Abstract
Initiating and maintaining behavior change is key to the prevention and treatment of most preventable chronic medical and psychiatric illnesses. The cultivation of mindfulness, involving acceptance and nonjudgment of present-moment experience, often results in transformative health behavior change. Neural systems involved in motivation and learning have an important role to play. A theoretical model of mindfulness that integrates these mechanisms with the cognitive, emotional, and self-related processes commonly described, while applying an integrated model to health behavior change, is needed. This integrative review (1) defines mindfulness and describes the mindfulness-based intervention movement, (2) synthesizes the neuroscience of mindfulness and integrates motivation and learning mechanisms within a mindful self-regulation model for understanding the complex effects of mindfulness on behavior change, and (3) synthesizes current clinical research evaluating the effects of mindfulness-based interventions targeting health behaviors relevant to psychiatric care. The review provides insight into the limitations of current research and proposes potential mechanisms to be tested in future research and targeted in clinical practice to enhance the impact of mindfulness on behavior change.
Keywords: health behavior, mental disorders, mindfulness, motivation, neuroscience, self-management, self-regulation
INTRODUCTION
Health behavior refers to any behavior that affects physical or mental health or quality of life.1 Unhealthy behaviors such as tobacco smoking, alcohol and substance use, excessive eating, and nonadherence to medical regimens account for a substantial proportion of global disease morbidity and mortality, and for 40%–50% of the risk for early death in the United States.2–6 All-cause mortality is inversely associated with healthy lifestyle behaviors, and changes in unhealthy behaviors can lead to improved physical and mental health outcomes.7 Despite widespread awareness, it remains exceptionally difficult to initiate and maintain health behavior change.2
Health behavior theories are used to understand and predict health behaviors,8–16 and several behavior-change interventions have become popular.17,18 A growing body of evidence suggests that mindfulness-based interventions (MBIs) are effective in reducing harmful health behaviors,19 catalyzing chronic disease self-management and health behavior change,20 and improving physical and mental health outcomes.21–23 This article provides a narrative review with three main aims: (1) to define mindfulness and describe the evolving context and content for the MBI movement, (2) to describe an updated “mindful self-regulation” model that integrates motivation and learning mechanisms essential for behavior change and is grounded in emerging neuroscientific evidence, and (3) to synthesize current clinical research on MBIs targeting health behaviors relevant to psychiatry.
MINDFULNESS AND MBIs
Mindfulness is commonly defined as the awareness that arises when paying attention to the present moment nonjudgmentally.24 In 1881, the English scholar Rhys Davids translated the word mindfulness from the Pali word sati found in Buddhist texts, which meant “memory, recollection, calling-to-mind, being-aware-of, certain specified facts”25 but which has also been described as “lucid awareness”26 or “bare attention.”27 The terms mindfulness and meditation are increasingly conflated. General integrative practices (e.g., visualization, yoga) are often described as “mindfulness” in public discourse, diluting the word’s meaning. Importantly, not all meditation is mindfulness and not all mindfulness is meditation. Meditation is a practice that self-regulates the body and mind by engaging a specific attentional set.28 In mindfulness meditation (MM), the practice is to pay attention to present-moment experience with an orientation of curiosity, openness, acceptance, nonreactivity, and nonjudgment.29,30
Several core types of MM are taught in MBIs, along an attentional continuum that ranges from focused attention, which involves directing and sustaining attention on an object, disengaging from distractors (e.g., mind wandering), and returning attention to the object, to open monitoring, which has no explicit focus but cultivates metacognitive monitoring with a nonreactive awareness of the flow of cognition, emotions, and sensations.31 MBIs also use other evocative meditations to cultivate specific emotions (e.g., compassion, loving-kindness) that support MM practice.32,33 MM may produce relaxation in the body (i.e., the relaxation response, a voluntary, wakeful, hypometabolic state of parasympathetic dominance),34 but relaxation is not necessarily the objective. Rather, MM is an active and intentional practice of cultivating awareness of present-moment experience that may include strong emotions, difficult thoughts, or unpleasant sensations.35 MM cultivates both awareness and equanimity, an even-minded mental state or dispositional tendency toward all experiences/objects, regardless of their affective valence (pleasant/unpleasant/neutral).33 Several valuable models describe potential psychological and neurobiological mechanisms through which MM could exert its salutary effects.30,36–45
Persistent tensions have emerged throughout the MBI movement between (1) adaptation/openness to change versus fidelity/quality/safety, (2) drives for innovation/novelty versus ownership/tradition, and (3) non-attachment to labels versus valuing lineage with respect for teachers. To avoid confusion and to remain inclusive and neutral to these natural tensions, we describe a brief history of the movement—providing context for, and meaning to, various definitions.
Jon Kabat-Zinn began developing the first MBI, mindfulness-based stress reduction (MBSR), in 1977, integrating Buddhist insight (Pali: Vipassana) meditation,46,47 other contemplative practices (e.g., Zen, yoga),47,48 and modern psychological theories about stress and stress coping for application in health care.49–52 This work spawned a new secular, mainstream pedagogy for MM training, with a package of practices (i.e., body scan, mindful breathing, sitting meditation, informal mindfulness) bundled in an eight-week program that was designed to cultivate mindful attention in daily life, thereby helping patients to cope with stress, pain, and other chronic conditions. The first adaptation of MBSR, mindfulness-based cognitive therapy for depression,53–56 constituted, along with MBSR, the first generation of MBIs.57 More than a decade later, these approaches would come to be called mindfulness-based programs (MBPs), which have in common the “systematic and sustained training in formal and informal MM practices (for both teacher and participants).”57,58 Crane and colleagues57 distinguish MBPs from general MBIs, which were adapted from MBSR and mindfulness-based cognitive therapy; although these approaches also focus on cultivating MM practice, they have not always followed the same teacher-training process or other MBP standards. Together MBIs and MBPs focus on MM practice and differ from mindfulness-informed interventions,59 or “third-wave” interventions60 (e.g., dialectical behavior therapy [DBT], acceptance and commitment therapy [ACT]),61,62 which feature mindfulness as a component within a larger suite of techniques and mechanisms of change without an explicit focus on MM practice.57,59 Research publications on MBIs began increasing exponentially in the 2000s, in parallel with the proliferation of MBIs for specific conditions, and by 2020, MBIs have emerged for many chronic mental and physical illnesses.21,63,64 Academic mindfulness centers also emerged as dissemination nodes for MBPs,65 encouraging standards for formal teacher training and teacher competency assessments to ensure program integrity.66
This review will focus primarily on the areas with the strongest evidence relating to mindfulness and behavior change. We will describe and expand existing models of mindful self-regulation based on neurobiological mechanisms of mindfulness, motivation, and learning.38,67,68 Then we will review data from meta-analyses and well-designed randomized, controlled trials (RCTs) of MBPs affecting health behaviors. Given the more heterogeneous nature of related interventions (e.g., MBIs, DBT, ACT, mindful self-compassion, integrative mind-body therapy),61–63,69,70 we will limit references to these interventions except when MBP research is scarce. It should be noted, however, that DBT and ACT have made a substantial contribution to the understanding of behavior change, with strong meta-analytic evidence for a range of psychiatric disorders—which has contributed to a broader reconceptualization of the mechanisms of behavior change brought about by third-wave cognitive and behavioral therapies.60,71
MINDFUL SELF-REGULATION
Self-regulation is the ability to adaptively regulate one’s attention, emotions, cognition, and behavior to respond effectively to internal as well as environmental demands.72–74 Self-regulation impairment is linked to poorer outcomes in school/academics75,76 and also to poorer physical77,78 and mental health.79–84 Self-regulation theory proposes several critical processes for people to initiate and maintain behavior change and to prevent self-regulatory failure,73 including the capacity for standard setting, motivation to meet standards, self-monitoring, and willpower,73,74,85,86 We will build on the seminal neuroscience-based frameworks proposed by Hölzel and colleagues38 and Vago and colleagues,40 which outlined several relevant synergistic neurocognitive systems that underlie the effects of mindfulness on self-regulation, including attentional control, cognitive control, emotion regulation, and self-related processes. Importantly, we will describe how these self-regulation mechanisms interact with basic neural mechanisms for motivation and learning, which are well studied in the addiction and behavioral medicine literature. We will describe how each of these systems may play a role in facilitating the way that MM affects a person’s capacity for behavior change (Figure 1). The reviews aim to fill the gap in previous models of mindfulness and self-regulation by describing how, as MM practice develops, it may begin to enhance motivation for change by affecting processes of reward, associative and extinction learning, and habit formation, thereby shifting the balance from unhealthy to healthier behavioral repertoires.
Figure 1.
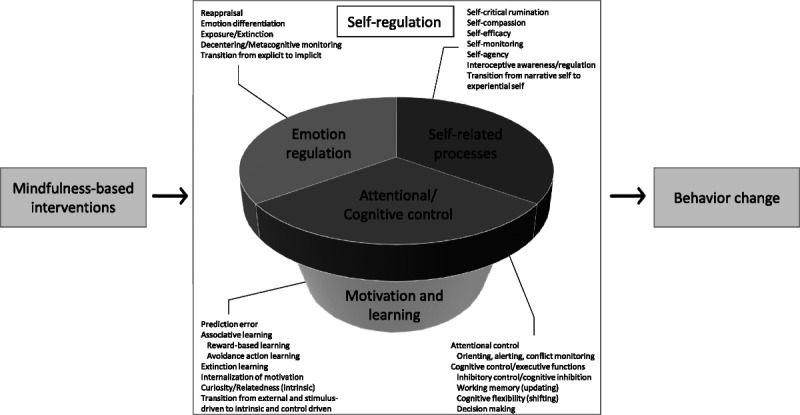
Mindfulness influences on self-regulation and behavior change.
Attention and Cognitive Control
Cognitive control is a fundamental capacity of human cognition that regulates access to specific goal-relevant information to facilitate the performance of specific behaviors.87–91 Executive functions are cognitive processes necessary for initiating and maintaining behavior change, and also for selecting and monitoring behavior toward attainment of goals; mental set shifting, information updating and monitoring, and inhibition are of particular importance.92 The subcomponents of cognitive control and executive function include attentional control/regulation,93,94 cognitive inhibition, inhibitory control, working memory, decision making, and cognitive flexibility.95 Attentional control can be further subdivided into (1) volitional orienting of attention to task-relevant information (e.g., breath, body sensations), (2) alerting to and successfully sustaining attention and vigilance for unexpected stimuli, and (3) conflict monitoring among task-relevant internal thoughts, feelings, and responses.96 These attentional processes contribute to recognizing both the consequences of ongoing unhealthy behavior and the affective precursors to avoidance or appetitive behaviors, contributing to adaptive behavior change.
MM may contribute to self-management of clinical symptoms, which are affected by unhealthy behaviors or maladaptive cognitive coping strategies, through explicit cognitive control processes. Two highly cited models38,40 suggest that mindfulness involves attention regulation (improvement in orienting, alerting/stability, bias, meta-awareness/monitoring)97–99 and inhibition/switching (decentering, inhibitory control, flexible engagement/disengagement).100,101 While individual studies support these models,102 meta-analyses of the effects of mindfulness on behavioral-cognitive assays demonstrate substantial heterogeneity,103,104 possibly related to diversity in mindfulness techniques, small sample sizes, nonspecific effects of common factors (e.g., group effects, empathic therapists), and multiple strategies for performing behavioral tasks. Moreover, populations with unique cognitive-dysfunction profiles (e.g., substance use, bipolar disorder, depression, age-related cognitive decline, or mild cognitive impairment)105–110 may experience improvement of disorder-specific dysfunction, whereas healthy participants may be sensitive to ceiling effects. In addition, the mindfulness effect may simply be making the brain more efficient, requiring less effort for a similar result.106
Functional neuroimaging research demonstrates that these interrelated cognitive control processes generally engage overlapping higher-order brain networks, including a central executive network, salience network, dorsal and ventral attention networks, and default mode network (DMN).111 These networks are anchored through a frontoparietal network that acts as a flexible hub interconnecting these networks, depending on the contextual and functional demands of cognition.112–116 This superordinate frontoparietal network, also referred to as the cognitive control network, includes the dorsolateral (dl) prefrontal cortex (PFC), posterior parietal cortex, anterior insula cortex, anterior cingulate cortex (ACC), and medial PFC.89–91,113,114 In the context of this flexible-hub framework, growing mechanistic evidence suggests that different types of MM engage associated frontoparietal network brain areas both structurally and functionally, differentially influencing psychological and cognitive outcomes.117,118 For example, studies show differences in brain activation and connectivity during focused-attention versus open-monitoring meditation,119 with focused attention engaging attentional control, whereas open-monitoring training engages labeling and emotional nonreactivity.120 A key aspect of cognitive control is the capacity to monitor for conflicts in information processing and to transmit these signals to other executive functions.87 This conflict-monitoring capacity has been associated with the ACC and seems to be enhanced with alterations in the ACC in the first few weeks of MM.121–123 Multiple fMRI studies suggest functional alterations between the ACC and insula in the context of monitoring for aversive stimuli during MM.123–126 Executive function is negatively affected by hippocampal dysfunction,127 whereas MBSR has been associated with increases in hippocampal volume,128 which can affect working memory performance.129 Inhibitory control is commonly associated with the dorsal ACC (dACC) or inferior frontal gyrus, which may be affected by culture or by developing mental habits of behavioral consistency.130 In meta-analyses, the dACC is often activated in studies of both focused-attention and open-monitoring meditation.117
Given that executive functions are critical for initiating and maintaining health behaviors, MBPs that enhance these processes may affect behavior-change capacity. By enhancing working memory and expanding attentional resources,131 MM may increase conscious awareness of behaviorally relevant external or internal stimuli (e.g., appetitive cues, stress- or craving-related body sensations), providing more time for higher-order cognitive functions, such as inhibitory control and other executive functions. These changes may help overcome prepotent motor responses, reduce the cognitive effort required for decision making about appetitive health behaviors, and diminish susceptibility to automatic behaviors in response to negative affect.106,132
Emotion Regulation
Emotions influence our perception, thinking, and behavior, and are made up of subjective, physiological, and behavioral components.133 Emotion regulation is the ability to modulate emotional experiences, enabling adaptive engagement with internal and external experience, which is essential for well-being and social adaptation.134,135 A variety of emotion-regulation strategies have been identified, including modifying the situation, altering attention toward it, modifying thoughts about it, and modulating the response to emotional experiences.136 Effective strategies decrease the subjective experience of negative emotion and its physiological correlates, and are associated with long-term efficacy in daily life.137 The best-studied strategy is cognitive reappraisal, the conscious reinterpretation of a situation in a way that alters its meaning and lessens the emotional impact. Reappraisal may be one of the mechanisms through which MM improves emotion regulation and ameliorates anxiety and depression.138,139 According to one model with empirical support, mindfulness facilitates reappraisal by interrupting automatic reactions, allowing for conscious reflection.38,140 With ongoing practice, some theorize that MM practitioners transition from using reappraisal strategies to cultivating states of nonappraisal and equanimity, though longitudinal research is needed.33,38,141 The available evidence also provides some support for exposure and extinction as key mechanisms for mindfulness-related emotion regulation. Rather than engaging in experiential avoidance142–144 or thought suppression,145 MBPs promote the ability to focus awareness on a difficult experience when it arises, creating a condition of exposure to negative emotional reactions.38,146 This change in focus is often aided by the capacity to shift experiential perspective— to step outside one’s immediate subjective experience to a more objective, non-identified awareness of one’s experience, which is called decentering,100 metacognitive monitoring, or meta-awareness.147,148 With practice, repeated acceptance and awareness of emotional and physiological responses lead to reduction and even extinction of emotional reactivity.149–151 Therefore, whereas meditation often causes state changes with enhanced autonomic parasympathetic activity, exposure through MM practice may create greater trait implicit control over parasympathetic tone, possibly initially through ACC control,152 and then possibly, with ongoing practice, through ventromedial (vm) PFC modulation of the amygdala.148,153 Finally, as people learn to be mindful of emotions, the capacity for emotion differentiation may be enhanced, which is associated with an enhanced ability for emotion regulation.154
Functional neuroimaging research implicates both distinct and overlapping networks involved in different emotion-regulation strategies. Explicit cognitive strategies like reappraisal are associated with activation of the frontoparietal executive network involved in selective attention, working memory, and response inhibition, and with deactivation of the amygdala.155 Neural mechanisms of mindfulness-based emotion regulation appear to differ, depending on the subjects’ experience level. Naive subjects given brief training in mindfulness induction for a laboratory study appear to employ top-down control by PFC regions in fashion similar to that of subjects instructed to use cognitive reappraisal.156 By contrast, for experienced meditators, downregulation of emotional reactivity when in a mindful state appears to involve deactivation of the DMN without deactivation of the amygdala.157 MBSR completers show decreased amygdala reactivity accompanied by increased amygdala–vmPFC functional coupling, consistent with the finding that symptom improvement in anxiety patients correlates with increased amygdala–vmPFC coupling after MBSR.153,158 Long-term meditators, in contrast to eight-week MBSR completers, employ implicit emotion-regulation systems involving the insula and vmPFC to modulate emotional reactivity.153 These findings suggest that, over time, long-term mindfulness practice promotes greater awareness and acceptance of emotional experience rather than the suppression of emotions by top-down inhibitory control.148,153,156,157
Healthy emotion regulation is important for behavior change to modulate emotions in alignment with one’s goals.159,160 Without it, feelings of stress, anxiety, and depression may thwart one’s intention to engage in health behaviors related, for example, to diet, exercise, or smoking—which promote positive health outcomes.161–164 Similarly, for patients with chronic illnesses facing a variety of physical and psychological challenges, emotion regulation is critical for maintaining optimal cognitive functioning and emotional balance.165 Mindfulness may also improve the chances of successful behavior change by increasing awareness of how emotions influence decisions and behaviors.137 A recent study of primary care patients with chronic illness reported that an eight-week MBI facilitated emotion regulation and catalyzed health behavior change.20 Our recent meta-analysis found that subjects receiving MBPs, compared to controls, significantly improved on emotion-regulation measures,166 suggesting that mindfulness may engage emotion-regulation processes that can improve behavioral outcomes.67,137,167,168
Self-Related Processes
Cognitive science describes a continuum of self-related processes that aligns closely with large-scale neural networks discovered through functional connectivity studies—networks that are affected by MM.
At one end of the self-related process continuum, the experiential self is the self-as-subject, the embodied self that is supported by phenomenological body awareness unextended in time—that is, the sense of “I am in this moment.”169–171 Interoception is the sensory experience of homeostatic afferents related to the body’s physiologic state, producing the feeling of present-moment self in the body.172 Broader definitions of interoceptive awareness include the tendency to listen to and trust body sensations as occurring within a dynamic relationship with appraisal and interoceptive regulation processes.173,174 Mindfulness training enhances interoceptive awareness and function.20 Most MM starts with the body and seems to develop greater interoceptive accuracy.175,176 Interoceptive dysfunction may lead to difficulties predicting body states and to allostatic dyscontrol.177 Interoceptive regulation may be enhanced through MM by increasing the capacity for perceptual-inference strategies (i.e., bringing the desired interoceptive state to what is sensed) instead of focusing only on active-inference strategies (i.e., trying to change the experience to the desired state).178 Numerous recent studies suggest an impact of MM on improving interoceptive measures.20,179 Meta-analysis and mediation studies are needed to examine the full impact of mindfulness on interoceptive awareness and its effect on behavior change.
Mindfulness neuroscience describes a phenomenological experiential-self network,171 involving activation of the anterior insula,40 which is altered after MM training.180 The insula provides an efficient means for processing large-scale interoceptive information in real time.181 Interoceptive activity and functional connectivity in the insula is disrupted in depression,182 which may be associated with a lack of emotional feeling in the body183 and may be associated with alexithymia.184,185 Functional connectivity studies of large-scale networks propose a key role of the insula in a salience network, which is posited to shift attention between internal (e.g., internal body sensations) and external stimuli (e.g., external perception) with dorsal attentional and ventral emotional components.111 Among MM practitioners, the experiential-self network may use moment-to-moment bodily experience in context to establish saliency for attention and regulation of cognitive resources.
At the other end of the self-related process continuum, a narrative self170 emerges during development, starting in late latency,186 then consolidating during adolescence187 and emerging adulthood,188 represented by autobiographical self-monitoring and social-cognitive and evaluative functions—in short, the self-as-object, “story of me as a person,” temporally extended into the past or future.170 These cognitive science concepts align with cognitive clinical models of self-related processes, which have an emphasis on self-discrepancy189 between the actual and idealized narrative self through positive (self-esteem and self-worth190) and negative self-evaluation191,192 (self-devaluation, self-criticism, and self-critical rumination).74,193,194 Emerging therapeutic approaches also include self-schema195–197 or multiple self-like parts198,199 to explain the clinical complexity of narrative self–related processes. The narrative self overlaps with many functions of the DMN, the most prominent large-scale brain network underlying self-related processes.200 The DMN engages medial cortical regions involved in self-monitoring, self-judgment, self-referential mental activity, episodic-memory retrieval, autobiographical memory, self-related social-cognitive processes, and value-based decision making.201,202 The DMN connects during adolescent identity formation,203 increasingly potentiating self-criticism and negative self-evaluative rumination. Among adults, high levels of DMN connectivity are associated with depression.204 Importantly, DMN activity and connectivity are reduced among experienced mindfulness meditators.205 In a recent meta-analysis, the posterior cingulate cortex, which is a core DMN node involved in self-related processing,206 is reliably deactivated during both focused-attention and open-monitoring MM.118
Rumination is a response to distress that involves repetitively and passively focusing on symptoms of distress and the possible causes and consequences of these symptoms.207,208 Rumination predicts depression,209 bulimia, substance use, self-injurious behaviors, impaired problem solving,208 and aggressive behaviors.210 One meta-analysis demonstrated that reductions in rumination partially mediated improved psychological functioning.151 Another recent meta-analysis found MBPs reduced negative self-related rumination, with a strong effect among six studies with inactive control groups, and potential for benefit among two studies with active controls.166 A meta-analysis of brain-imaging studies reports a strong association between DMN core regions, especially the dorsomedial (dm) PFC, and rumination.211 Reducing negative self-related rumination through MBPs may improve emotion regulation, reducing depressive symptoms and self-criticism. In this way, MM might prevent the detrimental repetition of negative global self-attributions that come when a person has a brief slip of unhealthy behavior after a period of sustained abstinence—which often leads persons to dive into a full-blown relapse, a process that Marlatt18 named the abstinence violation effect.
Other self-related processes on the continuum are the sense of agency212 related to the experience of one’s actions and decision making as an individual agentic self, and self-efficacy, which is one’s belief in one’s ability to succeed in specific situations or accomplish a task.213 A frontoparietal cognitive control network may provide flexible control in self-related processing214—involving coupling between other frontal networks, depending on internally or externally directed task demands.91,112,114,215 The overarching cognitive control network is therefore recruited to support control of belief and goal-directed strategies, flexibility creating a sense of self-agency that contributes to resiliency.216,217 The dlPFC, which is a core node of the central executive network, is often activated during MM; MM enhances connectivity between the dlPFC and other executive-function regions.218,219 As MM practice continues over time, the central executive network and other frontal networks may regulate the DMN in control of cognition.220
Two small studies have demonstrated increases in task-specific self-efficacy, though the increases were not statistically significant compared with controls.221,222 An uncontrolled, prospective cohort study reported increased chronic illness self-efficacy after eight weeks of MBSR but less self-efficacy at one year.223 Two larger RCTs of an eight-week MBP with self-efficacy as a secondary outcome reported within-group improvements in self-efficacy (d = 0.3 – 0.43), though this result was not significantly different from a low-dose mindfulness comparator.20,224 The ability to practice mindfulness may lead to a greater sense of one’s ability to make health behavior change; however, it is also possible that initial difficulty attaining expected levels of mindfulness practice may cause an opposite, deleterious effect on global self-efficacy and that the feedback from this failure may affect the capacity to succeed in self-regulation itself.225,226 Closer analysis of self-efficacy and self-agentic beliefs are needed to understand their role in mindful self-regulation models.
Finally, the warmth with which one relates to one’s self is a self-related process that affects self-regulation and behavior. Self-compassion involves responding with a warm, kind, and understanding orientation toward oneself, as one would to a close friend, when we suffer, fail, or feel inadequate.227 Self-compassion may be a mechanism through which MM supports behavior change228,229 and engagement in health-promoting behaviors230,231 in the context of diabetes,232 disordered eating,233 exercise-related goals in the face of setbacks,234 and sexual HIV risk behaviors.235 Self-compassion has been proposed to have a direct effect on self-regulation236 in part by neurobiologically mimicking a supportive compassionate other, activating the soothing-affiliation system.237 A meta-analysis demonstrated a strong effect of MBPs for increasing self-compassion in four studies with inactive controls (d = 0.73), though the result was insignificant versus active comparators.166 A rigorous RCT comparing an eight-week MBP versus a 60-minute mindfulness comparator reported significant effects of mindfulness dose on self-compassion (d = 0.41).20 MM lowered levels of self-criticism, which was associated with reduced activation in dmPFC nodes of the DMN,238 initially through dlPFC-mediated self-compassionate reappraisal strategies.239 Kindness toward self may clarify that one is worthy of being cared about, thereby enhancing motivation for self-care. MBPs focused primarily on attentional aspects of mindfulness in initial manuals/manuscripts, but a beneficial implicit “hidden curriculum” emerged for cultivating warmth and self-kindness.240 More recently, Kabat-Zinn241 clarified that “mindfulness” is the same as “heartfulness,” acknowledging the importance of love, kindness, and compassion. In this way, mindfulness practice may be described as “warmly being with present moment experience.” “Warm” mindfulness infused with self-compassion may be a more effective rapid emotion-regulation strategy than a response of “cool” mindful acceptance alone.242 Interventions and programs that focus explicitly on cultivating inner compassion, which includes and extends beyond self-kindness, may help facilitate behavior change, particularly for individuals who are prone to excess self-criticism, shame, or unworthiness.243
Motivation and Learning
In self-regulation theories, motivation relies on an anticipatory proactive system (i.e., setting standards) and a reactive negative feedback system (i.e., evaluative judgment) for reducing the discrepancy between goals/standards and behavior.72–74 Early self-regulation theories, based on control theory72 or homeostasis (feedback error correction),244 emphasize the role of evaluative judgment to generate motivation for change. Importantly, control of motivation can be stimulus driven in response to an external stimulus or control driven, which is motivated by, and directed toward, a specific outcome (e.g., intentions, goal setting).245 The motivation for unhealthy behavior is often driven by external and interoceptive stimuli246 through associative learning—for example, operant conditioning with positive or negative reinforcement. While MBPs may initially engage negative feedback systems utilizing discrepancy through evaluative judgment or predictive error to generate motivation for practice (e.g., “I hate being depressed, so I am motivated to practice mindfulness”), evaluative judgment is deemphasized during MBPs in favor of developing a focus on acceptance, intention setting, and attention toward experiential monitoring rather than self-evaluation.247–249
Evaluative judgment and feedback occur at least partially through the phasic activity of midbrain dopamine neurons in the ventral tegmental area that encode a prediction error used to guide associative learning throughout the frontal cortex and the basal ganglia.250 Activity in ventral tegmental area dopaminergic neurons that project to the nucleus accumbens (NAc) may signal that a person’s estimate of the value of current and future events is in error, and also indicate the error magnitude.251 This dopaminergic signaling process for reward-based learning begins with the acquisition of a reward after a behavior and leads to operant conditioning (e.g., incentive to repeat a pleasant, rewarding state). This gives way to wanting through incentive salience for cue-elicited behaviors,252 which causes automaticity and habit formation with the behavior eventually becoming epigenetically encoded in the dorsal striatum,253–255 making it harder to unlearn.256
Aversive learning happens through several mechanisms. Avoidance action learning, also referred to as negative reinforcement (e.g., action to avoid an unpleasant negative affect or aversive withdrawal state), depends on dopaminergic signaling in the NAc, though possibly through a different mechanism than approach learning.246,257 Pavlovian fear conditioning258 is due to signaling in the basolateral amygdala, which gets transmitted to the central amygdala, leading to the startle/freeze response to a stimulus.246,259–261 In cases where successful avoidance action takes place, however, a signal from the vmPFC blocks signal transmission to the central amygdala; instead of freezing, there is a predictive error signal in the NAc.246 Therefore, with aversive experiential learning, the freeze response and fear memory get conditioned first, but then successful avoidance action gets conditioned through engagement from the NAc and vmPFC, priming people to initiate avoidance action when a cue related to the previously aversive stimuli is experienced.246 Thus, the conditioned action urges that are at the heart of reward and experiential avoidance seem to be encoded in the prediction error in the NAc modulated by the vmPFC, which is the cortical region involved in subjective self-related valuation and self-regulatory goals.262–264
Fear memories either get continually reconsolidated after cue exposure or move toward extinction if the feared conditioned effects do not arise through a NMDA receptor–mediated process in the basolateral amygdala.265,266 Extinction learning is the process of inhibiting conditioned fear responses and developing new learning that competes with prior conditioning.266,267 It also involves prediction error–related vmPFC activity,268 which may explain why approach and avoidance conditioning often interact when trying to reverse conditioning.269,270 Therefore, both negative and positive reinforcement approaches may rely on this dopaminergic error-prediction system and modulation from the vmPFC self-related valuation system, which together are likely candidates for the negative feedback evaluative judgment system in self-regulation theory.
New theories based on recent neuroscientific developments also propose that prediction-error processes may be widely distributed throughout the brain’s architecture (including the insula) for interoceptive regulation and allostasis, with a key role in emotion and behavioral regulation.271,272 These neural models of allostasis propose that efficient self-regulation requires anticipating needs and preparing to satisfy them before they arise through a process of predictive error prevention.256
As described above, external rewards and punishments can lead to associative learning through Pavlovian and operant conditioning, and lead to habits that persist with ongoing positive and negative reinforcement. Exposure and associative learning can also be employed both for removing unhealthy habitual behavior and for developing and reinforcing healthy habitual behavior.41 Mindfulness practice, in particular, is itself a unique healthy behavior that may have the capacity to accelerate the process of extinguishing and replacing unhealthy behavioral repertoires.273,274 Traditionally, MM has been effectively taught in retreat settings lacking most behavior-activating cues,46 allowing interoceptive and cognitive exposure with reduced risk for actual harmful behaviors.275 In community MBPs, however, participants live in high-risk, cue-laden contexts,276 which can be more challenging. Despite this increased challenge, the social context of the group helps people spend time away from unhealthy behavior-activating cues and in a social environment that values collective learning of mindfulness.277 As community MBP practice continues, autonomic stability increases,152 allowing for a “window of tolerance,”278,279 within which exposure, response prevention, reconsolidation, associative learning, and extinction learning processes150,280 may begin to unwind the habit learning273 and fear conditioning281 that were maintaining unhealthy habits.
At around four weeks of practice, nonclinical MBI participants generally begin to automatically pay attention to the present moment.282 MM may be utilizing the same neural circuitry and associative-learning mechanisms to establish the habit of mindfulness, which can lead to a process of therapeutic staged neuroplasticity.283 Mindfulness practice associates readily available cues (e.g., the breath, present-moment sensations in the body, the physical experience of stress) with the internal mindful action of warmly being with present-moment experience with constant, accepting awareness of the experience’s changing nature—a process traditionally called Sampajanna in the Pali language, meaning “clear comprehension of impermanence.”26 This then sets in motion an automatic, internal behavioral repertoire that uses exposure and extinction processes to uproot deeply programmed, unhealthy conditioned behavioral patterns, while developing insight and ability to distinguish which behavioral patterns are healthier and do no harm.197,274,284 By combining this mindful acceptance with deepening interoceptive awareness, MM then begins to sidestep standard interoceptive feedback processes that drive automatic behaviors, thereby shifting interoceptive regulation toward use of the perceptual-inference instead of active-inference strategies. This change provides an efficient pathway for discrepancy resolution that reduces predictive errors and refines allostatic regulation.173,285 The stimulus-driven approach to learning and motivation dissipates as motivation for mindfulness becomes fully internalized and intrinsic motivation for healthy behaviors awakens.
Self-determination theory suggests motivation is derived from competence, relatedness, and autonomy.286 The motivation for initiating and maintaining behavior change exists on a continuum from amotivation to extrinsic (external pressure), introjected (internal pressure/guilt/shame), identified (feels useful/important), internalized (aligns with deeply held values), and most optimally intrinsic (interesting/enjoyable). Initially, mindfulness and paying attention may come from introjected or identified motivation (e.g., feeling I should meditate or that meditation is important for me). As practice continues and one witnesses the moment-to-moment consequences of unhealthy behaviors and identifies what is deeply valued, motivation for healthy behaviors become increasingly internalized, and people become self-motivated.74 As behavior aligns with internal standards, one develops more proactive systems (e.g., intention setting), reducing the burden from reliance on overreactive, judgment-driven negative feedback systems.287 Competence and autonomy are enhanced, and intrinsic motivations for wellness are progressively uncovered. Curiosity, which is a key aspect of the mindful state,101 may also modulate midbrain dopaminergic systems.288,289 Mindfully taking interest in health behaviors and its effects may generate greater levels of intrinsic motivation,287,290 enhancing overall motivational vigor and cognitive control through tonic dopamine release from the ventral tegmental area to the frontal central executive network regions.291–293 As mindfulness practice proceeds, mindful savoring of healthy, pleasant experiences may restructure reward processes and dopaminergic tone to reinstate value to natural rewards.294 Negative emotions have specific action urges, while positive emotions tend to broaden and build a person’s repertoire of thought-action patterns.295 Therefore, emotions are often experienced as intrinsic motivation, and emotion differentiation296 and reappraisal through mindfulness may help reduce emotionally driven unhealthy behaviors and build internalized and intrinsic motivation for healthy behaviors. Finally, kindness and compassion increase relatedness with others and potentially make people more sensitive to affiliative motivational systems, through which oxytocin may drive dopaminergic learning and reward in the ventral tegmental area and NAc.297,298
Mindful Self-Regulation: Synergy and Integration
Mindful self-regulation integrates attentional/cognitive control, emotion regulation, and self-related processes in synergy with mechanisms for motivation and learning as the practice of MM deepens. Mindful self-regulation starts with attentional control and curiosity about present-moment experience, leading to the development of interoceptive awareness and alternatives to self-critical rumination. Reappraisal of mental content, decentering, and acceptance downregulates autonomic reactivity, allowing for exposure to aversive internal stimuli and ultimately developing equanimity. Yet, for people with high levels of limbic dysregulation (e.g., unresolved trauma, marginalized or disempowered status) or baseline attentional/cognitive impairments, this standard, “cool” MM pathway offers some challenges. In this context, a “warm” MM pathway that starts with establishing safety through a “window of tolerance,” while cultivating self-compassion and inner warmth, may be more effective.299 By reducing self-criticism, autonomic reactivity, and internal conflict, the focus shifts from unhealthy patterns toward self-care.300 By slowly reducing the limbic load on cognitive control resources, attentional training becomes more accessible and effective. The most effective MM teachers often engage both pathways in tandem, helping practitioners more quickly come into smooth regulation and potentially reducing adverse experiences;301 yet, this key perspective has not been fully appreciated in previously proposed models of mindful self-regulation. As one begins to pay attention, consistent curiosity and kind awareness allow greater goal-driven control based on values, increased levels of internalized motivation, greater access to intrinsic motivation, and less reliance on stimulus-driven conditioning and evaluative negative feedback systems, eventually unwinding associative learning related to harmful behaviors. Behavior begins to emerge that puts positive cues in the environment, potentially activating healthy behaviors and supporting the behavior of mindful noticing itself, which leads to a positive feedback loop in favor of healthy behavior change. In this way, over time MM may cause an evolution toward greater efficiency in the human self-regulation system within a socio-environmental context, leading to greater feelings of interconnection and relatedness, and ultimately even supporting experiences of self-transcendence.40
MBIs’ EFFECTS ON PSYCHIATRICALLY RELEVANT BEHAVIOR CHANGE
Substance Use Disorders
Evidence supporting the impact of MBIs for alcohol (AUD) and substance use (SUD) disorders has been growing,302–310 supporting a few key mechanisms underlying the effect.41,273,311,312 A meta-analysis of 42 studies in 2017 reported a small effect of MBIs on substance misuse (standardized mean difference = −0.33) and a moderate effect on substance-related craving (standardized mean difference = −0.68).23 A three-arm RCT enrolled abstinent intensive-outpatient and inpatient residential treatment program completers with SUD (n = 286), comparing mindfulness-based relapse prevention versus relapse prevention versus treatment as usual on substance use outcomes over 12 months. This study demonstrated mindfulness-based relapse prevention had fewer drug use and heavy-drinking days at 12 months compared with relapse prevention alone.313 Mindfulness-based relapse prevention is the most commonly studied MBI for SUD, while other MBIs and mindfulness-informed interventions are also being studied for various substances and stages of treatment (e.g., mindfulness-oriented recovery enhancement).274,314–318 While the strength of evidence for mindfulness effects on certain SUDs during specific stages of treatment is strong (e.g., AUD),319 evidence for mindfulness and other SUDs is still emerging (e.g., methamphetamine, opioid use disorder).320–324
MBI studies for AUD/SUD support the general self-regulation mechanisms above while also focusing on disorder-specific deficits (e.g., reward processing, executive function, cue reactivity). For instance, mindfulness reduces impulsivity among people with opioid use disorder receiving methadone.197,325 MM may strengthen top-down cognitive control and repair executive-function deficits326 among people with SUD (e.g., working memory, inhibitory control)106,326 by increasing ACC/PFC activity and restoring frontostriatal connectivity.311 Mindfulness practice appears to partially decrease substance use through reductions in craving.327,328 Craving reduction may be from mindfulness strategies for decentering, acceptance, and attentional control that reduce intrusive cognitive elaboration (i.e., dwelling in positive recollections or attempts to suppress them) and that prevent cascades of emotional and physiologic reactivity.329 Mindfulness enhances emotion regulation, decoupling depression/negative affect from craving.327,328,330 MM encourages acceptance, reducing thought suppression,329 which may reduce craving since the suppression of thoughts/urges often amplifies craving.331 Mindfulness dampens limbic reactivity and enhances vagal tone,332 reducing the amplitude and elaboration of physiologic responses to stress and drug cues associated with craving.333,334 Mindfulness also seems to facilitate physiological recovery (e.g. high-frequency heart rate variability) with faster attentional disengagement after substance-related cues105,335 and stress.336 Evidence is also emerging that MM and mindful savoring practice may lead to restructuring reward processing,273,337 potentially remediating opioid use disorder–related hedonic dysregulation.338 By exposing practitioners to imaginal and interoceptive substance-related cues during practice and providing rewarding experiences (e.g., feelings of tranquility, curiosity about the novelty of present-moment experience), MM may allow extinction learning and a reversal of operant conditioning, unwinding years of habit formation.273 Despite the meta-analyses and efficacy and mechanistic studies supporting a role for mindfulness in AUD/SUD treatment, critical issues remain: establishing an evidence base to support real-world implementation in clinical settings; adapting interventions for various levels of care, patient readiness, and stages of treatment; determining the necessary dose of training at each level; and investigating issues of scalability for diverse populations.305–307
Eating Behavior/Diet
The efficacy of MBIs on food-related behavior and weight loss has been documented across multiple reviews and meta-analyses.339–346 Among RCTs, MBIs have large effects on the reduction of binge eating, emotional eating, and eating when not feeling physically hungry,339,340,344 and moderate effects on the improvement of eating attitudes.344 Small to moderate effects were noted for weight loss.339,344,347 MBIs that include both formal and informal practices (e.g., mindful eating)339 or that are combined with cognitive-behavioral therapy appear particularly beneficial.341,343
MBIs may promote enhanced self-regulation and interoceptive regulation through increased ability to notice automatic thoughts or affective cues, accurate appraisal of internal stimuli, or increased awareness of craving, hunger, fullness, and other factors influencing eating patterns.38,348–350 For example, mindful eating promotes present-moment enjoyment of food while reducing both overall caloric intake and craving-related eating.351,352 Across studies of individuals who are obese or overweight, MBIs reduced levels of depression and anxiety with medium effect.344 This improvement in psychological health may disrupt cycles of reactive or emotional eating, foster self-compassion, and improve self-concept.348,353,354 Overall, MBIs promote healthier behaviors around food and enhance psychological well-being, resulting in weight loss or weight maintenance. More research is needed to examine the efficacy of MBIs on sustained weight loss.
In line with broader research on eating-related behaviors and obesity, MBIs, including mindfulness-based eating awareness training (MB-EAT),354,355 appear useful for the treatment of binge eating disorder via similar mechanisms of action.340,356,357 In a meta-analysis, studies of persons with binge eating disorder demonstrated large effects for the reduction of eating pathology, emotional eating, negative affect, and body dissatisfaction, along with a small effect for weight loss.357 Additional research is needed to compare the efficacy of MBIs to traditional approaches (e.g., cognitive-behavioral therapy) for this pathology.358 Little is known about MBIs in bulimia nervosa and anorexia nervosa.356,358–362 Initial meta-analytical reports are favorable, showing reduced eating pathology, emotional eating, and body dissatisfaction with medium effect, as well as weight gain in some underweight participants.357 Across eating disorders, including binge eating disorder, compassion-focused techniques and mindfulness-informed interventions (e.g., DBT) may be useful.358,361 Given the unique clinical characteristics of restrictive eating disorders, mindful eating may be distressing for some individuals, especially with acute symptoms. While MBIs show promise, more rigorous research is needed to understand their utility for eating disorder treatment.
Tobacco Smoking
The past decade has seen an evolution of treatments and studies on MBIs for tobacco smoking cessation, with mixed evidence. Two meta-analyses, both of which included four smoking-specific RCTs, found that MBIs were superior to other evidence-based treatments. One reported a moderate effect (d = 0.42),22 and the other a relative risk of abstinence of 1.88 (1.04–3.40).363 A 2017 meta-analysis with ten RCTs found that mindfulness-informed interventions (including brief and mobile interventions) did not differ from comparators.364 In a now somewhat dated 2015 systematic review, only 13 of 198 articles on mindfulness and smoking were controlled empirical studies, with the majority being pilot or feasibility trials.365 The first RCT in 2011 compared mindfulness training to cognitive-behavioral therapy (American Lung Association’s Freedom from Smoking), in which they found a five-times greater cessation rate with mindfulness,366 which a secondary analysis demonstrated was moderated by baseline levels of nonjudgment, with less self-judgment of inner experience supporting greater cessation with mindfulness training.367 Another analysis showed mindfulness training decoupled key links in the smoking reinforcement-learning pathway (craving and smoking).368 As treatment has moved digital, app-based paradigms have been tested, reporting similar decoupling mechanisms.369,370 Recent work demonstrated that app-based mindfulness training serves to target DMN brain networks involved in “getting caught up” in craving206,371 in a dose-dependent manner, with the degree of brain activity reduction in the posterior cingulate cortex predicting smoking reductions, especially among women.372 More work is needed to replicate and extend findings.
Chronic Disease Self-Management
Self-management of chronic illness373,374 for common conditions375 is a priority for improving health care.376,377 As chronic physical illness is highly comorbid with mental illness,378 helping patients develop skills to self-manage chronic illness is essential in psychiatry. Chronic illness is often comorbid with anxiety, depression, trauma, and stress.379–381 Meta-analysis shows small effects for MBIs on enhancing quality of life and reducing anxiety, depression, and stress during chronic illness.21 Reducing mental health symptoms through MM may support greater chronic disease self-management. For instance, an eight-week MBI—integrated as health care treatment for primary care patients with comorbid mental and physical chronic illnesses—demonstrated increased rates of health-related action-plan initiation compared with participants randomized to a low-dose mindfulness comparator (OR = 2.91).20 A pilot eight-week MBSR group adapted for hypertension demonstrated significant changes in modifiable determinants of blood pressure—physical activity, diet, and alcohol consumption—for those who were nonadherent to American Heart Association guidelines at baseline, and changes were maintained at one year.382 Patients with chronic obstructive pulmonary disease who participated in an eight-week group program followed by ten monthly sessions reported increased health behavior changes and improvement in coping with illness.383 Qualitative findings from 41 individuals with long-term conditions participating in MBSR emphasized that “starting where I am” facilitated changes related to coping with and managing their illnesses.384 Mindfulness training helped lower blood glucose levels385 and hemoglobin A1c386 among those with type 2 diabetes but not among emerging adults with type 1 diabetes,387 suggesting further research is required.382 Longer-term continuation groups beyond eight weeks and the addition of kindness and compassion elements may be an important adaptation for helping those living with chronic illness.388
Violence, Suicide/Self-Injury, and Other High-Risk Behaviors
Impulsive violence and aggression are critical high-risk behaviors commonly monitored in psychiatry. A systematic review on the effect of mindfulness on aggression and violence included 22 adult studies (4 RCTs), concluding that MBIs and mindfulness-informed interventions (not including DBT) had a significant impact, with effect sizes from 0.21 to 0.87.389 Mindfulness skills may decrease impulsive thought and aggressive behavior through improved awareness of internal experience, reduction of experiential avoidance, and attentional shifting.390–392 An RCT with 58 patients with borderline personality disorder found decreased impulsive behavior after DBT versus treatment as usual.393 An RCT with 101 adults with recent partner aggression comparing ACT versus support group reported ACT was more efficacious in reducing physical and psychological aggression.394 An RCT with 56 healthy adults comparing MBSR versus waitlist reported MBSR decreased anger suppression and aggressive anger expression.395 In conclusion, empirical evidence suggests MBIs and mindfulness-informed interventions may reduce impulsive and aggressive behaviors. More methodologically rigorous research and meta-analyses are needed to confirm this hypothesis.
Dispositional mindfulness is negatively associated with suicidal ideation (SI)396,397 and nonsuicidal self-injury.398,399 DBT has the most evidence for decreasing suicidal and self-injurious behavior.400,401 In their systematic review, Chesin and colleagues402 found six studies of MBIs and suicidal behavior.403 Four studies reported inferential statistics on the effect of MBIs on SI, with three reporting significant reductions. The study that did not find a significant reduction had relatively low baseline rates of SI, suggesting a possible basement effect.404 Since that review, other studies have also shown salubrious effects of MBIs on SI,405,406 with MBIs appearing to uncouple the association between depressive symptoms and SI.407 MBIs remediate some cognitive factors and self-related processes shown to be risk factors for SI—for example, self-critical rumination, hopelessness, and cognitive reactivity to suicide408—but they do not mediate the improvement in SI.408 Thus, while MBIs may help reduce SI, more needs to be studied regarding potential mechanisms. The strongest evidence for nonsuicidal self-injury has been for DBT, which is effective in reducing nonsuicidal self-injury urges and behaviors in RCTs and meta-analyses, with particularly consistent and strong evidence among adolescents.401,409,410 Studies of the effects of MBIs on nonsuicidal self-injury have been proposed, but results have not yet been published to our knowledge. One RCT, however, and several open-label trials for ACT show promise.411,412
Dispositional mindfulness is positively correlated with inhibitory control and negatively correlated with impulsivity and with compulsive and high-risk sexual behavior.391,413–420 One RCT with 28 adults comparing 12 individual ACT sessions to a waitlist control condition to evaluate sexual impulsivity related to pornography showed a positive effect of the intervention on compulsive sexual behaviors.421 Cross-sectional data suggest that mindfulness training could reduce hypersexual behavior.420,422 Spiritual self-schema therapy, a psychotherapy that includes MM as its primary component, showed increased motivation to reduce HIV risk behavior (i.e., sex without a condom) in an RCT with 72 drug users,274 and completers of the intervention had decreased impulsiveness on the Barratt Impulsiveness Scale.197
DISCUSSION
Limitations of Current MBP Research
Many of the populations who may benefit from health-related behavior change—those with a disproportionate burden and comorbidity of chronic illness, substance use, and high-risk behaviors—are underrepresented in current research on mindfulness and compassion–based programs. These populations include trauma survivors,423,424 ethno-racial minorities425,426 (particularly those who identify as African American, Latinx, or indigenous), sexual or gender minorities,166,427,428 refugee/immigrant populations,429 and those at the intersection of these marginalized groups.430 While MBPs may be beneficial for addressing difficulties experienced by these populations (e.g., mindfulness-based relapse prevention may be more effective when delivered within groups composed primarily of ethnic/racial minorities),431,432 the current research base disproportionately represents well-educated, Caucasian, economically advantaged individuals.166,425 The paucity of ethno-racial diversity in both MBP researchers433 and MBP research participants166,425 mirrors the lack of diversity in psychological and biomedical research.434
While the level of MM practice engagement is often predictive of outcomes,435 trait mindfulness can be measured in the general non-meditating population, where it contributes to self-regulated behavior and positive affect.436 Moreover, even though eight weeks of MBP group training with a silent day of practice (23 hours in total) was more effective than a one-hour introduction to MM in catalyzing health behavior change, evidence supporting what dose intensity is required for behavior change is not yet definitive.20,437 Many doorways to discovering mindfulness likely exist, and those that are culturally inclusive of marginalized populations are more likely to be experienced as open doors, supporting greater access.438 While MBPs are well researched, with reliable dose-related effects within certain demographic groups,435,439 MBPs as currently designed are unlikely to be the exclusive optimal format for all. Innovations like rolling admissions in mindfulness-based relapse prevention represent an initial step toward accessibility.440 Overall, demands for the consistency and integrity of MBPs need to be balanced with cultural accessibility in clinical dissemination research.
The future accessibility, relevance, and ethical dissemination of existing MBPs will depend on adequate training of diverse MBP teachers/facilitators and on research agendas that prioritize overlapping areas of cultural humility, cultural accessibility, and trauma-sensitive delivery of MBPs, particularly for those affected by historical and intergenerational traumas.441 Given the potential relationship between interoception and social power,442 internalized oppression,443 and chronic illness,173,444,445 future research is needed on interventions that cultivate embodiment and interoception,285 including movement,446 drumming,447,448 music,449–452 and dance453—which may be more culturally accessible and specifically helpful for people with intergenerational trauma,454 and serve to foster social connectedness for marginalized populations with chronic illnesses.453
Future Directions: Adverse Effects, Trauma-Informed Training, Dose Effects
Adverse effects have been largely undocumented in the MBP research field. A systematic review of mindfulness-based stress-reduction or cognitive-therapy RCTs reported that only 15.6% of 231 studies included any statement about adverse events.455 Yet, potential adverse effects may include panic, physical pain, reexperiencing of traumatic memories, and dissociative symptoms.301 More needs to be understood about how program, participant, and teacher/leader factors contribute to adverse events.456 Britton457 and Grant and Schwartz458 propose a research agenda that takes into account that unwanted effects may emerge when aspects of mindfulness, such as decentering, focus on body sensations, and present-moment focus, are overemphasized. As the forms of adverse effects and reactions to symptoms vary based on individual and context, teachers and leaders should train in how to best monitor for, and respond to, adverse effects in MBP research.459,460
Program design and training must be sensitive to potential adverse effects experienced by trauma survivors. A majority of individuals will experience a traumatic life event, and a subset of these will develop posttraumatic stress disorder (PTSD).461 During MBPs, trauma survivors may be more likely to experience certain adverse effects such as traumatic flashbacks301 and dissociation.462 Trauma-informed training assumes that everyone might have a trauma history and focuses on offering choice, de-shaming adverse effects, supporting individual agency, and responding skillfully to trauma-related effects when they arise.424,460 MBPs have the potential to substantially reduce PTSD symptomology and to support neurobiological changes in networks implicated in PTSD psychopathology.111,463–469 Future research is needed on interventions that incorporate self-compassion, as it may mitigate and transform the shame-based nature of PTSD.470 When patients with PTSD are immersed within a safe, validating, healing community, such as well-designed trauma-informed MBP groups featuring self-compassion, they are likely to successfully initiate meaningful behavior changes.20
Finally, future clinical trials should include validated assays in clinical settings measuring the impact of dose effects on the self-regulation components described herein, and the extent to which each component mediates health behavior change.471 More dismantling and dose-response studies could help clarify the most active components and their individual contributions.120,472 Care should be taken with this investigative approach, however, since it carries risks of oversimplifying MBPs to just a collection of techniques in a toolbox.473 When mindfulness programs are offered solely from this instrumental dimension of a skill to be acquired,241 then the synergistic, holistic, and seemingly paradoxical approach to cultivating mindfulness, which many patients experience as engaging and deeply healing in MBPs, may be unwittingly sacrificed.
CONCLUSION
A growing evidence base supports the benefits of mindfulness for behavior change. A mindful self-regulation model based on an integration of neuroscientific findings describes the complex and synergistic effects of attention/cognitive control, emotion regulation, and self-related processes, as well as motivation and learning mechanisms that may provide a unique pathway toward sustainable behavior change. While evidence supports the impact of mindfulness on behavior change for key health behaviors related to psychiatric practice, more high-quality research is needed, especially with objective measures, larger samples, replication studies, active controls, and formal monitoring of adverse events.474 The field will also benefit from additional research on the impact of integrating compassion practices and from a focus on trauma-sensitive adaptations for diverse populations.
Declaration of interest
Dr. Brewer is the founder of MindSciences, the company that developed the mindfulness app for smoking cessation described in this article. He owns stock in, and serves as a noncompensated scientist for, the company and has previously served on the board of directors. This financial interest has been disclosed to and is being managed by Brown University, in accordance with its Conflict of Interest and Conflict of Commitment policies.
Acknowledgments
We would like to thank Willoughby Britton, Marcelo Demarzo, Gaelle Desbordes, Rebecca Ferrer, Elizabeth Hoge, Jean King, Jared Lindahl, Ethan Moitra, Neusa Rocha, and Jason Samlin for their contributions to this project.
Footnotes
Supported by National Institutes of Health (NIH) Helping to End Addiction Long-Term (HEAL) Initiative, award nos. R21AT010125, R33AT010125 administered by the National Center for Complementary and Integrative Health (Dr. Schuman-Olivier); Brazil Ministry of Education CAPES scholarship no. 88887.363065/2019-00 (Dr. Trombka); NIH Science of Behavior Change Common Fund Program, award nos. UH2AT009145 and UH3AT009145 administered by the National Center for Complementary and Integrative Health (Dr. Loucks).
Contributor Information
Marcelo Trombka, Email: mtrombka@challiance.org.
David A. Lovas, Email: david.lovas@iwk.nshealth.ca.
Judson A. Brewer, Email: judson_brewer@brown.edu.
David R. Vago, Email: david.vago@vanderbilt.edu.
Richa Gawande, Email: rgawande@challiance.org.
Julie P. Dunne, Email: judunne@challiance.org.
Sara W. Lazar, Email: SLAZAR@mgh.harvard.edu.
Eric B. Loucks, Email: eric_loucks@brown.edu.
Carl Fulwiler, Email: cfulwiler@challiance.org.
REFERENCES
- 1.Tombor I, Michie S. Methods of health behavior change. In: Braddick O, ed. Oxford research encyclopedias: psychology. New York: Oxford University Press, 2017. [Google Scholar]
- 2.Nielsen L Riddle M King JW, et al. The NIH Science of Behavior Change Program: transforming the science through a focus on mechanisms of change. Behav Res Ther 2018;101:3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA 2004;291:1238–45. [DOI] [PubMed] [Google Scholar]
- 4.Danaei G Ding EL Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med 2009;6:e1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crimmins EM, Preston SH, Cohen B. International differences in mortality at older ages: dimensions and sources. Washington, DC: National Academies, 2011. [PubMed] [Google Scholar]
- 6.Schroeder SA. We can do better—improving the health of the American people. N Engl J Med 2007;357:1221–8. [DOI] [PubMed] [Google Scholar]
- 7.Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med 2012;55:163–70. [DOI] [PubMed] [Google Scholar]
- 8.Noar SM, Zimmerman RS. Health behavior theory and cumulative knowledge regarding health behaviors: are we moving in the right direction? Health Educ Res 2005;20:275–90. [DOI] [PubMed] [Google Scholar]
- 9.Michie H, West S, Campbell R, Brown R, Gainforth J, eds. The behaviour change wheel: a guide to designing interventions. London: Silverback, 2014. [Google Scholar]
- 10.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol 1983;51:390–5. [DOI] [PubMed] [Google Scholar]
- 11.Rosenstock IM. Why people use health services. Milbank Mem Fund Q 1966;44:94–124. [PubMed] [Google Scholar]
- 12.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol 2001;52:1–26. [DOI] [PubMed] [Google Scholar]
- 13.Painter JE, Borba CPC, Hynes M, Mays D, Glanz K. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med 2008;35:358–62. [DOI] [PubMed] [Google Scholar]
- 14.Glanz K, Rimer B. Theory at a glance: a guide for health promotion practice. San Francisco, CA: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute, 2005. [Google Scholar]
- 15.Ajzen I. Theories of cognitive self-regulation: the theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179–211. [Google Scholar]
- 16.Perkins HW. Social norms and the prevention of alcohol misuse in collegiate contexts. J Stud Alcohol Suppl 2002;(14):164–72. [DOI] [PubMed] [Google Scholar]
- 17.Miller WR, Rollnick S. Motivational interviewing: helping people change. 3rd ed New York: Guilford, 2013. [Google Scholar]
- 18.Marlatt GA, Donovan DM. Relapse prevention: maintenance strategies in the treatment of addictive behaviors. 2nd ed New York: Guilford, 2005. [Google Scholar]
- 19.Salmoirago-blotcher E, Hunsinger M, Morgan L, Fischer D, Carmody J. Mindfulness-based stress reduction and change in health-related behaviors. 2013;18:243–7. [Google Scholar]
- 20.Gawande R To MN Pine E, et al. Mindfulness training enhances self-regulation and facilitates health behavior change for primary care patients: a randomized controlled trial. J Gen Intern Med 2019;34:293–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carlson LE. Mindfulness-based interventions for physical conditions: a narrative review evaluating levels of evidence. ISRN Psychiatry 2012;2012:651583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldberg SB Tucker RP Greene PA, et al. Mindfulness-based interventions for psychiatric disorders: a systematic review and meta-analysis. Clin Psychol Rev 2018;59:52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li W, Howard MO, Garland EL, Mcgovern P, Lazar M. Mindfulness treatment for substance misuse: a systematic review and meta-analysis. J Subst Abuse Treat 2017;75:62–96. [DOI] [PubMed] [Google Scholar]
- 24.Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain and illness. New York: Delacorte, 1990. [Google Scholar]
- 25.Sun J. Mindfulness in context: a historical discourse analysis. Contemp Buddhism 2014;15:394–415. [Google Scholar]
- 26.Bodhi B. What does mindfulness really mean? A canonical perspective. Contemp Buddhism 2011;12:19–39. [Google Scholar]
- 27.Nyanaponika T. The heart of Buddhist meditation (Satipaṭṭhāna): a handbook of mental training based on the Buddha’s way of mindfulness, with an anthology of relevant texts translated from the Pali and Sanskrit. London: Rider, 1962. [Google Scholar]
- 28.Cahn BR, Polich J. Meditation states and traits: EEG, ERP, and neuroimaging studies. Psychol Bull 2006;132:180–211. [DOI] [PubMed] [Google Scholar]
- 29.Bishop SR Lau M Shapiro S, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract 2004;11:230–41. [Google Scholar]
- 30.Baer RA. Mindfulness training as a clinical intervention: a conceptual and clinical review. Clin Psychol Sci Pract 2003;10:125–43. [Google Scholar]
- 31.Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends Cogn Sci 2008;12:163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hofmann SG, Grossman P, Hinton DE. Loving-kindness and compassion meditation: potential for psychological interventions. Clin Psychol Rev 2011;31:1126–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Desbordes G Gard T Hoge EA, et al. Moving beyond mindfulness: defining equanimity as an outcome measure in meditation and contemplative research. Mindfulness (N Y) 2014;(January):356–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benson H, Beary JF, Carol MP. The relaxation response. Psychiatry 1974;37:37–46. [DOI] [PubMed] [Google Scholar]
- 35.Edenfield TM, Saeed SA. An update on mindfulness meditation as a self-help treatment for anxiety and depression. Psychol Res Behav Manag 2012;5:131–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. J Clin Psychol 2006;62:373–86. [DOI] [PubMed] [Google Scholar]
- 37.Brown KW Ryan RM Creswell JD, et al. Mindfulness: theoretical foundations and evidence for its salutary effects. Psychol Inq 2007;18:211–37. [Google Scholar]
- 38.Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci 2011;6:537–59. [DOI] [PubMed] [Google Scholar]
- 39.Grabovac AD, Lau MA, Willett BR. Mechanisms of mindfulness: a Buddhist psychological model. Mindfulness (N Y) 2011;2:154–66. [Google Scholar]
- 40.Vago DR, Silbersweig DA. Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Front Hum Neurosci 2012;6:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brewer JA, Elwafi HM, Davis JH. Craving to quit: psychological models and neurobiological mechanisms of mindfulness training as treatment for addictions. Psychol Addict Behav 2013;27:366–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Garland EL, Froeliger B, Howard MO. Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface. Front Psychiatry 2014;4:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alsubaie M Abbott R Dunn B, et al. Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: a systematic review. Clin Psychol Rev 2017;55:74–91. [DOI] [PubMed] [Google Scholar]
- 44.Creswell JD. Mindfulness interventions. Annu Rev Psychol 2017;68:491–516. [DOI] [PubMed] [Google Scholar]
- 45.Creswell JD, Lindsay EK, Villalba DK, Chin B. Mindfulness training and physical health: mechanisms and outcomes. Psychosom Med 2019;81:224–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bowen S Witkiewitz K Dillworth TM, et al. Mindfulness meditation and substance use in an incarcerated population. Psychol Addict Behav 2006;20:343–7. [DOI] [PubMed] [Google Scholar]
- 47.Kabat-Zinn J. Some reflections on the origins of MBSR, skillful means, and the trouble with maps. Contemp Buddhism 2011;12:281–306. [Google Scholar]
- 48.Husgafvel V. On the Buddhist roots of contemporary non-religious mindfulness practice: moving beyond sectarian and essentialist approaches. Temenos 2016;52:87–126. [Google Scholar]
- 49.Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med 1985;8:163–90. [DOI] [PubMed] [Google Scholar]
- 50.Kabat-Zinn J Massion AO Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry 1992;149:936–43. [DOI] [PubMed] [Google Scholar]
- 51.Kabat-Zinn J Wheeler E Light T, et al. Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA). Psychosom Med 1998;60:625–32. [DOI] [PubMed] [Google Scholar]
- 52.Davidson RJ Kabat-Zinn J Schumacher J, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosom Med 2003;65:564–70. [DOI] [PubMed] [Google Scholar]
- 53.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford, 2002. [Google Scholar]
- 54.Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol 2000;68:615–23. [DOI] [PubMed] [Google Scholar]
- 55.Williams JM, Teasdale JD, Segal ZV, Soulsby J. Mindfulness-based cognitive therapy reduces overgeneral autobiographical memory in formerly depressed patients. J Abnorm Psychol 2000;109:150–5. [DOI] [PubMed] [Google Scholar]
- 56.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression. 2nd ed New York: Guilford, 2013. [Google Scholar]
- 57.Crane RS Brewer J Feldman C, et al. What defines mindfulness-based programs? The warp and the weft. Psychol Med 2016;47:990–9. [DOI] [PubMed] [Google Scholar]
- 58.Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract 2003;10:144–56. [Google Scholar]
- 59.Shapero BG, Greenberg J, Pedrelli P, de Jong M, Desbordes G. Mindfulness-based interventions in psychiatry. Focus (Madison) 2018;16:32–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hayes SC. Acceptance and commitment therapy and the new behavior therapies: mindfulness, acceptance, and relationship. In: Hayes SC, Follete VM, Lineahn MM, eds. Mindfulness and acceptance: expanding the cognitive-behavioral tradition. New York: Guilford, 2004. [Google Scholar]
- 61.Linehan MM, Schmidt H, 3rd, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. Am J Addict 1999;8:279–92. [DOI] [PubMed] [Google Scholar]
- 62.Hayes SC, Strosahl K, Wilson KG. Acceptance and commitment therapy: the process and practice of mindful change. 2nd ed New York: Guilford, 2012. [Google Scholar]
- 63.Cullen M. Mindfulness-based interventions: an emerging phenomenon. Mindfulness (N Y) 2011;2:186–93. [Google Scholar]
- 64.Keng S-L, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: a review of empirical studies. Clin Psychol Rev 2011;31:1041–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Barnes N, Hattan P, Black DS, Schuman-Olivier Z. An examination of mindfulness-based programs in US medical schools. Mindfulness (N Y) 2017;8:489–94. [Google Scholar]
- 66.Crane RS, Kuyken W. The mindfulness-based interventions: teaching assessment criteria (MBI:TAC): reflections on implementation and development. Curr Opin Psychol 2019;28:6–10. [DOI] [PubMed] [Google Scholar]
- 67.Loucks EB Schuman-Olivier Z Britton WB, et al. Mindfulness and cardiovascular disease risk: state of the evidence, plausible mechanisms, and theoretical framework. Curr Cardiol Rep 2015;17:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tang Y-Y, Holzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci 2015;16:213–25. [DOI] [PubMed] [Google Scholar]
- 69.Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol 2013;69:28–44. [DOI] [PubMed] [Google Scholar]
- 70.Tang Y-Y, Posner MI, Rothbart MK. Meditation improves self-regulation over the life span. Ann N Y Acad Sci 2014;1307:104–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dimidjian S, Arch JJ, Schneider RL, Desormeau P, Felder JN, Segal ZV. Considering meta-analysis, meaning, and metaphor: a systematic review and critical examination of “third wave” cognitive and behavioral therapies. Behav Ther 2016;47:886–905. [DOI] [PubMed] [Google Scholar]
- 72.Carver CS, Scheier MF. On the self-regulation of behavior. New York: Cambridge University Press, 1998. [Google Scholar]
- 73.Baumeister RF, Heatherton TF. Self-regulation failure: an overview. Psychol Inq 1996;7:1–15. [Google Scholar]
- 74.Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Decis Process 1991;50:248–87. [Google Scholar]
- 75.Blair C, Razza RP. Relating effortful control, executive function, and false belief understanding to emerging math and literacy ability in kindergarten. Child Dev 2007;78:647–63. [DOI] [PubMed] [Google Scholar]
- 76.Duckworth AL, Tsukayama E, May H. Establishing causality using longitudinal hierarchical linear modeling: an illustration predicting achievement from self-control. Soc Psychol Personal Sci 2010;1:311–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Evans GW, Fuller-Rowell TEDS. Childhood cumulative risk and obesity: the mediating role of self-regulatory ability. Pediatrics 2012;129:e68–73. [DOI] [PubMed] [Google Scholar]
- 78.Trindade A. The longitudinal effects of emotion regulation on physical and psychological health: a latent growth analysis exploring the role of cognitive fusion in inflammatory bowel disease. Br J Health Psychol 2017;23:171–85. [DOI] [PubMed] [Google Scholar]
- 79.Forbes EE, Dahl RE. Neural systems of positive affect: relevance to understanding child and adolescent depression? Dev Psychopathol 2005;17:827–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Amstadter A. Emotion regulation and anxiety disorders. J Anxiety Disord 2008;22:211–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shiels K, Hawk LH., Jr Self-regulation in ADHD: the role of error processing. Clin Psychol Rev 2010;30:951–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kuntsche E, Knibbe R, Engels R, Gmel G. Drinking motives as mediators of the link between alcohol expectancies and alcohol use among adolescents. J Stud Alcohol Drugs 2007;68:76–8. [DOI] [PubMed] [Google Scholar]
- 83.Deblois ME, Kubzansky LD. Childhood self-regulatory skills predict adolescent smoking behavior. Psychol Health Med 2016;21:138–51. [DOI] [PubMed] [Google Scholar]
- 84.Zlotnick C Wolfsdorf BA Johnson B, et al. Impaired self-regulation and suicidal behavior among adolescent and young adult psychiatric inpatients. Arch Suicide Res 2003;7:149–57. [Google Scholar]
- 85.Wagner DD, Heatherton TF. Self-regulation and its failure: the seven deadly threats to self-regulation. In: Mikulincer M, Shaver PR, Borgida E, Bargh JA, eds. APA handbook of personality and social psychology, vol. 1: Attitudes and social cognition. Washington DC: American Psychological Association, 2014. [Google Scholar]
- 86.Baumeister RF, Tice DM, Vohs KD. The strength model of self-regulation: conclusions from the second decade of willpower research. Perspect Psychol Sci 2018;13:141–5. [DOI] [PubMed] [Google Scholar]
- 87.Botvinick MM, Braver TS, Barch DM, Carter CS, Cohen JD. Conflict monitoring and cognitive control. Psychol Rev 2001;108:624–52. [DOI] [PubMed] [Google Scholar]
- 88.Miller EK. The prefrontal cortex and cognitive control. Nat Rev Neurosci 2000;1:59–65. [DOI] [PubMed] [Google Scholar]
- 89.Cole MW, Schneider W. The cognitive control network: integrated cortical regions with dissociable functions. Neuroimage 2007;37:343–60. [DOI] [PubMed] [Google Scholar]
- 90.Botvinick M, Braver T. Motivation and cognitive control: from behavior to neural mechanism. Annu Rev Psychol 2015;66:83–113. [DOI] [PubMed] [Google Scholar]
- 91.Breukelaar IA Antees C Grieve SM, et al. Cognitive control network anatomy correlates with neurocognitive behavior: a longitudinal study. Hum Brain Mapp 2017;38:631–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: a latent variable analysis. Cogn Psychol 2000;41:49–100. [DOI] [PubMed] [Google Scholar]
- 93.Eysenck MW, Derakshan N, Santos R, Calvo MG. Anxiety and cognitive performance: attentional control theory. Emotion 2007;7:336–53. [DOI] [PubMed] [Google Scholar]
- 94.Randall JG, Oswald FL, Beier ME. Mind-wandering, cognition, and performance: a theory-driven meta-analysis of attention regulation. Psychol Bull 2014;140:1411–31. [DOI] [PubMed] [Google Scholar]
- 95.Diamond A. Executive functions. Annu Rev Psychol 2013;64:135–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Posner MI, Petersen SE. The attention system of the human brain. Annu Rev Neurosci 1990;13:25–42. [DOI] [PubMed] [Google Scholar]
- 97.Jha AP, Krompinger J, Baime MJ. Mindfulness training modifies subsystems of attention. Cogn Affect Behav Neurosci 2007;7:109–19. [DOI] [PubMed] [Google Scholar]
- 98.Flavell JH. Metacognition and cognitive monitoring: a new area of cognitive-developmental inquiry. Am Psychol 1979;34:906–11. [Google Scholar]
- 99.Hussain D. Meta-cognition in mindfulness: a conceptual analysis. Psychol Thought 2015;8:132–41. [Google Scholar]
- 100.Safran J, Segal ZV. Interpersonal process in cognitive therapy. Oxford: Jason Aronson, 1996. [Google Scholar]
- 101.Lau MA Bishop SR Segal ZV, et al. The Toronto Mindfulness Scale: development and validation. J Clin Psychol 2006;62:1445–67. [DOI] [PubMed] [Google Scholar]
- 102.Heeren A, Van Broeck N, Philippot P. The effects of mindfulness on executive processes and autobiographical memory specificity. Behav Res Ther 2009;47:403–9. [DOI] [PubMed] [Google Scholar]
- 103.Chiesa A, Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: a systematic review and meta-analysis. Psychiatry Res 2011;187:441–53. [DOI] [PubMed] [Google Scholar]
- 104.Lao S-A, Kissane D, Meadows G. Cognitive effects of MBSR/MBCT: a systematic review of neuropsychological outcomes. Conscious Cogn 2016;45:109–23. [DOI] [PubMed] [Google Scholar]
- 105.Garland EL, Boettiger CA, Gaylord S, Chanon VW, Howard MO. Mindfulness is inversely associated with alcohol attentional bias among recovering alcohol-dependent adults. Cogn Ther Res 2012;36:441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Andreu CI, Cosmelli D, Slagter HA, Franken IHA. Effects of a brief mindfulness-meditation intervention on neural measures of response inhibition in cigarette smokers. PLoS One 2018;13:e0191661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Stange JP Eisner LR Holzel BK, et al. Mindfulness-based cognitive therapy for bipolar disorder: effects on cognitive functioning. J Psychiatr Pract 2011;17:410–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Shapero BG, Greenberg J, Mischoulon D, Pedrelli P, Meade K, Lazar SW. Mindfulness-based cognitive therapy improves cognitive functioning and flexibility among individuals with elevated depressive symptoms. Mindfulness (N Y) 2018;9:1457–69. [Google Scholar]
- 109.Gard T, Hölzel BK, Lazar SW. The potential effects of meditation on age-related cognitive decline: a systematic review. Ann N Y Acad Sci 2014;1307:89–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wong WP, Coles J, Chambers R, Wu DB-C, Hassed C. The effects of mindfulness on older adults with mild cognitive impairment. J Alzheimers Dis Rep 2017;1:181–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bressler SL, Menon V. Large-scale brain networks in cognition: emerging methods and principles. Trends Cogn Sci 2010;14:277–90. [DOI] [PubMed] [Google Scholar]
- 112.Cole MW, Reynolds JR, Power JD, Repovs G, Anticevic A, Braver TS. Multi-task connectivity reveals flexible hubs for adaptive task control. Nat Neurosci 2013;16:1348–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Schultz DH Ito T Solomyak LI, et al. Global connectivity of the fronto-parietal cognitive control network is related to depression symptoms in the general population. Netw Neurosci 2018;3:107–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zanto TP, Gazzaley A. Fronto-parietal network: flexible hub of cognitive control. Trends Cogn Sci 2013;17:602–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Amer T, Campbell KL, Hasher L. Cognitive control as a double-edged sword. Trends Cogn Sci 2016;20:905–15. [DOI] [PubMed] [Google Scholar]
- 116.Dixon ML De La Vega A Mills C, et al. Heterogeneity within the frontoparietal control network and its relationship to the default and dorsal attention networks. Proc Natl Acad Sci U S A 2018;115:E1598–E1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Fox KCR Nijeboer S Dixon ML, et al. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci Biobehav Rev 2014;43:48–73. [DOI] [PubMed] [Google Scholar]
- 118.Fox KCR Dixon ML Nijeboer S, et al. Functional neuroanatomy of meditation: a review and meta-analysis of 78 functional neuroimaging investigations. Neurosci Biobehav Rev 2016;65:208–28. [DOI] [PubMed] [Google Scholar]
- 119.Marzetti L, Di Lanzo C, Zappasodi F, Chella F, Raffone A, Pizzella V. Magnetoencephalographic alpha band connectivity reveals differential default mode network interactions during focused attention and open monitoring meditation. Front Hum Neurosci 2014;8:832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Britton WB Davis JH Loucks EB, et al. Dismantling mindfulness-based cognitive therapy: creation and validation of 8-week focused attention and open monitoring interventions within a 3-armed randomized controlled trial. Behav Res Ther 2018;101:92–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Botvinick MM, Cohen JD, Carter CS. Conflict monitoring and anterior cingulate cortex: an update. Trends Cogn Sci 2004;8:539–46. [DOI] [PubMed] [Google Scholar]
- 122.Pozuelos JP, Mead BR, Rueda MR, Malinowski P. Short-term mindful breath awareness training improves inhibitory control and response monitoring. Prog Brain Res 2019;244:137–63. [DOI] [PubMed] [Google Scholar]
- 123.Tang Y-Y, Lu Q, Feng H, Tang R, Posner MI. Short-term meditation increases blood flow in anterior cingulate cortex and insula. Front Psychol 2015;6:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hölzel BK Ott U Hempel H, et al. Differential engagement of anterior cingulate and adjacent medial frontal cortex in adept meditators and non-meditators. Neurosci Lett 2007;421:16–21. [DOI] [PubMed] [Google Scholar]
- 125.Nakata H, Sakamoto K, Kakigi R. Meditation reduces pain-related neural activity in the anterior cingulate cortex, insula, secondary somatosensory cortex, and thalamus. Front Psychol 2014;5:1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Haase L Thom NJ Shukla A, et al. Mindfulness-based training attenuates insula response to an aversive interoceptive challenge. Soc Cogn Affect Neurosci 2014;11:182–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Frodl T Schaub A Banac S, et al. Reduced hippocampal volume correlates with executive dysfunctioning in major depression. J Psychiatry Neurosci 2006;31:316–23. [PMC free article] [PubMed] [Google Scholar]
- 128.Hölzel BK Carmody J Vangel M, et al. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res 2011;191:36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Greenberg J, Romero VL, Elkin-Frankston S, Bezdek MA, Schumacher EH, Lazar SW. Reduced interference in working memory following mindfulness training is associated with increases in hippocampal volume. Brain Imaging Behav 2019;13:366–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Pornpattananangkul N Hariri AR Harada T, et al. Cultural influences on neural basis of inhibitory control. Neuroimage 2016;139:114–26. [DOI] [PubMed] [Google Scholar]
- 131.Slagter HA Lutz A Greischar LL, et al. Mental training affects distribution of limited brain resources. PLoS Biol 2007;5:e138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Garland EL, Bryan MA, Priddy SE, Riquino MR, Froeliger B, Howard MO. Effects of mindfulness-oriented recovery enhancement versus social support on negative affective interference during inhibitory control among opioid-treated chronic pain patients: a pilot mechanistic study. Ann Behav Med 2019;53:865–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gross JJ, Thompson R. Emotion regulation: conceptual foundations. In: Gross JJ, ed. Handbook of emotion regulation. New York: Guilford, 2007. [Google Scholar]
- 134.Gross J, John O. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol 2003;85:348–62. [DOI] [PubMed] [Google Scholar]
- 135.Ng W, Diener E. Personality differences in emotions: does emotion regulation play a role? J Individ Differ 2009;30:100–6. [Google Scholar]
- 136.Gross JJ. The emerging field of emotion regulation: an integrative review. Rev Gen Psychol 1998;2:271–99. [Google Scholar]
- 137.Werner K, Gross JJ. Emotion regulation and psychopathology: a conceptual framework. In: Kring AM, Sloan DM, eds. Emotion regulation and psychopathology: a transdiagnostic approach to etiology and treatment. New York: Guilford, 2010;13–37. [Google Scholar]
- 138.Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol 2010;78:169–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Goyal M Singh S Sibinga EMS, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med 2014;174:357–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Garland EL, Hanley AW, Goldin PR, Gross JJ. Testing the mindfulness-to-meaning theory: evidence for mindful positive emotion regulation from a reanalysis of longitudinal data. PLoS One 2017;12:e0187727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Garland EL, Hanley A, Farb NA, Froeliger BE. State mindfulness during meditation predicts enhanced cognitive reappraisal. Mindfulness (N Y) 2015;6:234–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Hayes SC Strosahl K Wilson KG, et al. Measuring experiential avoidance: a preliminary test of a working model. Psychol Rec 2004;54:553–78. [Google Scholar]
- 143.Abramowitz JS, Blakey SM, eds. Clinical handbook of fear and anxiety: maintenance processes and treatment mechanisms. Washington, DC: American Psychological Association, 2020. [Google Scholar]
- 144.Chawla N, Ostafin B. Experiential avoidance as a functional dimensional approach to psychopathology: an empirical review. J Clin Psychol 2007;63:871–90. [DOI] [PubMed] [Google Scholar]
- 145.Bowen S, Witkiewitz K, Dillworth TM, Marlatt GA. The role of thought suppression in the relationship between mindfulness meditation and alcohol use. Addict Behav 2007;32:2324–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Treanor M. The potential impact of mindfulness on exposure and extinction learning in anxiety disorders. Clin Psychol Rev 2011;31:617–25. [DOI] [PubMed] [Google Scholar]
- 147.Bernstein A, Hadash Y, Lichtash Y, Tanay G, Shepherd K, Fresco DM. Decentering and related constructs: a critical review and metacognitive processes model. Perspect Psychol Sci 2015;10:599–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Guendelman S, Medeiros S, Rampes H. Mindfulness and emotion regulation: insights from neurobiological, psychological, and clinical studies. Front Psychol 2017;8:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Björkstrand J Schiller D Li J, et al. The effect of mindfulness training on extinction retention. Sci Rep 2019;9:19896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sevinc G Hölzel BK Greenberg J, et al. Strengthened hippocampal circuits underlie enhanced retrieval of extinguished fear memories following mindfulness training. Biol Psychiatry 2019;86:693–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev 2015;37:1–12. [DOI] [PubMed] [Google Scholar]
- 152.Tang Y-Y Ma Y Fan Y, et al. Central and autonomic nervous system interaction is altered by short-term meditation. Proc Natl Acad Sci U S A 2009;106:8865–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kral TRA, Schuyler BS, Mumford JA, Rosenkranz MA, Lutz A, Davidson RJ. Impact of short- and long-term mindfulness meditation training on amygdala reactivity to emotional stimuli. Neuroimage 2018;181:301–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Barrett LF, Gross J, Christensen TC, Benvenuto M. Knowing what you’re feeling and knowing what to do about it: mapping the relation between emotion differentiation and emotion regulation. Cogn Emot 2001;15:713–24. [Google Scholar]
- 155.Etkin A, Büchel C, Gross JJ. The neural bases of emotion regulation. Nat Rev Neurosci 2015;16:693–700. [DOI] [PubMed] [Google Scholar]
- 156.Lutz J Herwig U Opialla S, et al. Mindfulness and emotion regulation—an fMRI study. Soc Cogn Affect Neurosci 2013;9:776–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Taylor VA Grant J Daneault V, et al. Impact of mindfulness on the neural responses to emotional pictures in experienced and beginner meditators. Neuroimage 2011;57:1524–33. [DOI] [PubMed] [Google Scholar]
- 158.Hölzel BK Hoge EA Greve DN, et al. Neural mechanisms of symptom improvements in generalized anxiety disorder following mindfulness training. Neuroimage Clin 2013;2:448–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Gross JJ. Emotion regulation in adulthood: timing is everything. Curr Dir Psychol Sci 2001;10:214–9. [Google Scholar]
- 160.Gross JJ, Muñoz RF. Emotion regulation and mental health. Clin Psychol Sci Pract 1995;2:151–64. [Google Scholar]
- 161.Smyth JM, Arigo D. Recent evidence supports emotion-regulation interventions for improving health in at-risk and clinical populations. Curr Opin Psychiatry 2009;22:205–10. [DOI] [PubMed] [Google Scholar]
- 162.Groesz LM McCoy S Carl J, et al. What is eating you? Stress and the drive to eat. Appetite 2012;58:717–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Chew B-H, Shariff-Ghazali S, Fernandez A. Psychological aspects of diabetes care: effecting behavioral change in patients. World J Diabetes 2014;5:796–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Appleton AA, Loucks EB, Buka SL, Kubzansky LD. Divergent associations of antecedent- and response-focused emotion regulation strategies with midlife cardiovascular disease risk. Ann Behav Med 2014;48:246–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.de Ridder D, Geenen R, Kuijer R, van Middendorp H. Psychological adjustment to chronic disease. Lancet 2008;372:246–55. [DOI] [PubMed] [Google Scholar]
- 166.Britton W Loucks E King J, et al. Meta-analytic review of self-regulation processes in mindfulness-based cognitive therapy and mindfulness-based stress reduction. PROSPERO 2016: CRD42016051765. https://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42016051765
- 167.Brewer JA, Elwafi HM, Davis JH. Craving to quit: psychological models and neurobiological mechanisms of mindfulness training as treatment for addictions. Psychol Addict Behav 2013;27:366–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Fulwiler C, Brewer JA, Sinnott S, Loucks EB. Mindfulness-based interventions for weight loss and CVD risk management. Curr Cardiovasc Risk Rep 2015;9:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Zahavi D. The experiential self: objections and clarifications. In: Siderits M, Thompson E, Zahavi D, eds. Self, no self? Perspectives from analytical, phenomenological, and Indian traditions. Oxford: Oxford University Press, 2011. [Google Scholar]
- 170.Gallagher S. Philosophical conceptions of the self: implications for cognitive science. Trends Cogn Sci 2000;4:14–21. [DOI] [PubMed] [Google Scholar]
- 171.Farb NA Segal ZV Mayberg H, et al. Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Soc Cogn Affect Neurosci 2007;2:313–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Craig AD. Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiol 2003;13:500–5. [DOI] [PubMed] [Google Scholar]
- 173.Khoury NM, Lutz J, Schuman-Olivier Z. Interoception in psychiatric disorders: a review of randomized, controlled trials with interoception-based interventions. Harv Rev Psychiatry 2018;26:250–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Mehling WE, Acree M, Stewart A, Silas J, Jones A. The multidimensional assessment of interoceptive awareness, version 2 (MAIA-2). PLoS One 2018;13:e0208034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kerr C, Sacchet M, Lazar S, Moore C, Jones S. Mindfulness starts with the body: somatosensory attention and top-down modulation of cortical alpha rhythms in mindfulness meditation. Front Hum Neurosci 2013;7:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Bornemann B, Herbert BM, Mehling WE, Singer T. Differential changes in self-reported aspects of interoceptive awareness through 3 months of contemplative training. Front Psychol 2014;5:1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Harshaw C. Interoceptive dysfunction: toward an integrated framework for understanding somatic and affective disturbance in depression. Psychol Bull 2015;141:311–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Farb N Daubenmier J Price CJ, et al. Interoception, contemplative practice, and health. Front Psychol 2015;6:763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Loucks EB Nardi WR Gutman R, et al. Mindfulness-based blood pressure reduction (MB-BP): stage 1 single-arm clinical trial. PLoS One 2019;14:e0223095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Farb NA, Segal ZV, Anderson AK. Mindfulness meditation training alters cortical representations of interoceptive attention. Soc Cogn Affect Neurosci 2013;8:15–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Damasio A, Damasio H, Tranel D. Persistence of feelings and sentience after bilateral damage of the insula. Cereb Cortex 2012;23:833–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Avery JA, Drevets WC, Moseman SE, Bodurka J, Barcalow JC, Simmons WK. Major depressive disorder is associated with abnormal interoceptive activity and functional connectivity in the insula. Biol Psychiatry 2014;76:258–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Nummenmaa L, Glerean E, Hari R, Hietanen JK. Bodily maps of emotions. Proc Natl Acad Sci U S A 2014;111:646–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Murphy J, Brewer R, Hobson H, Catmur C, Bird G. Is alexithymia characterised by impaired interoception? Further evidence, the importance of control variables, and the problems with the heartbeat counting task. Biol Psychol 2018;136:189–97. [DOI] [PubMed] [Google Scholar]
- 185.Herbert BM, Herbert C, Pollatos O. On the relationship between interoceptive awareness and alexithymia: is interoceptive awareness related to emotional awareness? J Pers 2011;79:1149–75. [DOI] [PubMed] [Google Scholar]
- 186.Reese E, Yan C, Jack F, Hayne H. Emerging identities: narrative and self from early childhood to early adolescence. In: McLean KC, Pasupathi M, eds. Narrative development in adolescence: creating the storied self. New York: Springer, 2010. [Google Scholar]
- 187.Habermas T, Bluck S. Getting a life: the emergence of the life story in adolescence. Psychol Bull 2000;126:748–69. [DOI] [PubMed] [Google Scholar]
- 188.McLean KC, Breen AV. Selves in a world of stories during emerging adulthood. In: Arnett JJ, ed. The Oxford handbook of emerging adulthood. New York: Oxford University Press, 2016. [Google Scholar]
- 189.Higgins ET. Self-discrepancy: a theory relating self and affect. Psychol Rev 1987;94:319–40. [PubMed] [Google Scholar]
- 190.Pelham BW, Swann WB. From self-conceptions to self-worth: on the sources and structure of global self-esteem. J Pers Soc Psychol 1989;57:672–80. [DOI] [PubMed] [Google Scholar]
- 191.Goldin PR, Jazaieri H, Ziv M, Kraemer H, Heimberg R, Gross JJ. Changes in positive self-views mediate the effect of cognitive-behavioral therapy for social anxiety disorder. Clin Psychol Sci 2013;1:301–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Clore J, Gaynor S. Self-statement modification techniques for distressed college students with low self-esteem and depressive symptoms. Int J Behav Consult Ther 2006;2:314–31. [Google Scholar]
- 193.Blatt SJ, Quinlan DM, Chevron ES, McDonald C, Zuroff D. Dependency and self-criticism: psychological dimensions of depression. J Consult Clin Psychol 1982;50:113–24. [DOI] [PubMed] [Google Scholar]
- 194.Watkins E, Teasdale JD. Rumination and overgeneral memory in depression: effects of self-focus and analytic thinking. J Abnorm Psychol 2001;110:353–7. [DOI] [PubMed] [Google Scholar]
- 195.Markus H. Self-schemata and processing information about the self. J Pers Soc Psychol 1977;35:63–78. [Google Scholar]
- 196.Rafaeli E, Bernstein DP, Young J. Schema therapy: distinctive features. New York: Routledge, 2011. [Google Scholar]
- 197.Margolin A, Schuman-Olivier Z, Beitel M, Arnold RM, Fulwiler CE. A preliminary study of spiritual self-schema (3-S+) therapy for reducing impulsivity in HIV-positive drug users. J Clin Psychol 2007;63:979–99. [DOI] [PubMed] [Google Scholar]
- 198.Shadick NA Sowell NF Frits ML, et al. A randomized controlled trial of an internal family systems-based psychotherapeutic intervention on outcomes in rheumatoid arthritis: a proof-of-concept study. J Rheumatol 2013;40:1831–41. [DOI] [PubMed] [Google Scholar]
- 199.Schwartz RC. Moving from acceptance toward transformation with internal family systems therapy (IFS). J Clin Psychol 2013;69:805–16. [DOI] [PubMed] [Google Scholar]
- 200.Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL. A default mode of brain function. Proc Natl Acad Sci U S A 2001;98:676–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci 2008;1124:1–38. [DOI] [PubMed] [Google Scholar]
- 202.Andrews-Hanna JR. The brain’s default network and its adaptive role in internal mentation. Neuroscientist 2012;18:251–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Fair DA Cohen AL Dosenbach NU, et al. The maturing architecture of the brain’s default network. Proc Natl Acad Sci U S A 2008;105:4028–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Lois G, Wessa M. Differential association of default mode network connectivity and rumination in healthy individuals and remitted MDD patients. Soc Cogn Affect Neurosci 2016;11:1792–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Brewer JA, Worhunsky PD, Gray JR, Tang YY, Weber J, Kober H. Meditation experience is associated with differences in default mode network activity and connectivity. Proc Natl Acad Sci U S A 2011;108:20254–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Brewer JA, Garrison KA, Whitfield-Gabrieli S. What about the “self” is processed in the posterior cingulate cortex? Front Hum Neurosci 2013;7:647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. J Abnorm Psychol 1991;100:569–82. [DOI] [PubMed] [Google Scholar]
- 208.Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspect Psychol Sci 2008;3:400–24. [DOI] [PubMed] [Google Scholar]
- 209.Wilkinson PO, Croudace TJ, Goodyer IM. Rumination, anxiety, depressive symptoms and subsequent depression in adolescents at risk for psychopathology: a longitudinal cohort study. BMC Psychiatry 2013;13:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Borders A, Giancola PR. Trait and state hostile rumination facilitate alcohol-related aggression. J Stud Alcohol Drugs 2011;72:545–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Zhou H-X Chen X Shen Y-Q, et al. Rumination and the default mode network: meta-analysis of brain imaging studies and implications for depression. Neuroimage 2020;206:116287. [DOI] [PubMed] [Google Scholar]
- 212.Moore JW. What is the sense of agency and why does it matter? Front Psychol 2016;7:1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191–215. [DOI] [PubMed] [Google Scholar]
- 214.Vago DR, Zeidan F. The brain on silent: mind wandering, mindful awareness, and states of mental tranquility. Ann N Y Acad Sci 2016;1373:96–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Spreng RN, Sepulcre J, Turner GR, Stevens WD, Schacter DL. Intrinsic architecture underlying the relations among the default, dorsal attention, and frontoparietal control networks of the human brain. J Cogn Neurosci 2013;25:74–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Miller GE Chen E Armstrong CC, et al. Functional connectivity in central executive network protects youth against cardiometabolic risks linked with neighborhood violence. Proc Natl Acad Sci 2018;115:12063–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Neiss MB, Stevenson J, Sedikides C, Kumashiro M, Finkel EJ, Rusbult CE. Executive self, self-esteem, and negative affectivity: relations at the phenotypic and genotypic level. J Pers Soc Psychol 2005;89:593–606. [DOI] [PubMed] [Google Scholar]
- 218.Tomasino B, Fabbro F. Increases in the right dorsolateral prefrontal cortex and decreases the rostral prefrontal cortex activation after-8 weeks of focused attention based mindfulness meditation. Brain Cogn 2016;102:46–54. [DOI] [PubMed] [Google Scholar]
- 219.Taren AA Gianaros PJ Greco CM, et al. Mindfulness meditation training and executive control network resting state functional connectivity: a randomized controlled trial. Psychosom Med 2017;79:674–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Bauer CCC, Whitfield-Gabrieli S, Díaz JL, Pasaye EH, Barrios FA. From state-to-trait meditation: reconfiguration of central executive and default mode networks. eNeuro 2019;6:ENEURO.0335–18.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Wells RE, Burch R, Paulsen RH, Wayne PM, Houle TT, Loder E. Meditation for migraines: a pilot randomized controlled trial. Headache 2014;54:1484–95. [DOI] [PubMed] [Google Scholar]
- 222.Gross CR Kreitzer MJ Reilly-Spong M, et al. Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: a randomized controlled clinical trial. Explore (NY) 2011;7:76–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.McCubbin T, Dimidjian S, Kempe K, Glassey MS, Ross C, Beck A. Mindfulness-based stress reduction in an integrated care delivery system: one-year impacts on patient-centered outcomes and health care utilization. Perm J 2014;18:4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Gawande R Pine E Griswold T, et al. Insurance-reimbursable mindfulness for safety-net primary care patients: a pilot randomized controlled trial. Mindfulness (N Y) 2019;10:1744–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Burnette JL, O’Boyle EH, VanEpps EM, Pollack JM, Finkel EJ. Mind-sets matter: a meta-analytic review of implicit theories and self-regulation. Psychol Bull 2013;139:655–701. [DOI] [PubMed] [Google Scholar]
- 226.Bandura A, Locke EA. Negative self-efficacy and goal effects revisited. J Appl Psychol 2003;88:87–99. [DOI] [PubMed] [Google Scholar]
- 227.Germer CK, Neff KD. Self-compassion in clinical practice. J Clin Psychol 2013;69:856–67. [DOI] [PubMed] [Google Scholar]
- 228.Kuyken W Watkins E Holden E, et al. How does mindfulness-based cognitive therapy work? Behav Res Ther 2010;48:1105–12. [DOI] [PubMed] [Google Scholar]
- 229.Van Dam NT, Sheppard SC, Forsyth JP, Earleywine M. Self-compassion is a better predictor than mindfulness of symptom severity and quality of life in mixed anxiety and depression. J Anxiety Disord 2011;25:123–30. [DOI] [PubMed] [Google Scholar]
- 230.Sirois FM, Kitner R, Hirsch JK. Self-compassion, affect, and health-promoting behaviors. Health Psychol 2015;34:661–9. [DOI] [PubMed] [Google Scholar]
- 231.Dunne S, Sheffield D, Chilcot J. Brief report: self-compassion, physical health and the mediating role of health-promoting behaviours. J Health Psychol 2016;23:993–9. [DOI] [PubMed] [Google Scholar]
- 232.Ferrari M, Dal Cin M, Steele M. Self-compassion is associated with optimum self-care behaviour, medical outcomes and psychological well-being in a cross-sectional sample of adults with diabetes. Diabet Med 2017;34:1546–53. [DOI] [PubMed] [Google Scholar]
- 233.Kelly AC, Carter JC. Self-compassion training for binge eating disorder: a pilot randomized controlled trial. Psychol Psychother 2015;88:285–303. [DOI] [PubMed] [Google Scholar]
- 234.Semenchuk BN, Strachan SM, Fortier M. Self-compassion and the self-regulation of exercise: reactions to recalled exercise setbacks. J Sport Exerc Psychol 2018;40(1):31–9. [DOI] [PubMed] [Google Scholar]
- 235.Dawson Rose C Webel A Sullivan KM, et al. Self-compassion and risk behavior among people living with HIV/AIDS. Res Nurs Health 2014;37:98–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Terry ML, Leary MR. Self-compassion, self-regulation, and health. Self Identity 2011;10:352–62. [Google Scholar]
- 237.Gilbert P. Compassion and cruelty. In: Compassion and cruelty: a biopsychosocial approach. London: Brunner-Routledge, 2005. [Google Scholar]
- 238.Lutz J Bruhl AB Doerig N, et al. Altered processing of self-related emotional stimuli in mindfulness meditators. Neuroimage 2016;124(Pt A):958–67. [DOI] [PubMed] [Google Scholar]
- 239.Lutz J Berry MP Napadow V, et al. Neural activations during self-related processing in patients with chronic pain and effects of a brief self-compassion training—a pilot study. Psychiatry Res Neuroimaging 2020;304:111155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Elana R. The heart of mindfulness-based stress reduction: a MBSR guide for clinicians and clients. Ashland, OR: Pesi, 2017. [Google Scholar]
- 241.Kabat-Zinn J. Too early to tell: the potential impact and challenges—ethical and otherwise—inherent in the mainstreaming of dharma in an increasingly dystopian world. Mindfulness (N Y) 2017;8:1125–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Diedrich A, Hofmann SG, Cuijpers P, Berking M. Self-compassion enhances the efficacy of explicit cognitive reappraisal as an emotion regulation strategy in individuals with major depressive disorder. Behav Res Ther 2016;82:1–10. [DOI] [PubMed] [Google Scholar]
- 243.Gilbert P, Procter S. Compassionate mind training for people with high shame and self-criticism: overview and pilot study of a group therapy approach. Clin Psychol Psychother 2006;13:353–79. [Google Scholar]
- 244.Cannon WB. The wisdom of the body. 2nd ed.Oxford: Norton, 1939. [Google Scholar]
- 245.O’Doherty JP, Cockburn J, Pauli WM. Learning, reward, and decision making. Annu Rev Psychol 2017;68:73–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.LeDoux JE, Moscarello J, Sears R, Campese V. The birth, death and resurrection of avoidance: a reconceptualization of a troubled paradigm. Mol Psychiatry 2017;22:24–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Shapiro SL, Schwartz GE. The role of intention in self-regulation: toward intentional systemic mindfulness. In: Boekaerts M, Pintrich PR, Zeidner M. Handbook of self-regulation. San Diego, CA: Academic, 2000. [Google Scholar]
- 248.Schwartz GE. Psychobiology of health: a new synthesis. In: Hammonds BL, Scheirer CJ, eds. Master lecture series, vol. 3: Psychology and health. Washington, DC: American Psychological Association, 1984. [Google Scholar]
- 249.Davidson RJ, Schwartz GE, Rothman LP. Attentional style and the self-regulation of mode-specific attention: an electroencephalograhic study. J Abnorm Psychol 1976;85:611–21. [DOI] [PubMed] [Google Scholar]
- 250.Morris G, Nevet A, Arkadir D, Vaadia E, Bergman H. Midbrain dopamine neurons encode decisions for future action. Nat Neurosci 2006;9:1057–63. [DOI] [PubMed] [Google Scholar]
- 251.Glimcher PW. Understanding dopamine and reinforcement learning: the dopamine reward prediction error hypothesis. Proc Natl Acad Sci U S A 2011;108(suppl 3):15647–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Berridge KC, Robinson TE. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res Brain Res Rev 1998;28:309–69. [DOI] [PubMed] [Google Scholar]
- 253.Brewer JA, Potenza MN. The neurobiology and genetics of impulse control disorders: relationships to drug addictions. Biochem Pharmacol 2008;75:63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Malvaez M, Wassum KM. Regulation of habit formation in the dorsal striatum. Curr Opin Behav Sci 2018;20:67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Malvaez M Greenfield VY Matheos DP, et al. Habits are negatively regulated by histone deacetylase 3 in the dorsal striatum. Biol Psychiatry 2018;84:383–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Sterling P. Allostasis: a model of predictive regulation. Physiol Behav 2012;106:5–15. [DOI] [PubMed] [Google Scholar]
- 257.Castro DC, Bruchas MR. A motivational and neuropeptidergic hub: anatomical and functional diversity within the nucleus accumbens shell. Neuron 2019;102:529–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Hunt WA, Matarazzo JD, Weiss SM, Gentry WD. Associative learning, habit, and health behavior. J Behav Med 1979;2:111–24. [DOI] [PubMed] [Google Scholar]
- 259.Maren S, Fanselow MS. The amygdala and fear conditioning: has the nut been cracked? Neuron 1996;16:237–40. [DOI] [PubMed] [Google Scholar]
- 260.Sengupta A Yau JOY Jean-Richard-Dit-Bressel P, et al. Basolateral amygdala neurons maintain aversive emotional salience. J Neurosci 2018;38:3001–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Skelly MJ, Ariwodola OJ, Weiner JL. Fear conditioning selectively disrupts noradrenergic facilitation of GABAergic inhibition in the basolateral amygdala. Neuropharmacology 2017;113(Pt A):231–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.D’Argembeau A. On the role of the ventromedial prefrontal cortex in self-processing: the valuation hypothesis. Front Hum Neurosci 2013;7:372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Hiser J, Koenigs M. The multifaceted role of the ventromedial prefrontal cortex in emotion, decision making, social cognition, and psychopathology. Biol Psychiatry 2018;83:638–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Berkman ET, Livingston JL, Kahn LE. Finding the “self” in self-regulation: the identity-value model. Psychol Inq 2017;28:77–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Lee JLC, Milton AL, Everitt BJ. Reconsolidation and extinction of conditioned fear: inhibition and potentiation. J Neurosci 2006;26:10051–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Myers KM, Davis M. Mechanisms of fear extinction. Mol Psychiatry 2007;12:120–50. [DOI] [PubMed] [Google Scholar]
- 267.Milad MR, Quirk GJ. Fear extinction as a model for translational neuroscience: ten years of progress. Annu Rev Psychol 2012;63:129–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Lange I Goossens L Michielse S, et al. Neural responses during extinction learning predict exposure therapy outcome in phobia: results from a randomized-controlled trial. Neuropsychopharmacology 2020;45:534–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Nasser HM, McNally GP. Neural correlates of appetitive-aversive interactions in Pavlovian fear conditioning. Learn Mem 2013;20:220–8. [DOI] [PubMed] [Google Scholar]
- 270.Bulganin L, Bach D, Wittmann B. Prior fear conditioning and reward learning interact in fear and reward networks. Front Behav Neurosci 2014;8:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Barrett LF, Quigley KS, Hamilton P. An active inference theory of allostasis and interoception in depression. Philos Trans R Soc Lond B Biol Sci 2016;371:20160011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Barrett LF. The theory of constructed emotion: an active inference account of interoception and categorization. Soc Cogn Affect Neurosci 2017;12:1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Brewer J. Mindfulness training for addictions: has neuroscience revealed a brain hack by which awareness subverts the addictive process? Curr Opin Psychol 2019;28:198–203. [DOI] [PubMed] [Google Scholar]
- 274.Margolin A, Beitel M, Schuman-Olivier Z, Avants SK. A controlled study of a spirituality-focused intervention for increasing motivation for HIV prevention among drug users. AIDS Educ Prev 2006;18:311–22. [DOI] [PubMed] [Google Scholar]
- 275.Khoury B, Knäuper B, Schlosser M, Carrière K, Chiesa A. Effectiveness of traditional meditation retreats: a systematic review and meta-analysis. J Psychosom Res 2017;92:16–25. [DOI] [PubMed] [Google Scholar]
- 276.Marlatt GA, Gordon JR. Relapse prevention: maintenance strategies in the treatment of addictive behaviors. New York: Guilford, 1985. [Google Scholar]
- 277.Cormack D, Jones FW, Maltby M. A “collective effort to make yourself feel better”: the group process in mindfulness-based interventions. Qual Health Res 2017;28:3–15. [DOI] [PubMed] [Google Scholar]
- 278.Siegel DJ. The developing mind: toward a neurobiology of interpersonal experience. New York: Guilford, 1999. [Google Scholar]
- 279.Corrigan FM, Fisher JJ, Nutt DJ. Autonomic dysregulation and the Window of Tolerance model of the effects of complex emotional trauma. J Psychopharmacol 2011;25:17–25. [DOI] [PubMed] [Google Scholar]
- 280.Kummar AS. Mindfulness and fear extinction: a brief review of its current neuropsychological literature and possible implications for posttraumatic stress disorder. Psychol Rep 2017;121:792–814. [DOI] [PubMed] [Google Scholar]
- 281.Hölzel BK Brunsch V Gard T, et al. Mindfulness-based stress reduction, fear conditioning, and the uncinate fasciculus: a pilot study. Front Behav Neurosci 2016;10:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Demarzo MMP Montero-Marin J Cuijpers P, et al. The efficacy of mindfulness-based interventions in primary care: a meta-analytic review. Ann Fam Med 2015;13:573–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Kalivas PW, O’Brien C. Drug addiction as a pathology of staged neuroplasticity. Neuropsychopharmacology 2008;33:166–80. [DOI] [PubMed] [Google Scholar]
- 284.Marcotte D, Avants SK, Margolin A. Spiritual self-schema therapy, drug abuse, and HIV. J Psychoactive Drugs 2003;35:389–91. [DOI] [PubMed] [Google Scholar]
- 285.Farb N Daubenmier J Price CJ, et al. Interoception, contemplative practice, and health. Front Psychol 2015;6:763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Deci EL, Ryan RM. The “what” and “why” of goal pursuits: human needs and the self-determination of behavior. Psychol Inq 2000;11:227–68. [Google Scholar]
- 287.Schultz P, Ryan R. The “why,” “what,” and “how” of healthy self-regulation: mindfulness and well-being from a self-determination theory perspective. In: Ostafin BD, Robinson MD, Meier BP, eds. Handbook of mindfulness and self-regulation. New York: Springer, 2015. [Google Scholar]
- 288.Gruber MJ, Ranganath C. How curiosity enhances hippocampus-dependent memory: the prediction, appraisal, curiosity, and exploration (PACE) framework. Trends Cogn Sci 2019;23:1014–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Gruber MJ, Gelman BD, Ranganath C. States of curiosity modulate hippocampus-dependent learning via the dopaminergic circuit. Neuron 2014;84:486–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Deci EL, Ryan RM, Schultz PP, Niemiec CP. Being aware and functioning fully: mindfulness and interest taking within self-determination theory. In: Brown KW, Creswell JD, Ryan RM, eds. Handbook of mindfulness: theory, research, and practice. New York: Guilford, 2015. [Google Scholar]
- 291.Manohar SG, Finzi RD, Drew D, Husain M. Distinct motivational effects of contingent and noncontingent rewards. Psychol Sci 2017;28:1016–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Beierholm U Guitart-Masip M Economides M, et al. Dopamine modulates reward-related vigor. Neuropsychopharmacology 2013;38:1495–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Yee DM, Braver TS. Interactions of motivation and cognitive control. Curr Opin Behav Sci 2018;19:83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Garland EL, Froeliger B, Howard MO. Effects of mindfulness-oriented recovery enhancement on reward responsiveness and opioid cue-reactivity. Psychopharmacol 2014;231:3229–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Fredrickson BL. The broaden-and-build theory of positive emotions. Philos Trans R Soc Lond B Biol Sci 2004;359:1367–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Vandercammen L, Hofmans J, Theuns P. Relating specific emotions to intrinsic motivation: on the moderating role of positive and negative emotion differentiation. PLoS One 2014;9:e115396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Bora E, Yucel M, Allen NB. Neurobiology of human affiliative behaviour: implications for psychiatric disorders. Curr Opin Psychiatry 2009;22:320–5. [DOI] [PubMed] [Google Scholar]
- 298.Engen HG, Singer T. Compassion-based emotion regulation up-regulates experienced positive affect and associated neural networks. Soc Cogn Affect Neurosci 2015;10:1291–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.da Silva J. Trauma-sensitive mindfulness: practices for safe and transformative healing. Trans Anal J 2018;48:288–90. [Google Scholar]
- 300.Renpenning K, Taylor SG, eds. Self-care theory in nursing: selected papers of Dorothea Orem. New York: Springer, 2003. [Google Scholar]
- 301.Lindahl JR, Fisher NE, Cooper DJ, Rosen RK, Britton WB. The varieties of contemplative experience: a mixed-methods study of meditation-related challenges in Western Buddhists. PLoS One 2017;12:e0176239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Dakwar E, Levin FR. The emerging role of meditation in addressing psychiatric illness, with a focus on substance use disorders. Harv Rev Psychiatry 2009;17:254–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Hoppes K. The application of mindfulness-based cognitive interventions in the treatment of co-occurring addictive and mood disorders. CNS Spectr 2006;11:829–51. [DOI] [PubMed] [Google Scholar]
- 304.Zgierska A, Rabago D, Chawla N, Kushner K, Koehler R, Marlatt A. Mindfulness meditation for substance use disorders: a systematic review. Subst Abuse 2009;30:266–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Sancho M De Gracia M Rodriguez RC, et al. Mindfulness-based interventions for the treatment of substance and behavioral addictions: a systematic review. Front Psychiatry 2018;9:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Priddy SE, Howard MO, Hanley AW, Riquino MR, Friberg-felsted K, Garland EL. Mindfulness meditation in the treatment of substance use disorders and preventing future relapse: neurocognitive mechanisms and clinical implications. Subst Abuse Rehabil 2018;16:103–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Spears CA. Mindfulness-based interventions for addictions among diverse and underserved populations. Curr Opin Psychol 2019;30:11–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Byrne SP, Haber P, Baillie A, Costa DSJ, Fogliati V, Morley K. Systematic reviews of mindfulness and acceptance and commitment therapy for alcohol use disorder: should we be using third wave therapies? Alcohol Alcohol 2019;54:159–66. [DOI] [PubMed] [Google Scholar]
- 309.Brewer JA, Bowen S, Smith JT, Marlatt GA, Potenza MN. Mindfulness-based treatments for co-occurring depression and substance use disorders: what can we learn from the brain? Addiction 2010;105:1698–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Black DS. Mindfulness-based interventions: an antidote to suffering in the context of substance use, misuse, and addiction. Subst Use Misuse 2014;49:487–91. [DOI] [PubMed] [Google Scholar]
- 311.Tang YY, Posner MI, Rothbart MK, Volkow ND. Circuitry of self-control and its role in reducing addiction. Trends Cogn Sci 2015;19:439–44. [DOI] [PubMed] [Google Scholar]
- 312.Garland EL, Howard MO. Mindfulness-based treatment of addiction: current state of the field and envisioning the next wave of research. Addict Sci Clin Pract 2018;13:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Bowen S Witkiewitz K Clifasefi SL, et al. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry 2014;71:547–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Garland EL, Schwarz NM, Kelly A, Whitt A, Howard MO. Mindfulness-oriented recovery enhancement for alcohol dependence: therapeutic mechanisms and intervention acceptability. J Soc Work Pract Addict 2012;12:242–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Price CJ, Thompson EA, Crowell S, Pike K. Longitudinal effects of interoceptive awareness training through mindful awareness in body-oriented therapy (MABT) as an adjunct to women’s substance use disorder treatment: a randomized controlled trial. Drug Alcohol Depend 2019;198:140–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Vidrine JI Spears CA Heppner WL, et al. Efficacy of mindfulness-based addiction treatment (MBAT) for smoking cessation and lapse recovery: a randomized clinical trial. J Consult Clin Psychol 2016;84:824–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Tang YY, Tang R, Posner MI. Brief meditation training induces smoking reduction. Proc Natl Acad Sci U S A 2013;110:13971–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Luoma JB, Kohlenberg BS, Hayes SC, Fletcher L. Slow and steady wins the race: a randomized clinical trial of acceptance and commitment therapy targeting shame in substance use disorders. J Consult Clin Psychol 2012;80:43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Bowen S Witkiewitz K Clifasefi SL, et al. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry 2015;71:547–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Glasner-Edwards S Mooney LJ Ang A, et al. Mindfulness based relapse prevention for stimulant dependent adults: a pilot randomized clinical trial. Mindfulness (N Y) 2017;8:126–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Hamidi F, Kheiran S. Mindfulness-based relapse prevention to reduce high risk behaviors of people addicted to methamphetamine. Int J High Risk Behav Addict 2019;8:e92609. [Google Scholar]
- 322.Chen XJ Wang DM Zhou LD, et al. Mindfulness-based relapse prevention combined with virtual reality cue exposure for methamphetamine use disorder: study protocol for a randomized controlled trial. Contemp Clin Trials 2018;70:99–105. [DOI] [PubMed] [Google Scholar]
- 323.Bloom-Foster J, Mehl-Madrona L. An ultra-brief mindfulness-based intervention for patients in treatment for opioid addiction with buprenorphine: a primary care feasibility pilot study. J Altern Complement Med 2020;26:34–43. [DOI] [PubMed] [Google Scholar]
- 324.Sokol R, LaVertu AE, Morrill D, Albanese C, Schuman-Olivier Z. Group-based treatment of opioid use disorder with buprenorphine: a systematic review. J Subst Abuse Treat 2018;84:78–87. [DOI] [PubMed] [Google Scholar]
- 325.Yaghubi M, Zargar F, Akbari H. Comparing effectiveness of mindfulness-based relapse prevention with treatment as usual on impulsivity and relapse for methadone-treated patients: a randomized clinical trial. Addict Health 2017;9:156–65. [PMC free article] [PubMed] [Google Scholar]
- 326.Valls-Serrano C, Caracuel A, Verdejo-Garcia A. Goal management training and mindfulness meditation improve executive functions and transfer to ecological tasks of daily life in polysubstance users enrolled in therapeutic community treatment. Drug Alcohol Depend 2016;165:9–14. [DOI] [PubMed] [Google Scholar]
- 327.Witkiewitz K, Bowen S. Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. J Consult Clin Psychol 2010;78:362–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Garland EL, Roberts-Lewis A, Kelley K, Tronnier C, Hanley A. Cognitive and affective mechanisms linking trait mindfulness to craving among individuals in addiction recovery. Subst Use Misuse 2014;49:525–35. [DOI] [PubMed] [Google Scholar]
- 329.Bowen S, Witkiewitz K, Dillworth TM, Marlatt GA. The role of thought suppression in the relationship between mindfulness meditation and alcohol use. Addict Behav 2007;32:2324–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Levin ME, Luoma JB, Haeger JA. Decoupling as a mechanism of change in mindfulness and acceptance: a literature review. Behav Modif 2015;39:870–911. [DOI] [PubMed] [Google Scholar]
- 331.Moss AC, Erskine JAK, Albery IP, Allen JR, Georgiou GJ. To suppress, or not to suppress? That is repression: controlling intrusive thoughts in addictive behaviour. Addict Behav 2015;44:65–70. [DOI] [PubMed] [Google Scholar]
- 332.Price CJ, Merrill JO, McCarty RL, Pike KC, Tsui JI. A pilot study of mindful body awareness training as an adjunct to office-based medication treatment of opioid use disorder. J Subst Abuse Treat 2020;108:123–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Brewer JA Sinha R Chen JA, et al. Mindfulness training and stress reactivity in substance abuse: results from a randomized, controlled stage I pilot study. Subst Abus 2009;30:306–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Westbrook C, Creswell JD, Tabibnia G, Julson E, Kober H, Tindle HA. Mindful attention reduces neural and self-reported cue-induced craving in smokers. Soc Cogn Affect Neurosci 2013;8:73–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Garland EL. Trait mindfulness predicts attentional and autonomic regulation of alcohol cue-reactivity. J Psychophysiol 2011;25:180–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Carroll H, Lustyk MKB. Mindfulness-based relapse prevention for substance use disorders: effects on cardiac vagal control and craving under stress. Mindfulness (N Y) 2018;9:488–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Garland EL. Restructuring reward processing with mindfulness-oriented recovery enhancement: novel therapeutic mechanisms to remediate hedonic dysregulation in addiction, stress, and pain. Ann N Y Acad Sci 2016;1373:25–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Garland EL, Atchley RM, Hanley AW, Zubieta J-K, Froeliger B. Mindfulness-oriented recovery enhancement remediates hedonic dysregulation in opioid users: neural and affective evidence of target engagement. Sci Adv 2019;5:eaax1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Carrière K, Khoury B, Günak MM, Knäuper B. Mindfulness-based interventions for weight loss: a systematic review and meta-analysis. Obes Rev 2017;19:164–77. [DOI] [PubMed] [Google Scholar]
- 340.Godfrey KM, Gallo LC, Afari N. Mindfulness-based interventions for binge eating: a systematic review and meta-analysis. J Behav Med 2014;38:348–62. [DOI] [PubMed] [Google Scholar]
- 341.Katterman SN, Kleinman BM, Hood MM, Nackers LM, Corsica JA. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eat Behav 2014;15:197–204. [DOI] [PubMed] [Google Scholar]
- 342.Mantzios M, Wilson JC. Mindfulness, eating behaviours, and obesity: a review and reflection on current findings. Curr Obes Rep 2015;4:141–6. [DOI] [PubMed] [Google Scholar]
- 343.O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes Rev 2014;15:453–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Rogers JM, Ferrari M, Mosely K, Lang CP, Brennan L. Mindfulness-based interventions for adults who are overweight or obese: a meta-analysis of physical and psychological health outcomes. Obes Rev 2016;18:51–67. [DOI] [PubMed] [Google Scholar]
- 345.Olson KL, Emery CF. Mindfulness and weight loss: a systematic review. Psychosom Med 2015;77:59–67. [DOI] [PubMed] [Google Scholar]
- 346.Warren JM, Smith N, Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: effectiveness and associated potential mechanisms. Nutr Res Rev 2017;30:272–83. [DOI] [PubMed] [Google Scholar]
- 347.Roche AI, Kroska EB, Denburg NL. Acceptance- and mindfulness-based interventions for health behavior change: systematic reviews and meta-analyses. J Context Behav Sci 2019;13(April):74–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Brewer JA Ruf A Beccia AL, et al. Can mindfulness address maladaptive eating behaviors? Why traditional diet plans fail and how new mechanistic insights may lead to novel interventions. Front Psychol 2018;9:1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Reed JR, Yates BC, Houfek J, Pullen CH, Briner W, Schmid KK. Eating self-regulation in overweight and obese adults: a concept analysis. Nurs Forum 2015;51:105–16. [DOI] [PubMed] [Google Scholar]
- 350.Baer RA, Fischer S, Huss DB. Mindfulness and acceptance in the treatment of disordered eating. J Ration Emot Cogn Behav Ther 2005;23:281–300. [Google Scholar]
- 351.Arch JJ, Brown KW, Goodman RJ, Della Porta MD, Kiken LG, Tillman S. Enjoying food without caloric cost: the impact of brief mindfulness on laboratory eating outcomes. Behav Res Ther 2016;79:23–34. [DOI] [PubMed] [Google Scholar]
- 352.Mason AE, Jhaveri K, Cohn M, Brewer JA. Testing a mobile mindful eating intervention targeting craving-related eating: feasibility and proof of concept. J Behav Med 2018;41:160–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Caldwell K, Baime M, Wolever R. Mindfulness based approaches to obesity and weight loss maintenance. J Ment Health Couns 2012;34:269–82. [Google Scholar]
- 354.Kristeller JL, Wolever RQ. Mindfulness-based eating awareness training for treating binge eating disorder: the conceptual foundation. Eat Disord 2011;19:49–61. [DOI] [PubMed] [Google Scholar]
- 355.Kristeller JL, Epel E. Mindful eating and mindless eating: the science and the practice. In: Amanda I, Ngnoumen CT, Langer EJ, eds. The Wiley Blackwell handbook of mindfulness. Malden, MA: Wiley, 2014. [Google Scholar]
- 356.Godsey J. The role of mindfulness based interventions in the treatment of obesity and eating disorders: an integrative review. Complement Ther Med 2013;21:430–9. [DOI] [PubMed] [Google Scholar]
- 357.Turgon R, Ruffault A, Juneau C, Blatier C, Shankland R. Eating disorder treatment: a systematic review and meta-analysis of the efficacy of mindfulness-based programs. Mindfulness (N Y) 2019;10:2225–44. [Google Scholar]
- 358.Linardon J, Fairburn CG, Fitzsimmons-Craft EE, Wilfley DE, Brennan L. The empirical status of the third-wave behaviour therapies for the treatment of eating disorders: a systematic review. Clin Psychol Rev 2017;58:125–40. [DOI] [PubMed] [Google Scholar]
- 359.Dunne J. Mindfulness in anorexia nervosa: an integrated review of the literature. J Am Psychiatr Nurses Assoc 2017;24:109–17. [DOI] [PubMed] [Google Scholar]
- 360.Masuda A, Hill ML. Mindfulness as therapy for disordered eating: a systematic review. Neuropsychiatry (London) 2013;3:433–47. [Google Scholar]
- 361.Pisetsky EM, Schaefer LM, Wonderlich SA, Peterson CB. Emerging psychological treatments in eating disorders. Psychiatr Clin North Am 2019;42:219–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Wanden-Berghe RG, Sanz-Valero J, Wanden-Berghe C. The application of mindfulness to eating disorders treatment: a systematic review. Eat Disord 2010;19:34–48. [DOI] [PubMed] [Google Scholar]
- 363.Oikonomou MT, Arvanitis M, Sokolove RL. Mindfulness training for smoking cessation: a meta-analysis of randomized-controlled trials. J Health Psychol 2017;22:1841–50. [DOI] [PubMed] [Google Scholar]
- 364.Maglione MA Maher AR Ewing B, et al. Efficacy of mindfulness meditation for smoking cessation: a systematic review and meta-analysis. Addict Behav 2017;69:27–34. [DOI] [PubMed] [Google Scholar]
- 365.de Souza ICW de Barros VV Gomide HP, et al. Mindfulness-based interventions for the treatment of smoking: a systematic literature review. J Altern Complement Med 2015;21:129–40. [DOI] [PubMed] [Google Scholar]
- 366.Brewer JA Mallik S Babuscio TA, et al. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alcohol Depend 2011;119:72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Schuman-Olivier Z, Hoeppner BB, Evins AE, Brewer JA. Finding the right match: mindfulness training may potentiate the therapeutic effect of nonjudgment of inner experience on smoking cessation. Subst Use Misuse 2014;49:586–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Elwafi HM, Witkiewitz K, Mallik S, Thornhill TA, Brewer JA. Mindfulness training for smoking cessation: moderation of the relationship between craving and cigarette use. Drug Alcohol Depend 2013;130:222–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Garrison KA, Pal P, Rojiani R, Dallery J, O’Malley SS, Brewer JA. A randomized controlled trial of smartphone-based mindfulness training for smoking cessation: a study protocol. BMC Psychiatry 2015;15:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Garrison KA, Pal P, O’Malley SS, Pittman BP, Gueorguieva R, Brewer JA. Craving to quit: a randomized controlled trial of smartphone app-based mindfulness training for smoking cessation. Nicotine Tob Res 2018;22:324–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Garrison KA, Santoyo JF, Davis JH, Thornhill TA, Kerr CE, Brewer JA. Effortless awareness: using real time neurofeedback to investigate correlates of posterior cingulate cortex activity in meditators’ self-report. Front Hum Neurosci 2013;7:440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Janes AC Datko M Roy A, et al. Quitting starts in the brain: a randomized controlled trial of app-based mindfulness shows decreases in neural responses to smoking cues that predict reductions in smoking. Neuropsychopharmacology 2019;44:1631–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Swendeman D, Ingram BL, Rotheram-Borus MJ. Common elements in self-management of HIV and other chronic illnesses: an integrative framework. AIDS Care 2009;21:1321–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J Public Health 2014;104:e25–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Ornstein SM, Nietert PJ, Jenkins RG, Litvin CB. The prevalence of chronic diseases and multimorbidity in primary care practice: a PPRNet report. J Am Board Fam Med 2013;26:518–24. [DOI] [PubMed] [Google Scholar]
- 376.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA 2002;288:2469–75. [DOI] [PubMed] [Google Scholar]
- 377.Kanaan SB. Promoting effective self-management approaches to improve chronic disease care: lessons learned. Oakland, CA: California HealthCare Foundation, 2008. [Google Scholar]
- 378.Scott KM Lim C Al-Hamzawi A, et al. Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry 2016;73:150–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA 2007;298:1685–7. [DOI] [PubMed] [Google Scholar]
- 380.Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders. Prev Chronic Dis 2005;2:A14. [PMC free article] [PubMed] [Google Scholar]
- 381.Kessler RC, DuPont RL, Berglund P, Wittchen HU. Impairment in pure and comorbid generalized anxiety disorder and major depression at 12 months in two national surveys. Am J Psychiatry 1999;156:1915–23. [DOI] [PubMed] [Google Scholar]
- 382.Loucks EB, Gilman SE, Britton WB, Gutman R, Eaton CB, Buka SL. Associations of mindfulness with glucose regulation and diabetes. Am J Health Behav 2016;40:258–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Benzo RP. Mindfulness and motivational interviewing: two candidate methods for promoting self-management. Chron Respir Dis 2013;10:175–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Ludwig K Haindl A Laufs R, et al. Self-regulation in preschool children’s everyday life: exploring day-to-day variability and the within- and between-person structure. J Self Regul Regul 2016;2:99–117. [Google Scholar]
- 385.Youngwanichsetha S, Phumdoung S, Ingkathawornwong T. The effects of mindfulness eating and yoga exercise on blood sugar levels of pregnant women with gestational diabetes mellitus. Appl Nurs Res 2014;27:227–30. [DOI] [PubMed] [Google Scholar]
- 386.Armani Kian A Vahdani B Noorbala AA, et al. The impact of mindfulness-based stress reduction on emotional wellbeing and glycemic control of patients with type 2 diabetes mellitus. J Diabetes Res 2018;2018:1986820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Ellis DA Carcone AI Slatcher R, et al. Efficacy of mindfulness-based stress reduction in emerging adults with poorly controlled, type 1 diabetes: a pilot randomized controlled trial. Pediatr Diabetes 2019;20:226–34. [DOI] [PubMed] [Google Scholar]
- 388.Homan KJ, Sirois FM. Self-compassion and physical health: exploring the roles of perceived stress and health-promoting behaviors. Health Psychol Open 2017;4:2055102917729542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Gillions A, Cheang R, Duarte R, Kingdom U, Ireland N. The effect of mindfulness practice on aggression and violence levels in adults: a systematic review. Aggress Violent Behav 2019;48:104–15. [Google Scholar]
- 390.Stratton KJ. Mindfulness-based approaches to impulsive behaviors. New School Psychol Bull 2006;4:49–71. [Google Scholar]
- 391.Peters JR, Erisman SM, Upton BT, Baer RA, Roemer L. A preliminary investigation of the relationships between dispositional mindfulness and impulsivity. Mindfulness 2011;2:228–35. [Google Scholar]
- 392.Singh NN, Wahler RG, Adkins AD, Myers RE. Soles of the feet: a mindfulness-based self-control intervention for aggression by an individual with mild mental retardation and mental illness. Res Dev Disabil 2003;24:158–69. [DOI] [PubMed] [Google Scholar]
- 393.Verheul R, Van den Bosch L, Koeter M, de Ridder M. Dialectical behaviour therapy for women with borderline personality disorder: 12-month, randomised clinical trial in the Netherlands. Br J Psychiatry 2003;182:135–40. [DOI] [PubMed] [Google Scholar]
- 394.Zarling A, Lawrence E, Marchman J. A randomized controlled trial of acceptance and commitment therapy for aggressive behavior. J Consult Clin Psychol 2015;83:199–212. [DOI] [PubMed] [Google Scholar]
- 395.Robins CJ, Keng S, Ekblad AG, Brantley JG. Effects of mindfulness-based stress reduction on emotional experience and expression: a randomized controlled trial. J Clin Psychol 2012;68:117–31. [DOI] [PubMed] [Google Scholar]
- 396.Cheng S, Banks K, Bartlett BA, Miguel GS, Vujanovic AA. Posttraumatic stress and mindfulness facets in relation to suicidal ideation severity among psychiatric inpatients. Mindfulness (N Y) 2017;9:761–72. [Google Scholar]
- 397.Zeng W, Ma Z, Li H. Mindfulness and suicidal ideation in Chinese older adults: perceived stress as mediator. Soc Behav Pers 2017;45:733–40. [Google Scholar]
- 398.Garisch JA, Wilson MS. Prevalence, correlates, and prospective predictors of non-suicidal self-injury among New Zealand adolescents: cross-sectional and longitudinal survey data. Child Adolesc Psychiatry Ment Health 2015;9:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Heath NL, Carsley D, De Riggi ME, Mills D, Mettler J. The relationship between mindfulness, depressive symptoms, and non-suicidal self-injury amongst adolescents. Arch Suicide Res 2016;20:635–49. [DOI] [PubMed] [Google Scholar]
- 400.Méndez-Bustos P, Calati R, Rubio-Ramírez F, Olié E, Courtet P, Lopez-Castroman J. Effectiveness of psychotherapy on suicidal risk: a systematic review of observational studies. Front Psychol 2019;10:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.DeCou CR, Comtois KA, Landes SJ. Dialectical behavior therapy is effective for the treatment of suicidal behavior: a meta-analysis. Behav Ther 2019;50:60–72. [DOI] [PubMed] [Google Scholar]
- 402.Chesin M, Interian A, Kline A, Benjamin-Phillips C, Latorre M, Stanley B. Reviewing mindfulness-based interventions for suicidal behavior. Arch Suicide Res 2016;20:507–27. [DOI] [PubMed] [Google Scholar]
- 403.Le TN, Gobert JM. Translating and implementing a mindfulness-based youth suicide prevention intervention in a native American community. J Child Fam Stud 2013;24:12–23. [Google Scholar]
- 404.Barnhofer T, Crane C, Hargus E, Amarasinghe M, Winder R, Williams JMG. Mindfulness-based cognitive therapy as a treatment for chronic depression: a preliminary study. Behav Res Ther 2009;47:366–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Lu R Zhou Y Wu Q, et al. The effects of mindfulness training on suicide ideation among left-behind children in China: a randomized controlled trial. Child Care Health Dev 2019;45:371–9. [DOI] [PubMed] [Google Scholar]
- 406.Forkmann T, Brakemeier E-L, Teismann T, Schramm E, Michalak J. The effects of mindfulness-based cognitive therapy and cognitive behavioral analysis system of psychotherapy added to treatment as usual on suicidal ideation in chronic depression: results of a randomized-clinical trial. J Affect Disord 2016;200:51–7. [DOI] [PubMed] [Google Scholar]
- 407.Barnhofer T Crane C Brennan K, et al. Mindfulness-based cognitive therapy (MBCT) reduces the association between depressive symptoms and suicidal cognitions in patients with a history of suicidal depression. J Consult Clin Psychol 2015;83:1013–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Chesin MS, Benjamin-Phillips CA, Keilp J, Fertuck EA, Brodsky BS, Stanley B. Improvements in executive attention, rumination, cognitive reactivity, and mindfulness among high–suicide risk patients participating in adjunct mindfulness-based cognitive therapy: preliminary findings. J Altern Complement Med 2016;22:642–9. [DOI] [PubMed] [Google Scholar]
- 409.McCauley E Berk MS Asarnow JR, et al. Efficacy of dialectical behavior therapy for adolescents at high risk for suicide a randomized clinical trial. JAMA Psychiatry 2018;75:777–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Mehlum L Ramberg M Tørmoen AJ, et al. Dialectical behavior therapy compared with enhanced usual care for adolescents with repeated suicidal and self-harming behavior: outcomes over a one-year follow-up. J Am Acad Child Adolesc Psychiatry 2016;55:295–300. [DOI] [PubMed] [Google Scholar]
- 411.Rees CS, Hasking P, Breen LJ, Lipp OV, Mamotte C. Group mindfulness based cognitive therapy vs group support for self-injury among young people: study protocol for a randomised controlled trial. BMC Psychiatry 2015;15:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Tighe J, Nicholas J, Shand F, Christensen H. Efficacy of acceptance and commitment therapy in reducing suicidal ideation and deliberate self-harm: systematic review. JMIR Ment Health 2018;5:e10732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Oberle E, Schonert-reichl KA, Lawlor MS, Kimberly C. Mindfulness and inhibitory control in early adolescence. J Early Adolesc 2012;32:565–88. [Google Scholar]
- 414.Eisenlohr-Moul TA, Peters JR, Pond RS, DeWall CN. Both trait and state mindfulness predict lower aggressiveness via anger rumination: a multilevel mediation analysis. Mindfulness (N Y) 2016;7:713–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Kelley TM, Lambert EG. Mindfulness as a potential means of attenuating anger and aggression for prospective criminal justice professionals. Mindfulness (N Y) 2012;3:261–74. [Google Scholar]
- 416.Feldman G, Greeson J, Renna M, Robbins-Monteith K. Mindfulness predicts less texting while driving among young adults: examining attention- and emotion-regulation motives as potential mediators. Pers Individ Dif 2011;51:856–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Murphy C, Mackillop J. Living in the here and now: interrelationships between impulsivity, mindfulness, and alcohol misuse. Psychopharmacology (Berl) 2012;219:527–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Black DS, Sussman S, Johnson CA, Milam J. Testing the indirect effect of trait mindfulness on adolescent cigarette smoking through negative affect. J Subst Abuse 2012;17:417–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Lakey CE, Campbell WK, Warren K, Goodie AS. Dispositional mindfulness as a predictor of the severity of gambling outcomes. Pers Individ Dif 2007;43:1698–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Shorey RC, Elmquist J, Gawrysiak MJ, Anderson S, Stuart GL. The relationship between mindfulness and compulsive sexual behavior in a sample of men in treatment for substance use disorders. Mindfulness (N Y) 2016;7:866–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Crosby JM, Twohig MP, Crosby JM. Acceptance and commitment therapy for problematic internet pornography use: a randomized trial. Behav Ther 2016;47:355–66. [DOI] [PubMed] [Google Scholar]
- 422.Reid RC, Bramen JE, Anderson A, Cohen MS. Mindfulness, emotional dysregulation, impulsivity, and stress proneness among hypersexual patients. J Clin Psychol 2014;70:313–21. [DOI] [PubMed] [Google Scholar]
- 423.Brattström O, Eriksson M, Larsson E, Oldner A. Socio-economic status and co-morbidity as risk factors for trauma. Eur J Epidemiol 2014;30:151–7. [DOI] [PubMed] [Google Scholar]
- 424.Goodman A, Sommers-Flanagan J, Treleaven DA. Trauma-sensitive mindfulness: practices for safe and transformative healing. J Contemp Psychother 2018;49:127–8. [Google Scholar]
- 425.Waldron EM, Hong S, Moskowitz JT, Burnett-Zeigler I. A systematic review of the demographic characteristics of participants in US-based randomized controlled trials of mindfulness-based interventions. Mindfulness (N Y) 2018;9:1671–92. [Google Scholar]
- 426.Cook BL, Trinh N-H, Li Z, Hou SS-Y, Progovac AM. Trends in racial-ethnic disparities in access to mental health care, 2004–2012. Psychiatr Serv 2017;68:9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Budge SL, Adelson JL, Howard KAS. Anxiety and depression in transgender individuals: the roles of transition status, loss, social support, and coping. J Consult Clin Psychol 2013;81:545–57. [DOI] [PubMed] [Google Scholar]
- 428.Gilman SE, Cochran SD, Mays VM, Hughes M, Ostrow D, Kessler RC. Risk of psychiatric disorders among individuals reporting same-sex sexual partners in the National Comorbidity Survey. Am J Public Health 2001;91:933–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.Khullar D, Chokshi DA. Challenges for immigrant health in the USA—the road to crisis. Lancet 2019;393:2168–74. [DOI] [PubMed] [Google Scholar]
- 430.Crenshaw KW. Twenty years of critical race theory: looking back to move forward. Conn Law Rev 2011;43:1253–354. [Google Scholar]
- 431.Witkiewitz K, Greenfield BL, Bowen S. Mindfulness-based relapse prevention with racial and ethnic minority women. Addict Behav 2013;38:2821–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Greenfield BL, Roos C, Hagler KJ, Stein E, Bowen S, Witkiewitz KA. Race/ethnicity and racial group composition moderate the effectiveness of mindfulness-based relapse prevention for substance use disorder. Addict Behav 2018;81:96–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Proulx J Croff R Oken B, et al. Considerations for research and development of culturally relevant mindfulness interventions in American minority communities. Mindfulness (N Y) 2018;9:361–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health 2014;104:e16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med 2008;31:23–33. [DOI] [PubMed] [Google Scholar]
- 436.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol 2003;84:822–48. [DOI] [PubMed] [Google Scholar]
- 437.Carmody J, Baer RA. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. J Clin Psychol 2009;65:627–38. [DOI] [PubMed] [Google Scholar]
- 438.Davidson RJ, Kaszniak AW. Conceptual and methodological issues in research on mindfulness and meditation. Am Psychol 2015;70:581–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Norris CJ, Creem D, Hendler R, Kober H. Brief mindfulness meditation improves attention in novices: evidence from ERPs and moderation by neuroticism. Front Hum Neurosci 2018;12:315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 440.Roos C, Kirouac M, Stein E, Wilson A, Bowen S, Witkiewitz K. An open trial of rolling admission mindfulness-based relapse prevention (Rolling MBRP): feasibility, acceptability, dose-response relations, and mechanisms. Mindfulness (N Y) 2019;10:1062–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.Mohatt NV, Thompson AB, Thai ND, Tebes JK. Historical trauma as public narrative: a conceptual review of how history impacts present-day health. Soc Sci Med 2014;106:128–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Moeini-Jazani M, Knoeferle K, de Molière L, Gatti E, Warlop L. Social power increases interoceptive accuracy. Front Psychol 2017;8:1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.Krieger N. Living and dying at the crossroads: racism, embodiment, and why theory is essential for a public health of consequence. Am J Public Health 2016;106:832–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 444.Quadt L, Critchley HD, Garfinkel SN. The neurobiology of interoception in health and disease. Ann N Y Acad Sci 2018;1428:112–28. [DOI] [PubMed] [Google Scholar]
- 445.Khalsa SS Adolphs R Cameron OG, et al. Interoception and mental health: a roadmap. Biol Psychiatry Cogn Neurosci Neuroimaging 2018;3:501–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 446.van der Kolk BA Stone L West J, et al. Yoga as an adjunctive treatment for posttraumatic stress disorder. J Clin Psychiatry 2014;75:e559–65. [DOI] [PubMed] [Google Scholar]
- 447.Geller S. Cultivation of therapeutic presence: therapeutic drumming and mindfulness practices. Tijdschr Clientgerichte Psychother 2009;47:273–87. [Google Scholar]
- 448.Fancourt D, Perkins R, Ascenso S, Carvalho LA, Steptoe A, Williamon A. Effects of group drumming interventions on anxiety, depression, social resilience and inflammatory immune response among mental health service users. PLoS One 2016;11:e0151136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Travis R, Gann E, Crooke AHD, Jenkins SM. Hip hop, empowerment, and therapeutic beat-making: potential solutions for summer learning loss, depression, and anxiety in youth. J Hum Behav Soc Environ 2019;29:744–65. [Google Scholar]
- 450.Levy I, Emdin C, Adjapong ES. Hip-hop cypher in group work. Soc Work Groups 2018;41:103–10. [Google Scholar]
- 451.Mindful. Hip-hop state of mind. 2020. https://www.mindful.org/hip-hop-state-mind/
- 452.Mindful Life Project. MLP resources. ND. http://mindfullifeproject.org/resources/
- 453.Grasser LR, Al-Saghir H, Wanna C, Spinei J, Javanbakht A. Moving through the trauma: dance/movement therapy as a somatic-based intervention for addressing trauma and stress among Syrian refugee children. J Am Acad Child Adolesc Psychiatry 2019;58:1124–6. [DOI] [PubMed] [Google Scholar]
- 454.Stanek D. Bridging past and present: embodied intergenerational trauma and the implications for dance/movement therapy. Body Mov Dance Psychother 2014;10:94–105. [Google Scholar]
- 455.Wong SYS, Chan JYC, Zhang D, Lee EKP, Tsoi KKF. The safety of mindfulness-based interventions: a systematic review of randomized controlled trials. Mindfulness (N Y) 2018;9:1344–57. [Google Scholar]
- 456.Baer R, Crane C, Miller E, Kuyken W. Doing no harm in mindfulness-based programs: conceptual issues and empirical findings. Clin Psychol Rev 2019;71:101–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.Britton WB. Can mindfulness be too much of a good thing? The value of a middle way. Curr Opin Psychol 2019;28:159–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Grant AM, Schwartz B. Too much of a good thing: the challenge and opportunity of the inverted U. Perspect Psychol Sci 2011;6:61–76. [DOI] [PubMed] [Google Scholar]
- 459.Bent S, Padula A, Avins AL. Brief communication: better ways to question patients about adverse medical events. Ann Intern Med 2006;144:257–61. [DOI] [PubMed] [Google Scholar]
- 460.Treleaven D. Trauma-sensitive mindfulness: practices for safe and transformative healing. Trans Anal J 2018;48:288–90. [Google Scholar]
- 461.Afifi T, Asmundson G, Sareen J. Epidemiology of traumatic events and posttraumatic stress disorder. In: Nutt DJ, Stein MB, Zohar J, eds. Post traumatic stress disorder: diagnosis, management and treatment. Boca Raton, FL: Taylor & Francis, 2009. [Google Scholar]
- 462.Compson J. Meditation, trauma and suffering in silence: raising questions about how meditation is taught and practiced in Western contexts in the light of a contemporary trauma resiliency model. Contemp Buddhism 2014;15:274–97. [Google Scholar]
- 463.Boyd JE, Lanius RA, McKinnon MC. Mindfulness-based treatments for posttraumatic stress disorder: a review of the treatment literature and neurobiological evidence. J Psychiatry Neurosci 2018;43:7–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 464.Polusny MA Erbes CR Thuras P, et al. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. JAMA 2015;314:456–65. [DOI] [PubMed] [Google Scholar]
- 465.Kearney DJ, McDermott K, Malte C, Martinez M, Simpson TL. Effects of participation in a mindfulness program for veterans with posttraumatic stress disorder: a randomized controlled pilot study. J Clin Psychol 2012;69:14–27. [DOI] [PubMed] [Google Scholar]
- 466.Banks K, Newman E, Saleem J. An overview of the research on mindfulness-based interventions for treating symptoms of posttraumatic stress disorder: a systematic review. J Clin Psychol 2015;71:935–63. [DOI] [PubMed] [Google Scholar]
- 467.King AP Erickson TM Giardino ND, et al. A pilot study of group mindfulness-based cognitive therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD). Depress Anxiety 2013;30:638–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 468.Kearney DJ, Malte CA, McManus C, Martinez ME, Felleman B, Simpson TL. loving-kindness meditation for posttraumatic stress disorder: a pilot study. J Trauma Stress 2013;26:426–34. [DOI] [PubMed] [Google Scholar]
- 469.Bormann JE, Oman D, Walter KH, Johnson BD. Mindful attention increases and mediates psychological outcomes following mantram repetition practice in veterans with posttraumatic stress disorder. Med Care 2014;52:S13–8. [DOI] [PubMed] [Google Scholar]
- 470.Herman JL. Posttraumatic stress disorder as a shame disorder. In: Shame in the therapy hour. Dearing RL, Tangney JP, eds. Washington, DC: American Psychological Association, 2011. [Google Scholar]
- 471.Dimidjian S, Segal ZV. Prospects for a clinical science of mindfulness-based intervention. Am Psychol 2015;70:593–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Stein E, Witkiewitz K. Dismantling mindfulness-based programs: a systematic review to identify active components of treatment. Mindfulness (N Y) 2020;25 Jul [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 473.Powell SK. Mindfulness: another tool in the case managers’ toolbox. Prof Case Manag 2014;19:159–60. [DOI] [PubMed] [Google Scholar]
- 474.Van Dam NT van Vugt MK Vago DR, et al. Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect Psychol Sci 2018;13:36–61. [DOI] [PMC free article] [PubMed] [Google Scholar]


