Abstract
To reduce the risk of wrong-patient errors, safety experts recommend limiting the number of patient records providers can open at once in electronic health records (EHRs). However, it is unknown whether health care organizations follow this recommendation or what rationales drive their decisions. To address this gap, we conducted an electronic survey via 2 national listservs. Among 167 inpatient and outpatient study facilities using EHR systems designed to open multiple records at once, 44.3% were configured to allow ≥3 records open at once (unrestricted), 38.3% allowed only 1 record open (restricted), and 17.4% allowed 2 records open (hedged). Decision-making centered on efforts to balance safety and efficiency, but there was disagreement among organizations about how to achieve that balance. Results demonstrate no consensus on the number of records to be allowed open at once in EHRs. Rigorous studies are needed to determine the optimal number of records that balances safety and efficiency.
Keywords: electronic health records, health information technology, wrong-patient errors, patient safety
INTRODUCTION
The use of health information technology has grown dramatically in the United States over the past decade, with more than 4000 hospitals1 and nearly 600 000 ambulatory care providers2,3 using electronic health record (EHR) systems when caring for patients. Many EHR vendors design systems that can be configured to open multiple patient records at a time to enable users to work efficiently when providing care for more than 1 patient concurrently. However, reports of wrong-patient errors within EHR systems4–9 have led health information technology safety experts to recommend limiting the number of patient records providers can open to 1 at a time.10–13 It is unknown whether health care organizations follow this recommendation or what rationales may drive their decisions. To address this gap, we conducted a national survey via the American Medical Informatics Association and the Association of Medical Directors of Information Systems listservs.
METHODS
Data collection
The aims of the survey were to determine the maximum number of patient records organizations configured their EHRs to allow open at once and describe the rationales for making these decisions. In March 2014, we posted an electronic survey on the American Medical Informatics Association and Association of Medical Directors of Information Systems listservs, followed by 3 reminders posted throughout the month. Respondents were asked the following: (1) to identify their EHR vendor, (2) to specify the current number of records their organization’s EHR was configured to allow a single user to open at once, and (3) to provide the rationale for their decision. Questions were asked for both inpatient and outpatient EHR systems. The survey also asked for organization characteristics. For the question “What is the current number of records your [inpatient, outpatient] EHR is configured to allow opened at once?” responses were selected using a dropdown list and included 1, 2, 3, 4, 5, more than 5, and not applicable (do not use EHR). Responses to all other questions were free text.
Analysis
Because we expected that some organizations utilized different EHR systems in inpatient and outpatient facilities, we used the study facility as the unit of analysis. An organization was represented once in the analysis but may have reported on an inpatient EHR, outpatient EHR, or both. We defined the vendor-designed maximum as the maximum number of records that an EHR system was capable of opening, and the organization-configured maximum as the current number of records chosen by the organization to allow users to open concurrently in the EHR. As some EHR systems allow only 1 record open by design, we excluded from the analysis systems not capable of opening multiple records at once. We categorized the organization-configured maximum number of records allowed open as 1 (“restricted”), 2 (“hedged”), or ≥3 (“unrestricted”) and calculated frequencies overall and for inpatient and outpatient study facilities separately. We also calculated frequencies for organization characteristics.
For the open-ended question eliciting the rationale behind the organization-configured maximum number of records allowed open, we applied qualitative content analysis14 to summarize the data according to the predefined categories and to examine other categories that emerged from the responses. This study was deemed exempt by the Albert Einstein College of Medicine Institutional Review Board.
RESULTS
Organization characteristics
Respondents from 112 organizations completed the survey; because we posted the survey on listservs, we could not calculate the response rate. Of the 112 responding organizations, 79 used EHRs in both inpatient and outpatient study facilities, 25 in only inpatient facilities, and 8 in only outpatient facilities. Thus, EHR configurations in a total of 191 study facilities were examined. All major EHR vendors were represented; Epic, Cerner, Allscripts, Meditech, and Siemens were the most commonly used EHR systems in both inpatient and outpatient study facilities. The organizations were widely distributed across the United States, including 25 organizations in the South, 16 in the West, 32 in the Midwest, and 32 in the Northeast (7 responses were missing).
EHR characteristics
EHRs in the 191 study facilities were examined, of which 104 were inpatient and 87 were outpatient facilities. Overall, 167 of the 191 study facilities (87.4%) used an EHR with a vendor-designed maximum that allowed multiple records open at once, and the percentage was similar for inpatient (91 of 104; 87.5%) and outpatient study facilities (76 of 87; 87.4%). In the remaining 24 study facilities, the vendor-designed maximum was only 1 record open at a time, and these were excluded from analysis.
Organization-configured maximum number of records open in EHRs
Of the 167 study facilities included in the analysis, the organization-configured maximum number of records was unrestricted in 44.3% of systems (≥3 records open), restricted in 38.3% (only 1 record open), and hedged in 17.4% (2 records open) (Table 1). These findings were consistent in inpatient and outpatient settings and across the different EHR vendor systems.
Table 1.
Organization-configured number of records allowed open in EHR systems vendor-designed to open multiple records at once
| Study facilities | Unrestricted (≥3 records) (%) | Restricted (1 record) (%) | Hedged (2 records) (%) | Total EHRs |
|---|---|---|---|---|
| Inpatient | 38 (41.8) | 37 (40.7) | 16 (17.6) | 91 |
| Outpatient | 36 (47.4) | 27 (35.5) | 13 (17.1) | 76 |
| Overall | 74 (44.3) | 64 (38.3) | 29 (17.4) | 167 |
EHR, electronic health record.
Rationale for EHR configuration
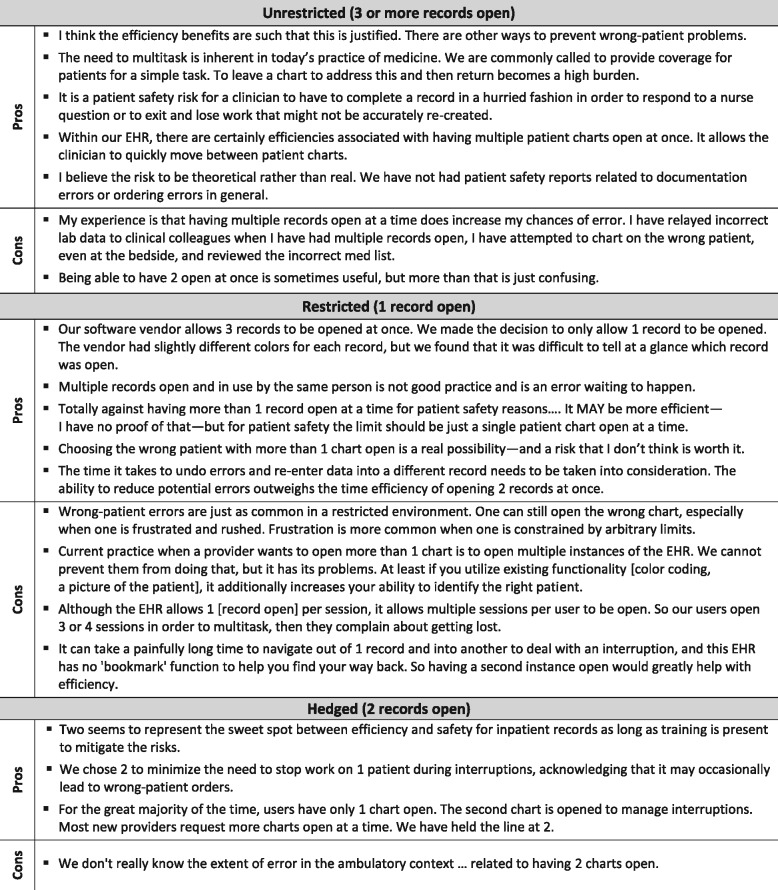
Decision-making about the maximum number of records allowed open in EHRs was driven by efforts to balance safety and efficiency; however, there was considerable disagreement about the optimal approach. Comments illustrating each of the predefined categories of organization-configured maximum number of records allowed open are presented in Figure 1 .
Figure 1.
Comments about the organization-configured number of patient records allowed open in EHR systems vendor-designed to open multiple records at once. EHR, electronic health record.
Unrestricted (configured for ≥3 records open at once): In unrestricted environments, increased efficiency was noted as justifying potential safety risks. Respondents highlighted other ways to minimize risk, including patient-verification alerts, color-coding, and patient photographs, although they acknowledged that these methods are not used consistently. Some respondents who worked in an unrestricted EHR environment stated that, to their knowledge, their organization did not experience excessive wrong-patient error reports.
Restricted (configured for only 1 record open): In restricted environments, respondents expressed the conviction that any potential increase in efficiency was not worth an increased risk of wrong-patient errors. However, several respondents reported that some providers working in a restricted environment used workarounds, such as opening multiple instances of the EHR in multiple browsers or on multiple computers, and expressed concern that these practices could pose even greater risk for error.
Hedged (configured for a maximum of 2 records open): In organizations that hedged, respondents reported that this approach represented the “sweet spot” that balanced safety and efficiency. As echoed by many respondents, regardless of the configuration of their organization’s EHR, having 2 records open allows providers to multitask and better manage interruptions. However, respondents acknowledged that the extent to which providers choose to open multiple records and the magnitude of increased efficiency and/or risk are unknown.
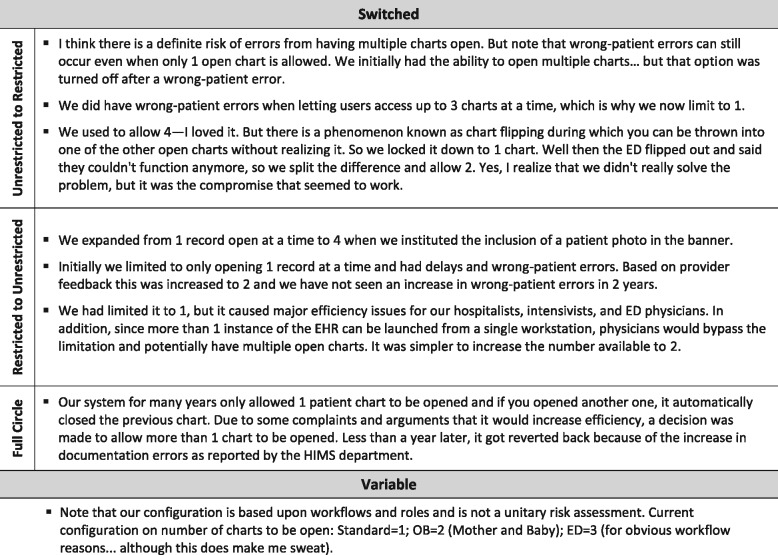
Two other categories emerged in the qualitative analysis: switched and variable (Figure 2 ). Although asked about the current number of records allowed open at once, reported in Table 1, some respondents described situations where their organization changed from one configuration to another (switched) or allowed different configurations based on provider role or setting (variable). These categories are not mutually exclusive: an organization may currently hedge, but also may have switched from an unrestricted or restricted configuration.
Figure 2.
Unexpected findings about organization-configured number of records allowed open in EHR systems vendor-designed to open multiple records at once at once. EHR, electronic health record; HIMS, Health Information Management System; OB, Obstetrics; ED, Emergency Department.
Switched: There were organizations that switched from an unrestricted to a more restricted environment, in some cases based on experiencing an error. Others switched from a restricted to an unrestricted environment based on perceived inefficiency and provider feedback (ie, “frustration”). One organization switched from restricted to unrestricted and back to restricted due to an increase in reported errors.
Variable: Some respondents reported variable standards for the number of records allowed open depending on the provider role or setting, eg, 1 record for most inpatient settings versus multiple records for the emergency department, obstetrics, and ambulatory settings. Others advocated a different number of records allowed open based on type of provider, eg, 1 for physicians and 2 for nursing staff.
DISCUSSION
Results of this national survey representing diverse geographic areas and all the leading EHR vendors demonstrate that a majority of respondents are not adhering to expert recommendations to limit the number of patient records open to 1 at a time. In fact, we found that approximately the same percentage of systems allowed at least 3 records open as adhered to the guidelines that suggest limiting to 1 record open. A smaller percentage sought a middle ground and split the difference, permitting 2 records to be open at once. These findings were consistent in inpatient and outpatient settings and across EHR vendor systems.
Respondents’ comments suggest that decision-making was based on efforts to balance safety and efficiency, but there was considerable disagreement among organizations about how to achieve that balance. Several respondents cited the inefficiency of restricting providers to a single record open at a time but generally considered this approach the safer option. In a prior survey conducted by Levin et al.,15 chief medical information officers attributed the ability to view multiple records simultaneously as a cause of wrong-patient errors and believed this feature should be deactivated. Our survey found that being restricted to 1 record open at a time prompted some providers to launch multiple instances of the EHR as a workaround, using multiple browsers or multiple computers. This could pose greater risk than configuring the EHR to open multiple records using existing functionality. The finding that organizations switched from one configuration to another, and that different configurations were allowed based on different provider roles or settings, further illustrates the lack of evidence-based decision-making.
Several expert guidelines warn that opening multiple patient records simultaneously increases the risk of patient identification errors. The Office of the National Coordinator for Health Information Technology states that data can be entered “incorrectly into the electronic record due to multiple records being open.”10 In its Patient Identification SAFER Guide,11 the agency recommends restricting “the number of patient records that can be displayed on the same computer at the same time to one, unless other patient records are opened as ‘Read Only’ and are clearly differentiated.” This recommendation also appears in a Joint Commission Sentinel Event Alert, Safe Use of Health Information Technology.12
However, no studies to date have established an association between risk of wrong-patient errors and the number of records open at once. In a study by Galanter et al.,16 60% of wrong-patient errors occurred when at least 2 records were open simultaneously, but due to methodologic limitations, investigators could not quantify the relationship between the number of records open and the risk of errors. The absence of evidence may explain the lack of adherence to expert recommendations and the lack of consensus found in our survey. In addition, while patient safety is paramount, these recommendations do not take into account the real-world, day-to-day demands on health care providers.
Limitations
Our study has several limitations. Because we posted the survey on listservs, we could not calculate the response rate and the number of respondents likely represents a small sample. Therefore, these results should not be considered representative of general practice. However, our results highlight the lack of consensus on an important patient safety issue in the absence of evidence. In addition, since the finding that organizations switched or had variable (ie, role- or department-specific) configurations emerged in the analysis, we could not quantify how frequently these occurred. Finally, we did not verify the specifications of each system with EHR vendors as to all the possible variations in configuration of the number of records open. However, as reported, the vast majority of systems were vendor-designed to allow multiple records open at once and could be restricted as determined by the organization.
CONCLUSIONS/IMPLICATIONS
Our results show that decision-making about the number of patient records to be allowed open in EHRs is based on efforts to balance efficiency and safety, but in the absence of evidence, there is a lack of consensus and failure to adhere to safety expert recommendations. No studies to date have demonstrated whether multiple records open increases the risk of wrong-patient errors, to what degree, and whether any increase in risk is dependent on the number of records. (Is 4 more dangerous than 3? Is 3 worse than 2? Is 1 the safest?) The mechanisms by which opening multiple patient records can lead to wrong-patient errors and the magnitude of this risk need to be established in order to guide evidence-based decision-making about safe implementation of EHR systems. Given the near-universal use of EHRs, rigorous studies using valid measures of safety17 and productivity are needed to inform decision-makers about how to configure their systems to maximize efficiency and minimize risk.
FUNDING
This project was supported by grant number R21HS023704 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
References
- 1. Office of the National Coordinator for Health Information Technology. Certified Health IT Vendors and Editions Reported by Hospitals Participating in the Medicare EHR Incentive Program, Health IT Quick-Stat #29. dashboard.healthit.gov/quickstats/pages/FIG-Vendors-of-EHRs-to-Participating-Hospitals.php. July 2016. Accessed September 30, 2016.
- 2. Office of the National Coordinator for Health Information Technology. Office-based Physician Electronic Health Record Adoption: 2004–2014, Health IT Quick-Stat #50. dashboard.healthit.gov/quickstats/pages/physician-ehr-adoption-trends.php. September 2015. Accessed September 30, 2016.
- 3. Office of the National Coordinator for Health Information Technology. Data Documentation, Office-based Health Care Providers. 2011–2013. http://dashboard.healthit.gov/datadashboard/documentation/ska-data-documentation.php Accessed September 30, 2016.
- 4. Koppel R, Metlay JP, Cohen A et al. . Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;29310:1197–203. [DOI] [PubMed] [Google Scholar]
- 5. Harrison MI, Kopel R, Bar-Lev S. Unintended consequences of information technologies in health care: an interactive sociotechnical analysis. J Am Med Inform Assoc. 2007;145:542–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ash JS, Sittig DF, Poon EG, Guappone K, Campbell E, Dykstra RH. The extent and importance of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2007;144:415–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2006;135:547–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sittig DF, Ash JS. Clinical Information Systems: Overcoming Adverse Consequences. Boston, MA: Jones and Bartlett; 2010. [Google Scholar]
- 9. Ash J, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc. 2003;11:104–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Office of the National Coordinator for Health Information Technology. Anticipating Unintended Consequences of Health Information Technology and Health Information Exchange: How to Identify and Address Unsafe Conditions Associated with Health IT. 2013; https://www.healthit.gov/sites/default/files/How_to_Identify_and_Address_Unsafe_Conditions_Associated_with_Health_IT.pdf. Accessed September 30, 2016. [Google Scholar]
- 11. Office of the National Coordinator for Health Information Technology. Patient Identification SAFER Guide. https://www.healthit.gov/safer/guide/sg006. Accessed August 31, 2016.
- 12. The Joint Commission. Safe use of health information technology. Sentinel Event Alert #54, March 31, 2015. Accessed September 26, 2016. [PubMed] [Google Scholar]
- 13. Paparella SF. Accurate patient identification in the emergency department: meeting the safety challenges. J Emerg Nurs. 2012;384:364–67. [DOI] [PubMed] [Google Scholar]
- 14. Krippendorff K. Content Analysis: An Introduction to its Methodology, 3rd ed Thousand Oaks, CA: Sage Publications; 2013. [Google Scholar]
- 15. Levin HI, Levin JE, Docimo SG. “I meant that med for Baylee not Bailey!”: a mixed method study to identify incidence and risk factors for CPOE patient misidentification. AMIA Annu Symp Proc. 2012;2012:1294–301. [PMC free article] [PubMed] [Google Scholar]
- 16. Galanter W, Falck S, Burns M, Laragh M, Lambert BL. Indication-based prescribing prevents wrong-patient medication errors in computerized provider order entry (CPOE). J Am Med Inform Assoc. 2013;203:477–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Adelman JS, Kalkut GE, Schechter CB et al. . Understanding and preventing wrong-patient electronic orders: a randomized controlled trial. J Am Med Inform Assoc. 2013;202:305–10. [DOI] [PMC free article] [PubMed] [Google Scholar]