleptic treatment of agitation in dementia. J Geriatr Psychiatry Neurol. 1995;8(1):S28–S39. [DOI] [PubMed] [Google Scholar]
- 26.Goodman CW, Brett AS. A Clinical Overview of Off-label Use of Gabapentinoid Drugs. JAMA Intern Med. 2019;179(5):695–701. [DOI] [PubMed] [Google Scholar]
- 27.Williams JW Jr, Ranney L, Morgan LC, Whitener L. How reviews covered the unfolding scientific story of gabapentin for bipolar disorder. Gen Hosp Psychiatry. 2009;31(3):279–287. [DOI] [PubMed] [Google Scholar]
- 28.Vasudev A, Shariff SZ, Liu K, et al. Trends in Psychotropic Dispensing Among Older Adults with Dementia Living in Long-Term Care Facilities: 2004–2013. Am J Geriatr Psychiatry. 2015;23(12):1259–1269. [DOI] [PubMed] [Google Scholar]
- 29.Ivers NM, Taljaard M, Giannakeas V, Reis C, Williams E, Bronskill S. Public reporting of antipsychotic prescribing in nursing homes: population-based interrupted time series analyses. BMJ Quality & Safety. 2019;28(2):121–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Westbury J, Gee P, Ling T, Kitsos A, Peterson G. More action needed: Psychotropic prescribing in Australian residential aged care. Aust N Z J Psychiatry. 2019;53(2):136–147. [DOI] [PubMed] [Google Scholar]
- 31.Smeets CHW, Gerritsen DL, Zuidema SU, et al. Psychotropic drug prescription for nursing home residents with dementia: prevalence and associations with non-resident-related factors. Aging & Mental Health. 2018;22(9):1244–1252. [DOI] [PubMed] [Google Scholar]
- 32.Gustafsson M, Sandman PO, Karlsson S, Gustafson Y, Lövheim H. Association between behavioral and psychological symptoms and psychotropic drug use among old people with cognitive impairment living in geriatric care settings. Int Psychogeriatr. 2013;25(9):1415–1423. [DOI] [PubMed] [Google Scholar]
- 33.Department of Health and Human Services. Centers for Medicare and Medicaid Services. Release of report: “Freedom from unnecessary physical restraints: two decades of national progress in nursing home care”. Published November 2008. Accessed on May 5, 2020 Available at https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Policy-and-Memos-to-States-and-Regions-Items/CMS1217030. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


