Abstract
Objective: We sought to understand how patients and primary care teams use secure messaging (SM) to communicate with one another by analyzing secure message threads from 2 Department of Veterans Affairs facilities.
Methods: We coded 1000 threads of SM communication sampled from 40 primary care teams.
Results: Most threads (94.5%) were initiated by patients (90.4%) or caregivers (4.1%); only 5.5% were initiated by primary care team members proactively reaching out to patients. Medication renewals and refills (47.2%), scheduling requests (17.6%), medication issues (12.9%), and health issues (12.7%) were the most common patient-initiated requests, followed by referrals (7.0%), administrative issues (6.5%), test results (5.4%), test issues (5.2%), informing messages (4.9%), comments about the patient portal or SM (4.1%), appreciation (3.9%), self-reported data (2.8%), life issues (1.5%), and complaints (1.5%). Very few messages were clinically urgent (0.7%) or contained other potentially challenging content. Message threads were mostly short (2.7 messages), comprising an average of 1.35 discrete content types. A substantial proportion of issues (24.2%) did not show any evidence of being resolved through SM. Time to response and extent of resolution via SM varied by message content. Proactive SM use by teams varied, but was most often for test results (32.7%), medication-related issues (21.8%), medication renewals (16.4%), or scheduling issues (18.2%).
Conclusions: The majority of messages were transactional and initiated by patients or caregivers. Not all content categories were fully addressed over SM. Further education and training for both patients and clinical teams could improve the quality and efficiency of SM communication.
Keywords: personal health records, secure messaging, primary health care, patient-doctor communication, message content
BACKGROUND AND SIGNIFICANCE
Secure messaging (SM), or secure patient-provider e-mail, has been increasingly adopted by health care systems. SM facilitates communication between visits1 and has emerged as a key component of patient-centered care.2–4 The Health Information Technology for Economic and Clinical Health Act of 2009 is driving patient use of SM, a core requirement for Stage 2 Meaningful Use.5
Several large health systems that implemented SM prior to the Health Information Technology for Economic and Clinical Health Act have reported on its impact. Kaiser Permanente found positive impacts on quality of care6,7 and member loyalty,7,8 without significant increases in workload.7 A systematic review revealed moderate evidence that SM was associated with increased patient satisfaction and with glycemic control among patients with diabetes, with weaker evidence for management of other chronic conditions or utilization.9 More information on how patients and providers use SM may yield greater understanding of its potential to have a positive impact.
The Department of Veterans Affairs (VA) provides health care to over 6 million veterans. VA began offering SM in 2008 through My HealtheVet (MHV), its patient portal and personal health record. Since 2011, patients with authenticated MHV accounts can communicate securely online with their primary care providers; subsequently, access has expanded to include specialty care. As of September 2016, over 1.88 million patients had opted in.
SM adoption in the VA system has been facilitated by positive patient attitudes10 and clinician endorsement.11–13 Patients and providers have noted dramatic and positive consequences regarding access, communication, and patient-provider relationships.13,14 Providers cite benefits such as avoiding telephone challenges, user convenience and efficiency, ability to communicate between visits, and greater patient engagement, satisfaction, and trust.13 Patients report high satisfaction with how SM enhances communication.14 However, relatively little is known about how SM is used to communicate and resolve patient requests, especially in a vulnerable population of veterans known to be older and to bear a greater burden of chronic disease and disability.15–17 Previous papers outside the VA have addressed SM content,1,18–25 message length,1,22 readability,26 response timeliness,18,19,27 and fulfillment of patient requests.22 However, most previous studies were limited in scope, addressing 1 or more but not all of the above areas, and were typically far smaller in sample size, usually drawing on data from just 1 site.
As part of a larger VA Central Institution Review Board–approved study examining VA primary care teams’ experiences using SM and its integration into clinical workflow,28 we analyzed SM threads to explore (1) how patients used SM to communicate with primary care teams (ie, message content, length) and (2) how clinical teams responded to patients’ messages (ie, response timeliness, message fulfillment, readability) or proactively reached out via SM.
METHODS
Data
We sampled primary care teams from 2 large, urban VA medical centers in the northeast (Site 1) and northwest (Site 2) United States that had been using SM for at least 5 years and their affiliated community clinics. As part of a larger study of SM-related clinical workflow,28 we sought variation in how SM teams handled messages. Teams determined their preferred workflow; any team member including the provider could open or respond to messages, and teams varied significantly in terms of provider involvement. In general, messages were opened by non-providers and triaged to appropriate team members. All team members were notified when a message “escalated” by not being completed within 3 business days as required. Utilizing administrative statistics, we selected 20 SM teams per facility to represent local heterogeneity based on (1) direct use of SM by the primary care provider (MD or nurse practitioner) on the team, (2) volume of incoming messages, and (3) rates of message “escalation.” At least 1 women’s health care clinic SM team was included per site. To ensure an adequate number of messages for assessment, teams with <100 incoming messages over the previous 5 months were excluded.
We selected 25 threads (strings of related messages) per team for analysis for this paper. Each team’s threads could only be sorted alphabetically or chronologically. To vary the day of the week and time of the month when messages were sent, we alphabetized patient surnames within teams, picking the most recent message sent during our time frame by the first patient whose surname began with each letter of the alphabet. Complete data were obtained for 1000 message threads initiated between January 1 and April 15, 2013. Threads were read carefully to identify cases where a patient had replied to a prior SM instead of composing a new message. In these instances, the most recent string was kept as the thread for analysis.
Coding messages and threads
Messages were characterized at the message level and the thread level for several attributes. All threads were coded for the number of messages per thread, content of messages (content categories, flags for challenging/problematic content), and extent to which the team responded to and resolved patients’ requests within SM. We coded at the message level for sender type, time/date sent, word length, and readability of message.
Message content categories
A preliminary coding scheme for message thread content categories was developed based on the “taxonomy of requests by patients.”29,22,25 This taxonomy, previously applied to SM content,24 was used as the basis of categorizing not only message content (eg, tests, appointments, specialty provider referrals) but also how the clinical team responded to and resolved patient issues, described below. Both domains of message content and message resolution were further modified based on research about secure e-mail,30,31 the study team’s personal experiences with SM, and in-depth qualitative interviews with 8 primary care teams (part of the larger study).28 A small number of threads and messages were iteratively coded by 2 trained researchers; questions and discrepancies were brought to the full team, which met weekly to develop and refine the coding categories. Final content categories and illustrative examples are shown in Table 1.
Table 1.
Message content categories
| Message content code | Description of content area | Example of type of message |
|---|---|---|
| Health issues | Physical or mental health problem or concern not coded as a medication issue or test issue | “My right shoulder has been extremely sore for more than a month. I can't lift my right arm up and to the side without great pain. This has been over a month and is getting worse.” |
| Medication renewal or refill | Request for refill or renewal of a medication or medical supply | “Please renew my prescription to oxycodone HCL 5 mg tab. Please have pharmacy mail to me.” |
| Medication issue | Medication or supply issue that is not a refill/renew request or a problem with receiving the medication in mail (eg, questions about dose or side effects) | “I’m sending a list of vitamins and supplements I take. Please have the doctor make sure they are OK to take, and don’t counteract what I take for my Parkinsons.” |
| Test issue | Patient questions about testing, choosing among testing options, why a test is important, preparing for a test, requesting a test | “Did you want me to get lab work done before I see you?” |
| Test result | Request for or discussion of test results | “Thanks for sending me the test results. I still have a question for the doctor about the numbers that you gave me.” |
| Self-reporting | Patient-reported readings or measurements (eg, blood pressure or blood glucose levels) | “Blood pressure at this time is 110/64.” |
| FYI informing | Patient sharing information “for your information (FYI)” with no additional discussion and does not fit other category (eg, inform about non-VA care or test result) | “Just to keep you posted. EKG done yesterday. Blood work & urine done this AM.” |
| Scheduling | Schedule an appointment, test, or procedure | “I would like to set up an appointment for a physical.” |
| Referral | Request referral to a specialist | “I would like to be referred to MOVE! to help me with some weight loss. I also need you to set up an appointment for my knees and lower back. I’m having a great deal of pain in both, been injured in the past. Thank you.” |
| Administrative | Administrative issues other than appointment scheduling | “I didn’t receive my medication in the mail.” |
| Life issue | Any contextual issues that are not strictly biomedical and are about the patient’s life context | “We’re having lots of changes with my mom. Hospice people are coming here but now they’re talking about putting her in a nursing home. They say they can help her all the time.” |
| MHV/SM technology-related | Issues related to My HealtheVet or secure messaging technology | “Can I access my blood test results using this software (My HealtheVet)?” |
| Appreciation | Expressing appreciation beyond a simple thank you | “I do want to take a minute to thank you for your help. It is a different world going through a pain-free day. You have been kind and caring and I do really appreciate it!!!” |
| Complaint | Complaining about care, services, MHV, etc. | “First and foremost…and I would think you would be aware of this by now, [patient first name] is NOT my Dad…he's my husband.” |
| Other | Content not captured by the above categories | “Both of my accu-chek meters are reading E-9 when trying to get a reading. I think it's the battery, but I don't know how to fix it. Tell me how or what to do.” |
Threads were coded for multiple applicable content categories. For the category of health issue, we coded multiple health issues if they were raised in the same message thread. Message content was viewed and categorized from the perspective of the patient sender. For example, a patient request for referral to an orthopedic specialist for a joint symptom was coded as an appointment request rather than a health issue.
Potentially challenging or problematic messages
In addition to being coded for content, patient messages were flagged for being nonclinical (social communication unrelated to medical care), confusing (rambling, nonsensical), sensitive (personally sensitive content such as sexual issues or domestic violence), urgent (acute health issue of sufficient severity that there was the potential that lack of timely medical attention would be life-threatening or would result in harm), or containing offensive language (verbal abuse, swearing, threats). These categories were identified as being potentially problematic or challenging to address during interviews with primary care teams.28
Resolution using SM
All messages in threads were examined to assess the degree to which the health care team used SM to address the issues raised by patients/caregivers. For each content category present, the issue or request was coded as fully addressed, partially addressed, acknowledged, or having no evidence of being resolved through SM. We noted if a patient message was forwarded to another team member or if the team indicated that further communication should be expected by SM or by phone.
Sender type
Each message was coded for the sender type: patient, caregiver, primary care provider (physician or nurse practitioner), registered nurse, licensed practical nurse, medical assistant or health technologist, pharmacist, other provider, or other nonprovider.
Time/date sent
For each thread, we counted the total number of individual messages and recorded the date and time of each message. The total number of hours from the first message to the first team reply was recorded, as was the total number of hours from the first to last message in the thread. If resolution did not happen through SM, that thread was excluded from the calculation. We also examined variations in time of thread initiation (during weekday clinic hours, weeknight [evening before a weekday], and weekend) and whether messages were responded to within 3 days as expected.
Message length and readability
Microsoft Word was used to calculate word count (excluding message headers and signature blocks) and readability for each message. The Flesch Reading Ease Score, from 0 (very difficult and confusing) to 100 (very easy to understand), was calculated for all messages. A period was added at the end of the text when none was present to enable calculating a score. A score of 60–70 represents text that is readily understood by 8th- to 9th-grade students. For each thread, we calculated the mean readability score for patient/caregiver messages and for team messages. For each thread with at least 1 message from a patient/caregiver and 1 or more from a team member, we calculated a difference score to examine within-thread differences in readability.
Interrater reliability
Two coders initially jointly coded threads while refining the coding dictionary. Then, after separately coding 40 of the same threads (122 messages), we calculated the percent of absolute agreement between the coding of all message content variables, as well as Cohen’s κ. Coders achieved 92.5–100% agreement on all content categories, with Cohen’s κ showing substantial (κ > 0.61) or almost perfect (κ > 0.81) agreement32,33 for all, except characterization of patient health issues (Cohen’s κ = 0.46). Once the coders achieved acceptable interrater reliability, they coded separately, consulting each other or the principal investigator as needed.
Data entry and analysis
Coded data were entered into an Access database via an Infopath form. Univariate statistics for each categorization were calculated overall and by site. Fisher’s exact test was used to detect differences in the distribution of categorizations across sites. Paired t test was used to test for within-thread differences in readability of patient/caregiver and team messages. All analyses were performed using SAS version 9.3 (Cary, NC, USA).
RESULTS
Thread length and message senders
The 1000 threads in the study contained a total of 2715 messages, and threads ranged in length from 1 to 10 messages (mean 2.7), with 61.5% of threads completed in 2 messages and 89.43% of threads completed in 4 messages or fewer. In all, 94.5% of threads were initiated by patients (N = 904) or family caregivers on behalf of patients (N = 41), and 5.5% (N = 55) of threads were initiated by primary care teams. Overall, 53.2% of all messages were sent by patients, 12.5% by registered nurses, 11.9% by licensed practical nurses, 10.5% by MDs, 6.1% by medical assistants or health techs, 2.5% by family members/caregivers, 1.2% by pharmacists, 1.0% by nurse practitioners, and 0.4% by other providers. Figure 1 shows who was involved in sending and responding to messages from patient accounts and primary care teams.
Figure 1.
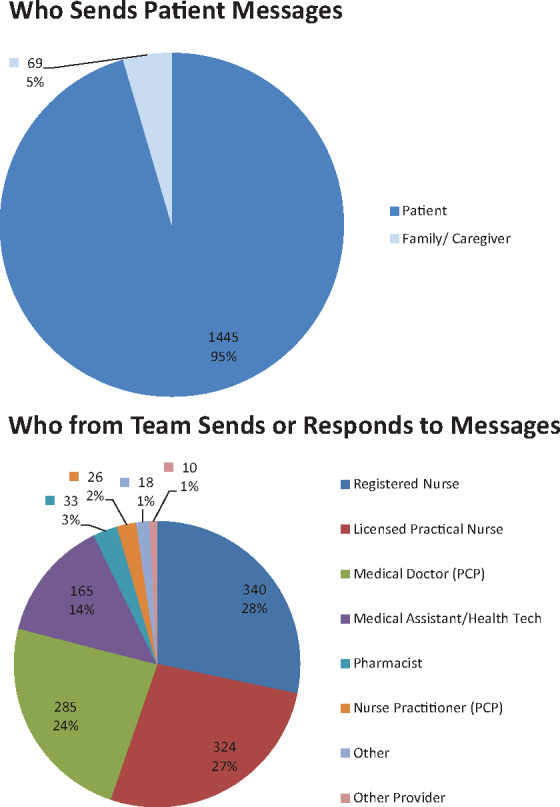
Percentage of messages by sender type.
Message content
Table 2 contains information on the content of threads initiated by patients or caregivers (N = 945 threads). Overall, a majority of messages were focused on medication renewal/refill requests (47.2% of threads), scheduling issues (17.6%), medication issues unrelated to renewals/refills (12.9%), and health issues (12.7%). Among the messages containing questions about health issues, the majority (91.1%) contained only 1 health issue (mean 1.11 health issues/thread), with a maximum of 3 health issues. Patients also used SM to request referrals (7.0%), address administrative concerns (6.5%), request or discuss test results (5.4%), ask about testing issues (5.2%), inform their clinical teams about relevant information (denoted “FYI,” or for your information) (4.9%), ask about MHV or SM (4.1%), communicate their appreciation to the clinical team (3.9%), self-report health data (2.8%), or offer a complaint (1.5%). The majority of messages (71.6%) contained only 1 of the above content types, 22.5% contained 2 types, 4.7% contained 3 types, and 1.2% contained 4 or 5 types.
Table 2.
Content of patient- or caregiver-initiated message threads
| Message content categories | Overall (N = 945) |
Site 1 (N = 461) |
Site 2 (N = 484) |
Difference between sites |
||||
|---|---|---|---|---|---|---|---|---|
| N (%) of messages with content | Mean hours to first reply | N (%) of messages with content | Mean hours to first reply | N (%) of messages with content | Mean hours to first reply | Message content (Fisher’s exact test) | Time to first reply(t test) | |
| Medication renewal or refill | 446 (47.2) | 28.0 | 221 (47.9) | 19.3 | 225 (46.5) | 37.1 | 0.6958 | <.0001 |
| Scheduling | 166 (17.6) | 19.7 | 113 (24.5) | 15.7 | 53 (11.0) | 29.1 | <.0001 | 0.0020 |
| Medication issue | 122 (12.9) | 38.5 | 49 (10.6) | 37.8 | 73 (15.1) | 38.9 | 0.0421 | 0.9472 |
| Health issue | 120 (12.7) | 28.9 | 33 (7.2) | 19.9 | 87 (18.0) | 33.2 | <.0001 | 0.0764 |
| Referral | 66 (7.0) | 31.4 | 43 (9.3) | 25.5 | 23 (4.8) | 42.3 | 0.0070 | 0.0931 |
| Administrative | 61 (6.5) | 34.4 | 23 (5.0) | 27.6 | 38 (7.9) | 38.4 | 0.0851 | 0.2886 |
| Test result | 51 (5.4) | 28.0 | 22 (4.8) | 11.0 | 29 (6.0) | 40.1 | 0.4721 | 0.0404 |
| Test issue | 49 (5.2) | 36.9 | 27 (5.9) | 44.4 | 22 (4.5) | 27.1 | 0.3819 | 0.6260 |
| FYI informing | 46 (4.9) | 25.1 | 22 (4.8) | 22.2 | 24 (5.0) | 28.2 | 1.0000 | 0.5195 |
| My HealtheVet/ SM-related | 39 (4.1) | 27.1 | 26 (5.6) | 15.4 | 13 (2.7) | 52.9 | 0.0322 | 0.0007 |
| Appreciation | 37 (3.9) | 22.1 | 30 (6.5) | 14.7 | 7 (1.4) | 49.8 | <.0001 | 0.0029 |
| Self-reporting | 26 (2.8) | 24.9 | 17 (3.7) | 14.4 | 9 (1.9) | 53.0 | 0.1108 | 0.0207 |
| Life issue | 14 (1.5) | 21.6 | 10 (2.2) | 9.5 | 4 (0.8) | 130.3 | 0.1084 | <.0001 |
| Complaint | 14 (1.5) | 28.8 | 11 (2.4) | 26.7 | 3 (0.6) | 38.2 | 0.0303 | 0.6818 |
| Other | 14 (1.5) | 15.0 | 12 (2.6) | 12.5 | 2 (0.4) | 34.9 | 0.0059 | 0.2956 |
As shown in Table 2, patients at both sites had similar rates of SM use for medication renewals/refills, test issues, test results, FYI, administrative requests, and self-reporting. There were significant differences in SM use for other purposes. Site 1 patients were significantly more likely to use SM for scheduling, referral requests, communication regarding SM or the MHV portal, appreciation, complaints, or sending other types of messages. Patients at Site 2 were more likely to use SM to raise health issues with their clinical teams and raise medication issues.
Very few messages initiated by patients contained clinically urgent content (0.7%), offensive or threatening language (0.2%), or nonclinical (2.2%), confusing (1.6%), or sensitive topics (0.7%) (Table 3). Patients at Site 1 were more likely to send nonclinical messages (P < .0001) and marginally more likely to send urgent or confusing messages (P = .0633 and .0688, respectively). Urgent messages included concerns about rapid weight change in a cardiac patient, rapid weight change related to a new prescription, shortness of breath related to a new medication, hematuria, and an urgent mental health issue, and one patient wrote to follow up on an urgent care visit after being instructed to go to the emergency department instead.
Table 3.
Frequency of potentially challenging or problematic secure message content in patient/caregiver-initiated threads
| Type of content | Description | Overall, N = 945 (%) | Site 1, N = 461(%) | Site 2, N = 484 (%) | Fisher's exact test for site differences |
|---|---|---|---|---|---|
| Urgent | Health issues or content of sufficient severity that absence of immediate medical attention could be life-threatening or cause serious harm to patient (eg, shortness of breath) | 7 (0.7) | 6 (1.3) | 1 (0.2) | 0.0633 |
| Offensive language | Verbal abuse, swearing, threatening | 2 (0.2) | 0 (0.0) | 2 (0.4) | 0.4998 |
| Nonclinical | Sharing nonclinical information (not including life issues that could affect daily living, such as transportation) | 21 (2.2) | 20 (4.3) | 1 (0.2) | <0.0001 |
| Confusing | Rambling, nonsensical; stream of consciousness or unclear | 15 (1.6) | 11 (2.4) | 4 (0.8) | 0.0688 |
| Sensitive | Personally sensitive content such as sexual issues, substance use, domestic violence | 7 (0.7) | 3 (0.7) | 4 (0.8) | 1.0000 |
Length and readability of secure messages
On average, messages were short and became shorter as the thread progressed. The mean word count was 61.8 words for the first message in a thread, 35.8 words for the second, 34.3 for the third, and 36.3 for the fourth, with subsequent messages getting progressively shorter and averaging 18–35 words.
The average Flesch Reading Ease Score was 72.25 (SD 17.99) for patient and caregiver messages and 72.20 (SD 18.17) for clinical team messages. Overall, the average message was written at a 7th-grade reading level. There were 868 threads that included both patient/provider and team messages. The mean within-thread difference in readability was 0.04 (SD 24.9), and the difference score was normally distributed, indicating that threads were roughly equal regarding whether the patient/caregiver message had the higher or lower readability score. Paired t tests failed to detect a significant patient/caregiver team difference in readability (P = .9601). There were also no differences across sites in readability.
Message resolution within SM and response time
Overall, message resolution within SM ranged from 86.3% of requests for test results being fully addressed to only 41.3% of threads containing informing communication being fully addressed by the team (see Table 4 for complete results). The content categories least likely to be resolved within SM were life issues (57.1% with unknown resolution), complaints (42.9%), informing messages (39.1%), self-reporting messages (38.5%), appreciative messages (37.8%), and health issues (31.7%). The only significant difference between sites was in the resolution of patient requests for medication renewal/refill. Patients at Site 1 were significantly less likely (8.1% at Site 1 vs 13.3%, P < .0001) to not receive confirmation of their renewal/refill through SM.
Table 4.
Message resolution within SM by message content category
| Message content | Overall (N = 945) |
||||
|---|---|---|---|---|---|
| N and percentage of patient-initiated messages | Message resolution |
||||
| Fully addressed | Partially addressed | Acknowledged | None/Don’t Know | ||
| Medication renew or refill | 446 (47.2) | 350 (78.5) | 47 (10.5) | 1 (0.2) | 48 (10.8) |
| Scheduling | 166 (17.6) | 130 (78.8) | 12 (7.3) | 0 (0.0) | 23 (13.9) |
| Medication issue | 122 (12.9) | 79 (64.8) | 17 (13.9) | 1 (0.8) | 25 (20.5) |
| Health issue | 120 (12.7) | 68 (56.7) | 12 (10.0) | 2 (1.7) | 38 (31.7) |
| Referral | 66 (7.0) | 51 (77.3) | 7 (10.6) | 1 (1.5) | 7 (10.6) |
| Administrative | 61 (6.5) | 48 (78.7) | 3 (4.9) | 0 (0.0) | 10 (16.4) |
| Test result | 51 (5.4) | 44 (86.3) | 3 (5.9) | 0 (0.0) | 4 (7.8) |
| Test issue | 49 (5.2) | 41 (83.7) | 4 (8.2) | 0 (0.0) | 4 (8.2) |
| FYI informing | 46 (4.9) | 19 (41.3) | 7 (15.2) | 2 (4.3) | 18 (39.1) |
| MHV/SM/technology-related | 39 (4.1) | 30 (76.9) | 0 (0.0) | 0 (0.0) | 8 (20.5) |
| Appreciation | 37 (3.9) | 23 (62.2) | 0 (0.0) | 0 (0.0) | 14 (37.8) |
| Self-reporting | 26 (2.8) | 15 (57.7) | 0 (0.0) | 1 (3.8) | 10 (38.5) |
| Life issue | 14 (1.5) | 6 (42.9) | 0 (0.0) | 0 (0.0) | 8 (57.1) |
| Complaint | 14 (1.5) | 8 (57.1) | 0 (0.0) | 0 (0.0) | 6 (42.9) |
| Other | 14 (1.5) | 7 (50.0) | 0 (0.0) | 1 (7.1) | 6 (42.9) |
On average, messages tended to receive an initial response within 24 h if they expressed appreciation (mean time to first response, 22.1 h), discussed life issues (21.6 h), made scheduling requests (19.7 h), or fit no other common categories (15.0 h). Messages related to self-reporting (mean 24.9 h), informing (25.1 h), MHV or SM (27.1 h), test results (28.0 h), medication refills/renewals (28.0 h), health issues (28.9 h), referral requests (31.4 h), or complaints (28.8 h) were generally first answered between 24 and 36 h. Only questions about test issues (36.9 h), administrative issues (34.4 h), and medication issues (38.5 h) took longer to receive an initial response. The vast majority of threads (96.5%) met the VA requirement for an initial response within 3 business days, although this varied slightly by site (99.3% at Site 1, 93.6% at Site 2). Messages containing life issues (10.0% escalation) and health issues (7.8%) were most likely to escalate.
The average time until the patient’s issue or request was resolved (ie, hours from start to finish for a thread in which the request was acknowledged and partially or fully addressed, excluding messages with no evidence of response within SM) varied more significantly by content category. Mean time to resolution ranged from a high average of 82.5 h for medication issues to a low of 15.3 h for messages that did not fit any other category. Almost all content categories had a mean completion time <72 h, with the exception of questions related to medications (82.5 h to completion) or complaints (81.0 h to completion). The majority of threads (87%) were resolved within 3 business days. Figure 2 shows how time to initial response and resolution varied by message content category.
Figure 2.
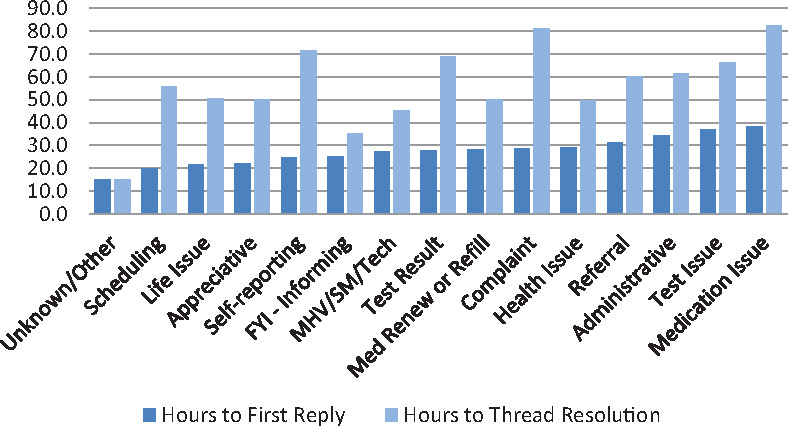
Mean hours (including evenings, holidays, and weekends) from patient message to first response and to thread resolution by message type (only messages fully resolved, partially resolved, or acknowledged within SM are included).
Message timing
The majority of threads (N = 586) were initiated during clinic hours (7 a.m. to 5 p.m.), whereas the rest were sent on weeknights (5 p.m. to 7 a.m. the night before a weekday, N = 260) or weekends (5 p.m. on Friday to 5 p.m. on Sunday, N = 154). The average patient waiting time for a first reply for threads initiated during clinic hours (25.8 h) or on a weeknight (27.8 h) was shorter than for threads begun over a weekend (58.1 h).
Primary care team–initiated messages
Only 55 out of 1000 threads were initiated by a clinical team member. Most of these messages were to report test results (32.7%) or to address a medication-related issue (21.8%), a medication renewal (16.4%), or a scheduling issue (18.2%). There was significant site-level variation: the majority of Site 1 messages were to deliver test results, whereas Site 2 did not initiate SM for test results at all. The reverse was true for administrative messages initiated by the clinical team (0% of Site 1 messages vs 25.0% of Site 2 messages).
DISCUSSION
This study sought to characterize how SM is used by patients and primary care teams in the context of a large, integrated health care system.
Almost all message threads (94.5%) were initiated by patients or their delegates. Caregivers sent 2.5% of messages and initiated 4.1% of threads. While MHV does not yet allow a patient to delegate access to a family member or caregiver, some patients appear to have already authorized caregivers to communicate with their clinical teams on their behalf.
The most common patient messages were transactional, focusing on medication renewal/refill requests (47.2% of threads), scheduling, referral, and administrative issues. A notable portion of messages addressed medication (12.9%) and health (12.7%) issues, suggesting that SM could potentially substitute for some telephone or in-person encounters. A prior VA study14 found that important factors in patient use of SM were convenience and easy communication with a health care team 24/7 without needing to repeatedly convey personal health issues during the telephone triage process. Patients perceived SM as preventing unnecessary visits and enabling communication on sensitive topics that can be embarrassing to discuss.14
The average thread contained 2.7 messages, with nearly two-thirds of exchanges being completed after a single reply from the health care team. This is similar to reports outside of VA7 finding that most threads comprise 2–4 messages. Messages were also fairly short, on average. Although this study was not designed to capture team workload, other studies have reported that primary care teams receive a mean 4.8 patient messages daily,7 or 18.9 messages per 100 patients per month,34 with an average time of 2.3 min for physicians to respond.35 It is still unknown whether time spent on SM is offset by reductions in other work, such as telephone calls with patients.36 Future research should study the impact on clinical workload and explore possible time savings from using SM in lieu of telephone calls or visits.
Patient use of SM for urgent medical issues is a provider concern, as messages may not be immediately read. A study of 16 physician “super users” of secure e-mail at Kaiser Permanente and Group Health revealed that 31% identified misuse of e-mail for urgent conditions as a concern.37 Another study found that 3.5% of messages contained urgent clinical content. In our study, only 0.7% of patient-initiated messages contained content deemed clinically urgent in nature. While the SM application informs patients not to use it for urgent issues, more prominent warnings and enhanced patient education regarding contacting health care teams for any acute symptoms may be warranted.
A potential concern regarding the use of SM by health care teams is that messages may be written at a level too difficult for patients with low literacy to understand. Our results suggest this was not the case; messages at both study sites were written at the 7th-grade level and clinicians’ responses matched the readability of patient messages. Observed readability in this study was similar to that reported from an analysis of SM at a safety net clinic, where readability of clinical team messages was also well matched to patient messages.38
Within the VA system, the expectation is that messages from patients will be responded to and completed within 3 business days, and 96.5% of threads met that expectation. The majority of messages received a first response in under 48 h, and the mean time to completion was under 72 h for most message categories.
Messages in certain categories were often not fully or partially addressed using SM. Previous work outside of VA also found 11% of SM with no known outcome.24 In some cases, health care team members may have felt that a message did not require a response (eg, self-reporting or FYI informing messages). In other cases, clinicians may have perceived that a patient message demanded telephone outreach or that a call would facilitate obtaining the necessary clinical details to more quickly determine the appropriate course of action (eg, for an acute health issue). This study evaluated the use of SM communication only, and did not examine electronic health record (EHR) documentation of telephone contact. Future studies should examine how often patients receive telephone responses to their messages, and how often patient issues communicated by SM are fully resolved via other channels. However, it also appears that in many instances of less complex messages, health care team members may not optimize the use of SM by responding directly and completely to patients. Further training for clinical team members could improve the utility of SM in at least some cases.
Few message threads (5.5% overall) were initiated by health care team members. This is lower than in other systems, where primary care teams have initiated at least 11% of SM threads39 and leveraged SM for system-generated appointment reminders or test results.7 Clearly, there is much potential for clinical teams to leverage SM and enhance communication with patients between visits, improving the quality and efficiency of upcoming clinic visits through pre-visit planning or medication reconciliation.40 Prior research suggests that patients are far more likely to adopt SM if their providers support and use online communication,41,42 and proactive use is one way to communicate that to patients. Currently, SM is not fully integrated into the EHR, requiring a separate login process. Future integration of SM into the EHR and a new workload credit for SM are expected to improve provider adoption.
Limitations
At the time this study was conducted, both sites had been using SM for approximately 5 years. However, compared with some other systems in 2013, SM adoption and volume were still low and some patients and teams were recent adopters. It is possible that message content and resolution, including rates of problematic use, may evolve over time based on user characteristics and experience and should be monitored over time.
Teams were selected to represent within-site variations in provider engagement in SM, message volume, and triage practices and are not necessarily representative of the average SM team. Provider or primary care team engagement with SM may shape patient adoption and the types of messages patients are encouraged to send. This may account for some of the site-level differences in the content and volume of nonclinical messages, as well as in how messages are resolved. Future work should examine how organizational and contextual factors impact SM use.
CONCLUSION
While patients’ SM content was similar at 2 VA sites, we observed some differences in response time by primary care teams and the level of resolution for similar types of issues. Significant team- and facility-level variation in how SM is used suggests room for improvement in effective triaging of messages, quality of responses to patients, and proactive use of SM to improve communication and continuity between visits. Patient SM templates for certain message types (eg, health issues) may help improve timely, full resolution of requests by encouraging the inclusion of relevant clinical details. Improved patient training may further prevent use of SM for potentially urgent problems.
Funding
This research was funded by VA QUERI RRP 11-409 and by VA Career Development Award CDA10-210 to SLS.
Competing interests
None.
Contributors
All authors contributed to the data collection and/or analysis and the writing of this manuscript.
ACKNOWLEDGMENTS
We would like to acknowledge the support of Kim Nazi, PhD, from the Veterans and Consumer Health Informatics Office for facilitation of this research. We would like to acknowledge the many contributions of Erin Schwartz, PhD, to the overall study.
References
- 1. Roter DL, Larson S, Sands DZ, Ford DE, Houston T. Can e-mail messages between patients and physicians be patient-centered? Health Commun. 2008;231:80–86. [DOI] [PubMed] [Google Scholar]
- 2. Ralston JD, Martin DP, Anderson ML et al. Group health cooperative's transformation toward patient-centered access. Med Care Res Rev. 2009;666:703–24. [DOI] [PubMed] [Google Scholar]
- 3. Hogan TP, Wakefield B, Nazi KM, Houston TK, Weaver FM. Promoting access through complementary eHealth technologies: recommendations for VA's Home Telehealth and personal health record programs. J Gen Intern Med. 2011;26 (Suppl 2):628–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen C, Garrido T, Chock D, Okawa G, Liang L. The Kaiser Permanente Electronic Health Record: transforming and streamlining modalities of care. Health Aff (Millwood). 2009;282:323–33. [DOI] [PubMed] [Google Scholar]
- 5. Kruse CS, Argueta DA, Lopez L, Nair A. Patient and provider attitudes toward the use of patient portals for the management of chronic disease: a systematic review. J Med Internet Res. 2015;172:e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhou YY, Kanter MH, Wang JJ, Garrido T. Improved quality at Kaiser Permanente through e-mail between physicians and patients. Health Aff (Millwood). 2010;297:1370–75. [DOI] [PubMed] [Google Scholar]
- 7. Garrido T, Meng D, Wang JJ, Palen TE, Kanter MH. Secure e-mailing between physicians and patients: transformational change in ambulatory care. J Ambul Care Manage. 2014;373:211–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Turley M, Garrido T, Lowenthal A, Zhou YY. Association between personal health record enrollment and patient loyalty. Am J Manag Care. 2012;187:e248–53. [PubMed] [Google Scholar]
- 9. Goldzweig CL, Towfigh AA, Paige NM et al. Systematic Review: Secure Messaging Between Providers and Patients, and Patients' Access to Their Own Medical Record: Evidence on Health Outcomes, Satisfaction, Efficiency, and Attitudes. VA Evidence-based Synthesis Program #05-226 Washington, DC: Department of Veterans Affairs (US); 2012. [PubMed] [Google Scholar]
- 10. Haun JN, Lind JD, Shimada SL, Simon SR. Evaluating Secure Messaging from the Veteran Perspective: Informing the Adoption and Sustained Use of a Patient-Driven Communication Platform. Ann Anthropol Pract. 2013;372:57–74. [Google Scholar]
- 11. Weppner WG, Ralston JD, Koepsell TD et al. Use of a shared medical record with secure messaging by older patients with diabetes. Diabetes Care. 2010;3311:2314–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kittler AF, Carlson GL, Harris C et al. Primary care physician attitudes towards using a secure web-based portal designed to facilitate electronic communication with patients. Inform Prim Care. 2004;123:129–38. [DOI] [PubMed] [Google Scholar]
- 13. Nazi KM. The personal health record paradox: health care professionals' perspectives and the information ecology of personal health record systems in organizational and clinical settings. J Med Internet Res. 2013;154:e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Haun JN, Lind JD, Shimada SL et al. Evaluating user experiences of the secure messaging tool on the Veterans Affairs patient portal system. J Med Internet Res. 2014;163:e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Halzack NM, Miller TR. Patients Cared for by the Veterans Health Administration Present Unique Challenges to Health Care Providers. American Society of Anesthesiologists Health Policy Research Policy Brief. 2014;23:1–4. [Google Scholar]
- 16. Eibner C, Krull H, Brown KM et al. Current and projected characteristics and unique health care needs of the patient population served by the Department of Veterans Affairs. Rand Health Quart. 2016;54:13. [PMC free article] [PubMed] [Google Scholar]
- 17. Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;16021:3252–57. [DOI] [PubMed] [Google Scholar]
- 18. Serrato CA, Retecki S, Schmidt DE. MyChart: a new mode of care delivery. 2005 Personal Health Link Research Report. Permanente J. 2007;112:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. North F, Crane SJ, Stroebel RJ, Cha SS, Edell ES, Tulledge-Scheitel SM. Patient-generated secure messages and eVisits on a patient portal: are patients at risk? J Am Med Inform Assoc. 2013;206:1143–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. White CB, Moyer CA, Stern DT, Katz SJ. A content analysis of e-mail communication between patients and their providers: patients get the message. J Am Med Inform Assoc. 2004;114:260–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Leong SL, Gingrich D, Lewis PR, Mauger DT, George JH. Enhancing doctor-patient communication using email: a pilot study. J Am Board Family Pract. 2005;183:180–88. [DOI] [PubMed] [Google Scholar]
- 22. Sittig DF. Results of a content analysis of electronic messages (email) sent between patients and their physicians. BMC Med Inform Decis Mak. 2003;3:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cronin RM, Fabbri D, Denny JC, Jackson GP. Automated classification of consumer health information needs in patient portal messages. AMIA Annu Symp Proc. 2015;2015:1861–70. [PMC free article] [PubMed] [Google Scholar]
- 24. Mirsky JB, Tieu L, Lyles C, Sarkar U. A mixed-methods study of patient-provider e-mail content in a safety-net setting. J Health Commun. 2016;211:85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lin CT, Wittevrongel L, Moore L, Beaty BL, Ross SE. An Internet-based patient-provider communication system: randomized controlled trial. J Med Internet Res. 2005;74:e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mirsky JB, Tieu L, Lyles C, Sarkar U. Readability assessment of patient-provider electronic messages in a primary care setting. J Am Med Inform Assoc. 2016;231:202–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rohrer JE, North F, Angstman KB, Oberhelman SS, Meunier MR. Timely response to secure messages from primary care patients. Qual Manag Health Care. 2013;222:161–66. [DOI] [PubMed] [Google Scholar]
- 28. Ozkaynak M, Johnson S, Shimada S et al. Examining the multi-level fit between work and technology in a secure messaging implementation. AMIA Annu Symp Proc. 2014;2014:954–62. [PMC free article] [PubMed] [Google Scholar]
- 29. Kravitz RL, Bell RA, Franz CE. A taxonomy of requests by patients (TORP): a new system for understanding clinical negotiation in office practice. J Fam Pract/ 1999;4811:872–78. [PubMed] [Google Scholar]
- 30. Byrne JM, Elliott S, Firek A. Initial experience with patient-clinician secure messaging at a VA medical center. J Am Med Inform Assoc. 2009;162:267–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tang PC, Black W, Young CY. Proposed criteria for reimbursing eVisits: content analysis of secure patient messages in a personal health record system. AMIA Annu Symp Proc. 2006:764–68. [PMC free article] [PubMed] [Google Scholar]
- 32. Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;375:360–63. [PubMed] [Google Scholar]
- 33. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;331:159–74. [PubMed] [Google Scholar]
- 34. Crotty BH, Tamrat Y, Mostaghimi A, Safran C, Landon BE. Patient-to-physician messaging: volume nearly tripled as more patients joined system, but per capita rate plateaued. Health Aff (Millwood). 2014;3310:1817–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kummervold PE, Johnsen JA. Physician response time when communicating with patients over the Internet. J Med Internet Res. 2011;134:e79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Liederman EM, Lee JC, Baquero VH, Seites PG. Patient-physician web messaging. The impact on message volume and satisfaction. J Gen Intern Med. 2005;201:52–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Johnson LW, Garrido T, Christensen K, Handley M. Successful practices in the use of secure e-mail. Permanente J. 2014;183:50–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mirsky JB, Tieu L, Lyles C, Sarkar U. Readability assessment of patient-provider electronic messages in a primary care setting. J Am Med Inform Assoc. 2016;231:202–06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ralston JD, Rutter CM, Carrell D, Hecht J, Rubanowice D, Simon GE. Patient use of secure electronic messaging within a shared medical record: a cross-sectional study. J Gen Intern Med. 2009;243:349–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Heyworth L, Paquin AM, Clark J et al. Engaging patients in medication reconciliation via a patient portal following hospital discharge. J Am Med Inform Assoc. 2014;21(e1):e157–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wade-Vuturo AE, Mayberry LS, Osborn CY. Secure messaging and diabetes management: experiences and perspectives of patient portal users. J Am Med Inform Assoc. 2013;203:519–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lyles CR, Sarkar U, Ralston JD et al. Patient-provider communication and trust in relation to use of an online patient portal among diabetes patients: The Diabetes and Aging Study. J Am Med Inform Assoc. 2013;206:1128–31. [DOI] [PMC free article] [PubMed] [Google Scholar]


