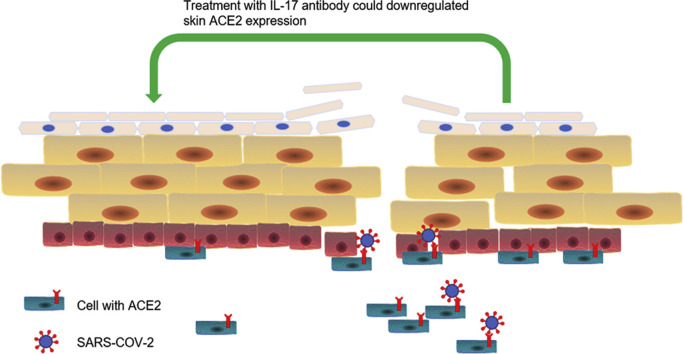
Graphical abstract
Key words: ACE2, atopic dermatitis, COVID-19, IL-17 antibody, psoriasis, SARS-COV-2
To the Editor: In the era of the coronavirus disease 2019 (COVID-19) pandemic, debates have emerged on whether biologics might increase the risk of contracting the disease.1 Interleukin (IL) 17 is a biologic that is widely used in dermatology. There were reports that viral reactivation, although extremely low, could be detected during the use of IL-17 antibody (160 mg subcutaneously at Week 0, followed by 80 mg at Weeks 2, 4, 6, 8).2 This led to concerns in using the IL-17 antibody because it was believed that it could make patients more susceptible to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). When we read the article by Sun et al3 in a recently published issue, a question occurred to us: If skin is a target of SARS-CoV-2, what might be the consequence of using the IL-17 antibody?
Angiotensin-converting enzyme 2 (ACE2) is the main entrance receptor for SARS-CoV-2. Its expression is associated with the risk of making the target tissue susceptible to infection by SARS-CoV-2. Therefore, downregulating the expression of ACE2 could decrease the risk of COVID-19. To evaluate the influence of IL-17 antibody on skin ACE2 expression, we randomly selected 5 psoriasis patients who were treated with IL-17 antibody (Taltz, Eli Lilly and Company, Indianapolis, IN). The skin lesions of these patients were biopsied on week 0 and week 8 and prepared for RNA sequencing. The skin ACE2 expression of patients who underwent the antibody therapy for 8 weeks (0.36 ± 0.10; n = 5) was downregulated compared with that at week 0 (1.24 ± 0.50; n = 5), when the IL-17 antibody treatment had just begun (P < .05, paired t test). To confirm the result, we also selected 3 patients to compare the skin ACE2 expression at weeks 0 and 8 with immunofluorescence. Immunofluorescence staining revealed that the fluorescence intensity of ACE2 was downregulated in the skin at week 8 (0.84 ± 0.26; n = 3) compared with that before the IL-17 antibody treatment (9.23 ± 2.33; n = 3; P < .05; unpaired t test). Hence, either the messenger RNA or protein of ACE2 obtained from psoriasis patients can reveal that IL-17 antibody treatment remarkably reduces ACE2 expression.
Our above-mentioned work proves that IL-17 antibody treatment during the COVID-19 pandemic is not contraindicated. Elevated ACE2 expression and detection of SARS-CoV-2 in the skin4 of COVID-19 patients implied skin was a potential host of SARS-CoV-2. After IL-17 antibody treatment, the skin ACE2 expression was downregulated, which meant IL-17 antibody could decrease the risk of COVID-19 through lessening the cells that could interact with SARS-CoV-2. Additionally, IL-17 antibody could reverse the deteriorated barrier and inflammatory status in the skin of psoriasis patients, which meant less microbe infection. Herein, the specific microbe could be SARS-CoV-2. To our knowledge, until now there has been no evidence that COVID-19 can be spread by contact with skin. However, SARS-CoV-2 could survive on skin for about 9 hours,5 which indicates that it might be transmitted through skin in certain skin conditions such as psoriasis. Thus, whether IL-17 antibody could reduce the COVID-19 risk through reversing the inflammatory skin status with a deteriorated barrier and preventing SARS-CoV-2 transmission should be further discussed.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
IRB approval status: Not applicable.
Reprints not available from the authors.
References
- 1.Lebwohl M., Rivera-Oyola R., Murrell D.F. Should biologics for psoriasis be interrupted in the era of COVID-19? J Am Acad Dermatol. 2020;82(5):1217–1218. doi: 10.1016/j.jaad.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Snast I., Atzmony L., Braun M., Hodak E., Pavlovsky L. Risk for hepatitis B and C virus reactivation in patients with psoriasis on biologic therapies: a retrospective cohort study and systematic review of the literature. J Am Acad Dermatol. 2017;77(1):88–97.e5. doi: 10.1016/j.jaad.2017.01.037. [DOI] [PubMed] [Google Scholar]
- 3.Sun Y., Zhou R., Zhang H., et al. Skin is a potential host of SARS-CoV-2: a clinical, single-cell transcriptome-profiling and histological study. J Am Acad Dermatol. 2020;83(6):1755–1757. doi: 10.1016/j.jaad.2020.08.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colmenero I., Santonja C., Alonso-Riaño M., et al. SARS-CoV-2 endothelial infection causes COVID-19 chilblains: histopathological, immunohistochemical and ultrastructural study of seven paediatric cases. Br J Dermatol. 2020;183(4):729–737. doi: 10.1111/bjd.19327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirose R., Ikegaya H., Naito Y., et al. Survival of SARS-CoV-2 and influenza virus on the human skin: importance of hand hygiene in COVID-19. Clin Infect Dis. 2020:ciaa1517 doi: 10.1093/cid/ciaa1517. [DOI] [PMC free article] [PubMed] [Google Scholar]