Abstract
Objective
The collection and use of a family health history are important for assessing the patient’s risk of disease, but history taking is often impeded by practical barriers in the office. Provision for patient-computer dialogue, linked with the electronic health record, may enable patients to contribute their history while bypassing these barriers. We sought to assess the patient experience using such a tool.
Materials and Methods
We linked the family history module of a computer-based medical history to the patient portal of a large academic health system. The interview consisted of 39 primary questions with a predetermined high test-retest reliability. Patients’ results were structured and summarized, and available within their electronic health record. Patients optionally completed a survey about their experience. We inductively analyzed free-text responses collected between 2014 and 2016.
Results
Among 97 781 patient portal users, 9562 patients accessed and 4223 patients completed the family medical history interview. Of these patients, 1451 completed our survey. Main themes that were identified included (1) patient empowerment, (2) anticipated value, (3) validity concerns, (4) privacy concerns, and (5) reflections on patient-computer dialogue. Patients also provided suggestions for the improvement of future family history tools.
Discussion
Patients providing their family health information is an example of collaborative electronic work with clinicians and was seen as valuable by those who participated. Concerns related to contextual information and uncertainty need to be addressed.
Conclusions
Patient-computer dialogue to collect family medical history empowered patients and added perceived value and efficiency to the patient experience of care.
Keywords: medical history taking, patient portals, consumer health informatics, ambulatory care information systems
INTRODUCTION
The family history is a time-honored and highly regarded component of the patient's medical history. Yet, problems with the traditional method of taking and recording the family history serve to limit both the clinical use and scientific study of the information obtained.1–5 The incompleteness of the history due to time limitations beyond the clinician’s control, the unavoidable inconsistencies over time in the clinician’s wording of questions and manner of presentation have motivated clinicians and researchers alike to turn to structured questionnaires,6 and our experience with the interactive computer dialogue with the patient7–9 to obtain the family history.
Our computer-based family history is 1 of 24 modules of a general-purpose computer-based medical history designed for patients to take in their homes over the Internet.9 In a study of the potential clinical usefulness of this history when taken by patients before their initial visit with their primary care doctors, patients and doctors responded favorably to the history and to the usefulness of the summary, which was available on their doctors’ computer screens at the time of their visit.9 The doctors were in favor of the immediate, routine implementation of the family and social histories while suggesting revisions in the summaries of the other modules. Accordingly, as a first step, we decided to make the family history module available to all Beth Israel Deaconess Medical Center patients with access to our portal PatientSite and study the extent to which patients would avail themselves of the program voluntarily and, together with their clinicians, find the program to be helpful.
OBJECTIVE
A 2014 systematic review of electronic family history tools previously identified that existing tools were useful for identifying risk, but none were integrated with electronic health records (EHRs), and authors noted that further research and implementation assessments were warranted.10 As we implemented the family history module into our patient portal for all patients, we sought to better understand the implementation and experience from the patient perspective.
MATERIALS AND METHODS
Computer-based family history interview
Developed on the basis of our experience over the years7,8 the computer-based family history consists of 39 “primary” questions asked of all patients about the incidence of familial diseases, as well as multiple qualifying questions to enable patients to specify relationships to family members with histories of familial diseases.
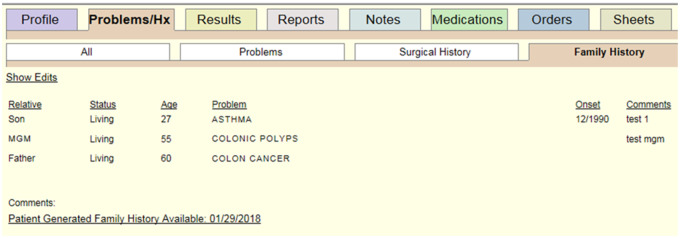
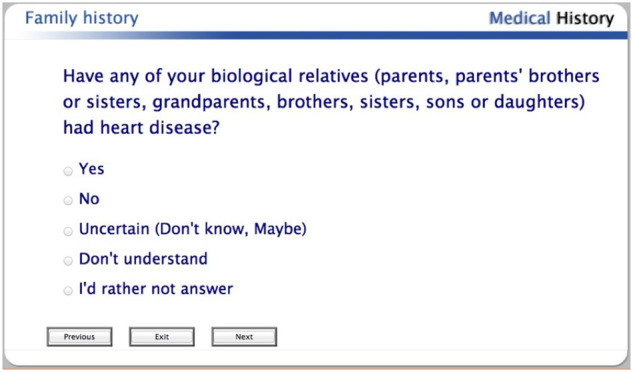
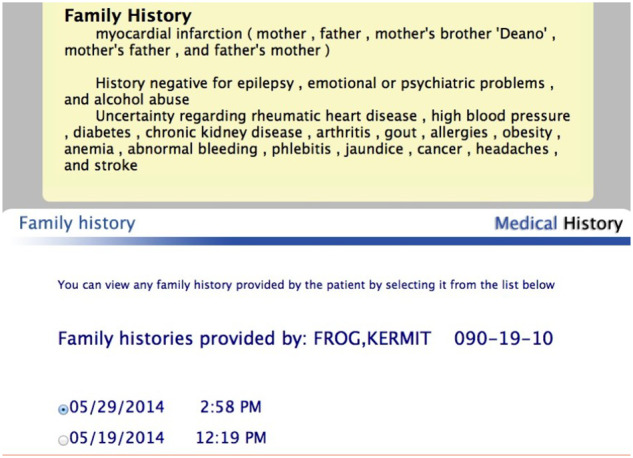
The interview begins with explanatory screens to introduce the patient to the interview and explain the domain of the family history questions. The questions are presented to patients on their computer screens over a secure patient portal PatientSite, which is integrated with the Online Medical Record of Beth Israel Deaconess Medical Center.11 Patients respond either by clicking on their answer from a list of choices or by typing on their keyboard for text and numerical entries (Figure 1). Once the interview is completed, the patient’s results are summarized in a narrative form and presented back to the patient, where they can make additional comments (Figure 2). Once satisfied, the patient submits the history to the system, which can be reviewed at an upcoming appointment within the EHR. Patients can also return to update their family history at any time. Clinicians are notified by a passive alert in the form of a hyperlink with the most recent date of completion, prompting them to review the patient’s entry within their usual workflow (Figure 3).
Figure 1.
Screenshot of family history interview, with standard response categories.
Figure 2.
Screenshot of summarized results, viewable by the patient and the clinician. Data remain in structured fields but summarized in narrative form for ease of review.
Figure 3.
Screenshot of clinician view of the electronic medical record with link to the summarized results.
Implementation of the family history interview
On January 20, 2014, we made the family history available to all patients of Beth Israel Deaconess Medical Center who were registered for use of PatientSite.12 Patients gained access to the history by clicking on “Records” on their PatientSite website, which advanced them to the link labeled “View, Update, or Provide Family History.” We made no formal announcements of the history’s availability and made no requests for patients to use it. Use was to be at once voluntary and patient-initiated.
Survey development and implementation
When patients had completed the family history interview or exited from it before completion, they were asked to assess their experience with a brief survey, which asked them how and why they accessed the interview, what were their perceptions of its value, strengths and limitations, and what suggestions they might have for improving the program. This feedback survey was anonymous and not linked to specific patients. The survey was approved as exempt by the Beth Israel Deaconess Medical Center Institutional Review Board on the basis of quality improvement.
Each of the patients’ free text comments offered during the survey was reviewed and coded inductively by 2 members of the project team (ASB, BHC). Individual concepts were reconciled through a consensus achieved in a series of meetings. After a final concept set was identified, comments were re-reviewed and coded.13 Repeated concepts across questions were aggregated into themes using constant comparison.14 Project team members used NVivo 11.4 (QSR International, Melbourne, Australia) to manage the qualitative data.
RESULTS
Between 2014 and 2016, 97 781 patients had accounts on PatientSite. Of these, 9562 (10%) patients accessed the family history interview on their own without prompting. We observed 4223 (42% of 9562 patients) of these patients complete the family history interview and submit it to their care providers through the EHR for review. Of these patients, 1451 (34%) completed the survey. (Table 1). Most participants (n = 1371, 94%) found the survey incidentally while reviewing their records within the portal. The majority of respondents (n = 1165, 80%) reported using the interview to ensure their doctors had the most accurate and complete information, while 233 (16%) participants did it out of curiosity. Of patients who either started or completed the interview, 1022 (70%) agreed or strongly agreed that the history was helpful to them as a patient (Supplementary Appendix 2). Among patients who accessed the interview, 753 patients provided free-text data, which were analyzed qualitatively.
Table 1.
Age and sex demographics of patients utilizing the family history interview, 2014–2016 (N = 4223)
| Age | ||
|---|---|---|
| <20 y | 10 (0.2) | 0.2% |
| 20-29 y | 440 (10.4) | 10.4% |
| 30-39 y | 519 (12.3) | 12.3% |
| 40-49 y | 610 (14.4) | 14.4% |
| 50-59 y | 1024 (24.2) | 24.2% |
| 60-69 y | 1033 (24.5) | 24.5% |
| >70 y | 587 (13.9) | 13.9% |
| Sex | ||
| Male | 1444 (34.2) | 34.2% |
| Female | 2779 (65.8) | 65.8% |
Values are n (%).
Qualitative analysis
We identified 5 main themes from patients’ responses to the survey: (1) patient empowerment (n = 75); (2) anticipated value for future risk prediction (n = 121); (3) concerns about validity (n = 34); (4) privacy concerns, including of family members (n = 40); and (5) reflections on patient-computer dialogue (n = 273). We also identified unintended uses of the family history tool (n = 22), including patients using it to provide information or corrections about their own medical history.
Patient empowerment
Many patients felt invited to help their clinicians manage their health history; they felt welcomed and able to share information they had not previously shared with their doctor. They felt that the information was important and that their participation in the process would result in better care. As one person mentioned, “It's nice to have the opportunity to have a well-combined family history to print out for my treatment team.” Patients liked having an opportunity to ensure that their record was up to date, and offered comments such as “liked that I was asked these questions” and “liked that you cared.” One patient mentioned that “I liked it. Makes me feel safer.”
Patients also found the process to be helpful to them, representing information that they could bring forward to their clinician as well as to use for their own purposes. One patient noted, “ I have never been asked for such a thorough family history. As I was filling it out I became aware of trends in the family with same illnesses or similar issues.” Another noted, “I like that it makes the patient evaluate their family’s medical history and how it could affect them.”
Patients noted that their home environment was more conducive to remembering or researching details of family illnesses than their doctor’s office, where they often felt under time pressures and likely to forget information. A patient noted that it was “More helpful to do this ‘at home’ where I have access to ages of family members and time to remember their illnesses.” Similarly, another patient noted that the interview “allowed time to think. [I] might have withheld some info in face-to-face.” And another patient offered that “By having the time to think about each question I was able to get a clearer image of the question while thinking about all family members. There was no pressure of time limits.” Further, we learned from patients’ comments that the interview prompted a discussion with family members that reminded the patient of familial problems or brought them to mind anew.
Patients had the opportunity to review their family history summary, as recorded in the EHR. In some cases, they suggested that it would have been helpful if they could have made corrections in their summary and to have provided information that was missing. “There was some information in my family history [presumably missing from the computer-based history] that I never discussed with my doctor. There were some updates to my family history that I wanted my doctor to know about.”
Anticipated value of the family history for future risk prediction
Patients voiced optimism that their family history would help predict their risk for familial problems and that it would be helpful as well to the broader research community. Patients perceived that completing the interview would help to better inform their clinicians and help to avoid the need to provide the same information multiple times. “It is nice to complete this before my appointment. I have had 4 PCPs [primary care physicians] at [this] practice and going over my family history for the fourth time did not appeal to me when I wanted to use my annual physical time to focus on my health and not my family history that I have already gone over multiple times.” And as another patient noted, this previsit history “will save time at the office visit.”
We heard from patients who were hopeful that participating would help doctors plan for the future. In the words of one patient, “now she'll be able to quickly rule out conditions that I'm not at risk for and focus on the ones that could be a problem.” Another patient offered, “I think it is a great tool to help doctors connect the dots in my health history and perhaps keep me from getting the same cancers my relatives had.”
On the other hand, some patients were more circumspect, pointing out that their family history is but one part of a larger conversation about health risk: “Rather a blunt instrument with general questions. Not sure if it will useful, but sets the stage for more specific questions, I suppose, when health issues arise.” And patients wanted to make sure they would have the opportunity to discuss the implications of their family history: “I would like my doctor to discuss with me the implications of the information I have provided.”
In addition to the perceived value to them and their clinicians, some patients pointed out that their family history could provide value to other patients through clinical research. Two comments illustrated this point: “Medical science will benefit from family histories,” and “I feel it is important for my doctor to know this [family] history and also for research.” And another patient commented that “This information might be useful in conjunction with the Precision Medicine Initiative and with major population genetic projects as HapMap 1000 Genome etc.”
Concerns about validity
We identified concerns from patients that they might not be able to reliably recall their family members’ histories. “Because I cannot recall or do not know the ailments of my relatives, I feel this family history has a lot of gaps, and therefore may not be as useful as it could be.” And in another patient’s words, “The information will invariably be incomplete due to people's memories and deaths of people with most complete memories of family history.” Another patient suggested, “There should have been an option for ‘probably’ because I don’t always have exact answers for my family history, but it's probably worth noting that my grandfather died in his 40s of some sort of heart disease.” Patients also had questions about how to add the appropriate context of the problem, such as occupational exposures or smoking history.
Some patients reported concerns about the format of the interview questions. “Like many multiple-choice surveys, this doesn't quite permit an accurate representation of the overall facts related to all of the question areas.” And one patient summarized, “Family history is far more complex than questions represented in this survey.” And another patient discontinued the survey, noting that “Your questions can only be answered in a specific way. I refuse to give false information.” And one patient was concerned that the history would bias the doctor: “I’m afraid that doctors are predetermined to diagnose when they see family history.”
Concerns about privacy
We identified concerns about patients’ privacy and the privacy of their family members, with the consequences of having information documented and available when seeking employment or health-related insurance. Although their family history was protected together with all Beth Israel Deaconess Medical Center’s electronic medical records, patients wanted “some [further] assurance about confidentially.” One patient noted, “Although I benefited from filling it out, I wonder about the privacy of my information and hope that it will be secure.” Another patient commented that “My only fear is any potential vulnerability if the information is visible to health insurers in the future as the national health insurance picture changes. I hope (and trust) that [hospital] will keep the information truly confidential.” And another patient noted, “The only reason I felt safe in answering this quiz is that thanks to President Obama, I don't have to worry about family history or preexisting conditions threatening my access to insurance.”
Some patients were reluctant to provide the names of relatives because they were concerned for their privacy. “I declined to give my siblings’ names. They have not given me permission to reveal their medical histories.” Similarly, another patient noted, “I wasn’t happy about having to give specific names and ages of people—I worry about the possibility of security/privacy leak.”
Patient-computer dialogue
Several patients noted in their comments that the family history module was a helpful way to work through their history. One patient noted, “It was easy to use. After the first few questions, I could anticipate the sequence and responses. Although a bit long, the repetition made it easy to continue and complete,” and another commented, “The interview covered my relatives’ medical problems. The use of mouse clicks worked well because I could concentrate on the subject at hand.” One patient suggested that “it might be better to organize it by relative rather than by disease.” One patient summarized that the interview was “necessarily tedious.” And another patient noted, “It is not granular enough. Trying to fit people in general categories is difficult.” And another volunteered, “I'd like more clarity about whether the term ‘heart disease’ includes strokes, heart attacks, bypass surgery, etc. I’m not clear on the differences and I bet others aren't as well.” One patient commented that they “would feel answers were more helpful in [an] interview with [a] knowledgeable person who could ask questions that might help explain some answers- get more details.”
Unintended use of the family history module
Some patients used the family history interview to provide information about themselves. One patient tried to update the medication list: “I wanted to have a space to add meds that were left out of my history” while another tried to update the medical history: “I needed to update MY history that I had cancer and it did not ask.”
Suggestions for improvement of the family history module
Patients offered suggestions for topics to explore further, such as dementia, autoimmune conditions, autonomic dysfunction, environmental exposure, osteoporosis, specific hereditary or genetic syndromes, and use of opiates; there were several requests for more detail about pulmonary and cardiovascular diseases. Further, there were requests to expand the list of relatives to include grandchildren, great aunts and uncles, and cousins. Patients who were adopted wished to be able to provide information known about their biological relatives, patients with half-siblings suggested that the interview make it easier to denote information about them, and patients would have liked better editing provisions—ways to make it easier for them to change their responses upon further reflection.
DISCUSSION
In the 2 years following initial implementation of the family history, 4223 patients provided information about their family history, and 1451 of these patients provided information about their experience. Our qualitative analysis identified major themes regarding their engagement and participation, including their concerns over the validity of their answers, protection of the privacy of their relatives, and reflections on the process of human-computer interaction. This work builds on prior research that has shown the electronic collection of medical histories to be well received by patients and clinicians,9,15–17 and more specifically with this study, that family history collection tool is generally found to be useful by patients for collecting and using the information to help with decisions.18 The experience of patients completing the family history provides lessons for future iterations and implementations of electronic family history collection.
Patient-professional collaborative work
Patients reported feeling that they were making a valuable contribution to their care by ensuring that clinicians had information about their family to predict future risk of conditions, and they felt empowered to participate in their care. The Systems Engineering Initiative for Patient Safety second iteration,19 and its related Patient Work Model,20 provide a good lens to identify this patient contribution as collaborative work. Where previously the curation of history information was once solely in the domain of the clinician, it may be more appropriate to consider it shared work. The patient portal provides infrastructure for patients to use collaborative applications, such as this interview for family history. This is a more focused example of patients providing their own history, which is currently being explored and piloted as part of the OurNotes project, an extension of the OpenNotes Research that invites patients to review notes and then contribute their history for their next visit, co-creating the note with clinicians.21
In our implementation, we hyperlinked to the patient’s interview responses within the workflow of the clinicians who were updating family history (Figure 3); clinicians would then review the responses with the patient and make changes in the EHR as appropriate. This step retained data provenance and addressed patient questions about the validity of their responses by ensuring that clinicians reviewed, discussed, and then accepted updates to the record. Rather than alerting clinicians about new data outside of visits, we opted for visible but passive alerts in the EHR that suggest review during encounters, given that past research has shown few clinicians act on alerts,22 and to not increase alert fatigue of primary care physicians. This followed the workflow that we have found to be successful for other patient-entered data, including advanced directives.23
Interview format
When creating a tool to elicit family history, a number of strategic choices must be made, including the format of the tool, and how the process is laid out. We opted for an interview format, based on previous experience.7–9 Computer interviews are indefatigable and provide for consistency where clinicians may be prone to take shortcuts or other omissions depending on other pressures. We found evidence that even patients self-censor during clinician-led interviews to focus on other matters at hand, with a feeling that the home-based interview provided better efficiency. The interview requires more of the patient’s time but helps patients with the process of recalling family members in a systematic way that they may not have otherwise. One major drawback of the current implementation is that there is not an editing function, which many patients sought. Patients found that the interview forced a review of medical conditions that they otherwise might have omitted and that it was helpful to guide patients through the process.
Patients perceived the tension between the depth of the interview and both breadth and length. We identified that patients who knew of specific conditions, including specific genetic syndromes, sought to record these in their records through the interview. This desire was balanced with patients finding that the interview was somewhat lengthy and that additional questions may be untenable. In this way, a refinement may be made to start with broader categories and then allow specificity and granularity while enabling structured data through controlled vocabularies. Ultimately, patients may wish to choose from different formats, matching to their needs and available time.
Addressing concerns and next steps
Patients raised important questions about the role of contextual information when responding to questions, the validity of their responses, and the privacy of relatives and related implications, such as insurability. An open question is how much contextual information will be helpful in family history, such as occupational exposures, diet, and health-seeking behaviors. Such contextual data may be helpful, such as reporting tobacco or alcohol use which may influence disease risk, or common environmental exposures, but it may be less consequential for inherited cancer patterns. Our participants were concerned about the privacy of relatives, particularly when labeling them by name, a program feature to keep track of individuals. Making naming optional and being transparent about data security policies in clear lay terms, may help assuage these concerns.
Future iterations of family history tools may incorporate the interview component into other tools, including pedigrees, such as seen with other tools.24,25 Asking some screening questions at the beginning, especially about more rare conditions or genetic syndromes, where known, may help balance the breadth and depth. The availability of genomic sequencing may alter the role of family history tools, as both whole exome and whole genomic sequencing become less expensive and more available for routine care, such as for pharmacogenomics or cancer risk prediction. Family history tools may help stratify who may benefit from genetic testing or aid in the discovery of as-yet-unidentified hereditary conditions. Providing clinical decision support based on the structured family history data is the next step, given that research has shown increases in risk-appropriate screenings26 or genetic counseling referrals.27,28
The following limitations for this study should be considered. This was a convenience sample of patient portal users who were motivated to volitionally contribute their family health history to the medical record, and a subset (34%) of patients completed a survey about their experience. However, this represents a rich source for qualitative analysis of free-text responses, enabling us to reach thematic saturation. We did not specifically assess the time to complete the interview, though we heard from patients that it was both quick and long and expect the length of time spent to vary depending on the number of relatives and conditions know to the patient. Last, this study did not ascertain the experiences within office visits, or track action taken on responses, and this should be assessed in future research.
While we did not specifically track clinician feedback for this analysis, feedback from clinicians has generally been positive regarding having the data at hand to prompt further discussion and clarification as needed. Patient entries were generally viewed as a conversation starter rather than a definitive history. Clinicians made requests that patient entries be able to autopopulate structured fields within the EHR after clinician verification.
CONCLUSION
This study, reporting on the experience of over 1400 patients who provided their family health history through a patient portal, identified that such patient-professional collaborative work empowered patients and added perceived value and efficiency to the patient experience of care. Patients sought to have such data available for risk prediction or for research purposes, but raised concerns about the privacy of their relatives and of uncertainty in their responses. Notably, over 9500 patients participated in the family history interview without any formal announcement. These patients were willing to provide data to further their care and help with their diagnoses, while others felt it was helpful to have a complete record or to help with future records-based research studies. We also found that patients did use the tool to report their own medical history or to submit changes to the record. This unintended use of this tool and speaks to additional functionality that patients desire, and a willingness to take an active role in managing their health.
AUTHOR CONTRIBUTIONS
ASB, BHC, HBK, CS, and WVS designed and developed the interview. ASB and BHC conducted the analysis. All authors contributed to drafting or editing the manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank Dr Steven Horng, MD, and the BIDMC Information Systems team for their help during this evaluation.
Conflict of interest statement
CS serves as a consultant for Cerner and Allscripts, a member of the physician advisory board of Elsevier, a council member of Health on the Net foundation, and a shareholder and director at Intelligent Medical Objects. BHC serves as an advisor for Buoy Health.
REFERENCES
- 1. Berg AO, Baird MA, Botkin JR, et al. National institutes of health state-of-the-science conference statement: family history and improving health. Ann Intern Med 2009; 15112: 872–7. [DOI] [PubMed] [Google Scholar]
- 2. Qureshi N, Wilson B, Santaguida P, et al. Collection and use of cancer family history in primary care. Evid Rep Technol Assess 2007; 159: 1–84. [PMC free article] [PubMed] [Google Scholar]
- 3. Rich EC, Burke W, Heaton CJ, et al. Reconsidering the family history in primary care. J Gen Intern Med 2004; 193: 273–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Flynn BS, Wood ME, Ashikaga T, Stockdale A, Dana GS, Naud S.. Primary care physicians' use of family history for cancer risk assessment. BMC Fam Pract 2010; 11: 45.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Endevelt R, Goren I, Sela T, Shalev V.. Family history intake: a challenge to personalized approaches in health promotion and disease prevention. Isr J Health Policy Res 2015; 4: 60.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Welch BM, Dere W, Schiffman JD.. Family health history: the case for better tools. JAMA 2015; 31317: 1711–2. [DOI] [PubMed] [Google Scholar]
- 7. Slack WV, Hicks GP, Reed CE, Van Cura LJ.. A computer-based medical-history system. N Engl J Med 1966; 2744: 194–8. [DOI] [PubMed] [Google Scholar]
- 8. Slack WV, Kowaloff HB, Davis RB, Delbanco T, Locke SE, Bleich HL.. Test-retest reliability in a computer-based medical history. J Am Med Inform Assoc 2011; 181: 73–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Slack WV, Kowaloff HB, Davis RB, et al. Evaluation of computer-based medical histories taken by patients at home. J Am Med Inform Assoc 2012; 194: 545–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. de Hoog CL, Portegijs PJ, Stoffers HE.. Family history tools for primary care are not ready yet to be implemented. A systematic review. Eur J Gen Pract 2014; 202: 125–33. [DOI] [PubMed] [Google Scholar]
- 11. Sands D, Halamka J.. PatientSite: patient-centered communication, services, and access to information. In: Nelson R, Ball M, eds. Consumer Informatics. New York: Springer; 2003: 20–32. [Google Scholar]
- 12. Crotty BH, Tamrat Y, Mostaghimi A, Safran C, Landon BE.. Patient-to-physician messaging: volume nearly tripled as more patients joined system, but per capita rate plateaued. Health Aff (Millwood) 2014; 3310: 1817–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bradley EH, Curry LA, Devers KJ.. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res 2007; 424: 1758–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Glaser BG. The constant comparative method of qualitative analysis. Soc Prob 1965; 124: 436–45. [Google Scholar]
- 15. Fuller M, Myers M, Webb T, Tabangin M, Prows C.. Primary care providers' responses to patient-generated family history. J Genet Counsel 2010; 191: 84–96. [DOI] [PubMed] [Google Scholar]
- 16. Doerr M, Edelman E, Gabitzsch E, Eng C, Teng K.. Formative evaluation of clinician experience with integrating family history-based clinical decision support into clinical practice. J Pers Med 2014; 42: 115–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Arora S, Goldberg AD, Menchine M.. Patient impression and satisfaction of a self-administered, automated medical history-taking device in the Emergency Department. West J Emerg Med 2014; 151: 35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wu RR, Orlando LA, Himmel TL, et al. Patient and primary care provider experience using a family health history collection, risk stratification, and clinical decision support tool: a type 2 hybrid controlled implementation-effectiveness trial. BMC Family Pract 2013; 14: 111.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics 2013; 5611: 1669–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Valdez RS, Holden RJ, Novak LL, Veinot TC.. Transforming consumer health informatics through a patient work framework: connecting patients to context. J Am Med Inform Assoc 2015; 221: 2–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mafi JN, Gerard M, Chimowitz H, Anselmo M, Delbanco T, Walker J.. Patients contributing to their doctors' notes: insights from expert interviews. Ann Intern Med 2018; 1684: 302–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Volk LA, Staroselsky M, Newmark LP, et al. Do physicians take action on high risk family history information provided by patients outside of a clinic visit? Stud Health Technol Inform 2007; 129 (Pt 1): 13–7. [PubMed] [Google Scholar]
- 23. Bajracharya AS, Crotty BH, Kowaloff HB, Safran C, Slack WV.. Improving health care proxy documentation using a web-based interview through a patient portal. J Am Med Inform Assoc 2016; 233: 580–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cohn WF, Ropka ME, Pelletier SL, et al. Health Heritage(c) a web-based tool for the collection and assessment of family health history: initial user experience and analytic validity. Public Health Genom 2010; 13 (7–8): 477–91. [DOI] [PubMed] [Google Scholar]
- 25. Hulse NC, Ranade-Kharkar P, Post H, Wood GM, Williams MS, Haug PJ.. Development and early usage patterns of a consumer-facing family health history tool. In: AMIA Annu Symp Proc 2011; 2011: 578–87. [PMC free article] [PubMed] [Google Scholar]
- 26. Rubinstein WS, Acheson LS, O’Neill SM, et al. Clinical utility of family history for cancer screening and referral in primary care: a report from the Family Healthware Impact Trial. Genet Med 2011; 1311: 956–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vogel TJ, Stoops K, Bennett RL, Miller M, Swisher EM.. A self-administered family history questionnaire improves identification of women who warrant referral to genetic counseling for hereditary cancer risk. Gynecol Oncol 2012; 1253: 693–8. [DOI] [PubMed] [Google Scholar]
- 28. Buchanan AH, Christianson CA, Himmel T, et al. Use of a patient-entered family health history tool with decision support in primary care: impact of identification of increased risk patients on genetic counseling attendance. J Genet Counsel 2015; 241: 179–88. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.