Abstract
Background and Objectives:
Exposure to early‐life trauma may lead to maladaptive characteristics such as alexithymia, and thus to poorer emotional regulation. This relationship may also be influenced by exposure to substances prenatally. We hypothesized that increased alexithymia would be seen in those with prenatal cocaine exposure (PCE). Additionally, we hypothesized that early-life trauma would be associated with alexithymia, and that alexithymia would be associated with poor emotional reappraisal and emotional suppression.
Methods:
A moderated mediation model was developed to examine whether the hypothesized indirect relationship between trauma and emotional reappraisal through alexithymia was different in young adults with and without PCE (Total N = 57). Thirty-seven young adults with PCE and 20 with no such exposure, all of whom were members of a longitudinal cohort, were recruited for the study, and data concerning childhood trauma, alexithymia, and emotional regulation were collected. Intercorrelations were performed between the scores on each measure and moderated mediation models were constructed separately with emotional neglect or emotional abuse as the independent variable and emotional reappraisal or emotional suppression as the dependent variable.
Results:
PCE status was associated with alexithymia, and alexithymia mediated the relationship between emotional neglect and emotional reappraisal in individuals with PCE but not those without.
Discussion and Conclusions:
The data suggest that alexithymia is a mechanism underlying poor use of emotional reappraisal in PCE individuals.
Scientific Significance:
Individuals with early-life trauma and substance exposure may represent a vulnerable population, and alexithymia may play a key role in the development of emotional regulation skills in this population
INTRODUCTION
Individuals with prenatal cocaine exposure (PCE) may be particularly vulnerable to early-life stressors. Children with PCE who experienced childhood maltreatment demonstrate increased stress responses compared with those exposed to childhood maltreatment without PCE.1 Emotion-regulation difficulties are associated with mental illness and substance abuse.2 Here, we sought to examine childhood trauma and how it relates to emotion-regulation difficulties in individuals with and without PCE. We examine potential mechanisms by which trauma may be associated with emotion-regulation difficulties, including alexithymia, which has been demonstrated to be positively associated with emotional-regulation difficulties in both healthy3 and autistic4 populations. We test a model that posits that early-life trauma will be associated with alexithymia, which, in turn, may worsen emotion-regulation difficulties.Further, individuals with PCE may show increased vulnerability to maladaptive outcomes of early-life trauma, such that emotional regulation will be more impaired and alexithymia increased in individuals with PCE.
Exposure to trauma such as parental neglect and abuse in childhood is typically detrimental to development and later well-being.5 Investigations of childhood trauma have identified emotional neglect, emotional abuse, physical neglect, physical abuse, and sexual abuse as major components of early-life trauma, which have been investigated using validated instruments like the Childhood Trauma Questionnaire (CTQ).6 The presence of emotional neglect and emotional abuse in childhood is commonly linked to adult psychopathology including depressive7 and substance-use disorders.8 For brevity, in this paper, we collectively refer to these components simply as “trauma” unless we are discussing a specific component.
An important mechanism underlying the relationship between trauma and mental illness may involve trauma’s effects on emotion-regulation capabilities.9 Longitudinal investigations suggest that emotion-regulation impairment is a mechanism by which trauma contributes to later-life mental illness.10 Individuals who experience different types of trauma may adopt different emotion-regulation strategies.Two strategies include suppression, a potentially harmful tendency to ignore or tamp down one’s emotional responses, or reappraisal, a more beneficial strategy to change one’s thoughts about a stimulus.2 Suppression involves being aware of one’s emotion to consciously force it out of awareness and masking one’s physical reactions to emotions.11 Reappraisal refers to cognitive change, in this case involving challenging interpretations or one’s own physical responses and reframing one’s perspective so that emotional situations are less intense.12 Emotional neglect and abuse have previously been related to increased use of suppression strategies and decreased use of reappraisal strategies in adults with major depression.13
However, the mechanisms by which trauma may lead to poor emotional regulation are not fully understood. One potential pathway may involve alexithymia. Alexithymia is characterized by difficulty identifying and describing one’s emotions and a tendency to focus on external, rather than internal, experiences.14 Alexithymia is common in individuals with mental illness, including depressive, anxiety, psychosomatic, and substance-use disorders.15 It is also commonly associated with exposure to traumatic experiences and posttraumatic stress disorder16 and has been specifically related to childhood emotional neglect.17 Inability to identify one’s emotions may contribute to poorer regulation of those emotions. In turn, early-life trauma may lead to alexithymia, which may then complicate reappraisal of emotions, as emotions one cannot identify are likely harder to regulate. The relationships between early-life trauma, alexithymia, and emotional regulation deserve more investigation.
We present a potential theory by which early-life trauma, specifically emotional neglect and abuse, may contribute to poor emotion regulation, via the characteristic of alexithymia, and how this process may be worsened in individuals with PCE. Emotional intelligence can be considered as a learned skill.18 If an individual’s parents or guardians do not present a child with emotional enrichment, including guidance on how to label their emotions, an individual’s ability to identify their own emotions may be affected. Further, emotionally abusive behavior may present an uncertain environment where a child may improperly label emotions as negative when they are punished for expressing them or may avoid dwelling on their emotions at all to avoid punishment. Both situations may contribute to increased emotional uncertainty, and thus to alexithymia. From there, difficulties labeling emotions or an avoidance of emotion may lead to diminished tendencies to properly regulate emotions, as reappraising how one feel’s when one is not sure how one feels or is trying to avoid feeling at all may be more difficult. Finally, the prenatal environment may alter neural substrates underlying emotional-regulation circuits. PCE is an important consideration. Environments with parental substance abuse may lead to increased trauma exposure.19 Further, neurocognitive correlates of PCE may include altered stress responsivity20 and poorer self-monitoring.21 These factors may heighten vulnerability to trauma exposure. In individuals with PCE, who may experience higher levels of arousal, failure to provide emotional guidance via neglect or increased punishment of expressed emotion via abuse may worsen emotional-regulation tendencies. As a result, PCE status may influence relationships between trauma, alexithymia, and emotional regulation.
Here, we sought to investigate different types of childhood trauma, including emotional neglect, emotional abuse, physical neglect, physical abuse, and sexual abuse, as well as alexithymia and emotional regulation, in a cohort of young adults with and without PCE who have been followed since birth. Following the theorized model, we hypothesized that individuals with PCE would have increased exposure to trauma, including emotional neglect and abuse, and would demonstrate higher alexithymia. We also hypothesized that increased trauma exposure would lead to alexithymia, and that alexithymia would in turn lead to poorer emotion-regulation strategies, including increased use of suppression and reduced use of reappraisal, similar to what has been found in individuals with autism.4 Further, we hypothesized that this relationship would be moderated by PCE status. To explore this hypothesis, we performed correlations between our variables of interest, testing for relationships that would allow for investigation using a regression model. The theoretical moderated mediation model posited that alexithymia would mediate the relationship between the independent variable of childhood trauma and dependent variables of reappraisal or suppression, separately, and that this relationship would be moderated by PCE status.
METHODS
Participants
Participants were recruited from a cohort involved in a longitudinal, 25-year study examining effects of PCE on physical, cognitive, social, and emotional development. All children in the PCE group were exposed to cocaine and possibly other drugs in utero. Nondrug-using mothers and their children were enrolled to serve as a control group. The sample was recruited at birth over a 5-year period and children and their parents have been seen biannually since. Families were originally recruited when they presented for prenatal care at the Women’s Center of the Yale-New Haven Hospital or, in the case of no prenatal care, when they were admitted to the postpartum ward. Maternal cocaine use was determined based on maternal self-report, on urine toxicology during pregnancy or following delivery, and on meconium toxicology in the infant. The larger sample from which the children for this study were drawn consisted of 81% African-American, 6.5% Hispanic, and 12.5% Caucasian children, all of whom come from the greater New Haven area.22,23
From this larger sample, we recruited 37 young adults (average age: 23.3 years, SD = 1.6, 18 female/19 male) with PCE and 20 young adults (average age: 22.4 years, SD = 1.7, 8 female/10 male) with no prenatal drug exposure (NDE), for a total of 57 participants.
Of this subsample, 72% were African-American, 8% were Hispanic, and 17% were Caucasian, with one participant reporting as “other.” Participants from the subsample did not differ significantly from the larger sample on race (σ = 2.01, P = .15), gender (σ = 46, P = .49), or socioeconomic status (σ = 66, P = .41). During twice-yearly visits when participants were 17 to 19 years of age, they completed the brief form of the CTQ.24 At the ages of 21 to 25, if they qualified for the study, expressed interest in participating, and willingness to complete questionnaires, they were recruited for this study. Participants were between the ages of 20 and 25 years during recruitment for this study component.
Among mothers of the PCE individuals in this specific cohort, 16% reported some marijuana use, 51% reported some alcohol use, and 64% reported nicotine use during the last 30 days of gestation. Simultaneous use of multiple substances is common in individuals using cocaine. Since not every PCE adolescent was exposed to other substances, and every mother in the PCE group indicated cocaine use, for the purposes of this study, we focused upon cocaine exposure. Among NDE individuals, mothers reported using no substance use during pregnancy, although two of the mothers reported some tobacco use in their lifetime.
We did not find support for differences between groups in gender distribution (C = 0.38, P = .54), socioeconomic status as indicated by the mother’s years of education (C = 0.10, P = .74), though there was a difference in ethnicity/race (C = 10.8, P = .002), with a larger percentage of Caucasian individuals in the NDE group. There was a marginal difference in age (F = 3.85, P = .055), with the NDE group (22.45, SD = 1.76) slightly younger than the PCE group (23.05, SD = 1.74).
Questionnaires
Childhood Trauma Questionnaire
The CTQ is designed to measure histories of abuse and neglect in childhood.6 The questionnaire consists of 28 items that measure five types of maltreatment, including emotional, physical, and sexual abuse, and emotional and physical neglect, using 5-point Likert scales that rate how true items were as they were growing up (never true to very often true).Scores are generated for each type of maltreatment, with higher scores indicating more maltreatment. Each participant completed the questionnaire twice at the ages of 17 to 18 years, and the scores were averaged.
Alexithymia: 20-Item Toronto Alexithymia Scale
The 20-Item Toronto Alexithymia Scale (TAS-20)25 is widely used in clinical and research settings for the assessment of alexithymia. The instrument consists of 20 statements that participants are requested to rate on how much they agree or disagree with the ability of the statement to describe their behavior on 5-point Likert-type scales ranging from 1 (strongly disagree) to 5 (strongly agree). Total scores for the TAS-20 range from 20 to 100 with higher scores indicating increased alexithymia. The TAS-20 was administered when participants were between the ages of 20 and 25 years.
Emotion Regulation Questionnaire
The Emotion Regulation Questionnaire (ERQ) assesses regulation strategies of cognitive reappraisal and emotional suppression.2 The ERQ is a self-report scale with Likert-type responses with a two-factor structure with adequate internal consistency for cognitive reappraisal (CR) (reappraisal: α = .75 to .82) and expressive suppression (ES) (suppression: α = .68 to .76) subscales. Responses for each scale are summed, and higher scores indicate greater use of CR or ES. The ERQ was administered when participants were between the ages of 20 and 25 years.
Analysis and Theoretical Model
Data analysis was performed in IBM SPSS Statistics version 24.26 Descriptive statistics for gender, age, alexithymia (TAS-20 total score), Reappraisal (ERQ reappraisal subscale score), Suppression (ERQ suppression subscale score), and emotional neglect, emotional abuse, physical neglect, physical abuse, and sexual abuse (subscales of the CTQ) were examined. Correlations were performed between scores on the TAS-20, the reappraisal and suppression subscales, and the subscales of the CTQ. To construct our mediation models, we followed criteria established by Hayes et al.27,28 Criteria require that the causal variable must be correlated with both the outcome variable and the mediator. Factors with significant intercorrelations that met these criteria were subsequently entered into moderated mediation models. Scores on the CTQ subscales, ERQ subscales, TAS-20, and PCE status were entered respectively as independent, dependent, mediator, and moderator variables. Models were tested separately for each CTQ and ERQ subscale using SPSS PROCESS,27 which utilizes bootstrapping. This is a robust method for models involving mediation, and generates an approximation of the distribution of a statistic by repeated random sampling, which is effective in handling data from limited sample sizes. Models were tested with 5000 resamples and 95% confidence intervals (95% CI) were calculated. Significance was set at P = .05 and when 95% CI did not include zero. A significant moderation was determined when PCE status, and the PCE status and trauma interaction term were significantly associated with outcome variables.
SPSS PROCESS utilizes ordinary least squares regression analysis, a widely used method that minimizes the summed squared differences between observed and expected values for fitting linear statistical models.28 The moderated mediation analyses utilized the default model 8 embedded within SPSS PROCESS to examine the direct path between childhood trauma and emotion-regulation strategies, their indirect paths through alexithymia, and whether these relationships differed by PCE status. Interactions and main effects, as well as indices of mediation and moderation, were calculated together in SPSS process as one moderated mediation model (model 8). We did not modify for additional paths in the moderated mediation model. Age was included as a covariate considering the marginal difference in age between groups.
RESULTS
Trauma Exposure, Alexithymia, and Emotional Regulation
Thirty-seven PCE individuals and 20 NDE individuals completed the CTQ, TAS-20, and ERQ. We found no support for group differences on trauma exposure for any of the CTQ subscales or when examining emotion-regulation strategies. Individuals with PCE showed marginally higher alexithymia scores (F = 3.95, P = .052). Table 1 illustrates the means and standard deviations by group.
TABLE 1.
Comparisons for alexithymia, emotional regulation, and trauma exposure between the PCE and NDE groups
| PCE (n = 37) | NDE (n = 20) | |||||
|---|---|---|---|---|---|---|
| Measure | Mean | SD | Mean | SD | F | P |
| TAS-20 | 49.18 | 12.90 | 42.25 | 11.88 | 3.95 | .05 |
| Reappraisal | 32.97 | 7.36 | 30.80 | 6.40 | 1.14 | .29 |
| Suppression | 16.85 | 5.60 | 16.00 | 6.44 | 0.27 | .60 |
| Emotional neglect | 10.40 | 4.40 | 10.02 | 4.58 | 0.09 | .76 |
| Emotional abuse | 7.55 | 2.89 | 7.27 | 3.15 | 0.11 | .73 |
| Physical neglect | 7.82 | 2.93 | 7.50 | 3.19 | 0.00 | .95 |
| Physical abuse | 6.77 | 2.62 | 6.72 | 2.87 | 0.00 | .95 |
| Sexual abuse | 6.27 | 2.86 | 5.82 | 2.06 | 0.38 | .54 |
Bolded indicates marginal significance.
NDE = nondrug-exposed; PCE = prenatally cocaine-exposed; TAS-20 =20‐Item Toronto Alexithymia Scale.
Correlations
Intercorrelations between childhood trauma, alexithymia, reappraisal, and suppression across all participants independent of PCE status are shown (Table 2).
TABLE 2.
Intercorrelations between childhood trauma, alexithymia, reappraisal, and suppression across all participants independent of PCE status
| TAS-20 Total | Suppression | Reappraisal | Emotional neglect | Emotional abuse | Physical neglect | Physical abuse | Sexual abuse | |
|---|---|---|---|---|---|---|---|---|
| Suppression | 0.334* | 1 | ||||||
| Reappraisal | −0.346** | 0.076 | 1 | |||||
| Emotional neglect | 0.333* | 0.162 | −0.332* | 1 | ||||
| Emotional abuse | 0.259* | 0.06 | −0.287* | 0.583** | 1 | |||
| Physical neglect | 0.227 | 0.224 | −0.314* | 0.767** | 0.552** | 1 | ||
| Physical abuse | 0.19 | 0.042 | −0.276* | 0.448** | 0.605** | 0.617** | 1 | |
| Sexual abuse | 0.246 | 0.218 | −0.119 | 0.590** | 0.658** | 0.570** | 0.684** | 1 |
PCE = prenatally cocaine-exposed; TAS-20 = 20-Item Toronto Alexithymia Scale.
Correlation significant at the 0.05 level (two-tailed).
Correlation significant at the 0.01 level (two-tailed).
Emotional suppression was correlated with alexithymia (r = .334, P = .013). There were no correlations between emotional suppression and any other variables (all P > .05).
Physical neglect was not correlated with TAS-20 scores (r = .227, P = .089), but correlated negatively with reappraisal (r = −.314, P = .020). Similarly, physical abuse was not correlated with TAS-20 scores (r = .19, P = .156), but correlated negatively with reappraisal (r = −.276, P = .042). Sexual abuse was not correlated with either TAS-20 scores (r = .246, P = .065) or with reappraisal (r = −.119, P = .38).
Emotional neglect positively correlated with TAS-20 scores (r = .33, P = .011) and negatively correlated with reappraisal (r = −.33, P = .013). Similarly, emotional abuse positively correlated with TAS-20 scores (r = .25, P = .050) and negatively correlated with reappraisal (r = −.28, P = .034). Additionally, TAS-20 scores negatively correlated with reappraisal (r = −.34, P = .010).
Emotional neglect and abuse were thus entered into two separate moderated mediation models as the independent variable. Additionally, as emotional abuse and neglect showed significant associations with reappraisal, but not suppression measures, models only included reappraisal as the dependent variable.
Moderated Mediation Analysis
Emotional Neglect
Results of a mediation analysis of the overall model between emotional neglect and reappraisal scores through alexithymia, with the moderator of PCE status are shown in Figure 1.
FIGURE 1.
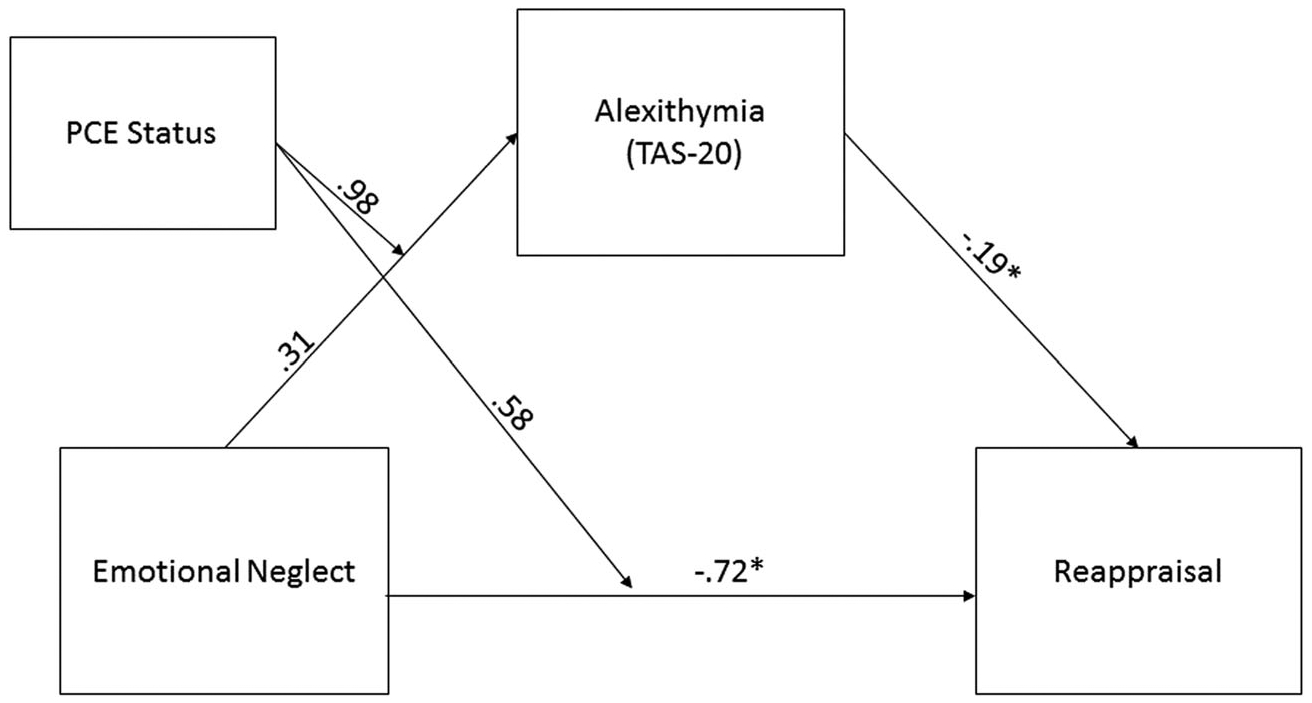
Moderated mediation for emotional neglect. PCE = prenatally cocaine-exposed; TAS-20 = 20-Item Toronto Alexithymia Scale.
The model accounted for significant variance in emotional reappraisal (R2 = 0.50, F(5, 49) = 3.36, P = .011). Emotional neglect was not associated with alexithymia (b = 0.31, SE = 0.61, P = .61, 95% CI = −0.91, 1.53). PCE status (b = −3.97, SE = 8.6, P = .64, 95% CI = −21.29, 13.34), and the PCE status and emotional neglect interaction term (b = 0.98, SE = 0.76, P = .20, 95% CI = −0.56, 2.52) were not associated with alexithymia. Alexithymia (b = −0.19, SE = 0.07, P < .01, 95% CI = −0.34, −.047) and emotional neglect (b = −0.72, SE = 0.32, P = .029, 95% CI = −1.37, −.075) were associated with emotional reappraisal. However, PCE status (b = −2.63, SE = 4.5, P = .56, 95% CI = −11.77, 6.50) and the PCE status and emotional neglect interaction term (b = 0.58, SE = 0.41, P = .15, 95% CI = −0.23, 1.41) were not associated with emotional reappraisal.
For those with PCE, the indirect effect of emotional neglect on reappraisal was significant (b = −0.25, SE = 0.14, 95% CI = −0.57, −0.035). For those with NDE, the indirect effect of emotional neglect on reappraisal was not significant (b = −0.061, SE = 0.13, 95% CI = −0.40, 0.15). Together, these results indicate that alexithymia statistically mediated the association between emotional neglect and emotional reappraisal only in individuals with PCE. Furthermore, as a significant index of difference between conditional indirect effects was not observed (b = −0.19, SE = 0.18, 95% CI = −0.60, 0.13), a moderated mediation could not be concluded.
Emotional Abuse
Results of a mediation analysis of the overall model between emotional abuse and reappraisal scores through alexithymia with the moderator of PCE status are shown in Figure 2.
FIGURE 2.
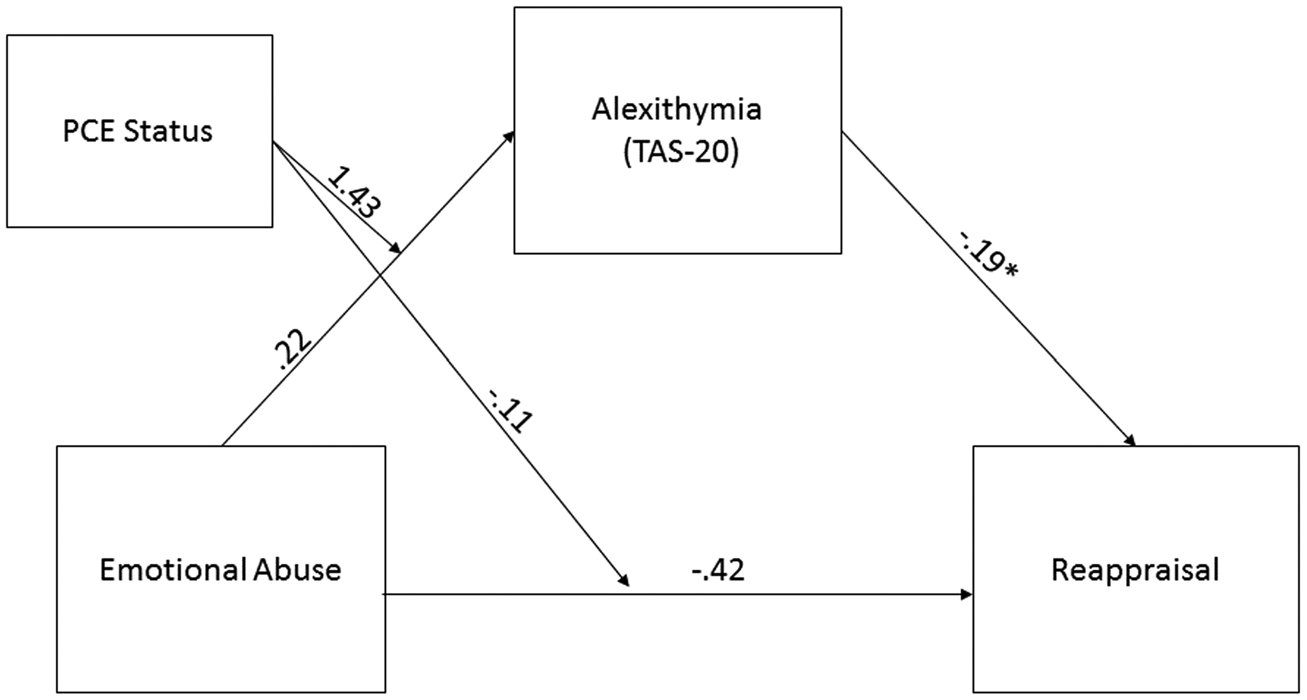
Moderated mediation for emotional abuse. PCE = prenatally cocaine-exposed; TAS-20 = 20-Item Toronto Alexithymia Scale.
The overall model accounted for significant variance in emotional reappraisal (R2 = 0.46, F(5, 49) = 2.71, P < .05). Emotional abuse was not associated with alexithymia (b = 0.22, SE = 0.91, P = .24, 95% CI = −1.61, 2.05). PCE status (b = −4.37, SE = 9.3, P = .81, 95% CI = −23.26,14.31), and its interaction with emotional abuse (b = 1.43, SE = 1.18, P = .23, 95% CI = −0.93, 3.81) were not associated with alexithymia. In this model, alexithymia (b = −0.19, SE = 0.07, P = .013, 95% CI = −0.34, −0.042) was associated with emotional reappraisal, but not PCE status (b = −2.63, SE = 4.5, P = .56, 95% CI = −5.65, 14.15), its interaction with emotional abuse (b = −0.11, SE = 0.63, P = .85, 95% CI = −1.38, 1.15), or the variable of emotional abuse (b = −42, SE = 0.48, P = .37, 95% CI = −1.39, 0.533).
For those with PCE, the indirect effect of emotional abuse on reappraisal through alexithymia was significant (b = −0.31, SE = 0.20, 95% CI = −0.81, −0.021). For those with NCE, the indirect effect of emotional abuse on reappraisal was not significant (b = −0.041, SE = 0.22, 95% CI = −0.42, 0.40). Together, these results indicate a statistically significant mediation relationship in which emotional abuse, through its association with alexithymia, contributes to emotional reappraisal in individuals with PCE. However, no significant index of difference between conditional indirect effects was observed (b = −0.27, SE = 0.30, 95% CI = −1.009, 0.13), and thus no significant moderated mediation could be concluded.
Additional Analyses
Results of a mediation analysis of the overall models between emotional neglect, emotional abuse (IVs), and emotional suppression scores (DV) through alexithymia (mediator), with the moderator of PCE status, were performed by the request of a reviewer. However, these models were not significant.
By request of a reviewer, mediation of emotional reappraisal from emotional neglect and abuse through alexithymia in the total sample, using PCE status as a covariate, was examined using SPSS PROCESS model 4. The most salient results from that analysis are described here. The overall model for emotional neglect was significant for reappraisal (R2 = 0.22, F(3, 51) = 4.9, P = .0045). There was a significant indirect effect of emotional neglect on reappraisal through alexithymia (b = −0.16, SE = 0.10, 95% CI = −0.41, −0.071). Similarly, the overall model for emotional abuse was significant for reappraisal (R2 = 0.21, F(3, 51) = 4.6, P = .0057). However, there was not a significant indirect effect of emotional abuse on reappraisal through alexithymia in the total sample (b = −0.20, SE = 0.14, 95% CI = −0.52, 0.016).
DISCUSSION
We examined a role for trauma on emotional regulation, a construct related to mental health.10 We further examined a mediating role of alexithymia, and tested whether the indirect effect through alexithymia was potentially moderated by PCE status. The theory behind this model was that early-life trauma exposure would contribute to increased avoidance and lessened understanding of one’s emotions. This would in turn contribute to alexithymia, which could then result in poorer ability to regulate emotions. Finally, we hypothesized that individuals with PCE would be more vulnerable to early-life trauma, showing increased alexithymia and poorer regulation. Our hypotheses were partially supported by the data.
The scores for individual traumas in this sample were generally low, and the average exposure in each group indicated no or low rates of trauma on each of the subscales of the CTQ. There were no group differences between those with PCE and those with NDE in terms of exposure to any type of trauma measured by the CTQ. There were also no indications of altered reappraisal or suppression strategies between groups. This finding is somewhat surprising considering the literature on PCE, which indicates increased aggression and externalizing behavior in adolescence.29 However, individuals with PCE demonstrated higher alexithymia scores. This may indicate a tendency toward increased emotional dissociation or avoidance,30 potentially due to increased stress response reported previously in individuals with PCE.31
Our investigations into relationships between early-life trauma, alexithymia, and emotional regulation in individuals with NDE and PCE indicated that early-life emotional neglect and abuse may contribute to poorer emotional reappraisal through effects on alexithymia, consistent with our hypothesis and consistent with literature on the link between alexithymia and emotional functioning.32 While physical neglect and abuse were not associated with alexithymia, our correlations indicated that these indices of physical trauma were negatively correlated with emotional reappraisal. Sexual abuse, which may have severe detrimental effects on mental health,5 was not correlated with any measures of interest, though the frequency of sexual abuse in our sample measured via the CTQ was very low.
The moderated mediation models of emotional abuse and neglect indicated that the mediating effect of alexithymia on emotional neglect’s and abuse’s relationships with reappraisal were present in individuals with PCE, but not those with NDE, and the mediation effect did not significantly differ by PCE status. The results of the inclusion of PCE status as a covariate in the full sample also indicated that PCE status may play a role in the indirect relationship between different types of trauma, alexithymia, and reappraisal. This relationship between trauma, alexithymia, and emotional reappraisal may speak to the alterations in emotional expressivity seen in PCE individuals in many age ranges, including less emotional expression in infancy,33 increased stress and frustration in childhood,34 and alterations in neural and physiological responses to stress in adolescence.31 Alterations in stress responses at younger ages may make individuals with PCE more vulnerable to emotional neglect and abuse, resulting in higher alexithymia and poorer reappraisal abilities in young adulthood. Our data are consistent with this interpretation and those reported previously1 indicating increased avoidance and disengagement in PCE adolescents who had also been exposed to childhood maltreatment. In our sample, the data suggest increased response to stress due to PCE coupled with emotional neglect or abuse that may have result in an alexithymic coping style, and thus poorer ability to reappraise emotions as young adults.
Other factors, including parenting quality and parent-child relationships, warrant consideration. While our sample did not indicate increased emotional neglect or abuse in young adults with PCE, it is possible that the quality of parent-child interaction differed in individuals with PCE. Parents who continue using substances may show increased aggression toward or increased withdrawal from their offspring, as has been seen in cocaine-using parents of toddlers.35 In addition, toddlers of substance-using mothers with mental illness may show an increased likelihood of presenting with disorganized attachment.36 Further, drug-abusing parents may be more likely to use emotion-avoidant language,37 suggesting that alexithymic-style avoidance may be common in parents of PCE children and may contribute to poor parent-child interactions.
Finally, mention should be made of potential genetic contribution to emotional‐regulation difficulties that may be present in both parents and PCE children. Potential genetic differences in emotional regulation present in adults who use substances, including serotonin transporter differences linked to emotional regulation,38 may be passed on to children. Genetic contributions should be considered in future studies.
A strength of this study is the longitudinal sample and approach. All participants have been followed since birth, and exposure status was documented. Early‐life trauma was examined once participants reached adulthood and alexithymia and emotional regulation were examined later, strengthening the conclusions drawn from our moderated mediation model, although a fully longitudinal approach to our model would have collected alexithymia data before emotional- regulation data. While we focused upon significant correlations and used somewhat conservative criteria to construct our mediation models in order to avoid potential false positives, an additional limitation is potential intercorrelations between our alexithymia, regulation, and trauma measures, which allows for the potential for suppression effects that may affect results. The strong theoretical basis of our investigation, which is that alexithymia may contribute to poorer ability to reappraise emotions one has difficulties identifying, may lessen the impact of these limitations. Other limitations include the somewhat small sample, which is a result of following a specific population over a long period and attrition that accompanies the longitudinal design. Future studies with larger longitudinal samples should investigate the relationships between trauma, alexithymia, and regulation, and thus may be able to draw firmer conclusions. Our small sample size is alleviated somewhat by the use of boostrapping in our models, which provides a relatively more powerful way to estimate confidence intervals based on resampling.
In sum, our data suggest that childhood trauma is associated with poorer emotion-regulation strategies, specifically emotional reappraisal, in young adults. Further, the effects of emotional neglect and abuse specifically are mediated by alexithymia in individuals with PCE. Our data suggest that individuals with PCE may be especially vulnerable to early-life trauma and more likely to use alexithymic coping styles and potentially avoidant emotion-processing strategies. Future work should examine parent-child interactions in substance-using mothers and emotional responding in PCE individuals to further investigate these potential vulnerabilities. In addition, future work could investigate if emotional reappraisal in this population is associated with increased risk of mental illness or substance misuse.
Acknowledgments
KPM receives support from K01DA042937. MNP receives support from the Connecticut Council on Problem Gambling, and the Connecticut Department of Mental Health and Addiction Services. Beyond funding, the funding agencies had no further role in the writing of the report or in the decision to submit the paper for publication.
Footnotes
Declaration of Interest
Dr Potenza has consulted for and advised Opiant Therapeutics, AXA, Game Day Data and the Addiction Policy Forum; received research support (to Yale) from the Mohegan Sun Casino and the National Center for Responsible Gaming; participated in surveys, mailings, or telephone consultations related to drug addiction, impulse control disorders or other health topics; consulted for and/or advised legal and gambling entities on issues related to impulse control and addiction; provided clinical care in the Connecticut Department of Mental Health and Addiction Services Problem Gambling Services Program; performed grant reviews for the National Institutes of Health and other agencies; has guest-edited journal sections; given academic lectures in grand rounds, CME events and other clinical/scientific venues; and generated books or chapters for publishers of mental health texts. The other authors report no conflict of interest with respect to the content of this manuscript.
REFERENCES
- 1.Min MO, Minnes S, Kim JY, et al. Association of prenatal cocaine exposure, childhood maltreatment, and responses to stress in adolescence. Drug Alcohol Depend. 2017;177:93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85:348–362. [DOI] [PubMed] [Google Scholar]
- 3.Swart M, Kortekaas R, Aleman A. Dealing with feelings: characterization of trait alexithymia on emotion regulation strategies and cognitive-emotional processing. PLoS One. 2009;4:e5751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morie KP, Jackson S, Zhai ZW, et al. Mood disorders in high- functioning autism: the importance of alexithymia and emotional regulation. J Autism Dev Disord. 2019;49:2935–2945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gilbert R, Widom CS, Browne K, et al. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. [DOI] [PubMed] [Google Scholar]
- 6.Bernstein DP, Ahluvalia T, Pogge D, et al. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry. 1997;36:340–348. [DOI] [PubMed] [Google Scholar]
- 7.Bernet CZ, Stein MB. Relationship of childhood maltreatment to the onset and course of major depression in adulthood. Depress Anxiety. 1999;9:169–174. [PubMed] [Google Scholar]
- 8.Khoury L, Tang YL, Bradley B, et al. Substance use, childhood traumatic experience, and posttraumatic stress disorder in an urban civilian population. Depress Anxiety. 2010;27:1077–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marusak HA, Martin KR, Etkin A, et al. Childhood trauma exposure disrupts the automatic regulation of emotional processing. Neuropsychopharmacology. 2015;40:1250–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heleniak C, Jenness JL, Stoep AV, et al. Childhood maltreatment exposure and disruptions in emotion regulation: a transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cognit Ther Res. 2016;40:394–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldin PR, McRae K, Ramel W, et al. The neural bases of emotion regulation: reappraisal and suppression of negative emotion. Biol Psychiatry. 2008;63:577–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cutuli D Cognitive reappraisal and expressive suppression strategies role in the emotion regulation: an overview on their modulatory effects and neural correlates. Front Syst Neurosci. 2014;8:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carvalho Fernando S, Beblo T, Schlosser N, et al. The impact of self- reported childhood trauma on emotion regulation in borderline personality disorder and major depression. J Trauma Dissociation. 2014;15:384–401. [DOI] [PubMed] [Google Scholar]
- 14.Taylor GJ. Alexithymia: concept, measurement, and implications for treatment. Am J Psychiatry. 1984;141:725–732. [DOI] [PubMed] [Google Scholar]
- 15.Taylor GJ, Bagbry RM, Parker JD. Disorders of Affect Regulation: Alexithymia in Medical and Psychiatric Illness. Cambridge: Cambridge University Press; 1997. [Google Scholar]
- 16.Frewen PA, Pain C, Dozois DJ, et al. Alexithymia in PTSD: psychometric and FMRI studies. Ann N Y Acad Sci. 2006;1071:397–400. [DOI] [PubMed] [Google Scholar]
- 17.Aust S, Hartwig EA, Heuser I, et al. The role of early emotional neglect in alexithymia. Psychol Trauma Theory Res Pract Pol. 2013;5:225–232. [Google Scholar]
- 18.Salovey P, Mayer JD. Emotional intelligence. Imagin Cogn Pers. 1990;9:185–211. [Google Scholar]
- 19.Parolin M, Simonelli A, Mapelli D, et al. Parental substance abuse as an early traumatic event. Preliminary findings on neuropsychological and personality functioning in young drug addicts exposed to drugs early. Front Psychol. 2016;7:887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yip SW, Lacadie CM, Sinha R, et al. Prenatal cocaine exposure, illicit- substance use and stress and craving processes during adolescence. Drug Alcohol Depend. 2016;158:76–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morie KP, Wu J, Landi N, et al. Feedback processing in adolescents with prenatal cocaine exposure: an electrophysiological investigation. Dev Neuropsychol. 2018;43:183–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mayes LC, Molfese DL, Key AP, et al. Event-related potentials in cocaine-exposed children during a Stroop task. Neurotoxicol Teratol. 2005;27:797–813. [DOI] [PubMed] [Google Scholar]
- 23.Bridgett DJ, Mayes LC. Development of inhibitory control among prenatally cocaine exposed and non-cocaine exposed youths from late childhood to early adolescence: the effects of gender and risk and subsequent aggressive behavior. Neurotoxicol Teratol. 2011;33:47–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–190. [DOI] [PubMed] [Google Scholar]
- 25.Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto Alexithymia Scale—I. Item selection and cross-validation of the factor structure. J Psychosom Res. 1994;38:23–32. [DOI] [PubMed] [Google Scholar]
- 26.IBM Corp. IBM SPSS Statistics for Windows, Version 24. Armonk, NY: IBM Corp; 2016. [Google Scholar]
- 27.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: The Guilford Press; 2013. [Google Scholar]
- 28.Hayes AF, Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behav Res Methods. 2009;41:924–936. [DOI] [PubMed] [Google Scholar]
- 29.Bennett D, Bendersky M, Lewis M. Preadolescent health risk behavior as a function of prenatal cocaine exposure and gender. J Dev Behav Pediatr. 2007;28:467–472. [DOI] [PubMed] [Google Scholar]
- 30.Venta A, Hart J, Sharp C. The relation between experiential avoidance, alexithymia and emotion regulation in inpatient adolescents. Clin Child Psychol Psychiatry. 2013;18:398–410. [DOI] [PubMed] [Google Scholar]
- 31.Chaplin TM, Freiburger MB, Mayes LC, et al. Prenatal cocaine exposure, gender, and adolescent stress response: a prospective longitudinal study. Neurotoxicol Teratol. 2010;32:595–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laloyaux J, Fantini C, Lemaire M, et al. Evidence of contrasting patterns for suppression and reappraisal emotion regulation strategies in alexithymia. J Nerv Ment Dis. 2015;203:709–717. [DOI] [PubMed] [Google Scholar]
- 33.Bendersky M, Lewis M. Arousal modulation in cocaine-exposed infants. Dev Psychol. 1998;34:555–564. [PMC free article] [PubMed] [Google Scholar]
- 34.Mayes LC, Grillon C, Granger R, et al. Regulation of arousal and attention in preschool children exposed to cocaine prenatally. Ann N Y Acad Sci. 1998;846:126–143. [PubMed] [Google Scholar]
- 35.Eiden RD, Schuetze P, Colder CR, et al. Maternal cocaine use and mother-toddler aggression. Neurotoxicol Teratol. 2011;33:360–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Espinosa M, Beckwith L, Howard J, et al. Maternal psychopathology and attachment in toddlers of heavy cocaine-using mothers. Infant Ment Health J. 2001;22:316–333. [Google Scholar]
- 37.Borelli JL, West JL, Decoste C, et al. Emotionally avoidant language in the parenting interviews of substance-dependent mothers: associations with reflective functioning, recent substance use, and parenting behavior. Infant Ment Health J. 2012;33:506–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hariri AR, Mattay VS, Tessitore A, et al. Serotonin transporter genetic variation and the response of the human amygdala. Science. 2002;297:400–403. [DOI] [PubMed] [Google Scholar]


