Occupational risk tools relating to COVID-19 infection currently suffer from limitations including abridging risk ratios, use of hard bordered categories, the rigid linking of risk score to outcome and focus on relative rather than absolute risk. Critically, most occupational risk assessment tools fail to include assessment of the level of work-based environmental risk and its mitigation (which together determine risk of exposure to and acquisition of infection) and simply focus on personal attributes (which only determine the impact of infection once acquired).
Here we use healthcare workers and data from the United Kingdom as an example for this argument, though it also applies to many other working environments and countries. In the UK an estimated three quarters of a million individuals who withdrew from community contact because of personal risk factors (shielded) returned to their workplace in August. Many are healthcare workers. The British Medical Association published a briefing on returning to work and emphasises that all staff should have “timely, individual and bespoke COVID-19 risk assessments” [1]. Given the need to “communicate realistic levels of risk… to allow informed personal decisions in a setting of necessary uncertainty” [2], several occupational risk tools have been produced for healthcare workers [3], [4], [5], [6]. Early tools inevitably relied on limited scientific information, but more recent ones use information from large epidemiological datasets of COVID-19 in general practice [7] or in hospitalised patients [8]. These enable an individual's characteristics to be used to calculate the relative risk of death compared to a low risk reference individual [7]. All occupational risk tools use age, sex at birth, ethnicity and co-morbidities as variables and a minority include some measures of social circumstances. Given the potential complexity of incorporating these variables, simplification strategies have included: abridging risk ratios by allocating a point for each (roughly) doubling of risk; grouping ranges of risk into discrete categories of risk (‘RAG-rating’ or ‘low to very high’) and linking these categories to prescribed workplace adaptations (e.g. unrestricted work, or work-restricted to certain patient groups) or actions (e.g. staff redeployment or home working).
However, risk-stratification tools have several significant limitations that healthcare workers and employers must consider before policymaking. First, all tools focus on relative risk (multipliers of risk). This identifies who is more at risk, but not by how much, nor whether absolute risk is actually low, intermediate or high. In a low-risk setting (e.g. between pandemic surges) multiplying a very low risk by a relative risk of three, four or even five will not increase absolute risk substantially. However, when overall risk is increased (e.g. during a pandemic surge) these multipliers will have dramatically higher impacts on absolute risk for the higher risk individuals and on the differences between individuals.
Second, particularly where multiple risk factors co-exist, smoothing relative risk ratings into a points score can lead to loss of accuracy compared to simply using reported ratios.
Third, categorisation is artificial, as risk is a continuous, not a categorical variable. For those who fall either side of a boundary, their risk will be almost identical, but their allocated categories will differ and any linked pre-defined actions may result in two individuals of almost identical risk being treated quite differently. Consider a tool that uses age or adjusted-age as a surrogate of risk and classifies those with an adjusted-age <50 as low risk and between 50 and 69 as moderate risk. Those categorised low risk are designated suitable for unrestricted workplace activity while moderate risk triggers working restrictions. In reality, risk of mortality from COVID-19 increases approximately 12% per year of age [9]. Now, consider three individuals whose tool-adjusted-ages are 49, 50 and 69 years. This means that although the individual who is adjusted-age 50 has no more than a 12% difference in mortality compared to the individual who is adjusted-age 49, they are treated differently as they fall into different categories. Conversely the individual who is adjusted-age 69 and has an approximately 10-fold (i.e. 1000%) greater risk of dying is treated the same as the individual who is adjusted-age 50. Smoothing of boundaries may partially address this problem, but arbitrary categorisation with linked actions makes risk tools imprecise and inflexible.
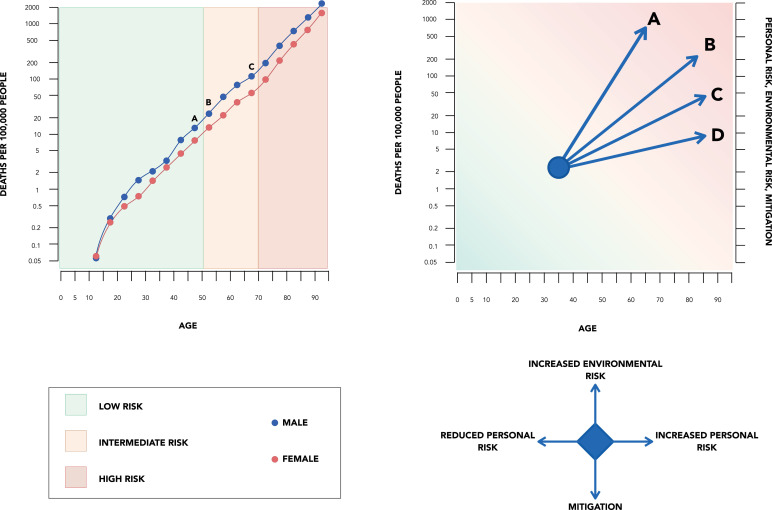
Fourth, and perhaps most important, by focusing only on ‘personal factors’ the scores fail to incorporate the interaction between these and the working environment. In very broad terms, the environment impacts on a person's risk of contracting the infection while personal factors impact on disease severity: both are critical in determining the risk of a poor outcome. Environmental risks include local viral transmission rates, how the individual commutes and workplace factors. For a healthcare worker, workplace factors include the disease prevalence within the hospital, workplace behaviours, their professional role, seniority, the extent of their patient contact in general or specifically with COVID-19 infected patients. Risk may be mitigated by workforce planning, patient streaming by risk of infection, masque wearing and infection control precautions including (but not restricted to) use of personal protective equipment (PPE). Given the importance of environmental exposure and mitigation strategies on the likelihood of acquiring infection and therefore on absolute risk of harm, it is troubling that most current risk tools do not explicitly incorporate them Fig. 1 [10].
Fig. 1.
Upper and lower left: the categories of increased risk are rigid and do not account for personal risk or mitigation. Upper and lower right: a continuum of risk is shown and the tool allows for interpretation based on personal, environmental risk and its mitigation.
Occupational risk assessment should include assessment of the level of work-based environmental risk and its mitigation (to assess risk of becoming infected) as well as personal attributes (to assess the potential impact of infection). Assessment should capture both relative and absolute risk. Environmental risk (e.g. variation in community or hospital prevalence) and mitigation measures (e.g. an inability to isolate infected patients or a lack of PPE) inevitably vary during the phases of the pandemic and this means that a ‘one-off’ risk assessment is unlikely to be sufficient. Assessments should be repeated when circumstances (whether environmental or personal) change. Finally, any risk assessment, particularly as there remains much uncertainty in many of the tools, should merely be the starting point for a discussion and agreed personalised plan. Current risk tools need adaptation to remain relevant, particularly as we enter a winter of uncertainty.
Declaration of Competing Interest
None
References
- 1.BMA. Briefing on supporting staff who are shielding to return to work. 2020. https://www.bma.org.uk/media/2854/bma-briefing-on-supporting-return-to-work-july2020.pdf (Accessed 17 august 2020)
- 2.Smith G.D., Spiegelhalter D. Shielding from covid-19 should be stratified by risk. BMJ. 2020;369:m2063. doi: 10.1136/bmj.m2063. [DOI] [PubMed] [Google Scholar]
- 3.Khunti K., de Bono A., Browne I., Greenhalgh T., Hanif W., Majeed A., Patel K., Razaq A., Smeeth L. Risk reduction framework for NHS staff at risk of COVID-19 infection. 2020. Available from https://www.fom.ac.uk/covid-19/update-risk-reduction-framework-for-nhs-staff-at-risk-of-covid-19-infection (Accessed 17 August 2020)
- 4.Welsh Government. COVID-19 workforce risk assessment tool. 2020. https://gov.wales/covid-19-workforce-risk-assessment-tool (Accessed 17 August 2020)
- 5.Strain W.D., Jankowski J., Davies A., English P.M.B., Friedman E., McKeown H., Sethi S., Rao M. Risk stratification tool for healthcare workers during the CoViD-19 pandemic; using published data on demographics, co-morbid disease and clinical domain in order to assign biological risk. MedRxiv. 2020 doi: 10.1101/2020.05.05.20091967. published online 15 June. [DOI] [Google Scholar]
- 6.Coggon D., Croft P., Cullinan P., Williams A. Assessment of workers vulnerability to COVID-19 using COVID-age. 2020. Medrxiv published on line 25 May doi: 10.1101/2020.05.21.20108969. [DOI] [PMC free article] [PubMed]
- 7.Williamson E.J., Walker A.J., Bhaskaran K. OpenSAFELY: factors associated with COVID-19 death in 17 million patients. Nature. 2020 doi: 10.1038/s41586-020-2521-4. Published online 8 July. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Docherty A.B., Harrison E.M., Green C.A. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spiegelhalter D. What have been the fatal risks of Covid, particularly to children and younger adults? Medium. June 2020 https://medium.com/wintoncentre/what-have-been-thefatal-risks-of-covid-particularly-to-children-and-younger-adults-a5cbf7060c49 (accessed 17 August 2020) [Google Scholar]
- 10.Cook T.M. Risk to health from COVID-19 for anaesthetists and intensivists - a narrative review. Anaesthesia. 2020;75:1494–1508. doi: 10.1111/anae.15220. [DOI] [PMC free article] [PubMed] [Google Scholar]